Intracellular Cytokine Staining Flow Cytometry: A Comprehensive Guide from Fundamentals to Clinical Translation
This article provides a comprehensive overview of intracellular cytokine staining (ICS) flow cytometry, a powerful technique for single-cell analysis of immune function.
Intracellular Cytokine Staining Flow Cytometry: A Comprehensive Guide from Fundamentals to Clinical Translation
Abstract
This article provides a comprehensive overview of intracellular cytokine staining (ICS) flow cytometry, a powerful technique for single-cell analysis of immune function. Tailored for researchers and drug development professionals, it covers foundational principles, detailed methodological protocols, and advanced applications in drug discovery and clinical trials. The content also addresses common troubleshooting challenges and offers optimization strategies to enhance assay robustness. Furthermore, it explores validation frameworks and comparative analyses with other immunoassays, providing a complete resource for implementing ICS in translational research and biomarker development.
Unlocking Cellular Secrets: The Core Principles and Power of ICS Flow Cytometry
What is ICS? Defining the Technique for Single-Cell Functional Analysis
Intracellular Cytokine Staining (ICS) is a powerful flow cytometry-based technique that enables researchers to detect cytokine production at the single-cell level. Unlike bulk secretion assays that measure cytokine concentrations in supernatants, ICS provides precise information about the frequency, phenotype, and functional capacity of individual cytokine-producing cells within heterogeneous populations [1] [2]. This method has become indispensable in immunology research, particularly for characterizing T-cell responses in vaccine development, cancer immunotherapy, and autoimmune disease [3] [4].
The fundamental principle behind ICS involves stimulating cells, inhibiting cytokine secretion to cause intracellular accumulation, then using fluorescently-labeled antibodies to detect cytokines within permeabilized cells [1] [5]. This approach allows simultaneous assessment of cytokine production and cell surface markers, providing a comprehensive view of immune cell identity and function [3].
Core Principles and Technical Advantages
Cytokines are signaling proteins crucial for both physiological immune responses and pathological inflammation [1]. ICS captures these transient expressions by using protein transport inhibitors like brefeldin A or monensin during cell stimulation. These compounds disrupt protein secretion by inhibiting Golgi apparatus function, causing cytokines to accumulate inside the cell where they become accessible for antibody staining after permeabilization [1] [5].
Key advantages of ICS include:
- Multiparameter Analysis: Simultaneous detection of multiple cytokines and surface markers [3]
- Precise Identification: Direct correlation of cytokine production with specific cell subsets [1]
- Functional Phenotyping: Identification of polyfunctional T-cells producing multiple cytokines [3]
- High Sensitivity: Detection of rare antigen-specific T-cell populations [4]
Compared to other cytokine detection methods like ELISA or Luminex, ICS provides superior resolution of cellular origins, making it particularly valuable for understanding complex immune responses [1].
Experimental Workflow and Methodologies
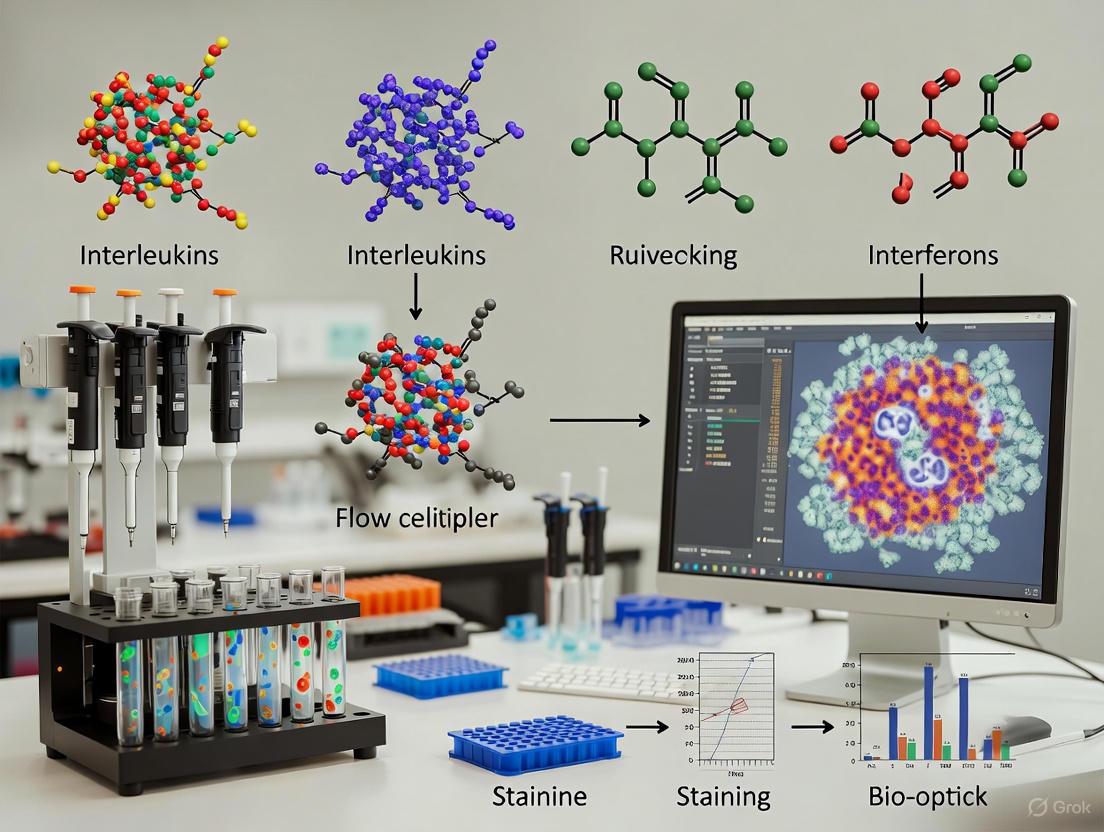
The following diagram illustrates the core ICS workflow, from cell preparation to final analysis:
Detailed Step-by-Step Protocol
1. Cell Preparation and Stimulation
- Source Materials: Use peripheral blood mononuclear cells (PBMC), whole blood, or tissue-derived cells [3] [4]. For tissues, mechanical dissociation followed by enzymatic treatment (e.g., 1 mg/ml collagenase IV) may be necessary [6].
- Stimulation Conditions: Incubate cells (0.5-1×10⁶ cells/mL) with specific antigens (peptide pools, proteins) or mitogens (PMA/ionomycin) [3] [7]. Typical stimulation periods range from 4-12 hours at 37°C [5] [2].
- Secretion Inhibition: Add brefeldin A (GolgiPlug) or monensin at stimulation start (for peptides) or after 2 hours (for proteins requiring processing) [3]. These inhibitors are typically used at 1:1000 dilution [6].
2. Cell Staining and Processing
- Surface Staining: First, stain for surface markers (CD3, CD4, CD8) using fluorescent antibodies in suspension buffer (PBS with 5-10% FCS) for 30 minutes at 4°C [8] [6]. Include viability dye (e.g., Live/Dead Fixable stains) to exclude dead cells [7] [8].
- Fixation and Permeabilization: Fix cells with 1-4% paraformaldehyde for 15-20 minutes on ice [8]. Permeabilize using saponin-based buffers (e.g., BD Cytofix/Cytoperm) or commercial kits for 10-15 minutes at room temperature [3] [8].
- Intracellular Staining: Incubate cells with fluorochrome-conjugated anticytokine antibodies (IFN-γ, IL-2, TNF-α, etc.) for 30 minutes to overnight at 4°C [3] [8].
3. Data Acquisition and Analysis
- Acquire data on a flow cytometer with appropriate laser and filter configurations [3].
- Use single-stain controls for compensation and fluorescence-minus-one (FMO) controls for accurate gating [2].
- Analyze data using sequential gating: exclude doublets and dead cells, gate on lymphocytes, then on specific immune subsets before assessing cytokine production [9].
Critical Reagents and Research Solutions
Table 1: Essential Reagents for Intracellular Cytokine Staining
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Stimulation Agents | PMA/Ionomycin [2], peptide pools [3], SEB [3] | Activates signaling pathways to induce cytokine production; PMA/ionomycin for nonspecific stimulation; antigens for specific responses |
| Secretion Inhibitors | Brefeldin A [5], Monensin [3] | Blocks Golgi-mediated transport causing intracellular cytokine accumulation; choice affects certain markers (e.g., monensin preferred for CD107) [3] |
| Fixation Reagents | Paraformaldehyde (1-4%) [8], commercial fixatives (BD Cytofix) [6] | Preserves cellular structure and crosslinks proteins; concentration affects epitope preservation |
| Permeabilization Detergents | Saponin [8], Triton X-100 [10] | Creates membrane pores allowing antibody access; saponin preferred for cytokine staining while harsher detergents (Triton) improve nuclear antigen access |
| Antibody Panels | Anti-cytokine Abs (IFN-γ, IL-2, TNF-α) [3], surface markers (CD3, CD4, CD8) [7] | Fluorochrome brightness should match antigen abundance (bright dyes for low-expression cytokines) [3] [2] |
| Blocking Reagents | Fc receptor block [7], serum (FBS) [8] | Reduces nonspecific antibody binding; critical for improving signal-to-noise ratio |
Methodological Variations and Optimization
Stimulation Conditions for Different Readouts
Table 2: Optimization Guidelines for Key Cytokines and Markers
| Target | Stimulation Duration | Recommended Secretion Inhibitor | Special Considerations |
|---|---|---|---|
| IFN-γ, TNF-α, IL-2 | 6-12 hours [3] | Brefeldin A [3] | Standard protocol works well for most pro-inflammatory cytokines |
| CD107, CD154 | 5-6 hours [3] | Monensin [3] | Requires adding staining antibodies during stimulation; monensin prevents degradation |
| IL-10, TGF-β | 12-24 hours [3] | Monensin [3] | Serum-free medium recommended for TGF-β to avoid blocking by serum TGF-β |
| Transcription Factors | Varies by target | Combination approach [10] | May require specialized permeabilization (e.g., "Dish Soap Protocol") [10] |
Panel Design and Fluorochrome Selection
Effective multicolor ICS requires careful panel design. The general rule is to match fluorochrome brightness with antigen abundance [3] [2]:
- Bright fluorochromes (PE, Alexa Fluor 647): Best for low-abundance cytokines (IL-2, IL-4) or markers requiring high-resolution sensitivity [3]
- Medium fluorochromes (PE-Cy5, PerCP-Cy5.5): Suitable for intermediate-expression targets (TNF-α, IFN-γ) [3]
- Dim fluorochromes (FITC, Pacific Blue): Appropriate for highly expressed surface markers (CD3, CD4, CD8) [3]
Antibody titration is essential for optimal signal-to-noise ratio, as overstaining increases background while understaining risks missing low-abundance cytokines [2].
Advanced Applications and Current Developments
Research and Clinical Applications
ICS has become a cornerstone technique in multiple research areas:
- Vaccine Development: Measuring antigen-specific T-cell responses to vaccine candidates [1]
- Cancer Immunotherapy: Monitoring functional responses of CAR-T cells and other immunotherapies [1] [4]
- Autoimmune Diseases: Characterizing dysregulated cytokine profiles in pathological inflammation [1]
- Infectious Diseases: Evaluating cellular immunity to pathogens like SARS-CoV-2 [6]
Recent Methodological Innovations
Recent advances have addressed specific technical challenges in ICS:
- "Dish Soap Protocol": A novel approach using commercial dishwashing detergent (Fairy/Dawn) in fixation/permeabilization buffers enables simultaneous detection of transcription factors, cytokines, and fluorescent proteins at significantly reduced cost [10].
- Standardization Initiatives: The Human ImmunoPhenotyping Consortium (HIPC) has developed standardized, lyophilized reagent panels to reduce cross-study variability [9].
- Artifact Recognition: Recent research identified that PMA stimulation can activate neutrophils in crude samples, causing hydrogen peroxide-mediated death of cytokine-producing T cells [6]. This artifact can be mitigated by using antigen-specific stimulation instead of PMA or adding catalase to degrade H₂O₂ [6].
Technical Considerations and Troubleshooting
Common Challenges and Solutions
- High Background: Ensure proper Fc receptor blocking using commercial blockers or serum [5] [8]. Titrate all antibodies to optimize signal-to-noise ratio [2].
- Weak Signal: Verify stimulation efficiency using positive controls (e.g., SEB). Check secretion inhibitor activity and expiration dates [2].
- Poor Cell Viability: Limit stimulation with brefeldin A to 6 hours or less to maintain viability [5]. Process cells gently to prevent mechanical damage [8].
- Compensation Issues: Use single-stain controls with the same antibodies as experimental samples, particularly important for tandem dyes (PE-Cy7, APC-Cy7) prone to degradation [3].
Standardization and Reproducibility
Significant variability in ICS results can occur between laboratories, with one study reporting inter-laboratory coefficients of variation from 17% to 44% [9]. Key strategies to enhance reproducibility include:
- Using lyophilized, pre-configured reagent plates [9]
- Implementing automated gating algorithms to reduce subjective bias [9]
- Maintaining consistent stimulation conditions across experiments [2]
- Detailed record-keeping of reagent lots and protocol deviations [2]
Intracellular Cytokine Staining remains a powerful and evolving technology for single-cell functional analysis in immunology research. When properly optimized and controlled, ICS provides unparalleled insights into the functional status of immune cells, bridging the gap between phenotypic characterization and functional assessment. As standardization improves and new methodologies emerge, ICS continues to be an indispensable tool for both basic immunology and translational research in drug development.
In the field of intracellular cytokine staining (ICS) for flow cytometry, the accurate detection of cytokine-producing cells is paramount for advancing research in immunology, vaccine development, and therapeutic drug monitoring. The foundation of successful ICS lies in the precise and temporal inhibition of protein secretion, a process critically mediated by the Golgi apparatus. Within this context, brefeldin A and monensin have emerged as indispensable pharmacological tools for blocking this secretory pathway, thereby enabling the accumulation of cytokines within the cell for robust detection via flow cytometry. This application note details the mechanistic actions, comparative performance, and optimized implementation of these Golgi-blocking agents, providing researchers and drug development professionals with a structured framework to enhance assay sensitivity and data fidelity in intracellular cytokine staining workflows.
Mechanism of Action: How Golgi-Blocking Agents Work
Disruption of Intracellular Protein Transport
Brefeldin A and monensin disrupt protein transport through distinct yet complementary mechanisms, ultimately preventing cytokine secretion and facilitating their intracellular accumulation.
Brefeldin A initiates a rapid and reversible disassembly of the Golgi apparatus into the endoplasmic reticulum (ER). It specifically inhibits guanine nucleotide exchange factors (GEFs) for ADP-ribosylation factors (ARFs), which are essential for the formation of COPI-coated vesicles. Without functional COPI vesicles, retrograde transport from the Golgi to the ER continues unabated, while anterograde transport from the ER to the Golgi is halted. This leads to a complete fusion of the Golgi with the ER, effectively shutting down the central sorting hub of the secretory pathway [11].
Monensin operates as a carboxylic ionophore that selectively exchanges monovalent cations, such as Na+ and K+, across biological membranes. Within the acidic environment of the Golgi apparatus, this ion exchange disrupts the critical ionic gradients and pH balance required for enzymatic modification (such as glycosylation) and vesicular trafficking. The collapse of the internal Golgi environment inhibits the formation of secretory vesicles destined for the plasma membrane, causing proteins like cytokines to accumulate within the compromised Golgi compartments [12] [11].
Table 1: Comparative Mechanisms of Golgi-Blocking Agents
| Feature | Brefeldin A | Monensin |
|---|---|---|
| Primary Molecular Target | ARF GEFs / COPI vesicle formation [11] | Ionic gradients across Golgi membranes [12] |
| Effect on Golgi Structure | Causes fusion with the Endoplasmic Reticulum [11] | Disrupts internal ionic balance and integrity [13] |
| Primary Site of Action | Interface between ER and Golgi [11] | Medial- and trans-Golgi compartments [12] |
| Reversibility | Reversible upon washout [11] | Largely irreversible [11] |
Visualizing the Mechanism and Workflow
The following diagram illustrates the distinct mechanisms of brefeldin A and monensin within a generalized intracellular cytokine staining workflow, from cell stimulation to flow cytometric analysis.
Diagram 1: Mechanism and workflow of Golgi-blocking agents in ICS.
Comparative Evaluation of Brefeldin A and Monensin
Efficacy and Toxicity Profile
A comparative study specifically evaluated the capacity of monensin and brefeldin A for the flow cytometric determination of interleukin-1 beta (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α) in human monocytes. The findings provide critical quantitative insights for reagent selection [14].
- Cell Viability: The viability of monocytes, as measured by propidium iodide exclusion, was slightly lower in monensin-treated cultures compared to brefeldin A-treated cultures, indicating a potentially higher cytotoxic profile for monensin under the tested conditions [14].
- Spontaneous Cytokine Production: After 8 hours of culture without stimulation, the percentages of IL-6 and TNF-α-producing monocytes were significantly lower in monensin-treated samples than in brefeldin A-treated samples. This suggests brefeldin A may be more effective at trapping constitutively produced cytokines [14].
- Stimulated Cytokine Production: In lipopolysaccharide (LPS)-stimulated monocytes, the measured intracellular production of IL-1β, IL-6, and TNF-α was increased in brefeldin A-inhibited monocytes compared to those treated with monensin. The fluorescence intensity, measured in Molecules of Equivalent Soluble Fluorochrome (MESF) units, was also higher with brefeldin A, pointing to a greater accumulation of cytokines per cell [14].
The study concluded that for the flow cytometric determination of these specific monocytic cytokines, brefeldin A is a more potent, effective, and less toxic inhibitor of cytokine secretion than monensin [14].
Table 2: Quantitative Comparison in Monocyte Cytokine Staining
| Performance Metric | Brefeldin A | Monensin | Experimental Context |
|---|---|---|---|
| Cell Viability | Slightly Higher [14] | Slightly Lower [14] | 8-hour culture, human monocytes [14] |
| Spontaneous IL-6/TNF-α+ Cells | Significanty Higher [14] | Significanty Lower [14] | 8-hour unstimulated culture [14] |
| Stimulated Cytokine MESF | Increased [14] | Lower [14] | LPS-stimulated, 8-hour culture [14] |
| Recommended Use Case | Potent and effective for IL-1β, IL-6, TNF-α [14] | Varies by cytokine and cell type | Human monocytes [14] |
Practical Application and Selection Guide
The choice between brefeldin A and monensin is not universally prescribed but should be optimized for specific experimental systems.
- Optimal Usage: Empirical evidence supports the combined use of brefeldin A and monensin in many ICS protocols to ensure comprehensive inhibition across different cytokine and cell type combinations. This combination leverages the distinct mechanisms of both agents to maximize cytokine retention [11].
- Cell Type Considerations: The superior performance of brefeldin A for cytokines like IL-1β, IL-6, and TNF-α in monocytes is well-documented [14]. However, the optimal inhibitor can vary for other cytokines (e.g., IL-10, IL-12) or in different cell types, such as T lymphocytes. Therefore, inhibitor titration and comparison are recommended during assay development.
- Temporal Considerations: Both inhibitors are typically added concurrently with the stimulating agent. The standard incubation period for stimulation and transport inhibition is 4 to 6 hours, though this should be optimized based on the kinetics of the cytokine of interest [11]. Extended incubation times, particularly beyond 8 hours, may exacerbate the slight toxicity associated with monensin [14].
Detailed Experimental Protocol for Intracellular Cytokine Staining
This protocol provides a step-by-step methodology for detecting cytokine production in immune cells, incorporating the use of Golgi-blocking agents, as synthesized from current resources [12] [11].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for ICS
| Reagent/Material | Function/Description | Example |
|---|---|---|
| Cell Stimulation Cocktail | Activates immune cells to induce cytokine production. Often contains PMA & Ionomycin. | Invitrogen Cell Stimulation Cocktail [12] |
| Brefeldin A Solution | Protein transport inhibitor that disassembles the Golgi apparatus. | eBioscience Brefeldin A [12] |
| Monensin Solution | Protein transport inhibitor that disrupts Golgi ionic balance. | Included in some stimulation cocktails [12] |
| Fixation Buffer | Cross-links proteins and preserves cellular integrity (e.g., 4% PFA). | Commercial fixation/permeabilization kits [11] |
| Permeabilization Buffer | Contains detergents (e.g., saponin) to perforate membranes for antibody access. | Commercial fixation/permeabilization kits [11] |
| Flow Cytometry Staining Buffer | PBS-based buffer with BSA for antibody dilution and washing. | eBioscience Flow Cytometry Staining Buffer [12] |
| Antibody Panel | Fluorochrome-conjugated antibodies against surface markers and cytokines. | User-defined, validated clones |
Step-by-Step Procedure
Cell Preparation and Stimulation:
- Isolate immune cells (e.g., PBMCs from whole blood using Ficoll density gradient centrifugation or from lymphoid tissue by mechanical disruption) and resuspend in complete RPMI 1640 medium at a concentration of 1–3 × 10^6 cells/mL [12] [11].
- Distribute cells into a 96-well round-bottom plate. Add the stimulation cocktail (e.g., 50 ng/mL PMA with 500 ng/mL Ionomycin for polyclonal T-cell activation) to the test wells. Include unstimulated controls (medium only) to measure background cytokine production [11].
- Incubate the plate for 1–2 hours in a humidified 37°C, 5% CO₂ incubator to allow for cell activation and initiation of cytokine transcription [11].
Inhibition of Protein Transport:
- Add protein transport inhibitors to all wells (including unstimulated controls). Final working concentrations are typically 10 µg/mL for brefeldin A and 2 µM for monensin [11]. Many commercial cocktails provide pre-mixed formulations.
- Return the plate to the 37°C incubator and continue the incubation for an additional 4–6 hours (for a total stimulation time of 5–8 hours) to allow for sufficient cytokine production and accumulation [12] [11].
Cell Harvest and Surface Staining:
- After stimulation, centrifuge the plate and wash the cells twice with cold Flow Cytometry Staining Buffer.
- Resuspend the cell pellet in a pre-titrated antibody cocktail against surface markers (e.g., anti-CD3, CD4, CD8) diluted in staining buffer. Include a viability dye to exclude dead cells.
- Incubate for 20–30 minutes at 4°C in the dark [11].
Fixation and Permeabilization:
- Wash the cells twice with staining buffer to remove unbound antibodies.
- Fix the cells by resuspending the pellet in a commercial fixation solution (e.g., 4% paraformaldehyde) and incubate for 20 minutes at room temperature in the dark [11].
- Wash the cells once with staining buffer, then resuspend in a commercial permeabilization buffer. This and all subsequent steps until the final wash require the cells to be maintained in permeabilization buffer to prevent membrane resealing [11].
Intracellular Cytokine Staining:
- Centrifuge the cells and resuspend the pellet in an antibody cocktail against intracellular targets (e.g., IFN-γ, IL-4, TNF-α) diluted in permeabilization buffer.
- Incubate for 30 minutes at room temperature or 4°C in the dark [11].
Data Acquisition and Analysis:
- Perform a final wash with permeabilization buffer, followed by a wash with regular staining buffer.
- Resuspend the cells in an appropriate volume of staining buffer or fixative and acquire data on a flow cytometer.
- Establish a gating strategy that sequentially selects for single cells, viable cells, the lymphocyte population, and specific subsets (e.g., CD3+CD4+ T cells) before finally analyzing cytokine expression. Set positive gates for cytokines using the fluorescence-minus-one (FMO) or unstimulated controls [11].
Brefeldin A and monensin are foundational reagents in the intracellular cytokine staining workflow, enabling high-resolution analysis of immune cell function at the single-cell level. While both agents effectively block the Golgi apparatus, their distinct mechanisms of action lead to differences in efficacy, toxicity, and potential cell-type specificity. The comparative data indicates that brefeldin A may offer superior performance for certain cytokines like IL-1β, IL-6, and TNF-α in monocytes. However, the strategic combination of both inhibitors often provides the most robust solution for comprehensive cytokine detection across heterogeneous cell populations. Adherence to the detailed protocols and quality control measures outlined herein will empower researchers to generate reliable, high-quality data critical for advancing immunology research and therapeutic development.
Intracellular cytokine staining (ICS) is a cornerstone technique for evaluating immune function at the single-cell level. Unlike surface phenotyping or bulk assays, ICS provides direct insight into what immune cells are doing, not just what they look like, by detecting cytokine production within individual cells [2]. This powerful method is particularly invaluable when characterizing T-cell responses, uncovering cytokine production patterns, or tracking immune modulation in disease models and clinical trials, such as those for HIV-1 vaccines [15]. However, the multi-step ICS process can be deceptively tricky, requiring careful execution to generate reproducible, high-quality data. This application note provides a detailed, step-by-step protocol to guide researchers from sample preparation to data analysis.
The following diagram illustrates the complete ICS workflow, from cell stimulation to final data acquisition:
Materials and Reagents
Key Research Reagent Solutions
The following table details essential reagents and their critical functions in the ICS protocol:
| Reagent Category | Specific Examples | Function in ICS Protocol |
|---|---|---|
| Stimulation Agents | Peptide pools (e.g., HIV-1 PTE), PMA/lonomycin, anti-CD3/CD28 antibodies | Activate T-cells to trigger intracellular cytokine synthesis [2] [15]. |
| Secretion Inhibitors | Brefeldin A, Monensin | Disrupt Golgi apparatus to trap cytokines inside the cell for detection [2]. |
| Viability Marker | Live/Dead Fixable Violet/Blue/Green Stains | Distinguish live from dead cells to exclude false-positive events from analysis [15]. |
| Surface Stain Antibodies | Fluorochrome-conjugated mAbs against CD3, CD4, CD8 | Identify specific cell lineages (e.g., T-helper cells, cytotoxic T-cells) before fixation [2]. |
| Fixation & Permeabilization Buffers | Paraformaldehyde-based fixative (e.g., FACSLyse), saponin-based perm buffer (e.g., FACSPerm) | Stabilize cell structure and create pores in the membrane for intracellular antibody access [2] [15]. |
| Intracellular Antibodies | Fluorochrome-conjugated mAbs against cytokines (IFN-γ, IL-2, TNF-α, IL-4) | Detect and quantify the cytokine proteins produced by the stimulated cells [2] [15]. |
Step-by-Step Experimental Protocol
Cell Stimulation
Purpose: To activate T-cells and initiate cytokine production.
- Use previously frozen PBMCs that have been thawed and rested overnight [15].
- Stimulate cells for 6 hours using the appropriate stimulus [2].
- For antigen-specific responses, use peptide pools (e.g., 15-amino acid peptides based on global PTE for HIV-1) [15].
- For a positive control, use the superantigen Staphylococcal Enterotoxin B (SEB) or PMA/lonomycin [2] [15].
- Always include an unstimulated control (no stimulant) to establish baseline cytokine levels [2].
Blocking Cytokine Secretion
Purpose: To trap synthesized cytokines within the cell for subsequent detection.
- Add brefeldin A or monensin at the start of the stimulation period [2].
- These inhibitors disrupt protein transport through the Golgi apparatus, preventing cytokine release into the supernatant and allowing intracellular accumulation [2].
Cell Staining
A. Surface Staining
- Perform surface staining before fixation, especially for fixation-sensitive epitopes (e.g., CCR7, CD62L) [2].
- Stain with fluorochrome-conjugated antibodies against surface markers (e.g., CD3, CD4, CD8) and a viability dye to exclude dead cells [15].
B. Fixation and Permeabilization
- Fix cells with paraformaldehyde-based fixative (e.g., FACSLyse) to stabilize cell structure and cross-link proteins [15].
- Permeabilize cells with saponin-based buffers (e.g., FACSPerm) to dissolve cholesterol in membranes, allowing intracellular antibodies to enter [2] [15].
C. Intracellular Staining
- Stain fixed and permeabilized cells with fluorochrome-conjugated antibodies against intracellular cytokines (e.g., IFN-γ, TNF-α, IL-2, IL-17A) [2] [15].
- Critical: Antibody titration is essential. Overstaining increases background, while understaining risks missing low-expressing cells [2].
Data Acquisition on a Flow Cytometer
- Acquire samples on a flow cytometer equipped with multiple lasers (e.g., a 4-laser BD LSR II) [15].
- Before acquisition, standardize the instrument using rainbow calibration beads to ensure consistent PMT voltages and laser alignment across experiments [15].
- Use a High Throughput Sampler (HTS) for processing 96-well plates to increase efficiency and standardization [15].
Data Analysis and Gating Strategy
Essential Controls for Reliable Data
The integrity of ICS data hinges on the inclusion of proper controls, which help distinguish real biological signals from background and technical artifacts.
| Control Type | Purpose | Essential for |
|---|---|---|
| Unstimulated Control | Reveals baseline cytokine levels and sets a true negative population for gating [2]. | Defining positive events for low-frequency responses. |
| Single-Stained Controls | Used to calculate compensation and correct for fluorescence spillover between channels [2]. | Accurate multi-color fluorescence measurement. |
| FMO (Fluorescence Minus One) Controls | Help set gates for dim cytokine signals, especially in complex multi-color panels [2]. | Correct gating strategy and boundary placement. |
Gating Hierarchy for Data Analysis
A sequential gating strategy is required to accurately identify the rare population of cytokine-producing T cells. The following diagram outlines the standard gating logic:
- Exclude Doublets and Dead Cells: Begin by gating on single cells using FSC-A versus FSC-H to exclude cell aggregates ("doublets") [16]. Next, gate on viability dye-negative cells to exclude dead cells, which often cause nonspecific antibody binding [2].
- Identify Lymphocytes: Gate on the lymphocyte population based on forward scatter (FSC, indicating cell size) and side scatter (SSC, indicating cell granularity) properties [16] [15].
- Define T-Cell Lineage: Within lymphocytes, select CD3+ T cells. Further subset into helper T cells (CD3+CD4+) or cytotoxic T cells (CD3+CD8+) [15].
- Quantify Cytokine-Positive Cells: Finally, identify the percentage of cytokine-positive cells within the CD4+ or CD8+ parent populations [16] [15]. Use FMO controls to accurately set the positive gate, especially for dim cytokines.
Quantitative Data Interpretation
The percentage of cytokine-positive cells is calculated based on the gating hierarchy. If you analyze a subpopulation, you must back-calculate to the total population. For example, if 30.1% of the total cells are neutrophils, and 14.5% of those neutrophils express IL-17a, then the percentage of IL-17a-expressing neutrophils in the total sample is 4.36% (30.1 × 0.145) [16].
Troubleshooting and Best Practices
Panel Design for High-Quality Results
- Match Fluorophore Brightness to Antigen Abundance: Use bright fluorophores (e.g., PE, APC) for low-expression cytokines and dimmer dyes for highly expressed surface markers (e.g., CD4, CD8) [2].
- Validate Reagents: Use antibodies and buffers confirmed to work in ICS applications. Some antibody clones do not recognize their epitopes after fixation/permeabilization [2].
- Standardize Workflows: Maintain consistent stimulation times, temperatures, and reagent concentrations across all samples and experiments to minimize variability [2].
Gating Recommendations
- Avoid Overly Tight Gates: Narrow gates can exclude real biological populations. Use FMO controls to guide gate boundaries objectively [2].
- Use Back-Gating: Confirm that cytokine-positive events fall within your intended parent population (e.g., CD3+CD4+) to verify population identity [2].
- Apply Consistent Gating Hierarchy: Use the same gating logic and positioning across all samples in a dataset to reduce subjective bias and improve comparability [2].
When performed meticulously, intracellular cytokine staining is a powerful technique that provides unparalleled insight into immune cell function. By following this standardized protocol—paying close attention to stimulation conditions, reagent validation, proper controls, and a consistent gating strategy—researchers can generate reliable, high-quality data. This enables robust profiling of immune responses in contexts ranging from basic immunology research to clinical trials for vaccines and therapeutics [2] [15].
Why Choose ICS? Key Advantages over ELISA and ELISpot Assays
Intracellular Cytokine Staining (ICS) coupled with flow cytometry represents a powerful methodology for deep immune profiling at the single-cell level. Within the context of advanced thesis research on cellular immune responses, ICS provides unique advantages that complement and, in specific applications, surpass other established techniques like the Enzyme-Linked Immunosorbent Assay (ELISA) and the Enzyme-Linked Immunospot (ELISpot) assay. While ELISA quantifies soluble analyte concentrations in supernatants and ELISpot enumerates analyte-secreting cells, ICS allows for the simultaneous detection of intracellular cytokine production and definitive cell surface marker expression, enabling precise phenotypic characterization of antigen-responsive lymphocyte subsets [17] [18] [19]. This application note details the key advantages of ICS, provides a direct quantitative comparison with other methods, and outlines a detailed protocol for its implementation in research and drug development.
Comparative Analysis of Immunological Assays
The choice between ELISA, ELISpot, and ICS is dictated by the specific research question. The table below summarizes the core characteristics of each technique.
Table 1: Key Characteristics of ELISA, ELISpot, and ICS Assays
| Feature | ELISA | ELISpot | ICS |
|---|---|---|---|
| What is Detected | Soluble proteins (e.g., cytokines, antibodies) in a liquid sample [17] [18] | Number of individual cells actively secreting a target protein [17] [18] | Intracellular cytokines and cell surface markers [20] [19] |
| Sample Type | Serum, plasma, cell culture supernatant [17] [18] | Live cells (e.g., PBMCs) [18] [21] | Live cells (e.g., PBMCs, whole blood) [20] |
| Sensitivity | Moderate to High [17] [18] | Very High (can detect 1 in 1,000,000 cells) [19] [22] | Lower than ELISpot (detection limit ~0.02%) [19] |
| Resolution | Bulk population measurement [18] | Single-cell (secretory activity) [18] [22] | Single-cell (phenotype and function) [19] |
| Key Output | Total protein concentration (e.g., pg/mL) [17] [18] | Frequency of secreting cells (SFU/million cells) [20] [18] | Percentage of cytokine-positive cells within defined subsets (e.g., CD4+, CD8+) [20] [23] |
| Phenotyping Capacity | No | No | Yes (Multiparameter flow cytometry) [23] [19] |
| Throughput | High (easily automated) [18] [21] | Moderate (manual cell handling) [18] [21] | Moderate (dependent on flow cytometer capacity) |
Quantitative Data from Comparative Studies
Direct comparisons between these assays highlight their performance differences. A 2022 study comparing ICS and ELISpot for evaluating T-cell responses to SARS-CoV-2 found that ELISpot was more sensitive for detection. In paucisymptomatic COVID-19 patients, only 44% showed a positive T-cell response with ICS, whereas 67% were positive with ELISpot [20] [24]. The magnitude of responses was also low, with ICS detecting a median of 0.12% cytokine-positive T cells, and ELISpot detecting a median of 61 Spot-Forming Cells (SFCs) per million PBMCs [20]. An earlier comparative study on HIV and CMV responses noted that while results between ELISpot and ICS correlated well, the two assays have distinct strengths and weaknesses, with ICS providing superior immunophenotyping capabilities [23].
Key Advantages of Intracellular Cytokine Staining
The principal strengths of ICS make it an indispensable tool for mechanistic immunology studies and high-resolution immune monitoring.
- Multiparameter Phenotyping: The most significant advantage of ICS is the ability to concurrently identify the cytokine profile and the lineage of the responding cell. By using antibodies against cell surface markers (e.g., CD3, CD4, CD8, CD45RA, CCR7) and intracellular cytokines (e.g., IFN-γ, IL-2, TNF-α), researchers can identify whether a response is primarily driven by CD4+ T-helper cells, CD8+ cytotoxic T cells, or specific memory subsets (e.g., central memory, effector memory) [20] [23]. This is crucial for understanding the quality of an immune response.
- Functional Analysis of Complex Populations: ICS allows for the deep functional characterization of rare cell populations. It can be used to profile T-cell polyfunctionality—the ability of a single cell to produce multiple cytokines simultaneously (e.g., IFN-γ⁺IL-2⁺TNF-α⁺), which is often a correlate of potent, protective immunity in viral infections and vaccine responses.
- Direct Correlation of Phenotype and Function: Unlike ELISpot, which requires cell separation for phenotyping, ICS directly links a cell's identity with its functional capacity in a single assay [19]. This provides a more integrated view of the immune response without the need for inferential data from separate experiments.
Detailed ICS Protocol for the Evaluation of Antigen-Specific T Cells
The following protocol is adapted from methodologies described in the search results and standardizes the process for evaluating human T-cell responses to viral antigens, such as SARS-CoV-2 [20].
Research Reagent Solutions and Materials
Table 2: Essential Reagents and Materials for ICS
| Item | Function/Description |
|---|---|
| Heparinized Blood or PBMCs | Source of lymphocytes; PBMCs are isolated via Ficoll density gradient centrifugation [20]. |
| Peptide Pools | Overlapping 15-mer peptides spanning antigens of interest (e.g., SARS-CoV-2 spike protein) to stimulate T cells [20] [23]. |
| Cell Stimulation Cocktail | Brefeldin A (BFA) or Monensin: Added to culture to inhibit protein transport, thereby accumulating cytokines intracellularly [20]. |
| Flow Cytometry Antibodies | Fluorochrome-conjugated antibodies against surface markers (CD3, CD4, CD8) and intracellular cytokines (IFN-γ, IL-2, etc.) [20]. |
| Fixation/Permeabilization Buffer | Reagents to fix cells and permeabilize membranes, allowing intracellular staining [20]. |
| Flow Cytometer | Instrument for acquiring and analyzing the multi-parameter data. |
Step-by-Step Experimental Workflow
Step 1: Cell Preparation and Stimulation
- Isolate PBMCs from fresh heparinized blood using Ficoll density gradient centrifugation. Cryopreserved PBMCs can be used after proper thawing and resting for at least 4 hours in complete RPMI medium at 37°C [20].
- Plate 0.5-1 x 10⁶ PBMCs per well in a 96-well U-bottom plate. Centrifuge and resuspend cells in stimulation media.
- Stimulate cells with peptide pools (e.g., 1 µg/mL per peptide) [20]. Include controls:
- Negative Control: DMSO or media alone.
- Positive Control: A strong polyclonal stimulator like phytohaemagglutinin (PHA) or anti-CD3/CD28 antibodies.
- Add Brefeldin A (e.g., 10 µg/mL) after the first hour of stimulation to block cytokine secretion [20].
- Incubate cells for 18 hours at 37°C, 5% CO₂ [20].
Step 2: Cell Surface Staining
- After stimulation, transfer cells to a FACS tube and wash with cold PBS or FACS buffer.
- Resuspend the cell pellet and stain with surface marker antibodies (e.g., anti-CD3, CD4, CD8) for 20-30 minutes at 4°C in the dark.
- Wash cells to remove unbound antibody.
Step 3: Intracellular Staining
- Fix and permeabilize cells using a commercial fixation/permeabilization kit according to the manufacturer's instructions.
- Centrifuge and resuspend the fixed/permeabilized cells in permeabilization buffer containing fluorochrome-conjugated antibodies against intracellular cytokines (e.g., anti-IFN-γ, IL-2).
- Incubate for 30-60 minutes at 4°C in the dark.
- Wash cells with permeabilization buffer, then resuspend in FACS buffer for acquisition.
Step 4: Flow Cytometry Acquisition and Analysis
- Acquire data on a flow cytometer, collecting a minimum of 100,000 lymphocyte events per sample [20].
- Analyze data using flow cytometry software (e.g., Kaluza, FlowJo).
- Identify lymphocytes by forward and side scatter, then gate on singlets.
- Gate on T-cell populations (e.g., CD3⁺CD4⁺ or CD3⁺CD8⁺).
- The frequency of antigen-specific T cells is determined by the percentage of cytokine-positive cells within the gated population after subtracting the background from the negative control.
Diagram 1: ICS staining workflow.
The choice of an immunological assay should be driven by the specific research goals. For the straightforward quantification of total cytokine output, ELISA remains a robust and high-throughput option. For the highly sensitive enumeration of rare, antigen-specific, cytokine-secreting cells, ELISpot is the superior tool [20] [22]. However, when the research objective requires a deep, mechanistic understanding of the immune response—specifically, the precise identification of which cell subsets are responding and their functional potential—Intracellular Cytokine Staining (ICS) is the unequivocal method of choice. Its capacity for multiparameter phenotyping and functional analysis at the single-cell level makes it an essential technique in the modern immunologist's toolkit for advanced thesis research, vaccine development, and therapeutic drug monitoring.
Intracellular cytokine staining (ICS) combined with flow cytometry is a powerful methodology for assessing T-cell immune responses at the single-cell level. Unlike alternative approaches such as enzyme-linked immunospot (ELISpot) or ELISA, ICS enables the simultaneous assessment of multiple phenotypic, differentiation, and functional parameters of responding T-cells, most notably the expression of multiple effector cytokines [25]. This technique provides critical insights into T helper cell polarization, effector function, and therapeutic response monitoring by capturing transient cytokine expression patterns within heterogeneous immune cell populations [26]. For researchers in vaccine development and immunotherapeutic drug discovery, establishing a robust ICS toolkit is essential for generating reliable, high-resolution data on immune cell functional heterogeneity.
The ICS workflow consists of multiple interdependent stages, each requiring specific hardware and reagent solutions. The fundamental process involves cell stimulation to activate cytokine production, blockade of protein transport to accumulate cytokines intracellularly, cell fixation and permeabilization to allow antibody access, and finally, staining with fluorophore-conjugated antibodies for flow cytometric detection [2]. Understanding the requirements at each stage is crucial for establishing a successful ICS platform capable of generating publication-quality data.
Essential Hardware and Instrumentation
Core Laboratory Equipment
A properly equipped laboratory is fundamental for implementing reliable ICS protocols. The necessary equipment spans cell culture, sample processing, and analytical instrumentation.
Table 1: Essential Hardware for ICS Workflows
| Equipment Category | Specific Instruments | Key Specifications |
|---|---|---|
| Cell Culture Equipment | CO₂ incubator, Biological safety cabinet, Inverted microscope | 37°C, 5% CO₂, humidified environment; Cell viability assessment >90% |
| Sample Processing | Refrigerated centrifuge with plate carriers, Multichannel pipettes, Vortex mixer | 400-600 × g force; 8- and 12-channel pipettes for high-throughput |
| Flow Cytometry | Flow cytometer with multiple lasers, Cell strainer caps | 15+ color capability; Appropriate laser/filter configurations |
| Support Equipment | Timer with multiple alarms, Water bath, -80°C freezer | Precise incubation timing; Reagent pre-warming; Cryopreservation |
The flow cytometer represents the most critical analytical instrument, with modern multi-parameter instruments increasingly allowing for the measurement of simultaneous expression of numerous markers [25]. For cytokine detection where positive populations may represent 0.1% of events or less, instruments with sensitive detection systems and appropriate laser configurations are essential [25]. The availability of multiple lasers (blue, red, violet, UV) and filter sets dictates the complexity of antibody panels that can be implemented.
Workflow Visualization
The following diagram illustrates the complete ICS workflow, from sample preparation to data analysis:
Critical Reagents and Their Functions
Core Reagent Solutions
Successful implementation of ICS requires carefully selected reagents at each process stage. The specific formulation of these reagents significantly impacts assay sensitivity and reproducibility.
Table 2: Essential ICS Reagents and Their Functions
| Reagent Category | Specific Examples | Function | Technical Considerations |
|---|---|---|---|
| Stimulation Reagents | PMA (5-50 ng/mL), Ionomycin (250-500 ng/mL), Antigen-specific peptides, Anti-CD3/CD28 antibodies | Activates intracellular signaling pathways to induce cytokine gene expression | PMA/ionomycin causes CD4 downregulation; Concentration optimization required |
| Protein Transport Inhibitors | Brefeldin A (10 μg/mL), Monensin (2 μM), Commercial cocktails (GolgiPlug, GolgiStop) | Disrupts Golgi apparatus function causing intracellular cytokine accumulation | Brefeldin A may decrease CD14 staining; Limit exposure to 4-6 hours |
| Fixation Reagents | Paraformaldehyde (2-4%), Commercial fixation buffers (Intracellular Fixation Buffer) | Crosslinks proteins to preserve cellular structure and prevent cytokine leakage | Standardized fixation time (20-60 min) critical for consistency |
| Permeabilization Reagents | Saponin (0.1-0.5%), Commercial permeabilization buffers, "Dish soap" formulations | Creates pores in membrane allowing antibody access to intracellular targets | Continuous presence required during intracellular staining steps |
| Staining Antibodies | Anti-cytokine mAbs (IFN-γ, TNF-α, IL-2, IL-4, etc.), Surface marker mAbs (CD3, CD4, CD8), Isotype controls | Specific detection of cellular markers and intracellular cytokines | Titration required; Match fluorophore brightness to antigen abundance |
Recent innovations in permeabilization solutions include cost-effective alternatives such as "Burton's Better Buffer," which utilizes dishwashing detergent (Fairy/Dawn) to achieve simultaneous efficient detection of transcription factors, cytokines, and endogenous fluorescent proteins [10]. This formulation (2% formaldehyde with 0.05% Fairy and 0.5% Tween) provides a 100-fold cost reduction compared to commercial buffers while maintaining performance for most intracellular staining protocols other than phospho-flow [10].
Research Reagent Solutions
The selection of appropriate reagent systems depends on the specific intracellular targets and experimental requirements. The following table outlines specialized solutions for different applications:
Table 3: Research Reagent Solutions for Specific Applications
| Application Target | Recommended Buffer System | Key Components | Optimal Use Cases |
|---|---|---|---|
| Cytokines/Chemokines | Intracellular Fixation & Permeabilization Buffer Set | Formaldehyde fixation, saponin-based permeabilization | Cytoplasmic proteins, secreted proteins following activation |
| Transcription Factors | Foxp3/Transcription Factor Staining Buffer Set | Combined fixation/permeabilization in single step | Nuclear antigens, transcription factor detection |
| Phospho-Signaling Proteins | Fixation/Methanol Protocol | Formaldehyde fixation, methanol permeabilization | Phosphorylated signaling molecules (MAPK, STAT proteins) |
| Multiparameter Applications | "Dish Soap Protocol" (Burton's Better Buffer) | Formaldehyde with Fairy detergent and Tween-20 | Simultaneous detection of cytokines, transcription factors, fluorescent proteins |
Experimental Protocols
Standardized ICS Protocol
The following detailed protocol provides a robust methodology for detecting cytokine production in individual cells using flow cytometry, with an estimated duration of 6.5 hours and cost of approximately $675 USD for 20 samples with controls [26].
Step 1: Cell Preparation and Stimulation Isolate immune cells (PBMCs, splenocytes, or tissue-derived lymphocytes) and adjust concentration to 1-2 × 10⁶ cells/mL in complete culture medium. Verify cell viability exceeds 90% using trypan blue exclusion. Distribute cells into 96-well round-bottom plates with 200 μL cell suspension per well. Add stimulation cocktails at optimized concentrations: 50 ng/mL PMA and 500 ng/mL ionomycin for polyclonal activation, or antigen-specific concentrations determined through dose-response experiments. Include unstimulated controls and single-stimulus controls. Incubate plates in CO₂ incubator at 37°C for 1-2 hours to allow initial cellular activation [26].
Step 2: Protein Transport Inhibition Add protein transport inhibitors including brefeldin A (10 μg/mL) and monensin (2 μM) to all wells. These inhibitors block Golgi apparatus function and endoplasmic reticulum transport, causing cytokines to accumulate within producing cells rather than being released into culture medium. Continue incubation for additional 4-6 hours depending on cytokine kinetics, with most cytokines requiring 4-5 hours total stimulation time for optimal detection. Monitor incubation timing precisely as extended culture can lead to cell death and reduced cytokine detection [26].
Step 3: Surface Staining Transfer stimulated cells to fresh 96-well plates and wash twice with cold staining buffer. Add surface marker antibodies including lineage markers (CD3, CD4, CD8) and activation markers (CD69, CD25) diluted in staining buffer. Include viability dyes to exclude dead cells from analysis. Incubate for 20 minutes at 4°C in darkness. Wash cells twice with staining buffer to remove unbound surface antibodies [26].
Step 4: Fixation and Permeabilization Add fixation solution (commercial IC Fixation Buffer or 4% paraformaldehyde) to cells and incubate for 20 minutes at room temperature. Wash cells once with staining buffer, then add permeabilization buffer (commercial buffer or 0.1% saponin). Maintain cells in permeabilization buffer throughout intracellular staining to prevent membrane resealing [27] [26].
Step 5: Intracellular Cytokine Staining Add intracellular cytokine antibodies diluted in permeabilization buffer. Include multiple cytokines of interest such as IFN-γ, TNF-α, IL-2, IL-4, IL-17 based on expected T helper cell responses. Use isotype control antibodies to assess non-specific binding. Incubate for 30 minutes at room temperature or 4°C. Protect samples from light during incubation [26].
Step 6: Sample Acquisition Wash cells three times with permeabilization buffer, followed by one wash with regular staining buffer. Resuspend cells in appropriate volume of staining buffer (200-300 μL) for immediate analysis. Store samples at 4°C in darkness if analysis cannot be performed immediately, but analyze within 24 hours for optimal signal preservation [26].
Sample Processing Decision Framework
The choice of sample material represents a critical early decision in experimental design. The following diagram outlines the decision process for selecting appropriate sample processing methods:
Quality Control and Troubleshooting
Essential Experimental Controls
Implementing appropriate controls is fundamental for generating reliable ICS data. The required controls help distinguish real signals from background and ensure accurate data interpretation.
- Unstimulated Control: Reveals baseline cytokine levels and sets a true negative population for gating [2]. This control identifies cells with non-specific activation from handling or contamination.
- Single-Stained Controls: Required for proper compensation between fluorophores in multicolor panels [2]. Prepare using compensation beads or cells stained with single antibodies identical to experimental samples.
- FMO (Fluorescence Minus One) Controls: Help set gates for dim cytokine signals, especially in complex panels [2]. These controls contain all antibodies except one, identifying spreading error and background.
- Biological Positive Control: A donor sample with known response helps troubleshoot variability across experiments [2]. Typically uses strong polyclonal activators like PMA/ionomycin.
Troubleshooting Common Challenges
Even with optimized protocols, researchers may encounter technical challenges that affect data quality.
Low Cytokine Signal Detection Insufficient cytokine detection may result from suboptimal stimulation conditions, inadequate protein transport inhibition, or antibody performance issues [26]. Optimize stimulation duration and concentration through time-course and dose-response experiments. Verify protein transport inhibitor activity and consider combining brefeldin A with monensin for enhanced retention of certain cytokines. Test antibody performance using known positive controls and consider alternative clones or fluorophore conjugates if signals remain weak.
High Background in Unstimulated Controls Elevated background cytokine signals may indicate cellular activation during processing, contamination, or non-specific antibody binding [26]. Minimize cell handling time and maintain samples at 4°C when possible. Verify culture medium quality and replace if bacterial contamination is suspected. Optimize antibody concentrations through titration experiments and include additional wash steps to reduce non-specific binding.
Poor Cell Viability After Stimulation Reduced cell viability may result from toxic stimulation conditions, extended culture times, or inappropriate culture conditions [26]. Optimize stimulation conditions using viability assessments at multiple time points. Verify CO₂ incubator conditions including temperature, humidity, and gas concentrations. Consider using alternative stimulation protocols or reducing stimulation strength for sensitive cell populations.
Establishing a robust ICS toolkit requires careful consideration of both hardware instrumentation and reagent systems. The essential components include access to flow cytometers capable of multiparameter detection, standardized stimulation and inhibition reagents, and optimized fixation/permeabilization systems tailored to specific intracellular targets. By implementing the standardized protocols, quality control measures, and troubleshooting approaches outlined in this application note, researchers can generate reliable, high-quality ICS data for vaccine development and immunotherapeutic drug discovery. The continuous optimization of each workflow component ensures that ICS remains a powerful methodology for probing immune function at the single-cell level, providing critical insights into mechanistic immunology and therapeutic efficacy.
From Bench to Bedside: Methodological Protocols and Translational Applications
Within the framework of intracellular cytokine staining (ICS) flow cytometry research, selecting the appropriate T-cell stimulation protocol is paramount for generating accurate, reproducible, and biologically relevant data. The choice between antigen-specific and polyclonal activation dictates the scope and specificity of the immune response that can be observed. Antigen-specific stimulation reveals the functional capacity of T-cell clones responsive to a particular pathogen, autoantigen, or vaccine component, while polyclonal activation provides a broad overview of the entire T-cell repertoire's functional potential [28] [29]. This application note delineates optimized protocols for both approaches, providing detailed methodologies, comparative analysis, and practical guidance for researchers and scientists in drug development.
Comparative Analysis of Activation Methods
The following table summarizes the core characteristics, applications, and key readouts for antigen-specific and polyclonal stimulation protocols, guiding the selection of the appropriate method for a given research objective.
Table 1: Comparison of Antigen-Specific and Polyclonal Activation Protocols for ICS
| Feature | Antigen-Specific Stimulation | Polyclonal Stimulation |
|---|---|---|
| Principle | Activation via T-cell receptor (TCR) engagement by specific peptide-MHC complexes [29]. | Bypasses TCR with chemical activators like PMA (phorbol myristate acetate) and Ionomycin [28]. |
| Primary Application | Quantification and characterization of rare, antigen-responsive T-cell populations (e.g., in infection, cancer, autoimmunity, vaccine studies) [29] [30]. | Assessment of the total functional potential and polyfunctionality of T-cell compartments (e.g., vitreous vs. blood T-cells) [28]. |
| Key Readouts | Frequency of cytokine-producing cells, phenotype (memory/effector), and polyfunctional profiles of antigen-specific clones [28] [29]. | Maximum cytokine production capacity, T-cell polyfunctionality, and overall functional integrity of T-cell populations [28]. |
| Typical Stimulation Duration | Longer (6-24 hours): Allows for processing, presentation, and TCR engagement [29]. | Shorter (4-6 hours): Direct and rapid activation of signaling pathways [29]. |
| Critical Optimization Parameters | Antigen concentration, duration of stimulation, use of co-stimulatory antibodies [29]. | Dose of PMA and Ionomycin, duration to avoid over-stimulation and cell death [29]. |
Experimental Protocols
Optimized Antigen-Specific Stimulation Protocol
This protocol is designed to detect low-frequency, antigen-specific T cells, such as those responding to viral antigens (e.g., SARS-CoV-2 Spike protein) or retinal autoantigens, with high sensitivity and minimal background [28] [30].
Workflow Overview:
Step-by-Step Methodology:
Sample Preparation: Isolate Peripheral Blood Mononuclear Cells (PBMCs) from whole blood using density gradient centrifugation. Resuspend cells in complete RPMI culture medium at a concentration of 5-10 × 10^6 cells/mL [29] [30].
Antigen Stimulation:
- Aliquot 0.5-1 million PBMCs per well into a 96-well U-bottom or V-bottom plate.
- Stimuli: Use relevant antigenic peptides (e.g., pooled MTb peptides, SARS-CoV-2 Spike protein peptides, or retinal autoantigen IRBP) [28] [30]. A negative control (DMSO or media alone) and a positive control (PMA/Ionomycin) must be included.
- Antigen Concentration: Systematically titrate the antigen dose. Optimal concentrations often range from 1-10 µg/mL for peptides, but this requires empirical determination for each antigen [29].
- Co-stimulation: Add anti-CD28 and anti-CD49d monoclonal antibodies (each at 1 µg/mL) to provide crucial secondary signals for efficient T-cell activation, enhancing the frequency of detectable cytokine-positive cells [29].
Inhibition of Protein Transport: Add a protein transport inhibitor such as Brefeldin A (BFA, typically at 10 µg/mL) or Monensin to the culture. This blocks cytokine secretion, allowing for intracellular accumulation. Note: BFA should not be left in cultures for more than 8-10 hours to avoid altered cell morphology and decreased positive events [29].
Incubation: Incubate cells for 6-24 hours at 37°C in a 5% CO2 humidified incubator. The optimal duration depends on the antigen and cytokine being studied.
Cell Staining and Acquisition:
- Surface Staining: Transfer cells to a staining plate, wash, and resuspend in a blocking solution containing Fc receptor block (e.g., normal mouse and rat serum) to reduce non-specific antibody binding [31]. Incubate for 15 minutes at room temperature (RT) in the dark. Add a master mix of fluorescently conjugated surface antibodies (e.g., anti-CD3, CD4, CD8, CD45RO, CCR7, CD69, CD137) and incubate for 30-60 minutes at RT [28] [31] [30].
- Fixation and Permeabilization: Wash cells and resuspend in a commercial fixation/permeabilization solution (e.g., Cytofix/Cytoperm) following the manufacturer's instructions. Incubate for 20-30 minutes at RT [31] [32].
- Intracellular Staining: Wash cells with a permeabilization buffer. Resuspend the cell pellet in a master mix of antibodies against cytokines (e.g., IFN-γ, TNF-α, IL-2) and, if required, transcription factors. Incubate for 30-60 minutes at RT in the dark [28] [29].
- Acquisition: Wash cells and resuspend in FACS buffer for immediate acquisition on a flow cytometer. For spectral cytometers, the use of tandem dye stabilizer in the buffer is recommended to preserve signal integrity [31].
Optimized Polyclonal Stimulation Protocol
This protocol uses PMA and Ionomycin to unleash the maximum cytokine response from T cells, useful for assessing overall immune competence and polyfunctional potential [28] [29].
Workflow Overview:
Step-by-Step Methodology:
Sample Preparation: Prepare a single-cell suspension of PBMCs or tissue-derived lymphocytes (e.g., from vitreous fluid) as described in Section 3.1 [28].
Polyclonal Stimulation:
- Aliquot 0.5-1 million cells per well.
- Stimuli: Add PMA and Ionomycin at optimized concentrations. A common working concentration is 50 ng/mL for PMA and 1 µg/mL for Ionomycin, but titration is essential [29].
- Critical Note: PMA/Ionomycin is a potent stimulus that can rapidly induce activation-induced cell death. The stimulation time should be strictly limited.
Inhibition of Protein Transport: Add Brefeldin A simultaneously with or immediately after the stimulators.
Incubation: Incubate cells for a shorter duration of 4-6 hours at 37°C, 5% CO2. Prolonged incubation can lead to increased cellular debris and non-specific death.
Cell Staining and Acquisition: Follow the same staining procedure outlined in Step 5 of Section 3.1. The analysis often focuses on polyfunctional T cells that produce multiple cytokines (e.g., TNF-α+IFN-γ+IL-2+) simultaneously [28].
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for ICS Assays
| Reagent / Material | Function / Application | Examples & Notes |
|---|---|---|
| Co-stimulatory Antibodies | Enhances T-cell activation and cytokine production during antigen-specific stimulation [29]. | Anti-CD28 and anti-CD49d antibodies (1 µg/mL each). |
| Protein Transport Inhibitors | Blocks Golgi-mediated secretion, allowing intracellular cytokine accumulation [29]. | Brefeldin A (BFA) or Monensin. Limit BFA exposure to 8-10 hours [29]. |
| Fc Receptor Blocking Reagent | Reduces non-specific antibody binding, improving signal-to-noise ratio [31]. | Normal serum from the host species of the staining antibodies (e.g., rat, mouse). |
| Tandem Dye Stabilizer | Prevents degradation of sensitive tandem fluorophores, crucial for multi-color panels [31]. | Commercial Brilliant Stain Buffer or similar. Essential for overnight staining or spectral cytometry. |
| Activation-Induced Markers (AIM) | Allows identification of antigen-specific T cells without intracellular staining [30]. | Surface expression of CD69, CD137 (4-1BB), OX40 (CD134). Can be combined with ICS [30]. |
| Fixation/Permeabilization Kit | Preserves cellular structure and allows intracellular antibody access. | Commercial kits (e.g., BD Cytofix/Cytoperm, Foxp3/Transcription Factor Staining Buffer Set). |
Critical Factors for Protocol Optimization
Successful ICS assays require meticulous optimization of key parameters:
- Antigen and Stimulator Titration: The concentration of antigenic peptides or PMA/Ionomycin must be empirically determined for each system to maximize the specific signal while minimizing background and toxicity [29] [32].
- Duration of Stimulation: Antigen-specific responses generally require longer incubation (up to 24 hours), whereas polyclonal responses are rapid and should be limited to 4-6 hours [29].
- Cell Viability and Number: Standardize cell numbers per well to reduce batch effects and ensure a single-cell suspension to avoid clogging the cytometer and poor data quality [31] [33].
- Multipanel Design and Controls: For high-parameter flow cytometry, panel design must account for fluorophore brightness and spectral overlap. Essential controls include unstimulated (background) controls, positive controls (PMA/Ionomycin), and fluorescence-minus-one (FMO) controls for accurate gating [34] [33].
- Data Analysis: Employ tools like FlowSOM or SPICE to analyze high-dimensional data and polyfunctional profiles of T cells, which can reveal critical differences, such as the dominance of polyfunctional CD8+ T cells in disease sites [28].
For researchers conducting intracellular cytokine staining flow cytometry, selecting the appropriate sample type is a critical first step that fundamentally influences experimental outcomes. The choice between whole blood (WB) and peripheral blood mononuclear cells (PBMCs) presents a strategic dilemma, balancing physiological relevance against practical handling considerations. This guide provides a detailed comparison of these sample matrices, focusing on their application in immunophenotyping and intracellular cytokine detection—a cornerstone technique for evaluating immune cell function in research and drug development.
Evidence confirms that immunophenotyping results show minimal differences between freshly isolated and cryopreserved PBMCs, enabling valuable batch analysis for cohort studies [35]. However, significant profile differences emerge when these samples are compared to whole blood, necessitating careful selection based on the specific research objectives [35]. Furthermore, recent advances in 2025 demonstrate that whole blood can serve as a viable alternative to PBMCs for immunometabolic profiling, particularly beneficial for studies in resource-limited settings [36].
Technical Comparison: Whole Blood vs. PBMCs
Key Characteristics and Applications
| Feature | Whole Blood (WB) | PBMCs |
|---|---|---|
| Physiological Context | Maintains all blood components; considered closer to in vivo state [36] [37] | Isolated mononuclear cells; lacks granulocytes [36] |
| Primary Components | Plasma, RBCs, platelets, leukocytes (including granulocytes) [38] | Lymphocytes (T cells, B cells, NK cells), monocytes, dendritic cells [38] |
| Processing Requirements | Minimal processing; can be used directly [37] | Requires density gradient centrifugation (e.g., Ficoll) [38] [36] |
| Stability Timeline | Optimal within 24-48 hours for fresh untreated samples [37] | Can be cryopreserved for long-term storage and batched analysis [35] [37] |
| Ideal Applications | Receptor occupancy assays, absolute cell counting, immunophenotyping [37] | Batched analysis, longitudinal studies, rare cell population analysis [35] [37] |
| Logistical Considerations | Time-sensitive processing; shipping challenges [37] | Centralized processing possible; enables multi-center studies [35] [37] |
| Impact on Cell Ratios | Preserves native immune cell frequencies [35] | Alters native ratios; granulocytes are lost during isolation [35] [36] |
Impact on Immune Cell Population Frequencies
Recent comparative studies have quantified how sample processing affects the observed frequencies of key immune populations, with particular relevance for intracellular cytokine staining workflows:
| Cell Population | WB vs. Fresh PBMCs | WB vs. Cryopreserved PBMCs | Fresh vs. Cryopreserved PBMCs |
|---|---|---|---|
| CD4+ T Helper Cells | Lower in WB [35] | Lower in WB [35] | No major differences [35] |
| T Regulatory Cells (Tregs) | Higher in WB [35] | Higher in WB [35] | No major differences [35] |
| CD8+ T Cytotoxic Cells | Higher in WB [35] | Higher in WB [35] | No differences observed [35] |
| NK Cells (CD56+) | Lower in WB [35] | Lower in WB [35] | No differences observed [35] |
| B Cells (CD19+) | Higher in WB [35] | Higher in WB [35] | No differences observed [35] |
| Monocyte Subsets | Information not compared | Information not compared | No differences observed [35] |
Practical Protocols for Intracellular Cytokine Staining
Protocol A: Two-Step Staining for Cytoplasmic Cytokines
This protocol is optimized for detecting cytokines and other secreted proteins, requiring both fixation and permeabilization steps to access intracellular compartments [27].
Materials and Reagents
- Intracellular Fixation & Permeabilization Buffer Set (Thermo Fisher, cat. no. 88-8824) [27]
- Flow Cytometry Staining Buffer (Thermo Fisher, cat. no. 00-4222) [27]
- Protein Transport Inhibitors (Brefeldin A or Monensin) (Thermo Fisher, cat. no. 00-4506/00-4505) [27]
- Fixable Viability Dyes (eFluor series) to exclude dead cells [27]
- Stimulation Agents: Cell Stimulation Cocktail (500X) (for T cells: PMA/ionomycin; for monocytes: LPS) [27]
Staining Workflow
Cell Stimulation & Secretion Inhibition
- Prepare single-cell suspension from WB or PBMCs
- Stimulate cells with appropriate activator (PMA/ionomycin for T cells; LPS for monocytes)
- Add protein transport inhibitor (Brefeldin A or Monensin) for final 4-6 hours of culture to block cytokine secretion [27]
Surface Marker Staining
- Transfer 1-2×10^6 cells to FACS tubes
- Wash with PBS containing 2% FBS
- Stain with fluorochrome-conjugated surface antibodies for 20-30 minutes on ice
- Wash twice with cold staining buffer [27]
Fixation and Permeabilization
- Fix cells with 100-200µL IC Fixation Buffer for 20-60 minutes at room temperature, protected from light
- Add 2mL 1X Permeabilization Buffer, centrifuge at 400-600×g for 5 minutes
- Repeat permeabilization wash step [27]
Intracellular Staining
- Resuspend cell pellet in 100µL 1X Permeabilization Buffer
- Add predetermined concentration of anticytokine antibodies
- Incubate 20-60 minutes at room temperature, protected from light
- Wash twice with 2mL 1X Permeabilization Buffer [27]
Data Acquisition
- Resuspend cells in Flow Cytometry Staining Buffer
- Acquire on flow cytometer within 24 hours for optimal results [27]
Protocol B: One-Step Staining for Nuclear Antigens
This streamlined protocol combines fixation and permeabilization for detecting transcription factors and nuclear antigens, particularly useful for characterizing T-cell differentiation states.
Materials and Reagents
- Foxp3/Transcription Factor Staining Buffer Set (Thermo Fisher, cat. no. 00-5523) [27]
- Fixable Viability Dyes (eFluor series) [27]
- Fc Receptor Blocking Solution (optional, to reduce nonspecific binding) [27]
Staining Workflow
Surface Marker Staining
- Prepare single-cell suspension
- (Optional) Stain with viability dye
- Stain surface markers as described in Protocol A, steps 2-4 [27]
Simultaneous Fixation/Permeabilization
- After final wash, resuspend cell pellet in residual buffer
- Add 1mL freshly prepared Foxp3 Fixation/Permeabilization working solution
- Incubate 30-60 minutes at room temperature, protected from light [27]
Intracellular Staining
- Add 2mL 1X Permeabilization Buffer, centrifuge at 400-600×g for 5 minutes
- Discard supernatant, resuspend in 100µL 1X Permeabilization Buffer
- Add antibodies against nuclear antigens (transcription factors)
- Incubate 30-60 minutes at room temperature, protected from light [27]
Data Acquisition
- Wash twice with 2mL 1X Permeabilization Buffer
- Resuspend in Flow Cytometry Staining Buffer for acquisition [27]
Sample Preparation Workflow
The following diagram illustrates the key decision points in preparing whole blood and PBMC samples for intracellular cytokine staining:
The Scientist's Toolkit: Essential Research Reagents
| Reagent Category | Specific Examples | Function in Intracellular Staining |
|---|---|---|
| Cell Processing | Ficoll density gradient, RBC lysis buffer | PBMC isolation, RBC removal from whole blood [38] [36] |
| Viability Assessment | Fixable Viability Dyes (eFluor series) | Distinguish live/dead cells; critical for accurate analysis [27] |
| Stimulation & Inhibition | PMA/lonomycin, LPS, Brefeldin A, Monensin | Activate immune cells; block cytokine secretion for detection [27] |
| Buffers & Permeabilization | Intracellular Fixation & Permeabilization Buffer Set, Foxp3/Transcription Factor Buffer Set | Enable antibody access to intracellular compartments [27] |
| Blocking Reagents | Fc Receptor Block, True-Stain Monocyte Blocker | Reduce nonspecific antibody binding [39] [36] |
| Antibody Cocktails | Fluorochrome-conjugated antibodies against surface markers and cytokines | Specific detection of target immune populations and cytokines [27] [40] |
| Cryopreservation Media | CryoStor-CS10, DMSO/FBS mixtures | Maintain cell viability during frozen storage [35] [36] |
Strategic Implementation in Clinical Research
Case Study: Receptor Occupancy Assay Development
Precision for Medicine successfully developed a receptor occupancy (RO) assay for monitoring target engagement of a monoclonal antibody targeting co-stimulatory molecules on CD4+ and CD8+ T cells. Faced with dispersed geography and 48-hour sample stability constraints, they implemented fixed whole blood as the sample matrix. After feasibility studies identifying Smart Tube Proteomic fixative as optimal, they demonstrated 120-day stability at -80°C, enabling batched analysis and robust data generation across multiple clinical sites [37].
Standardization for Multicenter Trials
For a global oncology study with sites in Spain, Turkey, and Israel, researchers implemented a 15-color immunophenotyping panel using Cyto-Chex BCT tubes for direct blood collection. Through rigorous standardization of shipping conditions (4°C) and analysis timeline (within 96 hours), they achieved consistent resolution of T-cell, NK-cell, B-cell, and monocyte subsets across all sites. This approach demonstrates that with careful validation, complex immunophenotyping can be successfully implemented in global trials using standardized whole blood processing [37].
The choice between whole blood and PBMCs for intracellular cytokine staining represents a balance between physiological relevance and practical considerations. Whole blood offers superior preservation of native immune contexts and is ideal for receptor occupancy assays and absolute cell counting, while PBMCs provide flexibility for batch analysis and longitudinal studies. Critically, researchers should avoid direct comparison of results obtained from different sample types without establishing cross-validation data, as immune cell frequencies differ significantly between these matrices. By aligning sample selection with specific research objectives and implementing the standardized protocols outlined in this guide, researchers can generate robust, reproducible data for both basic immunology research and clinical drug development programs.
Multiparameter Panel Design for Deep Immune Profiling
Deep immune profiling via multiparameter flow cytometry is a powerful technique for investigating cellular heterogeneity and functional states at the single-cell level. For researchers in intracellular cytokine staining, designing a robust multicolor panel is a critical step that balances marker necessity with technical feasibility. This application note provides a structured framework for developing high-parameter panels, focusing on standardized protocols for reproducible immunophenotyping and intracellular cytokine detection, essential for drug development and mechanistic studies.
Panel Design Fundamentals
Know Your Instrument Configuration
The first step in panel design involves understanding the technical specifications of your flow cytometer. The optical configuration—including the number and type of lasers and the number of detectors with their specific filter sets—dictates which fluorophores can be detected effectively [41]. Modern cytometers used for high-parameter panels typically feature three laser lines (blue: 488 nm, red: 633/635 nm, violet: 405 nm) [42]. Before selecting fluorophores, consult your instrument's manual or core facility manager to confirm its optical configuration and ensure your panel is compatible [41].
Fluorophore Selection and Antigen Matching
Strategic pairing of fluorophores with target antigens is crucial for panel performance. The core principle is to match fluorophore brightness with antigen expression levels:
- Bright Fluorophores (e.g., PE, APC): Use for detecting low-density antigens or characterizing rare cell populations [41].
- Medium/Dim Fluorophores (e.g., FITC, PerCP): Use for identifying highly expressed, often bimodal, "on-off" antigens [41] [42].
Minimizing spectral overlap is another key consideration. Choose fluorophores with little to no overlap in their emission spectra where possible. When overlap is unavoidable, it must be corrected through fluorescence compensation [41]. The EuroFlow Consortium's work on standardized 8-color panels provides a validated foundation, pre-selecting FITC and PE for the blue laser, APC for the red laser, and comparing options like Pacific Blue vs. Horizon V450 for the violet laser [42].
Table 1: Common Fluorophores and Their Typical Applications in Panel Design
| Fluorophore | Laser Line | Relative Brightness | Recommended for Antigen Expression Level | Notes |
|---|---|---|---|---|
| FITC | Blue (488 nm) | Medium | High | Pre-selected in EuroFlow standards [42] |
| PE | Blue (488 nm) | High | Low | Bright; ideal for low-density antigens [41] |
| APC | Red (633/635 nm) | High | Low | Bright; ideal for low-density antigens [41] |
| PerCP-Cy5.5 | Blue (488 nm) | Low | High | Used for third blue laser detector [42] |
| PE-Cy7 | Blue (488 nm) | Medium | Medium/High | Used for fourth blue laser detector [42] |
| Pacific Blue | Violet (405 nm) | Medium | Medium | Evaluated for violet laser detector [42] |
Gating Strategy and Marker Classification
Establishing a hierarchical gating strategy before finalizing the panel is a best practice. This framework helps assess the practical impact of spillover spreading on resolving critical populations, especially those expressing low-abundance targets [43]. Classify your antigens into categories based on expression density and biological importance to guide fluorophore assignment [43]:
- Primary Markers: High-density, often bimodal antigens used for core population identification (e.g., CD45, CD3, CD4, CD8).
- Secondary Markers: High to mid-density antigens with gradient expression for subtyping.
- Tertiary Markers: Low-density or critical functional antigens (e.g., phosphorylated proteins, cytokines).
Optimized Protocols for Intracellular Staining
Sample Preparation and Staining Protocol
The following methodology, adapted from studies on human minor salivary glands, is optimized for intracellular protein detection, such as phosphorylated signaling proteins, and can be applied to cytokine research [44].
Key Materials:
- Fresh tissue or cell samples (e.g., PBMCs, tissue biopsies)
- Tissue Dissociation Kit (e.g., Human Multi Tissue Dissociation Kit A, Miltenyi Biotec) [44]
- Fixation Buffer (e.g., BD Cytofix Fixation Buffer) [44]
- Permeabilization Buffer (e.g., BD Phosflow Perm Buffer III) [44]
- Fluorochrome-conjugated antibodies against surface and intracellular targets
- Flow cytometer with minimum 8-color configuration
Detailed Step-by-Step Procedure:
Tissue Dissociation:
- For tissue samples, immediately place in ice-cold RPMI medium after collection.
- Remove fibrous tissue and mince into ~0.5 mm pieces using a scalpel. Avoid excessive mincing.
- Digest tissue using a validated dissociation kit (e.g., Human Multi Tissue Dissociation Kit A) in a mechanical dissociator with heated sleeves at 37°C.
- Filter the resulting single-cell suspension through 70 µm and 30 µm filters. Centrifuge at 300 × g for 10 minutes at 4°C and wash twice [44].
Cell Surface Staining:
- Resuspend the single-cell suspension in staining buffer. Stain with titrated, fluorochrome-conjugated antibodies against surface markers (e.g., CD45, CD3, CD4, CD8) for 30 minutes at room temperature in the dark.
- Wash cells to remove unbound antibody [44].
Fixation and Permeabilization:
- Fix cells using a formaldehyde-based fixation buffer (e.g., BD Cytofix) for 2 hours at 4°C. Wash with staining buffer.
- Permeabilize cells using 100 µL of ice-cold methanol-based perm buffer (e.g., BD Phosflow Perm Buffer II) for 30 minutes at -20°C. Wash with staining buffer [44]. Note: Methanol-based buffers are optimal for detecting intracellular phosphorylated proteins.
Intracellular Staining:
- Stain with titrated antibodies against intracellular targets (e.g., cytokines, pIRF3, pNF-κB) overnight at 4°C in the dark [44]. Note: Overnight incubation can enhance signal for some low-abundance targets.
- Wash cells thoroughly and resuspend in staining buffer for acquisition.
Data Acquisition:
- Acquire data on a flow cytometer calibrated with appropriate compensation controls. Include single-stain controls and fluorescence-minus-one (FMO) controls for accurate gating and compensation [43].
Titration and Quality Control
Antibody titration is essential for optimal signal-to-noise ratio. Titrate each antibody using serial dilutions on control cells (e.g., PBMCs for common immune markers, relevant cell lines for specialized markers) to determine the concentration that provides the best separation between positive and negative populations [44] [43].
For quality control, perform Fluorescence Minus One (FMO) controls. These controls contain all antibodies in the panel except one and are critical for setting accurate gates, especially for dimly expressed antigens and in densely populated regions of the fluorescence landscape [43].
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for Multiparameter Flow Cytometry
| Item | Function/Application | Example Products/Citations |
|---|---|---|
| Tissue Dissociation Kits | Generate single-cell suspensions from solid tissues for analysis. | Human Multi Tissue Dissociation Kit A (Miltenyi Biotec) [44] |
| Fixation Buffers | Preserve cell structure and surface marker epitopes, halting cellular processes. | BD Cytofix Fixation Buffer [44] |
| Permeabilization Buffers | Enable antibodies to access intracellular antigens by disrupting the cell membrane. | BD Phosflow Perm Buffer II (methanol-based) [44] |
| Viability Dyes | Distinguish live from dead cells, improving data quality by excluding artifacts. | Zombie Aqua Viability Dye (BioLegend) [43] |
| Compensation Beads | Serve as uniform positive and negative controls for setting fluorescence compensation. | CompBeads (BD Biosciences) [43] |
| Backbone Antibodies | Identify major cell lineages (e.g., T cells, B cells, myeloid cells) for population gating. | CD45, CD3, CD19, CD11b [44] [43] |
| Intracellular Target Antibodies | Probe functional and signaling states (e.g., cytokines, phospho-proteins). | Anti-pIRF3, anti-pNF-κB [44] |
| Cryopreservation Medium | Maintain cell viability for long-term storage and batch analysis of samples. | Freezing medium (90% FBS + 10% DMSO) [43] |
Experimental Workflow and Signaling Pathway Visualization
The following diagram illustrates the complete integrated workflow for sample processing, staining, and data analysis, highlighting key decision points.
Diagram 1: Integrated workflow for intracellular multiparameter flow cytometry.
For intracellular cytokine staining, understanding the relevant signaling pathways is key. The diagram below models a generalized cytokine signaling pathway, representative of pathways like Type-I Interferon, which can be investigated using these methods [44].
Diagram 2: Generalized cytokine signaling pathway for intracellular detection.
Multiparameter flow cytometry is an indispensable tool for deep immune profiling in therapeutic development. Success hinges on a methodical approach to panel design, incorporating instrument knowledge, strategic fluorophore-antigen pairing, and rigorous standardization. The protocols and frameworks presented here, including optimized intracellular staining and standardized panel design principles, provide a robust foundation for generating high-quality, reproducible data in cytokine research and drug development programs.
Intracellular cytokine staining (ICS) coupled with flow cytometry is a powerful methodology enabling quantitative, single-cell analysis of cytokine production in heterogeneous cell populations. Within drug discovery, this technique provides critical functional data during the early phases of hit identification and lead optimization. By enabling researchers to simultaneously monitor specific cytokine modulation alongside cell surface and intracellular markers, ICS delivers multidimensional data essential for evaluating compound efficacy, selectivity, and mechanism of action in physiologically relevant models [45] [46]. This application note details standardized protocols and analytical frameworks for implementing ICS to accelerate the discovery of immunomodulatory therapeutics.
Application in Drug Discovery Workflow
ICS integrates seamlessly into the established drug discovery pipeline, providing functional data at critical decision points.
Table 1: ICS Applications in Early Drug Discovery
| Discovery Stage | Primary ICS Application | Key Measured Parameters | Impact on Decision-Making |
|---|---|---|---|
| Hit Identification | Phenotypic screening of compound libraries [47] | Cytokine expression frequency and intensity; Cell viability and activation markers [45] | Identifies initial compounds ("hits") that modulate biologically relevant cytokine pathways. |
| Lead Optimization | Profiling compound series for potency and selectivity [45] [46] | Dose-response curves (EC50/IC50); Cell-type specific cytokine production; Phospho-protein signaling downstream of cytokine receptors [45] | Guides chemical optimization by ranking analogs based on functional potency and predictive safety. |
| Translational Research | Biomarker analysis in preclinical models and early clinical trials [45] | Correlation of cytokine modulation with PK/PD and efficacy endpoints [45] | Supports biomarker strategy and provides pharmacodynamic evidence of target engagement. |
The power of ICS in phenotypic screening is exemplified by its use in identifying modulators of T-regulatory (Treg) cell function. One high-throughput screen of over 250,000 compounds used ICS and other flow cytometric measures to discover molecules that altered Treg proliferation and function, successfully narrowing the field to a manageable number of confirmed hits for further study [47]. Furthermore, phospho-flow cytometry, an extension of ICS, has been instrumental in optimizing selectivity for kinase targets, such as distinguishing JAK1 from JAK2 inhibitor activity in primary immune cells [45] [46].
Diagram 1: ICS Experimental Workflow
Key Experimental Protocols
Protocol 1: High-Throughput ICS for Compound Screening
This protocol is designed for profiling small molecule or biologic libraries in 96-well or 384-well plate formats to identify modulators of cytokine production [47].
Materials:
- Primary human immune cells (e.g., PBMCs, CD4+ T cells) or relevant cell lines.
- Compound library and appropriate vehicle controls.
- Cell stimulation cocktail (e.g., PMA/Ionomycin, specific antigen peptides).
- Brefeldin A or Monensin to inhibit cytokine secretion.
- Fluorochrome-conjugated antibodies against surface markers (e.g., CD3, CD4, CD8).
- Fixation/Permeabilization buffer system.
- Fluorochrome-conjugated antibodies against intracellular cytokines (e.g., IFN-γ, IL-2, TNF-α, IL-17).
- High-throughput flow cytometer with automated plate sampler.
Methodology:
- Cell Plating and Compound Treatment: Plate cells in 96-well or 384-well U-bottom plates. Add compounds and incubate (e.g., 1-24 hours, compound-dependent).
- Cell Stimulation and Cytokine Accumulation: Add cell stimulation cocktail concurrently with, or following, compound treatment. Add protein transport inhibitor (e.g., Brefeldin A) and incubate for an additional 4-6 hours [47].
- Cell Harvest and Surface Staining: Centrifuge plates, resuspend cells in staining buffer containing surface marker antibodies, and incubate for 30 minutes at 4°C in the dark.
- Fixation and Permeabilization: Centrifuge, remove supernatant, and resuspend cell pellet in fixation/permeabilization buffer. Incubate for 20-60 minutes at 4°C in the dark.
- Intracellular Staining: Wash cells with permeabilization buffer. Resuspend in permeabilization buffer containing pre-titrated cytokine antibodies. Incubate for 30-60 minutes at 4°C in the dark.
- Data Acquisition: Wash cells and resuspend in flow cytometry buffer. Acquire data on a high-throughput flow cytometer, collecting >10,000 events per well of the population of interest [47].
Protocol 2: Multiparametric ICS for Lead Optimization
This protocol focuses on deep immunophenotyping to evaluate compound potency, selectivity, and mechanism of action on specific cell subsets within complex cultures.
Materials:
- As in Protocol 1, with expanded antibody panel for deeper subset analysis (e.g., CD45RA, CCR7, CD25, CD127, transcription factors).
- Reference compounds with known mechanisms.
Methodology:
- Dose-Response Treatment: Treat cells with a serial dilution of lead compounds and controls for a predetermined time.
- Stimulation and Staining: Follow steps 2-5 from Protocol 1, using an expanded, multicolor antibody panel (e.g., 10+ colors) to enable deep immunophenotyping.
- High-Parameter Data Acquisition: Acquire data on a flow cytometer capable of detecting 10 or more colors. Use fluorescence minus one (FMO) controls and biological controls to establish accurate gating boundaries [48].
- Advanced Data Analysis: Analyze data using sequential gating strategies. First, gate out debris and dead cells, then identify major lineages, and finally gate on subpopulations of interest to quantify cytokine responses. Use FMO controls to guide placement of positive/negative gates for dimly expressed cytokines [48].
The Scientist's Toolkit: Research Reagent Solutions
The successful implementation of ICS relies on critical reagents and rigorous validation.
Table 2: Essential Reagents for ICS Flow Cytometry
| Reagent Category | Specific Examples | Critical Function | Validation & Selection Tips |
|---|---|---|---|
| Cell Activation | PMA/Ionomycin, Antigenic Peptides, CD3/CD28 Beads | Induces cytokine production for measurement. | Titrate for optimal signal-to-noise; match to biological context. |
| Protein Transport Inhibitors | Brefeldin A, Monensin | Blocks cytokine secretion, enabling intracellular accumulation. | Test for cytotoxicity and optimal incubation time. |
| Fixation/Permeabilization Buffers | Commercial kits (e.g., FoxP3 Transcription Factor Staining Buffer Set) | Makes intracellular epitopes accessible to antibodies. | Must be validated for each antibody clone and target epitope [49]. |
| Validated Antibody Clones | Anti-IFN-γ (4S.B3), Anti-IL-17 (BL168), Anti-TNF-α (MAb11), Anti-phospho-Proteins (e.g., pAkt, pSTAT) | Specific detection of target cytokines and signaling molecules. | Consult compatibility tables for fixation methods [49]. Prioritize bright fluorochromes for low-abundance cytokines [48]. |
| Fluorochrome Conjugates | Brilliant Violet, Alexa Fluor, PE, APC series | Provides detectable signal for each parameter. | Pair bright fluorochromes with low-density antigens and dim fluorochromes with highly expressed antigens [50] [48]. |
Data Analysis and Technical Considerations
Robust data analysis is paramount for extracting meaningful conclusions from complex ICS datasets.
- Gating Strategy and Controls: Begin by gating on single, live cells. Use FMO controls to accurately define positive populations, especially for dim cytokines or new panels [48]. For phospho-target analysis, include unstimulated biological controls to establish baseline signaling.
- Quantification and Normalization: Report both the frequency of cytokine-positive cells (%) and the intensity of cytokine expression (Mean or Median Fluorescence Intensity, MFI). For screening, results are often normalized to vehicle control (e.g., % inhibition or % activation).
- Panel Design for Multicolor Experiments: In 10-color experiments, the complexity is significant, with 1,024 possible population combinations [48]. Panel design must account for fluorochrome brightness and antigen density, pairing dim markers with bright fluorochromes [50] [48]. Always consult published panels (e.g., OMIPs) as a starting point [48].
Diagram 2: ICS Data Analysis Gating Strategy
Intracellular cytokine staining by flow cytometry is an indispensable tool for modern drug discovery, providing unparalleled depth of functional insight at the single-cell level. The protocols and frameworks outlined herein provide a robust foundation for deploying ICS in high-throughput screening and lead optimization campaigns. Adherence to best practices in panel design, experimental control, and data analysis ensures the generation of high-quality, reproducible data, ultimately de-risking the selection of novel therapeutic candidates for immunomodulatory diseases.
Intracellular Cytokine Staining (ICS) is a powerful flow cytometry-based technique that enables researchers to detect and quantify cytokine production at the single-cell level. This capability is particularly valuable in clinical trials for monitoring vaccine responses and cell therapies, as it provides critical insights into the functional status of immune cells. Unlike bulk cytokine measurement techniques such as ELISA, ICS allows for the precise identification of which cell subsets are producing specific cytokines, while simultaneously characterizing cell surface phenotypes [1]. In the context of vaccine development, this technique has become indispensable for evaluating cellular immunogenicity—a key objective in phase I and II clinical trials where only candidates with sufficient immunogenicity progress to larger phase III studies [51].
The fundamental principle behind ICS involves stimulating immune cells, typically peripheral blood mononuclear cells (PBMCs), with specific antigens or non-specific activators, followed by the inhibition of protein secretion to cause cytokine accumulation within intracellular compartments [1]. Cells are then fixed, permeabilized to allow antibody access, and stained with fluorochrome-conjugated antibodies against target cytokines and cell surface markers. This process enables the detection of antigen-specific T-cell responses by characterizing cytokine-producing CD4+ and CD8+ T cells after ex vivo stimulation with vaccine antigens [51]. For example, in HIV vaccine trials, cellular responses are often measured by enumerating IFN-γ-, IL-2-, and TNF-α-producing T cells after stimulation with pools of HIV peptides contained in the vaccine sequence [51].
Applications in Vaccine Development
Assessing Cellular Immunogenicity
Vaccine efficacy depends on generating robust and durable immune responses, with T-cell immunity playing a crucial role in protection against intracellular pathogens and viruses. ICS provides a powerful platform for quantifying and characterizing these T-cell responses in vaccine clinical trials. The conventional statistical approach for analyzing ICS data in vaccine trials involves subtracting the response observed in non-stimulated cells from each stimulated condition of a given sample, followed by inter- or intra-arm comparison of the distribution of percentages of cytokine-producing cells [51]. However, emerging statistical methods propose bivariate linear models that simultaneously include both non-specific and specific responses as dependent variables for more accurate estimation of vaccine effects [51].
The application of ICS in vaccine trials extends beyond mere quantification of responding cells. The technique's multiparameter capability allows researchers to:
- Identify polyfunctional T-cell subsets that produce multiple cytokines simultaneously
- Correlate specific cytokine profiles with protective immunity
- Track the persistence of vaccine-induced memory T-cell responses
- Evaluate responses to different vaccine components or formulations
Monitoring Cell Therapies
In the rapidly advancing field of cell therapy, ICS plays an equally critical role in functional characterization and monitoring of cellular products. For Chimeric Antigen Receptor (CAR) T-cells, tumor-infiltrating lymphocytes (TILs), and other engineered cell therapies, ICS can be employed to assess functional potency, measure pharmacodynamic changes, and monitor therapeutic efficacy [1] [52]. When paired with cell therapy monitoring, ICS methods allow researchers to evaluate the functional response of the cell therapy throughout the course of treatment [1].
Key applications of ICS in cell therapy development include:
- Functional Pharmacokinetics: Direct measurement of intact cell therapy populations and their functional characteristics over time [52]
- Effector Function Assessment: Evaluation of cytokine production profiles associated with therapeutic efficacy
- Immunogenicity Assessments: Detection of cellular immune responses against cell therapeutics that may impact safety and efficacy [52]
- Product Potency Testing: Characterization of cytokine secretion profiles as part of comprehensive product release criteria
For cell therapies, the flexibility of ICS assays allows researchers to tailor stimulation conditions to the specific mechanism of action of the therapeutic, whether through non-specific stimulation with pathway activators like PMA and ionomycin, or antigen-specific stimulation using target peptides or proteins [1].
Key Methodologies and Protocols
Standard ICS Protocol for Cytoplasmic Proteins
The following two-step protocol is recommended for the detection of cytoplasmic proteins, cytokines, and other secreted proteins in individual cells following activation in vitro or in vivo [27]. This protocol allows simultaneous analysis of cell surface molecules and intracellular antigens at the single-cell level.
Materials Required:
- 12x75 mm round bottom test tubes or 96-well V- or U-bottom microtiter plates
- Fixable Viability Dyes (optional)
- Directly conjugated antibodies against target antigens
- Intracellular Fixation & Permeabilization Buffer Set (e.g., cat. no. 88-8824)
- Flow Cytometry Staining Buffer
- Cell stimulation reagents (e.g., Cell Stimulation Cocktail, Protein Transport Inhibitors)
Table 1: Key Reagents for ICS Protocol
| Reagent Category | Specific Examples | Function |
|---|---|---|
| Stimulation Agents | PMA/Ionomycin, antigenic peptides, LPS | Activate immune cells to induce cytokine production |
| Protein Transport Inhibitors | Brefeldin A, Monensin | Block cytokine secretion, causing intracellular accumulation |
| Fixation/Permeabilization Reagents | Intracellular Fixation Buffer, Permeabilization Buffer | Stabilize cell structure and enable antibody access to intracellular compartments |
| Staining Reagents | Fluorochrome-conjugated antibodies, viability dyes | Enable detection of target antigens and exclusion of dead cells |
Experimental Procedure:
Cell Preparation and Stimulation: Prepare a single-cell suspension from PBMCs or whole blood. Stimulate cells with the appropriate antigen or mitogen based on the experimental question. For T-cell cytokine detection, a combination of PMA (a protein kinase C activator) and Ionomycin (a calcium ionophore) can be used. For monocyte stimulation, lipopolysaccharide (LPS) may be appropriate [27].
Secretion Inhibition: Add protein transport inhibitors such as Brefeldin A or Monensin during the final hours of stimulation. The appropriate stimulation conditions and kinetics vary depending on cell type and the specific cytokine being assayed [27].
Surface Marker Staining: Stain cells with fluorochrome-conjugated antibodies against cell surface markers. All staining should be performed on ice or at 4°C with minimal exposure to light [27].
Fixation and Permeabilization: After the last wash, fix cells with IC Fixation Buffer (100-200 μL depending on plate or tube format) and incubate for 20-60 minutes at room temperature protected from light. Then, add 2 mL of 1X Permeabilization Buffer and centrifuge. Repeat this permeabilization wash step [27].
Intracellular Staining: Resuspend the cell pellet in 100 μL of 1X Permeabilization Buffer and add directly conjugated primary antibodies for detection of intracellular antigen(s). Incubate for 20-60 minutes at room temperature protected from light [27].
Washing and Analysis: Wash cells twice with Permeabilization Buffer, then resuspend in an appropriate volume of Flow Cytometry Staining Buffer for acquisition on a flow cytometer [27].
Alternative Protocols for Specific Applications
One-Step Protocol for Nuclear Proteins: For detection of nuclear antigens such as transcription factors, a one-step fixation/permeabilization protocol using the Foxp3/Transcription Factor Staining Buffer Set is recommended. This protocol combines fixation and permeabilization into a single step and is also useful for detection of many cytokines [27].
Methanol-Based Protocol for Phosphorylated Signaling Molecules: For some phosphorylated signaling molecules such as MAPK and STAT proteins, a fixation/methanol protocol may be preferable. Methanol better preserves certain phosphorylation epitopes and may be required for optimal detection of phosphoproteins [27].
Innovative "Dish Soap Protocol": Recent research has introduced a cost-effective alternative using dishwashing detergent (commercially known as Fairy, Dawn, or Dreft) to create "Burton's Better Buffer." This protocol reportedly enables simultaneous efficient detection of transcription factors, cytokines, and endogenous fluorescent proteins, overcoming limitations of commercial buffers [10]. The protocol involves fixation with 2% formaldehyde containing 0.05% Fairy detergent and 0.5% Tween, followed by permeabilization with PBS containing 0.05% Fairy detergent [10].
Experimental Design and Workflow
The successful implementation of ICS in clinical trial monitoring requires careful experimental design and optimization. The following workflow diagram illustrates the key stages in a comprehensive ICS experiment:
Critical Optimization Steps
Stimulation Conditions: The choice of stimulation conditions depends on the specific research question. For antigen-specific responses, pools of peptides representing vaccine antigens are used. For maximal cytokine induction, non-specific stimulants like PMA and ionomycin are employed. The duration of stimulation varies by cytokine—typically 4-6 hours for most cytokines, but up to 12-24 hours for some like IL-10 [53].
Panel Design: Careful multicolor panel design is essential for successful ICS experiments. Key considerations include:
- Matching fluorophore brightness with antigen abundance (bright fluorophores for low-density antigens)
- Minimizing spectral overlap between fluorophores
- Including appropriate controls (fluorescence minus one controls, isotype controls, unstimulated controls)
- Incorporating viability dyes to exclude dead cells [41]
Gating Strategy: A typical ICS gating strategy includes sequential steps: exclusion of doublets and dead cells, identification of lymphocytes, selection of T-cell populations (CD4+ vs CD8+), and finally analysis of cytokine-positive cells within these populations.
Technical Considerations and Best Practices
Sample Processing and Handling
The source of immune cells for ICS assays is most often whole blood or PBMCs. Each source has distinct advantages: whole blood contains all major immune cell types but requires immediate processing, while PBMCs can be cryopreserved for later analysis but lack granulocytes [54]. For vaccine trials, PBMCs are commonly used due to the practicality of batch testing and the ability to perform longitudinal studies from the same donor [54].
Critical considerations for sample handling include:
- Cryopreservation Effects: PBMC cryopreservation can influence cellular viability, phenotype, and functional state due to intracellular ice crystal formation during freezing [54]
- Time to Processing: Whole blood samples should be processed within 24-48 hours of collection, while PBMCs are typically isolated within 8-24 hours
- Assay Variability: Implementing standardized protocols across multiple clinical sites is essential for reproducible results in multicenter trials
Statistical Analysis of ICS Data
The analysis of ICS data in clinical trials presents specific statistical challenges. Conventional approaches often use binary criteria to report the proportion of vaccine recipients with a "positive" response, or subtract the response in non-stimulated cells from stimulated conditions [51]. However, these approaches have limitations:
Table 2: Statistical Methods for ICS Data Analysis
| Method | Approach | Advantages | Limitations |
|---|---|---|---|
| Binary Response Analysis | Classifies subjects as responders/non-responders based on predefined thresholds | Simple interpretation, clinically relevant | Loss of information, reduced statistical power |
| Background Subtraction | Subtracts non-specific response from antigen-specific response | Attempts to isolate antigen-specific response | Can increase measurement error, may bias distribution |
| Bivariate Modeling | Simultaneously models specific and non-specific responses using regression | More accurate effect estimation, controls type-I error | More complex implementation required |
Simulation studies have shown that bivariate models effectively control type-I errors while maintaining statistical power across different population sizes [51]. These models are particularly valuable when there is correlation between non-specific and specific responses, which conventional approaches fail to accommodate.
Essential Reagents and Materials
Successful implementation of ICS assays requires careful selection of reagents and materials. The following table summarizes key solutions and their functions:
Table 3: Research Reagent Solutions for ICS Assays
| Reagent Category | Specific Products | Function and Application |
|---|---|---|
| Fixation/Permeabilization Kits | Intracellular Fixation & Permeabilization Buffer Set (Thermo Fisher) | Detection of cytoplasmic proteins and cytokines |
| Transcription Factor Buffers | Foxp3/Transcription Factor Staining Buffer Set (Thermo Fisher) | Detection of nuclear antigens and transcription factors |
| Protein Transport Inhibitors | Brefeldin A, Monensin, Protein Transport Inhibitor Cocktail | Block cytokine secretion, enabling intracellular accumulation |
| Cell Stimulation Reagents | Cell Stimulation Cocktail (PMA/ionomycin), antigen peptides | Activate immune cells to induce cytokine production |
| Flow Cytometry Buffers | Flow Cytometry Staining Buffer, FACS Buffer | Maintain cell viability and reduce nonspecific binding during staining |
| Viability Dyes | Fixable Viability Dyes eFluor series | Distinguish live/dead cells to improve data quality |
| Alternative Protocols | "Dish Soap Protocol" using Fairy/Dawn detergent | Cost-effective buffer for simultaneous detection of transcription factors and fluorescent proteins [10] |
Intracellular Cytokine Staining represents a cornerstone technique in clinical trial monitoring for both vaccine responses and cell therapies. Its ability to provide multiparameter data at the single-cell level offers unparalleled insights into the functional immune responses critical for evaluating product immunogenicity and efficacy. As the fields of vaccinology and cell therapy continue to advance, refinements in ICS methodologies—including improved fixation/permeabilization techniques, more sophisticated multicolor panels, and advanced statistical analysis approaches—will further enhance its utility in clinical development programs. By implementing robust, standardized ICS protocols and adhering to best practices in experimental design and analysis, researchers can generate high-quality data to support the development of next-generation vaccines and immunotherapies.
T-cell exhaustion is a state of T-cell dysfunction that arises in chronic diseases, notably cancer, and is characterized by progressive loss of effector functions, sustained expression of inhibitory receptors, and altered metabolic states [55] [56]. This phenomenon poses a significant barrier to effective anti-tumor immunity and represents a major challenge for immunotherapies, including immune checkpoint inhibitors (ICIs) and adoptive cell therapies like CAR-T [55] [57]. Intracellular cytokine staining (ICS) by flow cytometry serves as a gold-standard methodology for functionally assessing this exhausted state at the single-cell level, providing critical insights into cytokine production profiles that are central to evaluating T-cell function and therapeutic efficacy [1] [58]. This application note details a standardized framework for modeling and evaluating T-cell exhaustion, with protocols designed for integration within a broader research thesis on ICS flow cytometry.
Key Hallmarks and Molecular Basis of T-Cell Exhaustion
T-cell exhaustion is not a binary state but a differentiation pathway driven by persistent antigen exposure. Its molecular basis is rooted in distinct transcriptional and epigenetic reprogramming that stabilizes the dysfunctional phenotype [56].
Defining Phenotypic and Functional Hallmarks
Exhausted T cells (TEX) demonstrate a continuum of dysfunction, distinct from anergy and senescence [56]. The core hallmarks include:
- Progressive Loss of Effector Function: Cytokine production is lost in a hierarchical manner, typically beginning with IL-2, followed by TNF-α, and finally IFN-γ. Cytotoxic potential, through granzyme B release, is also severely impaired [55] [56].
- Sustained Expression of Inhibitory Receptors: Exhausted T cells overexpress a spectrum of immune checkpoint molecules, including PD-1, TIM-3, LAG-3, TIGIT, and CTLA-4 [55] [59] [56]. Co-expression of multiple receptors signifies a greater degree of exhaustion.
- Proliferative Impairment: The capacity to expand in response to antigenic stimulation is markedly reduced [55].
- Metabolic Alterations: Exhausted T cells exhibit a low spare respiratory capacity, increased mitochondrial mass, and elevated levels of reactive oxygen species (ROS) [55].
- Epigenetic Locking: A defining feature is a stable, repressive chromatin landscape that suppresses effector gene programs and maintains high expression of inhibitory receptors. This "epigenetic lock" makes the exhausted state largely irreversible, even after antigen removal or PD-1/PD-L1 blockade [56].
Heterogeneity within the Exhausted T-Cell Pool
The exhausted T-cell compartment is not uniform. Single-cell analyses have revealed a hierarchical organization, primarily consisting of:
- Progenitor Exhausted T Cells (TEX-prog): These cells have a TCF1+ PD-1int phenotype, retain self-renewal capacity, and are critical for responding to ICB therapy. They produce IFN-γ but lack terminal effector functions [60] [56].
- Terminally Exhausted T Cells (TEX-term): These cells have a PD-1hi TOXhi phenotype, possess minimal proliferative potential, exhibit severe functional impairment, and are largely resistant to reinvigoration by ICB alone [60] [56].
Table 1: Core Hallmarks of T-Cell Exhaustion
| Hallmark Category | Key Features | Primary Analytical Method |
|---|---|---|
| Surface Phenotype | Sustained high co-expression of PD-1, TIM-3, LAG-3, TIGIT | Multicolor Flow Cytometry |
| Functional Capacity | Loss of polyfunctionality; reduced IFN-γ, TNF-α, IL-2 production | Intracellular Cytokine Staining (ICS) |
| Proliferation | Reduced expansion and Ki67 expression upon re-stimulation | EdU/CFSE dilution, Ki67 staining |
| Cytotoxicity | Impaired Granzyme B release and target cell killing | Cytotoxicity assays, GZMB staining |
| Metabolic State | Low spare respiratory capacity, high mitochondrial mass | Seahorse Analyzer, MitoTracker |
| Epigenetic State | Stable repressive chromatin at effector gene loci | ATAC-seq, ChIP-seq, DNA methylation |
Establishing an In Vitro Model of T-Cell Exhaustion
Robust and reproducible models are essential for studying the mechanisms of T-cell exhaustion and screening potential reversal strategies.
Chronic Antigen Stimulation Model
This protocol, adapted from [55], uses repeated TCR stimulation to mimic persistent antigen exposure.
Diagram 1: In Vitro T-Cell Exhaustion Model Workflow
Materials:
- Source Cells: CD8+ T cells from OT-I transgenic mice (or other TCR-transgenic systems) or human PBMCs.
- Stimulation: CD3/CD28 Dynabeads [59], cognate peptide (e.g., SIINFEKL for OT-I cells) [55], or antigen-presenting cells.
- Cytokines: Recombinant human or mouse IL-2 and IL-15.
Detailed Protocol:
- Isolation and Initial Stimulation: Isolate naive CD8+ T cells from spleens of OT-I mice using a commercial isolation kit. Seed cells in culture medium and stimulate with their cognate peptide (e.g., 1µM SIINFEKL) in the presence of IL-2 (e.g., 20 ng/mL) [55].
- Re-stimulation Cycles: Every 48 hours, re-stimulate the T cells with fresh cognate antigen and IL-2. After the second re-stimulation, supplement the culture medium with IL-15 (e.g., 10 ng/mL) to promote survival [55].
- Maintenance and Harvest: Continue the cycle of re-stimulation and rest for up to seven rounds. Harvest cells for analysis after the final rest period. Exhausted phenotypes typically emerge after 3-5 stimulations [55] [59].
Validation: The resulting cells should be characterized for the hallmarks in Table 1. Specifically, they should show high co-expression of PD-1, LAG-3, and TIM-3 [55] [59], reduced production of IFN-γ and TNF-α upon re-stimulation (measured by ICS), and reduced proliferative capacity [55].
Comprehensive Protocol: Intracellular Cytokine Staining for Functional Assessment
ICS is a critical tool for quantifying the functional impairment of exhausted T cells by measuring their cytokine production capacity at a single-cell level [1] [58].
Staining Protocol
Principle: Live cells are stimulated to produce cytokines, but a protein transport inhibitor is added to cause cytokines to accumulate within the Golgi and cellular cytoplasm. Cells are then fixed, permeabilized, and stained with fluorescent antibodies against intracellular cytokines for detection by flow cytometry [1] [58].
The Scientist's Toolkit: Essential Reagents for ICS Table 2: Key Research Reagent Solutions for Intracellular Cytokine Staining
| Reagent / Solution | Function / Purpose | Example |
|---|---|---|
| Cell Stimulation Cocktail | Activates T cells via TCR and costimulation pathways, inducing cytokine production. | PMA (e.g., 50 ng/mL) + Ionomycin (e.g., 500 ng/mL) [60] [58] |
| Protein Transport Inhibitors | Blocks Golgi apparatus function, preventing cytokine secretion and enabling intracellular accumulation. | Brefeldin A (e.g., 10 µg/mL) and/or Monensin (e.g., 2 µM) [1] [58] |
| Fixative Solution | Crosslinks proteins to preserve cellular morphology and prevent cytokine leakage. | 2-4% Paraformaldehyde (PFA) [58] [10] |
| Permeabilization Buffer | Solubilizes lipid membranes to allow intracellular antibody access. Contains detergents. | Saponin-based buffers (e.g., 0.1% Saponin) [58] [10] or "Dish Soap" buffer (0.05% Fairy) [10] |
| Fluorophore-Conjugated Antibodies | Detection of surface markers (pre-permeabilization) and intracellular cytokines (post-permeabilization). | Anti-CD3, CD8, CD4, PD-1; anti-IFN-γ, TNF-α, IL-2 [58] [59] |
Step-by-Step Methodology:
- Cell Preparation and Stimulation:
- Resuspend exhausted or control T cells at 1-2 x 10⁶ cells/mL in complete culture medium [58].
- Distribute cells into a 96-well round-bottom plate. Include unstimulated controls (medium only) and positive controls (PMA/ionomycin) for gating and background subtraction [58].
- Add stimulation agent. For antigen-specific stimulation, use cognate peptide. For polyclonal stimulation, use PMA (e.g., 50 ng/mL) and ionomycin (e.g., 500 ng/mL) [60] [58].
- Incubate plate for 1-2 hours in a 37°C, 5% CO₂ incubator.
Inhibition of Cytokine Secretion:
Surface Antigen Staining:
- Transfer cells to a fresh plate and wash twice with cold FACS buffer (PBS with BSA/serum) [58].
- Resuspend cell pellet in a master mix of antibodies against surface markers (e.g., anti-CD3, CD4, CD8, PD-1) diluted in FACS buffer. Include a viability dye to exclude dead cells.
- Incubate for 20 minutes at 4°C in the dark. Wash twice with cold FACS buffer.
Fixation and Permeabilization:
- Resuspend cells thoroughly in 200 µL of fixative (e.g., 2% PFA) and incubate for 20 minutes at room temperature in the dark [58] [10].
- Wash cells once with FACS buffer.
- For standard protocols, resuspend cells in 100 µL of permeabilization buffer (e.g., 0.1% saponin or 0.05% Fairy dish soap in PBS [10]) and incubate for 15-30 minutes at room temperature. Cells must be kept in permeabilization buffer for all subsequent steps to prevent membrane resealing.
Intracellular Cytokine Staining:
- Without washing, add antibodies against intracellular targets (e.g., IFN-γ, TNF-α, IL-2, Granzyme B) directly in permeabilization buffer.
- Incubate for 30 minutes at room temperature or overnight at 4°C in the dark [58] [10].
- Wash cells twice with permeabilization buffer, followed by one final wash with regular FACS buffer.
Data Acquisition and Analysis:
- Resuspend cells in FACS buffer and acquire data on a flow cytometer.
- Use unstimulated controls to set gates for cytokine-positive populations. Analyze the frequency of cytokine-producing cells within your T-cell subsets of interest (e.g., live CD8+ T cells).
Data Interpretation and Troubleshooting
Analysis: The functional quality of T cells is best assessed by polyfunctionality—the ability to produce multiple cytokines simultaneously (e.g., IFN-γ+ TNF-α+). Exhausted T cells show a marked reduction in these polyfunctional populations compared to effector or memory T cells [55] [60].
Table 3: Troubleshooting Common ICS Challenges
| Problem | Potential Cause | Solution |
|---|---|---|
| Low Cytokine Signal | Suboptimal stimulation; inactive inhibitors; poor antibody penetration. | Titrate stimulation concentrations; ensure fresh inhibitors; optimize permeabilization detergent/concentration [58]. |
| High Background (Unstimulated Controls) | Non-specific antibody binding; cellular activation during processing. | Titrate all antibodies; include Fc receptor block; minimize cell handling time [58]. |
| Poor Cell Viability Post-Stimulation | Stimulation toxicity; extended culture. | Reduce PMA/ionomycin concentration; shorten stimulation time; check incubator conditions [58]. |
| Loss of Fluorescent Protein Signal | Excessive crosslinking from fixation. | Use a optimized fixation/permeabilization buffer like "Burton's Better Buffer" which balances epitope retention and fluorophore preservation [10]. |
Investigating Pathways and Therapeutic Reversal
Understanding the signaling pathways that drive and maintain exhaustion is key to developing reversal strategies.
Key Signaling Pathways in T-Cell Exhaustion
Multiple interconnected pathways contribute to T-cell exhaustion. Two major pathways are the PD-1/PD-L1 axis and the newly identified CD47-thrombospondin-1 (TSP-1) pathway.
Diagram 2: Key Signaling Pathways in T-Cell Exhaustion and Therapeutic Intervention
Strategies for Reversing Exhaustion
The pathways above are targets for therapeutic intervention aimed at reversing T-cell exhaustion.
- Immune Checkpoint Blockade (ICB): Antibodies targeting PD-1/PD-L1 can partially reinvigorate exhausted T cells, particularly the progenitor exhausted (PD-1int) subset, leading to improved cytokine production and tumor control [60] [57].
- Targeting Novel Pathways: Blocking the interaction between CD47 on T cells and TSP-1 from tumors, using tools like the TAX2 peptide, has been shown to prevent exhaustion and synergize with anti-PD-1 therapy in preclinical models [57].
- Epigenetic Therapies: Given the "epigenetic lock," strategies targeting DNA methyltransferases (DNMTs) or histone modifiers (EZH2, BET family proteins) are being explored to make exhausted T cells more responsive to ICB [56].
- Agonistic Antibodies: The addition of a CD137 (4-1BB) agonist to a regimen of vaccine and anti-PD-1 therapy has been shown to enhance clonal expansion of CD8+ T cells and improve anti-tumor responses, as demonstrated in a pancreatic cancer clinical trial [61].
The in vitro model and ICS protocols detailed herein provide a robust, standardized framework for investigating T-cell exhaustion. The ability to quantitatively assess both phenotypic markers and, crucially, functional cytokine output is indispensable for evaluating the efficacy of novel therapeutic combinations. As the field moves beyond PD-1/PD-L1, targeting alternative pathways like CD47/TSP-1 and leveraging epigenetic reprogramming represent promising frontiers for overcoming exhaustion and improving outcomes in immuno-oncology.
Solving the Puzzle: Expert Troubleshooting and Optimization Strategies for Robust ICS Data
In the field of immunology and drug development, intracellular cytokine staining (ICS) by flow cytometry serves as the gold standard methodology for measuring functional immune responses at the single-cell level [62]. This technique provides critical insights into T helper cell polarization, effector function, and therapeutic response monitoring in vaccine research, immunotherapy development, and autoimmune disease studies [62]. However, the technical complexity of ICS, which combines cellular stimulation, protein transport inhibition, permeabilization, and intracellular antibody staining, introduces multiple potential failure points that can result in weak or absent signal detection [62] [63]. Such signal failure compromises data quality, leads to inaccurate biological interpretations, and represents a significant waste of precious research samples and resources. This application note establishes a systematic diagnostic framework to troubleshoot and resolve signal detection issues in ICS flow cytometry, enabling researchers to generate robust, reproducible data with clearly identifiable cytokine-positive cell populations and minimal background staining [62].
A Structured Diagnostic Framework
Weak or absent signals in ICS flow cytometry can originate from multiple points in the experimental workflow. The following systematic approach facilitates efficient problem identification and resolution by categorizing potential failure points into distinct technical domains.
Diagnostic Decision Workflow
The diagram below outlines a step-by-step logical pathway for diagnosing the root cause of signal failure in intracellular cytokine staining experiments.
Comprehensive Troubleshooting Guide
The table below expands on the diagnostic workflow by detailing specific causes and solutions for each major problem category encountered in ICS experiments.
| Problem Area | Specific Cause | Recommended Solution |
|---|---|---|
| Cell Stimulation & Health | Suboptimal stimulation conditions [62] | Perform time-course and dose-response experiments for PMA/ionomycin (e.g., 50 ng/mL PMA, 500 ng/mL ionomycin) [62]. |
| Inadequate protein transport inhibition [62] | Use combination of brefeldin A (10 μg/mL) and monensin (2 μM) for enhanced cytokine retention [62]. | |
| Poor cell viability post-stimulation [62] | Limit total stimulation time to 4-6 hours; verify incubator conditions (37°C, 5% CO₂) [62]. | |
| Fixation & Permeabilization | Over-fixation abrogating nuclear antigen detection [10] | Use "Burton's Better Buffer" (2% formaldehyde, 0.05% Fairy, 0.5% Tween) for balanced TF and GFP detection [10]. |
| Inconsistent permeabilization efficiency [62] | Standardize fixation/permeabilization timing; verify buffer pH; use commercial kits for reproducibility [62]. | |
| Epitope damage from harsh fixatives [10] | Test milder formaldehyde concentrations (e.g., 2% vs 4%); avoid over-fixation beyond 30 minutes [10]. | |
| Antibody Reagents | Antibody concentration too low [63] | Titrate all antibodies using fixed/permeabilized cells; increase concentration if signal remains weak [63]. |
| Fluorophore-antigen density mismatch [41] | Use brightest fluorophores (PE, APC) for low-density cytokines; dimmer fluorophores for abundant targets [41]. | |
| Non-specific binding blocking detection [31] | Implement Fc receptor blocking with anti-CD16/32 antibody or normal serum from antibody host species [31] [7]. | |
| Instrument Configuration | Improper laser or filter setup [41] | Verify instrument configuration matches fluorophore requirements; check laser alignment and detector sensitivity [41]. |
| Incorrect compensation [41] | Use single-color controls with same fixation/permeabilization; apply compensation from far-red to lower spectrum [41]. | |
| Detector voltage too low [41] | Adjust PMT voltages using unstained and single-color controls to ensure proper signal detection in linear range [41]. |
Detailed Experimental Protocols
Optimized Intracellular Cytokine Staining Protocol
The following protocol incorporates critical steps for signal optimization based on recent methodological advances in the field [62].
Duration: Approximately 6.5 hours (including stimulation, staining, and processing) [62]
Materials and Reagents:
- Cell stimulation cocktail (PMA/ionomycin or antigen-specific stimuli) [62]
- Protein transport inhibitors (Brefeldin A, Monensin) [62]
- Intracellular Fixation & Permeabilization Buffer Set (or commercial equivalent) [27]
- Fluorescently-conjugated antibodies against surface markers and cytokines [62]
- Flow cytometry staining buffer (PBS with BSA/serum and optional sodium azide) [31]
- Blocking reagents (Fc receptor block, normal serum) [31]
- 96-well round-bottom plates [62]
- Refrigerated centrifuge with plate carriers [62]
Procedure:
Cell Stimulation
- Prepare single cell suspension (PBMCs, splenocytes) at 1-2 × 10⁶ cells/mL in complete culture medium [62].
- Distribute cells into 96-well round-bottom plates (200 μL/well) [62].
- Add stimulation cocktails: 50 ng/mL PMA + 500 ng/mL ionomycin for polyclonal activation, or antigen-specific concentrations determined empirically [62].
- Incubate plates at 37°C, 5% CO₂ for 1-2 hours to allow cellular activation [62].
Protein Transport Inhibition
Surface Staining with Blocking
- Transfer cells to fresh 96-well plates and wash twice with cold staining buffer [62].
- Resuspend cells in 20 μL blocking solution containing normal serum from antibody host species (e.g., rat serum for rat antibodies) and incubate 15 minutes at room temperature in dark [31].
- Add surface marker antibodies (CD3, CD4, CD8, etc.) diluted in staining buffer and incubate 20 minutes at 4°C in darkness [62].
- Wash cells twice with staining buffer to remove unbound antibodies [62].
Fixation and Permeabilization
- Fix cells by adding 200 μL IC Fixation Buffer and incubating 20-60 minutes at room temperature in dark [27].
- Centrifuge and discard supernatant [27].
- Add 200 μL 1X Permeabilization Buffer, centrifuge, and discard supernatant [27].
- For challenging targets (transcription factors + cytokines), use "Burton's Better Buffer" (2% formaldehyde with 0.05% Fairy dish soap) for enhanced detection [10].
Intracellular Staining
- Resuspend cells in 100 μL Permeabilization Buffer [27].
- Optional: Add 2% normal serum for additional blocking during intracellular staining [27].
- Add intracellular cytokine antibodies (IFN-γ, TNF-α, IL-2, etc.) diluted in Permeabilization Buffer [62].
- Incubate 30 minutes at room temperature or overnight at 4°C for enhanced detection of low-abundance targets [27] [10].
- Wash twice with Permeabilization Buffer followed by one wash with regular staining buffer [62].
Sample Acquisition
Alternative Protocol for Combined Transcription Factor and Cytokine Detection
For experiments requiring simultaneous detection of transcription factors and cytokines, often challenging with standard buffers, the following "Dish Soap Protocol" has demonstrated superior performance [10].
Materials:
- Fixative: 2% formaldehyde with 0.05% Fairy dish soap and 0.5% Tween-20 [10]
- Permeabilization Buffer: PBS with 0.05% Fairy dish soap [10]
- FACS Buffer: PBS with fetal bovine serum or BSA and EDTA [10]
Procedure:
- Perform surface staining as described in steps 1-4 of the optimized ICS protocol [10].
- After surface staining, centrifuge cells and resuspend in 200 μL fixative [10].
- Incubate 30 minutes at room temperature in dark (perform in fume hood) [10].
- Centrifuge and remove supernatant [10].
- Resuspend in 100 μL perm buffer and incubate 15-30 minutes at room temperature [10].
- Blocking may be done at this stage by adding Fc receptor block or serum to the perm buffer [10].
- Wash twice in FACS buffer [10].
- Stain overnight in FACS buffer at 4°C [10].
- Wash twice in FACS buffer and acquire samples on flow cytometer [10].
The Scientist's Toolkit: Essential Research Reagents
Successful intracellular cytokine staining requires careful selection and application of specific reagents, each serving a critical function in the experimental workflow.
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Stimulation Reagents | PMA/Ionomycin [62]; Antigen-specific peptides [7]; Cell Stimulation Cocktail (plus protein transport inhibitors) [27] | Activates signaling pathways to induce cytokine production; use at optimized concentrations (e.g., 50 ng/mL PMA + 500 ng/mL ionomycin for T cells) [62]. |
| Protein Transport Inhibitors | Brefeldin A (10 μg/mL) [62]; Monensin (2 μM) [62]; Protein Transport Inhibitor Cocktail [27] | Blocks Golgi-mediated secretion, causing intracellular cytokine accumulation; often used in combination for enhanced retention [62]. |
| Fixation/Permeabilization Buffers | Intracellular Fixation & Permeabilization Buffer Set [27]; Foxp3/Transcription Factor Staining Buffer Set [27]; "Burton's Better Buffer" (2% formaldehyde + dish soap) [10] | Preserves cellular structure while enabling antibody access to intracellular targets; selection depends on target location (nuclear vs. cytoplasmic) [27] [10]. |
| Blocking Reagents | Anti-CD16/32 antibody [7]; Normal serum from antibody host species [31]; Fc receptor block [31] | Reduces non-specific antibody binding via Fc receptors; critical for improving signal-to-noise ratio [31] [7]. |
| Signal Enhancement Reagents | Brilliant Stain Buffer [31]; Tandem stabilizer [31] | Prevents dye-dye interactions and tandem dye degradation; particularly important for polymer dyes and tandem fluorophores [31]. |
Weak or absent signals in intracellular cytokine staining represent a multidimensional challenge requiring systematic investigation across the entire experimental workflow. By implementing the structured diagnostic framework and optimized protocols outlined in this application note, researchers can methodically identify failure points and apply evidence-based solutions. Recent methodological advances, including novel fixation-permeabilization buffers incorporating dish soap detergents, have expanded technical capabilities for challenging applications such as simultaneous detection of transcription factors and cytokines [10]. Through rigorous validation of stimulation conditions, fixation-permeabilization efficiency, antibody performance, and instrument configuration, researchers can achieve robust, reproducible intracellular cytokine detection essential for accurate characterization of immune responses in basic research and drug development contexts.
Combating High Background and Non-Specific Staining
Within the broader research on intracellular cytokine staining (ICS) in flow cytometry, achieving a high signal-to-noise ratio is paramount for data accuracy and reproducibility. High background and non-specific staining represent significant technical hurdles that can obscure true positive signals, particularly when analyzing rare cell populations or low-abundance cytokines. These artifacts can stem from various sources, including suboptimal fixation and permeabilization, inadequate antibody titration, or poor instrument calibration [64] [65]. This application note provides a detailed, actionable framework for researchers to identify, troubleshoot, and prevent the common causes of high background, thereby enhancing the reliability of intracellular cytokine data in drug development and immunology research.
Troubleshooting Guide: Common Causes and Solutions
A systematic approach is essential for diagnosing the root causes of excessive background fluorescence. The following table summarizes frequent issues, their underlying causes, and validated solutions.
Table 1: Troubleshooting Guide for High Background and Non-Specific Staining
| Problem Observed | Potential Cause | Recommended Solution |
|---|---|---|
| No signal or weak fluorescence intensity | The intracellular target is not accessible due to inadequate permeabilization [64]. | Ensure adequate permeabilization for internal staining. Verify that the permeabilization buffer system (e.g., detergent vs. alcohol) is appropriate for the target antigen (cytoplasmic vs. nuclear) [27]. |
| The fluorochrome conjugate is too large for intracellular staining [64]. | Use fluorochromes with low molecular weight for intracellular staining to improve antibody motility and cell entry. | |
| High background / Non-specific staining | The antibody concentration is too high [64]. | Titrate all antibodies to determine the optimal concentration that minimizes non-specific binding while retaining a strong specific signal. |
| The gain is too high or the offset is too low on the flow cytometer [64]. | Re-configure the instrument using a positive control. Adjust the offset to reduce background from small particles and decrease the gain. | |
| Inadequate washing, leading to trapped excess antibody [64]. | Ensure adequate washing steps are performed. Include detergents like Tween or Triton in the wash buffers to improve removal of unbound antibody [64] [10]. | |
| Non-specific binding of the secondary antibody [64]. | Select a secondary antibody that does not cross-react with non-target species in the sample. | |
| Sample autofluorescence [64]. | Include an unstained cell control to gauge the level of autofluorescence. | |
| High side scatter background | Cell lysates or bacterial contamination creating small particles [64]. | Ensure samples are fresh and prepared correctly. Avoid excessive centrifugal force or vortexing. Maintain sterile techniques to prevent contamination. |
| Two or more cell populations observed | Cell doublets are present [64]. | Gently mix the cell suspension before staining and acquisition. Filter cells through a nylon mesh (e.g., 30 µm) to remove clumps. |
Detailed Experimental Protocols
Standardized Two-Step Protocol for Intracellular Cytokines
This protocol is recommended for the detection of cytoplasmic proteins, cytokines, or other secreted proteins and allows for the simultaneous analysis of cell surface molecules [27]. The fixation step stabilizes cellular structures, while permeabilization creates pores allowing antibody access to the interior.
Materials:
- Intracellular Fixation & Permeabilization Buffer Set (e.g., Thermo Fisher, cat. no. 88-8824) [27]
- Flow Cytometry Staining Buffer (e.g., cat. no. 00-4222) [27]
- Protein Transport Inhibitor (e.g., Brefeldin A or Monensin) [27]
- Fixable Viability Dye (FVD) - recommended [27]
- Directly conjugated antibodies against surface markers and cytokines
Procedure (in 96-well plate format):
- Cell Stimulation & Harvest: Prepare a single-cell suspension. Activate cells using an appropriate stimulus (e.g., PMA/Ionomycin for T cells, LPS for monocytes) in the presence of a protein transport inhibitor (e.g., Brefeldin A) for the final hours of culture to block cytokine secretion [27].
- Viability Staining (Optional): Stain cells with a Fixable Viability Dye (FVD) according to manufacturer's instructions to label dead cells for subsequent exclusion during analysis [27].
- Surface Stain: Stain cell surface markers in staining buffer on ice or at 4°C, protected from light. Wash cells to remove unbound antibody [27].
- Fixation: After the final wash, resuspend the cell pellet in residual volume (~100 µL). Add 200 µL of IC Fixation Buffer to each well and pipette to mix thoroughly. Incubate for 20-60 minutes at room temperature, protected from light [27].
- Permeabilization: Centrifuge samples and discard the supernatant. Add 200 µL of 1X Permeabilization Buffer to each well, centrifuge, and discard the supernatant. Repeat this wash step once [27].
- Intracellular Stain: Resuspend the cell pellet in ~100 µL of 1X Permeabilization Buffer. Add directly conjugated antibodies for intracellular cytokine detection. Incubate for at least 30 minutes at room temperature, protected from light [27].
- Final Washes: Add 200 µL of 1X Permeabilization Buffer to each well, centrifuge, and discard the supernatant. Repeat this wash step once [27].
- Acquisition: Resuspend the stained cells in an appropriate volume of Flow Cytometry Staining Buffer. Analyze by flow cytometry [27].
Innovative "Dish Soap Protocol" for Multiplexed Staining
Recent advancements have introduced cost-effective "home-brew" buffers to overcome limitations of commercial kits, particularly for simultaneous detection of transcription factors, cytokines, and fluorescent proteins, which often have conflicting buffer requirements [10]. The following protocol uses a dish soap detergent-based buffer.
Materials:
- Fairy dish soap (or equivalent, e.g., Dawn, Dreft) [10]
- Fixative: 2% formaldehyde with 0.05% Fairy and 0.5% Tween-20 [10]
- Perm Buffer: PBS with 0.05% Fairy [10]
- FACS Buffer: PBS with 2.5% FBS and 2mM EDTA [10]
Procedure:
- Surface Stain: Perform surface staining as normal. Count cells, block Fc receptors, stain with surface marker antibodies, and wash [10].
- Fixation: Centrifuge cells and discard the supernatant. Resuspend the cell pellet in 200 µL of fixative. Incubate for 30 minutes at room temperature in the dark (perform in a fume hood). Centrifuge and remove the supernatant, disposing of formaldehyde waste appropriately [10].
- Permeabilization & Blocking: Resuspend the cell pellet in 100 µL of perm buffer. Incubate for 15-30 minutes at room temperature. Blocking may be done at this stage by adding the blocking serum directly to the perm buffer [10].
- Intracellular Stain: Wash cells twice in FACS buffer. Resuspend in antibody cocktail diluted in FACS buffer and stain overnight at 4°C. Note: Additional permeabilization is not required during this step [10].
- Acquisition: Wash cells twice in FACS buffer and acquire on a flow cytometer [10].
The Scientist's Toolkit: Essential Research Reagents
The selection of appropriate reagents is critical for the success of any intracellular staining experiment. The following table catalogs key solutions and their specific functions.
Table 2: Key Research Reagent Solutions for Intracellular Staining
| Reagent / Material | Function & Application |
|---|---|
| Intracellular Fixation & Permeabilization Buffer Set [27] | A standardized commercial system for detecting cytoplasmic cytokines and chemokines. The fixative cross-links proteins to preserve structure, while the detergent-based permeabilization buffer creates pores in the membrane. |
| Foxp3/Transcription Factor Staining Buffer Set [27] | A commercial buffer set that combines fixation and permeabilization in a single step. It is optimized for nuclear antigens like transcription factors but is also useful for many cytokines [27] [7]. |
| Protein Transport Inhibitors (Brefeldin A, Monensin) [27] | Critical reagents for cytokine staining. They disrupt protein secretion from the Golgi apparatus, causing cytokines to accumulate inside the cell, thereby enhancing the detection signal. |
| Fixable Viability Dyes (FVD) [27] | Amine-reactive dyes that covalently bind to dead cells before fixation. They are essential for excluding dead cells during analysis, which are a major source of non-specific background staining [27]. |
| Dish Soap Detergent (e.g., Fairy/Dawn) [10] | A low-cost, effective surfactant used in "home-brew" permeabilization buffers (e.g., Burton's Better Buffer). It facilitates simultaneous staining of transcription factors and fluorescent proteins, which can be challenging with standard buffers [10]. |
| Quantibrite Beads / Quantum Simply Cellular Beads [66] | Fluorescent calibration beads used for quantitative flow cytometry (QFCM). They convert median fluorescence intensity (MFI) into absolute numbers, such as Antigen Binding Capacity (ABC), enabling standardization across experiments and sites [66]. |
Workflow and Standardization Strategies
Adherence to a strict experimental workflow and post-acquisition reporting standards is crucial for minimizing variability and ensuring data integrity.
Data Acquisition and Reporting Standards
To ensure reproducibility and facilitate peer review, comprehensive documentation of the methodology is required [65].
- Experimental Information: Detail cell preparation methods, including proteases, fixatives, permeabilization reagents, and all fluorescent reagents with vendor, catalog number, and clone designation [65].
- Instrumentation: Specify the flow cytometer model, manufacturer, software, laser lines, and optical filters used [65].
- Data Analysis: Outline the gating strategy, including light scatter, live-dead, doublet exclusion, and fluorescence gates. State the controls used to set gates (e.g., FMO controls) and the software for analysis [65].
Optimizing Fixation and Permeabilization for Different Antigen Targets
In the field of drug discovery and development, intracellular cytokine staining (ICS) via flow cytometry has become an indispensable technique for elucidating cellular effector functions and immune responses at a single-cell level. As the number of drug modalities increases, there is a growing drive to identify meaningful biomarkers and evaluate pharmacokinetic and pharmacodynamic relationships, making robust flow cytometric assays crucial for translational research [45]. The critical foundation of any successful ICS experiment lies in the optimal fixation and permeabilization of cells, processes that must be precisely tailored to the subcellular localization and biochemical properties of the target antigen. Proper technique preserves cellular structure while allowing antibody access to intracellular epitopes, directly impacting data quality and experimental reproducibility [8] [27]. This application note provides detailed methodologies for optimizing these essential sample preparation steps within the broader context of intracellular cytokine staining research, with specific consideration for applications in immunology, oncology, and preclinical drug development.
Theoretical Principles of Fixation and Permeabilization
The Role of Fixation and Permeabilization in Antigen Accessibility
Fixation and permeabilization are sequential chemical processes that modify cellular structure to enable intracellular antibody binding. Fixation stabilizes cellular proteins and structures by cross-linking or precipitating biomolecules, thereby preserving the cellular architecture and preventing degradation [8]. Permeabilization creates pores in the lipid membranes, allowing relatively large antibody molecules to access intracellular compartments [27].
The light scatter properties of cells can be altered by fixation and permeabilization treatments, which must be considered during subsequent flow cytometric analysis and gating [8]. Furthermore, these processes may increase non-specific background staining, which can be mitigated by including extra protein such as BSA or fetal calf serum (FCS) in the staining buffer [27].
Antigen Localization Dictates Method Selection
The subcellular localization of the target antigen is the primary determinant for selecting appropriate fixation and permeabilization methods:
- Cytoplasmic proteins (e.g., cytokines, chemokines): Require mild detergent-based permeabilization after formaldehyde fixation [27].
- Nuclear proteins (e.g., transcription factors): Often perform best with combined fixation/permeabilization protocols using specialized commercial buffer systems [27].
- Cytoskeletal, viral, and some enzyme antigens: Typically give optimal results when fixed with high concentrations of acetone, alcohol, or formaldehyde [8].
- Phosphorylated signaling proteins (e.g., MAPK, STAT proteins): May require methanol-based fixation protocols to preserve epitope integrity [27].
Table 1: Fixation and Permeabilization Methods Based on Antigen Localization
| Antigen Category | Example Targets | Recommended Fixation | Recommended Permeabilization |
|---|---|---|---|
| Secreted Proteins | Cytokines (IFN-γ, TNF-α, IL-2, IL-4) | 1-4% Paraformaldehyde | Mild detergents (Saponin, Tween-20) |
| Nuclear Proteins | Transcription factors (FOXP3) | Commercial fixation/permeabilization concentrates | Commercial permeabilization buffers |
| Cytosolic Proteins | Kinases, metabolic enzymes | Acetone or Alcohol | Triton X-100 or NP-40 |
| Signaling Proteins | Phospho-proteins (MAPK, STAT) | Methanol (-20°C) | Intrinsic (methanol also permeabilizes) |
The following workflow diagram outlines the decision-making process for selecting the appropriate protocol based on the target antigen:
Experimental Protocols
Protocol A: Two-Step Method for Cytoplasmic Proteins
This protocol is recommended for detecting cytoplasmic proteins, cytokines, or other secreted proteins in individual cells following activation in vitro or in vivo [27].
Materials Required
- Intracellular Fixation & Permeabilization Buffer Set (e.g., Thermo Fisher cat. no. 88-8824) [27]
- Flow Cytometry Staining Buffer (e.g., Thermo Fisher cat. no. 00-4222) [27]
- Protein Transport Inhibitors: Brefeldin A Solution (e.g., Thermo Fisher cat. no. 00-4506) or Monensin Solution (e.g., Thermo Fisher cat. no. 00-4505) [27]
- Cell Stimulation Cocktail (plus protein transport inhibitors) (500X) (e.g., Thermo Fisher cat. no. 00-4975) [27]
- Fixable Viability Dyes (optional but recommended) [27]
- Directly conjugated antibodies against target antigens
Step-by-Step Procedure
Cell Preparation and Stimulation:
- Prepare a single-cell suspension with viability of 90-95% [8].
- For cytokine detection, stimulate cells with appropriate activating agents (e.g., PMA/ionomycin for T cells, LPS for monocytes) in the presence of protein transport inhibitors (Brefeldin A or Monensin) for the final hours of culture to enable intracellular cytokine accumulation [27].
Surface Staining:
Fixation:
- After the final wash of surface staining, resuspend cell pellet in residual volume (approximately 100 µL).
- Add 100 µL of IC Fixation Buffer and vortex gently to mix.
- Incubate for 20-60 minutes at room temperature, protected from light [27].
Permeabilization:
- Add 2 mL of 1X Permeabilization Buffer and centrifuge at 400-600 × g for 5 minutes at room temperature. Discard supernatant.
- Repeat the wash step with Permeabilization Buffer.
- Resuspend the fixed cell pellet in 100 µL of 1X Permeabilization Buffer [27].
Intracellular Staining:
- Add directly conjugated primary antibodies for detecting intracellular antigens.
- Incubate for 20-60 minutes at room temperature, protected from light.
- Wash twice with 2 mL of 1X Permeabilization Buffer.
- Resuspend stained cells in an appropriate volume of Flow Cytometry Staining Buffer for acquisition [27].
Protocol B: One-Step Method for Nuclear Proteins
This protocol combines fixation and permeabilization into a single step and is recommended for nuclear antigens such as transcription factors [27].
Materials Required
- Foxp3/Transcription Factor Staining Buffer Set (e.g., Thermo Fisher cat. no. 00-5523) [27]
- Flow Cytometry Staining Buffer (e.g., Thermo Fisher cat. no. 00-4222) [27]
- Normal Serum (e.g., Normal Mouse or Rat Serum) for blocking [27]
- Fixable Viability Dyes (optional but recommended) [27]
- Directly conjugated antibodies
Step-by-Step Procedure
Cell Preparation:
- Prepare a single-cell suspension with high viability (90-95%) [8].
- No prior stimulation is required for constitutive nuclear proteins.
Surface Staining:
- Perform cell surface marker staining following standard protocols.
- Include viability staining if desired.
Combined Fixation/Permeabilization:
- After the final wash of surface staining, thoroughly resuspend cell pellet.
- Add 1 mL of freshly prepared Foxp3 Fixation/Permeabilization working solution.
- Incubate for 30-60 minutes at room temperature, protected from light.
- Centrifuge at 400-600 × g for 5 minutes and discard supernatant [27].
Intracellular Staining:
- Wash cells once with 2 mL of 1X Permeabilization Buffer.
- Resuspend cells in 100 µL of 1X Permeabilization Buffer.
- [Optional] Block with 2% normal serum for 15 minutes at room temperature.
- Add directly conjugated antibodies for nuclear antigens without washing.
- Incubate for at least 30 minutes at room temperature, protected from light.
- Wash twice with 2 mL of 1X Permeabilization Buffer.
- Resuspend in Flow Cytometry Staining Buffer for analysis [27].
Protocol C: Methanol Fixation for Phosphorylated Signaling Proteins
This protocol is recommended for some phosphorylated signaling proteins that may not work well with standard buffer systems [27].
Materials Required
- Methanol (pre-cooled to -20°C)
- Flow Cytometry Staining Buffer (e.g., Thermo Fisher cat. no. 00-4222) [27]
- Fixable Viability Dyes
- Directly conjugated antibodies
Step-by-Step Procedure
Cell Preparation and Stimulation:
- Prepare single-cell suspension as described in Protocol A.
- Stimulate cells with appropriate activating conditions if examining inducible phosphorylation events.
Surface Staining (optional):
- Note that methanol fixation may destroy some surface epitopes.
- If required, perform surface staining before fixation using antibodies known to be methanol-resistant.
Methanol Fixation:
- After stimulation, centrifuge cells and remove supernatant completely.
- Gently resuspend cell pellet in pre-cooled 90% methanol (-20°C).
- Incubate for 10 minutes at -20°C [8].
- Note: Acetone fixation (10-15 minutes on ice) may be used as an alternative for some antigens, as acetone also permeabilizes cells [8].
Rehydration and Staining:
- Add 2 mL of Flow Cytometry Staining Buffer to rehydrate cells.
- Centrifuge at 400-600 × g for 5 minutes and discard supernatant.
- Repeat wash step.
- Proceed with intracellular staining as described in Protocol A.
Reagent Selection Guide
The choice of detergents for permeabilization should be guided by the target antigen's subcellular localization and epitope sensitivity:
Table 2: Permeabilization Detergents and Their Applications
| Detergent Type | Examples | Concentration | Mechanism | Suitable For | Limitations |
|---|---|---|---|---|---|
| Harsh Detergents | Triton X-100, NP-40 | 0.1-1% in PBS | Partially dissolves nuclear membrane | Nuclear antigen staining | May disrupt protein epitopes |
| Mild Detergents | Tween 20, Saponin, Digitonin | 0.2-0.5% in PBS | Creates pores without dissolving membranes | Cytoplasmic antigens, plasma membrane proteins | May not provide sufficient access to nuclear targets |
Troubleshooting and Optimization
Common Challenges and Solutions
- High Background Staining: Increase blocking step duration; optimize detergent concentration; include protein (BSA or FCS) in staining buffers; ensure adequate washing steps [8] [27].
- Poor Signal Resolution: Titrate antibody concentrations; verify fixation and permeabilization efficiency; check protein transport inhibitor efficacy for cytokines [27].
- Loss of Cell Surface Epitopes: For methanol-sensitive epitopes, perform surface staining before fixation; test alternative fixation methods [27].
- Altered Light Scatter Properties: Adjust gating strategies as permeabilization affects forward and side scatter profiles; use viability dyes and lineage markers for accurate population identification [8].
Validation and Controls
Appropriate controls are essential for validating intracellular staining assays:
- Stimulation Controls: Include both stimulated and unstimulated cells for cytokine detection [67].
- Isotype Controls: Use matched isotype antibodies at the same concentration as specific antibodies.
- Compensation Controls: Utilize single-stained controls for multicolor panels to account for spectral overlap [68].
- Cell Type-Specific Controls: For complex multicolor panels, employ relevant cell types known to express target antigens during validation [67].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Intracellular Staining
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Fixation Reagents | 1-4% Paraformaldehyde, Methanol, Acetone | Preserves cellular structure and antigen integrity | Paraformaldehyde: general use; Methanol: phospho-proteins; Acetone: cytoskeletal antigens [8] [27] |
| Permeabilization Detergents | Saponin, Triton X-100, Tween-20, Commercial kits | Creates membrane pores for antibody access | Saponin: mild, reversible; Triton X-100: strong, nuclear targets [8] |
| Protein Transport Inhibitors | Brefeldin A, Monensin | Blocks cytokine secretion, enabling intracellular accumulation | Essential for cytokine detection; typically added last 4-18 hours of culture [67] [27] |
| Viability Dyes | Fixable viability dyes (e.g., eFluor series), 7-AAD, DAPI | Distinguishes live/dead cells | DNA-binding dyes (7-AAD, DAPI) cannot be used with fixed cells [8] |
| Commercial Buffer Systems | Intracellular Fixation & Permeabilization Buffer Set, Foxp3/Transcription Factor Staining Buffer Set | Optimized, standardized reagents | Provide consistency and reproducibility [27] |
| Fc Receptor Blocking | Normal serum, species-specific IgG, anti-CD16/CD32 | Reduces nonspecific antibody binding | Critical for reducing background in immune cells [8] |
Optimizing fixation and permeabilization conditions is a critical prerequisite for robust intracellular flow cytometric analysis in drug discovery and development research. The methodologies presented here provide a framework for researchers to tailor their sample preparation to specific antigen targets, thereby ensuring accurate assessment of biomarker modulation, target engagement, and cellular responses in both preclinical models and clinical trials. By implementing these standardized protocols with appropriate controls and validation strategies, scientists can generate high-quality, reproducible data essential for advancing therapeutic candidates through the drug development pipeline.
Fluorochrome Selection and Panel Design to Minimize Spillover
In the realm of intracellular cytokine staining flow cytometry, the precise selection of fluorochromes and the strategic design of multicolor panels are paramount for generating high-quality, reproducible data. This methodology is especially critical in drug development for accurately characterizing immune cell subsets, evaluating cytokine production in T-cells, and monitoring therapeutic responses. The fundamental challenge in multicolor panel design lies in effectively managing fluorescence spillover, a phenomenon where the emission spectrum of one fluorophore is detected in the channel assigned to another, thereby compromising data resolution and accuracy. This application note provides a detailed framework for designing robust flow cytometry panels, with a specific focus on protocols for intracellular cytokine staining and strategies to minimize spectral spillover, thereby enhancing the reliability of research outcomes.
Principles of Fluorochrome Selection
The core of effective panel design lies in matching the physical properties of fluorochromes with the biological context of the target antigens and the technical specifications of the flow cytometer.
- Antigen Density and Fluorochrome Brightness: A foundational rule is to pair bright fluorochromes with low-density antigens and dim fluorochromes with highly expressed antigens [69]. Markers can be categorized as:
- Primary antigens: Expressed at high density, often defining cell lineages.
- Secondary antigens: Often expressed over a continuum.
- Tertiary antigens: Critical markers expressed at low density, such as many cytokines and transcription factors [69].
- Spectral Overlap: The emission spectrum of every fluorophore has a unique width and shape. This emission can spill into the detection channels of neighboring fluorophores [70]. This spillover is not merely an issue of signal intensity; when mathematically corrected, it introduces a "spillover spreading error" that can obscure the resolution of dimly expressed markers [70].
- Tandem Dye Considerations: Tandem dyes, which utilize FRET (Förster Resonance Energy Transfer) to create unique emission peaks, are essential for expanding panel size. However, they can be susceptible to photobleaching and instability, which may lead to donor emission "unquenching" and increased spillover into the donor channel [70] [71]. Quality control of tandem dyes is therefore essential.
Instrument Configuration and Spectral Spillover
Understanding the flow cytometer's configuration is a non-negotiable prerequisite for panel design. The instrument's lasers, optical filters, and detection system define the possible fluorochrome choices and their potential for spillover [69].
Spectral vs. Conventional Flow Cytometry: Conventional flow cytometers use optical filters to direct specific wavelength ranges to each detector. Spillover in this system is managed through a mathematical process called compensation [70]. In contrast, spectral flow cytometers capture the full emission spectrum of each fluorophore across all detectors. Spillover is then resolved through unmixing algorithms, which can differentiate fluorophores with highly overlapping spectra more effectively [72]. Table 1 provides a selection guide for fluorophores on a common 3-laser spectral analyzer, showcasing combinations that were previously challenging, such as distinguishing PerCP from PerCP-eFluor 710 [72].
Table 1: Fluorophore Selection Guide for a 3-Laser Spectral Flow Cytometer
| Emission Range (nm) | Recommended Fluorophores | Emission Max (nm) | Fluorescent Proteins | Other Dyes |
|---|---|---|---|---|
| 400-500 | Alexa Fluor 405, Super Bright 436, eFluor 450, Pacific Blue | 421, 436, 450, 455 | Azurite, CFP, TagBFP | Brilliant Violet 421, Horizon V450 |
| 500-600 | Pacific Orange, eFluor 506 | 550, 510 | EGFP, EYFP | Horizon V500, Brilliant Violet 510 |
| 600-700 | Super Bright 645, Qdot 655 | 645, 655 | - | Brilliant Violet 605, Brilliant Violet 650 |
| 700-800 | Super Bright 780, Qdot 800 | 780, 790 | - | Brilliant Violet 711, Brilliant Violet 785 |
| 500-600 (Green Laser) | Alexa Fluor 488, FITC, PE | 520, 520, 576 | EGFP, RFP | Horizon BB515, VioBright FITC |
| 600-700 (Green Laser) | PE-Cyanine5, PerCP, PE-Cyanine5.5 | 670, 675, 690 | - | PE CF594, Horizon BB700 |
| 700-880 (Green Laser) | PE-Cyanine7, PerCP-eFluor 710, PE-Alexa Fluor 700 | 780, 710, 720 | - | PE Vio770, PerCP-Vio 710 |
The spillover-spreading matrix (SSM) is a critical tool for panel design. It quantitatively represents the degree to which one fluorophore's signal spreads into another's detection channel [70]. When consulting an SSM, a general rule of thumb is that combinations with values above 10 require careful scrutiny and should be avoided for markers that are co-expressed on the same cell population [70].
Quantitative Spillover and Staining Index Data
Empirical data is crucial for making informed decisions. The staining index (SI) provides a quantitative measure of a fluorochrome's ability to distinguish a positive signal from background noise. Figure 4 from the search results ranks 53 fluorophores based on their decreasing SI value, serving as an essential reference for selecting the most effective fluorophore for a given application [72].
Furthermore, spread matrices, often provided by reagent manufacturers or panel design software, are indispensable. These matrices visually represent the level of spillover spreading between all fluorophore pairs in a panel. Darker red shading in such a matrix indicates a higher level of spread, signaling a combination that needs closer attention during panel design and data interpretation [72].
Table 2: Key Metrics for Selected Fluorophores in Spectral Flow Cytometry
| Fluorophore | Excitation Laser | Emission Max (nm) | Relative Brightness | Staining Index Ranking [72] | Key Compatibility Notes |
|---|---|---|---|---|---|
| Brilliant Violet 421 | Violet | 421 | High | Varies by instrument | Check similarity index with dyes like StarBright Violet 440 [70]. |
| Alexa Fluor 488 | Blue | 520 | High | High | Compatible with EGFP; consider spillover into FITC channel [72]. |
| PE | Blue | 576 | Very High | Very High | Bright; ideal for low-density antigens. Tandem dyes require QC [69] [71]. |
| APC | Red | 660 | High | High | Can be distinguished from Alexa Fluor 647 on spectral cytometers [72]. |
| PE-Cy7 | Blue | 780 | High | High | Tandem dye; monitor stability to prevent unquenching and spillover [70]. |
| PerCP-eFluor 710 | Blue | 710 | Medium | Medium | Can be discriminated from PerCP on spectral systems via far-red channels [72]. |
A Unified Protocol for Intracellular Cytokine Staining
The following detailed protocol is optimized for the simultaneous detection of cytokines, transcription factors, and endogenous fluorescent proteins, integrating a novel, cost-effective permeabilization solution.
Surface Stain and Fixation
- Cell Preparation: Harvest and wash cells, then resuspend in a suspension buffer (e.g., PBS with 5-10% FCS) at a concentration of 0.5–1 x 10^6 cells/mL [8].
- Viability Staining: Resuspend the cell pellet in an appropriate amine-reactive viability dye (e.g., LIVE/DEAD Fixable Red Dead Cell Stain) and incubate for 20 minutes at room temperature in the dark. Choose a dye whose emission does not overlap with your key fluorophores [7] [8].
- Fc Receptor Blocking: Incubate cells with an FcR blocking reagent (e.g., purified anti-CD16/CD32 antibody, human IgG, or 2-10% serum) for 30-60 minutes at 4°C to prevent non-specific antibody binding [7] [8].
- Surface Marker Staining: Stain cells with pre-titrated antibodies against surface markers (e.g., CD3, CD4, CD8) for 30 minutes at 4°C in the dark [7]. Wash cells twice with suspension buffer.
- Fixation: Resuspend the cell pellet in 200 µl of fixative. The "Dish Soap Protocol" utilizes a novel fixative containing 2% formaldehyde, 0.05% Fairy dish soap, and 0.5% Tween-20. Incubate for 30 minutes at room temperature in a fume hood [10].
Permeabilization and Intracellular Stain
- Permeabilization: Centrifuge cells and remove the formaldehyde-containing supernatant. Resuspend the pellet in 100 µl of perm buffer (PBS with 0.05% Fairy dish soap). Incubate for 15-30 minutes at room temperature. Additional blocking can be performed at this stage by adding the block directly to the perm buffer [10].
- Intracellular Antibody Staining: Without washing out the perm buffer, add antibodies against intracellular targets (e.g., IFN-γ, transcription factors) and incubate overnight at 4°C in the dark. The protocol notes that additional permeabilization is neither necessary nor recommended [10].
- Acquisition: Wash cells twice in FACS buffer and acquire data on a flow cytometer. For transcription factors and cytokines, the use of the Foxp3/transcription factor buffer set is also a validated approach [7].
ICS Experimental Workflow
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Intracellular Cytokine Staining
| Reagent / Material | Function / Purpose | Example Products / Formulations |
|---|---|---|
| Fc Receptor Block | Prevents non-specific antibody binding via Fc receptors. | Purified anti-CD16/CD32 [7], human IgG, 2-10% goat serum [8]. |
| Amine-Reactive Viability Dye | Distinguishes live from dead cells; fixable for use after staining. | LIVE/DEAD Fixable Aqua/Red Dead Cell Stain [7]. |
| Fixative | Preserves cellular structure and crosslinks proteins. | 2-4% Paraformaldehyde (PFA) [8]; "Burton's Better Buffer" (2% PFA, 0.05% Fairy, 0.5% Tween) [10]. |
| Permeabilization Buffer | Disrupts membranes to allow antibody entry into the cell. | Saponin, Triton X-100 [8]; "Perm Buffer" (0.05% Fairy in PBS) [10]; Foxp3/Transcription Factor Buffer Set [7]. |
| Protein Transport Inhibitor | Allows cytokine accumulation inside cells for detection. | Brefeldin A-containing cocktail [7]. |
| Wash / Staining Buffer | Medium for washing and resuspending cells. | PBS with 2-10% FBS/BSA and optional EDTA [10] [8]. |
| Spectral Flow Cytometer | Instrument for high-parameter analysis with unmixing capability. | Cytek Aurora, Sony SA3800 [72]. |
Panel Design Workflow and Validation
A systematic approach to panel design is critical for success. The process can be broken down into five key steps [69]:
- Define Your Experimental Hypothesis: Identify the biological question, the specific cell populations of interest, and the cellular location (surface or intracellular) of your targets [69].
- Marker Selection: Choose markers that define your populations of interest, paying close attention to their expression levels (high, continuum, low) and potential co-expression patterns [69].
- Know Your Flow Cytometer: Understand the instrument's laser wavelengths, the number of detectors per laser, and the optical filters available. This information dictates which fluorochromes can be detected [69].
- Fluorochrome Assignment: Use tools like spectrum viewers and spillover-spreading matrices to assign fluorochromes to markers. The goal is to pair bright fluorochromes with low-density antigens and minimize spillover between fluorochromes used on co-expressed markers [69] [72] [70].
- Panel Review and Validation: Titrate all antibodies and include the necessary controls: compensation controls (single-stained beads or cells), fluorescence-minus-one (FMO) controls to set gates accurately, and biological controls [69].
Panel Design Workflow
In the realm of intracellular cytokine staining (ICS) for flow cytometry, the reliability of experimental data is paramount, particularly in translational research and drug development. The fixation and permeabilization steps required to access intracellular antigens introduce significant technical challenges, including increased autofluorescence, heightened non-specific antibody binding, and alterations in light scatter properties [27]. Without appropriate controls, these factors can compromise data integrity, leading to both false positive and false negative results. Proper implementation of Fluorescence Minus One (FMO), isotype, and viability controls is therefore not merely a technical formality but a critical component of rigorous experimental design [73] [74]. This application note details the strategic deployment of these essential controls within ICS assays, providing validated protocols to ensure the accurate identification and quantification of cytokine-producing cells.
The Control Trinity: Purposes and Applications
Defining the Core Controls
The following table summarizes the primary applications and limitations of the three critical controls in ICS flow cytometry.
Table 1: Key Characteristics of Critical Flow Cytometry Controls
| Control Type | Primary Function | Optimal Use Case | Common Misapplications |
|---|---|---|---|
| Viability Staining | Discriminate live/dead cells; reduce artifacts from dead cells [73] | All intracellular staining experiments; essential when using fixed/permeabilized cells [75] | Using DNA-binding dyes (PI, 7-AAD) in fixation protocols requiring permeabilization [75] |
| FMO Control | Accurately set boundaries for positive/negative populations; account for fluorescence spread [73] [76] | Defining positivity for low-abundance cytokines or markers with extensive spectral overlap [73] | Using an unstained control instead of an FMO to set gates in multicolor panels [73] |
| Isotype Control | Qualitatively assess background from non-specific antibody binding [73] [74] | Verifying effectiveness of Fc receptor blocking; assessing cellular "stickiness" [74] | Using to set positive/negative gates; subtracting values from specific antibody signal [74] |
Strategic Implementation in Experimental Design
The decision-making process for incorporating these controls is visualized in the following workflow.
For intracellular cytokine staining, viability controls are non-negotiable. The fixation and permeabilization process can exacerbate the autofluorescence and non-specific binding characteristic of dead cells, potentially leading to inaccurate cytokine frequency measurements [73] [75]. FMO controls are particularly crucial in multicolor ICS panels to correctly identify populations positive for cytokines that are produced at low frequencies or whose expression is continuous rather than bimodal [73] [76]. Isotype controls have a more limited, specific role; they are useful for troubleshooting high background staining and verifying the efficacy of Fc receptor blocking steps but should not be used for setting positivity gates [74].
Detailed Experimental Protocols
Protocol for Viability Staining and Intracellular Cytokine Staining
This protocol integrates a viability dye with intracellular cytokine staining, using a formaldehyde/saponin method suitable for detecting cytoplasmic proteins like cytokines [53] [27].
Materials & Reagents:
- Cell Preparation: Single-cell suspension of stimulated cells (e.g., PBMCs).
- Stimulation & Transport Inhibition: Cell Stimulation Cocktail (e.g., PMA/Ionomycin), Protein Transport Inhibitor (e.g., Brefeldin A or Monensin) [1] [27].
- Viability Stain: Fixable Viability Dye (FVD) - e.g., eFluor 780 [27]. Note: Do not use DNA-binding dyes like PI or 7-AAD as they are incompatible with permeabilization.
- Surface Stain: Antibodies against surface markers (e.g., CD4, CD8).
- Fixation & Permeabilization: Intracellular Fixation & Permeabilization Buffer Set (e.g., Thermo Fisher, cat. no. 88-8824) [27].
- Intracellular Stain: Antibodies against intracellular cytokines (e.g., IFN-γ, IL-2).
- Staining Buffer: Flow Cytometry Staining Buffer (PBS with BSA or FBS) [27].
Procedure:
- Stimulation: Stimulate cells with the appropriate antigen or mitogen (e.g., PMA/Ionomycin) for the required duration (e.g., 4-6 hours for T cells). Add a protein transport inhibitor like Brefeldin A for the final 2-4 hours of culture to cause cytokine accumulation within the cell [1] [53].
- Viability Staining: After stimulation, wash cells and resuspend in PBS. Stain with the Fixable Viability Dye according to the manufacturer's instructions. This step must be performed before fixation. [27]
- Surface Staining: Wash away excess viability dye. Resuspend the cell pellet in staining buffer and incubate with antibodies against surface markers for 20-30 minutes on ice or at 4°C, protected from light [27].
- Fixation: Wash cells to remove unbound surface antibodies. Thoroughly resuspend the cell pellet in the residual volume (≈100 µL) and add 100-200 µL of IC Fixation Buffer. Vortex and incubate for 20-60 minutes at room temperature, protected from light [27].
- Permeabilization: Add 2 mL of 1X Permeabilization Buffer and centrifuge. Discard the supernatant. Repeat this wash step once [27].
- Intracellular Staining: Resuspend the fixed and permeabilized cell pellet in 100 µL of 1X Permeabilization Buffer. Add directly conjugated antibodies against intracellular cytokines and incubate for 20-60 minutes at room temperature, protected from light. All subsequent steps must be done in permeabilization buffer. [27]
- Washing and Acquisition: Wash cells twice with 2 mL of 1X Permeabilization Buffer to remove unbound antibody. Resuspend the final cell pellet in an appropriate volume of Flow Cytometry Staining Buffer and acquire data on a flow cytometer [27].
Protocol for FMO Control Preparation
FMO controls are essential for accurate gating in multicolor ICS panels. The following describes a master mix strategy for their preparation [76].
Procedure:
- Panel Definition: Identify the specific fluorochrome for which positivity is difficult to determine due to spectral overlap or a dim signal.
- Master Mix Creation: For a given FMO control (e.g., IFN-γ-FITC FMO), create a master mix of antibodies containing all antibodies in the panel except for the one being controlled (IFN-γ-FITC).
- Staining: Add this master mix to a separate aliquot of cells (that has undergone the same stimulation, viability, and surface staining steps as the full stain sample).
- Parallel Processing: This FMO control tube must be fixed, permeabilized, and washed in parallel with the fully stained sample.
- Acquisition and Gating: Acquire the FMO control and use it to set the negative-positive boundary for the channel of the omitted antibody.
The Scientist's Toolkit: Essential Research Reagents
Successful execution of controlled ICS experiments relies on a suite of specialized reagents. The following table catalogs these key materials and their critical functions.
Table 2: Essential Reagents for Intracellular Cytokine Staining and Controls
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Cell Stimulators | PMA (Phorbol ester) & Ionomycin (Calcium ionophore); specific antigen peptides [1] [53] | Provides a non-specific or antigen-specific activation signal to immune cells, triggering cytokine production pathways. |
| Protein Transport Inhibitors | Brefeldin A; Monensin [1] [27] | Disrupts Golgi apparatus function, preventing cytokine secretion and allowing intracellular accumulation for detection. |
| Viability Dyes | Fixable Viability Dyes (e.g., eFluor 450, eFluor 780); amine-reactive dyes [75] [27] | Distinguishes live from dead cells via membrane integrity/esterase activity; critical for pre-fixation use. |
| Fixation/Permeabilization Kits | Intracellular Fixation & Permeabilization Buffer Set (for cytokines); Foxp3/Transcription Factor Staining Buffer Set (for nuclear antigens) [27] | Fixatives cross-link proteins to preserve structure; detergents (e.g., saponin) solubilize membranes for antibody access. |
| Blocking Reagents | Fc Receptor Blocking Solution; Normal Serum (e.g., Mouse, Rat) [73] [27] | Binds to Fc receptors on myeloid cells, preventing non-specific binding of antibodies via their Fc region. |
| Compensation Beads | Anti-Ig Capture Beads; UltraComp Beads [75] | Used with single-stained samples to calculate the compensation matrix and correct for spectral spillover. |
| Validated Antibody Panels | Pre-titrated, conjugated antibodies against surface markers, cytokines, and transcription factors. | Ensures specificity and optimal signal-to-noise ratio; reduces validation workload for the researcher. |
Data Interpretation and Analysis
Gating Strategy and Control Integration
A hierarchical gating strategy that integrates all controls is vital for clean data. The following diagram outlines a standard workflow for analyzing ICS data, highlighting where each control is applied.
- Viability Control: The viability dye-negative population is gated to exclude dead cells. This significantly reduces background autofluorescence and non-specific antibody binding, providing a cleaner baseline for subsequent analysis [73] [75].
- FMO Control: Once the population of interest (e.g., CD4+ T cells) is identified in the fully stained sample, the FMO control is used to set the gate for the cytokine-positive population. The boundary is placed at the edge of the negative population in the FMO tube, ensuring that signal from spectral spillover is not misinterpreted as true positivity [73] [76].
- Isotype Control: The isotype control is not used for gating. Instead, it serves as a qualitative check. If the staining intensity of the isotype control in the population of interest is high, it indicates potential issues with non-specific binding or insufficient Fc receptor blocking that need to be addressed protocolically [74].
Troubleshooting Common Issues
- High Background in Isotype Control: Implement an Fc receptor blocking step by adding a specific blocking reagent or excess immunoglobulin (e.g., normal serum) prior to antibody staining [73] [74].
- Poor Separation in FMO Control: Re-titrate the antibody for the problematic channel to improve the signal-to-noise ratio. Ensure the compensation matrix was correctly calculated using bright, single-stained controls (beads or cells) [73] [75].
- Low Cell Recovery Post-Staining: The fixation and permeabilization process can be harsh. Ensure centrifugation speeds are not excessive and that cells are handled gently during washing steps. Using a well-formulated permeabilization buffer is critical [27].
- Loss of Fluorescent Protein Signal (e.g., GFP): Standard transcription factor buffers can destroy fluorescent proteins. Consider optimized fixation/permeabilization buffers, such as the "Dish Soap Protocol" which uses a dishwashing detergent-based formula, to better preserve these signals while allowing nuclear access [10].
Best Practices for Sample Handling and Processing
In the field of intracellular cytokine staining (ICS) for flow cytometry, rigorous sample handling and processing is not merely a preliminary step but the foundational determinant of experimental success. This application note details the critical procedures required to preserve biological relevance and ensure the accuracy of single-cell cytokine data, framed within the broader research context of understanding immune cell function in health, disease, and therapeutic intervention. The methodologies outlined herein are designed to provide researchers, scientists, and drug development professionals with a reliable framework for generating high-quality, reproducible data that can accurately inform on complex immune responses [5] [77].
Critical Parameters for Sample Processing
Successful intracellular cytokine detection hinges on the optimization of several key parameters during sample preparation. The table below summarizes these critical variables and their recommended specifications to guide experimental design.
Table 1: Key Parameters for Intracellular Cytokine Staining Sample Preparation
| Parameter | Recommended Specification | Purpose & Rationale |
|---|---|---|
| Cell Stimulation | PMA (e.g., 50 ng/mL) & Ionomycin (e.g., 500 ng/mL) or antigen-specific stimuli [78] | Provides a strong polyclonal activation signal to T cells, inducing cytokine production. |
| Stimulation Duration | 1-2 hours initial activation, then 4-6 hours with transport inhibitors (4-5 hours total common) [78] | Allows for cytokine gene transcription and subsequent protein synthesis and accumulation. |
| Protein Transport Inhibition | Brefeldin A (e.g., 10 µg/mL) and/or Monensin (e.g., 2 µM) [78] | Blocks Golgi-mediated secretion, causing cytokines to accumulate inside the cell for detection. |
| Fixation | 1-4% Paraformaldehyde for 10-60 minutes at room temperature [27] [79] | Stabilizes cellular structures and cross-links proteins, preventing cytokine leakage. |
| Permeabilization | Detergents like Saponin (e.g., 0.1%) or Triton X-100 in an ongoing buffer [27] [79] | Creates pores in the membrane, allowing intracellular access for antibodies. |
| Cell Viability | >90% viability at start; use of viability dyes is critical [78] | Dead cells cause non-specific antibody binding and must be excluded from analysis. |
Adherence to these parameters mitigates common pitfalls such as low cytokine signal, high background in unstimulated controls, and poor cell viability, which can severely compromise data interpretation [78].
Experimental Protocols
Cell Stimulation and Surface Staining
Objective: To activate cells for cytokine production and stain for surface markers prior to fixation and permeabilization.
Duration: Approximately 6-8 hours.
Materials:
- Complete cell culture medium with serum
- Cell stimulation cocktail (e.g., PMA/Ionomycin) [78]
- Protein transport inhibitors (Brefeldin A, Monensin) [78]
- Flow Cytometry Staining Buffer (PBS with BSA/serum) [27]
- Antibodies for cell surface markers (e.g., CD3, CD4, CD8)
- Fixable Viability Dye (FVD) [27]
- 96-well round-bottom plates
Procedure:
- Prepare Cell Suspension: Isolate immune cells (e.g., PBMCs) and adjust concentration to 1-2 x 10⁶ cells/mL in complete pre-warmed medium [78].
- Stimulate Cells: Distribute 200 µL of cell suspension per well into a 96-well plate. Add stimulation cocktails according to experimental conditions. Include unstimulated controls (medium alone) to assess background cytokine production. Incubate plates for 1-2 hours in a 37°C, 5% CO₂ incubator [78].
- Inhibit Protein Transport: Add protein transport inhibitors (e.g., Brefeldin A to 10 µg/mL) to all wells. Continue the incubation for an additional 4-6 hours. Adhere precisely to timing, as extended culture can lead to cell death [5] [78].
- Harvest and Stain for Viability: Transfer cells to a fresh plate and wash twice with cold staining buffer. Resuspend cells in staining buffer containing a Fixable Viability Dye and incubate for 20-30 minutes on ice or at 4°C in the dark [27] [78].
- Stain Surface Markers: Without washing out the viability dye, add directly conjugated antibodies for cell surface markers. Incubate for 20 minutes at 4°C in the dark [27].
- Wash: Wash cells twice with cold staining buffer to remove unbound antibodies. The cells are now ready for fixation [27].
Fixation, Permeabilization, and Intracellular Staining
Objective: To preserve cellular integrity, permeabilize membranes, and stain for accumulated intracellular cytokines.
Duration: Approximately 2 hours.
Materials:
- Intracellular Fixation Buffer (e.g., 1-4% PFA) [79]
- Permeabilization Buffer (e.g., Saponin-based) [27] [79]
- Antibodies against intracellular cytokines (e.g., IFN-γ, TNF-α, IL-2)
- Flow Cytometry Staining Buffer
Procedure:
- Fix Cells: After the final wash from surface staining, discard the supernatant and resuspend the cell pellet in 100-200 µL of Intracellular Fixation Buffer. Incubate for 20-60 minutes at room temperature, protected from light. Caution: Perform this step in a fume hood when using PFA [27] [10].
- Wash and Permeabilize: Centrifuge cells and discard the fixation buffer. Wash cells once with staining buffer. Add 200 µL of Permeabilization Buffer to the cell pellet, centrifuge, and discard the supernatant. Resuspend the cells in 100 µL of Permeabilization Buffer [27]. Note: Saponin-mediated permeabilization is reversible, so cells must be kept in permeabilization buffer for all subsequent steps to maintain antibody access [79].
- Intracellular Staining: Add directly conjugated antibodies for intracellular cytokines, diluted in Permeabilization Buffer, to the cell suspension. Incubate for 30 minutes at room temperature in the dark [27] [78].
- Final Washes: Wash cells twice with Permeabilization Buffer to remove unbound intracellular antibody. Perform a final wash with regular Staining Buffer to remove detergent before analysis. Resuspend cells in an appropriate volume of Staining Buffer for acquisition on the flow cytometer [27] [78].
Diagram 1: ICS Experimental Workflow
The Scientist's Toolkit: Essential Reagents and Materials
A successful intracellular cytokine staining experiment requires a suite of specialized reagents. The following table catalogs the core solutions and their critical functions within the protocol.
Table 2: Key Research Reagent Solutions for Intracellular Cytokine Staining
| Reagent Solution | Function | Examples & Notes |
|---|---|---|
| Cell Stimulation Cocktail | Activates intracellular signaling pathways to induce cytokine gene expression and synthesis. | PMA/lonomycin for polyclonal T-cell activation; antigen-specific peptides for antigen-specific responses [78]. |
| Protein Transport Inhibitors | Blocks cytokine secretion via the Golgi apparatus, leading to intracellular accumulation. | Brefeldin A, Monensin; often used in combination for enhanced retention of certain cytokines [5] [78]. |
| Fixation Buffer | Crosslinks cellular components, preserving cellular morphology and immobilizing intracellular antigens. | 1-4% Paraformaldehyde; concentration and time can affect epitope integrity [27] [79]. |
| Permeabilization Buffer | Solubilizes lipid membranes to allow intracellular antibody access while maintaining cell structure. | Saponin, Triton X-100, Tween-20; choice depends on target (e.g., saponin for cytokines) [27] [79]. |
| Fc Receptor Block | Blocks non-specific binding of antibodies to Fc receptors on immune cells, reducing background. | Purified IgG or specific blocking antibodies; critical for myeloid cells and activated lymphocytes [5] [79]. |
| Fixable Viability Dye | Covalently labels amines in dead cells, allowing their exclusion during analysis. | Essential for eliminating false positives from non-specifically staining dead cells [5] [27]. |
Data Analysis and Troubleshooting
Flow Cytometry Data Analysis Workflow
Following sample acquisition, a systematic analytical approach is required to accurately identify and quantify cytokine-positive cells.
Diagram 2: Data Analysis Gating Strategy
Key Analysis Steps:
- Exclude Dead Cells and Doublets: Begin analysis by gating on cells with normal forward scatter (FSC) and side scatter (SSC) properties. Subsequently, exclude dead cells using the viability dye channel and exclude doublets by plotting FSC-Height versus FSC-Area to gate on single cells [5] [16].
- Identify Cell Populations: Progressively gate on your population of interest, for example, lymphocytes, then CD3+ T cells, and finally CD4+ or CD8+ T cell subsets [16].
- Set Cytokine-Positive Gates: The threshold for positive cytokine staining must be established using rigorous controls. Fluorescence Minus One (FMO) controls and unstimulated samples are essential for distinguishing true positive signals from background autofluorescence and non-specific antibody binding [16]. Isotype controls are less preferred as they do not account for non-specific staining specific to the antibody clone and fluorophore [78].
- Quantify Results: Report both the frequency of cytokine-positive cells within the parent population and the Median Fluorescence Intensity (MFI), which provides a relative measure of the amount of cytokine produced per cell [16].
Troubleshooting Common Issues
Even with optimized protocols, challenges can arise. The table below outlines common problems, their potential causes, and recommended solutions.
Table 3: Troubleshooting Guide for Intracellular Cytokine Staining
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low Cytokine Signal | Suboptimal stimulation; inactive transport inhibitor; antibody issues. | Perform dose-response and time-course stimulation experiments; verify inhibitor activity; titrate antibodies [78]. |
| High Background in Unstimulated Controls | Non-specific antibody binding; cellular activation during handling; contamination. | Titrate antibodies; include Fc receptor block; minimize cell handling time; use fresh, sterile media [5] [78]. |
| Poor Cell Viability Post-Stimulation | Over-stimulation; extended culture; toxic reagents. | Optimize stimulation strength and duration; verify incubator conditions; assess viability at multiple time points [78]. |
| High Variation Between Replicates | Inconsistent cell numbers; uneven processing; unstable cytometer. | Standardize cell counting; use multi-channel pipettes for high-throughput steps; perform cytometer QC daily [78]. |
| Loss of Surface Antigen Signal | Fixation too harsh or prolonged. | Optimize fixation concentration and time; verify antibody clones are compatible with fixation conditions [27]. |
Mastering sample handling and processing is a critical competency in intracellular cytokine staining flow cytometry. The protocols and best practices detailed in this application note provide a robust foundation for generating reliable, high-quality data that can withstand rigorous scientific scrutiny. By meticulously controlling from cell stimulation through to final data analysis, researchers can confidently utilize this powerful technique to uncover novel insights into immune function, disease mechanisms, and the mode of action of therapeutic agents.
Beyond the Benchmark: Validating ICS Assays and Comparative Performance Analysis
In the field of immunology research and diagnostic development, accurately measuring T-cell responses is critical for advancing our understanding of infectious diseases, vaccine efficacy, and immunotherapies. Two prominent techniques have emerged for this purpose: Intracellular Cytokine Staining (ICS) using flow cytometry and QuantiFERON assays that detect interferon-gamma (IFN-γ) release. While both methods ultimately measure cytokine production as a readout of immune activation, they differ fundamentally in their technical approaches, performance characteristics, and applications. This application note provides a direct comparison of these methodologies, focusing on their relative sensitivity and specificity, to guide researchers in selecting the optimal approach for their experimental and clinical objectives.
Technical Principles and Mechanisms
Intracellular Cytokine Staining (ICS)
ICS is a flow cytometry-based technique that enables detection of cytokine production at the single-cell level. The assay involves stimulating cells ex vivo, typically with antigens or nonspecific activators, in the presence of protein transport inhibitors such as Brefeldin A that prevent cytokine secretion, leading to intracellular accumulation. Cells are then fixed, permeabilized, and stained with fluorescently-labeled antibodies against specific cytokines and cell surface markers, allowing for precise identification of the frequency, phenotype, and functional capacity of cytokine-producing cells [7] [1].
QuantiFERON Assays
QuantiFERON assays are bulk population measurements based on enzyme-linked immunosorbent assay (ELISA) or enzyme-linked immunospot (ELISPOT) methodologies. These tests detect IFN-γ released into the supernatant (ELISA) or captured on a membrane (ELISPOT) by T-cells in response to Mycobacterium tuberculosis-specific antigens (ESAT-6 and CFP-10). The key distinction is that QuantiFERON provides a composite measure of T-cell response without revealing the specific cellular sources or phenotypic characteristics of the responding cells [80] [81].
Performance Comparison: Sensitivity and Specificity
Diagnostic Performance in Tuberculosis Detection
Multiple studies have directly compared the performance of ICS and QuantiFERON technologies, particularly in the context of tuberculosis detection. The table below summarizes key performance metrics from clinical studies:
Table 1: Comparative Performance of IGRA Methods in TB Diagnosis
| Assay Method | Technique | Sensitivity (%) | Specificity (%) | Study Population |
|---|---|---|---|---|
| X-DOT-TB | ELISPOT-based IGRA | 79.5 (95% CI: 77.4-81.5) | 85.1 (95% CI: 83.2-87.0) | Pakistani population, high TB burden [80] |
| QFT-Plus | ELISA-based IGRA | 55.7 (95% CI: 52.9-58.5) | 78.1 (95% CI: 75.3-80.9) | Pakistani population, high TB burden [80] |
| QFT-Plus vs. QFT-GIT | ELISA-based IGRA | 1.3% higher (95% CI: -0.3 to 2.9) | 0.9% lower (95% CI: -2.4 to 0.6) | Meta-analysis of multiple studies [81] |
| Tuberculin Skin Test (TST) | Skin induration | 35.8 (95% CI: 34.4-37.1) | 82.2 (95% CI: 80.3-84.1) | Pakistani population, high TB burden [80] |
Key Performance Observations
- ELISPOT-based IGRAs (X-DOT-TB) demonstrate significantly higher sensitivity (79.5%) compared to ELISA-based formats (QFT-Plus at 55.7%) in high TB-burden, BCG-vaccinated populations [80].
- The QuantiFERON technology platform shows consistent performance across generations, with QFT-Plus demonstrating similar sensitivity and specificity to its predecessor QFT-GIT [81].
- Both IGRA methods outperform the traditional Tuberculin Skin Test (TST) in sensitivity while maintaining comparable specificity [80].
Detailed Experimental Protocols
ICS Protocol with Optimized Dish Soap Method
The following protocol, adapted from the "Dish Soap Protocol" utilizing "Burton's Better Buffer," enables simultaneous efficient detection of transcription factors, cytokines, and endogenous fluorescent proteins at substantially reduced cost compared to commercial buffers [10].
Surface Staining and Fixation
- Perform surface staining as normal: Count cells, block Fc receptors using anti-CD16/32 antibody or serum, stain with surface marker antibodies, and wash [10] [7].
- After surface staining, centrifuge cells at 400-600 × g for 5 minutes at room temperature and discard supernatant.
- Resuspend cell pellet in 200 µl fixative (2% formaldehyde with 0.05% Fairy dish soap and 0.5% Tween-20). Incubate 30 minutes at room temperature in the dark in a fume hood.
- Centrifuge 5 minutes at 600 × g, remove supernatant, and dispose of formaldehyde-containing buffers appropriately [10].
Permeabilization and Intracellular Staining
- Resuspend in 100 µl perm buffer (PBS with 0.05% Fairy dish soap). Incubate 15-30 minutes at room temperature. Fc receptor blocking may be repeated at this stage.
- Wash twice in FACS buffer (PBS with 2.5% FBS and 2mM EDTA).
- Stain overnight with antibodies against intracellular targets (cytokines, transcription factors) in FACS buffer at 4°C.
- Wash twice in FACS buffer and acquire samples on a flow cytometer [10].
Reagent Formulations
- Fixative: 2% formaldehyde with 0.05% Fairy dish soap and 0.5% Tween-20
- Permeabilization Buffer: PBS with 0.05% Fairy dish soap
- FACS Buffer: PBS with 2.5% FBS and 2mM EDTA [10]
QuantiFERON Assay Protocol
Blood Collection and Stimulation
- Collect blood samples by venipuncture directly into QuantiFERON blood collection tubes.
- Include four tubes: Nil (background control), Mitogen (positive control), TB1 (CD4+ T-cell stimulus), and TB2 (CD4+ and CD8+ T-cell stimulus) for QFT-Plus.
- Invert tubes 10 times immediately after collection to ensure mixing of antigens.
- Incubate tubes within 16 hours of collection at 37°C for 16-24 hours [80] [81].
Plasma Separation and IFN-γ Detection
- After incubation, centrifuge tubes and collect plasma supernatant.
- Measure IFN-γ concentration in plasma samples using ELISA.
- Calculate results: Subtract Nil value from TB Antigen and Mitogen values. QFT-Plus is considered positive if TB Antigen response is ≥0.35 IU/mL IFN-γ and above 25% of Nil value [81].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for ICS and QuantiFERON Assays
| Reagent | Function | Application | Example Formulations |
|---|---|---|---|
| Protein Transport Inhibitors | Inhibits protein secretion, causing intracellular cytokine accumulation | ICS | Brefeldin A, Monensin [7] [1] |
| Fixation Reagents | Crosslinks proteins to maintain cellular structure during permeabilization | ICS | 2-4% Paraformaldehyde, "Burton's Better Buffer" with dish soap [10] |
| Permeabilization Detergents | Solubilizes membranes to enable antibody access to intracellular targets | ICS | Saponin, Fairy dish soap, Tween-20, Triton X-100 [10] |
| Mycobacterium tuberculosis Antigens | Stimulates MTb-specific T-cells to produce IFN-γ | QuantiFERON | ESAT-6, CFP-10, synthetic peptide chains [80] [81] |
| Fc Receptor Blocking Agents | Reduces nonspecific antibody binding | Both ICS and QuantiFERON | Anti-CD16/32 antibodies, serum proteins [7] |
| Cell Stimulation Cocktails | Activates T-cells through nonspecific signaling pathways | ICS | PMA and Ionomycin [1] |
Critical Methodological Considerations
Advantages and Limitations of ICS
Key Advantages:
- Single-cell resolution enables identification of specific cytokine-producing cell subsets and their phenotypic characteristics [1]
- Multiparameter analysis allows simultaneous assessment of multiple cytokines and cell surface markers [77]
- Flexible experimental design accommodates various stimulation conditions and staining panels [1]
Technical Limitations:
- Requires specialized equipment (flow cytometer) and technical expertise
- More variable between laboratories compared to standardized kit-based methods
- Cell fixation and permeabilization can damage certain epitopes and affect antibody binding [10]
Advantages and Limitations of QuantiFERON
Key Advantages:
- Standardized format ensures consistency across laboratories and studies [81]
- Simpler workflow requires less specialized equipment and training
- High throughput capacity suitable for large clinical studies and screening programs [80]
Technical Limitations:
- No cellular resolution cannot identify specific T-cell subsets responsible for response [80]
- Limited to IFN-γ detection unlike ICS which can measure multiple cytokines
- Reduced sensitivity in immunocompromised populations and young children [81]
The choice between ICS and QuantiFERON methodologies depends heavily on the specific research questions and clinical applications. ICS provides superior cellular resolution and multidimensional data on immune cell function, making it ideal for mechanistic studies, vaccine development, and immunotherapy monitoring. In contrast, QuantiFERON offers standardized, reproducible results suitable for clinical diagnostics and large-scale screening programs, particularly for tuberculosis infection.
Recent advancements in ICS protocols, particularly the development of cost-effective fixation and permeabilization buffers using dish soap detergents, have addressed previous limitations in simultaneous detection of transcription factors, cytokines, and fluorescent proteins [10]. Meanwhile, improvements in QuantiFERON technology, including the addition of CD8+ T-cell targeting antigens in QFT-Plus, aim to enhance detection sensitivity in challenging populations [81].
Researchers should consider their specific needs for cellular resolution, throughput, and clinical applicability when selecting between these powerful techniques for assessing cellular immune responses.
Within the framework of intracellular cytokine staining (ICS) flow cytometry research, a comprehensive immune response profile is not achieved through a single, isolated technique. ICS provides unparalleled detail on cellular source and co-expression patterns but exists within a broader ecosystem of immunoassays. Correlative data from other modalities are often essential to validate findings and build a complete picture of immune functionality. This application note details the core principles, protocols, and synergistic relationships between ICS, the Enzyme-Linked Immunosorbent Assay (ELISA), the Enzyme-Linked ImmunoSpot (ELISpot) assay, and bead-based multiplex immunoassays. By understanding the specific output and application of each method, researchers can design robust experimental strategies for advanced immunology research and drug development.
Core Assay Principles and Comparative Analysis
The selection of an appropriate immunoassay is dictated by the specific research question, whether it pertains to the concentration of a soluble analyte, the frequency of analyte-secreting cells, or the complex phenotype of the responding cells.
- ELISA (Enzyme-Linked Immunosorbent Assay): A plate-based assay designed for the detection and quantification of soluble proteins, such as cytokines, antibodies, or hormones, in biological fluids like serum, plasma, or cell culture supernatant [18] [17]. It provides a bulk measurement of analyte concentration but no information on the cellular source [18].
- ELISpot (Enzyme-Linked ImmunoSpot): A highly sensitive immunoassay for the enumeration of individual cells actively secreting a specific protein [82] [18]. Unlike ELISA, it provides a functional readout and can detect rare antigen-specific T or B cells within a population of peripheral blood mononuclear cells (PBMCs) [82] [17].
- Multiplex Bead-Based Assays (e.g., Luminex): These assays leverage microspheres (beads) embedded with varying ratios of fluorescent dyes, creating a family of combinatorially colored labels [83]. Each bead set can be coated with a capture antibody for a different analyte, allowing for the simultaneous quantification of multiple analytes from a single, small-volume sample [82] [84].
- Intracellular Cytokine Staining (ICS) with Flow Cytometry: A powerful technique that enables the simultaneous assessment of multiple phenotypic (e.g., CD4, CD8), differentiation, and functional (i.e., cytokine production) parameters at the single-cell level [25]. It allows for the identification of polyfunctional T-cells expressing multiple effector molecules simultaneously [25].
Comparative Assay Characteristics
The table below summarizes the key characteristics of these techniques to guide assay selection.
Table 1: Comparative Analysis of Key Immunoassay Modalities
| Feature | ELISA | ELISpot | Multiplex Bead Assay | ICS/Flow Cytometry |
|---|---|---|---|---|
| What is Detected | Soluble protein concentration | Number of protein-secreting cells | Concentration of multiple soluble proteins | Intracellular cytokines & cell surface markers |
| Sample Type | Serum, plasma, supernatant | Live cells (e.g., PBMCs) | Serum, plasma, supernatant | Live cells (e.g., PBMCs, whole blood) |
| Sensitivity | Moderate to High | Very High [85] [17] | Moderate to High | High |
| Resolution | Bulk population, no cellular data | Single-cell (secretion activity) | Bulk population, no cellular data | Single-cell (phenotype & function) |
| Readout | Optical Density (OD) by plate reader | Spot-forming units (SFU) by ELISpot reader | Median Fluorescence Intensity (MFI) by flow-based reader | Fluorescence by flow cytometer |
| Multiplexing Capacity | Single-plex (unless using specific multiplex kits) [18] | Possible with FluoroSpot (different fluorophores) [18] | High (dozens of analytes simultaneously) [82] [84] | Very High (10+ parameters simultaneously) [25] |
| Key Advantage | Robust, quantitative, widely established | Functional, detects rare cell frequency | High-throughput, multi-analyte profile from small sample | Phenotypic and functional polyfunctional analysis |
| Primary Limitation | No cellular resolution | No phenotypic data on secreting cells | No cellular resolution | Technically complex, data analysis expertise required |
Detailed Experimental Protocols
Sandwich ELISA Protocol
The sandwich ELISA is the most common format for quantitative protein analysis due to its high specificity and sensitivity [18].
Key Reagents:
- Coating Buffer: 100 mM carbonate/bicarbonate buffer, pH 9.6.
- Capture Antibody: Specific to the target protein.
- Blocking Buffer: 1-5% BSA or casein in PBS.
- Sample & Standard: Matrix-matched to the sample.
- Detection Antibody: Biotinylated antibody specific to a different epitope on the target protein.
- Streptavidin-Enzyme Conjugate: Typically Horseradish Peroxidase (HRP) or Alkaline Phosphatase (AP).
- Substrate: TMB (colorimetric) for HRP.
Step-by-Step Workflow:
- Coat Plate: Dilute the capture antibody in coating buffer. Add 100 µL per well of a 96-well plate and incubate overnight at 4°C.
- Wash: Discard the solution and wash the plate 3 times with a wash buffer (e.g., PBS with 0.05% Tween-20).
- Block: Add 200 µL of blocking buffer per well and incubate for 1-2 hours at room temperature. Wash as before.
- Add Sample & Standard: Add 100 µL of sample or standard dilution per well. Incubate for 2 hours at room temperature (or as optimized). Wash.
- Detect: Add 100 µL of the biotinylated detection antibody. Incubate for 1-2 hours at room temperature. Wash.
- Add Enzyme Conjugate: Add 100 µL of streptavidin-HRP conjugate. Incubate for 30-60 minutes at room temperature in the dark. Wash thoroughly.
- Develop: Add 100 µL of substrate solution (e.g., TMB). Incubate for 5-30 minutes in the dark until color develops.
- Stop & Read: Add 50 µL of stop solution (e.g., 1M H₂SO₄ for TMB). Read the optical density immediately at the appropriate wavelength (e.g., 450 nm).
ELISpot Protocol
ELISpot is ideal for quantifying antigen-specific T-cell responses, such as those secreting IFN-γ [18] [83].
Key Reagents:
- ELISpot Plates: 96-well plates with PVDF or nitrocellulose membranes.
- Coating Antibody: Specific to the target cytokine (e.g., anti-IFN-γ).
- Cell Culture Medium: Complete RPMI with appropriate supplements.
- Stimulants: Antigen peptides, PMA/Ionomycin (positive control).
- Detection Antibody: Biotinylated antibody specific to the target cytokine.
- Streptavidin-Enzyme Conjugate & Insoluble Substrate: (e.g., Streptavidin-AP with BCIP/NBT).
Step-by-Step Workflow:
- Coat Plate: Dilute the capture antibody in sterile PBS. Add 100 µL per well and incubate overnight at 4°C or for 2 hours at 37°C.
- Wash & Block: Wash plates 3 times with sterile PBS. Add 200 µL of cell culture medium per well and block for at least 30 minutes at 37°C.
- Stimulate Cells: Prepare a single-cell suspension of PBMCs. Discard the blocking medium from the plate and add cells (e.g., 50,000-400,000 per well) along with the antigen stimulant or control. Incubate for 16-48 hours at 37°C, 5% CO₂. Do not disturb the plates during this incubation.
- Lysing Cells: After incubation, carefully remove cells and medium. Wash plates thoroughly with deionized water followed by wash buffer to lyse and remove all cells.
- Detect: Add the biotinylated detection antibody and incubate for 2 hours at room temperature. Wash.
- Add Enzyme Conjugate: Add streptavidin-enzyme conjugate and incubate for 1-2 hours at room temperature. Wash.
- Develop: Add the precipitating substrate solution (e.g., BCIP/NBT for AP). Incubate until distinct spots emerge. Stop the reaction by washing with tap water.
- Air Dry & Analyze: Allow the plate to air dry completely in the dark. Count the spots using an automated ELISpot reader system.
Intracellular Cytokine Staining (ICS) Protocol for Flow Cytometry
This protocol enables the detection of cytokines retained within the cell following protein transport inhibition [7] [25].
Key Reagents:
- Cell Stimulation Cocktail: Antigen (e.g., peptide pool) or mitogen (e.g., PMA/Ionomycin).
- Protein Transport Inhibitor: Brefeldin A or Monensin.
- Viability Dye: e.g., LIVE/DEAD Fixable Stain.
- Surface Stain Antibodies: e.g., anti-CD3, anti-CD4, anti-CD8.
- Fixation/Permeabilization Buffers: Commercial kits (e.g., Foxp3/Transcription Factor Staining Buffer Set) or custom buffers [10].
- Intracellular Stain Antibodies: e.g., anti-IFN-γ, anti-IL-2, anti-TNF-α.
Step-by-Step Workflow:
- Stimulate Cells: Seed cells (e.g., PBMCs or splenocytes) at 1-2 × 10⁶ cells/well in a 96-well plate. Add stimulant and protein transport inhibitor. Incubate for 4-18 hours at 37°C, 5% CO₂ [7] [25].
- Surface Stain (Optional Live Cell Stain): After stimulation, stain cells with a viability dye. Wash cells. Incubate with an Fc receptor blocking antibody. Stain with surface marker antibodies diluted in FACS buffer. Wash.
- Fix and Permeabilize: Resuspend cell pellet in fixation/permeabilization buffer (e.g., 2% formaldehyde with detergents [10]) and incubate for 30-60 minutes at room temperature in the dark. Wash.
- Intracellular Stain: Resuspend fixed and permeabilized cells in permeabilization buffer containing antibodies against intracellular cytokines (and/or transcription factors). Incubate for 30 minutes at room temperature or overnight at 4°C [10]. Wash.
- Acquire & Analyze: Resuspend cells in FACS buffer and acquire on a flow cytometer. Analyze data using specialized software (e.g., FlowJo), gating on live, single cells of interest.
Integrated Data Interpretation and Synergy
The true power of these techniques is realized when they are used as complementary, rather than competing, assays. The data they generate intersect to provide a multi-layered understanding of an immune response.
Figure 1: A decision tree for selecting the appropriate immunoassay based on the research question and sample type. The pathway connects the initial question to the recommended assay and its resulting data type.
Correlative Data Analysis
For example, in a vaccine development study:
- ELISpot can first be used to identify the frequency of IFN-γ-producing T-cells in vaccinated subjects, confirming a cellular immune response [18] [17].
- ICS and Flow Cytometry can then be applied to phenotype these responding cells, revealing whether they are CD4+ or CD8+ T-cells, and to assess if they are polyfunctional (co-producing IFN-γ, TNF-α, and IL-2) – a feature often associated with superior immune protection [25].
- ELISA or a Multiplex Assay on the culture supernatant or patient serum can quantify the total magnitude of the cytokine response (e.g., IFN-γ in pg/mL) and provide context on the broader cytokine milieu (e.g., levels of IL-5, IL-10, IL-6) [18] [84].
This integrated approach reveals not only that a response occurred, but its cellular composition, functional quality, and soluble magnitude. A study comparing IL-10 detection methods noted that while ELISpot and flow cytometry are good complementary methods, ELISpot was more consistent in detecting IL-10 production from human PBMCs under certain conditions [85].
Essential Research Reagent Solutions
The following table outlines key reagents and materials required to establish these core immunoassay modalities.
Table 2: Key Research Reagent Solutions for Featured Assays
| Reagent / Material | Function / Description | Primary Application(s) |
|---|---|---|
| Pre-coated ELISA Plates | Microplates pre-coated with a capture antibody for specific targets, reducing hands-on time and improving consistency. | ELISA |
| PVDF Membrane Plates | 96-well plates with a polyvinylidene fluoride membrane to capture secreted proteins directly beneath cells. | ELISpot |
| Combinatorially Dyed Beads | Fluorescently coded microspheres (e.g., 280nm-5μm); each bead set can be conjugated to a different capture antibody. | Multiplex Bead Assays [83] |
| Protein Transport Inhibitors | Brefeldin A or Monensin; block protein secretion, allowing cytokines to accumulate inside the cell for detection. | ICS/Flow Cytometry [7] [25] |
| Fixation/Permeabilization Buffers | Reagents that preserve cell structure and create pores in membranes for intracellular antibody access. Critical for transcription factor staining. | ICS/Flow Cytometry [10] |
| Biotinylated Antibodies & Streptavidin-Enzyme | A universal detection system providing signal amplification through the high-affinity biotin-streptavidin interaction. | ELISA, ELISpot |
| Viability Dyes | Fluorescent dyes that selectively stain dead cells, allowing for their exclusion during flow cytometry analysis. | ICS/Flow Cytometry [7] |
| Polychromatic Flow Cytometry Panels | Pre-optimized or custom antibody panels for simultaneous detection of multiple cell surface and intracellular targets. | ICS/Flow Cytometry [25] |
ELISpot, ELISA, multiplex assays, and ICS flow cytometry are not redundant techniques but rather complementary pillars of modern immunology research. ELISA and multiplex assays excel at providing quantitative, bulk protein data, ELISpot offers exceptional sensitivity for detecting the frequency of rare, functionally active cells, and ICS flow cytometry uniquely reveals the phenotype and polyfunctional capacity of responding cells. A well-designed study, particularly within the context of vaccine development, immunotherapy monitoring, or biomarker discovery, will strategically combine these modalities. This integrated approach, guided by a clear understanding of each assay's strengths as outlined in this note, empowers researchers to build a comprehensive and mechanistically insightful model of the immune response.
Standardization Strategies for Multi-Site Clinical Trials
In the field of clinical research, multi-site trials are essential for enrolling diverse patient populations and enhancing the statistical power of studies. However, the generation of comparable and high-quality flow cytometry data across different geographic locations presents significant challenges [86]. Intracellular cytokine staining (ICS), a cornerstone technique for evaluating functional immune responses at the single-cell level, is particularly vulnerable to technical variability [87] [25]. This application note details standardized protocols and harmonization strategies, framed within the context of intracellular cytokine staining research, to ensure data consistency and reliability in multi-center clinical trials. The procedures outlined herein are designed for researchers, scientists, and drug development professionals engaged in immune monitoring for vaccine research, immunotherapy development, and autoimmune disease studies [87].
Critical Challenges in Multi-Site Flow Cytometry
Multi-site ICS flow cytometry studies must overcome several key sources of variability to ensure data integrity and meaningful cross-site comparisons.
- Instrument Configuration: Differences in flow cytometer manufacturers, models, laser power, and optical filters across sites can lead to substantial variation in fluorescence measurements [88] [41].
- Reagent Variability: Different lots of antibodies and staining reagents can introduce pre-analytical error, affecting staining intensity and the resolution of cell populations [86] [88].
- Sample Processing: Inconsistencies in cell stimulation, fixation, permeabilization, and staining procedures profoundly impact cytokine detection and cell viability [87] [25].
- Data Analysis Discrepancies: Divergent gating strategies and compensation practices between operators can result in inconsistent population enumeration and biomarker quantification [65] [88].
Standardization and Harmonization Workflow
A successful multi-site trial requires an integrated, proactive approach to standardization that covers the entire experimental lifecycle, from pre-acquisition to data analysis. The following workflow provides a visual overview of this comprehensive process, with each component detailed in the sections that follow.
Pre-Acquisition Standardization Strategies
Instrument Calibration and Quality Control
Rigorous instrument calibration is the foundation of reproducible flow cytometry data across multiple sites.
Laser Alignment and Voltage Standardization: Use commercially available calibration beads, such as CS&T or Rainbow beads, to align photomultiplier tube (PMT) voltages across all instruments in the network [86]. This ensures that identical fluorescence signals are measured with the same sensitivity on different machines.
Longitudinal Performance Tracking: Implement a daily quality control (QC) procedure using stable reference materials, such as eight-peak beads, to monitor instrument performance over time [86] [88]. Site-specific biological control samples (e.g., cryopreserved PBMCs from a single donor) should be run periodically (e.g., quarterly) and after any major instrument service to track population resolution and enumeration stability [86].
Reagent and Sample Processing Standardization
Lyophilized Antibody Cocktails: To minimize technical error and batch-to-batch variability, employ pre-mixed, lyophilized antibody cocktails for staining [86]. This approach eliminates pipetting errors and ensures that all sites use identical antibody formulations and concentrations.
Validated Sample Protocols: Develop and distribute a detailed Manual of Procedures (MOP) that standardizes every step of sample handling [86]. For ICS, this is particularly critical during the stimulation and intracellular staining phases.
Table 1: Key Controls for ICS Assay Standardization
| Control Type | Purpose | Implementation in Multi-Site Trials |
|---|---|---|
| Unstimulated Control | Measures background cytokine production | Use identical culture medium and serum across all sites [25] |
| Positive Control | Verifies assay functionality | Standardize PMA/Ionomycin concentrations and stimulation duration [87] |
| Fluorescence Minus One (FMO) | Determines accurate gating boundaries | Provide lyophilized FMO cocktails for key cytokines/chemokine receptors [86] |
| Isotype Control | Assesses non-specific antibody binding | Use matched isotype clones from the same vendor and lot [87] |
Standardized Intracellular Cytokine Staining Protocol
The following detailed protocol is optimized for multi-site implementation, with specific attention to critical standardization points. The estimated duration is 6.5 hours, with a cost of approximately $675 USD for 20 samples with controls [87].
Cell Stimulation and Protein Transport Inhibition
- Prepare Cell Samples: Isolate PBMCs using standardized density gradient centrifugation across all sites. Adjust cell concentration to 1-2 × 10⁶ cells/mL in pre-defined complete culture medium [87]. Verify cell viability exceeds 90% before proceeding.
- Execute Cell Stimulation: Distribute cells into 96-well round-bottom plates. Add stimulation cocktails according to the predefined experimental design:
- For polyclonal activation: Use 50 ng/mL PMA and 500 ng/mL Ionomycin [87].
- For antigen-specific responses: Use standardized antigen concentrations determined through prior dose-response experiments.
- Include unstimulated controls (medium alone) and positive controls in every experiment.
- Inhibit Protein Transport: Add protein transport inhibitors (10 μg/mL Brefeldin A and 2 μM Monensin) to all wells after the initial 1-2 hours of stimulation [87]. Continue incubation for an additional 4-6 hours (total stimulation time: 4-5 hours for optimal cytokine detection) [87].
Cell Staining and Fixation
- Surface Marker Staining: Transfer stimulated cells to fresh plates and wash twice with cold staining buffer. Add surface marker antibodies (e.g., CD3, CD4, CD8) diluted in standardized staining buffer. Incubate for 20 minutes at 4°C in darkness [87]. Include a viability dye to exclude dead cells from analysis.
- Fix and Permeabilize Cells: After surface staining, fix cells using a standardized fixative. Recent research indicates that a formulation of 2% formaldehyde with 0.05% dish soap detergent (e.g., Fairy, Dawn) and 0.5% Tween provides an optimal balance for preserving both cytokine signals and fluorescent protein reporters while allowing antibody access to intracellular and nuclear epitopes [10]. Incubate for 30 minutes at room temperature. After fixation, permeabilize cells using a buffer containing 0.05% dish soap detergent for 15-30 minutes at room temperature [10].
- Intracellular Cytokine Staining: Add intracellular cytokine antibodies (e.g., IFN-γ, TNF-α, IL-2, IL-4, IL-17) diluted in permeabilization buffer. Incubate for 30 minutes at room temperature or overnight at 4°C depending on antibody requirements [87] [10].
Data Acquisition
- Final Processing: Wash cells three times with permeabilization buffer, followed by one wash with regular staining buffer. Resuspend cells in an appropriate volume of staining buffer or fixative for flow cytometric analysis [87].
- Standardized Acquisition: Acquire samples on flow cytometers calibrated according to the harmonization procedures in Section 4.1. Collect a minimum number of events as defined by statistical requirements for the target populations, particularly important for rare cytokine-producing cells [65].
The following diagram illustrates the core workflow of the ICS procedure, highlighting critical control points where standardization is essential for multi-site consistency.
Data Harmonization and Analysis
Computational Normalization
Even with meticulous pre-acquisition standardization, post-acquisition data normalization may be necessary to correct for residual inter-site and longitudinal variations.
Intra-center Normalization: Develop an R script to normalize results over the study period for each center based on the targets of the initial harmonization [88]. This script can:
- Extract the MFI of eight-peak beads from daily QC files.
- Define transformation parameters to normalize FCS files using linear regression.
- Apply normalization to correct for instrument drift over time [88].
Batch Effect Correction: Create scripts (e.g., in Python) to correct data between different reagent lots and after calibration procedures repeated during long-term studies [88].
Standardized Gating and Analysis
Automated Gating Strategies: To minimize inter-operator variability, employ supervised machine learning-based approaches for automated population gating [88]. These algorithms can be built using training datasets gated manually by a central reference operator, ensuring consistency across all sites [88].
Centralized Analysis: For studies without automated gating capabilities, have a single expert operator perform all data analysis or establish rigorous gating guidelines with representative examples to ensure consistent application across sites [25] [88].
Table 2: Quantitative Data Harmonization Results from Multi-Site Studies
| Harmonization Metric | Pre-Harmonization CV | Post-Harmonization CV | Implementation Method |
|---|---|---|---|
| MFI of Membrane Markers | 10-15% [88] | <5% [88] | PMT alignment with calibration beads & computational normalization |
| Population Frequencies | Not reported | 2.3% (neutrophils) to 17.7% (monocytes) [88] | Standardized antibody cocktails & automated gating |
| Instrument Sensitivity | Variable between sites | CV <2.5% on bead standards [88] | Daily QC with 8-peak beads & longitudinal tracking |
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials critical for implementing standardized intracellular cytokine staining across multiple sites.
Table 3: Essential Research Reagents for Standardized Multi-Site ICS
| Reagent / Material | Function | Standardization Considerations |
|---|---|---|
| Lyophilized Antibody Cocktails | Multiparameter cell staining | Pre-mixed formulations reduce technical error; use same vendor and lot across sites [86] |
| Calibration Beads (CS&T/Rainbow) | Instrument calibration | Align PMT voltages across different cytometers; track performance over time [86] |
| Protein Transport Inhibitors | Intracellular cytokine accumulation | Standardize concentrations of Brefeldin A (10 μg/mL) and Monensin (2 μM) [87] |
| Dish Soap Detergent-based Buffer | Cell permeabilization | Enables simultaneous detection of cytokines and transcription factors; use specified brands (e.g., Fairy, Dawn) [10] |
| Viability Dye | Exclusion of dead cells | Prevents false-positive signals; titrate to optimal concentration (e.g., 1:500 for Zombie Aqua) [86] |
| Stimulation Cocktails | Cell activation | Standardize PMA/Ionomycin concentrations and stimulation duration across sites [87] |
Implementing robust standardization strategies for intracellular cytokine staining in multi-site clinical trials is technically challenging but achievable through a comprehensive approach. Success requires harmonization across all phases of the workflow: instrument calibration using standardized beads, standardized reagents and staining protocols, computational normalization of data, and consistent gating strategies. By adopting these practices, researchers can generate high-quality, comparable flow cytometry data across multiple geographic locations, enhancing the reliability and impact of multicenter clinical trials in immunology and drug development.
The functional capacity of T-cells is a critical determinant of effective immunity against pathogens and cancer. Polyfunctional T-cells—those capable of simultaneously producing multiple cytokines like IFN-γ, TNF-α, and IL-2—represent a superior class of immune responders correlated with protective immunity [89]. In infant BCG vaccination studies, the frequency of IFN-γ+TNF-α+IL-2+ CD4+ T-cells directly correlated with enhanced inhibition of mycobacterial growth, establishing polyfunctional responses as a key immune correlate of protection [89]. Similarly, in advanced cancer immunotherapies, CD19 CAR-T products exhibiting polyfunctional signatures demonstrate superior anti-tumor efficacy, highlighting their importance in clinical outcomes [90]. This application note provides detailed protocols and analytical frameworks for standardized assessment of polyfunctional T-cells, enabling robust quantification of these critical immune correlates.
Key Research Reagent Solutions
Successful profiling of polyfunctional T-cells requires carefully selected reagents optimized for intracellular target detection. The table below summarizes essential solutions and their applications:
Table 1: Key Research Reagents for Intracellular Cytokine Staining
| Reagent Solution | Specific Function | Application Examples |
|---|---|---|
| Intracellular Fixation & Permeabilization Buffer Set [27] | Fixes cellular structures while creating pores for antibody access | Optimal for cytoplasmic proteins, cytokines, and chemokines |
| Foxp3/Transcription Factor Staining Buffer Set [27] | Combined fixation/permeabilization in a single step | Recommended for nuclear antigens, transcription factors |
| Fixation/Methanol Protocol [27] | Strong fixation and permeabilization | Required for certain phosphorylated signaling proteins (MAPK, STAT) |
| Protein Transport Inhibitors (Brefeldin A, Monensin) [27] | Blocks cytokine secretion, enabling intracellular accumulation | Essential for cytokine detection assays during cell stimulation |
| Cell Stimulation Cocktails (PMA/Ionomycin) [27] [90] | Activates T-cells to induce cytokine production | Used with transport inhibitors for polyfunctional cytokine profiling |
| Fixable Viability Dyes [27] | Identifies non-viable cells to exclude from analysis | Critical for eliminating false positives from dead cells |
Quantitative Correlates of Polyfunctional T-cells
Comprehensive studies across vaccination and immunotherapy contexts have established quantitative relationships between polyfunctional T-cell responses and functional outcomes.
Table 2: Polyfunctional T-cell Correlates of Protection
| Experimental Context | Polyfunctional T-cell Population | Correlated Protective Outcome | Significance |
|---|---|---|---|
| BCG-vaccinated infants [89] | IFN-γ+TNF-α+IL-2+ CD4+ T-cells | Enhanced PBMC-mediated mycobacterial growth inhibition | Dominant response at 4 months and 1 year post-vaccination; significant correlation with growth inhibition |
| CD19 CAR-T cell therapy [90] | Polyfunctional (2+ cytokine) CD4+ and CD8+ CAR-T cells | Therapeutic efficacy against B-cell malignancies | Marked heterogeneity in cytokine secretions; polyfunctional subsets specific to antigen stimulation |
| BCG-vaccinated infants [89] | IL-17+ CD4+ T-cells | Early post-vaccination immune responses | Significantly enhanced at 4 months but not sustained at 1 year post-BCG |
Experimental Protocols for Polyfunctional T-cell Analysis
Protocol A: Two-Step Intracellular Staining for Cytoplasmic Proteins
This protocol is optimized for detecting cytokines and other cytoplasmic proteins while preserving cell surface marker information [27].
Materials
- Intracellular Fixation & Permeabilization Buffer Set [27]
- Flow Cytometry Staining Buffer
- Protein Transport Inhibitors (Brefeldin A or Monensin) [27]
- Cell Stimulation Cocktail (PMA/Ionomycin) [27]
- Fluorochrome-conjugated antibodies against surface markers and cytokines
- Fixable Viability Dyes [27]
Staining Procedure
Cell Preparation & Stimulation: Prepare single-cell suspension and stimulate with appropriate activators (e.g., PMA/Ionomycin for T-cells) in the presence of protein transport inhibitors for 4-16 hours to allow cytokine accumulation [27] [90].
Surface Marker Staining:
Fixation and Permeabilization:
- Thoroughly resuspend cell pellet in 100 μL IC Fixation Buffer
- Incubate 20-60 minutes at room temperature, protected from light
- Add 2 mL 1X Permeabilization Buffer, centrifuge, and discard supernatant
- Repeat permeabilization wash [27]
Intracellular Staining:
- Resuspend cells in 100 μL 1X Permeabilization Buffer
- Add directly conjugated anti-cytokine antibodies
- Incubate 20-60 minutes at room temperature, protected from light
- Wash twice with 2 mL 1X Permeabilization Buffer [27]
Sample Acquisition:
Protocol B: One-Step Fixation/Permeabilization for Nuclear Proteins
This streamlined protocol is ideal for transcription factors and nuclear antigens while simultaneously preserving surface epitopes [27].
Materials
- Foxp3/Transcription Factor Staining Buffer Set [27]
- Fluorochrome-conjugated antibodies
- Normal serum for blocking (optional)
Staining Procedure
Surface Staining: Complete surface marker staining as described in Protocol A, steps 1-2.
Fixation/Permeabilization:
- After final wash, resuspend cells in 1 mL freshly prepared Foxp3 Fixation/Permeabilization working solution
- Incubate 30-60 minutes at room temperature, protected from light
- Wash with 2 mL 1X Permeabilization Buffer [27]
Intracellular Staining:
- Resuspend cells in 100 μL 1X Permeabilization Buffer
- [Optional] Block with 2% normal serum (15 minutes, room temperature)
- Without washing, add directly conjugated antibodies against nuclear antigens
- Incubate 30-60 minutes at room temperature, protected from light
- Wash twice with 2 mL 1X Permeabilization Buffer [27]
Sample Acquisition: Resuspend in staining buffer for flow cytometric analysis.
Standardized Flow Cytometry Configuration
Consistent instrument setup is essential for reproducible polyfunctional T-cell data across experiments and laboratories:
- Instrument Setup: Follow standardized protocols for photomultiplier tube voltages, fluidics, and laser delays [42]
- Fluorochrome Selection: Implement 8-color panels with optimal fluorochrome combinations to minimize spectral overlap while maximizing resolution [42]
- Compensation Controls: Use single-stained controls for proper compensation of spectral overlap [42]
- Gating Strategy: Include viability dye exclusion, doublet discrimination, lymphocyte gating, and subset identification (CD4+/CD8+) before cytokine analysis [27]
Workflow Visualization
Data Analysis and Interpretation
Defining Polyfunctional Populations
Polyfunctional T-cells are identified through sequential bivariate gating of cytokine expressions, with true polyfunctional populations exhibiting simultaneous production of multiple cytokines rather than mixture of single producers [89] [90]. Advanced analytical approaches include:
- Boolean Gating: Combined use of logical gates to identify all possible cytokine combination profiles
- Polyfunctionality Index: Quantitative scoring of the breadth and intensity of cytokine production
- Dimensionality Reduction: t-SNE or PCA visualization to identify functional clusters within heterogeneous T-cell populations [90]
Correlation with Functional Outcomes
The protective capacity of polyfunctional T-cells is established through direct correlation with functional readouts:
- Mycobacterial Growth Inhibition: BCG-induced polyfunctional CD4+ T-cells significantly correlate with controlled mycobacterial replication in vitro [89]
- Tumor Control: CD19 CAR-T products enriched for polyfunctional subsets demonstrate enhanced anti-tumor efficacy and persistence in patients [90]
- Vaccine Efficacy: Polyfunctional responses serve as superior predictors of vaccine-mediated protection compared to single-cytokine readouts
Troubleshooting and Optimization
Common Challenges
- High Background Staining: Increase protein content (BSA/FCS) in staining buffers; optimize antibody concentrations; include viability dye exclusion [27]
- Poor Cytokine Signals: Optimize stimulation duration and reagent concentrations; verify protein transport inhibitor efficacy [27]
- Loss of Surface Epitopes: Test alternative fixation methods; titrate formaldehyde concentration; consider methanol-compatible antibodies for phospho-proteins [27]
- Spectral Overlap: Implement careful fluorochrome panel design with minimal spillover; use compensation matrices and single-stained controls [42]
Methodological Validation
- Controls: Include unstimulated controls, fluorescence-minus-one (FMO) controls, and isotype controls
- Reproducibility: Implement standardized instrument settings and SOPs across experiments [42]
- Specificity: Verify antibody performance in appropriate buffer systems through empirical testing [27]
Comprehensive analysis of polyfunctional T-cells through standardized intracellular cytokine staining provides critical insights into protective immunity across vaccination and immunotherapy contexts. The protocols and analytical frameworks presented here enable robust quantification of these superior immune effectors, establishing them as key correlates of protection in both basic research and clinical applications.
Navigating the Challenges of Rare Cell Population Analysis
The detection and analysis of rare cell populations, defined as those representing less than 0.01% of the total cellular population, present significant challenges in flow cytometry research, particularly within the context of intracellular cytokine staining (ICS) [92]. These rare populations—such as antigen-specific T cells, circulating tumor cells, or stem cells—often hold crucial information about immune responses, disease progression, and therapeutic efficacy [92] [93]. The statistical constraints of Poisson statistics, combined with technical limitations in assay sensitivity and specificity, create a complex analytical landscape that requires specialized methodologies [94]. This application note provides a comprehensive framework for navigating these challenges, integrating current statistical principles with optimized ICS protocols to enable reliable rare cell detection in drug development and clinical research settings.
Statistical Foundations of Rare Event Analysis
Poisson Statistics and Precision Requirements
In rare event analysis, conventional Gaussian statistics no longer apply; instead, Poisson statistics dominate, where the mean and variance of the distribution equal the number of positive events [94]. This fundamental statistical shift has profound implications for experimental design:
- The coefficient of variation (CV) for rare populations is determined by the formula: CV = 1/√N, where N represents the number of positive events collected [94]
- With only 2 positive events, the CV reaches approximately 71%, while 100 events reduce the CV to about 10% [94]
- Inter-laboratory CVs can exceed 40% for populations below 0.1%, with the highest variability (57-82%) observed for populations below 0.01% [94]
Table 1: Event Collection Requirements for Rare Population Analysis
| Desired CV | Number of Positive Events Required | Total Events at 0.01% Frequency | Acquisition Time* |
|---|---|---|---|
| 40% | 6 | 62,500 | ~1.7 minutes |
| 20% | 25 | 250,000 | ~6.9 minutes |
| 10% | 100 | 1,000,000 | ~27.8 minutes |
| 5% | 400 | 4,000,000 | ~1.9 hours |
| 1% | 10,000 | 100,000,000 | ~46.3 hours |
Assuming acquisition at 10,000 events per second [94]
Determining Statistical Significance
Assay reproducibility becomes paramount for demonstrating significance in rare event analysis [94]. Researchers must:
- Compare positive samples against appropriate negative controls to establish baseline levels [94]
- Conduct power calculations to determine the necessary sample replicates and event counts [94]
- Recognize that even 12-14 positive events may provide accurate data when supported by proper controls and experimental design [94]
Optimized ICS Protocol for Rare Cell Detection
Sample Preparation and Stimulation
The following protocol adapts standard intracellular cytokine staining specifically for rare population detection:
Step 1: Cell Preparation and Stimulation
- Isolate immune cells (PBMCs, splenocytes, or tissue-derived lymphocytes) and adjust concentration to 1-2 × 10⁶ cells/mL in complete culture medium [95]
- Verify cell viability exceeds 90% using trypan blue exclusion [95]
- Distribute cells into 96-well round-bottom plates with 200 μL cell suspension per well [95]
- Add stimulation cocktails: 50 ng/mL PMA with 500 ng/mL ionomycin for polyclonal activation, or antigen-specific peptides at optimized concentrations [95]
- Include unstimulated controls and single-stimulus controls to assess background cytokine production [95]
- Incubate plates in CO₂ incubator at 37°C for 1-2 hours [95]
Step 2: Protein Transport Inhibition
- Add protein transport inhibitors: brefeldin A (10 μg/mL) and monensin (2 μM) to all wells [95]
- Continue incubation for additional 4-6 hours (total stimulation time: 4-5 hours for most cytokines) [95]
- Monitor timing precisely, as extended culture can lead to cell death and reduced cytokine detection [95]
Step 3: Surface Staining with Viability Discrimination
- Transfer stimulated cells to fresh 96-well plates and wash twice with cold staining buffer [95]
- Add surface marker antibodies (CD3, CD4, CD8, etc.) diluted in staining buffer for 20 minutes at 4°C in darkness [95]
- Include viability dyes (e.g., SYTOX AADvanced, Viobility Fixable Dyes) to exclude dead cells, which cause non-specific antibody binding and false-positive signals [95] [93]
- Wash cells twice with staining buffer to remove unbound antibodies [95]
Step 4: Fixation and Permeabilization
- Add fixation solution and incubate for 20 minutes at room temperature [95]
- For simultaneous detection of transcription factors and cytokines, use "Burton's Better Buffer" containing 2% formaldehyde with 0.05% Fairy dish soap and 0.5% Tween-20 [10]
- Wash cells once with staining buffer, then add permeabilization buffer containing 0.1% saponin or the dish soap-based perm buffer [95] [10]
- Maintain cells in permeabilization buffer throughout intracellular staining to prevent membrane resealing [95]
Step 5: Intracellular Cytokine Staining
- Add intracellular cytokine antibodies (IFN-γ, TNF-α, IL-2, IL-4, IL-17, IL-10) diluted in permeabilization buffer [95]
- Incubate for 30 minutes at room temperature or overnight at 4°C for enhanced detection of low-abundance targets [95] [10]
- Include isotype control antibodies to assess non-specific binding and establish gating boundaries [95]
- Use Fc receptor blocking reagents prior to staining to reduce non-specific antibody binding [93]
Step 6: Sample Acquisition
- Wash cells three times with permeabilization buffer, followed by one wash with regular staining buffer [95]
- Resuspend cells in 200-300 μL of staining buffer or fixative [95]
- Acquire samples immediately or store at 4°C in darkness for analysis within 24 hours [95]
Diagram 1: Rare Cell ICS Workflow
Technical Strategies for Enhanced Rare Cell Detection
Sample Pre-Enrichment Techniques
For populations below 0.001%, pre-enrichment strategies dramatically improve detection efficiency:
- Magnetic bead enrichment using antibody-conjugated magnetic beads (e.g., Miltenyi Biotec, IMAG system, Dynabeads) can enrich populations from 0.01% to 0.1% in approximately 45 minutes [94]
- This enrichment reduces sorting time from 83 minutes to 10 minutes when processing 100 million cells, improving cell health by faster return to culture conditions [94]
- Hypotonic lysis of red blood cells preserves rare nucleated populations while eliminating the majority of background cells [92]
- No-lyse/no-wash or lyse/no-wash procedures minimize cell loss during processing steps [93]
Instrumentation and Acquisition Optimization
Acoustic focusing flow cytometry represents a significant advancement for rare cell analysis:
- Acquisition rates of 1,000 μL per minute enable collection of 1 million events in 3 minutes, 13 seconds—19.7 times faster than conventional hydrodynamic focusing at high flow rates [93]
- Higher throughput allows analysis of larger sample volumes without compromising data quality [92] [93]
- Ultrasonic waves focus cells for laser interrogation, reducing sample clogging and supporting large sample volumes [92]
Table 2: Acquisition Rate Comparison
| Instrument Type | Flow Rate | Time for 10⁶ Events | Relative Speed |
|---|---|---|---|
| Hydrodynamic Focusing | High | 63 minutes, 33 seconds | 1x |
| Acoustic Focusing | 200 μL/min | 13 minutes, 20 seconds | 4.8x |
| Acoustic Focusing | 500 μL/min | 5 minutes, 47 seconds | 11.0x |
| Acoustic Focusing | 1,000 μL/min | 3 minutes, 13 seconds | 19.7x |
Data adapted from Thermo Fisher Scientific application note [93]
Panel Design and Fluorophore Selection
Effective panel design is critical for rare population identification:
- Use brightest fluorophores (PE, APC) for low-abundance targets or rare populations, and dimmer fluorophores for highly expressed antigens [41]
- Implement compound gating using multiple positive identifiers and "dump channels" to exclude dead cells, aggregates, and unwanted populations [93]
- Employ fluorescent-minus-one (FMO) controls to establish accurate gating boundaries and distinguish positive from negative populations [93]
- Design panels with minimal spectral overlap, prioritizing fluorophores with distinct emission spectra to reduce compensation complexity [41]
Troubleshooting and Quality Control
Common Challenges and Solutions
Low Cytokine Signal Detection
- Optimize stimulation duration and concentration through time-course and dose-response experiments [95]
- Combine brefeldin A with monensin for enhanced retention of certain cytokines [95]
- Test antibody performance using known positive controls and consider alternative clones or fluorophore conjugates [95]
High Background in Unstimulated Controls
- Minimize cell handling time and maintain samples at 4°C to prevent inadvertent activation [95]
- Verify culture medium quality and replace if bacterial contamination is suspected [95]
- Optimize antibody concentrations through titration and include additional wash steps [95]
Poor Cell Viability After Stimulation
- Assess viability at multiple time points to identify optimal activation windows [95]
- Verify CO₂ incubator conditions (temperature, humidity, gas concentrations) [95]
- Consider alternative stimulation protocols or reduced stimulation strength for sensitive cells [95]
Inconsistent Permeabilization Efficiency
- Standardize fixation and permeabilization timing using batch processing [95]
- Verify permeabilization buffer preparation and pH [95]
- Consider commercial kits with validated protocols if homemade solutions produce inconsistent results [95]
Quality Control Measures
Implement rigorous quality control procedures to ensure assay consistency:
- Include positive and negative controls in every experiment to verify assay performance [95]
- Monitor key performance indicators: cell viability post-stimulation, stimulation index ratios, and background fluorescence levels [95]
- Establish standard operating procedures for cell stimulation, staining protocols, and data acquisition to minimize inter-operator variability [95]
- Conduct regular antibody performance validation using known positive samples [95]
Diagram 2: Troubleshooting ICS for Rare Cells
Research Reagent Solutions
Table 3: Essential Reagents for Rare Cell ICS
| Reagent Category | Specific Examples | Function in Rare Cell ICS |
|---|---|---|
| Cell Stimulation | PMA/Ionomycin cocktail, Antigen-specific peptides | Activates target T-cell populations for cytokine production [95] |
| Protein Transport Inhibitors | Brefeldin A (10 μg/mL), Monensin (2 μM) | Blocks Golgi-mediated secretion, causing intracellular cytokine accumulation [95] |
| Viability Stains | SYTOX AADvanced, Viobility Fixable Dyes, 7-AAD | discriminates live/dead cells to reduce false positives [93] |
| Fixation/Permeabilization | Commercial kits, PFA/Saponin, Dish Soap Buffer | Preserves cellular structure while allowing antibody access to intracellular targets [95] [10] |
| Magnetic Enrichment | Miltenyi Biotec kits, Dynabeads, IMAG system | Pre-enriches rare populations to improve detection efficiency [94] [92] |
| Surface Marker Antibodies | CD3, CD4, CD8, CD45, Lineage markers | Identifies cell populations and enables gating strategies [95] [93] |
| Cytokine Antibodies | IFN-γ, TNF-α, IL-2, IL-4, IL-17, IL-10 | Detects intracellular cytokine production in specific cell subsets [95] |
| Red Cell Lysis | High-Yield Lyze Solution, ammonium chloride | Removes erythrocytes with minimal loss of rare nucleated cells [92] [93] |
The successful detection and analysis of rare cell populations in intracellular cytokine staining requires an integrated approach addressing statistical, technical, and methodological challenges. By implementing Poisson-aware experimental designs, employing strategic pre-enrichment techniques, optimizing instrumentation parameters, and adhering to rigorous quality control measures, researchers can reliably detect and characterize rare cell populations down to 0.0001% frequency. The protocols and strategies outlined in this application note provide a framework for advancing research in vaccine development, immunotherapy assessment, and autoimmune disease studies where rare antigen-specific T cells serve as critical biomarkers of immune competence and therapeutic efficacy.
Conclusion
Intracellular cytokine staining flow cytometry stands as an indispensable tool in modern immunology and drug development, providing unparalleled insights into immune function at the single-cell level. By mastering its foundational principles, optimizing methodological approaches, and implementing rigorous troubleshooting and validation protocols, researchers can reliably generate high-quality data to advance therapeutic development. The future of ICS lies in continued technological refinements for higher-parameter analysis, increased standardization for multi-center trials, and deeper integration into biomarker strategies for precision medicine. As drug modalities continue to evolve, the ability of ICS to provide functional pharmacodynamic data will be crucial for translating preclinical findings into clinical success, particularly in the realms of immuno-oncology, vaccine development, and cell therapies.
References
- 1. Intracellular Cytokine Staining Assays - Functional ... [https://kcasbio.com/blogs/intracellular-cytokine-staining-assays-functional-assessment-using-flow-cytometry/]
- 2. How to get reliable data from intracellular cytokine staining [https://www.abcam.com/en-us/stories/articles/intracellular-cytokine-staining-best-practices]
- 3. Multiparameter Intracellular Cytokine Staining - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4219546/]
- 4. Intracellular cytokine staining (ICS) [https://cellcarta.com/intracellular-cytokine-staining-ics/]
- 5. Best Practices for Cytokine Analysis [https://www.bdbiosciences.com/en-us/learn/science-thought-leadership/blogs/cytokine-analysis-best-practices]
- 6. An Artifact in Intracellular Cytokine Staining for Studying T ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.759188/full]
- 7. 2.5. Flow Cytometry Intracellular Cytokine Staining [https://bio-protocol.org/exchange/minidetail?id=10098015&type=30]
- 8. Flow Cytometry Protocol | Abcam [https://www.abcam.com/en-us/technical-resources/protocols/flow-cytometry-for-intracellular-and-extracellular-targets]
- 9. Standardizing Flow Cytometry Immunophenotyping ... [https://www.nature.com/articles/srep20686]
- 10. Introducing the Dish Soap Protocol: A Unified Approach for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447862/]
- 11. Intracellular Cytokine Staining Protocol [https://anilocus.com/intracellular-cytokine-staining-protocol/?srsltid=AfmBOooubalGQwG4f8A6vAX34k8qHVkA6cWvOVGbae-7cwmB4mlfcXdF]
- 12. Stimulation of Cytokine Production in Immune Cells Protocol [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/immunology-at-work/immunology-protocols/stimulation-cytokine-production-immune-cells.html]
- 13. High Throughput Analysis of Golgi Structure by Imaging ... [https://www.nature.com/articles/s41598-017-00909-y]
- 14. Evaluation of monensin and brefeldin A for flow cytometric ... [https://pubmed.ncbi.nlm.nih.gov/11449408/]
- 15. Development of an automated analysis system for data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2591089/]
- 16. Data analysis in flow cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/data-analysis-in-flow-cytometry]
- 17. ELISA vs ELISpot: Select The Right Assay For Your Research [https://viraxbiolabs.com/elisa-vs-elispot-select-the-right-assay-for-your-research/]
- 18. ELISA versus ELISpot: Which assay is right for your ... [https://www.mabtech.com/knowledge-hub/elisa-versus-elispot-which-assay-right-your-research]
- 19. Unique-Strengths of ELISPOT for T Cell Diagnostics Protocol [https://www.creative-diagnostics.com/unique-strengths-of-elispot-for-t-cell-diagnostics-protocol.htm]
- 20. Comparison between enzyme‐linked immunospot assay and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9449588/]
- 21. ELISA vs. ELISpot: Which assay is right for your research? [https://www.bio-connect.nl/news/elisa-vs-elispot-which-assay-is-right-for-your-research/]
- 22. ELISPOT Assays [https://immunospot.eu/elispot-assays]
- 23. Comparison of the ELISPOT and cytokine flow cytometry ... [https://www.sciencedirect.com/science/article/abs/pii/S0022175903003636]
- 24. Comparison between enzyme-linked immunospot assay ... [https://pubmed.ncbi.nlm.nih.gov/36169252/]
- 25. Intracellular Cytokine Staining and Flow Cytometry [https://pmc.ncbi.nlm.nih.gov/articles/PMC4569436/]
- 26. Intracellular Cytokine Staining Protocol [https://anilocus.com/intracellular-cytokine-staining-protocol/?srsltid=AfmBOorwcCGNWjSgDAxrfRR2PzZSZCFplAxMCyjk28w6FWaFTvkp4iBI]
- 27. Staining Intracellular Antigens for Flow Cytometry [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/staining-intracellular-antigens-flow-cytometry.html]
- 28. Antigen‐specific polyfunctional cytotoxic T cells differentiate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081828/]
- 29. Intracellular cytokine staining for the characterization and ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202306000041]
- 30. An optimized flow cytometry protocol for simultaneous ... [https://www.sciencedirect.com/science/article/pii/S002217592300025X]
- 31. Optimization of the Blocking and Signal Preservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462741/]
- 32. Flow Cytometry Optimization: Sample Prep, Staining & ... [https://www.bosterbio.com/protocol-and-troubleshooting/flow-cytometry-optimization?srsltid=AfmBOorIceVDJwYxikJg8_chCK0FJ4H7S3AsfaWc3qB0sdCzyRaQchUX]
- 33. An Update on Flow Cytometry Analysis of Hematological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190783/]
- 34. Spectral Flow Cytometry: The Current State and Future of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193525/]
- 35. Flow Cytometric Immunophenotyping: Minimal Differences in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11505181/]
- 36. Comparison of immunometabolic profiles in whole blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12604536/]
- 37. Choosing the Optimal Sample Type for Flow Cytometry [https://www.precisionformedicine.com/blog/choosing-the-optimal-sample-type-for-flow-cytometry-key-considerations-and-case-studies/]
- 38. Peripheral Whole Blood vs. PBMCs [https://www.akadeum.com/blog/what-are-pbmc-human-pbmc-cells-peripheral-blood-vs-whole-blood/?srsltid=AfmBOoqGY30TEtshXqYZlFYOCCmLi_2rtqU9QYXgkDmKfWsQ9YpKag3E]
- 39. Spectral Panel Design [https://fluorofinder.com/spectral-panel-design-2/]
- 40. Standardisation of flow cytometry for whole blood ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0217163]
- 41. Designing a multicolor flow cytometry protocol [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/designing-a-multicolor-protocol]
- 42. EuroFlow standardization of flow cytometer instrument ... [https://www.nature.com/articles/leu2012122]
- 43. A comprehensive multiparameter flow cytometry panel for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10508641/]
- 44. Multiparameter flow cytometry enables immune profiling ... [https://www.frontiersin.org/journals/dental-medicine/articles/10.3389/fdmed.2025.1590516/full]
- 45. Applications of Flow Cytometry in Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11011675/]
- 46. Applications of Flow Cytometry in Drug Discovery and ... [https://www.mdpi.com/1422-0067/25/7/3851]
- 47. Advancing Drug Discovery: The Power of Flow Cytometry ... [https://kcasbio.com/blogs/advancing-drug-discovery-the-power-of-flow-cytometry-in-compound-screening/]
- 48. 7 Advanced Flow Cytometry Data Analysis Tips For Multi ... [https://expertcytometry.com/flow-cytometry-data-analysis-tips-for-multi-color-experiments/]
- 49. Protocol Compatibility Table for Immune Signaling and ... [https://www.cellsignal.com/learn-and-support/reference-tables/flow-protocol-compatibility?srsltid=AfmBOoqKnHqgKOC5DGypD-ktl8Yb-faIttYV_u2-hkpV2pnkkeKh4BqO]
- 50. Implementing A Higher Color Flow Cytometry System [https://www.cytometry.org/newsletters/eICCS-2-3/article6.php]
- 51. Analyzing cellular immunogenicity in vaccine clinical trials [https://www.sciencedirect.com/science/article/abs/pii/S0022175919303151]
- 52. Flow Cytometry Assays for Cell Therapy [https://www.bioagilytix.com/blog/flow-cytometry-assays-for-cell-therapy/]
- 53. Intracellular Cytokine Staining: Number 1 - Flow Cytometry [https://flowcytometry.medicine.uiowa.edu/intracellular-cytokine-staining-number-1]
- 54. Methods integrating innate and adaptive immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12133800/]
- 55. Simulating CD8 T cell exhaustion [https://pmc.ncbi.nlm.nih.gov/articles/PMC12268933/]
- 56. Frontiers | Epigenetic regulation of CD8+ T cell exhaustion [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1700039/full]
- 57. Reviving Exhausted Immune Cells Boosts Tumor Elimination [https://news.weill.cornell.edu/news/2025/11/reviving-exhausted-immune-cells-boosts-tumor-elimination]
- 58. Intracellular Cytokine Staining Protocol [https://anilocus.com/intracellular-cytokine-staining-protocol/?srsltid=AfmBOorcuy8A7fKGOrvpAZ26lv1yiBfYfkwL2Jx6qwwMnXe-Ty7hu5oH]
- 59. T-Cell Exhaustion [https://www.sartorius.com/en/applications/life-science-research/high-throughput-screening-by-cytometry/t-cell-exhaustion]
- 60. Progenitor exhausted PD-1+ T cells are cellular targets of ... [https://www.nature.com/articles/s44161-025-00713-2]
- 61. CD137 agonism enhances anti-PD1 induced activation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11730579/]
- 62. Intracellular Cytokine Staining Protocol [https://anilocus.com/intracellular-cytokine-staining-protocol/?srsltid=AfmBOop8N5Nc-VUixHr8j5kiaZpnsYplzJFcJD0yuTAz3yL8p2Ow9PG4]
- 63. Intracellular Staining for Flow Cytometry Protocol ... [https://www.creativebiolabs.net/intracellular-staining-for-flow-cytometry.htm]
- 64. Troubleshooting Flow Cytometry [https://www.hycultbiotech.com/flow-cytometry/troubleshooting/]
- 65. Publishing flow cytometry data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2822558/]
- 66. Quantitative Flow Cytometry: Applications & Benefits [https://kcasbio.com/blogs/understanding-quantitative-flow-cytometry/]
- 67. Maximizing Insights, Minimizing Animal Testing: A Framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898573/]
- 68. Blog Post - Seeing in Full Color – Selecting the Right ... [https://www.cerbaresearch.com/article/blog-post-seeing-in-full-color-selecting-the-right-reagents-and-instrumentation-for-your-flow-cytometry-assay/]
- 69. Panel Design [https://www.bdbiosciences.com/en-us/resources/panel-design]
- 70. Spectral Spillover in Flow Cytometry [https://fluorofinder.com/spectral-spillover/]
- 71. Choosing Fluorophores for Microscopy and Flow Cytometry [https://bitesizebio.com/30265/choosing-fluorophore-palette/]
- 72. A Guide to Spectral Flow Cytometry Fluorophore Selection [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/flow-cytometry/flow-cytometry-learning-center/flow-cytometry-resource-library/flow-cytometry-methods/spectral-flow-cytometry-fluorophore-selection.html]
- 73. Recommended controls for flow cytometry | Abcam [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/recommended-controls-for-flow-cytometry]
- 74. When To Use (And Not Use) Flow Cytometry Isotype Controls - ExpertCytometry [https://expertcytometry.com/when-to-use-and-not-use-flow-cytometry-isotype-controls/]
- 75. Introduction to Multiparametric Flow Cytometry and Analysis of High-Dimensional Data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7868168/]
- 76. FMO Protocol | Flow Cytometry Core | ECU [https://medicine.ecu.edu/flow-core/fmo-protocol/]
- 77. Optimized Intracellular Staining Reveals Heterogeneous ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.654094/full]
- 78. Intracellular Cytokine Staining Protocol [https://anilocus.com/intracellular-cytokine-staining-protocol/?srsltid=AfmBOopfQ2q4zu_RMfvTtu1w2YnDWfXZ4sPUOyth-nKZ5gwGtoGs5Irx]
- 79. (IC) Intracellular Staining Flow Cytometry Protocol Using ... [https://www.rndsystems.com/resources/protocols/flow-cytometry-protocol-staining-intracellular-molecules-using-detergents]
- 80. Comparison of interferon gamma release assays and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521551/]
- 81. Comparing the Diagnostic Performance of QuantiFERON ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8423471/]
- 82. ELISA, ELISPOT and alternative assays [https://pivotalscientific.com/scientific-library/elisa-elispot-and-alternative-assays/]
- 83. Multiplexed Elispot Assay - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2665127/]
- 84. Cell Signaling ELISA Kits and Multiplex Immunoassays [https://www.thermofisher.com/us/en/home/life-science/antibodies/immunoassays/immunoassay-research-areas/cell-signaling-elisa-kits-immunoassays.html]
- 85. Comparing Flow Cytometry and ELISpot for Detection of IL- ... [https://pubmed.ncbi.nlm.nih.gov/38502389/]
- 86. Standardization of flow cytometry and cell sorting to enable a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9997938/]
- 87. Intracellular Cytokine Staining Protocol [https://anilocus.com/intracellular-cytokine-staining-protocol/?srsltid=AfmBOorPDYeQr3Wzs8oFkWz2rwnTAB2k25WdTXbiKL3ciChcW2iLqHfQ]
- 88. Standardization procedure for flow cytometry data ... [https://www.nature.com/articles/s41598-020-68468-3]
- 89. CD4 Polyfunctional - T with in vitro mycobacterial... cells correlate [https://pubmed.ncbi.nlm.nih.gov/27622301/]
- 90. Single-cell multiplexed cytokine profiling of CD19 CAR- T reveals... cells [https://jitc.biomedcentral.com/articles/10.1186/s40425-017-0293-7]
- 91. Intracellular Cytokine Staining: Number 2 | Flow Cytometry [https://flowcytometry.medicine.uiowa.edu/intracellular-cytokine-staining-number-2]
- 92. Newsletter: Analysis of Rare Cell Populations [https://fluorofinder.com/analysis-of-rare-cell-populations/]
- 93. Rare-Event Detection Using Flow Cytometry [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-71/bioprobes-71-flow-cytometry-rare-event-detection.html]
- 94. Statistical Challenges Of Rare Event Measurements In Flow ... [https://expertcytometry.com/statistical-challenges-of-rare-event-measurements-in-flow-cytometry/]
- 95. Intracellular Cytokine Staining Protocol [https://anilocus.com/intracellular-cytokine-staining-protocol/?srsltid=AfmBOopWfVpPMrqCAywjUwqj6b7YX0BffedkpZFDq2PqWP1r3hW5M0cv]