Laser-Tissue Interactions: Fundamentals, Clinical Applications, and Future Directions for Biomedical Research
This article provides a comprehensive examination of the fundamental principles and modern applications of laser-tissue interactions for researchers, scientists, and drug development professionals.
Laser-Tissue Interactions: Fundamentals, Clinical Applications, and Future Directions for Biomedical Research
Abstract
This article provides a comprehensive examination of the fundamental principles and modern applications of laser-tissue interactions for researchers, scientists, and drug development professionals. It explores the underlying physical mechanisms including optical properties, thermal effects, and selective photothermolysis. The content details advanced computational modeling approaches, reviews current clinical applications across medical specialties, and analyzes optimization strategies for improving efficacy and safety. Through comparative analysis of laser systems and validation methodologies, this resource serves as both a foundational reference and forward-looking guide to emerging trends in laser-based biomedical technologies.
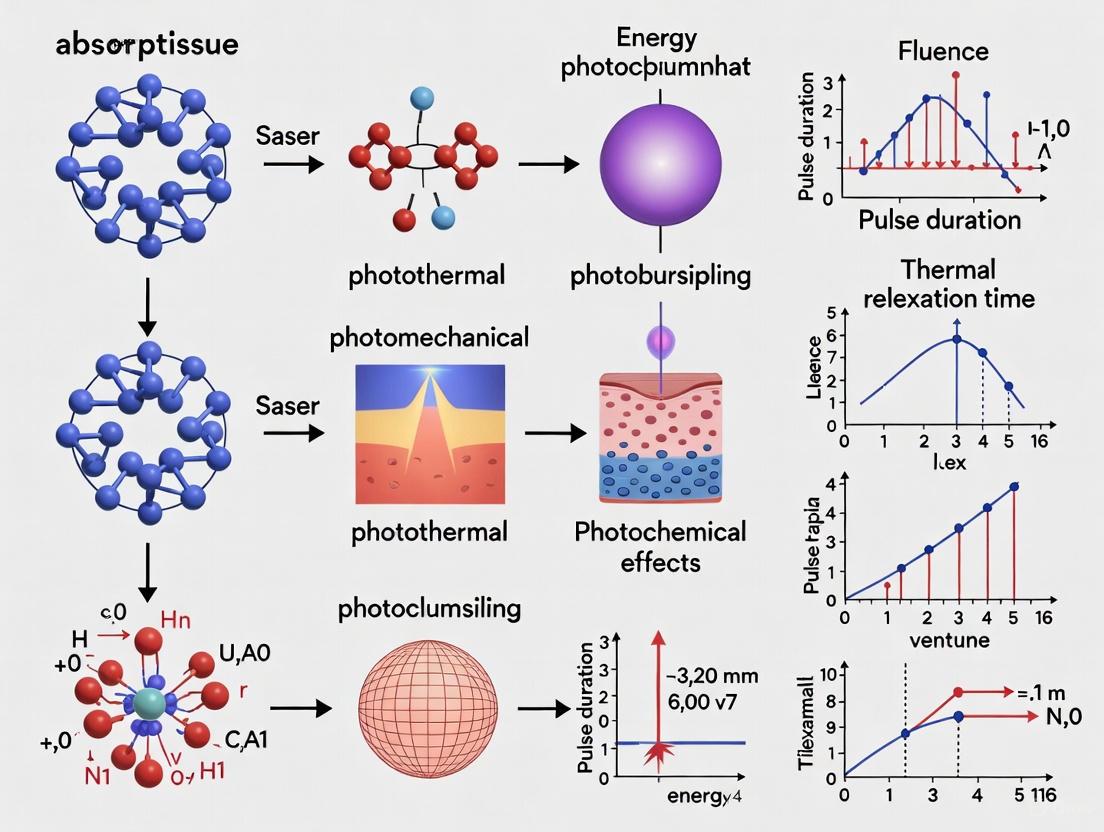
Fundamental Principles of Laser-Tissue Interactions: From Photons to Biological Effects
The interaction between laser light and biological tissue is fundamentally governed by the tissue's optical properties, primarily absorption and scattering. These properties determine how light energy is distributed within tissue, ultimately controlling the efficacy of both diagnostic and therapeutic laser applications in medicine and research. The propagation of light through biological tissues is characterized by absorption and scattering effects; absorption relates to the presence of chromophores (e.g., oxy-hemoglobin, deoxy-hemoglobin, water, lipid, and collagen), while scattering depends on inhomogeneities or fluctuations of the refractive index at the wavelength scale [1]. In the UV and visible spectral ranges, absorption limits light penetration to superficial tissue layers, whereas in the red and near-infrared (NIR) spectral region (approximately 600–1100 nm), known as the "therapeutic window," scattering dominates over absorption, allowing photons to penetrate deeply into tissues [1].
When laser light is applied to tissue, approximately 4–7% of the incident energy is reflected at the air-tissue interface due to the difference in refractive indices [2]. The remaining light may be absorbed by the tissue, transmitted through it, or scattered within it. Absorption refers to how tissues take up light energy, which is then converted into other forms, such as heat, leading to photothermal effects, or triggering photochemical reactions [3] [4]. Scattering causes the photon path to deviate from a straight line, diffusing light into the tissue rather than allowing it to travel in a linear fashion [3]. The combined effect of absorption and scattering determines penetration depth, defined as the depth at which light intensity decreases to 1/e (approximately 37%) of its original surface value [5]. These three factors—absorption, scattering, and penetration—are interrelated; increased scattering or absorption in tissue results in decreased penetration [3].
Understanding these optical properties is crucial for numerous biomedical applications, including photothermal therapy, photodynamic therapy, photobiomodulation, surgical ablation, and diagnostic imaging. This guide provides a comprehensive technical overview of the optical properties of biological tissues, with quantitative data, experimental methodologies, and practical resources for researchers and drug development professionals.
Fundamental Principles of Light Transport in Tissue
Key Optical Properties and Their Definitions
The propagation of light in biological tissues is quantitatively described by several key parameters:
- Absorption Coefficient (μₐ): This measures the probability of light absorption per unit path length in the tissue. It is expressed in units of cm⁻¹. A higher μₐ indicates that light is more readily absorbed, limiting its penetration. Absorption is primarily governed by chromophores present in the tissue [6] [1].
- Scattering Coefficient (μₛ): This defines the probability of light scattering per unit path length (cm⁻¹). Biological tissues are highly scattering due to variations in refractive index at cellular and subcellular levels [7] [1].
- Reduced Scattering Coefficient (μₛ′): In tissues, scattering is often anisotropic, with a preference for the forward direction. The reduced scattering coefficient, calculated as μₛ′ = μₛ(1 - g), accounts for this anisotropy and represents the equivalent isotropic scattering coefficient. Here, g is the anisotropy factor, which ranges from 0 for perfectly isotropic scattering to nearly 1 for highly forward-directed scattering [6] [1].
- Penetration Depth (δ): This is a critical parameter indicating the effective depth to which light can penetrate before being significantly attenuated. It is derived from the absorption and reduced scattering coefficients. When μₐ << 3μₛ′, it can be approximated as δ(λ) = 1 / √[3μₐ(λ)(μₐ(λ) + μₛ′(λ))] [6].
- Thermal Relaxation Time (TRT): This is the time required for tissue to dissipate about 50% of the thermal energy delivered by a laser pulse through conduction. Understanding TRT is essential for minimizing collateral thermal damage in laser-based surgeries and therapies [2].
The Role of Chromophores
Chromophores are molecules that absorb specific wavelengths of light. The primary chromophores in biological tissues and their absorption characteristics are:
- Hemoglobin: Found in blood, it absorbs strongly in the blue and green regions of the spectrum. Both oxygenated and deoxygenated hemoglobin have an absorption peak around 806 nm, while oxygenated hemoglobin also has a significant absorption region around 900 nm [3].
- Melanin: Located in the skin, it absorbs strongly across the ultraviolet and visible spectrum, with absorption decreasing as wavelength increases [3].
- Water: The most abundant molecule in the body. It has relatively low absorption in the visible and NIR regions but shows strong absorption peaks in the infrared, particularly at wavelengths like 1940 nm, 2780 nm, and 2940 nm [3] [4].
- Lipids/Fat: Absorbs light in the NIR, with a dominant peak at 930 nm [3].
The inverse relationship between a photon's energy and its wavelength (λ = hc/E, where h is Planck's constant and c is the speed of light) means that shorter wavelengths possess higher energy but are more readily absorbed by chromophores, thus penetrating less deeply. Longer wavelengths in the NIR region have lower energy but encounter less absorption, allowing for deeper tissue penetration [3] [4].
Quantitative Data on Tissue Optical Properties
The optical properties of tissues vary significantly depending on tissue type, physiological state, and the wavelength of incident light. The following tables consolidate quantitative data from recent experimental studies.
Table 1: Absorption (μₐ) and Reduced Scattering (μₛ′) Coefficients of Human Upper Urinary Tract Tissues (400-700 nm range, measured via DIS and IMC) [6].
| Tissue Type | μₐ at 450 nm (cm⁻¹) | μₛ′ at 450 nm (cm⁻¹) | μₐ at 600 nm (cm⁻¹) | μₛ′ at 600 nm (cm⁻¹) | μₐ at 650 nm (cm⁻¹) | μₛ′ at 650 nm (cm⁻¹) |
|---|---|---|---|---|---|---|
| Ureter | ~2.5 | ~25 | ~0.8 | ~18 | ~0.4 | ~16 |
| Fatty Tissue | ~0.7 | ~12 | ~0.3 | ~10 | ~0.2 | ~9 |
| Ureteral Carcinoma | ~4 | ~20 | ~1.2 | ~15 | ~0.6 | ~13 |
| Renal Pelvic Carcinoma | ~3.5 | ~22 | ~1 | ~16 | ~0.5 | ~14 |
Table 2: Absorption Coefficients (α) and Penetration Depth Rankings in Porcine Oral Gingival Tissue for Common Dental Laser Wavelengths [2].
| Laser Wavelength (nm) | Laser Type | Absorption Coefficient, α (cm⁻¹) | Ranking (Most to Least Absorbed) |
|---|---|---|---|
| 2940 | Er:YAG | 144.8 | 1 (Most Absorbed) |
| 2780 | Er,Cr:YSGG | ~120* | 2 |
| 450 | Blue Diode | 26.8 | 3 |
| 480 | Blue Diode | ~22* | 4 |
| 532 | KTP | ~18* | 5 |
| 1341 | Nd:YAP | ~15* | 6 |
| 632 | He-Ne | ~13* | 7 |
| 940 | Diode | ~11.5* | 8 |
| 980 | Diode | ~10.8* | 9 |
| 1064 | Nd:YAG | ~10.2* | 10 |
| 810 | Diode | 9.6 | 11 (Least Absorbed) |
Note: Values marked with an asterisk () are estimated from the ranking data provided in the source study [2].*
Table 3: Projected Light Penetration Depth (δ) in Human and Porcine Tissues [6].
| Tissue Type | δ at 450 nm (mm) | δ at 600 nm (mm) | δ at 650 nm (mm) |
|---|---|---|---|
| Human Ureter | ~0.20 | ~0.45 | ~0.55 |
| Human Fatty Tissue | ~0.55 | ~0.90 | ~1.05 |
| Human Ureteral Carcinoma | ~0.18 | ~0.35 | ~0.45 |
| Human Renal Pelvic Carcinoma | ~0.19 | ~0.40 | ~0.50 |
| Porcine Ureter | ~0.20 | ~0.45 | ~0.45 |
| Porcine Fatty Tissue | ~0.50 | ~0.85 | ~1.00 |
Experimental Methods for Characterizing Optical Properties
Accurate measurement of tissue optical properties is fundamental for research and clinical protocol development. Several well-established experimental techniques are employed.
Double Integrating Sphere (DIS) System with Inverse Monte Carlo (IMC)
This method is considered a gold standard for measuring the optical properties of ex vivo tissue samples.
- Principle: A tissue sample is illuminated with a focused, collimated light beam. A double integrating sphere setup simultaneously measures the total transmittance (Tₜ) and diffuse reflectance (Rd) from the sample. These measured values are then used in an Inverse Monte Carlo (IMC) simulation to iteratively determine the absorption (μₐ) and reduced scattering (μₛ′) coefficients that would produce the measured Tₜ and Rd [6].
- Protocol:
- Sample Preparation: Fresh tissue samples are collected and cut into specific geometries (e.g., 1 cm cubes). Sample thickness is precisely measured with a micrometer. Samples are sandwiched between glass slides and kept hydrated with saline to prevent dehydration and maintain optical properties [6].
- System Calibration: The DIS system is calibrated using diffuse reflectance standards and transmittance filters to ensure measurement accuracy [6].
- Measurement: The sample is placed at the input port of the DIS. Light from a broadband source (e.g., xenon lamp) is directed onto the sample. The spheres collect all transmitted and reflected light, which is then guided to a spectrometer for analysis [6].
- Inverse Monte Carlo Analysis: The measured Rd and Tₜ are input into an IMC model. The model varies μₐ and μₛ′ until the computed Rd and Tₜ match the experimental values within an acceptable error margin, thus yielding the final optical properties [6].
Kubelka-Munk (KM) Model
The KM model is a simpler, two-flux approximation method widely used to determine optical properties from reflectance and transmittance measurements.
- Principle: This model provides a mathematical framework to calculate the absorption (K) and scattering (S) coefficients based on the measured diffuse reflectance and transmittance of a tissue sample. Its major advantage is the direct analytical relationship between the coefficients and the measurements, avoiding complex computations [7].
- Protocol:
- Tissue samples are prepared similarly to the DIS method, with careful control of thickness.
- An integrating sphere coupled with a spectrometer is used to measure the total reflectance and transmittance of the tissue sample at specific laser wavelengths (e.g., 808, 830, 980 nm) [7].
- The Kubelka-Munk equations are applied to the measured data to derive the absorption and scattering coefficients. This model is particularly effective for optically thick samples where the light distribution is fully diffuse [7].
Time-Domain Diffuse Optics (TD-DO)
Time-domain techniques offer the highest information content for in-depth tissue characterization, particularly in living systems.
- Principle: The tissue is illuminated with an ultrashort picosecond laser pulse. A fast detector records the temporal distribution of the photons' time-of-flight (DTOF) as they are re-emitted from the tissue. Absorption affects the late-arriving photons (longer path lengths), while scattering influences the early part and the temporal broadening of the DTOF [1].
- Protocol:
- A pulsed laser source and time-correlated single-photon counting (TCSPC) electronics are used.
- The source and detector are placed on the tissue surface (reflectance geometry) or on opposite sides (transmittance geometry).
- The measured DTOF is fitted with a solution to the photon diffusion equation to extract μₐ and μₛ′. This method allows for depth-resolved assessment of optical properties and is less affected by superficial tissue color [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimentation in tissue optics requires specific tools and materials. The following table details key components used in the featured experiments.
Table 4: Essential Materials and Equipment for Tissue Optics Research.
| Item | Function/Application | Example from Literature |
|---|---|---|
| Double Integrating Sphere | Simultaneously measures total transmittance and diffuse reflectance from tissue samples, enabling accurate determination of optical properties [6]. | 4P-GPS-033-SL (Labsphere) [6] |
| Spectrometer | Detects and analyzes the spectrum of light transmitted through or reflected from tissue samples. | Maya2000Pro (Ocean Insight) [6] |
| Optical Parametric Oscillator (OPO) | A tunable laser system that generates specific wavelengths across a broad spectrum, allowing for wavelength-dependent studies. | VIS-OPO and MIR-OPO (Laserspec) [2] |
| Tissue Stabilization Setup | Holds tissue samples at a fixed thickness and prevents dehydration during measurements, ensuring consistent and reliable data. | Custom metal stabilization device with glass slides [2] |
| Calibrated Power Meter | Measures the absolute power of laser light before and after interaction with tissue, crucial for calculating attenuation. | Gentec-EO power meter [2] |
| Diffuse Reflectance Standards | Certified reference materials used to calibrate integrating sphere systems before tissue measurements. | SRS-99-010, SRS-10-010 (Labsphere) [6] |
| Fresh Ex Vivo Tissues | Biological samples from animal or human sources, used as models to study optical properties. | Porcine gingiva [2], human ureter and carcinomas [6], bovine adipose, chicken skin [7] |
Advanced Concepts and Research Applications
Photobiomodulation (PBM) and Dosimetry
Photobiomodulation therapy utilizes low-intensity light to stimulate biological processes. Its effectiveness is highly dependent on accurate dosimetry.
- Biphasic Dose Response: The therapeutic effect of PBM follows a biphasic pattern, often referred to as the Arndt-Schulz law. Very low doses may have no effect, moderate doses stimulate a positive therapeutic response, and excessively high doses can become inhibitory [5]. This makes precise dose delivery critical.
- Light Penetration and Dose: The penetration depth of PBM light in skin is the depth at which intensity falls to 37% (1/e) of its surface value [5]. Effective treatment of deep tissues requires wavelengths with sufficient penetration depth to deliver an adequate energy density to the target. Key parameters include wavelength, power density (irradiance, W/cm²), and energy density (fluence, J/cm²) [5].
Plasmonic Photothermal Therapy (PPTT)
PPTT is an advanced cancer treatment that combines the deep penetration of NIR light with the highly localized absorption of plasmonic nanoparticles.
- Principle: Gold nanoparticles (AuNPs) are introduced into tumor tissue. When irradiated with NIR light tuned to their localized surface plasmon resonance (LSPR) wavelength, the AuNPs efficiently absorb light and convert it into heat, selectively ablating the tumor [8].
- Optimization: The efficacy of PPTT depends on optimizing nanoparticle parameters (size, shape, composition) to match the LSPR to the tissue's optical window (700–1300 nm) and accounting for the thermal and optical properties of the specific target tissue [8]. Computational modeling, such as using Mie theory to calculate absorption cross-sections, is essential for protocol design [8].
Thermal therapy represents a cornerstone of modern medical treatment, leveraging controlled energy delivery to achieve precise biological effects. The fundamental principle underpinning all thermal therapies is selective photothermolysis, a theory described by Rox Anderson in 1983 that establishes the requirements for confining thermal damage to specific targets without affecting surrounding tissue [9]. This theoretical framework enables the entire spectrum of thermal interventions, from gentle hyperthermia to aggressive ablation, by providing the scientific basis for laser-tissue interactions [9].
The therapeutic landscape of thermal medicine spans a continuum defined by temperature ranges and their corresponding biological effects. Hyperthermia typically operates in the 39°C to 42°C range, focusing on physiological modulation and sensitization of tissue to other treatments [10]. In contrast, thermal ablation employs temperatures exceeding 44°C to achieve direct cellular destruction through protein denaturation and immediate necrosis [10]. The distinction between these modalities is not merely temperature-dependent but also defined by their mechanism of action, therapeutic objectives, and technical implementation.
Table 1: Fundamental Thermal Therapy Classifications
| Therapy Type | Temperature Range | Primary Mechanism | Therapeutic Objective |
|---|---|---|---|
| Mild Hyperthermia | 39°C - 42°C | Protein activation, membrane fluidity | Radiotherapy/chemotherapy sensitization |
| Moderate Hyperthermia | 42°C - 45°C | Heat shock protein induction, metabolic alteration | Immunological activation, drug delivery enhancement |
| Thermal Ablation | >44°C - 60°C | Protein denaturation, immediate coagulation | Direct tumor destruction |
| Irreversible Electroporation | Variable with significant Joule heating | Nanoscale membrane defects with thermal components | Non-thermal dominant cell death with thermal effects |
Hyperthermia: Mechanisms and Biological Effects
Molecular and Cellular Responses
Hyperthermia exerts its therapeutic effects through multifaceted biological mechanisms that operate at molecular, cellular, and tissue levels. At the molecular scale, heat shock proteins (HSPs) serve as critical mediators of the cellular stress response. These molecular chaperones, including HSP27, HSP47, HSP60/HSP10, HSP70, and HSP90, stabilize and repair damaged proteins, prevent harmful interactions between misfolded proteins, and facilitate the removal of defective cellular components [10]. The heat shock response represents a sequential information transmission process through the localized activity of these molecular chaperones [10].
The immunomodulatory effects of hyperthermia represent one of its most significant therapeutic mechanisms, particularly in oncology. Hyperthermia fundamentally alters the tumor microenvironment (TME) by promoting immunogenic cell death (ICD), enhancing the activity of immune cells including neutrophils, natural killer (NK) cells, and dendritic cells, and reducing immunosuppressive conditions [10]. This transformative capability allows hyperthermia to convert immunologically "cold" tumors with minimal immune infiltration into "hot" tumors characterized by significant immune cell presence and pro-inflammatory activity, thereby increasing their susceptibility to immune-mediated destruction [10].
Technical Implementation Modalities
Hyperthermia delivery systems encompass diverse technological approaches, each with specific tissue penetration characteristics and clinical applications. Magnetic hyperthermia therapy (MHT) utilizes magnetic nanoparticles (MNPs) that generate localized heat when exposed to an alternating magnetic field (AMF), achieving deep tissue penetration through Néel and Brownian relaxation mechanisms [11]. This approach enables intracellular hyperthermia when combined with cell-targeting ligands, resulting in direct therapeutic heating of cancer cells [11].
Other hyperthermia technologies include radiofrequency energy-based ablation, microwave-based approaches, laser interstitial thermal therapy, nanoparticle-driven photothermal therapy, high-intensity focused ultrasound (HIFU) ablation, and systemic whole-body hyperthermia (WBH) [10]. Each modality offers distinct advantages in terms of penetration depth, spatial precision, and temperature control, making them suitable for different clinical scenarios.
Table 2: Hyperthermia Delivery Technologies and Characteristics
| Technology | Energy Source | Penetration Depth | Temperature Control | Primary Applications |
|---|---|---|---|---|
| Magnetic Hyperthermia (MHT) | Alternating magnetic field | Deep tissue (cm) | Moderate via nanoparticle concentration | Deep-seated tumors, combination therapies |
| Focused Ultrasound (HIFU) | Ultrasound waves | Several centimeters | High via real-time monitoring | Non-invasive ablation, targeted therapy |
| Laser Interstitial Therapy | Laser light | Limited (mm-cm) | High via fiber optic placement | Precise intracranial lesions, minimal access surgery |
| Radiofrequency Ablation | Radiofrequency current | Moderate (cm) | Moderate via impedance monitoring | Liver tumors, cardiac arrhythmias |
| Whole-Body Hyperthermia | External heating devices | Systemic | Challenging | Metastatic disease, immunomodulation |
| Photothermal Therapy | Light with nanoparticles | Shallow (mm) | Moderate | Superficial tumors, combination approaches |
Thermal Ablation: Mechanisms and Applications
Direct Thermal Destruction Mechanisms
Thermal ablation operates through direct energy delivery to achieve rapid and substantial tissue destruction. The primary mechanism involves protein denaturation that occurs when tissues are heated above 44°C, leading to immediate cellular necrosis and coagulation [10]. As temperatures increase further, more aggressive effects manifest, including carbonization at approximately 150°C-200°C and vaporization above 200°C, resulting in direct tissue removal [12]. The therapeutic objective of ablation is complete destruction of targeted tissue volumes while preserving surrounding healthy structures.
The clinical application of thermal ablation requires precise temperature monitoring to ensure efficacy while minimizing collateral damage. Fiber Bragg gratings (FBGs) have emerged as optimal sensing solutions for thermal monitoring during radiofrequency, laser, and microwave ablation procedures [12]. These sensors provide critical temperature feedback to control the ablation process, enabling investigation of different treatment parameters and quantification of factors such as proximity to blood vessels, perfusion effects, and tissue-specific responses [12].
Hybrid and Non-Thermal Ablation Modalities
The ablation landscape includes innovative approaches that combine thermal and non-thermal mechanisms. Irreversible electroporation (IRE) represents a particularly significant hybrid modality that primarily induces cell death through the formation of nanoscale defects in cellular membranes when exposed to brief, high-voltage electric pulses [13]. While the fundamental IRE mechanism occurs independently of thermally-induced processes, the application of therapeutic electric pulses inevitably results in secondary Joule heating of the tissue [13].
The distinction between IRE as a biophysical cellular response and IRE as a therapeutic ablation technique is crucial. When applied appropriately, it is possible to exploit the non-thermal cell death mechanism to destroy targeted tissue volumes without inducing clinically relevant thermal damage [13]. However, aggressive energy regimes in clinical pulse protocols can generate significant thermal effects that must be carefully managed through protocol design, utilization strategies, and specialized pulse delivery devices [13]. This nuanced understanding enables clinicians to maintain IRE as the predominant tissue death modality while minimizing therapy-limiting thermal damage to critical structures.
Experimental Methodologies and Research Protocols
In Vitro Hyperthermia and Ablation Assessment
Standardized experimental protocols are essential for evaluating thermal therapy efficacy and mechanisms. For magnetic hyperthermia assessment, researchers typically prepare cell cultures in standard media and suspend iron oxide nanoparticles (10-50 nm diameter) at concentrations ranging from 0.1-2 mg/mL [11]. Cells are incubated with nanoparticles for 4-24 hours to ensure cellular uptake, followed by exposure to an alternating magnetic field (100-400 kHz, 10-30 kA/m) for 30-60 minutes. During exposure, temperature monitoring via fiber optic sensors maintains the target hyperthermia range (41°C-45°C), and viability is assessed 24-48 hours post-treatment using MTT and apoptosis assays [11].
For laser ablation studies, the experimental workflow involves calibrating laser systems (typically diode or Nd:YAG lasers) to deliver specific fluences (20-100 J/cm²) at appropriate wavelengths for the target chromophore [9]. Tissue phantoms or cell cultures are positioned at standardized distances, and temperature monitoring using infrared cameras or embedded thermocouples records spatial and temporal thermal profiles. Researchers document specific treatment endpoints, including immediate color changes, swelling patterns, and the absence of adverse reactions such as blistering or cavitation, which represent danger signs [9]. Post-treatment analysis includes histological examination for coagulation necrosis dimensions and zone of apoptotic transition.
In Vivo Translation and Thermal Monitoring
Translational research protocols for thermal therapies require sophisticated monitoring and control systems. In preclinical models, researchers implant tumor xenografts subcutaneously in immunocompromised mice or utilize syngeneic models in immunocompetent animals [10]. For hyperthermia studies, animals receive localized heating via focused ultrasound or systemic warming in controlled environmental chambers, maintaining core temperatures of 39.5°C±0.5°C for 60 minutes [10]. Temperature verification occurs via rectal probes, and immune profiling follows at multiple timepoints through flow cytometry of blood, spleen, and tumor tissues.
Advanced thermal monitoring represents a critical component of ablation research. Multiplexed fiber Bragg grating (FBG) arrays provide distributed temperature sensing with high spatial resolution during radiofrequency, laser, and microwave ablation procedures [12]. These systems enable real-time thermal feedback for controlled energy delivery, allowing investigators to correlate thermal dose with resultant tissue effects and quantify the impact of physiological factors such as perfusion and proximity to vascular structures [12].
Research Reagents and Technical Solutions
Table 3: Essential Research Reagents for Thermal Therapy Investigations
| Reagent/Category | Specific Examples | Research Function | Technical Considerations |
|---|---|---|---|
| Magnetic Nanoparticles | Iron oxide NPs (Fe₃O₄), Doped ferrites | Heat generation under alternating magnetic fields | Size (10-50 nm), coating (PEG, silica), functionalization (targeting ligands) |
| Photosensitizers | Copper sulfide NPs, Carbon dots, Organic dyes | Light absorption and thermal energy conversion | Extinction coefficient, photostability, biocompatibility |
| Temperature Sensors | Fiber Bragg gratings (FBGs), Infrared cameras | Real-time thermal monitoring during ablation | Spatial resolution, response time, multiplexing capability |
| Cell Viability Assays | MTT, Calcein-AM/propidium iodide, ATP assays | Quantification of treatment efficacy post-hyperthermia | Timing (24-72 hours), compatibility with nanoparticles |
| Immunological Reagents | Cytokine ELISA kits, Flow cytometry antibodies | Evaluation of immune modulation following hyperthermia | Panel design for innate/adaptive immune cells |
| Animal Models | Subcutaneous xenografts, Genetically engineered models | In vivo evaluation of thermal therapies | Tumor volume monitoring, thermal application challenges |
Visualization of Thermal Therapy Mechanisms
Thermal interaction mechanisms span a sophisticated continuum from physiological modulation in hyperthermia to direct destruction in ablation therapies. The fundamental understanding of laser-tissue interactions and selective photothermolysis provides the theoretical foundation for these interventions [9]. Current research gaps include insufficient studies on thermal therapies in diverse skin types, with most device safety data initially established on lighter skin tones before limited translation to darker skin [9]. Future directions should focus on optimizing combination approaches, such as magnetic hyperthermia with chemodynamic therapy [11] or hyperthermia with immunotherapy [10], while advancing thermal monitoring technologies to enhance precision and personalized treatment application across diverse patient populations.
Selective photothermolysis is a foundational concept in modern laser medicine that enables the precise targeting of specific structures within biological tissues. First articulated by Anderson and Parrish in 1983, this principle revolutionized dermatologic laser therapies by providing a scientific framework for selective thermal damage of microscopic targets with spatial precision previously unattainable [14] [15]. The core innovation lies in the selective absorption of pulsed radiation by specific chromophores, generating confined thermal damage to intended targets while preserving surrounding tissue. This paradigm forms the basis for numerous medical applications including vascular lesion treatment, hair removal, pigmented lesion correction, and various aesthetic procedures [14] [16]. Understanding selective photothermolysis is essential for researchers and clinicians working at the intersection of photobiology and therapeutic applications, as it provides the theoretical underpinnings for optimizing laser parameters to achieve predictable clinical outcomes across diverse tissue types.
Theoretical Foundations of Selective Photothermolysis
The Anderson-Parrish Principle
The theoretical framework of selective photothermolysis, as established by Anderson and Parrish, relies on three carefully optimized laser parameters that must be matched to the thermal and optical properties of the target tissue [14]. The mechanism operates through selective absorption of light by naturally occurring or artificially introduced chromophores, with subsequent conversion of light energy to thermal energy, resulting in localized thermal damage. The specificity of this interaction is governed by the relationship between laser pulse duration and the thermal relaxation time (TRT) of the target—the time required for the target to cool to half its peak temperature after energy absorption [14] [17]. When pulse duration is shorter than or equal to the TRT, thermal energy remains confined to the target structure, enabling precise photothermolysis. This principle has been extended to account for non-uniform absorption within targets, where heat diffusion from highly absorbing to weakly absorbing regions can achieve complete target destruction—a concept particularly relevant for hair follicle damage where melanin distribution is non-uniform [15].
Chromophores in Biological Tissues
The efficacy of selective photothermolysis depends fundamentally on the presence and concentration of light-absorbing molecules known as chromophores. The primary endogenous chromophores in human skin each exhibit distinct absorption spectra, determining their responsiveness to specific laser wavelengths [14] [16]:
- Melanin: Found in hair follicles, epidermis, and pigmented lesions, melanin demonstrates broad absorption across the ultraviolet to near-infrared spectrum (300-1200 nm), making it the primary target for hair removal and pigmented lesion treatment [15].
- Hemoglobin/Oxyhemoglobin: Present in blood vessels and vascular lesions, these chromophores exhibit strong absorption peaks in the 418, 542, and 577 nm ranges, enabling effective treatment of vascular conditions such as telangiectasias, port-wine stains, and hemangiomas [14] [16].
- Water: As a universal tissue component, water absorption increases significantly at wavelengths above 1100 nm, peaking at approximately 3000 nm, which facilitates ablative procedures using CO₂ (10,600 nm) and Er:YAG (2940 nm) lasers [14].
The presence of competing chromophores in the treatment area presents a significant consideration, particularly in darker skin types where epidermal melanin can absorb energy intended for deeper targets, increasing complication risks [16].
Table 1: Primary Endogenous Chromophores and Their Laser Applications
| Chromophore | Absorption Peaks | Primary Applications | Representative Lasers |
|---|---|---|---|
| Melanin | 300-1200 nm (broad) | Hair removal, pigmented lesions | Ruby (694 nm), Alexandrite (755 nm), Diode (810 nm), Nd:YAG (1064 nm) [15] |
| Hemoglobin/Oxyhemoglobin | 418, 542, 577 nm | Vascular lesions, vascular anomalies | Pulsed dye laser (585-595 nm), KTP (532 nm) [14] [16] |
| Water | >1100 nm (peak ~3000 nm) | Skin resurfacing, ablation | CO₂ (10,600 nm), Er:YAG (2940 nm) [14] |
Critical Laser Parameters
The Three Key Parameters
Successful selective photothermolysis requires precise optimization of three interdependent laser parameters, each playing a distinct role in achieving selective target damage [14]:
Wavelength: The laser wavelength must correspond to the absorption peak of the target chromophore while considering competing absorbers and depth of the target. Longer wavelengths generally penetrate deeper into tissue but may have lower absorption by the target chromophore. The optimal wavelength balances sufficient absorption by the target with adequate penetration depth and minimal competition from other chromophores [14] [16].
Pulse Duration: This critical parameter must be equal to or shorter than the thermal relaxation time (TRT) of the target to confine thermal damage. TRT is proportional to the square of the target size, meaning larger targets require longer pulse durations. For example, a small blood vessel (0.1 mm diameter) has a TRT of approximately 1-10 ms, while a hair follicle (0.3 mm diameter) has a TRT of approximately 10-100 ms [14] [15].
Fluence: The energy delivered per unit area (J/cm²) must be sufficient to raise the target temperature to a threshold that causes irreversible damage (typically above 60-70°C for protein denaturation) while avoiding excessive energy that could cause nonspecific tissue injury or insufficient energy that fails to destroy the target [14] [16].
Table 2: Laser Parameters for Common Clinical Applications
| Application | Target Chromophore | Typical Wavelength | Pulse Duration | Fluence Range |
|---|---|---|---|---|
| Hair Removal | Melanin (hair follicle) | 755 nm (Alexandrite), 810 nm (Diode), 1064 nm (Nd:YAG) [15] | 5-100 ms (adjusted to hair follicle size) [15] | 10-40 J/cm² [16] |
| Facial Telangiectasia | Hemoglobin | 532 nm (KTP), 585-595 nm (PDL) [14] | 1-50 ms (adjusted to vessel diameter) [14] | 6-10 J/cm² (varies by device) |
| Pigmented Lesions | Melanin | 532 nm (Q-switched), 755 nm (Alexandrite) [14] | 10-100 nanoseconds (Q-switched) [14] | 2-8 J/cm² (varies by device) |
| Skin Resurfacing | Water | 10,600 nm (CO₂), 2940 nm (Er:YAG) [14] | 0.1-1 ms (ablative) | Varies significantly |
Thermal Relaxation Time and Tissue Effects
The thermal relaxation time (TRT) represents a fundamental concept in selective photothermolysis, defining the time required for a heated target to dissipate approximately 63% of its thermal energy to the surrounding tissue through conduction [17]. This parameter is mathematically related to the square of the target size, making larger targets require significantly longer cooling times. The relationship between pulse duration and TRT directly determines the spatial confinement of thermal damage—when pulse duration exceeds TRT, heat diffusion causes collateral injury to surrounding tissues [14] [17].
Laser-induced thermal effects follow a predictable temperature-dependent progression, with distinct biological responses occurring at specific temperature thresholds [17]:
- 40-50°C: Hyperthermia range characterized by reversible molecular bond disruption, enzyme activity reduction, and membrane alterations.
- 60-80°C: Protein denaturation, collagen coagulation, and irreversible cell necrosis occur—the primary target range for most selective photothermolysis procedures.
- 100°C: Water vaporization with bubble formation and thermal decomposition of tissue fragments.
- >100°C: Carbonization with release of carbon atoms and tissue blackening.
- >300°C: Tissue melting with complete architectural destruction.
Table 3: Temperature-Dependent Tissue Effects in Laser-Tissue Interactions
| Temperature Range | Biological Effect | Clinical Significance | Reversibility |
|---|---|---|---|
| 40-50°C | Hyperthermia: enzyme activity reduction, cell membrane alteration | Target for hyperthermia-based therapies | Reversible |
| 60-80°C | Protein denaturation, coagulation, necrosis | Primary target for most photothermolysis procedures | Irreversible |
| 100°C | Vaporization, thermal decomposition (ablation) | Tissue ablation, skin resurfacing | Irreversible |
| >100°C | Carbonization | Generally undesirable side effect | Irreversible |
| >300°C | Melting | Generally undesirable side effect | Irreversible |
Experimental Methodology and Research Protocols
Standardized Experimental Framework
Research in selective photothermolysis requires meticulous experimental design to isolate and evaluate individual parameters. A standardized protocol for investigating laser-tissue interactions should incorporate the following methodological considerations:
Target Selection and Characterization: Prior to laser exposure, targets (e.g., hair follicles, blood vessels, artificial chromophores) must be precisely characterized regarding size, depth, chromophore concentration, and surrounding tissue properties. Histological analysis, spectrophotometry, and high-resolution imaging provide essential baseline data [14] [15].
Parameter Optimization Matrix: Systematic investigation should employ a factorial design varying wavelength, pulse duration, and fluence across predetermined ranges. Each parameter combination requires sufficient replicates to establish statistical significance, with appropriate controls for tissue variability [14] [17].
Thermal Monitoring: Real-time temperature monitoring during laser exposure is essential using infrared thermography, thermocouples, or fluorescent thermal probes. This enables correlation of laser parameters with actual tissue temperature profiles and verification of theoretical models [17].
Outcome Assessment: Post-treatment evaluation should include immediate assessment (erythema, edema), short-term effects (coagulation, necrosis), and long-term outcomes (tissue regeneration, scarring). Histological analysis with standard staining (H&E, Masson's trichrome) provides microscopic evidence of selective damage [15].
Research Reagent Solutions and Essential Materials
Table 4: Essential Research Materials for Selective Photothermolysis Investigations
| Reagent/Material | Function/Application | Research Utility |
|---|---|---|
| Ex Vivo Tissue Models | Simulating human skin response | Provides controlled environment for parameter optimization without patient risk [17] |
| Artificial Chromophores | Standardized light absorbers | Enables controlled studies of absorption parameters without biological variability [14] |
| Thermographic Cameras | Non-contact temperature mapping | Quantifies spatial and temporal temperature distribution during laser exposure [17] |
| Histology Stains (H&E, Trichrome) | Tissue structure visualization | Demonstrates microscopic selective damage and collateral tissue effects [15] |
| Optical Phantoms | Simulating tissue optical properties | Provides standardized medium for light distribution studies [17] |
| Cell Viability Assays | Assessing cellular response to thermal injury | Quantifies threshold for irreversible cellular damage [17] |
Research Workflow and Decision Framework
The following diagram illustrates the systematic decision process for designing selective photothermolysis experiments and applications:
This workflow emphasizes the iterative nature of parameter optimization in selective photothermolysis research, where histological feedback informs subsequent parameter adjustments to achieve maximal selectivity.
Advanced Considerations and Research Directions
Extended Theory and Computational Modeling
The extended theory of selective photothermolysis addresses scenarios where chromophore distribution within targets is non-uniform, as occurs in hair follicles where melanin is concentrated in specific regions rather than distributed evenly [15]. In such cases, weakly absorbing areas may be destroyed through heat diffusion from highly absorbing regions, requiring adjustments to standard parameters. Computational modeling using Monte Carlo simulations for light transport and finite element analysis for heat distribution provides powerful tools for predicting these complex interactions [18] [17]. The Arrhenius formalism enables quantification of thermal damage kinetics through the relationship: Ω(𝑡) = 𝐴∫exp(−𝐸/𝑅𝑇(𝑡'))𝑑𝑡', where A is the frequency factor, E is the activation energy, R is the universal gas constant, and T(t') is temperature history [17]. This mathematical approach allows researchers to predict cell viability following laser exposure and optimize protocols for specific tissue effects.
Emerging Applications and Technological Innovations
Recent advances in selective photothermolysis research have expanded beyond traditional dermatologic applications. In ophthalmology, IPL technology has been adapted for managing meibomian gland dysfunction in dry eye disease [16]. Novel approaches combining selective photothermolysis with photodynamic therapy enhance precision in oncologic applications. Fractional laser technology represents another evolution of the principle, creating microscopic treatment zones of thermal injury surrounded by unaffected tissue to accelerate healing [18]. Research continues into new chromophore targets, including exogenous absorbers such as gold nanoparticles and indocyanine green for deeper tissue applications. The integration of real-time thermal imaging with closed-loop parameter adjustment systems represents the next frontier in smart laser therapies that automatically adapt to individual tissue responses [17].
Within the fundamental research of laser-tissue interactions, understanding the thermal effects on biological tissues is paramount. The specific tissue effect is predominantly a function of the peak temperature achieved and the duration of exposure. This guide provides a detailed examination of the three primary temperature-dependent effects: coagulation, vaporization, and carbonization, which are critical for applications ranging from surgical oncology to drug delivery system development.
The following table summarizes the key parameters and characteristics associated with each thermal effect.
Table 1: Temperature-Dependent Tissue Effects and Parameters
| Thermal Effect | Temperature Range (°C) | Primary Mechanism | Macroscopic Appearance | Key Biomolecular Alterations |
|---|---|---|---|---|
| Coagulation | 60 - 90 | Protein Denaturation & Enzyme Inactivation | Opaque, blanched white | Hemoglobin precipitation, collagen hyalinization, loss of enzymatic activity. |
| Vaporization | ≥ 100 | Liquid-to-Gas Phase Transition of Cellular Water | Tissue ablation, plume generation | Cellular architecture destroyed; immediate volumetric removal. |
| Carbonization | ≥ 150 - 200 | Dehydration & Pyrolysis of Organic Matrices | Blackened, charred eschar | Molecular breakdown into elemental carbon and volatile gases. |
Detailed Mechanisms and Experimental Analysis
Coagulation
Coagulation is a non-ablative process resulting from the denaturation of proteins and nucleic acids. The structural integrity of cells is compromised without immediate tissue removal.
- Experimental Protocol for In Vitro Coagulation Threshold Analysis:
- Sample Preparation: Prepare thin sections (e.g., 1 mm) of ex vivo liver or muscle tissue and place them in a temperature-controlled saline bath.
- Thermal Exposure: Using a heated probe or low-power laser (e.g., Nd:YAG at 1064 nm), expose tissue samples to a fixed temperature (e.g., 50, 60, 70, 80, 90°C) for a standardized duration (e.g., 10 seconds).
- Histological Analysis: Fix samples in formalin, embed in paraffin, section, and stain with Hematoxylin and Eosin (H&E). Analyze under a microscope for signs of coagulation: loss of cellular detail, eosinophilic (pink) cytoplasm, and pyknotic nuclei.
- Viability Staining: Alternatively, use a fluorescent live/dead assay (e.g., Calcein-AM/Ethidium homodimer-1) on cell cultures exposed to the same thermal conditions. Quantify the percentage of non-viable (coagulated) cells via flow cytometry or fluorescence microscopy.
Vaporization
Vaporization is an ablative process where tissue is removed through the rapid conversion of intracellular and extracellular water into steam. This process requires the latent heat of vaporization and results in precise cutting or ablation.
- Experimental Protocol for Vaporization Efficiency Measurement:
- Setup: Use a high-power, strongly absorbed laser (e.g., CO₂ laser at 10.6 µm or Er:YAG at 2.94 µm) directed at a tissue phantom (e.g., hydrated gelatin) or ex vivo tissue.
- Ablation: Fire the laser in a pulsed mode with controlled energy fluence (J/cm²) and pulse duration.
- Measurement: Measure the volume of the resulting ablation crater using optical coherence tomography (OCT) or confocal microscopy. Alternatively, weigh the sample before and after ablation to determine mass loss.
- Data Analysis: Plot the ablation depth or mass loss against the applied energy fluence. The slope of the linear region represents the ablation efficiency (µm/J or mg/J).
Carbonization
Carbonization occurs at extreme temperatures under conditions of limited oxygen, leading to the pyrolysis of proteins and carbohydrates into elemental carbon and smoke.
- Experimental Protocol for Carbonization Onset Determination:
- Setup: Employ a continuous-wave laser (e.g., diode laser) with a small spot size focused on a dry tissue sample (e.g., desiccated skin or pure collagen sheet) to minimize vaporization.
- Exposure: Apply increasing power densities until visible blackening is observed.
- Spectroscopic Analysis: Use a Raman spectrometer to analyze the treated spot. The appearance of characteristic G and D bands (~1580 cm⁻¹ and ~1350 cm⁻¹) confirms the formation of disordered carbon structures, signifying carbonization.
- Thermal Imaging: Simultaneously, use an infrared thermal camera to correlate the visible onset of carbonization with the surface temperature of the tissue.
Visualizing Thermal Effect Pathways and Workflows
Thermal Effects Pathway
Thermal Effect Experiment Workflow
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials for Thermal Effect Studies
| Item | Function / Application |
|---|---|
| Ex Vivo Tissue Models (Porcine/ bovine liver, skin) | Standardized, reproducible substrate for initial laser-tissue interaction studies and protocol development. |
| 3D Cell Culture Spheroids | More physiologically relevant in vitro model for studying thermal effects on tumor microenvironments. |
| H&E Staining Kit | Standard histological stain for visualizing general tissue architecture and coagulative necrosis post-exposure. |
| Calcein-AM / EthD-1 Viability/Cytotoxicity Kit | Fluorescent assay for quantitatively distinguishing live (green) from dead/coagulated (red) cells. |
| Formalin Solution (10% Neutral Buffered) | Tissue fixative for preserving tissue morphology after thermal treatment for histological analysis. |
| Hydrated Gelatin Phantoms | Tissue-simulating material with tunable optical properties for controlled ablation (vaporization) studies. |
| Raman Spectrometer System | For non-destructive, label-free chemical analysis to definitively identify carbonization via characteristic spectral bands. |
| Infrared Thermal Camera | To measure surface temperature in real-time during thermal exposure, correlating visual effects with temperature. |
The interaction of laser light with biological tissues and synthetic agents generates two primary mechanical phenomena: photoacoustic effects and vapor bubble dynamics. These interconnected processes form a critical foundation for advanced biomedical applications, including therapeutic drug delivery, precise tissue ablation, and cutting-edge medical imaging techniques. The photoacoustic effect describes the conversion of absorbed light energy into acoustic waves through rapid thermoelastic expansion [19]. When short-pulsed laser light illuminates an absorbing material, the absorbed energy causes localized heating and subsequent thermoelastic expansion, generating broadband acoustic waves that can be detected using conventional ultrasound transducers [20]. This light-in-sound-out principle enables photoacoustic imaging (PAI) to combine the rich contrast of optical absorption with the deep penetration and high resolution of ultrasound imaging [19].
Vapor bubble dynamics encompasses the formation, expansion, and collapse of gaseous cavities within liquids, driven by laser energy deposition. These dynamics occur when laser intensity exceeds specific thresholds, causing rapid phase transitions in the absorbing medium or in specialized phase-change contrast agents [21] [22]. The resulting bubbles undergo complex evolution governed by inertial forces, surface tension, and surrounding pressure fields, generating powerful mechanical effects including shockwaves and high-velocity micro-jets that can be harnessed for therapeutic purposes [23] [24]. Understanding the fundamental physics governing these mechanical interactions is essential for optimizing their application in biomedical research and clinical practice.
Laser-Tissue Interaction Mechanisms
Laser light interacts with biological tissues through several primary mechanisms, with the specific outcome determined by laser parameters (wavelength, pulse duration, fluence) and tissue properties (absorption, scattering). The four fundamental light-tissue interactions are transmission, reflection, scattering, and absorption [25]. For mechanical bioeffects, absorption is the most critical interaction, as it initiates the energy conversion processes that generate both photoacoustic signals and vapor bubbles.
Photothermal interactions occur when laser energy is converted to heat, raising tissue temperature. The biological response depends on the magnitude and duration of temperature increase: enzymatic deactivation occurs at 40–45°C, protein denaturation at 60°C, and vaporization at 100°C [25]. When laser energy is delivered in pulses shorter than the thermal relaxation time of the target tissue, selective photothermolysis can be achieved, allowing precise targeting of specific chromophores with minimal collateral damage [25].
Photoacoustic interactions represent a specialized form of photothermal interaction where confined, rapid heating generates acoustic waves rather than bulk thermal damage. This occurs when short laser pulses (typically nanoseconds) are absorbed, creating rapid thermoelastic expansion that produces detectable ultrasound waves [20]. The initial pressure (P) of the generated photoacoustic wave is governed by the equation: P = Γ·T · σ · μa · F, where Γ is the Grüneisen parameter (dimensionless), σ is the heat conversion efficiency, μa is the optical absorption coefficient, and F is the optical fluence [20].
Cavitation interactions involve the formation of vapor bubbles when laser energy is absorbed by water or other volatile components, causing rapid vaporization. For infrared lasers such as Ho:YAG (λ = 2.08 μm) and Er:YAG (λ = 2.94 μm) that are strongly absorbed by water, this occurs through direct absorption by the tissue water content [23]. The resulting bubbles undergo complex expansion and collapse cycles, generating substantial mechanical forces that can be harnessed for tissue ablation or disrupted to minimize collateral damage [23].
Quantitative Parameters and Threshold Data
The mechanical effects of laser-tissue interactions are governed by precise physical parameters that determine the efficacy and safety of biomedical applications. The tables below summarize key quantitative relationships and threshold values essential for experimental design.
Table 1: Key Parameters in Photoacoustic Effect and Bubble Dynamics
| Parameter | Symbol | Description | Typical Range/Value |
|---|---|---|---|
| Grüneisen Parameter | Γ | Dimensionless parameter describing thermoelastic conversion efficiency | Tissue-dependent (0.1-0.5) |
| Optical Absorption Coefficient | μₐ | Measure of how strongly a medium absorbs light at specific wavelength | Varies by tissue and wavelength (0.1-1000 cm⁻¹) |
| Optical Fluence | F | Optical energy delivered per unit area | Limited by MPE (Maximum Permissible Exposure) |
| Heat Conversion Efficiency | σ | Fraction of absorbed energy converted to heat | σ = 1 - φ (where φ is fluorescence quantum yield) |
| Normalized Distance | γ | Ratio of distance from bubble center to boundary over maximum bubble radius (h/Rmax) | γ < 2 for material removal; optimal at 0.1-0.7 [23] |
| Micro-jet Velocity | vⱼₑₜ | Velocity of collapsing bubble micro-jet | 40-150 m/s (dependent on γ) [23] |
| Hydrodynamic Impact Pressure | Pᵢₘₚₐcₜ | Pressure generated by micro-jet impingement | 5-210 MPa [23] |
Table 2: Laser and Material Properties for Bubble Dynamics
| Factor | Impact on Bubble Dynamics | Experimental Notes |
|---|---|---|
| Laser Pulse Duration | Short pulses (<1 μs) produce regular circular bubbles; long pulses (>100 μs) create elongated, irregular bubbles [24] | Pulse duration determines bubble shape and oscillation characteristics |
| Normalized Distance (γ) | Determines bubble collapse symmetry and micro-jet direction; γ = h/Rmax where h is distance to boundary and Rmax is maximum bubble radius [23] | Optimal tissue ablation observed at γ ≤ 0.7; micro-jet velocity and impact pressure strongly γ-dependent |
| Surface Roughness | Critical in distant-field cleaning effects; textured surfaces enable localized cavitation and enhance bacterial disruption [26] | Smooth surfaces suppress fluid dynamics in constrained geometries |
| Perfluorocarbon Boiling Point | Lower boiling point PFCs (C₃F₈: -36.7°C; C₄F₁₀: -1.96°C; C₅F₁₂: 29.24°C) enable vaporization at lower laser fluence [22] | PFC selection allows tuning of optical droplet vaporization threshold |
Experimental Methodologies and Protocols
High-Speed Imaging of Cavitation Bubble Dynamics
The experimental setup for investigating laser-induced cavitation bubbles typically includes a pulsed laser system, a high-speed imaging camera, and a transparent containment vessel. For Ho:YAG laser ablation studies (λ = 2.08 μm, pulse width = 300 μs, pulse energy = 2 J), bone specimens are affixed in a quartz tank filled with liquid medium, and the optical fiber is positioned perpendicular to the tissue surface with a specific stand-off distance [23]. The high-speed camera (e.g., Photron SA6) captures bubble dynamics at frame rates up to 75 kHz with exposure times as short as 13 μs, synchronized with laser firing [24]. Temporal analysis focuses on identifying key stages: initial bubble formation (Frame A), growth stage (Frames B-D), collapse initiation (Frame E), micro-jet development (Frames F-G), and final implosion (Frame H) [23]. Quantitative measurements include bubble radius versus time, micro-jet velocity, and collapse timing, with particular attention to the normalized distance γ = h/Rmax, which significantly influences bubble behavior and tissue effects [23].
Optical Droplet Vaporization Threshold Measurements
The protocol for determining optical droplet vaporization (ODV) thresholds utilizes gold nanoparticle-templated perfluorocarbon (PFC) droplets with varying core materials [22]. Microbubbles are fabricated using lipid shells (DAPC, DSPE-PEG2K, DSPE-PEG2K-B) and different PFC gas cores (C₃F₈, C₄F₁₀, C₅F₁₂) through sonication or amalgamation methods, followed by condensation into droplets through cooling and pressurization (~50 psi) [22]. The droplet suspension is placed in an optical cuvette and exposed to pulsed laser light at varying fluence levels (typically in the near-infrared range). Vaporization is detected visually by the appearance of bubbles or acoustically using a hydrophone. The threshold fluence is recorded as the minimum laser energy required to consistently vaporize droplets, with studies demonstrating that lower boiling point PFCs (C₃F₈ < C₄F₁₀ < C₅F₁₂) require lower vaporization fluences [22]. Size distribution analysis via dynamic light scattering confirms droplet stability and monodispersity before experimentation.
Photoacoustic Signal Characterization
Photoacoustic signal generation and detection protocols involve preparing tissue-mimicking phantoms with embedded optical absorbers or contrast agents [20] [19]. The experimental setup includes a tunable pulsed laser system (typically Nd:YAG with OPO or titanium-sapphire), ultrasound transducers with appropriate center frequencies (1-50 MHz depending on resolution requirements), and data acquisition hardware. For quantitative PA measurements, the locally available fluence (F) must be calibrated using a power meter, and the absorption coefficient (μₐ) of the target chromophore should be verified spectrophotometrically. The generated PA signals are averaged multiple times to improve signal-to-noise ratio, and spectral unmixing techniques are applied when multiple contrast agents are present [20]. Critical parameters to record include laser wavelength, pulse duration, pulse repetition rate, transducer characteristics, and sample temperature.
Figure 1: Photoacoustic Signal Generation Workflow
Advanced Dynamics and Specialized Phenomena
Non-Spherical Bubble Collapse and Micro-Jet Formation
When cavitation bubbles form near boundaries (tissue surfaces, surgical tools), they collapse asymmetrically, generating high-velocity micro-jets directed toward the adjacent surface. This non-spherical collapse occurs when the normalized distance γ = h/Rmax is less than approximately 2, with the most significant effects observed at γ ≤ 0.7 [23]. High-speed imaging studies reveal that micro-jet velocity increases as γ decreases, reaching values of 40-150 m/s depending on the specific geometry and laser parameters [23]. The resulting hydrodynamic impact pressure can reach 210 MPa, substantially exceeding the yield strength of most biological tissues and enabling mechanical tissue removal [23]. This phenomenon explains the enhanced ablation efficiency observed in liquid-assisted laser surgery, where the confined liquid layer facilitates mechanical tissue removal through micro-jet impingement and toroidal vortex run-off effects [23].
Cascaded Cavitation with Pulse Trains
A novel regime of laser cavitation emerges when using trains of microsecond laser pulses with inter-pulse periods shorter than the bubble lifetime. In this cascaded cavitation, subsequent laser pulses in the train pass through the gas phase of the initial bubble and evaporate additional liquid at the gas-liquid interface [24]. This produces elongated, complex-shaped bubbles with significantly larger volumes (4.6 mm length for 7-pulse train versus 3.8 mm for single pulse in experimental conditions) [24]. The practical implication is enhanced energy deposition and potentially more efficient tissue ablation or fragmentation, particularly relevant for lithotripsy and other surgical applications where extended bubble dimensions could improve therapeutic outcomes.
Optical Droplet Vaporization for Contrast Enhancement
Liquid perfluorocarbon droplets incorporating optical absorbers can be vaporized through photothermal heating using pulsed lasers, a process termed optical droplet vaporization (ODV) [22]. These phase-change agents serve as dual-mode contrast agents, providing initial photoacoustic contrast through their absorbing components and generating enhanced ultrasound contrast after vaporization into gas-filled microbubbles [22] [27]. The ODV threshold depends critically on the PFC core material, with lower boiling point PFCs (C₃F₈ < C₄F₁₀ < C₅F₁₂) vaporizing at lower laser fluences [22]. This tunability enables the design of droplet populations with specific activation thresholds, potentially allowing for spatially selective activation in complex biological environments.
Figure 2: Cascaded Cavitation with Laser Pulse Trains
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Experimental Materials
| Reagent/Material | Function/Application | Technical Specifications |
|---|---|---|
| Perfluorocarbon Droplets | Phase-change contrast agents for ODV; can be vaporized by laser or ultrasound [21] [22] | Core options: C₃F₈ (bp -36.7°C), C₄F₁₀ (bp -1.96°C), C₅F₁₂ (bp 29.24°C); size: submicron to several microns [22] |
| Gold Nanoparticles | Light absorbers for enhancing ODV efficiency; can be incorporated in droplet shells or attached to surfaces [22] | Typical sizes: 5-50 nm; surface functionalization with avidin-biotin chemistry for specific binding [22] |
| Lipid Shell Components | Stabilizing shells for microbubbles and droplets; provide biocompatibility and functionalization sites [22] | Common lipids: DAPC, DSPE-PEG2K, DSPE-PEG2K-B; molar ratios typically 90:9:1 [22] |
| Copper Sulfate Solution | Tissue-simulating phantom material with controlled absorption properties [24] | μₐ ≈ 10.7 cm⁻¹ at 1000 nm; mimics liver (4 cm⁻¹) and brain (5 cm⁻¹) absorption [24] |
| High-Speed Camera Systems | Visualization of bubble dynamics with microsecond temporal resolution [23] [24] | Frame rates: 75 kHz; exposure time: 13 μs; resolution: 1024×1024 pixels [24] |
| PVDF Hydrophones | Acoustic detection of shock waves and bubble oscillations [24] | Bandwidth: 100 kHz-100 MHz; sensitivity: 0.48 μV/Pa [24] |
Applications in Biomedical Research and Therapeutics
The controlled application of photoacoustic effects and vapor bubble dynamics enables numerous advanced biomedical applications with both diagnostic and therapeutic functions. In photoacoustic imaging, exogenous contrast agents including methylene blue, indocyanine green, and gold nanoparticles provide enhanced contrast for visualizing optically transparent structures like lymphatic vessels and tumors [20]. The combination of optical absorption contrast with ultrasound detection depth enables functional imaging of physiological parameters including blood oxygen saturation, total hemoglobin concentration, and biomarker distribution [19].
In therapeutic applications, laser-induced cavitation bubbles facilitate precise mechanical tissue ablation with minimal thermal damage. The hydrodynamic effects of bubble collapse—particularly micro-jet impingement—enable efficient hard tissue ablation in orthopedic and dental procedures when properly calibrated for normalized distance (γ) [23]. In soft tissues, the mechanical effects of bubble dynamics can enhance drug delivery by increasing cell membrane permeability or disrupting vascular barriers [21] [24].
Phase-change droplet agents provide unique capabilities for both imaging and therapy. These droplets can be activated in specific locations through optical or acoustic triggering, generating microbubbles that provide enhanced ultrasound contrast or therapeutic effects through localized mechanical action [22] [27]. This activation can be spatially and temporally controlled, enabling targeted interventions with reduced systemic effects. Recent applications have expanded to include tissue regeneration, where precisely controlled cavitation dynamics may stimulate beneficial biological responses [21].
Mechanical interactions involving photoacoustic effects and vapor bubble dynamics represent a sophisticated domain of laser-tissue interactions with broad applicability in biomedical research and clinical practice. The fundamental physics governing these phenomena—including the photoacoustic wave generation equation, bubble dynamics equations, and phase transition thermodynamics—provide a theoretical foundation for designing targeted interventions. Experimental methodologies employing high-speed imaging, acoustic detection, and specialized contrast agents enable detailed investigation of these complex processes. As research continues to advance understanding of these mechanical interactions, particularly through the development of tunable phase-change agents and optimized laser parameters, applications in precise tissue ablation, controlled drug delivery, and multimodal imaging will continue to expand, offering new opportunities for scientific discovery and clinical innovation.
Advanced Computational Modeling and Clinical Translation of Laser Therapies
The study of laser-tissue interactions is a cornerstone of modern biophotonics and therapeutic medical device development. Accurate predictive models are essential for optimizing treatment efficacy and ensuring patient safety, as they provide insights into complex, coupled physical phenomena that are difficult to measure experimentally. At the heart of these models lie two critical computational frameworks: bioheat equations, which govern the transfer of thermal energy within biological systems, and thermal fluid-structure interaction (Thermal-FSI) models, which describe the coupled mechanical and fluid-dynamic response of tissue to thermal loads [28] [29]. These frameworks enable researchers and drug development professionals to simulate and understand the fundamental processes occurring during laser-based therapies, such as the temperature-driven ablation of dermatological lesions or the thermal coagulation of blood vessels. The evolution from classical analytical models to sophisticated, multiphysics numerical simulations represents a significant advancement in the field, allowing for patient-specific treatment planning and the development of novel laser applications [30].
This technical guide provides an in-depth examination of these core frameworks. It details the underlying principles, mathematical formulations, and implementation methodologies that are vital for constructing robust computational models of laser-tissue interactions. By integrating these frameworks, researchers can move beyond simplistic temperature predictions to a more holistic view that includes stress development, tissue deformation, and phase changes, thereby capturing the true multiphysics nature of the interaction.
Bioheat Transfer Models: From Classical to Advanced Formulations
Bioheat transfer models simulate how thermal energy propagates and is distributed within living tissues. This is crucial for predicting the extent of thermal damage during laser procedures.
The Foundation: Pennes Bioheat Equation
Introduced in 1948, the Pennes bioheat equation remains the most widely used model for simulating heat transfer in biological tissue [30]. It formulates the energy balance by accounting for key physiological heat sources and sinks. Its general form is expressed as:
[ \rho c \frac{\partial T}{\partial t} = k \Delta T + \rhob cb \omegab (Tb - T) + E ]
where (E = Qr + Qm) represents the combined external laser heating ((Qr)) and metabolic heat generation ((Qm)) [30]. The model's robustness stems from its incorporation of several phenomenological mechanisms:
- Thermal conduction ((k \Delta T)): Heat diffusion through the tissue.
- Blood perfusion ((\rhob cb \omegab (Tb - T))): Heat exchange between flowing blood and the surrounding tissue.
- Metabolic heat generation ((Q_m)): Heat produced by cellular metabolism.
- Spatial heating ((Q_r)): Energy deposited by an external source, such as a laser.
Despite its widespread use, the classical Pennes model is derived from Fourier's law, which assumes infinite speed of heat propagation, a limitation that becomes significant in applications involving very short laser pulses or extremely localized heating [30].
Advanced Non-Fourier Formulations
To address the limitations of the classical model, advanced formulations incorporate a thermal relaxation time ((\tau_q)), which represents the finite time required for a heat flux to establish following a temperature gradient. This leads to a more physically realistic model of heat transfer, especially under rapid heating conditions [31] [30].
The Cattaneo-Vernotte model modifies the classical Fourier law, resulting in a hyperbolic partial differential equation that supports thermal wave propagation at a finite speed [30]. This non-Fourier framework is critical for modeling laser-tissue interactions with high spatial and temporal precision.
Further refinements include the fractional-order bioheat model, which captures memory-dependent and non-local heat transport phenomena. Experimental validations using ex-vivo tissue samples (e.g., kidney, heart, liver) have demonstrated that fractional models predict temperature trajectories with lower mean absolute error (MAE) and root-mean-square error (RMSE) compared to classical models [31]. Another advanced approach integrates the telegraph equation into the bioheat model, providing a robust framework for simulating localized point heating of diseased tissue, effectively represented using Dirac delta functions [30].
Table 1: Comparison of Key Bioheat Transfer Models
| Model | Governing Principle | Key Parameter | Advantages | Limitations |
|---|---|---|---|---|
| Classical Pennes [30] | Fourier's Law | Blood Perfusion Rate ((\omega_b)) | Simple, computationally efficient | Infinite heat propagation speed |
| Cattaneo-Vernotte (Non-Fourier) [30] | Hyperbolic Heat Wave | Thermal Relaxation Time ((\tau_q)) | Finite heat speed, accurate for short pulses | More complex numerical implementation |
| Fractional-Order [31] | Fractional Calculus | Fractional Order ((\alpha)) | Captures memory effects, high accuracy | Computationally intensive, parameter sensitivity |
| Telegraph Equation [30] | Damped Wave Equation | Relaxation Time Parameter | Models wave-like and diffusive behavior | Complex analytical solutions |
Thermal Fluid-Structure Interaction (Thermal-FSI) Models
While bioheat models predict temperature fields, Thermal-FSI models describe the complex, coupled thermomechanical response of tissue, including deformation, fluid expansion, and stress generation. This is vital for predicting mechanical outcomes like scarring or tissue rupture.
Core Components of a Thermal-FSI Framework
A comprehensive Thermal-FSI framework for laser-tissue interaction integrates several physical domains [28]:
- Optical Energy Deposition: Laser light transport in tissue is typically modeled using the diffusion approximation of the radiative transport equation, accounting for scattering and absorption.
- Bioheat Transfer: The deposited energy serves as a source term in a bioheat equation (e.g., Pennes or a non-Fourier variant) to calculate the transient temperature field.
- Phase Change and Fluid Dynamics: The model accounts for fluid expansion and water vaporization within the tissue, leading to pressure buildup.
- Nonlinear Tissue Mechanics: The temperature and pressure fields act as loads on the tissue structure, which is modeled using hyperelastic material laws to predict deformation and stress.
The Arbitrary Lagrangian-Eulerian (ALE) Formulation
A critical numerical technique for implementing Thermal-FSI is the Arbitrary Lagrangian-Eulerian (ALE) formulation [28]. This method combines the strengths of Lagrangian and Eulerian descriptions, making it ideally suited for problems involving large deformations and moving boundaries, such as those induced by laser ablation. The ALE framework allows for the independent movement of the computational mesh, enabling accurate tracking of the deforming tissue structure (a Lagrangian strength) while efficiently handling fluid flow and phase changes (an Eulerian strength). This capability is indispensable for simulating the coupled thermal, mechanical, and fluidic effects during laser therapy [28].
Constitutive Modeling of Tissue
Biological tissues exhibit nonlinear, hyperelastic mechanical behavior. Early FSI models often assumed isotropic, linear elasticity, but more accurate approaches require advanced constitutive models. For skin and other soft tissues, the Ogden and Yeoh models for hyperelasticity are frequently employed [28]. These models can capture the large-strain, stress-strain responses of compressible rubber-like solids, providing a more realistic representation of tissue deformation under thermal stress than linear models.
Experimental Protocols and Methodologies
Validating computational models requires rigorous experimental protocols. The following methodologies are commonly employed in the field.
Protocol 1: Validating Fractional-Order Bioheat Models
This protocol outlines the steps for experimentally validating a fractional-order bioheat model against ex-vivo data [31].
- Tissue Sample Preparation: Obtain 30 ex-vivo tissue samples (e.g., liver, kidney, heart). Maintain samples at room temperature (20–25 °C).
- Thermophysical Property Measurement: Characterize each sample by measuring its thermal diffusivity (D), conductivity (k), and volumetric specific heat capacity (Ch). Reported values are approximately (\rho \approx 1050\ kg/m^3), (D \approx 0.15\ mm^2/s), and (k \approx 0.5\ W/m\°C) [31].
- Controlled Laser Heating: Perform controlled surface laser heating on the samples (e.g., liver) while using infrared thermography to record the spatiotemporal temperature evolution.
- Computational Simulation: Simulate the identical experimental setup using both the classical ((\alpha = 1)) and fractional ((0 < \alpha < 1)) bioheat models.
- Model Agreement Assessment: Quantify the agreement between measured and simulated temperature data using:
- Mean Absolute Error (MAE)
- Root-Mean-Square Error (RMSE)
- Residual analysis
- Bland-Altman plots
- Sensitivity Analysis: Perform a sensitivity analysis to determine how the fractional order (\alpha) controls the pace of thermal penetration and the extent of predicted thermal zones.
Protocol 2: Coupled Thermal-FSI Analysis of Laser Treatment
This protocol details the setup for a coupled multiphysics simulation to optimize laser treatment for dermatological lesions like neurofibromatosis type 1 [28] [32].
- Problem Definition: Model a three-dimensional geometry of neurofibromatosis-affected skin.
- Laser Parameters: Define a 975 nm diode laser in continuous mode, selected for its optimal penetration within the "therapeutic window" of biological tissue [28].
- Multiphysics Model Setup:
- Optical Module: Implement the diffusion approximation to the radiative transport equation to model laser energy deposition.
- Thermal Module: Solve the transient bioheat equation to obtain the temperature field over a typical exposure time (e.g., 3 seconds).
- FSI Module: Couple the thermal solution to a hyperelastic mechanical model (Ogden/Yeoh) within an ALE formulation to simulate fluid expansion, vaporization, and tissue deformation.
- Simulation and Output: Run the coupled simulation to compute time-dependent fields of temperature, vapor fraction, pressure, and stress.
- Safety Threshold Analysis: Analyze results to ensure intra-tissue pressure remains below critical thresholds (e.g., 817 kPa) to minimize scarring risks, thereby optimizing laser parameters for therapeutic efficacy and safety [28] [32].
Successful implementation of these computational frameworks relies on a suite of software tools and theoretical resources.
Table 2: Research Reagent Solutions for Computational Modeling
| Tool / Resource | Type | Primary Function | Application Example |
|---|---|---|---|
| COMSOL Multiphysics [30] | Commercial Software | Finite Element Analysis for coupled physics | Numerical validation of analytical bioheat models; coupled Thermal-FSI simulation. |
| MATHEMATICA [30] | Commercial Software | Symbolic and Numerical Computing | Deriving closed-form analytical solutions for the Pennes bioheat equation. |
| Arbitrary Lagrangian-Eulerian (ALE) [28] | Numerical Formulation | Handling large deformations and fluid-structure interaction | Core component of a Thermal-FSI framework for tracking deforming skin tissue. |
| Ogden & Yeoh Models [28] | Constitutive Model | Describing nonlinear, hyperelastic material behavior | Representing the large-strain mechanical response of skin tissue in a mechanical simulation. |
| Dirac Delta Function [30] | Mathematical Function | Representing a localized point source of heat | Modeling the highly focused heating of diseased tissue by a laser beam in an analytical solution. |
| Telegraph Equation [30] | Hyperbolic PDE | Modeling damped wave propagation | Incorporating non-Fourier heat conduction effects with finite thermal wave speed in bioheat transfer. |
Computational frameworks based on bioheat equations and Thermal-FSI models are indispensable for advancing the fundamentals of laser-tissue interaction research. The journey from the classical Pennes equation to advanced non-Fourier and fractional-order models has significantly improved the predictive accuracy of temperature distributions. When these thermal models are coupled with sophisticated Thermal-FSI techniques using the ALE formulation and hyperelastic material laws, researchers gain a powerful, multiphysics toolset. This integrated approach enables the virtual optimization of laser parameters—such as wavelength, power, and exposure time—to maximize therapeutic outcomes while maintaining strict safety thresholds for temperature, pressure, and stress. For researchers and drug development professionals, mastering these frameworks is key to innovating next-generation laser therapies, reducing reliance on costly and time-consuming empirical trials, and ultimately improving patient care.
Medical laser systems represent a cornerstone of modern therapeutic and diagnostic interventions, with their efficacy fundamentally governed by the precise selection of wavelength and operational modes. These parameters directly dictate the nature of laser-tissue interactions, determining outcomes in procedures ranging from surgical ablation to photobiomodulation. Within the broader context of laser-tissue interactions research, understanding these core principles is essential for developing standardized protocols, ensuring reproducible results, and advancing clinical applications. This technical guide provides an in-depth analysis of these critical parameters, framing them within the experimental and practical needs of the scientific community. The objective is to establish a foundational framework that supports rigorous research methodology and accelerates innovation in medical laser applications.
Fundamental Laser Parameters and Tissue Interactions
The interaction between laser light and biological tissue is a complex process determined by a set of interdependent physical parameters. The wavelength of the laser light is the primary factor influencing the penetration depth and the type of chromophore targeted (e.g., hemoglobin, melanin, or water) [33]. Shorter wavelengths (approximately 200–600 nm) are absorbed superficially, while longer wavelengths in the red and near-infrared spectrum (650–1200 nm) penetrate deeper into tissue [33].
The operational mode of a laser—whether continuous wave (CW) or pulsed—determines the temporal profile of energy delivery. Continuous wave lasers provide a constant power output, while pulsed lasers emit light in short bursts, allowing for higher peak powers and reduced thermal diffusion, a principle critical to selective photothermolysis [33]. The interplay between pulse width and the thermal relaxation time (TRT) of the target tissue is crucial for confining thermal damage [33].
Power density (or irradiance, measured in W/cm²) and energy density (or fluence, measured in J/cm²) are derived metrics that define the intensity and total energy delivered per unit area, respectively [33]. These, along with the spot size of the beam, are fundamental to calculating the precise dose administered to the target tissue. As shown in Figure 1, these parameters form a logical hierarchy for system configuration.
Figure 1. Logical Workflow for Configuring Medical Laser Parameters. This diagram outlines the decision-making sequence for selecting core laser parameters to achieve a defined biological effect, culminating in experimental validation.
Wavelength Selection: Mechanisms and Applications
Wavelength selection is not arbitrary; it is guided by the optical properties of the target tissue and the desired therapeutic outcome. The absorption characteristics of specific chromophores vary significantly across the optical spectrum.
Table 1: Chromophore Absorption Peaks and Corresponding Medical Laser Applications
| Chromophore | Peak Absorption Wavelength(s) | Primary Medical Applications | Laser Type Examples |
|---|---|---|---|
| Water | >1200 nm (e.g., 1450 nm, 1940 nm, 10,600 nm) [33] | Ablative skin resurfacing, dental procedures [33] | Er:YAG (2940 nm), CO₂ (10,600 nm) |
| Hemoglobin | ~540 nm (green), ~575 nm (yellow), ~800-1100 nm (near-IR) [33] | Treatment of vascular lesions (e.g., port-wine stains, telangiectasias) [34] | Pulsed dye laser (585-595 nm), KTP (532 nm) |
| Melanin | Broad absorption from UV to near-IR, peak in UV-visible range [33] | Hair removal, treatment of pigmented lesions [34] | Alexandrite (755 nm), Ruby (694 nm) |
| Cytochrome c oxidase | ~600-900 nm (Red/NIR) [35] | Low-Level Laser Therapy (LLLT) for wound healing, pain reduction, anti-inflammation [33] [35] | GaAlAs (810 nm), He-Ne (632.8 nm) |
The selection process involves a trade-off between absorption and scattering. While shorter wavelengths may be strongly absorbed by a target chromophore, longer wavelengths generally experience less scattering in tissue, enabling deeper penetration. This is why LLLT for deep-seated conditions typically utilizes wavelengths between 600 nm and 1100 nm [33]. Furthermore, technological advancements like spatiotemporal mode-locking (STML) in multimode fibers are now enabling more powerful and controlled lasers that can maintain stability across multiple modes, enhancing power output and enabling advanced beam shaping for applications in precision fabrication and nonlinear microscopy [36].
Operational Modes: Continuous Wave vs. Pulsed Lasers
The choice between continuous wave and pulsed operation is dictated by the desired tissue effect—specifically, whether the goal is a photochemical, thermal, or mechanical interaction.
- Continuous Wave (CW) Mode: A CW laser emits a steady, constant beam of light. It is typically used in applications where a sustained thermal effect is desired, such as tissue coagulation, vaporization, or non-thermal photobiomodulation in LLLT [33]. The primary controlled parameter is exposure time.
- Pulsed Mode: Pulsed lasers emit high-energy light in short bursts (from milliseconds to femtoseconds). This mode is critical for confining thermal damage to a specific target. The principle of selective photothermolysis dictates that for precise thermal confinement, the pulse width should be equal to or shorter than the thermal relaxation time (TRT) of the target structure [33]. This prevents heat from diffusing to and damaging surrounding tissues. Pulsed modes are essential for tattoo removal, lithotripsy, and precise surgical ablation [34].
Table 2: Comparison of Laser Operational Modes and Their Characteristics
| Parameter | Continuous Wave (CW) Mode | Pulsed Mode |
|---|---|---|
| Beam Characteristic | Constant, steady output | Short, high-energy bursts |
| Primary Thermal Effect | Sustained, diffuse heating | Rapid, confined heating |
| Key Principle | Power density (W/cm²) over time | Selective photothermolysis |
| Peak Power | Relatively low | Can be orders of magnitude higher than average power |
| Typical Applications | Coagulation, LLLT, some types of skin resurfacing | Tattoo removal, pigment treatment, lithotripsy, precise cutting |
The pulse width parameter is closely related to the thermal relaxation time (TRT). For optimal results, the pulse width is often recommended to approximate half of the TRT [33]. Figure 2 illustrates the relationship between key parameters—power density, spot size, and pulse width—and their collective impact on the resulting tissue effect.
Figure 2. Relationship Between Laser Parameters and Tissue Effects. The interplay of power density, spot size, and pulse width collectively determines the dominant mechanism of laser-tissue interaction.
Experimental Protocols for Laser Parameter Analysis
Robust experimental methodology is essential for validating laser parameters and their biological effects. The following protocols provide a framework for critical analyses in laser-tissue interactions research.
Protocol: Measuring Protective Material Transmittance
This protocol is crucial for ensuring accurate dosimetry when materials are used to protect laser equipment from contamination, as their attenuation can significantly alter the delivered dose [35].
- Sample Preparation: Obtain samples of materials commonly used to wrap laser emitters, such as Polyvinyl chloride (PVC) films, condoms, plastic bags, latex surgical gloves, and kinesiology tape [35].
- Instrumentation: Use a spectrophotometer (e.g., Varian Cary 50) capable of scanning the relevant spectrum (e.g., 190 nm to 1100 nm). Allow the instrument to warm up for at least 30 minutes prior to measurement [35].
- Measurement Procedure: Place a single layer of each test material in the optical path within the spectrophotometer's dark chamber. This setup mimics clinical wrapping conditions.
- Data Collection: Perform transmittance (τ) measurements at fine intervals (e.g., 1 nm). Transmittance is defined as τ = I / I₀, where I is the transmitted intensity and I₀ is the incident intensity [35].
- Data Analysis: Calculate the optical density (Dλ) for each wavelength using the formula Dλ = -log₁₀(τλ). This parameter is critical for quantifying attenuation and is used in international safety standards [35].
- Application: Identify the material with the lowest optical density at the specific laser wavelength intended for use to ensure minimal interference with the prescribed dose.
Protocol: Modeling Laser-Tissue Interactions
Computational modeling provides a non-invasive method to predict laser effects and plan experiments.
- Software Selection: Utilize multiphysics simulation software such as COMSOL Multiphysics (v6.2 or newer) [33].
- Define Geometry and Properties: Create a model representing the tissue structure. Input optical properties (absorption coefficient μa, scattering coefficient μs, anisotropy factor g, refractive index n) derived from the scientific literature. For soft tissue, typical values are μa ≈ 0.1–10 cm⁻¹, μs ≈ 10–100 cm⁻¹, g ≈ 0.8–0.9, and n ≈ 1.37–1.40 [33].
- Set Laser Parameters: Configure the model with the laser parameters under investigation, including wavelength, power density, spot size, and pulse duration.
- Simulate and Analyze: Run the simulation to model light propagation (e.g., using a Monte Carlo or diffusion approximation model) and subsequent thermal effects (using the bioheat equation). The output can predict metrics such as photon deposition depth and subsurface temperature gradients [33].
- Validation: Corroborate model predictions with experimental data, such as high-speed video and thermal imaging of laser interactions with tissue phantoms or ex vivo samples [37].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimentation in medical laser research requires carefully selected materials and equipment. The following table details key items for a standard research toolkit.
Table 3: Essential Research Materials for Laser-Tissue Interaction Studies
| Item | Function/Application | Technical Notes |
|---|---|---|
| Polyvinyl Chloride (PVC) Film | Protective barrier for laser emitters to prevent contamination during procedures on open wounds [35]. | Exhibits the highest transmittance (>90% for some brands at 660-808 nm) among common polymeric materials, minimizing dose attenuation [35]. |
| Laser Protective Eyewear | Essential personal protective equipment (PPE) for operators and patients to prevent ocular damage from stray reflections [38] [35]. | Optical density (OD) must be specified for the specific laser wavelength in use. Standards (ANSI Z136.7) provide testing and labeling guidelines [38]. |
| Tissue Phantoms | Simulate the optical (μa, μs) and thermal properties of human tissue for controlled, reproducible ex vivo testing [33] [37]. | Can be fabricated from materials like Intralipid, India ink, and agar to mimic specific tissue types for protocol development and validation. |
| High-Speed & Thermal Cameras | Visualize and quantify the dynamic laser-tissue interaction, including rapid mechanical events (e.g., bubble formation) and spatial temperature profiles [37]. | Critical for validating computational models and understanding the mechanisms of action of pulsed laser treatments. |
| Spectrophotometer | Characterize the optical properties (transmittance, reflectance) of both biological samples and protective materials [35]. | Used to measure the precise transmittance of protective films and calculate their optical density per Equation 2 [35]. |
| Multimode Fiber Lasers | Enable research into high-power, spatiotemporal mode-locked (STML) lasers for advanced applications [36]. | Allow control of individual transverse modes (e.g., LP01, LP11) to enhance power output and enable complex beam shaping (e.g., quasi-flat-top beams) [36]. |
The strategic selection of wavelength and operational modes forms the bedrock of effective and predictable medical laser applications. As research continues to unravel the complexities of laser-tissue interactions, the adoption of standardized reporting guidelines for these parameters—as called for by recent studies—is paramount for ensuring reproducibility and scientific rigor [33]. Future advancements will be driven by a synergistic combination of sophisticated computational modeling, rigorous experimental validation, and innovative laser technologies like STML. By adhering to a disciplined framework for parameter selection and reporting, researchers and clinicians can continue to expand the frontiers of laser medicine, enabling more precise, safe, and effective therapeutic outcomes.
Laser-tissue interactions represent a cornerstone of modern medical science, enabling precise, minimally invasive interventions across diverse clinical specialties. The fundamental physics of laser light—including its monochromaticity, coherence, and collimation—allows for selective targeting of specific chromophores within biological tissues [25]. The therapeutic outcome of laser applications is governed by the interplay between laser parameters (wavelength, pulse duration, fluence, and spot size) and tissue optical properties (absorption, scattering, and thermal relaxation) [39] [25]. This whitepaper provides a comprehensive technical examination of how these core principles translate into specialized applications within dermatology, ophthalmology, and orthopedics, contextualized within contemporary research frameworks. Understanding these tissue-specific paradigms is essential for researchers and drug development professionals advancing therapeutic laser technologies.
Fundamental Laser-Tissue Interaction Mechanisms
Laser energy interacts with biological tissues through several primary mechanisms, each dominating under specific parameter combinations and yielding distinct biological effects.
- Photochemical Interactions: Involve the absorption of light by endogenous or exogenous chromophores, leading to chemical reactions. The primary clinical application is photodynamic therapy (PDT), where photosensitizing drugs activated by specific laser wavelengths generate cytotoxic singlet oxygen [39].
- Photothermal Interactions: The most prevalent mechanism in medical lasers, where photon absorption converts light energy to heat, inducing localized thermal effects. Tissue response depends critically on the achieved temperature and rate of heating [25]:
- 40°C-45°C: Enzyme deactivation occurs.
- >60°C: Protein denaturation, coagulation, and necrosis.
- >100°C: Vaporization of tissue water and subsequent ablation.
- Photoablation: Primarily mediated by mid-infrared lasers (e.g., Er:YAG at 2940 nm) that are strongly absorbed by tissue water, leading to direct molecular bond breaking and precise tissue removal with minimal thermal damage to surrounding structures [25] [40].
- Plasma-Induced Ablation and Photodisruption: Occur with extremely high-intensity pulsed lasers (e.g., Nd:YAG), where optical breakdown generates ionized plasma, leading to mechanical disruption of tissue via shock waves and cavitation bubbles [39].
Table 1: Fundamental Laser-Tissue Interaction Mechanisms
| Interaction Mechanism | Primary Laser Parameters | Biological Effects | Key Applications |
|---|---|---|---|
| Photochemical | Low power, continuous wave | Chemical activation of photosensitizers | Photodynamic therapy |
| Photothermal | Pulsed or continuous, moderate fluence | Heating, coagulation, vaporization | Vascular lesions, hair removal, coagulation |
| Photoablation | Mid-infrared wavelengths, pulsed | Precise tissue removal | Skin resurfacing, bone cutting |
| Plasma-Induced/Photodisruption | Ultra-short pulses, high intensity | Mechanical disruption | Lithotripsy, posterior capsulotomy |
Diagram 1: Fundamental laser-tissue interaction mechanisms and their biological effects.
The principle of selective photothermolysis, introduced by Anderson and Parrish in 1983, remains fundamental to understanding targeted laser therapies [25]. This theory states that by selecting a laser wavelength well-absorbed by the target chromophore and a pulse duration shorter than or equal to the target's thermal relaxation time, thermal damage can be confined precisely to the target structure. This principle underlies most modern laser applications across medical specialties.
Dermatology Applications
Dermatology leverages the diverse interactions between laser light and skin chromophores—primarily melanin, hemoglobin, and water—to treat a wide array of conditions from vascular lesions to cosmetic concerns.
Fractional Laser Skin Resurfacing
Fractional photothermolysis represents a significant advancement in laser dermatology, creating microscopic treatment zones (MTZs) of thermal injury while sparing surrounding tissue to accelerate healing [41]. Recent research on the 1927 nm fractional thulium fiber laser (FTL) demonstrates its intermediate position in the ablation spectrum due to its water absorption coefficient.
Table 2: 1927 nm Fractional Thulium Laser-Tissue Interactions by Pulse Energy
| Pulse Energy | MTZ Diameter (μm) | Ablation Depth (μm) | Observed Tissue Effects |
|---|---|---|---|
| 3 mJ | 213 (C1 tip) | 93 | Subepidermal clefts or epidermal disruption under intact stratum corneum |
| 15 mJ | N/A | N/A | Expanded thermal effects laterally and vertically |
| 20 mJ | 357 (C1 tip) | 101 | Frank ablation extending to superficial dermis |
Experimental Protocol: Fractional Thulium Laser Analysis
Objective: To characterize the range of laser-tissue interactions produced by 1927 nm fractional thulium fiber laser at different pulse energies in in vivo human skin [41].
Materials and Methods:
- Laser Device: 1927 nm fractional thulium fiber laser (LaseMD, Lutronic) with two laser tips (C1: 200 μm spot size, 100 spots/cm²; C5: 350 μm spot size, 225 spots/cm²).
- Laser Parameters: Single pass at 0, 3, 15, or 20 mJ pulse energy at fixed 20-watt power.
- Imaging Modalities:
- Line-field confocal OCT (LC-OCT): DeepLive instrument (DAMAE Medical) with 1.0 μm resolution for cross-sectional and en-face imaging.
- Optical coherence tomography (OCT): VivosightDX system (Michelson Diagnostics) with <7.5 μm lateral resolution, 6×6 mm field-of-view.
- Evaluation Metrics: Qualitative MTZ morphology description, semiquantitative measurement of MTZ diameter and ablation depth using proprietary software (18 distinct MTZs analyzed per condition).
- Statistical Analysis: Descriptive statistics with means and ranges for MTZ dimensions.
Key Findings: The 1927 nm FL produced a spectrum of effects from nonablative to ablative depending on pulse energy. Lower energies (3 mJ) created limited epidermal effects, while higher energies (15-20 mJ) resulted in wider MTZs and deeper ablation extending to the superficial dermis [41].
Vascular and Pigmented Lesion Treatment
The selective targeting of hemoglobin and melanin using appropriate laser parameters enables effective treatment of vascular and pigmented lesions while minimizing collateral damage [25]. Key considerations include:
- Vascular lesions: Pulsed dye lasers (585-595 nm) target oxyhemoglobin with pulse durations matched to blood vessel thermal relaxation times.
- Pigmented lesions: Q-switched lasers (ns pulse durations) generate photomechanical effects that disrupt melanosomes.
- Surface cooling: Precooling, parallel cooling, or postcooling techniques protect the epidermis and improve selectivity for deeper targets [25].
Ophthalmology Applications
Ophthalmic laser applications demand exceptional precision in targeting ocular tissues while preserving delicate surrounding structures, particularly in retinal therapies where laser energy must pass through transparent media to reach pigmented structures.
Computational Modeling in Retinal Laser Therapy
Accurate computational models of laser-eye interactions require precise optical and thermal parameters of ocular tissues. A 2025 review highlighted critical data requirements for improving model accuracy [42].
Table 3: Essential Ocular Tissue Parameters for Computational Modeling
| Tissue Parameter | Significance in Modeling | Research Gaps Identified |
|---|---|---|
| Density | Influences thermal capacity and diffusion | Limited experimental data for some ocular tissues |
| Specific Heat | Determines temperature rise from absorbed energy | Inconsistencies in literature values |
| Thermal Conductivity | Governs heat dissipation rate | Variation in measurement methodologies |
| Refractive Index | Affects light distribution within tissues | Wavelength-specific data needed |
| Absorption Coefficient | Critical for predicting energy deposition | Particularly important at 577 nm wavelength |
Experimental Protocol: Retinal Laser Therapy Modeling
Objective: To develop improved computational models for predicting outcomes of retinal laser therapy by compiling accurate optical and thermal parameters of ocular tissues [42].
Data Collection Methodology:
- Literature Review: Extensive search for peer-reviewed measurements of ocular tissue properties.
- Parameter Extraction: Focus on density, specific heat, thermal conductivity, refractive index, and absorption coefficient at 577 nm wavelength.
- Methodology Assessment: Critical evaluation of experimental techniques used in source studies.
- Reliability Analysis: Assessment of parameter consistency across studies and identification of outliers.
Key Findings: The review identified a concerning tendency in the literature to rely on pre-existing parameter values without clear justification or understanding of original measurement contexts. This practice propagates uncertainties through computational models and highlights the need for new, carefully designed experimental studies to establish definitive ocular tissue properties [42].
Laser Surgical Procedures in Ophthalmology
- LASIK Procedures: Latest techniques utilize femtosecond lasers for corneal flap creation, offering improved precision over mechanical microkeratomes [39] [43].
- Posterior Capsulotomy: Nd:YAG lasers perform non-thermal photodisruption to open opaque posterior capsules following cataract surgery [39].
- Retinal Photocoagulation: Argon (488/514 nm) and frequency-doubled Nd:YAG (532 nm) lasers create controlled thermal lesions to treat diabetic retinopathy, retinal tears, and other retinal disorders [42].
Orthopedics Applications
Laser applications in orthopedics focus primarily on bone ablation and soft tissue management, with emerging research demonstrating advantages over traditional mechanical instruments.
Laser Bone Ablation
Laser bone ablation offers significant advantages over traditional mechanical tools, including non-contact operation, reduced thermal damage, minimal pressure and vibration, and the ability to create complex geometric cuts [40].
Table 4: Comparative Analysis: Laser vs. Mechanical Bone Ablation
| Parameter | Laser Ablation | Traditional Mechanical Instruments |
|---|---|---|
| Tissue Contact | Non-contact | Direct contact required |
| Thermal Effects | Controlled, minimal necrosis | Significant heat generation causing osteonecrosis |
| Pressure/Vibration | Minimal | Significant pressure and vibration |
| Geometric Flexibility | High (complex shapes possible) | Limited by tool geometry |
| Infection Risk | Reduced (no instrument contact) | Potentially higher |
| Noise Generation | Lower | Significantly higher |
Bibliometric analysis reveals growing research interest in laser bone ablation, with the United States as the leading contributor and "ablation," "Er:YAG laser," and "bone" as the most frequent keywords [40]. Research trends indicate increasing focus on laser osteotomy, bone tumor ablation, and robot-guided applications.
Experimental Protocol: High-Intensity Laser Therapy for Post-Lumbar Surgery Syndrome
Objective: To evaluate the efficacy of high-intensity laser therapy (HILT) in patients with Post-Lumbar Surgery Syndrome (PLSS) [44].
Study Design:
- Participants: 96 patients with PLSS, divided into Group A (oral medication only) and Group B (HILT plus oral medication).
- Laser Parameters: LTS-1500 device (LITE-CURE), 1064 nm wavelength, 12 W power, continuous bio-stimulation mode, 10 J/cm² dosage, 4 treatments every other day.
- Assessment Methods:
- Clinical Outcomes: Visual Analog Scale (VAS) for pain and Oswestry Disability Index (ODI) at baseline, 1 week, 1, 3, 6, and 12 months post-treatment.
- Imaging Analysis: MRI quantification of paraspinal muscle fat infiltration (PMFI) at L4/L5 using ImageJ software pseudo-coloring technique.
- Statistical Analysis: Repeated measures ANOVA with Greenhouse-Geisser correction, generalized eta-squared (ges) effect sizes, Bonferroni correction for multiple comparisons.
Key Findings: The HILT group demonstrated significantly lower VAS scores at 3 and 6 months and lower ODI scores at 12 months compared to medication-only controls. Notably, HILT significantly reduced paraspinal muscle fat infiltration progression (2.87% increase vs. 8.26% in controls), suggesting structural preservation benefits beyond symptomatic relief [44].
Diagram 2: Orthopedic laser application workflow for post-lumbar surgery syndrome.
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Materials for Laser-Tissue Interaction Studies
| Research Tool | Function/Application | Example Use Cases |
|---|---|---|
| Line-Field Confocal OCT (LC-OCT) | High-resolution (∼1 μm) non-invasive imaging of laser-tissue interactions | Visualization of microthermal treatment zone morphology in dermatology [41] |
| Optical Coherence Tomography (OCT) | Deeper penetration (1 mm) imaging of tissue effects | Tracking spatiotemporal healing process after fractional laser exposure [41] |
| Monte Carlo Simulations | Mathematical modeling of photon transport in turbid tissues | Predicting light distribution in ocular tissues for treatment planning [39] [42] |
| Kubelka-Munk Theory | Analytical solution for light propagation in scattering media | Modeling diffuse reflectance in skin and other layered tissues [39] |
| Pseudocoloring Image Analysis | Quantification of tissue composition changes | Measuring paraspinal muscle fat infiltration in orthopedic laser studies [44] |
Tissue-specific laser applications in dermatology, ophthalmology, and orthopedics demonstrate how fundamental interaction principles translate into specialized therapeutic approaches. Dermatology leverages chromophore-selective targeting for precise treatment of skin conditions. Ophthalmology requires exquisite precision in retinal therapies supported by accurate computational models. Orthopedics utilizes the ablative and thermal properties of lasers for bone and soft tissue procedures with advantages over traditional mechanical tools. Continuing research into laser-tissue interactions, supported by advanced imaging and computational modeling, will further refine these applications and expand their clinical utility across medical specialties.
The interaction of laser light with biological tissue forms the foundational basis for photobiomodulation (PBM) and photodynamic therapy (PDT). These non-invasive therapeutic modalities leverage the principles of photophysics and photochemistry to elicit targeted biological responses. Photobiomodulation is defined as a form of light therapy that utilizes non-ionizing light sources, including lasers, light-emitting diodes (LEDs), and broad-spectrum lamps, to deliver light energy in the visible and near-infrared (NIR) spectrum (400-1400 nm) to produce physiological responses without thermal damage [45]. In contrast, photodynamic therapy is a photochemical process that requires three key components: a photosensitizing agent, light of a specific wavelength, and tissue oxygen. Upon light activation, the photosensitizer catalyzes the generation of reactive oxygen species (ROS), primarily singlet oxygen, which induces selective cytotoxicity in target cells [46]. The therapeutic efficacy of both modalities is governed by the fundamental principles of light propagation in tissue, including absorption, scattering, and penetration depth, which are in turn determined by optical properties of the tissue and the specific parameters of the light applied [47].
Fundamental Mechanisms of Action
Photobiomodulation: Mechanisms at the Cellular Level
PBM operates primarily through photophysical and photochemical events that alter cellular function. The three primary proposed mechanisms involve intracellular, membrane, and extracellular targets.
Mitochondrial Cytochrome C Oxidase (CcO) Activation
The most investigated mechanism of PBM involves the intracellular targeting of mitochondrial cytochrome c oxidase (CcO), a key enzyme in the electron transport chain capable of absorbing red and near-infrared light [45]. Absorption of photons by CcO induces transient increases in ATP production and reactive oxygen species (ROS), which initiate signaling cascades promoting cellular proliferation, survival, and repair. Evidence for CcO participation includes increased expression and activity of CcO following light exposure, as assessed by immunohistochemistry, histochemistry, and cell extract assays [45]. The absorption of light by CcO also triggers the release of nitric oxide (NO), enhancing cerebrovascular delivery of oxygen to metabolically active tissues [45]. Transcranial PBM in human studies has been shown to induce up-regulation of oxidized CcO in the brain, initiating a series of reactions linked to energy production: (1) CcO photon absorption, (2) CcO oxidation, (3) proton pumping and NO release, (4) CcO-catalyzed oxygen reduction to water, (5) ATP synthesis by oxidative phosphorylation, and (6) coupled hemoglobin oxygen transport [45].
Cell Membrane Transporter and Receptor Modulation
A second mechanism involves light-sensitive cell membrane transporters and receptors, including opsins, AHR, and transient receptor potential (TRP) channels [45]. Research indicates that laser light (640 nm) can act specifically on TRPV2 receptors, triggering an immune response in human mast cells with potential clinical implications for analgesia [45]. Photostimulation of retinal ganglion cells has also been shown to trigger membrane potentials through activation of TRPV4 receptors that open sodium and calcium channels [45]. Light absorption by these membrane proteins affects G-protein-coupled receptor (GPCR) signaling and ion flux, particularly calcium, leading to downstream changes in cellular signaling.
Extracellular Transforming Growth Factor-β1 (TGF-β1) Activation
The third mechanism involves the extracellular activation of transforming growth factor-β1 (TGF-β1), a cytokine that regulates immune responses and stem cell differentiation [45]. PBM treatment induces reactive oxygen species (ROS) in a dose-dependent manner, which in turn activates a redox-sensitive site within TGF-β1 to promote differentiation of host stem cells and support tissue regeneration, as demonstrated in dental tissue models [45].
Photodynamic Therapy: Cytotoxic Mechanisms
PDT exerts its effects through photochemical reactions that generate cytotoxic agents. The process begins when a photosensitizer (PS) molecule absorbs a photon of appropriate wavelength, transitioning from its ground state (S0) to an excited singlet state (S1), then to a triplet excited state (T1) via intersystem crossing [46]. From the T1 state, two primary photochemical reaction pathways can occur:
- Type I Reaction: The photosensitizer in the T1 state reacts directly with biomolecules such as proteins or lipids, resulting in the formation of radicals that initiate free radical chain reactions.
- Type II Reaction: Energy transfer from the T1 state photosensitizer to molecular oxygen (O₂) generates highly reactive singlet oxygen (¹O₂), which can damage membranes, proteins, and DNA, leading to cellular apoptosis or necrosis [46].
Mitochondrial membrane damage following PDT increases the Bax/Bcl-2 ratio, leading to subsequent activation of caspase-9, which cleaves and activates caspase-3 and -7, triggering poly[ADP-ribose] polymerase 1 (PARP-1) cleavage and DNA fragmentation [46]. The type II reaction pathway predominates in most current PDT applications, though both reaction types can occur simultaneously, competing with each other depending on the PS type, tissue oxygen concentration, and environmental pH [46].
Table 1: Key Characteristics of PBM and PDT
| Parameter | Photobiomodulation (PBM) | Photodynamic Therapy (PDT) |
|---|---|---|
| Primary Mechanism | Photophysical & photochemical modulation | Photochemical destruction |
| Light Parameters | Low-power (typically ≤500 mW), non-thermal | Higher power, may generate heat |
| Oxygen Dependency | Not required | Essential |
| Cellular Outcome | Enhanced proliferation, repair, reduced inflammation | Cell death via apoptosis/necrosis |
| Key Molecular Target | Cytochrome c oxidase | Various cellular components |
| Primary Applications | Tissue repair, pain control, anti-inflammatory | Oncology, antimicrobial treatments |
Key Experimental Parameters and Dosimetry
PBM Dosimetry Considerations
Effective PBM therapy requires careful optimization of multiple parameters. The wavelength determines tissue penetration and specific biological effects, with red light (600-700 nm) used for superficial tissues and NIR light (780-1100 nm) for deeper tissues [48]. The absorption of cytochrome c oxidase shows a trough in the 700-800 nm range, making this range mostly inefficient for treatment [48]. Additional critical parameters include irradiance, fluence (energy density), pulse structure, treatment interval, and coherence. Dosimetric studies are essential to identify optimal parameters that maximize therapeutic effects while minimizing risk of paradoxical responses from excessive energy [49]. A biphasic dose-response relationship is often observed, where lower doses are frequently more effective than higher ones [49].
Table 2: Optimized PBM Parameters for Specific Conditions
| Condition | Wavelength (nm) | Fluence (J/cm²) | Power Output | Treatment Protocol |
|---|---|---|---|---|
| Diabetic Neuropathy | 630-670 & 808-904 | 3-10 J/cm² | 45-100 mW | Minimum 12 sessions [50] |
| Nerve Regeneration | 904 & 650 (combination) | 9 J per session | 22 mW (laser), 10 mW (LEDs) | 14 sessions every 48 hours [51] |
| COPD (Experimental) | 660 | 1-3 J (optimal) | 100 mW | 15 consecutive days [49] |
PDT Photosensitizers and Activation Parameters
PDT efficacy depends heavily on the properties of the photosensitizer. An ideal PS should have strong absorption in the "therapeutic window" (600-800 nm), high singlet oxygen quantum yield, selective accumulation in target tissue, low dark toxicity, and rapid clearance from the body [46]. First-generation photosensitizers like Photofrin (approved by FDA in 1993) suffered from limitations including prolonged skin photosensitivity and weak absorption at therapeutic wavelengths [46]. Second-generation photosensitizers include Foscan (5,10,15,20-tetra(m-hydroxyphenyl)chlorin), activated at 652 nm; Purlytin (tin ethyl etiopurpurin), activated at 664 nm; and Lu-tex (lutetium texaphyrin), activated at 732 nm [46]. Recent research focuses on nanoscale delivery systems that offer improved solubility in physiological environments, selective tumor accumulation, prolonged photoactivity, and lower therapeutic doses [46].
Experimental Protocols and Methodologies
Protocol for PBM in Nerve Regeneration
A study investigating PBM effects on crush-type inferior alveolar nerve (IAN) injuries provides a robust experimental model [51]. The methodology can be summarized as follows:
- Animal Model: 24 Wistar Albino rats (300-350 g) divided into 4 groups: Sham/Control (n=8), P1 (n=8), and P2 (n=8).
- Nerve Injury: Right IANs exposed and crushed with micro forceps for 30 seconds.
- PBM Treatment:
- Group P1: Received PBMT with a combination of 904 nm, 22 mW GaAlAs infrared laser and 650 nm, 10 mW InGaAlP LEDs, 9 J energy for 14 sessions, once every two days.
- Group P2: Received 940 nm InGaAsP diode laser with same treatment frequency and energy.
- Sham-control: Received placebo treatment with laser probe turned off.
- Assessment: On postoperative day 28, samples from damaged nerve areas analyzed by histomorphometric methods assessing axon number, axon area, and myelin thickness.
- Results: While the control group showed the highest axon number (4438.2) and myelin sheath thickness (2.21 ± 0.30 μm), both PBM groups outperformed the sham-control group in axon number and axon area, indicating positive effects on nerve regeneration and maturation [51].
Protocol for PDT Bioenergetics Assessment
A systematic analysis of PDT effects on cellular bioenergetics utilized extracellular flux analysis to quantify impacts on oxidative phosphorylation and glycolysis [52]:
- Cell Culture: A549 lung adenocarcinoma cells maintained under standard conditions.
- Treatment Groups:
- PDT agents: Ru(II) polypyridyl complexes acting as photosensitizers.
- PACT agents: Ru(II) complexes acting as photoactivated chemotherapeutics.
- Traditional agents: Structurally related compounds with thermally labile chloride ligands.
- Bioenergetic Analysis: Seahorse extracellular flux analyzer used to assess oxidative phosphorylation and glycolysis before and after light activation.
- Key Findings: PDT agents induced a "quiescent bioenergetic response" from mitochondrial respiration shutdown. Loss of oxidative phosphorylation was followed by disrupted glycolysis after an initial compensatory increase. In contrast, PACT agents had minimal impact on cellular respiration, suggesting fundamentally different mechanisms of action [52].
Signaling Pathways and Molecular Mechanisms
The following diagrams illustrate key signaling pathways for PBM and PDT, generated using Graphviz DOT language with high color contrast for clarity.
PBM Signaling Pathways
Diagram 1: PBM Mitochondrial Signaling. This diagram illustrates the primary PBM mechanism involving photon absorption by cytochrome c oxidase (CcO), leading to increased ATP production, transient ROS increases, and nitric oxide release, ultimately activating signaling pathways that promote cellular repair and anti-inflammatory responses [45].
PDT Cytotoxic Mechanisms
Diagram 2: PDT Cytotoxic Mechanisms. This diagram shows the photochemical reactions in PDT where light-activated photosensitizers (PS) generate cytotoxic free radicals (Type I) or singlet oxygen (Type II), leading to cellular damage and apoptosis [46] [52].
The Scientist's Toolkit: Essential Research Materials
Table 3: Key Research Reagent Solutions for Phototherapy Studies
| Reagent/Equipment | Function/Application | Specific Examples |
|---|---|---|
| Light Sources | Delivery of specific wavelengths for photoactivation | Diode lasers (GaAlAs, InGaAsP), LEDs, Broad-spectrum lamps [48] |
| Photosensitizers | Light absorption and energy/electron transfer | Photofrin, Foscan, Purlytin, Lu-tex, Phthalocyanines [46] |
| Cell Lines | In vitro assessment of phototherapeutic effects | A549 lung adenocarcinoma cells [52] |
| Animal Models | In vivo evaluation of therapeutic efficacy | Rat inferior alveolar nerve crush model [51], Mouse COPD model [49] |
| Analytical Instruments | Quantification of biological responses | Seahorse extracellular flux analyzer [52], Flow cytometer, Histomorphometry tools |
Photobiomodulation and photodynamic therapy represent distinct but complementary approaches within the broader context of laser-tissue interactions research. While PBM utilizes low-intensity light to modulate cellular function and promote repair processes, PDT employs photoactivated cytotoxic reactions for selective tissue destruction. The therapeutic efficacy of both modalities depends on precise parameter optimization, including wavelength, fluence, power density, and treatment timing. Future research directions include the development of advanced photosensitizers with improved tumor selectivity and activation profiles, standardized dosimetry protocols for specific clinical applications, and integration of omics technologies with artificial intelligence to optimize treatment parameters [53]. Elucidation of the precise molecular mechanisms underlying these phototherapies will continue to enhance their translational potential across diverse medical specialties, from oncology and neurology to regenerative medicine and beyond.
Translational research, often described as the "bench-to-bedside" process, is the critical discipline of harnessing knowledge from basic scientific research to drive clinical applications, ultimately creating novel diagnostics, treatments, and preventive strategies for human disease [54]. This process forms an essential bridge between basic laboratory research and clinical practice, ensuring that scientific discoveries actually reach patients [54]. In the specific field of laser-tissue interactions research, this translates to developing laser-based medical devices, diagnostic techniques, and therapeutic protocols from fundamental principles of photobiology and photophysics into validated clinical tools. The ultimate goal is to ensure that discoveries advancing into human trials possess the highest possible chance of success in terms of both safety and efficacy, thereby decreasing the overall cost and time of developing new medical products [54].
However, the path from a preclinical finding to an approved clinical application is notoriously challenging. A significant rift, often termed the "Valley of Death," exists between basic research (bench) and clinical application (bedside) [54]. This is widely recognized in both academia and industry, characterized by high attrition rates where over 95% of drugs entering human trials fail, and the return on investment has been limited in terms of clinical impact [54]. Understanding the frameworks, challenges, and best practices for navigating this translational pathway is therefore fundamental for researchers and drug development professionals.
The Translational Research Framework
Translational research is not a linear path but a continuous, iterative process encompassing multiple, interdependent phases with frequent feedback loops [54]. The operational phases of translational research are often described as T0 through T4, providing a map for the journey from fundamental discovery to population health impact.
Diagram 1: The iterative, multi-phase nature of translational research (T0-T4) with critical feedback loops, highlighting the "Valley of Death" between bench and bedside.
As illustrated in Diagram 1, the process spans from T0 (basic research discovery) through T4 (public health impact), with the transition from T1 (preclinical research) to T2 (clinical proof-of-concept) representing the most significant hurdle - the "Valley of Death" [54]. This phase transition requires functional interactions between academia, government, industry (biotech and large pharma), and the community to be successful [54]. For laser-tissue research, this means close collaboration between laser physicists, biologists, clinical researchers, and eventually, practicing physicians to ensure that fundamental discoveries about how laser energy interacts with cellular and tissue components can be safely and effectively translated into clinical applications.
Quantitative Landscape of Translation
The challenging nature of the translational pathway is starkly illustrated by key quantitative metrics. The following table summarizes the formidable statistics and probabilities associated with drug development and translational research.
Table 1: Quantitative Metrics of the Drug Development and Translation Process
| Metric | Value | Context and Implications |
|---|---|---|
| Overall Likelihood of Approval | 0.1% [54] | For every drug that gains FDA approval, more than 1,000 are developed but fail. |
| Clinical Trial Attrition Rate | >95% [54] | The vast majority of drugs entering human trials fail to gain regulatory approval. |
| Average Time from Discovery to Approval | >13 years [54] | Represents a significant investment of time before a discovery benefits patients. |
| Average Cost to Develop a New Drug | ~$2.6 billion [54] | A 145% increase, correcting for inflation, over the estimate made in 2003. |
| Phase III Failure Rate | ~50% [54] | Nearly half of all experimental drugs fail in large-scale Phase III trials. |
| Failure Due to Lack of Efficacy/Safety | ~90% [55] | The primary causes of failure are lack of clinical effectiveness and unforeseen safety issues. |
These statistics underscore the immense challenges. The high failure rates and costs highlight the critical need for more robust preclinical models and predictive assays to better de-risk candidates before they enter the costly clinical trial phases. In laser medicine, this translates to the need for highly predictive models that can accurately forecast clinical outcomes based on preclinical laser parameter testing.
Case Studies: Lessons from Targeted Therapy Development
EGFR-Targeted Agents: Successes and Failures
The development of Epidermal Growth Factor Receptor (EGFR) targeted agents for solid malignancies provides powerful, real-world examples of both the potential and the pitfalls of translational research.
Table 2: Key Translational Lessons from EGFR-Targeted Agent Development
| Agent / Context | Preclinical Finding | Clinical Result | Translational Lesson Learned |
|---|---|---|---|
| Cetuximab/Panitumumab in Colorectal Cancer (CRC) | Efficacy shown in xenograft models; EGFR overexpression initially considered key for patient selection [56]. | Patients with EGFR-negative tumors also responded [56]. | Erroneous Biomarker: The initial biomarker (EGFR overexpression) was inaccurately applied. Retrospective analysis revealed KRAS mutation as a key resistance biomarker [56]. |
| Gefitinib/Erlotinib in Non-Small Cell Lung Cancer (NSCLC) | Initial development was not based on a predefined molecular target [56]. | Retrospective analysis of responder tumors identified activating EGFR mutations as the predictive biomarker [56]. | "Bedside-to-Bench" Feedback: Clinical observation drove the discovery of the correct biomarker, leading to a more targeted and effective clinical application [56]. |
| Erlotinib in Pancreatic Cancer | Modest tumor reduction in limited preclinical models (e.g., L3.6pl xenograft) [56]. | Phase III trial showed a statistically significant but clinically minimal overall survival increase of 0.33 months [56]. | Weak Preclinical Rationale: Underwhelming and limited preclinical data failed to predict marginal clinical benefit, highlighting the need for more robust and predictive models [56]. |
| EGFR + VEGF Inhibitor Combinations | Striking synergistic tumor growth inhibition in CRC and NSCLC models [56]. | Clinical trials showed increased toxicity and decreased progression-free survival [56]. | Model Discordance: Preclinical models overestimated efficacy, likely due to factors like tumor heterogeneity and inability to predict clinical toxicity in murine models [56]. |
Experimental Protocols: From In Vitro to In Vivo
The following detailed methodology outlines a standard protocol for evaluating a targeted therapy, such as an EGFR inhibitor, which can be adapted for testing laser-based therapeutic strategies.
Protocol 1: In Vitro Assessment of Target Inhibition and Cellular Response
- Objective: To determine the biological effects of a targeted agent (e.g., EGFR TKI) or a specific laser parameter on cancer cell lines in vitro.
- Materials:
- Cell Lines: A panel of relevant cancer cell lines (e.g., NSCLC lines with/without EGFR mutations, CRC lines with/without KRAS mutations).
- Test Agent/Laser System: Serial dilutions of the small-molecule inhibitor (e.g., Gefitinib, Erlotinib) or a calibrated laser system with tunable parameters (wavelength, power, pulse duration).
- Reagents: Cell culture media, phospho-specific antibodies for Western Blot (e.g., anti-pEGFR), cell viability assay kits (e.g., MTT, CellTiter-Glo), apoptosis assay kits (e.g., Annexin V staining).
- Methodology:
- Culture & Plate Cells: Maintain cells in standard conditions. Plate in multi-well plates for assays.
- Dose/Treatment Response: Treat cells with a range of concentrations of the inhibitor or laser parameters. Include vehicle/control treated wells.
- Proof of Mechanism (24h post-treatment): Lyse cells and perform Western Blotting to assess inhibition of the target pathway (e.g., reduction in pEGFR and downstream pERK).
- Phenotypic Response (72-96h post-treatment): Perform cell viability assays to generate dose-response curves and calculate IC50 values. Use apoptosis assays to confirm cell death mechanism.
- Data Analysis: Compare IC50 values and degree of pathway inhibition across cell lines with different genetic backgrounds (e.g., EGFR mutant vs. wild-type) to establish a preliminary predictive biomarker.
Protocol 2: In Vivo Efficacy Study in Patient-Derived Xenograft (PDX) Models
- Objective: To evaluate the efficacy and biomarker-based patient selection strategy of a targeted agent or laser therapy in a more physiologically relevant in vivo model.
- Materials:
- Animal Model: Immunocompromised mice (e.g., NSG mice) engrafted with well-characterized PDX tissues representing different molecular subtypes [56].
- Test Agent/Laser System: Formulated drug for in vivo delivery or a clinical-grade laser system with appropriate applicators.
- Equipment: Calipers for tumor measurement, in vivo imaging system (optional).
- Methodology:
- Engraftment and Randomization: Allow PDX tumors to establish. When tumors reach a predefined volume (~150-200 mm³), randomize mice into treatment and control groups (n=8-10 per group).
- Dosing/Treatment Regimen: Administer the drug at its maximum tolerated dose (or laser at therapeutic parameters) via the planned clinical route. Control groups receive vehicle or sham laser treatment.
- Efficacy Monitoring: Measure tumor volumes and animal weights 2-3 times per week. Calculate tumor growth inhibition (TGI %).
- Endpoint Analysis: At the end of the study, harvest tumors for immunohistochemical (IHC) analysis to confirm target modulation in vivo.
- Data Analysis: Correlate the degree of TGI with the molecular characteristics of each PDX model (e.g., KRAS status). A successful result shows significantly greater efficacy in models bearing the sensitive biomarker profile.
The Scientist's Toolkit: Research Reagent Solutions
Successful translational research relies on a suite of essential materials and model systems. The following table details key components of the translational scientist's toolkit, with specific considerations for laser-tissue interaction research.
Table 3: Essential Research Reagents and Models for Translational Research
| Tool / Reagent | Function in Translational Research | Specific Consideration for Laser-Tissue Research |
|---|---|---|
| Genetically Engineered Cell Lines | To study the function of specific genes (oncogenes, tumor suppressors) and their pathways in vitro. | Used to model the effect of laser energy on cells with specific genetic drivers of disease. |
| Patient-Derived Xenograft (PDX) Models | To maintain the stromal architecture and genetic heterogeneity of human tumors in vivo, improving clinical predictivity [56]. | Critical for testing laser therapies on human tumor biology in an in vivo context, assessing thermal damage, and penetration depth. |
| Phospho-Specific Antibodies | To provide "proof of mechanism" by measuring inhibition or activation of the target pathway (e.g., pEGFR, pAKT, pERK) via Western Blot or IHC [56]. | Can be used to detect laser-induced cellular stress responses or activation/inhibition of signaling pathways post-irradiation. |
| Tissue Microarrays (TMAs) | To rapidly analyze biomarker expression across hundreds of patient samples simultaneously by IHC. | Enable high-throughput analysis of laser-induced tissue effects or biomarker expression pre- and post-treatment in diverse tissue types. |
| Clinical-Grade Laser Systems | To bridge the gap between laboratory experiments and clinical application. | Systems used in preclinical studies should have direct translational paths to devices used in clinical trials, with matching wavelengths and emission modes. |
Critical Challenges and Strategies for Success
The "Valley of Death" is perpetuated by a confluence of scientific, operational, and financial obstacles. A primary scientific challenge is the limited predictive utility of traditional preclinical models [54]. While animal models are useful for understanding disease pathobiology, targets and drugs developed in animals often fail in human studies due to irreproducible data, ambiguous models, and species-specific differences [54]. Furthermore, a poor initial hypothesis that is irrelevant to human disease is a fundamental flaw that no amount of technical excellence can overcome [57].
Operationally, a lack of collaboration and communication between basic scientists and clinicians creates significant silos [57]. A successful translational research program must encourage meaningful cross-talk so that clinicians understand new laboratory findings and basic scientists understand the most pressing clinical issues [57]. Funding is another major hurdle. The translational gap is also a funding gap, where promising early discoveries lack the support to advance through the costly steps of therapeutic development [54] [57].
To overcome these challenges, researchers and institutions should adopt the following strategies:
- Focus on Human Relevance: Start with a clinically relevant question and use human tissues and data to validate targets early [57].
- Employ Predictive Models: Prioritize the use of clinically relevant models, such as PDX models, which were crucial in retrospectively validating KRAS mutation as a biomarker of resistance to EGFR therapy [56].
- Foster Deep Collaboration: Build integrated teams where "two interested and motivated parties [are] both driving a ship in the same direction" [57].
- Plan for the "Valley of Death": Seek partnerships with academia, government agencies, and industry to secure the funding and expertise required to cross the translational gap [57]. The era of the "'family farmer' researcher... is ending" [57].
- Incorporate Biomarker Strategies: From the outset, work to identify patient selection biomarkers that can define a responsive population, increasing the likelihood of clinical trial success.
The journey from bench to bedside is a complex, iterative, and challenging but essential process. By learning from past failures and successes, such as those in EGFR targeting, and by implementing robust experimental designs, predictive models, and collaborative frameworks, the scientific community can improve the efficiency of translating groundbreaking discoveries into life-saving clinical applications. For the field of laser-tissue interactions, this means rigorously applying these translational principles to ensure that innovations in laser technology reliably and safely progress to improve patient care and public health.
Optimization Strategies and Safety Protocols for Enhanced Laser Efficacy
Laser ablation has become an indispensable tool in both materials processing and surgical applications, valued for its precision, minimal invasivity, and controllability. The fundamental challenge confronting researchers and practitioners alike lies in optimizing laser parameters to maximize material or tissue removal rates while simultaneously minimizing collateral thermal damage. This technical guide examines the core principles governing this balance, framing the discussion within the broader context of laser-tissue interaction research essential for advancing therapeutic applications and drug development methodologies.
The efficacy of laser-based approaches—whether for manufacturing or medicine—stems from controlled energy deposition at the micro and nano scales. However, the thermal energy required for ablation inevitably conducts into surrounding regions, potentially creating heat-affected zones (HAZ), microcracks, charring, or necrosis in biological tissues. Understanding and controlling these effects requires a multidisciplinary approach that draws from optics, thermal dynamics, and material science. This guide synthesizes current research to provide a comprehensive framework for parameter optimization, with particular emphasis on experimental protocols and quantitative decision-making.
Theoretical Foundations of Laser-Tissue Interactions
Laser ablation involves the removal of material through irradiation with high-intensity laser pulses. The process initiates when the absorbed laser energy exceeds the threshold required for phase changes, leading to vaporization and ejection of material. The competing objectives of efficient ablation and minimal thermal damage create a complex optimization landscape where multiple parameters exhibit strong interdependencies.
The primary thermal damage mechanism in biological tissues is protein denaturation, which occurs when tissues are exposed to temperatures above 60°C for sufficient duration. The extent of damage depends not only on the peak temperature but also on the exposure time, following Arrhenius-type kinetic models. In surgical contexts, uncontrolled thermal spread can compromise healing and functional outcomes. Research on soft tissue surgery with CO₂ lasers has demonstrated that the heat-affected zone can range from 120-160μm for pulsed modes compared to 400-800μm for continuous wave operation, highlighting the critical importance of temporal parameters [58].
The absorption characteristics of the target material dictate the initial energy coupling efficiency. Biological tissues contain varying water content, and different laser wavelengths interact distinctively with these components. For instance, the strong absorption of CO₂ laser radiation (10.6μm) by water makes it particularly effective for cutting hydrated soft tissues, while lasers in the near-infrared spectrum (e.g., 980nm) penetrate more deeply and may be preferable for other therapeutic objectives [58].
Table 1: Laser Wavelength Applications in Biological Tissues
| Laser Type | Wavelength | Primary Absorber | Typical Applications |
|---|---|---|---|
| CO₂ | 10.6 μm | Water | Soft tissue incision, ablation |
| Er:YAG | 2.94 μm | Water | Precise hard and soft tissue ablation |
| Diode | 800-980 nm | Hemoglobin, pigment | Photocoagulation, hyperthermia |
| Nd:YAG | 1064 nm | Pigment-dependent | Deep coagulation, hyperthermia |
Critical Parameters in Laser Ablation
Energy Parameters
The fluence (energy per unit area) and power settings fundamentally govern the ablation process. The ablation threshold represents the minimum fluence required to initiate material removal, while excessive fluence wastes energy and increases thermal penetration. Research on efficient ablation suggests an optimal ratio of laser peak fluence to ablation threshold close to e² ≈ 7.4 for maximal material removal rate [59]. This principle holds across various materials, though the specific threshold values differ substantially between tissues and non-biological materials.
Power control directly influences the thermal profile. In soft tissue surgery, studies have identified laser power and scan speed as the parameters with the strongest influence on cut quality, with their combination being more significant than either parameter alone [58]. The line energy (power/speed) serves as a useful composite parameter for initial optimization, though the individual components still require fine-tuning.
Temporal Parameters
Pulse duration critically affects the thermal confinement and consequent damage zone. Ultrashort pulses (femtosecond to picosecond) typically produce smaller heat-affected zones than nanosecond or microsecond pulses due to reduced thermal diffusion during the energy deposition. However, nanosecond lasers often achieve higher ablation rates at the same average power due to different ablation mechanisms and present practical advantages for industrial and medical use [60].
The pulse repetition rate determines the time between successive pulses and influences heat accumulation. At high repetition rates (>10 kHz), consecutive pulses may interact with a pre-heated zone or with plasma and ejected material from previous pulses, potentially reducing ablation efficiency through shielding effects [60]. Managing these cumulative thermal effects is essential for controlling collateral damage.
Spatial and Scanning Parameters
Beam characteristics and scanning patterns significantly influence ablation efficiency and thermal profiles. The spot size determines the power density for a given pulse energy, while the scanning speed and pulse-to-pulse overlap control exposure time per area. Studies on metal ablation have shown that material removal rate increases monotonically with pulse duration up to a characteristic repetition rate where pulse energy and average power are maximal [60].
Spatial overlaps must be optimized to balance processing speed with quality. In laser engraving applications, surface roughness is mainly influenced by line-to-line and pulse-to-pulse overlaps, with larger overlaps generally leading to lower roughness but longer processing times [60]. Process optimization indicates that operating with parameters resulting in the highest material removal rate yields the best ratio between removal rate and surface roughness at approximately 50% overlap of laser pulses [60].
Angular effects become significant when processing curved surfaces. The incidence angle (β between laser beam and surface normal) and path angle (γ between scanning direction and laser beam axis) modulate power density distribution and affect processing quality. For fused silica ablation, the incidence angle reduces effective power (P' = P·cosβ), distorts the beam spot from circular to elliptical, and alters material absorptivity according to Fresnel equations [61].
Table 2: Optimization Guidelines for Key Laser Parameters
| Parameter | Efficiency Optimization | Thermal Damage Minimization | Composite Metric |
|---|---|---|---|
| Fluence | 5-10× ablation threshold | 2-3× ablation threshold | ≈7.4× threshold [59] |
| Pulse Duration | Nanosecond range | Femtosecond-picosecond range | Application-dependent |
| Repetition Rate | Maximum at f₀ characteristic | Lower to allow cooling | Material-dependent [60] |
| Spot Overlap | 30-50% | 50-70% | ~50% for best MRR/Ra ratio [60] |
| Scanning Speed | Higher speeds | Moderate speeds for control | Paired with power (line energy) |
Experimental Methodologies for Parameter Optimization
Protocol for Ablation Threshold Determination
Objective: To determine the single-pulse and multi-pulse ablation thresholds of target materials or tissues.
Materials:
- Pulsed laser system with controllable fluence
- Target samples (e.g., tissue phantoms, ex vivo tissues, or reference materials)
- Positioning system for precise sample movement
- Profilometry or microscopy for crater characterization
- Environmental chamber (if controlling atmosphere)
Procedure:
- Prepare uniform samples with appropriate surface characteristics.
- Set laser to single-pulse mode with well-characterized beam profile.
- Create a matrix of exposure sites with systematically varied fluence levels.
- Apply precisely N pulses (N=1, 10, 100, 1000) to each site.
- Characterize ablation craters using optical microscopy or profilometry.
- Measure crater diameters D and plot D² against ln(F₀).
- Extract threshold fluence Fth from the intercept using the relationship: D² = 2w₀²ln(F₀/Fth(N)) [59].
- Determine incubation factor ξ from the dependence Fth(N) = Fth(1)·N^(ξ-1).
Data Analysis: The ablation threshold decreases with increasing pulse number due to incubation effects. The determined threshold values establish the minimum fluence required for material removal and provide the reference for setting optimal processing fluence.
Protocol for Thermal Damage Assessment
Objective: To quantify thermal damage in tissues or heat-affected zones in materials under different laser parameters.
Materials:
- Laser system with controllable parameters (power, speed, pulse duration)
- Histological preparation equipment for tissue samples
- Microtome for sectioning
- Staining reagents (H&E, viability stains)
- Thermal camera system (if real-time monitoring)
- Microscopy with image analysis capability
Procedure:
- Prepare samples with consistent properties and dimensions.
- Define test matrix covering power, speed, pulse duration, and repetition rate.
- Apply laser treatment according to predefined patterns.
- For tissues: process for histology, section through treated areas, stain with H&E and viability markers.
- For materials: prepare cross-sections and etch to reveal HAZ.
- Image sections and quantify damage zones using standardized scoring systems.
- Correlate damage extent with laser parameters and thermal models.
Scoring System: For tissue studies, implement a previously validated scoring system that evaluates:
- Cut quality and smoothness
- Carbonization extent
- Coagulation zone width
- Structural integrity preservation [58]
High-Speed Imaging of Ablation Dynamics
Objective: To visualize material ejection, plasma formation, and shielding effects during laser ablation.
Materials:
- Pulsed laser system
- High-speed camera with appropriate temporal resolution (ns scale)
- Synchronization electronics
- LED illumination sources
- Processing chamber with viewing port
Procedure:
- Configure high-speed camera with appropriate magnification and framing rate.
- Synchronize laser triggering with camera acquisition.
- Set up illumination to highlight ejected material.
- Record ablation events at varied repetition rates and fluences.
- Analyze sequence of images for plasma formation dynamics and material ejection patterns.
- Correlate visual observations with measured ablation rates and thermal damage.
Applications: This methodology enables direct observation of shielding phenomena where plasma or ejected material from previous pulses interferes with subsequent pulses, particularly at high repetition rates (>10 kHz) [60]. These effects significantly impact ablation efficiency and must be considered in parameter optimization.
Modeling and Computational Approaches
Computational models provide powerful tools for predicting ablation outcomes and optimizing parameters without extensive experimental trials. Finite element models can simulate the temperature distribution and thermal damage in tissues or materials during laser irradiation.
Thermal Modeling Framework
Pennes' bioheat equation forms the foundation for modeling thermal effects in biological tissues:
$$ρcp\frac{∂T}{∂t} = ∇·(k∇T) + ωρcp(Ta - T) + Qm + Qlaser$$
Where ρ is density, cₚ is specific heat, k is thermal conductivity, ω is blood perfusion rate, Tₐ is arterial temperature, Qm is metabolic heat generation, and Qlaser is laser heat source.
For non-biological materials, the simplified heat conduction equation applies:
$$ρcp\frac{∂T}{∂t} = ∇·(k∇T) + Qlaser$$
The laser heat source term depends on the absorption coefficient and laser parameters:
$$Qlaser = μa·I(r,t)$$
Where μ_a is the absorption coefficient and I(r,t) is the spatiotemporal distribution of laser intensity.
Multi-Objective Optimization Framework
Advanced optimization approaches combine computational models with genetic algorithms to identify optimal parameter sets. For prostate cancer treatment using laser-induced hyperthermia, researchers have implemented a multi-objective genetic algorithm coupled with finite element simulations to maximize tumor necrosis while minimizing damage to healthy tissue [62].
The optimization workflow involves:
- Defining decision variables (laser power, exposure time, number of fibers, placement)
- Establishing objective functions (tumor damage to be maximized, healthy tissue damage to be minimized)
- Running iterative simulations to map the Pareto front of optimal solutions
- Selecting the best compromise solution using criteria such as the utopian criterion
This approach has demonstrated capability to achieve complete tumor necrosis with acceptable damage to healthy prostate (e.g., 188 mm³ in optimized solutions) [62].
Diagram 1: Multi-objective optimization workflow for laser parameter selection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Equipment for Laser-Tissue Interaction Studies
| Item | Function | Application Notes |
|---|---|---|
| Tissue Phantoms | Simulate optical and thermal properties of real tissues | Allow standardized testing before biological samples |
| Histological Stains (H&E, Viability) | Visualize cellular structure and viability | Quantify thermal damage extent in biological tissues |
| Thermochromic Materials | Visualize temperature distributions | Calibrate thermal models and identify hot spots |
| High-Speed Camera | Capture ablation dynamics | Reveal plasma formation and material ejection processes |
| Beam Profiling System | Characterize spatial energy distribution | Essential for accurate fluence calculation |
| Artificial Neural Networks | Model complex parameter relationships | Predict outcomes beyond linear regression capabilities [62] |
Optimizing laser parameters to balance ablation efficiency and thermal damage requires a systematic approach that integrates theoretical principles, experimental validation, and computational modeling. The key insight emerging from recent research is that no single parameter operates in isolation; rather, the optimal solution lies in carefully balanced combinations tailored to specific materials and applications.
For researchers in laser-tissue interactions, this guide provides a foundation for designing experiments and interpreting results within a coherent conceptual framework. The continued refinement of laser technologies, coupled with advanced modeling approaches, promises enhanced capabilities for precise material processing and surgical interventions with minimized collateral damage. Future advancements will likely focus on real-time feedback systems that dynamically adjust parameters based on observed tissue response, further improving the precision and safety of laser-based procedures.
In the field of laser-tissue interactions, the management of thermal energy is a cornerstone for both efficacy and safety. The fundamental difference between Continuous Wave (CW) and Pulsed Wave (PW) laser delivery lies in their temporal emission profiles, which directly dictates the thermal outcome in biological tissues. CW lasers emit a constant, unbroken beam of light, leading to sustained heating [63]. In contrast, PW lasers deliver energy in short, high-power bursts interspersed with "quench periods" or off-times, allowing for tissue cooling [64] [65]. This whitepaper provides an in-depth technical analysis of the thermal implications of both delivery modes, framed within the context of foundational laser-tissue research. It is structured to equip researchers and drug development professionals with the quantitative data and methodological knowledge necessary to design rigorous experiments and develop safer therapeutic applications.
Core Principles and Thermal Implications
The temporal structure of laser emission is the primary determinant of heat accumulation. In CW mode, the constant energy delivery results in a linear accumulation of heat within the tissue. Without periods for heat dissipation, this can lead to elevated skin surface temperatures and potential thermal damage, even at lower power densities [64] [65].
PW operation fundamentally alters this thermal dynamic. The high peak power of each pulse enables efficient ablation or photobiomodulation, while the subsequent off-time—the "quench period"—allows the targeted tissue to dissipate heat through a process known as thermal relaxation [64] [66]. This pulsed delivery spreads the total energy over a longer duration, mitigating cumulative thermal buildup at the surface and enabling deeper penetration of light while maintaining a safer superficial temperature [64]. An analogy for this effect is moving a finger rapidly through a candle flame versus holding it in the flame; the former delivers energy with minimal thermal damage due to the brief interaction time [65].
A critical concept in PW laser operation is peak power. While the average power of a pulsed laser might be low, the peak power (the power within each individual pulse) can be extraordinarily high. For example, a laser displaying 5 watts of average power in free-running pulsed mode can have a peak power of 10,000 watts per pulse [65]. This high peak power is essential for processes like hard tissue ablation, where a rapid, powerful energy burst is needed to efficiently remove material with minimal heat transfer to the surroundings [65].
Quantitative Data Comparison
The following tables synthesize key quantitative differences between CW and PW laser modalities, focusing on parameters critical for thermal management in research settings.
Table 1: Comparative Analysis of CW and Pulsed Laser Systems
| Parameter | Continuous Wave (CW) Laser | Pulsed Wave (PW) Laser |
|---|---|---|
| Power Delivery | Constant, uninterrupted beam [63] | Short, high-peak-power bursts [63] |
| Thermal Profile | Sustained heating, linear heat accumulation [65] | Intermittent heating with cooling periods (thermal relaxation) [64] [65] |
| Heat-Affected Zone (HAZ) | Larger HAZ due to prolonged exposure [66] [63] | Minimal HAZ [66] [63] |
| Peak Power | Equal to average power [65] | Can be orders of magnitude higher than average power (e.g., 10,000 W peak from 5 W average) [65] |
| Precision | Suitable for processes where precision is less critical [63] | Very high precision due to short pulse durations and minimal thermal spread [63] |
| Primary Thermal Risk | Uncontrolled temperature rise, leading to patient discomfort and potential thermal damage [64] | Minimal tissue heating when parameters are optimized; risk is lower and more controlled [64] [65] |
Table 2: Experimental Parameters and Thermal Outcomes from a Deep Tissue Simulation Study [64]
| Parameter | Continuous Wave (CW) Model | Pulsed Wave (PW) Model |
|---|---|---|
| Wavelength | 1064 nm | 1064 nm |
| Peak/Average Power | Not explicitly stated (Constant output) | 60 W (Peak Power) |
| Pulse Width / Interaction Time | Not Applicable (Continuous) | 2 ms |
| Duty Cycle | 100% | 10% |
| Beam Size | 20 mm | 20 mm |
| Irradiation Time | 300 s | 300 s |
| Final Skin Surface Temperature | Higher than PW (>42.5°C) | 42.5°C |
| Achieved Fluence in Deep Tissue | Lower than PW (<4.2 J/cm²) | ~4.2 J/cm² |
Experimental Protocols for Thermal Analysis
To validate and characterize the thermal management strategies of laser systems, researchers can employ the following detailed methodologies, which integrate computational and experimental approaches.
Protocol 1: Computational Modeling of Deep Tissue Photobiomodulation
This protocol is adapted from a study investigating transdermal deep tissue light therapy for the human knee [64].
- Objective: To maximize light fluence in deep muscle tissue while minimizing skin temperature rise using high-intensity 1064 nm laser.
- Materials & Setup:
- Software: COMSOL Multiphysics v5.6 software or equivalent finite element modeling package [64].
- Geometric Model: A 3D anatomically correct human knee model reconstructed from Visible Human Project data, comprising layers of skin (epidermis, dermis), fat, muscle, bone, and cartilage/meniscus [64].
- Governing Equations:
- Light Propagation: The Radiative Transfer Equation (RTE) in the form of a diffusion approximation (Equation 1 in [64]) to calculate fluence rate distribution. Key input parameters are the optical properties of each tissue layer (absorption coefficient μa, reduced scattering coefficient μs').
- Heat Transfer: The time-dependent bioheat transfer equation (Equation 2 in [64]) to compute temperature rise. This incorporates heat from light absorption (Qlight = μaΦ) and heat transfer from blood perfusion (Qbio).
- Laser Parameters:
- PW Configuration: Set peak power to 60 W, pulse width to 2 ms, duty cycle to 10% (frequency 50 Hz), and beam diameter to 20 mm [64].
- CW Configuration: Use equivalent average power as the PW laser for a direct comparison.
- Procedure:
- Mesh the 3D knee geometry using the software's built-in tools.
- Assign measured optical and thermal properties to each tissue layer from published literature [64].
- Apply the laser source as a boundary condition to the skin surface.
- Run a coupled simulation solving the RTE and bioheat equations concurrently for a simulated time of 300 seconds.
- Post-process the results to extract the spatial distribution of fluence and the temperature at the skin surface and in the deep muscle tissue over time.
- Outcome Measures: The primary outcomes are the final skin surface temperature and the fluence (J/cm²) achieved in the innermost muscle tissue after 300 seconds of irradiation [64].
Protocol 2: Comparative Analysis of Welding Effects in Biological Analogs
This protocol, derived from materials science research, can be adapted using biological phantoms or tissue samples to study fundamental interaction parameters [67].
- Objective: To compare the interaction of CW and PW lasers under similar conditions of power density and interaction time.
- Materials & Setup:
- Lasers: A CW fiber laser and a PW laser (e.g., Nd:YAG).
- Sample Material: For initial method validation, use standardized materials like stainless steel shims. For biological research, transition to ex vivo tissue samples or tissue-mimicking phantoms with known optical and thermal properties.
- Beam Profiling Equipment: To accurately measure beam diameter and spatial power distribution [67].
- Thermal Camera: A high-speed infrared camera to monitor surface temperature dynamics in real-time.
- Procedure:
- Parameter Matching: For a valid comparison, match the key interaction parameters between CW and PW modes:
- Experimental Run: Conduct a series of exposures on the sample material, varying the power density while keeping interaction time and beam diameter constant.
- Thermal Monitoring: Use the thermal camera to record the peak temperature and the rate of temperature decay after each exposure or pulse.
- Outcome Measures:
- Penetration Depth/Efficiency: Measure the depth of the affected zone (e.g., coagulation, ablation). Studies show PW can achieve higher penetration depth under similar average power density and interaction time [67].
- Thermal Damage Zone: Quantify the lateral extent of the heat-affected zone around the primary interaction site.
- Thermal Recovery Kinetics: Analyze the cooling curve from the thermal camera data to characterize the tissue's thermal relaxation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Laser-Tissue Thermal Research
| Item | Function/Description | Example in Context |
|---|---|---|
| Finite Element Modeling Software | Solves coupled physics equations (light propagation, heat transfer) in complex biological geometries. | COMSOL Multiphysics with an anatomically accurate 3D knee model [64]. |
| High-Speed Infrared Thermal Camera | Non-contact, real-time monitoring of surface temperature dynamics with high spatial and temporal resolution. | Measuring peak temperature and cooling rates during and after laser pulses [67]. |
| Tissue Phantoms | Synthetic materials with tunable optical properties (μa, μs') that mimic biological tissues for standardized testing. | Used for initial calibration and validation of laser parameters before moving to ex vivo tissue [64]. |
| Beam Profiler | Measures laser beam diameter, spatial intensity profile (e.g., Gaussian, top-hat), and power density distribution. | Critical for accurately calculating the power density delivered to the target, a key input parameter [67]. |
| Pulsed Laser System with Tunable Parameters | A laser source where pulse duration, repetition rate (Hz), and pulse energy can be independently controlled. | Enables systematic study of how pulse width and duty cycle affect thermal buildup and relaxation [64] [65]. |
Visualizing Thermal Management Strategies
The following diagrams illustrate the core logical relationships and experimental workflows governing thermal management in CW and PW laser delivery.
Thermal Management Logic Flow
Computational Modeling Workflow
Cooling Methodologies and Thermal Damage Mitigation Techniques
The fundamental challenge in laser-based medical applications lies in controlling thermal energy deposition within biological tissues. The principle of selective photothermolysis guides most laser treatments, aiming to confine thermal damage to specific target chromophores while preserving surrounding healthy tissue [68]. However, the complex, multi-layered nature of skin and the dynamic changes in tissue optical properties during heating create a challenging environment for precise thermal control. Understanding these interactions is crucial for developing effective cooling strategies that mitigate collateral damage while achieving therapeutic objectives.
Thermal damage to tissue follows a non-linear relationship with temperature and exposure time. Research on porcine dermis reveals that minimal changes occur at 37°C and 43°C, while a critical threshold exists between 50°C and 60°C where significant alterations in optical properties begin [69]. At 60°C, substantial increases in reduced scattering coefficients (μs′) occur alongside variable changes in absorption coefficients (μa) across different wavelength regions [69]. The Arrhenius damage model quantitatively describes this relationship, showing an exponential increase in damage with rising temperature [69] [70]. This model integrates with heat transfer simulations to predict tissue necrosis and coagulation, providing a mathematical foundation for understanding thermal damage accumulation during laser procedures.
Fundamental Principles of Tissue Cooling
Heat Transfer Mechanisms in Biological Tissues
Cooling methodologies exploit three primary heat transfer mechanisms to protect epidermal layers during laser treatments. Conductive cooling occurs when a cooled substance or device directly contacts the skin, transferring thermal energy away from the tissue through direct molecular interaction [71]. This approach forms the basis for contact cooling devices utilizing sapphire tips, metal plates, or chilled gels. Convective cooling relies on fluid movement to carry heat away from the tissue surface, implemented through cold air convection systems that circulate cooled air across the treatment area [71]. Evaporative cooling utilizes phase change principles, where a cryogen spray absorbs thermal energy as it transitions from liquid to gas state upon contacting the skin [71]. Each mechanism offers distinct advantages for specific clinical scenarios, with varying efficiency in heat extraction capacity and depth of penetration.
The theory of spatial selectivity underpins all epidermal cooling strategies, enabling maintenance of lower temperatures at the epidermal level while achieving therapeutic temperatures at deeper target structures [71]. This thermal gradient allows clinicians to deliver higher fluence laser beams to target chromophores within blood vessels, hair follicles, or other structures while preventing damage to superficial layers. Advanced modeling approaches, including the Dual-Phase-Lag heat conduction model, provide sophisticated frameworks for simulating temperature distribution in multi-layered skin structures subjected to laser irradiation, incorporating distinct optical and thermal properties of different skin layers [72].
Thermal Damage Thresholds in Skin Tissue
Table 1: Temperature Thresholds and Tissue Effects in Laser-Tissue Interactions
| Temperature Range | Biological Effects | Optical Property Changes | Clinical Applications |
|---|---|---|---|
| 37°C - 43°C | Minimal tissue alteration; hyperthermia effects | Minimal changes in μa and μs′ [69] | Mild hyperthermia; sensitization for combination therapies [73] |
| 43°C - 50°C | Protein denaturation begins; erythema | Slight increases in both μa and μs′ [69] | Photodynamic therapy enhancement; hyperthermia treatment [73] |
| 50°C - 60°C | Coagulation necrosis; collagen contraction | Significant alterations begin; substantial increases in μs′ [69] | Thermal ablation; vessel coagulation; hair removal |
| 60°C - 70°C | Immediate coagulation; cellular dehydration | Significant increases in μs′; variable μa changes [69] | Lesion ablation; skin resurfacing |
| >70°C | Carbonization; vaporization | Progressive structural breakdown [69] | Ablative procedures; tissue incision |
The data in Table 1 demonstrates the progressive nature of thermal damage, highlighting the critical threshold between 50°C and 60°C where significant changes in tissue optical properties occur [69]. These alterations include not only immediate structural changes but also modified light-tissue interactions that affect subsequent laser pulses during treatment. The Arrhenius formalism effectively models this damage accumulation, relating the rate of tissue damage to temperature exposure through an exponential relationship that accounts for both temperature and time factors [69] [70].
Cooling Modalities: Technical Specifications and Mechanisms
Contact Cooling Systems
Contact cooling devices operate through direct physical interaction with the skin surface, facilitating heat transfer through conduction. These systems are categorized into active and passive approaches based on their heat management mechanisms.
Sapphire tip cooling represents a sophisticated active contact method where optically transparent sapphire crystals, maintained at precisely controlled temperatures (typically 0°C to 4°C), are integrated into laser handpieces [71]. These systems provide continuous cooling before, during, and after laser emission, with temperature regulation achieved through thermoelectric elements or circulating liquid cooling agents. The high thermal conductivity of sapphire enables efficient heat extraction, though the non-transparent nature of some implementations can obscure the treatment area. These systems require meticulous maintenance, including regular cleaning every 5-10 pulses to remove debris and proper disinfection between patients to prevent cross-contamination [71].
Passive contact methods include ice packs, ice cubes, and chilled aqueous gels that extract heat through energy transfer from warm skin to the colder substance. Ice cube cooling offers simplicity but presents challenges including variable cooling rates, potential for uneven contact, and patient discomfort from melting water [71]. Chilled hydrocolloid gel pads pre-cooled to approximately 8°C provide an alternative approach, though their effectiveness is limited by rapid temperature increase from 23.5°C to 27°C within 60 seconds of application [71]. Additionally, these pads can scatter laser light and obscure the treatment area, reducing procedural precision.
Non-Contact Cooling Systems
Non-contact cooling methods remove heat without physical interaction with the skin, eliminating the risk of compression-induced alterations in tissue geometry or optical properties.
Dynamic Cooling Devices (DCD) utilize precisely timed pulses of cryogen (typically R-134a tetrafluoroethane with boiling point of -26.2°C) delivered in programmed durations of 10-100 milliseconds immediately before laser exposure [71]. This approach achieves rapid surface temperature reduction to between 5°C and -9°C, approximately twice as effective as contact cooling methods [71]. The cryogen spray creates selective cooling limited to approximately 200μm of superficial tissue, allowing safe use of higher fluences while minimizing patient discomfort. DCD systems coordinate cryogen delivery and laser pulses through integrated software control, ensuring consistent thermal protection with each laser pulse regardless of operator technique.
Cold air convection systems generate high-velocity streams of cooled air directed across the treatment area, utilizing the principle of forced convection to enhance heat transfer rates. These systems provide continuous cooling throughout procedures without interfering with visual access to the treatment field. While less precise than DCD for very short pulse durations, cold air systems excel in extended procedures where ongoing thermal protection is required, particularly for larger treatment areas.
Table 2: Technical Comparison of Cooling Modalities
| Parameter | Sapphire Contact Cooling | Cryogen Spray (DCD) | Cold Air Convection | Ice Pack Cooling |
|---|---|---|---|---|
| Cooling Mechanism | Conduction | Evaporation | Convection | Conduction |
| Cooling Depth | 0.5-1mm | ~200μm | 0.1-0.5mm | 1-2mm |
| Temperature Achieved | 0°C to 4°C | -9°C to 5°C | 10°C to 20°C | 0°C to 10°C |
| Spatial Selectivity | Moderate | High | Low | Low |
| Effect on Laser Viewing | May obstruct view | No obstruction | No obstruction | Obstructs view |
| Optimal Pulse Duration | >10ms [71] | <5ms [71] | >100ms | >50ms |
| Advantages | Continuous cooling; skin compression | Precise timing; high heat extraction | Large area treatment; no consumables | Low cost; readily available |
| Limitations | Requires cleaning; expensive equipment | Consumable cryogen; loud operation | Less precise; air turbulence | Messy; temperature variability |
Experimental Approaches for Cooling Methodology Evaluation
Protocol: Evaluating Cooling Efficacy in Laser Exposures
This protocol outlines a standardized methodology for quantifying the protective efficacy of cooling systems during laser exposure, utilizing a combination of tissue phantom models and experimental measurements.
Materials and Equipment:
- Double-integrating sphere system (e.g., 3.3″ Spectralon spheres with 1.5″ sample port) [69]
- Tunable laser source (400-1100 nm wavelength range) [69]
- Thermocouple array or infrared thermal camera
- Tissue-simulating phantoms with standardized optical properties
- Cooling device under evaluation (contact or non-contact)
- Data acquisition system for temperature monitoring
Experimental Procedure:
- Sample Preparation: Prepare porcine dermis samples with standardized thickness (1.19±0.29mm) by coring 10-mm-diameter columns from tissue specimens and sectioning using a dissection microscope [69]. Maintain hydration by immersion in 0.9% normal saline solution for maximum 15 minutes before testing.
Baseline Optical Characterization: Mount samples between fused silica windows and measure baseline absorption (μa) and reduced scattering (μs′) coefficients using the double-integrating sphere system with inverse adding-doubling (IAD) analysis across the 400-1100 nm spectrum [69].
Thermal Exposure with Cooling: Apply the cooling modality according to manufacturer specifications while delivering laser energy at clinically relevant parameters. For temperature evaluation, place thermocouples at strategic depths (epidermal, mid-dermal, and deep dermal positions) or utilize infrared thermal imaging for surface temperature mapping.
Post-Exposure Analysis: Repeat optical property measurements immediately following thermal exposure to quantify cooling-induced preservation of native tissue optical properties.
Histological Correlation: Process tissue samples for histological analysis (H&E staining) to evaluate the depth and extent of thermal damage, correlating with temperature profiles and optical property changes.
Data Analysis: Calculate the thermal protection factor (TPF) as the ratio of laser energy required to produce equivalent damage with versus without cooling. Quantify changes in optical properties before and after exposure, focusing on the specific wavelength ranges relevant to the laser system under investigation. Apply the Arrhenius damage integral to model cumulative thermal damage based on recorded temperature-time profiles [69] [70].
Advanced Temperature Monitoring and Control Systems
Sophisticated temperature regulation represents a critical advancement in thermal damage mitigation. Proportional-Integral-Derivative (PID) control systems modulate laser intensity based on real-time surface temperature feedback, maintaining target temperatures with minimal overshoot [72]. Experimental validation using agar-based phantoms demonstrates strong agreement between simulated and actual temperature distributions, confirming model reliability [72].
Magnetic Resonance-guided thermal therapy (MRgHT) provides non-invasive temperature monitoring through temperature-sensitive magnetic resonance parameters, generating real-time thermal maps during treatment [73]. This approach enables precise spatial and temporal control of thermal dosing, particularly valuable for irregularly shaped treatment volumes or proximity to critical structures.
Diagram 1: Temperature Control System
Research Reagent Solutions and Experimental Materials
Table 3: Essential Research Materials for Thermal Damage Studies
| Item | Specifications | Research Application | Function |
|---|---|---|---|
| Double-Integrating Sphere System | Two 3.3″ Spectralon spheres; 1.5″ sample port [69] | Optical property quantification | Measures tissue reflectance and transmittance to calculate μa and μs′ |
| Inverse Adding-Doubling Algorithm | Software implementation of IAD method | Optical property determination | Derives absorption and scattering coefficients from sphere measurements |
| Gold Nanoparticles | PEG-coated nanorods; tuned plasmonic peaks [70] | Photothermal therapy research | Enhances selective energy absorption at specific wavelengths |
| Thermocouple Array | Micro-thermocouples (<100μm diameter) | Temperature monitoring | Provides direct tissue temperature measurement at multiple depths |
| Tissue Phantoms | Agar-based with standardized optical properties [72] | System validation | Simulates tissue optical behavior for controlled experimentation |
| Cryogen Spray System | Programmable DCD with R-134a refrigerant [71] | Cooling efficacy studies | Delivers precisely timed cryogen spurts for epidermal protection |
| Sapphire Contact Cooling | Thermoelectric cooled sapphire tips [71] | Contact cooling investigations | Provides conductive cooling with optical access |
| PID Temperature Controller | Computer-interfaced with thermocouple input [72] | Feedback system studies | Maintains target temperature through laser power modulation |
Emerging Technologies and Future Directions
Nanoparticle-Enhanced Selective Photothermolysis
The integration of gold nanoparticles (AuNPs) as photothermal transducers represents a paradigm shift in precision thermal therapies. AuNPs exhibit a unique property known as Localized Surface Plasmon Resonance (LSPR), where surface electrons collectively oscillate when exposed to light of resonant wavelengths [70]. This phenomenon creates pronounced absorption peaks that can be precisely tuned from visible to near-infrared (NIR) regions by adjusting nanoparticle dimensions and shape [70]. Gold nanorods stabilized by poly(ethylene glycol) layers have been identified as particularly effective photothermal transducers when activated by 808nm and 980nm lasers, wavelengths that correspond to tissue transparency windows where absorption by endogenous chromophores is minimized [70].
The enhanced permeability and retention (EPR) effect in tumor tissues promotes selective accumulation of AuNPs due to leaky vasculature and impaired lymphatic drainage [70]. This selective targeting, combined with the ability to functionalize nanoparticle surfaces with specific biomolecules, enables highly precise thermal ablation of pathological tissues while sparing healthy structures. Experimental studies demonstrate that AuNP-mediated photothermal therapy can achieve cytotoxic temperature elevations confined to nanoparticle-laden tissues, with temperature increases proportional to laser fluence and nanoparticle concentration [70].
Advanced Modeling of Laser-Tissue Interactions
Sophisticated computational models have become indispensable tools for optimizing cooling strategies and predicting thermal damage. While Monte Carlo simulations effectively model light transport in tissues, they require coupling with thermal models to comprehensively predict laser-tissue interactions [69]. Finite element multiphysics simulations offer a more holistic approach by integrating heat transfer and damage accumulation dynamics [69].
The Dual-Phase-Lag model has emerged as a particularly valuable framework for simulating temperature distribution in multi-layered skin structures subjected to pulsed laser irradiation [72] [70]. This model incorporates the distinct optical and thermal properties of different skin layers, significantly enhancing the accuracy of heat transfer analysis compared to traditional Pennes bioheat models. When combined with the Arrhenius damage formalism, these models can quantitatively predict the extent of protein denaturation and cellular damage based on temperature-time histories [69] [70].
Diagram 2: Nanoparticle Enhanced Photothermolysis
The strategic implementation of cooling methodologies represents a critical component in the safe and effective application of laser technologies in medicine. As research continues to elucidate the complex relationships between laser parameters, tissue optical properties, and thermal damage thresholds, cooling strategies have evolved from simple adjuvant techniques to sophisticated, integrated systems that actively shape therapeutic outcomes. The future of thermal damage mitigation lies in the continued development of smart systems that dynamically respond to real-time tissue feedback, increasingly selective nanoparticle-mediated approaches, and the refinement of computational models that can precisely predict thermal effects in individual patients. These advances will expand the therapeutic window of laser-based treatments, enabling higher efficacy with reduced morbidity across an expanding range of clinical applications.
Laser osteotomy, the process of using laser energy to cut or ablate bone, presents a promising alternative to conventional mechanical tools like oscillating saws and drills. It offers significant advantages, including high precision, minimal collateral damage, non-contact operation, and compatibility with intelligent and robotic surgical systems [74]. However, its translation from laboratory research to widespread clinical bedside application is hindered by two primary categories of challenges: ablation efficiency and the lack of real-time sensory feedback [74] [75]. The relatively lower ablation efficiency of lasers compared to mechanical tools can prolong surgical duration and associated risks, while the absence of tactile and visual feedback prevents surgeons from discerning the exact location and depth of the incision during procedures [74] [75]. This in-depth technical guide examines these core challenges within the framework of laser-tissue interactions, reviews recent advances and effective strategies for improvement, and provides detailed methodologies for researchers working at the intersection of medical technology and drug development.
Core Challenge: Ablation Efficiency and Optimization Strategies
The efficiency of laser bone ablation is not governed by a single parameter but is the result of a complex interplay of laser properties, tissue characteristics, and procedural techniques.
Fundamental Mechanisms and Influencing Factors
The interaction between laser light and bone tissue is primarily thermomechanical. The goal is to achieve precise material removal while minimizing thermal necrosis to the surrounding tissue. Bone, as a composite material, has optical and structural properties that significantly influence its absorption of laser energy. The key to efficiency lies in optimizing laser parameters to maximize the conversion of light energy into tissue ablation while minimizing passive heat diffusion. Critical factors influencing this process include:
- Laser Parameters: Wavelength, pulse energy, pulse duration, repetition rate, and spot size [74].
- Target Bone Quality: Mineral density, water content, and microvascular structure [74].
- Procedural Techniques: Cooling methodologies (e.g., spray cooling) and scanning strategies [74].
Evidence-Based Optimization Protocols
Recent research has focused on developing optimization protocols tailored to different laser types. The following table summarizes effective strategies for improving ablation efficiency, balancing maximal tissue removal with minimal collateral damage.
Table 1: Laser Parameter Optimization for Improved Ablation Efficiency
| Laser Type/Strategy | Key Optimization Parameters | Reported Effect on Efficiency | Considerations for Collateral Damage |
|---|---|---|---|
| Er:YAG Laser (λ ≈ 2.94 µm) | High water absorption, pulsed mode | High ablation efficiency in bone | Minimal thermal necrosis due to high absorption in water [74] |
| Ultrashort Pulsed Lasers (e.g., Femtosecond) | Extremely short pulse duration (10⁻¹⁵ s) | High precision via non-linear absorption; reduced heat accumulation | Significantly reduced thermal and mechanical damage zones [74] |
| Strategies: Scanning Patterns | High-speed scanning, beam shaping | More uniform energy distribution, faster material removal | Prevents heat buildup in a single spot, reducing charring [74] |
| Strategies: Cooling Methods | Simultaneous air/water spray cooling | Protects peripheral tissue from thermal damage | Allows use of higher power densities without increasing necrosis [74] |
Core Challenge: Real-Time Monitoring and Feedback Systems
The lack of sensory feedback during laser surgery is a critical barrier. Researchers are developing innovative monitoring techniques to provide surgeons with real-time data on incision profile and tissue perfusion.
Monitoring the Incision Profile
A novel method for tracking the three-dimensional lesion profile in real-time involves the detection of acoustic shock waves generated during the ablation process. This technique uses time-of-flight data from multiple acoustic detectors to triangulate the exact location of the laser-tissue interaction. One study demonstrated that incisions up to 9 mm in depth in fresh bovine tissue could be monitored with an accuracy of below 0.5 mm in all three dimensions, showing good agreement with histological examinations [75]. This approach holds promise for delivering high-precision, real-time feedback without contacting the surgical field.
Monitoring Tissue Perfusion with Laser Speckle Contrast Imaging (LSCI)
LSCI has emerged as a powerful, non-invasive tool for visualizing blood flow perfusion in real-time, which is critical in surgeries where vascular compromise can lead to severe complications like spinal cord ischemia [76] [77] [78].
LSCI functions by analyzing the speckle pattern generated when laser light illuminates tissue. Moving red blood cells cause this pattern to blur, and the degree of blurring can be quantified to compute a blood flow velocity index or Laser Speckle Perfusion Units (LSPUs), creating a 2D perfusion map [79] [77]. Its key advantages are its dye-free nature, non-invasiveness, and exceptional temporal resolution, allowing for continuous visualization of blood flow [76].
Table 2: Real-Time Monitoring Technologies in Laser-Assisted Surgeries
| Monitoring Technology | Primary Measurand | Key Advantages | Limitations & Challenges |
|---|---|---|---|
| Acoustic Shock Wave Detection | 3D Incision profile & depth | High accuracy (<0.5 mm); real-time feedback | Requires multiple acoustic detectors; signal processing complexity [75] |
| Laser Speckle Contrast Imaging (LSCI) | Microvascular blood flow (Perfusion Units) | Non-invasive, dye-free, real-time, high resolution | Sensitive to motion artifacts; provides flow velocity index, not absolute flow [76] [79] [77] |
| Indocyanine Green Videoangiography (ICG-VA) | Macrovascular anatomy & patency | High contrast visualization of vessel anatomy | Requires dye injection; not continuous; limited number of injections per procedure [79] |
| Magnetic Resonance Thermal Imaging | Real-time temperature mapping | Direct thermal monitoring; allows for feedback control | Expensive; limited to MR-guided procedures (e.g., LITT) [80] |
Clinical and Preclinical Validation of LSCI:
- Spinal Osteotomy: A clinical study used LSCI to monitor spinal cord blood flow (SCBF) during spinal deformity osteotomy. The technology successfully captured significant hemodynamic changes during different stages of surgery, including a decrease in blood flow perfusion post-osteotomy and vascular diameter changes during spinal shortening. This data helped explore safe limits for osteotomy shortening to protect spinal cord function [78].
- Intestinal Surgery: In a porcine model for intestinal ischemia, researchers successfully established a quantitative cut-off value of 69 LSPUs to differentiate between ischemic and well-perfused tissue with a sensitivity of 0.94 and specificity of 0.87. This demonstrates the potential of LSCI to provide objective, quantitative data for intraoperative decision-making [77].
- Cerebrovascular Surgery: The SurgeON system, a microscope-integrated LSCI system, provided real-time, high-resolution visualization of cerebral blood flow in preclinical models. It enabled detection of acute perfusion changes with a latency of less than 50 milliseconds, proving advantageous over ICG-VA for continuous feedback [79].
Experimental Protocols for Key Research Areas
Protocol: Quantifying Laser Ablation Efficiency in Bone
This protocol is designed to systematically evaluate the efficiency of different laser systems in ablating bone tissue.
- Sample Preparation: Use fresh, hydrated cortical bone samples (e.g., bovine or porcine femur). Machine samples into standardized blocks and maintain hydration with physiological saline.
- Laser Setup: Place the laser system on a stable optical table. Employ a motorized XYZ translation stage to move the bone sample relative to a fixed laser beam for controlled scanning.
- Parameter Definition: Independent variables include laser wavelength, pulse energy, pulse repetition rate, spot diameter, and scan speed.
- Ablation Procedure: Program the translation stage to create a grid of ablation craters or linear incisions. Apply simultaneous air/water cooling if being tested as a variable.
- Efficiency Metric Quantification:
- Ablation Volume: Measure crater dimensions using white light interferometry or confocal microscopy. Calculate volume.
- Ablation Rate: Divide ablation volume by the total irradiation time.
- Thermal Damage Zone: Histologically process sectioned samples (e.g., H&E staining) and measure the width of thermal necrosis adjacent to the ablation crater.
- Data Analysis: Correlate ablation rates and thermal damage zones with laser parameters to identify optimal settings.
Protocol: Real-Time Hemodynamic Monitoring with LSCI in Osteotomy
This protocol outlines the use of LSCI to monitor spinal cord blood flow during a preclinical spinal osteotomy model, as referenced in recent studies [76] [78].
- Animal Model and Surgical Preparation: Utilize a relevant animal model (e.g., New Zealand white rabbit). Induce general anesthesia and perform a dorsal midline incision to expose the vertebrae and spinal cord at the target level (e.g., L4-L5).
- LSCI System Setup: Position the LSCI camera (e.g., RFLSI III system) perpendicular to the exposed spinal cord, maintaining a fixed distance (e.g., 20-30 cm). Calibrate the system according to manufacturer specifications. Ensure operating room lights are dimmed during imaging.
- Baseline Data Acquisition: Record baseline LSCI data (blood flow perfusion in Perfusion Units - PU, and posterior spinal artery diameter) before any osteotomy is performed.
- Osteotomy and Sequential Monitoring: Perform a standardized pedicle subtraction osteotomy (PSO). Acquire LSCI data at critical stages:
- Pre-osteotomy (Baseline)
- Post-osteotomy completion
- Post-osteotomy site compression
- Post-dura removal (if applicable)
- Data Analysis: Use the LSCI system's software to quantify perfusion units and vessel diameters at each region of interest (ROI) for all time points. Perform statistical analysis (e.g., paired t-tests) to compare changes from baseline.
LSCI Monitoring Workflow for Osteotomy
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Laser Osteotomy Studies
| Item/Category | Function & Application in Research | Specific Examples / Notes |
|---|---|---|
| Pulsed Laser Systems | Source of ablative energy for cutting bone; defined by wavelength & pulse duration. | Er:YAG (λ=2.94µm), CO₂ (λ=10.6µm), Femtosecond lasers (e.g., Ti:Sapphire) [74] |
| Fresh Bone Samples | Ex vivo substrate for ablation efficiency studies; must be hydrated. | Bovine or porcine cortical bone; maintained in physiological saline [74] [75] |
| Motorized Translation Stage | Provides precise, computer-controlled movement of sample or laser beam. | Enables creation of standardized ablation craters and incisions for repeatable experiments |
| LSCI System | Real-time, non-invasive imaging of microvascular blood flow perfusion. | RFLSI III system; PerfusiX-Imaging system for laparoscopic use [76] [77] |
| Acoustic Sensor Array | Detection of shock waves for real-time 3D incision profile monitoring. | Used with time-of-flight algorithms to reconstruct ablation front location [75] |
| Histology Stains | Post-ablation analysis of tissue damage and thermal necrosis. | Hematoxylin and Eosin (H&E) to measure zone of thermal alteration [74] |
| Calibration Phantoms | Ensures accuracy and reproducibility of optical imaging systems. | Reflectance phantom (for LSCI daily calibration); flow phantom (for weekly validation) [76] |
Overcoming the challenges in laser osteotomy requires a multi-faceted approach. Future progress hinges on the development of intelligent feedback systems that integrate real-time monitoring data—from acoustic shock wave detection, LSCI, and thermal imaging—to dynamically control laser parameters during surgery [74] [75]. Furthermore, addressing the bone quality variable through systematic experiments and creating patient-specific models will be crucial for robust clinical application [74]. The continued advancement and integration of these technologies promise to transform laser osteotomy from a promising laboratory technique into a reliable, efficient, and safe clinical reality that can transform conventional orthopedic surgical approaches.
Safety Thresholds and Tissue-Specific Treatment Windows
The efficacy and safety of medical laser applications are governed by the precise interplay between laser parameters and the optical properties of biological tissues. A fundamental understanding of laser-tissue interactions is paramount for researchers developing laser-based therapies and safety standards. This guide details the core principles, quantitative safety thresholds, and experimental methodologies that define the treatment windows for effective and safe laser use in medical applications. The deterministic nature of these interactions allows researchers to predict biological outcomes—from therapeutic bio-stimulation to irreversible thermal damage—based on specific laser settings [81].
Fundamental Laser Properties and Tissue Interaction Mechanisms
Essential Laser Properties
Laser light possesses four unique properties that distinguish it from ordinary light and are critical for medical applications [81]:
- Coherence: Laser light waves are in phase both spatially and temporally. This property, derived from stimulated emission, is the most fundamental and allows laser energy to be concentrated effectively [81].
- Monochromaticity: Laser light consists of photons of a single, characteristic wavelength. This enables selective targeting of tissue chromophores based on their absorption spectra [81].
- Directionality: The laser beam exhibits minimal divergence, allowing it to maintain high energy density over long distances and be focused onto very small spots for precise interventions [81].
- High Intensity/Brightness: As a result of directionality and coherence, lasers can achieve extremely high power densities, which translate to potent tissue effects when focused [81].
Primary Laser-Tissue Interaction Mechanisms
The interaction of laser light with tissue is primarily determined by the laser wavelength and the optical properties of the target tissue. The main interaction mechanisms are [81]:
- Photothermal Interaction: The most common mechanism, where light energy is absorbed and converted into heat, leading to effects ranging from hyperthermia to vaporization.
- Photochemical Interaction: Involves the use of light to initiate or accelerate chemical reactions, such as in Low-Level Laser Therapy (LLLT) or Photodynamic Therapy (PDT).
- Photoablative Interaction: High-intensity pulsed lasers can break molecular bonds directly, ablating tissue with minimal thermal damage to surrounding areas.
- Stimulated Emission: The foundational process for laser operation itself, where an incoming photon stimulates an excited atom to emit a second photon identical in phase, direction, and wavelength [81].
Quantitative Safety Thresholds and Damage Data
Establishing safety thresholds is critical for protecting both patients and operators. The damage threshold is typically defined as the radiant exposure (energy per unit area, J/cm²) or irradiance (power per unit area, W/cm²) associated with a 50% probability of creating a minimum visible lesion (ED₅₀) [82].
Skin Damage Thresholds for Near-Infrared Lasers
Table 1: Experimental ED₅₀ Damage Thresholds for Porcine Skin Exposed to 1319-nm Laser Radiation [82]
| Exposure Duration (s) | Beam Diameter (cm, 1/e²) | Post-Exposure Observation Time | ED₅₀ Threshold (J/cm²), Peak Radiant Exposure |
|---|---|---|---|
| 0.4 | 0.98 | 1 hour | 35.5 |
| 1.0 | 0.98 | 1 hour | 36.1 |
| 3.0 | 0.98 | 1 hour | 32.1 |
| 3.0 | 1.96 | 1 hour | 37.1 |
| 0.4 | 0.98 | 24 hours | Slight increase from 1-hour value |
| 1.0 | 0.98 | 24 hours | Slight increase from 1-hour value |
| 3.0 | 0.98 | 24 hours | 28.6 |
Histopathological Damage Characteristics
The nature of tissue damage varies with the exposure level relative to the ED₅₀ threshold [82]:
- Near-Threshold Level: Damage characteristics include gathering of nuclear chromatin and cell vacuolation in the epidermis, and deposition of blood cells in capillary vessels.
- Apparently Above-Threshold Level: Damage is more severe, featuring obvious stretching of nuclear chromatin in the epidermis, closing of capillary lumen, structural change of collagen fibers, and coagulative necrosis of hair follicle cells. Damage can penetrate deep into the fatty tissue.
Experimental Protocols for Determining Laser Safety Thresholds
In-Vivo Skin Damage Threshold Determination
The following methodology, adapted from a porcine skin study, provides a robust protocol for determining ED₅₀ [82].
Objective: To determine the ED₅₀ damage threshold and characterize histopathological damage from 1319-nm laser radiation.
Materials and Reagents: Table 2: Research Reagent Solutions and Essential Materials
| Item Name | Function/Description |
|---|---|
| Diode-Pumped Continuous-Wave Nd:YAG Laser | Light source emitting at 1319 nm wavelength. |
| Guizhou Miniature Pigs | In-vivo animal model; porcine skin is histologically similar to human skin. |
| Electronically Controlled Mechanical Shutter | Precisely controls laser exposure duration. |
| Calibrated Laser Power Meters (e.g., Ophir) | Measures incident laser power and ensures power stability during exposure. |
| Beam Splitter (Fused Quartz) | Reflects a constant proportion of laser power to a reference power meter for stability monitoring. |
| Histopathology Staining Reagents | For processing and analyzing skin biopsies to characterize tissue damage. |
Experimental Procedure:
Laser Calibration and Setup:
- Position the laser system and ensure stable output.
- Place a calibrated laser power meter at the target surface to measure the power incident on the skin.
- Use a beam splitter and a reference power meter to monitor laser power stability throughout the experiment.
- Characterize the beam diameter (e.g., 0.98 cm or 1.96 cm 1/e² diameter).
Animal Preparation and Exposure:
- Anesthetize the animal model according to approved ethical guidelines.
- Position the target skin area perpendicular to the laser beam.
- For each exposure site, deliver a single pulse of laser radiation at a specific power and duration (e.g., 0.4, 1.0, 3.0 s).
- Administer a range of radiant exposures (J/cm²) to different sites to generate a dose-response curve.
Lesion Determination and Analysis:
- Examine each exposure site for damage at predetermined post-exposure times (e.g., 1 hour and 24 hours).
- A positive damage endpoint is typically defined as a minimally visible lesion.
- Use Bliss probit analysis (or similar statistical method) on the dose-response data to calculate the ED₅₀ threshold and its confidence intervals.
Histopathological Examination:
- At a later time point (e.g., 48 hours post-exposure), harvest skin samples from exposed sites.
- Process the tissue for histological analysis (fixation, sectioning, staining with H&E).
- Examine under a microscope to characterize the depth and nature of tissue damage (e.g., epidermal vacuolation, collagen changes, coagulative necrosis).
Visualization of Laser-Tissue Interaction and Experimental Workflow
Standardized Reporting Guidelines for Laser Therapy Research
To improve the clarity, reproducibility, and scientific rigor of laser-based medical studies, researchers should adopt standardized reporting guidelines. Key parameters that must be documented include [83]:
- Wavelength (nm): Directly influences tissue penetration and chromophore targeting.
- Power Density or Irradiance (W/cm²): The power delivered per unit area.
- Energy (J): The total energy delivered per pulse (for pulsed lasers).
- Energy Density or Radiant Exposure (J/cm²): The total energy delivered per unit area, a critical dosimetry parameter.
- Beam Characteristics: Including spot size, profile, and mode structure.
Common issues in the literature include missing data, miscalculated doses, and unverified device specifications. Adhering to a structured checklist for reporting treatment protocols enhances the accuracy, transparency, and comparability of laser-based studies [83].
The deterministic relationship between laser parameters and tissue effects provides a scientific foundation for establishing safety thresholds and treatment windows. Quantitative ED₅₀ data, such as the 28.6-37.1 J/cm² range for 1319-nm laser exposure on porcine skin, forms the basis for safety standards like the American National Standards Institute Z136 series on Maximum Permissible Exposures (MPEs) [82]. A rigorous experimental approach, combined with comprehensive histopathological analysis and adherence to standardized reporting guidelines, is essential for advancing the field of laser-tissue interactions and ensuring the safe and effective application of laser technology in medicine. Future work should focus on expanding the damage threshold database across more wavelengths and exposure durations, and correlating experimental findings with computational models.
Validation Methodologies and Comparative Analysis of Laser Technologies
In the field of laser-tissue interactions research, experimental validation is paramount for translating theoretical models into clinically reliable applications. The fundamental principles of laser-tissue interactions involve complex photothermal, photochemical, and photomechanical processes that require rigorous experimental verification [4]. Among the most critical techniques for this validation are thermography, which provides real-time spatial and temporal mapping of temperature distributions, and histological analysis, which offers post-processing microscopic assessment of tissue effects. These methodologies form the cornerstone of experimental validation in photomedicine, enabling researchers to correlate predictive models with actual biological outcomes. This technical guide examines the principles, protocols, and applications of these indispensable techniques within the context of laser-tissue interactions research, providing a comprehensive framework for their implementation in scientific studies and therapeutic development.
Fundamentals of Laser-Tissue Interactions
Laser-tissue interaction is governed by the interplay between laser parameters (wavelength, pulse duration, power density) and tissue properties (optical, thermal, and structural characteristics). The primary chromophores in biological tissues—melanin, hemoglobin, water, and hydroxyapatite—exhibit wavelength-dependent absorption profiles that determine the nature and extent of laser effects [4]. When laser energy is delivered to tissue, it may be reflected, scattered, transmitted, or absorbed, with absorbed energy being converted primarily to heat, leading to various temperature-dependent tissue effects.
The thermal effects on biological tissues follow a predictable progression based on achieved temperatures: hyperthermia (40-50°C) causes reversible molecular changes and reduced enzyme activity; coagulation (60-80°C) induces irreversible protein denaturation; vaporization (100°C) transforms tissue water to steam; carbonization (>100°C) desiccates and blackens tissue; and melting (>300°C) produces tissue fusion [17]. The 60°C threshold is particularly critical as it represents the point where most biological effects become irreversible, making accurate temperature monitoring essential for controlled therapeutic outcomes.
Table 1: Thermal Effects of Laser Energy on Biological Tissues
| Temperature Range | Biological Effects | Clinical Significance |
|---|---|---|
| 37°C | Normal physiological temperature | Baseline state |
| 45-50°C | Hyperthermia, reduced enzyme activity, cell immobility | Reversible effects |
| 60-80°C | Protein denaturation, coagulation, necrosis | Irreversible tissue damage |
| 100°C | Vaporization, thermal decomposition | Ablation with tissue removal |
| >100°C | Carbonization | Tissue blackening, smoke formation |
| >300°C | Melting | Tissue fusion |
Thermography in Laser-Tissue Research
Principles and Techniques
Infrared thermography (IRT) is a non-invasive, non-contact imaging technique that detects infrared radiation emitted by the body surface and converts it into temperature maps called thermograms [84]. This method leverages the principle that all objects above absolute zero emit infrared radiation, with intensity proportional to their temperature. Modern infrared cameras can detect minute temperature differences as subtle as 0.02°C with high spatial resolution, making them ideal for monitoring laser-induced thermal changes in tissues [84].
Medical thermography encompasses several modalities: passive thermography measures naturally occurring temperature distributions without external stimulation; active thermography applies thermal stimuli to assess dynamic thermal responses; and dynamic thermography records temperature evolution over time [84]. In laser-tissue interactions research, thermography enables real-time monitoring of temperature distributions, allowing researchers to validate theoretical models and optimize laser parameters for specific applications.
Experimental Protocols and Setup
A standardized protocol for thermographic validation in laser-tissue studies involves several critical steps. First, the thermal camera must be calibrated and positioned perpendicular to the tissue surface at an appropriate distance to ensure accurate temperature measurement and minimize angular distortion. Environmental conditions must be controlled, with stable room temperature (20-24°C) and humidity (40-60%) maintained throughout experiments to reduce thermal artifacts [84].
The laser delivery system should be configured to irradiate the target tissue with precisely controlled parameters (wavelength, power, spot size, exposure duration). Simultaneously, the thermal camera acquires sequential images at a frame rate sufficient to capture transient thermal phenomena—typically ranging from milliseconds for pulsed lasers to seconds for continuous-wave applications [85]. For in vivo studies, additional considerations include tissue perfusion effects and the potential need for respiratory or motion compensation in living subjects.
Figure 1: Thermographic Experimental Workflow for Laser-Tissue Validation
Data Interpretation and Analysis
Thermographic data analysis involves both qualitative assessment of thermal patterns and quantitative evaluation of temperature distributions, gradients, and temporal profiles. Key parameters include maximum temperature rise, spatial extent of specific temperature thresholds, thermal diffusion rates, and thermal dose accumulation [85]. Advanced analysis may incorporate mathematical models such as the Pennes bioheat equation to correlate surface temperatures with subsurface thermal profiles:
The Pennes bioheat equation is expressed as:
ρc(∂T/∂t) = ∇·(k∇T) + ρ_b*c_b*ω_b*(T_b - T) + Q_m + Q_r [86]
Where ρ is tissue density, c is specific heat capacity, k is thermal conductivity, ρb and cb are blood density and specific heat, ωb is blood perfusion rate, Tb is arterial blood temperature, Qm is metabolic heat generation, and Qr is heat source from laser radiation.
Table 2: Thermal Properties of Biological Tissues Relevant to Thermography
| Tissue Type | Thermal Conductivity (W/mK) | Heat Capacity (J/kgK) | Blood Perfusion Rate (ml/min/g) |
|---|---|---|---|
| Skin | 0.21-0.41 | 3300-3600 | 0.15-0.20 |
| Muscle | 0.45-0.55 | 3500-3800 | 0.02-0.07 |
| Fat | 0.16-0.21 | 2200-2500 | 0.012-0.015 |
| Brain | 0.48-0.57 | 3600-3800 | 0.46-1.0 |
Applications and Validation Studies
Thermography has been extensively employed to validate finite element models of laser-tissue interactions. In one notable study, researchers used thermographic measurements to compare continuum and vascular models of laser irradiation on excised rat skin and live mouse tissue [85]. The vascular model, which incorporated discrete blood vessels and perfusion effects, demonstrated superior predictive capability for in vivo conditions, accurately capturing the cooling effect of blood flow in perfused tissues.
Another application involves monitoring laser interstitial thermal therapy (LITT) for neurological disorders. In a recent study, researchers developed a finite element model for 1,064 nm LITT and validated it through in vivo experiments on canine models and human epilepsy patients [86]. Magnetic resonance thermometry correlated with surface thermography measurements confirmed the model's accuracy in predicting both temperature profiles and ablation zones, enabling improved preoperative planning for laser ablation procedures.
In dental research, thermography has proven valuable for visualizing thermal developments during laser irradiation of oral mucosa models. A novel tissue model system demonstrated distinct thermal patterns for different laser wavelengths (445 nm vs. 810 nm) at identical power settings (2W continuous wave for 10 seconds), with the 445 nm laser producing significantly higher temperatures (151°C vs. 62°C) at the epithelial-subepithelial interface [87].
Histological Analysis in Laser-Tissue Research
Principles and Tissue Processing
Histological analysis represents the gold standard for post-treatment assessment of laser effects on biological tissues, providing detailed microscopic evaluation of structural changes at the cellular level [88]. This technique enables qualitative and quantitative assessment of thermal damage zones, inflammation responses, healing progression, and distribution of degradation products in the surrounding tissue.
Proper histological processing involves sequential steps: fixation preserves tissue structure using agents like formalin; dehydration removes water through graded alcohol solutions; embedding infiltrates tissue with supporting media such as paraffin or resin; sectioning cuts embedded tissue into thin slices (typically 5-15 μm) using a microtome; and staining enhances contrast for microscopic visualization [88] [89]. For hard tissues or implants containing metal components, specialized processing techniques may be required, including plastic embedding and diamond-edged sectioning.
Staining Techniques and Interpretation
A variety of staining methods enable specific identification of tissue structures and laser-induced changes:
Hematoxylin and Eosin (H&E): The most common staining method, with hematoxylin coloring nuclei blue and eosin coloring cytoplasm and connective tissue pink [88]. This general stain provides overview of tissue architecture and cellular morphology.
Masson's Trichrome: Differentiates connective tissue (blue) from cellular components (red), useful for identifying collagen reorganization and fibrosis in response to thermal injury [88].
Specialized stains: Tartrate-resistant acidic phosphatase identifies osteoclasts; Turnbull blue and Prussian blue evaluate iron ions in tissue; immunofluorescence staining detects specific protein markers [88].
Histological assessment of laser effects focuses on identifying zones of thermal alteration characterized by changes in tissue morphology, collagen denaturation, nuclear pyknosis or disappearance, and vacuolization. The thermal damage zone is typically measured from the ablation crater edge to normal tissue, with precise quantification of coagulation thickness providing critical validation data for thermal models.
Figure 2: Histological Processing Workflow for Laser-Tissue Analysis
Quantitative Histomorphometry
Advanced computational tools enable quantitative analysis of histological specimens, moving beyond qualitative assessment to precise morphometric measurements. Digital histopathology platforms like ImageJ, CellProfiler, and QuPath facilitate automated segmentation of tissue regions, cell counting, damage zone quantification, and spatial distribution analysis of specific cell types [88]. These tools can calculate the percentage of new bone formation in osseous tissues, measure thermal coagulation thickness, and assess inflammatory cell infiltration in response to laser treatment.
For thermal damage assessment, the Arrhenius integral formalism provides a mathematical framework for correlating thermal history with tissue necrosis:
Ω(t) = A ∫₀ᵗ exp(-E/RT(t')) dt'
Where Ω is the damage integral, A is the frequency factor, E is the activation energy, R is the universal gas constant, and T is absolute temperature [17]. This model allows researchers to predict the extent of tissue damage based on temperature-time histories and validate these predictions against histological measurements.
Applications in Laser-Tissue Interaction Studies
Histological analysis has been instrumental in characterizing the effects of various laser parameters on different tissue types. A comprehensive review of 28 studies examining oral soft tissue biopsies found that while all laser wavelengths produced some degree of thermal effect at incision margins, this did not generally hinder histological diagnosis when appropriate parameters were used [90]. The carbon dioxide (CO₂) laser was the most extensively studied, followed by diode lasers (940-980 nm), Nd:YAG (1064 nm), and Er:YAG (2940 nm) lasers.
In bone tissue studies, histological analysis has revealed important insights into laser-osseous interactions. Following laser ablation, distinct histological zones are typically observed: a superficial carbonization layer, an underlying zone of thermal necrosis, a region of reversible thermal damage, and finally normal tissue. The thickness of these zones varies significantly with laser parameters, particularly wavelength and pulse duration, with shorter pulsed lasers generally producing narrower thermal damage zones.
Histological validation has been crucial for optimizing laser settings in dermatological applications. Studies comparing continuous-wave versus pulsed laser irradiation have demonstrated histologically that pulsed lasers can achieve higher peak temperatures with less collateral thermal damage, supporting their use for precise cutaneous procedures where preservation of surrounding tissue is critical [85].
Integrated Validation Approaches
Correlative Methodology
The most comprehensive validation of laser-tissue interactions combines thermographic and histological techniques in a correlative approach. Real-time thermography captures dynamic temperature fields during laser exposure, while subsequent histological analysis provides post-treatment confirmation of biological effects. Together, these methods enable researchers to establish precise temperature-threshold relationships for specific tissue effects and validate computational models against both physical measurements (temperature) and biological outcomes (tissue damage).
This integrated approach was effectively demonstrated in a study comparing short-pulse and continuous-wave laser irradiation, where thermographic measurements showed that pulsed lasers produced higher initial temperature rises and thermal doses than continuous-wave lasers of equal average power [85]. Histological analysis corroborated these findings, revealing corresponding differences in the extent and characteristics of thermal damage zones in tissue samples.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Laser-Tissue Interaction Studies
| Item | Function | Application Notes |
|---|---|---|
| Infrared Thermal Camera | Non-contact temperature mapping | Requires appropriate spectral range for tissue temperatures; calibration critical |
| Laser Systems | Controlled energy delivery to tissue | Wavelength selection based on target chromophores; precise power control essential |
| Formalin Solution | Tissue fixation preserves morphology | Typically 10% neutral buffered formalin; adequate fixation time required |
| Paraffin Embedding Medium | Tissue support for sectioning | Alternative resins for hard tissues or implants |
| H&E Staining Kit | Basic cellular morphology assessment | Standard for initial tissue evaluation |
| Specialized Stains | Specific tissue component identification | Masson's Trichrome for connective tissue; Prussian blue for iron |
| Microtome | Thin sectioning of embedded tissues | Section thickness typically 5-15μm |
| Light Microscope | Histological specimen visualization | Digital imaging capabilities recommended for analysis |
| Image Analysis Software | Quantitative histomorphometry | ImageJ, CellProfiler, or commercial alternatives |
Thermography and histological analysis represent complementary pillars of experimental validation in laser-tissue interactions research. Thermography provides non-invasive, real-time monitoring of temperature distributions, enabling validation of computational models and dynamic control of laser parameters. Histological analysis offers irreplaceable microscopic assessment of tissue effects, confirming biological outcomes and establishing correlation between thermal history and tissue response. Together, these techniques form a robust validation framework that bridges the gap between theoretical predictions and biological reality, supporting the continued advancement of laser-based medical therapies. As laser technologies evolve and new applications emerge, the sophisticated application of these validation methodologies will remain essential for ensuring both efficacy and safety in photomedicine.
The interaction between laser light and biological tissue represents a cornerstone of modern therapeutic and diagnostic applications. Within this domain, two fundamental parameters—wavelength and pulse duration—exert profound influence over treatment efficacy and safety. Wavelength determines the depth of light penetration and its absorption by specific tissue chromophores, while pulse duration governs the nature of energy delivery and subsequent thermal effects. This whitepaper synthesizes current research to provide a comprehensive technical analysis of how these parameters interact with biological tissues, offering researchers in laser-tissue interactions a structured framework for experimental design and parameter selection. The precise control of these variables enables optimization of outcomes across diverse applications ranging from photobiomodulation and pain management to precise surgical ablation.
Wavelength-Dependent Tissue Interactions
Fundamental Optical Properties in Biological Tissues
The propagation of laser light through biological tissue is governed primarily by absorption and scattering phenomena. These processes are strongly wavelength-dependent due to the specific absorption spectra of key tissue chromophores, including hemoglobin, melanin, water, and lipids [2] [91]. The collective absorption profiles of these components create what is known as the "therapeutic window" or "optical window" in the near-infrared (NIR) region between approximately 650-1350 nm, where light penetration is maximized due to relatively low absorption and scattering coefficients [92] [91].
When laser light impinges on tissue, approximately 4-7% of the incident energy is typically reflected at the air-tissue interface due to differences in refractive index [2]. The remaining energy undergoes exponential attenuation as it propagates through tissue, a phenomenon quantitatively described by the Beer-Lambert law [2]. The depth at which light intensity falls to 1/e (approximately 37%) of its surface value is defined as the optical penetration depth (δ), which is inversely related to the absorption coefficient (μa) and reduced scattering coefficient (μs') [2].
Comparative Analysis of Common Wavelengths
Table 1: Absorption Coefficients and Penetration Depth of Laser Wavelengths in Biological Tissues
| Wavelength (nm) | Absorption Coefficient (α, cm⁻¹) | Relative Penetration Depth | Primary Chromophores | Representative Applications |
|---|---|---|---|---|
| 450 (Blue) | 26.8 [2] | Shallow | Hemoglobin | Vaporization, coagulation [93] |
| 532 (Green) | Moderate [2] | Shallow | Hemoglobin, melanin | Pigment treatment, vascular lesions |
| 671 (Red) | Lower than 532 nm [92] | Moderate | Hemoglobin, melanin | Photobiomodulation, superficial treatments [92] |
| 810 (NIR) | 9.60 [2] | Deep | Water, hemoglobin | Deep tissue photobiomodulation [2] |
| 905 (NIR) | N/A | Deep | Water, hemoglobin | Musculoskeletal treatment [91] |
| 980 (NIR) | Higher than 810 nm [2] | Moderate | Water (absorption peak) | Soft tissue surgery |
| 1064 (NIR) | Lower than 905 nm [91] | Very Deep | Water, hemoglobin | Deep tissue therapy, pain management [64] [91] |
| 2940 (Er:YAG) | 144.8 [2] | Very Shallow | Water | Precise ablation, dental procedures [2] |
Among the tested wavelengths in ex vivo porcine gingival tissue, 810 nm exhibited the lowest absorption (α = 9.60 cm⁻¹), indicating the deepest potential penetration, while the Er:YAG laser at 2940 nm demonstrated the highest absorption (α = 144.8 cm⁻¹) [2]. The complete ranking of absorption from highest to lowest is: 2940 nm > 2780 nm > 450 nm > 480 nm > 532 nm > 1341 nm > 632 nm > 940 nm > 980 nm > 1064 nm > 810 nm [2].
Comparative studies between 905 nm and 1064 nm wavelengths have demonstrated that 1064 nm light consistently achieves higher transmittance through both porcine skin and bovine muscle tissue, with the most significant differences (up to 5.9%) observed in the upper 10 mm of tissue [91]. This advantage diminishes with increasing tissue thickness, highlighting the wavelength-dependent nature of light propagation through different tissue geometries and compositions.
Thermal Relaxation Time (TRT) Considerations
The thermal relaxation time (TRT) represents the time required for a targeted tissue to dissipate approximately 63% of the absorbed thermal energy to its surrounding structures. This parameter is critically important for minimizing collateral thermal damage during laser procedures. TRT is directly proportional to the square of the optical penetration depth and inversely proportional to the thermal diffusivity of the tissue [2]. Consequently, wavelengths with deeper penetration (such as 1064 nm and 810 nm) exhibit longer TRT, allowing for more extended pulse durations without significant conductive heat transfer to adjacent structures.
Pulse Duration Effects on Laser-Tissue Interactions
Continuous Wave versus Pulsed Wave Delivery
Laser systems can deliver energy in either continuous wave (CW) or pulsed wave (PW) modes, each with distinct advantages and limitations for specific applications. CW lasers provide constant power output, which can be effective for certain therapeutic applications but poses challenges with uncontrolled temperature elevation in superficial tissues during deep tissue treatments [64].
PW lasers introduce "quench periods" (pulse OFF times) between energy deliveries, allowing for heat dissipation and significantly reducing cumulative thermal buildup [64]. This enables the safe use of higher peak power densities than would be achievable with CW applications, thereby enhancing therapeutic efficacy while maintaining safety margins [64]. Research has demonstrated that PW irradiation achieves lower skin temperatures compared to CW exposure under comparable energy delivery conditions, supporting the rationale for PW configurations in clinical applications where thermal safety is paramount [64].
Pulse Duration Parameters and Thermal Effects
The thermal response of biological tissues to laser irradiation is governed not only by wavelength but also critically by pulse duration. Different pulse durations activate distinct thermal mechanisms that significantly influence the surgical effect and collateral damage.
For high-intensity deep tissue therapy at 1064 nm, optimized parameters include pulse widths of 2 ms with a 10% duty cycle and 50 Hz frequency, which achieved the lowest skin surface temperature (42.5°C) while maintaining effective fluence (approximately 4.2 J/cm²) at depth [64]. These parameters intentionally allow controlled thermal diffusion to regulate surface temperature, making them suitable for non-ablative, high-intensity laser therapy applications targeting deep tissue [64].
Advanced Pulsing Schemes
Recent research has explored sophisticated pulsing strategies to optimize therapeutic outcomes. Dual-pulse schemes with specific energy distribution ratios represent an innovative approach to enhancing efficacy while minimizing adverse effects. In pigment treatment using 1064 nm Q-switched Nd:YAG lasers, a dual-pulse mode with an 8:2 energy distribution ratio (D8:2) demonstrated superior performance compared to single-pulse or equal-energy dual-pulse modes [94].
This approach delivers an initial suprathreshold fluence pulse for effective ablation followed by a subthreshold fluence pulse that modulates biological responses. The D8:2 scheme achieved a 75% reduction in melanophore count compared to 54% for single pulses, while simultaneously minimizing laser-induced thermal damage and downregulating melanogenesis-related genes (SOX10, MITFa, TYR, TYRP1b, and DCT) [94].
Similarly, in ultrafast laser processing of fused silica, intensity ramp modulation significantly influences ablation efficiency. Downward ramp modulation (starting with high intensity pulses) demonstrated significantly enhanced ablation efficiency compared to upward ramps, attributed to reduced ablation threshold through defect formation by initial intense pulses [95]. This incubation effect—where preceding pulses influence the absorption and ablation characteristics for subsequent pulses—persists across repetition rates from 100 Hz to 1 MHz [95].
Experimental Methodologies for Parameter Analysis
Measurement of Penetration Depth and Absorption
Table 2: Key Research Reagent Solutions for Laser-Tissue Interaction Studies
| Material/Equipment | Specification | Function/Application |
|---|---|---|
| Porcine tissue samples | Gingival, skin, or liver tissue | Ex vivo model for laser-tissue interaction studies [2] [93] |
| Bovine muscle tissue | Fresh specimens from commercial sources | Penetration depth measurements in muscular tissue [91] |
| Optical Parametric Oscillator (OPO) system | Visible-range (VIS-OPO) with BBO crystal | Generation of specific wavelengths (450-1341 nm) [2] |
| Infrared OPO system | MIR-OPO with LiNbO3 crystal | Generation of mid-infrared wavelengths (2780-2940 nm) [2] |
| Power measurement system | Gentec-EO power meter or thermal power sensor | Quantification of input/output laser power [2] [91] |
| Beam profiling camera | LT665 with BeamGage software | Spatial intensity distribution analysis [91] |
| Fast photodiode sensor | FPD-VIS300 with oscilloscope | Temporal pulse profile characterization [91] |
| Glass slides | FOCTEK IN140728-15 with minimal attenuation | Tissue mounting for transmission measurements [2] |
| COMSOL Multiphysics | v5.6 with finite element method | Computational modeling of light and heat transport [64] |
| Monte Carlo simulation | MCX code for light transport | 3D modeling of light distribution in tissues [93] |
The experimental workflow for determining wavelength-specific tissue absorption and penetration depth follows a systematic approach as illustrated below:
For ex vivo measurements, tissues are harvested immediately post-slaughter and processed within 2 hours to maintain optical properties [2]. Samples are typically cut to standardized dimensions (e.g., 1.5 cm × 1.5 cm) with varying thicknesses (0.50-1.00 mm) measured using calibrated electronic micrometers [2]. Each sample is mounted between glass slides with minimal light attenuation in a stabilization device to ensure consistent orientation and prevent dehydration during testing [2].
Laser irradiation is performed across multiple wavelengths (e.g., 450, 480, 532, 632, 810, 940, 980, 1064, 1341, 2780, and 2940 nm) using Optical Parametric Oscillator (OPO) systems at controlled power levels (typically 100 mW with 1 mm spot size) in continuous wave mode [2]. Input and output powers are measured using calibrated power meters, enabling transmittance calculation through the Beer-Lambert law: I = I₀e^(-αx), where I is transmitted intensity, I₀ is incident intensity, α is absorption coefficient, and x is tissue thickness [2].
Computational Modeling of Light and Heat Transport
Computational approaches provide powerful tools for analyzing laser-tissue interactions without extensive experimental trials. The finite element method implemented in platforms like COMSOL Multiphysics enables coupled modeling of light propagation and heat transfer using the radiative transfer equation (RTE) and bioheat transfer equation [64].
The RTE in its diffusion approximation form is expressed as:
1/c · ∂ϕ(r,t)/∂t - ∇·[D(r,t)∇ϕ(r,t)] + μₐϕ(r,t) = S(r,t)
where ϕ is light irradiance (W/cm²), D is diffusion coefficient (cm), μₐ is absorption coefficient (cm⁻¹), c is light speed in tissue (m/s), and S is light source (W/cm³) [64].
The bioheat equation accounts for thermal effects:
ρCₚ · ∂T/∂t + ∇·(-k∇T) = Qlight + Qbio
where ρ is density (kg/m³), Cₚ is heat capacity (J·kg⁻¹·K⁻¹), k is thermal conductivity (W·m⁻¹·K⁻¹), Qlight is heat from light absorption (μₐΦ), and Qbio is heat transfer from blood perfusion [64].
Monte Carlo simulations offer an alternative approach for modeling light transport in complex tissues, particularly valuable for predicting vaporization and coagulation regions by incorporating dynamic changes in optical properties during laser exposure [93]. These methods allow researchers to model the effects of various laser parameters (wavelength, power, pulse duration, spot size) on light distribution and subsequent thermal effects before conducting physical experiments.
Threshold Determination and Incubation Effects
The ablation threshold represents a critical parameter for laser applications involving tissue removal. For Q-switched Nd:YAG laser treatment of pigmented lesions, the ablation threshold for zebrafish melanophores was determined to be approximately 0.53 J/cm² (66.0 mJ) through probit analysis of morphological changes following single-pulse irradiation at varying energy levels [94].
The incubation effect—reduction in ablation threshold with multiple pulses—follows an exponential relationship described by:
Fth(N) = Fth,∞ + [Fth,¹ - Fth,∞] · e^(-k(N-1))
where Fth(N) is the multi-pulse threshold fluence, Fth,¹ is the single-pulse threshold, Fth,∞ is the saturation threshold for large N, and k is the incubation coefficient [96]. This model accurately describes the saturation of threshold fluence observed at higher pulse counts (N > 100) in various materials including biological tissues and synthetic dielectrics [96].
The strategic selection of wavelength and pulse duration parameters represents a fundamental aspect of optimizing laser-based therapeutic applications. Wavelength determines the depth of penetration and primary absorption characteristics, while pulse duration governs the thermal interaction profile and potential for collateral damage. The integration of robust experimental methodologies with advanced computational modeling provides researchers with powerful tools for parameter optimization across diverse applications. As laser technology continues to evolve, sophisticated pulsing schemes and real-time parameter modulation hold significant promise for enhancing treatment efficacy while minimizing adverse effects. This systematic analysis provides researchers with a comprehensive framework for selecting and optimizing these critical parameters based on specific therapeutic objectives and target tissue characteristics.
Accurate thermal prediction is a cornerstone of modern laser-tissue interactions research, directly impacting the efficacy and safety of medical procedures ranging from tumor ablation to dermatological treatments. The selection of an appropriate heat transfer model is critical for simulating these complex biothermal events. For decades, the Pennes Bioheat model has served as the foundational framework for such analyses. However, its limitations in capturing micro-scale effects and fast transient phenomena have prompted the development of more sophisticated theories, notably the Dual-Phase Lag (DPL) model [97] [98]. Within the broader context of laser-tissue research fundamentals, this whitepaper provides an in-depth technical comparison of these predominant models, evaluating their theoretical foundations, predictive accuracy, and appropriate application domains to guide researchers and drug development professionals in optimizing thermal therapies.
The Pennes Bioheat Transfer Model, introduced in 1948, revolutionized bioheat modeling by incorporating the effects of blood perfusion and metabolic heat generation into a relatively simple formulation [99] [100]. Despite its widespread use, the model assumes instantaneous heat propagation, a limitation that becomes particularly significant during short-pulse laser exposures where thermal wave effects dominate. The Dual-Phase Lag model, developed by Tzou, addresses this fundamental limitation by introducing two phase lag times (τq for the heat flux and τT for the temperature gradient) that account for the finite propagation speed of thermal energy and microstructural interactions between tissue and blood vessels [97] [100]. Understanding the relative strengths and limitations of these models is essential for advancing predictive capabilities in thermal treatment planning.
Theoretical Foundations and Model Formulations
Pennes Bioheat Transfer Model
The classical Pennes bioheat equation formulates heat transfer in biological tissues through a diffusion-based approach. Its derivation begins with the conservation of energy applied to a vascularized, finite tissue volume, resulting in a partial differential equation that accounts for key physiological heat sources and sinks [101] [99]. The standard form of the Pennes equation is expressed as:
$$ρt Ct \frac{∂Tt}{∂t} = ∇ · (kt ∇Tt) + ωb ρb Cb (Ta - Tt) + Q{met} + Q{ext}$$
where $ρt$, $Ct$, and $Tt$ represent the density, specific heat, and temperature of tissue, respectively; $kt$ denotes tissue thermal conductivity; $ωb$ is the blood perfusion rate; $ρb$, $Cb$, and $Ta$ are the density, specific heat, and arterial temperature of blood; $Q{met}$ represents metabolic heat generation; and $Q{ext}$ accounts for external heating sources such as laser energy [101] [99].
The model simplifies complex vascular architectures by treating blood perfusion as a spatially homogeneous source/sink term, parameterized through the perfusion rate $ωb$. This formulation assumes that heat exchange between blood and tissue occurs primarily in the microvasculature (capillaries), and that blood enters the tissue volume at arterial temperature $Ta$ and equilibrates instantaneously to the local tissue temperature [101]. While this approach neglects the directional nature of blood flow and specific vascular geometries, it provides a computationally efficient framework that has demonstrated reasonable accuracy for many macroscopic thermal analyses.
Dual-Phase Lag Model
The Dual-Phase Lag model addresses non-Fourier heat conduction behaviors that become significant in microscale heat transfer and ultra-fast thermal processes. It introduces temporal lags between the heat flux vector and the temperature gradient, modifying the classical Fourier law to [97] [98]:
$$q(r, t + τq) = -k ∇T(r, t + τT)$$
where $q$ is the heat flux vector, $τq$ is the phase lag of the heat flux accounting for the finite propagation time of thermal signals, and $τT$ is the phase lag of the temperature gradient representing the microstructural interaction time between tissue and blood vessels. Through Taylor series expansion and substitution into the energy equation, the DPL bioheat equation becomes:
$$∇ · (kt ∇Tt) + τT \frac{∂}{∂t} [∇ · (kt ∇Tt)] = \left(1 + τq \frac{∂}{∂t}\right) \left[ ρt Ct \frac{∂Tt}{∂t} - ωb ρb Cb (Ta - Tt) - Q{met} - Q{ext} \right]$$
The phase lag times $τq$ and $τT$ are critical parameters that introduce wave-like and microstructural interaction effects into the heat transfer formulation. Physically, $τq$ represents the time delay required for heat accumulation before heat flow commences, while $τT$ accounts for the time needed for molecular interactions to establish a temperature gradient [98] [100]. These parameters transform the mathematical character of the governing equation from purely parabolic (Pennes) to hyperbolic or mixed-type, enabling more accurate modeling of thermal wave propagation during short-pulse laser exposures where thermal non-equilibrium effects dominate.
Table 1: Key Parameters in Bioheat Transfer Models
| Parameter | Symbol | Units | Pennes Model | DPL Model | Typical Values in Biological Tissues |
|---|---|---|---|---|---|
| Thermal Conductivity | $k_t$ | W/m·K | Primary mechanism | Primary mechanism | 0.5-0.628 (skin) [99] |
| Tissue Density | $ρ_t$ | kg/m³ | Required | Required | 1000-1005 (skin) [99] |
| Tissue Specific Heat | $C_t$ | J/kg·K | Required | Required | 4187-4200 (skin) [99] |
| Blood Perfusion Rate | $ω_b$ | s⁻¹ | Homogeneous term | Homogeneous term | 0.00187 (general) [99] |
| Metabolic Heat Generation | $Q_{met}$ | W/m³ | Source term | Source term | 1190 (general) [99] |
| Heat Flux Lag Time | $τ_q$ | s | Not applicable | Critical parameter | 0.464-6.825 [100] |
| Temperature Gradient Lag Time | $τ_T$ | s | Not applicable | Critical parameter | 0.464-6.825 [100] |
Comparative Analysis of Predictive Accuracy
Temperature Distribution Predictions
The predictive accuracy of Pennes and DPL models diverges significantly in scenarios involving rapid thermal transients and micro-scale heat transfer. In cardiac laser ablation simulations, the DPL model demonstrates superior capability in capturing the temperature dynamics and lesion formation compared to the classical Fourier-based Pennes model [97]. The higher-order formulation of the DPL model more accurately represents the finite propagation speed of thermal waves, resulting in more realistic predictions of the thermal penetration depth and lesion geometry, particularly during the critical initial seconds of laser exposure.
Research on skin tissue thermomechanical behavior further highlights these differences. The DPL model predicts a more gradual temperature rise with steeper thermal gradients than the Pennes model, significantly affecting the predicted region of thermal damage [98]. This distinction becomes crucial in dermatological laser applications where precise control of thermal damage depth is essential for protecting underlying tissues. The phase lag parameters enable the DPL model to account for the finite time required for thermal energy to transfer between the tissue matrix and blood vessels, a microstructural effect entirely neglected in the Pennes formulation.
Thermal Damage Assessment
The accuracy of thermal damage predictions directly impacts treatment outcomes in laser-based therapies. Comparative studies implementing a three-state cell death model (normal, vulnerable, dead states) reveal substantial differences in predicted ablation zones between the Pennes and DPL formulations [97]. The DPL model consistently predicts more confined thermal damage profiles with sharper transitions between necrotic and healthy tissue, particularly in anisotropic tissues like cardiac muscle where thermal conductivity varies with direction.
Numerical simulations of laser ablation for arrhythmia treatment demonstrate that the classical Pennes model tends to overestimate the lesion size compared to experimental observations, while the DPL model provides more clinically accurate predictions of the irreversible damage boundary [97]. This overprediction by the Pennes model stems from its assumption of instantaneous heat propagation, which does not account for the wave-like behavior of heat transfer at short time scales. The improved correlation of the DPL model with experimental outcomes underscores its value in treatment planning where precision is critical for balancing therapeutic efficacy with tissue preservation.
Table 2: Model Performance Across Key Application Domains
| Application Domain | Pennes Model Performance | DPL Model Performance | Key Differentiating Factors |
|---|---|---|---|
| Continuous Wave Laser Heating | Adequate for macroscopic predictions | Moderately improved accuracy | Blood perfusion dominance reduces model differences |
| Short-Pulse Laser Ablation | Significant overestimation of lesion size | High accuracy in lesion boundary prediction | Thermal wave effects captured by DPL phase lags |
| Skin Tissue Thermal Response | Reasonable for slow heating protocols | Superior for rapid heating and cooling | Microstructural tissue-blood interactions |
| Cardiac Tissue Ablation | Limited accuracy due to anisotropy | Excellent prediction of anisotropic lesion shape | Direction-dependent phase lag effects |
| Thermal Therapy with Large Vessels | Poor accuracy near vasculature | Improved vessel-tissue interaction modeling | Enhanced boundary condition formulation |
Experimental Protocols and Methodologies
Cardiac Laser Ablation Protocol
The comparative evaluation of bioheat models in cardiac tissue requires a standardized experimental and computational framework. A representative protocol involves a three-dimensional computational domain representing cardiac tissue with incorporated rotational anisotropy to mimic the fibrous structure of myocardium [97]. The optical-thermal coupling is implemented through the Optical Diffusion Approximation (ODA) model to describe laser-tissue interaction, with a laser ablation phase of 30 seconds at 3 W power delivery, followed by a 270-second relaxation period to observe thermal dissipation.
Critical to this protocol is the parameterization of cardiac optical properties: absorption coefficient (μa = 30 m⁻¹), scattering coefficient (μs = 1.775×10⁴ m⁻¹), and anisotropy factor (g = 0.964) [97]. The thermal solution incorporates temperature-dependent thermal conductivity (k₀ = 0.518 W/m·K, k₁ = -0.0005 K⁻¹) and specific heat (c₀ = 3017 J/kg·K, c₁ = -0.0042 K⁻¹) to account for tissue property changes during heating. The three-state cell death model parameters include frequency factors and activation energies that transition at the critical 55°C threshold, accurately representing the temperature-dependent kinetics of protein denaturation and cellular necrosis [97].
Multi-Layered Skin Tissue Analysis
For cutaneous applications, a multi-layered skin model (epidermis, dermis, subcutaneous tissue) subjected to repetitive pulsed and continuous laser heating provides a framework for comparing model performance [102]. The experimental protocol incorporates thermomechanical analysis to evaluate not only thermal predictions but also resulting tissue deformation—a critical factor in treatment planning. The laser-tissue interaction follows the selective photothermolysis principle, where pulse duration is matched to the target's thermal relaxation time [25].
The numerical implementation utilizes the finite difference method with implicit schemes to handle the stability requirements of the DPL equations [103] [100]. Spatial discretization must adequately resolve thermal boundary layers near the skin surface and around discrete blood vessels, typically requiring grid spacing of 10-50 μm. Boundary conditions include a ramp-type heat flux on the skin surface to simulate clinical laser exposure protocols, with temperature measurements at multiple depths to validate the predicted thermal profiles [98]. The DPL parameters (τq, τT) are varied within reported physiological ranges (0.464-6.825 seconds) to quantify their influence on the simulated temperature distributions [100].
Diagram 1: Bioheat Model Comparison Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Bioheat Validation Experiments
| Category | Specific Item/Technique | Research Function | Application Context |
|---|---|---|---|
| Computational Tools | FEniCSx Finite Element Library | Solves coupled optical-thermal models | Implementation of DPL and Pennes equations [97] |
| Custom Finite Difference Codes | Handles temperature-dependent parameters | Modeling melting/resolidification in metal films [103] | |
| Experimental Monitoring | Thermocouple Arrays | Direct temperature measurement at multiple depths | Validation of simulated thermal profiles [100] |
| Infrared Thermography | Non-contact surface temperature mapping | Spatial temperature distribution validation [98] | |
| Tissue Phantoms | Agar-based Thermal Phantoms | Simulate tissue optical/thermal properties | Controlled experimental validation [97] |
| Multi-layered Skin Equivalents | Reproduce anatomical structure | Depth-dependent thermal response analysis [102] | |
| Laser Systems | Q-Switched Nd:YAG Lasers | Short-pulse delivery for wave effect studies | DPL model validation under transient conditions [25] |
| Continuous Wave Diode Lasers | Steady-state heating protocols | Pennes model validation [25] | |
| Analysis Software | MATLAB/Python with FDM Toolkit | Numerical solution of DPL equations | Parametric studies of phase lag times [100] |
Diagram 2: Laser-Tissue Interaction and Model Selection Logic
The comparative analysis of Bioheat and Dual-Phase Lag models reveals a nuanced landscape for thermal prediction in laser-tissue interactions. The Pennes model maintains utility for macroscopic analyses with continuous wave lasers or slower thermal processes where its computational efficiency provides practical advantages. However, the DPL model demonstrates superior predictive accuracy for short-pulse laser applications, microscale analyses, and scenarios requiring precise thermal damage assessment in heterogeneous tissues [97] [98]. The incorporation of phase lag times (τq, τT) enables the DPL formulation to capture non-Fourier effects that significantly influence temperature distributions and resulting tissue damage patterns.
Future research should prioritize the experimental determination of phase lag parameters across diverse tissue types and physiological conditions, as these values currently exhibit considerable variability in literature [100]. Additionally, the integration of DPL formulations with advanced optical models and three-state damage kinetics represents a promising path toward comprehensive predictive frameworks for laser-tissue interactions. As laser technologies continue evolving toward shorter pulses and more targeted applications, the adoption of higher-order thermal models like DPL will become increasingly essential for translating computational predictions into safe and effective clinical outcomes.
Clinical Outcome Assessments (COAs) are essential tools in clinical research and medical product development that measure how a patient feels, functions, or survives [104]. These assessments provide critical evidence for evaluating treatment efficacy and safety from multiple perspectives, forming a bridge between clinical data and meaningful patient benefits. Within laser-tissue interactions research, COAs deliver the methodological framework necessary to quantify the therapeutic benefits and safety profiles of laser-based interventions, translating physical laser parameters into clinically meaningful endpoints.
The U.S. Food and Drug Administration (FDA) recognizes four primary types of COAs, each serving distinct purposes in clinical evaluation [105]. Patient-Reported Outcomes (PROs) are collected directly from patients without clinician interpretation, capturing symptoms, functional status, and health-related quality of life. Clinician-Reported Outcomes (ClinROs) rely on clinical judgment and interpretation of observable signs or behaviors. Observer-Reported Outcomes (ObsROs) come from individuals who regularly observe patients (such as parents or caregivers) but lack special medical training. Performance Outcomes (PerfOs) involve standardized tasks completed by patients under controlled conditions, objectively measuring functional performance.
COA Implementation in Clinical Research
Regulatory Framework and Current Guidelines
The regulatory landscape for COAs has evolved significantly, emphasizing patient-focused drug development. In October 2025, the FDA released its final guidance, "Patient-Focused Drug Development: Selecting, Developing, or Modifying Fit-for-Purpose Clinical Outcome Assessments," the third in a four-part series on incorporating patient experience data into medical product development and regulatory decision-making [106]. This guidance provides a roadmap for outcome measurement in clinical trials: understanding the disease or condition; conceptualizing clinical benefits and risk; selecting/developing the outcome measure; and developing a conceptual frame to arrive at a fit-for-purpose COA [106].
Recent trends demonstrate growing regulatory acceptance of COAs. From 2012 to 2022, the proportion of FDA labels incorporating nonmandatory COAs increased from 18.6% to 28.4%, representing a 65.7% increase in the average number of nonmandatory COAs per label [107]. Health Technology Assessment (HTA) bodies in Europe show even higher incorporation rates, with 58.1% of HTAs reporting at least one nonmandatory COA [107]. This trend reflects a shift toward greater patient centricity in both regulatory and reimbursement decisions.
Table 1: COA Utilization Across Clinical Trials (2018-2023 Analysis)
| Domain | Number of Identified COAs | Percentage Distribution | Most Common Specific Measures |
|---|---|---|---|
| Patient-Reported Outcomes (PROs) | 83 | 77% | Short Form-36 (SF-36), Impact of Weight on Quality of Life Lite Clinical Trials [105] |
| Performance Outcomes (PerfOs) | 24 | 22% | 6-minute walk test [105] |
| Composite PRO-ClinRO Measures | 1 | 1% | N/A [105] |
| Digital Health Technologies (DHTs) | 2 | N/A | Wearable fitness trackers [105] |
Table 2: Endpoint Construction from COAs in Clinical Trials
| Endpoint Type | Number of Trials | Percentage of Trials | Most Frequently Measured Domains |
|---|---|---|---|
| Co-primary or Key Secondary | 25 | 34% | Physical function, symptom reduction [105] |
| Secondary or Supportive | 63 | 86% | Health-related quality of life, mental health metrics [105] |
| Exploratory | 8 | 11% | Novel digital biomarkers, emerging symptom clusters [105] |
COA Applications in Laser-Tissue Interactions Research
Efficacy Metrics for Laser Interventions
In laser-tissue interactions research, COAs provide critical efficacy metrics that complement traditional biomedical measurements. The fundamental principle of selective photothermolysis, developed in 1983, dictates that laser energy can be precisely confined to specific tissue targets without affecting surrounding structures [9]. COAs translate these physical interactions into meaningful clinical benefits across multiple domains:
- Dermatologic Applications: PRO measures capture patient-reported improvements in aesthetic appearance, scar quality, pigmentation disorders, and skin texture following laser interventions [34]. The Dermatology Life Quality Index (DLQI) represents a validated PRO measure specifically for dermatologic applications.
- Ophthalmic Applications: PerfOs measure visual acuity, contrast sensitivity, and intraocular pressure following selective laser trabeculoplasty (SLT) for glaucoma or laser capsulotomy [108]. These objective performance measures complement patient-reported visual function.
- Functional Improvements: PerfOs such as the 6-minute walk test objectively quantify functional capacity enhancements following laser-based interventions for various conditions [105].
Safety Profiling Through COAs
Safety assessment in laser-based therapies requires comprehensive capture of adverse events and unintended effects through multiple COA modalities:
- ClinROs for Objective Safety Measures: Trained clinicians document observable adverse effects including blistering, scarring, hypopigmentation, hyperpigmentation, and textural changes using standardized grading scales [9]. These assessments are particularly crucial for establishing safety profiles across different skin types.
- PROs for Patient Experience of Safety: Patients directly report symptoms including pain, discomfort, pruritus, and sensory changes following laser procedures, providing essential data on treatment tolerability [109].
- ObsROs for Special Populations: For pediatric patients or individuals unable to self-report, caregiver observations provide critical safety data regarding behavioral changes, discomfort manifestations, and functional limitations post-intervention.
The growing emphasis on treating diverse skin types has highlighted significant research gaps in laser safety. As noted by Dr. Arielle Kauvar, "When lasers or other kinds of energy devices are first developed, for safety reasons, they're always tested on lighter skin tones. After that, it seems like most of them are tested on Asian skin types; there's a huge literature. The literature and the studies for Brown and Black skin are few and far between" [9]. This disparity underscores the need for more comprehensive safety assessment across diverse populations.
Methodological Framework for COA Implementation
Experimental Design and Workflow
Implementing COAs in laser-tissue interactions research requires systematic experimental design to ensure reliable, valid, and regulatory-grade data collection. The following workflow outlines the key methodological stages:
Diagram 1: COA Implementation Workflow. This diagram outlines the sequential process for implementing Clinical Outcome Assessments in research studies, from initial planning through regulatory application.
Research Reagent Solutions for COA Studies
Table 3: Essential Methodological Components for COA Implementation
| Component | Function | Implementation Examples |
|---|---|---|
| Validated COA Instruments | Ensure measurement reliability, validity, and sensitivity to change | SF-36 for quality of life; DLQI for dermatology-specific impact; Visual Function Questionnaires [105] [107] |
| Electronic Clinical Outcome Assessment (eCOA) Platforms | Standardize data collection, reduce administrative burden, improve data quality | Tablet- or smartphone-based administration with built-in compliance checks and real-time data capture [109] |
| Digital Health Technologies (DHTs) | Capture objective functional and behavioral data in real-world settings | Wearable activity monitors, sensor-based mobility trackers, digital symptom diaries [109] [105] |
| Rater Training Programs | Standardize administration and scoring across sites and clinicians | Certification programs for ClinRO administration; standardized patient interviews for PRO collection [109] |
| Statistical Analysis Plans | Pre-specify analytical methods for COA data to minimize bias | Detailed specifications for handling missing data, multiplicity adjustments, and defining clinically important differences [104] |
Advanced Applications and Future Directions
Digital Health Technologies and Artificial Intelligence
The integration of Digital Health Technologies (DHTs) with traditional COAs represents a transformative advancement in clinical assessment. DHTs including wearable sensors, activity monitors, and smartphone-based applications can continuously capture real-world functional data, providing complementary objective measures to patient-reported experiences [109]. This combination of sensor-based DHTs and eCOA presents clear opportunities for more detailed perspectives on the trial participant's health status and experience, with the added potential to increase engagement and reduce burden [109].
Artificial intelligence applications in COA administration and analysis are rapidly evolving. Current implementations focus on administrative task automation, including document preparation and data management [109]. The C-Path's Clinical Outcome Assessment Program recently highlighted that while human oversight remains necessary when using AI to analyze transcripts or prepare patient-facing documents, more immediate efficiencies can be gained using AI for administrative tasks [109]. Future research directions include natural language processing of unstructured patient narratives and machine learning algorithms for identifying novel response patterns.
Regulatory Strategy and Evidence Planning
Effective COA implementation requires strategic evidence planning throughout the development lifecycle. Stakeholders throughout the drug development lifecycle use patient-centered evidence to answer different questions, and therefore, the evidence needs to be packaged differently to address their specific needs [109]. Regulatory agencies focus on benefit-risk assessment of efficacy and safety of treatments, while health technology assessment agencies are concerned about value and cost-effectiveness of treatments, and different evidence is needed in each case [109].
Strategic evidence generation should begin early in development, with thoughtful planning between outcomes researchers and clinical operation teams being essential to optimizing COA data collection and interpretation [109]. Trial design and plans for interpreting COA data to support COA-based efficacy endpoints need to be planned a priori to maximize the utility and usability of COA data [109]. This approach ensures that COA evidence can be fully leveraged in demonstrating the patient experience with new therapies to inform regulatory, reimbursement, and treatment decisions.
Clinical Outcome Assessments represent a critical methodological framework for evaluating the efficacy and safety of laser-based interventions and other medical technologies. By systematically capturing the patient experience through multiple assessment modalities, COAs provide essential evidence linking technical parameters to clinically meaningful benefits. The evolving regulatory landscape emphasizes fit-for-purpose assessment strategies, with increasing incorporation of digital health technologies and electronic assessment platforms. As laser-tissue interactions research advances to address more complex medical challenges, robust COA implementation will remain fundamental to demonstrating both the therapeutic value and safety profile of these innovative interventions.
Laser technologies have revolutionized medical treatments by enabling precise interactions with biological tissues. The efficacy and safety of these interventions are fundamentally governed by the principles of laser-tissue interactions, which include photothermal, photomechanical, and photochemical effects [25]. The ongoing evolution of laser systems focuses on optimizing these interactions to achieve specific clinical outcomes, particularly by controlling pulse duration, wavelength, and energy delivery parameters [110].
Emerging laser systems are increasingly characterized by their ultrashort pulse durations—moving from nanosecond to picosecond and femtosecond domains—and strategic wavelength selection to target specific tissue chromophores. These advancements aim to maximize therapeutic effects while minimizing collateral damage through enhanced precision and controlled energy deposition [111]. This whitepaper provides a comprehensive technical analysis of current emerging laser technologies, comparing their relative advantages and limitations within a framework of fundamental laser-tissue interaction research.
Fundamental Laser-Tissue Interactions
Laser light can interact with biological tissues through several primary mechanisms that determine the subsequent biological effects. Understanding these interactions is crucial for selecting appropriate laser parameters for specific applications.
Key Interaction Mechanisms
The fundamental interactions between laser light and tissue include:
- Absorption: The transfer of photon energy to the tissue, which is highly dependent on the presence of specific chromophores such as melanin, hemoglobin, and water [25]. The absorption spectra of these chromophores vary significantly across wavelengths, directly influencing penetration depth and therapeutic effect.
- Scattering: The redirection of light within the tissue, which affects the spatial distribution of energy and ultimately determines the treatment volume and depth [25].
- Transmission: The passage of light through tissue without significant interaction, which becomes more relevant for wavelengths within the "therapeutic window" (approximately 650-1350 nm) where absorption is minimal [91].
- Reflection: The rebounding of light from the tissue surface, typically accounting for 4-7% of incident light at perpendicular incidence [25].
The dominant interaction mechanism depends on both laser parameters (wavelength, pulse duration, fluence) and tissue properties (chromophore composition, optical density, structural organization).
Relationship Between Pulse Duration and Tissue Effects
Table 1: Laser-Tissue Interaction Mechanisms Based on Pulse Duration
| Pulse Duration | Primary Interaction | Biological Effects | Representative Applications |
|---|---|---|---|
| Continuous Wave (CW) | Photothermal | Bulk heating, coagulation, hyperthermia | Tissue welding, vascular lesions |
| Long-pulse (ms-μs) | Photothermal | Selective photothermolysis | Hair removal, vascular treatments |
| Short-pulse (ns) | Photomechanical/Photothermal | Cavitation, vaporization, pressure waves | Pigmented lesion treatment, lithotripsy |
| Ultrashort (ps-fs) | Photodisruption, Plasma-induced ablation | Minimal thermal damage, precise cutting | Corneal surgery, precise tissue ablation |
The pulse duration of laser emission significantly influences the dominant tissue interaction mechanism. Continuous wave and long-pulsed lasers primarily produce photothermal effects, where light energy is converted to heat, leading to tissue coagulation, vaporization, or carbonization depending on the achieved temperature [25]. As pulse durations shorten to the nanosecond domain and below, photomechanical effects become increasingly significant. These include pressure wave generation, cavitation, and photodisruption, which can mechanically disrupt tissue structures without substantial thermal damage [112] [110].
The thermal confinement time—the point at which heat diffusion becomes negligible during the laser pulse—is crucial for understanding these effects. For most soft tissues, thermal confinement occurs with pulse durations shorter than approximately 1 microsecond. When pulses are shorter than this threshold, heat diffusion to surrounding tissues is minimized, enabling highly precise ablation with minimal collateral thermal damage [111].
Emerging Laser Modalities and Technical Specifications
Recent advancements in laser technology have focused on specific parameter optimizations to enhance therapeutic outcomes across medical specialties.
High-Intensity Laser Therapy (HILT) with Pulsed Emission
Traditional continuous-wave (CW) high-power lasers have shown effectiveness in deep tissue treatment but often cause significant surface heating, which can limit the deliverable energy to deeper target tissues. Emerging evidence suggests that pulsed wave emission at 1064 nm wavelength can enhance deep tissue penetration while mitigating unwanted thermal effects on superficial structures [113].
A comparative study investigating continuous versus pulsed wave transdermal deep tissue therapy demonstrated that pulsed irradiation with specific parameters (60 W peak power, 2 ms pulse width, 50 Hz frequency, 10% duty cycle) resulted in significantly lower skin surface temperature (42.5°C after 300 s) compared to continuous wave operation, while achieving higher fluence in deep muscle tissue (approximately 4.2 J/cm²) [113]. This enhanced performance is attributed to the photoacoustic component of HILT, where high-peak, short-pulse emission generates pressure waves exceeding 10 kPa in water and approximately 100 kPa in vivo—sufficient to trigger mechanotransduction and cellular differentiation processes [110].
The Pulse Energy Dose (PED) has been proposed as a practical metric for determining whether a laser system exceeds the photomechanical threshold while remaining within the thermoelastic safety regime. True HILT systems are characterized by kilowatt-range peak power, microsecond pulses, high pulse energy (hundreds of mJ/cm² to several J/cm²), and very low duty cycles (<1%) that consistently produce therapeutic pressure waves [110].
Short-Pulsed Lasers for Selective Treatment
Short-pulsed lasers in the nanosecond and picosecond domains represent significant advancements for selective treatment of pigmented tissues and precise ablation.
Nanosecond Lasers for Pigmented Lesions
Nanosecond lasers with 532 nm wavelength are widely used for treating pigmented lesions due to their selective absorption by melanin and pulse durations shorter than the thermal relaxation time of melanosomes (approximately 50-500 ns) [112]. This parameter optimization enables selective photothermolysis of melanin-containing structures while minimizing thermal diffusion to surrounding tissues.
Experimental studies using optical phantoms with uniform melanosome distribution have demonstrated that cavitation bubbles—indicative of melanosome disruption—increase rapidly at a fluence threshold of approximately 1.37 J/cm² and reach saturation at higher fluences [112]. Furthermore, increasing spot size was shown to promote cavitation at greater depths, highlighting the importance of considering both irradiation fluence and spot size for controlling treatment depth in pigmented lesions.
Picosecond Myocardial Ablation
The development of a fully fiber-integrated 2 µm thulium-doped picosecond laser system (1962 nm wavelength, 45 ps pulse width) has demonstrated significant potential for precise myocardial ablation in cardiac applications [111]. This wavelength corresponds with a strong water absorption peak (absorption coefficient of 129.2 cm⁻¹), enabling efficient energy deposition in water-rich myocardial tissue with minimal penetration depth.
Parameter optimization studies using fresh porcine myocardial tissue demonstrated controllable ablation depths up to 0.55 mm and areas up to 4.07 mm², with minimal thermal damage areas of 1.02 mm², by adjusting laser power (1.0-3.0 W) and scanning speed (1-2.5 mm/s) [111]. The picosecond pulse duration, shorter than the thermal relaxation time of myocardial tissue, facilitates rapid energy deposition before significant thermal diffusion occurs, thereby confining thermal effects to a highly localized region.
Femtosecond Laser Systems for Precision Procedures
Femtosecond lasers represent the current frontier in precision laser applications, particularly in ophthalmic surgery. The VisuMax 800 femtosecond laser system (Zeiss), with a pulse frequency of 2 MHz compared to the previous generation's 500 kHz, demonstrates the trend toward faster processing times and enhanced precision [114].
In ophthalmic applications, this technology enables procedures such as Small Incision Lenticule Extraction (SMILE) for vision correction, which offers a minimally invasive alternative to traditional LASIK by creating only a small incision rather than a corneal flap [114]. Clinical studies have shown significantly reduced docking time (46.53 ± 11 seconds versus 68.25 ± 15 seconds) and total surgical time (4.52 ± 2.33 minutes versus 6.22 ± 2.04 minutes) with the second-generation system compared to its predecessor, while maintaining comparable visual outcomes [114].
The precision of femtosecond lasers stems from their ability to confine laser energy through nonlinear absorption processes, enabling tissue disruption at the sub-micron level with minimal collateral damage. This precision has expanded their application beyond ophthalmology to include precise tissue cutting in various surgical specialties.
Comparative Analysis of Laser Technologies
Table 2: Comparative Technical Specifications of Emerging Laser Systems
| Laser Technology | Wavelength (nm) | Pulse Duration | Peak Power | Penetration Depth | Primary Applications |
|---|---|---|---|---|---|
| Pulsed HILT | 1064 | 2 ms | 60 W | Deep tissue (~cm) | Musculoskeletal pain, deep tissue repair |
| Nanosecond (Nd:YAG) | 532 | 50 ns | High (kW-MW) | Superficial-mid (mm) | Pigmented lesions, tattoo removal |
| Picosecond (Tm-doped) | 1962 | 45 ps | High (MW-GW) | Superficial (μm-mm) | Precise myocardial ablation, micromachining |
| Femtosecond (VisuMax) | 1040-1060 | 200-500 fs | Very High (GW-TW) | Precise superficial (μm) | Corneal surgery, precise tissue cutting |
Wavelength-Dependent Tissue Penetration
The penetration depth of laser light in biological tissue is strongly wavelength-dependent due to the absorption spectra of endogenous chromophores. Comparative ex vivo studies of 905 nm and 1064 nm laser light penetration in porcine skin and bovine muscle tissue have demonstrated consistently higher transmittance for 1064 nm light through both tissue types [91]. The most significant differences (up to 5.9%) were observed in the upper 10 mm of tissue, with differences diminishing at greater depths.
This wavelength-dependent penetration profile results from competing absorption characteristics: while absorption by melanin and hemoglobin decreases with increasing wavelength, water absorption is approximately twice as strong at 1064 nm compared to 905 nm [91]. The net effect in skin tissue—which contains significant melanin—generally favors deeper penetration at 1064 nm, though the differences are relatively modest within the therapeutic window.
Advantages and Limitations by Application
Table 3: Application-Based Comparison of Laser Technologies
| Application Domain | Preferred Laser Technology | Key Advantages | Principal Limitations |
|---|---|---|---|
| Deep Tissue Therapy | Pulsed HILT (1064 nm) | Enhanced deep penetration, reduced surface heating, photoacoustic effects | Requires precise parameter control, limited clinical adoption |
| Pigmented Lesions | Nanosecond (532 nm) | Selective melanosome disruption, minimal thermal damage | Risk of hypopigmentation at high fluences, depth control challenges |
| Precise Cardiac Ablation | Picosecond (1962 nm) | Minimal thermal damage, high precision, fiber-deliverable | Limited ablation depth, requires parameter optimization |
| Corneal Surgery | Femtosecond (1040-1060 nm) | Extreme precision, minimal collateral damage, visual outcomes | High cost, significant learning curve, procedure-specific complications |
Deep Tissue Applications
Pulsed high-intensity laser therapy at 1064 nm offers significant advantages for deep tissue applications, particularly in musculoskeletal disorders. The combination of relatively long pulse durations (millisecond domain) and high peak powers enables therapeutic effects at centimeter-level depths while minimizing superficial heating [113] [110]. The addition of photoacoustic effects—pressure waves that propagate beyond optical penetration depths—may further enhance neuromodulatory and tissue regenerative outcomes through mechanotransductive mechanisms [110].
The primary limitation of this approach is the requirement for precise parameter control to maintain pressure waves within the therapeutic window (typically 10-100 kPa) while avoiding potentially damaging pressure levels. Furthermore, the classification of HILT systems remains inconsistent, with some commercially available devices labeled as high-intensity failing to generate sufficient photoacoustic components for mechanotransductive effects [110].
Selective Ablation Applications
Short-pulsed lasers (nanosecond to femtosecond) excel in selective ablation applications but present distinct limitations. Nanosecond lasers effectively target pigmented structures but face challenges in controlling treatment depth, particularly for dermal lesions where visual endpoints like immediate whitening provide subjective guidance [112]. Quantitative studies suggest that both fluence and spot size must be optimized to control the spatial distribution of cavitation events in the tissue depth dimension.
Picosecond myocardial ablation demonstrates exceptional precision with minimal thermal damage but is limited by relatively shallow ablation depths (maximum 0.55 mm in myocardial tissue) [111]. This necessitates multiple passes for larger ablation volumes and requires precise control of scanning parameters.
Femtosecond laser systems in ophthalmology provide unparalleled precision but introduce unique challenges including a significant learning curve, higher complication rates during the initial adoption period (specifically anterior capsule tears in cataract surgery—1.84% for FLACS versus 0.22% for conventional techniques), and substantial equipment costs that impact cost-effectiveness despite clinical advantages [114] [115].
Experimental Methodologies and Protocols
Protocol for Assessing Laser-Tissue Penetration
The evaluation of laser light penetration in biological tissues follows standardized methodologies employing ex vivo tissue models and high-fidelity measurement systems:
Tissue Preparation: Fresh porcine or bovine tissue specimens are sectioned into blocks of varying thickness (typically 2-20 mm) using precise surgical instruments. Tissue thickness is verified using medical ultrasound equipment with measurements at multiple positions to ensure uniformity [91].
Laser Parameter Setting: Lasers are configured to specific parameters (wavelength, pulse duration, repetition rate, fluence) based on the experimental objectives. For comparative studies, multiple wavelengths (e.g., 905 nm and 1064 nm) may be tested while maintaining constant average power [91].
Transmission Measurement: The laser emitter is positioned perpendicular to the tissue surface, with a thermal power sensor placed beneath the specimen to measure transmitted light intensity. Measurements are recorded for each tissue thickness, with empty measurements serving as baseline reference [91].
Data Analysis: Transmittance values are calculated as the ratio of transmitted to incident light intensity. The Beer-Lambert law is applied to determine penetration depth, with corrections for reflection losses at tissue-air interfaces [91].
This methodology enables quantitative comparison of different laser parameters and tissue types, providing critical data for optimizing clinical treatment protocols.
Protocol for Evaluating Ablation Efficiency
The assessment of laser ablation efficiency incorporates multidisciplinary approaches:
Tissue Model Preparation: Fresh myocardial or other target tissue is sectioned into standardized blocks (e.g., 10 × 5 × 5 mm) with careful attention to surface flatness to ensure consistent spot size and energy density [111].
Parameter Optimization: Laser power (1.0-3.0 W for myocardial ablation) and scanning speed (1-2.5 mm/s) are systematically varied while maintaining other parameters constant (spot size, pulse duration, wavelength) [111].
Ablation Assessment: Following laser application, tissues undergo comprehensive analysis including:
- Optical microscopy for ablation morphology dimensions (depth, area)
- Scanning electron microscopy for ultrastructural changes
- Histological staining (H&E, etc.) for thermal damage assessment and tissue structure preservation [111]
Thermal Modeling: Finite element models simulate temperature fields and predict ablation thresholds, enabling correlation between experimental findings and theoretical predictions [111].
This integrated approach facilitates both empirical measurement and theoretical understanding of laser-tissue ablation dynamics.
Research Reagent Solutions and Essential Materials
Table 4: Essential Research Materials for Laser-Tissue Interaction Studies
| Material/Reagent | Specifications | Research Application | Critical Function |
|---|---|---|---|
| Optical Phantoms | Gelatin-based with Intralipid scatterer (2 vol%), melanosome suspension | Simulating tissue optical properties | Provides reproducible experimental environment with controlled optical properties [112] |
| Porcine/Bovine Tissue | Fresh tissue specimens, precise thickness sections (2-20 mm) | Ex vivo penetration and ablation studies | Models human tissue interaction; requires freshness for optical property maintenance [91] |
| Polyvinyl Chloride (PVC) Film | 0.01 mm thickness, medical grade | Laser emitter protection | Minimal beam attenuation (high transmittance) while preventing contamination [35] |
| Thermal Power Sensor | Model 50(150)A-BB-26-PPS or equivalent | Laser power measurement | Quantifies output power and transmission through tissues [91] |
| Beam Profiling Camera | LT665 with BeamGage software | Spatial intensity distribution analysis | Characterizes beam profile, spot size, and intensity distribution [91] |
| Fast Photodiode Sensor | FPD-VIS300 with oscilloscope | Temporal pulse characterization | Records pulse duration, shape, and temporal profile [91] |
Visualization of Laser-Tissue Interaction Mechanisms
Laser-Tissue Interaction Pathways
This diagram illustrates the fundamental relationships between laser parameters, tissue properties, interaction mechanisms, and resulting biological effects—critical considerations for researchers designing laser-based therapies.
Experimental Workflow for Laser-Tissue Studies
This workflow outlines the key methodological phases for conducting rigorous laser-tissue interaction research, from sample preparation through data analysis and theoretical modeling.
Emerging laser technologies demonstrate a clear trend toward optimized parameter combinations that enhance precision while minimizing collateral tissue damage. The strategic selection of wavelength, pulse duration, and energy delivery parameters enables researchers and clinicians to target specific chromophores and control interaction mechanisms for tailored therapeutic outcomes.
The ongoing refinement of pulsed laser systems—from nanosecond to femtosecond domains—continues to expand the possibilities for selective treatments with minimal thermal footprint. Meanwhile, advancements in high-intensity laser therapy with optimized pulsed emission patterns offer new approaches for deep tissue applications through combined photothermal and photoacoustic mechanisms.
Future developments in laser-tissue interactions will likely focus on further personalization of treatment parameters based on individual tissue characteristics, expanded wavelength options targeting novel chromophores, and integration of real-time monitoring technologies to guide parameter adjustment during procedures. These advancements will continue to bridge fundamental research with clinical applications, offering increasingly precise and effective laser-based interventions across medical specialties.
Conclusion
The field of laser-tissue interactions represents a rapidly advancing frontier in biomedical science, bridging fundamental physics with clinical application. The integration of sophisticated computational models with empirical validation has enabled unprecedented precision in therapeutic laser applications across medical specialties. Future directions will focus on intelligent feedback systems, multimodal real-time monitoring, and specialized hardware development to further enhance precision and safety. As computational models become more sophisticated and laser technologies more refined, the potential for personalized, minimally invasive treatments will continue to expand, ultimately transforming conventional surgical approaches and enabling novel therapeutic strategies for complex medical conditions.
References
- 1. A review on time domain diffuse optics: principles and ... [https://link.springer.com/article/10.1007/s40766-025-00067-2]
- 2. Absorption, Thermal Relaxation Time, and Beam ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469200/]
- 3. Absorption, scattering, and penetration [https://www.lasertherapyinstitute.org/post/absorption-scattering-and-penetration]
- 4. Current Concepts of Laser–Oral Tissue Interaction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7558496/]
- 5. Photobiomodulation in biological tissues: Light penetration ... [https://www.sciencedirect.com/science/article/abs/pii/S0143816625000399]
- 6. Measurement of tissue optical properties in the 400 to 700 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11629118/]
- 7. Optical Characterization of Biological Tissues Based on ... [https://www.mdpi.com/2075-4418/12/11/2846]
- 8. Optimizing plasmonic photothermal therapy a numerical ... [https://www.nature.com/articles/s41598-025-95798-x]
- 9. Gaps Remain in Research on Laser, Energy-Based Device ... [https://www.ajmc.com/view/gaps-remain-in-research-on-laser-energy-based-device-safety-for-skin-of-color-arielle-kauvar-md]
- 10. From cold to hot: mechanisms of hyperthermia in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1487296/full]
- 11. The evolution of integrated magnetic hyperthermia and ... [https://pubs.rsc.org/en/content/articlehtml/2025/na/d4na01004c]
- 12. A review on radiofrequency, laser, and microwave ... [https://www.sciencedirect.com/science/article/pii/S2589004223023374]
- 13. Implications and considerations of thermal effects when ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6680146/]
- 14. Understanding Laser-Tissue Interaction – Anderson ... [https://www.johnhoopman.com/laser-anderson-principles/]
- 15. Laser Hair Removal - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK507861/]
- 16. Intense Pulsed Light (IPL) Therapy - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK580525/]
- 17. Mechanisms of Laser-Tissue Interaction: II. Tissue Thermal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4295363/]
- 18. Laser-Tissue Interactions [https://link.springer.com/book/10.1007/978-3-030-11917-1]
- 19. What Is Photoacoustic Imaging [https://www.visualsonics.com/photoacoustics-pa]
- 20. Contrast Agents for Photoacoustic Imaging: A Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9406114/]
- 21. Bubble nucleation and dynamics in acoustic droplet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10517405/]
- 22. Engineering optically triggered droplets for photoacoustic ... [https://opg.optica.org/boe/abstract.cfm?uri=boe-5-12-4417]
- 23. Dynamics characteristics of a laser-induced non-spherical ... [https://www.sciencedirect.com/science/article/abs/pii/S0143816621003626]
- 24. Cascaded Cavitation Bubble Excited by a Train of ... [https://www.mdpi.com/2304-6732/12/9/927]
- 25. LASER-tissue interactions [https://www.sciencedirect.com/science/article/abs/pii/S0738081X05001513]
- 26. The effect of surface roughness on the Er:YAG laser ... [https://www.sciencedirect.com/science/article/pii/S1350417725002378]
- 27. Microbubbles and Nanodrops for photoacoustic tomography [https://www.sciencedirect.com/science/article/abs/pii/S1359029421000480]
- 28. A thermal-FSI framework for optimizing laser treatment ... [https://www.sciencedirect.com/science/article/abs/pii/S0021929025005093]
- 29. A Computational Framework for Multiphysics and ... [https://opg.optica.org/abstract.cfm?uri=boda-2021-DTu3A.4]
- 30. The Key Role of Thermal Relaxation Time on the Improved ... [https://www.mdpi.com/1996-1944/18/15/3524]
- 31. Fractional-order bioheat modeling for enhanced prediction ... [https://ui.adsabs.harvard.edu/abs/2025JTBio.13304287F/abstract]
- 32. A thermal-FSI framework for optimizing laser treatment ... [https://pubmed.ncbi.nlm.nih.gov/41072091/]
- 33. and Low-Level Laser Therapy in Medical Research Articles [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515686/]
- 34. Fundamentals and Laser Safety: Core Principles for ... [https://learn.aslms.org/products/fundamentals-and-laser-safety-core-principles-for-clinical-applications-on-demand-2025]
- 35. Comparison of the light transmission in protecting films ... [https://woundsinternational.com/journal-articles/comparison-of-the-light-transmission-in-protecting-films-used-in-laser-photodynamic-therapy/]
- 36. New laser technology enhances power by controlling light ... [https://news.ssbcrack.com/new-laser-technology-enhances-power-by-controlling-light-modes-individually/]
- 37. Course Medical Laser Tissue Interactions during SPIE ... [https://efomp.org/index.php?r=events/view&id=358]
- 38. ANSI Z136.7 (2025) - Testing and Labeling of Laser ... [https://www.lia.org/store/ansi-z1367-2025-testing-and-labeling-laser-protective-equipment?srsltid=AfmBOopin1NBGJvV_6aE7jXV6V3HbQo4pNrl5mMgcKCnzu0fIJpetCy-]
- 39. Laser-Tissue Interactions: Fundamentals and Applications [https://www.amazon.com/Laser-Tissue-Interactions-Fundamentals-Markolf-Niemz/dp/3030119165]
- 40. Global trends of laser bone ablation: bibliometric analysis ... [https://www.frontiersin.org/journals/surgery/articles/10.3389/fsurg.2025.1461319/full]
- 41. Imaging 1927 nm Fractional Thulium Laser‐Tissue Interactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12264580/]
- 42. A review of optical and thermal eye tissue parameters for ... [https://pubmed.ncbi.nlm.nih.gov/39773849/]
- 43. Laser-Tissue Interactions: Fundamentals and Applications [https://www.barnesandnoble.com/w/laser-tissue-interactions-markolf-h-niemz/1132543414]
- 44. Efficacy analysis of high-intensity laser therapy for post ... [https://www.nature.com/articles/s41598-025-14986-x]
- 45. Light buckets and laser beams [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181550/]
- 46. The Current State of Research in the Field of Photosensitizers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609273/]
- 47. Laser-Tissue Interactions: Fundamentals and Applications [https://scispace.com/papers/laser-tissue-interactions-fundamentals-and-applications-q92aaptbot]
- 48. Tailoring photobiomodulation to enhance tissue regeneration [https://www.sciencedirect.com/science/article/abs/pii/S0142961224001571]
- 49. Effect of Photobiomodulation Therapy in an Experimental ... [https://www.mdpi.com/2313-5786/5/4/33]
- 50. Dosimetric parameters and clinical outcomes of ... [https://pubmed.ncbi.nlm.nih.gov/41091232/]
- 51. Investigation of the effect of photobiomodulation therapy with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497345/]
- 52. Photodynamic therapy photosensitizers and photoactivated ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d4sc05393a]
- 53. Photobiomodulation in fibroblasts: from light to healing ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1675619/full]
- 54. Lost in translation: the valley of death across preclinical and ... [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-019-0050-7]
- 55. Text has minimum contrast[proposed] | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/afw4f7/proposed/]
- 56. From Bench to Bedside: Lessons Learned in Translating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3787906/]
- 57. Bench to Bedside: Translating Science from the Lab ... [https://www.docwirenews.com/post/bench-to-bedside-translating-science-from-the-lab-to-the-clinic]
- 58. Relevant parameters for laser surgery of soft tissue - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10787782/]
- 59. Advanced laser scanning for highly-efficient ablation and ... [https://www.nature.com/articles/s41598-018-35604-z]
- 60. The Influence of the Processing Parameters on the Laser ... [https://www.mdpi.com/2079-4991/12/2/232]
- 61. Theoretical and experimental investigations of angular ... [https://opg.optica.org/oe/abstract.cfm?uri=oe-33-10-21236]
- 62. Multi-objective optimization framework to plan laser ... [https://www.sciencedirect.com/science/article/pii/S0169260725002445]
- 63. Continuous Wave Laser vs Pulsed Laser [https://lasersonly.com/blogs/posts/continuous-wave-laser-vs-pulsed-laser?srsltid=AfmBOop2dmY6KYmyhFq2FS0mhMayadLqkrJ7kDITzHXnrbYxmSH2Dg0A]
- 64. Comparative Analysis of Pulsed and Continuous Wave ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245496/]
- 65. Thermal and Physical Implications of Pulsed Versus ... [https://www.dentalcare.com/en-us/ce-courses/ce394/thermal-and-physical-implications-of-pulsed-versus-continuous-emissions]
- 66. Pulse vs. CW Laser Cleaner: A 2025 Buyer's Guide - Riselaser [https://riselaser.net/pulse-vs-cw-laser-cleaning-machines-the-complete-guide.html]
- 67. Comparison of continuous wave and pulsed wave laser ... [https://www.sciencedirect.com/science/article/abs/pii/S0143816613000134]
- 68. 瘢痕的激光治疗进展- PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11103056/]
- 69. Thermal damage induced changes in optical properties of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515067/]
- 70. Laser irradiation of human skin tissue after gold ... [https://www.nature.com/articles/s41598-025-17459-3]
- 71. Cooling Devices in Laser therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5227072/]
- 72. Enhancing laser therapy procedure through surface ... [https://www.sciencedirect.com/science/article/pii/S0306456525000634]
- 73. 《中国肿瘤防治核心科普知识(2025)》——热疗技术篇 [http://www.caca.org.cn/system/2025/04/08/030136814.shtml]
- 74. From bench to bedside: recent advances and effective ... [https://pubmed.ncbi.nlm.nih.gov/41032096/]
- 75. Real-time monitoring of incision profile during laser surgery ... [https://pubmed.ncbi.nlm.nih.gov/24339173/]
- 76. Real-time monitoring of spinal cord hemodynamics with ... [https://www.frontiersin.org/journals/surgery/articles/10.3389/fsurg.2025.1578420/full]
- 77. Real-time quantification of laser speckle contrast imaging ... [https://link.springer.com/article/10.1007/s00464-024-11076-3]
- 78. Monitoring the changes of spinal artery blood flow (SCBF) ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03291-y]
- 79. Intraoperative Laser Speckle Contrast Imaging For Real- ... [https://www.nature.com/articles/s41598-020-64492-5]
- 80. Quantitative Volumetric Analysis Following Magnetic ... [https://www.sciencedirect.com/science/article/abs/pii/S1878875017320211]
- 81. An Overview of Laser Principle, Laser-Tissue Interaction Mechanisms and Laser Safety Precautions for Medical Laser Users [https://scialert.net/fulltext/?doi=ijp.2011.149.160]
- 82. Porcine skin damage thresholds and histological damage characteristics from 1319-nm laser radiation - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6997579/]
- 83. and Low-Level Laser Therapy in Medical Research Articles [https://pubmed.ncbi.nlm.nih.gov/41089935/]
- 84. Use of Infrared Thermography in Medical Diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10744680/]
- 85. Model development and experimental validation for ... [https://pubmed.ncbi.nlm.nih.gov/26349633/]
- 86. Modeling and in vivo experimental validation of 1064 nm ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2023.1237394/full]
- 87. Presenting a novel model to visualize the interaction ... [https://www.sciencedirect.com/science/article/pii/S030057122500380X]
- 88. Histological Analysis - an overview [https://www.sciencedirect.com/topics/engineering/histological-analysis]
- 89. Histological and Histochemical Methods - Theory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4800257/]
- 90. The Impact of Laser Thermal Effect on Histological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9955047/]
- 91. Comparison of the Penetration Depth of 905 nm and 1064 ... [https://www.mdpi.com/2227-9059/11/5/1355]
- 92. Theoretical and experimental study of laser irradiation in ... [https://www.sciencedirect.com/science/article/abs/pii/S0030401825004377]
- 93. In silico design of blue laser soft tissue vaporization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159099/]
- 94. Effect of dual optical pulse scheme with supra and ... [https://www.nature.com/articles/s41598-025-07902-w]
- 95. Intensity Modulation Effects on Ultrafast Laser Ablation ... [https://www.mdpi.com/2079-4991/15/5/377]
- 96. Threshold fluence and incubation during multi-pulse ... [https://opg.optica.org/oe/abstract.cfm?uri=oe-30-25-44908]
- 97. Higher-order thermal modeling and computational analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12055662/]
- 98. The heat transfer in skin tissues under the general two- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11585752/]
- 99. Bio-Heat Models Revisited: Concepts, Derivations ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2019.00189/full]
- 100. Dual-phase lag model of heat transfer between blood ... [https://www.aimspress.com/article/doi/10.3934/mbe.2021081?viewType=HTML]
- 101. A Generic Bioheat Transfer Thermal Model for a Perfused ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2737815/]
- 102. Bioheat vs. Dual-Phase Lag Model Perspective [https://www.sciencedirect.com/science/article/pii/S2666202725003179]
- 103. Modelling of thin metal film heating using the dual-phase ... [https://www.sciencedirect.com/science/article/pii/S0017931023002417]
- 104. Clinical Outcome Assessments in Regulatory Success [https://www.biomedstat.com/knowledge-base/clinical-outcome-assessments-in-regulatory-success]
- 105. The evaluation of clinical outcomes assessments and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11842654/]
- 106. FDA Presses Forward on Patient-Focused Drug Development ... [https://www.akingump.com/en/insights/blogs/eye-on-fda/fda-presses-forward-on-patient-focused-drug-development-releases-final-guidance-focused-on-fit-for-purpose-clinical-outcome-assessments]
- 107. The Increasing Use of Clinical Outcome Assessments in ... [https://www.sciencedirect.com/science/article/pii/S1098301525023617]
- 108. LP-Laser Tissue Interactions [https://www.aoa.org/affiliate-association-resources/ce-catalog/lp-laser-procedures/lp-laser-tissue-interactions]
- 109. 2025 Clinical Outcome Assessment Program Annual ... [https://c-path.org/2025-clinical-outcome-assessment-program-annual-meeting-recap/]
- 110. A Biophysical Framework for High-Intensity Laser Therapy Based on ... [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.20944/preprints202510.1732.v1]
- 111. Mechanism analysis of 2 µm thulium-doped picosecond ... [https://opg.optica.org/oe/fulltext.cfm?uri=oe-33-5-10419]
- 112. Spatial distribution of light-melanosome interaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125047/]
- 113. Comparative Analysis of Pulsed and Continuous Wave ... [https://pubmed.ncbi.nlm.nih.gov/40384056/]
- 114. Advancements in femtosecond laser technology benefit ... [https://www.ophthalmologytimes.com/view/advancements-in-femtosecond-laser-technology-benefit-surgeons-and-patients]
- 115. The Benefits and Drawbacks of Femtosecond Laser- ... [https://research.sightsavers.org/gap-map/the-benefits-and-drawbacks-of-femtosecond-laser-assisted-cataract-surgery/]