Monte Carlo Simulation for Light Propagation in Tissue: A Comprehensive Guide for Biomedical Research and Drug Development
This article provides a comprehensive exploration of Monte Carlo (MC) simulation for modeling light propagation in biological tissue, a gold-standard technique in biomedical optics.
Monte Carlo Simulation for Light Propagation in Tissue: A Comprehensive Guide for Biomedical Research and Drug Development
Abstract
This article provides a comprehensive exploration of Monte Carlo (MC) simulation for modeling light propagation in biological tissue, a gold-standard technique in biomedical optics. Tailored for researchers, scientists, and drug development professionals, it covers the foundational physics of light-tissue interactions and the core principles of the MC method. The scope extends to practical implementation using established software tools, advanced applications in photoacoustic imaging and optogenetics, and strategies for optimizing computational efficiency and model accuracy. A strong emphasis is placed on validation protocols, comparing MC results with experimental data and alternative models, and discussing its critical role in virtual clinical trials for accelerating the development of optical imaging and therapeutic technologies.
The Physics of Light in Tissue and Core Principles of the Monte Carlo Method
The study of light-tissue interactions forms the foundational basis for a wide array of non-operative diagnostic methods and therapeutic applications in modern medicine. Optical techniques including diffuse reflection spectroscopy (DRS), near infrared spectroscopy (NIRS), diffuse optical tomography (DOT), Raman imaging, fluorescence imaging, optical microscopy, optical coherence tomography (OCT), and photoacoustic (PA) imaging have emerged as powerful tools in biomedicine, offering the significant advantage of utilizing non-ionizing radiation while maintaining non-invasiveness [1]. The potential of these modalities remains far from fully explored, driving continued research into the fundamental principles governing light propagation through biological media.
At the heart of understanding these optical techniques lies the complex interplay between light and the intricate structural components of biological tissue. When photons encounter tissue, they undergo a series of interactions including absorption, scattering, and potential fluorescence re-emission that collectively determine the spatial and temporal distribution of light within the medium. Modeling these interactions accurately is essential for advancing both diagnostic imaging capabilities and light-based therapies such as photodynamic therapy (PDT) [2].
The Monte Carlo (MC) simulation approach has established itself as the gold standard for modeling light propagation in scattering and absorbing media like biological tissue [1] [3]. This computational method provides a flexible framework for simulating the random walk of photons as they travel through tissue, undergoing absorption and scattering events based on the statistical probabilities derived from the optical properties of the medium. For researchers investigating light-tissue interactions, MC methods offer unparalleled accuracy in predicting light distribution in complex, heterogeneous tissue geometries that defy analytical solutions.
Fundamental Optical Properties of Tissue
The propagation of light in biological tissues is governed by three fundamental optical properties that determine how photons interact with the medium: the absorption coefficient, the scattering coefficient, and the anisotropy factor. These parameters collectively define the behavior of light as it travels through tissue and forms the basis for all computational models of light transport.
Absorption Coefficient (μa)
The absorption coefficient (μa) represents the probability of photon absorption per unit infinitesimal path length in a medium [1]. This parameter is intrinsically linked to the molecular composition of the tissue, as different chromophores—including hemoglobin, melanin, water, and lipids—exhibit distinct absorption spectra across the electromagnetic spectrum. In biological tissues, absorption coefficients can vary significantly depending on the wavelength and tissue type. In the red and near-infrared regions (λ > 625 nm), μa typically ranges between 0.01 and 0.5 cm⁻¹, while at shorter wavelengths (λ < 625 nm), absorption increases substantially, with values ranging from 0.5 to 5 cm⁻¹ due primarily to hemoglobin absorption [4]. The strong absorption of hemoglobin at visible wavelengths has important implications for fluorescence molecular tomography (FMT) and bioluminescence tomography (BLT) of fluorescent proteins and luciferase, whose emission peaks fall within these highly absorptive regions [4].
Scattering Coefficient (μs) and Reduced Scattering Coefficient (μ's)
The scattering coefficient (μs) quantifies the probability of a photon scattering event per unit path length and primarily depends on the density and size distribution of microscopic spatial variations in refractive index within the tissue [1]. These variations arise from subcellular structures, cell membranes, and extracellular matrix components. In biological tissues, μs typically ranges between 10 and 200 cm⁻¹ across visible and near-infrared wavelengths [4]. A more clinically relevant parameter is the reduced scattering coefficient (μ's), defined as μ's = (1 - g)μs, where g is the anisotropy factor [4]. This parameter accounts for the net effect of scattering after considering the directional preference of scattering events. Typical reduced scattering coefficients in tissues range between 4 and 15 cm⁻¹ and exhibit slight wavelength dependence [4].
Anisotropy Factor (g)
The anisotropy factor (g) represents the mean cosine of the scattering angle and quantifies the directional preference of scattering events within tissue [1]. This parameter ranges from -1 (perfect backscattering) to +1 (perfect forward scattering), with g = 0 representing isotropic scattering. In biological tissues, light scattering is strongly forward-peaked, with g typically varying between 0.5 and 0.95 depending on the specific tissue type [4]. This strong forward scattering behavior significantly influences light penetration depth and the overall distribution of light within tissue.
Table 1: Representative Ranges of Optical Properties in Biological Tissues
| Optical Property | Symbol | Typical Range | Wavelength Dependence |
|---|---|---|---|
| Absorption Coefficient | μa | 0.01-5 cm⁻¹ | Strong; varies with chromophore concentration |
| Scattering Coefficient | μs | 10-200 cm⁻¹ | Moderate; generally decreases with increasing wavelength |
| Reduced Scattering Coefficient | μ's | 4-15 cm⁻¹ | Moderate; generally decreases with increasing wavelength |
| Anisotropy Factor | g | 0.5-0.95 | Weak; may vary with tissue microstructure |
The relationship between these optical properties defines two important metrics for light transport: the mean free path (mfp), which is the average distance between interaction events (1/(μs + μa)), and the transport mean free path (tmfp), which represents the distance over which photon direction becomes randomized (1/(μ's + μa)) [4]. These parameters play a crucial role in determining the appropriate modeling approach for light propagation in different tissue types and geometries.
Monte Carlo Simulation of Light Transport
Monte Carlo (MC) simulation represents the most accurate and flexible approach for modeling light propagation in biological tissues, particularly in cases involving complex geometries, heterogeneous optical properties, or non-diffusive regimes where simplified models fail. The MC method treats light as a series of photon packets that undergo stochastic interactions—including absorption, scattering, and boundary effects—as they travel through the tissue medium [1] [2]. By simulating a sufficiently large number of photon trajectories, MC methods can provide highly accurate solutions to the radiative transfer equation (RTE) that governs light transport in scattering media.
Fundamental Principles of MC Simulation
In MC simulations, a large number of photons (conceptually represented as photon packets with statistical weight) are propagated through the tissue medium under study [1]. Each photon packet begins with an initial statistical weight (W₀) and undergoes a random walk process through the tissue, with interactions governed by the optical properties of the medium: refractive index (n), absorption coefficient (μa), scattering coefficient (μs), and scattering anisotropy (g) [1]. The simulation tracks each photon through a sequence of elementary steps: generation of the photon path length, scattering, and refraction/reflection at boundaries.
The core of the MC approach lies in its statistical treatment of photon transport. The path length between interactions is sampled from an exponential distribution based on the total attenuation coefficient (μt = μa + μs). At each interaction point, the photon packet may be absorbed or scattered, with the probability of absorption given by μa/μt. To conserve energy while maintaining computational efficiency, the "Russian roulette" method is often employed when the statistical weight of a photon packet becomes small, giving the photon a chance to continue with increased weight (n·W, where n is between 10-20) or be terminated [1]. While this approach saves computational resources, it can introduce uncertainty in the distribution of photon paths and presents challenges in physical interpretation.
Scattering Phase Functions
The direction of photon scattering at each interaction point is determined by a scattering phase function, which describes the angular distribution of scattered light. The most commonly used phase function in tissue optics is the Henyey-Greenstein (HG) phase function, expressed as:
[ p(\cos\theta) = \frac{1 - g^2}{2(1 + g^2 - 2g\cos\theta)^{3/2}} ]
where θ is the polar scattering angle and g is the anisotropy factor [1]. The azimuthal angle φ is typically assumed to be uniformly distributed between 0 and 2π, calculated as φ = 2πξ, where ξ is a uniformly distributed random number between 0 and 1 [1].
While the Henyey-Greenstein function is widely used due to its mathematical simplicity and ability to represent the strongly forward-peaked scattering typical of biological tissues, it is not the only option. Several authors have introduced Markov chain solutions to model photon multiple scattering through turbid media via more complex anisotropic scattering processes, such as Mie scattering [1]. These approaches can effectively handle non-uniform phase functions and absorbing media by converting the complex multiple scattering problem into a matrix form, computing transmitted/reflected photon angular distributions through relatively simple matrix multiplications [1].
Advanced MC Implementation Considerations
Modern MC implementations for light transport in tissues have evolved to address various computational and practical challenges. The use of graphics processing units (GPUs) has enabled near real-time simulation of complex, three-dimensional samples based on clinical CT images, facilitating applications in treatment planning for procedures such as interstitial photodynamic therapy [2]. These advanced MC models can incorporate various fiber geometries, including physically accurate representations of cylindrical diffusing fibers used in clinical applications [2].
For specialized tissues with aligned cylindrical microstructures (e.g., muscle, skin, bone, tooth), MC simulations can employ more specific phase functions, such as those for infinitely long cylinders, to accurately capture the pronounced anisotropic light scattering effects that produce directionally dependent reflectance patterns [5]. These implementations demonstrate how MC methods can be adapted to address the unique optical characteristics of different tissue types.
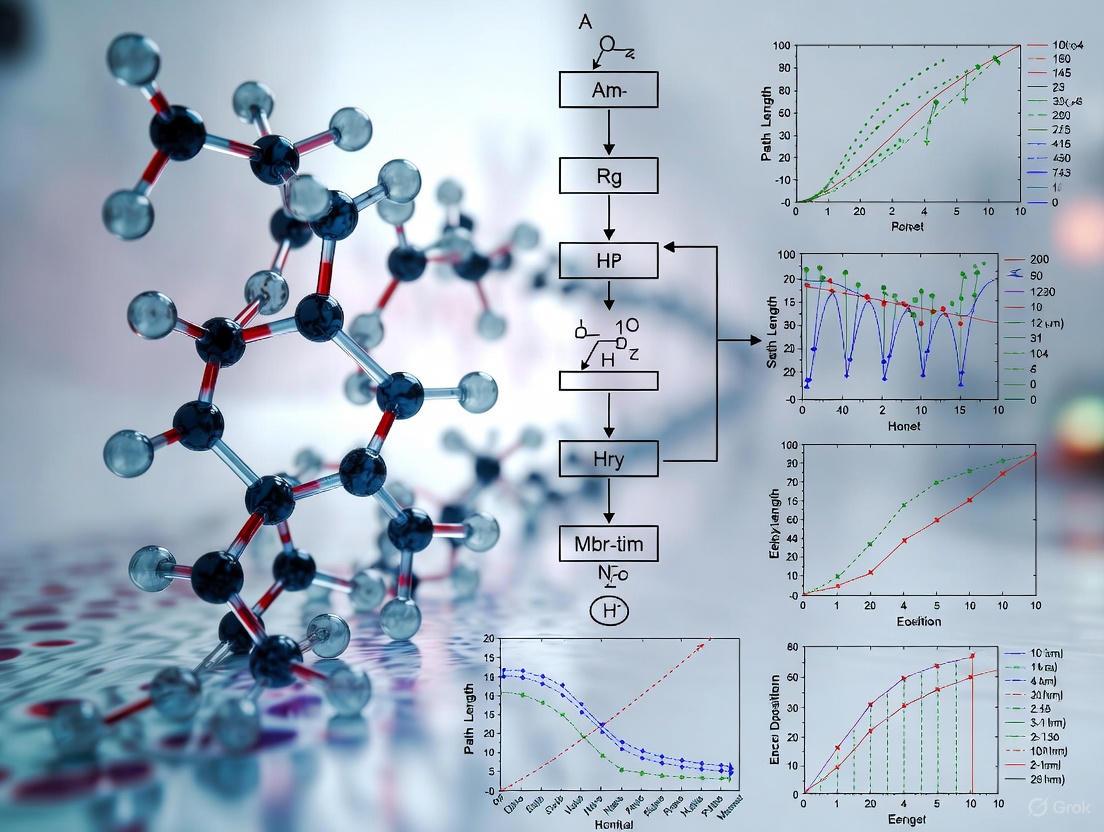
Diagram 1: Monte Carlo photon propagation workflow showing key decision points and processes.
Experimental Determination of Optical Properties
Accurate determination of optical properties is a prerequisite for meaningful MC simulations of light-tissue interactions. Several experimental approaches have been developed to measure these parameters, with the integrating sphere system coupled with inverse solving algorithms representing one of the most widely used methodologies.
Integrating Sphere Measurements and IAD Algorithm
The single-integrating sphere (SIS) system combined with the inverse adding-doubling (IAD) algorithm provides a robust approach for determining the optical properties of biological tissues across the visible and near-infrared spectrum [3]. This methodology involves measuring both total diffuse reflectance (Rt) and total transmittance (Tt) from tissue samples of known thickness, then applying the IAD algorithm to extract the absorption and scattering parameters.
A typical SIS setup consists of an integrating sphere (e.g., 36 mm diameter with a 9 mm sample port) with an inner surface coated with polytetrafluoroethylene (PTFE), which provides high, uniform reflectivity (approximately 0.90) [3]. The system includes a broadband light source such as a 150 W adjustable power halogen lamp and a Vis-NIR spectrometer covering wavelengths from 400 to 1000 nm [3]. All measurements should be conducted within a light-proof enclosure to eliminate interference from ambient light.
For biological tissues like potato tubers used in model studies, samples are typically sectioned into approximately 2 mm thick slices from the inner medulla tissues [3]. Each slice is measured in both reflection and transmission modes by adjusting the sphere configuration. The resulting Rt and Tt values serve as inputs to the IAD algorithm, which computationally solves the inverse problem to determine the optical properties that would produce the measured reflectance and transmittance values.
Table 2: Key Components of Single-Integrating Sphere System for Optical Property Determination
| Component | Specification | Function |
|---|---|---|
| Integrating Sphere | 36 mm diameter, PTFE coating (R ≈ 0.90) | Collects and uniformly distributes reflected or transmitted light |
| Light Source | 150 W halogen lamp, 400-1000 nm | Provides broadband illumination for spectral measurements |
| Spectrometer | USB2000+, 400-1000 nm range | Measures intensity of reflected/transmitted light at different wavelengths |
| Sample Port | 9 mm diameter | Standardized opening for consistent sample measurement |
| Enclosure | Light-proof | Eliminates ambient light interference during measurements |
Complementary Physicochemical Characterization
To correlate optical properties with underlying tissue structure and composition, complementary physicochemical characterization is often performed on the same sampling regions used for optical measurements. These analyses may include:
Color measurement using a digital colorimeter expressed in the CIE Lab* color space, where L* represents lightness, a* indicates green-red tendency, and b* represents blue-yellow tendency [3]. The overall color difference (ΔE) is calculated as the Euclidean distance in this color space.
Dry matter (DM) content determination by drying tissue samples at 105°C until constant mass is achieved [3].
Microstructural analysis using scanning electron microscopy (SEM), where samples are sectioned into slices (e.g., 10 mm × 10 mm × 2 mm), dehydrated, freeze-dried, and sputter-coated with gold prior to imaging [3].
These complementary measurements help establish relationships between tissue microstructure, biochemical composition, and optical properties, providing deeper insight into the fundamental factors governing light-tissue interactions.
Beyond MC: Alternative Modeling Approaches
While MC simulation offers high accuracy and flexibility for modeling light transport in tissues, its computational intensity has motivated the development of alternative approaches that provide different trade-offs between accuracy, speed, and implementation complexity.
Simplified Spherical Harmonics (SPN) Equations
The simplified spherical harmonics (SPN) equations represent a higher-order approximation to the radiative transfer equation that significantly improves upon the diffusion approximation while being less computationally expensive than full spherical harmonics (PN) or discrete ordinates (SN) methods [4] [6]. The SPN method approximates the RTE by a set of coupled diffusion-like equations with Laplacian operators, avoiding the complexities of the full PN approximation which involves mixed spatial derivatives [4].
The SPN equations are particularly valuable for modeling light propagation in regimes where the diffusion approximation fails, including situations involving strong absorption (μₐ ≪ μ'ₛ is not satisfied), small tissue geometries, and regions near sources or boundaries [4] [6]. For example, in small animal imaging or when using visible light in fluorescence molecular tomography, absorption coefficients can be sufficiently high (0.7-2.7 cm⁻¹ for highly vascularized tissues) to invalidate the diffusion approximation [4]. In such cases, the error of fluence calculated near sources between the diffusion approximation and SPN models can be as large as 60% [6].
The SPN method offers several advantages: it captures most transport corrections to the diffusion approximation, requires solving fewer equations than full PN or SN methods, can be implemented using standard diffusion solvers, and avoids the ray effects that plague SN methods [4]. A disadvantage is that SPN solutions do not converge to exact transport solutions as N → ∞; rather, for each problem there is an optimal N that yields the best solution [4].
Beam Spread Function (BSF) Approach
For specific applications such as optogenetics, where estimating light transmission through brain tissue is crucial for controlling neuronal activation, the beam spread function (BSF) approach provides an analytical alternative to MC simulations [1]. The BSF method approximates light distribution in strongly scattering media by accounting for higher-order photons propagating via multiple paths of different lengths, and can also calculate time dispersion of light intensity [1].
In optogenetics applications, the BSF approach has demonstrated good agreement with both numerical MC simulations and experimental measurements in mouse brain cortical slices, yielding a cortical scattering length estimate of approximately 47 μm at λ = 473 nm [1]. This approach offers significantly faster simulation times than MC methods while maintaining comparable accuracy for specific problem geometries.
Reduced Models for Multiple Scattering
Beyond the comprehensive approaches of MC and SPN methods, several reduced models have been developed specifically for multiple scattering processes. These include the Random Walk theorem, empirical predictions, and adding-doubling methods [1]. These approaches typically employ simplified analytical expressions to predict behaviors such as the distribution of total transmission, average scattering cosine, and traveled distance.
While these reduced models provide reasonable results for some averaged observations, they have limitations in distinguishing between similar phase functions with identical anisotropy factors but different probability density functions, and in handling anisotropic scattering, absorbing media, and non-uniform distributions of optical density [1]. Nevertheless, they offer valuable computational efficiency for specific applications where their simplifying assumptions remain valid.
Applications and Case Studies
The principles of light-tissue interactions and MC simulation find application across diverse domains, from biomedical optics to agricultural product inspection. Examining specific case studies illustrates how these fundamental concepts are implemented in practical scenarios.
Case Study 1: Blackheart Detection in Potatoes
In agricultural applications, MC simulations have been employed to investigate light propagation in healthy versus blackhearted potato tissues, revealing significant differences in optical properties that enable non-destructive detection of this physiological disorder [3]. Studies have shown that blackhearted tissues exhibit substantially increased absorption coefficients (μa) in the 550-850 nm range and elevated reduced scattering coefficients (μ's) across the entire Vis-NIR region compared to healthy tissues [3].
MC simulations of light propagation in these tissues demonstrated that both photon packet weight and penetration depth were significantly lower in blackhearted tissues, with healthy tissues achieving approximately 6.73 mm penetration at 805 nm compared to only 1.30 mm in blackhearted tissues [3]. The simulated absorption energy was higher in blackhearted tissues at both 490 nm and 805 nm, suggesting these wavelengths are particularly effective for blackheart detection [3]. These findings were leveraged to develop Support Vector Machine Discriminant Analysis (SVM-DA) models that achieved 95.83-100.00% accuracy in cross-validation sets, confirming the robustness of optical features for reliable blackheart detection [3].
Case Study 2: Orah Mandarin Quality Assessment
Another agricultural application involves using MC simulations to optimize quality assessment of orah mandarins using Vis/NIR spectroscopy in diffuse reflection mode [7]. As a multi-layered fruit with thick skin, the optical properties of different tissue layers (oil sac layer, albedo layer, and pulp tissue) significantly affect quality evaluation signals.
Researchers measured the optical parameters of each tissue layer using a single integrating sphere system with the IAD method and established a three-layer concentric sphere model for MC simulations [7]. The simulations revealed that light was primarily absorbed within the fruit tissue, with transmitted photons accounting for less than 4.2% of the total [7]. As the source-detector distance increased, the contribution rates of the outer layers (oil sac and albedo) decreased while the pulp tissue contribution increased, leading to the recommendation of a 13-15 mm source-detector distance for optimal detection devices that maintain high pulp signal contribution while obtaining sufficient diffuse reflectance strength [7].
Case Study 3: Photodynamic Therapy Treatment Planning
In clinical medicine, MC simulations have been implemented for treatment planning in photodynamic therapy (PDT), where accurate modeling of light propagation is essential for determining the light dose delivered to both target tissues and surrounding normal structures [2]. Researchers have developed MC modeling spaces that represent complex, three-dimensional samples based on patient CT images, incorporating various fiber geometries including physically accurate representations of cylindrical diffusing fibers used for interstitial PDT [2].
These GPU-accelerated MC implementations enable near real-time simulation of light distribution in patient-specific anatomy, significantly improving treatment planning capabilities for conditions such as head and neck cancer [2]. This application demonstrates the critical importance of accurate light propagation models for ensuring therapeutic efficacy while minimizing damage to healthy tissues.
Table 3: Research Reagent Solutions for Optical Tissue Property Determination
| Item | Function/Application | Specifications |
|---|---|---|
| Integrating Sphere | Collects and integrates reflected or transmitted light | 36 mm diameter, PTFE coating (R ≈ 0.90), 9 mm sample port |
| Halogen Lamp Source | Provides broadband illumination for spectral measurements | 150 W adjustable power, 400-1000 nm range |
| Vis-NIR Spectrometer | Measures intensity of light at different wavelengths | USB2000+, 400-1000 nm range |
| Colorimeter | Quantifies tissue color in standardized color space | CIE Lab* color space, measures L, a, b* values |
| Scanning Electron Microscope | Analyzes tissue microstructure at high resolution | Zeiss Sigma 300, requires gold sputter coating of samples |
The study of light-tissue interactions through the fundamental mechanisms of absorption, scattering, and anisotropy provides the essential foundation for advancing both diagnostic and therapeutic applications in biomedical optics. Monte Carlo simulation stands as the gold standard for modeling these complex interactions, offering unparalleled accuracy in predicting light distribution in heterogeneous tissue geometries that defy analytical solutions. The continued development of efficient MC implementations, including GPU-accelerated algorithms and specialized approaches for tissues with specific microstructural characteristics, promises to further expand the applications of these modeling techniques across medical and agricultural domains.
As optical technologies continue to evolve, the integration of accurate light propagation models with patient-specific anatomical data and real-time monitoring capabilities will enable increasingly sophisticated applications in areas ranging from cancer therapy to functional brain imaging. The fundamental principles of light-tissue interactions—governed by the interplay of absorption, scattering, and anisotropy—will remain central to these advances, providing the theoretical framework through which light-based technologies can be optimized for specific clinical and research applications.
The Radiative Transfer Equation (RTE) as the Theoretical Foundation
The Radiative Transfer Equation (RTE) is the fundamental integro-differential equation that describes the propagation of electromagnetic radiation through a medium that absorbs, emits, and scatters energy [8]. It serves as the cornerstone for modeling light transport in various fields, including astrophysics, atmospheric science, and crucially, biomedical optics where it enables the quantitative analysis of light interaction with biological tissues [8] [9].
The RTE strikes a balance between the complex, exact nature of Maxwell's equations and the practical need for a solvable model. While Maxwell's equations provide a complete electromagnetic description, they are often intractable for modeling light propagation in dense, random media like biological tissue. The RTE, in contrast, offers a robust phenomenological framework that has been shown to be a corollary of statistical electromagnetics, bridging the gap between fundamental physics and practical application [9].
In the context of biomedical optics, the RTE provides the theoretical basis for predicting how light energy distributes in tissue, which is essential for developing diagnostic and therapeutic technologies such as photodynamic therapy, diffuse optical tomography, and optical coherence tomography [10] [2]. Its solution enables researchers to relate measurable optical signals (e.g., reflectance, transmittance) to the intrinsic optical properties of tissue, thereby forming the foundation for many inverse problems in medical imaging.
Mathematical Formulation of the RTE
The RTE describes the change in spectral radiance, ( I_\nu(\mathbf{r}, \hat{\mathbf{n}}, t) ), at a point ( \mathbf{r} ), in the direction ( \hat{\mathbf{n}} ), at time ( t ), and for a frequency ( \nu ). This quantity represents the amount of energy flowing through a unit area, per unit time, per unit solid angle, per unit frequency interval [8]. The general form of the time-dependent RTE is given by:
[ \frac{1}{c} \frac{\partial I\nu}{\partial t} + \hat{\Omega} \cdot \nabla I\nu + (\kappa{\nu,s} + \kappa{\nu,a}) \rho I\nu = j\nu \rho + \frac{\kappa{\nu,s} \rho}{4\pi} \int{\Omega} I_\nu d\Omega ]
Here, ( c ) is the speed of light, ( \kappa{\nu,s} ) and ( \kappa{\nu,a} ) are the scattering and absorption coefficients per unit mass, respectively, ( \rho ) is the density of the medium, and ( j_\nu ) is the emission coefficient per unit mass [8]. The integral term on the right-hand side accounts for in-scattering of radiation from all other directions into the direction of interest ( \hat{\mathbf{n}} ).
For many steady-state biomedical applications, the time-independent form of the RTE is sufficient. The single-speed, time-independent version can be written as [11]:
[ \Omega \cdot \nabla \Psi(\mathbf{r}, \Omega) + \sigmat(\mathbf{r}) \Psi(\mathbf{r}, \Omega) = \sigmas(\mathbf{r}) \int_{S^2} \Psi(\mathbf{r}, \Omega') p(\mathbf{r}, \Omega \leftarrow \Omega') d\Omega' + Q(\mathbf{r}, \Omega) ]
In this formulation, ( \Psi(\mathbf{r}, \Omega) ) is the radiation intensity at point ( \mathbf{r} ) in direction ( \Omega ), ( \sigmat ) is the total interaction coefficient (( \sigmat = \sigmas + \sigmaa )), ( \sigmas ) and ( \sigmaa ) are the scattering and absorption coefficients, ( p ) is the scattering phase function, and ( Q ) is the internal radiation source.
Table 1: Key Variables in the Radiative Transfer Equation
| Symbol | Description | Units |
|---|---|---|
| ( I_\nu ), ( \Psi ) | Spectral radiance / Radiation intensity | ( W \cdot m^{-2} \cdot sr^{-1} ) |
| ( \sigmaa ), ( \kappa{\nu,a} ) | Absorption coefficient | ( m^{-1} ) |
| ( \sigmas ), ( \kappa{\nu,s} ) | Scattering coefficient | ( m^{-1} ) |
| ( \sigma_t ) | Total interaction coefficient (( \sigmaa + \sigmas )) | ( m^{-1} ) |
| ( p ) | Scattering phase function | ( sr^{-1} ) |
| ( g ) | Scattering anisotropy factor | Dimensionless |
The Scattering Phase Function and Anisotropy
The scattering phase function ( p(\mathbf{r}, \Omega \leftarrow \Omega') ) describes the probability that radiation coming from direction ( \Omega' ) is scattered into direction ( \Omega ). In biological tissues, scattering is typically anisotropic, meaning it is not uniform in all directions. The Henyey-Greenstein phase function is commonly used to model this anisotropy in tissue optics [10]:
[ p(\cos \theta) = \frac{1}{4\pi} \frac{1 - g^2}{(1 + g^2 - 2g \cos \theta)^{3/2}} ]
where ( \theta ) is the scattering angle, and ( g ) is the anisotropy factor, which ranges from -1 (perfect backscattering) to 1 (perfect forward scattering). For most biological tissues, ( g ) ranges from 0.7 to 0.99, indicating strongly forward-directed scattering [10].
The RTE-Monte Carlo Connection
The Monte Carlo (MC) method provides a powerful computational approach for solving the RTE when analytical solutions are intractable. Rather than seeking a closed-form solution, MC simulations model photon transport as a random walk process, statistically simulating the individual interactions of photons with the medium based on the same fundamental optical properties that appear in the RTE [10].
Each photon or photon packet is tracked as it undergoes absorption, scattering, and boundary interactions according to probability distributions derived directly from the RTE's coefficients. The equivalence between the MC approach and the RTE is well-established; MC is essentially a statistical method for solving the RTE by simulating the underlying physical processes it describes [10] [12].
The following diagram illustrates the conceptual relationship between the RTE and Monte Carlo simulations, and how they form the foundation for applications in biomedical optics:
The diagram above shows how the RTE provides the theoretical foundation for understanding light propagation in tissue, while the Monte Carlo method offers a numerical approach to solve the RTE, together enabling various biomedical applications.
Advantages of Monte Carlo for Biomedical Applications
Monte Carlo simulations offer several distinct advantages for modeling light transport in biological tissues:
Accuracy: MC methods can be made arbitrarily accurate by increasing the number of photons traced, often making them the "gold standard" against which other methods are compared [10] [11].
Flexibility: MC can handle complex, heterogeneous geometries (e.g., layered tissues, blood vessels) and arbitrary boundary conditions that would be intractable for analytical RTE solutions [2].
Comprehensive Data Collection: Simulations can simultaneously track multiple physical quantities (e.g., absorption distribution, fluence rate, pathlength) with any desired spatial and temporal resolution [10].
The main limitation of conventional MC methods is their computational expense, though recent advances in variance reduction techniques, GPU acceleration, and hybrid methods have significantly improved efficiency [11] [2].
Monte Carlo Implementation: From RTE to Practice
Translating the RTE into a practical Monte Carlo simulation involves converting the continuous equation into a discrete stochastic model. The following diagram illustrates the core workflow of a typical MC simulation for photon transport in tissue:
Key Implementation Steps
Photon Initialization: Photon packets are launched with specific initial positions, directions, and weights (typically set to 1). For a pencil beam incident perpendicular to a tissue surface, initialization would be [10]:
- Position: ( x=0, y=0, z=0 )
- Direction cosines: ( \mux=0, \muy=0, \mu_z=1 )
Step Size Selection: The distance a photon travels between interactions is sampled from the probability distribution derived from Beer-Lambert's law [10]: [ s = -\frac{\ln \xi}{\mut} ] where ( \xi ) is a uniformly distributed random number in (0,1], and ( \mut = \mua + \mus ) is the total attenuation coefficient.
Absorption and Weight Update: At each interaction site, a fraction of the photon weight is absorbed [10]: [ \Delta W = \frac{\mua}{\mut} W ] The remaining weight continues propagating: ( W \leftarrow W - \Delta W ).
Scattering: A new propagation direction is calculated by sampling the scattering phase function. For the Henyey-Greenstein phase function, the scattering angle θ is determined by [10]: [ \cos \theta = \frac{1}{2g} \left[ 1 + g^2 - \left( \frac{1-g^2}{1-g+2g\xi} \right)^2 \right] \quad \text{if} \quad g \neq 0 ] The azimuthal angle φ is uniformly distributed: ( \varphi = 2\pi\xi ).
Advanced Monte Carlo Techniques
To address the computational challenges of conventional MC methods, several advanced techniques have been developed:
Variance Reduction: Methods like implicit capture (photon packets rather than individual photons) and importance sampling significantly improve efficiency without sacrificing accuracy [10] [11].
Accelerated Convergence: New algorithms that couple forward and adjoint RTE solutions can achieve geometric convergence, offering orders-of-magnitude improvement in computational efficiency [11].
GPU Parallelization: Implementing MC algorithms on graphics processing units enables near real-time simulation for complex geometries, making clinical applications feasible [2].
Experimental Protocols and Validation
Validating MC simulations against experimental measurements is crucial for establishing their reliability in biomedical applications. The following protocol outlines a typical validation approach using tissue-simulating phantoms:
Phantom Preparation and Experimental Setup
Phantom Fabrication: Create tissue-simulating phantoms with known optical properties using materials such as:
- Polydimethylsiloxane (PDMS) as a base matrix
- Titanium dioxide or polystyrene microspheres as scattering agents
- India ink or other dyes as absorbing agents [13]
Optical Property Characterization: Independently measure the absorption coefficient ((\mua)), scattering coefficient ((\mus)), and anisotropy factor ((g)) of the phantom using techniques such as:
- Integrating sphere measurements
- Inverse adding-doubling method
- Spatial frequency domain imaging
Experimental Measurement: Set up the optical system (e.g., fiber-based spectrometer, optical coherence tomography system) to measure light transport through the phantom, recording parameters such as:
- Diffuse reflectance
- Transmittance
- Fluence rate distribution [13]
Simulation Parameters and Comparison
MC Simulation Setup: Configure the MC simulation with the measured optical properties and matching source-detector geometry.
Photon Count: Simulate a sufficient number of photon packets (typically (10^6)-(10^9)) to achieve acceptable statistical uncertainty.
Validation Metrics: Compare simulation results with experimental measurements using:
- Root mean square error (RMSE)
- Coefficient of determination (R²)
- Visual comparison of spatial/temporal distributions
Table 2: Essential Research Reagent Solutions for Experimental Validation
| Reagent/Material | Function in Experiment | Typical Concentrations |
|---|---|---|
| Polydimethylsiloxane (PDMS) | Tissue-simulating base matrix | N/A (bulk material) |
| Titanium Dioxide (TiO₂) | Scattering agent | 0.1-2% by weight |
| Polystyrene Microspheres | Controlled scattering particles | 0.5-3% suspension |
| India Ink | Absorption agent | 0.001-0.1% by volume |
| Nylon Fibers | Raman scattering target | Varies with application |
| Intralipid | Commercial scattering standard | 1-20% dilution |
Applications in Tissue Research and Drug Development
The RTE-based Monte Carlo approach has enabled significant advances in numerous biomedical applications:
Photodynamic Therapy (PDT) Planning
MC simulations of light propagation allow clinicians to optimize light dose delivery for PDT. By modeling the specific anatomy of a patient (derived from CT or MRI scans), clinicians can calculate the fluence rate distribution throughout the treatment volume, ensuring that therapeutic light levels reach the target tissue while minimizing exposure to healthy structures [2]. This approach has been successfully applied for treatment planning in head and neck cancers, significantly improving treatment efficacy.
Surgical Guidance with Raman Spectroscopy
MC methods help establish the relationship between Raman sensing depth and tissue optical properties, which is crucial for interpreting spectroscopic data during surgery. Studies have shown that for a typical Raman probability of (10^{-6}), the sensing depth ranges between 10 and (600 \mu m) for absorption coefficients of 0.001 to (1.4 mm^{-1}) and reduced scattering coefficients of 0.5 to (30 mm^{-1}) [13]. This quantitative understanding enables more precise biopsy collection and tumor margin assessment.
Optical Coherence Tomography (OCT)
MC simulations of OCT systems incorporate wave-based phenomena like coherence and interference, providing a bridge between the particle-based RTE and the wave nature of light. Recent advances include modeling focusing Gaussian beams rather than infinitesimally thin beams, leading to more accurate simulations of modern OCT systems [14]. These simulations help solve inverse problems to extract tissue optical properties from OCT measurements.
Drug Development Applications
In pharmaceutical research, MC simulations support several critical activities:
Photosensitizer Dosimetry: Calculating light doses for activating photodynamic therapy agents in specific tissue geometries.
Treatment Planning: Optimizing light delivery systems for activating light-sensitive drug compounds.
Monitoring Therapeutic Response: Modeling changes in tissue optical properties resulting from treatment, which can serve as biomarkers of efficacy.
The Radiative Transfer Equation provides the essential theoretical foundation for understanding and modeling light transport in biological tissues. While the RTE itself is often analytically intractable for realistic tissue geometries, Monte Carlo methods offer a powerful, flexible, and accurate approach for solving it numerically. The synergy between the rigorous theoretical framework of the RTE and the practical computational capabilities of MC simulations has enabled significant advances in biomedical optics, particularly in therapeutic and diagnostic applications.
Ongoing research continues to enhance this partnership, with developments in accelerated convergence algorithms, GPU implementation, and more sophisticated models of tissue optics further strengthening the connection between theory and application. As these methods become more efficient and accessible, their impact on clinical practice and drug development is expected to grow, ultimately improving patient care through more precise optical-based therapies and diagnostics.
The propagation of light through biological tissue is governed by the Radiative Transfer Equation (RTE), a differential equation that describes the balance of energy as photons travel through, are absorbed by, and are scattered within a medium. For complex, heterogeneous geometries like human tissue, obtaining analytical solutions to the RTE is often impossible. The Monte Carlo (MC) method provides a powerful, flexible, and rigorous alternative by simulating the stochastic propagation of individual photons [10]. Instead of solving the RTE directly, MC models the local rules of photon transport as probability distributions, effectively tracing the random walks of millions of photons to build a statistically accurate picture of light distribution [10]. This technique is widely considered the gold standard for simulating light transport in tissues, particularly for biomedical applications such as photodynamic therapy, diffuse optical tomography, and radiation therapy planning [15] [10]. This guide details the core principles and practical implementation of the Monte Carlo method for solving the RTE, with a specific focus on applications in tissue research.
Theoretical Foundation: Linking Stochastic Sampling to the RTE
The fundamental principle of the Monte Carlo method for light transport is its equivalence to the RTE. The RTE itself describes the change in radiance, a measure of light energy, at a point in space and in a specific direction [16]. The MC approach stochastically models the same physical phenomena—the step size between photon interactions (absorption and scattering events) and the scattering angle when a deflection occurs [10].
The core of the method lies in interpreting the photon's history as a random walk, where each step is determined by sampling from probability distributions derived from the tissue's optical properties [17] [10]. These properties are:
- The Absorption Coefficient (µa): The probability of photon absorption per unit path length.
- The Scattering Coefficient (µs): The probability of photon scattering per unit path length.
- The Scattering Phase Function: The probability distribution of the scattering angle, θ, often characterized by the anisotropy factor, g, which is the weighted average of the cosine of the scattering angle [10].
When a sufficient number of photon packets are simulated, their collective behavior converges to the solution of the RTE. This makes MC a robust, albeit computationally intensive, method that can achieve arbitrary accuracy by increasing the number of photons traced, without the simplifying assumptions required by analytical models [10].
Table 1: Key Optical Properties and Their Roles in Monte Carlo Simulation
| Optical Property | Symbol | Role in Monte Carlo Simulation | Typical Values in Tissue |
|---|---|---|---|
| Absorption Coefficient | µₐ | Determines the fraction of photon weight absorbed at each interaction site. | Varies widely by wavelength and tissue type |
| Scattering Coefficient | µₛ | Inversely related to the mean free path between scattering events. | ~10-100 mm⁻¹ (highly tissue-dependent) |
| Anisotropy Factor | g | Describes the preferential direction of scattering; g=1 is forward, g=0 is isotropic. | 0.7 - 0.9 for most tissues [18] |
| Reduced Scattering Coefficient | µₛ' = µₛ(1-g) | A derived property useful in diffusion theory; represents the effective scattering after considering anisotropy. | Calculated from µₛ and g |
A Practical Implementation: The Photon Transport Algorithm
A typical MC simulation for a homogeneous medium involves launching photon packets and repeatedly subjecting them to a cycle of movement, absorption, and scattering until they exit the geometry or are terminated. The following workflow, detailed in [10], outlines this core algorithm.
Step 1: Launching a Photon Packet
To improve computational efficiency, photons are often grouped into packets with an initial weight, W, typically set to 1. The initial position and direction (defined by three direction cosines) are set based on the light source. For a pencil beam at the origin, perpendicular to the surface, the initialization is [10]:
- Position: ( x=0, y=0, z=0 )
- Direction Cosines: ( \mux=0, \muy=0, \mu_z=1 )
Step 2: Step Size Selection and Photon Movement
The distance, ( s ), a photon travels before an interaction is a random variable determined by the total interaction coefficient, ( \mut = \mua + \mus ), which represents the probability of any interaction per unit path length. The step size is sampled using [10]: [ s = -\frac{\ln \xi}{\mut} ] where ( \xi ) is a random number uniformly distributed between 0 and 1. The photon's coordinates are then updated: [ x \leftarrow x + \mux s, \quad y \leftarrow y + \muy s, \quad z \leftarrow z + \mu_z s ]
Step 3: Absorption and Scattering
At the interaction site, a fraction of the photon's weight is absorbed. This fraction is ( \Delta W = (\mua / \mut) W ). The remaining weight is scattered in a new direction [10]. The new direction is determined by the scattering phase function. The Henyey-Greenstein phase function is commonly used for tissue due to its accuracy and computational simplicity. The scattering angle, θ, and a uniformly sampled azimuthal angle, φ, are calculated [10]: [ \cos \theta = \frac{1}{2g} \left[ 1 + g^2 - \left( \frac{1-g^2}{1-g+2g\xi} \right)^2 \right] \quad ( \text{for } g \neq 0 ) ] [ \varphi = 2\pi\xi ] The photon's direction cosines are then updated based on these angles, and the cycle repeats from Step 2. A photon packet is terminated when its weight falls below a threshold, or it exits the simulated geometry.
Advanced Techniques: Condensed History for Accelerated Simulation
In biological tissue, scattering is often highly forward-peaked (g > 0.7), meaning photons undergo thousands of small-angle deflections per millimeter of travel [18]. Simulating each of these collisions individually in a "collision-by-collision" approach is computationally expensive. Condensed History (CH) methods address this by grouping multiple scattering events into a single "super-event," dramatically speeding up simulations with minimal loss of accuracy [18].
Two prominent CH models are:
- Similarity Theory (ST) Model: This model simplifies the problem by using an isotropic scattering phase function but with modified, lower scattering and absorption coefficients to preserve the overall transport characteristics [18].
- Discrete Scattering Angles (DSA) Model: This more sophisticated approach approximates the highly forward-peaked scattering phase function (e.g., Henyey-Greenstein) with a linear combination of delta functions. This method is designed to preserve the low-order angular moments of the original phase function, leading to higher accuracy than the ST model for a wide range of tissue optical properties [18].
Essential Computational Tools and Platforms
The computational demand of MC simulations has led to the development of specialized software platforms. The table below summarizes key tools used across different application scales in biomedical optics and therapy planning.
Table 2: Key Monte Carlo Simulation Platforms in Biomedical Research
| Platform Name | Primary Application Domain | Key Features & Strengths | Underlying Language/Code |
|---|---|---|---|
| EGSnrc | Radiation therapy dose calculation; Nanoparticle dose enhancement [15] | Electron and photon transport; Open-source; Customizable material files. | C++ |
| Geant4 | General purpose particle transport; Nanoparticle-enhanced radiotherapy [15] [19] | Models full Auger de-excitation cascades; Broad physics processes. | C++ |
| GPU-Accelerated Codes (e.g., gDRR, GGEMS) | Transmission & emission tomography (CT, PET, SPECT) [19] | Extreme speedups (100-1000x over CPU); Enables practical, large-scale applications. | CUDA, OpenCL |
| Custom MCML & Derivatives | Light transport in multi-layered tissues (historical and specialized use) | Standardized model for layered media; Extensive validation. | C |
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation and application of Monte Carlo models in tissue research require a combination of software and conceptual "reagents."
Table 3: Essential Research Reagent Solutions for Monte Carlo Studies
| Research Reagent | Function & Explanation | Example in Context |
|---|---|---|
| Henyey-Greenstein Phase Function | A mathematical function that models the angular distribution of single scattering events in biological tissue. | Serves as the scattering phase function for sampling new photon directions after a scattering event [10]. |
| Variance Reduction Techniques | Methods to decrease the statistical noise of the simulation without increasing the number of photon packets. | Using photon packets with weights instead of individual photons is a primary variance reduction technique [10]. |
| Digital Tissue Phantom | A computer model that defines the 3D geometry and spatial distribution of optical properties within a simulated tissue. | Used as the virtual environment in which photon packets propagate; can be simple slabs or complex, anatomically accurate models. |
| GPU Parallelization | The use of graphics processing units (GPUs) to run thousands of photon histories in parallel, drastically reducing computation time. | Essential for simulating large tissue volumes or obtaining high-precision results in a reasonable time frame [19]. |
| Optical Property Library | A curated database of the absorption and scattering coefficients (µₐ, µₛ) and anisotropy (g) for various tissue types at specific wavelengths. | Provides the critical input parameters that define how the simulated virtual tissue interacts with light. |
Applications in Biomedical Research and Therapeutics
The MC method's flexibility makes it indispensable in several advanced biomedical applications:
- Photodynamic Therapy (PDT): MC simulations model the light fluence distribution within tissue to ensure sufficient activating light reaches the target area, enabling precise dosimetry for effective treatment [10].
- Diffuse Optical Tomography (DOT): In this imaging technique, MC serves as the "forward model," predicting how light from a source will travel through tissue to reach a detector. This model is essential for reconstructing images of internal optical properties [10].
- Nanoparticle-Enhanced Radiotherapy: MC simulations, particularly using platforms like Geant4, are critical for calculating the Dose Enhancement Factor (DEF) when heavy nanoparticles like gold are introduced into tumor cells. They track the secondary electrons and photons released upon irradiation, providing a more complete picture of local energy deposition than analytical methods [15].
- Sensor and ADAS Development: Physically-based simulators like the SWEET platform use MC techniques to test and validate optical sensors (cameras, lidars) for autonomous vehicles by replicating their performance in adverse weather conditions like fog [16].
The Monte Carlo method provides a powerful and fundamentally rigorous framework for solving the Radiative Transfer Equation in complex, scattering-dominated media like biological tissue. By translating a deterministic differential equation into a stochastic process of photon trajectory sampling, it achieves a level of accuracy and flexibility that is difficult to match with purely analytical approaches. While computationally demanding, modern advancements, including GPU acceleration and sophisticated condensed history algorithms, continue to expand its practicality and scope. For researchers in optics, drug development, and therapeutic planning, mastering the Monte Carlo method is not merely an academic exercise but a critical tool for advancing the precision and efficacy of light-based technologies in medicine.
In the field of biomedical optics, the interaction of light with biological tissue is governed by a set of fundamental optical properties. Understanding these properties—the absorption coefficient (μa), the scattering coefficient (μs), and the anisotropy factor (g)—is paramount for advancing research in therapeutic and diagnostic applications, particularly when employing sophisticated modeling techniques like Monte Carlo simulations for light propagation in tissue. These parameters form the core of the radiative transfer equation (RTE), the fundamental mathematical model for describing photon transport in turbid media like biological tissue [20]. Accurately determining these properties enables researchers to predict how light will distribute within tissue, which is essential for developing both light-based therapies and diagnostic technologies.
This guide provides an in-depth technical examination of these core properties, framed within the context of computational modeling. A precise understanding of μa, μs, and g is not merely academic; it is the foundation for constructing accurate and predictive Monte Carlo models that can simulate light-tissue interactions in silico, thereby reducing the need for extensive and costly laboratory experiments [20] [21].
Defining the Core Optical Properties
The propagation of light through biological tissue is a complex process of absorption and scattering. The following properties quantitatively describe these interactions.
Absorption Coefficient (μa)
- Definition: The absorption coefficient (μa) defines the probability of a photon being absorbed per unit path length within a medium. It is measured in inverse centimeters (cm⁻¹) [20] [21].
- Physical Interpretation: A higher μa value indicates a greater likelihood of photon absorption. This coefficient is directly proportional to the concentration of absorbing chromophores within the tissue, such as hemoglobin, melanin, and water [21]. The absorption process converts light energy into other forms, such as heat or chemical energy.
- Role in the RTE: In the radiative transfer equation, the term
-μa * L(r, ŝ)represents the loss of radiance due to absorption [20]. - Dependence: The absorption coefficient μa typically exhibits a linear dependence on the concentration of the absorbing chromophore, even in highly dense media [22].
Scattering Coefficient (μs)
- Definition: The scattering coefficient (μs) defines the probability of a photon being scattered per unit path length within a medium. It is also measured in inverse centimeters (cm⁻¹) [20] [21].
- Physical Interpretation: Scattering redirects a photon's path without a loss of energy. The value of μs indicates the density of scattering particles in the tissue. Biological tissues are typically high-scattering media, meaning photons undergo numerous scattering events before being either absorbed or exiting the tissue.
- Role in the RTE: In the RTE, scattering contributes to both energy loss and gain. The term
-μs * L(r, ŝ)represents loss from the primary beam due to scattering away from directionŝ, while the integral term+ μs * ∫ p(ŝ, ŝ') L(r, ŝ') dΩ'represents the gain from light scattered from all other directionsŝ'into directionŝ[20].
Anisotropy Factor (g)
- Definition: The anisotropy factor (g) describes the average direction in which light is scattered during a single scattering event. It is defined as the mean cosine of the scattering angle θ [20].
- Physical Interpretation and Values: This is a dimensionless parameter ranging from -1 to +1.
- Role in the RTE: The anisotropy g is a key parameter of the scattering phase function,
p(ŝ, ŝ'), which describes the angular distribution of scattered light [20]. The Henyey-Greenstein phase function is commonly used in tissue optics to model this angular dependence [23].
The Reduced Scattering Coefficient (μs')
While not a fundamental property, the reduced scattering coefficient is a critical derived parameter for modeling light propagation in the diffusion regime.
- Definition:
μs' = μs * (1 - g)[cm⁻¹] [24]. - Purpose and Utility: It combines the scattering coefficient (μs) and the anisotropy (g) into a single parameter that describes the effectiveness of scattering in randomizing the direction of photon propagation. It represents the scattering coefficient that would be observed if all scattering events were isotropic (g=0). This parameter is essential for models that use the diffusion approximation of the RTE, as it defines the random walk step size of photons (
1/μs') in a predominantly scattering medium (whereμa << μs') [20] [24].
Table 1: Summary of Key Optical Properties and Their Roles
| Property | Symbol | Units | Definition | Role in Light Transport |
|---|---|---|---|---|
| Absorption Coefficient | μa | cm⁻¹ | Probability of absorption per unit path length | Determines energy deposition and attenuation. |
| Scattering Coefficient | μs | cm⁻¹ | Probability of scattering per unit path length | Determines how frequently a photon's path is redirected. |
| Anisotropy Factor | g | Dimensionless | Mean cosine of the scattering angle | Determines the preferred direction of scattering (forward/backward). |
| Reduced Scattering Coefficient | μs' | cm⁻¹ | μs' = μs(1 - g) | Governs the rate of directional randomization in dense scattering media. |
Mathematical Relationships and Light Transport Models
The interplay between the optical properties is formally captured by mathematical models of increasing complexity, from the exact but computationally expensive RTE to its simplified diffusion approximation.
The Radiative Transfer Equation (RTE)
The RTE is the most rigorous model for light propagation in a scattering and absorbing medium. It describes the change in radiance L(r, ŝ, t) at a position r, in direction ŝ, and at time t. The general form of the time-dependent RTE is [20]:
Where:
cis the speed of light in the medium.μ_t = μ_a + μ_sis the extinction coefficient.p(ŝ, ŝ')is the scattering phase function.S(r, ŝ, t)is the light source term.- The integral is over the
4πsolid angle.
The RTE states that the radiance in a specific direction changes due to (1) the spatial divergence of the beam, (2) loss from extinction (absorption and scattering away from ŝ), (3) gain from scattering from all other directions ŝ' into ŝ, and (4) the contribution from the light source [20].
The Diffusion Approximation
Solving the RTE is computationally challenging due to its high dimensionality. For media where scattering dominates absorption (μ_a << μ_s') and light distribution becomes nearly isotropic after many scattering events, the diffusion approximation offers a simpler, yet powerful, alternative.
The derivation involves expanding the radiance in spherical harmonics and retaining only the isotropic and first-order anisotropic terms [20]:
Here, Φ(r, t) is the fluence rate and J(r, t) is the current density. Substituting this into the RTE leads to two simplified equations. The vector form yields Fick's law, which defines the current density in terms of the gradient of the fluence rate [20]:
Where D is the diffusion coefficient, defined as D = 1 / (3(μ_a + μ_s')) or, more precisely, D = 1 / (3(μ_a + (1-g)μ_s)) [20].
Substituting Fick's law into the scalar form of the approximated RTE gives the diffusion equation [20]:
This equation is significantly easier to solve than the RTE and is accurate in regions far from light sources or boundaries, where the radiance is indeed nearly isotropic.
The following diagram illustrates the logical relationship between the optical properties, the RTE, and its approximations, culminating in the Monte Carlo solution.
Diagram 1: Relationship between optical properties and light transport models. Monte Carlo can model both the full RTE and validate diffusion theory.
Experimental Determination of Optical Properties
Accurately measuring μa, μs, and g is a central challenge in tissue optics. The methods generally involve measuring light signals after interaction with a sample and solving an "inverse problem" to deduce the properties.
Integrating Sphere-Based Techniques
The traditional and most established method involves using one or two integrating spheres to measure the total diffuse reflectance (Rd) and total diffuse transmittance (Td) of a tissue sample [23] [21].
- Procedure: A collimated light beam is incident on a sample. An integrating sphere collects all light diffusely reflected from the sample surface, while another (if used) collects all light diffusely transmitted through the sample. A third measurement of collimated transmittance (
Tc) through a thin sample is often used to determine the extinction coefficientμ_tdirectly via the Beer-Lambert law [23]. - Inverse Problem: The measured
RdandTdare compared to the values calculated by a forward model (e.g., Adding-Doubling method, Inverse Monte Carlo) for a given set ofμa,μs, andg. An iterative process is used to find the set of optical properties that minimizes the difference between measured and calculatedRdandTd[23] [21].
Advanced Non-Hemispherical Methods
Recent research focuses on developing methods that do not require bulky and complex integrating spheres.
- Principle: This approach uses a combination of non-hemispherical reflectance (
Rd), transmittance (Td), and forward transmittance (Tf) signals, measured with detectors placed close to the sample [23]. - Advantages: The
Tfsignal, which is dominated by single-scattering and ballistic photons, allows for the characterization of optically thick samples where collimated transmittance (Tc) is too weak to measure. Using multiple signals with different sensitivities to scattering and absorption (e.g.,Tfis sensitive to single scattering, whileRdis dominated by multiple scattering) improves the stability and uniqueness of the inverse solution forμa,μs, andg[23]. - Inverse Solution: As with sphere-based methods, the measured signals are compared to those calculated by a forward model (which must accurately account for boundary conditions and detector geometry) to retrieve the optical properties [23].
Table 2: Comparison of Experimental Methods for Determining Optical Properties
| Method | Measured Signals | Key Advantage | Key Limitation | Typical Forward Model |
|---|---|---|---|---|
| Dual Integrating Sphere | Total Diffuse Reflectance (Rd), Total Diffuse Transmittance (Td), often with Collimated Transmittance (Tc) | Gold standard; captures all diffuse light. | Complex setup; requires thin samples for Tc; time-consuming. | Adding-Doubling, Inverse Monte Carlo |
| Non-Hemispherical Multi-Signal | Non-hemispherical Rd, Td, and Forward Transmittance (Tf) | Can use a single, optically thick sample; more accessible instrumentation. | Requires precise modeling of detector geometry and boundaries. | Monte Carlo, Approximate RTE solvers |
The following diagram outlines the general workflow for an inverse method to determine optical properties, common to both approaches.
Diagram 2: Generalized workflow for inverse determination of optical properties.
The Scientist's Toolkit: Essential Research Reagents and Materials
Experimental work in tissue optics relies on a set of key materials and instruments. The following table details essential items used in the field, particularly for experiments aimed at determining optical properties.
Table 3: Essential Research Reagents and Instruments
| Item | Function & Application |
|---|---|
| Tissue Phantoms | Synthetic samples that mimic the optical properties of biological tissue. Often made from materials like Intralipid (scatterer) and ink or dyes (absorber). Used for calibration and validation of instruments and models [23] [22]. |
| Integrating Spheres | Hollow spherical devices with a highly reflective interior coating. Used to collect and homogenize all light diffusely reflected from or transmitted through a sample, allowing for a total power measurement [23]. |
| Tunable Light Source / Monochromator | A light source (e.g., a Xenon lamp) coupled with a monochromator to produce monochromatic light at specific wavelengths. Essential for performing spectral measurements to determine how μa and μs vary with wavelength [23]. |
| Sphere Suspensions (e.g., Polystyrene) | Well-characterized suspensions of microspheres with known size and refractive index. Used as standard scatterers in tissue phantoms and for validating measurement techniques against theoretical predictions like Mie theory [23] [22]. |
| Time-/Frequency-Domain instrumentation | Advanced systems that measure the temporal broadening of a short light pulse or the phase shift of an intensity-modulated beam after propagation through tissue. Provides more information for accurately separating μa and μs' compared to steady-state measurements [21]. |
Connection to Monte Carlo Simulations for Light Propagation
Monte Carlo (MC) simulations are a powerful and versatile numerical technique for modeling photon transport in tissue. Their relationship with the optical properties μa, μs, and g is foundational.
- Direct Implementation of Physics: MC methods simulate the random walk of individual photons as they travel through a medium defined by its optical properties. The probability of a photon being absorbed or scattered over a path length is directly governed by
μaandμs. If a scattering event occurs, the new direction of the photon is determined by the scattering phase function, for whichgis the key parameter (e.g., using the Henyey-Greenstein function) [20] [23]. - Gold Standard for Validation: Because MC simulations make minimal approximations (they can model the RTE exactly with a sufficient number of photons), they are often used as a gold standard to assess the accuracy of simpler models, such as solutions derived from the diffusion equation. As shown in the search results, the diffusion approximation introduces inaccuracies, particularly close to the light source and boundaries where the radiance is not isotropic; MC simulations accurately capture this complexity [20].
- Inverse Monte Carlo: This technique is used to determine optical properties experimentally. An MC model is run iteratively with guessed optical properties until its output (e.g., diffuse reflectance) matches the measured data from a real sample. The properties used in the final, matching simulation are taken to be the optical properties of the sample [21].
In summary, within a thesis on Monte Carlo modeling, the optical properties μa, μs, and g are not merely input parameters; they are the very language in which the tissue geometry and the physics of photon interaction are defined. A deep understanding of their definition, their mathematical relationships, and the experimental methods used to ascertain them is crucial for developing, validating, and interpreting sophisticated computational models of light propagation in biological tissue.
This technical guide details the core probability distributions and methodologies that form the foundation of the Monte Carlo (MC) method for simulating light propagation in biological tissues. Framed within a broader thesis on MC simulation for tissue research, this document provides researchers, scientists, and drug development professionals with the in-depth knowledge required to implement, understand, and critically evaluate these computational models.
The Monte Carlo method provides a rigorous, flexible approach for simulating photon transport in turbid media by modeling local interaction rules as probability distributions [10]. This approach is mathematically equivalent to solving the Radiative Transfer Equation (RTE) but avoids the simplifications required for analytical solutions, such as the diffusion approximation, which introduces inaccuracies near sources and boundaries [10]. Instead, MC methods track the random walks of individual photons or photon packets as they travel through tissue, with their paths determined by statistically sampling probability distributions for two key parameters: the step size between interaction sites and the scattering angle when a deflection occurs [25] [26]. The accuracy of MC simulations is limited only by the number of photons traced, making them the gold standard for simulated measurements in many biomedical applications, including biomedical imaging, photodynamic therapy, and radiation therapy planning [10] [27].
Core Probability Distributions in Photon Transport
The physical interaction between light and tissue is governed by the tissue's optical properties. The core probability distributions used in MC simulations directly derive from these properties.
The following table summarizes the essential optical properties and their corresponding probability distributions used in MC simulations.
Table 1: Core Optical Properties and Associated Probability Distributions
| Optical Property (Symbol) | Physical Meaning | Corresponding Probability Distribution | Key Sampling Formula |
|---|---|---|---|
| Absorption Coefficient (μₐ) | Probability of photon absorption per unit path length [28]. | Not used directly for path sampling; determines weight loss at interaction sites. | ( W \leftarrow W - \left( \frac{\mua}{\mut} \right) W ) [10] |
| Scattering Coefficient (μₛ) | Probability of photon scattering per unit path length [28]. | Used in the step size distribution. | ( s = -\frac{\ln(\xi)}{\mu_t} ) [10] [26] |
| Total Attenuation Coefficient (μₜ) | Probability of an interaction (absorption or scattering) per unit path length; μₜ = μₐ + μₛ [28]. | Step size (s) of a photon between interaction sites [10]. | ( s = -\frac{\ln(\xi)}{\mu_t} ) [10] [26] |
| Anisotropy Factor (g) | Mean cosine of the scattering angle [10]. | Scattering phase function, p(θ, φ), defining deflection angles θ and φ [10]. | ( \cos \theta = \frac{1}{2g}\left[1+g^2-\left( \frac{1-g^2}{1-g+2g\xi} \right)^2 \right] ) (g ≠ 0) [10] |
The Step Size Distribution
The step size, ( s ), is the distance a photon travels between two interaction sites (absorption or scattering events). The probability of a photon having a free path length of at least ( s ) is governed by the Beer-Lambert law, leading to an exponential probability density function (PDF) [10] [26]: [ p(s) = \mut e^{-\mut s} ] where ( \mut = \mua + \mus ) is the total attenuation coefficient. To sample a step size ( s ) from this distribution, the inverse cumulative distribution function (CDF) method is applied. The CDF, ( F(s) ), is integrated and set equal to a random number ( \xi ), uniformly distributed between 0 and 1 [26]: [ F(s) = \int0^s p(s') ds' = 1 - e^{-\mut s} = \xi ] Solving for ( s ) yields the sampling formula: [ s = -\frac{\ln(1-\xi)}{\mut} ] Since ( (1-\xi) ) is statistically equivalent to ( \xi ), the computationally efficient form is: [ s = -\frac{\ln(\xi)}{\mu_t} ]
The Scattering Angle Distributions
When a scattering event occurs, a new photon direction must be selected. This is defined by two angles: the deflection angle (θ) and the azimuthal angle (φ).
- Deflection Angle (θ): The Henyey-Greenstein phase function is most commonly used to model this in biological tissues, as it provides a good empirical match and is parameterized by the anisotropy factor ( g ) [10]. The PDF and its sampling formula are:
[ p(\cos \theta) = \frac{1}{2} \frac{1 - g^2}{(1 + g^2 - 2g \cos \theta)^{3/2}} ] [ \cos \theta = \begin{cases} \frac{1}{2g}\left[1 + g^2 - \left( \frac{1 - g^2}{1 - g + 2g\xi} \right)^2 \right] & \text{if } g \ne 0 \ 1 - 2\xi & \text{if } g = 0 \end{cases} ]
- Azimuthal Angle (φ): This angle is typically assumed to be uniformly distributed between 0 and ( 2\pi ) because scattering is symmetric around the photon's initial direction [10]. It is sampled simply as: [ \varphi = 2\pi\xi ]
After sampling ( \theta ) and ( \varphi ), the new photon direction cosines ( (\mux', \muy', \muz') ) are calculated from the old direction cosines ( (\mux, \muy, \muz) ) using a coordinate transformation [10].
Implementation Workflow for a Basic Monte Carlo Simulation
The following diagram and description outline the core algorithm of a photon packet MC simulation in a homogeneous medium.
Diagram 1: Photon packet life cycle workflow.
Experimental Protocol: Photon Packet Lifecycle
The MC algorithm simulates the propagation of millions of photon packets through a series of repeated steps [10] [26]. The following protocol details this process, corresponding to the workflow in Diagram 1.
Photon Packet Launch
- Initialization: Set the photon's initial coordinates. For a pencil beam at the origin, this is ( x=0, y=0, z=0 ).
- Direction: Initialize the direction cosines. For a beam normal to the surface, this is ( \mux=0, \muy=0, \mu_z=1 ) [10].
- Weight: Assign the photon packet a starting weight, typically ( W = 1 ).
Step Size Selection and Movement
- Sampling: Use the formula ( s = -\ln(\xi)/\mu_t ) to determine the distance to the next interaction site.
- Propagation: Update the photon's position: ( x \leftarrow x + \mux s ), ( y \leftarrow y + \muy s ), ( z \leftarrow z + \mu_z s ) [10].
Absorption and Weight Update
- Energy Deposit: At the interaction site, a fraction of the photon's weight is absorbed. The deposited energy is ( \Delta W = (\mua / \mut) W ).
- Weight Reduction: Update the photon packet weight: ( W \leftarrow W - \Delta W ). The value ( \Delta W ) can be recorded in a spatial array to map the absorption distribution [10].
Scattering and Direction Change
- Angle Sampling: Sample the scattering angle ( \theta ) using the Henyey-Greenstein formula and the azimuthal angle ( \phi ) uniformly.
- Coordinate Transformation: Calculate a new set of direction cosines ( (\mux', \muy', \mu_z') ) based on the sampled angles and the previous direction [10].
Photon Termination
- Russian Roulette: When the photon packet weight drops below a pre-defined threshold (e.g., 0.0001), the photon is playing a game of "Russian Roulette." It has a small chance (e.g., 1 in 10) of surviving, in which case its weight is increased by a factor of 10. If it loses, it is terminated [10] [25]. This variance reduction technique saves computation time on photons that contribute little to the final result.
- Boundary Interaction: If the photon packet moves to a boundary, it can be either reflected (based on Fresnel reflections) or transmitted out of the medium, at which point its trajectory is logged, and it is terminated [10].
This section catalogs key computational tools and methodological concepts essential for conducting research in this field.
Table 2: Key Resources for Monte Carlo Simulation in Biomedical Optics
| Resource / Concept | Type | Function and Application |
|---|---|---|
| MCML [25] | Software Code | A widely adopted, steady-state MC program for simulating light transport in multi-layered tissues. Considered a benchmark in the field. |
| GPU Acceleration [25] [29] | Hardware/Software Technique | Using graphics processing units (GPUs) to run parallelized MC simulations, offering orders-of-magnitude speed improvements. |
| Variance Reduction [10] [27] | Computational Method | Techniques like photon packet weighting and Russian Roulette that reduce statistical noise and computation time without biasing results. |
| Scaling/Perturbation Methods [30] [27] | Computational Method | Advanced algorithms that reuse photon path histories from a baseline simulation to model new scenarios, drastically accelerating studies involving parameter variations. |
| Artificial Intelligence (AI) [31] [29] | Computational Method | Deep learning models can act as surrogate models to predict MC-simulated dose distributions or light fluence in seconds, bypassing lengthy computations. |
| GATE/Geant4 [29] | Software Platform | Extensible software toolkits for simulating particle transport, widely used in medical physics for imaging and therapy dosimetry. |
| Tissue Optical Properties (μₐ, μₛ, g, n) [26] | Input Parameters | The critical set of wavelength-dependent parameters that define the simulated tissue's interaction with light. Accuracy here is paramount for meaningful results. |
| Convolution [25] | Post-Processing Technique | A mathematical operation used with MCML outputs to model the response to finite-sized beams of arbitrary shape, rather than just an infinitely narrow pencil beam. |
Advanced Methodologies and Future Directions
While the core distributions remain unchanged, the field is advancing rapidly to address the computational burden of traditional MC and to tackle more complex biological problems.
Acceleration through Scaling and AI: The significant computation time required for high-accuracy results is a major drawback. Recent research focuses on powerful acceleration algorithms. Scaling methods can achieve a 46-fold improvement in computational time for fluorescence simulations with minimal error [30]. Even more transformative is the integration of Artificial Intelligence (AI), where deep learning models can be trained to predict full MC-simulated dose distributions [31] or light fluence in a fraction of a second, acting as a near-instantaneous surrogate model [29].
Handling Tissue Complexity: Basic models assume homogeneous tissues, but real tissues are structurally complex. Advanced MC codes like
mcxyz.ccan model light transport in 3D heterogeneous tissues defined by voxelated volumes, where each voxel can be assigned unique optical properties [25] [26]. Furthermore, Markov Chain Monte Carlo (MCMC) methods, such as the Metropolis-Hastings algorithm, have been explored for efficient simulation in inhomogeneous tissues by allowing photons to make "large steps" through mutation rules [27].Inverse Problem Solving: MC methods are also crucial for solving the inverse problem—estimating a tissue's optical properties from experimental measurements (e.g., reflectance, transmittance). By combining MC simulations with optimization algorithms like Levenberg-Marquardt, researchers can iteratively adjust simulated optical properties until the simulation output matches the measured data [27]. This capability is vital for optical diagnosis and characterizing novel tissues.
The Henyey-Greenstein Phase Function and Alternative Scattering Models
Within the framework of Monte Carlo (MC) simulations for light propagation in biological tissue, accurately modeling the scattering behavior of photons is paramount. When a photon interacts with a tissue component, its new direction is determined by the scattering phase function. The Henyey-Greenstein (HG) phase function has been the de facto standard in biomedical optics for decades due to its mathematical simplicity and single-parameter nature. This technical guide provides an in-depth analysis of the HG function, its limitations, and advanced alternative models, contextualized for researchers developing MC simulations for drug development and tissue diagnostics.
The Henyey-Greenstein Phase Function
The HG phase function is an empirical, parameterized model that describes the probability of a photon scattering through a particular angle. It is defined by the following equation:
$$P_{HG}(\theta, g) = \frac{1}{4\pi} \frac{1 - g^2}{(1 + g^2 - 2g \cos\theta)^{3/2}}$$
where:
θis the scattering angle (0° for forward scattering, 180° for backward scattering).gis the anisotropy factor, ranging from -1 to 1.g = 0: Isotropic scatteringg > 0: Forward-scattering dominant (typical for biological tissues, ~0.7 - 0.99)g < 0: Backward-scattering dominant
The primary advantage of the HG function is its convenience. A single parameter, g, allows for easy integration into MC codes and can be empirically matched to measured tissue properties.
Limitations of the Henyey-Greenstein Model
Despite its widespread use, the HG phase function has significant drawbacks:
- Inaccurate Backscattering: It underestimates the probability of backscattering (θ ~ 180°), which is critical for reflectance-based measurements.
- Lack of Microphysical Basis: It is not derived from light scattering theory (e.g., Mie theory) and does not account for the internal structure of scattering particles.
- Single-Parameter Limitation: The single parameter
gis insufficient to capture the complex angular scattering profiles exhibited by real tissues, which contain diverse intracellular structures like nuclei, mitochondria, and collagen fibers.
Alternative Scattering Phase Functions
To address the limitations of the HG function, several alternative models have been developed. Their key characteristics are summarized in the table below.
Table 1: Comparison of Key Scattering Phase Functions for Tissue Optics
| Model Name | Key Parameters | Primary Advantage | Primary Disadvantage | Typical Application |
|---|---|---|---|---|
| Henyey-Greenstein (HG) | g (anisotropy) |
Mathematical simplicity; computational efficiency. | Poor accuracy for backscattering. | General-purpose MC simulation. |
| Modified HG (MHG) | g, α (weighting factor) |
Better fit to Mie theory by adding a backward peak. | Still empirical; requires two parameters. | Modeling reflectance spectra. |
| Two-Term HG (TTHG) | g_f, g_b, β or γ |
Separately models forward and backward lobes. | Requires three parameters; increased complexity. | Dense tissue with significant backscatter. |
| Mie Theory | x (size parameter), m (relative refractive index) |
Physically rigorous; based on first principles. | Computationally expensive; requires knowledge of particle properties. | Simulating scattering from known cell structures. |
| Rayleigh | --- (Molecular scale) | Simple analytical form for small particles. | Only valid for scatterers << wavelength. | Scattering by subcellular organelles. |
| Double-HG (DHG) | g_1, g_2, f (fraction) |
Flexible for fitting complex, bimodal distributions. | Three parameters; non-trivial parameter fitting. | Tissues with multiple dominant scatterer sizes. |
Modified Henyey-Greenstein (MHG) Function
The MHG function introduces a correction term to improve backscattering accuracy.
$$P{MHG}(\theta, g, \alpha) = \alpha \cdot P{HG}(\theta, g1) + (1-\alpha) \cdot P{HG}(\theta, g_2)$$
Often, g_1 is set to a positive value for forward scattering, and g_2 is set to 0 or a negative value to enhance the isotropic or backward component. The weight α controls the mixture.
Two-Term Henyey-Greenstein (TTHG) Function
A specific, widely-used case of the MHG function is the TTHG, which explicitly uses one term for forward scattering and one for backward scattering.
$$P{TTHG}(\theta, gf, gb, \gamma) = \gamma \cdot P{HG}(\theta, gf) + (1-\gamma) \cdot P{HG}(\theta, g_b)$$
Here, g_f is the forward anisotropy factor (typically >0), g_b is the backward anisotropy factor (typically <=0), and γ is the fractional contribution of the forward-scattering term.
Mie Theory-Based Scattering
Mie theory provides an exact analytical solution for the scattering of light by spherical particles. It is the gold standard for modeling scattering from cells and subcellular structures, which can often be approximated as spheres (e.g., nuclei, mitochondria). The phase function is given by a complex series expansion dependent on the size parameter x = 2πn_m r / λ (where r is particle radius, n_m is the refractive index of the medium, and λ is the wavelength) and the relative refractive index m = n_p / n_m (where n_p is the particle's refractive index).
Experimental Protocols for Phase Function Validation
Validating a phase function for a specific tissue type involves correlating MC simulation results with physical measurements.
Protocol 1: Goniometric Measurement of Scattering Profiles
- Sample Preparation: A thin slice of tissue (e.g., 100-200 µm) is prepared and placed between glass slides.
- Laser Illumination: A collimated, monochromatic laser beam (e.g., HeNe laser at 633 nm) is directed at the sample.
- Angular Detection: A photodetector (e.g., photomultiplier tube or spectrometer) is mounted on a rotating goniometer arm around the sample.
- Data Collection: The scattered light intensity is measured at small angular increments (e.g., 1° to 10°) from 0° to 180°.
- Data Analysis: The measured angular intensity profile
I(θ)is normalized to obtain the experimental phase function. This data is then fitted to HG, MHG, or TTHG models using a non-linear least squares algorithm to extract the parameters (g,α, etc.).
Protocol 2: Inverse Adding-Doubling (IAD) Method
- Bulk Measurement: The total reflectance (
R_d) and total transmittance (T_d) of a tissue sample with known thickness are measured using an integrating sphere. - MC Simulation Setup: An MC model is constructed with initial estimates for the absorption coefficient (
µ_a), scattering coefficient (µ_s), and phase function parameters (g). - Iterative Fitting: The IAD algorithm iteratively adjusts
µ_a,µ_s, andgin the MC simulation until the computedR_dandT_dmatch the experimentally measured values within a specified tolerance.
Diagram 1: Goniometric Measurement Workflow
Implementation in Monte Carlo Simulation
The core logic for implementing a phase function in an MC code involves sampling a new photon direction after a scattering event. The following diagram and workflow outline this process for a generic phase function.
Diagram 2: MC Phase Function Scattering Logic
Workflow for Sampling the HG Phase Function:
- Generate Random Numbers: Draw two independent, uniformly distributed random numbers,
ξ₁andξ₂, from the interval [0, 1]. - Calculate Scattering Angle
θ:- If
gis 0:cosθ = 2ξ₁ - 1 - If
gis not 0:cosθ = (1/(2g)) * [1 + g² - ((1 - g²)/(1 - g + 2gξ₁))² ]
- If
- Calculate Azimuthal Angle
ψ:ψ = 2πξ₂ - Update Photon Direction: The photon's direction cosines (
μx, μy, μz) are updated based onθandψusing rotation matrices.
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials for Scattering Experiments
| Item | Function in Research |
|---|---|
| Integrating Sphere | Measures total diffuse reflectance and transmittance from tissue samples, which are key inputs for the IAD method. |
| Goniometer System | Precisely measures the angular distribution of light scattered from a sample to determine the phase function directly. |
| Tissue Phantoms | Synthetic samples (e.g., with microspheres, lipids, ink) with precisely known optical properties, used to validate MC models and phase functions. |
| Monte Carlo Code | Custom or open-source software (e.g., MCML, TIM-OS) that implements scattering phase functions to simulate light propagation. |
| Collimated Laser Source | Provides a monochromatic, highly directional beam essential for goniometric measurements and phantom characterization. |
| Spectrometer | Resolves the wavelength dependence of scattering, crucial for understanding tissue composition across a spectrum. |
Implementing MC Simulations: Software, Workflows, and Cutting-Edge Biomedical Applications
Monte Carlo (MC) simulation is a stochastic computational technique that uses random sampling to model physical systems. It is widely regarded as the gold standard for modeling light propagation in biological tissues because it can provide precise solutions to the radiative transport equation (RTE) in complex, heterogeneous media [32]. The method tracks the random walks of numerous photons as they travel through tissue, with each photon's path determined by statistically sampling probability distributions for step size between scattering events and angular deflection per scattering event [25]. After propagating a sufficient number of photons, the net distribution of all photon paths yields an accurate approximation of light distribution in tissue [25]. The fundamental advantage of this approach lies in its ability to accurately model complex photon-tissue interactions, including absorption, scattering, and boundary effects, which are crucial for both diagnostic and therapeutic applications in biomedical optics.
The importance of MC methods in biomedical optics has spurred the development of numerous software platforms over the past several decades. This guide provides a comprehensive technical overview of established MC software tools, focusing on three critical categories: the pioneering MCML for multi-layered tissues, the voxel-based mcxyz.c for heterogeneous tissues, and modern GPU-accelerated platforms for dramatically improved computational performance. Understanding the capabilities, implementations, and appropriate applications of these tools is essential for researchers, scientists, and drug development professionals working in tissue optics, photomedicine, and related fields.
Historical Development and Key Platforms
The development of MC simulation for light transport in tissues has evolved significantly since its initial introduction. Table 1 summarizes the key historical milestones and the primary software platforms that have emerged, each building upon previous work while introducing new capabilities.
Table 1: Historical Development of Monte Carlo Software for Light Transport in Tissues
| Year(s) | Key Development | Primary Contributors | Software/Platform | Significant Innovation |
|---|---|---|---|---|
| 1985 | Early MC code for tissue | Steven Jacques | N/A | Implemented exponential probability for photon stepsize and lookup-table for scattering functions [33] |
| 1989 | Multi-layered tissue model | Marleen Keijzer | N/A | Introduced HOP, DROP, SPIN, CHECK steps (original Dutch names); cylindrical coordinates [33] |
| 1989 | Analytic sampling of Henyey-Greenstein function | Scott Prahl | N/A | Simplified code using Cartesian coordinates; demonstrated HG scattering accurately characterized tissue scattering [33] |
| 1992 | Multi-layered planar tissues with unique optical properties | Lihong Wang | MCML | Reorganized code for multiple planar layers; input/output file system; website distribution [25] [33] |
| 2005-2014 | Voxelated MC for heterogeneous tissues | Yin-chu Chen, Li Ting | mcxyz.c | Combined voxelated approaches; each voxel assignable different tissue type with unique optical properties [33] [34] |
| 2008 | GPU-accelerated MCML | Erik Alerstam et al. | CUDAMCML | Utilized NVIDIA graphics cards for significant speed acceleration [25] [33] |
| 2009 | First GPU MC engine for voxelized geometry | Badal and Badano | N/A | Achieved 27x speed-up with single GPU vs. single-core CPU [19] |
| 2010+ | Open-source, extensible MC platform | David Cuccia, Carole Hayakawa | MCCL | Object-oriented C#; cross-platform; multiple source, tissue, detector options [32] |
| 2018+ | OpenCL-based, multi-platform GPU MC | Qianqian Fang | MCX-CL | Portable across NVIDIA/AMD/Intel GPUs and CPUs; feature parity with MCX [35] |
The historical progression demonstrates a clear trajectory from specialized, single-purpose codes to increasingly flexible, high-performance platforms. The initial development of MCML established a robust foundation that has been cited thousands of times and has guided the design of diagnostic and therapeutic devices and clinical protocols [33]. The subsequent creation of voxel-based methods like mcxyz.c addressed the critical need for modeling complex tissue heterogeneities beyond simple layered structures [34]. More recently, the adoption of GPU acceleration has fundamentally transformed the practical utility of MC methods by reducing computation times from days or weeks to minutes or hours, enabling previously impractical simulations [19].
Comparative Analysis of Established MC Software
Core Algorithmic Foundations
All Monte Carlo simulations for light transport in tissue share common algorithmic foundations based on modeling the random walks of photons through turbid media. The simulation tracks photon packets as they undergo absorption and scattering events, with each interaction determined by sampling from probability distributions derived from the tissue's optical properties (absorption coefficient μa, scattering coefficient μs, and anisotropy g) [25]. The fundamental process involves repeated steps of photon movement (HOP), boundary checking (DROP and CHECK), and scattering (SPIN) [33]. What distinguishes the various software implementations is how they represent tissue geometry, handle boundary conditions, and leverage computational hardware.
Feature Comparison of Major Platforms
Table 2 provides a detailed technical comparison of the established MC software platforms, highlighting their respective capabilities, tissue representations, and performance characteristics.
Table 2: Technical Comparison of Established Monte Carlo Software Platforms
| Platform | Tissue Representation | Key Features | Performance | Primary Applications |
|---|---|---|---|---|
| MCML | Multi-layered planar tissues | Steady-state; infinitely narrow photon beam; internal energy deposition & fluence rate; CONV for finite beams [25] | Single CPU; precise for layered tissues | Light distributions in layered tissues like skin; interstitial light applications [25] [36] |
| mcxyz.c | 3D voxelated cube (typically 400×400×400 voxels) | Heterogeneous media; each voxel assigned unique optical properties; matched boundary conditions [25] [34] | Single CPU; computationally intensive for high-resolution volumes | Complex tissues with heterogeneities (tumors, blood vessels); photoacoustic simulation [37] [34] |
| GPU MCML (CUDAMCML) | Multi-layered planar tissues | Same physical model as MCML; optimized for GPU architecture [25] [33] | 100-1000x faster than CPU MCML [19] | Rapid simulation of layered tissues; parameter studies [25] |
| MCX/MCX-CL | 3D voxelated array | Multiple source types; time-resolved; boundary reflection; photon trajectory saving; cross-platform [35] | 100-1000x faster than CPU; runs on NVIDIA/AMD/Intel GPUs [35] | General-purpose heterogeneous tissue simulation; complex source patterns [35] |
| MCCL | Multi-layered with embedded objects (spheres, ellipsoids, cylinders) | Extensible C# architecture; perturbation MC; multi-processor CPU support; variance estimates [32] | Multi-CPU parallelization; optimized algorithms for specific geometries [32] | Educational use; method development; inclusion-based heterogeneities [32] |
Technical Specifications and Methodologies
MCML (Monte Carlo for Multi-Layered media) employs a 3D simulation architecture but stores results in an r-z array in cylindrical coordinates, denoting radial and depth positions [25]. Each layer can have unique optical properties (absorption μa, scattering μs, anisotropy g, and refractive index n). The program uses an infinitely narrow photon beam source, with convolution methods (CONV) available to model finite-sized beams [25]. The internal distribution of energy deposition and fluence rate within the multi-layered medium provides comprehensive information about light transport.
mcxyz.c implements a voxel-based Monte Carlo method where the tissue is defined as a cube with cube-shaped voxels [34]. Each voxel is assigned an integer value identifying a particular tissue type with unique optical properties (μa, μs, g). The simulation generates a map of the relative fluence rate throughout the volume [25]. The input files are created using MATLAB programs that define a palette of tissue types and their optical properties, simulation parameters, and the 3D tissue structure [34]. This approach enables modeling of complex anatomical structures but requires careful voxel assignment.
GPU-Accelerated Platforms (MCX, MCX-CL, CUDAMCML) leverage the massively parallel architecture of graphics processing units to dramatically accelerate simulations. Unlike CPU implementations that process photons sequentially, GPU platforms simulate thousands of photon paths concurrently through parallel threads [35]. MCX-CL specifically uses OpenCL for platform independence, allowing execution on NVIDIA, AMD, and Intel GPUs, as well as multi-core CPUs [35]. These implementations typically achieve speed-up factors of 100-1000× compared to optimized CPU code, making previously impractical simulations feasible [19] [35].
Experimental Protocols and Implementation
Standard Workflow for MC Simulations
The following diagram illustrates the generalized workflow for conducting Monte Carlo simulations of light propagation in tissues, which is common across most platforms with specific implementation differences:
Protocol for MCML Simulations
Objective: To simulate light distribution in a multi-layered tissue model using MCML.
Materials and Software:
- MCML executable (pre-compiled or self-compiled from source)
- Text editor for creating input files
- MATLAB or alternative for results visualization
- Optical properties for each tissue layer
Methodology:
- Create Input File: Prepare a text file (e.g.,
sample.mci) specifying:- Number of photons to simulate (typically 10^5-10^8)
- Number of tissue layers
- For each layer: thickness (cm), μa (cm⁻¹), μs (cm⁻¹), g, n
- Radial and depth bin numbers for output storage
- Random number seed
Execute Simulation: Run MCML with the input file from command line:
Process Results: Use provided MATLAB scripts (
lookmcml.m,getmcml.m) to:- Extract radial and depth-dependent reflectance and transmittance
- Visualize internal fluence rate distribution
- Calculate energy absorption in each layer
Convolution (Optional): For finite-sized beams, use CONV program with MCML output to model specific beam profiles.
Validation: Compare results with analytical solutions for simple cases or with published data [25].
Protocol for mcxyz.c Simulations
Objective: To simulate light distribution in a 3D heterogeneous tissue using mcxyz.c.
Materials and Software:
- mcxyz.c source code
- C compiler
- MATLAB with maketissue.m and lookmcxyz.m scripts
- Tissue optical properties definition
Methodology:
- Define Tissue Types: Modify
makeTissueList.mto specify optical properties for each tissue type at the desired wavelength [34].
Create Tissue Volume: Use
maketissue.mto:- Define voxel grid dimensions (typically 200×200×200)
- Assign tissue types to voxels to create anatomical structure
- Generate binary tissue file (
myname_T.bin) and header file (myname_H.mci)
Compile and Execute:
Visualize Results: Use
lookmcxyz.mto:- Display tissue structure in 2D slices
- Plot fluence rate distribution
- Calculate absorption distribution [34]
Applications: This approach is particularly valuable for modeling tissues with embedded structures like blood vessels, tumors, or anatomical features from medical images.
Protocol for GPU-Accelerated MCX Simulations
Objective: To rapidly simulate light transport in 3D heterogeneous media using GPU acceleration.
Materials and Software:
- MCX or MCX-CL binary appropriate for your GPU
- NVIDIA, AMD, or Intel GPU with recent drivers
- MATLAB or Python for data analysis (optional)
Methodology:
- Prepare Input Data:
- Create a 3D volume defining tissue types at each voxel
- Define optical properties for each tissue type
- Specify source characteristics (position, direction, type)
Configure Simulation (JSON format for MCX-CL):
Execute Simulation:
Process Output: Extract fluence rate, surface reflectance, or other detected photon data for analysis.
Performance Optimization: Adjust thread blocks and GPU settings based on specific hardware for optimal performance [35].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3 outlines key computational tools and resources essential for implementing Monte Carlo simulations in tissue optics research.
Table 3: Essential Research Reagent Solutions for Monte Carlo Simulations
| Tool/Resource | Function/Purpose | Availability | Implementation Notes |
|---|---|---|---|
| MCML Code | Gold standard for multi-layered tissue simulations | https://omlc.org/software/mc/ | Pre-compiled executables available; modifiable source code [25] |
| mcxyz.c Package | 3D heterogeneous tissue simulations with voxelated domains | https://omlc.org/software/mc/mcxyz/ | Requires MATLAB for input generation and output visualization [34] |
| MCX/MCX-CL Platform | GPU-accelerated Monte Carlo for rapid 3D simulations | http://mcx.space | Supports multiple GPU platforms; MATLAB/Python interfaces [35] |
| MCCL Suite | Extensible, object-oriented MC platform with multiple geometry support | https://github.com/VirtualPhotonics | Cross-platform C# implementation; professional documentation [32] |
| Tissue Optical Properties Database | Reference values for various tissues at different wavelengths | Integrated in mcxyz.c's spectralLIB.mat; literature sources | Critical for realistic simulations; wavelength-dependent [34] |
| MATLAB Visualization Scripts | Standardized result processing and visualization | Included with MCML and mcxyz.c distributions | Essential for interpreting simulation output; modifiable for custom plots [25] [34] |
Computational Workflows and Decision Pathways
Selecting the appropriate Monte Carlo platform depends on multiple factors including tissue complexity, computational resources, and specific research requirements. The following diagram illustrates the decision pathway for selecting the most appropriate MC method:
This decision pathway highlights how researchers should approach method selection based on their specific needs. For traditional layered tissues like skin, MCML remains the optimal choice due to its efficiency and precision for these structures [25]. For complex 3D heterogeneities, the decision branches based on available computational resources and specific requirements, with GPU-accelerated platforms providing the best performance for most applications [19] [35].
Monte Carlo simulation continues to be an indispensable tool in biomedical optics, with software platforms evolving to meet increasingly complex research needs. The established MCML code provides a robust foundation for multi-layered tissues, while mcxyz.c extends these capabilities to 3D heterogeneous environments. The recent development of GPU-accelerated platforms represents a transformative advancement, making previously impractical simulations feasible through massive parallelization.
As the field advances, several trends are emerging. Future developments will likely focus on improving hardware portability, modularizing GPU-based MC codes to adapt to evolving simulation needs, and integrating with emerging concepts like training machine learning with synthetic data, digital twins for healthcare, and virtual clinical trials [19]. The continued commitment to open-source code development, as demonstrated by platforms like MCCL, ensures that these powerful tools remain accessible to the broader research community [32].
For researchers selecting MC methods, the key considerations should align with their specific applications: MCML for layered tissues, mcxyz.c for voxel-based heterogeneities with limited GPU access, and GPU-accelerated platforms like MCX for maximum performance with complex 3D structures. As these tools continue to evolve, they will undoubtedly play an increasingly vital role in advancing both diagnostic and therapeutic applications of light in medicine and biology.
The accurate simulation of light propagation in biological tissue is a cornerstone of modern biomedical research, enabling advancements in diagnostic imaging, therapeutic applications, and drug development. Within this domain, Monte Carlo (MC) simulation has emerged as the gold standard for modeling the complex interactions between light and turbid media. These methods statistically simulate the random paths of millions of photons as they travel through tissue, undergoing absorption and scattering events based on the medium's optical properties. The fidelity of these simulations, however, is fundamentally dependent on the realism of the underlying tissue model. This technical guide details the construction of realistic tissue models, focusing on two complementary paradigms: multi-layered phantoms that replicate the stratified nature of biological tissues, and 3D voxel-based approaches that enable the modeling of complex, heterogeneous anatomical structures. Framed within the context of a broader thesis on Monte Carlo simulation for light-tissue interactions, this whitepaper provides researchers and drug development professionals with the experimental protocols and theoretical foundations necessary to implement these critical methodologies.
Multi-Layered Tissue Phantom Construction
Multi-layered phantoms are designed to mimic the stratified architecture of biological tissues, such as skin (comprising epidermis, dermis, and hypodermis) or organ-specific layered structures. These phantoms are essential for validating MC simulations and calibrating imaging systems that must account for depth-dependent variations in optical properties.
Core Materials and Formulations
The base materials for these phantoms must be selected for their tissue-mimicking optical properties, stability, and handling characteristics. Common choices include:
- Agarose-based Gels: Valued for their high melting point (≈80°C), which provides excellent thermal stability during experiments involving hyperthermia or prolonged use. A typical protocol involves homogeneously mixing agarose powder with evaporated milk (to enhance optical absorption), n-propanol (to adjust the speed of sound to tissue-relevant levels, e.g., 1540 m/s), Dulbecco's phosphate-buffered saline (DPBS), and silicon carbide powder (for scattering) [38].
- Polyvinyl Alcohol (PVA) Gels: These hydrogels are biocompatible and resemble the tissue extracellular matrix. Their optical scattering properties can be finely tuned through multiple freeze-thaw cycles or the addition of microspheres and nanoparticles [39].
- Silicone Rubbers and Epoxy Resins: These materials form durable, solid phantoms with long shelf lives that do not require special maintenance, making them ideal for repeated use in quality assurance [40] [41].
The optical properties of these base materials are programmed by adding specific agents:
- Absorbing Agents: India ink or carbon black powder are traditionally used to mimic light absorption by chromophores like hemoglobin [40].
- Scattering Agents: Intralipid, titanium dioxide (TiO₂), or silicon carbide powder are incorporated to replicate the scattering behavior of cellular and subcellular structures [38] [40].
Fabrication and Validation Protocol
The construction of a multi-layered phantom involves a sequential molding and casting process. The following protocol, adapted from established methods, ensures minimal interface artifacts and well-characterized layers [39]:
- Fabrication of the First Layer: Pour the liquid phantom material (e.g., agarose mixture) into a mold. Allow it to gel or cure completely.
- Surface Preparation: Once the first layer is solid, lightly score its surface with a blade or treat it with a solvent to ensure strong bonding with the subsequent layer.
- Casting Subsequent Layers: Carefully pour the liquid material for the second layer onto the prepared surface. Control the pouring temperature to prevent re-melting of the underlying layer.
- Curing and Demolding: Allow the full, multi-layered phantom to cure completely before demolding.
- Optical Characterization: Use an integrating sphere to measure the total transmittance and reflectance of a sample of each layer material. Apply the inverse adding-doubling (IAD) method to these measurements to calculate the absorption coefficient (μa) and reduced scattering coefficient (μs') for each layer—this serves as the ground truth for MC simulations [41].
Table 1: Typical Optical Properties of Multi-Layered Skin Phantom Components
| Skin Layer | Absorption Coefficient, μa (mm⁻¹) | Reduced Scattering Coefficient, μs' (mm⁻¹) | Thickness (mm) | Key Constituents Mimicked |
|---|---|---|---|---|
| Epidermis | 0.1 - 0.5 | 2 - 4 | 0.05 - 0.1 | Melanin, Keratin |
| Dermis | 0.01 - 0.05 | 1.5 - 2.5 | 1 - 2 | Hemoglobin, Collagen |
| Subcutis | 0.001 - 0.01 | 1 - 1.8 | 1 - 5 | Adipocytes, Blood Vessels |
Diagram 1: Multi-Layered Phantom Fabrication and Simulation Workflow.
3D Voxel-Based Modeling and Advanced Fabrication
For modeling complex, heterogeneous anatomical structures that cannot be simplified into layers, 3D voxel-based approaches are required. These models represent tissue as a three-dimensional grid of volume elements (voxels), where each voxel is assigned a unique set of optical properties.
Voxel-Based Monte Carlo Simulations
GPU-accelerated, voxel-based MC platforms have revolutionized the field by enabling rapid simulation of light transport in arbitrarily complex geometries.
- Platforms and Workflows: Frameworks like Monte Carlo eXtreme (MCX) are open-source and leverage GPU parallelization to achieve computational speeds that are orders of magnitude faster than CPU-based methods. A common application is modeling fluorescence, often implemented using a two-step simulation approach (MCX-ExEm):
- Excitation Simulation: The propagation of excitation light is simulated, and the energy deposited in fluorophore-containing voxels is recorded.
- Emission Simulation: The deposited energy is used as a source for a second simulation at the emission wavelength of the fluorophore [41].
- Geometry Definition: Complex 3D structures, such as those derived from medical imaging (CT, MRI) or digital atlases (e.g., Digimouse), can be converted into voxelized volumes for simulation [40] [41]. This allows for the creation of highly realistic "digital twins" of physical phantoms and biological tissues.
3D Printing of Complex Optical Phantoms
Additive manufacturing provides a direct pathway to fabricate physical phantoms from voxel-based digital models, bridging the gap between simulation and reality.
- Fused Deposition Modeling (FDM) with Dynamic Filament Mixing: This technique uses multi-filament extruders to dynamically mix commercially available polylactic acid (PLA) filaments in different ratios during the printing process. Gray filament acts as the absorber, white filament as the scatterer, and clear translucent filament as the base matrix. By programming the mixing ratios, one can achieve a wide range of tissue-mimicking optical properties within a single, contiguous, and anatomically complex phantom [40].
- Validation of a Linear-Mixing Model: Systematic characterization has validated a linear-mixing model between filament ratios and the resulting optical properties. This model allows researchers to predict the μa and μs' of a print based on the input ratios, with studies reporting an average error of 12–15% between predicted and measured values [40].
- Stereolithography (SLA): This method uses a laser to cure a photosensitive resin. By doping the resin with absorbing and scattering agents, phantoms with high spatial resolution and complex shapes can be produced, though often with a single homogeneous material composition per print [39].
Table 2: Comparison of 3D-Printed Phantom Fabrication Techniques
| Fabrication Technique | Base Materials | Key Advantage | Primary Limitation | Reported Spatial Resolution |
|---|---|---|---|---|
| FDM with Filament Mixing | PLA, ABS | Programmable heterogeneity with unlimited unique optical properties in a single print | Limited by nozzle diameter; potential for visual artifacts | ~200 μm layer thickness [40] |
| Stereolithography (SLA) | Photocuring Resins | High surface quality and geometric precision | Typically limited to single-material (homogeneous) prints | Tens of micrometers [39] |
| Inkjet/Stereolithography with Dopants | Resin with TiO₂, Ink | Can incorporate scattering and absorbing agents directly into resin | Requires laborious pre-printing material preparation | Highly dependent on laser spot size [39] |
Diagram 2: 3D Voxel-Based Digital Twin Creation Workflow.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs key materials and computational tools essential for developing and validating realistic tissue models for MC light propagation studies.
Table 3: Essential Research Reagents and Computational Tools
| Item Name | Function/Application | Technical Specification & Rationale |
|---|---|---|
| Low-Temperature Sensitive Liposomes (LTSLs) | Drug delivery vehicle; release cargo upon mild hyperthermia (35-37°C). Used to model spatially-controlled drug release in phantoms [38]. | Composition: DPPC:DSPE-PEG2000:MPPC (86:4:10). MPPC lysolipid facilitates rapid release near physiological temperatures [38]. |
| SIDA Fluorescent Dye | Near-infrared (NIR) model drug; self-quenching at high concentrations enables visualization of release from carriers like LTSLs [38]. | Hydrophilic (partition coefficient <0.005), reducing plasma protein binding. Peak absorbance/emission in NIR "tissue optical window" [38]. |
| Agarose (Low Gel Temperature) | Base matrix for gel-based phantoms. Provides high thermal stability (melting point ~80°C) and optical transparency [38]. | Mixed with evaporated milk (absorber), n-propanol (sound speed adjustment), and SiC (scatterer) to mimic soft tissue properties [38]. |
| Polylactic Acid (PLA) Filaments (Gray, White, Clear) | Feedstock for 3D printing tissue-mimicking phantoms via dynamic filament mixing [40]. | Gray: absorbing agent. White: scattering agent. Clear: base matrix. Enables programmable optical properties via linear mixing model [40]. |
| MCX (Monte Carlo eXtreme) | Open-source, GPU-accelerated software for simulating light transport in 3D voxelated media [41]. | Drastically reduces computation time vs. CPU. Essential for complex geometries and fluorescence (ExEm) simulations [41]. |
The progression from simple, homogeneous phantoms to sophisticated multi-layered and 3D voxel-based models represents a significant leap forward for research reliant on accurate light-tissue interaction modeling. Multi-layered phantoms provide a validated platform for studying depth-dependent phenomena and calibrating diagnostic systems. Simultaneously, the synergy between voxel-based MC simulations and advanced 3D printing fabrication creates a powerful闭环 (closed loop) for innovation. Researchers can now design a complex, heterogeneous phantom in silico, simulate its optical behavior with high accuracy, fabricate it directly via 3D printing, and use the physical object to validate and refine the computational model, thereby creating a faithful digital twin. This integrated approach, central to a modern thesis on Monte Carlo simulation, significantly accelerates the development and optimization of new biomedical optical devices, drug delivery systems, and therapeutic protocols, while reducing the reliance on extensive in vivo experimentation.
In the realm of biomedical optics, Monte Carlo (MC) simulation is widely regarded as the gold standard for modeling light transport in biological tissues [42]. This computational method provides a flexible and rigorous solution to the challenge of predicting how light propagates through complex, turbid media like human tissue. The accuracy of these simulations, however, depends critically on the precise definition of one fundamental component: the optical source. The source definition encompasses parameters such as spatial distribution, angular profile, intensity, and polarization, all of which profoundly influence the resulting light distribution within tissue [43] [42].
Understanding and correctly implementing different light source models is not merely an academic exercise; it has direct implications for optimizing diagnostic and therapeutic applications. In techniques such as functional near-infrared spectroscopy (fNIRS), photoacoustic imaging (PAI), optogenetics, and photodynamic therapy, the choice of illumination geometry affects penetration depth, resolution, and ultimately, the efficacy of the procedure [43]. This guide provides a comprehensive technical framework for defining light sources in MC simulations, serving researchers, scientists, and drug development professionals who require precise optical modeling for their work.
Theoretical Foundations of Light Transport in Tissues
The Radiative Transfer Equation and the Monte Carlo Approach
Light propagation in biological tissues is governed by the Radiative Transfer Equation (RTE), which describes the balance of energy as photons travel through a medium containing absorbing and scattering particles [44]. The RTE is an integro-differential equation that, for complex geometries and optical properties, often lacks analytical solutions. The Monte Carlo method addresses this challenge by providing a stochastic numerical approach that tracks the random walks of individual photons or photon packets as they interact with the simulated medium [42] [45].
The MC method involves simulating millions of photon trajectories, where each photon's path is determined by random sampling from probability distributions based on the optical properties of the tissue. Key interactions include absorption, where photons deposit their energy; elastic scattering, where photons change direction without energy loss; and boundary interactions, where refraction and reflection occur at tissue interfaces [42]. The cumulative results of these simulated photon histories provide accurate approximations of light distribution, including metrics such as fluence rate, absorbed energy, and diffuse reflectance.
Key Optical Properties Governing Light-Tissue Interactions
The interaction between light and tissue is quantified through several inherent optical properties, which must be defined for each tissue layer or region in a simulation:
- Absorption coefficient (μa): The probability of light absorption per unit path length, typically measured in mm⁻¹. This parameter depends on the concentration of chromophores such as hemoglobin, melanin, and water in the tissue [42].
- Scattering coefficient (μs): The probability of light scattering per unit path length (mm⁻¹), determined by the density and size of cellular structures, organelles, and other tissue components [42].
- Anisotropy factor (g): The average cosine of the scattering angles, ranging from -1 (perfect back-scattering) to +1 (perfect forward-scattering), with most biological tissues exhibiting strong forward scattering (g > 0.8) [42].
- Refractive index (n): Determines how light bends when passing between different media and affects reflection at boundaries according to Fresnel's equations [42].
These optical properties form the foundation upon which light source definitions operate, influencing how light from any source will ultimately be distributed within the tissue.
Light sources in MC simulations can be systematically categorized based on their geometric properties, which determine their initial conditions and computational implementation. The table below outlines the primary classifications and their characteristics.
Table 1: Geometric Classification of Light Sources in Monte Carlo Simulations
| Category | Source Type | Characteristics | Typical Applications |
|---|---|---|---|
| Point Sources | Pencil Beam | Highly directional, infinitesimal point origin [43] | Benchmark simulations, validation studies [46] |
| Isotropic Beam | Radiates equally in all directions [43] | Internal light sources (bioluminescence) [42] | |
| Cone Beam | Uniformly expands in a conical shape [43] | Endoscopic applications, focused delivery | |
| Arcsine | Wide viewing angle with cosine-squared distribution [43] | Specific illumination profiles | |
| Line Sources | Traditional Line | Photons emitted along a 1D line segment [43] | Slit-based imaging systems |
| Slit Source | Variant of line source with specific boundary conditions [43] | Dermatology, spectroscopy | |
| Surface Sources | Collimated Gaussian | Bell-shaped intensity profile, parallel rays [43] | Standard laser illumination |
| Angular Gaussian | Gaussian distribution over specific zenith angle [43] | Directional diffuse sources | |
| Planar | Uniform emission across a 2D surface [43] | Wide-field illumination | |
| Disk | Uniform emission from circular area [43] | Optical fiber delivery | |
| Fourier | Spatial frequency domain imaging [43] | Structured illumination imaging |
Advanced and Application-Specific Source Types
Beyond the basic geometric classifications, specialized source types have been developed to address specific research needs and experimental configurations:
Multi-angle wide-field illumination: Sources such as ring, cylindrical, and hemispherical geometries are employed in optoacoustic imaging systems to provide uniform illumination from multiple angles [47]. These complex sources require specialized MC implementations that can simultaneously generate random initial positions and directions for emitted photons.
Spatial frequency domain sources: Implementing 1D and 2D Fourier source types enables structured illumination imaging, where sinusoidal patterns at varying spatial frequencies are projected onto tissue surfaces to extract optical properties with enhanced resolution [43].
Oblique illumination sources: Sources with tilted incident angles relative to the tissue surface normal provide sensitivity to superficial tissue layers and are used in specialized probe geometries for reflectance spectroscopy [30].
Diagram 1: Classification hierarchy of light sources used in Monte Carlo simulations, showing the relationship between major categories and specific source types.
Implementing Source Definitions: Methodologies and Protocols
Mathematical Representation of Common Source Types
Each light source type requires precise mathematical definition to ensure accurate implementation in MC codes. The fundamental parameters include:
Pencil beam: Represented as an infinitesimally small point source emitting photons in a single direction, often defined as ( \delta(x-x0)\delta(y-y0)\delta(z-z_0) ) with initial direction vector ( \vec{v} = (0, 0, 1) ) for normal incidence [46].
Isotropic point source: Emits photons uniformly in all directions, with the direction vector given by ( \vec{v} = (\sin\theta\cos\phi, \sin\theta\sin\phi, \cos\theta) ), where ( \theta = \cos^{-1}(1-2R1) ) and ( \phi = 2\pi R2 ), with ( R1, R2 ) being random numbers uniformly distributed in [0,1] [42].
Gaussian beam: The intensity profile follows ( I(r) = I0 \exp(-2r^2/w0^2) ), where ( w_0 ) is the beam waist radius and ( r ) is the radial distance from the beam center [43]. The initial positions of photons are sampled from this distribution.
Ring source: For a ring of radius ( r ) in the plane ( z = z0 ), initial positions are given by ( \vec{rs} = (r\cos(2\pi R0), r\sin(2\pi R0), z0) ) with direction vector ( \vec{vs} = (-\cos(2\pi R0), -\sin(2\pi R0), 0) ) pointing inward, where ( R_0 ) is a random number in [0,1] [47].
Convolution Methods for Complex Source Modeling
A powerful technique for modeling complex extended sources involves the convolution approach, where the response to a simple pencil beam is calculated and then convolved with the desired source distribution [48]. This method leverages the linearity of the RTE to efficiently compute results for arbitrary source geometries without repeating full simulations for each source configuration.
The convolution method follows a systematic workflow:
Pencil beam simulation: Run an MC simulation for an infinitesimally narrow pencil beam incident on the tissue model, recording the resulting spatial distribution of absorbed energy or fluence.
Angular convolution: For sources with divergence or specific angular distributions, convolve the pencil beam response over the emission solid angle.
Spatial convolution: Mathematically convolve the angle-convolved result with the desired spatial distribution of the extended source.
This approach is computationally efficient as it separates the costly MC simulation from the source definition variations, allowing researchers to explore different source geometries through post-processing rather than repeated simulations [48].
Diagram 2: Workflow for the convolution method, showing how complex source distributions are derived from fundamental pencil beam simulations through sequential convolution operations.
Case Study: Systematic Comparison of 16 Source Types in Brain Tissue
A recent systematic study demonstrates the practical implementation and comparison of multiple source types in a realistic tissue model [43]. The experimental protocol provides a template for rigorous source evaluation:
Table 2: Optical Properties of Brain Tissue Layers at 800 nm [43]
| Tissue Layer | Thickness (mm) | Absorption Coefficient μa (mm⁻¹) | Scattering Coefficient μs (mm⁻¹) | Anisotropy Factor g | Refractive Index n |
|---|---|---|---|---|---|
| Scalp | 3 | 0.018 | 19.0 | 0.9 | 1.37 |
| Skull | 5 | 0.016 | 16.0 | 0.9 | 1.43 |
| Cerebrospinal Fluid | 2 | 0.004 | 2.4 | 0.9 | 1.33 |
| Gray Matter | 4 | 0.036 | 22.0 | 0.9 | 1.37 |
Simulation Parameters and Methodology:
- Simulation tool: MC simulations performed using the open-source 'mcxlab' MATLAB toolbox [43].
- Photon count: 10⁸ photons per simulation to ensure sufficient statistical accuracy.
- Tissue model: Four-layer brain model with dimensions 14×14×14 mm³ and grid size of 0.1 mm.
- Source position: All sources centered at position (x = 7 mm, y = 7 mm, z = 0 mm) with photons propagating vertically in the depth-increasing direction.
- Evaluation metrics: Optical propagating depth, distribution width, and absorption energy in each tissue layer.
This systematic approach enabled quantitative comparison of 16 different source types, revealing significant variations in penetration depth and distribution characteristics, with important implications for optimizing brain imaging modalities such as fNIRS and PAI [43].
Successful implementation of light source definitions in MC simulations requires both conceptual understanding and practical computational tools. The table below summarizes key resources available to researchers.
Table 3: Essential Computational Tools for Monte Carlo Light Transport Simulation
| Tool/Resource Name | Type | Key Features | Application Context |
|---|---|---|---|
| MCML | Software | Standard for multi-layered tissues; includes convolution utility [48] | General purpose light transport in layered tissues |
| mcxlab | MATLAB Toolbox | GPU-accelerated, supports various source types [43] | Rapid prototyping in MATLAB environment |
| MCX | Software | GPU-accelerated, flexible source modeling [47] | High-performance 3D simulations |
| bsf-light | Python Package | Replication of beam-spread function model [46] | Fast simulations as alternative to MC |
| IAD Algorithm | Algorithm | Calculates optical properties from reflectance/transmittance [49] | Determining tissue optical properties |
| Digimouse Atlas | Tissue Model | Realistic heterogeneous mouse phantom [47] | Preclinical simulation validation |
Advanced Topics and Future Directions
Acceleration Techniques for Complex Source Simulations
The computational demand of MC simulations, particularly for complex source geometries, has driven the development of various acceleration techniques:
GPU parallelization: Modern MC codes like MCX and MCOAI leverage graphics processing units to simultaneously track thousands of photon paths, achieving speed improvements of 10-100× compared to CPU implementations [47].
Scaling methods: These techniques allow researchers to reuse photon trajectory data from a baseline simulation for different optical properties, dramatically reducing computation time for parameter studies [30].
Perturbation and hybrid methods: These approaches combine the accuracy of MC with the speed of analytical approximations for specific problem types [42].
Emerging Applications and Source Innovations
The evolving landscape of biomedical optics continues to drive innovation in light source modeling:
Quantitative optoacoustic imaging: Advanced source models for multi-angle illumination schemes are essential for accurate reconstruction of chromophore concentrations in deep tissues [47].
Optogenetics stimulation: Precise light source definitions enable optimization of neural stimulation patterns while minimizing unwanted heating effects [43] [46].
Non-medical applications: The principles of light source modeling in turbid media are finding applications in diverse fields, including agriculture—such as detecting internal defects in potatoes [49]—and environmental science—such as studying light utilization in corals [44].
As Monte Carlo methods continue to evolve, the precise definition of light sources remains fundamental to advancing both theoretical understanding and practical applications in tissue optics. The framework presented in this guide provides researchers with the systematic approach needed to implement, evaluate, and optimize light source definitions for their specific research challenges.
The accurate simulation of diffuse reflectance is a critical capability in biomedical optics, enabling researchers to non-invasively probe the structural and functional properties of biological tissues. This whitepaper delineates a comprehensive workflow grounded in Monte Carlo (MC) simulation methodologies, which have emerged as the gold standard for modeling light propagation in complex, turbid media. The stochastic nature of MC methods allows for the flexible simulation of photon transport, providing a robust numerical approach to solving the radiative transfer equation (RTE) where analytical solutions are often intractable [27]. Within the context of a broader thesis on light propagation in tissue, this guide transitions from theoretical principles to practical implementation, addressing the needs of researchers, scientists, and drug development professionals engaged in optical diagnostics and therapeutic applications.
The application of these simulations spans a significant range, from optimizing photodynamic therapy protocols [27] and guiding bone-related orthopedic surgeries [50] to estimating tissue optical parameters for diagnostic purposes. This document provides an in-depth technical guide, incorporating structured data presentation, detailed experimental protocols, and mandatory visualizations to equip practitioners with the necessary tools to implement these techniques effectively.
Theoretical Foundations of Light Transport
Light propagation in biological tissue is governed by the interplay of absorption, scattering, and reflection events. The fundamental equation describing this phenomenon is the Radiative Transfer Equation (RTE), an integro-differential equation that quantifies the radiance at a point in space and time [27]. For a homogeneous medium, the RTE can be expressed as:
[ (\frac{1}{c} \frac{\partial}{\partial t} + \boldsymbol{\omega} \cdot \nabla + \mut(\mathbf{r})) L(\mathbf{r}, \boldsymbol{\omega}, t) = \mus(\mathbf{r}) \int_{4\pi} p(\boldsymbol{\omega}, \boldsymbol{\omega}') L(\mathbf{r}, \boldsymbol{\omega}', t) d\boldsymbol{\omega}' + Q(\mathbf{r}, \boldsymbol{\omega}, t) ]
where:
- ( L(\mathbf{r}, \boldsymbol{\omega}, t) ) is the radiance at position ( \mathbf{r} ), in direction ( \boldsymbol{\omega} ), at time ( t ) [W·m⁻²·sr⁻¹],
- ( c ) is the speed of light in the medium [m/s],
- ( \mu_a ) is the absorption coefficient [mm⁻¹],
- ( \mu_s ) is the scattering coefficient [mm⁻¹],
- ( \mut = \mua + \mu_s ) is the total attenuation coefficient [mm⁻¹],
- ( p(\boldsymbol{\omega}, \boldsymbol{\omega}') ) is the scattering phase function [-],
- ( Q(\mathbf{r}, \boldsymbol{\omega}, t) ) is the source term [W·m⁻³·sr⁻¹].
The scattering phase function, ( p(\boldsymbol{\omega}, \boldsymbol{\omega}') ), is frequently approximated by the Henyey-Greenstein function, which is parameterized by a single value, the anisotropy factor ( g ), representing the average cosine of the scattering angle [51]. For many biological tissues in the near-infrared spectrum, ( g ) typically ranges from 0.8 to 0.98, indicating strongly forward-directed scattering. More recent studies have highlighted the importance of higher-order scattering quantifiers, such as ( \gamma ) and ( \delta ), which are functions of the second and third Legendre moments of the phase function, for accurately modeling reflectance at small source-detector separations (sub-diffusive regimes) [51].
While the Diffusion Approximation offers a simplified, deterministic solution to the RTE under specific conditions (e.g., when scattering dominates absorption and far from sources and boundaries), its accuracy diminishes at high absorption and high anisotropy [52]. This limitation underscores the necessity for MC methods in a wide array of practical scenarios.
Monte Carlo Workflow for Diffuse Reflectance
The core of MC simulation involves tracking a statistically significant number of photon packets as they undergo random walks through the medium, with each step size and scattering angle determined by sampling the probability distributions derived from the tissue's optical properties. The following workflow diagram illustrates the logical sequence of this process.
Diagram 1: Logical flow of a Monte Carlo simulation for light propagation, depicting the lifecycle of a single photon packet and the data collection process.
Workflow Description
The MC simulation workflow, as illustrated in Diagram 1, can be broken down into the following key stages:
Initialization: The simulation commences with the definition of all input parameters. This includes the optical properties (absorption coefficient ( \mua ), scattering coefficient ( \mus ), and anisotropy factor ( g )) of the medium, the geometry of the light source (e.g., infinitely narrow beam, flat field, or Gaussian profile), and the structure of the tissue (e.g., semi-infinite, multi-layered, or 3D heterogeneous) [25] [27]. For layered tissues, the refractive index, thickness, and optical properties of each layer must be specified.
Photon Packet Launch: A photon packet, assigned an initial weight (typically 1.0), is launched from the source in a specified direction. The launch position and direction are determined by the source geometry.
Photon Propagation Loop:
- Step Size Calculation: The distance the photon packet will travel before interacting with a scatterer or absorber is computed. This step size, ( s ), is sampled from an exponential probability distribution: ( s = -\ln(\xi)/\mu_t ), where ( \xi ) is a uniformly distributed random number between 0 and 1.
- Absorption and Weight Update: The photon packet's weight is decremented by a factor proportional to the absorption coefficient at its current location. The deposited weight is recorded in a spatial grid for later calculation of the fluence rate.
- Boundary Interaction: The photon packet's path is checked for intersections with internal or external boundaries. If a boundary is encountered, the probability of reflection or transmission is calculated using Fresnel's equations, and the packet's direction and weight are updated accordingly [51].
- Scattering: The photon packet is redirected into a new propagation direction. The azimuthal angle is sampled uniformly from ( 0 ) to ( 2\pi ), while the deflection (polar) angle is sampled from the scattering phase function (e.g., Henyey-Greenstein).
Photon Termination: A photon packet is terminated using one of two methods. The Russian roulette technique is used when the packet's weight falls below a pre-defined threshold, randomly determining whether the packet is terminated or has its weight increased to continue propagation. Alternatively, the packet is terminated if it escapes the simulated volume and is not detected.
Data Collection and Repetition: When a photon packet is detected as reflected light, its weight and location (e.g., radial distance from the source) are recorded, contributing to the diffuse reflectance profile. Steps 2-5 are repeated for millions of photon packets to achieve a statistically significant result with low noise.
Post-processing: The raw data is processed to generate the final outputs, such as the spatially-resolved diffuse reflectance ( R(r) ), the total diffuse reflectance, or the internal fluence distribution ( \phi(z) ). Convolution techniques can be applied to results from an infinitely narrow beam to model the response to larger beam diameters [25].
Experimental Protocols and Validation
To bridge the gap between simulation and practical application, it is imperative to validate MC models against controlled experiments. The following section details a protocol for acquiring experimental diffuse reflectance spectra, a common validation benchmark.
Protocol: Extended-Wavelength Diffuse Reflectance Spectroscopy (EWDRS)
This protocol is adapted from recent work on animal tissues for bone-related biomedical applications [50].
1. Objective: To collect labeled, extended-wavelength DRS measurements from ex vivo biological tissue specimens for the purpose of model validation, machine learning training, and exploratory data analysis.
2. Materials and Reagents:
- Fresh Tissue Specimens: Ovine or porcine tissues (e.g., cortical bone, fat, muscle, brain), acquired and measured within a short post-slaughter window to preserve optical properties.
- Bone Cement Samples: For orthopedic application validation.
- Light Source: Tungsten-halogen lamp (e.g., 350–2400 nm wavelength range).
- Spectrometers: Dual-channel system covering ultraviolet to short-wave infrared (e.g., 355–1137 nm and 1095–1919 nm).
- Fiberoptic Probe: A bundle with a central illumination fiber and surrounding collection fibers, often held in a probe tip with specific reflective and epoxy fill properties [51].
- Data Acquisition Software: Custom or commercial software to control spectrometers and record signals.
3. Experimental Setup and Procedure:
- System Configuration: The light source illuminates the tissue surface via the central fiber of the probe. Back-scattered (diffusely reflected) light is collected by the detection fibers and guided to the two spectrometers for simultaneous detection across the broad wavelength range.
- Data Acquisition:
- Position the probe tip in gentle contact with the tissue specimen.
- For each measurement point, acquire multiple repeats (e.g., 5 repeats) to account for noise.
- Within each repeat, the visible/NIR spectrometer (355-1137 nm) might record 250 spectra with a short exposure time (e.g., 8 ms), while the SWIR spectrometer (1095-1919 nm) records a single spectrum with a longer exposure (e.g., 2 s) to achieve a sufficient signal-to-noise ratio.
- Measure tissues in a grid pattern (e.g., points ~5 mm apart) to account for spatial heterogeneity.
- Data Pre-processing:
- Perform dark current subtraction and calibration using a reflectance standard.
- Splice the spectra from the two spectrometers in their overlapping wavelength region (e.g., ~1095-1137 nm).
- Trim noisy spectral regions (e.g., beyond 1850 nm) [50].
4. Validation against MC Simulation:
- The experimentally measured diffuse reflectance spectrum is compared against a spectrum simulated using an MC model.
- The optical properties (( \mua ), ( \mus ), ( g )) of the tissue, which are wavelength-dependent, are used as inputs to the MC model.
- An inverse model is often employed: starting with an initial guess of the optical properties, the MC model is run iteratively, and its output is compared to the experimental data. The optical properties are adjusted until the simulated reflectance matches the measured data, thereby solving the inverse problem [27] [51].
Computational Tools and Performance
Various software implementations of the MC method are available, each with distinct features and optimizations. The table below summarizes key tools relevant to tissue optics research.
Table 1: Key Monte Carlo Simulation Software for Light Propagation in Tissues
| Software Name | Primary Features | Tissue Geometry | Language | Key References |
|---|---|---|---|---|
| MCML | Steady-state; infinitely narrow beam; multi-layered | Multi-layered, 2D axisymmetric | C | [25] [27] |
MCXYZ / mcxyz.c |
3D heterogeneous tissues; voxel-based | 3D heterogeneous (voxel cube) | C | [25] |
| CUDAMCML | GPU-accelerated version of MCML | Multi-layered, 2D axisymmetric | CUDA C | [25] |
| Fluorescent MC | Simulates fluorescence generation and propagation | Semi-infinite, slabs | C | [25] |
| Polarized Light MC | Tracks Stokes vector for polarized light propagation | Planar slab | Not Specified | [25] |
| tinymc.c / smallmc.c | Simple, educational codes for infinite/semi-infinite media | Infinite, Semi-infinite | C | [25] |
Selecting the appropriate tool depends on the specific research question. MCML is the most widely used for simulating diffuse reflectance from multi-layered tissues with radial symmetry. For complex 3D structures like brain tumors, MCXYZ is required [27]. When simulation speed is critical, especially for generating large training datasets for machine learning or solving inverse problems, GPU-accelerated implementations like CUDAMCML are indispensable.
Recent advances focus on overcoming performance bottlenecks. For instance, simulating a realistic optical fiber probe tip, which breaks radial symmetry, can slow simulations by over two orders of magnitude. One proposed framework uses an Artificial Neural Network (ANN)-based reflectance regression model (RRM) to map fast simulations from a simplified probe model to accurate results equivalent to those from a realistic model, dramatically reducing computation time [51].
The Scientist's Toolkit
Successful implementation of a diffuse reflectance simulation and validation pipeline requires a suite of essential materials and computational resources. The following table details key reagent solutions and materials used in the field.
Table 2: Essential Research Reagents and Materials for Experimental DRS
| Item Name | Function / Purpose | Example Specifications / Notes |
|---|---|---|
| Tissue-Mimicking Phantoms | Calibration and validation of systems and models; have well-defined optical properties. | Often composed of Intralipid (scatterer), India ink/ICG/Methylene Blue (absorber) [53]. Glass microspheres are an alternative scatterer, but may interact with some absorbers [53]. |
| Intralipid | A standardized lipid emulsion used as a scattering agent in liquid optical phantoms. | Provides a reproducible scattering background; concentration controls µs' [53]. |
| Absorbing Dyes | Introduce specific, tunable absorption features into phantoms. | India Ink (broadband), Indocyanine Green (ICG, ~800 nm peak), Methylene Blue (~660 nm peak) [53]. |
| Spectrometer | Detects the intensity of diffusely reflected light as a function of wavelength. | Often a dual-system: VIS/NIR (e.g., 355-1137 nm) and SWIR (e.g., 1095-1919 nm) [50]. |
| Tungsten-Halogen Lamp | Provides broadband, continuous spectrum illumination for reflectance spectroscopy. | Typical range: 350-2400 nm; power: ~8.8 mW [50]. |
| Fiberoptic Probe | Delives illumination light to the sample and collects diffusely reflected light. | Configurations vary (e.g., single fiber, multi-distance linear array). Probe tip details (steel reflectivity, epoxy fill) are critical for accurate simulation [51]. |
| Reference Standard | A material with known, stable reflectance used for system calibration. | e.g., Spectralon, a material with ~99% diffuse reflectance across a broad spectrum. |
The workflow for simulating diffuse reflectance, anchored by Monte Carlo methods, provides a powerful and versatile bridge from theoretical light transport to practical biomedical application. This guide has outlined the foundational theory, detailed the step-by-step computational workflow, provided a validated experimental protocol for data acquisition, and cataloged the essential tools of the trade. As the field progresses, the integration of these simulations with machine learning for rapid inverse problem-solving [50] [51] and the development of increasingly efficient, GPU-based codes will further solidify MC simulation as an indispensable technology in the researcher's toolkit. By adhering to the structured approach described herein, scientists and drug development professionals can confidently employ these techniques to advance optical diagnostics, therapeutic monitoring, and our fundamental understanding of light-tissue interactions.
Sentinel lymph node (SLN) biopsy is a critical procedure for staging cancers like melanoma and breast cancer, but the conventional standard-of-care, which utilizes technetium-99m (Tc-99m) lymphoscintigraphy, presents significant limitations including radiation exposure, logistical challenges, and potential delays in surgical workflow [54]. Photoacoustic imaging (PAI), a hybrid modality that combines optical contrast with ultrasound resolution, has emerged as a promising, non-radioactive alternative for SLN mapping [55] [56]. The efficacy of PAI hinges on the efficient delivery of light to target chromophores, such as the exogenous contrast agent indocyanine green (ICG), within the SLN. Optimizing this light delivery is paramount for achieving sufficient imaging depth and signal-to-noise ratio (SNR) for robust clinical detection. This technical guide explores advanced light delivery strategies within the context of SLN detection, framed by the principles of Monte Carlo simulation for predicting and enhancing light propagation in tissue.
Core Principles of Light Delivery and the Role of Monte Carlo Simulation
In PAI, short pulses of laser light are delivered to biological tissue, where they are absorbed by chromophores, leading to thermoelastic expansion and the generation of acoustic waves [56]. The initial pressure of the photoacoustic wave, as shown in Equation 1, is directly proportional to the local optical fluence (F), among other factors [56]. Therefore, maximizing and controlling the fluence at the target depth is the fundamental goal of light delivery optimization.
Equation 1: Initial Photoacoustic Pressure
p₀ = Γ * η_th * μ_a * F
Where:
p₀= Initial pressureΓ= Grüneisen parameterη_th= Photothermal conversion efficiencyμ_a= Optical absorption coefficientF= Local optical fluence
Monte Carlo (MC) simulations are a cornerstone technique for modeling the stochastic propagation of light in turbid media like tissue. By simulating the random walks of millions of photons, these simulations can predict the spatial distribution of light energy, or fluence, within a complex, multi-layered tissue model [57]. This predictive capability is invaluable for:
- Probe Design: Informing the optimal placement, angle, and configuration of optical fibers on an ultrasound transducer to maximize fluence at the expected depth of SLNs [58].
- Safety Analysis: Modeling the energy density deposited in superficial tissues to assess and mitigate the risk of thermal damage, a critical consideration for clinical translation [59].
- Protocol Development: Providing a theoretical basis for selecting parameters such as illumination geometry and beam profile to ensure uniform light distribution across the field of view [58].
For example, MC simulations have demonstrated that a smaller light incident angle relative to the transducer surface results in higher light fluence in deep tissue, directly motivating the development of co-axial illumination probes over traditional side-illumination geometries [58].
Light Delivery Strategies for Deep-Tissue Imaging
Overcoming the rapid attenuation of light in tissue is the primary challenge in imaging deep-seated SLNs. The following table summarizes key optimization strategies for light delivery.
Table 1: Light Delivery Optimization Strategies for Deep-Tissue PAI
| Strategy | Technical Implementation | Impact on Imaging Performance |
|---|---|---|
| Co-axial Illumination | Use of acoustic reflectors (e.g., double-reflector design) to align the optical illumination path with the acoustic detection path perpendicular to the tissue surface [58]. | Reduces effective light travel distance to target; provides slower light fluence decay with depth and more uniform illumination for uneven surfaces [58]. |
| Dynamic Light Delivery | Mechanically displacing the light source in a controlled, continuous circular motion (e.g., 1.5-mm radius) during imaging [59]. | Reduces local energy density and minimizes thermal damage (e.g., 80% reduction in hemorrhage depth) without statistically significant loss in SNR or gCNR [59]. |
| Dual-Wavelength Excitation | Employing two specific laser wavelengths (e.g., 800 nm and 860 nm) for ratiometric imaging of exogenous contrast agents like ICG [54] [60]. | Enables spectroscopic separation of the ICG signal from the background absorption of endogenous chromophores like hemoglobin and melanin, enhancing contrast and specificity [54]. |
Experimental Protocol: Double-Reflector Co-axial Illumination
The following workflow details the methodology for evaluating a double-reflector probe, a key co-axial illumination design.
Objective: To compare the imaging depth and uniformity of a double-reflector co-axial illumination system against a conventional side-illumination system [58]. Materials:
- Linear array ultrasound transducer (e.g., 5-8 MHz center frequency).
- Pulsed laser source (e.g., Nd:YAG laser with OPO).
- Double-reflector probe assembly (integrating transducer and parallel fiber bundles).
- Tissue-mimicking phantom: India ink-filled tubes embedded at 1 cm intervals (1-4 cm depth) in a scattering medium of 99.99% milk and 0.01% ink.
Procedure:
- System Setup: Assemble the double-reflector probe, ensuring the optical fibers are parallel to the transducer and the laser path is perpendicular to the transducer surface.
- Phantom Imaging: Immerse the probe in a coupling medium (water or gel) and scan over the phantom. Acquire PA data using identical laser parameters for both the double-reflector and side-illumination systems.
- In Vivo Imaging: Image a volunteer's forearm to visualize vascular structures. Scan an area of approximately 3.4 cm × 3.8 cm.
- Data Processing: Reconstruct depth-encoded maximum amplitude projection (MAP) images. Quantify the maximum imaging depth and signal-to-noise ratio (SNR) for both systems.
Expected Outcome: The double-reflector system should demonstrate a significantly greater imaging depth (e.g., 4 cm vs. 1.5 cm in phantoms) and reveal deeper vascular structures (e.g., 15 mm vs. 9 mm in vivo) compared to side-illumination, due to reduced fluence decay [58].
Application in SLN Detection: A Clinical Workflow
The integration of optimized light delivery is best understood in the context of a clinical SLN mapping procedure using ICG. The following diagram and table outline the end-to-end workflow and the essential research reagents involved.
Table 2: Research Reagent Solutions for SLN PAI
| Item | Function & Rationale |
|---|---|
| Indocyanine Green (ICG) | Exogenous contrast agent; absorbs strongly in the near-infrared spectrum, allowing deep tissue penetration and providing high contrast for SLN against the background [54]. |
| Dual-Wavelength Laser System | Light source capable of rapid switching between 800 nm and 860 nm; 800 nm is near ICG's peak absorption, while 860 nm is used for ratiometric imaging to suppress background from hemoglobin and melanin [54]. |
| Co-axial PAI Probe (e.g., Double-Reflector) | Integrated ultrasound and light delivery probe; its co-axial design maximizes light fluence at the SLN depth, which is crucial for generating a strong PA signal from ICG [58]. |
| Clinical Ultrasound Scanner | System for receiving and processing radio-frequency ultrasound data; synchronizes with the laser for PA data acquisition and can provide concurrent coregistered ultrasound images [55]. |
Experimental Protocol: ICG-Enhanced Dual-Wavelength SLN Mapping
This protocol is based on a recent clinical feasibility study [54].
Objective: To preoperatively map SLNs in patients with melanoma or breast cancer using ICG-enhanced, dual-wavelength PAI as an alternative to lymphoscintigraphy. Materials:
- Clinical PAI system with a linear array transducer.
- Tunable pulsed laser or laser system capable of emitting at 800 nm and 860 nm.
- Sterile Indocyanine Green (ICG) solution.
- Ultrasound gel for coupling.
Procedure:
- ICG Administration: Inject a standardized dose of ICG peritumorally or around the biopsy cavity.
- Waiting Period: Allow 15-60 minutes for ICG to migrate via lymphatic vessels to the SLN.
- Image Acquisition: Position the PAI probe over the expected lymphatic basin. Acquire coregistered PA data sequentially at 800 nm and 860 nm wavelengths. The laser fluence must remain within safety standards (e.g., < 20 mJ/cm² at skin surface).
- Ratiometric Processing: Process the acquired data to generate a ratiometric image (e.g., PA800/PA860). This algorithm suppresses signals from hemoglobin and melanin, leaving an ICG-specific signal map.
- SLN Identification: Identify the SLN in the resulting PA map as a localized region of high ICG-specific signal. Coregister this with the B-mode ultrasound image for anatomical context. The location can be marked on the skin for surgical guidance.
Key Quantitative Outcomes: In a clinical study, this method successfully identified 7 out of 11 SLNs with a maximum detection depth of 22 mm, demonstrating feasibility as an alternative to Tc-99m [54].
Optimizing light delivery is not merely an engineering improvement but a fundamental requirement for unlocking the full clinical potential of photoacoustic imaging in sentinel lymph node detection. Strategies such as co-axial illumination via reflector-based probes, motion-based dynamic light delivery for enhanced safety, and dual-wavelength excitation for specific contrast agent mapping have demonstrated significant improvements in imaging depth, signal quality, and patient safety. The use of Monte Carlo simulations provides a rigorous theoretical foundation for designing and validating these optimized light delivery systems. As these technologies continue to mature and integrate with clinical workflows, non-radioactive, photoacoustic SLN mapping is poised to become a viable and superior standard of care in oncologic surgery.
Optical techniques, such as optogenetic stimulation and calcium imaging, are key tools in modern neuroscience for manipulating and recording neuronal signals in the brain [61] [62]. Optogenetics enables precise control of genetically targeted neurons using light, offering significant advantages over electrical stimulation by providing higher spatial resolution and minimizing off-target effects [62]. However, a critical challenge persists: as light travels through neural tissue, it undergoes scattering and absorption, distorting the intended illumination profile and potentially compromising experimental precision [63]. Accurately modeling this light propagation is therefore fundamental to designing effective optogenetic experiments and interpreting their results.
Monte Carlo (MC) simulations are widely considered the "gold standard" for modeling light transport in turbid media like biological tissues due to their ability to accurately represent stochastic photon interactions [64] [3]. Despite their accuracy, MC methods are computationally expensive, often requiring substantial time and resources, which limits their utility for rapid prototyping and parameter exploration [61] [46]. To address this limitation, the Beam Spread Function (BSF) has been proposed as an efficient and accurate alternative for modeling light propagation, offering a more computationally tractable approach without sacrificing critical predictive capabilities [61] [65]. This whitepaper explores the integration of the BSF framework within the broader context of Monte Carlo-based research for advancing optogenetic applications.
Theoretical Foundations: From Pencil Beams to the Beam Spread Function
The Core Concept of the Beam Spread Function
The Beam Spread Function (BSF) describes the radiant intensity distribution resulting from a collimated beam of light as it propagates through an absorbing and scattering medium [65]. In essence, it quantifies how a perfectly directed beam "spreads out" due to interactions with the tissue. A closely related concept is the Point Spread Function (PSF), which describes the image of an ideal point source formed by an optical system after transmission through a scattering medium. For non-coherent imaging systems, the image formation process is linear in intensity, and the resulting image can be described as the convolution of the original object with the PSF [66]. Notably, under the principle of electromagnetic reciprocity, the BSF and PSF are numerically equivalent, meaning they contain the same fundamental information about light propagation in a given medium [65].
The BSF model implemented by Yona et al. and subsequently replicated and improved by Berling et al. utilizes a fundamental building block known as an infinitesimal pencil beam [61] [46]. This abstract representation models photons emitted from an infinitesimal point along a single direction (typically the z-axis). The model separates the light intensity at any point in the tissue (expressed in cylindrical coordinates ρ, z) into two distinct components:
Direct (un-scattered) photons: These photons travel from the source to the point without any scattering events. Their contribution is described by:
I_direct(ρ,z) = exp(-(μ_a + μ_s) * z) * δ(ρ)Here,μ_aandμ_sare the absorption and scattering coefficients, respectively, andδ(ρ)is the Dirac delta function, representing the infinitesimal width of the direct beam [61] [46].Scattered photons: This component accounts for photons that have been scattered at least once before reaching the point. Their contribution is more complex and is given by an integral over all possible multi-path times (τ), which represents the additional time taken due to scattering:
I_scatter(ρ,z) = ∫ [ (1 - exp(μ_s * z)) * exp(-μ_a * (z + c * τ)) * G(τ, z) * h(τ, ρ, z) ] dτThe functionG(τ, z)describes the distribution of multi-path times, whileh(τ, ρ, z)is a spatial-angular distribution function [61] [46]. The multi-path time moments required forG(τ, z)can be derived from the optical properties of the tissue, specifically the scattering coefficientμ_sand the anisotropy factorg[61].
From a Pencil Beam to a Practical Light Source
An optical fiber, a common tool in optogenetics, does not emit a single pencil beam but a cone of light. The model constructs this realistic emission profile through a two-step process:
- Angular Convolution: A light cone is formed by superposing an infinite number of pencil beams, uniformly distributed over the spherical cap defined by the optical fiber's numerical aperture (NA). This is a convolution over the azimuthal (φ) and polar (θ) angles [61].
- Spatial Convolution: The final model of light from a disk-shaped optical fiber is then generated by convolving the light cone over the physical emission surface of the fiber core [61] [46].
Table 1: Key Optical Properties for Modeling Light Propagation in Neural Tissue
| Parameter | Symbol | Typical Value/Example | Description |
|---|---|---|---|
| Absorption Coefficient | μ_a |
0.00006 μm⁻¹ [61] | Probability of light absorption per unit length. Related to tissue composition. |
| Scattering Coefficient | μ_s |
0.0211 μm⁻¹ [61] | Probability of light scattering per unit length. |
| Anisotropy Factor | g |
0.86 [61] | Measures scattering directionality; g=1 is perfectly forward-scattering. |
| Reduced Scattering Coefficient | μ'_s |
μ'_s = μ_s * (1 - g) [3] |
The effective scattering coefficient after accounting for anisotropy. |
| Refractive Index | n_tissue |
1.36 [61] | Determines the speed and bending of light within the tissue. |
| Penetration Depth | σ |
~6.73 mm (healthy potato @805 nm) [3] | Depth at which light intensity drops to 1/e (~37%) of its initial value. |
BSF vs. Monte Carlo: A Comparative Analysis
The Monte Carlo Gold Standard
Monte Carlo methods simulate light propagation by tracking the random walks of individual photons as they travel through tissue. Each photon's path is a stochastic process determined by the tissue's optical properties. Key steps in MC simulation include [64]:
- Randomly selecting the distance to the next interaction point based on the total attenuation coefficient.
- Transporting the photon to that location.
- Randomly determining the interaction type (absorption or scattering) based on partial cross-sections.
- If scattered, sampling a new direction from the phase function.
- Tracking the photon until it is absorbed, escapes the geometry, or its statistical weight becomes negligible.
MC methods are highly accurate because they can faithfully represent complex geometries and interaction statistics. They are particularly valuable for modeling the effects of discrete, strong scatterers like cell nuclei in brain tissue, which dramatically impact the light distribution [63]. However, this accuracy comes at a high computational cost, requiring the simulation of millions of photon histories to achieve statistically robust results [61] [46].
BSF as an Efficient Alternative
The BSF approach offers a different paradigm. Instead of tracking individual particles, it uses a probabilistic framework to describe the collective behavior of light. The replication of the Yona et al. model demonstrated that the BSF approach could achieve high prediction accuracy compared to MC models and experimental data, but with superior computational efficiency [61] [46]. The open-source replication by Berling et al. further enhanced this efficiency, enabling simulations of cortical volumes exceeding 1 mm³ to run in seconds on standard laptop hardware [61].
Table 2: Comparison of Light Simulation Techniques for Neural Tissue
| Feature | Monte Carlo Simulation | Beam Spread Function (BSF) |
|---|---|---|
| Underlying Principle | Stochastic tracking of individual photon packets [64]. | Analytical-probabilistic model based on pencil beam spreading [61]. |
| Computational Demand | Very high; requires significant resources for statistical accuracy [61] [46]. | Low to moderate; efficient enough for standard laptops [61]. |
| Accuracy | Considered the "gold standard" [3]; handles discrete scatterers well [63]. | High accuracy when validated against MC and experiments [61]. |
| Flexibility | High; can model complex geometries and heterogeneous tissues [63]. | Moderate; typically assumes homogeneous tissue properties. |
| Primary Use Case | Benchmarking, validation, and modeling complex/scattering-rich environments [63]. | Rapid prototyping, parameter screening, and applications requiring fast results [61]. |
| Accessibility | Requires expertise and computational resources; various software exists. | Improving with new open-source, FAIR-compliant implementations [61] [46]. |
Diagram 1: BSF Model Workflow. This diagram illustrates the sequential steps to model light from an optical fiber using the BSF approach.
Practical Implementation and Experimental Protocols
Protocol: Replicating and Using a BSF Model
The following methodology is based on the open-source replication of the Yona et al. model, which provides a practical tool for researchers [61] [46].
- Software Acquisition: Obtain the open-source Python package
bsf-light, available via the Python Package Index (PyPI) or Zenodo [61] [46]. - Parameter Definition: Configure the optical properties of the neural tissue and the light source.
- Tissue Properties: Define the absorption coefficient (
μ_a), scattering coefficient (μ_s), anisotropy factor (g), and refractive index (n_tissue). These can be taken from literature or experimentally measured. - Source Properties: Define the optical fiber's numerical aperture (NA) and core radius.
- Simulation Volume: Set the maximum radial distance (
xymax), depth (zmax), and step sizes (dxy,dz) for the output volume [61].
- Tissue Properties: Define the absorption coefficient (
- Numerical Calculation:
- The software calculates the direct component analytically.
- The scattered component is computed by numerically integrating over multi-path time (
τ), typically using logarithmic sampling for efficiency (n_tau_smpls=100). - Both components are convolved over the fiber's angular and spatial profiles using numerical integration with specified step sizes (e.g.,
nsteps_theta=24,nsteps_phi=24) [61] [46].
- Simulation Execution: Run the simulation, which outputs a 3D map of light intensity within the defined volume.
- Validation (Critical): Validate the BSF model results against a gold-standard Monte Carlo simulation for a specific set of parameters to ensure accuracy within acceptable bounds for your application [61].
Protocol: Validating a BSF Model Using Monte Carlo
This protocol outlines how to validate the output of a BSF model, a crucial step before relying on it for experimental design.
- Define a Benchmarking Scenario: Choose a specific set of tissue optical properties and source parameters.
- Run Monte Carlo Simulation:
- Use a well-established MC code (e.g., MCX - Monte Carlo eXtreme [3]).
- Configure the simulation geometry and optical properties to match the benchmarking scenario.
- Simulate a large number of photon packets (e.g., 10⁸ or more) to ensure low statistical noise [64] [3].
- Output the resulting 3D fluence rate or intensity map.
- Run BSF Simulation: Execute the BSF model for the identical benchmarking scenario.
- Quantitative Comparison:
- Extract 1D profiles (e.g, lateral spread at a specific depth, axial decay along the center) from both simulation outputs.
- Calculate quantitative metrics such as the root-mean-square error (RMSE) or the Pearson correlation coefficient (R²) between the MC and BSF results.
- A study replicating the Yona et al. model found high prediction accuracy when compared to MC simulations [61].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Modeling and Experimentation in Optogenetics
| Tool / Reagent | Type | Function & Application |
|---|---|---|
| bsf-light Python Package | Software | An open-source implementation of the BSF model for rapid simulation of light propagation in cortical tissue [61]. |
| Monte Carlo eXtreme (MCX) | Software | A high-performance, open-source MC simulator for 3D light transport in complex tissues; used as a gold standard for validation [3]. |
| Spatial Light Modulator (SLM) | Hardware | Used to "sculpt" light in 3D, creating specific illumination patterns (e.g., multiple foci) for optogenetic stimulation [63]. |
| Channelrhodopsin-2 (ChR2) | Protein | A light-sensitive ion channel used as an optogenetic actuator. Activated by blue light (~470 nm) to depolarize neurons [62]. |
| Opsins with Fast Kinetics (e.g., CheTA) | Protein | Engineered opsins with faster channel-closing kinetics than ChR2, enabling stimulation at higher frequencies (>200 Hz) [62]. |
| Laguerre-Gauss (LG) Beams | Optical Beam | Beams carrying Orbital Angular Momentum (OAM); studies suggest they may have higher transmittance through scattering tissues than standard Gaussian beams [67]. |
Diagram 2: Optogenetics Research Workflow. This diagram maps key tools to their roles in the optogenetics research pipeline.
The integration of Beam Spread Function modeling into the optogenetic toolkit represents a significant advancement for the field. While Monte Carlo simulations remain the undisputed benchmark for accuracy and are indispensable for understanding complex scattering environments and for final validation, the BSF approach provides a highly efficient and accessible alternative. The recent development of open-source, well-documented BSF software enables researchers to perform rapid, in-silico refinement of optical stimulator designs and accurately simulate the spatial reach of optogenetic stimulation on standard computing hardware [61]. This synergy between the efficient BSF and the rigorous MC framework empowers scientists to accelerate the development of precise optical interfaces, ultimately deepening our mechanistic understanding of brain circuitry and advancing therapeutic applications in neurostimulation.
Enabling Virtual Clinical Trials (VCTs) for Medical Imaging Device Validation
The development and regulatory approval of new medical imaging devices traditionally rely on extensive physical testing and clinical trials with human subjects. These processes are increasingly challenged by ethical limitations, high costs, lengthy timelines, and the difficulty of establishing ground truth in living systems [68]. Virtual Clinical Trials (VCTs), also known as in-silico trials, have emerged as a transformative methodology that uses computer simulations to evaluate medical device performance across virtual patient populations [69]. By replacing physical elements with computational models, VCTs provide researchers with precise controls and known ground truth that are impossible to achieve in clinical settings, enabling more efficient device optimization and validation while minimizing patient risk [68].
The accelerating complexity of medical imaging technology has outpaced traditional evaluation methods, creating a critical need for complementary validation approaches [68]. VCTs are particularly valuable for medical imaging devices that utilize light-tissue interactions, such as those employing photodynamic therapy, laser Doppler flowmetry, or near-infrared spectroscopy [70] [2]. Within this context, Monte Carlo (MC) simulation has established itself as the gold standard for modeling light propagation in biological tissues, providing a rigorous physical basis for simulating how imaging devices interact with virtual human anatomy [3] [71].
Core Components of a Virtual Clinical Trial Framework
Computational Anthropomorphic Phantoms
Computational phantoms serve as the virtual patient population in VCTs, providing the anatomical and physiological substrates upon which imaging simulations are performed. Unlike human subjects, these phantoms offer complete ground truth knowledge of internal anatomy, enabling precise validation of imaging device performance [68]. The table below summarizes the three principal categories of computational phantoms used in VCTs.
Table: Classification of Computational Phantoms for Virtual Clinical Trials
| Phantom Type | Anatomical Definition | Key Advantages | Primary Limitations |
|---|---|---|---|
| Mathematical Phantoms | Equations and geometric primitives [68] | Easy manipulation for anatomical variations and motion [68] | Limited anatomical realism [68] |
| Voxelized Phantoms | 3D cuboids from segmented medical images [68] | High anatomical accuracy based on real patient data [68] | Limited flexibility for anatomical changes; resolution-dependent [68] |
| Boundary Representation (BREP) | Advanced surface representations (NURBS, polygon meshes) [68] | Combines realism with mathematical flexibility [68] | Time-consuming segmentation process [68] |
| Tetrahedral Mesh Phantoms | Volumetric tetrahedral elements [68] | Direct input for MC codes; spatially varying material properties [68] | Computational complexity for detailed anatomy [68] |
Modern VCTs require phantoms that represent population diversity rather than single individuals. Recent advances have enabled the creation of extensive phantom libraries through deformation-based methods, where base phantoms are manipulated to match specific anthropometric characteristics such as height, weight, and body mass index [68]. Image registration techniques and deep learning algorithms for automatic multi-organ segmentation are further accelerating the development of diverse virtual patient populations, making large-scale VCTs statistically powerful and clinically relevant [68].
Imaging System Simulation Through Monte Carlo Methods
Monte Carlo simulations provide the physical engine for modeling light propagation from medical imaging devices through virtual patient anatomy. These methods treat light as discrete photon packets that undergo absorption, scattering, and boundary interactions (reflection and transmission) as they travel through biological tissues, with each interaction determined statistically based on the optical properties of the tissues [3] [2]. The fundamental physical principles underlying these simulations can be summarized through several key metrics:
- Absorption coefficient (μa): Represents the probability of photon absorption per unit path length, dependent on chemical composition including pigments, water content, and chromophores [3]
- Reduced scattering coefficient (μ's): Characterizes the scattering probability per unit path length, influenced by structural properties such as tissue density, porosity, and cellular organization [3]
- Penetration depth (σ): Defined as the depth at which incident light attenuates to 1/e (~37%) of its original intensity, calculated as σ = 1/√[3μa(μa+μ's)] [3]
- Anisotropy factor (g): Describes the preferred direction of scattering events, ranging from isotropic (g=0) to highly forward-directed scattering (g=1)
The accuracy of MC simulations in modeling light-tissue interactions has been extensively validated across multiple applications. For example, in assessing internal quality deterioration in agricultural products, MC simulations demonstrated significantly different light penetration characteristics between healthy and blackhearted potato tissues, with penetration depths of approximately 6.73 mm versus 1.30 mm at 805 nm respectively [3]. Similarly, in photodynamic therapy (PDT) planning for head and neck cancers, patient-specific MC simulations have enabled optimized light delivery to target tissues while sparing surrounding healthy structures [2].
Virtual Interpretation and Clinical Outcome Assessment
The final component of the VCT framework involves virtual interpretation of simulated imaging data and mapping to clinical outcomes. This typically involves encoding clinical decision-making logic based on consensus recommendations from clinical literature and establishing empirical correlations between simulated physics-based data and meaningful health-related outcomes [69]. For instance, in simulating stroke detection with electromagnetic tomography, the interpretation model would translate simulated dielectric property maps into diagnostic decisions about ischemic regions, which would then be mapped to predicted clinical outcomes such as recovery likelihood, hospitalization requirements, or mortality [69].
Monte Carlo Simulation Methodologies for Light Propagation
Fundamental Algorithms and Implementation Approaches
Monte Carlo simulation of light propagation in biological tissues follows a well-established stochastic framework where photon packets are tracked through a series of interactions until they are either absorbed, exit the tissue geometry, or their statistical weight becomes negligible [71]. The core algorithm involves four principal operations: propagation (hop), in which photons advance by a distance determined by the total attenuation coefficient; absorption (drop), where a portion of the photon weight is deposited in the local medium; scattering (spin), where the photon direction changes based on the scattering phase function; and boundary interactions, where Fresnel reflection and refraction occur at interfaces between materials with different refractive indices [71].
Table: Comparison of Monte Carlo Simulation Platforms for Biomedical Optics
| Platform Name | Core Methodology | Specialized Capabilities | Target Applications |
|---|---|---|---|
| MCML | Voxel-based with planar layers [70] | Standardized implementation for layered tissues [70] | Skin optics, superficial tissue measurements [70] |
| MCXYZ | General voxel-based medium interfaces [70] | Energy deposition simulation for thermal modeling [70] | Photothermal therapy, interstitial light applications [70] |
| MCX | Voxel-based with GPU acceleration [3] [7] | High-speed simulation of complex 3D volumes [3] | Heterogeneous tissues, patient-specific CT-based geometry [2] |
| mcxyzn | Enhanced voxel-based with gradient mapping [71] | Improved curved boundary handling via Sobel filtering [71] | Structures with significant curvature or oblique angles [71] |
| MC-Doppler | Voxel-free, vector-based ray tracing [70] | Doppler shift simulation for flowing media [70] | Laser Doppler flowmetry, lab-on-a-chip systems [70] |
Multiple implementation strategies have been developed to balance computational efficiency with anatomical accuracy. Voxel-based approaches represent tissue geometries as 3D grids of cuboidal elements, providing straightforward implementation and efficient memory usage but struggling with accurate representation of curved boundaries [71]. Tetrahedral mesh methods address this limitation by creating irregular meshes that better approximate curved surfaces, but require more complex mesh generation and ray-tracing algorithms [71]. Surface-based MC combines voxel-based propagation with explicit surface representations for boundary handling, while analytical geometry-based MC uses mathematical descriptions of tissue interfaces for highly accurate boundary representation at the cost of flexibility for complex anatomy [71] [70].
Advanced Techniques for Curved Boundary Handling
The discretization of curved anatomical surfaces into voxels introduces significant errors in modeling light-tissue interactions, particularly at boundaries where refractive index mismatches occur. Standard voxel-based MC methods approximate surface normals as aligned with the voxel facets, limiting them to six possible directions and resulting in inaccurate application of Fresnel equations [71]. Recent advances have addressed this limitation through gradient-based methods that estimate surface normals using 3D Sobel-Feldman operators, which calculate the spatial rate of change in refractive index across neighboring voxels [71]. These vector fields are subsequently smoothed to reduce discretization artifacts and better approximate true surface curvature, achieving angular errors as low as 1.36 degrees compared to maximum errors of 45 degrees with facet-normal approaches [71].
Alternative approaches abandon voxel-based representations entirely in favor of vector operations and analytical geometry. The MC-Doppler platform, for instance, uses mathematical descriptions of cylindrical and planar surfaces combined with ray-tracing algorithms to precisely calculate photon-boundary interactions without discretization artifacts [70]. This approach is particularly valuable for applications involving small-diameter tubes or tight curvatures, such as modeling light propagation through blood vessels or lab-on-a-chip microfluidic channels [70].
Acceleration Strategies and Computational Optimization
The computationally intensive nature of MC simulations has prompted development of numerous acceleration strategies. Graphics Processing Unit (GPU) implementation provides the most significant performance improvement, leveraging the massively parallel architecture of modern graphics cards to simulate millions of photon packets simultaneously [2]. Additional optimizations include photon packet termination when statistical weight falls below a predefined threshold, variance reduction techniques such as implicit capture where photons are not explicitly terminated but continue with reduced weight, and adaptive grid refinement that increases spatial resolution only in regions of interest [71] [2].
Experimental Protocols and Validation Methodologies
Standardized Protocol for VCT Execution
Implementing a rigorous Virtual Clinical Trial requires systematic execution through well-defined stages:
Define Clinical Question and Context of Use: Precisely specify the medical imaging device's intended use and the specific performance characteristics to be evaluated. For example, "Can electromagnetic tomography detect ischemic stroke based on dielectric images of the brain?" [69]
Develop Computational Device Model: Create a physics-based simulation of the imaging device that accurately represents its operational principles. For optical imaging devices, this typically involves implementing appropriate light sources (e.g., lasers, broad-spectrum sources), detection systems, and the governing physical equations (e.g., Maxwell's equations for EM propagation) [69]
Establish Virtual Patient Population: Generate a cohort of computational phantoms representing the target patient population, incorporating appropriate anatomical and physiological variability through statistical methods such as Vine Copula models or multiple imputation by chained equations (MICE) [69]
Implement Coupled Device-Tissue Model: Integrate the device model with patient anatomy to simulate their interaction, ensuring numerical stability and physical accuracy at their interface [69]
Execute Simulation and Record Outcomes: Run ensemble simulations across the virtual patient cohort, recording both the raw physical measurements (e.g., detected light intensity, spectral shifts) and derived clinical metrics [69]
Validate Against Experimental Data: Establish model credibility through hierarchical validation against benchtop experiments, phantom studies, and where available, limited clinical data [69]
The following workflow diagram illustrates the comprehensive VCT execution process:
Measurement of Tissue Optical Properties
Accurate characterization of tissue optical properties is fundamental to credible MC simulations. The standard methodology employs an integrating sphere system combined with the Inverse Adding-Doubling (IAD) algorithm to determine absorption and scattering coefficients across relevant wavelength ranges [3] [7]. The experimental protocol involves:
Sample Preparation: Tissue samples are sectioned into uniform slices (typically 1-3 mm thickness) using precision cutting tools. Samples should represent the anatomical regions of interest and be free of air bubbles or compression artifacts [3]
Reference Measurements: Baseline measurements are performed with the empty integrating sphere and with reference standards (typically Spectralon) to characterize system response [3]
Total Diffuse Reflectance (Rt) Measurement: The tissue sample is placed against the sphere's sample port with the light source illuminating the sample from outside the sphere, and reflected light is collected by a spectrometer [3]
Total Transmittance (Tt) Measurement: The sample is repositioned with the light source inside the sphere illuminating the sample, and transmitted light is measured [3]
IAD Algorithm Application: The measured Rt and Tt values are processed using the IAD algorithm to calculate the absorption coefficient (μa) and reduced scattering coefficient (μ's) at each wavelength [3]
This methodology has been successfully applied to characterize optical properties across diverse biological tissues, from potato tubers (for agricultural quality assessment) to human tissues (for medical device development) [3] [7].
Model Validation and Credibility Assessment
Establishing model credibility is essential for regulatory acceptance of VCT results. A hierarchical validation framework should address multiple levels:
- Component-Level Validation: Verify individual submodels against controlled experimental data. For example, validate optical property measurements against standard phantoms with known characteristics [69]
- Subsystem Validation: Test integrated model components, such as verifying light propagation algorithms in benchmark geometries with analytical solutions [69]
- System-Level Validation: Compare full simulation outputs against limited clinical studies or high-fidelity physical phantom experiments [69]
- Predictive Validation: Assess model ability to correctly predict outcomes outside the calibration dataset through prospective testing [69]
Quantitative validation metrics should include both physical measurements (e.g., mean squared error between simulated and measured reflectance, accuracy in predicting penetration depth) and clinical performance indicators (e.g., diagnostic sensitivity/specificity, detection thresholds) [3] [69].
Case Studies and Applications
Agricultural Product Quality Assessment
Monte Carlo simulations have demonstrated remarkable effectiveness in optimizing non-destructive quality assessment systems for agricultural products. In a comprehensive study of blackheart detection in potatoes, researchers measured optical properties of healthy and affected tissues using Vis-NIR spectroscopy with an integrating sphere system, then employed MC simulations to model light propagation [3]. The simulations revealed dramatically different penetration characteristics: healthy tissues permitted light penetration to approximately 6.73 mm at 805 nm, while blackhearted tissues limited penetration to only 1.30 mm at the same wavelength [3]. These findings informed the development of support vector machine discriminant analysis models that achieved 95.83-100% classification accuracy in cross-validation, demonstrating how MC simulations can guide optimal wavelength selection and detection geometry for maximum sensitivity to internal defects [3].
Similarly, in quality evaluation of Orah mandarins, MC simulations of light propagation through multi-layered fruit tissues (oil sac layer, albedo layer, and pulp) quantified the contribution of each layer to detected signals under different source-detector configurations [7]. The simulations revealed that transmitted photons accounted for less than 4.2% of total signal, with optimal source-detector distances of 13-15 mm maximizing pulp tissue contribution while maintaining sufficient signal strength [7]. This application demonstrates how MC methods can optimize detection system parameters for specific diagnostic tasks before physical prototype development.
Medical Device Development and Treatment Planning
In medical applications, MC simulations have been extensively applied to photodynamic therapy (PDT) planning, particularly for complex anatomical sites such as head and neck cancers [2]. Researchers have developed patient-specific MC models based on CT images that incorporate realistic representations of cylindrical diffusing fibers used for interstitial PDT [2]. These models enable precise calculation of light dose distributions in target tissues and surrounding critical structures, allowing clinicians to optimize fiber placement and treatment parameters before procedures [2]. The implementation of these models on GPUs provides near real-time simulation capabilities, making them practical for clinical workflow integration [2].
Laser Doppler flowmetry represents another area where MC simulations have contributed significantly to device development and signal interpretation. The MC-Doppler platform enables simulation of Doppler shifts from flowing media with fully customizable scattering phase functions and flow profiles, particularly valuable for through-transmission measurements in scattering samples like human milk [70]. By accurately simulating the relationship between flow characteristics and measured Doppler power spectra, these tools facilitate the development of quantitative flow measurement systems for biomedical applications ranging from lab-on-a-chip devices to clinical perfusion monitoring [70].
Table: Essential Computational Tools for Virtual Clinical Trials
| Tool Category | Specific Tools/Platforms | Primary Function | Application Context |
|---|---|---|---|
| Monte Carlo Simulation Platforms | MCX, MCML, mcxyzn, MC-Doppler [3] [71] [70] | Simulate light propagation in tissues | Device performance prediction, treatment planning [3] [2] |
| Computational Phantom Libraries | XCAT, UF Family, Virtual Population [68] | Provide anatomical models for virtual patients | Population-wide device validation [68] |
| Optical Property Measurement Systems | Integrating Sphere with IAD Algorithm [3] | Characterize tissue absorption and scattering coefficients | Model input parameterization [3] |
| GPU Computing Resources | NVIDIA CUDA, OpenCL [71] [2] | Accelerate computationally intensive simulations | High-throughput VCT execution [2] |
| Validation Frameworks | ASME V&V 40, FDA Digital Health Center of Excellence Guidance [69] | Establish model credibility for regulatory submission | Regulatory approval pathway [69] |
The following diagram illustrates the interconnected relationship between these toolkit components within a comprehensive VCT framework:
Virtual Clinical Trials supported by Monte Carlo light propagation simulations represent a paradigm shift in medical imaging device validation. By providing a computationally rigorous framework for evaluating device performance across diverse virtual populations, VCTs address critical limitations of traditional clinical trials while enhancing device optimization and patient safety. The integration of realistic computational phantoms with physics-based device simulations creates a powerful environment for assessing efficacy, optimizing design parameters, and establishing safety margins before first-in-human testing.
Future developments in VCT methodology will likely focus on several key areas: increased integration of artificial intelligence for both model generation and outcome analysis, enhanced multi-physics simulations coupling light propagation with thermal, mechanical, and biochemical processes, and development of standardized validation frameworks acceptable to regulatory bodies. As these computational approaches mature, VCTs are poised to become essential components of the medical device development pipeline, reducing time to market while improving device safety and efficacy through comprehensive virtual testing.
Optimizing MC Simulations: Managing Computational Cost and Improving Accuracy
In the field of biomedical optics, Monte Carlo (MC) simulations are widely regarded as the gold standard for modeling light propagation in biological tissues [72]. These simulations provide critical insights for diagnostic and therapeutic applications, from calculating light dose in photodynamic therapy to interpreting data from near-infrared spectroscopy [26]. At the heart of every Monte Carlo simulation lies a fundamental question: how many photon packets must be tracked to achieve statistically reliable results without incurring excessive computational costs? This trade-off between statistical uncertainty and computational expense represents a critical consideration for researchers designing simulation experiments for tissue optics, drug development research, and clinical protocol planning.
The core challenge stems from the statistical nature of the Monte Carlo method itself, which relies on tracking a finite number of photons through a medium where they undergo absorption and scattering events [26]. As with any statistical sampling approach, the precision of the results improves with the square root of the number of samples—in this case, photon packets. This paper provides a comprehensive technical framework for determining the optimal number of photons for Monte Carlo simulations in tissue optics, offering quantitative guidelines, detailed methodologies, and practical considerations for researchers across biomedical disciplines.
The Fundamental Trade-Off: Statistical Principles
Statistical Foundations of Monte Carlo Sampling
Monte Carlo simulations of light transport in biological tissues operate on the principle of statistical sampling of probability density functions (PDFs) that govern photon behavior [26]. Each photon packet undergoes a random walk through the simulated tissue, with step sizes between scattering events determined by sampling from an exponential distribution governed by the scattering coefficient (μs), and scattering angles determined by the anisotropy factor (g) [26]. The resulting light distribution is built from the aggregate paths of all simulated photons.
The statistical uncertainty in Monte Carlo results is inversely proportional to the square root of the number of photon packets simulated. This relationship follows the general principle of statistical sampling, where the standard error of the mean decreases as 1/√N, with N representing the number of independent samples. Consequently, to halve the statistical uncertainty, one must quadruple the number of simulated photons, leading to a rapid increase in computational demands.
Computational Cost Considerations
The computational cost of Monte Carlo simulations scales approximately linearly with the number of photon packets tracked. Each additional photon requires similar processing as it undergoes scattering, absorption, and potentially reflection or transmission events. However, the actual computation time per photon varies significantly based on tissue optical properties—highly scattering media with low absorption lead to longer photon paths and thus longer computation times per photon.
Modern approaches to managing this computational burden include GPU parallelization, which can accelerate simulations by orders of magnitude by tracking thousands of photons simultaneously [72]. Nevertheless, the fundamental trade-off remains: more photons yield better statistics but require more computational resources, whether measured in time, processing power, or energy consumption.
Quantitative Guidelines for Photon Numbers
General Recommendations for Different Application Scenarios
Based on analysis of current literature and simulation practices, the following table provides concrete recommendations for photon counts across different application scenarios in tissue optics research:
Table 1: Recommended Photon Numbers for Different Research Applications
| Application Scenario | Recommended Photon Count | Expected Statistical Uncertainty | Typical Computation Time | Key Considerations |
|---|---|---|---|---|
| Preliminary Testing | 10⁴ - 10⁵ | 1-3% | Seconds to minutes | Suitable for parameter space exploration and debugging simulation setups |
| Standard Dosimetry | 10⁵ - 10⁶ | 0.3-1% | Minutes to hours | Appropriate for most therapeutic dose calculations and general research [73] |
| Precision Spectroscopy | 10⁶ - 10⁷ | 0.1-0.3% | Hours to days | Required for Raman spectroscopy simulations and subtle spectral features [72] |
| Clinical Validation | 10⁷ - 10⁹ | <0.1% | Days to weeks | Necessary for protocol development requiring high statistical significance |
Specific Evidence-Based Recommendations
Recent research provides more specific guidance for particular applications. For medical linac beam calibration in radiation therapy, Monte Carlo uncertainty propagation studies have demonstrated that 10⁵ to 10⁶ simulations can achieve a 95% confidence interval of ±2.3% for photon beam calibration, which is considered clinically adequate [73]. These studies utilized the Mathematica programming environment and required approximately 1-2 seconds to complete 10⁶ calculations on a standard Core i7 laptop [73].
For Raman spectroscopy applications, which require modeling both Raman scattering and fluorescence background across a wide spectral range (800-2000 cm⁻¹), contemporary approaches using GPU-accelerated Monte Carlo implementations can achieve satisfactory results within approximately 20 minutes of computation time [72]. The exact photon requirements for these applications depend on the specific signal-to-noise ratio requirements and the complexity of the tissue model being simulated.
Methodological Framework for Determining Photon Numbers
Systematic Approach to Photon Count Determination
Researchers should adopt a systematic method for determining the appropriate number of photons for their specific application. The following workflow provides a structured approach:
Diagram 1: Photon Count Determination Workflow
Detailed Experimental Protocols
Convergence Testing Protocol
Convergence testing represents the most reliable method for determining appropriate photon counts for specific applications:
- Initialization: Run a preliminary simulation with 10⁴ photons to establish baseline metrics.
- Iterative Execution: Execute multiple simulations with increasing photon counts (e.g., 10⁴, 5×10⁴, 10⁵, 5×10⁵, 10⁶), ensuring identical simulation parameters except for photon count.
- Metric Tracking: For each run, record key output metrics such as:
- Fluence rate at regions of interest
- Reflectance or transmittance values
- Energy deposition in critical volumes
- Sampling volume or penetration depth statistics [74]
- Convergence Assessment: Calculate the relative difference between consecutive simulations for each metric. Convergence is typically achieved when relative differences fall below a predetermined threshold (e.g., 1% for preliminary studies or 0.1% for high-precision applications).
- Extrapolation: Use the observed convergence trend to estimate the photon count required to achieve the desired precision level.
Variance Estimation Protocol
Statistical uncertainty can be directly quantified through variance estimation:
- Multiple Runs: Execute 10-20 independent simulations with identical parameters and the same photon count.
- Statistical Analysis: Calculate the mean, standard deviation, and coefficient of variation (CV) for key output metrics across all runs.
- Precision Requirement Check: Ensure the CV meets the precision requirements of your application. If not, increase the photon count accordingly.
- Confidence Interval Establishment: Compute 95% confidence intervals for all metrics to quantify the statistical uncertainty.
This approach is particularly valuable for applications requiring rigorous uncertainty quantification, such as clinical protocol development or validation of experimental methods.
Computational Efficiency Optimization Strategies
Advanced Monte Carlo Techniques
Modern Monte Carlo implementations offer several strategies for maintaining statistical precision while reducing computational costs:
Table 2: Computational Efficiency Techniques
| Technique | Mechanism | Efficiency Gain | Implementation Considerations |
|---|---|---|---|
| GPU Parallelization | Simultaneous tracking of thousands of photons [72] | 10-100x acceleration | Requires specialized programming (CUDA, OpenCL) |
| "Isoweight" Method | Statistical generation of emission photons using inverse distribution method [72] | ~100x increase for Raman spectroscopy | Particularly effective for fluorescence and Raman simulations |
| Variance Reduction | Strategic weighting of photons in important regions | 2-10x acceleration | May introduce bias if improperly implemented |
| Multilayer Modeling | Optimized for layered tissues using MCML [25] | 3-5x acceleration | Limited to stratified tissue geometries |
Practical Implementation Considerations
When implementing efficiency strategies, researchers should consider:
- Hardware Selection: GPU acceleration typically provides the most significant performance improvements, with modern graphics cards capable of tracking millions of photons per second [72].
- Algorithm Selection: Choose specialized algorithms like MCML for layered tissues [25] or GPU-accelerated codes like MCX for complex heterogeneous tissues [72].
- Validation: Always validate that efficiency techniques do not introduce bias or artifacts in results, potentially by comparing with standard methods for a subset of cases.
- Resource Allocation: Balance computational resources between photon count and model complexity based on research priorities.
Software and Computational Tools
Table 3: Essential Monte Carlo Software Tools
| Tool Name | Primary Application | Key Features | Implementation Language |
|---|---|---|---|
| MCML | Multi-layered tissues [25] | Steady-state, well-validated | C |
| MCX | Heterogeneous tissues [72] | GPU acceleration, 3D voxel-based | CUDA/C++ |
| Monte Carlo eXtreme | General light transport [72] | Massive parallelization, efficiency | GPU/CUDA |
| mcsub.c | Basic slab geometries [25] | Simplicity, educational value | C |
| tiny_mc.c | Fundamental principles [25] | Single-page code, conceptual understanding | C |
Analytical and Validation Tools
Beyond simulation engines, researchers should employ appropriate analytical tools:
- Convergence Metrics: Scripts to calculate relative differences and coefficients of variation across simulation runs.
- Visualization Tools: Software for examining fluence distributions, such as the MATLAB scripts provided with MCML [25].
- Statistical Analysis Packages: Tools for computing confidence intervals and uncertainty propagation.
- Experimental Validation Protocols: Procedures for comparing simulation results with physical measurements using tissue phantoms [72].
Determining the appropriate number of photons for Monte Carlo simulations of light propagation in tissues requires careful consideration of statistical principles, computational resources, and research objectives. There is no universal number that serves all applications; rather, researchers must follow a systematic approach to balance precision and computational cost based on their specific needs.
The methodologies presented in this work provide a framework for making informed decisions about photon counts, from preliminary testing with 10⁴-10⁵ photons to high-precision clinical validation requiring 10⁷ or more photons. By employing convergence testing, variance estimation, and modern computational acceleration techniques, researchers can optimize their simulation protocols to yield statistically robust results within practical computational constraints.
As Monte Carlo methods continue to evolve with improved hardware acceleration and algorithmic sophistication [72] [75], the trade-offs between statistical uncertainty and computational cost will continue to shift. However, the fundamental principles outlined in this technical guide will remain relevant for researchers seeking to implement scientifically rigorous and computationally efficient light transport simulations in biological tissues.
Monte Carlo simulation has become the gold standard for modeling light propagation in biological tissues, a domain where exact analytical solutions to the radiative transport equation are often intractable for complex, heterogeneous media [1]. These simulations work by statistically modeling the random walks of countless photons as they travel through tissue, undergoing absorption, scattering, and boundary interactions [76]. While physically accurate, a significant drawback of this method is its characteristically slow convergence and high computational cost, as reducing the statistical uncertainty by half necessitates quadrupling the number of simulated particles [77].
Variance Reduction Techniques (VRTs) are a family of algorithms designed to mitigate this fundamental inefficiency. They manipulate the simulation to achieve a lower statistical error for the same computational cost, or conversely, the same error with less cost, without introducing systematic bias [78]. Within the specific context of a broader thesis on Monte Carlo simulation for light propagation in tissue research, two VRTs are of paramount importance: Russian Roulette and Particle Splitting. This technical guide provides an in-depth examination of these two core techniques, detailing their fundamental principles, implementation methodologies, and practical application within biomedical light transport studies.
Theoretical Foundations
Fundamentals of Monte Carlo Light Transport
In Monte Carlo simulations of light transport, photons or "photon packets" are traced through a defined tissue geometry. Their trajectories are a series of random steps, with each step length and scattering angle determined by sampling from probability distributions derived from the tissue's optical properties [76]. The key optical properties include:
- Absorption coefficient (μa): The probability of photon absorption per unit path length.
- Scattering coefficient (μs): The probability of photon scattering per unit path length.
- Anisotropy factor (g): The average cosine of the scattering angle, describing the directionality of scattering.
- Extinction coefficient (μt): The sum of the absorption and scattering coefficients (μt = μa + μs) [76] [79].
The probability that a photon travels a distance s without an interaction is described by an exponential distribution, ( p(s) = \mut e^{-\mut s} ), a direct consequence of the Beer-Lambert law [79]. A fundamental challenge in analog (unbiased) simulation is that many photons contribute little to the final measured signal—for instance, those absorbed deep within the tissue or scattered away from a detector. VRTs like Russian Roulette and Splitting address this by strategically reallocating computational resources.
The Principles of Russian Roulette and Splitting
Russian Roulette (RR) and Splitting are two sides of the same coin, both operating on the principle of weighted particles to maintain unbiased results while altering the number of simulated particles.
Russian Roulette is a particle-termination technique applied to paths with low expected contribution. When a photon packet's statistical weight falls below a predetermined threshold, it is given a chance ( p{rr} ) (e.g., 0.1) to survive. If it survives, its weight is increased by a factor of ( 1/p{rr} ); otherwise, it is terminated. This process preserves the average weight while saving computation on low-contribution paths [80] [1].
Particle Splitting is a particle-replication technique applied to paths with high expected contribution. Upon entering an important region or when its contribution is deemed high, a particle with weight W is split into ( Ns ) identical particles. Each new particle is assigned a weight of ( W/Ns ) and is tracked independently. This increases the number of samples in regions of interest, reducing local variance [81].
The following table summarizes the core attributes and objectives of these two techniques.
Table 1: Core Characteristics of Russian Roulette and Particle Splitting
| Feature | Russian Roulette (RR) | Particle Splitting |
|---|---|---|
| Primary Objective | Reduce computational cost by terminating low-contribution paths [80] | Reduce variance by increasing sampling in high-contribution regions [81] |
| Effect on Particle Count | Decreases | Increases |
| Typical Trigger | Low particle weight, deep within tissue, far from detector | High particle weight, entering a sensitive or scoring region |
| Weight Adjustment | Survival increases weight (( W{new} = W / p{rr} )) | Splitting reduces individual weight (( W{new} = W / Ns )) |
| Key Challenge | Premature termination of paths that might later contribute | Over-representation of correlated particle histories; can bias track structure analysis [81] |
Methodologies and Experimental Protocols
Implementation in Light Transport Simulations
Implementing RR and Splitting requires integrating decision points into the core photon-tracking loop. The following diagram illustrates a generalized workflow for a Monte Carlo simulation of light in tissue incorporating these VRTs.
Workflow Diagram Title: Monte Carlo Photon Transport with VRTs
The logic for applying these techniques can be based on several factors:
- Statistical Weight: The most common trigger for RR is the photon's weight falling below a threshold (e.g., 0.001) [1].
- Spatial Regions: Splitting can be triggered when a photon enters a specific tissue layer or a region of interest, such as a tumor volume.
- Path History: The number of scattering events (path depth) can inform decisions, as the contribution of deeply propagating photons often diminishes.
Advanced Protocols: Flagged Uniform Particle Splitting
In track structure simulations for nanodosimetry—where the precise spatial distribution of energy deposition events (e.g., for DNA damage studies) is critical—standard splitting can introduce bias. Split particles are correlated, and their combined interactions can be mistakenly classified as a single, dense cluster of events [81].
A sophisticated protocol to overcome this is Flagged Uniform Particle Splitting [81]. The experimental methodology is outlined below.
Table 2: Protocol for Flagged Uniform Particle Splitting in Track Structure Simulation
| Step | Action | Purpose & Details |
|---|---|---|
| 1. Region Definition | User defines a geometric "region of interest" (e.g., near a DNA fiber). | Confines splitting to where it is computationally most beneficial. |
| 2. Splitting Trigger | Apply splitting at the first ionization event caused by a secondary electron. | Focuses on the most impactful secondary particles; avoids complexity of repeated splitting. |
| 3. Particle Creation | The ionized electron is split into ( Ns ) electrons. The weight of each is set to ( W / Ns ). | Ensures energy conservation; the weighted sum of energies equals the original energy. |
| 4. Flag Assignment | Assign a unique SplitTrackID to every new split electron. This flag is inherited by all of its progeny. |
Allows for the identification of all particles originating from the same split event. |
| 5. Russian Roulette | Apply RR to low-energy secondaries. If energy < threshold, terminate with probability ( 1 - 1/Ns ) or keep with weight ( W * Ns ). | Prevents simulation from being bogged down by very low-energy, high-cost particles. |
| 6. Analysis & Reclassification | During analysis, use the SplitTrackID to reclassify ionization events from split tracks as belonging to separate, independent histories. |
Eliminates bias in cluster size counts by preventing correlated events from being over-counted as a single large cluster. |
This protocol was validated in TOPAS-nBio (a Geant4-DNA-based Monte Carlo tool) for simulating proton and carbon ion tracks. Results showed agreement within 1-2% of reference simulations without splitting, while significantly increasing computational efficiency [81].
Quantitative Performance Data
The effectiveness of VRTs is quantitatively measured by their relative efficiency, which can be defined as: [ \text{Relative Efficiency} = \left( \frac{1}{\text{Error}^2 \times \text{Time}} \right){\text{with VRT}} \ / \ \left( \frac{1}{\text{Error}^2 \times \text{Time}} \right){\text{without VRT}} ] A value greater than 1 indicates a net gain in efficiency.
Application of the flagged splitting protocol in nanodosimetry has demonstrated its significant value. The table below compiles key experimental results.
Table 3: Measured Relative Efficiency Gains from Particle Splitting in Nanodosimetry
| Simulation Endpoint | Radiation Type & Energy Trend | Relative Efficiency (at 128 split electrons) | Accuracy vs. Analog Simulation |
|---|---|---|---|
| Ionization Cluster Size Mean | 0.5-20 MeV Protons | Increased from 47.2 ± 0.2 to 66.9 ± 0.2 [81] | Within 1% (2 standard deviations) [81] |
| Ionization Cluster Size Mean | 1-20 MeV/u Carbon Ions | Decreased from 51.3 ± 0.4 to 41.7 ± 0.2 [81] | Within 1% (2 standard deviations) [81] |
| DNA SSB/DSB (DBSCAN) | 0.5-20 MeV Protons | Increased from 20.7 ± 0.1 to 50.2 ± 0.3 [81] | Within 1% (2 standard deviations) [81] |
| DNA SSB/DSB (DBSCAN) | 1-20 MeV/u Carbon Ions | Increased from 15.6 ± 0.1 to 20.2 ± 0.1 [81] | Within 1% (2 standard deviations) [81] |
| DNA SSB/DSB (Geometric) | 0.5-20 MeV Protons | Increased from 31.0 ± 0.2 to 58.2 ± 0.4 [81] | Within 2% (1 standard deviation) [81] |
The data shows that efficiency gains are highly dependent on the specific endpoint being scored and the type of primary radiation. The method is particularly effective for scoring complex biological damage like DNA strand breaks.
The Scientist's Toolkit
Successful implementation of these VRTs in light-tissue research relies on both software and conceptual tools. The following table details key resources.
Table 4: Essential Research Reagents and Computational Tools for VRT Implementation
| Tool Name / Concept | Type | Function in VRT Research |
|---|---|---|
| MCML | Software Code | A widely-used, standardized Monte Carlo program for light transport in multi-layered tissues. Serves as a trusted baseline for implementing and testing custom VRTs [25]. |
| GPU-Accelerated MCML (CUDAMCML) | Software Code | A version of MCML optimized for NVIDIA graphics cards. Drastically reduces simulation time, which is crucial for iterative testing and development of VRTs [25]. |
| Henyey-Greenstein Phase Function | Mathematical Model | The most common function used to sample scattering angles (anisotropy). It is integral to the scattering step in the Monte Carlo workflow [76] [1]. |
| TOPAS / TOPAS-nBio | Software Platform | A Monte Carlo simulation platform built on Geant4. It enables the implementation of advanced VRTs, like flagged splitting, for radiobiological studies [81]. |
| Statistical Weight (W) | Core Algorithm Variable | A floating-point number assigned to each photon packet representing its probabilistic strength. It is the fundamental variable manipulated by all weight-based VRTs [1]. |
| Beam Spread Function (BSF) | Analytical Model | An analytical approximation of light distribution. Can be used to validate the results of MC simulations with VRTs and to estimate optical parameters from measurements [1]. |
Within the rigorous framework of Monte Carlo simulation for light propagation in tissue, Russian Roulette and Particle Splitting stand as essential variance reduction techniques. Their strategic application allows researchers to reallocate finite computational resources from low-value photon paths to those that contribute significantly to the final observable—be it diffuse reflectance, fluorescence, or internal energy deposition. As demonstrated in advanced protocols like flagged splitting, these techniques can be implemented with careful safeguards to eliminate bias, even in highly sensitive applications like nanodosimetry and DNA damage simulation. Mastery of RR and Splitting is, therefore, not merely a computational optimization but a prerequisite for achieving statistically robust and computationally feasible results in complex, multi-scale biological light transport problems.
Handling Complex Geometries and Tissue Heterogeneities
Monte Carlo (MC) simulation has become an indispensable tool for modeling light propagation in biological tissues, a critical process for advancing therapeutic and diagnostic applications in medicine. While early models treated tissues as semi-infinite, homogeneous media, real-world clinical and research scenarios involve complex anatomical structures with intricate geometries and multi-layered compositions. These heterogeneities significantly influence light energy distribution, ultimately determining the efficacy of light-based therapies and accuracy of diagnostic methods. This technical guide examines contemporary methodologies for addressing these challenges within the framework of Monte Carlo modeling, providing researchers with practical approaches for enhancing simulation fidelity in biologically realistic contexts.
The accurate modeling of light-tissue interactions is particularly crucial in domains such as photodynamic therapy (PDT) and photothermal therapy (PTT), where precise light dosage directly correlates with treatment outcomes [57]. Furthermore, in drug development, advanced optical imaging techniques rely on understanding how light propagates through complex tissue structures to track drug distribution and target engagement at subcellular, cellular, and whole-organism levels [82]. This guide provides a comprehensive technical foundation for implementing Monte Carlo approaches that effectively handle geometrical complexity and tissue heterogeneity, with direct implications for therapeutic innovation and pharmaceutical development.
Computational Frameworks for Geometry Representation
Constructive Solid Geometry and Hybrid Approaches
The Monte Carlo N-Particle (MCNP) code exemplifies a robust approach for handling complex geometries through constructive solid geometry (CSG), where materials are defined within three-dimensional spaces bounded by first-, second-, and fourth-degree user-defined surfaces [83]. This method provides precise mathematical representations of geometrical boundaries, enabling accurate simulation of anatomical structures. For enhanced capability with irregular shapes, contemporary implementations support hybrid approaches that embed structured and unstructured meshes within CSG cells, offering an alternative pathway for defining complex anatomical geometries that defy simple mathematical description [83].
Voxel-Based and Tetrahedral Mesh Methodologies
For biological applications requiring anatomical accuracy from medical imaging data, voxel-based Monte Carlo methods have emerged as particularly valuable. The Monte Carlo eXtreme (MCX) framework employs voxel-based representations to study photon transmission patterns in heterogeneous tissues [7]. This approach enables direct translation of medical imaging data (CT, MRI) into simulation geometries, faithfully preserving anatomical complexity. For scenarios demanding higher computational efficiency with complex shapes, tetrahedral mesh-based implementations offer an advanced alternative, providing adaptive resolution that concentrates computational resources where most needed [84]. This flexibility makes tetrahedral approaches particularly suitable for simulating light transport in structures with curved surfaces and fine morphological details.
Table 1: Comparison of Geometry Representation Methods in Monte Carlo Simulation
| Method | Key Features | Advantages | Limitations | Representative Applications |
|---|---|---|---|---|
| Constructive Solid Geometry | Mathematical surface definitions | High precision for regular shapes | Complex to define irregular anatomy | Radiation dosimetry, detector design [83] |
| Voxel-Based | 3D grid of volume elements | Direct import from medical imaging | Stair-stepping artifacts at boundaries | Multi-layered fruit tissues, brain imaging [7] |
| Tetrahedral Mesh | Irregular 3D elements | Adapts to complex curved surfaces | Increased memory requirements | Complex-shaped turbid materials [84] |
| Hybrid CSG-Mesh | Combines CSG with embedded meshes | Balances precision and flexibility | Implementation complexity | Radiation transport in complex detectors [83] |
Modeling Approaches for Tissue Heterogeneities
Multi-Layered Tissue Architectures
Biological systems inherently exhibit layered structures with distinct optical properties at each organizational level. Research on Orah mandarin tissues provides an exemplary case study for modeling such heterogeneities, demonstrating a three-layer concentric sphere model comprising oil sac layer, albedo layer, and pulp tissue [7]. Each layer exhibits unique optical characteristics: the oil sac layer, rich in liposoluble pigments like carotenoids, shows peak absorption at 500 nm; the porous albedo layer displays higher reduced scattering coefficients; while the more translucent pulp tissue exhibits the lowest reduced scattering coefficient [7]. This hierarchical modeling approach directly translates to human tissues such as skin, which similarly comprises epidermal, dermal, and subcutaneous layers with distinct optical properties.
Monte Carlo simulations of such multi-layered systems reveal critical insights into light penetration dynamics. In the Orah mandarin model, light primarily absorbs within tissue, with transmitted photons accounting for less than 4.2% of the total [7]. Analysis of contribution rates shows that as source-detector distance increases, the signal contribution from superficial layers decreases while that from deeper layers increases, enabling optimization of detection parameters for specific tissue depths—a finding with direct relevance to transcutaneous measurement devices [7].
Inverse Methods for Optical Property Recovery
A significant challenge in heterogeneous tissue modeling lies in determining appropriate optical parameters for each tissue component. Inverse Monte Carlo methods have emerged as powerful approaches for addressing this challenge, enabling recovery of absorption and reduced scattering coefficients from measured data [84]. These methods employ physics-based inverse rendering that couples Monte Carlo simulation with optimization algorithms like Levenberg-Marquardt to iteratively adjust optical properties until simulated results match empirical observations [84].
This approach is particularly valuable for handling complex geometries where traditional measurement techniques face limitations. By leveraging edge effects like translucency and color gradients that arise in finite objects, inverse methods can differentiate between scattering and absorption contributions from just a single image [84]. For semi-infinite media, reflected light depends only on the quotient of μs and μa, but in geometrically complex samples, distinct edge phenomena provide the additional information necessary to separate these parameters during fitting procedures [84].
Experimental Protocols and Validation Methodologies
Protocol: Inverse Adding-Doubling for Optical Parameter Determination
The Inverse Adding-Doubling (IAD) method combined with integrating sphere measurements provides a standardized approach for determining baseline optical parameters of heterogeneous tissue components:
Sample Preparation: Prepare plane-parallel sections of specific tissue layers with uniform thickness. For biological tissues, cryosectioning often achieves the required geometrical precision while preserving optical properties [7].
Integrating Sphere Measurement: Place samples within a single integrating sphere system to measure total transmission, total reflection, and unscattered transmission across the target wavelength spectrum (typically 500-1050 nm for Vis/NIR applications) [7].
Parameter Recovery: Apply the IAD algorithm to the measured values to calculate the absorption coefficient (μa), scattering coefficient (μs), and anisotropy factor (g) for each tissue layer [7]. The reduced scattering coefficient is then derived as μs' = (1-g)μs.
Validation: Confirm results through comparison with established reference materials and by verifying that internal consistency checks within the IAD algorithm are satisfied.
Protocol: voxel-Based Monte Carlo Simulation for Heterogeneous Tissues
Implementing voxel-based MC simulation for complex, heterogeneous tissues involves the following methodological sequence:
Geometry Discretization: Convert the 3D tissue model into a voxelated grid, assigning each voxel optical properties (μa, μs, g, n) corresponding to the specific tissue type at that location [7].
Photon Injection: Launch photon packets from defined source positions with appropriate initial directionality, typically modeling optical fibers or laser sources relevant to the application.
Photon Transport: Simulate individual photon paths through the voxelated medium, at each step:
- Calculate interaction distance based on local total attenuation coefficient
- Determine collision type (absorption or scattering)
- Update photon weight based on absorption
- Change photon direction based on scattering phase function
- Apply boundary conditions at tissue interfaces [7]
Data Collection: Record photon positions, paths, and weights at specified detectors to simulate measurable signals such as diffuse reflectance.
Contribution Analysis: Quantify the relative contribution of different tissue layers to detected signals by tracking interaction statistics within each defined region [7].
Figure 1: Inverse Monte Carlo parameter recovery workflow using physics-based rendering and optimization.
Research Reagent Solutions for Optical Tissue Characterization
Table 2: Essential Materials and Computational Tools for Advanced Monte Carlo Studies
| Reagent/Software | Category | Function | Application Context |
|---|---|---|---|
| Single Integrating Sphere System | Measurement Hardware | Quantifies total transmission and reflection | Determining baseline optical properties of tissue samples [7] |
| Inverse Adding-Doubling Algorithm | Computational Method | Recovers μa, μs, and g from sphere measurements | Establishing reference optical parameters for simulation validation [7] |
| MCNP Code | Simulation Platform | General-purpose particle transport in complex 3D geometry | Medical physics, radiation dosimetry, detector design [83] |
| voxel-Based MCX | Specialized MC Software | Accelerated photon transport in heterogeneous media | Modeling light propagation in multi-layered biological tissues [7] |
| GPU-Accelerated MC | Computational Hardware | Massive parallelization of photon transport | Rapid simulation for iterative fitting procedures [84] |
| NIR-II Fluorophores | Contrast Agents | Enable deep-tissue optical imaging with reduced scattering | Tracking drug distribution in living systems [82] |
| Levenberg-Marquardt Algorithm | Optimization Method | Nonlinear least-squares parameter estimation | Inverse Monte Carlo for optical property recovery [84] |
Applications in Therapeutic and Diagnostic Development
Implications for Drug Development and Visualization
Advanced Monte Carlo methods directly impact pharmaceutical development by enabling precise tracking of drug distribution and target engagement. The integration of fluorescence imaging with accurate light propagation models allows researchers to monitor drug localization within living systems at multiple scales [82]. Super-resolution microscopy (SRM) reveals drug-target interactions at subcellular levels, while near-infrared II (NIR-II) imaging provides deeper tissue penetration for monitoring drug distribution in whole organisms [82]. These approaches are particularly valuable for validating targeted therapies, where understanding spatial distribution and temporal dynamics directly informs dosage optimization and treatment efficacy.
For instance, fluorescent labeling of drug compounds enables real-time observation of cellular uptake, subcellular localization, and metabolic processing [82]. MC simulations of light transport in heterogeneous tissues provide the essential foundation for interpreting these fluorescence signals, correcting for depth-dependent attenuation, and quantifying actual drug concentration from measured optical data. This capability is revolutionizing our understanding of pharmacokinetics and pharmacodynamics, particularly for drugs targeting specific organelles or cellular compartments.
Optimization of Therapeutic Applications
In light-based therapies including photodynamic therapy (PDT) and photothermal therapy (PTT), MC simulations of light propagation in complex anatomical geometries enable precise treatment planning and device optimization [57]. By accurately modeling how light distributes through heterogeneous tissues, clinicians can predict energy deposition patterns and adjust parameters to maximize target tissue exposure while minimizing damage to surrounding healthy structures [57]. This approach is particularly valuable for irregularly shaped tumors or tissues with complex layered structures.
Research in dermatology and oncology demonstrates how MC methods inform therapeutic device design through analysis of photon migration patterns [57]. For example, studies of source-detector distance optimization in diffuse reflectance measurements directly translate to improved detection geometries for clinical devices [7]. These advancements highlight the critical role of accurate light transport modeling in developing more effective and safer light-based therapeutic interventions.
Figure 2: Photon migration in multi-layered tissues showing depth-dependent contribution to detected signal at different source-detector distances.
The effective handling of complex geometries and tissue heterogeneities represents a critical frontier in Monte Carlo simulation of light propagation for biomedical applications. Through advanced geometry representation methods, multi-layer modeling approaches, and inverse parameter recovery techniques, researchers can now address biological complexity with unprecedented fidelity. These capabilities directly enhance drug development pipelines through improved visualization methodologies and optimize therapeutic outcomes through precise light dosimetry in anatomically accurate contexts. As computational power continues to grow and optical measurement techniques refine, Monte Carlo methods will increasingly serve as the fundamental bridge between theoretical models and clinical applications in photomedicine, ultimately enabling more effective, personalized light-based therapies and diagnostic approaches.
Overcoming Challenges in Modeling Anatomically Realistic Structures
The accuracy of Monte Carlo (MC) simulations for modeling light propagation in biological tissues is fundamentally constrained by the anatomical realism of the digital models used. Creating structurally precise, multi-layered tissue models remains a significant hurdle in biophotonics research. This guide details the methodologies for developing anatomically accurate models and integrating them into MC simulation frameworks, providing a robust foundation for advancing therapeutic and diagnostic applications, such as photodynamic therapy and cancer diagnostics [57] [2].
Core Challenges in Anatomical Modeling
Developing models that faithfully represent biological structures involves overcoming several key obstacles:
- Geometric Complexity: Biological tissues are rarely simple, homogeneous slabs. They often consist of multiple, curved layers with complex internal structures, such as subcutaneous veins or the distinct layers of fruit skin and pulp, which are difficult to voxelize accurately for MC simulations [85] [7].
- Optical Property Heterogeneity: Accurate MC simulations require the precise absorption coefficient (μa) and reduced scattering coefficient (μ’s) for each tissue type and layer. These properties vary significantly between tissue types and physiological states, as demonstrated by the notable increase in μa in blackhearted potato tissues compared to healthy ones [3].
- Data Acquisition and Processing: Translating clinical or experimental imaging data (e.g., CT, MRI) into a clean, watertight 3D mesh suitable for simulation is a non-trivial process. Automated segmentation of organs from DICOM data often requires manual refinement by medical experts to achieve sufficient accuracy [86] [87].
- Computational Demand: Simulating light propagation in large, high-resolution, and anatomically complex models using MC methods is computationally intensive. Leveraging GPU-accelerated MC platforms like Monte Carlo eXtreme (MCX) is often necessary to achieve practical simulation times [3] [2].
Methodologies for Developing Realistic Models
From Medical Imaging to 3D Digital Models
A proven workflow for creating accurate organ models utilizes open-source software and deep learning, facilitating the creation of models for surgical simulators, 3D printing, and augmented reality applications [86] [87].
Experimental Protocol:
- Software Required: 3D Slicer (with TotalSegmentator extension), Blender, and Python with libraries including Pydicom, NumPy, and Matplotlib [86] [87].
- Step 1: Data Conversion: Use a custom Python script to convert DICOM data into JPEG-format Multi-Planar Reconstruction (MPR) images for reference within 3D modeling software [87].
- Step 2: Automated Segmentation: Import DICOM data into 3D Slicer and use the AutoSegmentator extension (based on nnU-Net) to automatically extract surface data for 104 organs. Export this data in STL format [86] [87].
- Step 3: Data Alignment and Refinement: Import both the STL organ data and JPEG MPR images into Blender. Use custom Python scripts to align them in the same 3D space. Medical experts then manually refine the automatically extracted organ boundaries and add any missing structures based on the image data [86] [87].
- Step 4: Application: The resulting comprehensive anatomical dataset can be used for various applications, including 3D-printed simulators and surgical planning [86].
The following workflow diagram illustrates this multi-step process:
Multi-Layered Tissue Modeling for Optical Research
For optical applications, modeling often focuses on capturing the multi-layered nature of tissues and their respective optical properties. This is critical for simulating devices that operate in diffuse reflectance or transmittance modes [3] [7].
Experimental Protocol:
- Material: The study uses specific biological samples (e.g., Orah mandarin fruit or potato tubers) grouped by health status or tissue type [3] [7].
- Step 1: Measure Optical Properties: Use a single integrating sphere (SIS) system coupled with the inverse adding-doubling (IAD) algorithm to measure the total diffuse reflectance (Rt) and total transmittance (Tt) of thin tissue slices. Calculate the absorption (μa) and reduced scattering (μ’s) coefficients from these measurements [3] [7].
- Step 2: Construct a Multi-Layered Model: Based on the measured OPs, establish a multi-layer model. For Orah mandarin, this is a three-layer concentric sphere (oil sac, albedo, pulp). For potatoes, models can range from a simple 2mm slice to a "full-potato" model with peel, healthy tissue, and embedded blackhearted tissue [3] [7].
- Step 3: MC Simulation and Analysis: Implement the model and its OPs in a voxel-based MC simulator like MCX. Simulate photon transport to analyze key metrics such as penetration depth, spatial distribution of absorbed energy, and the contribution of different tissue layers to the detected signal [3] [7].
Quantitative Data from Anatomical Modeling Studies
The following tables consolidate key quantitative findings from recent studies that employed anatomical modeling and MC simulations.
Table 1: Optical Properties and Light Penetration in Biological Tissues
| Tissue Type / State | Wavelength (nm) | Absorption Coefficient (μa) | Reduced Scattering Coefficient (μ’s) | Penetration Depth (mm) | Source |
|---|---|---|---|---|---|
| Potato, Healthy | 805 | Low | High | ~6.73 | [3] |
| Potato, Blackhearted | 805 | Notably Increased | Increased | ~1.30 | [3] |
| Orah Mandarin, Oil Sac Layer | 500 | High (Peak) | - | - | [7] |
| Orah Mandarin, Albedo Layer | - | - | High (Porous) | - | [7] |
| Orah Mandarin, Pulp Tissue | 980 | Low (Water Absorption) | Low (Translucent) | Significant Decrease | [7] |
Table 2: Optimized Experimental Parameters from MC Simulations
| Application | Sample Type | Key Finding / Optimized Parameter | Recommended Value / Outcome | Source |
|---|---|---|---|---|
| Internal Defect Detection | Potato | Deeper light penetration & lower absorption in healthy tissues vs. blackhearted. | Wavelengths 490 nm & 805 nm are effective for detecting blackheart. | [3] |
| Diffuse Reflectance Detection | Orah Mandarin | Contribution of pulp tissue to signal increases with source-detector distance. | Optimal source-detector distance: 13-15 mm. | [7] |
| Interstitial Photodynamic Therapy | Human Abscess Cavities | Patient-specific planning based on CT scans improves eligibility and treatment planning. | Enables near real-time simulation with GPU-accelerated MC. | [2] |
The Scientist's Toolkit: Essential Research Reagents and Materials
This table details key software, materials, and algorithms essential for creating anatomically realistic models and performing subsequent MC simulations.
| Item Name | Function / Application | Specific Example / Note |
|---|---|---|
| 3D Slicer with TotalSegmentator | Open-source platform for automated segmentation of organs from DICOM data. | Based on nnU-Net; can extract 104 organs in bulk [86] [87]. |
| Blender | Open-source 3D computer graphics software used for refining, reconstructing, and assembling anatomical models. | Used with custom Python scripts for aligning image and model data [86] [87]. |
| Monte Carlo eXtreme (MCX) | Voxel-based, GPU-accelerated MC simulation platform for modeling light transport in turbid media. | Enables efficient simulation of complex, multi-layered models [3] [7]. |
| Single Integrating Sphere (SIS) + IAD | System for measuring total diffuse reflectance and transmittance to calculate optical properties (μa, μ’s). | Foundational for obtaining accurate input parameters for MC simulations [3] [7]. |
| Python (Pydicom, NumPy, Matplotlib) | Programming environment for automating DICOM data conversion, analysis, and integration tasks within the workflow. | Used for creating MPR images and custom scripts for Blender [86] [87]. |
The logical relationship between the core components of the modeling and simulation workflow is summarized in the following diagram:
Monte Carlo (MC) simulation has become an indispensable technique in biomedical optics for modeling light propagation in complex, turbid media like biological tissue. By using random sampling to statistically simulate the paths of millions of photons, these methods can accurately model phenomena where analytical solutions are infeasible. Recent advancements have expanded MC capabilities into specialized domains, particularly fluorescence propagation and polarization-sensitive interactions, which are critical for developing diagnostic and therapeutic applications [88] [70].
This technical guide synthesizes current methodologies for two advanced MC techniques: Fluorescence Monte Carlo (FMC) simulations, which model the excitation and emission pathways of fluorescent agents, and Polarized Light Monte Carlo (PLMC) simulations, which track the polarization state of light as it propagates through scattering media. Framed within the broader context of a thesis on MC for tissue research, this document provides a comprehensive resource for researchers and drug development professionals, offering detailed protocols, validated computational frameworks, and essential toolkits for implementing these cutting-edge simulations.
Theoretical Foundations
Core Principles of Monte Carlo in Light Propagation
At its core, a Monte Carlo simulation for light propagation models the random walk of photon packets as they travel through a medium with defined optical properties (absorption coefficient μa, scattering coefficient μs, anisotropy g, and refractive index n). Each photon's path is determined by a sequence of random decisions about the distance to the next scattering event, the new direction after scattering, and potential absorption or termination [89] [90].
The fundamental strength of the method lies in its ability to handle complex three-dimensional geometries and heterogeneous media that defy analytical solutions. Unlike deterministic models that yield a single outcome, MC simulations incorporate inherent uncertainties of light-tissue interactions, generating a probability distribution of possible outcomes. This provides a more realistic and comprehensive understanding of system behavior under uncertain conditions [89].
Fundamentals of Light-Tissue Interactions
Modeling light in tissue requires accounting for key physical interactions:
- Absorption: Energy transfer from light to the medium, quantified by
μa. - Scattering: Redirection of light by microscopic variations in refractive index, quantified by
μsandg. - Polarization: Alteration of the electromagnetic wave's orientation upon scattering.
- Fluorescence: Absorption at an excitation wavelength followed by re-emission at a longer, Stokes-shifted wavelength.
From Standard MC to Advanced Frameworks
Traditional MC models treated photon propagation as a scalar problem. However, advanced applications like fluorescence-guided surgery and polarization-sensitive microscopy require tracking additional photon states. Fluorescence MC extends the standard model by introducing a two-step process: first simulating excitation light propagation, then using the absorbed energy distribution as a source for emission light simulation [88]. Polarized Light MC adds further complexity by tracking the polarization state (e.g., Stokes vectors) of each photon packet at every scattering event, enabling simulation of phenomena like birefringence and differential polarization scattering [70] [91].
Fluorescence Monte Carlo (FMC) Simulations
Computational Framework and Workflows
The two-step MCX-ExEm framework provides a validated approach for fluorescence simulation. This GPU-accelerated method separates the excitation (Ex) and emission (Em) processes, leveraging the computational power of modern graphics cards to handle the high photon counts required for statistically robust results [88].
The following diagram illustrates the sequential workflow of this two-step process:
Step 1: Excitation Simulation
- A Monte Carlo simulation is run for the excitation wavelength (
λ_ex). - The physical quantity captured is the absorbed energy density within fluorophore-containing regions.
- This spatial map of absorbed energy defines the probability distribution for fluorescence emission.
Step 2: Emission Simulation
- The absorbed energy map from Step 1 serves as the source for a new MC simulation at the emission wavelength (
λ_em). - Critical consideration: optical properties (
μa,μs) must be updated forλ_emdue to wavelength-dependent effects. - The output is the spatiotemporal distribution of fluorescent light escaping the tissue [88].
Key Implementation Considerations
Computational Efficiency: The MCX-ExEm framework demonstrates that simulations with 10^7 photons for typical geometries can converge to <0.1% error and complete in seconds to minutes on a modern GPU (e.g., NVIDIA RTX 3090) [88]. For further acceleration, a scaling method has been demonstrated to achieve a 46-fold improvement in computational time while maintaining a mean absolute percentage error within 3% compared to independent simulations [92].
Fluorophore Characteristics: Accurate simulation requires incorporating the fluorophore's quantum yield (probability of emission per absorption event) and absorption spectrum. The model must also account for concentration-dependent effects like quenching, which MCX-ExEm has been shown to accurately capture at high concentrations [88].
Experimental Validation and Protocol
Robust validation of FMC simulations requires comparison against well-characterized physical phantoms. The following protocol outlines this process:
Table 1: Key Parameters for Fluorescence Phantom Experiments
| Parameter | Typical Range | Measurement Method | Notes |
|---|---|---|---|
| Fluorophore Concentration | nM to µM range | Serial dilution | Account for quenching at high concentrations [88] |
| Absorption Coefficient (μa) | 0.01 - 0.1 mm⁻¹ | Integrating sphere + inverse adding-doubling [88] | Wavelength-specific |
| Reduced Scattering Coefficient (μs') | 0.5 - 2.0 mm⁻¹ | Integrating sphere + inverse adding-doubling [88] | Wavelength-specific |
| Phantom Geometry | Complex 3D shapes | 3D printing [88] | Enables realistic anatomical models |
Experimental Materials:
- Solid Phantom Base: Epoxy or resin providing long shelf life and stability [88].
- Fluorophore: ICG (clinically relevant) or other target-specific agents [88].
- Scattering Agent: Titanium dioxide or polystyrene microspheres.
- Absorption Agent: India ink or other broadband absorbers.
- 3D Printing System: For creating complex, custom geometries [88].
Validation Procedure:
- Phantom Fabrication: Create solid phantoms with precisely controlled optical properties using epoxy/resin bases doped with fluorophores, scattering particles, and absorbers [88].
- Optical Characterization: Measure
μaandμs'of the phantom materials using an integrating sphere and inverse adding-doubling algorithm [88]. - Imaging Acquisition: Image the phantoms using a fluorescence imaging system with controlled illumination and detection settings.
- Simulation Execution: Run MCX-ExEm simulations using the measured optical properties and exact experimental geometry.
- Quantitative Comparison: Compare simulated and experimental fluorescence intensities across parameters like concentration, depth, and optical properties. Successful validation shows strong agreement (<5% deviation) across most regimes [88].
Polarized Light Monte Carlo (PLMC) Simulations
Computational Framework for Polarization Tracking
Polarized Light Monte Carlo simulations extend the basic MC method by tracking the polarization state of each photon packet throughout its propagation history. This is typically implemented by storing and updating a Stokes vector for each photon packet, which fully describes its polarization state. At every scattering event, the Stokes vector is multiplied by a Mueller matrix that characterizes how the scattering particle alters the polarization [70] [91].
The MC-Doppler platform exemplifies a modern, voxel-free approach to PLMC, using vector operations and analytical geometry to accurately model interactions with curved surfaces like flow tubes and cylindrical cuvettes [70].
The following diagram illustrates the core computation loop for tracking photon polarization:
Implementation Considerations for PLMC
Scattering Phase Functions: PLMC implementations require proper sampling of scattering angles (θ, φ) based on the medium's scattering phase function. The scattering inverse cumulative distribution functions (CDFs) are often implemented as cubic smoothing splines derived from the phase function, which can be customized for different polarization states [70].
Polarization-Sensitive Detection: To simulate polarization-sensitive imaging systems (e.g., polarization-modulation structured illumination microscopy), the detected photons must be processed through an optical element model (e.g., a polarizer) that operates on their Stokes vectors before final intensity calculation [91].
Computational Overhead: Tracking polarization adds approximately 20-30% computational overhead compared to scalar MC simulations due to the additional vector and matrix operations.
Experimental Protocol for PLMC Validation
Validating PLMC simulations requires specialized setups capable of measuring polarization-dependent signals:
Table 2: Polarized Measurement System Components
| Component | Function | Example Specifications |
|---|---|---|
| Polarized Light Source | Generate controlled polarization states | Linearly polarized laser (561 nm) [91] |
| Polarization Controllers | Modulate incident polarization | Liquid crystal modulators, rotating waveplates |
| Polarization-Sensitive Detector | Analyze output polarization states | Polarizing beamsplitters, imaging polarimeters |
| Sample Phantom | Provide known scattering properties | Polystyrene microspheres in suspension [70] |
| Flow System | Induce Doppler shifts (optional) | Syringe pump, flow chamber [70] |
Validation Procedure for Backscattering Geometry:
- Phantom Preparation: Create suspensions of monodisperse polystyrene beads (diameters 0.1-2.0 µm) in water or solid phantoms with known refractive indices [70].
- System Calibration: Align the polarization state generators and analyzers, correcting for system-induced polarization alterations.
- Data Acquisition: Measure backscattered polarization patterns or through-transmission Doppler power spectra for flowing samples [70].
- Simulation Execution: Run PLMC simulations with exact experimental parameters (optical properties, geometry, polarization states).
- Comparison: Match simulated and experimental polarization patterns or Doppler spectra. MC-Doppler has shown good agreement for scattering coefficients up to 5 mm⁻¹ [70].
The Scientist's Toolkit: Research Reagent Solutions
Implementing advanced MC simulations requires both computational tools and physical materials for validation. The following table catalogs essential resources mentioned in recent literature:
Table 3: Essential Research Reagents and Computational Tools
| Item | Function/Role | Example Products/Implementations |
|---|---|---|
| MCX-ExEm Framework | GPU-accelerated FMC simulation | Open-source MCX v2024.1 [88] |
| MC-Doppler Platform | Polarized MC for flowmetry | MATLAB-based, open-source [70] |
| Solid Phantom Materials | Stable, characterizable validation | Epoxy/resin bases with TiO₂/ink [88] |
| Clinical Fluorophores | Biologically relevant fluorescence | ICG, Cytalux, Lumisight [88] |
| Polystyrene Microspheres | Calibrated scatterers | Various diameters (0.1-10 µm) [70] |
| 3D Printing Systems | Complex phantom fabrication | Custom geometries [88] |
| Integrating Sphere Systems | Optical property characterization | Inverse adding-doubling method [88] |
Advanced Monte Carlo techniques for fluorescence and polarized light represent the cutting edge of computational biophotonics. The frameworks and protocols detailed in this guide provide researchers with robust tools for simulating complex light-tissue interactions with high physical accuracy. As these methods continue to evolve—driven by improvements in GPU acceleration, hybrid scaling algorithms, and experimental validation—they will play an increasingly vital role in accelerating the development of optical diagnostics, targeted therapies, and fundamental biomedical research. The integration of physically accurate simulations with well-characterized phantoms establishes a powerful foundation for digital twins in biomedical optics, potentially reducing the need for extensive in vivo experimentation while accelerating device development and optimization.
Leveraging High-Performance Computing and Quantum Simulation for Complex Problems
Monte Carlo (MC) simulation, a statistics-based computational method for modeling complex systems by estimating probability distributions from numerous independent random trials, has established itself as the gold standard for modeling photon migration in biological tissues [93] [94] [1]. Its superiority stems from an ability to accurately simulate light propagation in arbitrarily complex and heterogeneous media—such as the human brain, breast tissue, or fruits—where simplified models like the diffusion approximation fail, particularly in regions with low-scattering voids or strong absorption [93] [1]. However, this accuracy comes at a steep computational cost, often requiring hours or more of computation for realistic domain sizes, which has historically limited its practical application in day-to-day research and clinical analysis [93].
The emergence of high-performance computing (HPC) paradigms, particularly general-purpose computing on graphics processing units (GPGPU), has fundamentally transformed this landscape. By leveraging the massively parallel architecture of modern GPUs, researchers can now achieve acceleration ratios of over 300 times compared to conventional single-threaded CPU computation, making MC simulation a practical tool for widespread use [93]. This whitepaper provides an in-depth technical guide on leveraging these advanced computing technologies to solve complex problems in biomedical optics, drug development, and related fields, with a specific focus on light propagation in tissue.
High-Performance Computing Architectures for Monte Carlo
GPU Acceleration and Parallelization Strategies
The core of modern high-performance MC simulation lies in exploiting data-parallel architectures. Graphics Processing Units (GPUs) contain thousands of cores optimized for parallel execution, offering immense computational throughput for inherently parallel problems like photon transport [93]. In a typical GPU-accelerated MC implementation, thousands of simulation threads are launched simultaneously, with each thread independently simulating the propagation path of a photon or a sequence of photons [93].
Key to this parallelization is the efficient management of memory and computational resources. The thread hierarchy in programming models like CUDA allows for coordinated execution within blocks and efficient data sharing through fast shared memory [93]. A significant performance challenge in 3D simulations is managing concurrent memory writes (race conditions) when multiple photon packets deposit energy in the same voxel simultaneously. This can be addressed using atomic operations, which ensure data integrity but incur a performance cost, reducing acceleration ratios from over 300 to approximately 75 [93]. Alternative non-atomic approaches can be used when the probability of race conditions is low, particularly in voxels far from the source where photon density decreases exponentially [93].
Advanced Geometric Representations
The choice of geometric representation for the simulated tissue significantly impacts both accuracy and computational efficiency:
- Voxel-Based Models: Represent tissue as a 3D grid of cubic voxels, with each voxel assigned an integer identifier for a specific tissue type and its associated optical properties [26]. This approach is conceptually simple and easy to construct from medical image data but suffers from staircase artifacts at curved boundaries and can be computationally inefficient in low-scattering regions [95].
- Tetrahedral Mesh Models: Use irregular tetrahedra to discretize the tissue volume, providing a superior approximation of smooth surfaces and curved boundaries [95]. This is particularly important for accurately modeling refraction and reflection at tissue interfaces with refractive index mismatches (e.g., air-tissue boundaries or fluid-filled voids). Meshes also allow for more efficient computation in low-scattering regions and enable direct scoring of fluence through thin surface layers [95].
Table 1: Comparison of Geometric Representation Methods for Monte Carlo Simulation
| Feature | Voxel-Based Model | Tetrahedral Mesh Model |
|---|---|---|
| Geometry Definition | 3D cube with cubic voxels [26] | Volumetric mesh with tetrahedral elements [95] |
| Surface Approximation | Staircase artifacts at curves | Smooth surface approximation |
| Boundary Treatment | Approximate; refractive errors possible | Accurate refraction/reflection calculation |
| Memory Efficiency | Uniform, can be memory-intensive | Adaptive, more efficient for complex shapes |
| Implementation Complexity | Lower | Higher |
| Best For | Simple heterogeneities, image-based data | Complex anatomy with curved surfaces |
Efficient Random Number Generation
Monte Carlo simulations depend critically on the quality and speed of pseudo-random number generation (RNG). In parallel GPU implementations, this challenge is compounded as thousands of threads require independent random sequences. Two parallel RNG strategies have shown particular promise:
- Mersenne-Twister (MT): A widely respected RNG known for its extremely long period and high quality [93]. The SIMD-oriented Fast MT (SFMT) variant is particularly suitable for GPU implementation, where all threads in a block can share a common state vector of 624 32-bit integers [93].
- Chaotic Logistic-Lattice (LL) RNG: A floating-point-only random number generator based on a chaotic lattice, which offers computational advantages on GPU architectures by avoiding integer operations [93].
The selection of RNG can significantly impact overall simulation performance, with different generators offering varying trade-offs between statistical quality and computational speed.
Quantitative Performance Analysis
The computational benefits of HPC approaches to MC simulation are substantial and measurable. Benchmark studies demonstrate that a GPU-based algorithm using 1792 parallel threads can achieve an acceleration ratio exceeding 300 compared to conventional single-threaded CPU computation [93]. This performance gain enables simulations that previously required hours to be completed in minutes, making MC a practical tool for iterative research and development workflows.
Table 2: Performance Benchmarks of Monte Carlo Simulation Methods
| Performance Metric | Traditional CPU MC | GPU-Accelerated MC | GPU with Atomic Operations |
|---|---|---|---|
| Hardware | Single-core CPU | GPU with 1792 threads | GPU with 1792 threads |
| Acceleration Ratio | 1x (Baseline) | >300x | ~75x [93] |
| Computational Speed | Slow (hours for human head domain) [93] | Fast (minutes for comparable domain) | Medium-Fast |
| Memory Write Integrity | N/A (serial process) | Risk of race condition | Guaranteed integrity [93] |
| Typical Use Case | Legacy systems, verification | High-throughput simulation | Data-critical applications |
Performance optimization requires careful consideration of several parameters, including thread number per block, memory access patterns, and the choice of random number generator. Additionally, the implementation of efficient boundary handling for reflection and refraction at 3D interfaces is crucial for maintaining physical accuracy without sacrificing computational speed [93].
Experimental Protocols and Verification
Code Verification with Invariance Properties
A fundamental challenge in MC development is verifying that the implemented code produces physically accurate results. A powerful verification method leverages the Invariance Property (IP) of the mean path length, which states that for a medium with Lambertian entrance (homogeneous and isotropic illumination) and no absorption, the average path length (\langle L \rangle) spent by photons within the medium is constant and depends only on the geometry and refractive index, regardless of the internal distribution of scattering properties [94].
For a 3D medium, the predicted average path length is given by: [ \langle L \rangle{IP}^{3D} = 4 \frac{V}{S} nr^2 ] where (V) is the volume, (S) is the surface area, and (nr = n/ne) is the relative refractive index between the medium and external environment [94]. This relationship provides an exact reference value that can be used to verify MC codes with arbitrary accuracy as the number of simulated trajectories increases. The method is particularly sensitive for detecting inaccuracies in boundary treatments [94].
Validation Against Analytical Solutions
For specific simple geometries, MC simulation results can be validated against analytical solutions from transport theory. For example, in a homogeneous semi-infinite medium, the output of an MC simulation for time-resolved photon migration should demonstrate excellent agreement with the analytical solution derived from the diffusion approximation to the radiative transfer equation [93]. Such validation provides confidence in the physical correctness of the MC implementation before applying it to more complex, heterogeneous geometries.
Workflow for a Typical Simulation Experiment
The following diagram illustrates the logical workflow and key components of a comprehensive Monte Carlo simulation experiment for light propagation in biological tissue:
Diagram 1: Workflow of a Monte Carlo Simulation Experiment
Successful implementation of high-performance MC simulation requires both specialized software tools and an understanding of the optical properties that serve as inputs to the models.
Table 3: Essential Research Reagent Solutions for Monte Carlo Simulation
| Tool/Resource | Type | Function and Application | Key Features |
|---|---|---|---|
| FullMonte [95] | Software Platform | 3D tetrahedral-mesh MC simulator for complex tissues | High-performance C++ kernel, Tcl scripting, VTK/Paraview visualization |
| MCML [25] | Software Code | Steady-state MC for multi-layered tissues | Cylindrical symmetry, widely validated, multiple implementations |
| CUDAMCML [25] | Software Code | GPU-accelerated version of MCML | NVIDIA CUDA implementation, significant speedup |
| mcxyz [25] | Software Code | 3D voxel-based MC for heterogeneous tissues | Cubic voxel geometry, handles complex tissue structures |
| Tissue Optical Properties | Input Parameters | Absorption (μa), scattering (μs) coefficients, anisotropy (g), refractive index (n) | Define light-tissue interaction; measured via integrating sphere systems [7] |
| Single Integrating Sphere System | Laboratory Equipment | Measures tissue optical parameters using Inverse Adding-Doubling (IS-IAD) method [7] | Provides quantitative inputs for MC models for specific tissues |
Applications in Biomedical Research and Drug Development
The capabilities of high-performance MC simulation have enabled advanced applications across multiple domains of biomedical research:
Photodynamic Therapy (PDT) Planning
MC simulations are crucial for predicting light dose distribution (fluence) in tissues during photodynamic therapy, where light activates photosensitizing drugs to destroy target cells [95]. By accurately modeling light propagation in patient-specific anatomy derived from medical images, clinicians can optimize source placement and power settings to ensure therapeutic doses reach target regions while minimizing exposure to healthy tissue [95].
Non-Destructive Quality Assessment
In agricultural and food sciences, MC methods help optimize visible/near-infrared (Vis/NIR) spectroscopy systems for non-destructive quality assessment of fruits. For example, simulations of light propagation in Orah Mandarin tissues have revealed how different tissue layers (oil sac layer, albedo layer, and pulp) contribute to detected signals, enabling optimization of source-detector distances (e.g., 13-15 mm) to maximize signal from the pulp while maintaining sufficient reflectance intensity [7].
Optogenetics and Neurophotonics
MC simulations help design optogenetic experiments by predicting how light propagates through scattering brain tissue. This is essential for controlling neuron activation depths and avoiding thermal damage from excessive power density. Advanced approaches like the Beam Spread Function (BSF) method offer faster computation compared to traditional MC while maintaining accuracy for certain applications [1].
Advanced Imaging Techniques
MC methods support the development and interpretation of various optical imaging modalities, including:
- Diffuse Optical Tomography (DOT): Using surface measurements to reconstruct internal optical properties [1].
- Optical Coherence Tomography (OCT): Modeling coherent light propagation and interference [1].
- Polarimetry and Mueller Matrix Measurement: Simulating the propagation of polarized light to characterize tissue microstructure [1].
- Raman Spectroscopy: Modeling the migration of both excitation and Raman-shifted photons [1].
The integration of high-performance computing architectures with Monte Carlo simulation has transformed this statistical method from a theoretical gold standard into a practical tool for solving complex problems in biomedical optics and beyond. Through massive parallelization on GPU platforms, advanced geometric representations, and robust verification methodologies, researchers can now perform accurate simulations of light propagation in arbitrarily complex tissues with computational times compatible with research and clinical workflows. As these computational technologies continue to evolve, and as optical property databases for various tissues expand, the applications of high-performance MC simulation will further revolutionize optical diagnostics, therapeutic monitoring, and drug development processes.
Validating and Benchmarking MC Models Against Experiments and Alternative Methods
The development of robust optical medical imaging techniques, particularly those like oximetry that quantify blood oxygen saturation (sO₂), is fundamentally constrained by a significant challenge: the absence of reliable, non-invasive ground-truth measurements in vivo [96]. This validation gap impedes the clinical translation of new technologies. Within the broader thesis on Monte Carlo simulation for light propagation in tissue, this guide establishes a complementary experimental framework using physical tissue-mimicking phantoms. While Monte Carlo methods provide the theoretical underpinnings for modeling light transport, anthropomorphic phantoms provide the essential physical test objects required for empirical validation, standardization, and performance verification of both the algorithms and the imaging systems themselves [96] [97].
Experimental Protocols for Phantom Fabrication and Validation
The following section details a reproducible methodology for creating and validating anthropomorphic phantoms for oximetry, synthesizing current advanced practices.
Fabrication of Forearm Phantoms with Embedded Vessels
A recent protocol demonstrates the creation of structurally stable, anthropomorphic phantoms using a copolymer-in-oil base material [96].
1. Base Material Preparation:
- Materials: Polystyrene-block-poly(ethylene-ran-butylene)-block-polystyrene (SEBS), mineral oil, titanium dioxide (
TiO₂), and butylated hydroxytoluene (BHT) [96]. - Procedure:
TiO₂is first sonicated in mineral oil to disperse scattering particles. SEBS polymer and the antioxidant BHT are then added. The mixture is heated to 160°C in a silicone oil bath until fully liquefied, with stirring every 10 minutes. Finally, residual air bubbles are removed in a vacuum chamber [96].
2. Mimicking Optical Properties of Hemoglobin:
- Objective: Identify dye proxies that replicate the distinct absorption spectra (
μ_a) of oxyhemoglobin (HbO₂) and deoxyhemoglobin (Hb) across the near-infrared spectrum (700-850 nm) [96]. - Procedure: Candidate dyes are mixed into the base material, and their absorption spectra are characterized using a double-integrating sphere (DIS) system. A non-negative least square (NNLS) optimization algorithm is used to find a linear combination of dyes that best fits the target
HbO₂andHbspectra. Concentrations are iteratively adjusted to achieve the desired spectral match [96].
3. Creating Anthropomorphic Structure:
- Source Data: A high-resolution MRI dataset of a human forearm is segmented to isolate muscle and bone structures [96].
- Mold Fabrication: The segmented outer hull and bones are converted into 3D-printable models. The external mold is printed, and the bone structures are printed as positive features to be embedded within the phantom [96].
- Phantom Casting: The base material, loaded with optimized dye combinations, is cast into the 3D-printed mold. Vessel-like structures are embedded to create a morphologically realistic geometry with controlled
sO₂levels [96].
A Two-Step Phantom and Simulation Validation Method
For ocular oximetry, a powerful two-step validation strategy combining physical phantoms and Monte Carlo simulation has been developed to deconvolve confounding factors [97].
1. Tissue Phantom Investigation:
- Purpose: To isolate and study the impact of specific variables such as light scattering, blood volume fraction (BVF), and crystalline lens yellowing on oximetry measurements [97].
- Procedure: Phantoms with controlled variations in these parameters are constructed. The empirical oximetry technique is applied, and its performance is assessed as these confounding factors are systematically altered.
2. Monte Carlo Simulation Investigation:
- Purpose: To study the effect of the complex layered-structure of the eye fundus, which is difficult to replicate physically [97].
- Procedure: A multi-layered Monte Carlo model of the eye fundus is implemented. The impact of layers such as the retinal pigment epithelium (RPE) and the choroid, including their melanin concentration and blood oxygen saturation, can be investigated. This allows for the quantification of errors, such as the influence of the underlying choroidal circulation on retinal
sO₂measurements [97].
The Scientist's Toolkit: Research Reagent Solutions
The table below catalogs key materials used in the fabrication of advanced tissue-mimicking phantoms for optical imaging and oximetry.
Table 1: Essential Materials for Fabricating Tissue-Mimicking Phantoms
| Item Name | Function | Key Characteristics |
|---|---|---|
| SEBS Copolymer [96] | Base matrix for structurally stable phantoms. | Provides mechanical stability and transparency; compatible with oil-based dispersions. |
| Mineral Oil [96] | Dispersant for the phantom matrix. | Serves as the liquid medium for suspending scattering and absorbing agents. |
| Titanium Dioxide (TiO₂) [96] | Scattering agent. | Mimics the light scattering properties of biological tissues. |
| Proxy Dyes [96] | Mimics optical absorption of HbO₂ and Hb. |
Must have absorption spectra that can be optimized to match hemoglobin in the NIR range. |
| Agarose [98] | Gelling agent for hydrogel-based phantoms. | Versatile, provides favorable MRI relaxation properties; commonly used for MRI and optical phantoms. |
| Carrageenan [98] | Gelling agent. | Often used in combination with agar; noted for strength and minimal impact on T₂ MRI values. |
| Polyvinyl Alcohol (PVA) [98] | Base for cryogel phantoms. | Creates durable, reusable phantoms with tunable mechanical and optical properties. |
Workflow and Data Visualization
Anthropomorphic Phantom Fabrication and Validation Workflow
The following diagram illustrates the integrated workflow from medical imaging data to phantom validation, connecting the protocols described in Section 2.1.
Two-Step Phantom and Simulation Validation Strategy
This diagram outlines the logical flow of the two-step validation method that combines physical phantoms and Monte Carlo simulations, as detailed in Section 2.2.
Quantitative Data and Performance Metrics
Optical Properties of Hemoglobin and Phantom Materials
Critical to oximetry validation is the accurate mimicry of hemoglobin's optical absorption. The following table presents key properties and performance metrics derived from phantom studies.
Table 2: Absorption Properties and Phantom Performance Metrics
| Parameter | Description / Value | Context & Significance |
|---|---|---|
HbO₂ & Hb Absorption Spectra [96] |
Distinct peaks in visible/NIR. | Gold-standard reference for oximetry; target for proxy dye optimization. |
| Pearson Correlation Coefficient [96] | > 0.8 | Reported correlation between measured phantom absorption spectra and HSI/PAT data, indicating high fidelity. |
Phantom sO₂ Levels [96] |
0% to 100% (5 levels) | Range of oxygen saturation levels fabricated in phantom vessel-like structures for validation. |
| Scattering Anisotropy Factor (g) [96] | 0.7 | Typical value used for modeling light propagation in tissue-like phantom materials. |
| Refractive Index (n) [96] | 1.4 | Typical value assigned to phantom materials for inverse adding-doubling calculations. |
| Spectral Range for Oximetry [97] | 530 nm to 585 nm | Optimal range identified for ocular oximetry to minimize error from scattering and other chromophores. |
Advanced Tissue-Mimicking Materials for Multi-Modal Phantoms
Beyond the SEBS-based material, a systematic review identifies several gelling agents used for fabricating phantoms across imaging modalities.
Table 3: Common Gelling Agents and Their Properties in Phantom Fabrication
| Gelling Agent | Primary Modality | Key Advantages & Characteristics |
|---|---|---|
| Agar [98] | MRI, Optical | Most frequently used; versatile, favorable MRI signal properties, tunable relaxation times. |
| Carrageenan [98] | MRI, Optical | Often combined with agar; provides strength and has minimal impact on T₂ values. |
| Gelatin [98] | Optical, Ultrasound | Easy to work with; can be doped with various scatterers and absorbers. |
| Polyvinyl Alcohol (PVA) [98] | MRI, Ultrasound | Forms cryogels; durable, reusable, and can simulate soft tissue mechanics well. |
Monte Carlo (MC) simulation techniques stand as a cornerstone in computational physics, providing robust solutions for modeling stochastic processes where analytical methods are infeasible. Within medical physics research, particularly in studies of light propagation in tissue, MC methods are indispensable for predicting energy deposition, photon migration, and therapeutic efficacy in treatments like photodynamic therapy [57]. The reliability of these simulations, however, is entirely contingent upon rigorous validation and verification processes. This case study explores the critical practice of cross-validation through the lens of gamma radiation shielding—a domain where validation methodologies are highly mature. The principles and protocols elucidated herein provide a directly applicable framework for researchers employing MC simulations in light-tissue interaction studies, ensuring model fidelity and result credibility.
Core Principles of Monte Carlo Simulation and Validation
Monte Carlo methods encompass a broad class of computational algorithms that rely on repeated random sampling to obtain numerical results for deterministic problems [99]. Their application spans from modeling light transport in multi-layered tissues to predicting the attenuation of gamma rays through shielding materials.
The utility of these simulations in research hinges on their accuracy, making validation and verification (V&V) essential. In the context of MC simulations:
- Verification answers the question "Are we building the model correctly?" It is an objective process of ensuring the computational model correctly implements the intended underlying mathematical model and that there are no errors in the code or logic [100].
- Validation answers the question "Are we building the right model?" It is the subjective process of ensuring the computational model accurately represents the real-world system it is intended to simulate, typically through comparison with experimental data [100].
For light propagation studies, a validated model ensures accurate predictions of light distribution in tissue, which is critical for planning laser therapies, interpreting diagnostic data, and developing new light-based treatments.
Case Studies in Gamma Radiation Shielding
The field of radiation shielding provides exemplary cases of comprehensive MC model validation. The following studies illustrate robust cross-validation approaches.
PMMA-HgO Composites for Medical and Industrial Shielding
A 2025 study developed a novel poly(methyl methacrylate) (PMMA) composite reinforced with mercury oxide (HgO) for gamma radiation shielding, validating simulations against experimental data [101].
Experimental Protocol:
- Material Synthesis: PMMA was dissolved in dichloromethane using a magnetic stirrer. HgO powder filler (2.5–10 wt%) was added and dispersed uniformly via stirring. The composite was then cast and cured [101].
- Material Characterization: Field emission scanning electron microscopy (FESEM) confirmed a uniform distribution of HgO particles within the polymer matrix. X-ray diffraction (XRD) verified the crystalline structure of the HgO filler [101].
- Shielding Performance Evaluation: Attenuation measurements used a collimated 137Cs source emitting 662 keV gamma rays. A high-purity germanium (HPGe) detector measured transmitted intensity with and without the composite sample to determine the linear attenuation coefficient (LAC) [101].
Simulation Methodology:
- Two simulation platforms were used: MCNP6 and GEANT4.
- The models were designed to replicate the exact experimental geometry, source configuration, and shielding setup.
- Key parameters computed included the LAC, mass attenuation coefficient (MAC), half-value layer (HVL), tenth-value layer (TVL), and effective atomic number (Zeff) [101].
Cross-Validation Results: The simulated results from both MCNP6 and GEANT4 showed close agreement with experimental data, with discrepancies under 5%, thereby validating the reliability of the models [101]. The quantitative outcomes are summarized in the table below.
Table 1: Shielding parameters for PMMA-HgO composites at 662 keV [101].
| HgO Content (wt%) | Linear Attenuation Coefficient, μ (cm⁻¹) | Half-Value Layer, HVL (cm) | Effective Atomic Number, Zeff |
|---|---|---|---|
| 0% (Pure PMMA) | 0.044 | 15.47 | 3.6 |
| 2.5% | 0.057 | 12.09 | 3.7 |
| 5.0% | 0.071 | 9.78 | 3.8 |
| 7.5% | 0.083 | 8.33 | 4.0 |
| 10.0% | 0.096 | 7.19 | 4.1 |
Polyester-Barite-Tungsten Ternary Composites
A 2024 study investigated the photon-shielding properties of polyester-based composites containing barite (BaSO₄) and tungsten (W), employing a three-pronged validation approach [102].
Methodology:
- Theoretical Calculation: The WINXCOM database was used to compute theoretical mass attenuation coefficients [102].
- Monte Carlo Simulation: Simulations were performed using both MCNP6 and PHITS 3.22 codes, meticulously replicating the narrow-beam geometry of the experiment [102].
- Experimental Measurement: Attenuation used radioisotope sources (Ba-133, Cs-137, Co-60) covering 81 keV to 1332 keV. A high-purity germanium (HPGe) detector with a multi-channel analyzer recorded transmitted spectra [102].
Validation Outcome: The results from simulation, theoretical calculation, and experiment "all closely aligned," confirming the composites' shielding effectiveness and the accuracy of the simulation models across a broad energy range [102].
Cement Composites for Structural Shielding
Research from 2024 on modified cement composites further underscores the consistency of MC validation. This study used the Geant4 toolkit to calculate the mass attenuation coefficient of cement composites containing iron, strontium, zinc, and zirconium. The simulated results were compared with those from the Phy-X program, and a "good agreement" was found, validating the model's ability to assess radiation shielding capabilities for potential use in medical radiotherapy rooms [103].
A Generalized Validation Protocol for Monte Carlo Simulations
Synthesizing the methodologies from the cited cases and established best practices, the following workflow provides a generalized, robust protocol for validating MC simulations. This protocol is directly applicable to light propagation models and other computational physics domains.
Verification Phase: Ensuring Correct Implementation
- Code and Logic Checks: Scrutinize the simulation code for syntax errors, typos, and logical flaws. Using peer review and static analysis tools is recommended [100].
- Unit and Integration Testing: Test individual subroutines (e.g., for photon scattering, absorption) independently before testing the integrated model to ensure each component functions as intended [100].
- Convergence and Stability Analysis: Monitor the simulation's running averages to ensure stable output. A history plot of observations can reveal if the simulation is "getting stuck" [104]. The number of simulated particles must be sufficient to achieve a low relative error, often requiring millions of histories [101] [105].
Validation Phase: Ensuring Model Fidelity
- Benchmarking Against Standards: Compare simulation results with well-established analytical solutions, published data from benchmark problems, or outputs from trusted reference codes like XCOM [105] [102] [106].
- Experimental Validation: This is the most critical step.
- Controlled Experiment: Design a real-world experiment that precisely mirrors the simulation setup in geometry, material properties, and source configuration [101] [105].
- Data Collection: Acquire high-quality experimental data with careful attention to uncertainty analysis for all measurements [102].
- Quantitative Comparison: Statistically compare experimental and simulated results (e.g., using relative percent difference, chi-square tests). A common acceptance criterion in radiation shielding is a discrepancy under 5% [101].
- Sensitivity Analysis: Determine how the model's output is influenced by variations in its input parameters. This identifies the most influential and uncertain factors, guiding refinement efforts [100].
Bridging Gamma Shielding and Light-Tissue Research
The validation principles from gamma shielding are directly transferable to MC simulations of light propagation in tissue. The core challenge remains the same: demonstrating that a computational model faithfully represents physical reality. The diagram below illustrates this conceptual bridge and the shared validation ecosystem.
Key parallels include:
- Shared Workflow: Both fields rely on the iterative V&V process outlined in Section 4.
- Parameter Fidelity: Accurate input of optical properties (absorption coefficient μa, scattering coefficient μs, anisotropy g) for tissues is as crucial as accurate material density and elemental composition is for shielding materials.
- Software Tools: While gamma shielding uses MCNP and Geant4, light propagation research has dedicated, validated tools like MCML (Monte Carlo for Multi-Layered media) and its GPU-accelerated derivatives [25].
- Experimental Benchmarking: Just as shielding models are validated using physical phantoms, light propagation models are validated using tissue-simulating phantoms with known optical properties.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogues key materials and software tools essential for conducting and validating MC simulations in radiation shielding and related fields, as evidenced by the cited research.
Table 2: Essential research reagents, materials, and software tools for MC simulation and validation.
| Name/Item | Type | Primary Function | Example from Literature |
|---|---|---|---|
| MCNP (Monte Carlo N-Particle) | Software Code | General-purpose particle transport code for simulating radiation interaction and shielding. | MCNP6 used to simulate gamma attenuation in PMMA-HgO composites [101]. |
| GEANT4 (Geometry and Tracking) | Software Code | A toolkit for simulating the passage of particles through matter, widely used in particle and medical physics. | Used alongside MCNP6 for cross-verification in polymer composite studies [101] [106]. |
| PHITS | Software Code | General-purpose MC particle transport code for simulating the transport of all particles over wide energy ranges. | Employed with MCNP6 to validate shielding in polyester composites [102]. |
| MCML | Software Code | A specialized MC simulation for light transport in multi-layered tissues (steady-state) [25]. | Standard model for simulating light propagation in skin layers for therapeutic applications [57] [25]. |
| XCOM / WINXCOM / Phy-X | Database / Software | Provides theoretically calculated photon interaction cross-sections and attenuation coefficients for benchmark comparisons. | Used as a theoretical reference to validate MC and experimental results [105] [102] [103]. |
| High-Purity Germanium (HPGe) Detector | Laboratory Equipment | High-resolution gamma-ray spectroscopy for accurately measuring transmitted photon energy spectra in validation experiments. | Used to measure attenuation through polymer and ferrite samples [101] [102]. |
| High-Z Fillers | Material | Materials with high atomic number used to enhance the attenuation capability of a base matrix. | HgO in PMMA [101], Tungsten in polyester [102], Bi₂O₃ in polymers [101]. |
| Tissue Simulating Phantoms | Material | Materials with precisely known optical properties (μa, μs, g) used to experimentally validate light transport models. | Analogous to shielding composites; essential for benchmarking MCML simulations [57] [25]. |
This case study demonstrates that rigorous cross-validation is not merely a supplementary step but the very foundation of credible Monte Carlo simulation. The protocols established in gamma radiation shielding—employing multiple simulation codes, benchmarking against standard data, and conducting meticulous experimental comparisons—provide a powerful and directly applicable template for the light-tissue interaction research community. Adopting this disciplined framework ensures that MC models, whether predicting gamma ray attenuation or light fluence in a tumor, yield results that are not just computationally elegant but are quantitatively reliable and fit for their intended purpose in scientific discovery and clinical application.
The accurate simulation of light propagation in biological tissues is a cornerstone of modern biomedical research, enabling advancements in diagnostic imaging, therapeutic applications, and drug development. This complex process is governed by the interplay of absorption and scattering events within heterogeneous tissue structures. The radiative transfer equation (RTE) serves as the fundamental mathematical framework describing this phenomenon, yet obtaining analytical solutions for realistic tissue geometries remains challenging [107]. Consequently, researchers have developed various computational approximations to solve the RTE, each with distinct strengths, limitations, and domains of applicability.
Within the context of a broader thesis on Monte Carlo simulation for light propagation in tissue research, this technical guide provides a comprehensive comparative analysis of three principal computational approaches: the gold-standard Monte Carlo (MC) method, the computationally efficient Diffusion Theory (DT), and the emerging Markov Chain (MC) approximations. Understanding the relative performance characteristics of these methods is critical for researchers and drug development professionals seeking to select optimal modeling strategies for specific applications, ranging from interstitial photodynamic therapy [27] to non-invasive melanoma depth estimation [108] and optogenetics [1].
Theoretical Foundations of Light Propagation Models
The Radiative Transfer Equation (RTE)
Light propagation in biological tissue is primarily described by the Radiative Transfer Equation (RTE), which functions as a statistical energy balance equation for light transport within a medium [107]. The general form of the time-dependent RTE is expressed as:
$$\frac{1}{c}\frac{\partial L(\mathbf{r}, \mathbf{\hat{s}}, t)}{\partial t} = -\mathbf{\hat{s}} \cdot \nabla L(\mathbf{r}, \mathbf{\hat{s}}, t) - \mut L(\mathbf{r}, \mathbf{\hat{s}}, t) + \mus \int_{4\pi} L(\mathbf{r}, \mathbf{\hat{s}}', t) p(\mathbf{\hat{s}}' \cdot \mathbf{\hat{s}}) d\Omega' + S(\mathbf{r}, \mathbf{\hat{s}}, t)$$
Here, (L(\mathbf{r}, \mathbf{\hat{s}}, t)) represents the radiance at position (\mathbf{r}), in direction (\mathbf{\hat{s}}), and at time (t). The optical properties of the tissue are defined by the absorption coefficient ((\mua)), the scattering coefficient ((\mus)), and the total attenuation coefficient ((\mut = \mua + \mu_s)). The term (p(\mathbf{\hat{s}}' \cdot \mathbf{\hat{s}})) denotes the scattering phase function, which characterizes the probability of light scattering from direction (\mathbf{\hat{s}}') to (\mathbf{\hat{s}}), while (S(\mathbf{r}, \mathbf{\hat{s}}, t)) represents the light source [107]. The complexity of solving this integro-differential equation directly for biological tissues has motivated the development of the approximation methods discussed in this analysis.
Monte Carlo (MC) Method
The Monte Carlo method is a stochastic approach that simulates light propagation by tracking the random walks of millions of individual photons or photon packets as they travel through tissue [1] [107]. Each photon's trajectory is determined by random sampling from probability distributions derived from the tissue's optical properties—specifically, the absorption coefficient ((\mua)), scattering coefficient ((\mus)), scattering anisotropy ((g)), and refractive index ((n)) [1] [107]. A photon's path consists of a sequence of steps. The length of each step is randomly determined by the total attenuation coefficient, calculated as (s = -\ln(\xi)/\mut), where (\xi) is a uniformly distributed random number between 0 and 1 [107]. When a scattering event occurs, a new direction for the photon is selected based on the scattering phase function, with the Henyey-Greenstein phase function being commonly used for this purpose [1]. Absorption is typically handled by reducing the photon's statistical weight, (W), multiplicatively by a factor of (\mua/\mu_t) at each interaction. The "Russian roulette" technique is often employed to terminate photons with negligible weight, thereby optimizing computational efficiency [1]. The simulation concludes when photons either exit the tissue geometry or are completely absorbed. The MC method is regarded as the gold standard for accuracy in modeling light transport because it makes the fewest simplifying assumptions and can handle complex, heterogeneous tissue structures [107].
Diffusion Theory (DT) Approximation
Diffusion Theory represents the most widely adopted approximation of the RTE. It is derived under the fundamental assumption that the medium is highly scattering (i.e., (\mus' \gg \mua)) and that the radiance is almost isotropic [107]. Under these conditions, the RTE simplifies to a diffusion equation for the photon flux density, (\Phi(\mathbf{r})). For a steady-state problem, this equation is:
$$-\nabla \cdot D(\mathbf{r}) \nabla \Phi(\mathbf{r}) + \mu_a(\mathbf{r}) \Phi(\mathbf{r}) = S(\mathbf{r})$$
Here, (D(\mathbf{r})) is the diffusion coefficient, defined as (D = [3(\mua + (1-g)\mus)]^{-1}) [107]. This simplification transforms the complex RTE into a parabolic partial differential equation that is computationally more efficient to solve, often using numerical methods like the Finite Element Method (FEM). However, the accuracy of DT deteriorates in regions with low scattering, high absorption, and in the immediate vicinity of light sources and tissue boundaries [52] [107].
Markov Chain (MC) Approximations
Markov Chain approximations offer an alternative methodology by reformulating the photon scattering problem into a state-transition matrix framework [1]. In this model, the physical medium is discretized into a finite set of states, and the probabilistic transitions of photons between these states (e.g., scattering from one direction to another) are encoded within a transition probability matrix. The fundamental equation governing the evolution of the photon state probability distribution, (\mathbf{\pi}(n)), after (n) scattering events is given by:
$$\mathbf{\pi}(n) = \mathbf{\pi}(0) \mathbf{P}^n$$
Here, (\mathbf{\pi}(0)) is the initial state probability vector, and (\mathbf{P}) is the transition probability matrix whose elements (P_{ij}) define the probability of scattering from state (i) to state (j) [1]. This matrix formulation effectively converts the problem of simulating millions of random photon paths into a series of matrix multiplications. This approach is particularly adept at handling anisotropic scattering and complex phase functions, such as those derived from Mie theory, and it facilitates efficient parameter studies and inversion problems [1].
Quantitative Comparative Analysis
The table below summarizes the key performance characteristics and application domains of the three modeling approaches based on current literature.
Table 1: Quantitative Comparison of Light Propagation Models
| Feature | Monte Carlo (MC) | Diffusion Theory (DT) | Markov Chain (MC) Approx. |
|---|---|---|---|
| Theoretical Basis | Stochastic simulation of photon packets [107] | 1st-order approximation of RTE [107] | Matrix representation of state transitions [1] |
| Computational Cost | High (millions of photon tracks) [107] | Low (solving PDE) [107] | Moderate (matrix multiplications) [1] |
| Accuracy | Gold standard [107] | Accurate only for (\mus' \gg \mua), fails at boundaries & high absorption [52] [107] | Agrees well with MC for various media, handles anisotropy well [1] |
| Handling of Anisotropy | Uses phase functions (e.g., Henyey-Greenstein) [1] | Assumes near-isotropic radiance [107] | Accommodates non-uniform phase functions (e.g., Mie) [1] |
| Inverse Problem Capability | Possible but computationally intensive [27] | Standard for optical tomography [107] | Well-suited via matrix inversion [1] |
| Primary Application Scope | Heterogeneous tissues, validation of other models [27] [107] | Deep tissue imaging ((\mus' \gg \mua)) [107] | Anisotropic scattering, slab geometries [1] |
Experimental Protocols and Methodologies
Protocol for Standard Monte Carlo Simulation
The widely referenced MC algorithm for multi-layered tissues (MCML) involves a precise sequence of steps to track photon trajectories [107].
- Photon Initialization: A photon packet is launched with a specific starting location, direction, and an initial statistical weight, (W_0), typically set to 1 [107].
- Step Size Selection: A random step size, (s), is calculated for the photon's next move based on the total attenuation coefficient: (s = -\ln(\xi)/\mu_t), where (\xi) is a random number in (0,1] [107].
- Photon Movement & Absorption: The photon is moved by the distance (s). Its weight is decreased to account for absorption: (W{new} = W{old} \times (\mus / \mut)). The remaining weight is scattered.
- Scattering Event: A new propagation direction is calculated by sampling the scattering phase function (e.g., Henyey-Greenstein). The azimuthal angle (\phi) is sampled uniformly in [0, 2π), while the deflection angle (\theta) is sampled from the phase function's distribution [1].
- Boundary Handling: If the photon encounters a boundary between tissues with different refractive indices, a probability of internal reflection is calculated using Fresnel's equations. The photon is either reflected internally or transmitted out of the medium based on a random number decision [109].
- Photon Termination: The photon packet is terminated when its weight falls below a pre-defined threshold (e.g., 0.0001). The "Russian roulette" method gives the photon one chance in (m) (e.g., (m=10)) to survive with its weight multiplied by (m); otherwise, it is terminated [1].
- Data Recording: The simulation records the position and weight of absorbed photons (for 3D absorption maps) and the position, weight, and exit direction of photons that leave the medium (for reflectance and transmittance profiles) [109].
Protocol for Markov Chain Approximation
The implementation of a Markov Chain model for light propagation, as discussed in the literature, follows a structured mathematical procedure [1].
- State Space Definition: The continuous variables of photon position and direction are discretized to create a finite state space. For example, directions on the unit sphere can be discretized into a set of solid angles.
- Transition Matrix Construction: The core of the model is the transition probability matrix (\mathbf{P}). Each element (P_{ij}) of this matrix is computed based on the scattering phase function and represents the probability of a photon transitioning from state (i) (a specific position and direction) to state (j).
- Initial State Vector: The light source is defined by an initial state probability vector, (\mathbf{\pi}(0)). This vector is typically a one-hot encoded vector if all photons start in a single known state.
- State Propagation: The photon probability distribution after (n) scattering events is computed through iterative matrix multiplication: (\mathbf{\pi}(n) = \mathbf{\pi}(n-1) \mathbf{P}). This efficiently propagates the entire probability distribution forward in "scattering time."
- Absorption Modeling: Absorption can be incorporated by adding an "absorbing state" to the Markov chain from which there is no escape, or by scaling the state probabilities at each step by a survival probability derived from (\mu_a).
- Output Calculation: The final state probability distributions are used to compute measurable quantities of interest, such as the angular distribution of transmitted or reflected photons [1].
Experimental Validation with Tissue Phantoms
Empirical validation of these models is critical. A common methodology involves the use of tissue-simulating phantoms with well-controlled optical properties [108].
- Phantom Fabrication: Phantoms are created using materials such as intralipid (scattering agent), ink (absorption agent), and agarose or silicone (base matrix) to achieve specific values of (\mua) and (\mus').
- System Calibration: The imaging system (e.g., a camera and light source setup like OPTIMAP) is first calibrated using phantoms with known optical properties to establish a baseline and account for system-specific artifacts [108].
- Data Acquisition: Measurements are taken, typically of spatially-resolved diffuse reflectance. In one approach, a digital micromirror device (DMD) projects a structured dot-like pattern onto the phantom surface, and a near-infrared camera captures the diffuse halo of re-emitted light around each illumination point [108].
- Inverse Problem Solving: The measured diffuse reflectance profiles are fitted using a light propagation model (e.g., MC, DT, or Markov Chain) in an inverse problem framework to estimate the phantom's optical coefficients ((\mua), (\mus)). The accuracy of each model is assessed by comparing the estimated coefficients to the known true values of the phantom [27] [108].
Visualizing Model Workflows and Interactions
The following diagram illustrates the core logical structure and workflow of the three modeling approaches, highlighting their fundamental differences.
Figure 1: Workflow of Light Propagation Models. This diagram illustrates the fundamental operational sequences for the Monte Carlo (stochastic tracking), Diffusion Theory (deterministic PDE solving), and Markov Chain (matrix-based propagation) approaches.
Successful implementation of the models described in this guide often relies on both computational tools and physical materials for validation. The following table details key resources used in this field.
Table 2: Essential Research Reagents and Computational Tools
| Item Name | Type | Primary Function / Application |
|---|---|---|
| MCML Software [107] | Software | A standard MC simulation program for light propagation in multi-layered flat media. |
| MOSE (Molecular Optical Simulation Environment) [107] | Software | A versatile software environment for 2D and 3D MC simulation in complex media. |
| Intralipid [108] | Laboratory Reagent | A standardized fat emulsion commonly used as a scattering agent in tissue-simulating phantoms. |
| India Ink [108] | Laboratory Reagent | Used as a controlled absorption agent in the fabrication of optical tissue phantoms. |
| Agarose [108] | Laboratory Reagent | A gelling agent used to create solid, stable hydrogels that serve as the base matrix for tissue phantoms. |
| Digital Micromirror Device (DMD) [108] | Hardware | A spatial light modulator used in advanced imaging systems (e.g., OPTIMAP) to project structured illumination patterns onto a sample surface. |
| OPTIMAP Platform [108] | Hardware/Software | A low-cost, contact-free imaging platform that uses a DMD and camera for multisite acquisition of diffuse optical signals. |
This comparative analysis elucidates the distinct roles of Monte Carlo, Diffusion Theory, and Markov Chain approximations in modeling light propagation through biological tissues. The Monte Carlo method remains the undisputed benchmark for accuracy and flexibility, capable of modeling complex, heterogeneous tissues, albeit at a high computational cost. Diffusion Theory offers a highly efficient alternative that is sufficient for many applications involving deep-penetrating light in highly scattering tissues, but its inaccuracies in low-scattering, high-absorption, and boundary regions are a significant limitation. The Markov Chain approximation emerges as a powerful intermediary, combining the ability to handle complex scattering physics with a structured matrix-based framework that is less computationally demanding than pure MC simulation and is well-suited for inversion studies.
The future of the field lies in the intelligent integration of these methods. Hybrid models, which leverage the speed of DT or SPN approximations in suitable regions and the accuracy of MC in others, are already showing promise for achieving both computational efficiency and high accuracy [108] [107]. Furthermore, the application of these models to solve inverse problems—estimating tissue optical properties from surface measurements—is of paramount importance for clinical translation in areas such as melanoma depth estimation [27] [108] and monitoring photodynamic therapy outcomes [27]. As computational power increases and algorithms become more sophisticated, these light propagation models will continue to be indispensable tools for researchers and drug development professionals advancing optical technologies in medicine.
Within the field of biomedical optics, Monte Carlo (MC) simulations are considered the gold standard for modeling stochastic light propagation in complex, turbid media like biological tissue [3] [110]. The accuracy of these models is paramount, as they underpin critical applications including functional near-infrared spectroscopy (fNIRS), optogenetics, and non-destructive quality assessment in agriculture [111] [3] [110]. However, a model's theoretical sophistication is only as valuable as its empirical validation. This guide provides an in-depth technical framework for assessing the performance of MC light transport models, focusing on quantitative metrics and methodologies for establishing agreement with experimental data, a core component of rigorous computational research in this domain.
A significant challenge in the field is the scarcity of widely accepted reference values for tissue optical properties, often leading to highly variable experimental results [111]. Furthermore, the structural anisotropy of tissues, such as the organized axon bundles in white matter, complicates modeling by introducing directional dependence in light scattering, which traditional isotropic models fail to capture [111]. Therefore, a systematic approach to validation is not merely beneficial but essential for developing models that are quantitatively accurate and reliably inform both research and clinical applications.
Fundamental Concepts of Model Validation
Before applying specific metrics, it is crucial to define the object of validation. For MC models of light propagation, the primary physical quantities used for comparison include:
- Spatially-Resolved Diffuse Reflectance: The profile of light reflected from a tissue surface as a function of distance from the source.
- Time-Resolved Transmittance: The temporal spread of a short light pulse after transmission through a tissue sample.
- Penetration Depth: The depth at which the incident light intensity falls to 1/e (~37%) of its surface value [3].
- Internal Fluence Distribution: The spatial map of light energy absorption within the tissue volume.
Validation typically progresses through three tiers of increasing complexity:
- Benchmarking: Comparing simulation results against analytical solutions for simple, well-defined geometries.
- Phantom Studies: Using tissue-simulating phantoms with known optical properties to validate model predictions under controlled conditions [112].
- Biological Validation: The final and most rigorous stage, where model predictions are compared against measurements from actual biological tissues.
The following workflow outlines a structured approach for the latter two, experimental stages of validation.
Key Performance Metrics and Their Application
The choice of performance metric depends on the nature of the simulated and experimental data. The table below summarizes the primary quantitative metrics used for model validation.
Table 1: Key Performance Metrics for Model-Experiment Agreement
| Metric | Formula/Description | Application Context | Interpretation | ||
|---|---|---|---|---|---|
| Percent Difference | (\frac{ | V{exp} - V{sim} | }{V_{exp}} \times 100\%) | Validation of scalar quantities (e.g., total transmitted power, penetration depth) [113] [3]. | A value of < 10% is often considered excellent agreement in phantom studies [113]. |
| Coefficient of Determination (R²) | (1 - \frac{\sum (y{exp} - y{sim})^2}{\sum (y{exp} - \bar{y}{exp})^2}) | Assessing the goodness-of-fit for continuous data profiles (e.g., spatial reflectance, temporal point spread functions). | An R² value close to 1.0 indicates the model explains most of the variance in the experimental data. | ||
| Optical Fractional Anisotropy (OFA) | (\sqrt{\frac{1}{2} \frac{(Dx-Dy)^2+(Dy-Dz)^2+(Dz-Dx)^2}{Dx^2+Dy^2+D_z^2}}) [111] | Quantifying the accuracy of models in anisotropic tissues (e.g., white matter, muscle) [111]. | Ranges from 0 (isotropic) to 1 (perfectly anisotropic); should match values from DTI or other independent methods. | ||
| Median Error Reduction | Median of per-measurement-point error after applying a correction model. | Evaluating the effectiveness of models in correcting for physical artifacts (e.g., tissue curvature) [114]. | A significant reduction in median error indicates the model successfully corrects for the artifact. |
Case Studies in Metric Application
Validation with Phantoms and Simple Tissues: In a study on Cherenkov emission, a hybrid MC model showed an average percent difference of 6.2% when compared to measured emission from a blood and intralipid phantom, validating its accuracy for complex treatment plan modeling [113]. Similarly, in agricultural optics, MC simulations correctly predicted a significant difference in light penetration depth between healthy and blackhearted potato tissues (~6.73 mm vs. ~1.30 mm at 805 nm), which was consistent with the measured increase in absorption and scattering coefficients in diseased tissue [3].
Addressing Anisotropy with OFA: A key study on human brain white matter highlighted the limitations of isotropic models. The researchers introduced the Optical Fractional Anisotropy (OFA) metric, derived from the light diffusion tensor, to characterize the directional dependence of scattering correlated with local axon fiber orientation [111]. A successful model must not only fit reflectance data but also reproduce the experimentally determined OFA, moving beyond scalar metrics to tensor-based validation.
Correcting for Geometrical Effects: Research on near-infrared spectroscopy for diabetic foot ulcers used MC simulations to develop curvature correction models. Performance was assessed by how much the models reduced the median error in diffuse reflectance signals and derived hemoglobin parameters on wound-mimicking geometries [114]. This demonstrates the use of validation metrics to improve quantitative measurements in clinically challenging scenarios.
Experimental Protocols for Validation
A robust validation requires meticulous experimental methodology. The following protocols are commonly employed to generate high-quality data for comparison with MC simulations.
Time- and Space-Resolved Reflectance Measurements
This protocol is used for comprehensive characterization of light transport, especially in anisotropic tissues.
- Sample Preparation: Human or animal tissue samples are fixed and stored in formalin or phosphate-buffered saline to preserve structural integrity [111].
- Optical Gating: A pulsed laser source and a time-gated, spatially-resolved camera are used to image the transverse propagation of diffusely reflected light with high temporal and spatial resolution [111].
- Independent Orientation Validation: The local fiber orientation of the tissue (e.g., axon bundles in white matter) is independently determined using techniques like light sheet fluorescence microscopy or two-photon fluorescence microscopy [111]. This provides a ground truth for correlating with optical anisotropy.
- Data Acquisition: Diffuse reflectance profiles are captured along different directions relative to the fiber orientation and at multiple time points following the light pulse.
Integrating Sphere Systems for Bulk Optical Properties
This method is a standard for estimating the absorption ((\mua)) and reduced scattering coefficients ((\mus')) of a tissue sample, which are direct inputs to the MC model.
- Setup Configuration: The system comprises an integrating sphere with a reflective inner coating (e.g., PTFE), a broadband light source (e.g., halogen lamp), and a Vis-NIR spectrometer [3] [110].
- Measurement: A thin, uniformly sliced tissue sample is prepared. The sample is placed first over the sphere's sample port to measure total diffuse reflectance ((Rt)) and then placed at the exit port to measure total transmittance ((Tt)) [3].
- Inverse Adding-Doubling (IAD): The measured (Rt) and (Tt) are used as inputs to the IAD algorithm, which computes the intrinsic optical properties (\mua) and (\mus') of the sample [3] [112]. These values are used to parameterize the MC simulation.
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential materials and their functions for conducting experiments on light propagation in tissues.
Table 2: Essential Research Reagents and Materials for Light-Tissue Interaction Studies
| Item | Function/Description | Example Use Case |
|---|---|---|
| Titanium Dioxide (TiO₂) | Scattering agent suspended in a base material (e.g., mineral oil, polymer) to mimic tissue scattering [112]. | Key component of stable, tissue-mimicking phantom materials [112]. |
| Polystyrene-block-poly(ethylene-ran-butylene)-block-polystyrene (SEBS) | A stable copolymer used as a base material for durable, anthropomorphic phantoms [112]. | Creating forearm phantoms with vessel-like structures for oximetry validation [112]. |
| Proxy Dyes (e.g., for Hemoglobin) | Organic dyes with specific absorption spectra used to mimic the absorption profiles of oxy- and deoxyhemoglobin [112]. | Fabricating vessel phantoms with precisely controlled oxygen saturation levels for imaging studies [112]. |
| Intralipid | A fat emulsion commonly used as a standardized scattering medium in optical phantom studies [113] [3]. | Used in blood and intralipid phantoms to validate Cherenkov emission models [113]. |
| Neutral Buffered Formalin | A fixative solution used to preserve the structural integrity of post-mortem biological samples for optical measurements [111]. | Preparation of human brain tissue samples for anisotropic scattering measurements [111]. |
| Spatial Light Modulator (SLM) | A phase-modulating device used to generate structured light beams, such as those carrying Orbital Angular Momentum (OAM) [67]. | Studying the propagation of OAM beams through biological tissue to compare transmittance with Gaussian beams [67]. |
Accurately assessing the agreement between Monte Carlo simulations and experimental data is a critical, multi-faceted process. It requires moving beyond qualitative comparisons to a rigorous, quantitative framework that employs metrics like percent difference, R², and Optical Fractional Anisotropy, tailored to the specific research context. The protocols and tools detailed in this guide provide a pathway for researchers to validate their models against high-quality experimental data, from controlled phantom studies to complex biological tissues. As the field advances with applications in neuroimaging, cancer treatment, and precision agriculture, the commitment to robust model validation will ensure that MC simulations continue to be a trustworthy and powerful tool for probing the interaction of light with living systems.
In the field of biomedical optics, Monte Carlo (MC) simulations are considered the gold standard for modeling light propagation in biological tissues, providing rigorous solutions to the radiative transport equation for systems with complicated geometric and material features [115]. These simulations are particularly valuable in neuroscience for optimizing optical techniques such as optogenetic stimulation and calcium imaging, enabling researchers to identify the spatial reach of optogenetic stimulation inside cortical tissue and the spatial blurring of optically recorded neuronal activation [61] [46]. However, the computational cost and potential inaccuracies in model implementation can lead to significant discrepancies that limit their utility and reliability.
This technical guide examines the principal sources of error in simulations of light propagation in biological tissues, with a specific focus on Monte Carlo methods and alternative approaches. We present a systematic framework for identifying, quantifying, and correcting these errors to enhance simulation accuracy and computational efficiency, framed within the context of advancing optical techniques in neuroscience and biomedical research.
Simulations of light propagation in biological tissues are susceptible to several categories of error, each requiring distinct identification and correction strategies. The table below summarizes the major error sources and their impacts.
Table 1: Principal Sources of Error in Light Propagation Simulations
| Error Category | Specific Error Types | Impact on Simulation Results |
|---|---|---|
| Model Implementation Errors | Ambiguous mathematical formulations [61] [46], Incorrect parameter derivation [61] | Inconsistencies between published and simulated results, Restricted simulation volumes [61] |
| Computational Method Limitations | Excessive computational demands [61] [115], Finite sampling errors [115] | Limited practical application, Solution uncertainty scaling as 1/√N [115] |
| Optical Property Specification | Inaccurate absorption (μa) or scattering (μs) coefficients [3] | Incorrect penetration depth estimates [3], Flawed energy distribution maps |
| Variance Estimation Challenges | Inaccurate perturbation Monte Carlo (pMC) variance prediction [115] | Limited application range for pMC methods, especially in multispectral datasets [115] |
Model Implementation and Mathematical Ambiguities
A primary source of error in light propagation models stems from ambiguous mathematical formulations and incomplete documentation. The replication of the Yona et al. model revealed that the original implementation contained unresolved ambiguities in key aspects, particularly in the parametrization of the time dispersion distribution G, which depends on the first (μτ) and second (στ) moments of the multi-path time [61] [46].
The replication effort identified that the original article referenced McLean et al. for calculating these moments, but McLean et al. provided three different sets of equations without clear guidance on which to use [46]. The precise derivation by Lutomirski et al. enables calculation of the first moment μτ but not the second moment στ, as it depends on the second moment of the cosine of the scattering angle (⟨cos(θ)²⟩), which was not derivable from the provided references [46]. This mathematical ambiguity represents a critical source of potential error in model implementation.
Computational Efficiency and Sampling Errors
Traditional Monte Carlo methods suffer from excessive computational demands, making them impractical for many research applications [61]. The stochastic nature of these simulations carries with it a solution uncertainty that scales as 1/√N, where N is the number of photons simulated [115]. This fundamental limitation means that achieving high accuracy requires computationally expensive simulations with large photon counts.
In perturbation Monte Carlo (pMC) methods, which are designed to improve computational efficiency, a significant challenge arises from the inability to accurately predict the growth in pMC solution uncertainty with increasing perturbation size [115]. Without a method to quantify this relationship, the range of optical properties over which pMC can provide accurate predictions remains limited, particularly for multispectral datasets where variations in optical absorption and scattering properties can be substantial [115].
Error Correction Methodologies and Protocols
Model Clarification and Replication
To address implementation errors in the Yona et al. model, researchers undertook a systematic replication and correction process. The methodology involved:
Identifying Mathematical Ambiguities: The team analyzed three sets of equations for calculating the moments of multi-path time provided by McLean et al. and determined that the approximations by van de Hulst and Kattawar were the only ones that could be fully resolved, as they do not depend on the second moment of the squared scattering angle (⟨θ⁴⟩) [46].
Correcting Implementation Errors: The replication identified and corrected errors in the original MATLAB software that caused discrepancies between simulations and published results [61] [46].
Enhancing Computational Efficiency: Through optimization of the algorithm and parametrization of numerical integrals, the team improved computational efficiency by an order of magnitude, enabling simulations of cortical volumes exceeding 1 mm³ to run in seconds on standard laptop hardware [61] [46].
Open-Source Implementation: All resulting code was open-sourced with detailed documentation, adhering to FAIR principles to ensure broad utility for the neuroscience community [61] [46].
The parametrization for numerical integrals and sampling used in the corrected model is summarized in the table below.
Table 2: Parametrization for Numerical Integrals and Sampling in Corrected Model
| Parameter | Value | Unit | Description |
|---|---|---|---|
| Tissue Properties | |||
| n_tissue | 1.36 | Refractive index of cortical tissue | |
| mu_a | 0.00006 | μm⁻¹ | Absorption coefficient |
| mu_s | 0.0211 | μm⁻¹ | Scattering coefficient |
| g | 0.86 | Anisotropy factor | |
| Optical Fiber | |||
| NA | 0.37 | Numerical aperture of the fiber | |
| opt_radius | 100 | μm | Radius of the optical fiber |
| Sampling Parameters | |||
| ntausmpls | 100 | Number of time samples for multipath-time integral | |
| nsteps_theta | 24 | Number of angular steps in θ | |
| nsteps_phi | 24 | Number of angular steps in φ | |
| dxydirectdisk | 3 | μm | Stepsize for disk convolution of direct light |
| dxyscattereddisk | 10 | μm | Stepsize for disk convolution of scattered light |
Advanced Monte Carlo Techniques
For traditional Monte Carlo simulations, several advanced techniques have been developed to address errors and improve efficiency:
Perturbation Monte Carlo (pMC) Methods: pMC leverages correlated sampling by using a single set of random walks to analyze a reference system together with closely related systems with modified optical properties. The perturbed photon weight for the i-th photon (WP,i) with perturbed optical properties (μa,P, μs,P) is computed from the reference photon weight (WR,i) with reference optical properties (μa,R, μs,R) as follows [115]:
WP,i = WR,i (μs,P/μs,R)^ji exp[-(μt,P - μt,R)Li]
where ji is the number of collisions the i-th tallied photon experiences, and Li is the path length taken by the i-th photon prior to detection [115].
Variance Reduction Techniques: Researchers have developed methods to predict changes in pMC relative error using conventional error propagation methodology. This approach utilizes the variance, covariance, and skewness of the photon weight, path length, and collision distributions generated by the reference simulation, enabling estimation of pMC variance without explicit computation of perturbed photon weights [115].
Scaling Methods: For fluorescence simulations in multi-layered tissue models with oblique illumination and collection geometries, scaling methods have been developed that can achieve a 46-fold improvement in computational time while maintaining a mean absolute percentage error within 3% compared to independent simulations [30]. The methodology involves:
- Generating excitation and emission photon histories through baseline simulations.
- Scaling photon histories according to target optical properties to generate absorbed photon distribution A(x,y,z) at the excitation wavelength and emitted photon distribution E(x,y,z) at the emission wavelength.
- Calculating detected fluorescence intensity as FDetected = ∅eff ∑i,j{[∑k A(xi,yj,zk) * E(xi,yj,zk)] ⋅ P(xi,yj)}, where ∅_eff is the quantum yield of the tissue model [30].
Experimental Validation Protocols
To validate simulation results against experimental data, researchers have employed several methodological approaches:
Optical Properties Measurement: Using a single-integrating sphere (SIS) system with inverse adding doubling (IAD) algorithm to obtain optical properties. The system typically includes an integrating sphere with a sample port, an adjustable power halogen lamp, and a Vis-NIR spectrometer measuring wavelengths from 400 to 1000 nm [3].
Penetration Depth Calculation: Based on derived optical properties, the light penetration depth (σ) can be calculated as the level at which incident light is reduced to 1/e (~37%) in the tissue using the formula [3]:
σ = 1/√[3μa(μa + μ'_s)]
Monte Carlo Simulation in Homogeneous Tissues: Implementing voxel-based Monte Carlo simulation platforms such as Monte Carlo eXtreme (MCX) to simulate photon transport and compute optical attenuation characteristics based on estimated optical properties [3].
The following workflow diagram illustrates the comprehensive error identification and correction process for light propagation simulations:
The Scientist's Toolkit: Research Reagent Solutions
The table below summarizes essential computational tools and methodologies used in advanced light propagation simulations, with specific applications in error correction and validation.
Table 3: Research Reagent Solutions for Light Propagation Simulations
| Tool/Technique | Function | Application Context |
|---|---|---|
| Beam-Spread-Function (BSF) Model | Models light transport through cortical tissue using infinitesimal pencil beams [61] [46] | Alternative to MC simulations for optogenetic stimulation and calcium imaging setup design |
| Perturbation Monte Carlo (pMC) | Rapidly obtains estimates for systems slightly modified from reference using correlated sampling [115] | Solving inverse problems in diffuse optics; efficient analysis of closely related systems |
| Monte Carlo eXtreme (MCX) | Open-source, voxel-based Monte Carlo simulation platform [3] | Modeling photon transport and computing optical attenuation in biological tissues |
| Scaling Method for MC Fluorescence | Accelerates fluorescence simulations in multi-layered tissue models [30] | Efficient simulation of fluorescence spectra with oblique illumination/detection geometries |
| Single-Integrating Sphere (SIS) System | Measures total diffuse reflectance and transmittance for optical property determination [3] | Experimental validation of simulation results through optical properties measurement |
Accurate simulation of light propagation in biological tissues requires meticulous attention to potential error sources throughout the modeling process. Mathematical ambiguities, implementation errors, and computational limitations represent significant challenges that can be addressed through methodical replication, open-source implementation, and advanced Monte Carlo techniques including perturbation methods and variance reduction strategies.
The continuous refinement of these simulation methodologies, coupled with rigorous experimental validation using integrating sphere systems and comparative analysis with gold-standard Monte Carlo approaches, enables researchers to achieve increasingly accurate predictions of light behavior in complex biological environments. These advances are particularly valuable in the context of optical techniques in neuroscience, where precise understanding of light spread in cortical tissue is essential for both optogenetic stimulation and optical recording of neuronal activity.
As simulation methodologies evolve, the adoption of FAIR principles and open-source implementation will be crucial for ensuring transparency, reproducibility, and broad utility across the scientific community. Future research should focus on further enhancing computational efficiency while maintaining accuracy, particularly for complex multi-layered tissue models and multispectral applications.
The Role of MC in Calibrating and Informing Simplified Analytical Models
Monte Carlo (MC) simulations represent a gold standard in modeling light propagation within biological tissues, providing a robust stochastic framework for tracking photon trajectories through complex, multi-layered structures [116] [57]. These simulations account for critical optical phenomena, including absorption and scattering events, by leveraging random sampling techniques to solve the radiative transfer equation (RTE) [116]. Within the context of biomedical optics research, particularly for therapeutic and diagnostic applications such as photodynamic therapy and cancer detection, accurately modeling light distribution is paramount [57]. However, the high computational cost of MC methods often limits their direct use in iterative processes like treatment planning or real-time parameter estimation [116]. Consequently, a central challenge lies in leveraging the high accuracy of MC models to develop and calibrate faster, simplified analytical models—such as those based on the diffusion approximation—without sacrificing reliability [116]. This guide details the methodologies for using MC simulations as a foundational tool to inform, validate, and calibrate these simplified models, thereby enhancing their practical utility in clinical and research settings.
Theoretical Foundations of Light Propagation in Tissue
The interaction of light with tissue is primarily governed by its optical properties, which determine how light is absorbed and scattered. Accurate modeling requires a precise definition of these properties and the governing equations [116].
Key Optical Properties
The table below summarizes the fundamental parameters used to characterize tissue optical properties.
Table 1: Key Parameters for Quantifying Tissue Optical Properties
| Parameter | Symbol | Definition | Typical Order of Magnitude (NIR-I) |
|---|---|---|---|
| Absorption Coefficient | (\mu_a) | Probability of photon absorption per unit pathlength. | (0.1\ \text{cm}^{-1}) [116] |
| Scattering Coefficient | (\mu_s) | Probability of photon scattering per unit pathlength. | (100\ \text{cm}^{-1}) [116] |
| Reduced Scattering Coefficient | (\mu_s') | (\mus' = \mus(1-g)), represents the probability of equivalent isotropic scattering. | (10\ \text{cm}^{-1}) [116] |
| Anisotropy Factor | (g) | Average cosine of the scattering angle. | ~0.9 [116] |
Governing Equations and Simplified Models
The Radiative Transfer Equation (RTE) is the most comprehensive equation for describing light propagation in scattering media. It models the radiation through a medium affected by absorption, emission, and scattering [116]. Due to its complexity, several approximate solutions have been developed:
- Diffusion Approximation (DA): This is a first-order angular approximation to the RTE. It is valid in regimes where scattering dominates absorption ((\mus' \gg \mua)) and is accurate at distances far from the light source and after several scattering events have occurred. Its limitations include inaccuracies in low-scattering media, near sources, and in void-like regions [116].
- Beer-Lambert Law: This is the most straightforward model, relating the attenuation of light to the absorption coefficient and path length. It is inadequate for modeling bulk tissue where multiple scattering events are significant [116].
- Other Methods: These include the finite-element method, the adding-doubling method, random walk, and higher-order approximations to the RTE [116].
The Monte Carlo Method as a Gold Standard
The Monte Carlo method provides a flexible and accurate stochastic approach for simulating light transport by tracking the random walks of millions of photons through a medium defined by its optical properties ((\mua), (\mus), (g), (n)) [116] [57].
Workflow of a Standard MC Simulation
A typical MC simulation for light propagation follows a well-defined sequence of steps, as visualized below.
Diagram 1: Standard Monte Carlo simulation workflow for light propagation.
The process begins with defining the tissue model, including its geometry and optical properties [116] [7]. Photon packets are launched and propagated through the tissue in steps. At each step, the photon's weight is reduced due to absorption, and the photon is scattered into a new direction based on the anisotropy factor g [116]. This stochastic process continues until the photon's weight falls below a pre-set threshold or it exits the tissue geometry, at which point its data is recorded. The simulation aggregates data from millions of such photons to produce statistically robust results like spatial fluence rate distribution or diffuse reflectance [116].
Advanced MC Implementations and Acceleration
To address the high computational cost of traditional MC, several advanced implementations have been developed:
- White Monte Carlo: A single simulation is run, and the results are rescaled to cover a wide range of optical properties, drastically reducing the need for repeated simulations [116].
- Voxel-Based MC (e.g., MCX): Allows for modeling complex, heterogeneous geometries by representing the tissue as a 3D grid of voxels, each with assigned optical properties [7].
- Scaled MC: Uses scaling relations to quickly regenerate simulations for small inhomogeneities, speeding up the process for iterative optimization schemes [116].
Calibrating Simplified Models with MC Data
The primary role of MC simulations in this context is to generate high-fidelity data for calibrating the parameters of faster, simplified models. This process ensures the simplified model's output closely matches the gold-standard MC result over a defined range of optical properties.
Calibration Workflow and Parameter Search
The calibration process is an inverse problem that systematically adjusts the parameters of a simplified model to minimize its discrepancy from MC-generated reference data.
Diagram 2: Iterative workflow for calibrating simplified models using MC data.
The process begins by running MC simulations to generate a robust dataset of light transport outcomes (e.g., diffuse reflectance) across a range of optical properties [116]. A simplified model is then defined, and a quantitative Goodness-of-Fit (GOF) metric, such as Mean Squared Error (MSE), is selected to measure the discrepancy between the simplified model's output and the MC reference data [117]. A parameter search algorithm is employed to iteratively adjust the simplified model's parameters to minimize the GOF metric. The process continues until a stopping rule is met [117].
Parameter Search Algorithms
Various search algorithms can be used for the calibration process, each with its own advantages. The table below summarizes the most commonly used algorithms in biomedical model calibration.
Table 2: Common Parameter Search Algorithms for Model Calibration
| Algorithm | Description | Advantages / Disadvantages |
|---|---|---|
| Grid Search | Exhaustively searches over a discretized parameter space [117]. | Simple to implement, but computationally prohibitive for high-dimensional spaces [117]. |
| Random Search | Randomly samples parameter combinations from the defined space [117]. | More efficient than grid search for spaces with low effective dimensionality; a predominant method in cancer models [117]. |
| Nelder-Mead | A direct search method that uses a simplex to navigate the parameter space [117]. | Derivative-free, often more efficient than random search but can get stuck in local minima [117]. |
| Bayesian Optimization | Builds a probabilistic model of the objective function to direct future sampling [117]. | Highly efficient for expensive objective functions, but underutilized in some fields [117]. |
| Genetic Algorithm | A population-based metaheuristic inspired by natural selection [117]. | Good for global search in complex, non-convex spaces [117]. |
Experimental Protocols and Case Studies
Protocol: Calibrating a Diffusion Model for a Multi-Layered Tissue
This protocol outlines the steps to calibrate a simplified diffusion theory model using a voxel-based MC simulation for a multi-layered structure, such as skin or fruit.
- Define Tissue Geometry and Optical Properties: Establish a multi-layered model (e.g., epidermis, dermis, hypodermis for skin; or oil sac, albedo, pulp for fruit) [7]. For each layer, acquire or estimate the wavelength-dependent optical properties: (\mua), (\mus), (g), and (n).
- Generate MC Reference Data:
- Use a voxel-based MC tool like Monte Carlo eXtreme (MCX) to simulate photon propagation in the defined model [7].
- Configure the source type (e.g., point source, pencil beam) and detector positions.
- Run simulations for a sufficient number of photons (e.g., (10^7) to (10^9)) to achieve low statistical noise.
- Output key metrics such as the spatially-resolved diffuse reflectance, internal fluence rate, and the fractional energy absorbed per layer.
- Define the Simplified Model and GOF:
- Select a simplified model, such as a solution to the diffusion equation for a multi-layered slab [116].
- Choose a GOF metric. The Mean Squared Error (MSE) between the MC-derived diffuse reflectance and the simplified model's prediction across multiple source-detector distances is a common and effective choice [117].
- Execute Calibration:
- Select a parameter search algorithm. For a few parameters, the Nelder-Mead method is a good starting point due to its efficiency [117].
- Define the parameter bounds for the simplified model (e.g., adjustable effective scattering coefficients for each layer).
- Run the optimization loop, iteratively comparing the simplified model's output to the MC reference and updating parameters until the GOF is minimized or a stopping rule is triggered.
- Validate the Calibrated Model: Test the performance of the calibrated simplified model against a new set of MC data generated with optical properties not used in the calibration. This validates its predictive accuracy and generalizability.
Case Study: Optimizing Spectral Detection for Orah Mandarin
A recent study perfectly illustrates this calibration philosophy. Researchers aimed to optimize a Vis/NIR spectroscopy device for non-destructive quality assessment of Orah mandarin, a multi-layered fruit [7].
- MC as the Gold Standard: The optical properties ((\mua), (\mus')) of the fruit's three layers (oil sac, albedo, pulp) were measured. A voxel-based MC simulation was then used to model light propagation and quantify how much each tissue layer contributed to the detected diffuse reflectance signal at different source-detector distances [7].
- Informing Device Design: The MC simulations revealed that as the source-detector distance increased, the contribution of the pulp tissue to the detected signal also increased. Based on this MC-informed insight, the researchers determined that a source-detector distance of 13-15 mm was optimal. This configuration maximized the pulp signal while maintaining sufficient signal strength, thereby directly calibrating and informing the design of a practical, optimized device without building a single physical prototype [7].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Item / Tool | Function / Description | Relevance to MC and Model Calibration |
|---|---|---|
| Single Integrating Sphere System | Measures the reflectance and transmittance of thin tissue samples. | Used to acquire the baseline optical properties ((\mua), (\mus), (g)) of tissue samples, which are essential inputs for both MC and simplified models [7]. |
| Inverse Adding-Doubling (IAD) Method | A computational algorithm used to invert measured reflectance and transmittance data to calculate the intrinsic optical properties of a sample. | Often coupled with integrating sphere measurements to determine the absorption and scattering coefficients needed for simulations [7]. |
| Voxel-Based MC Platform (e.g., MCX) | A computationally efficient Monte Carlo simulator that models light transport in 3D heterogeneous media represented by voxels. | Enables simulation of light propagation in complex, multi-layered tissues, providing the gold-standard data for calibration [7]. |
| Goodness-of-Fit Metrics (e.g., MSE) | A quantitative measure of the discrepancy between the simulated or model output and the reference data. | The objective function for calibration; guides the parameter search algorithm toward optimal parameter sets [117]. |
| Parameter Search Library (e.g., SciPy) | Software libraries containing implementations of optimization algorithms like Nelder-Mead, Bayesian optimization, etc. | Provides the computational engine for automating the calibration process and finding the best-fitting parameters for the simplified model [117]. |
Monte Carlo simulations are indispensable for developing accurate, simplified models of light propagation in tissue. By serving as a numerically rigorous and flexible reference, MC methods enable the calibration of faster analytical models, such as those based on the diffusion approximation, ensuring their reliability across a wide range of biologically relevant conditions. The structured calibration workflow—involving generating MC data, defining a goodness-of-fit metric, and executing a parameter search—provides a robust framework for researchers. As MC algorithms continue to advance and computational power grows, the synergy between detailed stochastic simulations and efficient simplified models will remain a cornerstone of progress in biomedical optics, paving the way for more effective diagnostic and therapeutic applications.
Conclusion
Monte Carlo simulation remains an indispensable and powerful tool for modeling light propagation in tissue, providing unmatched flexibility and accuracy for tackling complex problems in biomedical research. By mastering its foundational principles, methodological applications, and optimization techniques, researchers can reliably predict light distributions in scenarios ranging from diagnostic imaging to targeted therapies. The future of MC simulation is directed toward greater integration with patient-specific data, the use of high-performance computing to manage immense complexity, and its pivotal role in the development of personalized nanomedicine and novel optical-based therapeutics. As these computational techniques continue to evolve, they will undoubtedly bridge the gap between fundamental research and clinical translation, accelerating innovation in drug development and medical technology.
References
- 1. Advances in the simulation of light–tissue interactions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6694345/]
- 2. Modelling of Light Propagation in Tissue - Projects [https://www.urmc.rochester.edu/labs/baran/projects/modelling-of-light-propagation-in-tissue]
- 3. Assessment of Optical Properties and Monte Carlo-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12197157/]
- 4. Light transport in biological tissue based on the simplified ... [https://www.sciencedirect.com/science/article/pii/S0021999106003421]
- 5. Anisotropy of light propagation in biological tissue [https://opg.optica.org/ol/abstract.cfm?uri=ol-29-22-2617]
- 6. Light transport in biological tissue using three-dimensional ... [https://pubmed.ncbi.nlm.nih.gov/19336841/]
- 7. Monte Carlo Simulation of Light Propagation in Orah ... [https://www.sciopen.com/article/10.12133/j.smartag.SA202505029]
- 8. Radiative transfer [https://en.wikipedia.org/wiki/Radiative_transfer]
- 9. Mishchenko 2003: Radiative transfer theory [https://www.giss.nasa.gov/pubs/abs/mi05800e.html]
- 10. Monte Carlo method for photon transport [https://en.wikipedia.org/wiki/Monte_Carlo_method_for_photon_transport]
- 11. Efficient, Automated Monte Carlo Methods for Radiation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3515075/]
- 12. Exact analytical solutions and corresponding Monte Carlo ... [https://www.sciencedirect.com/science/article/abs/pii/S002240732100234X]
- 13. Experimental validation of a spectroscopic Monte Carlo light ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7720906/]
- 14. Accurate Monte Carlo simulation of frequency‐domain optical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6492136/]
- 15. Monte Carlo and analytic simulations in nanoparticle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5033609/]
- 16. PN, double-PN and Monte Carlo frameworks [https://www.sciencedirect.com/science/article/abs/pii/S0022407325003735]
- 17. 16.2 Stochastic Progressive Photon Mapping [https://www.pbr-book.org/3ed-2018/Light_Transport_III_Bidirectional_Methods/Stochastic_Progressive_Photon_Mapping]
- 18. Condensed history Monte Carlo methods for photon ... [https://www.sciencedirect.com/science/article/abs/pii/S0021999107000770]
- 19. Review of GPU-based Monte Carlo simulation platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394928/]
- 20. chemeurope.com/en/encyclopedia/Radiative_transfer_equation_and... [https://www.chemeurope.com/en/encyclopedia/Radiative_transfer_equation_and_diffusion_theory_for_photon_transport_in_biological_tissue.html]
- 21. (PDF) Optical properties of biological tissues: a review [https://www.academia.edu/9081433/Optical_properties_of_biological_tissues_a_review]
- 22. Measurements of optical properties of high-density media [https://opg.optica.org/ao/abstract.cfm?uri=ao-42-19-4023]
- 23. Spectral determination of μa, μs and g from single and ... [https://www.sciencedirect.com/science/article/abs/pii/S0022407319308544]
- 24. ECE 532, 3. Optical Properties [https://omlc.org/classroom/ece532/class3/musp.html]
- 25. Monte Carlo Light Scattering Programs [https://omlc.org/software/mc/]
- 26. Tutorial on Monte Carlo simulation of photon transport in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9979671/]
- 27. Monte Carlo methods for light propagation in biological ... [https://www.sciencedirect.com/science/article/abs/pii/S0025556415001716]
- 28. Monte Carlo simulations for solving the radiative transfer ... [https://engineering.tufts.edu/bme/fantini/research/monte-carlo-simulations-solving-radiative-transfer-equation]
- 29. Monte Carlo simulations: The Virtual Sandbox for Medical ... [https://bioemtech.com/science-letter/monte-carlo-simulations-the-virtual-sandbox-for-medical-physics/]
- 30. Scaling method for efficient Monte Carlo simulation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532332/]
- 31. Deep learning-based prediction of Monte Carlo dose ... [https://www.sciencedirect.com/science/article/pii/S2405631625000405]
- 32. MCCL: an open-source software application for Monte ... [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-27/issue-8/083005/MCCL--an-open-source-software-application-for-Monte-Carlo/10.1117/1.JBO.27.8.083005.full]
- 33. History of Monte Carlo modeling of light transport in tissues ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9295704/]
- 34. mcxyz.c [https://omlc.org/software/mc/mcxyz/]
- 35. GPU-based Monte Carlo Simulations: MCXCL/README [https://mcx.space/wiki/index.cgi/wiki/index.cgi?action=browse&id=MCXCL/README&revision=1.4]
- 36. MCML [https://www.bilab2012.com/research/mcml]
- 37. Coupling 3D Monte Carlo light transport in optically ... [https://www.sciencedirect.com/science/article/pii/S2213597914000202]
- 38. A phantom for visualization of three-dimensional drug release ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3739833/]
- 39. Discovering new 3D bioprinting applications: Analyzing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7294689/]
- 40. Direct 3-D printing of complex optical phantoms using ... [https://www.nature.com/articles/s41598-025-94390-7]
- 41. Toward fluorescence digital twins [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-30/issue-S3/S34104/Toward-fluorescence-digital-twins--multi-parameter-experimental-validation-of/10.1117/1.JBO.30.S3.S34104.full]
- 42. Review of Monte Carlo modeling of light transport in tissues [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-18/issue-5/050902/Review-of-Monte-Carlo-modeling-of-light-transport-in-tissues/10.1117/1.JBO.18.5.050902.full]
- 43. Monte Carlo-Based Optical Simulation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10968032/]
- 44. Monte Carlo Modeling of Photon Propagation Reveals ... [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2016.01404/full]
- 45. Monte Carlo modeling of light transport in tissue (Steady ... [https://ohsu.elsevierpure.com/en/publications/monte-carlo-modeling-of-light-transport-in-tissue-steady-state-an-2]
- 46. An open-source replication for fast and accessible light ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330681]
- 47. Parallelized Monte Carlo Photon Transport Simulations for ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2020.00283/full]
- 48. Modeling Light Transport in Tissues [https://coilab.caltech.edu/research/modeling-light-transport-in-tissues]
- 49. Assessment of Optical Properties and Monte Carlo-Based ... [https://www.mdpi.com/1424-8220/25/12/3713]
- 50. Extended-wavelength diffuse reflectance spectroscopy ... [https://www.nature.com/articles/s41597-024-02972-3]
- 51. Fast and accurate Monte Carlo simulations of subdiffusive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7510928/]
- 52. Monte Carlo modeling of light propagation in highly ... [https://pubmed.ncbi.nlm.nih.gov/2606490/]
- 53. Optical Tomography and Spectroscopy of Tissue XVI | (2025) [https://www.spie.org/Publications/Proceedings/Volume/13314]
- 54. Dual-wavelength photoacoustic imaging of sentinel lymph ... [https://pubmed.ncbi.nlm.nih.gov/40686555/]
- 55. A clinical feasibility study of a photoacoustic finder for ... [https://www.sciencedirect.com/science/article/pii/S2213597925000394]
- 56. Advancements in photoacoustic detection techniques for ... [https://www.nature.com/articles/s44384-025-00005-w]
- 57. Monte Carlo Simulations of Light-Skin Interactions [https://pubmed.ncbi.nlm.nih.gov/41110580/]
- 58. Optimizing the light delivery of linear-array-based ... [https://www.nature.com/articles/s41598-018-31430-5]
- 59. Motion-based dynamic light delivery to minimize laser ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077845/]
- 60. Dual-wavelength photoacoustic imaging of sentinel lymph ... [https://www.sciencedirect.com/science/article/pii/S2213597925000709]
- 61. An open-source replication for fast and accessible light ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404466/]
- 62. Optical stimulation of neural tissue - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7353819/]
- 63. Scattering of Sculpted Light in Intact Brain Tissue, with ... [https://www.nature.com/articles/srep11501]
- 64. Monte Carlo Simulations of Particle Interactions with Tissue in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6874200/]
- 65. Beam and Point Spread Functions [https://www.oceanopticsbook.info/view/radiative-transfer-theory/level-2/beam-and-point-spread-functions]
- 66. Point spread function [https://en.wikipedia.org/wiki/Point_spread_function]
- 67. OAM light propagation through tissue | Scientific Reports [https://www.nature.com/articles/s41598-021-82033-6]
- 68. in Virtual : a review - PMC clinical trials medical imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC7148435/]
- 69. In Silico Clinical : Transforming Trials ... Medical Device Validation [https://www.linkedin.com/pulse/silico-clinical-trials-transforming-medical-device-jinesh-xzoxf]
- 70. Monte Carlo simulation platform for laser Doppler flowmetry [https://pmc.ncbi.nlm.nih.gov/articles/PMC12379725/]
- 71. Modeling voxel-based Monte Carlo light transport with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7040455/]
- 72. A Computationally Efficient Monte-Carlo Model for Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10069992/]
- 73. Monte Carlo evaluation of uncertainties in photon and electron ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11244687/]
- 74. Statistics of maximum photon penetration depth in a two- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10890894/]
- 75. NeuralRTE: Forward photon transport simulations in turbid ... [https://www.sciencedirect.com/science/article/pii/S0010482525012442]
- 76. 7.2 Monte Carlo simulations of light transport in tissues [https://fiveable.me/biophotonics/unit-7/monte-carlo-simulations-light-transport-tissues/study-guide/RkJDySdzV4dbyH9O]
- 77. Light Portals : : Light Transport Variance Reduction [https://escholarship.org/uc/item/2z2051bb]
- 78. Variance-Reduction Methods for Monte Carlo Simulation of ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2021.718873/full]
- 79. Monte Carlo Methods in Practice [https://www.scratchapixel.com/lessons/mathematics-physics-for-computer-graphics/monte-carlo-methods-in-practice/monte-carlo-simulation.html]
- 80. NRRS: Neural Russian Roulette and Splitting [https://arxiv.org/html/2510.07868v1]
- 81. Flagged uniform particle splitting for variance reduction in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5785278/]
- 82. Enhanced optical imaging and fluorescent labeling for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11143489/]
- 83. ® Website MCNP [https://mcnp.lanl.gov/]
- 84. Recovering the Reduced Scattering and Absorption ... [https://www.mdpi.com/2304-6732/12/11/1118]
- 85. Improving light propagation monte carlo simulations with ... [https://impact.ornl.gov/en/publications/improving-light-propagation-monte-carlo-simulations-with-accurate/]
- 86. Development of anatomically accurate digital organ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11981654/]
- 87. Development of anatomically accurate digital organ models ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0320816]
- 88. Toward fluorescence digital twins: multi-parameter ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119851/]
- 89. Mastering Monte Carlo Simulation: Techniques and ... [https://www.investglass.com/mastering-monte-carlo-simulation-techniques-and-applications-in-2025/]
- 90. What Is Monte Carlo Simulation? [https://www.ibm.com/think/topics/monte-carlo-simulation]
- 91. Background suppression structured illumination ... [https://www.sciencedirect.com/science/article/abs/pii/S0030399224005565]
- 92. Scaling method for efficient Monte Carlo simulation of ... [https://pubmed.ncbi.nlm.nih.gov/41112788/]
- 93. Monte Carlo simulation of photon migration in 3D turbid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2863034/]
- 94. Verification method of Monte Carlo codes for transport ... [https://www.nature.com/articles/s41598-021-98429-3]
- 95. - High , robustly verified performance simulation with... Monte Carlo [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-23/issue-08/085001/High-performance-robustly-verified-Monte-Carlo-simulation-with-FullMonte/10.1117/1.JBO.23.8.085001.full]
- 96. Anthropomorphic tissue-mimicking phantoms for oximetry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12267859/]
- 97. Monte-Carlo simulation and tissue-phantom model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9203094/]
- 98. Narrative review of tissue-mimicking materials for MRI ... [https://www.sciencedirect.com/science/article/pii/S107881742400292X]
- 99. Monte Carlo method [https://en.wikipedia.org/wiki/Monte_Carlo_method]
- 100. How to Validate and Verify Monte Carlo Simulation Models [https://www.linkedin.com/advice/0/how-do-you-validate-verify-accuracy-reliability]
- 101. Comparative analysis of Monte Carlo simulations and ... [https://www.nature.com/articles/s41598-025-14223-5]
- 102. Detailed Analysis of Gamma - Shielding Characteristics of Ternary... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11244092/]
- 103. Monte Carlo Simulation of Gamma and Neutron Shielding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11801086/]
- 104. How Can ı validate my Monte Carlo Simulation? [https://math.stackexchange.com/questions/1462985/how-can-%C4%B1-validate-my-monte-carlo-simulation]
- 105. Monte Carlo simulation of gamma ray shielding parameters ... [https://www.sciencedirect.com/science/article/abs/pii/S0029549313005529]
- 106. characteristics of various spinel ferrite... Gamma radiation shielding [https://pubs.rsc.org/en/content/articlehtml/2021/ra/d0ra08372k]
- 107. Harnessing the Power of Hybrid Light Propagation Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8601256/]
- 108. Rapid diffused optical imaging for accurate 3D estimation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11847144/]
- 109. Simulating Light Propagation through Biological Media ... [https://arxiv.org/abs/2405.06810]
- 110. Simulation and sensitivity analysis of light propagation in ... [https://www.sciencedirect.com/science/article/abs/pii/S0263224125007018]
- 111. Anisotropic light propagation in human brain white matter - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12510258/]
- 112. Anthropomorphic tissue-mimicking phantoms for oximetry ... [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-30/issue-7/076006/Anthropomorphic-tissue-mimicking-phantoms-for-oximetry-validation-in-multispectral-optical/10.1117/1.JBO.30.7.076006.full]
- 113. Hybrid Monte Carlo model for efficient tissue Cherenkov ... [https://www.sciencedirect.com/science/article/pii/S1120179725000663]
- 114. Mathematical modeling and analysis for tissue curvature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448248/]
- 115. Analysis of relative error in perturbation Monte Carlo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10245552/]
- 116. Tutorial on methods for estimation of optical absorption and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11166171/]
- 117. A Scoping Review on Calibration Methods for Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346156/]