Validating Monte Carlo Models with Experimental Tissue Data: A Comprehensive Guide for Biomedical Researchers
This article provides a comprehensive framework for the validation of Monte Carlo (MC) models against experimental tissue data, a critical step for ensuring reliability in biomedical research and drug development.
Validating Monte Carlo Models with Experimental Tissue Data: A Comprehensive Guide for Biomedical Researchers
Abstract
This article provides a comprehensive framework for the validation of Monte Carlo (MC) models against experimental tissue data, a critical step for ensuring reliability in biomedical research and drug development. It covers the foundational principles of MC simulation in radiation transport and tissue interaction, explores methodological applications across therapy, imaging, and dosimetry, addresses common troubleshooting and optimization challenges, and establishes robust protocols for quantitative validation and comparative analysis. Aimed at researchers and scientists, this guide synthesizes current best practices to enhance model accuracy, foster reproducibility, and accelerate the translation of computational findings into clinical applications.
The Bedrock of Accuracy: Core Principles of Monte Carlo Simulation and Tissue Equivalency
Monte Carlo (MC) simulations have become the computational gold standard in biomedical physics and engineering, providing unparalleled accuracy in modeling the stochastic nature of radiation and light transport within biological tissues [1]. Their role is critical in advancing medical imaging, radiation therapy treatment planning, and the development of new diagnostic techniques. However, the transformative potential of these methods hinges on their rigorous validation with experimental tissue data, ensuring that virtual models faithfully represent complex clinical realities. This guide compares leading Monte Carlo simulation platforms and methodologies, focusing on their performance in experimentally validated biomedical research contexts.
At its core, the Monte Carlo method is a computational technique that uses repeated random sampling to solve complex deterministic or stochastic problems [1]. In biomedical physics, it tracks the trajectories of individual particles—such as photons, electrons, or protons—as they travel through and interact with virtual models of human anatomy or medical devices.
A significant challenge in MC simulations is the high computational cost required to achieve statistically meaningful, low-noise results [2] [3]. This has driven the development of advanced acceleration strategies, which fall into two primary categories:
- Algorithmic & Hardware Acceleration: This includes scaling and perturbation methods that reduce the number of required simulations [2], and the use of Graphics Processing Unit (GPU) parallel computing. GPU-based MC platforms can achieve speedups of 100 to 1000 times over traditional Central Processing Unit (CPU) implementations, making large-scale simulations clinically feasible [4] [3].
- Artificial Intelligence (AI) Integration: Deep learning models are now being used as surrogate models to predict MC dose distributions in seconds, and to denoise results from shorter simulation runs [5] [1]. AI also leverages MC-simulated synthetic data for training, creating a powerful synergistic relationship [1].
Comparative Analysis of Monte Carlo Simulation Platforms
The following tables provide a detailed comparison of general-purpose and specialized MC simulation packages, highlighting their key characteristics and performance in experimentally validated scenarios.
Table 1: Comparison of General-Purpose Monte Carlo Simulation Platforms
| Platform/Toolkit | Primary Applications in Biomedicine | Key Features & Strengths | Documented Experimental Validation & Performance |
|---|---|---|---|
| GEANT4 [6] [3] | Proton therapy [3], brachytherapy dosimetry [3], general particle transport | Models complex geometries [3]; extensive physics models for particle interactions [3]. | Used as the engine for GATE, which is validated in dosimetry studies (e.g., 3D-printed phantom simulations) [6]. |
| GATE [6] [1] | PET, SPECT, CT simulation [1], radiation therapy [1] | User-friendly interface for GEANT4 [1]; simulates time-dependent processes (e.g., organ motion) [3]. | Validated for dosimetric accuracy in radionuclide therapy; showed PLA phantom dose difference of +1.7% to +5.6% in liver [6]. |
| EGSnrc [3] | External beam radiotherapy dosimetry [3] | High accuracy in electron and photon transport [3]; widely validated for clinical dosimetry [3]. | Considered a benchmark for dose calculation accuracy; however, can be computationally expensive [3]. |
| MCNP [3] | Radiation shielding, neutron therapy [3] | General-purpose code for neutron, photon, and electron transport [3]. | Applied in various diagnostic and therapeutic contexts [3]. |
| FLUKA [3] | Heavy ion therapy [3] | Robust nuclear interaction models [3]. | Valued for modeling nuclear interactions in therapeutic applications [3]. |
| TOPAS [3] | Proton therapy [3], adaptive treatment planning [3] | Customized for medical physics on top of GEANT4; high efficiency and ease of use [3]. | Popular in proton therapy research and planning [3]. |
Table 2: Performance of Specialized and Accelerated Monte Carlo Methods
| Method / Platform | Specific Application | Key Performance Metrics | Validation against Experiment/Independent MC |
|---|---|---|---|
| Scaling Method for Fluorescence [2] | Fluorescence spectroscopy in multi-layered skin tissue | Achieved 46-fold improvement in computational time [2]. | Mean absolute percentage error within 3% compared to independent MC simulations [2]. |
| GPU Acceleration [4] | General tomography (CT, PET, SPECT) | Speedups often exceeding 100–1000 times over CPU implementations [4]. | Provides essential support for developing new imaging systems with high accuracy [4]. |
| Deep Learning (CHD U-Net) [5] | Predicting MC dose in heavy ion therapy | Gamma Passing Rate up to 99% (3%/3mm criterion); prediction in seconds [5]. | Improved Gamma Passing Rate by 16% (1%/1mm) vs. traditional TPS algorithms [5]. |
| MCX-ExEm Framework [7] | Fluorescence in 3D-printed phantoms | Captured nonlinear quenching, depth-dependent attenuation accurately [7]. | Strong agreement across parameters; minor deviations in low-scattering/absorption regimes [7]. |
Experimental Validation Protocols
Validating MC simulations against controlled experimental data is crucial for establishing their credibility in biomedical research. The following are detailed methodologies from key studies.
Validation of Fluorescence Simulations with Solid Phantoms
This study aimed to validate a GPU-accelerated, voxel-based fluorescence MC framework for applications like fluorescence-guided surgery [7].
- Objective: To experimentally validate the MCX-ExEm framework's ability to model fluorescence under varying fluorophore concentrations, optical properties, and complex 3D geometries [7].
- Materials:
- Procedure:
- The optical properties (absorption, scattering) and fluorophore concentrations of the phantoms were precisely characterized [7].
- Experimental fluorescence measurements were obtained by imaging the phantoms [7].
- Simulations were run using the MCX-ExEm framework with the same parameters [7].
- The simulated and experimental fluorescence intensities were compared across all tested parameters, including quenching at high concentrations and depth-dependent effects [7].
- Outcome: The study demonstrated strong agreement between simulations and experiments, establishing a foundation for "fluorescence digital twins." Minor deviations occurred primarily where optical characterization was most challenging (e.g., low-scattering regimes) [7].
Dosimetric Validation Using 3D-Printed Phantoms
This research evaluated the dosimetric accuracy of 3D-printed materials (PLA and ABS) compared to real tissues in radionuclide therapy using MC simulations [6].
- Objective: To determine if 3D-printed PLA and ABS phantoms can accurately mimic real tissues for pre-treatment dosimetry in radioembolization [6].
- Materials:
- Procedure:
- The geometry was simulated with materials defined as PLA, ABS, and real organ densities (liver: ~1.06 g/cm³, lung: ~0.26-0.35 g/cm³) [6].
- An activity of 1 mCi of Tc-99m or Y-90 was placed in the tumor mimic [6].
- A DoseActor recorded the energy deposition (dose) in the liver and lung volumes [6].
- The dose distributions for PLA and ABS were compared to the dose in real organ densities to calculate percentage differences [6].
- Outcome: For Y-90, PLA showed a +1.7% dose difference in the liver, indicating it is highly suitable for representing high-density tissues. ABS showed large differences in the lungs (-34% to -35%), making it less suitable for very low-density tissues [6].
Validation of a Scaling Method for Fluorescence Spectroscopy
This work introduced a scaling method to accelerate MC simulations of fluorescence in multi-layered tissues with oblique illumination, a previously unsolved challenge [2].
- Objective: To develop and validate an efficient scaling MC algorithm for fluorescence simulation in multi-layered tissue models with oblique probe geometries [2].
- Materials:
- Procedure:
- Baseline Simulations: A single set of photon histories was generated at excitation and emission wavelengths for a baseline tissue model [2].
- Scaling: For a new set of optical properties, the recorded photon histories were scaled using multi-layered scaling relations, rather than running entirely new simulations [2].
- Comparison: The detected fluorescence intensity from the scaling method was compared against the results from independent, traditional MC simulations [2].
- Outcome: The scaling method achieved a 46-fold improvement in computational time while maintaining a mean absolute percentage error within 3%, demonstrating high accuracy and efficiency [2].
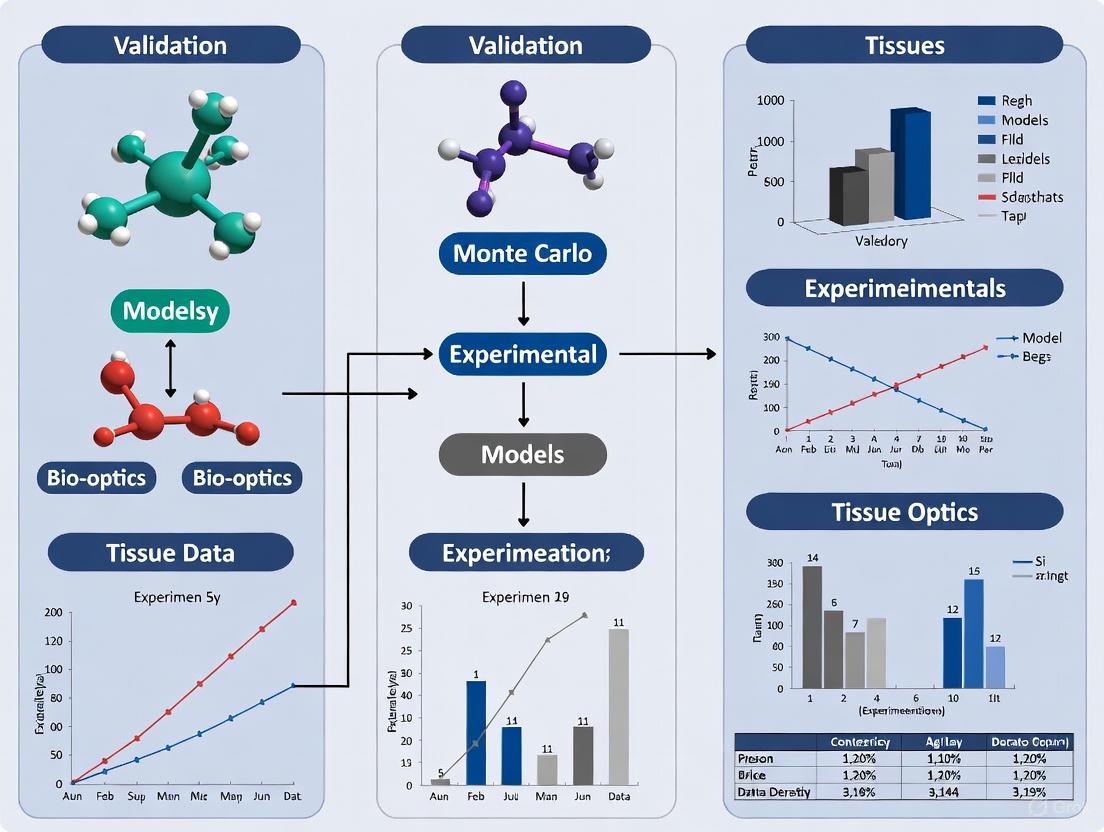
Research Workflow and Platform Selection
The following diagram illustrates a generalized workflow for conducting and validating a Monte Carlo study in biomedical physics, integrating the key concepts of acceleration and validation.
The Scientist's Toolkit
This table details essential materials, software, and reagents used in the featured experiments for MC simulation and validation.
Table 3: Essential Research Reagents and Materials for MC Validation
| Item | Function / Purpose | Example Use Case in Validation |
|---|---|---|
| 3D-Printed Phantoms (PLA, ABS) [6] [7] | Serve as physical models with known geometry and material properties to mimic human tissues and validate simulations. | Dosimetric validation in radionuclide therapy [6]; creating complex 3D geometries for fluorescence validation [7]. |
| Well-Characterized Optical Properties (μₐ, μₛ) [7] | Define the absorption and scattering coefficients of phantoms or tissues; critical input parameters for MC simulations. | Used as input for fluorescence MC simulations and to compare against experimental results [7]. |
| Radionuclides (Tc-99m, Y-90, Lu-177) [6] [8] | Act as radiation sources for simulating and validating internal dosimetry in diagnostic and therapeutic applications. | Simulating dose distribution from a tumor in radioembolization [6] [8]. |
| GATE/GEANT4 MC Platform [6] [3] [1] | A widely adopted software toolkit for simulating radiation transport in medical imaging and therapy. | Dosimetry studies in nuclear medicine [6]; simulating PET and SPECT systems [1]. |
| GPU Computing Cluster [4] | Provides massive parallel processing power to accelerate MC simulations, reducing computation time from days to hours or minutes. | Enabling practical, large-scale MC applications in tomography that are not feasible with CPU-based codes [4]. |
| DoseActor (in GATE) [6] | A sensitive detector component in MC simulations that records energy deposition (dose) in a defined 3D volume (voxels). | Calculating dose distributions in specific organs like liver and lungs from a simulated radionuclide source [6]. |
The Critical Role of Tissue-Equivalent Materials and Phantoms in Validation
In the field of medical physics and radiation research, the validation of computational models against reliable experimental data is a critical step in ensuring their accuracy and clinical applicability. This process relies heavily on the use of tissue-equivalent materials and anthropomorphic phantoms, which serve as standardized, reproducible, and ethically uncomplicated substitutes for human tissues. These tools are indispensable for bridging the gap between theoretical Monte Carlo simulations and real-world clinical applications, particularly in advanced radiotherapy techniques like proton therapy [9] [10] [11]. Without them, confident translation of novel techniques from the laboratory to the clinic would be severely hampered. This guide objectively compares the performance of various tissue-equivalent materials and the experimental protocols used to validate sophisticated Monte Carlo models, providing researchers with a clear framework for their critical work.
Performance Comparison of Tissue-Equivalent Materials
The efficacy of a phantom is fundamentally determined by the radiological properties of its constituent materials. Researchers have developed and characterized a wide array of materials to simulate biological tissues.
Table 1: Performance of Tissue-Equivalent Materials for Mouse Model Phantoms
| Tissue Type | Optimal Material Formulation | Measured Density (g/cm³) | CT Number (HU) | Key Properties |
|---|---|---|---|---|
| Lung | Polyurethane-Resin (1:1.3) [12] | 0.53 | -856.4 ± 46.2 | Low density, low effective atomic number (Zeff). |
| Soft Tissue | Resin-Hardener (1:1) [12] | 1.06 | 65.3 ± 8.4 | Matches electron density and attenuation of soft tissue. |
| Bone | Resin with 30% Hydroxyapatite [12] | 1.42 | 797.7 ± 69.2 | High density and Zeff due to calcium content. |
For ultrasound imaging, material requirements shift from radiological to acoustic properties. A systematic analysis identified that water-based materials most closely align with the needs of ultrasound phantoms, with Polyvinyl Alcohol (PVA) being a standout material for its ability to match the acoustic properties of various human tissues [13].
Table 2: Tissue-Mimicking Materials for Ultrasound Phantoms
| Material Category | Example Materials | Acoustic Properties | Best For |
|---|---|---|---|
| Water-Based | Agar, Gelatine, PVA, Polyacrylamide (PAA) [13] | Speed of Sound: 1425-1956 m/s [13] | General ultrasound; PVA matches many human tissues best. |
| Oil-Based | Paraffin gel, SEBS copolymers [13] | Speed of Sound: ~1425-1502 m/s [13] | Specialized applications requiring specific elastic properties. |
| Oil-in-Hydrogel | Agar/Gelatine with Safflower Oil [13] | Attenuation Coefficient: 0.1-0.59 dB/MHz/cm [13] | Creating heterogeneous tissue models. |
Experimental Validation of Monte Carlo Models: Protocols and Data
The true test of a Monte Carlo model lies in its validation against controlled physical experiments. The following case studies illustrate this critical process.
Protocol 1: Proton Range Verification with a Dual-Head PET System
- Objective: To validate a GATE Monte Carlo model for verifying proton beam range using an in-beam dual-head PET (DHPET) system by comparing simulated data against experimental measurements [9].
- Experimental Setup: A phantom (either HDPE or gel-water) was irradiated with monoenergetic proton beams. The resulting positron-emitting isotopes were detected by the DHPET system to determine the activity range and compare it to the proton's physical range [9].
- Monte Carlo Models Compared: The study evaluated three different nuclear models for predicting β+ isotope production:
- GEANT4 QGSP_BIC: A theoretical built-in hadronic physics model.
- EXFOR-based: Utilizes tabulated experimental cross-section data.
- NDS (Rodríguez-González et al.): An updated, optimized cross-section dataset [9].
- Performance Comparison:
- Dose Distribution: All models showed excellent agreement with the clinical treatment planning system (RayStation), with mean range deviations within ±0.2 mm [9].
- Activity Range Prediction: In a gel-water phantom, which more closely mimics human tissue, the NDS model demonstrated superior accuracy, closely matching the experimental data. The QGSP_BIC model underestimated the distal range by 2-4 mm, while the EXFOR model showed a slight overestimation [9].
This workflow from simulation to experimental validation is summarized below.
(caption: Workflow for Monte Carlo model validation in proton therapy)
Protocol 2: Prompt Gamma-Ray Spectroscopy for Proton Therapy
- Objective: To develop and validate Monte Carlo codes (GEANT4, MCNP6, FLUKA) for Prompt Gamma-Ray Spectroscopy (PGS), a real-time method for monitoring proton beam range [10].
- Experimental Setup: A PMMA (polymethyl methacrylate) block phantom was irradiated with protons of energies from 90 to 130 MeV. The resulting prompt gamma-rays were detected using a CeBr3 scintillator detector to obtain reference PGS spectra [10].
- Monte Carlo Models Compared: The study compared the performance of three major Monte Carlo codes in reproducing the experimental gamma-ray spectra.
- Performance Comparison:
- GEANT4 was the only code capable of successfully reproducing most prominent prompt gamma lines [10].
- FLUKA aligned better with experimental data for mid-range energies but overestimated the 4.44 MeV gamma line at higher energies [10].
- MCNP6 provided the closest match for the 4.44 MeV line at higher energies [10].
- All codes failed to accurately reproduce the 6.13 MeV oxygen de-excitation line, highlighting a universal limitation in existing nuclear data tables and underscoring the need for continued experimental research [10].
Essential Research Reagents and Materials
A well-equipped laboratory for phantom development and model validation requires a suite of specialized materials and instruments.
Table 3: Research Reagent Solutions for Phantom Fabrication and Validation
| Category | Item | Function & Application |
|---|---|---|
| Base Materials | Polyurethane, Epoxy Resin, Hydroxyapatite, Montmorillonite Nanoclay [12] | Primary components for constructing tissue-equivalent phantoms with tunable densities. |
| 3D Printing Mat. | Acrylonitrile Butadiene Styrene (ABS), VeroClear, Rigur, Accura Bluestone [12] | Used in additive manufacturing to create anatomically accurate phantom geometries. |
| Attenuators/Scatterers | Titanium Dioxide (TiO2), Aluminum Oxide (Al2O3), Graphite, Glass Microspheres [13] | Added to base materials to fine-tune acoustic and radiological properties like attenuation. |
| Standard Phantoms | Polymethylmethacrylate (PMMA) Blocks [10], ATOM Anthropomorphic Phantom [14] | Commercially available phantoms for system calibration and out-of-field dose measurement. |
| Detection Systems | Dual-Head PET [9], CeBr3 Scintillator [10], Thermoluminescent Dosimeters (TLDs) [14] | Instruments for capturing experimental data on radiation dose and isotope production. |
The critical role of tissue-equivalent materials and phantoms in validation is unequivocal. Quantitative comparisons reveal that no single material or Monte Carlo model is universally superior; the optimal choice is highly dependent on the specific application, whether it's simulating lung tissue for a small animal model or validating a nuclear physics model for proton range verification. The consistent finding across studies is that validation against controlled, well-characterized phantoms is non-negotiable. It is the only process that can identify subtle but critical discrepancies in computational models, thereby ensuring their reliability and ultimately safeguarding the quality and safety of future clinical applications. As Monte Carlo techniques and therapeutic technologies continue to evolve, so too must the sophistication and accuracy of the phantoms used to validate them.
Within the field of medical physics and radiation dosimetry, the accurate validation of Monte Carlo (MC) models relies on precise data concerning the radiological properties of both biological tissues and substitute materials. These properties—linear attenuation coefficients, stopping power, and interaction cross-sections—dictate how radiation travels through and deposits energy in matter. This guide provides a comparative analysis of these key properties across real tissues and commonly used tissue-equivalent materials, framing the data within the essential context of experimental validation for MC simulations. The convergence of experimental phantom studies and computational modeling forms the foundational thesis of modern, accurate radiological science.
Comparative Analysis of Radiological Properties
The performance of tissue-equivalent materials is quantified by how closely their radiological properties match those of real human tissues. Deviations in these properties can lead to significant inaccuracies in MC simulations, which in turn affect medical imaging quality and radiotherapy dose calculations.
Linear Attenuation Coefficients
The linear attenuation coefficient (μ) describes how easily a material can be penetrated by a beam of radiation, such as X-rays or gamma rays. A higher value indicates the material is more effective at attenuating the radiation.
The following table compares the mass attenuation properties of various tissue-equivalent materials against their target biological tissues [15] [16].
Table 1: Comparison of Mass Attenuation Coefficients and Effective Atomic Numbers
| Material Category | Specific Material / Tissue | Density (g/cm³) | Effective Z (Zₑff) | Deviation in Mass Attenuation Coefficient |
|---|---|---|---|---|
| Bone Equivalent | ICRU Cranial Bone (Standard) | - | - | Reference |
| Epoxy Resin + 30% CaCO₃ | 1.65 | 11.02 | +17.4% (at 40 keV) to +1.2% (at 150 keV) [15] | |
| Teflon (for Cortical Bone) | - | - | Absorbed ~50% less than masseter muscle at 50 keV [16] | |
| Soft Tissue Equivalent | ICRU Brain (Standard) | - | - | Reference |
| Epoxy Resin + 5% Acetone | - | 6.19 | +13.7% to +5.5% [15] | |
| PMMA (for Skin, Glands) | - | - | Generally absorbed less X-rays than real tissues [16] | |
| Water Equivalent | Water (Standard) | 1.00 | ~7.4 | Reference |
| Epoxy Resin-based CSF | - | - | +3.4% to +1.1% [15] |
Stopping Power and Dose Deposition
Stopping power quantifies the rate of energy loss by a charged particle (e.g., an electron or proton) as it travels through a material. In radiotherapy dosimetry, this is directly related to the absorbed dose.
The table below summarizes the performance of common 3D-printing materials in mimicking human tissue for dosimetric studies [6].
Table 2: Dosimetric Accuracy of 3D-Printed Phantom Materials in Radionuclide Therapy
| Material | Density (g/cm³) | Radionuclide | Tissue Organ | Dose Difference (%) |
|---|---|---|---|---|
| PLA (Polylactic Acid) | 1.24 [6] | Tc-99m | Liver | +5.6% [6] |
| Y-90 | Liver | +1.7% [6] | ||
| ABS (Acrylonitrile Butadiene Styrene) | 1.04 [6] | Tc-99m | Lungs | -35.3% to -40.9% [6] |
| Y-90 | Lungs | -34.2% to -34.9% [6] |
Experimental Protocols for Validation
The validation of MC models requires rigorous, well-documented experimental methodologies. The following sections detail protocols from key studies comparing tissue equivalents.
Monte Carlo Simulation for Dosimetric Accuracy
This protocol is adapted from a study investigating the tissue equivalence of 3D-printed PLA and ABS phantoms for radionuclide therapy [6].
Objective: To evaluate the dosimetric accuracy of PLA and ABS phantoms by comparing dose distributions to those in real tissues using MC simulations.
Workflow Overview:
Key Materials and Setup:
- Software: GATE/GEANT4 MC simulation package (v8.1) [6].
- Phantom Geometry: A cubic water phantom (700 x 700 x 700 mm³) containing liver (220 x 140 x 80 mm) and lung mimics, with a 10 mm spherical tumor in the liver [6].
- Materials: Real tissues, PLA (density 1.24 g/cm³), and ABS (density 1.04 g/cm³) were defined in the material database [6].
- Radiation Sources: Tc-99m (1 mCi) for imaging and Y-90 (1 mCi) for therapy simulations [6].
- Dosimetry: Dose was scored using a
DoseActorsegmented into 3D voxels (dosels). The dose distribution along anatomical planes was calculated and compared using C++ analysis code [6].
X-Ray Absorption in Tissue-Equivalent Polymers
This protocol outlines a method for validating tissue-equivalent materials using X-ray absorption studies, based on a study of mandibular tissues [16].
Objective: To compare the X-ray absorption of real mandibular tissues and their tissue-equivalent polymeric materials across a diagnostic energy range.
Workflow Overview:
Key Materials and Setup:
- Software: PHITS (Particle and Heavy Ion Transport code System) MC simulation program [16].
- Phantom Geometry: A detailed mandibular model with anatomical layers (skin, gland, muscle, bone). The thicknesses of real tissues and equivalent materials were carefully matched [16].
- Materials:
- Radiation Source: X-ray photons with energies from 50 to 100 keV in 5 keV increments, simulating a panoramic dental X-ray setup [16].
The Scientist's Toolkit
This section catalogs essential reagents, materials, and software used in the featured experiments, providing a quick reference for researchers designing similar validation studies.
Table 3: Essential Research Reagents and Materials for Radiological Validation
| Item Name | Function / Application | Specific Examples from Research |
|---|---|---|
| PLA (Polylactic Acid) | 3D-printing material for phantoms simulating high-density tissues [6]. | Represents liver tissue; shows +1.7% to +5.6% dose difference [6]. |
| ABS (Acrylonitrile Butadiene Styrene) | 3D-printing material for phantoms simulating low-density tissues [6]. | Represents lung tissue; shows ~ -35% dose difference [6]. |
| Epoxy Resin Composites | Customizable tissue substitute for various tissue types [15]. | Mimics cranial bone, brain, CSF, and eye lens with low deviation from ICRU standards [15]. |
| PMMA (Polymethyl Methacrylate) | Common tissue-equivalent polymer for soft tissue and dosimetry phantoms [16]. | Used to simulate skin, parotid gland, and other soft tissues in mandibular model [16]. |
| Teflon (Polytetrafluoroethylene) | Polymer used as a bone-equivalent material due to its higher atomic number [16]. | Simulates cortical bone in mandibular X-ray absorption studies [16]. |
| GATE/GEANT4 | Monte Carlo simulation platform for modeling particle transport in matter [6]. | Used to simulate radiation transport and dose deposition in radionuclide therapy [6]. |
| PHITS | General-purpose Monte Carlo code for simulating particle and heavy ion transport [16]. | Used to model X-ray absorption in a complex mandibular geometry [16]. |
| DoseActor | A sensitive detector within MC codes that records energy deposition in a defined volume [6]. | Used to voxelize geometry and score radiation dose for comparison [6]. |
Monte Carlo particle transport codes are indispensable tools in research and drug development, enabling high-fidelity simulations of radiation interactions with matter. Validating these simulations against experimental data, particularly with biological tissues and tissue substitutes, is a critical step for ensuring their reliability in preclinical and clinical applications. This guide provides an objective comparison of five major Monte Carlo codes—GEANT4, GATE, MCNP, PHITS, and PENELOPE—focusing on their performance and experimental validation.
Monte Carlo (MC) codes simulate the stochastic nature of radiation transport, providing insights into dose deposition, particle fluence, and nuclear interactions that are often difficult to measure directly. For research involving tissue data, the accuracy of these simulations is paramount. Validation typically involves comparing simulation results against benchmark measurements from well-characterized experimental setups, such as tissue-substitute phantoms, to quantify discrepancies in parameters like dose distribution, activity yield, or particle range.
The codes discussed here—GEANT4, GATE (which is built upon GEANT4), MCNP, PHITS, and PENELOPE (integrated into GEANT4 as a physics model)—represent some of the most widely used tools in the scientific community. Their performance varies significantly depending on the application, chosen physics models, and the specific experimental benchmarks used for comparison [17].
Comparative Performance Tables
The following tables summarize key characteristics and performance data of the major Monte Carlo codes, based on recent experimental validations.
Table 1: Overview of Major Monte Carlo Codes
| Code | Primary Developer | Notable Features | Common Applications in Research |
|---|---|---|---|
| GEANT4 | Geant4 Collaboration (CERN) | Extensive physics models, active development, open-source [18] | Hadron therapy, space science, high-energy physics [19] |
| GATE | OpenGATE Collaboration | GEANT4-based, dedicated to medical imaging and radiotherapy | PET range verification, dosimetry, scanner design [9] |
| MCNP6 | Los Alamos National Laboratory | Legacy code, trusted for neutron & photon transport | Shielding design, dosimetry, criticality safety [20] [21] |
| PHITS | JAEA, RIST | Capable of simulating heavy ion transport | Particle therapy, accelerator design, radiation protection [22] [23] |
| PENELOPE | University of Barcelona | Precise low-energy electron & photon transport | Dosimetry, microdosimetry, X-ray spectroscopy [17] |
Table 2: Experimental Validation in Proton Therapy Scenarios
| Application / Code | Key Performance Metric | Experimental Benchmark & Result |
|---|---|---|
| Prompt Gamma (PGS) for Range Verification [20] | ||
| GEANT4 | Accuracy in reproducing PG peaks | Successfully reproduced key de-excitation lines (e.g., 4.44 MeV from Carbon-12) [20] |
| MCNP6 | Accuracy in reproducing PG peaks | Failed to reproduce key de-excitation lines [20] |
| FLUKA | Accuracy in reproducing PG peaks | Failed to reproduce key de-excitation lines [20] |
| In-Beam PET for Range Verification [9] | ||
| GATE (QGSP_BIC model) | Activity range prediction in gel-water phantom | Underestimated distal activity range by 2–4 mm [9] |
| GATE (NDS cross-sections) | Activity range prediction in gel-water phantom | Best match with experimental data; mean deviation < 1 mm [9] |
| β+-emitter Production for PET [23] | ||
| PHITS | Yield of positron-emitting nuclides | Generally underestimates yields compared to experimental data [23] |
| GEANT4 | Yield of positron-emitting nuclides | Good agreement with experimental data for carbon and proton beams [23] |
Table 3: Performance in Photon Shielding and Attenuation
| Code | Scenario | Comparison with Experiment |
|---|---|---|
| GEANT4 | Mass Attenuation Coefficient (PE/HgO composite) | Excellent agreement (e.g., 0.0843 cm²/g vs. experimental 0.0843 ± 0.002 cm²/g) [21] |
| MCNP6 | Mass Attenuation Coefficient (PE/HgO composite) | Excellent agreement (e.g., 0.0833 cm²/g vs. experimental 0.0843 ± 0.002 cm²/g) [21] |
| PHITS | Linear Attenuation Coefficient (Tissue substitutes) | High correlation with experimental data; discrepancies < 5% for most energies [22] |
Detailed Experimental Protocols and Validation
Validation in Proton Therapy: Prompt Gamma Spectroscopy
Objective: To validate GEANT4, MCNP6, and FLUKA for simulating proton-induced prompt gamma-ray (PG) spectra, a method for real-time range verification in proton therapy [20].
- Experimental Setup: A 130 MeV proton beam was directed onto a target. The resulting PG spectra were measured using a 15.0 cm³ CeBr₃ detector placed at 90 degrees relative to the beam axis.
- Simulation Protocol: The simulations aimed to reproduce the PG spectra from the target. Various proton data libraries, physics models, and cross-section values were employed within each code.
- Key Findings: GEANT4 was the only code capable of successfully reproducing characteristic prompt gamma-ray peaks from key elements like Carbon-12 (4.44 MeV) and Oxygen-16 (6.13 MeV). This study highlighted the critical need for updated data tables in MC simulations for nuclear physics applications in medicine [20].
Validation in Proton Therapy: In-Beam PET
Objective: To develop and validate a GATE/GEANT4 model for proton range verification using a clinical dual-head PET (DHPET) system [9].
- Experimental Setup: In-beam PET data were acquired during proton irradiation of homogeneous (HDPE) and heterogeneous (gel-water) phantoms at Kaohsiung Chang Gung Memorial Hospital, Taiwan.
- Simulation Protocol: The entire process was simulated in GATE, including beam delivery, production of β+ isotopes (e.g., ¹¹C, ¹⁵O), and PET detection. Different nuclear models and cross-section datasets (QGSP_BIC, NDS, EXFOR) were evaluated.
- Key Findings: The choice of nuclear model significantly impacted accuracy. While the built-in QGSP_BIC model underestimated the distal activity range by 2–4 mm, using the external NDS (Nuclear Data Sheets) cross-section library resulted in the best agreement with experiments, with mean range deviations within 1 mm [9].
Validation for Photon Attenuation in Tissue Substitutes
Objective: To model and validate a system for measuring the linear attenuation coefficients (μ) of tissue substitute materials using the PHITS code [22].
- Experimental Setup: Ballistic gel tissue substitute samples were placed between a Ra-226 source and a NaI(Tl) detector. The detector was shielded with lead, and the source was collimated.
- Simulation Protocol: The experimental apparatus was precisely modeled in PHITS. The code simulated the transport of photons at specific energies (186.1–2204.1 keV) from the source through the samples to the detector.
- Key Findings: PHITS simulations showed a high correlation with experimental data, with discrepancies below 5% for most energies. When compared to theoretical NIST data, the differences were below 1%, demonstrating PHITS's high accuracy for modeling photon interactions in tissue-like materials [22].
The Scientist's Toolkit: Key Reagents and Materials
The following materials are essential for experimental validation of Monte Carlo simulations in a biomedical context.
Table 4: Essential Materials for Experimental Validation
| Material / Solution | Function in Validation |
|---|---|
| Tissue-Substitute Phantoms (e.g., ballistic gel, HDPE) | Mimics the radiation interaction properties of human tissue for controlled, reproducible benchmark measurements [9] [22]. |
| Cerium Bromide (CeBr₃) Scintillator | A radiation detector with good energy resolution, used for spectroscopy of prompt gamma rays [20]. |
| Sodium Iodide (NaI(Tl)) Scintillation Detector | A widely used detector for measuring gamma-ray flux and energy spectra in attenuation experiments [21] [22]. |
| Radioactive Sources (e.g., ¹³⁷Cs, ²²⁶Ra) | Provide known and stable gamma-ray emissions (e.g., 662 keV from ¹³⁷Cs) for calibrating detectors and validating simulations [21] [22]. |
| Bismuth Germanate (BGO) Detector Modules | Used in the detector blocks of positron emission tomography (PET) systems for in-beam range verification [9]. |
| Validated Cross-Section Libraries (e.g., NDS, EXFOR) | External datasets for nuclear reaction probabilities, often providing higher accuracy than default theoretical models in MC codes [9]. |
Workflow Diagram for Code Validation
The diagram below outlines the standard workflow for validating a Monte Carlo model against experimental data, a process critical for ensuring simulation reliability.
Model Validation Workflow
The comparative data indicates that no single Monte Carlo code is universally superior; performance is highly dependent on the specific application.
- GEANT4 and GATE demonstrate strong performance in medical physics, particularly for complex problems like prompt gamma simulation and PET verification. Their open-source nature and active development allow for continuous improvement and integration of more accurate physics models and cross-section data [20] [9] [18].
- MCNP6 remains a robust and reliable code for traditional applications such as photon shielding, showing excellent agreement with experimental attenuation measurements [21].
- PHITS is a capable tool for photon transport and heavy ion applications, though its performance in predicting certain nuclear fragmentation products (e.g., β+ emitters) may require further model development to match the accuracy of GEANT4 in some therapeutic scenarios [22] [23].
- Model Selection is Critical: The significant difference in results observed when using different physics models (e.g., QGSP_BIC vs. NDS cross-sections in GATE) underscores that the user's choice of physics settings is as important as the choice of the code itself [9]. Validation against experimental data is the only way to build confidence in a particular simulation setup.
For researchers validating models with experimental tissue data, the key is to select a code whose strengths align with the project's physical processes and to employ a rigorous, iterative validation workflow using well-characterized phantoms and detectors.
The fidelity of computational models to experimental reality forms the bedrock of scientific reliability in fields ranging from radiation therapy to drug development. Validation metrics serve as the crucial, quantitative bridge between simulation and experiment, providing the objective evidence needed to trust model predictions in critical applications. This guide systematically compares the performance of various validation approaches and metrics, with a particular focus on Monte Carlo (MC) simulation frameworks validated against experimental tissue data.
As computational models grow more complex, moving beyond simple point-to-point comparisons to multi-dimensional validation has become essential. Different applications demand specialized metrics sensitive to specific types of discrepancies, whether assessing radiation dose distributions for cancer treatment, verifying proton beam ranges in therapy, or quantifying drug responses in pharmaceutical screening. This comparative analysis examines the experimental protocols, performance characteristics, and appropriate applications of leading validation methodologies, providing researchers with the data needed to select optimal validation strategies for their specific domain.
Comparative Analysis of Validation Metrics and Methods
The table below summarizes key validation metrics across different domains, highlighting their applications, acceptance criteria, and performance characteristics based on recent experimental studies.
Table 1: Comprehensive Comparison of Validation Metrics and Methods
| Application Domain | Primary Metric(s) | Typical Acceptance Criteria | Performance & Limitations | Experimental Data Source |
|---|---|---|---|---|
| IOERT/IMRT/VMAT Dose Validation | Gamma analysis (dose difference + DTA) [24] [25] | 2%/1 mm to 3%/3 mm; >90-95% passing rate [24] [25] | 3%/3 mm may miss clinically relevant errors; 2%/1 mm more sensitive [25] | Water phantom measurements; diode/ion chamber arrays [24] [26] |
| Proton Range Verification | Activity range deviation; Distal fall-off alignment [9] | Mean range deviation <1 mm ideal; 2-4 mm may require model adjustment [9] | Highly dependent on nuclear cross-section data; NDS/EXFOR models show best accuracy [9] | Dual-head PET system; β+ emitter detection [9] |
| Radiation Shielding Evaluation | Linear/Mass Attenuation Coefficient; HVL/TVL [27] | Discrepancy <5% between simulation and experiment [27] | MCNP6 and GEANT4 show good agreement (<5%) with experimental measurements [27] | Cs-137 source (662 keV); PMMA-HgO composites [27] |
| Drug Response Quantification | Normalized Drug Response (NDR) [28] | Improved consistency (p<0.005) vs. PI and GR metrics [28] | Accounts for background noise and growth rates; wider spectrum of drug effects [28] | Cell viability assays (luminescence) [28] |
| 3D Dose Volume Validation | Dose-Volume Histogram (DVH) metrics [26] | PTV D95 difference <2% in error-free plans [26] | Sensitivity varies with plan complexity; may miss errors in simple plans [26] | ArcCHECK measurements with 3DVH software [26] |
Experimental Protocols for Validation Studies
Monte Carlo Model Validation for Radiation Therapy Systems
Recent research on IOERT accelerator validation exemplifies rigorous MC model testing. The LIAC HWL mobile accelerator model was implemented using PENELOPE/penEasy code with a hypothetical head geometry due to manufacturer disclosure limitations. The validation protocol involved comparing simulated and measured Output Factors (OFs), Percentage Depth Doses (PDDs), and Off-Axis Ratios (OARs) in a virtual water phantom for various applicator sizes (3-10 cm diameter), bevel angles (0°-45°), and energies (6, 8, 10, 12 MeV). Gamma analysis criteria of 2% dose difference and 1 mm distance-to-agreement were applied, with results showing >93% passing rates in most cases. The worst performance occurred with the smallest applicator (3 cm diameter) with 45° bevel angle at 6 MeV, where passing rates dropped to 85.7-86.1% [24].
Proton Range Verification via PET Detection
A comprehensive validation study for proton range verification utilized a dual-head PET (DHPET) system mounted on a rotating gantry in the treatment room. Researchers compared three nuclear models: the built-in GEANT4 QGSPBIC model, EXFOR-based cross-sections, and the updated NDS dataset. The experimental protocol involved irradiating high-density polyethylene (HDPE) and gel-water phantoms with monoenergetic proton beams (70-210 MeV), followed by PET imaging to detect positron-emitting isotopes (¹¹C, ¹⁵O) generated during irradiation. The distal fall-off of the activity distribution was compared to the dose fall-off from treatment planning system calculations. Results showed that NDS and EXFOR models achieved mean range deviations within 1 mm in HDPE phantoms, while QGSPBIC underestimated the distal range by 2-4 mm [9].
Advanced Validation Beyond Conventional Gamma Analysis
Studies have revealed limitations in conventional gamma analysis for IMRT/VMAT commissioning. When applying the typical 3%/3 mm criteria with global normalization, passing rates often exceeded 99% for per-beam analysis and 93.9-100% for composite plans - well above TG-119 action levels of 90% and 88%, respectively. However, more sensitive analysis using 2%/2 mm local normalization and advanced diagnostics like EPID-based measurements and dose profile examination uncovered systematic errors that caused target dose coverage loss up to 5.5% and local dose deviations up to 31.5%. These errors included TPS model limitations, algorithm inaccuracies, and QA phantom modeling issues [25].
Essential Research Tools and Reagents
Table 2: Key Research Reagent Solutions for Validation Experiments
| Tool/Reagent | Primary Function | Application Examples | Technical Notes |
|---|---|---|---|
| ArcCHECK with 3DVH Software | 3D dose measurement & reconstruction in patient geometry [26] | VMAT plan validation; DVH metric estimation [26] | Uses Planned Dose Perturbation (PDP) algorithm; requires complementary ion chamber measurement [26] |
| PENELOPE/penEasy MC Code | Electron and photon transport simulation [24] | IOERT accelerator modeling; dose distribution calculation [24] | Provides PSFs in IAEA format; supports hypothetical geometries when exact specs unavailable [24] |
| GATE Simulation Platform | GEANT4-based MC simulation for medical applications [9] | Proton therapy range verification; PET detector simulation [9] | Simulates entire chain from beam delivery to image reconstruction [9] |
| MCNP6 & GEANT4 Codes | General-purpose radiation transport simulation [27] | Shielding material evaluation; attenuation coefficient calculation [27] | MCNP6 highly accurate with established nuclear data; GEANT4 offers flexibility [27] |
| PMMA-HgO Composites | Novel shielding material for experimental validation [27] | Gamma shielding performance; composite material modeling [27] | HgO filler increases linear attenuation from 0.044 cm⁻¹ (pure PMMA) to 0.096 cm⁻¹ [27] |
| RealTime-Glo Assay | Cell viability measurement for drug screening [28] | NDR metric calculation; high-throughput drug profiling [28] | Luminescence-based; requires positive and negative controls for normalization [28] |
Visualizing Validation Workflows
Diagram 1: Model Validation Workflow. This diagram illustrates the comprehensive process for validating computational models against experimental data, highlighting the parallel paths of experimental measurement and simulation development that converge at the metric comparison stage.
Diagram 2: Validation Metric Taxonomy. This diagram categorizes the primary validation metrics used across different applications, showing how they specialize for particular validation scenarios while sharing the common goal of quantifying agreement between simulation and experiment.
Effective validation requires carefully selected metrics that are sensitive to the specific types of errors most likely to occur in a given application. While gamma analysis with 2%/1-2 mm criteria provides robust validation for photon and electron dose distributions, proton range verification demands specialized PET-based activity distribution comparison with attention to nuclear cross-section data. For 3D dose validation, DVH-based metrics offer clinical relevance but require understanding of their sensitivity limitations in different plan complexities.
The most successful validation approaches combine multiple complementary metrics rather than relying on a single test. As computational models continue to evolve toward more complex biological systems and real-time applications, validation methodologies must similarly advance with tighter tolerances, more diligent diagnostics, and multidimensional assessment strategies. The experimental data and comparative analysis presented here provide researchers with evidence-based guidance for selecting validation approaches that will ensure model reliability across medical physics and pharmaceutical development applications.
From Theory to Practice: Methodologies and Cutting-Edge Applications in Therapy and Imaging
Calibrating In-Vivo Monitoring Systems and Internal Dosimetry Phantoms
The validation of computational models with robust experimental data is a cornerstone of reliable internal dosimetry and in vivo monitoring. Within this framework, physical phantoms that mimic human anatomy and optical properties are indispensable for benchmarking and refining Monte Carlo (MC) simulations, which are a primary tool for modeling complex radiation and light transport phenomena [29] [30]. This guide objectively compares different calibration methodologies and phantom-based validation approaches, providing a structured overview of their performance, experimental protocols, and key applications. The focus is on providing researchers with comparative data to select appropriate techniques for validating their MC models, ultimately enhancing the accuracy of in vivo dose and physiological measurements.
Comparative Analysis of Phantom-Based Validation Methodologies
The table below summarizes the core characteristics, performance data, and applications of several phantom-based validation approaches identified in the literature.
Table 1: Comparison of Phantom-Based Validation Methodologies for Monte Carlo Models
| Methodology / System | Key Performance Metrics / Outcomes | Reported Limitations / Challenges | Primary Application Context |
|---|---|---|---|
| Tissue Phantom + MC Model for Ocular Oximetry [29] | Assessed impact of confounding factors (scattering, blood volume); quantified choroidal circulation effect on accuracy. | Complex layered structure of eye fundus difficult to replicate with phantoms; no gold-standard for validation. | Validation of diffuse reflectance-based ocular oximetry techniques. |
| EURADOS MC Intercomparison (Skull Phantoms) [30] | Good agreement between simulated and measured spectra for task 2A/2B; ~33% of participants needed simulation revisions. | Human error in simulations (e.g., inaccurate detector modeling, scoring errors); some physical phantoms not representative. | Calibration of germanium detector systems for in vivo monitoring of Am-241 in the skull. |
| Monte Carlo-Based Inverse Model for Tissue Optics [31] | Extracted optical properties with average error of ≤3% (hemoglobin phantoms) and ≤12% (Nigrosin phantoms). | Performance varies with absorber type (higher error for Nigrosin). | Extraction of absorption and scattering properties of turbid media from diffuse reflectance. |
| Noncontact Depth-Sensitive Fluorescence Validation [32] | Experimentally verified MC model of cone/cone-shell illumination; model provides fast, inexpensive optimization platform. | Experimental optimization of parameters (e.g., axicon lenses) is time-consuming and costly. | Optimization of noncontact, depth-sensitive fluorescence probes for epithelial tissue diagnostics. |
| EPID In Vivo Monitoring System (SunCHECK PerFRACTION) [33] | Dose calculation deviations <1.0% in water-equivalent regions; detected output variations within 1.2%; agreed with TLD audit within 2-3.7%. | Higher deviations (~7.3%) in highly heterogeneous (e.g., lung) regions, though results were expected. | In vivo dose verification for radiotherapy using Electronic Portal Imaging Device (EPID). |
Detailed Experimental Protocols
This section elaborates on the experimental methodologies that generated the data in the comparison table.
Two-Step Phantom and MC Validation for Ocular Oximetry
This protocol uses a hybrid approach to validate an ocular oximetry technique, isolating the effects of specific confounding factors [29].
- Tissue Phantom Construction: Phantoms are designed to investigate specific variables, such as scattering properties, blood volume fraction (BVF), and the spectral transmission of the crystalline lens.
- Phantom Measurement: The diffuse reflectance spectrum of the phantom is acquired using the oximetry device. The raw signal is processed to isolate the reflectance from the phantom itself by accounting for device-specific optical reflections and ambient radiation [29].
- Multi-Wavelength Oxygen Saturation Algorithm: The optical density (OD) spectrum is calculated. A modified Beer-Lambert law model is fitted to the OD spectrum to determine the concentrations of oxy- and deoxy-hemoglobin, incorporating empirical terms for scattering, melanin, and the crystalline lens [29]. The oxygen saturation is calculated as the ratio of oxygenated hemoglobin to total hemoglobin.
- Monte Carlo Simulation of Layered Structure: A separate MC model of the light propagation in the multi-layered eye fundus is developed. This model is used to study the effect of the fundus layered-structure, which is difficult to replicate with physical phantoms, and to quantify the impact of factors like choroidal blood oxygen saturation.
International MC Intercomparison Exercise for Skull Phantoms
This protocol, organized by EURADOS, outlines a standardized method for validating MC codes used in in vivo monitoring of radionuclides [30].
- Phantom Selection: Multiple anthropomorphic head phantoms are used, including a voxelized version of a real human skull (BfS phantom) with known 241Am activity and a physical CSR phantom.
- Reference Measurements: Participants are provided with measurement data from these phantoms using defined germanium detectors.
- Computational Tasks:
- Task 1: Participants simulate a predefined detector and phantom setup using their MC codes to check their ability to reproduce reference results.
- Task 2: Participants build a model of their own real detector and compare its simulated response with actual measurements from the BfS and CSR phantoms.
- Task 3: Participants simulate the entire geometry of a typical in vivo measurement as performed in their laboratory.
- Result Comparison and Analysis: The organizers compare the detection efficiencies and spectra reported by all participants against the master reference measurements to identify discrepancies and common sources of error.
Validation of an EPID-Based In Vivo Dosimetry System
This protocol evaluates the performance of a commercial software for in vivo dose monitoring during radiotherapy [33].
- Error Detection Capability:
- Output Variation: LINAC output is intentionally altered, and the system's calculated dose on the EPID plane is compared to ionization chamber measurements.
- Phantom Thickness Variation: The thickness of a homogeneous phantom is reduced by 2 cm during irradiation. The system's calculated 3D dose in a CBCT scan is compared to ionization chamber measurements.
- Independent Audit Comparison: Four different phantoms are irradiated based on an external audit program's instructions. The dose deviations reported by the software based on EPID measurements are compared against the deviations reported by the audit using TLDs.
- End-to-End Test with Heterogeneous Phantom: A volumetric modulated arc therapy (VMAT) plan is delivered to a heterogeneous phantom. The software calculates the 3D dose on a CBCT using log files and EPID-measured MLC positions. The calculated dose at specific points is compared to ionization chamber measurements placed within the phantom.
Signaling Pathways and Workflow Visualizations
The following diagrams illustrate the logical workflows for key validation methodologies described in this guide.
Ocular Oximetry Validation Workflow
MC Model & Phantom Validation Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below lists key materials and their functions as derived from the experimental protocols cited in this guide.
Table 2: Key Research Reagents and Materials for Phantom-Based Validation
| Item / Reagent | Function in Experimental Context | Example from Literature |
|---|---|---|
| Anatomical Phantoms | Physical models with known geometry and composition used as a substitute for human tissue to provide a ground truth for measurements and simulations. | BfS skull phantom (donor skull with known 241Am activity); two-layered tissue phantoms mimicking skin/eye fundus [30] [32]. |
| Hemoglobin Derivatives | Act as absorbers in liquid phantoms to simulate the spectral properties of blood for oximetry calibration. | Used in liquid phantoms with polystyrene spheres as scatterers to validate a Monte Carlo-based inverse model [31]. |
| Polystyrene Spheres | Common scattering agents in liquid phantoms used to simulate the light scattering properties of biological tissues. | Employed in tissue phantoms to provide a controlled reduced scattering coefficient [31]. |
| Electronic Portal Imaging Device (EPID) | A detector mounted on a linear accelerator used for transmission dosimetry and in vivo verification of radiation dose during radiotherapy. | Central component of the SunCHECK PerFRACTION system for performing 2D and 3D dose calculations during treatment [33]. |
| Germanium Detector | High-resolution radiation detector for measuring low-energy photons, essential for quantifying radionuclides like Am-241. | Used by participants in the EURADOS intercomparison for measuring spectra from skull phantoms [30]. |
| Ionization Chamber | A reference-grade instrument for absolute dose measurement in radiology, used to benchmark other dosimetry systems. | Used as a reference to measure introduced dose variations in EPID system tests [33]. |
| Axicon Lenses | Optical components that create a ring-shaped "cone shell" illumination, used to enhance depth sensitivity in non-contact optical measurements. | Implemented in a non-contact probe to achieve depth-sensitive fluorescence measurements from layered phantoms [32]. |
Proton Therapy Range Verification Using In-Beam PET and Monte Carlo Simulations
The superior dose conformity of proton therapy, characterized by the Bragg peak, allows for highly localized energy deposition within a tumor target. However, this advantage is counterbalanced by sensitivity to range uncertainties, which can lead to under-dosage of the tumor or overexposure of adjacent healthy tissues [34] [35]. In-vivo range verification is therefore critical for ensuring treatment quality. This guide compares two prominent techniques for non-invasive range verification: Positron Emission Tomography (PET) and Prompt Gamma Imaging (PGI), with a specific focus on the integral role of Monte Carlo (MC) simulations in developing and validating these methods. The content is framed within the broader thesis that rigorous validation of MC models against experimental tissue data is a prerequisite for their reliable application in clinical range verification.
Comparative Analysis of Range Verification Methods
The following table summarizes the core characteristics, performance data, and technological requirements of the two primary range verification methods discussed in this guide.
Table 1: Comparison of Range Verification Methods in Proton Therapy
| Feature | In-Beam PET | Prompt Gamma Imaging (PGI) |
|---|---|---|
| Physical Principle | Detection of annihilation photons (511 keV) from (\beta^+) emitters (e.g., (^{11})C, (^{15})O, (^{13})N, (^{18})F) produced by nuclear fragmentation [34] [36]. | Detection of high-energy photons emitted instantaneously during nuclear de-excitation [37] [34]. |
| Temporal Relationship | Integration occurs post-irradiation (seconds to minutes); activity represents a cumulative history of the beam path [34] [38]. | Direct, real-time monitoring during beam delivery [37]. |
| Key Performance Metrics | - F-18 PET matches planned dose fall-off within 1 mm [36].- Activity-range can be measured within 1.0 mm within few beam spills [38]. | - >90% accuracy in identifying range shifts ≥2 mm with (10^8) protons [37].- Area under ROC curve of 0.9 for a +1 mm shift at (1.6\cdot10^8) protons [37]. |
| Advantages | - Can utilize both in-beam and offline imaging [38].- Well-established imaging technology and reconstruction algorithms.- F-18 offers superior correlation with dose due to low positron energy [36]. | - True real-time feedback potential.- Higher signal yield compared to positron emitters.- No radioactive decay wait time. |
| Disadvantages/Challenges | - Biological washout of emitters can blur the activity distribution [34].- Low activity concentrations (Bq/ml range) post-irradiation require sensitive detectors [36]. | - Complex detector design and shielding requirements.- Requires sophisticated spectroscopy and timing electronics.- The emitted spectrum is a linear sum of elemental constituents, requiring spectral unfolding [37]. |
| MC Simulation Codes Used | GATE, MCNPX [38] | Geant4 [37] |
| Primary Clinical Role | Dose verification and post-facto range assessment, enabling adaptive therapy [36] [38]. | Real-time beam range monitoring and control [37]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Materials for Range Verification Experiments
| Item Name | Function/Application in Research |
|---|---|
| GAMOS | A Monte Carlo code based on Geant4, validated for brachytherapy and capable of simulating dose deposition in various tissues, including bone and brain [39]. |
| Geant4 | A versatile Monte Carlo platform widely used in particle therapy to simulate particle transport and nuclear interactions for detector design and signal prediction [37] [34]. |
| GATE | A specialized Monte Carlo toolkit based on Geant4, designed for PET and SPECT simulations. It is used to simulate scanner performance and image formation [38]. |
| PHITS | A general-purpose Monte Carlo code for transporting various particle types; used for modeling radiation interactions and calculating parameters like linear attenuation coefficients in tissue substitutes [40]. |
| PENELOPE | A Monte Carlo code integrated with the penEasy framework, used for modeling linear accelerators and validating dose distributions in complex geometries [24]. |
| NOVCoDA (NOVO Compact Detector Array) | A compact detector array using bar-shaped organic scintillators and silicon photomultipliers (SiPMs) for simultaneous imaging of prompt gamma rays and fast neutrons [37]. |
| Ballistic Gel (BGel) | A tissue-equivalent material used to fabricate physical phantoms for experimental calibration of radiation detectors and validation of MC simulations [40]. |
| Solid Water | A commercially available tissue-substitute phantom material used for detector calibration and dosimetric measurements. MC simulations provide conversion factors to translate dose from Solid Water to actual human tissues [39]. |
| LYSO and BGO Crystals | Scintillator materials used in PET detectors. LYSO offers fast timing and high efficiency, while BGO is common in clinical scanners. Their performance is evaluated for detecting low activity concentrations in proton therapy [36]. |
Experimental Protocols for Key Studies
Protocol: In-Beam PET for Intra-Treatment Adaptive Proton Therapy
This protocol, based on the work by Lou et al. [38], outlines the methodology for rapid beam-range verification using MC simulations and PET imaging.
Phantom and Beam Irradiation Simulation:
- Tool: MCNPX Monte Carlo package.
- Action: Simulate the irradiation of a uniform cylindrical PMMA phantom with a collimated 180 MeV pristine proton beam.
- Output: A high-fidelity spatial distribution of positron emitters ((^{11})C, (^{15})O, (^{13})N) generated within the phantom.
PET System and Data Acquisition Simulation:
- Tool: GATE Monte Carlo toolkit.
- Action: Simulate two PET geometries—a dual-panel rotational PET and a stationary brain PET with Depth-of-Interaction (DOI) capability—to model the detection of coincidence events from the generated activity.
- Parameters: Vary the number of beam spills, total acquisition time (during- and post-irradiation), crystal cross-section size, and crystal length.
Image Reconstruction and Data Analysis:
- Tool: List-mode Maximum-Likelihood Expectation-Maximization (MLEM) algorithm.
- Action: Reconstruct images from the simulated coincidence data.
- Measurement: Quantify the "positron activity-range" from the reconstructed images as a function of the accumulated statistics (number of coincidence events). The convergence of this measured range towards its final value is tracked as data statistics increase.
Protocol: Prompt Gamma-Ray Spectroscopy with NOVCoDA
This protocol summarizes the methodology for using prompt gamma-ray spectra to detect proton beam range shifts [37].
Monte Carlo Simulation and Spectral Library Creation:
- Tool: Geant4.
- Action: Perform MC simulations to generate a library of elemental prompt gamma-ray spectra for various constituent elements in the target.
- Assumption: The total measured prompt gamma-ray spectrum is modeled as a linear sum of these individual elemental spectra (Monte Carlo Library Least Squares Approach).
Range Shift Classification:
- Action: Simulate various proton beam range shifts in a target.
- Tool: Apply a Quadratic Discriminant Analysis (QDA) classifier to the simulated prompt gamma-ray spectra.
- Output: The classifier identifies and quantifies the magnitude of any present range shifts (e.g., +1 mm, -1 mm, ±2 mm).
Performance Evaluation:
- Metrics: Determine the accuracy of range shift classification and calculate the Area Under the Receiver Operating Characteristic (ROC) curve.
- Parameters: Evaluate these metrics as a function of incident proton intensity (number of protons) to establish the minimum required statistics for reliable detection.
Workflow and System Diagrams
The following diagrams illustrate the logical workflows for range verification and Monte Carlo model validation.
In-Beam PET Verification Workflow
Monte Carlo Model Validation Logic
In-beam PET and prompt gamma imaging offer complementary pathways toward solving the critical challenge of range verification in proton therapy. PET provides a direct method for dose verification with high spatial accuracy, as evidenced by its ability to correlate F-18 activity with dose fall-off within 1 mm [36]. Prompt gamma imaging, with its real-time capability and high classification accuracy for range shifts greater than 2 mm, is a powerful tool for live monitoring [37]. The effective development and clinical translation of both technologies are fundamentally reliant on high-fidelity Monte Carlo simulations. As the field progresses, the continued validation of these MC models against experimental data from tissue substitutes and clinical phantoms remains the cornerstone for building the confidence required to reduce safety margins and fully exploit the physical advantages of proton therapy.
Deep Learning for Rapid Monte Carlo Dose Prediction in Heavy Ion Therapy
In heavy ion therapy (HIT), the precision of dose calculation is paramount for maximizing tumor control while sparing surrounding healthy tissues. The Monte Carlo (MC) method is considered the gold standard for dose calculation due to its accurate modeling of complex particle transport physics. However, its extensive computational requirements, often taking hours or even days to complete a single simulation, have historically limited its routine clinical application [5] [41]. To address this critical bottleneck, deep learning (DL) has emerged as a powerful tool for predicting MC-simulated dose distributions (MCDose) in seconds rather than hours. These DL models learn the complex mapping from patient inputs, such as computed tomography (CT) images, to high-fidelity 3D dose distributions, achieving accuracy comparable to full MC simulations while offering the speed necessary for online adaptive radiotherapy and rapid quality assurance [42]. This guide provides a comparative analysis of current deep learning architectures for rapid MCDose prediction, detailing their experimental protocols, performance data, and the essential research tools required for their development and validation.
Methodologies and Experimental Protocols
Deep Learning Model Architectures
Several specialized convolutional neural network architectures have been proposed for MCDose prediction in HIT.
CHD U-Net (Cascade Hierarchically Densely Connected U-Net): This model features a two-stage, cascaded 3D U-Net architecture that incorporates dense connections. The first stage network takes CT images and the treatment planning system analytical dose (TPSDose) as inputs to generate an initial MCDose prediction. The second-stage network then refines this prediction using the first stage's input and output. Key components include dense convolution modules, dense downsampling modules, and skip connections that combine downsampled and upsampled feature maps. This design improves gradient flow and feature propagation, enabling more accurate dose prediction, particularly in critical regions like the Planning Target Volume (PTV) [5] [41].
CAM-CHD U-Net: An enhancement of the CHD U-Net, this model integrates a Channel Attention Mechanism (CAM) into the original architecture. The CAM allows the network to adaptively weight the importance of different feature channels, focusing computational resources on the most informative features for dose prediction. This has been shown to improve performance in complex anatomical regions [42].
Comparative Models (C3D and HD U-Net): These are baseline architectures used for performance comparison. The C3D is a simpler 3D convolutional network, while the HD U-Net is a hierarchically dense U-Net without the cascade structure of the CHD U-Net [5] [41].
Data Acquisition and Preprocessing
The development and validation of these models typically involve the following standardized protocol.
- Patient Data: Models are trained and tested on retrospective clinical data, including CT images, structure sets (delineating organs at risk and target volumes), and corresponding TPSDose distributions. Cohort sizes are often in the range of 67 head-and-neck patients and 30 thorax-and-abdomen patients [41].
- Ground Truth MCDose: The reference MCDose is calculated using full Monte Carlo simulation platforms like GATE/Geant4. Simulations use the same beam parameters (spot positions, energies, weights) as the clinical treatment plan and track a high number of particles (e.g., 10^8) to ensure statistical noise is kept below 1% [41] [9].
- Data Preprocessing: Input data (CT and TPSDose) are converted into 3D matrices. CT Hounsfield Units (HU) are typically cropped and normalized to a [0, 1] range. Dose values are also normalized. To optimize GPU memory usage, data is often downsampled (e.g., to 256x256x64 resolution). Online data augmentation techniques, including random flipping, rotation, and panning, are applied during training to improve model generalization [41].
Model Training and Evaluation
- Training Configuration: Models are implemented in frameworks like PyTorch and trained on high-performance GPUs (e.g., NVIDIA A6000). The Mean Absolute Error (MAE) between the predicted dose and the ground truth MCDose is commonly used as the loss function. Optimization is performed with the Adam optimizer, often incorporating techniques like deep supervision to improve learning in intermediate layers [41].
- Performance Metrics: The primary metric for evaluation is the Gamma Passing Rate (GPR), which provides a composite measure of dose difference and distance-to-agreement. Standard criteria used include 3%/3mm (clinically relevant) and more stringent 1%/1mm. Evaluation is performed separately for the PTV region and the entire body to ensure accuracy in both the target and overall dose distribution [5] [41] [42].
Diagram 1: Workflow for Deep Learning-based MCDose Prediction. This illustrates the two-stage cascade architecture of the CHD U-Net model and its validation process.
Performance Data and Comparative Analysis
Quantitative Performance Comparison
The following tables summarize the key performance metrics of different deep learning models for MCDose prediction, enabling an objective comparison.
Table 1: Gamma Passing Rate (GPR) performance comparison of different deep learning models for head-and-neck and thorax-abdomen patients. Performance is shown for both the Planned Target Volume (PTV) and the entire body under the 3%/3mm criterion.
| Anatomical Region | Model | GPR in PTV (%) | GPR in Body (%) |
|---|---|---|---|
| Head-and-Neck | CHD U-Net | 97 | 98 |
| C3D | 97 | 98 | |
| HD U-Net | 85 | 97 | |
| Thorax-Abdomen | CHD U-Net | 71 | 95 |
| C3D | 71 | 95 | |
| HD U-Net | 51 | 90 | |
| Table 1 Source: [5] [41] |
Table 2: Performance of the advanced CAM-CHD U-Net model for head-and-neck cancer patients, demonstrating improved accuracy over the base CHD U-Net.
| Metric | CAM-CHD U-Net Performance |
|---|---|
| GPR in PTV (3%/3mm) | 99.31% |
| GPR in Body (3%/3mm) | 96.48% |
| Reduction in Mean Absolute Difference (D5) | 46.15% |
| Calculation Time | A few seconds |
| Table 2 Source: [42] |
Table 3: Comparison of computational performance between traditional Monte Carlo simulation and the deep learning-based prediction approach.
| Method | Calculation Time | Hardware Requirements | Key Advantage |
|---|---|---|---|
| Full MC Simulation (GATE/Geant4) | Several minutes to hours | Two Intel Xeon Gold 6148 CPUs (80 parallel calculations) | Gold standard accuracy |
| DL Prediction (CHD U-Net) | A few seconds | Single NVIDIA A6000 GPU | Clinical feasibility & speed |
| Table 3 Source: [5] [41] |
Critical Analysis of Performance Data
The data reveals several key insights:
- Superior Performance of Advanced Architectures: The CHD U-Net consistently outperforms the simpler HD U-Net, particularly in the challenging thorax-abdomen region where anatomical heterogeneity is high. The 20% higher GPR in the PTV for this region underscores the importance of the cascade and dense connection architecture [5] [41].
- High Clinical Readiness: All advanced models (C3D, CHD U-Net, CAM-CHD U-Net) achieve GPRs exceeding 95% in the body for head-and-neck cases under the clinical 3%/3mm criterion. This indicates that the overall dose distribution is predicted with high accuracy. The CAM-CHD U-Net's >99% GPR in the PTV highlights a significant step towards clinical adoption [42].
- Anatomical Dependency: Performance is generally higher for head-and-neck patients compared to thorax-abdomen patients. This is likely due to greater tissue heterogeneity and organ motion in the thorax and abdomen, presenting a more complex prediction challenge [41].
This section catalogs the critical software, data, and hardware components required for developing and validating deep learning models for MCDose prediction.
Table 4: Key research reagents and solutions for deep learning-based Monte Carlo dose prediction.
| Tool Category | Specific Tool / Resource | Function and Application in Research |
|---|---|---|
| Monte Carlo Simulation Platform | GATE/Geant4 [41] [9] | Generates the ground truth MCDose for training and testing DL models; simulates particle transport and interactions. |
| Treatment Planning System (TPS) | matRad [41], RayStation [9] | Provides the analytical dose algorithm calculation (TPSDose) used as an input to the DL models. |
| Deep Learning Framework | PyTorch [41] | Provides the programming environment for building, training, and testing the 3D U-Net architectures. |
| Medical Imaging Data | Patient CT Images & Structure Sets [41] | Serves as the primary anatomical input for the DL model to learn the relationship between tissue density and dose deposition. |
| High-Performance Computing | NVIDIA GPU (e.g., A6000) [41] | Accelerates the training of large 3D convolutional networks, reducing computation time from days to hours. |
| Validation Metric | Gamma Passing Rate (GPR) [5] [41] [42] | The standard metric for quantitatively comparing predicted and ground truth dose distributions in clinical radiotherapy. |
Deep learning models, particularly advanced architectures like the CHD U-Net and CAM-CHD U-Net, have demonstrated remarkable feasibility for predicting Monte Carlo dose distributions in heavy ion therapy with high accuracy and sub-minute computational speeds. The experimental data confirms that these models can achieve gamma passing rates above 97% in many clinical scenarios, making them suitable for integration into clinical workflows for tasks such as online adaptive radiotherapy and rapid, independent quality assurance [5] [42]. The primary advantage lies in decoupling the accuracy of the Monte Carlo method from its prohibitive computational cost.
Future research in this field is directed towards several key areas:
- Improving Robustness in Heterogeneous Anatomies: Enhancing model performance in thorax and abdomen sites through more sophisticated architectures and training strategies remains a priority [41].
- Clinical Integration for Online Adaptation: The near-instantaneous prediction capability opens the door for real-time re-planning in online adaptive radiotherapy (OART), which is crucial for accounting for inter-fractional anatomical changes [42].
- Expansion to Other Modalities: While this guide focuses on heavy ion therapy, the underlying principles are being actively applied to proton therapy and other external beam radiotherapy modalities, promising widespread impact on radiation oncology [43].
GPU-Accelerated Monte Carlo for Real-Time Dosimetry in Interventional Radiology
In interventional radiology, the real-time estimation of patient radiation dose is a significant challenge. Conventional dosimetry methods, including thermoluminescent dosimeters (TLDs), struggle to provide comprehensive dose distribution data across extended organs like the skin, offering information only for specific points and with a time delay [44]. Monte Carlo (MC) simulations, which meticulously model the stochastic nature of particle transport, are considered the gold standard for radiation dose computation [4] [45] [46]. However, their widespread clinical adoption in interventional radiology has been hampered by extremely long computation times, often taking hours or days on central processing units (CPUs) [47] [44].
The emergence of graphics processing unit (GPU)-accelerated Monte Carlo codes has presented a paradigm shift, offering the potential for real-time or near-real-time dose assessment. By leveraging the massive parallel processing power of GPUs, these platforms can achieve speedups exceeding 100 to 1,000 times compared to traditional CPU-based MC codes [4]. This review objectively compares the performance of several GPU-accelerated MC platforms, validating their accuracy against established codes and experimental data, and examines their integration into the clinical workflow for interventional radiology.
Comparative Analysis of GPU-Accelerated Monte Carlo Platforms
The following table summarizes the key performance metrics of several GPU-accelerated Monte Carlo codes as validated in recent scientific literature.
Table 1: Performance Comparison of GPU-Accelerated Monte Carlo Platforms
| Platform Name | Primary Application Area | Benchmark Comparison | Reported Speedup | Accuracy/Validation Outcome |
|---|---|---|---|---|
| MC-GPU [44] | Interventional Radiology, CT | PENELOPE/penEasy | 14-18x faster (single GPU vs. 12 CPU cores) | Differences in mean organ doses < 1%; accurate skin dose mapping. |
| GPU-based code (unnamed) [48] | Internal Dosimetry (PET/CT) | GATE | Calculation time reduced to 0.1% of GATE time | Average organ dose difference of 0.651%; >90% of organ dose differences within 1%. |
| GARDEN [45] | External Beam Radiotherapy | GEANT4 | >2500x faster | Dose differences < 1%; gamma pass rates > 99.23% in clinical VMAT/IMRT plans. |
| Torch [46] | Radiopharmaceutical Therapy | OpenDose, OLINDA 2.0 | 2% uncertainty in 7-281 seconds on a laptop GPU | Organ S-values agreed within ±2% with reference standards. |
| ArcherQA-CK [49] | Radiotherapy (CyberKnife) | TPS-MC Algorithm | ~39x faster (1.66 min vs. 65.11 min) | High consistency with TPS-MC; identified errors in RayTracing algorithm in chest cases. |
Experimental Protocols for Validation
A critical component of integrating any new computational tool into a clinical or research setting is rigorous validation. The following section details the methodologies employed in key experiments to benchmark the accuracy of GPU-accelerated MC codes.
Validation Against Established Monte Carlo Codes
A foundational step in validating new GPU-based MC codes is a direct comparison against well-established, gold-standard CPU-based MC packages.
MC-GPU vs. PENELOPE/penEasy: In a study aligned with the MEDIRAD project, MC-GPU was validated for interventional radiology applications. Researchers simulated chest irradiation of the Duke anthropomorphic phantom using both MC-GPU and PENELOPE/penEasy. The mean doses across various tissues were calculated and compared, with results showing differences below 1%. This high degree of agreement demonstrates that MC-GPU faithfully replicates the physical interaction models of its well-validated predecessor [44].
Unnamed GPU code vs. GATE: For internal dosimetry in PET imaging, a GPU-based code utilizing the PENELOPE random hinge model was developed. Its performance was benchmarked against GATE, a widely adopted MC platform in nuclear medicine. The validation involved simulating the transport of 1E8 and 1E7 particles and comparing the resulting organ doses. The outcomes showed an average organ dose difference of 0.651%, with over 90% of organ dose differences falling within 1% of the GATE results, confirming its high accuracy [48].
Validation Against Experimental Measurements
Beyond software comparisons, validation against physical measurements is essential to ensure real-world accuracy.
MC-GPU vs. TLD Measurements: The reliability of MC-GPU was further tested by comparing its simulated doses against experimental measurements using TLDs. Measurements were conducted in two scenarios: a calibration laboratory setup and a realistic operating room environment. The comparisons were performed for various radiation qualities relevant to interventional radiology. The results showed that the doses calculated by MC-GPU agreed with the TLD measurements within the associated uncertainties, confirming its capability to accurately estimate patient dose in clinically realistic conditions [44].
Torch vs. Film Dosimetry: For radiopharmaceutical therapy, the Torch platform was validated in a physical experiment involving a custom-designed film phantom doped with Y-90. The dose distribution simulated by Torch was compared against both the measured film data and doses simulated by the EGSnrc MC code. The Torch-simulated doses agreed with both the measurements and the EGSnrc simulations to within 5% at each of the five depths measured in the phantom, demonstrating its accuracy for voxel-level dosimetry [46].
Research Reagents and Computational Tools
The following table catalogs the key software, hardware, and phantom tools that constitute the essential "research reagents" for this field.
Table 2: Essential Research Reagents for GPU-Accelerated Dosimetry Development
| Reagent / Tool Name | Type | Primary Function in Research |
|---|---|---|
| PENELOPE [48] [44] | Software (Physics Model) | Provides the underlying cross-sections and physics models for photon/electron transport in many GPU codes. |
| Geant4 [45] | Software (Physics Model) | A toolkit for simulating the passage of particles through matter; used as a benchmark for validation. |
| GATE [48] | Software (Monte Carlo Platform) | A widely used CPU-based MC platform in nuclear medicine, often serving as a reference standard. |
| Anthropomorphic Phantom [44] | Physical Phantom | Represents human anatomy for experimental dose measurements (e.g., with TLDs) to validate simulations. |
| GPU (NVIDIA series) [48] [46] | Hardware | Provides the massive parallel computational power necessary to achieve real-time simulation speeds. |
Workflow for Code Validation and Clinical Implementation
The process of validating and implementing a GPU-accelerated Monte Carlo code for clinical dosimetry follows a logical, multi-stage pathway. The diagram below illustrates this workflow, from initial development to final clinical application.
GPU-accelerated Monte Carlo simulations represent a transformative advancement for real-time dosimetry in interventional radiology. The experimental data conclusively demonstrates that these platforms, including MC-GPU, can achieve computational speedups of several orders of magnitude—reducing calculation times from hours to seconds or minutes—while maintaining an accuracy level within 1-2% of established gold-standard methods [48] [44] [45]. This breakthrough successfully balances the long-standing trade-off between dosimetric accuracy and computational efficiency.
The validation of these codes against both established Monte Carlo packages and direct experimental measurements provides a robust scientific foundation for their use in clinical research and practice. As these tools continue to evolve and integrate into clinical workflows, they hold the strong potential to fulfill the demand for automatic patient dose monitoring, enhance radiation protection, and ultimately improve the safety and efficacy of interventional radiological procedures.
Developing and Testing Novel Shielding Composites with Experimental and MC Validation
The advancement of radiation shielding materials is critically dependent on the development of reliable predictive models. As researchers seek alternatives to traditional materials like lead, the integration of experimental data with Monte Carlo (MC) simulation has emerged as a cornerstone of materials validation. This approach enables accurate prediction of shielding performance while reducing dependence on costly and time-consuming experimental iterations. The validation of MC models against experimental measurements provides a powerful framework for developing novel polymer composites with enhanced shielding capabilities, mechanical properties, and environmental safety profiles.
This comparative guide examines recently developed shielding composites with a focus on studies that have implemented robust experimental and MC validation methodologies. By analyzing the quantitative performance metrics and validation approaches across different material systems, this review provides researchers with critical insights for selecting appropriate material compositions and validation protocols for specific shielding applications.
Comparative Analysis of Novel Shielding Composites
Recent research has produced diverse polymer composites with varying filler materials, concentrations, and polymer matrices. The table below summarizes key developments and their validated performance metrics.
Table 1: Comparison of Novel Polymer-Based Shielding Composites
| Composite Material | Filler Content | Photon Energy | Key Shielding Parameters | Validation Methods | Reference |
|---|---|---|---|---|---|
| Polyester/HgO | 0-15 mol% HgO | 0.01-15 MeV (including 137Cs, 662 keV) | MAC: 0.0843 cm²/g (Hg5 sample at 662 keV); Density: 1.380-1.589 g/cm³ | Experimental, GEANT4, MCNP, Phy-X/PSD, XCOM | [21] |
| PMMA/HgO | 2.5-10 wt% HgO | 137Cs (662 keV) | LAC: 0.044→0.096 cm⁻¹; HVL: 15.47→7.19 cm; Zeff: 3.6→4.1 | Experimental, MCNP6, GEANT4 | [27] |
| LDPE/Bismuth Oxide | 25% Bi₂O₃ + 25% Cement | 60 keV | X-ray blockage: Up to 78%; Mean Free Path: 6-12× lower than pure LDPE | Experimental characterization | [50] |
| Polyaniline/Boron Composites | 1-5% BN | 137Cs (662 keV) | Improved neutron and gamma shielding | Theoretical, GEANT4, Experimental | [51] |
| Epoxy-based Brain Tissue Equivalents | 5% NaHCO₃ or 5% Acetone | 10-150 keV | Zeff: 6.19-6.47; Density: 1.18-1.25 g/cm³ | GATE MC simulations, XMuDat | [52] |
The quantitative data reveals several important trends. First, the incorporation of high-Z fillers consistently improves shielding performance across multiple polymer systems. For instance, both polyester/HgO and PMMA/HgO composites demonstrate enhanced attenuation capabilities with increasing filler content [21] [27]. Second, the validation methodologies show remarkable consistency in approach, with multiple studies employing dual MC codes (typically GEANT4 and MCNP) alongside experimental measurements to verify results [21] [27]. This multi-faceted validation approach provides greater confidence in the reported performance metrics.
Experimental and Simulation Protocols
Material Preparation and Characterization
The development of reliable shielding composites requires meticulous preparation and characterization protocols. For polyester/HgO composites, researchers prepared six samples with HgO content ranging from 0-15 mol% [21]. The process involved mixing polyester with a hardener (10% of PE amount), stirring until bubbles disappeared, then adding predetermined amounts of HgO powder. The composites were dried at room temperature for three days, with densities ranging from 1.380 to 1.589 g/cm³ [21]. Similarly, PMMA/HgO composites were synthesized by dissolving virgin PMMA resin in dichloromethane, filtering the solution, then adding HgO filler (2.5-10 wt%) and stirring for 20 minutes to ensure uniform dispersion [27].
Material characterization typically includes structural analysis using X-ray diffraction (XRD) to verify filler crystalline structure and scanning electron microscopy (SEM) to examine filler distribution within the polymer matrix. For PMMA/HgO composites, SEM micrographs confirmed uniform distribution of HgO particles with no significant agglomeration, while XRD patterns showed distinct crystalline phases of HgO within the amorphous polymer matrix [27]. These characterization steps are essential for correlating material structure with shielding performance.
Radiation Shielding Measurement Techniques
Experimental validation of shielding performance requires precise measurement setups. For polyester/HgO composites, researchers placed samples between a 137Cs source (662 keV, 20 mCi activity) and a NaI/Tl scintillation detector [21]. The source was protected by a Pb shield, with a Pb cubic collimator placed between the sample and detector. Similar configurations were used for PMMA/HgO composites, with measurements performed using a 137Cs source [27]. These standardized configurations ensure comparable results across different studies.
Key shielding parameters measured include:
- Linear attenuation coefficient (LAC): Measures how easily photons can penetrate a material
- Mass attenuation coefficient (MAC): Normalizes LAC to material density
- Half-value layer (HVL): Thickness required to reduce radiation intensity by half
- Tenth-value layer (TVL): Thickness required to reduce radiation intensity to one-tenth
- Mean free path (MFP): Average distance photons travel between interactions
- Effective atomic number (Zeff): Weighted average atomic number of a compound
Monte Carlo Simulation Methodologies
MC simulations provide theoretical validation of experimental results. Most studies employ multiple simulation tools to cross-verify results. For polyester/HgO composites, researchers used GEANT4-10.7 with G4EmPenelopePhysics and GammaNuclearPhysics physics lists to simulate photon interactions [21]. The "G4PSVolumeFlux" class was used to determine photons reaching the detector. Simultaneously, MCNP simulations were performed alongside calculations using online programs Phy-X/PSD and XCOM [21]. This multi-code approach enhances the reliability of simulation results.
For PMMA/HgO composites, researchers utilized both MCNP6 and GEANT4 [27]. MCNP6 is recognized for high accuracy in neutron and photon transport, typically within 5-10% of experimental results when using reliable nuclear data libraries. GEANT4 offers greater flexibility and detailed geometry handling, making it suitable for complex experimental setups [27]. Simulations typically run 1×10⁶ particles to maintain statistical errors below 2%, ensuring high-fidelity results [27].
Figure 1: The iterative process for validating shielding composites through experimental measurements and Monte Carlo simulations, demonstrating the closed-loop feedback for model refinement.
Performance Metrics and Comparative Analysis
The shielding effectiveness of novel composites is quantified through several key parameters. The table below provides a detailed comparison of these metrics across different material systems.
Table 2: Quantitative Shielding Performance Metrics for Polymer Composites
| Composite Type | Density (g/cm³) | LAC (cm⁻¹) | MAC (cm²/g) | HVL (cm) | Zeff | Discrepancy Between Exp & MC |
|---|---|---|---|---|---|---|
| Polyester/HgO (Hg5) | 1.589 | - | 0.0843 (at 662 keV) | - | - | <0.6% (for MAC) |
| PMMA/HgO (10 wt%) | - | 0.096 | - | 7.19 | 4.1 | <5% |
| Pure PMMA | - | 0.044 | - | 15.47 | 3.6 | - |
| LDPE + 15% Bi₂O₃ | - | - | - | - | - | - |
| Epoxy/5% NaHCO₃ | 1.25 | - | - | - | 6.47 | - |
The data demonstrates significant enhancement in shielding performance with high-Z filler incorporation. The PMMA/HgO composite with 10 wt% HgO shows more than double the attenuation capability (LAC increased from 0.044 to 0.096 cm⁻¹) compared to pure PMMA, with a corresponding 52% reduction in HVL (from 15.47 to 7.19 cm) [27]. This indicates that thinner sections of the composite can provide equivalent shielding compared to the pure polymer.
The exceptional agreement between experimental and simulation results (typically under 5% discrepancy) validates the use of MC tools for predictive shielding design [27]. This close alignment enables researchers to confidently use simulations for preliminary screening of potential composite formulations, reducing development time and costs.
The Researcher's Toolkit: Essential Materials and Methods
Successful development and validation of novel shielding composites requires specific research tools and methodologies. The following table summarizes key components of the experimental and computational toolkit.
Table 3: Essential Research Tools for Shielding Composite Development
| Tool Category | Specific Tools | Function in Research | Examples from Literature |
|---|---|---|---|
| Polymer Matrices | Polyester, PMMA, LDPE, Epoxy resin, Polyaniline | Base material providing structural integrity and processability | Polyester [21], PMMA [27], LDPE [50], Epoxy [52], Polyaniline [51] |
| High-Z Fillers | HgO, Bi₂O₃, BN, Cement with metal oxides | Enhance photon attenuation through photoelectric absorption | HgO [21] [27], Bi₂O₃ [50], BN [51] |
| Characterization Equipment | XRD, SEM, EDS, FTIR | Analyze structural properties, filler distribution, elemental composition | SEM/XRD [27], FTIR [51] |
| Radiation Sources | 137Cs (662 keV), X-ray systems | Experimental irradiation for shielding measurements | 137Cs [21] [27] [51] |
| Detection Systems | NaI/Tl scintillation detectors, Gamma cameras | Measure transmitted radiation through samples | NaI/Tl detector [21], Mediso AnyScan SCP [53] |
| Monte Carlo Codes | GEANT4, MCNP, GATE, PENELOPE | Simulate radiation transport and predict shielding performance | GEANT4/MCNP [21] [27], GATE [52] [53], PENELOPE [24] |
| Cross-Verification Tools | Phy-X/PSD, XCOM | Validate MC results using established databases | Phy-X/PSD, XCOM [21] |
Figure 2: Decision framework for selecting appropriate Monte Carlo codes based on research objectives and application requirements, highlighting the complementary strengths of different simulation tools.
The development of novel shielding composites has progressed significantly through the integrated application of experimental measurement and Monte Carlo validation. The consistent agreement between experimental results and MC simulations (typically under 5% discrepancy) across multiple studies [21] [27] demonstrates the maturity of these computational tools for predictive materials design. This validation framework enables researchers to confidently explore new material compositions with reduced experimental overhead.
Future developments in shielding composites will likely focus on multi-functional materials that provide protection against mixed radiation fields (gamma rays, neutrons, and charged particles) while offering additional advantages such as transparency, flexibility, or environmental sustainability. The continued refinement of MC models, coupled with advanced material characterization techniques, will accelerate the development of next-generation shielding solutions for medical, industrial, and space applications.
Hybrid Modeling Approaches for Complex Phenomena like Cherenkov Emission
In the study of complex physical phenomena such as Cherenkov emission, researchers often face a fundamental modeling challenge: purely physics-based models can be computationally prohibitive, while entirely data-driven approaches may lack physical plausibility and require impractical amounts of experimental data. Hybrid modeling emerges as a powerful methodology that combines first-principles physics with data-driven components, offering a balanced approach that leverages the strengths of both paradigms. This is particularly valuable in fields like medical physics and therapeutic agent development, where accurate simulation of particle interactions with biological tissues directly impacts treatment efficacy and safety.
Cherenkov radiation, the light emitted when charged particles travel through a dielectric medium at speeds exceeding the phase velocity of light in that medium, presents a quintessential example of such complexity. In radiation therapy, Cherenkov imaging provides valuable information for treatment plan verification, but the accurate modeling of this emission relative to dose distribution in highly modulated treatment plans remains challenging due to intricate light-tissue interactions that alter the emitted spectral signal [54]. Hybrid modeling approaches address this challenge by creating computationally efficient frameworks that maintain physical accuracy, enabling more effective translation between delivered radiation dose and observed Cherenkov signals in clinical settings.
Comparative Analysis of Hybrid Modeling Approaches
Hybrid modeling employs systematic design patterns that govern how first-principles (physics-based) models (denoted as 'P') and data-driven components (denoted as 'D') are integrated. These patterns provide reusable solutions to common modeling challenges across diverse application domains. The most relevant patterns for Cherenkov emission modeling include:
Delta Model: A foundational pattern where a first-principles model provides the baseline, and a data-driven component corrects for discrepancies or unmodeled phenomena [55]. This approach facilitates rapid prototyping, as modeling can begin with the physics-based component, with the data-driven element added incrementally as more data becomes available or higher precision is required.
Physics-Based Preprocessing: This pattern uses domain knowledge to transform input data before feeding it into a data-driven model [55]. By incorporating transformations derived from physical laws, this approach introduces valuable inductive biases, reduces data dimensionality, and enhances overall model efficiency and interpretability.
Composition Patterns: These govern the combination of base patterns into more complex hybrid models, allowing researchers to build sophisticated modeling frameworks tailored to specific challenges [56].
Hybrid Monte Carlo for Tissue Cherenkov Emission
A prominent example of hybrid modeling in practice is the 2-stage Monte Carlo approach developed for modeling Cherenkov emission in radiation therapy. This methodology leverages a traditional treatment planning system combined with an optical Monte Carlo simulation to create an efficient tool for modeling every beam control point in highly-modulated treatment plans [54] [57].
This hybrid approach demonstrates distinctive advantages over purely physics-based or completely data-driven alternatives. The model efficiently estimates Cherenkov emission for linear accelerator beams, showing clear trends of decreasing emission intensity with increasing beam energy and significant emission intensity variation with beam type. Experimental validation revealed that the largest change in observed intensity resulted from altering field size, with a 76% intensity decrease when moving from 20 cm down to 1 cm square fields. The model showed agreement with experimentally detected Cherenkov emission with an average percent difference of 6.2%, with the largest discrepancies occurring at the smallest beam sizes [54].
Table 1: Performance Comparison of Hybrid vs. Traditional Modeling Approaches
| Model Characteristic | Traditional Monte Carlo | Pure Data-Driven | Hybrid Approach |
|---|---|---|---|
| Computational efficiency | Low (complex/time-consuming) | Variable | High (enables full treatment plan modeling) |
| Physical plausibility | High | Low to medium | High (incorporates first principles) |
| Data requirements | Low | High | Medium |
| Validation against experimental phantom | Possible but computationally intensive | Dependent on training data scope | 6.2% average difference with experimental data |
| Adaptability to new treatment plans | Limited | Requires retraining | High (widely useable tool) |
Hybrid Modeling for Proton Range Verification
Another significant application of hybrid modeling in medical physics involves proton therapy range verification using positron emission tomography (PET). While not directly focused on Cherenkov emission, this application shares the fundamental challenge of accurately modeling particle interactions with biological tissues. Monte Carlo simulation remains the most reliable reference standard for PET-based range verification, though filtering approaches and deep learning methods offer superior computational efficiency [9].
These alternative approaches fundamentally rely on Monte Carlo-generated datasets for training and validation, creating a hybrid framework that combines rigorous physics-based simulation with efficient data-driven inference. Research has demonstrated that incorporating experimentally measured cross-sections into Monte Carlo simulations significantly improves accuracy in predicting activity distributions and subsequent range verification [9].
Table 2: Quantitative Performance of Nuclear Models in Proton Range Verification
| Nuclear Model | Mean Range Deviation (HDPE Phantom) | Mean Range Deviation (Gel-Water Phantom) | Activity Distribution Consistency |
|---|---|---|---|
| GEANT4 QGSP_BIC | 2-4 mm underestimation | 1-3 mm underestimation | Low |
| EXFOR-based | Within 1 mm | 1-2 mm underestimation | High |
| NDS | Within 1 mm | Within 1 mm | High |
Experimental Protocols and Methodologies
Two-Stage Monte Carlo for Cherenkov Emission
The hybrid 2-stage Monte Carlo approach for Cherenkov emission modeling follows a structured methodology that separates the radiation transport and optical emission simulations:
Beam Modeling Stage: The first stage leverages traditional treatment planning systems to simulate the radiation beam delivery through biological tissues, capturing the initial spatial distribution of charged particles that generate Cherenkov radiation.
Optical Simulation Stage: The second stage employs optical Monte Carlo simulation to model the propagation, scattering, and spectral alteration of Cherenkov light as it travels through tissue [54].
The emitted optical spectra are estimated for multiple clinical beam configurations, including 6, 10, and 15 MV photon beams, 6 MeV electron beams, various beam incidence angles in tissue, and square field sizes ranging from 1 cm to 20 cm. This comprehensive parameter space ensures the model's applicability across diverse clinical scenarios.
The model validation protocol involves comparison with measured Cherenkov emission from blood and intralipid optical phantoms, providing experimental verification of the simulation accuracy across different tissue-simulating materials [54].
Experimental Validation Framework for Ocular Oximetry
While focusing on a different application domain, the two-step validation method developed for ocular oximetry provides a valuable methodological framework applicable to Cherenkov emission studies. This approach combines tissue phantom models with Monte Carlo simulations to systematically assess the impact of multiple confounding factors [29].
The methodology includes:
Tissue Phantom Investigation: Using specially designed phantoms to study the impact of specific factors including scattering, blood volume fraction, and lens yellowing on the oximetry model.
Monte Carlo Simulation: Modeling light propagation in the layered structure of the eye fundus to understand how anatomical complexities affect measurements.
This combined approach allows researchers to quantify the impact of various physiological and instrumentation factors on measurement accuracy, providing a more comprehensive validation framework than either method alone [29].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of hybrid models for complex phenomena like Cherenkov emission requires specialized materials and computational tools. The following table summarizes key research reagent solutions employed in the featured experiments:
Table 3: Essential Research Reagents and Materials for Cherenkov Emission Studies
| Item | Function | Application Example |
|---|---|---|
| Blood and Intralipid Optical Phantom | Validates Cherenkov emission models by providing controlled experimental reference | Hybrid Monte Carlo model validation [54] |
| Graphene-hBN Hyperbolic Metamaterial | Enables on-chip Cherenkov radiation with low-energy electrons in terahertz range | Fundamental studies of Cherenkov emission mechanisms [58] |
| Liquid Argon (LAr) Detection Medium | Provides high scintillation light-yield environment for Cherenkov photon detection | Event-by-event identification of Cherenkov radiation [59] |
| GATE (Geant4 Application for Tomographic Emission) Simulation Platform | Monte Carlo framework for simulating particle interactions and detector responses | Proton range verification studies [9] |
| 22Na Calibration Source | Produces gamma-ray photons that Compton scatter to create relativistic electrons | Cherenkov light identification in sub-MeV range [59] |
Signaling Pathways and Theoretical Relationships
The underlying physical principles governing Cherenkov emission and its detection follow well-defined theoretical relationships that can be conceptualized as signaling pathways. Understanding these pathways is essential for developing effective hybrid models.
The Cherenkov emission process begins when a charged particle travels through a dielectric medium at a velocity (v) exceeding the phase velocity of light in that medium (c/n, where n is the refractive index). This creates a polarization wake in the medium, similar to a sonic boom, which subsequently relaxes by emitting coherent radiation at characteristic angles defined by the relationship cosθ = 1/(βn), where β = v/c [58] [59].
In biological applications, the emitted Cherenkov photons then undergo complex interactions with tissue components including scattering, absorption, and spectral alterations. These interactions create a discrepancy between the theoretically predicted and actually observable signals, necessitating the sophisticated hybrid modeling approaches described in this review [54].
Hybrid modeling approaches for complex phenomena like Cherenkov emission represent a significant advancement over traditional modeling paradigms. By strategically combining first-principles physics with data-driven components, these methods achieve an optimal balance between computational efficiency and physical accuracy that is particularly valuable in biomedical applications.
The 2-stage Monte Carlo model for tissue Cherenkov emission demonstrates how hybrid approaches can enable practical clinical applications that would be computationally prohibitive using traditional methods. Similarly, the hybrid frameworks developed for proton range verification show how physics-based simulations can enhance the reliability of data-driven methods by providing validated training data and fundamental constraints.
For researchers and drug development professionals, these hybrid modeling approaches offer powerful tools for treatment verification, dose optimization, and therapeutic agent development. The continued refinement of these methodologies, particularly through the systematic application of hybrid modeling design patterns, promises to further enhance their accuracy, efficiency, and applicability across diverse medical physics scenarios.
Navigating Challenges: Troubleshooting and Optimizing Your Monte Carlo Workflow
Monte Carlo (MC) simulation stands as the gold standard for modeling complex light-tissue interactions in biomedical research, particularly for validating models with experimental tissue data [4] [60]. These simulations enable researchers to precisely replicate the underlying physics of photon propagation through turbid media, providing essential support for applications in emission and transmission tomography, photodynamic therapy planning, and bioluminescence imaging [4] [60]. However, the computational expense of traditional CPU-based MC methods has historically constrained their practical application, often requiring days or weeks to achieve statistically significant results [4]. The intrinsic stochastic nature of MC algorithms, while ensuring accuracy, demands numerous random samples to converge toward reliable solutions, creating a significant bottleneck in research workflows [60].
The emergence of GPU-based parallel computing has fundamentally transformed this landscape, offering a cost-effective solution for MC acceleration [4]. Unlike CPUs designed for low-latency sequential processing, GPUs provide massively parallel architecture that can simultaneously execute thousands of independent photon transport calculations [61]. This architectural alignment with MC methodologies has enabled speedup factors ranging from 100 to 1000 times compared to single-threaded CPU implementations, making previously impractical simulations feasible within reasonable timeframes [4]. For researchers validating MC models with experimental tissue data, this performance leap enables more extensive parameter studies, higher-resolution simulations, and faster iteration cycles between computational predictions and empirical validation. The evolution of GPU technologies continues to unlock new possibilities, with emerging features like ray-tracing cores, tensor cores, and GPU-execution-friendly transport methods offering further opportunities for performance enhancement in biomedical simulation pipelines [4].
Comparative Analysis of GPU-Accelerated Monte Carlo Platforms
Performance Metrics and Feature Comparison
Table 1: Comparison of GPU-Accelerated Monte Carlo Simulation Platforms
| Platform | Acceleration | Speedup vs CPU | Geometry Support | Programming Framework | Key Features |
|---|---|---|---|---|---|
| FullMonteCUDA [60] | GPU | 288-936x (single-thread); 4-13x (vectorized multi-thread) | Tetrahedral meshes | CUDA | Photon packet weighting, hop-drop-spin algorithm, support for complex clinical models |
| MMCL [62] | GPU | Up to 420x | Tetrahedral meshes | OpenCL | Branchless-Badouel ray-tracing, dual-grid optimization, wide-field source support |
| Monte Carlo eXtreme (MCX) [61] | GPU | 300-400x | 3D voxels | NVIDIA CUDA | Persistent thread kernel, optimized memory utilization, fast ray-tracing |
| GPU-based MC Platforms [4] | GPU | 100-1000x (general range) | Voxels, tetrahedral meshes | CUDA, OpenCL | Emerging ray-tracing cores, tensor core utilization |
Table 2: Technical Specifications and Application Context
| Platform | Memory Optimization | Experimental Validation | Target Applications | Accessibility |
|---|---|---|---|---|
| FullMonteCUDA [60] | Efficient caching for irregular memory access | Benchmark models with complex meshes | Photodynamic therapy, bioluminescence imaging | Open-source (www.fullmonte.org) |
| MMCL [62] | Reduced memory latency, shared memory optimization | Wide range of complexity and optical properties | Diffuse optical tomography, fluorescence molecular tomography | Open-source (http://mcx.space/#mmc) |
| Monte Carlo eXtreme (MCX) [61] | Tuned GPU memory utilization, reduced data races | Photon migration in 3D turbid media | Time-resolved photon transport, brain scans | Freely available, 30,000+ users |
| GPU-based MC Platforms [4] | Modular architecture for evolving hardware | Tomography system designs | Virtual clinical trials, digital twins for healthcare | Various availability |
Critical Performance Trade-offs and Considerations
The comparative analysis of GPU-accelerated MC platforms reveals several critical trade-offs that researchers must consider when selecting tools for validating models with experimental tissue data. FullMonteCUDA demonstrates exceptional performance gains, particularly when compared to non-vectorized CPU code, though its advantage narrows when benchmarked against highly optimized, hand-vectorized multi-threaded CPU implementations [60]. This platform excels in scenarios requiring accurate modeling of complex anatomical boundaries, as offered by its tetrahedral mesh support, but requires substantial GPU memory resources for clinical-scale models [60].
MMCL prioritizes cross-platform compatibility through its OpenCL implementation, enabling execution across diverse GPU architectures from different vendors [62]. While this flexibility enhances accessibility, it may come with a performance penalty compared to native CUDA implementations specifically optimized for NVIDIA hardware [62]. The platform's branchless-Badouel ray tracer efficiently minimizes thread divergence, a common performance limitation in GPU computing, but implements complex vector operations that demand significant computational resources per photon step [62].
Monte Carlo eXtreme (MCX) focuses on voxel-based geometries, offering exceptional performance for structured domains but potentially sacrificing the anatomical accuracy achievable with unstructured meshes [61]. Its persistent thread kernel implementation demonstrates approximately 20% performance improvement across multiple GPU architectures, highlighting the importance of architecture-specific optimizations [61]. Researchers working with segmented medical imaging data often find voxel-based approaches more straightforward to implement, though with potential compromises in accurately representing curved tissue boundaries.
Experimental Protocols for GPU-Accelerated Monte Carlo Simulation
Benchmarking Methodologies and Validation Approaches
The experimental protocols for evaluating GPU-accelerated MC platforms employ rigorous benchmarking methodologies to ensure statistical reliability and physical accuracy. For FullMonteCUDA, validation involves comparing simulation results against both analytical solutions and experimental measurements across multiple benchmark models with varying complexity [60]. The platform utilizes the "hop-drop-spin" algorithm, where photon packets are launched with initial positions and directions, then undergo a sequence of steps: drawing a random step length based on attenuation coefficients, hopping (moving) along direction vectors, handling boundary crossings with Fresnel reflections and refraction, dropping weight (absorption), and spinning (scattering) with direction changes based on the Henyey-Greenstein scattering function [60]. This approach accurately models light propagation in complex tissues while maintaining computational efficiency through careful management of photon packet termination via Russian roulette weighting [60].
The MMCL platform employs a different methodological approach centered on its branchless-Badouel ray tracer, which formulates photon advancement as a series of five-step, four-component-vector operations [62]. This implementation maximizes GPU computational throughput by minimizing conditional branching and enabling efficient parallel execution. Validation protocols for MMCL include comparisons with state-of-the-art single-threaded CPU simulations across domains with varying optical properties and geometric complexities [62]. The platform supports comprehensive detected photon data collection, including partial pathlengths, scattering event counts, and momentum transfer, enabling rich comparison with experimental measurements [62]. Additionally, MMCL incorporates "photon replay" capabilities for constructing Jacobian matrices, essential for solving inverse problems in optical tomography [62].
For Monte Carlo eXtreme (MCX), experimental validation focuses on time-resolved photon migration in 3D turbid media [61]. Performance benchmarks compare execution times against single-threaded CPU implementations on Intel Core i7 processors, with specific attention to memory utilization patterns and thread divergence minimization [61]. The platform's persistent thread kernel implementation employs automatic tuning to optimize grid configuration for different GPU architectures, maximizing hardware utilization across generations from Fermi to Maxwell architectures [61]. Experimental protocols also verify numerical accuracy through comparison with established MC codes and analytical solutions in standardized geometries [61].
Diagram 1: GPU Monte Carlo Photon Transport Workflow. This diagram illustrates the core algorithm shared by platforms like FullMonteCUDA, showing the sequence of photon packet propagation, boundary handling, and termination checks [60].
Integration with Experimental Data Validation Pipelines
A critical aspect of modern GPU-accelerated MC platforms is their integration with experimental data validation pipelines. The DeepSMCP framework demonstrates this integration by combining deep learning with MC simulations, using a two-channel 3D U-net architecture to denoise MC dose distributions with high statistical uncertainty [63]. This approach reduces computation time by a factor of 340 while maintaining accuracy, with validation performed using Gamma passing rates (2% global, 2 mm, 10% threshold) comparing denoised and low-statistical-uncertainty MC dose distributions [63]. Such hybrid methodologies enable researchers to maintain high accuracy while dramatically reducing computational requirements for clinical applications.
For tomography applications, GPU-accelerated MC codes provide the computational performance needed for practical, large-scale applications that were previously infeasible with legacy general-purpose codes [4]. Validation protocols in this domain often involve comparing simulated projections with actual clinical CT and CBCT measurements, with MC simulations used to investigate new system designs, optimize reconstruction algorithms with artifact corrections, and develop spectral CT techniques [4]. The ability to rapidly simulate complex physical interactions in emerging tomography systems enables more robust validation against experimental tissue data, strengthening the role of computational methods in diagnostic imaging innovation.
Table 3: Essential Computational Resources for GPU-Accelerated Monte Carlo Research
| Resource Category | Specific Examples | Function in Research | Implementation Notes |
|---|---|---|---|
| GPU Hardware | NVIDIA GTX 980, modern NVIDIA GPUs (FullMonteCUDA) | Massively parallel computation of photon transport | Architecture-specific optimizations critical for performance |
| Programming Frameworks | CUDA, OpenCL | GPU kernel development and optimization | CUDA for NVIDIA-specific optimization, OpenCL for cross-vendor compatibility |
| Mesh Generation Tools | Tetrahedral mesh generators | Anatomically accurate tissue geometry representation | More accurate for boundaries than voxels but higher memory demands |
| Validation Datasets | Benchmark models with known solutions | Verification of simulation accuracy | Include various complexity levels and optical properties |
| Deep Learning Integration | 3D U-net architectures (DeepSMCP) | Denoising of high statistical uncertainty simulations | 340x efficiency gain demonstrated for dose calculations |
| Performance Analysis Tools | NVIDIA SASSI, profiling tools | Optimization and bottleneck identification | Architecture-specific tuning for different GPU generations |
The rapid evolution of GPU technologies continues to shape the landscape of MC simulations for biomedical research. Emerging trends include the leveraging of specialized GPU hardware such as ray-tracing cores and tensor cores to further accelerate computational performance [4]. The adoption of more GPU-execution-friendly transport methods represents another significant direction for innovation, potentially offering additional speedup while maintaining the physical accuracy essential for validating models with experimental tissue data [4]. These advancements will enable more sophisticated simulation scenarios, including the emerging concepts of training machine learning models with synthetic MC-generated data, developing digital twins for healthcare applications, and conducting comprehensive virtual clinical trials [4].
The ongoing challenge of balancing computational efficiency with anatomical accuracy will continue to drive innovation in geometry representation, with tetrahedral meshes, voxel-based approaches, and hybrid methods each finding application in specific research contexts. As GPU memory capacities increase and algorithms become more sophisticated, the scale and resolution of feasible simulations will expand accordingly, enabling researchers to address increasingly complex biological questions. The modularization of GPU-based MC codes to adapt to evolving simulation needs represents an important direction for future development, facilitating community collaboration and code reuse across research institutions [4]. For researchers focused on validating MC models with experimental tissue data, these advancements will provide increasingly powerful tools to bridge computational predictions and empirical observations, ultimately accelerating progress in biomedical discovery and therapeutic development.
Diagram 2: GPU-Accelerated Monte Carlo Validation Framework. This diagram shows the iterative workflow between experimental data and GPU-accelerated simulations, highlighting how acceleration strategies integrate into the research process for model validation [4] [60].
Overcoming Limited Manufacturer Disclosure in Linac Head Modeling
Monte Carlo (MC) simulations are essential for precise dose calculation in radiotherapy, directly impacting treatment efficacy and safety. A significant challenge in this field is the limited manufacturer disclosure of linear accelerator (linac) head geometries and internal component specifications. This restriction hinders the development of accurate simulation models, necessary for treatment planning, quality assurance, and system commissioning. This guide objectively compares the performance of alternative modeling methodologies researchers have developed to overcome this obstacle, validated against experimental dosimetric data.
Methodological Comparison for Incomplete Geometry Modeling
When precise manufacturer blueprints are unavailable, researchers employ several strategies to create accurate models. The following table summarizes the core approaches, their implementation, and key performance findings from recent studies.
| Modeling Approach | Core Principle | Reported Implementation | Key Performance Findings |
|---|---|---|---|
| Hypothetical Geometry [24] [64] | Construct a simplified but physically plausible linac head model, tuning key parameters against measurement data. | PENELOPE/penEasy for a Liac HWL IOERT accelerator; geometry defined by inner diameter, scattering foil, and exit window thickness [24] [64]. | Output factors matched measurement within 2.5%; PDDs/OARs achieved >93% gamma pass rate (2%/1mm) for most cases [24] [64]. |
| Virtual Source Model (VSM) [65] | Derive a parameterized source model from dose measurements in water, avoiding the need for explicit geometric details. | Geant4; model with primary (focal) and secondary (extra-focal) photon sources tuned to match measured dose distributions [65]. | Achieved agreement with experimental dose distributions within tolerance levels of 2%/2 mm for 6 MV photon beams (FF & FFF) [65]. |
| Platform Benchmarking [66] | Compare established Geant4-based platforms to identify performance trade-offs between accuracy and efficiency. | GATE (v9.1) vs. TOPAS (v3.9) for a Varian CLINAC IX; geometry based on available manufacturer data [66]. | TOPAS provided superior dosimetric agreement in deep dose regions; GATE offered marginally better computation times with advanced variance reduction [66]. |
Experimental Validation and Performance Data
Validation against experimental measurement is the cornerstone of establishing a model's credibility. The following table quantifies the performance of various models from the cited research, providing a basis for comparison.
| Study Focus / Linac Model | Monte Carlo Tool | Validation Metric | Quantitative Result vs. Experiment |
|---|---|---|---|
| Elekta Synergy (6 MV) [67] | Geant4 (Grid Computing) | Gamma Index (2%/2mm) | >98% of points passed for PDDs and profiles across field sizes (5x5 cm² to 20x20 cm²) [67]. |
| Varian CLINAC IX (6 MV) [66] | GATE & TOPAS | Percentage Depth Dose (PDD) | Both platforms showed good agreement; TOPAS superior in deep dose regions [66]. |
| Liac HWL (IOERT) [24] [64] | PENELOPE/penEasy | Output Factors (OF) | Mean agreement within 2.5% for all applicators and energies [24] [64]. |
| 6 MV Photon Beam Source Model [65] | Geant4 & DPM | Dose Distribution | Agreement within 2%/2 mm gamma criteria for 30x30 cm² field [65]. |
| Filter Design for FFF Linac [68] | EGSnrc | Local Dose Difference | Best filter (FakeBeam) showed average PDD deviation of -4.28 ± 1.88% (excluding build-up) [68]. |
Detailed Experimental Protocols
To ensure reproducibility, the following outlines the key methodological steps from the benchmarked studies.
Geometry Modeling and Source Parameter Tuning
- Hypothetical Geometry Construction: For the Liac HWL model, a simplified head geometry was built based on a previous design from the same company. Key undefined parameters (e.g., scattering foil thickness) were treated as variables for optimization [24] [64].
- Electron Source Characterization: In the absence of precise data, initial electron beam parameters (energy and spatial spread) are determined through an iterative tuning process. For example, one study found 7.0 MeV initial energy and a 0.2 cm FWHM Gaussian spatial distribution provided the best match for their Varian linac model [68].
- Virtual Source Model Derivation: This method bypasses geometry by building a parameterized model of the photon beam itself. The model in [65] used two sub-sources (primary and scattered) with fluence functions and energy spectra tuned exclusively against measured dose distributions in a water phantom.
Simulation Execution and Dose Calculation
- Phantom Setup: Simulations are typically validated by calculating dose in a virtual water phantom. For the Liac HWL validation, dose was calculated for various applicator sizes, bevel angles, and electron energies (6, 8, 10, 12 MeV) [24] [64].
- Variance Reduction: To achieve statistically significant results in feasible computation times, advanced techniques are essential. Studies utilized methods like phase space files (storing particle state information for reuse) and direct bremsstrahlung splitting (DBS) to improve simulation efficiency [66] [68].
Validation against Experimental Data
- Data Acquisition: Experimental benchmarks are acquired using ionization chambers in a water tank scanner under standard setup conditions (e.g., SSD = 100 cm) [66] [68].
- Gamma Analysis: This is the standard method for quantitative comparison, evaluating the combination of dose difference (e.g., 2%) and distance-to-agreement (e.g., 2 mm or 1 mm). A high percentage of points passing this test indicates a successful model [24] [67].
Research Workflow and Material Toolkit
Modeling Workflow Diagram
The following diagram illustrates the general workflow for developing and validating a linac model with limited data, integrating common steps from the cited methodologies.
The Scientist's Toolkit: Essential Research Reagents and Materials
This table lists key materials and computational tools referenced in the experimental protocols for linac model validation.
| Item / Solution | Function in Research | Specific Examples / Properties |
|---|---|---|
| Water Phantom | Acts as a standardized medium for measuring and validating dose distributions. | PTW MP3 water tank (30x30x30 cm³) with motorized ionization chamber for PDD and profile scans [66]. |
| Ionization Chamber | The primary detector for relative dose measurement in water. | Compact Chamber (CC13) with 0.13 cm³ active volume, used for high-resolution beam profiling [68]. |
| Tissue-Equivalent Phantoms | Used to simulate human tissue for more anatomically realistic validation. | PMMA and epoxy resin phantoms; used to evaluate tissue-air ratios (TAR) and attenuation properties [69]. |
| 3D Printing Filaments | Enable fabrication of custom, anthropomorphic phantoms for patient-specific validation. | PLA (density ~1.24 g/cm³) for high-density tissues; ABS (density ~1.04 g/cm³) for soft tissues [6]. |
| Phase Space File (PSF) | A pre-recorded particle state file used as a virtual source to drastically reduce computation time. | IAEA PHSP format files for Liac HWL provided at 6, 8, 10, and 12 MeV for research use [24] [64]. |
| Variance Reduction Techniques | Computational methods to increase simulation efficiency without sacrificing accuracy. | Directional Bremsstrahlung Split (DBS) and particle "kill" actors (e.g., in GATE) to focus CPU time on relevant particles [66] [68]. |
The inability to access detailed manufacturer specifications for linac heads is a significant but surmountable challenge in medical physics. As demonstrated, researchers can employ hypothetical geometries, virtual source models, and leverage the distinct strengths of simulation platforms like GATE and TOPAS to develop highly accurate models. The critical factor for success is rigorous experimental validation using standardized dosimetric protocols in water and tissue-equivalent phantoms. Quantitative metrics such as gamma analysis passing rates and dose difference comparisons confirm that these approaches can meet the stringent accuracy requirements needed for clinical applications, thereby ensuring reliable radiotherapy treatment planning and dose delivery.
Selecting and Tuning Nuclear Models and Cross-Section Data for Accuracy
For researchers in fields ranging from drug development to radiation therapy, Monte Carlo (MC) simulations have become an indispensable tool for predicting how radiation interacts with biological tissues. The accuracy of these simulations, however, is fundamentally dependent on the underlying nuclear models and cross-section data that describe the probabilities of particle interactions with atomic nuclei. Selecting appropriate nuclear data is not merely a technical preliminary but a critical determinant of the reliability of computational outcomes, especially when validating models against experimental tissue data [40]. Inaccuracies in these nuclear parameters can propagate through simulations, leading to significant errors in predicted dose distributions, radiation spectra, and ultimately, in the biological effect models that inform therapeutic decisions.
The challenge facing scientists is the existence of multiple nuclear data libraries—such as ENDF/B, JEFF, JENDL, and CENDL—each developed with different theoretical models and validated against different experimental datasets. These libraries can yield divergent results for the same simulation scenario. A recent study on Accelerator-Based Boron Neutron Capture Therapy (AB-BNCT) revealed that the choice of nuclear database could lead to variations in calculated neutron yield of up to 16.86% and discrepancies in fast neutron dose components exceeding 60% [70]. Such disparities far exceed the 5% error margin typically considered acceptable in clinical applications, highlighting the critical importance of informed nuclear data selection. This guide provides a structured comparison of available options and validation methodologies to help researchers navigate this complex landscape.
Comparative Analysis of Major Nuclear Data Libraries
Several major nuclear data libraries serve as foundational resources for Monte Carlo radiation transport codes. Each library has distinct origins, development priorities, and areas of specialized application.
ENDF/B (United States): Maintained by the Cross Section Evaluation Working Group (CSEWG), this library is widely considered a international standard. The ENDF/B-VIII.1 library introduced significant revisions to proton data libraries, which notably affected the simulated neutron spectra from 7Li(p,n) reactions crucial for BNCT research [70].
JENDL (Japan): Developed by the Japan Atomic Energy Agency, the JENDL-5.0 library has shown particular strengths in simulating certain medical isotope production pathways. Studies indicate it can produce substantially lower estimates of fast neutron components (by 23.42%-63.94%) compared to ENDF/B-VIII.1 [70].
JEFF (Europe): The Joint Evaluated Fission and Fusion library represents a collaborative European effort. It often occupies a middle ground in inter-library comparisons but may yield higher estimates of gamma-ray components in some simulations [70].
CENDL (China): The China Evaluation Nuclear Data Library has shown good agreement with JEFF-3.3 in some comparative studies, particularly for AB-BNCT applications [70].
RIPL-3 (Reference Input Parameter Library): This library serves as a complementary resource, providing input parameters for theoretical nuclear model calculations in software packages like TALYS, which is used for predicting photonuclear reaction cross-sections [71].
Quantitative Performance Comparison Across Applications
Table 1: Performance Comparison of Nuclear Data Libraries in Different Applications
| Application Domain | Library Compared | Key Performance Metric | Result & Variation | Clinical/Research Implication |
|---|---|---|---|---|
| AB-BNCT (7Li(p,n) reaction) | ENDF/B VIII.1 vs. JENDL-5.0 | Neutron yield | 16.86% difference | Directly impacts treatment time and source design |
| AB-BNCT (Beam Shaping Assembly) | ENDF/B VIII.1 vs. JENDL-5.0 | Fast neutron dose component (Df/Φepi) | 19.04%-63.94% higher in ENDF/B | Patient safety and normal tissue complication probability |
| AB-BNCT (Beam Shaping Assembly) | JEFF-3.3/CENDL-3.2 vs. ENDF/B | Gamma-ray dose component (Dγ/Φepi) | 6.79%-10.08% higher | Affects shielding design and whole-body dose |
| Photonuclear reactions (68Zn(γ,n)67Cu) | TALYS with different strength functions | 67Cu production cross-section | Model-dependent variation | Impacts production planning of medical isotopes [71] |
| Linear attenuation coefficient measurement | PHITS vs. NIST/XCOM | Theoretical agreement | "Good agreement" | Validates use of PHITS for tissue substitute characterization [40] |
Performance of Nuclear Models in TALYS for Photonuclear Reactions
The TALYS software package incorporates multiple models for calculating gamma-ray strength functions, which show varying performance across different nuclei:
- Phenomenological Models generally provide better agreement with experimental data for the majority of reactions involving Ni, Cu, and Zn isotopes [71].
- Microscopic Models demonstrate superior performance for specific cases such as the 61,64Ni(γ,n) reactions, where they more accurately reproduce experimental cross-sections [71].
- No Single Superior Model has been identified that works best for all reactions, emphasizing the need for case-specific model selection and validation [71].
Table 2: Optimal Strength Function Models in TALYS for Specific Photonuclear Reactions
| Nuclear Reaction | Best-Performing Model(s) | Nature of Model | Key Consideration |
|---|---|---|---|
| 58Ni(γ,n)57Ni | GFL, SML | Phenomenological | More reliable for this specific reaction |
| 60Ni(γ,n)59Ni | GFL, SML | Phenomenological | Consistent with experimental data |
| 61Ni(γ,n)60Ni | MGLO | Microscopic | Outperforms phenomenological models |
| 64Ni(γ,n)63Ni | MGLO | Microscopic | Superior agreement with measurements |
| 68Zn(γ,n)67Cu | KD | Phenomenological | Relevant for medical 67Cu production [71] |
Experimental Protocols for Validation
Methodology for Validating Linear Attenuation Coefficients
A comprehensive protocol for validating Monte Carlo models against experimental tissue data involves a systematic comparison of simulated parameters with empirical measurements:
Experimental Setup Configuration: Utilize a spectrometer system with a NaI(Tl) scintillator detector and radioactive sources (such as Ra-226 with principal gamma energies between 186.1 and 2204.1 keV). Tissue substitute samples, like ballistic gel (BGel), are positioned between the source and detector [40].
Measurement Procedure: Record the photon count rates both with (I) and without (I₀) the tissue substitute sample in place. The linear attenuation coefficient (μ) is then calculated using the Beer-Lambert law: μ = -ln(I/I₀)/x, where x represents the sample thickness [40].
Monte Carlo Simulation: Model the exact experimental geometry using radiation transport codes such as PHITS (version 3.32 or later). Simulate the experiment using the same source energies and geometry [40].
Theoretical Benchmarking: Compare both experimental and simulation results against theoretical values from established databases like NIST/XCOM [40].
Validation Criteria: Establish acceptance criteria for agreement between simulation and experiment. The validated computational model can then be used to understand limitations of the experimental setup and recommend correction factors if necessary [40].
Workflow for Nuclear Database Selection and Validation
The following diagram illustrates the systematic workflow for selecting and validating nuclear models and cross-section data:
Protocol for Inter-Database Comparison Studies
For comprehensive evaluation of nuclear database performance:
Two-Stage Modeling Approach:
- First, compare different proton libraries (ENDF/B VII.1/VIII.1, CP2020, JENDL-5.0) for particle yield calculations (e.g., neutron spectra from 2.8 MeV protons on lithium targets) [70].
- Second, use the resulting particle spectra as source terms for subsequent simulations of radiation transport through various materials, applying different neutron libraries (ENDF/B VIII.0/VIII.1, JEFF-3.3, CENDL-3.2, JENDL-5.0) [70].
Standardized Evaluation Metrics: Utilize internationally recognized beam quality parameters such as those recommended by the IAEA, including:
- Φepi: Epithermal neutron flux
- Df/Φepi: Fast neutron dose per epithermal neutron
- Dγ/Φepi: Gamma dose per epithernal neutron [70]
Root Cause Analysis: Employ cross-section replacement techniques to identify specific nuclides and reaction types responsible for observed discrepancies between libraries [70].
Essential Research Reagents and Computational Tools
The Scientist's Toolkit for Nuclear Data Validation
Table 3: Essential Resources for Nuclear Data Research and Validation
| Category | Specific Tool/Library | Primary Function | Application Context |
|---|---|---|---|
| Monte Carlo Codes | PHITS | Multi-purpose particle transport simulation | Modeling radiation interactions with matter [40] [70] |
| PENELOPE/penEasy | Electron and photon transport | IOERT accelerator modeling [24] | |
| Nuclear Data Libraries | ENDF/B-VIII.1 | Comprehensive neutron, proton, photon data | General purpose; AB-BNCT studies [70] |
| JENDL-5.0 | Comprehensive neutron, proton, photon data | Alternative for medical isotope production [70] | |
| RIPL-3 | Input parameters for nuclear model calculations | Theoretical cross-section calculations [71] | |
| Experimental Tools | NaI(Tl) Spectrometer | Gamma-ray spectroscopy | Experimental validation of attenuation coefficients [40] |
| HPGe Detector | High-resolution gamma spectroscopy | Precise radiation measurement [40] | |
| Reference Data | NIST/XCOM | Photon cross-section database | Theoretical benchmark for validation [40] |
| EXFOR | Experimental nuclear reaction data | Validation of theoretical models [71] | |
| Analysis Tools | TALYS | Nuclear reaction simulation | Prediction of reaction cross-sections [71] |
The selection and tuning of nuclear models and cross-section data represent a critical step in ensuring the accuracy of Monte Carlo simulations for medical applications. Based on the comparative analysis presented in this guide, the following recommendations emerge:
No single nuclear data library outperforms all others in every application. Researchers should select libraries based on their specific application (e.g., JENDL-5.0 for reduced fast neutron components in BNCT, or specific strength functions in TALYS for particular photonuclear reactions) [71] [70].
Multi-library comparison studies should be standard practice before committing to a single library for extensive simulations. Significant variations (up to 60% in some dose components) between libraries necessitate this prudent approach [70].
Validation against experimental data remains essential. Even the most sophisticated models require validation against empirical measurements, particularly when extending simulations to new energy ranges or material compositions [40].
Documentation of nuclear data selection rationale should be comprehensive. Research publications should explicitly state the libraries and models used, along with justification for their selection based on the specific application context.
As computational methods continue to advance, the integration of machine learning techniques with traditional nuclear data evaluation shows promise for addressing current limitations. Future work should focus on expanding experimental validation datasets, particularly for medical isotope production pathways and tissue-equivalent materials, to further refine the nuclear models that underpin accurate patient care in nuclear medicine and radiation therapy.
Managing Statistical Uncertainty and Optimizing Particle Numbers for Efficiency
Monte Carlo (MC) simulation is a computational algorithm that relies on repeated random sampling to obtain numerical results and is considered the most accurate method for dose calculation in radiotherapy treatments [72] [73]. However, a fundamental challenge exists: the inherent trade-off between the statistical uncertainty of the calculation and the associated computational cost [73]. A lower statistical uncertainty requires simulating a greater number of particle histories, leading to more accurate dose distributions but significantly longer calculation times [73]. This review objectively compares strategies for managing this trade-off within the specific context of validating MC models against experimental tissue data, a critical step for clinical application in areas such as proton therapy and intraoperative radiation therapy [9] [24].
Comparative Analysis of Uncertainty Management Approaches
The management of statistical uncertainty in MC simulations can be approached through traditional statistical control or emerging deep learning methods. The table below compares these core approaches.
Table 1: Comparison of Monte Carlo Uncertainty Management Approaches
| Approach | Core Principle | Key Performance Findings | Advantages | Limitations |
|---|---|---|---|---|
| Controlled Statistical Uncertainty [73] | Uses a pre-set, user-defined statistical uncertainty (e.g., 1-3% per plan) to determine the number of particle histories, terminating the simulation once this uncertainty is achieved. | In online adaptive prostate therapy, increasing uncertainty from 1% to 2-3% reduced calculation times by >1 minute with limited clinical impact: median accumulated target D98% reduction of 0.1 Gy [73]. | Considered the most accurate dose calculation method; direct control over statistical precision; validated in clinical TPS [73]. | Computational cost can be "staggeringly high"; high precision requires long runtimes, which can be a bottleneck [72] [73]. |
| Deep Learning Surrogates [5] | A deep learning model (e.g., CHD U-Net) is trained to predict the accurate MC-simulated dose distribution (MCDose) using inputs from faster, less accurate algorithms. | Achieved 99% and 97% gamma passing rate (3%/3mm) for head-and-neck and thorax-abdomen patients, respectively; prediction time reduced to a few seconds [5]. | Extreme speed (seconds); achieves MC-level accuracy; can replace TPS dose in clinical workflows for quality assurance [5]. | Fundamentally relies on MC-generated datasets for training and validation; model performance depends on training data quality and scope [9]. |
Detailed Experimental Protocols
Protocol for Validating Proton Range Verification with Dual-Head PET
This protocol, derived from Gao et al., details the experimental validation of an MC model for proton range verification [9].
- Experimental Setup: In-beam PET data were acquired using a dual-head PET (DHPET) system mounted on a rotating gantry port. Each detector head consisted of 36 modules of BGO (Bi₄Ge₃O₁₂) scintillators. Data were acquired during and for 10 minutes after proton irradiation [9].
- MC Simulation Setup: The entire process, including proton beam delivery, β+ isotope production, and PET detection, was simulated using the GATE (Geant4 Application for Tomographic Emission) platform. The beam model was tuned and commissioned against measured depth-dose profiles in water [9].
- Phantom Experiments: Experiments were performed using homogeneous high-density polyethylene (HDPE) and heterogeneous gel-water phantoms. The MC model's accuracy was assessed by comparing simulated and measured PET activity distributions [9].
- Nuclear Model Comparison: Three different nuclear reaction cross-section models were evaluated for their accuracy in predicting the activity range: the built-in GEANT4 QGSP_BIC hadronic model, the EXFOR-based cross-sections, and an updated dataset from Rodríguez-González et al. (NDS) [9].
- Validation Metrics: The primary metric was the deviation between the simulated and experimentally measured distal activity range (in mm) in the phantoms. For dose verification, depth-dose profiles and detector responses were compared [9].
Protocol for Evaluating MC Uncertainty in Online Adaptive Radiotherapy
This protocol, based on a study on prostate cancer patients, evaluates the clinical impact of higher statistical uncertainty settings in a fractionated treatment regimen [73].
- Patient Data and Planning: Twenty prostate cancer patients with one planning CT and five daily MRI scans were used. Reference plans were optimized in the Monaco TPS with a 1% MC uncertainty [73].
- Simulation of Daily Variations: Three modes of daily anatomical variations were simulated for each patient: rigid whole-body shifts, rigid prostate translations, and prostate rotations [73].
- Uncertainty Settings and Workflow: For each simulated daily scan, adaptive plans were generated using three MC statistical uncertainty settings: 1% (standard, MC1), 2% (MC2), and 3% (MC3). To ensure a fair comparison, plans from MC2 and MC3 were recalculated with a 1% uncertainty (MC2R, MC3R) [73].
- Dose Accumulation and Evaluation: For each mode of variation and MC setting, the five fraction plans were transformed back to the planning scan, and the dose was accumulated. Plan acceptability was judged based on clinical dose-volume criteria for the target (PTV D98%, D2%) and organs at risk (e.g., rectum V35Gy). The accumulated doses from higher uncertainty plans were compared to the standard (MC1) [73].
Workflow for Managing Statistical Uncertainty
The following diagram illustrates the logical decision process for selecting and applying a strategy to manage statistical uncertainty in MC simulations, based on the comparative data.
The Scientist's Toolkit: Key Research Reagents and Materials
The experimental validation of MC models relies on a suite of specialized software, hardware, and experimental setups. The table below details these essential components.
Table 2: Essential Research Toolkit for Monte Carlo Model Validation
| Tool Category | Specific Tool / Material | Function in Research |
|---|---|---|
| MC Simulation Software | GATE/GEANT4 [9], PENELOPE/penEasy [24], FLUKA [74] | Platforms to simulate particle transport and interactions in matter; the core engine for generating dose and isotope production predictions. |
| Treatment Planning System (TPS) | RayStation (RS) [9], Monaco [73] | Clinically deployed system used as a benchmark for dose calculation accuracy and for generating inputs for deep learning models. |
| Experimental Phantoms | High-Density Polyethylene (HDPE), Gel-Water Phantom [9], Virtual/Water Phantom [24] [73] | Tissue-equivalent materials or digital models used to experimentally measure or simulate dose distributions and activity ranges for model validation. |
| Nuclear Cross-Section Data | EXFOR Library [9], NDS (Rodríguez-González) [9], Built-in GEANT4 models (QGSP_BIC) [9] | Critical datasets and models that define the probabilities of nuclear interactions; fidelity is crucial for accurate prediction of positron-emitting isotopes. |
| Detection & Imaging Systems | Dual-Head PET (DHPET) [9], In-beam PET [9] | Systems to detect and image secondary particles (e.g., positron emitters) produced during irradiation for experimental range verification. |
| Validation Metrics & Software | Gamma Analysis [24] [73], Gamma Passing Rate (GPR) [5], Dose-Volume Histogram (DVH) [74] [73] | Quantitative tools and metrics to compare simulated and measured dose/activity distributions and assess clinical acceptability. |
Balancing Model Complexity with Computational Feasibility in Tissue Geometries
In the field of biomedical research, computational models, particularly those based on Monte Carlo methods, have become indispensable for simulating complex biological phenomena. However, a significant challenge persists: balancing the physical accuracy of these models, which often requires high complexity, with the practical limitations of computational resources. This guide objectively compares contemporary modeling approaches by examining their experimental validation, with a specific focus on applications involving realistic tissue geometries. The performance of each method is evaluated within the critical framework of validating Monte Carlo models against experimental tissue data, a cornerstone for building reliable, predictive tools in drug development and therapeutic innovation.
Comparative Analysis of Modeling Approaches
The table below summarizes the core methodologies, key performance metrics, and ideal use cases for different approaches to managing model complexity in tissue simulations.
| Modeling Approach | Core Methodology | Key Performance Metrics | Tissue Geometry Applications | Supporting Experimental Data |
|---|---|---|---|---|
| Deep Learning Surrogates [5] | A Cascade Hierarchically Densely 3D U-Net (CHD U-Net) trained to predict computationally intensive Monte Carlo dose (MCDose) using CT images and TPSDose as inputs. | • Gamma Passing Rate (GPR): 99% (head & neck) and 97% (thorax & abdomen) at 3%/3mm [5]• Speed: Prediction in a few seconds vs. hours for full MC [5] | Heavy ion therapy treatment planning for head-and-neck and thorax-and-abdomen patients [5]. | Validation on 67 head-and-neck and 30 thorax-and-abdomen patients [5]. |
| Full Monte Carlo Simulation [9] | GATE/GEANT4 simulation of proton therapy, tracking secondary particle production (e.g., positron-emitters) and transport for PET-based range verification. | • Range Prediction Accuracy: ~1 mm deviation with validated cross-section data (e.g., EXFOR, NDS) [9]• Dose Agreement: Good agreement with clinical treatment planning system (RayStation) [9] | Proton range verification in homogeneous (HDPE) and gel-water phantoms; can be extended to patient-specific CT geometries [9]. | Experimental validation using a dual-head PET system and phantoms; comparison of multiple nuclear cross-section models [9]. |
| Tissue Network Abstraction [75] [76] | Abstraction of tissues into spatial networks (cells as nodes, intercellular connections as edges) for topological analysis and generative modeling. | • Spatial Segregation (τ): Quantifies the number of fields of view needed to capture all cell phenotypes; higher in tumors [76].• Generative Model Fit: Ability to recapitulate observed tissue topology from local rules [75]. | Analysis of cellular organization in Drosophila wing epithelia, plant shoot apical meristem, human lymph node, and breast cancer tissues [75] [76]. | Validation using spatial transcriptomics (Visium) and multiplexed imaging (IMC) of healthy and diseased human tissues [76]. |
| Advanced MC for Novel Therapies [74] [77] | Customized FLUKA/PENELOPE subroutines to simulate novel treatment modalities, such as the convergent X-ray beam of the CONVERAY system or dosimetry for radiopharmaceutical therapy. | • Dose Conformation: Demonstrated high dose concentration within complex intracranial and pulmonary targets [74].• Dosimetry Agreement: Differences between software and reference MC data within ~±5% [77]. | CONVERAY: Intracranial and chest irradiations [74].RPT: Dosimetry validation using IEC NEMA Body Phantom [77]. | CONVERAY: Proof-of-concept MC study [74].RPT: Provides reference dosimetry for 177Lu, 131I, 90Y, etc. [77]. |
Detailed Experimental Protocols and Validation
A critical component of adopting any computational model is the rigorousness of its experimental validation. The following section details the protocols and benchmarks used for the approaches discussed.
Validation of Deep Learning Surrogates in Heavy Ion Therapy
Objective: To validate a deep learning (DL) model for rapid prediction of Monte Carlo-simulated dose distributions (MCDose) in heavy ion therapy (HIT), ensuring accuracy comparable to gold-standard MC methods but at a fraction of the computational time [5].
Materials & Methods:
- Data: Computed tomography (CT) images and corresponding treatment planning system dose (TPSDose) for 67 head-and-neck and 30 thorax-and-abdomen patients [5].
- Model Architecture: A Cascade Hierarchically Densely connected 3D U-Net (CHD U-Net) was developed and compared against alternative DL models (C3D and HD U-Net) [5].
- Training: The model was trained to map the input CT and TPSDose to the accurate MCDose.
- Validation Metric: The Gamma Passing Rate (GPR) was used as the primary metric, with a dose difference/distance-to-agreement criterion of 3%/3mm considered clinically relevant [5].
Key Outcome: The CHD U-Net model achieved a GPR of 99% for head-and-neck patients and 97% for thorax-and-abdomen patients across the entire body, demonstrating that the DL-predicted dose could replace TPSDose in the clinical HIT process due to its MC-like accuracy [5].
Experimental Validation of Monte Carlo for Proton Range Verification
Objective: To develop and validate a Monte Carlo simulation model for verifying proton range using an in-beam dual-head PET (DHPET) system, critically assessing the impact of different nuclear interaction cross-section models [9].
Materials & Methods:
- Phantoms: Homogeneous high-density polyethylene (HDPE) and gel-water phantoms [9].
- Imaging System: An in-beam dual-head PET system mounted on a proton therapy gantry [9].
- MC Simulation: The GATE (Geant4) platform was used to simulate the entire process: proton beam delivery, production of β+ isotopes (11C, 15O), their decay, and subsequent PET imaging [9].
- Compared Models: Three nuclear models were evaluated: the built-in GEANT4 QGSP_BIC model, the EXFOR-based cross-sections, and the updated dataset from Rodríguez-González et al. (NDS) [9].
- Validation Metric: Accuracy of predicting the proton range (distal fall-off) by comparing the simulated β+ activity distribution against the experimentally measured PET data [9].
Key Outcome: The study established that using validated, experimentally-based cross-section data (EXFOR, NDS) is crucial for accuracy. These models predicted the activity range within 1 mm in HDPE phantoms, whereas the theoretical QGSP_BIC model underestimated the range by 2–4 mm [9].
Spatial Sampling Analysis for Multiplexed Tissue Imaging
Objective: To establish a statistical framework for determining the optimal experimental design—specifically, the number and area of fields of view (FoVs)—for multiplexed imaging technologies to capture all cell phenotypes in a tissue sample [76].
Materials & Methods:
- Data: 22 spatial transcriptomic (Visium) datasets from 12 healthy and tumor human tissues, supplemented with large-area Imaging Mass Cytometry (IMC) data of human lymph nodes [76].
- Simulation: Repeated random sampling of non-overlapping FoVs of varying widths (e.g., 400 µm) from the large tissue maps was performed [76].
- Modeling: The relationship between the number of FoVs (r) and the number of recovered cell phenotype clusters (N(r)) was fit to the model: N(r) = N₀(1 - exp(-r/τ)), where N₀ is the total clusters and τ is a tissue-specific spatial segregation parameter [76].
- Validation Metric: The parameter τ, which indicates how many regions must be imaged to recover most known cell phenotypes, and its relationship with FoV width (τ(w) = C / w^α) [76].
Key Outcome: Tumor tissues were found to have a higher τ value than healthy tissues, meaning more and/or larger regions need to be imaged to capture their full cellular heterogeneity. This provides a quantitative guideline for designing efficient and effective multiplexed imaging experiments [76].
Visualizing Workflows and Relationships
The following diagrams illustrate the logical workflows and key relationships involved in balancing model complexity and feasibility.
Deep Learning Surrogate Model Workflow
Full Monte Carlo Experimental Validation
Complexity vs. Feasibility Relationship
The Scientist's Toolkit: Essential Research Reagents and Materials
This table details key reagents, software, and materials essential for conducting research in this field, as cited in the experimental protocols.
| Item Name | Function / Application | Specific Examples / Notes |
|---|---|---|
| GATE/GEANT4 [9] | A versatile Monte Carlo simulation platform for modeling particle transport in medical physics and radiology. | Used for proton therapy simulation, including beam delivery, isotope production, and PET detector response [9]. |
| FLUKA / PENELOPE [74] | Monte Carlo main codes for accurately simulating radiation transport and dosimetry effects in complex geometries. | Used to model novel radiotherapy devices (e.g., CONVERAY) and calculate patient-specific 3D dose distributions [74]. |
| Imaging Mass Cytometry (IMC) [76] | A multiplexed imaging technology for simultaneous detection of dozens of proteins on a single tissue section. | Used for deep spatial phenotyping of tissues (e.g., lymph node) to validate spatial sampling strategies [76]. |
| Visium Spatial Transcriptomics [76] | A technology that captures the entire transcriptome from a tissue section while retaining spatial location information. | Provides a reference "atlas" of cell phenotypes and their locations for designing multiplexed imaging experiments [76]. |
| IEC NEMA Body Phantom [77] | A standardized physical phantom used for validation and quality control in nuclear medicine and dosimetry. | Serves as a benchmark for end-to-end validation of radiopharmaceutical therapy (RPT) dosimetry workflows [77]. |
| Solid & 3D-Printed Phantoms [7] | Phantoms with well-characterized optical properties used to experimentally validate computational models. | Critical for creating "digital twins" and validating fluorescence Monte Carlo simulations under controlled conditions [7]. |
Adaptive Sampling and Search Algorithms for Enhanced Efficiency
In the realm of scientific research, particularly in fields requiring the analysis of highly complex systems like tissue data, computational efficiency is paramount. Adaptive sampling and search algorithms have emerged as powerful techniques to navigate vast decision spaces and optimize resource allocation. This guide focuses on the application of these algorithms, specifically Monte Carlo Tree Search (MCTS) and nanopore adaptive sampling tools, within a research context that prioritizes validation against experimental tissue data. The core challenge this addresses is balancing the need for comprehensive exploration with the practical constraints of computational time and cost, a common hurdle in studies involving intricate biological systems [78] [79] [72].
Monte Carlo methods, at their essence, are a broad class of computational algorithms that rely on repeated random sampling to obtain numerical results for problems that might be deterministic in principle but are too complex for direct solution [72]. The MCTS algorithm, a heuristic search algorithm, is a prominent example that has revolutionized decision processes in areas like game playing and is increasingly applied in scientific and engineering domains [78]. Its power lies in its ability to asymmetrically grow a search tree, concentrating computational efforts on the most promising regions of the search space [78].
Simultaneously, in the field of genomics, adaptive sampling has become a critical technology for real-time enrichment of target DNA sequences during nanopore sequencing. This process allows for the selective sequencing of genomic regions of interest—such as genes associated with cancer or hereditary diseases—while depleting unwanted background reads, thereby significantly improving sequencing efficiency and diagnostic accuracy [80]. The validation of computational models derived from such data, including those built using MCTS, against experimental tissue data is a cornerstone of robust scientific methodology, a process better described as "experimental corroboration" than mere validation [81].
This guide provides an objective comparison of current adaptive sampling and search tools, detailing their performance and experimental protocols to aid researchers in selecting the optimal algorithms for their specific research needs.
Core Algorithmic Principles
Monte Carlo Tree Search (MCTS)
Monte Carlo Tree Search is a heuristic search algorithm that combines the precision of tree search with the generality of random sampling. It is particularly effective for problems with enormous decision spaces, such as the game of Go, which has approximately 10¹⁷⁰ possible states [79]. Unlike exhaustive search methods, MCTS avoids exploring every possible move by balancing exploration and exploitation, using statistical sampling to guide decisions [79]. The algorithm operates through an iterative process consisting of four distinct phases [78] [79]:
- Selection: Starting from the root node (representing the current state), the algorithm traverses down the tree by selecting the most promising child nodes at each level. The most common selection rule is the Upper Confidence Bounds applied to Trees (UCT) formula, which balances moves with a high average reward (exploitation) against moves that have been tried less frequently (exploration) [78] [79].
- Expansion: When the selection phase reaches a leaf node (a node with potential children that haven't been simulated yet), the algorithm expands the tree by adding one or more child nodes representing possible actions from that state [78] [79].
- Simulation (Rollout): From the newly added node, a simulation is run to a terminal state (the end of the game or process). During this phase, moves are typically chosen randomly or using simple heuristics, making it computationally inexpensive [78] [79].
- Backpropagation: The result of the simulation is propagated back up the tree to the root node. All nodes visited during the selection phase have their statistics—namely, the visit count and the cumulative win/reward value—updated [78] [79].
The UCT formula used in the selection phase is:
UCB1(i) = (w_i / n_i) + c * sqrt(ln(N_i) / n_i)
Where w_i is the number of wins after the i-th move, n_i is the number of simulations for the node after the i-th move, N_i is the total number of simulations for the parent node, and c is an exploration parameter (theoretically √2) [78].
Table: The Four Phases of Monte Carlo Tree Search
| Phase | Core Function | Key Mechanism |
|---|---|---|
| Selection | Identifies the most promising path through the existing tree. | UCT formula balances known rewards (exploitation) and less-traveled paths (exploration). |
| Expansion | Grows the search tree based on new information. | Adds one or more child nodes to a leaf node, representing new possible states. |
| Simulation | Estimates the value of a new node. | Conducts a fast, random playout from the new node to a terminal state. |
| Backpropagation | Updates the tree with knowledge gained from the simulation. | Propagates the simulation result backward, updating visit counts and win scores for all ancestor nodes. |
The following diagram illustrates the logical flow and iterative nature of this four-phase process:
Diagram 1: The iterative four-phase cycle of the Monte Carlo Tree Search algorithm.
Adaptive Sampling in Nanopore Sequencing
Adaptive sampling is a feature of nanopore sequencing that enables real-time selective sequencing. It allows the sequencer to enrich target reads (e.g., from a specific gene or pathogen) and deplete unwanted reads (e.g., host DNA) during the sequencing run itself, without additional sample preparation [80]. The core mechanism involves the rapid classification of the initial segment of a DNA read and then applying a reverse voltage to eject off-target molecules from the pore before they are fully sequenced [80].
The tools that enable this functionality rely on one of three primary computational approaches for read classification [80]:
- Alignment-based: This method converts raw electronic signals into nucleotide sequences (basecalling) using tools like Guppy, and then aligns the sequences to a reference using tools like minimap2 to determine if the read originates from a target region.
- Raw signal-based: This approach compares the raw current signal directly against a simulated signal derived from a reference genome, using algorithms like dynamic time warping or probabilistic k-mer matching (e.g., UNCALLED, Sigmap), avoiding the computational cost of basecalling.
- Deep learning-based: This emerging method uses convolutional neural networks (e.g., SquiggleNet) trained on raw signals to classify target reads, potentially capturing additional information like DNA modification patterns.
The following workflow diagram maps the process of a nanopore adaptive sampling experiment, from sample loading to data analysis:
Diagram 2: The real-time decision-making workflow for adaptive sampling during nanopore sequencing.
Comparative Performance Analysis of Adaptive Sampling Tools
A comprehensive benchmarking study (2025) evaluated six widely used adaptive sampling tools under identical conditions to provide a fair and consistent comparison [80]. The study assessed performance across three distinct tasks: intraspecies enrichment of COSMIC cancer genes from human DNA, interspecies enrichment of Saccharomyces cerevisiae, and host background depletion of human DNA [80]. The study introduced two key metrics for evaluation [80]:
- Relative Enrichment Factor (REF): Measures the multiple increase in coverage depth of target regions compared to non-target regions within the adaptive sampling group. It indicates how effectively a tool retains target reads while discarding non-target reads.
- Absolute Enrichment Factor (AEF): Quantifies the multiple increase in coverage depth of target regions in the adaptive group compared to that in the control group. This metric provides a more comprehensive understanding of the actual increase in target data, as it is influenced by REF, maintenance of channel activity, and speed of read rejection.
Table: Benchmarking Results of Adaptive Sampling Tools (2025) [80]
| Tool | Computational Approach | Key Finding (Intraspecies Enrichment) | Key Finding (Host Depletion) | Overall Performance Summary |
|---|---|---|---|---|
| MinKNOW | Alignment-based | Achieved an AEF of 4.86 (highest). | Effective at depleting human host DNA. | Excellent all-around performer; prior option for most scenarios. |
| Readfish | Alignment-based | Showed generally excellent performance. | Effective at depleting human host DNA. | Generally excellent enrichment/depletion performance. |
| BOSS-RUNS | Alignment-based | Showed generally excellent performance. | Effective at depleting human host DNA. | Top-class performance, particularly in host depletion. |
| UNCALLED | Raw signal-based | Faster drop in active channels, lower total base output (1.76 Gb). | N/A | Experienced faster drops in active sequencing channels. |
| ReadBouncer | Alignment-based | Optimal maintenance of channel activity (4.2 Gb output). | N/A | Maintained channel activity well, generating high total base output. |
| SquiggleNet | Deep learning-based | N/A | Achieved top-class performance. | Remarkable classification efficiency and accuracy; promising for future development. |
The benchmarking concluded that the alignment-based approach, particularly when using Guppy for basecalling and minimap2 for read alignment, was the optimal read classification strategy with the highest accuracy [80]. Tools using this strategy (MinKNOW, Readfish, BOSS-RUNS) generally demonstrated excellent performance. Furthermore, the study highlighted that deep learning methods utilizing raw signals demonstrate higher accuracy and quicker read ejection, achieving top-class performance in host depletion and warranting greater emphasis in future software development [80].
Experimental Protocols for Validation
Benchmarking Adaptive Sampling Tools
The 2025 benchmarking study employed a rigorous and consistent experimental protocol to ensure an unbiased comparison [80].
- Experimental Setup: All experiments were performed on the same computer, sequencer, and flow cell type for an equal duration. Each flow cell was divided into two groups: a control group (256 channels with no adaptive sampling) and an adaptive group (256 channels running the adaptive sampling tool). This allowed for the correction of random bias from initial nanopore activity differences [80].
- Task Design:
- Intraspecies Enrichment: 373 COSMIC genes on human odd-numbered chromosomes, with a total search space of 45.0 Mb [80].
- Interspecies Enrichment: Enrichment of Saccharomyces cerevisiae reads from a mixed sample [80].
- Host Depletion: Depletion of human host DNA to improve the yield of non-human reads [80].
- Data Analysis: The output of the adaptive group was adjusted based on the control group's output. The key metrics of REF and AEF were calculated to evaluate the enrichment levels achieved by each tool [80].
Validating with Experimental Tissue Data
The process of computationally identifying key genes and then validating them with experimental tissue data is a critical practice in bioinformatics. A 2024 study on osteoarthritis (OA) provides a clear protocol for this type of validation [82].
- Computational Identification:
- Data Acquisition: Obtain relevant transcriptome and single-cell RNA sequencing (scRNA-seq) datasets from public repositories like the Gene Expression Omnibus (GEO) [82].
- Differential Expression Analysis: Use tools like the R package "limma" to identify Differentially Expressed Genes (DEGs) between disease (e.g., OA) and control groups [82].
- Machine Learning Filtering: Apply multiple machine learning algorithms (e.g., LASSO regression, Random Forest, Support Vector Machine) to the DEGs to narrow down characteristic "key" genes [82].
- Experimental Corroboration:
- In Vitro Validation: Isolate primary cells (e.g., chondrocytes from cartilage tissue) from both disease and healthy control samples [82].
- qPCR Analysis: Perform quantitative PCR (qPCR) on the RNA extracted from these cells to measure the expression levels of the computationally identified key genes. This step confirms whether the expression trends observed in the computational models (e.g., upregulation or downregulation) are consistent in actual biological samples [82].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key reagents, tools, and materials for adaptive sampling and validation experiments
| Item Name | Function / Application | Specific Examples / Notes |
|---|---|---|
| Nanopore Sequencer | Platform for real-time, adaptive sampling sequencing. | GridION, PromethION (Oxford Nanopore Technologies). |
| Adaptive Sampling Software | Determines read rejection/enrichment in real-time. | MinKNOW (integrated), Readfish, BOSS-RUNS, UNCALLED. |
| Basecalling Software | Translates raw current signals into nucleotide sequences. | Guppy, Bonito. A critical component for alignment-based tools. |
| Sequence Alignment Tool | Aligns basecalled reads to a reference genome. | Minimap2. Used by many alignment-based adaptive sampling tools. |
| Reference Genome | A digital sequence database used for read classification. | FASTA file of target (e.g., COSMIC genes) and non-target regions. |
| High-Quality DNA Sample | Input material for nanopore sequencing. | Requires high molecular weight DNA for best results. |
| R/Bioconductor Packages | For computational analysis and DEG identification. | "limma" for DEG analysis, "glmnet" for LASSO regression. |
| Cell Culture Reagents | For maintaining and expanding primary cell lines. | Used for in vitro validation of computational findings. |
| qPCR Reagents | For quantifying gene expression levels in tissue samples. | Includes primers, probes, reverse transcriptase, and SYBR Green. |
| Primary Cells/Tissue Samples | Biological material for experimental corroboration. | e.g., Human chondrocytes from OA and normal cartilage [82]. |
The comparative analysis of adaptive sampling and search algorithms reveals a rapidly evolving landscape. For nanopore sequencing, alignment-based tools like MinKNOW, Readfish, and BOSS-RUNS currently offer robust and reliable performance for a wide range of enrichment and depletion tasks, making them a recommended starting point for most applications [80]. However, emerging deep learning-based methods show significant promise in terms of speed and accuracy, indicating a likely direction for future development [80].
The MCTS algorithm provides a powerful, general-purpose framework for efficient decision-making in complex spaces, excelling by balancing exploration with exploitation [78] [79]. Its principles can be broadly applied to optimize research workflows beyond genomics.
Ultimately, the integration of these sophisticated computational techniques with rigorous experimental corroboration—such as qPCR validation of gene expression in tissue samples—forms the bedrock of credible research in the era of big data [81] [82]. By carefully selecting the appropriate algorithms and adhering to robust validation protocols, researchers can significantly enhance the efficiency and reliability of their scientific discoveries.
Ensuring Fidelity: Protocols for Quantitative Validation and Comparative Analysis
In computational biomedical research, establishing a model's fidelity requires rigorous benchmarking against experimental and theoretical reference data. This process transforms a simulation from a theoretical exercise into a validated scientific tool. Monte Carlo (MC) methods, which use random sampling to model complex physical systems, are particularly reliant on such validation frameworks. These methods are widely used in biomedical imaging research for estimating dose distributions, understanding photon-tissue interactions, and simulating image acquisition systems [83]. The core principle of validation is that a model must not only reproduce expected trends but also quantitatively match empirical measurements within defined statistical uncertainties.
This guide examines the establishment of gold standards in MC model validation, focusing on applications involving tissue data. We objectively compare validation methodologies and performance outcomes across multiple studies, providing researchers with a framework for assessing and improving their own computational models. The critical importance of this process is underscored by findings that unvalidated models can exhibit significant discrepancies—for instance, certain physics models in proton therapy simulations have demonstrated range deviations of 2–4 mm compared to experimental measurements [9].
Comparative Performance of Monte Carlo Models
Quantitative Validation in Proton Therapy and Tissue Characterization
Table 1: Performance Comparison of Monte Carlo Models in Medical Physics Applications
| Study Focus | Monte Carlo Platform | Validation Reference | Key Performance Metrics | Reported Discrepancies |
|---|---|---|---|---|
| Proton therapy range verification using dual-head PET [9] | GATE/GEANT4 | Experimental activity distribution in HDPE & gel-water phantoms | Activity range prediction accuracy (mean range deviation) | QGSP_BIC: Underestimated distal range by 2–4 mmNDS & EXFOR: Deviations within 1 mm (HDPE phantom) |
| Linear attenuation coefficient measurement [22] | PHITS | NIST XCOM theoretical data; Experimental measurements with Ra-226 source | Relative errors in spectra and linear attenuation coefficients (μ) | Spectra: <1.7% errorMonoenergetic energies: <1% errorμ values: <5% for most energies (12% at 186.1 keV) |
| Clinical CT imaging simulation [83] | GATE | Experimental CT data from Catphan CTP404 phantom | Hounsfield Unit (HU) accuracy for various materials | High contrast materials (Teflon): ~6% deviationLow contrast materials: ~15% deviation |
The comparative data in Table 1 reveals a critical finding: the choice of underlying physics models and cross-section data significantly impacts simulation accuracy, sometimes more than the Monte Carlo platform itself. For example, in proton therapy simulations, while the GATE platform itself is robust, the selection of nuclear models causes variations in range prediction accuracy exceeding 3 mm [9]. This deviation is clinically significant in proton therapy, where millimeter precision directly impacts tumor targeting and healthy tissue sparing.
Similarly, the PHITS code demonstrates exceptional accuracy when validating tissue substitute materials against NIST standards, with errors below 1% for most energy levels [22]. This high degree of precision establishes confidence in using MC methods for characterizing fundamental tissue properties essential for dosimetry. The outlier discrepancy of 12% at 186.1 keV highlights the importance of multi-energy validation, as certain energy ranges may present unique simulation challenges.
Performance Evaluation in Electromagnetic Simulations
Table 2: Accuracy Assessment of Personalized Head Models for EM Simulations
| Model Type | Segmentation Method | Tissue Types | SAR Evaluation Metric | Performance Outcome |
|---|---|---|---|---|
| PHASE (Personalized Head-based Automatic Simulation) [84] | Automated deep learning (SLANT, SimNIBS, GRACE) + CT thresholding | 14 tissue labels | Global SAR and localized SAR-10g vs. gold standard manual segmentation | Achieved comparable SAR accuracy to manually segmented models |
| Simplified head models [84] | Tissue grouping and aggregation | 3-4 tissue classes | Local SAR accuracy in multi-channel B1-shimming | Strong agreement with detailed models when statistical safety margin applied |
| Traditional manual segmentation [84] | Semi-automated expert annotation | 14 tissue types | Global and local SAR distributions | Considered gold standard but time-consuming and impractical for large-scale use |
Table 2 demonstrates that validation extends beyond physical measurements to anatomical modeling accuracy. The emergence of automated segmentation tools like PHASE represents a significant advancement, providing patient-specific head models that achieve comparable electromagnetic simulation accuracy to gold-standard manual segmentation [84]. This validation is crucial for applications like RF coil design and specific absorption rate (SAR) assessment in MRI, where accurate anatomical representation directly impacts safety predictions.
Research indicates that simplified models with only 3-4 tissue classes can maintain sufficient accuracy for certain applications when appropriate safety margins are applied [84]. This finding is particularly valuable for reducing computational complexity while preserving predictive validity, demonstrating that the appropriate validation framework depends on the specific clinical or research application.
Experimental Protocols for Model Validation
Proton Therapy Range Verification Protocol
The validation of Monte Carlo simulations for proton therapy range verification follows a meticulous protocol combining experimental measurements with computational modeling:
Experimental Setup: A dual-head PET (DHPET) system is mounted on a rotating gantry port with the detection center aligned to the gantry isocenter. Each detector head contains 36 detector modules composed of BGO (Bi₄Ge₃O₁₂) scintillator crystals. Measurements are performed using homogeneous high-density polyethylene (HDPE) and gel-water phantoms during proton irradiation [9].
Data Acquisition: During proton irradiation, positron-emitting isotopes (¹¹C, ¹⁵O, ¹³N) are produced through nuclear interactions. The PET system detects coincident gamma rays from positron annihilation, building spatial activity distributions. Beam delivery follows clinical protocols with monoenergetic proton beams ranging from 70-210 MeV [9].
Monte Carlo Simulation: The GATE platform models the entire process, including proton beam delivery, β+ isotope production, isotope decay, photon transport, coincidence detection, and image reconstruction. Crucially, different nuclear models (QGSP_BIC, NDS, EXFOR) are implemented to compare their predictive accuracy [9].
Validation Metrics: The primary validation metric is the activity range, defined as the distal position where activity falls to 50% of its maximum. This is compared to the proton beam's physical range. Additional metrics include depth-activity profiles and absolute activity distributions [9].
Tissue Attenuation Coefficient Measurement Protocol
Validating linear attenuation coefficients for tissue substitutes follows a different approach focused on fundamental material properties:
Experimental Apparatus: The configuration includes ballistic gel tissue substitute samples (10×10×2 cm³) positioned between a 3"×3" NaI(Tl) detector and a Ra-226 source. The detector is shielded with 5 cm thick lead blocks, and the source is collimated with an 8 mm aperture [22].
Photon Energy Spectrum: Multiple photon energies from the Ra-226 source are evaluated (186.1, 241.9, 295.2, 351.9, 609.3, 1759, and 2204.1 keV) to cover a broad energy range relevant to medical applications [22].
Computational Modeling: The PHITS Monte Carlo code simulates the exact experimental setup, tracking photon interactions through the tissue substitutes. Simulations typically require 1×10⁷ source particle histories to achieve sufficient statistical precision [22].
Validation Approach: The simulated linear attenuation coefficients (μ) are compared against both experimental measurements and theoretical values from the NIST XCOM database. Discrepancies are calculated as relative errors across the energy spectrum [22].
CT Imaging Simulation Validation Protocol
The validation of CT imaging simulations follows a comprehensive approach using standardized phantoms:
Phantom Configuration: The Catphan CTP404 phantom is used, containing modules with various material inserts (Teflon, Delrin, Acrylic, Polystyrene, LDPE, PMP, and Air) spanning a range of electron densities and atomic numbers [83].
Imaging Protocol: Scans are performed using a clinical PET/CT system (Siemens Biograph Horizon) with standardized clinical protocols. Both high (110 keV) and low (80 keV) energy settings are used, both with 2.5 mm Al filtration [83].
Simulation Approach: GATE models the CT system components including X-ray source, detector, and phantom geometry via modular macro files. Simulations typically run 100,000 particles to balance computational efficiency and statistical precision [83].
Validation Metrics: The primary validation metric is Hounsfield Unit (HU) accuracy for each material type, calculated by comparing simulated values against experimental measurements. Additional metrics include dose distribution and energy deposition patterns [83].
Monte Carlo Model Validation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials and Computational Tools for Validation Experiments
| Category | Specific Item | Function in Validation | Example Applications |
|---|---|---|---|
| Validation Phantoms | Catphan CTP404 [83] | Provides standardized materials with known properties for imaging system validation | CT imaging simulation validation |
| Homogeneous HDPE and gel-water phantoms [9] | Enables measurement of proton range and activity distributions in controlled media | Proton therapy range verification | |
| Ballistic gel tissue substitutes [22] | Simulates physical characteristics of human tissue for attenuation measurements | Linear attenuation coefficient studies | |
| Radioactive Sources | Ra-226 source [22] | Provides multiple photon energies for attenuation measurements across a broad spectrum | Linear attenuation coefficient validation |
| Positron-emitting isotopes (¹¹C, ¹⁵O, ¹³N) [9] | Created during proton irradiation for activity distribution measurement | In-beam PET range verification | |
| Detection Systems | Dual-head PET with BGO crystals [9] | Detects coincident gamma rays from positron annihilation | Proton range verification via PET |
| NaI(Tl) detector with lead shielding [22] | Measures photon transmission through tissue samples | Attenuation coefficient measurement | |
| Computational Tools | GATE/GEANT4 [9] [83] | Simulates particle transport and interactions in complex geometries | General-purpose MC simulation |
| PHITS [22] | Handles particle transport across wide energy ranges | Specialized for radiation transport | |
| Reference Data | NIST XCOM database [22] | Provides theoretical photon cross-section values | Gold standard for attenuation |
| EXFOR nuclear data library [9] | Contains experimental nuclear reaction cross-sections | Nuclear model validation |
The materials and tools summarized in Table 3 represent the essential components for establishing validation frameworks in Monte Carlo research. Phantom selection is particularly critical, as different applications require different validation geometries—from simple homogeneous blocks for fundamental measurements to complex anthropomorphic designs for clinical realism.
The choice of Monte Carlo platform should align with the specific application, with GATE/GEANT4 offering particular strengths for medical imaging simulations [9] [83], while PHITS provides specialized capabilities for radiation transport studies [22]. Access to authoritative reference databases like NIST XCOM and EXFOR is indispensable for proper validation, serving as the gold standard against which computational results are compared.
The establishment of gold standards through rigorous benchmarking against experimental and theoretical data remains fundamental to advancing Monte Carlo simulations in biomedical research. Our comparison of validation methodologies across multiple domains reveals that while specific protocols differ by application, the core principles of systematic comparison, quantitative discrepancy analysis, and iterative refinement remain constant.
The most successful validation frameworks incorporate multiple reference standards—combining experimental measurements with theoretical databases—to provide comprehensive assessment of model performance. Furthermore, the emergence of automated tools like PHASE for anatomical model generation demonstrates how validation protocols themselves are evolving to address new research challenges [84].
As Monte Carlo methods continue to expand their role in biomedical research and clinical applications, the development of more sophisticated validation frameworks will be essential. Future directions will likely include increased standardization of validation protocols, multi-institutional benchmarking initiatives, and the development of specialized validation phantoms for emerging technologies. Through continued refinement of these gold standards, the scientific community can enhance the reliability and impact of computational modeling in advancing human health.
Validating computational models against experimental data is a critical step in biomedical research, particularly when developing tools for therapeutic applications. This guide objectively compares two pivotal quantitative comparison techniques: Gamma Index Analysis and Statistical Testing. The context is the rigorous validation of Monte Carlo models against experimental tissue data, a common challenge in fields like radiotherapy treatment planning and optical tissue diagnostics. Gamma Index Analysis provides a spatially sensitive method for comparing dose or intensity distributions, commonly used in physical sciences. In parallel, traditional Statistical Testing offers a framework for inferring the significance of differences between datasets. For researchers and drug development professionals, understanding the strengths, applications, and limitations of each technique is essential for drawing reliable conclusions from complex biological and physical models. This guide details their methodologies, presents comparative data, and integrates them into a practical workflow for model validation.
Gamma Index Analysis
The Gamma Index (γ) is a robust, quantitative metric used to compare two-dimensional (2D) or three-dimensional (3D) dose or intensity distributions. It was designed to validate complex computational models and treatment plans against physical measurements in radiotherapy, and its use has expanded to other fields requiring spatial comparison [85]. The index simultaneously evaluates two critical parameters: Dose Difference (DD) and Distance to Agreement (DTA). By combining these into a single value, it provides a more comprehensive assessment than either measure alone. A γ value of ≤ 1 indicates that the comparison point passes the pre-defined criteria, signifying acceptable agreement between the measured and computed distributions [85] [86]. Common clinical standards for these criteria are 3% for DD and 3 mm for DTA for photon beams, with a 90% passing rate often considered acceptable [85].
Experimental Protocol for Model Validation
The following protocol, adapted from clinical quality assurance procedures, can be employed to validate a Monte Carlo model using Gamma Index Analysis [85].
Equipment and Materials:
- Computational Model: The Monte Carlo model to be validated (e.g., simulating light propagation in tissue or radiation dose deposition).
- Experimental Setup: A calibrated detector (e.g., a diode array like the PTW Octavius Detector 1500) embedded in a tissue-equivalent phantom.
- Data Acquisition System: Software to record measured data (e.g., VeriSoft).
- Treatment Planning System (TPS) or Equivalent: Software that houses the reference dataset generated by the computational model.
Procedure:
- Phantom Commissioning: The measurement phantom (e.g., Octavius 4D) must be commissioned for the specific experimental setup. This involves measuring percentage depth dose (PDD) for various field sizes and performing absolute dose calibration against a reference ionization chamber [85].
- Data Generation:
- Experimental Data: Place the phantom in the experimental setup (e.g., on a linac couch or optical bench). Deliver the treatment plan or expose the phantom to the relevant energy source. Acquire the measured dose/intensity distribution.
- Model Data: Use the Monte Carlo model to compute the expected dose/intensity distribution for the identical setup. Recalculate this distribution on the CT scan of the phantom to create the verification plan [85].
- Data Comparison: Import both the measured dataset and the model-predicted dataset into the analysis software.
- Gamma Index Calculation: In the software (e.g., VeriSoft), set the acceptance criteria (e.g., 3%/3mm). The analysis involves a search in the measured data for points that satisfy both the dose difference and distance-to-agreement criteria for each point in the model data [86]. The calculation can be performed in 2D, 3D, or volumetrically, and using either local or global normalization [85].
- Result Interpretation: The primary output is the percentage of points that have γ ≤ 1. A passing rate of ≥ 90% with 3%/3mm criteria is often considered clinically acceptable for radiotherapy, though the threshold may vary based on the required stringency for the specific model [85].
Key Research Reagent Solutions
The following table details essential materials and their functions for conducting Gamma Index Analysis.
| Item | Function in Experiment |
|---|---|
| Ionization Chamber (e.g., PTW semiflex 0.125 cc) | Provides absolute dose calibration for cross-checking detector array measurements and validating model output [85]. |
| Tissue-Equivalent Phantom (e.g., Octavius 4D) | Mimics the radiation absorption and scattering properties of human tissue, providing a realistic medium for experimental measurements [85]. |
| 2D Detector Array (e.g., PTW Detector 1500) | A high-resolution grid of ionization chambers (e.g., 1405 chambers) that measures a full 2D dose/intensity distribution simultaneously [85]. |
| Analysis Software (e.g., VeriSoft) | Computes the Gamma Index by comparing the measured and model-predicted datasets, applying the user-defined DD and DTA criteria [85]. |
Performance and Comparative Data
Gamma Index performance can vary based on analysis type and anatomical region. The following table summarizes findings from an institutional study [85].
| Analysis Type | Average Gamma Passing Rate (%) | Key Contextual Factor |
|---|---|---|
| Global 3D (Coronal) | 96.73 ± 2.35 [85] | Considered less stringent than local gamma [85]. |
| Global 3D (Transverse) | 93.36 ± 4.87 [85] | Performance can be axis-dependent [85]. |
| Local 2D | 78.23 ± 5.44 [85] | Considered more stringent than global gamma [85]. |
| Local 3D | 84.99 ± 4.24 [85] | More stringent than global 3D analysis [85]. |
Statistical Testing for Comparative Analysis
Statistical testing forms the backbone of inferential data analysis, allowing researchers to make objective decisions about their hypotheses. The core principle is to determine whether observed differences between groups or relationships between variables are statistically significant or likely due to random chance [87]. This process involves calculating a test statistic and a p-value. The p-value estimates the probability of obtaining the observed results if the null hypothesis (often stating no difference or no effect) were true. A p-value below a pre-determined threshold (the alpha value, commonly 0.05) leads to the rejection of the null hypothesis [87]. The choice of test depends on the research question, the type of data, the number of groups, and whether the data meets certain assumptions (e.g., normality, homogeneity of variance) [88].
Key Test Types and Selection Protocol
Selecting the correct statistical test is crucial for valid interpretation of experimental data from model validation studies [88].
Comparison Tests: Used to detect differences between group means.
- T-tests: Compare the means of precisely two groups. An independent (unpaired) t-test is for different populations (e.g., model output vs. experimental data from different samples), while a paired t-test is for the same subjects or populations measured under two conditions (e.g., the same phantom measured and then simulated) [87] [89].
- Analysis of Variance (ANOVA): Compares the means of three or more groups. A one-way ANOVA is used with one independent variable, while a two-way ANOVA assesses two independent variables [87] [89]. ANOVA will indicate if a significant difference exists somewhere among the groups but will not specify where. For this, post-hoc tests like Tukey's test (conservative) or Dunnett's test (when comparing all groups to a single control) are required [89].
Correlation Tests: Assess the strength and direction of a relationship between two continuous variables without implying causation.
Agreement Tests: Essential for model validation, as they assess how well two measurement techniques agree, which is a different question than whether they are correlated.
- Bland-Altman Plot: A graphical method to plot the difference between two measurements against their mean, highlighting any systematic bias and the limits of agreement [88].
- Intraclass Correlation Coefficient (ICC): A quantitative measure of reliability for numerical data from multiple observers or measurements [88].
Experimental Protocol for Statistical Validation
A generalized protocol for using statistical tests to validate a Monte Carlo model against experimental tissue data is as follows.
Step 1: Formulate the Hypothesis
- Null Hypothesis (H₀): There is no significant difference between the values predicted by the Monte Carlo model and the experimental measurements.
- Alternative Hypothesis (H₁): There is a significant difference between the model predictions and the experimental measurements.
Step 2: Characterize Your Data
- Type of Data: Determine if your data is continuous (e.g., dose value, oxygen saturation) or categorical.
- Check Assumptions:
- Normality: Use histograms, Q-Q plots, or statistical tests (e.g., Kolmogorov-Smirnov) to check if the residuals are normally distributed [87] [89].
- Homogeneity of Variance: Use an F-test or Levene's test to check if variances between groups are similar [89].
- Independence: Ensure data points are not influenced by each other.
Step 3: Select the Appropriate Test
- Refer to the flowchart in Section 3.4. For example, to compare the mean dose in a specific region of interest from a model versus an experiment, an independent t-test would be appropriate. To compare multiple regions simultaneously, a one-way ANOVA followed by a post-hoc test would be required.
Step 4: Run the Test and Interpret Results
- Calculate the test statistic and the p-value.
- If p < 0.05, reject the null hypothesis, suggesting a statistically significant difference between the model and experiment.
- If p ≥ 0.05, there is not enough evidence to reject the null hypothesis, indicating no statistically significant difference was detected.
Visualization of Statistical Test Selection
The diagram below outlines the decision-making process for choosing the correct statistical test for model validation.
Statistical Test Selection Flowchart
Integrated Workflow for Model Validation
The most robust model validation integrates both Gamma Index Analysis and Statistical Testing to leverage their complementary strengths. The Gamma Index provides a spatially resolved, pass/fail map of discrepancies, while statistical tests quantify the significance and magnitude of overall differences and agreements. The following workflow visualizes how these techniques can be combined to validate a Monte Carlo model against experimental tissue data.
Integrated Model Validation Workflow
Gamma Index Analysis and Statistical Testing are powerful, complementary techniques for the quantitative validation of Monte Carlo models against experimental tissue data. The Gamma Index excels in providing a spatially resolved, stringent assessment of agreement, making it indispensable for evaluating complex distributions in radiotherapy and optical tissue diagnostics. Statistical testing, with its diverse array of methods, is essential for making objective inferences about the significance of observed differences and the strength of relationships. For a robust validation framework, researchers should not choose one over the other but should integrate both. The combined workflow allows for a comprehensive assessment: the Gamma Index pinpoints where discrepancies occur, and statistical tests determine if those discrepancies are significant and quantify their magnitude. This multi-faceted approach provides the highest level of confidence for researchers and drug development professionals relying on the predictive accuracy of their computational models.
The validation of Monte Carlo (MC) simulation tools against experimental data is a critical step in advancing reliable computational models for radiation transport, a core aspect of thesis research in medical physics and radiation dosimetry. This case study objectively compares the performance of two prominent MC codes, MCNP6 and GEANT4, in modeling the gamma-ray shielding properties of a poly(methyl methacrylate) (PMMA) composite reinforced with mercury oxide (HgO). The analysis is grounded in experimental data, providing a concrete framework for evaluating the accuracy and reliability of these computational tools in a context relevant to tissue substitute research and shielding design [27].
Experimental Protocol and Material Synthesis
Composite Material Preparation
The PMMA-HgO composite was synthesized using a solution casting method to ensure a uniform dispersion of the filler within the polymer matrix [27] [90]. The procedural workflow is summarized in the diagram below:
Material Characterization: The structural integrity and morphology of the resulting composites were confirmed using X-ray diffraction (XRD) and Field Emission Scanning Electron Microscopy (FESEM). XRD analysis verified the retention of HgO's crystalline structure within the amorphous PMMA polymer, while FESEM micrographs demonstrated a uniform distribution of HgO particles with no significant agglomeration, indicating successful fabrication [27].
Gamma Shielding Measurement Setup
The experimental evaluation of shielding performance employed a 137Cs radioactive source, which emits gamma rays at a energy of 662 keV [27] [21]. The experimental setup is detailed in the diagram below:
The shielding parameters, including the linear attenuation coefficient (LAC), were derived from transmission measurements governed by the Beer-Lambert law: I = I₀e^(-μx), where I₀ and I are the incident and transmitted intensities, respectively, μ is the LAC, and x is the material thickness [40] [90].
Performance Comparison: MCNP6 vs. GEANT4 vs. Experiment
This section provides a objective comparison of the results obtained from experimental measurements and Monte Carlo simulations using MCNP6 and GEANT4.
Key Shielding Parameters at 662 keV
The following table summarizes the quantitative data for a PMMA-HgO composite with 10 wt% filler loading, offering a direct comparison of the outputs from the two simulation codes against experimental benchmarks [27].
Table 1: Comparison of Key Shielding Parameters for PMMA with 10 wt% HgO
| Shielding Parameter | Experimental Result | MCNP6 Simulation | GEANT4 Simulation | Discrepancy from Experiment |
|---|---|---|---|---|
| Linear Attenuation Coefficient, μ (cm⁻¹) | 0.096 | ~0.096 | ~0.096 | < 5% for both codes |
| Half-Value Layer, HVL (cm) | 7.19 | ~7.22 | ~7.22 | < 5% for both codes |
| Effective Atomic Number, Zₑₕᵻ | 4.1 | 4.1 | 4.1 | ~0% |
Comparative Analysis of Code Performance
Both MCNP6 and GEANT4 demonstrated excellent agreement with experimental results, with reported discrepancies consistently under 5% for key parameters like the linear attenuation coefficient (LAC) and half-value layer (HVL) [27]. This close alignment validates the reliability of the underlying physics models and cross-section data used by both codes for simulating gamma-ray interactions in composite materials at 662 keV.
- MCNP6: Noted for its high accuracy in neutron and photon transport, MCNP6 is often the preferred tool for shielding, dosimetry, and reactor calculations. Its strength lies in the use of established nuclear data libraries, which contribute to its precision in these applications [27].
- GEANT4: Praised for its superior flexibility and detailed geometry handling, GEANT4 is well-suited for complex simulations in detector design, medical physics, and space radiation studies. Its model-based approach offers great versatility, though it may be slightly less accurate than MCNP6 in specific nuclear engineering contexts [27].
The Scientist's Toolkit: Essential Research Materials
The following table catalogs the key reagents, materials, and software tools essential for research involving the development and validation of polymer composites for radiation shielding.
Table 2: Essential Research Reagents and Solutions for Shielding Composite Studies
| Research Reagent / Tool | Function and Application in Research |
|---|---|
| Poly(Methyl Methacrylate) (PMMA) | A transparent thermoplastic polymer serving as the lightweight, durable base matrix for the shielding composite [27] [90]. |
| Mercury Oxide (HgO) Powder | A high-atomic number (Z=80) filler material that enhances gamma-ray attenuation via photoelectric absorption [27] [21]. |
| Dichloromethane (CH₂Cl₂) | A solvent used in the solution casting method to dissolve PMMA resin, facilitating the incorporation and uniform dispersion of HgO filler [27]. |
| 137Cs Radioactive Source | A standardized gamma-ray source (662 keV) used for experimental evaluation of shielding performance [27] [21]. |
| NaI(Tl) Scintillation Detector | A radiation detector used in conjunction with a spectrometer to measure the intensity of gamma photons before and after passing through a test sample [27] [40]. |
| MCNP6 & GEANT4 Codes | Monte Carlo particle transport codes used to simulate radiation interactions with matter and computationally predict shielding parameters [27] [21]. |
| Phy-X/PSD & XCOM | Online databases and software tools used to calculate theoretical values of photon interaction cross-sections and attenuation coefficients for validation purposes [27] [21]. |
This case study demonstrates that both MCNP6 and GEANT4 are highly capable tools for simulating the gamma-ray shielding properties of PMMA-HgO composites, showing excellent agreement with experimental data. The choice between them can be guided by the specific research needs: MCNP6 is often favored for its high precision in nuclear applications, while GEANT4 offers unparalleled flexibility for modeling complex geometries. For thesis research focused on validating Monte Carlo models with experimental data, this work underscores the importance of a rigorous, multi-method approach. It provides a validated framework that can be extended to the study of other tissue-equivalent materials or novel composite shields, strengthening the link between computational prediction and experimental reality.
Proton therapy offers a significant advantage in radiation oncology due to the characteristic Bragg peak, which allows for highly conformal dose delivery to tumors while sparing surrounding healthy tissues. However, the full potential of this technique is limited by uncertainties in predicting the proton range within the patient. Even minor inaccuracies can lead to under-dosing the target volume or overdosing critical adjacent structures. Therefore, rigorous range verification methods are an essential component of quality assurance in proton therapy [9]. This case study examines the experimental validation of a Monte Carlo (MC) simulation model for proton range verification, focusing on its performance in two distinct phantom materials: a gel-water phantom and a high-density polyethylene (HDPE) phantom. The research is situated within the broader thesis that validating MC models with experimental tissue-equivalent data is crucial for advancing the accuracy and clinical reliability of proton therapy [9] [91].
Experimental Protocols and Methodologies
Phantom Configurations and Irradiation
The core of the experiment involved irradiating two different phantoms with proton beams and using an in-beam dual-head positron emission tomography (DHPET) system to image the resulting activity [9].
- Gel-Water Phantom: This phantom is designed to mimic the composition of human soft tissue, particularly its oxygen and water content. It is considered a more anthropomorphic material for experimental validation [9].
- HDPE Phantom: Composed of high-density polyethylene, this phantom is carbon-rich and lacks the oxygen content found in biological tissues. It serves as a well-understood material for initial benchmarking of the simulation models [9] [92].
- Beam Delivery: The phantoms were irradiated with monoenergetic proton beams. The experiments were conducted at the Kaohsiung Chang Gung Memorial Hospital (KCGMH) in Taiwan, using a DHPET system mounted on the rotating gantry port within the treatment room [9].
PET Image Acquisition and Data Processing
After irradiation, the induced positron-emitting isotopes (such as 11C, 15O, and 13N) were imaged.
- Imaging System: A dual-head PET (DHPET) system with BGO (Bismuth Germanate) crystals was used for in-beam data acquisition. This configuration allows for imaging shortly after irradiation, minimizing the impact of biological washout on the activity distribution [9].
- Data Analysis: The acquired PET data was used to reconstruct activity depth profiles. The primary metric for range verification was the distal activity fall-off, which was compared against the simulated fall-off from the Monte Carlo models [9].
Monte Carlo Simulation Framework
The GATE (Geant4 Application for Tomographic Emission) simulation platform was used to model the entire process [9].
- Simulation Scope: The MC workflow simulated proton beam delivery, the production of β+ isotopes within the phantom geometries, isotope decay, photon transport to the PET detectors, and the reconstruction of PET images.
- Compared Nuclear Models: The study critically evaluated the accuracy of three different nuclear reaction models for predicting activity:
- QGSP_BIC: The built-in theoretical hadronic physics model within GEANT4.
- EXFOR-based: A model incorporating experimentally measured cross-section data from the EXFOR library.
- NDS (New Dataset): An updated cross-section dataset provided by Rodríguez-González et al. (2022, 2023), which is optimized for PET-based proton range verification [9].
The diagram below illustrates the integrated workflow of the experiment and simulation.
Experimental and Simulation Workflow
Comparative Performance Data
The following tables summarize the key quantitative findings from the case study, comparing the performance of different nuclear models against experimental measurements in the two phantom types.
Table 1: Comparison of Mean Range Deviations for Different Nuclear Models
| Nuclear Model | HDPE Phantom (Mean Range Deviation) | Gel-Water Phantom (Mean Range Deviation) |
|---|---|---|
| QGSP_BIC | Underestimation by 2–4 mm | Underestimation by 1–2 mm |
| EXFOR-based | Within 1 mm | Underestimation by 1–2 mm |
| NDS (New Dataset) | Within 1 mm | Within 1 mm |
Source: Adapted from [9]
Table 2: Summary of Model Performance in Different Phantom Materials
| Phantom Material | Composition | Optimal Nuclear Model | Key Finding |
|---|---|---|---|
| HDPE | Carbon-rich, no oxygen | EXFOR-based and NDS | Both models achieved high accuracy, with range deviations within 1 mm [9]. |
| Gel-Water | Oxygen-rich, tissue-equivalent | NDS (New Dataset) | The updated NDS model provided the best match to experimental data, with range deviations within 1 mm [9]. |
The data demonstrates that the NDS model consistently delivered superior performance across both phantom types, achieving the highest agreement with experimental measurements. In contrast, the theoretical QGSP_BIC model showed a systematic underestimation of the proton range. The performance of the EXFOR-based model was material-dependent, excelling in HDPE but showing slight inaccuracies in the more clinically relevant gel-water phantom [9].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful replication of this study requires specific materials and tools. The table below lists key solutions used in the featured experiments.
Table 3: Key Reagents and Materials for Proton Range Verification Experiments
| Item | Function in the Experiment | Specification / Notes |
|---|---|---|
| Gel-Water Phantom | Mimics radiological properties of human soft tissue for anthropomorphic validation [9]. | Oxygen-rich composition; density ~1.01-1.13 g/cm³ [9] [92]. |
| HDPE Phantom | Provides a carbon-rich, well-characterized material for initial model benchmarking [9] [92]. | Density ~0.95 g/cm³; composition: 85.7% Carbon, 14.3% Hydrogen [92]. |
| In-Beam DHPET System | Enables imaging of positron-emitting isotopes immediately after proton irradiation [9]. | Utilizes BGO (Bi₄Ge₃O₁₂) detector crystals; mounted on gantry [9]. |
| GATE/GEANT4 MC Toolkit | Simulates the full chain of physics processes from proton interaction to PET image formation [9]. | Open-source platform; allows integration of different cross-section datasets [9]. |
| PAGAT Gel Dosimeter | An alternative polymer gel for 3D dose and beam profile characterization [93]. | Requires MRI or optical readout; shows quenching effect at the Bragg peak [93]. |
Nuclear Model Decision Pathway
The choice of nuclear cross-section model is critical for accurate MC prediction. The following diagram outlines a logical decision pathway for researchers based on the findings of this case study.
Nuclear Model Selection Guide
This case study demonstrates that the experimental validation of Monte Carlo models using tissue-equivalent phantoms is a critical step for improving the accuracy of proton range verification. The key finding is that the accuracy of nuclear reaction cross-section data is paramount; while standard theoretical models like QGSP_BIC exhibit significant range underestimation, data-driven models like NDS provide superior performance, especially in clinically relevant, oxygen-rich tissues. The systematic comparison in HDPE and gel-water phantoms underscores that model performance is highly material-dependent. For researchers, this implies that validation protocols must incorporate a range of tissue-equivalent materials to ensure clinical applicability. These findings strongly support the broader thesis that advancing proton therapy hinges on the continuous refinement and experimental benchmarking of Monte Carlo simulations against reliable experimental data.
Comparative Analysis of Different Monte Carlo Codes and Physics Models
Monte Carlo (MC) simulation techniques are indispensable in computational physics, providing a stochastic approach to modeling complex particle transport and interactions. In biomedical research, particularly in radiation therapy and dosimetry, the accuracy of these simulations directly impacts treatment planning efficacy and patient outcomes. This guide presents a comparative analysis of prominent Monte Carlo codes and their underlying physics models, framed within the critical context of validation against experimental tissue data. As these computational tools evolve to incorporate newer research findings, continuous benchmarking against empirical measurements becomes essential to ensure their reliability in clinical and research applications. This analysis synthesizes findings from recent benchmarking studies to objectively evaluate performance, identify limitations, and provide evidence-based recommendations for researchers and drug development professionals engaged in simulating biological effects of radiation.
Comparative Performance of Monte Carlo Codes
Code-Specific Architectures and Physics Models
Modern Monte Carlo codes for biomedical applications employ diverse computational architectures and physics models to balance calculation speed with physical accuracy.
GPU vs. CPU Architectures: Fast Monte Carlo codes leverage different hardware architectures to accelerate dose calculations. Codes like MOQUI and FRED utilize Graphics Processing Units (GPUs), enabling massive parallelization that significantly reduces computation time for complex simulations [43]. In contrast, MCsquare is designed for many-core Central Processing Unit (CPU) architectures, offering high performance on standard computing clusters [43]. This architectural difference impacts both implementation logistics and computational performance in research settings.
Physics Model Implementations: Variations in physics model implementations substantially influence simulation outcomes:
Electron Transport: Codes specializing in liquid water simulations, including Geant4-DNA, PHITS-TS, RITRACKS, NASIC, and PARTRAC, employ similar electron transport methodologies but diverge in cross-section models and datasets [94]. These differences become particularly pronounced at low energies (<100 eV), where statistical dispersion can exceed 70% relative standard deviation between codes [94].
Proton Therapy: For proton transport simulation, codes implement different modeling approaches for critical interactions. MCsquare uses a Gaussian distribution with Bohr relativistic correction for energy straggling and Rossi-Greisen variance for multiple Coulomb scattering [43]. MOQUI bases its cross-section data on Geant4 v10.6.p03, while FRED offers configurable scattering models, including single Gaussian and double Gaussian approximations with Rutherford correction [43].
Table 1: Architecture and Physics Models of Fast Monte Carlo Codes for Proton Therapy
| Code | Computational Architecture | Energy Straggling Model | Multiple Coulomb Scattering Model | Nuclear Interaction Data Source |
|---|---|---|---|---|
| MCsquare | Many-core CPU | Gaussian distribution with Bohr relativistic correction | Gaussian distribution with Rossi-Greisen variance using random hinge method | ICRU Report 63 |
| MOQUI | Single GPU | Gaussian perturbation with Bohr formula | Gaussian distribution with Rossi-Greisen variance | Geant4 QGSPBERTHP physics list |
| FRED | Multi-core CPU or Single/Multiple GPU | Landau-Vavilov for thin absorbers, Gaussian for thick absorbers | User-selectable: Single Gaussian or Double Gaussian with Rutherford correction | ICRU Report 63 with Fippel and Soukup model |
Quantitative Performance Benchmarking
Recent comparative studies provide quantitative metrics for evaluating Monte Carlo code performance across various biomedical applications.
Proton Therapy Dose Calculation: A 2025 comparative study of fast Monte Carlo codes for proton therapy evaluated performance using gamma pass rates (GPRs) when compared to treatment planning system calculations. The study analyzed 70 patient cases across multiple treatment sites (head and neck, brain, esophagus, lung, mediastinum, spine, and prostate) [43]. Results demonstrated that all commissioned codes achieved clinically acceptable 3D GPRs, ranging from 96.29% to 99.99% across all treatment sites [43]. Specifically, codes using single Gaussian models (typical of GPU implementations) achieved GPRs from 96.29% to 99.34%, while the double Gaussian model (typically CPU-based) achieved a superior range of 98.68% to 99.99% [43].
Low-Energy Electron Transport: A 2025 NASA-funded study revealed significant discrepancies among specialized Monte Carlo codes simulating electron interactions in liquid water, particularly at biologically relevant low energies [94]. For energies above approximately 1 keV, the relative standard deviation among codes averaged between 5-25%, with maximum relative differences of 20-100% [94]. Below 100 eV, these discrepancies increased substantially, with relative standard deviation reaching approximately 70% and maximum relative differences up to 700% [94]. This performance variation at low energies has crucial implications for simulating DNA damage, where such electrons play a key role.
Table 2: Performance Benchmarking of Monte Carlo Codes Across Applications
| Application Domain | Evaluated Codes | Performance Metric | Results | Energy Range |
|---|---|---|---|---|
| Proton Therapy | MCsquare, MOQUI, FRED | 3D Gamma Pass Rate vs. TPS | 96.29% - 99.99% | Clinical proton energies |
| Electron Transport in Water | Geant4-DNA, PHITS-TS, RITRACKS, NASIC, PARTRAC | Relative Standard Deviation | 5-25% (above 1 keV), up to ~70% (below 100 eV) | 20 eV - 100 keV |
| Electron Backscattering | G4EmPenelopePhysics, G4EmLivermorePhysics, G4EmStandardPhysicsoption3, G4EmStandardPhysicsoption4 | Significant differences in bremsstrahlung modeling | Differences observed between Penelope and other constructors | Clinical x-ray energies |
Geant4 Physics Constructors and Validation
The Geant4 toolkit offers multiple physics constructors specializing in different interaction models, with performance varying significantly across applications.
Electromagnetic Physics Constructors: The G4-Med benchmarking system, developed by the Geant4 Medical Simulation Group, evaluates various electromagnetic physics constructors for biomedical applications [95]. Their 2025 analysis revealed that parameters for multiple scattering in the G4EmStandardPhysicsoption3 constructor in Geant4 11.1, while improving electron backscattering modeling in high-atomic-number targets, proved inadequate for dosimetry of clinical x-ray and electron beams [95]. Consequently, these parameters were reverted to Geant4 10.5 values in version 11.2.1 [95]. Additionally, significant differences were observed in bremsstrahlung process modeling, particularly between G4EmPenelopePhysics and other constructors (G4EmLivermorePhysics, G4EmStandardPhysicsoption3, and G4EmStandardPhysics_option4) [95].
Hadronic Physics and Ion Therapy: For hadrontherapy applications, benchmarking studies show substantial improvements in Geant4 11.1 for modeling proton and carbon ion Bragg peaks at clinical energies, attributed to the adoption of ICRU90 for calculating low-energy proton stopping powers in water and implementation of the Linhard-Sorensen ion model [95]. Nuclear fragmentation tests relevant to carbon ion therapy revealed differences between Geant4 10.5 and 11.1, with the latter showing higher production of boron fragments, leading to better agreement with reference data [95].
Experimental Protocols and Validation Methodologies
Benchmarking Frameworks and Test Suites
Robust benchmarking frameworks are essential for standardized validation of Monte Carlo codes against experimental data.
G4-Med Benchmarking System: The G4-Med benchmarking suite, established in 2014 and continuously expanded, currently includes 23 tests that evaluate Geant4 from fundamental physical quantities to clinically relevant setups [95]. This comprehensive system categorizes tests into electromagnetic physics tests, hadronic nuclear cross-section tests, combined electromagnetic and hadronic physics tests, and Geant4-DNA tests [95]. New tests introduced since 2021 include benchmarking of Geant4-DNA physics and chemistry components, dosimetry for brachytherapy with sources, dosimetry for external x-ray and electron FLASH radiotherapy, experimental microdosimetry for proton therapy, and in vivo PET for carbon and oxygen beams [95].
Liquid Water Electron Transport Studies: The 2025 intercomparison of low-energy electron transport codes employed standardized calculations of electronic stopping power, pathlength and absorption ranges, dose-point kernels, and frequency-mean and dose-mean lineal energy for electron energies from 20 eV to 100 keV [94]. The uncertainty of each calculated quantity was evaluated using relative standard deviation and maximum relative difference, with ICRU Report 90 data used to benchmark medium- to high-energy code performance [94].
Clinical Validation Protocols
Clinical validation of Monte Carlo codes requires comparison with both experimental measurements and treatment planning systems.
Proton Beam Commissioning: In proton therapy validation studies, beam models are typically commissioned to match clinical beamlines. For example, in a 2025 comparative study, GPU codes utilized single 2D Gaussian models, while a CPU code employed a double 2D Gaussian model to model a clinical proton beamline at the University of Texas MD Anderson Cancer Center [43]. Validation included comparison with verification plans created in the clinical treatment planning system using 3D gamma analysis [43].
Code-Specific Validation Methods: Different codes implement distinct approaches for secondary particle handling and energy deposition:
MCsquare neglects secondary neutrons due to their minimal contribution to local dose deposition, produces but doesn't transport prompt gammas, locally deposits kinetic energy transferred to heavier recoil nuclei, and explicitly simulates other charged particles [43].
MOQUI locally deposits energy of electrons produced during simulation, neglects neutrons and photons, and explicitly simulates secondary protons similar to primary protons [43].
FRED only accounts for secondary protons and deuterons, depositing energy from all other interaction products locally [43].
Essential Research Tools and Reagents
The following research reagents and computational tools are essential for conducting Monte Carlo simulations and their experimental validation in biomedical research.
Table 3: Research Reagent Solutions for Monte Carlo Validation Studies
| Tool/Reagent | Function | Application Context |
|---|---|---|
| Geant4 Toolkit | Open-source Monte Carlo simulation toolkit for particle interactions and transport in matter | General-purpose medical physics simulations, including dosimetry and microdosimetry |
| Geant4-DNA Extension | Specialized physics models for low-energy interactions in liquid water | DNA damage studies, nanodosimetry, radiation chemistry |
| G4-Med Benchmarking Suite | Comprehensive test suite with 23 standardized tests for bio-medical physics | Validation of Geant4 physics models for medical applications |
| ICRU Report 90 Data | Reference data for electron and proton stopping powers | Benchmarking medium- to high-energy performance of Monte Carlo codes |
| Water Phantoms | Standardized medium for dosimetry measurements | Experimental validation of dose calculations in liquid water |
| Clinical Proton Beamline | Protons at energies of 62-67.5 MeV for bragg curve measurements | Hadrontherapy model validation, proton beam commissioning |
Workflow Visualization
The following diagram illustrates the logical workflow for benchmarking Monte Carlo codes against experimental data, as implemented in contemporary validation studies:
Monte Carlo Code Validation Workflow
Based on the comprehensive comparative analysis of Monte Carlo codes and physics models, the following evidence-based recommendations emerge for researchers and medical physicists:
Electromagnetic Physics Applications: For general electromagnetic physics simulations in biomedical contexts, G4EmStandardPhysics_option4 is recommended as the preferred electromagnetic constructor [95]. This recommendation is supported by comprehensive benchmarking through the G4-Med test suite, which evaluated performance across diverse scenarios from brachytherapy to megavoltage x-ray radiotherapy [95].
Hadrontherapy Applications: For proton and ion therapy simulations, the combination of QGSPBICHP physics list with G4EmStandardPhysics_option4 electromagnetic constructor provides optimal accuracy in modeling Bragg peaks and nuclear fragmentation processes [95]. This recommendation is substantiated by improved agreement with experimental Bragg peak measurements and fragment yield data in Geant4 11.1, attributable to the adoption of ICRU90 stopping powers and implementation of the Linhard-Sorensen ion model [95].
Code Selection Considerations: When selecting Monte Carlo implementations for specific clinical or research applications, researchers should consider the observed performance characteristics identified in comparative studies. For proton therapy dose calculation, all fast MC codes evaluated demonstrated clinically acceptable gamma pass rates (96.29%-99.99%), with double Gaussian models slightly outperforming single Gaussian implementations across most treatment sites [43]. For low-energy electron transport simulations, where significant inter-code discrepancies exist (particularly below 100 eV), researchers should exercise caution and consider multiple codes to estimate systematic uncertainties [94].
The continuous development and validation of Monte Carlo codes remain essential for advancing their application in biomedical research. The substantial differences observed among codes, especially at low energies, highlight the importance of experimental benchmarking and the need for further refinement of physics models to reduce uncertainties in critical applications such as DNA damage simulation and nanodosimetry.
Assessing the Impact of Tissue Heterogeneity and Anatomical Realism on Model Validity
Monte Carlo (MC) simulations have become the gold standard for modeling complex physical interactions in medical physics, particularly in radiation therapy and dosimetry [4] [96]. These stochastic methods provide unparalleled accuracy in simulating particle transport through biological tissues, making them indispensable for treatment planning and dose calculation [3]. However, the fundamental challenge facing all computational models lies in their faithful representation of real-world biological systems—specifically, how well they account for tissue heterogeneity and anatomical realism [6].
The validation of Monte Carlo models against experimental tissue data represents a critical frontier in biomedical research, bridging the gap between computational prediction and clinical application. As therapeutic technologies advance, the demand for models that accurately reflect the complex interplay of radiation with diverse biological structures has intensified [4]. This comparative guide examines current approaches to addressing tissue heterogeneity, evaluating their performance against experimental benchmarks, and identifying pathways toward more biologically faithful simulations.
Computational Approaches to Tissue Heterogeneity
Simplified Homogeneous Models
Traditional dose calculation algorithms often employ simplified geometry, representing anatomical structures as water-equivalent materials. This approach significantly reduces computational complexity but fails to capture the essential variations in tissue density and composition that significantly influence radiation transport [97]. For example, some analytical algorithms model all anatomical structures as water, with the exception of lungs which are represented as air-filled [97].
While these simplified models offer computational efficiency, their accuracy diminishes markedly in regions of high tissue heterogeneity. Experimental validations have demonstrated that such approaches can produce discrepancies exceeding 40% in out-of-field lung doses compared to measured data [97]. The primary limitation stems from inadequate accounting for differential scattering and absorption across tissue interfaces.
Advanced Heterogeneous Modeling
Modern Monte Carlo simulations address tissue heterogeneity by incorporating patient-specific anatomical data from CT or MRI imaging, creating voxelized geometries that preserve tissue density variations [3]. Advanced MC platforms like GATE/GEANT4, EGSnrc, and TOPAS enable precise modeling of particle interactions in complex, heterogeneous media by simulating radiation transport on a particle-by-particle basis [6] [3].
These platforms employ sophisticated physics lists that model fundamental interactions including photoelectric effect, Compton scattering, pair production, and radioactive decay processes [6]. The resulting simulations account for tissue-specific variations in radiation absorption and scattering, providing superior accuracy in dose calculations, particularly at tissue interfaces and in regions containing bone or air cavities [3].
Table 1: Major Monte Carlo Platforms for Modeling Tissue Heterogeneity
| Platform | Primary Applications | Tissue Modeling Capabilities | Computational Requirements |
|---|---|---|---|
| GATE/GEANT4 | Radionuclide therapy, PET/SPECT | Voxelized anatomical geometries, material composition definition | High (requires GPU acceleration) |
| EGSnrc | External beam radiotherapy, dosimetry | Accurate electron/photon transport in heterogeneous media | Moderate to High |
| TOPAS | Proton therapy, adaptive planning | Parameterized system for complex treatment geometries | High |
| FLUKA | Heavy ion therapy, shielding | Robust nuclear interaction models | High |
| MCNP | Neutron therapy, shielding | General particle transport in complex geometries | Moderate |
Experimental Validation Frameworks
Anthropomorphic Phantom Systems
Experimental validation of Monte Carlo models relies heavily on anthropomorphic phantoms that mimic human anatomy and tissue composition. These phantoms incorporate tissue-equivalent materials that replicate the radiological properties of actual human tissues [97]. For example, the ATOM phantom (CIRS) used in pediatric dose validation studies contains materials that simulate various tissue types and is pre-drilled at numerous positions for organ dosimetry using thermoluminescent detectors [97].
Recent advances have introduced 3D-printed phantoms using materials like Polylactic Acid (PLA) and Acrylonitrile Butadiene Styrene (ABS), which offer customizable anatomical geometries with tissue-equivalent properties [6]. PLA, with a physical density of 1.24 g/cm³, better represents high-density tissues, while ABS (density 1.04 g/cm³) is more suitable for simulating moderately low-density tissues [6].
Validation Metrics and Performance
The validity of Monte Carlo models is quantified through direct comparison between simulated and measured dose distributions. Performance is typically assessed using metrics such as percentage dose difference, gamma analysis, and statistical uncertainty measures [6] [97].
In experimental validations using anthropomorphic phantoms, advanced MC simulations consistently demonstrate superior performance compared to simplified algorithms. One comprehensive study evaluating out-of-field doses in pediatric radiotherapy found that MC simulations differed from experimental measurements by less than 20%, while analytical algorithms showed discrepancies up to 40% [97].
Table 2: Performance Comparison of Tissue Modeling Approaches
| Modeling Approach | Dose Accuracy in Homogeneous Tissue | Dose Accuracy in Heterogeneous Regions | Computational Efficiency | Experimental Validation Results |
|---|---|---|---|---|
| Analytical (Water-equivalent) | >95% (within field) | 60-80% (lung interfaces) | High | 40% discrepancy in lung doses [97] |
| Polymer 3D Printed Phantoms (PLA) | >95% (high-density tissues) | >95% (liver equivalents) | Medium | +5.6% DD difference in liver [6] |
| Polymer 3D Printed Phantoms (ABS) | 85-90% (high-density tissues) | >95% (lung equivalents) | Medium | -35.3% DD difference in lungs [6] |
| Advanced MC (GATE/GEANT4) | >99% | 95-98% | Low (without acceleration) | <20% discrepancy in out-of-field [97] |
| GPU-Accelerated MC | >99% | 95-98% | Medium to High | Up to 1000x speedup [4] |
Experimental Protocols for Model Validation
Protocol 1: Radionuclide Therapy Dosimetry
This protocol validates MC models for internal dosimetry in radionuclide therapy, particularly radioembolization for liver tumors [6]:
- Phantom Design: Construct anthropomorphic phantom representing average liver (220×140×80 mm) and lung volumes (left: 100×171×261 mm; right: 116×169×269 mm) with spherical tumor mimic (10 mm radius) in liver [6].
- Material Definition: Define tissue materials in the simulation with PLA (density: 1.24 g/cm³), ABS (density: 1.04 g/cm³), and true organ densities for comparison [6].
- Source Configuration: Incorporate radionuclides (Tc-99m for imaging: 1 mCi; Y-90 for treatment: 1 mCi) within tumor mimic [6].
- Dose Calculation: Implement DoseActor in GATE simulation to record energy deposition in 3D voxels (dosels) across defined volumes [6].
- Validation Metrics: Compute dose distribution differences (%) between simulated and experimental measurements for each tissue type [6].
Protocol 2: Out-of-Field Dose Assessment
This protocol validates MC models for assessing stray radiation in external beam radiotherapy, particularly relevant for secondary cancer risk evaluation [97]:
- Experimental Setup: Irradiate anthropomorphic phantom (e.g., ATOM representing 5-year-old child) with clinically relevant treatment plans (IMRT/VMAT) for brain tumor [97].
- Dosimetry System: Utilize thermoluminescent dosimeters (TLDs) such as natLiF:Mg,Cu,P (MCP-N) positioned at multiple locations within phantom [97].
- MC Simulation: Execute fast Monte Carlo code (e.g., PRIMO with 3×10⁹ histories) using actual chemical composition of phantom materials [97].
- Analysis: Compare simulated and measured doses across all TLD positions, with special attention to out-of-field regions and tissue interfaces [97].
- Uncertainty Quantification: Report statistical uncertainty (should not exceed 5% for out-of-field voxels) and experimental uncertainty (approximately 20% for TLD measurements) [97].
Model Validation Workflow: This diagram illustrates the comprehensive workflow for validating Monte Carlo models against experimental tissue data, encompassing anatomical realism, experimental measurement, computational simulation, and comparative validation phases.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials for Tissue Heterogeneity Research
| Item | Function | Application Context |
|---|---|---|
| Anthropomorphic Phantoms (ATOM) | Experimental dose measurement across anatomical locations | Benchmarking MC models in realistic geometries [97] |
| 3D Printing Filaments (PLA, ABS) | Customizable tissue-equivalent materials | Patient-specific phantom creation [6] |
| Thermoluminescent Dosimeters (TLDs) | Point dose measurements in phantoms | Experimental validation of simulated dose distributions [97] |
| GATE/GEANT4 MC Platform | Gold standard radiation transport simulation | Research-grade dose calculations in heterogeneous media [6] [3] |
| GPU Computing Clusters | Acceleration of MC simulations | Making high-fidelity simulations clinically feasible [4] |
| CT Imaging Data | Patient-specific anatomical geometry | Realistic tissue heterogeneity modeling [3] |
Performance Analysis and Discussion
Impact of Tissue Equivalency on Dose Accuracy
The choice of tissue-equivalent materials significantly influences model validity. Studies evaluating 3D-printed materials have demonstrated that PLA shows excellent agreement with real tissues for high-density organs like liver (+5.6% dose difference for Tc-99m, +1.7% for Y-90) [6]. In contrast, ABS better represents lung tissues but still shows substantial discrepancies (-35% to -41% dose differences), highlighting the challenge of accurately simulating low-density tissues [6].
The integration of patient-specific anatomical data from CT imaging has dramatically improved dose calculation accuracy in heterogeneous regions. Advanced MC models that incorporate these data can achieve accuracy exceeding 99% in homogeneous tissues and 95-98% in heterogeneous regions [3]. This represents a significant improvement over analytical algorithms, which may show accuracy reductions to 60-80% in heterogeneous regions like lung interfaces [97].
Computational Considerations
The primary limitation of advanced MC simulations remains their substantial computational demands. Traditional CPU-based implementations may require days or weeks for highly-precise simulations of complex anatomy [4]. However, GPU-based parallel computing has emerged as a transformative solution, providing speedup factors of 100-1000× over CPU implementations [4].
Recent innovations in AI-integrated MC simulations and variance reduction techniques further bridge the gap between accuracy and computational feasibility [3]. These hybrid approaches maintain the physical accuracy of MC methods while dramatically reducing computation time through deep learning-based surrogates for dose distribution predictions [3].
Material Selection Impact: This diagram illustrates the tissue equivalency decision process and performance outcomes for different phantom materials in Monte Carlo model validation, highlighting the trade-offs in material selection for specific tissue types.
The validity of Monte Carlo models in biomedical applications is inextricably linked to their treatment of tissue heterogeneity and anatomical realism. Advanced MC simulation platforms like GATE/GEANT4 consistently outperform simplified approaches, particularly in complex anatomical regions with significant density variations. The integration of realistic anatomical geometries from medical imaging, coupled with sophisticated radiation transport physics, enables dose calculation accuracy exceeding 95% even in challenging heterogeneous environments.
Experimental validation remains essential for establishing model credibility, with anthropomorphic phantoms and 3D-printed tissue equivalents providing critical benchmarks. While computational demands historically constrained MC implementation in clinical settings, GPU acceleration and AI-integrated approaches are rapidly overcoming these barriers. Future advancements will likely focus on improving tissue characterization methods, developing more accurate tissue-equivalent materials, and further reducing computational requirements through hybrid AI-MC frameworks. As these technologies mature, the gap between computational prediction and experimental reality will continue to narrow, ultimately enhancing treatment efficacy and patient safety across therapeutic applications.
Conclusion
The rigorous validation of Monte Carlo models with experimental tissue data is paramount for their credible application in biomedical research and clinical practice. This synthesis of foundational principles, methodological applications, optimization strategies, and validation protocols underscores a unified theme: accuracy and reliability are achieved through a continuous, iterative cycle of simulation and experimental benchmarking. The future of this field lies in harnessing advanced computing technologies like GPU acceleration and deep learning for greater speed and accessibility [citation:3][citation:6], developing more sophisticated and biologically realistic tissue models, and establishing standardized validation frameworks across institutions. These advancements will be crucial for improving treatment planning in radiation oncology, enhancing the safety of radiological procedures, developing next-generation medical devices, and ultimately, ensuring that computational predictions translate into tangible benefits for patient care.
References
- 1. Monte Carlo simulations: The Virtual Sandbox for Medical ... [https://bioemtech.com/science-letter/monte-carlo-simulations-the-virtual-sandbox-for-medical-physics/]
- 2. Scaling method for efficient Monte Carlo simulation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532332/]
- 3. Applications of Monte Carlo Simulations in Medical Physics [https://www.preprints.org/manuscript/202509.2179/v1]
- 4. Review of GPU-based Monte Carlo simulation platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394928/]
- 5. Deep learning-based prediction of Monte Carlo dose ... [https://www.sciencedirect.com/science/article/pii/S2405631625000405]
- 6. Investigation of the tissue equivalence of typical 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12209393/]
- 7. multi-parameter experimental validation of fluorescence ... [https://pubmed.ncbi.nlm.nih.gov/40443945/]
- 8. A proof-of-concept study of personalized dosimetry for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1600821/full]
- 9. Experimental validation of Monte Carlo simulation model ... [https://www.sciencedirect.com/science/article/abs/pii/S0969806X25007558]
- 10. A comparative analysis of GEANT4 , MCNP6 and FLUKA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12149693/]
- 11. Phantom studies in medical imaging (PSMI) - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583249/]
- 12. Characterization and evaluation of tissue-equivalent ... [https://www.sciencedirect.com/science/article/abs/pii/S0969806X25005262]
- 13. Tissue-Mimicking Material Fabrication and Properties for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11200625/]
- 14. Experimental Validation of an Analytical Program and a Monte ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9300838/]
- 15. Assessing radiological properties of novel tissue ... [https://www.sciencedirect.com/science/article/pii/S1738573325000932]
- 16. Comparison of X-Ray Absorption in Mandibular Tissues ... [https://www.mdpi.com/2076-3417/14/23/10879]
- 17. A Comparison Between GATE and MCNPX Monte Carlo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3967451/]
- 18. 2025 Planned Features - Geant4 - CERN [https://geant4.web.cern.ch/news/2025-03-11-planned-dev]
- 19. Geant4: A game changer in high energy physics and ... [https://www.sciencedirect.com/science/article/pii/S0167739X24002747]
- 20. A comparative analysis of GEANT4, MCNP6 and FLUKA ... [https://pubmed.ncbi.nlm.nih.gov/40066823/]
- 21. Experimental and simulation study of shielding features of ... [https://www.nature.com/articles/s41598-025-17942-x]
- 22. Modeling and validation of a system for measurement ... [https://pubmed.ncbi.nlm.nih.gov/40499323/]
- 23. Comparison of simulations with PHITS and HIBRAC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3941487/]
- 24. Development and validation of a Monte Carlo model of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12350822/]
- 25. Evaluating IMRT and VMAT dose accuracy - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8353583/]
- 26. Validation of Measurement Based Dose Volume Metrics for ... [http://clinmedjournals.org/articles/ijccr/international-journal-of-cancer-and-clinical-research-ijccr-3-070.php?jid=ijccr]
- 27. Comparative analysis of Monte Carlo simulations and ... [https://www.nature.com/articles/s41598-025-14223-5]
- 28. A normalized drug response metric improves accuracy and ... [https://www.nature.com/articles/s42003-020-0765-z]
- 29. - Monte simulation and Carlo - tissue for phantom of... model validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC9203094/]
- 30. EURADOS intercomparison exercise on MC modelling for ... [https://www.sciencedirect.com/science/article/abs/pii/S0969806X15001474]
- 31. -based inverse Monte for calculating Carlo optical... model tissue [https://opg.optica.org/ao/abstract.cfm?uri=ao-45-5-1062]
- 32. of Phantom for noncontact depth... validation Monte Carlo modeling [https://www.spiedigitallibrary.org/journals/JBO/volume-19/issue-08/085006/Phantom-validation-of-Monte-Carlo-modeling-for-noncontact-depth-sensitive/10.1117/1.JBO.19.8.085006.full]
- 33. Evaluation of an EPID in vivo monitoring system using local ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9797176/]
- 34. Range Verification Methods in Particle Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC4493660/]
- 35. Range uncertainties in proton therapy and the role of Monte ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3374500/]
- 36. Precise dose verification in proton therapy using Positron ... [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.1101/2025.08.02.25332864]
- 37. Range verification in proton therapy with computational ... [https://www.sciencedirect.com/science/article/pii/S0969806X25005882]
- 38. Monte Carlo simulation study of in-beam intra-treatment ... [https://mdanderson.elsevierpure.com/en/publications/monte-carlo-simulation-study-of-in-beam-intra-treatment-pet-imagi/]
- 39. Validation of GAMOS Monte Carlo simulation for 131 Cs ... [https://ui.adsabs.harvard.edu/abs/2025RaPC..22612268A/abstract]
- 40. Modeling and validation of a system for measurement ... [https://www.sciencedirect.com/science/article/abs/pii/S0969804325003215]
- 41. Deep learning-based prediction of Monte Carlo dose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11929889/]
- 42. Deep learning-based Monte Carlo dose prediction for ... [https://pubmed.ncbi.nlm.nih.gov/39871016/]
- 43. A comparative study of clinically used fast Monte Carlo dose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12457214/]
- 44. Validation of the MC-GPU Monte Carlo code against ... [https://www.sciencedirect.com/science/article/abs/pii/S1120179721000788]
- 45. A GPU-accelerated Monte Carlo dose engine for external ... [https://pubmed.ncbi.nlm.nih.gov/40438035/]
- 46. GPU-Accelerated Full Monte Carlo Affords Accurate Voxel ... [https://jnm.snmjournals.org/content/64/supplement_1/P989]
- 47. Optimizing dosimetry in Y-90 microsphere radioembolization [https://pmc.ncbi.nlm.nih.gov/articles/PMC12401777/]
- 48. GPU accelerated internal dose Monte Carlo simulation in ... [https://pubmed.ncbi.nlm.nih.gov/40205953/]
- 49. Clinical application of a GPU-accelerated monte carlo dose ... [https://ro-journal.biomedcentral.com/articles/10.1186/s13014-024-02446-1]
- 50. Novel Polymer Composites for Lead-Free Shielding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11014132/]
- 51. Neutron and gamma-ray shielding effectiveness of novel ... [https://www.sciencedirect.com/science/article/abs/pii/S0969806X24001671]
- 52. Fabrication of new tissue equivalent materials as brain ... [https://www.sciencedirect.com/science/article/abs/pii/S0167577X24020603]
- 53. Quantitative validation of Monte Carlo SPECT simulation [https://ejnmmiphys.springeropen.com/articles/10.1186/s40658-023-00581-4]
- 54. Hybrid Monte Carlo model for efficient tissue Cherenkov ... [https://www.sciencedirect.com/science/article/pii/S1120179725000663]
- 55. Hybrid Modeling [https://www.bosch-ai.com/research/fields-of-expertise/hybrid-modeling/]
- 56. Hybrid modeling design patterns [https://mathematicsinindustry.springeropen.com/articles/10.1186/s13362-024-00141-0]
- 57. Hybrid Monte Carlo model for efficient tissue Cherenkov ... [https://pubmed.ncbi.nlm.nih.gov/40088599/]
- 58. On-chip Cherenkov radiation tuning in 3.2-14 THz [https://www.nature.com/articles/s41467-025-63368-4]
- 59. First Event-by-Event Identification of Cherenkov Radiation ... [https://arxiv.org/html/2507.08886v3]
- 60. FullMonteCUDA: a fast, flexible, and accurate GPU ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6757465/]
- 61. From Games to Brains [https://www.mghpcc.org/from-games-to-brains/]
- 62. Graphics processing unit-accelerated mesh-based Monte ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6863969/]
- 63. DeepSMCP – Deep-learning powered denoising of Monte ... [https://www.sciencedirect.com/science/article/pii/S0939388925000340]
- 64. Development and validation of a Monte Carlo model ... [https://pubmed.ncbi.nlm.nih.gov/40804590/]
- 65. Elaboration and experimental validation of a Monte Carlo ... [https://www.sciencedirect.com/science/article/abs/pii/S0969806X22004911]
- 66. Methodological benchmarking of GATE and TOPAS for 6 ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2025.1671778/full]
- 67. Experimental validation of a linac head Geant4 model ... [https://impact.ornl.gov/en/publications/experimental-validation-of-a-linac-head-geant4-model-under-a-grid]
- 68. A Monte Carlo Study of Photon Beam Characteristics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7557471/]
- 69. Evaluation of tissue-air ratios (TAR) for various tissue- ... [https://www.sciencedirect.com/science/article/abs/pii/S1574181825000370]
- 70. 蒙特卡罗模拟中核反应截面数据库对AB-BNCT中子束品质 ... [https://www.ebiotrade.com/newsf/2025-8/20250812004836654.htm]
- 71. The comparison of theoretical model calculations and ... [https://www.sciencedirect.com/science/article/pii/S0168583X20303979]
- 72. Monte Carlo method [https://en.wikipedia.org/wiki/Monte_Carlo_method]
- 73. Evaluating the effect of higher Monte Carlo statistical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11405816/]
- 74. Development and Validation of Monte Carlo Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11988178/]
- 75. Tissues as networks of cells: towards generative rules of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10369035/]
- 76. Optimizing multiplexed imaging experimental design ... [https://www.nature.com/articles/s41592-022-01692-z]
- 77. Monte Carlo-based end-to-end approach for validation of ... [https://jnm.snmjournals.org/content/66/supplement_1/251808]
- 78. Monte Carlo tree search [https://en.wikipedia.org/wiki/Monte_Carlo_tree_search]
- 79. Monte Carlo Tree Search (MCTS) in Machine Learning [https://www.geeksforgeeks.org/machine-learning/monte-carlo-tree-search-mcts-in-machine-learning/]
- 80. A comprehensive benchmarking of adaptive sampling tools ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12442282/]
- 81. Re-evaluating experimental validation in the Big Data Era [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02292-4]
- 82. Identification and experimental validation of key genes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11402953/]
- 83. Validation of GATE-Based Monte Carlo Simulation for ... [https://www.sciencedirect.com/science/article/abs/pii/S0969806X25008564]
- 84. PHASE: Personalized Head-based Automatic Simulation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515100/]
- 85. Gamma Index Analysis as a Patient-Specific Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9626372/]
- 86. A comparison of the gamma index analysis in various ... [https://www.sciencedirect.com/science/article/abs/pii/S0167814013004593]
- 87. Choosing the Right Statistical Test | Types & Examples [https://www.scribbr.com/statistics/statistical-tests/]
- 88. Choosing the Correct Statistical Test - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8327789/]
- 89. Deep Dive: Statistical Tests (Comparisons) [https://blog.addgene.org/deep-dive-statistical-tests-comparisons]
- 90. PMMA reinforced with high-Z fillers for gamma radiation ... [https://www.sciencedirect.com/science/article/abs/pii/S003238612500686X]
- 91. Proton range verification in inhomogeneous tissue: Treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5837130/]
- 92. Feasibility study of using fall‐off gradients of early and late ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5462437/]
- 93. Suitability of Polyacrylamide-Based Dosimetric Gel for ... [https://www.mdpi.com/2310-2861/11/10/794]
- 94. Intercomparison of Low-Energy Electron Transport ... [https://ntrs.nasa.gov/citations/20250006356]
- 95. Results of a Geant4 benchmarking study for bio‐medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12059550/]
- 96. Monte Carlo Simulations of Particle Interactions with Tissue ... [https://www.sciencedirect.com/science/article/pii/S2331518023000410]
- 97. Experimental Validation of an Analytical Program and a ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.882506/full]