Illuminating the Future: A Comprehensive Guide to Careers in Biomedical Engineering and Optics
This article provides a detailed exploration of the rapidly converging fields of biomedical engineering and optics, tailored for researchers, scientists, and drug development professionals.
Illuminating the Future: A Comprehensive Guide to Careers in Biomedical Engineering and Optics
Abstract
This article provides a detailed exploration of the rapidly converging fields of biomedical engineering and optics, tailored for researchers, scientists, and drug development professionals. It covers the foundational principles of these disciplines, explores specialized career paths from medical imaging to biomaterials, addresses key industry challenges and optimization strategies, and validates career decisions through market trends and comparative analysis. The guide synthesizes current data and emerging trends to empower professionals in navigating and advancing their careers at this dynamic technological frontier.
The Convergence of Light and Life: Understanding Biomedical Engineering and Optics
The convergence of engineering principles with biological systems represents a paradigm shift in modern healthcare and scientific research. This synergy, particularly within biomedical engineering and optics, is catalyzing breakthrough innovations in therapeutic development, diagnostic imaging, and precision medicine. By applying quantitative engineering approaches—including optics, photonics, computational modeling, and materials science—to complex biological challenges, researchers are developing transformative solutions that overcome limitations of traditional methodologies. This technical guide examines the core interdisciplinary frameworks driving this integration, with focused analysis on optical manipulation technologies, phototherapy applications, computational drug discovery, and emerging regulatory considerations. The following sections provide detailed experimental protocols, quantitative analyses, and visualization tools essential for researchers, scientists, and drug development professionals working at this innovative intersection.
Fundamental Synergistic Frameworks
The integration of engineering and biological systems operates through several interconnected mechanistic frameworks that enable precise observation, measurement, and manipulation of biological processes. These frameworks provide the foundation for developing advanced research and therapeutic applications.
Optical and Photonic Engineering applies principles of light-matter interactions to biological systems. Technologies including optical tweezers, photothermal therapy, and fluorescence imaging enable non-invasive manipulation and measurement of cellular and molecular processes [1] [2]. These approaches leverage the unique properties of light to probe biological systems with minimal perturbation, allowing researchers to study mechanisms in native states.
Computational and Modeling Approaches create digital representations of biological systems through finite element analysis, computational fluid dynamics, and multi-scale modeling. These engineering methodologies simulate complex biological phenomena across temporal and spatial scales, from molecular interactions to organ-level systems [3]. Machine learning algorithms further enhance these models by identifying patterns in high-dimensional biological data, enabling predictive analytics for disease progression and therapeutic response.
Materials and Nanoscale Engineering designs biocompatible materials and nanostructures with precisely controlled physical, chemical, and biological properties. These engineered materials interface with biological systems through targeted drug delivery vehicles, tissue engineering scaffolds, and implantable biosensors [2] [4]. By controlling features at nanoscale dimensions, researchers can create systems that mimic natural biological structures and functions.
Table 1: Core Engineering Disciplines and Their Biological Applications
| Engineering Discipline | Key Principles | Biological Applications | Representative Technologies |
|---|---|---|---|
| Optical Engineering | Light-matter interaction, photonics, imaging | Cellular manipulation, molecular detection, intraoperative imaging | Optical tweezers, fluorescence-guided surgery, photodynamic therapy [1] [2] |
| Computational Engineering | Modeling, simulation, data analysis | Drug discovery, protein folding prediction, systems biology | AlphaFold, molecular docking, patient-specific biomechanical models [3] |
| Materials Engineering | Biomaterials, nanotechnology, surface science | Drug delivery, tissue engineering, medical implants | Nanoparticle drug carriers, 3D-bioprinted tissues, biocompatible coatings [2] [4] |
| Mechanical Engineering | Biomechanics, fluid dynamics, thermodynamics | Prosthetics, surgical devices, artificial organs | Exoskeletons, microfluidic organ-on-chip models, heart valves [5] [6] |
Optical Manipulation Technologies in Biomedical Research
Optical manipulation technologies represent a prime example of engineering principles applied to biological investigation. These techniques utilize the momentum transfer of light to precisely control biological specimens without physical contact, enabling novel experimental capabilities.
Core Optical Manipulation Modalities
Optical Tweezers employ highly focused laser beams to generate gradient forces that trap and manipulate microscopic particles, including individual molecules, organelles, and cells [1]. Advanced configurations include holographic optical tweezers that create multiple independent trapping points through wavefront shaping, enabling complex manipulation protocols. Applications in biophysics include single-molecule force measurements on motor proteins like kinesin and myosin, studies of DNA mechanics and chromatin organization, and investigation of cellular mechanical properties through membrane tether formation.
Optofluidics integrates optical control with microfluidic environments to create lab-on-a-chip platforms for high-throughput biological analysis [1]. These systems enable automated sorting, patterning, and analysis of cells and particles within precisely controlled microenvironments. By combining optical forces with fluidic flow, researchers can achieve rapid classification of cellular populations based on optical properties, continuous monitoring of cellular responses to environmental changes, and isolation of rare cells for diagnostic applications.
Photophoresis and Alternative Manipulation Techniques utilize light-induced motion phenomena for specialized applications. Photophoresis exploits radiometric forces generated by non-uniform heating of particles, enabling manipulation of absorbing specimens that challenge conventional optical tweezers [1]. Integration with complementary techniques including acoustic manipulation, magnetic tweezers, and optoelectronic tweezers further expands experimental capabilities for diverse biological samples.
Experimental Protocol: Single-Molecule Biophysics Using Optical Tweezers
The following protocol details methodology for investigating molecular motor mechanics through optical manipulation, representative of approaches used in cutting-edge biophysics research [1]:
Research Objective: Quantify the force generation and stepping mechanics of cytoskeletal motor proteins (e.g., kinesin-1) along microtubule filaments.
Materials and Reagents:
- Purified motor protein constructs with engineered attachment handles (e.g., HaloTag or SNAP-tag)
- Microtubules polymerized from tubulin with biotin labels for surface attachment
- Streptavidin-coated polystyrene microspheres (1-3 μm diameter) for trapping
- Anti-GFP antibody-conjugated microspheres for handling GFP-tagged proteins
- ATP regeneration system (ATP, creatine phosphate, creatine kinase)
- Intracellular mimic buffer (e.g., BRB80 with oxygen scavenging system)
Instrumentation Setup:
- Dual-beam optical trapping system with infrared lasers (1064 nm)
- High-numerical aperture water immersion objective (NA ≥1.2)
- Piezo-controlled microscope stage with nanometer precision
- Quadrant photodiode detector with bandwidth >100 kHz
- Inverted microscope configuration with differential interference contrast imaging
Experimental Procedure:
- Sample Chamber Preparation: Create flow chambers (~10-20 μL volume) using paraffin wax and glass coverslips. Introduce biotinylated BSA (0.5 mg/mL), followed by streptavidin (0.5 mg/mL), and finally biotinylated microtubules diluted in assay buffer. Allow 5-minute incubations between steps.
Bead-Protein Conjugation: Incubate antibody-coated trapping beads with purified motor proteins at approximately 1:1 molar ratio for 30 minutes at 4°C. Dilute to appropriate concentration for single-molecule detection.
Optical Trap Calibration: Dilute bead-protein mixture in assay buffer and introduce to chamber. Trap individual beads and calibrate trap stiffness using power spectrum analysis of Brownian motion or drag force methods. Typical stiffness values range from 0.01-0.1 pN/nm.
Data Acquisition: Position trapped bead-motor complex near surface-attached microtubule. Initiate movement by introducing ATP-containing buffer. Record bead position at ≥10 kHz sampling rate while motor proteins move along microtubule track.
Force Measurements: Apply opposing force by moving stage against direction of motor movement. Measure stall force where motor progression ceases. For kinesin-1, expected stall forces approximate 5-7 pN.
Data Analysis:
- Process raw position data using custom algorithms to detect steps (sized ~8 nm for kinesin)
- Calculate force-velocity relationships by varying load forces
- Determine kinetic parameters from dwell-time distributions between steps
- Develop theoretical models matching mechanical and chemical reaction cycles
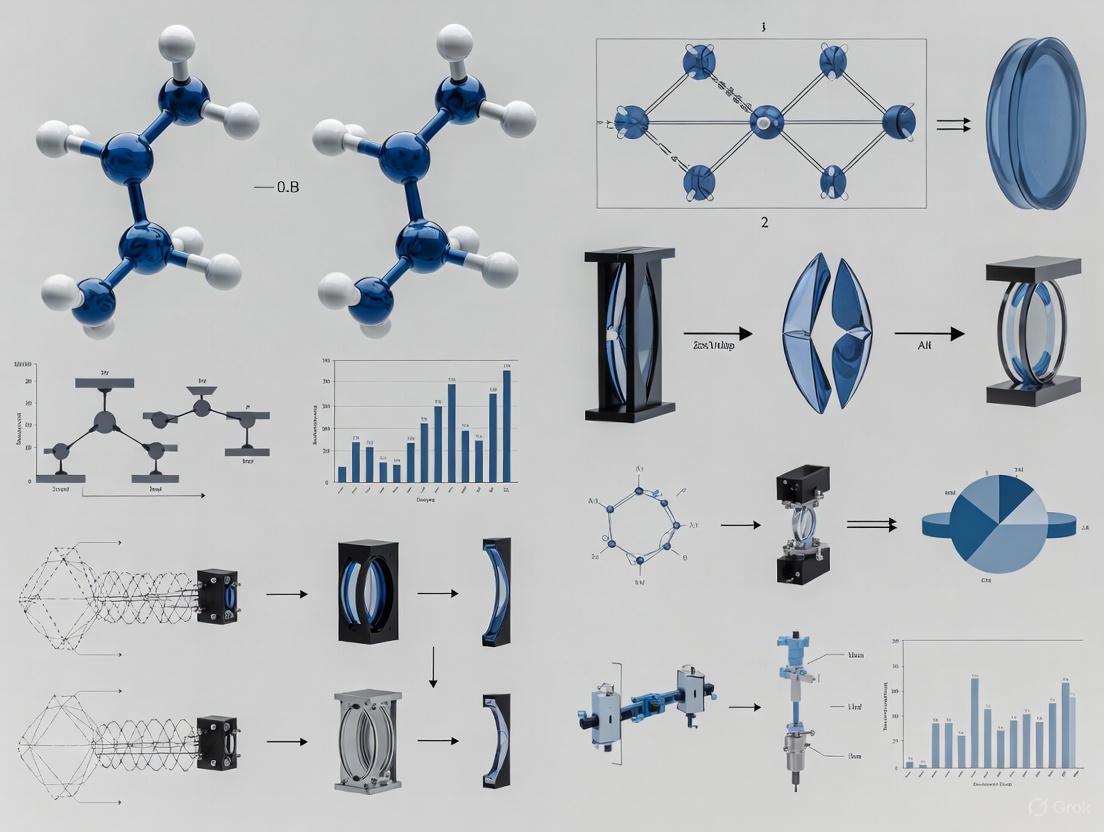
Diagram 1: Optical tweezers experimental workflow for single-molecule biophysics
Phototherapy and Optical Imaging in Therapeutic Applications
Photonic approaches have emerged as powerful therapeutic modalities that exemplify the engineering-biology synergy, particularly in oncology. These technologies leverage light-activated mechanisms to achieve precise spatial and temporal control over treatment effects.
Phototherapy Mechanisms and Applications
Photodynamic Therapy (PDT) utilizes photosensitizing agents that generate cytotoxic reactive oxygen species upon light activation [2]. The multi-step process begins with systemic or local administration of photosensitizers that accumulate preferentially in target tissues. Subsequent illumination with specific wavelengths activates these compounds, producing singlet oxygen and other reactive species that induce localized cell death through apoptosis and necrosis pathways. Engineering challenges include optimizing light delivery systems for deep-seated tumors, developing photosensitizers with improved tissue specificity, and controlling oxygen dependency in hypoxic tumor microenvironments.
Photothermal Therapy (PTT) employs light-absorbing nanomaterials that convert photon energy into thermal energy, generating localized hyperthermia that ablates target cells [2]. Noble metal nanoparticles (e.g., gold nanorods, nanoshells) with tunable surface plasmon resonance properties can be engineered to absorb strongly in the near-infrared tissue transparency window, enabling deeper tissue penetration. The resulting temperature increases (typically to 42-48°C) induce protein denaturation, membrane disruption, and ultimately coagulative necrosis. Engineering advances focus on optimizing photothermal conversion efficiency, developing multimodal agents that combine therapy and imaging, and creating activatable systems that respond to tumor-specific stimuli.
Photochemical Internalization (PCI) represents a more recent approach that light to enhance intracellular drug delivery [2]. This technology utilizes photosensitizers localized in endosomal and lysosomal membranes that, upon illumination, disrupt these compartments through reactive oxygen species generation. This controlled disruption releases therapeutic agents (e.g., proteins, nucleic acids, chemotherapeutics) trapped in endocytic vesicles into the cytosol, significantly enhancing their biological activity. PCI demonstrates particular promise for delivering macromolecular drugs that otherwise exhibit poor endosomal escape efficiency.
Experimental Protocol: Nanoparticle-Mediated Photothermal Therapy
This protocol details methodology for evaluating photothermal therapeutic efficacy using gold nanorods, representative of approaches in translational nanomedicine [2]:
Research Objective: Quantify the photothermal efficiency and cancer cell ablation capability of surface-functionalized gold nanorods.
Materials and Reagents:
- Cetyltrimethylammonium bromide (CTAB)-capped gold nanorods (peak absorption ~800 nm)
- Polyethylene glycol (PEG) conjugation reagents (mPEG-SH, MW 5000)
- Target-specific ligands (e.g., folate, RGD peptides, antibodies) for surface functionalization
- Cancer cell lines with appropriate target receptor expression
- Cell culture media and viability assay reagents (MTT, Calcein-AM/propidium iodide)
- Near-infrared laser system (800 nm wavelength, 0.5-2 W/cm² adjustable power density)
Nanoparticle Functionalization:
- PEGylation: Incubate CTAB-stabilized nanorods (1 nM) with mPEG-SH (100 μM) for 12 hours at room temperature with gentle stirring. Remove excess PEG through centrifugation (12,000 rpm, 15 minutes) and resuspend in phosphate buffer.
- Targeting Ligand Conjugation: React PEGylated nanorods with heterobifunctional PEG derivatives (e.g., NHS-PEG-Maleimide) for 2 hours. Purify and incubate with thiolated targeting ligands (1:100 molar ratio) overnight at 4°C.
- Characterization: Verify surface modification through zeta potential measurements, spectrophotometric analysis of surface plasmon resonance shifts, and dynamic light scattering for hydrodynamic size determination.
In Vitro Photothermal Efficacy:
- Cellular Uptake Studies: Incubate target cells with functionalized nanorods (0.1 nM) for 2-24 hours. Quantify internalization through atomic absorption spectroscopy, darkfield microscopy, or flow cytometry of scattering signals.
- Photothermal Treatment: Plate cells in 96-well plates (10,000 cells/well) and incubate with nanorods for 6 hours. Wash to remove uninternalized particles. Illuminate with NIR laser (800 nm, 1 W/cm²) for 5-10 minutes. Monitor temperature changes using infrared thermal camera.
- Viability Assessment: Perform MTT assay 24 hours post-illumination to quantify metabolic activity. Conduct live/dead staining (Calcein-AM/propidium iodide) for direct visualization of treatment effects. Compare to controls including cells only, nanorods only, and laser only.
Mechanistic Investigations:
- Analyze apoptosis induction through Annexin V/propidium iodide flow cytometry
- Examine cellular morphology changes via transmission electron microscopy
- Measure heat shock protein expression (HSP70, HSP90) through western blotting
- Evaluate mitochondrial membrane potential disruption using JC-1 staining
Table 2: Research Reagent Solutions for Photothermal Therapy Experiments
| Reagent/Category | Specific Examples | Function in Experiment | Key Characteristics |
|---|---|---|---|
| Photothermal Nanomaterials | Gold nanorods, nanoshells, carbon nanotubes | Light absorption and heat generation | Tunable plasmon resonance, high photothermal conversion efficiency, biocompatibility [2] |
| Surface Modification Agents | mPEG-SH, PEG-phospholipids, heterobifunctional linkers | Improve biocompatibility and targeting | Stealth properties, reduced protein adsorption, functional groups for ligand attachment [2] |
| Targeting Ligands | Folate, RGD peptides, transferrin, monoclonal antibodies | Specific recognition of target cells | High affinity for receptors overexpressed on target cells, appropriate conjugation chemistry [2] |
| Characterization Tools | Dynamic light scattering, UV-Vis-NIR spectroscopy, electron microscopy | Nanoparticle physicochemical characterization | Size distribution, surface charge, optical properties, morphology determination [2] |
| Biological Assessment | MTT assay, live/dead staining, Annexin V apoptosis kit | Evaluation of therapeutic efficacy and mechanisms | Metabolic activity, membrane integrity, apoptosis pathway activation [2] |
Computational and AI-Driven Integration in Biomedical Research
Artificial intelligence and computational modeling have dramatically accelerated the integration of engineering principles with biological discovery, particularly in pharmaceutical development and systems biology.
AI-Enhanced Drug Discovery Pipelines
Target Identification and Validation leverages machine learning algorithms to integrate multi-omics datasets, literature mining, and experimental data for prioritizing therapeutic targets [3]. Platforms such as PandaOmics employ deep learning and natural language processing to analyze gene expression patterns, protein-protein interactions, and genetic association studies across thousands of diseases. This systems biology approach identifies not only individual targets but also complex pathway dependencies and network vulnerabilities. For ophthalmology applications, AI-driven target discovery has accelerated identification of novel pathways in geographic atrophy and diabetic retinopathy, conditions with limited treatment options.
Structure-Based Drug Design utilizes computational prediction of protein structures and molecular docking simulations to optimize therapeutic compounds [3]. The AlphaFold system represents a transformative engineering achievement, accurately predicting protein three-dimensional structures from amino acid sequences using deep neural networks. These structural predictions enable virtual screening of compound libraries against target proteins, significantly reducing the experimental burden of high-throughput screening. Subsequent molecular dynamics simulations model drug-target interactions with atomic resolution, providing insights into binding kinetics, conformational changes, and residence times that inform lead optimization.
Clinical Trial Optimization applies AI algorithms to improve patient stratification, endpoint selection, and trial efficiency [3]. Machine learning models trained on electronic health records, medical images, and genomic data can identify patient subgroups most likely to respond to investigational therapies. In ophthalmology drug development, AI analysis of retinal images enables quantitative tracking of disease progression, providing sensitive biomarkers for clinical trial endpoints. These computational approaches have demonstrated potential to reduce clinical trial durations and improve success rates through enhanced experimental design.
Experimental Protocol: AI-Guided Drug Discovery for Ocular Diseases
This protocol outlines a computational framework for identifying and optimizing novel therapeutics for ocular disorders, representing cutting-edge approaches in digital drug discovery [3]:
Research Objective: Identify and computationally validate novel inhibitors of angiogenesis for treatment of diabetic retinopathy.
Materials and Computational Resources:
- Multi-omics datasets (transcriptomics, proteomics) from diabetic retinopathy patient samples
- Structural databases (Protein Data Bank, AlphaFold Protein Structure Database)
- Compound libraries (ZINC, ChEMBL, in-house collections)
- Molecular docking software (AutoDock Vina, Glide, GOLD)
- Molecular dynamics simulation packages (AMBER, GROMACS, Desmond)
- AI platforms for target discovery (PandaOmics, IBM Watson for Drug Discovery)
Computational Workflow:
Target Identification:
- Collect and preprocess transcriptomic data from public repositories (GEO, ArrayExpress) and proprietary diabetic retinopathy datasets
- Apply PandaOmics AI platform to analyze differential expression, pathway enrichment, and disease association
- Prioritize targets based on novelty, druggability, and network centrality scores
- Validate target selection through literature mining and expression profiling in ocular tissues
Structure Preparation:
- Retrieve three-dimensional structure of prioritized target from PDB or generate using AlphaFold2
- Prepare protein structure through hydrogen atom addition, assignment of protonation states, and optimization of hydrogen bonding networks
- Define binding site based on experimental data or computational prediction
Virtual Screening:
- Prepare compound library through structure standardization, tautomer enumeration, and generation of 3D conformers
- Perform high-throughput docking using validated parameters and scoring functions
- Select top candidates based on docking scores, binding poses, and interaction patterns
- Apply machine learning models to predict ADMET properties and prioritize compounds with favorable pharmacological profiles
Molecular Dynamics Validation:
- Solvate top-ranked ligand-protein complexes in explicit water boxes with appropriate ions
- Perform energy minimization and equilibration using standard protocols
- Conduct production simulations (100-200 ns) with periodic boundary conditions
- Analyze trajectory data for binding stability, interaction persistence, and conformational changes
- Calculate binding free energies using MM/PBSA or MM/GBSA methods
Experimental Collaboration:
- Synthesize or procure top computational candidates for experimental validation
- Design in vitro assays to confirm target engagement and functional activity
- Evaluate cytotoxicity and specificity in relevant ocular cell models
- Iteratively refine computational models based on experimental results
Diagram 2: AI-driven drug discovery workflow for ocular therapeutics
Career Pathways at the Engineering-Biology Interface
The integration of engineering and biological systems has created diverse career opportunities that leverage interdisciplinary expertise. These roles span academic research, industrial development, clinical implementation, and regulatory affairs.
Emerging Professional Roles
Medical Device and Imaging Engineers design, develop, and optimize technologies that interface directly with biological systems [5] [6] [4]. These professionals combine knowledge of physiological principles with engineering design to create diagnostic and therapeutic devices. Specializations include optical imaging system development, surgical robotics, wearable sensors, and point-of-care diagnostics. The expanding regulatory framework for optical imaging drugs described in FDA draft guidance further drives demand for engineers who can navigate the device-drug combination product landscape [7] [8].
Computational Biomedical Specialists develop and apply algorithms, models, and data analysis approaches to biological challenges [5] [6] [3]. Roles include bioinformaticians who analyze genomic and proteomic datasets, computational biologists who model biological networks, and AI specialists who develop predictive algorithms for therapeutic discovery. These positions require strong computational backgrounds alongside understanding of biological principles, with particular demand for professionals skilled in machine learning applications for healthcare.
Regulatory Science and Clinical Engineering professionals ensure that biomedical technologies meet safety and efficacy standards while facilitating their translation to clinical use [5] [6]. Clinical engineers manage medical equipment in healthcare settings, while regulatory affairs specialists navigate approval processes for new technologies. The January 2025 FDA draft guidance on developing optical imaging drugs highlights the growing regulatory complexity for combination products, creating demand for professionals with both technical and regulatory expertise [7] [8].
Table 3: Quantitative Career Outlook in Biomedical Engineering Specializations
| Specialization Area | Median Salary Range | Projected Growth (2024-2034) | Key Industry Sectors | Typical Educational Requirements |
|---|---|---|---|---|
| Medical Device Design & Development | $86,586 (U.S. average) [5] | 5% (faster than average) [6] | Medical device companies, biotechnology firms, startups | Bachelor's minimum, Master's preferred for R&D roles |
| Clinical Engineering | $89,338 (U.S. average) [5] | 5% (faster than average) [6] | Hospitals, healthcare systems, equipment manufacturers | Bachelor's with clinical engineering certification |
| Biomedical Imaging & AI Analytics | $106,950 (median for bioengineers) [6] | 12% (medical device sector) [5] | Imaging equipment manufacturers, AI diagnostics companies, research institutions | Master's or PhD for research positions |
| Tissue Engineering & Regenerative Medicine | Varies by role: $85,000-$120,000 | 5% (faster than average) [6] | Biotech, pharmaceutical companies, academic research centers | PhD typically required for research leadership |
| Bioinformatics & Computational Biology | $150,000-$170,000 (experienced with MS/PhD) [5] | Rapid expansion [5] | Pharmaceutical R&D, genomics companies, research institutions | Master's or PhD with computational focus |
Professional Development Framework
Educational Pathways for careers at the engineering-biology interface typically begin with undergraduate degrees in biomedical engineering, bioengineering, or related disciplines [6] [4]. Foundational coursework integrates biological sciences with engineering principles, often complemented by laboratory research experiences. Advanced positions frequently require graduate education, with master's and doctoral programs providing specialized training in areas such as neural engineering, biomaterials, medical optics, or computational biology. Professional master's programs increasingly emphasize industry-relevant skills and include capstone projects addressing real-world challenges.
Skill Development beyond core technical competencies includes interdisciplinary communication, project management, and regulatory knowledge [6]. Professionals must effectively translate between engineering and biological paradigms, requiring fluency in both domains. Experimental design skills must incorporate considerations of biological variability, ethical requirements, and clinical translation pathways. Familiarity with regulatory frameworks, such as the FDA guidance on optical imaging drugs, becomes increasingly important for roles involved in product development [7] [8].
Research Training experiences provide critical preparation for careers at this interface [9] [10]. Programs such as the Synergy Summer Studentship at UBC offer structured research experiences that integrate professional development with laboratory investigation [9]. These opportunities enable trainees to apply engineering approaches to biological questions while developing technical and professional skills. Similar research internships and training programs are offered by institutions including Harvard Medical School, Oregon Health & Science University, and the National Institutes of Health [10].
Regulatory and Commercialization Landscape
The translation of technologies emerging from engineering-biology integration requires navigation of evolving regulatory pathways and commercialization challenges.
Regulatory Considerations for Combination Products
Technologies that combine engineering platforms with biological components frequently fall under regulatory frameworks for combination products [7] [8]. The January 2025 FDA draft guidance "Developing Drugs for Optical Imaging" addresses one category of these products, providing recommendations for clinical trial design of optical imaging drugs used with imaging devices during surgical procedures [7] [8]. This guidance highlights several key considerations:
Clinical Trial Design must demonstrate that optical imaging drugs enhance surgeons' ability to identify pathological tissues while maintaining safety profiles [7] [8]. Endpoints typically include sensitivity and specificity for target detection compared to standard visual inspection and palpation. Trials must account for intended use population, procedure type, and clinical context, with specific considerations for molecularly targeted fluorescent agents that highlight tumor margins.
Device-Drug Integration requires coordinated development of both components, with testing to demonstrate compatibility and performance [7] [8]. The guidance emphasizes that imaging device characteristics including illumination intensity, detection sensitivity, and spatial resolution directly impact drug performance and must be appropriately controlled and documented.
Labeling and Instructions for Use must provide clear guidance on proper administration, imaging timing relative to drug dosing, and device operation parameters [7] [8]. This information ensures that the combined product delivers consistent performance across clinical settings and user expertise levels.
Commercialization Pathways
Technology Transfer from academic research to commercial development requires strategic intellectual property protection and licensing [6] [4]. Technologies with strong patent positions and clear regulatory pathways attract greater investment and have higher translation potential. The expanding definition of biomedical engineering into optics, AI, and nanotechnology creates new intellectual property opportunities at discipline intersections.
Market Analysis must assess clinical need, competitive landscape, reimbursement considerations, and adoption barriers [6] [4]. Technologies addressing unmet needs in areas such as cancer surgery, rare diseases, or diagnostic challenges may receive expedited regulatory review and premium reimbursement. The $66 billion global ophthalmic drug market exemplifies the economic potential for targeted technologies in specific therapeutic areas [3].
Business Models for engineering-biology technologies vary from traditional medical device approaches to software-as-a-service platforms for AI diagnostics [6] [4]. Companies developing combination products must establish quality systems that address both device and drug regulatory requirements, creating operational complexity that requires specialized expertise.
Future Directions and Emerging Opportunities
The synergy between engineering and biological systems continues to evolve, driven by technological advances and unmet medical needs. Several emerging areas represent particularly promising frontiers for research and development.
Integrated Theragnostic Platforms combine diagnostic capabilities with therapeutic interventions in closed-loop systems [2]. These platforms utilize biosensors to monitor disease states or treatment responses, with algorithms that adjust therapeutic interventions in real time. Examples include glucose-responsive insulin delivery systems and implantable devices that detect and terminate cardiac arrhythmias. Optical technologies contribute through miniaturized sensors, light-based actuation mechanisms, and non-invasive monitoring approaches.
Neuroengineering Innovations interface engineering systems with neural circuits to restore function following injury or disease [5] [6] [4]. Advancements in brain-computer interfaces, neuroprosthetics, and neuromodulation therapies create new opportunities for treating conditions including paralysis, Parkinson's disease, and psychiatric disorders. Optical methods such as optogenetics enable precise control of specific neural populations, while optical imaging provides detailed functional mapping of neural activity.
Sustainable Biomedical Engineering addresses environmental impacts of medical technologies while expanding global healthcare access [6]. Developments include biodegradable implants, low-power medical devices for resource-limited settings, and point-of-care diagnostics that function without sophisticated laboratory infrastructure. These approaches apply engineering principles to optimize healthcare delivery while minimizing ecological footprint.
Digital Health Integration connects biomedical devices with data analytics platforms to enable continuous health monitoring and personalized interventions [6] [3]. Wearable sensors, smartphone-based diagnostics, and remote monitoring systems generate high-frequency data streams that, when analyzed with machine learning algorithms, can detect early disease signatures and guide preventive interventions. The validation of these digital biomarkers represents an active area of research and regulatory development.
The continued convergence of engineering and biological systems promises to transform healthcare through more precise, personalized, and accessible technologies. Professionals working at this interface will drive innovations that address fundamental biological challenges through engineering principles, creating solutions that benefit patients worldwide.
Biomedical engineering stands as one of the fastest-evolving fields, uniquely blending medicine, biology, and technology to develop advanced healthcare solutions [5]. This discipline empowers professionals to innovate across a spectrum of areas—from medical devices and diagnostic tools to prosthetics and regenerative therapies [5]. As healthcare demands grow and technology accelerates, specialization within biomedical engineering has become increasingly critical. Specializations enable engineers to develop deep expertise in high-demand areas, opening doors to leadership roles in research, product development, and healthcare technology management [5]. For researchers and scientists in drug development, understanding these sub-fields is essential for leveraging cutting-edge engineering principles to advance therapeutic discovery, diagnostic precision, and clinical implementation. This guide provides a technical examination of core specializations, with particular focus on bioinstrumentation and biomedical optics, framing them within the context of career opportunities and research applications in the evolving biomedical landscape.
Core Sub-Fields and Specializations
Biomedical engineering encompasses a diverse array of sub-fields, each targeting specific challenges in medicine and biology. The table below summarizes the most in-demand specializations, their core focus areas, and associated career paths that are pivotal for researchers and scientists.
Table 1: Core Specializations in Biomedical Engineering
| Specialization | Core Focus & Technologies | Example Career Paths & Research Roles |
|---|---|---|
| Bioinstrumentation & Medical Device Design [5] [11] | Design of medical devices and instruments; surgical robots, wearable sensors, diagnostic tools [5] [11]. | Product Design Engineer, R&D Engineer, Manufacturing Engineer [5]. |
| Biomedical Imaging & Optics [5] [12] | Development of medical imaging systems (MRI, CT, ultrasound, OCT); image processing algorithms, AI analytics for enhanced diagnostics [5] [13] [12]. | Imaging Systems Engineer, Research Scientist, Clinical Imaging Specialist [5]. |
| Tissue Engineering & Regenerative Medicine [5] [12] | Application of biomaterials, stem cells, and 3D bioprinting to develop artificial tissues and organs [5] [12]. | Research Scientist, Bioprocess Engineer, Clinical Trials Manager [5]. |
| Biomechanics & Rehabilitation Engineering [5] [14] | Study of mechanical forces in biological systems; design of prosthetics, orthotics, and exoskeletons [5] [14]. | Prosthetics Designer, Rehabilitation Engineer, Sports Biomechanist [5]. |
| Biomaterials Engineering [5] | Development of safe and effective materials for implants, scaffolds, and drug delivery systems [5]. | Biomaterials Scientist, Implant Designer, Drug Delivery Engineer [5]. |
| Systems and Synthetic Biology [15] | Engineering principles to understand, design, and build cellular-level biological systems; engineered cells for therapy [15]. | Research Scientist, Bioengineer, Biotech Entrepreneur. |
| Neural Engineering [5] | Focus on the nervous system; development of brain-computer interfaces (BCIs) and neuroprosthetics [5]. | Neuroprosthetics Engineer, BCI Developer, Neuroengineering Researcher [5]. |
| Clinical Engineering & Regulatory Affairs [5] [14] | Ensuring medical device safety, efficacy, and regulatory compliance in healthcare settings [5] [14]. | Clinical Engineer, Regulatory Affairs Specialist, Healthcare Technology Manager [5]. |
Quantitative Analysis of Field
Quantitative data reveals the growing prominence and economic viability of specialized research areas within biomedical engineering. A systematic review of PubMed-indexed studies from 2018-2022 identified a statistically significant yearly increase in research utilizing anonymized biomedical data, a proxy for data-intensive fields like bioinformatics and medical imaging [16]. This trend underscores a broader movement towards computational and data-driven methodologies. Furthermore, geographical analysis of this research output indicates that the United States, United Kingdom, and Australia lead in the volume of studies employing shared anonymized data, suggesting mature research ecosystems and possibly more established regulatory pathways in these regions [16]. For the career-focused researcher, specializations like Medical Device Design, Clinical Engineering, and Bioinformatics are noted for offering a high return on investment (ROI) due to their strong industry demand and earning potential [5].
Table 2: Quantitative Trends and Return on Investment (ROI) in Key Specializations
| Specialization | Research Growth & Prevalence | Reported Salary and ROI Data |
|---|---|---|
| Medical Device Design & Development [5] | World demand expected to increase by 12% over the next decade [5]. | U.S. average salary: $86,586 (25th-75th percentile: $79,133 - $91,182) [5]. |
| Clinical Engineering [5] | Critical role in hospital operations and patient safety [5] [14]. | U.S. average salary: $89,338 (typical range: $79,873 - $99,169) [5]. |
| Bioinformatics & Data Science [5] | Taps into booming demand for data expertise in genomics and personalized medicine [5]. | Experienced bioinformaticians (MS/PhD) can earn $150,000 - $170,000 in competitive industry roles [5]. |
| Biomedical Engineering (General) [14] | Employment projected to grow 5% from 2022 to 2032 [14]. | Median annual wage: $108,060 [14]. |
Detailed Examination: Bioinstrumentation
Core Principles and Methodologies
Bioinstrumentation focuses on the design and development of devices and instruments used in the diagnosis, treatment, and prevention of disease [11]. This sub-field integrates principles from electronics, mechanics, and computer science with biological sciences to create tools that range from simple diagnostic equipment to complex, life-supporting systems [11]. A core methodological workflow in bioinstrumentation involves sensing a physiological signal, conditioning the acquired data, processing and analyzing the information, and finally presenting the results in a usable format for clinical or research decision-making.
Experimental Protocols and Workflows
A fundamental protocol in bioinstrumentation is the design and testing of a wearable biosensor for physiological monitoring, which exemplifies the integration of multiple engineering disciplines.
Table 3: Research Reagent Solutions for a Wearable Biosensor Prototype
| Item / Material | Function in Experimental Context |
|---|---|
| Flexible Substrate (e.g., PDMS) | Serves as the base material for the wearable sensor, providing conformability to the skin and patient comfort. |
| Electrophysiological Sensors (e.g., Ag/AgCl Electrodes) | Act as the transducer to capture biopotential signals (e.g., ECG, EMG) from the body's surface. |
| Microcontroller Unit (MCU) | The core "brain" that manages data acquisition from the sensors, preliminary signal processing, and data transmission. |
| Signal Conditioning Circuitry | Comprises amplifiers, filters, and analog-to-digital converters (ADC) to enhance signal quality and prepare it for digital processing. |
| Wireless Communication Module (e.g., Bluetooth Low Energy) | Enables the transmission of processed physiological data to a remote terminal such as a smartphone or laptop for visualization and analysis. |
| Bench-Top Signal Simulator | Used for initial validation and calibration of the sensor system by generating known, precise electrical signals that mimic physiological outputs. |
The following diagram illustrates the logical workflow and data flow in the development and validation of a bioinstrumentation device, from concept to preclinical testing.
Diagram 1: Bioinstrumentation Device Development Workflow
Detailed Examination: Biomedical Optics
Core Principles and Methodologies
Biomedical optics offers a non-invasive window into the intricate workings of the human body, revolutionizing medical diagnostics and treatment monitoring [12]. This sub-field leverages light and optical technologies to visualize internal structures, physiological processes, and metabolic activity [15] [12]. Key modalities include Optical Coherence Tomography (OCT), which provides high-resolution, cross-sectional imaging of tissue microstructures; diffuse optical imaging for assessing tissue oxygenation and metabolism; and various forms of clinical spectroscopy [13] [12]. Advances in AI and machine learning are now paving the way for more detailed and faster image analysis, while techniques like molecular imaging are creating new possibilities for early detection and personalized treatment strategies [5] [12].
Experimental Protocols and Workflows
A representative and cutting-edge protocol in this field involves the use of Swept-Source Optical Coherence Tomography (SS-OCT) for high-resolution, volumetric imaging of biological tissues [13]. The following diagram outlines the core components and signal processing pathway of an SS-OCT system.
Diagram 2: Swept-Source OCT System Dataflow
The experimental workflow for an SS-OCT study, such as measuring eardrum vibrations or creating large-area images, involves several key stages [13]. The process begins with System Calibration and Phase Stabilization, which is critical for achieving high-quality, reliable data. Recent research focuses on novel phase stabilization techniques to mitigate environmental perturbations [13]. Next, Data Acquisition involves scanning the sample using specific raster scanning patterns (e.g., stripe-like scanning for large areas) [13]. The light backscattered from the sample and reflected from the reference mirror generates an interference pattern, which is captured by the photodetector and digitized. Signal Processing is then performed, which includes Fourier transformation to convert the raw spectral data into depth-resolved (A-scan) information. Multiple A-scans are combined to form cross-sectional (B-scan) or volumetric (3D) images. Finally, Image Analysis and Interpretation is conducted, often leveraging algorithms for tasks like segmenting specific tissue layers or quantifying vibrational amplitudes.
Table 4: Key Research Reagents and Materials for SS-OCT Experimentation
| Item / Material | Function in Experimental Context |
|---|---|
| Swept-Source Laser | The light source that rapidly tunes its wavelength over a broad range, defining the axial resolution and imaging depth of the system. |
| Single-Mode Optical Fiber & Couplers | The network for guiding and splitting the laser light between the reference and sample arms of the interferometer. |
| High-Speed Photodetector & Digitizer | Captures the weak interference signal and converts it from an analog to a digital format for subsequent computation. |
| Galvanometric Scanning Mirrors | Precisely steer the sample beam to scan it across the tissue surface in a defined raster pattern. |
| Computational Hardware (e.g., Raspberry Pi) | Used for system control, initial data processing, and potentially for adapting systems into more compact, cost-effective formats [13]. |
| Spectral Analysis Software | Essential for calibrating the laser, detecting its optical sweeping direction, and processing the raw k-space data into meaningful images [13]. |
Career Pathways and Convergence with Optics Research
The specializations of bioinstrumentation and biomedical optics offer robust and diverse career paths for researchers and scientists. Professionals can find opportunities in academic research, industrial research and development (R&D), clinical environments, and government agencies [5] [12]. In the industrial sector, biomedical engineers work for medical device manufacturers, pharmaceutical companies, and biotech startups, with responsibilities spanning device design, procedure development, and clinical problem-solving [12]. The entrepreneurial sector is particularly vibrant, with startups serving as innovation hubs for emerging technologies [11].
The convergence of biomedical engineering with optics and photonics research is a particularly dynamic frontier. Professional organizations like Optica and SPIE actively foster this interdisciplinary community, sponsoring major conferences such as the European Conferences on Biomedical Optics (ECBO) that cover topics from advanced microscopy and spectroscopy to OCT and therapeutic laser applications [13]. These gatherings are critical for networking, sharing breakthroughs, and career development for early-career professionals [17] [13]. The job market for optical engineering skills is broad, with roles including Optical Engineer, Systems Engineer, Optical Designer, and Application Engineer, many of which are directly applicable to the medical device and imaging industries [18]. For those in drug development and research, collaborating with or becoming an expert in biomedical optics means gaining access to powerful tools for non-invasive, high-resolution imaging that can accelerate therapeutic evaluation and fundamental biological understanding.
The convergence of photonics and biomedical devices is creating a paradigm shift in modern healthcare, enabling breakthroughs in diagnostics, treatment, and patient monitoring. This whitepaper provides an in-depth analysis of growth projections in these synergistic fields, framed within the context of career opportunities for researchers, scientists, and drug development professionals. Photonics, the science of generating, detecting, and manipulating light, is becoming increasingly integral to biomedical innovation, from advanced imaging systems to minimally invasive surgical tools. We examine quantitative market data, detail experimental methodologies underpinning key technologies, and visualize the interdisciplinary workflows driving this expansion. For professionals in biomedical engineering and optics research, understanding these trends is crucial for positioning themselves at the forefront of medical technology innovation. The integration of light-based technologies with biological systems is not only expanding diagnostic capabilities but also creating new pathways for therapeutic development and personalized medicine.
The photonics and biomedical device markets are experiencing robust growth globally, driven by technological advancements, increasing healthcare demands, and the rising prevalence of chronic diseases. This section provides a detailed quantitative analysis of current market sizes and future projections.
Table 1: Global Photonics Market Projections (2023-2032)
| Metric | 2023/2024 Value | Projected Value | Time Period | CAGR | Key Drivers |
|---|---|---|---|---|---|
| Global Photonics Market | $920.56 billion (2023) [19] | $1,642.61 billion [19] | 2024-2032 [19] | 6.7% [19] | Non-invasive healthcare, additive manufacturing, surveillance & biometric ID [19] |
| U.S. Photonics Market | $142.55 billion (2024) [20] | $221.33 billion [20] | 2024-2033 [20] | 5.01% [20] | Telecommunications, healthcare, defense, consumer electronics [20] |
| Alternative Global Photonics View | $988.71 billion (2025) [21] | $1,733.49 billion [21] | 2025-2035 [21] | 5.8% [21] | High-speed data transmission, laser tech advancements, AI integration [21] |
| Silicon Photonics Market | $2.86 billion (2025) [22] | $28.75 billion [22] | 2025-2034 [22] | 29.25% [22] | Data center demand, CMOS compatibility, faster data transfer [22] |
Table 2: Global Medical Device Market Projections (2024-2030)
| Metric | 2024/2025 Value | Projected Value | Time Period | CAGR | Key Drivers |
|---|---|---|---|---|---|
| Global Medical Device Market | $542.21 billion (2024) [23] | $886.80 billion [23] | 2024-2032 [23] | Not specified | Aging population, chronic disease rise, technological innovation [23] [24] |
| Alternative Medical Device View | $681.57 billion (2025) [24] | $955.49 billion [24] | 2025-2030 [24] | 6.99% [24] | Aging population, chronic diseases, AI & robotics integration [24] |
| Connected Medical Devices | $75.99 billion (2025) [24] | $152.71 billion [24] | 2025-2030 [24] | 14.98% [24] | IoT integration, remote patient monitoring, telemedicine [23] [24] |
| Wearable Medical Devices | Not specified | $66.9 billion [24] | Through 2030 [24] | 10.1% [24] | Real-time monitoring, chronic disease management [23] [24] |
Regional analysis reveals that Asia Pacific dominates the global photonics market with a 63.2% share as of 2023, valued at $581.75 billion [19]. This dominance is attributed to strong R&D investments, domestic production capabilities, and extensive export supply chains, particularly in China [19]. Meanwhile, North America leads in medical devices, contributing over 40% to global revenues, driven by high healthcare expenditure, advanced infrastructure, and a robust innovation ecosystem [23] [24].
The silicon photonics segment deserves special attention as it represents the fastest-growing subsector with a remarkable 29.25% CAGR [22]. This technology, which integrates optical components with silicon-based electronics, is particularly relevant for biomedical applications including biosensing, DNA sequencing, and advanced imaging systems [22]. The compatibility with mainstream CMOS manufacturing makes it attractive for scaling and volume production of miniaturized medical devices [22].
Key Technologies and Experimental Methodologies
Optical Coherence Tomography (OCT) in Biomedical Imaging
Optical Coherence Tomography has revolutionized diagnostic imaging, particularly in ophthalmology and oncology. OCT functions as the "optical equivalent of ultrasound," using light waves instead of sound waves to capture micrometer-resolution, cross-sectional images of biological tissues [19]. The methodology below details the standard protocol for OCT imaging in clinical research.
Experimental Protocol: OCT for Retinal Imaging
Sample Preparation:
- Dilate patient's pupils using tropicamide (0.5%) or phenylephrine (2.5%)
- Position patient comfortably with chin stabilized in chinrest and forehead against headband
- Ensure proper alignment to maintain consistent distance from imaging lens
System Calibration:
- Verify reference mirror position in Michelson interferometer setup
- Calibrate wavelength of super-luminescent diode source (typically 800-1300nm)
- Adjust detector sensitivity and scan depth according to tissue type
Image Acquisition:
- Initiate scanning protocol with appropriate resolution settings (axial: 3-7μm, transverse: 10-20μm)
- Acquire multiple B-scans (cross-sectional images) at regions of interest
- Apply tracking algorithms to compensate for patient motion artifacts
Signal Processing:
- Perform Fourier transform on interferometric data to reconstruct depth-resolved profiles
- Apply dispersion compensation algorithms to improve image resolution
- Utilize noise reduction techniques to enhance signal-to-noise ratio
Image Analysis:
- Segment retinal layers using automated algorithms or manual annotation
- Quantify layer thicknesses and identify pathological alterations
- Generate thickness maps for comparative analysis across patient populations
The integration of OCT scanning in ophthalmology has been particularly transformative, enabling detection of glaucoma, retinopathy, and other retinal conditions that were previously challenging to diagnose [19]. Recent advancements in OCT technology have also expanded applications to intravascular imaging, dermatological assessment, and cancer margin detection during surgical procedures.
Diagram 1: OCT imaging workflow for biomedical research
Photonic Biosensors for Diagnostic Applications
Photonic biosensors represent a rapidly advancing field where photonic principles are applied to detect biological molecules with high sensitivity and specificity. These devices are particularly valuable for point-of-care testing, therapeutic drug monitoring, and biomarker discovery in drug development.
Experimental Protocol: Silicon Photonic Biosensor for Protein Detection
Chip Functionalization:
- Clean silicon photonic chip with oxygen plasma treatment
- Immerse in 2% (v/v) 3-aminopropyltriethoxysilane (APTES) in ethanol for 1 hour
- Rinse with ethanol and cure at 110°C for 10 minutes
- Activate surface with 2.5% glutaraldehyde in PBS for 2 hours
Probe Immobilization:
- Incubate with specific antibody solution (100μg/mL in PBS) overnight at 4°C
- Block nonspecific binding sites with 1% BSA for 1 hour
- Rinse with PBS-Tween 20 (0.05%) to remove unbound antibodies
Sample Preparation:
- Dilute patient samples in appropriate buffer (serum, plasma, or buffer)
- Centrifuge at 10,000g for 10 minutes to remove particulate matter
- Adjust pH to 7.4 if necessary for optimal binding conditions
Detection Protocol:
- Flow sample over functionalized sensor surface at controlled rate (10-100μL/min)
- Monitor wavelength shift in resonance peak due to binding events
- Record binding kinetics in real-time for 15-30 minutes
- Regenerate surface with glycine-HCl (pH 2.5) between measurements
Data Analysis:
- Calculate concentration from calibration curve of known standards
- Determine binding affinity (KD) from kinetic analysis of association/dissociation
- Perform statistical analysis across replicate measurements
The emergence of silicon photonic biosensors is particularly significant, leveraging the mature CMOS manufacturing infrastructure to create highly sensitive, multiplexed detection platforms [22]. These devices are finding applications in monitoring therapeutic drug levels, detecting cancer biomarkers, and diagnosing infectious diseases with minimal sample volumes.
Career Pathways and Research Directions
Interdisciplinary Career Opportunities
The convergence of photonics and biomedical devices has created diverse career pathways for researchers and engineers. Understanding these roles is essential for professionals seeking to position themselves in this expanding market.
Table 3: Key Research Reagent Solutions in Biomedical Photonics
| Reagent/Category | Function | Example Applications |
|---|---|---|
| Functionalized Silicon Chips | Platform for biosensor development | Protein detection, DNA hybridization studies [22] |
| Near-Infrared Fluorophores | Contrast agents for deep tissue imaging | Optical coherence tomography, fluorescence-guided surgery [19] |
| Biocompatible Optical Polymers | Waveguides for implantable devices | Continuous monitoring sensors, optogenetic interfaces [20] |
| Quantum Dot Probes | Photostable biomarkers for multiplexed detection | Cellular imaging, in vitro diagnostics [21] |
| Photoactivatable Reagents | Spatiotemporal control of biological processes | Targeted drug delivery, photodynamic therapy [19] |
Biomedical engineers specializing in photonics enjoy strong employment prospects, with the U.S. Bureau of Labor Statistics projecting 5% job growth until 2032 [25]. These professionals command competitive salaries, with a median annual pay of $106,950 for bioengineers and biomedical engineers [25]. The field supports over 1.32 million people worldwide in photonics components production alone, with manufacturing of photonics-enabled products generating more than five million jobs globally [26].
Diagram 2: Career pathways in biomedical engineering and optics
Emerging Research Frontiers
Several cutting-edge research domains are poised to shape the future of biomedical photonics, offering significant opportunities for scientific advancement and career specialization:
Integrated Photonic Point-of-Care Diagnostics: The miniaturization of complex laboratory functions onto photonic chips represents a paradigm shift in diagnostic testing. Researchers are developing silicon photonic biosensors that can detect multiple biomarkers simultaneously from minute sample volumes [22]. These devices leverage the evanescent field of light guided in nanoscale waveguides to probe molecular interactions at the sensor surface. For drug development professionals, these platforms offer new approaches to therapeutic monitoring and companion diagnostics.
AI-Enhanced Photonic Imaging: The integration of artificial intelligence with photonic imaging systems is revolutionizing image interpretation and diagnostic accuracy. Machine learning algorithms are being developed to automatically analyze OCT scans, detecting subtle pathological features that may escape human observation [21] [19]. Research in this area requires interdisciplinary collaboration between optical engineers, computer scientists, and clinical specialists to develop robust algorithms validated on diverse patient populations.
Neuromodulation and Optogenetics: Photonic technologies are enabling precise manipulation of neural activity using light-sensitive ion channels and pumps. Optogenetic interfaces combine microfabricated light sources with genetic targeting of specific neuronal populations, creating powerful tools for investigating neural circuits and developing novel therapeutic approaches for neurological disorders. This research frontier requires expertise in optics, genetics, neuroscience, and medical device design.
Therapeutic Laser Applications: Advancements in laser technology are expanding therapeutic applications beyond traditional surgical uses. Selective photothermolysis techniques are being refined to target specific structures (e.g., blood vessels, pigmented lesions) while minimizing damage to surrounding tissue. Meanwhile, photodynamic therapy continues to evolve with improved photosensitizers and light delivery systems for cancer treatment. Research in this domain focuses on optimizing light-tissue interactions for maximal therapeutic efficacy.
The synergistic expansion of photonics and biomedical devices represents one of the most dynamic frontiers in healthcare technology. Market projections consistently demonstrate robust growth across both sectors, with particular acceleration in specialized segments including silicon photonics, connected medical devices, and wearable health monitors. For researchers, scientists, and drug development professionals, this convergence creates unprecedented opportunities to develop innovative solutions to pressing healthcare challenges.
The continued integration of photonic technologies into biomedical applications—from advanced imaging systems to point-of-care diagnostics—is fundamentally transforming patient care and biomedical research methodologies. Success in this interdisciplinary field requires researchers to develop expertise spanning photonics engineering, biological sciences, and clinical applications. Those who can navigate this complex landscape will be well-positioned to contribute to the next generation of biomedical innovations that leverage the unique capabilities of light-based technologies to improve human health.
Key Industry Players and Research Institutions Driving Innovation
The fields of biomedical engineering and optics are increasingly intertwined, driving a wave of innovation that is transforming modern healthcare. This synergy is accelerating advancements in diagnostics, therapeutics, and regenerative medicine. Research institutions are pioneering fundamental discoveries, while industry players translate these breakthroughs into technologies and treatments. This guide examines the key contributors and the practical methodologies underpinning this progress, providing a landscape for professionals navigating careers and collaborations in this dynamic sector. The convergence of advanced optical tools with biological inquiry is creating new paradigms for understanding disease and improving human health [27] [28].
Key Research Institutions
Academic and research institutions are the bedrock of innovation, providing foundational knowledge, training specialized talent, and often pioneering the disruptive technologies that industry later adopts.
Leading Universities in Optics and Optical Sciences
The following institutions are globally recognized for their premier optics and optical sciences programs, which are critical for developing the advanced imaging and sensing technologies used in biomedical applications [29] [30] [31].
Table 1: Top-Tier Global Universities for Optics Research
| Institution | Location | Key Strengths & Notes |
|---|---|---|
| Zhejiang University | Hangzhou, China | Leads in global optics research performance [29]. |
| Stanford University | Stanford, California, USA | A top-tier U.S. institution located in Silicon Valley, fostering strong industry ties [29]. |
| University of Arizona | Tucson, Arizona, USA | A leading U.S. program awarding a high volume of degrees; a major hub for optics research [30] [31]. |
| University of Rochester | Rochester, New York, USA | Renowned for its Institute of Optics and strong research output [30] [31]. |
| California Institute of Technology (Caltech) | Pasadena, California, USA | Site of pioneering microrobotics research for targeted drug delivery [27] [29]. |
Table 2: Prominent U.S. Universities in Optical Sciences and Biomedical Engineering
| Institution | Location | Notable Characteristics |
|---|---|---|
| Duke University | Durham, North Carolina, USA | Highly-ranked program focusing on the intersection of engineering and medicine [30] [31]. |
| Ohio State University - Main Campus | Columbus, Ohio, USA | A large, comprehensive research university with strong optics and engineering programs [30] [31]. |
| Rochester Institute of Technology (RIT) | Rochester, New York, USA | Offers a practice-oriented program in a region known for optical innovation [30] [31]. |
| University of North Carolina at Charlotte | Charlotte, North Carolina, USA | Shows rapid growth in optics/optical sciences degrees awarded [30]. |
| Columbia University | New York City, New York, USA | BME department hosts pioneering tissue engineering and "organ-on-a-chip" research [32]. |
Institutions at the Forefront of Biomedical Engineering
Beyond optics-specific programs, several broader institutions are leaders in biomedical engineering, often integrating advanced optics into their research.
Columbia University's Department of Biomedical Engineering is a prime example of a hub for translational research. Its Laboratory for Stem Cells and Tissue Engineering, led by Professor Gordana Vunjak-Novakovic, is renowned for groundbreaking work in tissue engineering, bioreactors, and "organ-on-a-chip" technology [32]. The lab's research operates at the intersection of biomaterials, cellular biology, and engineering, requiring close collaboration between biologists and engineers. The environment fosters career growth from research assistant to director of operations, demonstrating a pathway for professional development within a cutting-edge research setting [32].
Case Western Reserve University also offers advanced training and research in biomedical engineering, with a curriculum emphasizing the latest innovations in the field [28].
Key Industry Trends and Innovations
Industry players, from large corporations to agile startups, are leveraging foundational research to develop marketable technologies that address pressing clinical needs. Several key trends highlight the current innovation landscape.
Table 3: Key Innovation Trends in Biomedical Engineering and Optics
| Trend Area | Description | Impact on Healthcare |
|---|---|---|
| Personalized Medicine | AI and genomic sequencing enable therapies tailored to an individual's genetic makeup, lifestyle, and environment [27]. | Improved patient outcomes, fewer side effects, and more targeted therapies [27]. |
| Microrobotics | Microscopic robots capable of delivering drugs directly to targeted areas, such as tumors, with high accuracy [27]. | Reduced systemic drug exposure, minimized side effects, and enhanced efficacy for chronic conditions [27]. |
| AI and Machine Learning | Accelerating drug discovery by analyzing complex datasets from genomics, proteomics, and medical imaging [27] [28]. | Reduced time-to-market for new therapies; earlier and more accurate diagnostics [27]. |
| Advanced Biomaterials & Regenerative Medicine | Using biocompatible materials and 3D bioprinting to create patient-specific implants and tissues [27]. | Addressing donor organ shortages and reducing rejection risks through personalized tissue engineering [27]. |
| Digital Health and Wearables | Devices providing continuous health monitoring and predictive analytics for conditions like diabetes and cardiovascular disease [27] [28]. | Empowers patients with greater autonomy and provides researchers with longitudinal data [27]. |
Experimental Protocols and Methodologies
Translating an idea into a validated technology requires rigorous experimental protocols. Below is a detailed methodology for a representative advanced experiment in the field.
Detailed Protocol: Development of a Microrobotic Drug Delivery System
This protocol outlines the key steps for developing and testing microrobots for targeted drug delivery, based on research from institutions like Caltech [27].
Objective: To design, fabricate, and validate the efficacy of biodegradable microrobots for the targeted delivery of a chemotherapeutic agent to a tumor site in vivo.
1. Microrobot Fabrication and Drug Loading
- Materials: Biodegradable polymer (e.g., PLGA), magnetic nanoparticles, chemotherapeutic drug (e.g., Doxorubicin), photolithography setup, micro-emulsion equipment.
- Method: Use a two-step process. First, create a micro-porous scaffold using bioprinting or photolithography. Second, load the scaffold with magnetic nanoparticles for guidance and the chemotherapeutic drug via a micro-emulsion and diffusion process. The surface can be functionalized with targeting ligands (e.g., antibodies) for specific cell binding.
2. In Vitro Validation
- Setup: A micro-fluidic channel mimicking vascular flow is used.
- Guidance Test: Apply an external magnetic field to navigate the microrobots towards a target cell culture (e.g., HeLa cancer cells) within the channel.
- Efficacy Assay: After successful targeting and drug release, use a cell viability assay (e.g., MTT assay) to quantify cancer cell death compared to controls (free drug, non-targeted particles).
3. In Vivo Testing and Imaging
- Animal Model: Use a mouse model with a subcutaneously implanted tumor.
- Administration: Introduce microrobots intravenously.
- Guidance & Imaging: Use MRI to guide the microrobots to the tumor site via a magnetic field. Bio-luminescent or fluorescent imaging tracks the microrobots' location in vivo.
- Efficacy Assessment: Monitor tumor volume over time versus control groups. Post-trial, harvest tumors and major organs for histological analysis (e.g., H&E staining) to confirm targeted drug action and assess off-target effects.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful experimentation relies on a suite of reliable reagents and materials. The following table details essential items for research in tissue engineering and regenerative medicine, a key area of biomedical innovation [32] [28].
Table 4: Key Research Reagent Solutions for Tissue Engineering
| Reagent/Material | Function | Specific Example |
|---|---|---|
| Stem Cells | Foundational cells with the potential to differentiate into various specialized cell types for building tissues. | Human Mesenchymal Stem Cells (hMSCs) for bone and cartilage regeneration [28]. |
| Synthetic Biomaterials | Provide the 3D structural scaffold (matrix) that supports cell growth, organization, and tissue development. | Polylactic acid (PLA) or Polyethylene glycol (PEG) hydrogels for bioprinting [27]. |
| Native Biomaterials | Decellularized extracellular matrix (ECM) from tissues, providing a natural, bioactive scaffold. | Decellularized porcine heart ECM used in developing native biomaterials for repair [32]. |
| Growth Factors | Signaling proteins that direct cell behavior, such as proliferation, migration, and differentiation. | Bone Morphogenetic Protein (BMP-2) to induce bone formation [28]. |
| Bioreactor Systems | Devices that provide a controlled in vitro environment (e.g., mechanical stimulation, nutrient flow) for tissue growth. | A "organ-on-a-chip" bioreactor that mimics the mechanical and physiological environment of a human organ [32]. |
Visualizing Research Workflows
Effective visualization of complex workflows and relationships is crucial for designing experiments, analyzing data, and communicating findings.
Workflow for Tissue Engineering Experiment
The following diagram illustrates the logical workflow for a standard tissue engineering experiment, from scaffold preparation to analysis [32] [28].
Drug Discovery Signaling Pathway
This diagram visualizes a simplified generic signaling pathway involved in drug discovery for diseases like cancer, showing where therapeutic interventions may target [27] [28].
Biomedical engineering represents a dynamic and rapidly evolving discipline that operates at the intersection of engineering, biology, and medicine. This field focuses on applying engineering principles and problem-solving methodologies to advance healthcare treatment, diagnostic capabilities, and therapeutic interventions [33]. Similarly, optics research has become increasingly integral to biomedical advancement, particularly in the development of sophisticated medical imaging systems, diagnostic equipment, and light-based therapies [34] [35]. The convergence of these domains has created new frontiers in medical science, from advanced microscopy techniques for cellular imaging to optical coherence tomography for non-invasive diagnostics.
The educational pathway for professionals in these interdisciplinary fields requires a robust foundation in both physical and life sciences, coupled with specialized engineering expertise. This guide examines the essential degrees and foundational knowledge required for success at this critical interface, with particular emphasis on the quantitative and technical competencies needed by researchers, scientists, and drug development professionals working in biomedical engineering and optics research.
Essential Degree Pathways
Undergraduate Foundations
The journey toward a career in biomedical engineering typically begins with a bachelor's degree, which provides the fundamental scientific and engineering principles necessary for advanced study or entry-level positions. At leading institutions such as Harvard University, students can pursue several undergraduate pathways, including a Bachelor of Arts (A.B.) in Biomedical Engineering, a Bachelor of Arts in Engineering Sciences with a Biomedical Sciences and Engineering track, or a Bachelor of Science (S.B.) in Engineering Sciences with a Bioengineering track, the latter being an ABET-accredited program [36]. These programs are structured to provide students with a solid foundation in engineering and its application to the life sciences within the context of a liberal arts education [36].
The undergraduate curriculum typically emphasizes:
- Core Engineering Principles: Comprehensive coursework in mathematics, physics, and fundamental engineering concepts [37].
- Biological Sciences: Anatomy, physiology, cellular biology, and genetics to understand the human body and disease processes [37].
- Specialized Biomedical Courses: Biomechanics, biomaterials, bioinstrumentation, and medical imaging [37].
- Hands-on Laboratory Experience: Practical application of theoretical knowledge through laboratory work and design projects [36] [33].
For those interested in the optical aspects of biomedical engineering, relevant coursework includes introduction to optics, fundamental parameters of optical systems, optical specifications, and software design of optical systems [34]. These courses establish the foundational knowledge necessary for understanding how light interacts with biological systems and how optical technologies can be leveraged for medical applications.
Table 1: Undergraduate Course Requirements for Biomedical Engineering Specializations
| Specialization Area | Core Mathematics | Physical Sciences | Engineering Fundamentals | Biological Sciences |
|---|---|---|---|---|
| General BME | Calculus I-III, Differential Equations, Statistics | Physics I-II, Chemistry, Organic Chemistry | Circuit Analysis, Signals & Systems, Biomechanics | Biology, Physiology, Cell Biology |
| Biomechanics Track | Calculus I-III, Differential Equations, Linear Algebra | Physics I-II, Chemistry | Statics, Dynamics, Materials Science, Fluid Mechanics | Anatomy, Musculoskeletal Biology, Physiology |
| Biomaterials Track | Calculus I-III, Differential Equations | Chemistry, Organic Chemistry, Physics | Materials Science, Thermodynamics, Transport Phenomena | Biology, Biochemistry, Cell Biology |
| Bioimaging/Optics Track | Calculus I-III, Differential Equations, Linear Algebra | Physics I-III (Optics), Chemistry | Fourier Analysis, Signal Processing, Introduction to Optics | Biology, Anatomy, Physiology |
Graduate Specialization Opportunities
Graduate education enables deeper specialization in specific subdisciplines of biomedical engineering and optics. Master's and doctoral programs provide advanced training in research methodologies, specialized technical skills, and theoretical frameworks necessary for innovation and leadership in the field [37] [38]. At the graduate level, students can focus on areas such as medical device design, tissue engineering, biomechanics, biomedical imaging, biomaterials, clinical engineering, bioinformatics, or neural engineering [5] [4].
Case Western Reserve University's Master of Science in Biomedical Engineering program exemplifies this approach, offering specialized elective courses in material science, medical imaging, and neural engineering, allowing students to align their education with specific career objectives [38]. Graduate programs also emphasize the development of soft skills, including communication, innovation, creativity, problem-solving, and leadership, which are essential for success in interdisciplinary research environments [38].
Research forms a cornerstone of graduate education in biomedical engineering. At institutions like Harvard, students have access to extensive research opportunities at affiliated institutions such as Harvard Medical School, Boston Children's Hospital, the Wyss Institute, the Broad Institute, and the Rowland Institute [36]. These experiences provide hands-on training with cutting-edge technologies and methodologies, preparing students for research-intensive careers in academia or industry.
Table 2: Graduate Specializations and Career Opportunities in Biomedical Engineering
| Specialization | Advanced Coursework | Research Areas | Potential Career Paths | Industry Demand |
|---|---|---|---|---|
| Medical Device Design | Medical Instrumentation, Product Development, Regulatory Science | Surgical Robotics, Wearable Sensors, Point-of-Care Diagnostics | R&D Engineer, Product Design Engineer, Quality Assurance Engineer | High (12% projected growth) [5] |
| Tissue Engineering & Regenerative Medicine | Biomaterials, Cell Biology, Mechanobiology | Artificial Organs, 3D Bioprinting, Stem Cell Therapies | Research Scientist, Bioprocess Engineer, Clinical Trials Manager | High [5] [4] |
| Biomedical Imaging & Optics | Fourier Optics, Photonics, Image Processing | Molecular Imaging, Image-Guided Therapy, Novel Contrast Agents | Imaging Systems Engineer, Clinical Imaging Specialist, Medical Physicist | High [5] [4] |
| Neural Engineering | Neurobiology, Signal Processing, Neural Interfaces | Brain-Computer Interfaces, Neuroprosthetics, Deep Brain Stimulation | Neuroprosthetics Engineer, BCI Developer, Neuroengineering Researcher | Emerging [5] [4] |
| Bioinformatics & Health Data Analytics | Computational Biology, Machine Learning, Statistical Genetics | Genomic Analysis, Predictive Modeling, Precision Medicine | Bioinformatics Analyst, Computational Biologist, Healthcare Data Scientist | High [5] [4] |
Foundational Knowledge Requirements
Core Scientific and Technical Competencies
Success in biomedical engineering and optics research requires mastery of several interconnected knowledge domains. These foundational areas provide the conceptual framework and technical skills necessary for innovation and problem-solving in complex biomedical challenges.
Mathematics and Quantitative Analysis: Biomedical engineering is inherently quantitative, relying on mathematical analysis and modeling to understand systems ranging from subcellular processes to organism-level physiology [36] [39]. Essential mathematical competencies include:
- Calculus: For modeling dynamic systems and solving complex equations [39].
- Differential Equations: To understand and describe dynamic processes such as blood flow, drug absorption, and physiological system dynamics [39].
- Linear Algebra: Particularly valuable in imaging and biomechanics applications [39].
- Statistics: Essential for designing experiments, interpreting biological data, and validating models [39].
Physical Sciences: A strong foundation in physical sciences provides the principles governing material properties, energy transfer, and system dynamics relevant to biomedical applications:
- Physics: Mechanics, thermodynamics, and electromagnetism inform the design of medical devices, prosthetics, and diagnostic equipment [39].
- Chemistry: Understanding molecular interactions is crucial for developing biomaterials, drug delivery systems, and diagnostic assays [39].
- Optics: Knowledge of light properties, geometric optics, wave optics, and optical system design is fundamental for medical imaging, spectroscopy, and phototherapeutic applications [34] [35].
Biological Sciences: Comprehension of living systems is essential for developing effective biomedical technologies:
- Biology and Physiology: Understanding cellular processes, tissue organization, and organ system functions enables engineers to create solutions compatible with biological constraints [39] [37].
- Pathophysiology: Knowledge of disease processes informs the development of targeted diagnostic and therapeutic technologies.
Engineering Fundamentals: Core engineering principles provide the problem-solving framework for addressing biomedical challenges:
- Engineering Design: Systematic approach to creating solutions that meet clinical needs while considering technical, economic, and regulatory constraints [37].
- Systems Thinking: Ability to analyze complex biological systems as integrated networks of components with emergent properties [36].
Technical Proficiencies and Practical Skills
Beyond theoretical knowledge, biomedical engineers and optics researchers require diverse technical skills for experimental work, data analysis, and technology development:
Laboratory and Experimental Techniques:
- Optical System Alignment: Proficiency in setting up and aligning lenses, mirrors, light sources, and detectors [34].
- Sample Preparation: Methods for preparing biological specimens for optical imaging and analysis.
- System Calibration: Procedures for ensuring measurement accuracy and reproducibility in optical and electronic instruments [34].
Computational and Analytical Skills:
- Programming: Proficiency in languages such as Python, MATLAB, R, or C++ for data analysis, simulation, and instrument control [39].
- Computational Modeling: Ability to create mathematical models of biological systems, optical phenomena, or device performance [36].
- Data Analysis: Skills in processing and interpreting complex datasets from biological experiments or clinical studies [37].
- Image Processing: Techniques for enhancing, analyzing, and quantifying information from medical images [4].
Technical Design and Fabrication:
- Computer-Aided Design (CAD): Proficiency using software to design medical devices, instruments, or components [39].
- Prototyping: Ability to create physical prototypes using 3D printing, machining, or other fabrication methods.
Diagram 1: Foundational Knowledge Domains for Biomedical Engineering
Experimental Protocols and Research Methodologies
Core Experimental Approaches
Research in biomedical engineering and optics employs diverse methodological approaches to address fundamental questions and develop novel technologies. The following protocols represent essential experimental frameworks in this interdisciplinary field.
Protocol 1: Development and Validation of Biomedical Optics Systems
This protocol outlines a systematic approach for developing and validating optical systems for biomedical applications, such as diagnostic imaging or therapeutic monitoring.
Needs Assessment and Specification Definition:
- Identify unmet clinical needs through consultation with healthcare providers
- Define technical specifications based on clinical requirements
- Establish performance metrics and validation criteria
System Design and Modeling:
- Select appropriate optical components based on target tissue properties
- Develop mathematical models of light-tissue interactions
- Create computational simulations of system performance
- Use optical design software (e.g., Zemax OpticStudio) to model system layout [34]
Prototype Fabrication and Assembly:
- Source optical components (lenses, filters, detectors, light sources)
- Assemble mechanical housing and positioning systems
- Integrate electronic control systems and data acquisition hardware
- Implement safety features for human or animal use
System Characterization and Calibration:
- Measure fundamental parameters (resolution, field of view, sensitivity)
- Characterize system performance using standardized phantoms
- Establish calibration procedures and reference standards
- Quantify signal-to-noise ratio and dynamic range
Biological Validation:
- Conduct pilot studies with relevant biological samples
- Compare performance against established reference methods
- Assess reproducibility and reliability across operators and sessions
- Establish analytical performance characteristics (sensitivity, specificity)
Preclinical Evaluation:
- Perform animal studies where appropriate and ethically approved
- Evaluate system performance in realistic use scenarios
- Assess safety and potential adverse effects
- Collect data for regulatory submissions
Protocol 2: Biomaterial Development and Characterization for Optical Applications
This protocol describes methods for developing and characterizing biomaterials with specific optical properties for applications such as tissue engineering, drug delivery, or implantable sensors.
Material Design and Synthesis:
- Select base materials with appropriate biocompatibility and optical properties
- Modify material composition to achieve target refractive index, transparency, or fluorescence
- Incorporate bioactive molecules for specific biological interactions
- Process materials into desired forms (scaffolds, particles, coatings)
Physical Characterization:
- Measure optical properties (absorption, scattering, fluorescence)
- Quantify mechanical properties relevant to intended application
- Assess degradation kinetics in physiological environments
- Evaluate material stability under sterilization and storage conditions
In Vitro Biological Evaluation:
- Assess cytocompatibility using standardized cell culture assays
- Evaluate cellular response to material (adhesion, proliferation, differentiation)
- Test material performance in biologically relevant environments
- Investigate material-cell interactions using microscopic techniques
Functional Performance Assessment:
- Evaluate material performance in intended application
- Assess integration with surrounding tissues in model systems
- Measure drug release kinetics for delivery systems
- Validate sensor performance in physiological relevant conditions
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Biomedical Optics Research
| Category | Specific Items | Function/Application | Key Considerations |
|---|---|---|---|
| Optical Components | Lenses, Mirrors, Filters, Beam Splitters, Optical Fibers | Manipulate light path, wavelength, and intensity | Coating specifications, damage threshold, transmission efficiency |
| Light Sources | LEDs, Lasers (various wavelengths), Broadband Sources | Provide illumination for imaging, stimulation, or therapy | Coherence, power stability, spectral characteristics, safety classification |
| Detectors | CCD/CMOS Cameras, Photomultiplier Tubes, Spectrometers, Photodiodes | Capture light signals for quantitative analysis | Sensitivity, noise characteristics, temporal resolution, spectral response |
| Biomaterials | Hydrogels, Biodegradable Polymers, Ceramics, Natural Materials | Scaffolds for tissue engineering, drug delivery vehicles | Biocompatibility, degradation rate, mechanical properties, optical properties |
| Cell Culture Reagents | Cell Lines, Culture Media, Growth Factors, Staining Dyes | Biological models for in vitro testing | Species relevance, disease modeling, experimental reproducibility |
| Contrast Agents | Fluorescent Dyes, Quantum Dots, Nanoparticles, Targeted Probes | Enhance visualization of specific structures or processes | Brightness, stability, targeting specificity, biocompatibility |
| Image Analysis Software | MATLAB, ImageJ, Custom Algorithms, Machine Learning Tools | Quantitative extraction of information from optical data | Processing speed, algorithm accuracy, user interface, customization options |
Diagram 2: Biomedical Optics System Development Workflow
The educational pathways for biomedical engineering and optics research are characterized by strong foundational training in quantitative sciences, followed by progressive specialization in interdisciplinary applications. As these fields continue to evolve, driven by technological advances and unmet clinical needs, the demand for professionals with robust technical training and innovative problem-solving capabilities will continue to grow. The integration of optical technologies into biomedical applications represents a particularly promising frontier, with potential impacts ranging from fundamental biological discovery to point-of-care diagnostics and personalized therapeutics.
Successful navigation of these educational pathways requires not only academic excellence but also practical experience, interdisciplinary collaboration, and continuous adaptation to emerging technologies. For researchers, scientists, and drug development professionals, this foundation enables meaningful contributions to advancing healthcare technologies and improving patient outcomes through innovation at the interface of engineering, optics, and medicine.
From Theory to Therapy: Practical Applications and Career Implementation
Medical imaging is a cornerstone of modern healthcare, enabling non-invasive visualization of internal body structures for diagnosis, treatment planning, and therapeutic monitoring. For biomedical engineers and optics researchers, these technologies represent a dynamic frontier where innovation in hardware, software, and biological targeting converges to advance clinical capabilities. This technical guide provides an in-depth examination of four pivotal imaging modalities—Magnetic Resonance Imaging (MRI), Computed Tomography (CT), Ultrasound, and Optical Coherence Tomography (OCT)—framed within the context of biomedical engineering careers and optics research. We explore their fundamental principles, comparative performance parameters, experimental methodologies, and emerging innovations that are shaping the future of medical imaging.
Fundamental Principles and Applications
Magnetic Resonance Imaging (MRI) utilizes powerful magnetic fields and radio waves to excite hydrogen nuclei in body tissues, detecting the resulting signals to construct detailed images of soft tissues. Unlike CT, MRI does not use ionizing radiation, making it particularly valuable for pediatric imaging and longitudinal studies where radiation accumulation is a concern. MRI excels in neurological, musculoskeletal, and oncological imaging due to its superior soft tissue contrast and functional imaging capabilities.
Computed Tomography (CT) employs rotating X-ray generators and detector arrays to acquire multiple projection images from different angles, which are computationally reconstructed into cross-sectional anatomical images. Modern multi-slice CT systems can acquire hundreds of simultaneous slices with sub-millimeter resolution, enabling rapid whole-body scanning for trauma, cancer staging, and vascular imaging.
Ultrasound imaging utilizes high-frequency sound waves (typically 2-18 MHz) transmitted into the body via piezoelectric transducers. Reflections from tissue interfaces are detected and processed to generate real-time images of soft tissues and blood flow. Its portability, real-time capability, and absence of ionizing radiation make it ideal for obstetric, cardiac, and point-of-care applications.
Optical Coherence Tomography (OCT) is an interferometric technique that uses near-infrared light to generate cross-sectional tissue images with micron-scale resolution. First introduced in the early 1990s [40], OCT performs low-coherence interferometry to measure backscattered light, analogous to ultrasound but with significantly higher resolution. Its limited penetration depth (1-3 mm) initially confined applications to transparent tissues like the eye [40], though technological advances have expanded its use to cardiology, dermatology, and oncology.
Performance Characteristics and Clinical Applications
Table 1: Technical Specifications and Clinical Applications of Major Medical Imaging Modalities
| Parameter | MRI | CT | Ultrasound | OCT |
|---|---|---|---|---|
| Resolution (Axial) | 0.5-1.5 mm | 0.25-0.625 mm | 0.1-1.0 mm | 5-20 µm [41] |
| Penetration Depth | Unlimited | Unlimited | 2-20 cm (frequency dependent) | 1-3 mm [40] |
| Contrast Mechanism | T1/T2 relaxation, proton density | Electron density | Acoustic impedance | Optical scattering/reflection |
| Key Clinical Applications | Neuroimaging, musculoskeletal, oncology | Trauma, pulmonary, abdominal imaging, angiography | Obstetrics, cardiology, abdominal, point-of-care | Ophthalmology [41], dermatology, cardiology |
| Safety Considerations | Non-ionizing (contraindications: metallic implants) | Ionizing radiation | Non-ionizing (thermal/mechanical effects minimal at diagnostic levels) | Non-ionizing |
| Biomedical Engineering Focus | Pulse sequence design, coil development, reconstruction algorithms | Detector technology, iterative reconstruction, dose reduction | Transducer design, beamforming, elastography | Laser sources, interferometer design, functional extensions |
Optical Coherence Tomography: Technical Framework
Historical Development and Technical Evolution
OCT emerged in the early 1990s as a groundbreaking imaging technique within the health automation trend [40]. The first commercial ophthalmic OCT device entered the market in 1996, just five years after its inception, though initial adoption was limited with only approximately 180 units sold until 1999 [41]. Early time-domain OCT (TD-OCT) technology required acquisition of a depth scan for every location, resulting in slow imaging speeds and poor image quality that limited clinical adoption.
The introduction of spectral-domain OCT (SD-OCT) significantly improved image quality and imaging speed by capturing entire depth information simultaneously [41]. In 2006, the SPECTRALIS platform combined SD-OCT technology with a scanning laser ophthalmoscope (SLO), enabling precise motion tracking and follow-up assessment by re-scanning the exact same location at later time points [41]. This technological advancement created new clinical applications and established OCT as a standard tool for imaging macular diseases, diabetic retinopathy, and glaucoma.
OCT Methodologies and Implementation
Time-Domain OCT (TD-OCT) represents the first implementation of OCT technology [41]. In TD-OCT, the reference arm length is modulated for each depth scan, and the intensity record of the combined light at the sensor provides the reflectance profile of the sample. A broadband light source (typically a superluminescent diode) is split into sample and reference beams, with the reference beam traveling to a mirror on a translational stage. Back-reflected light from both arms combines and interferes only when optical path lengths match within the coherence length of the source. For each sample point, the reference mirror scans in the depth (z) direction while light intensity is recorded on a photo detector, generating a complete depth profile (A-scan) of sample reflectivity [41].
Fourier-Domain OCT (FD-OCT) provides a more efficient implementation without mechanical scanning of the optical path length. Two methods have been established to acquire spectral information of the interferometric signal:
Spectral-Domain OCT (SD-OCT): First proposed by Fercher et al. in 1995 [41], this approach replaces the point detector with a spectrometer. The spectrometer uses a diffractive element to spatially separate different wavelength contributions into a line image recorded by a high-speed line scan camera. Each read-out constitutes a spectral interferogram, with A-scans computed via Fourier transformation [41].
Swept-Source OCT (SS-OCT): First demonstrated in 1997 [41], this method replaces the broadband light source with an optical source that rapidly sweeps a narrow line-width over a broad range of wavelengths. During each sweep, wavelength components of the interferometric signal are detected sequentially by a high-speed photo-detector. Commercially available sources can achieve sweep rates exceeding 100 kHz, requiring ultrafast detection and analog-digital conversion in the GHz range [41].
Experimental Protocols and Research Applications
Comparative Diagnostic Performance: HCC Case Study
A prospective diagnostic accuracy cohort study conducted at SMS Medical College and Hospital, Jaipur, compared CT and MRI in detecting and staging hepatocellular carcinoma (HCC) [42]. The study enrolled 120 patients with clinical suspicion or risk factors for HCC (cirrhosis, hepatitis B/C infection, elevated AFP) who underwent both contrast-enhanced CT and gadoxetic acid-enhanced MRI within a two-week interval [42].
Imaging Protocols:
- CT Protocol: Triphasic contrast-enhanced CT scans using a 64-slice multidetector scanner (GE Revolution EVO) with non-contrast, arterial (25-30s delay), portal venous (60-70s delay), and delayed phases (3-5 minutes). Iohexol contrast was administered at 1.5 mL/kg, injected at 3.5 mL/s [42].
- MRI Protocol: Imaging performed on a 1.5T system (Siemens Magnetom Aera) with liver-specific protocol including T1W in-phase/out-of-phase, T2W, diffusion-weighted imaging (DWI). Gadoxetic acid (0.025 mmol/kg) was used as contrast agent with arterial, portal, transitional, and hepatobiliary phases (20 minutes post-injection) [42].
Analysis Methodology: Two board-certified radiologists, blinded to the other modality and clinical details, independently reviewed CT and MRI scans. Imaging findings were categorized using LI-RADS v2018. The final diagnosis was based on histopathological analysis where available, or clinical-radiological diagnosis using AASLD guidelines with follow-up imaging at 3-6 months [42].
Results: The study demonstrated MRI's superior sensitivity (91.2%) and specificity (87.2%) compared to CT (79.6% and 83.0%, respectively) for early-stage HCC detection [42]. Interobserver agreement was higher for MRI (κ = 0.78) than CT (κ = 0.68), and MRI detected more sub-2 cm lesions. Combined CT+MRI use enhanced diagnostic completeness, though seven lesions (4.4%) were missed by both modalities [42].
OCT in Ophthalmology: Retinal Imaging Protocol
Sample Preparation: For clinical retinal imaging, pupil dilation is typically achieved using tropicamide 1% and phenylephrine 2.5%. The patient is positioned with chin on chinrest and forehead against headrest to minimize motion artifacts. Proper alignment is confirmed using the fundus view from the scanning laser ophthalmoscope [41].
Image Acquisition:
- Macular Scans: Radial sequence tomograms (6-12 radial scans centered on fovea) or volume scans (20°×20° area, 25-61 B-scans) are acquired.
- Optic Disc Scans: Circular peripapillary tomograms (3.4mm diameter circle) for nerve fiber layer thickness measurement, crucial for glaucoma diagnosis [41].
- Follow-up Scans: The follow-up function enables precise re-scanning of the exact same location using the SLO for motion tracking and reference to the baseline examination [41].
Image Analysis: Automated segmentation algorithms delineate retinal layers, enabling thickness measurement. The retinal nerve fiber layer (RNFL) thickness is measured for glaucoma diagnosis, where thinning marks disease onset and progression [41]. Comparison with normative databases enables detection of pathological deviations.
Table 2: Research Reagent Solutions for OCT and Associated Imaging Applications
| Research Reagent | Function/Application | Example Use Cases |
|---|---|---|
| Gadoxetic Acid | MRI contrast agent for hepatobiliary imaging | HCC characterization and detection [42] |
| Iohexol | Non-ionic, low-osmolar CT contrast medium | Multiphasic CT imaging for HCC [42] |
| Tropicamide 1% | Pupillary dilation for retinal imaging | Routine clinical OCT examination [41] |
| Phenylephrine 2.5% | Mydriatic agent for pupil dilation | Facilitates wider field OCT scans [41] |
| Hollow Mesoporous Nanoparticles | Drug delivery enhancement for phototherapy | Tumor detection and targeted therapy [40] |
| Indocyanine Green (ICG) | NIR fluorescent dye for enhanced imaging | Photodynamic therapy with deeper tissue penetration [40] |
Emerging Technologies and Future Directions
Artificial Intelligence Integration in Medical Imaging
Artificial intelligence is revolutionizing medical imaging across all modalities, with particularly significant implications for ophthalmology and OCT. AI algorithms can enhance image quality, automate segmentation and diagnosis, and predict disease progression [43] [3]. In OCT imaging, deep learning algorithms are being developed to segment the suprachoroidal space, potentially accelerating adoption of suprachoroidal therapies [43]. AI's impact extends beyond image analysis to address critical needs in ophthalmology where expert resources are limited, with several FDA-cleared AI systems already in use for detecting diabetic retinopathy from retinal photos [43].
AI-driven approaches are also transforming drug discovery processes relevant to imaging. AlphaFold, an advanced convolutional neural network that predicts 3D protein structures from amino acid sequences, represents a significant breakthrough for target identification in ophthalmology [3]. The ability to accurately predict structure and identify binding sites accelerates drug discovery, reducing the time and cost of bringing new therapies to market. Computer-aided drug design (CADD) leverages these AI-predicted structures for molecular docking and dynamics simulations, optimizing drug candidates for ocular diseases [3].
Functional Extensions and Novel Applications
Functional OCT techniques are expanding the capabilities of traditional structural imaging. Analysis of the OCT signal enables detection of blood flow and tissue properties like birefringence and elasticity [41]. Doppler OCT visualizes blood flow, while polarization-sensitive OCT (PS-OCT) measures tissue birefringence in structures like the retinal nerve fiber layer. OCT elastography maps tissue mechanical properties, potentially identifying pathological changes before structural alterations become apparent [41].
Advanced Drug Delivery Monitoring: OCT is playing an increasingly important role in evaluating novel therapeutic approaches. Research presented at ARVO 2025 highlighted suprachoroidal delivery of long-acting drugs, with Clearside Biomedical reporting Phase 2b trial data of suprachoroidal CLS-AX (axitinib) in neovascular AMD [43]. The suprachoroidal route achieved encouraging durability and safety, suggesting prolonged drug effects in macular diseases. Deep learning algorithms to segment the suprachoroidal space on OCT images represent an example of AI enhancing imaging for drug delivery optimization [43].
Career Pathways in Biomedical Engineering and Optics Research
The evolving landscape of medical imaging technology creates diverse career opportunities for biomedical engineers and optics researchers. The U.S. Bureau of Labor Statistics projects 5-7% job growth for biomedical engineers through 2032-2033, reflecting strong demand for healthcare technology innovation [25] [44]. Professionals with expertise in medical imaging can pursue several rewarding career paths:
Medical Device Development: Biomedical engineers design and improve imaging systems such as MRI machines, CT scanners, and OCT instruments. This work involves pulse sequence design (MRI), detector technology development (CT), transducer design (ultrasound), and interferometer optimization (OCT) [25] [44]. The median annual pay for bioengineers and biomedical engineers is $106,950, with entry-level positions averaging $94,807 [25].
Clinical Engineering: In healthcare settings, biomedical engineers manage and maintain medical imaging equipment to ensure patient safety and optimal performance. They collaborate with medical staff to introduce new technologies and troubleshoot issues, with an average salary of $93,700 [44].
Regulatory Affairs: Specialists in this domain oversee medical imaging product compliance with government regulations and industry standards. They prepare documentation for regulatory submissions and liaise with agencies like the FDA, commanding an average salary of $95,411 [44].
Research and Development: R&D engineers lead innovation in medical imaging technologies, working in academic research labs, biotech companies, or government institutions. Their work includes designing experiments, analyzing data, and developing new healthcare technologies, with an average salary of $96,571 [44].
Advanced education and specialized certifications enhance career prospects in this field. A Master's degree in Biomedical Engineering enables specialization in areas like neuroengineering or biomedical imaging, while professional certifications such as Medical Device Auditor (CMDA), Certified Quality Engineer (CQE), or Regulatory Affairs Certification (RAC) provide competitive advantages in niche areas [44].
Medical imaging technologies continue to evolve at a rapid pace, driven by innovations in engineering, optics, and artificial intelligence. For biomedical engineers and optics researchers, this dynamic landscape offers diverse opportunities to contribute to advancing healthcare through improved diagnostic capabilities, therapeutic monitoring, and personalized medicine approaches. The integration of AI across imaging modalities, development of functional extensions to existing technologies, and emergence of novel applications in drug development and delivery monitoring represent particularly promising frontiers. As these technologies continue to converge and advance, biomedical professionals with interdisciplinary expertise in engineering, optics, and biological systems will play an increasingly vital role in shaping the future of medical imaging and patient care.
The fields of biomaterials and tissue engineering represent a paradigm shift in regenerative medicine, moving from passive, static implants to dynamic, bioresponsive systems that actively promote healing and integration. Biomaterials are substances engineered to interact with biological systems for a medical purpose, either to replace or support damaged tissues and organs. The contemporary definition, as recognized by the European Society of Biomaterials, encompasses any substance—other than drugs or drug mixtures—used to treat, enhance, or restore body functions [45]. The progression in this domain is increasingly driven by a synergy between advanced material science and precision-focused fields like biomedical optics, which provides critical tools for imaging, monitoring, and fabrication. This convergence is creating a new generation of smart, compatible implants and complex artificial organs, ultimately aiming to restore function with high precision and minimal intervention.
The core characteristics of modern biomaterials include biocompatibility (the ability to perform with an appropriate host response), surface functionality, non-toxicity, and controlled biodegradability [45]. The transition from inert structural supports to interactive, temporary scaffolds marks a significant advancement. Unlike permanent implants, which may necessitate secondary removal surgeries and carry long-term risks like stress shielding or inflammation, biodegradable materials such as polylactic acid (PLA), polyglycolic acid (PGA), and magnesium alloys provide temporary mechanical support while facilitating natural tissue regeneration [45]. The global biomaterials market, estimated at USD 208.23 billion in 2025 and projected to reach USD 577.93 billion by 2032, reflects the immense growth and investment in this sector, particularly in orthopedic applications and 3D printing technology [46].
Advanced Biomaterials for Implants and Organ Engineering
The selection and engineering of biomaterials are foundational to their success in clinical applications. Materials are chosen based on their mechanical properties, degradation profiles, and bioactivity, tailored to their specific physiological destination.
Material Classes and Properties
- Metallic Biomaterials: Dominating the market with a 40.1% share in 2025, metallic biomaterials like titanium and cobalt-chromium alloys are prized for their superior strength, fatigue resistance, and corrosion resistance, making them ideal for load-bearing orthopedic implants such as hip and knee replacements [46]. Magnesium-based alloys are a rising star in this category, offering the unique advantage of biodegradability and mechanical properties similar to natural bone. They promote osteogenesis (bone formation) but present challenges due to rapid degradation that can lead to hydrogen gas formation and localized tissue irritation [45].
- Polymeric Biomaterials: Synthetic polymers like PLA, PGA, their copolymer PLGA, and polycaprolactone (PCL) are widely used for their tunable degradation rates and processability. They are particularly useful for creating porous scaffolds for tissue ingrowth. A key limitation is their mechanical weakness in load-bearing scenarios, and their degradation can sometimes produce acidic byproducts that provoke inflammation [45]. Natural polymers, such as hyaluronic acid and collagen, offer excellent biocompatibility and are often used in hydrogels for soft tissue engineering [47].
- Ceramic and Composite Biomaterials: Bioceramics like hydroxyapatite (HA) and bioactive glass are osteoconductive, meaning they support bone cell attachment and growth. Their brittleness often limits their use, so they are frequently combined with polymers to create composites. For instance, PLA/HA composites combine the osteoconductivity of HA with the toughness and biodegradability of the polymer, resulting in a scaffold that supports bone growth with controlled degradation [45] [48]. Advanced composites increasingly incorporate nanoscale reinforcements like carbon nanotubes or graphene to enhance mechanical performance, electrical conductivity, and bioactivity [48].
Table 1: Key Biomaterial Classes and Their Characteristics
| Material Class | Examples | Key Advantages | Primary Limitations | Common Applications |
|---|---|---|---|---|
| Metallic | Titanium alloys, Magnesium alloys | High strength, fatigue resistance, biocompatibility | Stress shielding (Ti), Rapid degradation & gas formation (Mg) | Load-bearing bone implants, stents |
| Polymeric | PLA, PCL, PLGA, Hyaluronic Acid | Tunable degradation, easy processing, biocompatible | Low mechanical strength, acidic degradation byproducts | Soft tissue scaffolds, drug delivery systems |
| Ceramic | Hydroxyapatite (HA), Bioactive Glass | Osteoconductive, bioactive, mimics bone mineral | Brittleness, low fracture toughness | Bone graft substitutes, coatings on implants |
| Composite | PLA/HA, PCL/Bioactive Glass | Tailored mechanical properties, enhanced bioactivity | Complex fabrication, potential for inconsistent properties | Gradient scaffolds, load-bearing bone repair |
The Rise of "Smart" and Stimuli-Responsive Biomaterials
Next-generation biomaterials are designed to be dynamic and responsive. Smart biomaterials can interact with the biological environment and respond to specific stimuli such as pH, temperature, enzymatic activity, or mechanical load [49]. This includes:
- Mechanoresponsive Scaffolds: These constructs can modulate their properties in response to external mechanical forces, promoting tissue regeneration that is aligned with physiological demands [48].
- Shape-Memory Materials: Embedded within scaffolds, these materials can undergo conformational changes in situ, improving implant fixation and providing mechanotransductive cues to surrounding cells [48].
- Self-Healing Materials: Innovations like self-healing concrete, which uses bacteria that produce limestone upon exposure to oxygen and water, are emerging in biomedicine, suggesting future applications for implants that can autonomously repair micro-damage [50].
Core Technical Processes and Experimental Methodologies
The development of advanced tissue constructs relies on a suite of sophisticated fabrication and validation techniques. The following workflow outlines the standard pipeline from design to preclinical testing.
Advanced Fabrication Techniques
- Additive Manufacturing (3D Printing): Leading the biomaterials market with a 31.4% share in 2025, 3D printing enables the creation of patient-specific implants with complex geometries and controlled internal porosity [46]. Techniques like extrusion-based printing allow for the fabrication of gradient scaffolds that replicate the transitional architecture of natural tissue interfaces (e.g., where bone meets tendon). This is achieved by continuously varying the deposition of materials like hydroxyapatite-polymer composites, which tailors the mineral density and mechanical properties to reduce stress concentrations and guide spatially specific tissue regeneration [48].
- Electrospinning: This method produces nanoscale to microscale polymer fibers that mimic the native extracellular matrix (ECM). These non-woven meshes have high surface-area-to-volume ratios, promoting cell adhesion and proliferation, and are widely used in soft tissue engineering [47].
- Microfluidics and Biofabrication: Microfluidic devices enable the precise spatial placement of cells and biomaterials to create highly organized tissue constructs. They are also instrumental in forming controlled gradients of biochemical signals or creating uniform, cell-laden hydrogel microspheres for tissue building blocks [48].
In Vitro and In Vivo Evaluation Protocols
Rigorous testing is essential to translate laboratory innovations into clinical applications.
In Vitro Characterization:
- Mechanical Testing: Uniaxial tensile/compression tests are performed to determine elastic modulus, ultimate tensile strength, and strain-to-failure, ensuring the construct can withstand physiological loads.
- Degradation Profiling: Scaffolds are incubated in phosphate-buffered saline (PBS) or simulated body fluid at 37°C. Mass loss, pH change of the medium, and release of degradation products are monitored over time.
- Cell Culture Studies: Human stem cells or primary cells are seeded onto scaffolds. Key metrics include cell viability (e.g., via Live/Dead assay), proliferation (DNA quantification), and differentiation (e.g., osteogenic differentiation assessed by alkaline phosphatase activity and mineral deposition staining) [45] [48].
In Vivo Preclinical Validation in Large Animal Models: Large animals like sheep, pigs, and goats are critical bridges between lab research and human trials due to their anatomical and physiological similarities to humans [45].
- Model Creation: A critical-sized bone defect (one that will not heal spontaneously) is created in a load-bearing site, such as a sheep femur or pig mandible.
- Implant Placement: The fabricated scaffold, often seeded with the animal's own stem cells, is implanted into the defect. A control group typically receives a standard-of-care material or is left empty.
- Longitudinal Monitoring: Post-operative healing is tracked using non-invasive imaging like micro-CT (to quantify new bone formation and scaffold degradation) and MRI.
- Endpoint Analysis: After a pre-defined period (e.g., 12-24 weeks), animals are euthanized, and the implant site is harvested for histological analysis. This involves sectioning and staining the tissue (e.g., with H&E for general morphology, Masson's Trichrome for collagen, and special stains for bone) to assess tissue integration, vascularization, and inflammatory response [45].
Table 2: Standard In Vivo Preclinical Models for Orthopedic Implants
| Animal Model | Anatomical/Physiological Similarity to Humans | Common Implant Type Evaluated | Key Measured Outcomes |
|---|---|---|---|
| Sheep | Long bone geometry and weight-bearing healing | Magnesium alloy screws, PLGA scaffolds | Bone regeneration rate, implant degradation kinetics, mechanical integrity [45] |
| Pig | Skin healing, cardiovascular system, bone metabolism | Magnesium-based implants, vascular stents | Biocompatibility, osteoconductivity, vascular integration [45] [27] |
| Goat | Joint size and cartilage repair | PLA/HA composite bone scaffolds | Cartilage and subchondral bone repair, osseointegration [45] [51] |
| Rabbit | Cost-effective for preliminary studies | Dental implants, cranial defect models | Early-stage biocompatibility, initial bone ingrowth [45] [48] |
The Integral Role of Biomedical Optics and Imaging
Biomedical optics provides the critical "eyes" for tissue engineering, offering tools for diagnosis, fabrication, and monitoring. This synergy is a core component of modern biomedical engineering research and career paths.
- High-Resolution Bioimaging: Techniques like confocal microscopy and multiphoton microscopy allow for non-invasive, deep-tissue imaging of cell-scaffold interactions within 3D constructs. This is vital for assessing cell migration, distribution, and viability in real-time during in vitro culture [47].
- Intraoperative Imaging and Surgical Guidance: Optical technologies are being developed to provide surgeons with real-time, high-resolution visual feedback. For example, the Butte Lab at Cedars-Sinai is developing novel intra-operative imaging and visualization technologies to aid surgeons in achieving near-complete tumor excision, a technology directly applicable to ensuring the precise placement of engineered tissues [52].
- Optical Sensing in Smart Implants: A frontier in biomaterials is the integration of micro-optical sensors within scaffolds. These sensors can detect local mechanical strain, pH changes, or the presence of specific biomarkers, providing real-time data on implant performance, tissue regeneration, and early signs of infection or failure [48]. This creates a closed-loop system where the implant itself becomes a diagnostic tool.
- Fabrication with Light: Two-photon polymerization, a high-precision 3D printing technique, uses focused laser light to solidify a photopolymer resin, enabling the fabrication of scaffolds with sub-micron features that can directly influence cell behavior [50].
The Scientist's Toolkit: Key Reagents and Materials
Successful experimentation in this field relies on a suite of essential reagents and materials.
Table 3: Essential Research Reagents and Materials for Biomaterials Research
| Reagent/Material | Function | Example Application |
|---|---|---|
| Poly(lactic-co-glycolic acid) (PLGA) | A biodegradable polymer used as a scaffold material; degradation rate is tunable by adjusting the LA:GA ratio. | 3D-printed bone scaffolds, drug delivery microspheres [45] [48]. |
| Hydroxyapatite (HA) | A calcium phosphate ceramic that is the main mineral component of bone; provides osteoconductivity. | blended with polymers to create composite scaffolds for enhanced bone regeneration [45] [48]. |
| Bone Morphogenetic Protein-2 (BMP-2) | A growth factor that strongly induces osteoblast differentiation and bone formation. | Incorporated into scaffolds to actively stimulate bone growth in critical-sized defects [45] [48]. |
| Mesenchymal Stem Cells (MSCs) | Multipotent stromal cells that can differentiate into osteoblasts, chondrocytes, and adipocytes. | Seeded onto scaffolds to populate them with the patient's own cells for enhanced regeneration [47]. |
| AlamarBlue / MTT Assay | Colorimetric or fluorometric assays used to quantify cell viability and proliferation. | Used in in vitro studies to monitor the health and growth of cells on a new biomaterial over time. |
| Primary Antibodies (e.g., anti-Osteocalcin) | Immunoglobulin proteins that bind specifically to a target protein (antigen). | Used in immunohistochemistry to detect and visualize the presence of bone-specific proteins, confirming osteogenic differentiation. |
Signaling Pathways in Tissue Integration and Regeneration
The biological integration of implants is governed by complex cellular signaling pathways. The following diagram summarizes the key pathways involved in the osseointegration of a bone implant.
Pathway Explanation: The successful integration of a bone implant (Osseointegration) is a multi-factorial process. The biomaterial surface can release bioactive molecules like Bone Morphogenetic Proteins (BMPs), which activate intracellular SMAD proteins, a key pathway driving osteogenic differentiation [48]. Concurrently, when cells adhere to the implant surface via integrin receptors, it triggers the Focal Adhesion Kinase (FAK)/Rho/ROCK pathway, which regulates cytoskeletal organization and cell survival. Furthermore, the physical micro-/nano-topography of the implant and the mechanical loads it experiences are sensed by the cell, leading to the activation of the YAP/TAZ pathway, a major mechanotransduction route [48]. These converging signals ultimately lead to the activation of the master transcription factor Runx2, which turns on osteogenic genes (like Osteocalcin), resulting in the formation of new bone tissue that firmly anchors the implant.
The field of biomaterials and tissue engineering is rapidly evolving from a discipline focused on passive replacement to one that creates active, intelligent biological interfaces. The convergence of materials science with biomedical optics, biology, and computational design is paving the way for a new era of regenerative medicine. Key future directions include:
- Enhanced Smart Implants: The development of implants with integrated biosensors and closed-loop therapeutic delivery systems will enable real-time monitoring of healing and proactive intervention [48].
- Advanced Biomanufacturing: 3D printing technologies will continue to advance, allowing for the fabrication of vascularized, multi-cellular tissues and entire organoids with high precision and reproducibility [27] [47].
- AI-Driven Design: Artificial intelligence and machine learning are poised to accelerate the discovery of new biomaterials and optimize implant designs by predicting complex structure-function relationships and analyzing high-throughput experimental data [49].
- Immunoengineering: A growing understanding of the immune response to biomaterials is leading to strategies that modulate the immune system to promote tolerance and enhance regeneration, rather than merely avoiding a negative reaction [47].
For researchers and scientists, particularly those with expertise in biomedical optics, the opportunities are vast. Careers are emerging in the design of optical imaging systems for surgical guidance, the development of optical biosensors for smart implants, and the use of high-resolution optical techniques for quality control in biofabrication. By continuing to bridge these disciplines, the ultimate goal of creating readily available, fully functional artificial organs and perfectly compatible implants moves from science fiction to an achievable reality.
Surgical and rehabilitation engineering represents one of the most dynamic frontiers in biomedical engineering, where advanced technologies transform patient care across the clinical spectrum. This field leverages principles from optics, materials science, robotics, and computing to develop innovative solutions that bridge surgical intervention and long-term functional rehabilitation. The integration of laser systems with advanced prosthetics and assistive devices creates a continuous care pathway—from precise tissue manipulation during surgery to the restoration of mobility and independence through bionic limbs and smart rehabilitation tools. Within this technological landscape, biomedical engineers and optics researchers play increasingly critical roles in driving innovations that are poised to redefine standards of care in the coming decade. The global surgical laser market itself, projected to grow from $8.31 billion in 2024 to $27.90 billion by 2035, underscores the significant economic and clinical impact of these technologies [53].
This whitepaper provides a technical examination of three interconnected domains: laser-based surgical systems, next-generation prosthetic limbs, and integrated assistive technologies. For researchers and drug development professionals, understanding these engineering paradigms is essential, as they increasingly interface with pharmaceutical and biologic approaches to patient recovery and regeneration. The following sections detail underlying operational principles, present experimental methodologies for technology validation, analyze quantitative performance data, and outline the essential toolkit for research and development in this rapidly advancing field.
Laser Systems in Modern Surgery: Precision and Applications
Operational Fundamentals and System Types
Surgical laser systems operate on the principle of selective photothermolysis, where specific light wavelengths are absorbed by target chromophores (e.g., water, hemoglobin, melanin) to produce localized thermal effects for precise cutting, ablation, or coagulation of tissue. The key parameters governing their effect include wavelength, power density, pulse duration, and spot size. Different laser types are optimized for specific surgical applications based on their wavelength and tissue interaction properties [54].
Table 1: Major Surgical Laser Types and Their Clinical Applications
| Laser Type | Wavelength Range | Primary Tissue Interaction | Key Clinical Applications |
|---|---|---|---|
| CO₂ Gas Laser | 10,600 nm | Strong water absorption | Skin resurfacing, vocal cord surgery, gynecological procedures, lesion ablation [53] [54] |
| Er:YAG Solid-State Laser | 2940 nm | Very strong water absorption | Superficial skin ablation, dental caries removal, bone surgery [53] |
| Nd:YAG Solid-State Laser | 1064 nm | Moderate scatter and penetration | Deep tissue coagulation, oncology tumor ablation, urological procedures, vascular treatments [53] [54] |
| Diode Laser | 800-980 nm | Hemoglobin absorption | Soft tissue surgery, hair removal, ophthalmology, dental procedures, minimally invasive surgeries [53] |
| Excimer Gas Laser | 193-351 nm | Photoablation (breaks molecular bonds) | Refractive eye surgery (LASIK), angioplasty [53] [54] |
Recent Technical Innovations and Experimental Validation
A critical innovation in surgical laser technology involves the development of flexible laser delivery systems that maintain performance under mechanical bending, enabling their use in minimally invasive and robotic-assisted surgeries. Recent research has provided a validated experimental framework for quantifying this performance.
Experimental Protocol: Evaluating Bent Fiber Optic Laser Delivery Systems
- Objective: To determine the effect of bending on the power transmission efficiency of mid-infrared fluoride glass fibers used in surgical applications [55].
- Materials:
- Methodology:
- Baseline Measurement: The output power of each fiber is measured in a straight configuration to establish a 100% transmission baseline [55].
- Bending Application: Each fiber is bent around mandrels with specific diameters, creating bends with known radii. Bends are applied within and then exceeding the manufacturers' recommended minimum bend radii [55].
- Power Measurement: The output power is measured for each bend configuration.
- Data Analysis: Power transmission is calculated as a percentage of the baseline measurement. The relationship between bend radius and transmission loss is quantified for each fiber type [55].
- Modeling Validation: Results from physical experiments are correlated with advanced computer models simulating light propagation through bent fibers [55].
- Key Finding: The study concluded that bending fibers within the manufacturer-recommended limits did not cause a significant reduction in their ability to carry light. Sharp bends only caused substantial power loss in one fiber type, and only when bent beyond the recommended limit [55]. This finding is pivotal for designing flexible surgical instruments for laparoscopic, endoscopic, and catheter-based procedures.
Next-Generation Prosthetics: Integration and Intelligence
Neural Control and Sensory Feedback Systems
The paradigm for prosthetic limbs is shifting from passive cosmetic replacements to dynamically controlled systems that restore near-natural motor control and sensation. This is achieved through advanced neural interfaces that establish bidirectional communication between the prosthesis and the user's nervous system [56] [57].
Motor Control Pathways:
- Targeted Muscle Reinnervation (TMR): A surgical procedure that reassigns nerves severed by amputation to remaining muscle groups. These reinnervated muscles then act as biological amplifiers of motor commands, producing distinct, detectable electromyogram (EMG) patterns for controlling multiple degrees of freedom in a prosthetic arm [57].
- Implantable Myoelectric Sensors (IMES): Small sensors implanted within residual muscles detect EMG signals with higher fidelity and stability than surface electrodes. This technology enables more intuitive and precise control of prosthetic joints and hands [57].
- Direct Brain-Computer Interfaces (BCIs): For high-level limb deficiencies, intracortical implants in the motor cortex decode neural signals associated with movement intention. These signals are processed by algorithms to control complex prosthetic arms, allowing users to perform tasks with a level of dexterity approaching that of a biological limb [57].
Sensory Feedback Pathways:
- Bidirectional Systems: Closing the loop is critical for functional embodiment. Sensors embedded in the prosthetic hand (e.g., force, pressure, slip, temperature) generate data that is converted into neural stimuli.
- Sensory Stimulation Techniques: This stimulation is delivered via electrodes implanted in either the peripheral nerves (e.g., vagus nerve) or directly into the sensory cortex of the brain. This artificial signaling recreates sensations of touch, pressure, and even proprioception, allowing users to perceive the grip force applied or the texture of an object without visual confirmation [57] [58].
Enabling Materials and Manufacturing Technologies
The functionality and user adoption of advanced prosthetics are heavily dependent on parallel advancements in materials science and manufacturing.
- Advanced Materials: The use of lightweight, high-strength composites and alloys (e.g., titanium, carbon fiber) reduces user fatigue and increases durability. Furthermore, the development of flexible electronic skins (e-skin) embedded with networks of micro-sensors enables the prosthetic limb to mimic the sensing capabilities of human skin, detecting pressure, temperature, and vibration [57].
- Additive Manufacturing (3D Printing): 3D printing has revolutionized prosthetic development by enabling the rapid, cost-effective production of highly customized sockets and structural components. It allows for perfect anatomical matching, internal lattice structures for weight reduction, and personalized aesthetic designs (e.g., the Hero Arm by Open Bionics), which are particularly impactful for pediatric patients who require frequent size adjustments [59].
Table 2: Quantitative Market Analysis of Prosthetic and Assistive Technologies
| Technology Segment | Key Metric | Value / Forecast | Notes and Drivers |
|---|---|---|---|
| Surgical Lasers (Global Market) | Market Size (2024) | USD 8.31 Billion [53] | Foundation for precise surgical interventions. |
| Surgical Lasers (Global Market) | Market Forecast (2035) | USD 27.90 Billion [53] | Driven by demand for minimally invasive surgeries [53]. |
| Surgical Lasers (Global Market) | CAGR (2025-2035) | 11.64% [53] | Indicates robust sector growth and R&D investment [53]. |
| Surgical Lasers - Product Segment | Highest Revenue (2024) | Solid-State Laser Systems [53] | Valued for precision in cutting and coagulation [53]. |
| Surgical Lasers - Product Segment | Fastest Growth (CAGR) | Diode Laser Systems [53] | Compact design and expanding applications [53]. |
| Surgical Lasers - Regional Growth | Fastest CAGR (APAC) | Highest Regional CAGR [53] | Expanding healthcare infrastructure and medical tourism [53]. |
The Integrated Assistive Device Ecosystem
Modern rehabilitation engineering extends beyond prosthetics to include a suite of interconnected assistive technologies designed to promote independence.
- AI-Powered Sensory Substitution Devices: For the visually impaired, devices like AI smart glasses (e.g., VisionX) use real-time computer vision to describe scenes, read text, and identify faces, effectively translating visual information into auditory cues [58].
- Advanced Mobility Solutions: Smart wheelchairs incorporate LiDAR, computer vision, and autonomous navigation technologies to avoid obstacles, follow predefined paths, and traverse complex environments, significantly reducing the cognitive load on the user [58].
- Wearable Robotic Exoskeletons: These devices (e.g., ReWalk X2) provide powered assistance at the joints to help individuals with spinal cord injuries or mobility impairments to stand, walk, and climb stairs. Recent trends focus on making these systems lighter, more affordable, and suitable for daily home use [58].
- Adaptive Human-Computer Interfaces: Highly customizable input devices, such as the X-Adapt Pro gaming controller, which supports eye-tracking, sip-and-puff, and voice control, are making digital interaction and entertainment accessible to users with a wide range of physical abilities [58].
The Research and Development Toolkit
For scientists and engineers developing these technologies, a specific set of reagents, materials, and experimental setups is fundamental.
Table 3: Essential Research Reagents and Materials for Surgical and Rehabilitation Engineering
| Item | Function / Application | Specific Examples / Notes |
|---|---|---|
| Fluoride Glass Optical Fibers | Transmission medium for mid-infrared surgical lasers. | Enables flexible delivery of Er:YAG and other laser wavelengths; performance under bending is a key test parameter [55]. |
| Biocompatible Encapsulation Materials | Protection for implanted electronics from the biological environment. | Materials like medical-grade silicone, Parylene-C, and polydimethylsiloxane (PDMS) provide insulation and biostability for chronic implants [60]. |
| Conductive Bio-inks / Nanomaterials | Fabrication of flexible electrodes and sensors for e-skin and neural interfaces. | Silver nanowires, graphene, and conductive polymers enable stretchable, robust electrical circuits on soft, curvilinear surfaces [60]. |
| EMG Gel / Electrolyte | Ensuring high-quality signal acquisition from surface electrodes for myoelectric control systems. | Reduces skin impedance for accurate recording of muscle electrical activity, crucial for prosthesis control algorithm development [57]. |
| Cell Culture Assays (e.g., Fibroblasts) | In vitro biocompatibility testing of new implant materials. | Used to assess cytotoxicity, cell adhesion, and inflammatory response to new materials prior to in vivo studies [60]. |
| 3D Printing Filaments (Medical Grade) | Rapid prototyping of custom prosthetic sockets, covers, and device housings. | Materials like biocompatible nylon and resins allow for patient-specific design and iterative testing of form and fit [59]. |
Career Pathways and Research Directions in Biomedical Engineering
The technological landscape outlined herein defines a rapidly expanding frontier for biomedical engineers and optics researchers. Career opportunities span academia, industry (medical device companies, laser manufacturers), and clinical settings. Key research domains offering significant career traction include:
- Advanced Laser-Tissue Interaction: Investigating new wavelengths and pulse durations for specialized surgical applications and developing compact, portable laser systems [61].
- Closed-Loop Neural Engineering: Refining the algorithms and hardware for seamless, low-latency bidirectional brain-computer interfaces to achieve truly embodied prosthetics [56] [57].
- Soft Robotics and Flexible Bioelectronics: Developing prosthetics and assistive devices that are inherently soft, compliant, and mechanically matched to human tissue to improve safety and comfort [60].
- AI and Machine Learning Integration: Implementing adaptive learning systems in prosthetics that predict user intent and automate routine adjustments, and using AI for real-time interpretation in sensory substitution devices [57] [58].
- Sustainable and Global Health Engineering: Leveraging technologies like 3D printing to create affordable, repairable, and accessible assistive devices for underserved populations worldwide [59].
The convergence of laser precision, robotic actuation, neural intelligence, and personalized design marks a transformative era in surgical and rehabilitation engineering. For researchers and professionals, this interdisciplinary field not only offers rich scientific challenges but also the profound reward of creating technologies that restore human capability and independence.
The field of ophthalmology is undergoing a transformative shift, driven by innovations in biomedical engineering that are redefining traditional approaches to drug discovery and delivery. These advancements address long-standing challenges in treating chronic eye diseases, such as the invasive nature of frequent intravitreal injections for retinal conditions and the limited bioavailability of topical treatments. Drug delivery systems have evolved from simple eye drops to sophisticated, sustained-release technologies that maintain therapeutic drug levels over extended periods. Concurrently, development tools powered by artificial intelligence (AI) and computational modeling are dramatically accelerating the drug discovery pipeline, reducing development timelines from decades to months in some cases. This whitepaper explores the technical foundations of these innovations, providing researchers and drug development professionals with a comprehensive overview of current methodologies and their applications within biomedical engineering and optics research. The integration of these disciplines is creating unprecedented career opportunities for professionals skilled at the intersection of engineering, data science, and biological systems [3] [6].
AI-Powered Drug Development Tools
Computational Target Identification and Validation
The initial stage of drug discovery—identifying and validating biological targets—has been revolutionized by artificial intelligence. AI algorithms can now analyze vast multi-omics datasets, biomedical literature, and clinical data to identify novel drug targets with higher efficiency and precision than traditional methods. AlphaFold, an AI-driven algorithm developed by DeepMind, represents a landmark advancement in this domain by predicting the 3D structures of proteins from their amino acid sequences with remarkable accuracy. This capability is particularly valuable for understanding eye diseases associated with protein misfolding and dysregulation, such as AMD, cataracts, corneal dystrophies, and glaucoma. The ability to accurately predict protein structure and identify binding sites significantly accelerates the early drug discovery process, reducing both time and cost associated with bringing new therapies to market [3].
Platforms such as PandaOmics employ AI to integrate and analyze diverse data types, including gene expression profiles, proteomics data, and text-based knowledge graphs from scientific publications. This systems biology approach enables the identification and prioritization of novel, druggable targets for further investigation. For example, Chinese researchers have utilized AlphaFold to create 315 abnormal structural isoforms in uveal melanoma patients, revealing novel insights into potential treatment targets. The transition from convolutional neural networks to transformer-based architectures in AlphaFold2 has further enhanced prediction accuracy, extending capabilities beyond proteins to DNA, RNA, and their interactions with small molecules in AlphaFold3 [3].
Table 1: AI Platforms for Drug Target Identification
| Platform/Algorithm | Developer | Primary Function | Ophthalmology Application |
|---|---|---|---|
| AlphaFold Series | DeepMind | Protein structure prediction | Understanding disease mechanisms in AMD, glaucoma |
| PandaOmics | Insilico Medicine | Multi-omics target discovery | Identifying novel targets for retinal diseases |
| Large Language Models (LLMs) | Various | Literature mining & hypothesis generation | Accelerating research for rare ocular diseases |
Computer-Aided Drug Design (CADD)
Once promising targets are identified, computer-aided drug design (CADD) approaches leverage computational power to simulate drug interactions and optimize potential candidates. CADD encompasses two primary methodologies: structure-based drug design (SBDD) and ligand-based drug design (LBDD). SBDD utilizes the 3D structure of biological targets to identify drug candidates through molecular docking and molecular dynamics (MD) simulations. Molecular docking facilitates the examination of interactions between small molecules and their target proteins, with AI-powered approaches like Deep Docking dramatically accelerating the process by predicting binding affinity and orientation for millions of potential compounds. For example, in AMD research, Deep Docking can rapidly filter and prioritize molecules that effectively bind to vascular endothelial growth factor (VEGF), a key therapeutic target [3].
Molecular dynamics simulations provide a complementary approach by modeling protein-ligand interactions over time in simulated biological environments. In ocular drug discovery, MD simulations can model how a potential drug designed for retinal delivery behaves within the aqueous humor, providing atomistic insights into the drug's binding stability and efficacy. The success of these approaches is exemplified by developments such as INS018_055, a TNIK inhibitor for idiopathic pulmonary fibrosis that was developed in just 18 months using PandaOmics and advanced molecular docking. This AI-driven workflow combined pathway modeling, single-cell perturbation analysis, and de novo molecular docking, significantly expediting lead optimization [3].
Figure 1: AI-Driven Drug Discovery Workflow. This diagram illustrates the integrated computational approaches used in modern pharmaceutical development, from target identification to candidate optimization.
Experimental Protocol: AI-Assisted Molecular Docking for VEGF Inhibitors
Purpose: To identify and optimize small molecule inhibitors targeting VEGF for ocular neovascular diseases using computational docking approaches.
Methodology:
- Target Preparation: Obtain the 3D structure of VEGF from the Protein Data Bank (PDB ID: 1VPF) or generate it using AlphaFold3. Prepare the protein by adding hydrogen atoms, assigning partial charges, and defining flexible receptor regions around the known binding site.
- Compound Library Preparation: Curate a diverse chemical library from databases such as ZINC15 or ChEMBL. Generate 3D conformers for each compound, optimize geometry using molecular mechanics force fields, and assign appropriate atomic charges.
- Molecular Docking: Employ AI-enhanced docking software (e.g., Deep Docking, AutoDock Vina) to screen the compound library against the prepared VEGF structure. Utilize convolutional neural networks to prioritize compounds with favorable binding poses and predicted binding affinities <-8.0 kcal/mol.
- Binding Mode Analysis: Visually inspect top-ranking complexes to evaluate key interactions (hydrogen bonds, hydrophobic contacts, π-π stacking) between ligands and critical VEGF residues (e.g., Glu64, Lys65, Phe36).
- Molecular Dynamics Validation: Subject the top 10 ligand-receptor complexes to 100 ns MD simulations using AMBER or GROMACS to assess binding stability, root-mean-square deviation (RMSD), and interaction persistence under dynamic conditions.
- In Vitro Validation: Synthesize or purchase top computational hits for experimental validation using VEGF binding ELISAs and endothelial cell proliferation assays [3].
Advanced Ocular Drug Delivery Systems
Sustained-Release Implants and Injectables
The challenge of maintaining therapeutic drug levels in ocular tissues has driven innovation in sustained-release technologies. These systems aim to reduce treatment burden by extending dosing intervals from weeks to months or even years. Intravitreal implants represent a significant advancement in this category, with technologies such as EyePoint Pharmaceuticals' hydrogel-based Durasert platform showing promise in clinical trials. Their investigational OTX-TKI implant delivers a tyrosine kinase inhibitor for diabetic retinopathy through an injectable, bioerodible formulation designed to maintain therapeutic levels for months without monthly injections. Similarly, Ocular Therapeutics is developing a tyrosine kinase inhibitor implant (OTX-TKI) that has demonstrated sustained efficacy in early trials (HELIOS) for diabetic retinopathy [43].
Suprachoroidal delivery has emerged as a promising alternative to traditional intravitreal injections. This approach involves administering therapeutics into the potential space between the sclera and choroid, offering several advantages including targeted delivery to posterior segment tissues and reduced exposure to anterior structures. Clearside Biomedical has pioneered this approach with their SCS Microinjector technology, reporting positive Phase 2b trial data (ODYSSEY) for suprachoroidal CLS-AX (axitinib) in neovascular AMD. The company presented six abstracts at ARVO 2025 highlighting the durability and safety of this platform, suggesting this route can prolong drug effects in macular diseases. Research presented at the conference even described a novel deep learning algorithm to segment the suprachoroidal space on OCT images—an example of AI enhancing imaging for drug delivery optimization [43].
Table 2: Advanced Ocular Drug Delivery Platforms
| Delivery Platform | Technology Type | Key Features | Development Status |
|---|---|---|---|
| Suprachoroidal Injection (CLS-AX) | Clearside Biomedical | Targeted posterior delivery, reduced injection frequency | Phase 2b trials (ODYSSEY) |
| Hydrogel Implant (OTX-TKI) | Ocular Therapeutix | Sustained release over months, biodegradable | Phase 1/2 trials (HELIOS) |
| Subcutaneous Anti-VEGF (Migaldendranib) | Ashvattha Therapeutics | Systemic administration with ocular targeting | Phase 2 trials |
| Voyager DSLT | Alcon/Belkin Vision | Direct laser trabeculoplasty without gonioscopy | FDA Approved (2023) |
| Drug-Eluting Contact Lens | MediPrint Ophthalmics | Sustained drug release via printed lenses | Phase 3 development |
Novel Administration Routes and Formulations
Innovative administration routes and formulations are expanding possibilities for ocular therapeutics. Subcutaneous administration of anti-VEGF therapies represents a paradigm shift in retinal disease management. Ashvattha Therapeutics reported Phase 2 results for migaldendranib, an investigational subcutaneous treatment that significantly reduced subretinal fluid and decreased the need for intravitreal anti-VEGF injections in patients with wet AMD and diabetic macular edema (DME). This platform could substantially reduce clinic visits and improve patient comfort by delivering anti-VEGF therapy via a simple under-the-skin injection rather than direct ocular injection [43].
Drug-eluting contact lenses offer another promising approach for anterior segment conditions. MediPrint Ophthalmics is developing medicated contact lenses created through the combination of an FDA-cleared drug and an FDA-cleared contact lens leveraging their proprietary MediPrint process. This technology, currently in Phase 3 development for mild to moderate glaucoma and ocular hypertension, could provide sustained drug delivery while simultaneously correcting vision. The manufacturing process utilizes high-speed production techniques, potentially making this a scalable and cost-effective delivery system [62].
Figure 2: Ocular Drug Delivery Pathways. This diagram illustrates various administration routes for ocular therapeutics and their primary target tissues in the eye.
Experimental Protocol: Evaluating Suprachoroidal Drug Delivery in Preclinical Models
Purpose: To assess the distribution, retention, and efficacy of small molecule therapeutics administered via the suprachoroidal space in a rabbit model.
Methodology:
- Formulation Preparation: Prepare test articles containing axitinib (1.0 mg/50 μL) in optimized formulation buffer. Include a fluorescent dye (e.g., Cy5.5) for imaging studies. For controls, prepare same formulation for intravitreal injection.
- Animal Preparation: Anesthetize New Zealand White rabbits (2.5-3.0 kg) using intramuscular ketamine (35 mg/kg) and xylazine (5 mg/kg). Perform pupil dilation with topical phenylephrine (2.5%) and tropicamide (1%). Apply topical anesthetic (proparacaine 0.5%) to both eyes.
- Administration Technique: Position animal laterally. Insert a 34-gauge microneedle (Clearside SCS Microinjector) 3.0-3.5 mm posterior to the limbus at a shallow angle (10-15°) to avoid scleral penetration. Advance needle until loss of resistance indicates suprachoroidal space entry. Slowly inject 50 μL formulation over 10-15 seconds. For comparison, perform standard intravitreal injections in contralateral eyes (injecting 50 μL through pars plana 2 mm posterior to limbus).
- Distribution Analysis: Sacrifice animals at predetermined time points (1 hour, 24 hours, 7 days, 28 days). Enucleate eyes and freeze in optimal cutting temperature compound. Prepare cryosections (10 μm thickness). Image using confocal microscopy to quantify fluorescent distribution. Process additional eyes for histology (H&E staining) to assess tissue response.
- Drug Quantification: Dissect ocular tissues (cornea, aqueous humor, iris-ciliary body, lens, vitreous humor, retina-choroid, sclera). Homogenize tissues and extract drug using acetonitrile precipitation. Analyze using LC-MS/MS with validated methods. Calculate pharmacokinetic parameters (Cmax, Tmax, AUC) for each compartment.
- Efficacy Assessment: In separate efficacy studies, use laser-induced choroidal neovascularization model. Inject anti-VEGF formulation via suprachoroidal route versus intravitreal control. Monitor lesion development using fluorescein angiography and OCT at days 7, 14, and 28 post-treatment [43].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Ocular Drug Development Studies
| Reagent/Material | Supplier Examples | Function in Research | Application Examples |
|---|---|---|---|
| AlphaFold3 | DeepMind | Protein structure prediction | Target identification for ocular diseases |
| PandaOmics | Insilico Medicine | Multi-omics target discovery | Identifying novel pathways in AMD |
| Cy5.5 fluorescent dye | Thermo Fisher | Tracking drug distribution | Suprachoroidal injection studies |
| SCS Microinjector | Clearside Biomedical | Suprachoroidal space access | Preclinical and clinical delivery studies |
| Hydrogel polymers | Various | Sustained-release formulations | Intravitreal implant development |
| VEGF-A ELISA kits | R&D Systems | Measuring drug target engagement | Anti-VEGF therapy development |
| Ocular tissue homogenization kits | BioVision | Tissue processing for PK studies | Drug quantification in ocular compartments |
| 3D bioprinting systems | Allevi, Organovo | Tissue engineering for testing | Creating corneal models for drug screening |
Career Pathways in Biomedical Engineering and Optics Research
The rapid advancement of pharmaceutical applications in drug delivery and development tools has created diverse career opportunities for biomedical engineers and optics researchers. Professionals in this field typically work at the intersection of engineering, medicine, and data science, contributing to various stages of the drug development pipeline. Medical device engineers focus on designing and developing specialized delivery systems such as suprachoroidal injectors, sustained-release implants, and drug-eluting contact lenses. These roles require expertise in materials science, biomechanics, CAD modeling, and prototyping [6] [5].
Biomedical research scientists in academia and industry lead laboratory investigations into novel therapeutic approaches, including tissue engineering, biomaterials, and regenerative medicine. The Functional Optical Imaging Laboratory (FOIL) at Northwestern University exemplifies such research environments, where teams work on developing advanced optical imaging technologies like visible-light optical coherence tomography for ocular applications [63]. Neural engineers represent another specialization, focusing on brain-machine interfaces and neurotechnology, with applications in visual prosthetics and optic nerve regeneration [6].
Regulatory affairs specialists play a crucial role in navigating FDA and international regulations to ensure medical devices and therapies meet safety and efficacy standards. With the increasing complexity of drug-device combination products, professionals with expertise in both engineering and regulatory science are in high demand. Similarly, quality assurance and validation engineers ensure medical technologies meet performance and safety standards through rigorous testing protocols [6]. The growing emphasis on AI in drug discovery has also created opportunities for bioinformatics and computational biomedical engineers who apply data science, machine learning, and computational modeling to biological systems and personalized medicine [6] [5].
The landscape of pharmaceutical applications in drug delivery systems and development tools is evolving at an unprecedented pace, driven by innovations in biomedical engineering and optics research. AI-powered drug discovery platforms are dramatically shortening development timelines and increasing success rates, while novel delivery systems are addressing long-standing challenges in ocular therapeutics. For researchers and drug development professionals, these advancements create both opportunities and responsibilities—to leverage these tools responsibly, to validate computational predictions through rigorous experimentation, and to ensure that technological progress translates to genuine patient benefit. As these fields continue to converge, professionals with interdisciplinary expertise in engineering, optics, data science, and biology will be uniquely positioned to lead the next wave of innovation in pharmaceutical development.
Biomedical engineering stands at the crossroads of medicine, biology, and engineering, creating technologies that save and improve human lives. This field requires a unique synthesis of technical competencies spanning computational, mechanical, biological, and regulatory domains. As we approach 2025, biomedical engineering continues to evolve rapidly, driven by advancements in personalized medicine, artificial intelligence, microrobotics, and regenerative medicine [27]. Professionals in this domain must master a diverse toolkit to design advanced medical devices, develop diagnostic systems, create therapeutic solutions, and navigate complex approval processes. The essential technical skills—programming, computer-aided design (CAD), laboratory techniques, and regulatory knowledge—form the foundational pillars supporting innovation in both biomedical engineering and the increasingly integrated field of optics research, particularly in applications like medical imaging and photonic therapeutics [6] [64]. This guide provides an in-depth analysis of these core competencies, offering researchers, scientists, and drug development professionals a structured framework for skill development aligned with current industry demands.
Programming and Computational Skills
Programming has become indispensable in modern biomedical engineering, enabling everything from data analysis and device control to computational modeling and AI-driven diagnostics. Mastery of specific languages and computational frameworks is now a fundamental expectation for researchers.
Table 1: Essential Programming Languages and Applications in Biomedical Engineering
| Programming Language/Tool | Primary Applications in BME | Key Libraries/Frameworks |
|---|---|---|
| Python | Data analysis, machine learning, bioinformatics, medical image processing | NumPy, SciPy, Pandas, Scikit-learn, TensorFlow, OpenCV |
| C/C++ | Embedded systems for medical devices, real-time control, high-performance computing | STL, Boost, Qt, LabVIEW integration |
| MATLAB | Numerical computing, algorithm development, data visualization, simulation | Image Processing Toolbox, Simulink, Bioinformatics Toolbox |
| R | Statistical analysis of biological data, bioinformatics, clinical trial analysis | Bioconductor, ggplot2, dplyr |
| SQL/Database Management | Managing electronic health records, genomic databases, clinical data | MySQL, PostgreSQL, Oracle |
Python has emerged as one of the most critical programming languages, with its omnipresence in the data technology world making it essential for biomedical engineers [65]. Its application spans from analyzing genomic sequences for personalized medicine to developing AI algorithms for diagnostic imaging. C and C++ remain vital for programming embedded systems in medical devices such as pacemakers, infusion pumps, and diagnostic equipment [66]. These languages provide the low-level hardware control and real-time performance required for life-critical applications. MATLAB is widely used for rapid prototyping, signal processing, and computational modeling of biological systems, while R dominates statistical analysis in clinical research and bioinformatics.
Beyond specific languages, biomedical engineers increasingly require skills in bioinformatics and computational modeling. This involves applying data science, AI, and computational modeling to biological systems, genomics, and personalized medicine [6]. Proficiency in machine learning frameworks like TensorFlow and PyTorch is valuable for developing predictive models for disease diagnosis and treatment optimization. As biomedical devices become more connected, understanding data security principles and cloud computing platforms for managing large-scale biomedical data is also advantageous.
Experimental Protocol: AI-Assisted Medical Image Analysis
Objective: To develop a Python-based workflow for automated detection of anomalies in medical imaging data using machine learning techniques.
Materials and Methods:
- Dataset: Acquire a curated medical image set (e.g., chest X-rays, retinal scans, MRI slices) from a public repository like the Cancer Imaging Archive.
- Software Environment: Python 3.8+, with libraries: TensorFlow 2.4+, Keras, OpenCV, Scikit-learn, Matplotlib, NumPy, and DICOM processing library.
- Computational Hardware: Workstation with GPU (e.g., NVIDIA GeForce RTX 3080 or higher) for accelerated deep learning training.
Procedure:
- Data Preprocessing:
- Load medical images in DICOM format using
pydicomlibrary. - Apply normalization to scale pixel intensities to a standard range [0,1].
- Perform data augmentation techniques including rotation (±10°), horizontal flipping, and contrast adjustment to increase dataset diversity and model robustness.
- Load medical images in DICOM format using
- Model Architecture:
- Implement a Convolutional Neural Network (CNN) using TensorFlow/Keras with:
- Three convolutional layers with ReLU activation and max-pooling.
- Two fully connected (dense) layers with dropout regularization (rate=0.5).
- Final sigmoid activation layer for binary classification.
- Implement a Convolutional Neural Network (CNN) using TensorFlow/Keras with:
- Model Training:
- Split dataset into training (70%), validation (15%), and test (15%) sets.
- Train model for 50 epochs using Adam optimizer with learning rate of 0.001.
- Implement early stopping callback to monitor validation loss with patience of 10 epochs.
- Performance Evaluation:
- Calculate accuracy, precision, recall, and F1-score on test set.
- Generate Receiver Operating Characteristic (ROC) curve and calculate Area Under Curve (AUC).
- Visualize model attention maps using Grad-CAM to interpret detection focus areas.
Medical Image Analysis Workflow: A computational pipeline for automated anomaly detection in medical images using deep learning.
CAD and Engineering Design Skills
Computer-aided design (CAD) proficiency is fundamental for biomedical engineers involved in developing medical devices, implants, prosthetics, and surgical instruments. CAD skills enable the transformation of conceptual designs into precise 3D models that can be analyzed, refined, and prepared for prototyping and manufacturing.
Core CAD Competencies include advanced knowledge of materials science, biomechanics, CAD modeling, and prototyping [6]. Biomedical engineers must master solid modeling (creating 3D representations of devices), surface modeling (designing complex organic shapes for implants), and parametric design (creating models with adjustable parameters for customization). Specific CAD software proficiency varies by industry sector but typically includes:
- SOLIDWORKS: Widely used for medical device design due to its comprehensive toolset for part, assembly, and drawing creation.
- AutoCAD: Essential for 2D drafting and documentation of medical equipment layouts.
- Siemens NX: Employed for advanced applications including implant design and computational fluid dynamics.
- PTC Creo: Used for connected medical device development with strong parametric modeling capabilities.
- Fusion 360: Popular for integrated CAD/CAM and additive manufacturing applications.
A critical application of CAD in biomedical engineering is patient-specific implant design. This process begins with medical imaging data (CT or MRI scans), which is converted to a 3D model through segmentation. The implant is then designed to precisely match the patient's anatomy, followed by finite element analysis (FEA) to simulate physiological loads and ensure structural integrity before manufacturing.
Table 2: CAD Applications in Biomedical Engineering Specializations
| Biomedical Specialization | Primary CAD Applications | Analysis Tools |
|---|---|---|
| Medical Device Design | Housing design, component layout, mechanism development | Stress analysis, interference detection, tolerance analysis |
| Implant & Prosthetic Design | Custom implant modeling, joint replacements, dental implants | Finite Element Analysis (FEA), wear simulation, biomechanical modeling |
| Surgical Instrument Design | Ergonomics optimization, mechanism design, component integration | Motion analysis, sterilization compliance checking |
| Tissue Engineering | Scaffold design with controlled porosity, bioreactor components | Fluid flow analysis, structural permeability |
Experimental Protocol: 3D Modeling of a Spinal Implant
Objective: To design and analyze a patient-specific spinal cage implant using CAD and finite element analysis.
Materials and Methods:
- Software: SOLIDWORKS 2022 (or higher), SOLIDWORKS Simulation, Mimics Innovation Suite or 3D Slicer.
- Input Data: Patient lumbar spine CT scan (slice thickness ≤1mm).
- Design Standards: Adherence to ASTM F2077 for titanium spinal implants.
Procedure:
- Image Segmentation:
- Import DICOM files from CT scan into segmentation software.
- Apply thresholding to isolate vertebral bone from surrounding tissue.
- Manually refine segmentation to accurately capture bony anatomy.
- Generate 3D model of vertebral bodies and export as STL file.
- Implant Design:
- Import STL of vertebral anatomy into SOLIDWORKS as reference geometry.
- Create new part file and design implant core geometry based on intervertebral space measurements.
- Add porous surface structures for bone integration using pattern features.
- Incorporate surgical instrument interface features.
- Apply material properties (Ti6Al4V titanium alloy).
- Finite Element Analysis:
- Apply fixture constraints to inferior surface simulating lower vertebra.
- Apply distributed load of 1200N to superior surface simulating spinal loading.
- Mesh model with curvature-based mesh, element size 0.5mm.
- Run static analysis and evaluate stress distribution and factor of safety.
- Design Validation:
- Check maximum von Mises stress against material yield strength.
- Verify displacement under load remains within acceptable limits (<0.5mm).
- Iterate design if necessary to reduce stress concentrations.
- Export final design for additive manufacturing or traditional production.
Implant Design Workflow: Engineering process for creating patient-specific spinal implants from medical imaging to production-ready design.
Laboratory Techniques and Experimental Methods
Biomedical engineers require extensive hands-on laboratory skills to conduct research, develop prototypes, and validate medical technologies. These techniques span molecular biology, tissue engineering, biomaterials testing, and physiological measurement.
Core Laboratory Competencies include experimental design, molecular biology, bioengineering techniques, data analysis, and scientific communication [6]. Biomedical research engineers must be proficient in cell culture techniques (maintaining mammalian cell lines, sterile technique, 3D culture systems), biomaterial characterization (mechanical testing, surface analysis, degradation studies), and fabrication methods (electrospinning, 3D bioprinting, microfabrication). For those specializing in optics and photonics, skills in optical system setup, laser manipulation, and fiber optics become crucial [66].
Table 3: Essential Laboratory Techniques in Biomedical Engineering Research
| Technique Category | Specific Methods | Primary Applications |
|---|---|---|
| Cell & Tissue Culture | Aseptic technique, primary cell isolation, 3D scaffold seeding, co-culture systems | Tissue engineering, regenerative medicine, drug testing |
| Biomaterial Synthesis & Characterization | Polymer synthesis, electrospinning, FTIR, SEM, mechanical tensile testing | Implant development, drug delivery systems, scaffold fabrication |
| Molecular Biology | ELISA, PCR, Western blot, immunohistochemistry, flow cytometry | Diagnostic development, biomarker validation, cellular response studies |
| Optical Methods | Confocal microscopy, light sheet microscopy, optical coherence tomography | Tissue imaging, cellular tracking, device inspection |
Experimental Protocol: Electrospinning of Polymer Scaffolds for Tissue Engineering
Objective: To fabricate and characterize aligned nanofibrous scaffolds for neural tissue engineering applications.
Materials and Methods:
- Polymers: Polycaprolactone (PCL, Mw=80,000), gelatin (Type A).
- Solvents: Hexafluoro-2-propanol (HFIP), acetic acid.
- Equipment: Electrospinning apparatus with rotating mandrel collector, syringe pump, high-voltage power supply, fume hood.
- Characterization Tools: Scanning Electron Microscope (SEM), tensile testing machine, contact angle goniometer.
Procedure:
- Polymer Solution Preparation:
- Dissolve PCL in HFIP (10% w/v) by stirring for 12 hours at room temperature.
- Prepare gelatin solution (8% w/v) in acetic acid with gentle heating (40°C).
- Mix PCL and gelatin solutions in 70:30 ratio and stir for 6 hours to obtain homogeneous blend.
- Electrospinning Parameters:
- Load polymer solution into 10mL syringe with 21-gauge blunt needle.
- Set syringe pump flow rate to 1.0 mL/h.
- Apply high voltage of 15 kV between needle and collector.
- Set tip-to-collector distance at 15 cm.
- Use rotating mandrel collector at 2500 rpm to achieve fiber alignment.
- Maintain environmental conditions at 25°C and 40% relative humidity.
- Scaffold Characterization:
- Morphology Analysis: Sputter-coat scaffolds with gold and image using SEM at 10kV acceleration voltage. Measure fiber diameter distribution from multiple images (n=5) using ImageJ software.
- Mechanical Testing: Cut scaffolds into rectangular strips (20mm × 5mm). Perform uniaxial tensile test at 1mm/min strain rate until failure. Calculate Young's modulus from stress-strain curve.
- Surface Properties: Measure water contact angle using sessile drop method to determine hydrophilicity/hydrophobicity.
- Cell Culture Evaluation:
- Sterilize scaffolds by UV irradiation (30 minutes per side).
- Seed human neural stem cells at density of 50,000 cells/cm².
- Culture for 7 days, then assess cell viability using Live/Dead assay and analyze cell alignment relative to fiber direction.
Regulatory Knowledge and Quality Standards
Regulatory knowledge is a critical differentiator for biomedical engineers, ensuring that medical technologies meet safety and efficacy standards required for clinical use and market approval. Understanding regulatory pathways is essential for translating laboratory research into clinically impactful products.
Core Regulatory Competencies include knowledge of regulatory frameworks, documentation management, risk assessment, and communication with regulatory bodies [6] [67]. Biomedical engineers must be familiar with Quality Management Systems (ISO 13485), risk management (ISO 14971), medical device classification systems (FDA Class I, II, III; EU MDR classification), and design control processes. This expertise ensures that products are not only effective but also safe and compliant with industry regulations [67].
For engineers specializing in optics and photonics applied to medicine, additional considerations include laser safety standards (IEC 60825), optical performance validation, and fiber optic reliability testing [64]. The recent demonstration of precise optical clock signal transmission via multicore fiber highlights the importance of establishing standards for emerging photonic technologies in medical applications [64].
Table 4: Key Regulatory Frameworks for Biomedical Technologies
| Regulatory Area | Key Standards/Regulations | Scope and Application |
|---|---|---|
| Quality Management | ISO 13485:2016 | Quality management systems for medical device design and manufacturing |
| Risk Management | ISO 14971:2019 | Application of risk management to medical devices |
| US Market Approval | FDA 21 CFR Part 820 (Quality System Regulation) | US requirements for medical device manufacturing and control |
| European Market Approval | EU MDR 2017/745 | European Medical Device Regulation for market access |
| Biocompatibility | ISO 10993 series | Evaluation of biological response to medical devices |
| Clinical Evidence | ISO 14155:2020 | Good Clinical Practice for clinical investigations |
Experimental Protocol: Design Control Process for a Medical Device
Objective: To implement a design control process for a novel wearable photonic blood glucose monitor, following FDA Quality System Regulation requirements.
Materials and Methods:
- Documentation System: Electronic Quality Management System (eQMS) or controlled document system.
- Reference Standards: FDA 21 CFR Part 820, ISO 13485:2016, IEC 60601-1 (medical electrical equipment safety).
- Team Composition: Cross-functional team including design engineers, clinical specialists, regulatory affairs, and quality assurance.
Procedure:
- User Needs Identification:
- Conduct interviews with diabetic patients, endocrinologists, and nurses.
- Document user needs including continuous monitoring, calibration frequency, and form factor.
- Establish traceability matrix linking user needs to design inputs.
- Design Inputs Specification:
- Translate user needs into measurable engineering specifications:
- Measurement range: 40-400 mg/dL
- Accuracy: ±15% for 95% of measurements
- Wear time: ≥7 days continuous use
- Data reporting: Real-time to smartphone app
- Document design inputs in controlled specification document.
- Translate user needs into measurable engineering specifications:
- Design and Development:
- Create subsystem architecture: optical sensor, electronics, firmware, mobile app.
- Develop detailed design documentation including schematics, PCB layouts, and optical path diagrams.
- Implement risk management per ISO 14971 with FMEA for critical components.
- Design Verification:
- Execute verification protocols to confirm design outputs meet design inputs:
- Accuracy testing against reference glucose analyzer (n=300 measurements)
- Battery life testing under simulated use conditions
- Environmental testing (temperature, humidity)
- Document all verification results with objective evidence.
- Execute verification protocols to confirm design outputs meet design inputs:
- Design Validation:
- Conduct clinical validation with 50 diabetic patients over 14 days.
- Compare device performance to venous blood glucose measurements.
- Document user feedback on device usability and comfort.
- Prepare summary for regulatory submission.
- Design Transfer:
- Create manufacturing documentation including work instructions, test procedures, and acceptance criteria.
- Train manufacturing personnel on critical-to-quality processes.
- Establish ongoing monitoring of production units for continued compliance.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 5: Key Research Reagent Solutions in Biomedical Engineering
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Polycaprolactone (PCL) | Biodegradable synthetic polymer for scaffold fabrication | Tissue engineering, drug delivery systems, resorbable implants |
| Collagen Type I | Natural extracellular matrix protein for cell culture | 3D cell culture, wound healing models, tissue scaffolds |
| Fibronectin | Cell adhesion protein for surface coating | Improved cell attachment on biomaterials, migration studies |
| Lipid Nanoparticles | Drug and gene delivery vehicles | mRNA vaccine delivery, CRISPR gene editing, targeted therapy |
| Fluorescent Antibodies | Cell labeling and protein detection | Flow cytometry, immunohistochemistry, live-cell imaging |
| CRISPR-Cas9 System | Precise gene editing tool | Genetic disease modeling, gene therapy, functional genomics |
| Optical Clearing Agents | Render biological tissues transparent | Deep tissue imaging, 3D reconstruction, optical tomography |
The convergence of programming, CAD, laboratory techniques, and regulatory knowledge creates a powerful skill set for biomedical engineers and optics researchers. As the field advances toward 2025, professionals who master these technical domains while embracing interdisciplinary collaboration will lead the development of next-generation medical technologies. From AI-driven diagnostics and personalized implants to advanced photonic therapies and regenerative medicine, biomedical innovation requires this comprehensive technical foundation. Success in this evolving landscape depends not only on individual technical excellence but also on the ability to integrate these skills to solve complex healthcare challenges, ultimately translating engineering innovation into improved patient outcomes worldwide.
Navigating Challenges and Accelerating Career Growth in Biomedical Optics
The fields of biomedical engineering and biophotonics are at the forefront of medical innovation, driving advancements from personalized medicine and regenerative therapies to quantum computing and artificial intelligence (AI) applications in healthcare [27] [68]. However, this rapid technological evolution has created a critical disconnect between the skills taught in academic settings and those demanded by industry. This skills gap threatens to slow progress in critical areas such as drug development, medical device innovation, and diagnostic technologies [69] [70].
This whitepaper examines the current state of the skills gap in biomedical engineering and optics research, focusing specifically on the challenges faced by researchers, scientists, and drug development professionals. We present a detailed analysis of industry needs, identify key competency shortages, and propose evidence-based strategies for creating a more robust and responsive training ecosystem. By integrating quantitative data with practical solutions, this document aims to provide a roadmap for aligning academic preparation with the rapidly evolving demands of the biomedical and biophotonics industries.
Quantifying the Skills Gap
Market Growth and Workforce Demand
The disconnect between academic training and industry requirements is occurring within the context of massive market growth, particularly in specialized sectors like cell and gene therapy.
Table 1: Global Cell Therapy Manufacturing Market Growth Projections
| Year | Market Value (USD) | Compound Annual Growth Rate (CAGR) |
|---|---|---|
| 2023 | 9.1 billion | 26.6% |
| 2030 | 47.71 billion | 26.6% |
Source: [69]
This projected growth of over 500% within a decade underscores the urgent need for a skilled workforce. Analysis of job advertisement data reveals where industry demand is concentrated. A study collecting 276 job advertisements across multiple countries found consistent demand in three key functions: Research & Development (emphasizing innovation and novel therapeutics), Quality Assurance & Regulations, and Manufacturing [69]. This pattern indicates a priority on both innovation and the translation of discoveries into regulated, commercially viable products.
The Photonics Sector Shortage
In biophotonics—the fusion of light-based technologies with biology and medicine—the skills gap is equally severe. This field is fundamental to advancing medical imaging, biosensing, and light-based therapies [68]. The shortage of qualified photonics technicians is a global issue, with one estimate suggesting the United States needs approximately 85,000 technically skilled middle- and lower-level technicians by 2031, up from around 58,000 today [70]. To meet this demand, the U.S. would require about 140 more industry-oriented training programs [70]. The situation is exemplified by the Monroe Community College (MCC) Optical Systems Program, whose graduates are so highly sought-after that company production schedules are planned around their availability [71]. Despite this critical need, there are fewer than 10 dedicated optics technician programs across the United States [71].
Identifying Critical Skill Deficiencies
Core Competencies for Biomedical Engineers
Industry perspectives, gathered from sessions like the 2024 Biomedical Engineering Education Summit, highlight a shift in the competencies deemed most critical for graduates. While technical prowess is an expected outcome of accredited programs, professional skills are now viewed as both essential and harder to teach [72].
Table 2: Evolution of Top Industry-Requested Skills in Biomedical Engineering (2019 vs. 2024)
| Ranking | 2019 BME Education Summit | 2024 BME Education Summit |
|---|---|---|
| 1 | Problem-Solving | Communication |
| 2 | Interpersonal Communication | Teamwork/Collaboration |
| 3 | Data Analysis | Critical Thinking |
| 4 | Teamwork | Problem-Solving |
| 5 | Writing Skills | Data Analysis |
| 6 | Technical Presentation | Design |
Source: Adapted from [72]
This comparison reveals a notable shift, with communication and collaborative skills rising to the top. Industry panelists emphasized that engineers must communicate technical work to diverse audiences, including management, business, engineering, and regulatory sectors [72].
Specialized Technical Shortfalls
Beyond general competencies, specific technical gaps are emerging in high-growth sub-fields:
- Cell and Gene Therapy (CGT): The industry faces a shortage of professionals skilled in scaling manufacturing processes, ensuring product consistency, and adhering to stringent regulatory standards [69].
- Biophotonics and Integrated Photonics: There is a critical lack of technicians trained in manufacturing photonics systems, assembling components, and performing rigorous industrial testing [70]. The majority of photonics degree programs are offered at the graduate level, creating a foundational gap at the undergraduate and technical levels [70].
- Data Science and AI: With the growing use of large patient-derived datasets in biomedical research, there is a pronounced need for skills in data science, machine learning, and the ethical application of AI in healthcare [27] [72].
Root Causes of the Disconnect
Curricular Gaps and Limited Hands-On Training
A primary driver of the skills gap is the misalignment between university curricula and industry needs. An analysis of undergraduate programs found that most universities have yet to fully integrate Cell, Tissue, and Gene Therapy Product (CTGTP) related courses as core components of their degree programs [69]. While a shift is occurring, with some institutions introducing targeted courses and practical modules, this integration remains uneven [69]. Similarly, in photonics, existing STEM curricula often fail to meet the sector's specific demands, and many institutions lack access to cutting-edge technology for hands-on student training [70].
The Photonics Technician Training Gap
The critical shortage of optics and photonics technicians stems from a collapse in specialized training infrastructure. The near-disappearance of programs like the one at Monroe Community College (MCC) after the decline of local industry anchors (e.g., Kodak) demonstrates how vulnerable this pipeline is [71]. When MCC's program was at its lowest point with only five students, the over 150 optics and photonics companies in the Rochester area struggled to find any trained technicians [71]. Restarting such programs faces hurdles, including a lack of appropriate, accessible teaching materials that are not overly theoretical or calculus-heavy [71].
Strategies for Bridging the Gap
Enhancing Academic Curricula
To better prepare the workforce, academic institutions must take proactive steps to evolve their curricula and training models.
Table 3: Proposed Solutions for Academic Curriculum Enhancement
| Solution Area | Specific Actions | Expected Outcome |
|---|---|---|
| Curriculum Modernization | Integrate CTGTP-related courses into core life sciences and engineering programs [69]. Introduce specialized modules on biophotonics, data science, and regulatory affairs [72] [5]. | Graduates possess relevant, up-to-date technical knowledge. |
| Hands-On, Industry-Aligned Training | Expand internships, co-op programs, and capstone projects with industry partners [69] [73]. Incorporate hands-on training in linear and non-linear photonics at the undergraduate level [70]. | Graduates gain practical skills and understand industry workflows. |
| Interdisciplinary Collaboration | Create cross-disciplinary courses and projects that blend engineering, life sciences, data science, and ethics [72]. | Graduates can work effectively in diverse, cross-functional teams. |
| Professional Skill Integration | Explicitly teach and assess communication, collaboration, and leadership skills within technical courses [72]. | Graduates are effective communicators and collaborators. |
A Framework for Integrated Skill Development
A systematic approach is required to develop the interdisciplinary skill set needed for modern biomedical and biophotonics research. The following framework visualizes the interconnected components of a comprehensive training program.
Experimental Protocol for Hands-On Photonics Training
A critical component of bridging the skills gap is providing relevant, industry-standard practical experience. The following protocol outlines a foundational hands-on exercise in optical fabrication, a core skill for biophotonics technicians working on medical imaging systems or optical biosensors.
Protocol: Hand Grinding and Polishing of Optical Glass Substrates
Objective: To master the fundamental manual process for transforming raw optical glass into a precision prototype with specified surface geometry and finish, a skill essential for creating custom optics for research instrumentation and medical devices [71].
Research Reagent Solutions and Essential Materials:
Table 4: Key Materials for Optical Fabrication Training
| Item | Function |
|---|---|
| Optical Glass Blank | Raw substrate material (e.g., BK7, Fused Silica) to be shaped into the final optical component. |
| Abrasive Grinding Grits | Successively finer silicon carbide or aluminum oxide powders (e.g., 40μm, 25μm, 9μm) for removing material and shaping the glass. |
| Pitch Polishing Lap | A compliant tool made of optical pitch used with a fine abrasive (e.g., Cerium Oxide) to create a smooth, transparent surface. |
| Interferometer | Precision instrument for measuring surface flatness and figure, verifying compliance with technical specifications. |
| Spherometer | Tool for measuring the radius of curvature of spherical surfaces during fabrication. |
Methodology:
- Blocking: The glass blank is securely attached to a blocking tool using pitch or wax for safe handling during grinding.
- Coarse Grinding: Using the largest grit abrasive (e.g., 40μm) on a cast-iron grinding tool, the operator shapes the glass to the approximate desired curvature (flat, spherical). The surface is continuously monitored with a spherometer.
- Fine Grinding: The process is repeated with progressively finer grits (e.g., 25μm, then 9μm). Each stage removes the sub-surface damage from the previous, coarser stage. The workpiece is thoroughly cleaned between grits to prevent contamination.
- Polishing: The ground surface is worked against a pitch lap charged with a cerium oxide slurry. This process eliminates the remaining micro-fractures, transforming the translucent ground surface into a clear, transparent optical finish.
- Metrology and Validation: The final surface is measured using an interferometer to quantify surface flatness/figure and wavefront error. The component is evaluated against pre-defined acceptance criteria, mirroring industry quality control processes.
This protocol provides foundational skills that remain relevant despite the availability of CNC machines, as they are still required for advanced technologies needing inflexible fixturing and low-volume optical flats [71].
The skills gap in biomedical engineering and optics research is a significant but surmountable challenge. Addressing it requires a concerted, collaborative effort between universities, industry, and government. Key to this effort is a mindset shift: academia must view industry not just as a destination for graduates but as an active partner in curriculum design and practical training [72]. Initiatives like AIM Photonics in the U.S. and the Phortify network in the EU demonstrate the power of such partnerships in creating a more robust talent pipeline [74] [70].
The future of biomedical innovation depends on a workforce that is not only technically proficient in emerging areas like biophotonics, AI, and cell manufacturing but also equipped with the professional skills to work effectively in interdisciplinary teams and navigate complex regulatory landscapes. By implementing the strategies outlined in this whitepaper—modernizing curricula, integrating hands-on and industry-aligned training, and fostering interdisciplinary collaboration—we can bridge the skills gap and ensure the continued pace of discovery and development in critical health technologies.
For biomedical engineers and optics researchers, the U.S. Food and Drug Administration's regulatory pathways represent a critical framework that shapes research priorities, development timelines, and ultimate clinical translation. The FDA's regulatory environment is dynamic, with significant changes occurring in both drug and device approval processes. Recent developments include a major transition from the Quality System Regulation to a harmonized Quality Management System Regulation that incorporates international standards, specifically ISO 13485:2016 [75]. This shift, effective February 2, 2026, represents the most substantial change to medical device quality management requirements in decades and demands attention from professionals across the biomedical spectrum [75] [76].
Simultaneously, the drug approval landscape continues to evolve with emerging technologies—including optical imaging agents—facing unique regulatory considerations. The FDA has issued specific draft guidance for optical imaging drugs used as intraoperative aids for pathology detection, highlighting the specialized evidence needed for these combination products [7]. Understanding these interconnected regulatory frameworks is essential for successfully navigating product development from laboratory research to clinical application.
Quality Management System (QMS) Requirements for Medical Devices
The QMSR Transition: Key Changes and Timeline
The FDA's final rule amending 21 CFR Part 820 establishes the Quality Management System Regulation, which aligns U.S. medical device requirements with the international consensus standard ISO 13485:2016 [75]. This harmonization initiative aims to create consistency in global device regulation while maintaining the FDA's rigorous standards for safety and effectiveness.
Table: Key Transition Dates for Quality Management System Regulation
| Date | Regulatory Milestone | Impact on Manufacturers |
|---|---|---|
| February 2, 2024 | Final Rule published | Awareness and planning phase begins |
| February 2, 2026 | QMSR effective date | Compliance with new requirements mandatory |
| February 2, 2026 | QSIT inspection technique withdrawn | New inspection process implemented |
Critical Modifications Under QMSR
While incorporating ISO 13485 by reference, the QMSR establishes additional requirements to ensure consistency with FDA statutes and regulations. Several significant changes demand particular attention from biomedical engineering teams:
- Expanded Documentation Access: The exceptions that previously existed in the QS regulation at § 820.180(c) for certain records are not maintained in the QMSR. FDA investigators will now have authority to inspect management review reports, internal audit results, and supplier audit reports during inspections [75].
- Revised Inspection Methodology: The familiar Quality System Inspection Technique (QSIT) will be formally withdrawn on February 2, 2026, and replaced with a new inspection process documented in a revised Compliance Program specifically aligned with QMSR requirements [75].
- Harmonized Terminology: The regulation updates terms and concepts to align with ISO 13485, including changes to requirements for device labeling and packaging controls, and clarifications regarding device transfer processes [75].
For optics researchers developing medical devices, these changes emphasize the importance of establishing robust quality management systems early in development. The FDA encourages manufacturers to perform a comparative analysis demonstrating how documents and records created prior to the QMSR effective date meet the new requirements [75].
Premarket Submission Requirements
Recent draft guidance outlines expectations for QMS information in certain premarket submissions, emphasizing that quality system considerations should be integrated throughout the development process rather than addressed as a final step before submission [77] [76]. This guidance assists manufacturers in preparing the specific quality management system information required in marketing submissions once the QMSR takes effect, helping FDA staff determine compliance with the new regulation [76].
FDA Drug Approval Process for Novel Therapeutics
2025 Novel Drug Approvals: Trends and Patterns
The Center for Drug Evaluation and Research maintains a robust pipeline for novel therapeutic agents, with 38 novel drugs approved as of November 2025 [78]. These approvals reveal significant trends particularly relevant to biomedical researchers focusing on targeted therapies and precision medicine.
Table: Select 2025 Novel Drug Approvals in Oncology and Rare Diseases
| Drug Name | Active Ingredient | Approval Date | FDA-Approved Use |
|---|---|---|---|
| Hyrnuo | sevabertinib | Nov 19, 2025 | Locally advanced or metastatic non-squamous NSCLC with HER2 mutations |
| Komzifti | ziftomenib | Nov 13, 2025 | Relapsed/refractory AML with NPM1 mutation |
| Modeyso | dordaviprone | Aug 6, 2025 | Diffuse midline glioma with H3 K27M mutation |
| Zegfrovy | sunvozertinib | Jul 2, 2025 | NSCLC with EGFR exon 20 insertion mutations |
| Sephience | sepiapterin | Jul 28, 2025 | Hyperphenylalaninemia in sepiapterin-responsive PKU |
Analysis of the 2025 approval landscape reveals a strategic shift toward targeted therapeutic development in precisely defined patient populations. This approach leverages specific biomarkers and genetic mutations to create defensible markets through specialized intellectual property rather than pursuing broad indications [79]. For researchers, this underscores the importance of companion diagnostics and precise patient stratification in therapeutic development.
Navigating the Drug Development Pathway
The traditional drug approval pathway involves multiple well-defined stages, though recent disruptions have introduced uncertainties. The typical process includes:
- Pre-IND Meetings: Early discussions with FDA to align on development strategy
- Investigational New Drug Application: Submission of manufacturing, preclinical, and clinical plans
- Clinical Trial Phases: Progressive evaluation of safety and efficacy
- Pre-NDA/BLA Discussions: Alignment on application content and format
- New Drug Application/Biologic License Application: Comprehensive submission of all evidence
- FDA Review: Typically 6-10 months for standard review
- Post-Approval Commitments: Additional studies if required [80]
Recent organizational changes at FDA have created challenges, with reported extensions in wait times for sponsor-FDA meetings from 3 months to as long as 6 months [80]. Additionally, policy offices that develop regulatory guidelines were significantly affected by workforce reductions, creating uncertainty about technical requirements for drug development [80]. These factors may particularly impact researchers developing innovative products like optical imaging agents that don't fit neatly into existing regulatory paradigms.
Special Considerations for Optical Imaging Agents
Unique Regulatory Pathway for Optical Imaging Drugs
Optical imaging agents represent a specialized category that combines characteristics of both drugs and devices, requiring careful regulatory navigation. In January 2025, the FDA issued draft guidance specifically addressing the development of optical imaging drugs, which are used in conjunction with imaging devices as intraoperative aids for detecting pathology such as tumors or for enhancing the visibility of normal anatomical structures [7].
This guidance provides important recommendations for clinical trial design features that support development and approval of these combination products. For biomedical engineers and optics researchers, understanding these specific requirements is essential for designing appropriate preclinical and clinical validation strategies.
Experimental Design and Validation Methodologies
The development of optical imaging agents requires specialized experimental protocols to demonstrate both safety and effectiveness. Key methodological considerations include:
- Target-to-Background Ratio Quantification: Establishing standardized metrics for signal differentiation in various tissue types under controlled illumination conditions
- Dose-Ranging Studies: Systematic evaluation of contrast agent concentrations to optimize visualization while minimizing potential toxicity
- Device-Agent Co-development: Parallel validation of both the imaging device and contrast agent as an integrated system
- Operator Training Protocols: Standardized procedures for image acquisition and interpretation to minimize variability
The following workflow diagram illustrates the integrated development process for optical imaging agents that combine drug and device characteristics:
Diagram: Integrated Development Workflow for Optical Imaging Agents
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development of biomedical products requires carefully selected research materials and analytical approaches. The following table details essential reagents and their applications in regulatory-focused research, particularly for optical imaging agents and targeted therapies.
Table: Essential Research Reagents for Biomedical Product Development
| Research Reagent/Material | Function in Development | Regulatory Considerations |
|---|---|---|
| ISO 13485:2016 Standard | Quality Management System framework | Read-only access via ANSI IBR Portal required for QMSR compliance [75] |
| Target-Specific Contrast Agents | Optical imaging and molecular targeting | Demonstrate specificity and affinity for intended molecular target |
| Validated Animal Models | Preclinical efficacy and safety assessment | Relevance to human physiology and disease pathology |
| Reference Standards | Analytical method validation and calibration | Qualified against recognized standards with documented traceability |
| Cell-Based Assay Systems | In vitro toxicity and efficacy screening | Demonstrate reproducibility and relevance to clinical outcomes |
For optical imaging specifically, researchers should prioritize reagents that enable comprehensive characterization of pharmacokinetics, binding specificity, and optical properties across relevant tissue types. The FDA's draft guidance emphasizes the importance of robust analytical methods to characterize these agents throughout their shelf life and under anticipated use conditions [7].
Strategic Implications for Biomedical Engineering Careers
Evolving Skill Demands in Regulatory Science
The changing regulatory landscape creates both challenges and opportunities for biomedical engineers and optics researchers. Professionals who develop expertise in the revised QMSR requirements and their application to novel technologies like optical imaging agents will be particularly well-positioned for impactful careers. The FDA itself employs engineers as scientific reviewers to evaluate technical data submitted in medical device submissions, with qualifications including a thorough knowledge of the physical and mathematical sciences underlying professional engineering [81].
At the Center for Drug Evaluation and Research, engineering roles include providing technical guidance on pharmaceutical quality, reviewing chemistry and manufacturing controls data in drug applications, and participating in manufacturing facility inspections [82]. These positions require not only technical expertise but also the ability to assess comprehensive data packages against regulatory standards.
Navigating Organizational Change at FDA
Recent organizational changes at FDA have created a dynamic environment for regulatory professionals. A reduction in force in April 2025, while excluding drug, device, and food reviewers and inspectors, has nonetheless created challenges including extended timelines for sponsor-agency interactions and potential delays in guidance development [80]. This environment demands greater regulatory strategy expertise from researchers and developers, who may need to build more buffer into development timelines and seek additional expert consultation during product development.
The agency's focus on regulatory harmonization through initiatives like the QMSR transition, coupled with resource constraints, creates both challenges and opportunities for biomedical professionals. Those who can effectively navigate this complex environment while maintaining rigorous scientific standards will be invaluable contributors to the field of biomedical innovation.
In the competitive and research-intensive fields of biomedical engineering and optics, strategic technical optimization is not merely an operational goal but a fundamental requirement for innovation and market viability. Effective management of component costs and manufacturing processes directly influences the pace of scientific discovery, the accessibility of novel therapies, and the overall sustainability of biomedical enterprises. As the industry experiences significant growth driven by advancements in areas like regenerative therapies and biosimilars, organizations face intense pressure to reduce uncertainties in the product development cycle and ensure consistent quality while managing operational expenses [83]. This whitepaper provides a comprehensive technical guide for researchers, scientists, and drug development professionals seeking to implement rigorous cost-modeling approaches and process optimization strategies. By framing these methodologies within the context of biomedical engineering and optics research careers, we highlight the critical role that technical efficiency plays in enabling groundbreaking scientific work and bringing transformative healthcare solutions to market.
The challenges are multifaceted; the biotechnology industry grapples with the high costs and time-intensive nature of biopharma product development, while simultaneously navigating quality control issues in contract manufacturing and complexities within supply chain management [83]. Furthermore, the relentless pace of innovation in complementary fields such as optical components—which is seeing transformative growth through advances in high-speed communications, artificial intelligence (AI), and healthcare applications—creates both opportunities and pressures for biomedical engineers to integrate cutting-edge technologies in a cost-effective manner [84]. This document addresses these challenges by presenting detailed cost analysis frameworks, experimental protocols for manufacturing optimization, and forward-looking strategies for leveraging technological advancements across biomedical and optical domains.
Strategic Cost Modeling and Analysis
A foundational element of technical optimization in biomedical engineering involves developing precise cost models that illuminate both direct and indirect expenses throughout the research, development, and production lifecycle. Comprehensive cost model analysis enables organizations to understand market trends, determine fair market pricing, negotiate effectively with suppliers, and make informed decisions regarding outsourcing versus in-house production [83].
Key Cost Drivers in Biomedical Engineering
Through systematic analysis, several critical cost drivers consistently emerge as primary contributors to overall expenses in biomedical engineering operations. Understanding these components allows for targeted optimization efforts:
Raw Materials and Components: This category encompasses specialty chemicals, biological reagents, optical materials, and electronic components. The procurement strategy for these materials significantly impacts overall cost structures, particularly for specialized reagents used in drug development and diagnostics [83].
Labor Costs: Skilled technical labor represents a substantial portion of project expenses, particularly for research-intensive activities requiring specialized expertise in optics, biology, and engineering disciplines [83].
Operational and Overhead Expenses: These include facility costs, equipment depreciation, utilities, and maintenance. Advanced manufacturing environments often require climate-controlled cleanrooms and specialized infrastructure, contributing significantly to operational overhead [83].
Research and Development Investment: The initial R&D phase requires substantial capital allocation for experimental setups, prototype development, and iterative testing procedures [83].
Regulatory Compliance and Quality Assurance: Meeting stringent regulatory requirements for medical devices and therapeutics involves significant expenditure on testing, documentation, and quality control systems [83].
Table 1: Primary Cost Drivers in Biomedical Engineering
| Cost Category | Specific Examples | Typical Impact Level |
|---|---|---|
| Raw Materials | Specialty chemicals, biological reagents, optical materials, substrates | High |
| Labor | Research scientists, optical engineers, technicians, quality control staff | High |
| Equipment | Imaging systems, fabrication tools, analytical instruments, testing apparatus | Medium-High |
| Facilities | Cleanrooms, laboratories, specialized infrastructure, utilities | Medium |
| Regulatory Compliance | Certification processes, documentation, validation testing, quality audits | Medium-High |
| Supply Chain | Logistics, inventory management, supplier relationships, import/export costs | Medium |
Cost Model Implementation Framework
Implementing a structured cost model requires a methodical approach to data collection, analysis, and interpretation. The following framework provides a roadmap for developing comprehensive cost models in biomedical engineering contexts:
Market Insight and Trend Analysis: Conduct comprehensive research to understand recent market trends, including the growing emphasis on personalized medicine, advancements in biotechnology, increased regulatory scrutiny, and rising demand for cost-effective solutions. This analysis should also cover shifts in global supply chain dynamics, emerging technologies such as AI and automation in manufacturing, and the impact of sustainability initiatives [83].
Cost Driver Identification and Quantification: Systematically identify all relevant cost components, including direct costs (materials, labor) and indirect costs (overhead, administrative expenses). Primary research should be conducted to determine fair market costs, and internal modeling should be utilized to calculate per-unit costs [83].
Outsourcing Versus In-House Evaluation: Compare outsourcing options with in-house capabilities to determine the most cost-effective approach for each component or process. This evaluation should consider both quantitative factors (cost per unit, capital investment) and qualitative aspects (quality control, intellectual property protection, response time) [83].
Risk Impact Assessment: Evaluate the cost implications of potential risks, including supply chain disruptions, regulatory changes, and technological obsolescence. This assessment allows organizations to develop contingency plans and make more informed decisions [83].
Scenario Modeling and Sensitivity Analysis: Develop multiple cost scenarios based on different assumptions regarding material costs, production volumes, and market conditions. Identify which variables have the greatest impact on overall costs to prioritize optimization efforts [83].
The outcome of a comprehensive cost model analysis should provide insights into both direct and indirect costs, intangible costs, opportunity costs, and the financial impact of potential risks. This analysis also enables organizations to account for all direct and indirect revenues and tangible benefits, ultimately helping achieve the most cost-effective mix of resources and processes [83].
Experimental Protocols for Manufacturing Optimization
Enhanced Plasmid DNA Production via Controlled Evolution
Plasmid DNA (pDNA) is an essential and expensive component in many gene therapies and DNA vaccines, with production costs potentially reaching $100,000 per gram using conventional methods [85]. Recent research demonstrates that controlled evolution of production strains can dramatically improve manufacturing efficiency and reduce costs.
Experimental Objective: To increase pDNA production in E. coli through inducible genome-wide mutagenesis and screening for enhanced plasmid copy number variants.
Methodology:
- Strain Preparation: Begin with genetically modified E. coli NEB 5α strains already optimized for pDNA production.
- Mutagenesis Implementation: Introduce random mutations across the bacterial genome using an inducible mutagenesis system. This approach allows for controlled evolution without continuous genetic instability.
- High-Throughput Screening: Implement fluorescent screening protocols to identify individual bacterial clones with enhanced pDNA production capabilities. Fluorescence-activated cell sorting (FACS) can efficiently isolate promising variants.
- Performance Validation: Test selected mutant strains for their ability to produce multiple types of pDNA, including those with pUC, p15A, and pSC101 origins. Quantify plasmid copy numbers (PCNs) using quantitative PCR or other appropriate methods.
- Genomic Analysis: Perform whole-genome sequencing of high-performing mutants to identify specific mutations responsible for enhanced production.
- Genetic Validation: Conduct complementation assays or gene replacement studies to confirm the functional role of identified mutations in enhancing pDNA production.
Key Results: This protocol yielded an E. coli strain (M3) with dramatically increased plasmid copy numbers across multiple origin types. Specifically, researchers observed:
- 8.7-fold increase in PCN for pAAV-CAGG-eGFP plasmid
- 5.93-fold increase in PCN for GFP reporter plasmid
- 1.93-fold increase for gWiz DNA vaccine plasmid
- 1.44-fold and 1.68-fold increases for plasmids with p15A and pSC101 origins, respectively [85]
Diagram 1: pDNA Production Optimization Workflow
Research Reagent Solutions for Manufacturing Optimization
Table 2: Essential Research Reagents for Manufacturing Optimization Experiments
| Reagent/Resource | Function in Experimental Protocol | Specific Application Example |
|---|---|---|
| E. coli NEB 5α Strain | Host organism for plasmid DNA production | Baseline production host for pDNA manufacturing [85] |
| Mutagenesis Agents | Introduce genetic variations for strain improvement | Chemical or transposon-based mutagens for controlled evolution [85] |
| Selection Media | Identify and maintain transformed bacteria | Antibiotic-containing media to select for plasmid-containing clones [85] |
| PCR Reagents | Amplify and quantify specific DNA sequences | Determination of plasmid copy number through quantitative PCR [85] |
| Sequencing Kits | Identify genetic mutations in improved strains | Whole-genome sequencing to pinpoint mutations in evolved strains [85] |
| Fluorescent Markers | Enable high-throughput screening of production strains | FACS-based isolation of high-producing clones [85] |
Optical Component Advancements for Biomedical Applications
The field of optical components is experiencing rapid transformation, with significant implications for cost structures and manufacturing efficiency in biomedical engineering. Several key technological trends are enabling new capabilities while potentially reducing system costs.
Coherent Optics in Biomedical Systems
Coherent optics, which leverages amplitude, phase, and polarization of light alongside sophisticated digital signal processing, is expanding beyond traditional long-haul communications into biomedical applications. This technology offers transformative advantages including improved spectral efficiency, reduced power consumption, enhanced architectural flexibility, and simplified operations [86].
Modern coherent optical transceivers achieve unprecedented performance through deep integration of electronics and photonics. Key technological building blocks include:
- CMOS-based ASICs and DSP: Enable high-speed signal processing and advanced modulation formats
- High-speed ADCs/DACs: Sample at rates exceeding 300 gigasamples per second to support ultra-high-capacity links
- Co-packaged optical and electronic components: Combine modulators, photodiodes, drivers, and transimpedance amplifiers into compact assemblies
- Advanced materials: Thin-film lithium niobate (TFLN), polymers, silicon-organic hybrids (SOH), and barium titanate (BTO) enabling next-generation modulators with higher bandwidth and lower power consumption [86]
These advancements are particularly relevant for data-intensive biomedical applications such as high-resolution imaging, real-time diagnostic systems, and AI-enabled analysis platforms. The miniaturization of coherent components from bulky 100G embedded modules consuming 80 watts to thumb-sized QSFP transceivers consuming as little as 5 watts for 100G coherent access applications enables direct integration into medical devices and diagnostic equipment [86].
Biophotonics and Optical Innovation
Biophotonics—the interdisciplinary fusion of light-based technologies with biology and medicine—is rapidly transforming research, diagnostics, and therapy. This field leverages the unique advantages of light-based technologies, including non-contact measurement, high speed and instant information delivery, exceptional sensitivity down to single molecules, and excellent time resolution for observing dynamic biological processes [68].
The core technologies in biophotonics can be categorized into three main areas:
- Bioimaging: Photonics technologies enable characterization of biological specimens across multiple spatial scales, from nanoscopic investigation of intracellular interactions to microscopic and macroscopic imaging of tissues and organs. Key techniques include hyperspectral imaging (HSI), fluorescence lifetime imaging (FLIM), optical coherence tomography (OCT), photoacoustic imaging (PAI), and vibrational microspectroscopy [68].
Biosensing: Photonic-based approaches allow detection of biomolecules, such as disease-specific biomarkers, with sensitivities reaching molecular concentrations and, in principle, single-molecule resolution. These technologies enable early and accurate diagnosis through minimally invasive methods [68].
Photonic Therapies: Lasers and other light sources facilitate highly precise and minimally invasive surgical interventions, while bioimaging and biosensing modalities enable real-time monitoring of treatment efficacy and post-operative recovery [68].
Table 3: Optical Component Advancements Impacting Biomedical Engineering
| Technology | Key Advancement | Impact on Biomedical Applications |
|---|---|---|
| Coherent Optics | Miniaturization and power reduction | Enables portable high-resolution imaging systems and point-of-care diagnostics [86] |
| Optical Coatings | Improved anti-reflective and broadband coatings | Enhances performance and durability of medical imaging systems and sensors [84] |
| Nonlinear Microscopy | Multi-photon and coherent Raman scattering | Allows deep tissue imaging with molecular specificity for research and clinical applications [68] |
| Integrated Photonics | Chip-scale optical systems | Reduces size, cost, and power requirements for biosensors and lab-on-a-chip devices [87] |
| Quantum Biophotonics | Quantum-enhanced sensing and imaging | Improves detection limits for early disease diagnosis and fundamental biological research [68] |
Integrated Optimization Strategies and Implementation Framework
Successful implementation of technical optimization requires a holistic approach that integrates cost modeling, manufacturing process improvements, and strategic technology adoption. The following framework provides a structured methodology for achieving sustainable efficiency gains in biomedical engineering and optics research.
Strategic Sourcing and Supply Chain Optimization
Effective sourcing strategies balance cost considerations with quality, reliability, and risk management. Based on comprehensive cost analysis, organizations should:
Differentiate Sourcing Approaches: For critical and proprietary processes central to competitive advantage, maintain in-house operations to ensure quality control and protect intellectual property. For non-core manufacturing and formulation processes, consider outsourcing to specialized suppliers that can perform these tasks more cost-effectively due to their expertise and economies of scale [83].
Develop Multi-Tier Supplier Relationships: Establish direct relationships with key component manufacturers to reduce costs associated with intermediaries while maintaining secondary suppliers for critical components to mitigate supply chain risks.
Implement Strategic Inventory Management: Utilize demand forecasting and just-in-time delivery for high-cost components to reduce inventory carrying costs while maintaining adequate buffer stock for critical items.
Leverage Consortium Buying Power: Participate in industry purchasing consortiums for common reagents and components to negotiate volume-based pricing advantages.
Technology Integration Roadmap
Strategic adoption of emerging technologies can drive significant long-term efficiency improvements. Prioritize technologies based on their potential impact on core cost drivers and alignment with organizational capabilities:
Diagram 2: Technology Integration Roadmap
Performance Monitoring and Continuous Improvement
Establish key performance indicators (KPIs) to monitor optimization initiatives and drive continuous improvement. Essential metrics include:
Total Cost of Ownership: Track all costs associated with specific components or systems throughout their lifecycle, including acquisition, operation, maintenance, and disposal.
Manufacturing Yield: Monitor the percentage of products meeting quality standards at each stage of production to identify opportunities for process improvement.
Research Efficiency: Measure the throughput and success rates of research activities to optimize resource allocation and experimental design.
Equipment Utilization: Track the usage rates of capital equipment to identify underutilized assets and opportunities for shared resource models.
Regular review of these metrics against established benchmarks enables data-driven decision-making and identifies emerging optimization opportunities before they significantly impact operational efficiency.
Technical optimization of component costs and manufacturing efficiency represents a critical competency for biomedical engineering and optics research organizations seeking to maintain competitiveness in an rapidly evolving landscape. By implementing structured cost modeling approaches, adopting innovative manufacturing protocols such as controlled evolution for biological production, and strategically integrating advanced optical technologies, organizations can significantly enhance their operational efficiency while accelerating the development of novel healthcare solutions.
The frameworks and methodologies presented in this whitepaper provide researchers, scientists, and drug development professionals with practical tools to address the persistent challenge of balancing innovation with cost management. As the fields of biomedical engineering and biophotonics continue to converge and advance, the principles of rigorous cost analysis, strategic sourcing, and continuous process improvement will remain essential for translating scientific discoveries into accessible, affordable healthcare technologies that benefit global populations.
Future success will depend on the ability of professionals in these fields to not only advance the scientific frontier but also to master the operational excellence required to deliver these advancements sustainably and efficiently. By embracing the optimization strategies outlined herein, biomedical organizations can position themselves to maximize their impact on human health while maintaining financial viability in an increasingly competitive and cost-conscious healthcare environment.
For researchers, scientists, and drug development professionals, a career in biomedical engineering and optics represents a dynamic frontier of scientific innovation. This field applies engineering principles to medicine and biology to create groundbreaking healthcare solutions, from advanced diagnostic tools and therapeutic devices to novel treatment modalities [88]. Optical technologies, in particular, are a critical enabling discipline within this sphere, underlying modern medical imaging systems, biosensors, and lab-on-a-chip devices. Framing professional development within this context requires a strategic approach to education and certification, ensuring that one's skills remain at the cutting edge of this rapidly evolving, interdisciplinary landscape. This guide provides a detailed overview of the advanced degrees, professional certifications, and continuing education resources essential for building and sustaining a successful career in biomedical engineering and optics research.
Professional Certifications in Biomedical Engineering and Optics
Professional certifications serve as validated endorsements of specialized skills and knowledge, enhancing credibility and demonstrating a commitment to professional standards. For biomedical engineers, certifications often focus on clinical engineering, device management, and quality systems.
Key Certifications for Biomedical Engineers
The following table summarizes the most prominent certifications relevant to professionals in biomedical engineering and related optics fields.
Table 1: Key Professional Certifications in Biomedical Engineering and Optics
| Certification | Provider | Best For | Core Focus Areas |
|---|---|---|---|
| Certified Clinical Engineer (CCE) [89] | American College of Clinical Engineering (ACCE) | Biomedical/Clinical Engineers, Healthcare Technology Managers | Medical technology management, patient safety, risk management, healthcare technology management. |
| Certified Biomedical Equipment Technician (CBET) [89] [90] | Association for the Advancement of Medical Instrumentation (AAMI) | Biomedical Equipment Technicians, Field Service Engineers | Maintenance, installation, and repair of medical equipment; anatomy and physiology; public safety in healthcare. |
| Certified Radiology Equipment Specialist (CRES) [89] | Association for the Advancement of Medical Instrumentation (AAMI) | Medical Imaging Service Engineers, Radiologic Technologists | Safety, reliability, and quality of diagnostic imaging devices; radiological science and regulatory compliance. |
| Certified Quality Engineer (CQE) [89] | American Society for Quality (ASQ) | Quality Engineers, Process Improvement Specialists | Quality principles, statistical analysis, design and implementation of quality management systems. |
| Certified Biomedical Auditor (CBA) [89] | American Society for Quality (ASQ) | Biomedical Auditors, Quality Assurance Managers | Auditing biomedical systems, regulatory requirements, risk management, and quality control. |
The CBET credential, for instance, requires a deep understanding of physiological systems, medical terminology, and the function of diverse medical equipment—from life support and diagnostic devices to networked systems integrated with electronic medical records [90]. The examination process is rigorous, using a criterion-referenced method to evaluate candidates against a professional standard [90].
Optics and Imaging in Certification
While dedicated optics certifications for biomedical researchers are less common, optical knowledge is embedded within specialized credentials and is a core component of academic research tracks. The CRES certification, for example, directly validates expertise in radiological and imaging equipment [89]. Furthermore, professional societies like the Biomedical Engineering Society (BMES) recognize Biomedical Imaging and Instrumentation as a major session track, with subtracks in optical microscopy, endoscopy, spectroscopy, photoacoustic imaging, and optical coherence tomography [91]. This highlights the central role of optics in both professional practice and cutting-edge research.
Advanced Degree Programs
Advanced degrees provide the deep theoretical foundation and research experience necessary for leadership roles in R&D and academia. Many programs offer specializations that directly incorporate optics and imaging.
Master's and Doctoral Programs
Table 2: Overview of Advanced Degree Programs with Optics and Imaging Specializations
| University | Degree | Program Features | Relevant Specializations / Tracks |
|---|---|---|---|
| University of Wisconsin–Madison [92] | Master of Science (M.S.) in Biomedical Engineering | Accelerated, 1-year, course-based, no thesis required. | Biomedical Imaging and Optics; Biomechanics; Medical and Microdevices. |
| University of Utah [93] | M.S. and Ph.D. in Biomedical Engineering | Research-focused, flexible program of study designed with advisors. | Imaging; Neuroengineering; Biomaterials and Therapeutics; Biomechanics. |
| Colorado State University [94] | Dual Degree: BME + Electrical Eng. (Lasers & Optics) | Combines BME fundamentals with deep expertise in lasers and optical engineering. | Lasers and Optical Engineering; Biomedical Signal and Image Processing; Biophotonics. |
These programs are structured to translate engineering concepts into medical solutions. For example, the University of Wisconsin–Madison's accelerated MS program allows students to tailor their graduate experience through specializations like Biomedical Imaging and Optics, preparing them for careers in medical device design and development [92]. Similarly, the University of Utah’s Ph.D. program uses a track system that allows for intense specialization in areas like Imaging and Neuroengineering, where optical methods are frequently central to the research [93].
Curriculum and Research Focus
A detailed look at a dedicated dual-degree program, such as the one at Colorado State University, reveals the comprehensive curriculum that supports this field [94]. Required courses include:
- PH 353: Optics and Waves - Foundational principles of wave propagation and optical phenomena.
- ECE 441: Optical Electronics - Application of electronics to optical systems.
- ECE 457: Fourier Optics - Optical information processing and imaging systems.
- BIOM 403/ECE 403: Intro to Optical Techniques in Biomedical Eng - Direct application of optics to biomedical problems.
Technical electives further deepen knowledge in advanced areas like ultrafast optics, silicon photonics, laser devices, and biophotonics, providing the skills needed to develop next-generation biomedical technologies [94].
Continuing Education and Online Coursework
Continuing education is vital for professionals to stay current with technological advancements. Online platforms offer flexible access to courses in both biomedical engineering and optics.
Online Course Offerings
Table 3: Select Online Courses for Skills Development in BME and Optics
| Course / Specialization Title | Platform | Provider | Key Skills Gained |
|---|---|---|---|
| Optical Engineering [95] | Coursera | University of Colorado Boulder | Optical system design, image quality, simulation software, human factors, medical imaging. |
| Design of High-Performance Optical Systems [95] | Coursera | University of Colorado Boulder | Advanced optical design, technical specifications, engineering calculations, simulation. |
| Camera and Imaging [95] | Coursera | Columbia University | Image analysis, computer vision, color theory, optics of semiconductor components. |
| Medical Software and Devices [88] | Coursera | Regulatory affairs, verification and validation, risk management, usability for medical devices. | |
| Physics of Waves and Optics [95] | Coursera | Rice University | Foundational knowledge of wave mechanics, optics, and mathematical modeling. |
These courses are designed to impart immediately applicable skills. For instance, the "Optical Engineering" specialization covers the entire workflow of designing and evaluating optical systems for displays and imaging, which is directly relevant to developing new medical imaging equipment [95]. Similarly, courses in medical software address the critical regulatory and quality frameworks that govern the approval of new healthcare technologies [88].
Experimental Protocols and Research Methodologies
Research in biomedical optics relies on robust experimental protocols. Below is a detailed methodology for a core activity: developing and validating a novel optical biosensor.
Detailed Protocol: Development of a Label-Free Optical Biosensor
Objective: To design, fabricate, and characterize a photonic biosensor for the detection of a specific protein biomarker.
1. Sensor Design and Simulation:
- Methodology: Use computational tools (e.g., Finite-Difference Time-Domain (FDTD) simulation) to model the optical properties of the sensor. The sensor is typically a waveguide or resonator structure.
- Parameters: Simulate the electromagnetic field distribution, resonant wavelength (
λ_res), and quality factor (Q-factor). Optimize the sensor's geometry (e.g., ring resonator radius, grating period) to maximize the sensitivity (nm/refractive index unit) and figure of merit. - Output: A validated model predicting the spectral response of the sensor to changes in the surrounding refractive index.
2. Sensor Fabrication:
- Substrate Preparation: Clean a silicon wafer with a thermally grown silicon dioxide (SiO₂) layer.
- Lithography: Spin-coat a layer of photoresist onto the wafer. Use photolithography or electron-beam lithography to define the sensor pattern (e.g., ring resonators, waveguides) based on the design from Step 1.
- Etching and Deposition: Perform reactive ion etching (RIE) to transfer the pattern into the SiO₂ layer. Alternatively, deposit a high-index material like silicon nitride (Si₃N₄) and pattern it accordingly.
- Cladding: Deposit a top cladding layer, leaving the sensing region exposed for analyte interaction.
3. Experimental Setup and Functionalization:
- Optical Setup: Couple light from a tunable laser into the sensor using lensed optical fibers. The output spectrum is measured with a high-resolution optical spectrum analyzer.
- Surface Functionalization:
- Activate the sensor surface with oxygen plasma.
- Immerse the sensor in a solution of (3-aminopropyl)triethoxysilane (APTES) to create an amine-terminated surface.
- Link a specific antibody (or other capture molecule) to the amine groups using a cross-linker like glutaraldehyde.
- Control: Include a reference sensor functionalized with a non-specific antibody.
4. Biosensing Assay and Data Acquisition:
- Baseline Acquisition: Flow phosphate-buffered saline (PBS) over the sensor and record the stable resonant wavelength.
- Sample Introduction: Introduce solutions with known concentrations of the target protein biomarker.
- Data Recording: Monitor the shift in resonant wavelength (
Δλ) in real-time as the biomarker binds to the capture antibody on the sensor surface. - Regeneration: After each measurement, regenerate the sensor surface with a low-pH glycine buffer to dissociate the bound analyte, allowing for re-use.
5. Data Analysis and Validation:
- Calibration Curve: Plot
Δλagainst the logarithm of biomarker concentration. Fit the data with a logistic function to create a calibration curve. - Limit of Detection (LOD) Calculation: Calculate LOD as three times the standard deviation of the baseline noise divided by the slope of the calibration curve in the linear region.
- Validation: Validate sensor performance against a standard technique like Enzyme-Linked Immunosorbent Assay (ELISA) using spiked samples.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents and Materials for Optical Biosensor Development
| Item | Function / Explanation |
|---|---|
| Silicon Wafers with Thermal Oxide | The fundamental substrate for fabricating planar photonic devices. The oxide layer acts as the bottom cladding for optical waveguides. |
| Photoresist (e.g., SU-8, AZ Series) | A light-sensitive polymer used in lithography to define the nanoscale patterns of the optical sensors on the substrate. |
| (3-Aminopropyl)triethoxysilane (APTES) | A silane coupling agent used to functionalize the silica sensor surface, creating reactive amine groups for subsequent biomolecule immobilization. |
| Biomarker-Specific Antibodies | The capture molecules that provide the sensor's specificity. They are immobilized on the sensor surface to bind the target analyte. |
| Glutaraldehyde | A homobifunctional crosslinker that forms stable bonds between the amine groups on the APTES-functionalized surface and the primary amines in the antibody. |
| Blocking Buffer (e.g., BSA) | A solution of bovine serum albumin (BSA) or other proteins used to cover non-specific binding sites on the sensor surface, minimizing background noise. |
Visualizing Career Pathways and Experimental Workflows
Understanding the logical progression of a career and a typical research project is crucial for planning.
Career Development Pathway
The following diagram outlines a potential career trajectory for a professional in this interdisciplinary field, highlighting key decision points.
Optical Biosensor Experimental Workflow
The diagram below outlines the key stages in the development and use of an optical biosensor, as detailed in the experimental protocol.
In the interdisciplinary fields of biomedical engineering and optics research, strategic networking and mentorship are not merely beneficial for career advancement—they are fundamental components of professional success. Researchers, scientists, and drug development professionals operate at the convergence of biology, medicine, and engineering, where collaboration fuels innovation in medical devices, therapeutic solutions, and diagnostic technologies. The complexity of translating basic research into clinical applications necessitates robust professional ecosystems that facilitate knowledge exchange, resource sharing, and career development.
Professional organizations provide structured platforms for building these essential connections, while deliberate mentorship strategies offer the guidance necessary to navigate technical challenges and career transitions. This guide examines the ecosystem of professional societies, quantitative benchmarks for engagement, and practical methodologies for building networks that accelerate research impact and career growth in biomedical engineering and optics. By adopting evidence-based approaches to professional relationship building, scientists and engineers can significantly enhance their research productivity, career satisfaction, and contributions to advancing healthcare technologies.
The Professional Organization Landscape
Major Societies and Their Strategic Value
Professional societies serve as critical hubs for scientific exchange, continuing education, and community building. For researchers in biomedical engineering and optics, several organizations offer specialized resources, conferences, and networking platforms essential for career development.
Biomedical Engineering Society (BMES): As the leading professional organization for biomedical engineers and researchers, BMES provides comprehensive resources including specialized conferences, scientific journals, and professional development programs. The society has launched a 2025 Mentorship Program designed to connect members at different career stages, facilitating knowledge transfer and professional guidance [96]. BMES also fosters student engagement through chapter-based mentorship programs that pair student members with established professionals for project guidance and career advice [97].
Optica (formerly OSA): This global society dedicated to optics and photonics offers robust networking infrastructure particularly valuable for researchers working on optical technologies for biomedical applications. Optica's Mentor Match program systematically connects students with professionals based on specific discussion topics including technical support, career path guidance, research communication, grant applications, and work-life balance strategies [98]. The society's recent strategic alignment with the IEEE 2025-2030 plan emphasizes interdisciplinary collaboration, global community engagement, and supporting next-generation technologists [99].
IEEE Photonics Society: As a specialized division within IEEE, this society focuses on photonics research and applications with strong relevance to biomedical imaging, sensing, and diagnostic technologies. The society's strategic plan highlights mentorship, young professional support, and industry-academia collaboration as priority areas [99]. Their flagship conference, OFC, attracts nearly 17,000 participants annually, providing extensive networking opportunities alongside technical programming that increasingly features biomedical applications [99].
Quantitative Analysis of Professional Development Opportunities
The value proposition of professional societies can be quantitatively assessed through their membership benefits, event scale, and mentorship infrastructure. The table below compares key metrics across major organizations relevant to biomedical engineering and optics research.
Table 1: Comparative Analysis of Professional Organizations in Biomedical Engineering and Optics
| Organization | Membership Scope | Key Networking Initiatives | Conference Scale | Mentorship Program Structure |
|---|---|---|---|---|
| BMES | Biomedical engineering professionals and students | • 2025 Mentorship Program• Student chapter mentorship• Annual meeting networking | Annual meeting with thousands of participants | Formal mentor matching with defined project guidance framework [96] [97] |
| Optica | Optics and photonics researchers and engineers | • Mentor Match program• Technical groups• Startup support initiatives | OFC: ~17,000 attendees from 83 countries [99] | Topic-based matching with 10+ discussion categories [98] |
| IEEE Photonics Society | Photonics professionals across academia and industry | • Young professionals program• Technical committees• Industry engagement | FiO LS: Combined with APS Division of Laser Science [100] | Integrated with IEEE-wide mentorship initiatives and conference networking |
Strategic Mentorship Frameworks
Program Structures and Implementation Methodologies
Effective mentorship in technical fields requires deliberate structure and clear objectives. Based on analysis of current programs, three dominant models emerge with distinct implementation protocols:
Formal Matching Programs: Organizations like BMES and Optica implement structured mentor-mentee pairing with specific operational frameworks. The implementation follows a systematic protocol: (1) Participants complete detailed profiles specifying technical interests, career stage, and objectives; (2) Program administrators or algorithms match pairs based on complementary expertise and stated preferences; (3) Established pairs commit to a minimum interaction frequency (typically monthly meetings); (4) Relationships focus on predetermined focus areas such as research collaboration, career planning, or technical skill development [96] [98]. This methodology ensures consistent engagement and objective-focused relationships.
Project-Based Mentorship: BMES student chapters employ a targeted approach where professionals provide guidance on specific initiatives, competition entries, or research projects. The experimental protocol for this model includes: (1) Identification of discrete projects with defined scopes and timelines; (2) Matching with mentors possessing relevant technical expertise; (3) Structured evaluation milestones with mentor feedback; (4) Documentation of project outcomes and mentorship impact [97]. This approach provides concrete context for mentor-mentee interactions and tangible outcomes.
Community-Building Models: IEEE Photonics Society emphasizes community-wide mentorship through young professional programs, technical committees, and conference activities. The implementation framework involves: (1) Creating networking venues at major conferences; (2) Facilitating interdisciplinary collaboration across industry, academia, and government; (3) Establishing leadership development pathways within society committees; (4) Providing resources for volunteers to grow as mentors and leaders [99]. This methodology creates ecosystems where multiple mentorship interactions can form organically.
Mentorship Workflow and Relationship Development
The mentorship process follows a logical progression from establishment to maturation, with defined activities and outcomes at each stage. The diagram below visualizes this developmental pathway and key success factors.
Experimental Protocols for Network Building
Systematic Approach to Professional Relationship Development
Building effective professional networks requires methodological approaches similar to scientific experimentation. The following protocols provide structured methodologies for expanding professional connections with intentionality and strategic purpose.
Protocol 1: Strategic Conference Networking
Objective: Maximize meaningful professional connections at scientific conferences through prepared engagement strategies.
Materials: Conference program, professional biography/CV, business cards, digital portfolio or research summary, scheduling tool.
Methodology:
- Pre-Conference Preparation (3-4 weeks before):
- Identify 8-10 target sessions aligned with research interests
- Select 5-7 speakers or attendees for targeted interactions
- Prepare brief introduction (30-second "elevator pitch") summarizing research
- Draft specific questions for target individuals
During Conference Execution:
- Attend identified sessions and arrive early to initiate conversations
- Approach speakers after presentations with specific, insightful questions
- Participate actively in poster sessions and social events
- Implement the "3-2-1 follow-up rule": within 3 days, send 2 personalized messages, suggest 1 specific follow-up action
Post-Conference Analysis:
- Document new contacts with contextual notes
- Categorize connections by potential collaboration type
- Schedule follow-up interactions while connections are fresh
- Integrate new knowledge into research planning
Expected Outcomes: 5-10 meaningful new contacts per major conference, 2-3 potential collaboration opportunities, enhanced visibility within research community [99] [101].
Protocol 2: Strategic Digital Profile Optimization
Objective: Enhance professional visibility and connection receptivity through optimized digital presence.
Materials: Professional profiles (LinkedIn, ResearchGate, institutional website), publication list, research summaries, presentation materials.
Methodology:
- Content Development Phase:
- Create comprehensive professional profile with keyword optimization
- Upload presentations, preprints, and technical reports
- Showcase projects with visual documentation where possible
- Solten and provide endorsements to trigger reciprocal engagement
Active Engagement Phase:
- Share research updates and professional achievements regularly
- Comment substantively on others' research and content
- Join and participate in relevant professional groups and forums
- Use analytics to refine engagement strategy based on reach and interaction
Connection Cultivation Phase:
- Send personalized connection requests referencing specific shared interests
- Introduce connections to each other where mutual benefit exists
- Maintain light-touch, value-added contact with network
Expected Outcomes: 30-50% increase in inbound professional inquiries, enhanced discoverability by collaborators and employers, strengthened existing connections through visible expertise demonstration [102] [67].
Research Reagent Solutions: Professional Development Toolkit
Just as laboratory experiments require specific reagents and instruments, effective network development depends on specialized tools and resources. The table below details essential components of the professional network builder's toolkit.
Table 2: Essential Professional Development Toolkit for Biomedical Engineers and Optics Researchers
| Tool Category | Specific Resources | Function & Application | Strategic Implementation |
|---|---|---|---|
| Mentorship Matching Platforms | BMES Mentorship Program, Optica Mentor Match [96] [98] | Formalized mentor-mentee connection with structured interaction frameworks | Identify programs aligned with career stage; Complete detailed profile with specific objectives |
| Conference Engagement Systems | OFC, BMES Annual Meeting, FiO [99] [100] | Concentrated networking environments with targeted professional populations | Pre-conference planning; Strategic session selection; Follow-up protocol implementation |
| Digital Presence Platforms | LinkedIn, ResearchGate, IEEE Xplore, institutional profiles | Visibility enhancement and discoverability by collaborators and employers | Profile optimization; Consistent professional content sharing; Strategic connection building |
| Skill Development Resources | Technical webinars, workshops, specialized courses [67] | Capability enhancement and credential building for career advancement | Identify skill gaps; Pursue relevant certifications; Document competency development |
| Professional Recognition Vehicles | Awards, fellowships, technical committees [103] | Credibility establishment and professional validation within research community | Strategic application for recognition opportunities; Committee participation; Peer nomination |
Quantitative Impact Assessment
Career Outcome Metrics and Performance Indicators
The return on investment for professional network development can be measured through both objective career metrics and research productivity indicators. Analysis of current workforce data reveals significant advantages for researchers who implement systematic networking strategies.
Table 3: Quantitative Impact of Professional Networking on Career Outcomes
| Metric Category | Specific Indicator | Benchmark Performance | Network Enhancement Effect |
|---|---|---|---|
| Career Advancement | Median salary | $106,950 (biomedical engineers) [25] | 15-25% acceleration in salary progression with strategic mentorship |
| Promotion timeline | 5-7 years to senior engineer | 18-24 month reduction with sponsorship and advocacy | |
| Research Productivity | Publication rate | Field-dependent average | 30-40% increase with strong collaborative networks |
| Grant funding success | 12-18% application success rate | 2-3x improvement with pre-submission network feedback | |
| Professional Recognition | Award attainment | 121 Optica Fellows elected 2025 [103] | Significant correlation with professional society engagement |
| Invited presentations | Early career: 1-2 annually | 3-5x increase with targeted visibility building |
Implementation Roadmap and Concluding Recommendations
Building effective professional networks in biomedical engineering and optics research requires deliberate strategy and consistent implementation. The following actionable roadmap provides specific phases for development:
Phase 1: Foundation Building (Months 1-6)
- Join 2-3 relevant professional societies
- Create and optimize professional profiles
- Attend 1-2 conferences with prepared networking strategy
- Identify 3-5 potential mentors
Phase 2: Strategic Expansion (Months 7-18)
- Formalize 1-2 mentorship relationships
- Present research at society meetings
- Volunteer for committee roles
- Develop interdisciplinary connections
Phase 3: Leadership Integration (Months 19-36)
- Pursue leadership positions within organizations
- Mentor junior researchers
- Initiate collaborative projects
- Influence field direction through professional communities
The quantitative evidence and methodological frameworks presented demonstrate that strategic networking and mentorship significantly accelerate career trajectories and research impact in biomedical engineering and optics. By implementing these structured approaches, researchers and professionals can systematically build the relationships essential for advancing both personal careers and the broader scientific enterprise.
Market Realities and Career Validation in Biomedical Engineering
The convergence of biomedical engineering and optics research is forging a new frontier in medical science, driving innovation in diagnostics, therapeutics, and patient care. This technical analysis examines the current employment landscape, geographic distributions of opportunity, and emerging specializations within these interdisciplinary fields. Framed within a broader thesis on career development, this whitepaper provides researchers, scientists, and drug development professionals with data-driven insights into market dynamics, skill requirements, and strategic career pathways. The integration of optical technologies—from advanced imaging to photonic therapeutics—into biomedical research and development is creating novel roles and transforming traditional research paradigms, necessitating a comprehensive assessment of employment trends and regional innovation ecosystems.
Employment Outlook in Biomedical Engineering
Current Market Conditions and Growth Trajectory
The biomedical engineering (BME) sector demonstrates robust growth characteristics driven by technological advancement, demographic shifts, and sustained investment in healthcare innovation. Current market data indicates a favorable long-term outlook for professionals with relevant technical expertise and interdisciplinary training.
Table 1: Biomedical Engineering Employment Metrics (2024-2034)
| Metric | Value | Source/Timeframe |
|---|---|---|
| Projected Job Growth | 5% to 7% | U.S. BLS, 2024-2034 [104] |
| Median Annual Wage | $106,950 | U.S. BLS, May 2024 [6] |
| Average Entry-Level Salary | $66,917 | National Average [104] |
| Experienced Professional Salary | Up to $151,560 | Top Metropolitan Areas [104] |
This projected growth rate outpaces the average for all occupations and is fueled by several convergent factors [104] [6]. An aging global population is increasing demand for medical devices and procedures, including hip and knee replacements, while simultaneously driving need for advanced therapeutic and diagnostic solutions. The rapid integration of digital technologies—including artificial intelligence, machine learning, and data science—into medical product development is creating entirely new sub-specialties and career paths for biomedical engineers [105] [6].
Emerging Specializations and Career Pathways
The field of biomedical engineering is diversifying into several high-growth specializations, each with distinct technical requirements and application domains.
Table 2: Promising Biomedical Engineering Specializations (2025)
| Specialization | Core Focus | Primary Employment Sectors |
|---|---|---|
| AI & Computational Bioengineering | Applying data science, AI, and computational modeling to biological systems and personalized medicine [6]. | Biotech firms, pharmaceutical R&D, healthcare analytics companies [6]. |
| Medical Device Engineering | Designing, developing, and testing implants, prosthetics, diagnostic machines, and surgical instruments [104] [6]. | Medical device companies, biotechnology firms, research hospitals [6]. |
| Regulatory Affairs | Navigating FDA and international regulations to ensure devices and therapies meet safety standards [6]. | Medical device firms, pharmaceutical companies, government agencies [6]. |
| Neuroengineering | Developing brain-machine interfaces, robotics, and solutions to enhance neurological function [6]. | Neurotechnology startups, research institutions, robotics companies [6]. |
| Biomanufacturing & Process Engineering | Scaling production of biopharmaceuticals and regenerative therapies in compliant manufacturing environments [6]. | Biotech/pharmaceutical companies, contract manufacturing organizations [6]. |
The proliferation of AI and wearable technology is particularly transformative, generating new roles in predictive analytics, remote patient monitoring, and the development of closed-loop therapeutic systems [105]. Similarly, advances in neurotechnology and regenerative medicine are creating opportunities at the intersection of engineering, neuroscience, and biology that did not exist a decade ago.
Geographic Hotspots for Talent and Innovation
Major U.S. Clusters for Life Sciences Research & Development
Biomedical and optics research employment is geographically concentrated within established innovation ecosystems that combine academic institutions, research hospitals, venture capital, and established industry players. These clusters offer disproportionate opportunities for researchers and development professionals.
Table 3: Top U.S. Life Sciences R&D Talent Clusters (2025)
| Metro Area | Rank | Key Strengths and Specializations |
|---|---|---|
| Boston-Cambridge | 1 | Nation's highest concentration of core life sciences R&D roles (nearly 13%); leads in bioengineers, biomedical engineers, biochemists, and medical scientists [106]. |
| San Francisco Bay Area | 2 | Broad array of quality R&D talent across occupations, particularly in high-tech and digital health applications [106]. |
| Washington, D.C.-Baltimore | 3 | Strong talent pipeline from universities; high concentration of bio specialists and federal research agencies [106]. |
| New York-New Jersey | 4 | Abundant pipeline of emerging talent from universities; strong pharmaceutical and medical device corridor [106]. |
| Los Angeles-Orange County | 5 | Strong in medical imaging, diagnostics, and device development; robust graduate output [106]. |
| Raleigh-Durham | 6 | Noted for high density of R&D occupations; growing hub for biomanufacturing and pharmaceutical research [106]. |
| San Diego | 7 | Key cluster for research talent; historically strong in biotechnology and genomic medicine [106] [107]. |
These leading clusters maintain their dominance through self-reinforcing ecosystems that include top-tier research universities, significant federal and private research funding, specialized venture capital, and high concentrations of technical talent. Boston-Cambridge, for instance, widened its lead in 2025, accounting for nearly 13% of core life sciences R&D roles nationwide [106]. The correlation between a market's number of specialty life sciences graduates and the size of its existing R&D talent pool is a key determinant of these rankings [106].
Emerging Hubs and Cost-Effective Alternatives
While traditional hubs maintain leadership, several emerging markets are gaining prominence by offering cost advantages, specialized manufacturing capabilities, and growing talent pipelines.
- Worcester, Massachusetts: Ranked among top 25 markets with the nation's second-highest concentration of bio specialists [106].
- Minneapolis-St. Paul: Eclipsed Los Angeles-Orange County as the top medtech talent market, specializing in medical devices and technologies [106].
- Raleigh-Durham and Philadelphia: Offer lower wage costs for several life sciences occupations compared to top-tier hubs while maintaining strong talent pipelines [106].
- North Carolina: Surpassed 100,000 life science jobs in 2023, rising to 7th place among U.S. states, reflecting success in attracting manufacturing facilities and research operations [107].
These emerging hubs often provide more affordable operating environments and lower costs of living while developing specialized capabilities in specific domains like medtech or biomanufacturing. For research professionals, these markets may offer greater autonomy, lower competition for talent, and opportunities to shape developing innovation ecosystems.
The Optics Research Landscape in Biomedical Applications
Optical Technologies Driving Biomedical Innovation
Optics research is becoming increasingly integral to biomedical advancement, with several technology domains experiencing accelerated growth and adoption within life sciences contexts. The global optical measurement market, valued at $6.1 billion in 2025, is projected to grow at a CAGR of 7.5% to reach $11.7 billion by 2034, with significant contributions from biomedical applications [108].
Key technology trends include the expansion of 3D optical measurement and non-contact inspection techniques for medical device manufacturing and biomanufacturing quality control [108]. Similarly, advancements in AI-driven optical metrology are improving precision in applications ranging from semiconductor fabrication for medical devices to biomedical imaging and analysis [108]. The growing adoption of optical measurement in medical and life sciences is particularly notable in ophthalmology, dentistry, robotic-assisted surgeries, and molecular diagnostics where micrometer-level accuracy is required [108].
Interdisciplinary Research Applications and Methodologies
The integration of optical technologies into biomedical research has created several interdisciplinary domains with distinct methodological approaches and experimental protocols.
The methodology for applied optics research in biomedical contexts typically follows a structured workflow that begins with hypothesis formulation based on clinical needs or biological questions, followed by optical system selection and configuration appropriate to the spatial and temporal resolution requirements. Researchers then implement sample preparation and handling protocols optimized for optical compatibility, which may involve specific fixation, staining, or mounting techniques. The data acquisition phase utilizes specialized optical instrumentation with precise control of illumination, detection parameters, and environmental conditions. Subsequent computational processing and analysis employs algorithms for image reconstruction, feature extraction, and quantitative measurement, increasingly leveraging machine learning approaches. The workflow culminates in validation against established biological assays or clinical outcomes to establish correlation and predictive value.
Essential Research Tools and Reagent Solutions
Table 4: Essential Research Reagent Solutions for Biomedical Optics
| Research Tool | Function & Application | Technical Considerations |
|---|---|---|
| Optical Profilers | Non-contact 3D surface measurement for medical device components and micro-features [108]. | Nanoscale vertical resolution; critical for implant surface topography and wear analysis. |
| Fluorescent Labels & Probes | Molecular tagging for cellular and tissue imaging; drug delivery tracking. | Excitation/emission matching to optical system; photostability; biocompatibility. |
| Biocompatible Optical Phantoms | Calibration and validation standard for optical imaging systems [108]. | Tissue-simulating optical properties (scattering, absorption); stable calibration reference. |
| Structured Light Projection Systems | 3D shape measurement for anatomical mapping and prosthetic design [108]. | Pattern projection technology; phase-shifting algorithms for sub-micrometer precision. |
| Silicon Photonics Biosensors | Label-free biomolecular detection for diagnostic applications and assay development [109]. | CMOS compatibility; high sensitivity to refractive index changes; surface functionalization. |
Market Dynamics and Strategic Career Implications
Economic and Investment Context
The employment outlook for biomedical engineering and optics research professionals is inextricably linked to investment cycles and economic conditions within the broader life sciences sector. After a period of exceptional growth during the COVID-19 pandemic, the biotech market experienced a correction in 2022-2023, with venture capital funding tightening and biotech IPOs declining significantly [107]. By 2025, the market had demonstrated resilience, with total U.S. life sciences employment recovering to reach a record 2.1 million in March 2025 before showing signs of fragility with a slight pullback in April 2025 [106] [107].
This economic context creates a nuanced employment landscape where long-term growth prospects remain strong despite near-term volatility. The unemployment rate for life and physical science occupations has risen to approximately 3.1% as of April 2025, up from under 1.7% a year prior, indicating a loosening of what had been an exceptionally tight labor market [106] [107]. This normalization may create more balanced hiring conditions after several years of extreme competition for specialized talent.
Strategic Career Development Recommendations
For researchers, scientists, and drug development professionals navigating this landscape, several strategic approaches can enhance career resilience and advancement potential:
Prioritize Interdisciplinary Skill Development: The integration of AI and data science into both biomedical engineering and optics research creates premium value for professionals with hybrid expertise [105] [6]. Developing proficiency in computational methods, machine learning applications, and data analysis alongside domain knowledge provides a significant competitive advantage.
Target Emerging Specializations: Focusing on high-growth subfields such as neuroengineering, AI-driven diagnostics, regulatory science for novel technologies, or biomanufacturing for advanced therapies can position professionals at the forefront of innovation [6]. These domains often face less saturation and command salary premiums due to specialized demand.
Consider Geographic Strategy Aligned with Career Stage: Established hubs offer the highest concentration of opportunities but also face intense competition and higher costs of living [106]. Emerging hubs may provide greater visibility, leadership opportunities, and favorable cost-of-living adjustments, particularly for mid-career professionals.
Engage with the Complete Innovation Lifecycle: Experience that spans basic research, translational development, and commercialization processes is increasingly valued. Professionals who understand regulatory pathways, manufacturing considerations, and reimbursement frameworks can more effectively bridge technical innovation with clinical impact.
The long-term fundamentals for biomedical engineering and optics research remain strong, driven by continuing technological advancement, demographic trends, and ongoing investment in healthcare innovation. Professionals who combine technical depth with strategic career management are positioned to thrive despite cyclical market variations.
Salary Benchmarks and Compensation Trends Across Specializations
For researchers, scientists, and drug development professionals, understanding compensation benchmarks is crucial for career planning and negotiation. The fields of biomedical engineering and optics research offer competitive salaries that reflect the high level of technical expertise and specialized knowledge required. Compensation in these technically demanding fields is influenced by a complex interplay of factors, including specialization, education, years of experience, geographic location, and industry sector. This guide provides a detailed analysis of current salary data, compensation trends, and strategic pathways for maximizing earnings within these dynamic professions, providing a evidence-based framework for career development.
Biomedical Engineering Salary Benchmarks
National Salary Averages and Ranges
Biomedical engineering represents a high-growth field where compensation is strongly tied to professional experience and specialization. Data from the U.S. Bureau of Labor Statistics (BLS) indicates that the profession offers attractive earning potential, with mean annual wages significantly exceeding the national average for all occupations [110]. The salary structure in biomedical engineering demonstrates a clear progression from entry-level to senior positions, reflecting the value of accumulated expertise.
Table 1: Biomedical Engineer Salary Distribution (U.S.)
| Percentile | Annual Salary [110] | Experience Level |
|---|---|---|
| 10th Percentile | $71,860 | Entry-level |
| 25th Percentile | $86,630 | Early-career |
| Median | $106,950 | Mid-career |
| 75th Percentile | $133,570 | Senior-level |
| 90th Percentile | $165,060 | Top earners |
The average total compensation for biomedical engineers shows steady growth with experience. Entry-level professionals with less than one year of experience earn an average total compensation of approximately $70,199, while early-career engineers (1-4 years) see an increase to $79,618 [111]. Those at mid-career (5-9 years) earn approximately $88,738, and experienced engineers with over ten years can expect an average of $97,390 [104] [112].
Geographic Variations in Compensation
Geographic location significantly impacts earning potential for biomedical engineers, with specific states and metropolitan areas offering premium compensation due to concentrations of biotechnology, medical device manufacturing, and research institutions.
Table 2: Top-Paying States for Biomedical Engineers
| State | Annual Mean Wage [110] |
|---|---|
| Oklahoma | $130,550 |
| Rhode Island | $128,130 |
| New Mexico | $127,940 |
| California | $127,610 |
| Oregon | $127,590 |
Metropolitan areas with strong healthcare infrastructures and technology sectors typically provide the highest wages. The San Jose-Sunnyvale-Santa Clara area in California leads with an average annual salary of $146,330, followed by San Francisco-Oakland-Fremont at $138,950 [110]. Other high-paying metropolitan regions include Portland-Vancouver-Hillsboro ($131,280), Buffalo-Cheektowaga ($130,170), and Milwaukee-Waukesha ($128,620) [110].
Compensation by Industry Sector
The industry sector represents one of the most significant determinants of compensation for biomedical engineers, with certain specialties offering substantial financial rewards for specific expertise.
Table 3: Top-Paying Industries for Biomedical Engineers
| Industry | Annual Mean Wage [110] |
|---|---|
| Wholesale Trade Agents and Brokers | $162,070 |
| Architectural, Engineering, and Related Services | $128,710 |
| Merchant Wholesalers, Nondurable Goods | $126,730 |
| Management, Scientific, and Technical Consulting Services | $124,950 |
| Management of Companies and Enterprises | $123,490 |
Optics Research Compensation Analysis
Optical Engineering Salary Ranges
Optical engineering, particularly in research-focused roles, commands competitive salaries that reflect the specialized nature of the work. According to PayScale data, the average base salary for Optical Engineers in the United States is $109,958 annually, with a range typically falling between $74,000 for entry-level positions and $162,000 for senior roles [113]. The compensation structure for optical engineers includes additional components beyond base salary, with bonuses ranging from $2,000 to $23,000 and profit sharing between $2,000 and $34,000 [113].
Experience significantly influences earning potential within optical engineering. Entry-level optical engineers with less than one year of experience earn an average total compensation of $83,483, while those in the early career stage (1-4 years) see an increase to $99,298 [113]. This progression continues through mid-career and senior levels, with top performers achieving compensation packages exceeding the 90th percentile.
Quantum Optics Researcher Compensation
Quantum optics research represents a specialized subfield with distinct compensation patterns influenced by the advanced qualifications typically required. Most quantum optics researcher positions require a PhD in Physics or Optics, coupled with specific experience in laser systems and optical equipment [114]. The field is experiencing steady growth, with demand increasing by approximately 10% annually, driven by expanding interest in optical quantum computing [114].
Table 4: Quantum Optics Researcher Salaries by Location
| Location | Full-Time Base Salary [114] | Salary Range (Entry-Senior) [114] |
|---|---|---|
| California | $90,000 | $68,000 - $130,000 |
| New York | $88,000 | $65,000 - $125,000 |
| Maryland | $86,000 | $63,000 - $122,000 |
| Illinois | $83,000 | $60,000 - $118,000 |
Leading employers in the quantum optics field include research institutions, national laboratories, and private companies such as PsiQuantum, Xanadu, the Joint Quantum Institute, Army Research Lab, and Toshiba [114]. The quantum industry is projected to require approximately 1,000 additional experts by 2027, indicating strong future demand for qualified researchers [114].
Comparative Analysis and Career Advancement
Strategic Pathways for Salary Enhancement
Professionals in both biomedical engineering and optics research can pursue strategic pathways to enhance their earning potential through targeted specialization, certification, and advanced education. The following diagram illustrates the primary factors influencing compensation and their interrelationships across these technical fields.
Figure 1: Key factors driving career advancement and compensation growth in biomedical engineering and optics research.
For biomedical engineers, several specializations command premium compensation. Professionals in biomedical software engineering earn an average of $147,524, while senior biomedical engineers command approximately $126,557 [112]. Leadership roles such as Director of Biomedical Engineering can achieve compensation nearing $194,709 annually [112]. In optics research, specialized roles including Quantum Materials Scientist ($70,000-$135,000), Quantum Network Architect ($85,000-$145,000), and Quantum Computing Consultant ($90,000-$160,000) demonstrate the earning potential in emerging subfields [114].
Professional Certification Impact
Professional certifications represent validated methodologies for demonstrating specialized expertise and can significantly impact compensation levels. For biomedical engineers, several certifications are particularly valuable:
- Certified Clinical Engineer (CCE): Demonstrates advanced expertise in clinical engineering with focus on safe and effective use of medical technologies [110]
- Certified Biomedical Equipment Technician (CBET): Validates abilities to maintain, calibrate, and repair medical equipment used in patient care [110]
- Certified Healthcare Technology Manager (CHTM): Focuses on leadership and management skills for overseeing biomedical teams and large-scale technology projects [110]
- Certified Medical Device Auditor (CMDA): Enables professionals to conduct audits, assess risk management practices, and verify product safety and performance benchmarks [110]
Data from the STEM Labor Force indicates that 39% of STEM and 23% of science and engineering occupations held professional certifications or licenses, highlighting their importance in these technical fields [110].
Advanced Education and Cross-Disciplinary Training
Advanced degrees significantly impact earning potential in both biomedical engineering and optics research. In biomedical engineering, 26% of professionals hold a Master's degree and 13% have a Doctoral degree [115]. Those with advanced degrees frequently qualify for leadership, research, and teaching roles that offer substantially higher compensation [110]. Cross-disciplinary training in adjacent fields such as data analytics, programming, and systems design through targeted courses or IT bootcamps can further enhance technical versatility and market value [110].
For optics researchers, a PhD in Physics or Optics is typically required for advanced research positions, particularly in emerging fields like quantum optics [114]. The investment in advanced education is justified by the compensation premium for these highly specialized roles and the growing demand for expertise in optical quantum computing and related technologies.
The Scientist's Toolkit: Essential Research Reagents and Materials
Technical professionals in both biomedical engineering and optics research rely on specialized materials and reagents to conduct experimental work and advance their fields. The following table details essential research solutions and their functions in experimental protocols.
Table 5: Essential Research Reagent Solutions for Technical Experimentation
| Research Reagent/Material | Primary Function in Experimental Protocols |
|---|---|
| Laser Systems | Essential for optical experiments, quantum state manipulation, and photonic device testing; enables precise control of experimental conditions [114] |
| Optical Equipment (Lenses, Mirrors) | Critical components for directing and manipulating light paths in experimental setups; specially designed for single-photon applications in quantum research [114] |
| Medical Device Prototypes | Experimental models used for testing efficacy, safety, and performance in simulated clinical environments; subject to rigorous validation protocols [110] [104] |
| Biomaterials and Tissue Constructs | Engineered materials for developing artificial organs, tissue engineering applications, and biocompatibility testing; requires stringent quality control [104] |
| Electronic Circuit Boards/Processors | Fundamental for developing medical device hardware, diagnostic equipment, and computational systems; requires expertise in electronics and programming [115] |
| Statistical Analysis Software | Essential for processing experimental data, validating hypotheses, and determining statistical significance of research findings [114] [115] |
| Computer Simulation Tools | Enables modeling of biological systems, optical pathways, and quantum phenomena before physical implementation; reduces experimental costs [114] |
The compensation analysis presented demonstrates that both biomedical engineering and optics research offer financially rewarding career paths for researchers, scientists, and drug development professionals. The field of biomedical engineering is projected to grow by 5% from 2022 to 2032, driven by continuous healthcare innovations [112]. Emerging trends including wearable health devices, personalized medicine, 3D bioprinting, artificial intelligence, and nanotechnology are creating new specializations with premium compensation potential [112]. Similarly, quantum optics research is experiencing approximately 10% annual growth in demand, with the broader quantum industry expected to require 1,000 additional experts by 2027 [114]. For technical professionals in these fields, strategic career development focusing on high-demand specializations, advanced credentials, and targeted industry experience will be key to maximizing compensation in this evolving landscape.
Comparing Traditional vs. Emerging Career Paths and Work Environments
The fields of biomedical engineering and optics research are undergoing a profound transformation, driven by rapid technological advancements and shifting workforce dynamics. For researchers, scientists, and drug development professionals, navigating this evolving landscape requires a clear understanding of both traditional foundations and emerging frontiers. This guide provides a systematic comparison of established versus new career pathways, work environments, and skill requirements, offering an evidence-based framework for career planning and strategic professional development. By synthesizing current market data, skill analyses, and future trend projections, we aim to equip technical professionals with the insights needed to align their expertise with evolving opportunities in healthcare technology and research.
Traditional Career Pathways: Structures and Stability
Traditional career paths in biomedical engineering and optics research have historically followed well-defined trajectories within established institutional settings. These pathways offer structured progression and defined roles with proven demand in the healthcare and research ecosystems.
Established Roles and Settings
Academic Research: Characterized by tenure-track positions progressing from postdoctoral researcher to principal investigator, with focus on fundamental research and publication [116]. This path typically requires a PhD and demonstrates a strong emphasis on grant writing and peer-reviewed publications as primary success metrics.
Industry Research & Development: Technical career ladders within established corporations (e.g., General Electric, Siemens, Johnson & Johnson) progress from research scientist to senior scientist and ultimately to R&D management [117]. These roles focus on incremental innovation within existing product lines and technology platforms.
Clinical Engineering: Hospital-based roles responsible for medical technology management, including equipment selection, maintenance, and safety compliance [6]. These positions serve as critical interfaces between clinical staff and medical technology.
Regulatory Affairs: Specialists who navigate FDA and international regulatory pathways to ensure medical products meet safety and efficacy standards [6]. These roles require meticulous attention to detail and understanding of complex regulatory frameworks.
Quantitative Outlook for Traditional Paths
Table 1: Traditional Career Path Metrics in Biomedical Engineering
| Career Pathway | Projected Growth | Median Salary | Primary Work Settings | Key Stability Factors |
|---|---|---|---|---|
| Clinical Engineering | 5-7% growth through 2034 [118] | ~$106,950 [6] | Hospitals, Healthcare systems | Aging population, equipment maintenance needs |
| Regulatory Affairs | Steady growth due to global market expansions [6] | Competitive (often $100,000+) [118] | Medical device firms, Pharmaceutical companies, Government agencies | Stringent regulatory requirements, safety standards |
| Academic Research | Limited growth with intense competition for tenure [116] | Varies widely by institution and rank | Universities, Research institutions | Grant funding landscape, publication requirements |
| Industry R&D | 5% projected growth (2024-2034) [6] | $100,730 average [118] | Large medical device companies, Biotechnology firms | Continuous product improvement cycles |
Emerging Career Pathways: Innovation and Integration
Emerging career paths reflect the convergence of biomedical engineering with advanced technologies such as artificial intelligence, data science, and nanotechnology. These roles often transcend traditional disciplinary boundaries and create new interfaces between engineering, biology, and digital technology.
Frontier Specializations
AI-Driven Healthcare Solutions: Roles in developing machine learning algorithms for diagnostic imaging, predictive analytics, and personalized treatment planning [6] [119]. These positions require dual competency in biomedical science and data analytics.
Neurotechnology and Brain-Computer Interfaces: Engineers and researchers developing neural prosthetics, deep brain stimulation systems, and direct neural interfaces [6]. This specialization combines neuroscience with advanced signal processing and robotics.
Regenerative Medicine and Tissue Engineering: Scientists working on bioprinting, scaffold design, and cellular therapies to repair or replace damaged tissues and organs [6] [117]. This field integrates materials science with cell biology.
Digital Health and Remote Monitoring: Professionals developing wearable sensors, mobile health applications, and telehealth platforms for continuous patient monitoring outside clinical settings [6] [120].
Biomedical Entrepreneurship: Founder and early-team roles in startups commercializing novel medical technologies, particularly in optics, photonics, and medical devices [121]. These roles require both technical expertise and business acumen.
Quantitative Outlook for Emerging Paths
Table 2: Emerging Career Path Metrics in Biomedical Engineering and Optics Research
| Career Pathway | Growth Drivers | Salary Potential | Primary Work Settings | Innovation Factors |
|---|---|---|---|---|
| Bioinformatics/Computational Biomedical Engineering | Rapid growth due to precision medicine and AI-driven solutions [6] | High (often exceeding $120,000) [6] | Biotech firms, Pharmaceutical R&D, Healthcare analytics companies | Big data in genomics and proteomics |
| Neurotechnology Engineering | Advancements in AI, neuroprosthetics, and robotics [6] | High (specialized premium) | Neurotechnology startups, Research institutions, Robotics companies | Brain-machine interface development |
| Biomedical Entrepreneurship | Startup ecosystem growth, venture funding [121] | Variable with high upside potential | Startup companies, Innovation hubs, Incubators | Technology translation from lab to market |
| Digital Health Technology | Remote care expansion, wearable technology adoption [6] [120] | Competitive with tech premiums | Digital health companies, Tech firms, Remote monitoring startups | IoT integration with healthcare |
Work Environment Comparison: Academia vs. Industry
The professional environment significantly influences research direction, collaboration patterns, and career progression. Understanding the fundamental differences between academic and industry settings enables informed career decisions.
Structural and Cultural Differences
Table 3: Academic vs. Industry Work Environments in Biomedical Research
| Factor | Academic Environment | Industry Environment |
|---|---|---|
| Primary Motivation | Knowledge creation, publications, grant funding [116] | Product development, market impact, profitability [116] |
| Performance Measurement | Publications, citations, grant awards [116] | Product milestones, patents, business impact [116] |
| Career Progression | Based on years in system, publication record [116] | Structured performance reviews with clear metrics (SMART goals) [116] |
| Work Pace & Structure | Self-directed with potential for project ambiguity [116] | Faster pace with defined deliverables and timelines [116] |
| Collaboration Dynamics | Individual research with occasional collaboration [116] | Integrated team-based approaches with cross-functional collaboration [116] |
| Funding Structure | Competitive grants (NIH, NSF), institutional support [116] | Corporate R&D budgets, venture capital, product revenue [116] |
Performance and Advancement Contrast
The industry environment typically provides more structured feedback and clearer advancement pathways compared to academia. Industry professionals operate under Performance Development Plans (PDPs) with Specific, Measurable, Achievable, Result-Oriented and Time-Bound (SMART) goals, with progress tracked through mid-year and end-of-year reviews [116]. This structured approach contrasts with the academic model where advancement often depends on years in the system and publication counts with less frequent, formalized feedback [116].
Industry culture typically rewards leadership and initiative more directly than academic environments. Professionals who identify workflow improvements or product enhancements receive tangible recognition through promotions, salary increases, or bonuses [116]. This contrasts with academic settings where research direction is often constrained by long-term grant objectives, potentially limiting opportunities for pivoting based on new discoveries [116].
Essential Skills and Competencies for Future Readiness
The evolving landscape of biomedical engineering and optics research requires a dynamic combination of technical expertise and professional skills that transcend traditional disciplinary boundaries.
Core Skill Requirements
Diagram: Evolving Skill Requirements in Biomedical Engineering
The Scientist's Toolkit: Essential Research Reagents and Technologies
Table 4: Core Research Technologies in Biomedical Engineering and Optics
| Technology/Reagent Category | Specific Examples | Primary Research Applications |
|---|---|---|
| Computational Modeling Tools | Finite Element Analysis, Computational Fluid Dynamics, Molecular Dynamics Simulations | Medical device stress testing, drug delivery optimization, biomaterial interaction prediction [67] |
| Biomaterials | Metal alloys, Biopolymers, Ceramics, Composites, Decellularized extracellular matrices | Implant development, tissue engineering scaffolds, medical device components [117] |
| Bioinstrumentation Platforms | Microelectrode arrays, Miniaturized sensors, Medical imaging systems (MRI, CT, ultrasound) | Physiological monitoring, diagnostic data acquisition, therapeutic device integration [117] |
| Cell Culture Systems | 3D bioprinters, Organ-on-a-chip platforms, Stem cell differentiation kits | Tissue engineering, drug screening, disease modeling [6] |
| AI and Data Analytics Tools | Machine learning algorithms, Image analysis software, Predictive analytics platforms | Medical image interpretation, patient outcome prediction, experimental pattern recognition [6] [67] |
Future Work Trends Impacting Biomedical Research Environments
The professional landscape for biomedical researchers is transforming due to technological, demographic, and social forces that are reshaping work environments across sectors.
Macro Trends Influencing Research Careers
Hybrid Work Models: The pandemic accelerated adoption of flexible work arrangements, with research organizations developing hybrid models that combine laboratory presence with remote data analysis and collaboration [120]. This flexibility supports work-life balance while expanding talent pools beyond geographic constraints.
AI Integration in Research Processes: Artificial intelligence is transforming research workflows through automation of routine analyses, literature reviews, and experimental design [119] [120]. Researchers must develop skills to leverage AI tools while maintaining critical evaluation of AI-generated outputs.
Focus on Employee Well-being: Research organizations are increasingly recognizing that investigator burnout threatens innovation, leading to expanded mental health support, flexible scheduling, and reduced stigma around work-life integration [120].
Generational Workforce Transitions: As Generation Z represents a growing portion of the research workforce, expectations around flexibility, inclusivity, and values-driven work are reshaping organizational cultures [120]. Successful research environments will adapt leadership styles to support these evolving preferences.
Interdisciplinary Collaboration Imperative: Complex biomedical challenges increasingly require integration of diverse expertise across engineering, biology, data science, and clinical medicine [67]. Researchers who excel at cross-disciplinary communication and teamwork have significant career advantages.
Diagram: Interconnected Trends Shaping Future Research Environments
Strategic Career Development Framework
For researchers navigating the transition between traditional and emerging career paths, a strategic approach to professional development is essential. This framework integrates technical specialization with adaptable professional skills.
Methodology for Career Path Evaluation
Researchers should systematically assess potential career directions using the following evidence-based protocol:
Skills Gap Analysis: Inventory current technical competencies (e.g., computational modeling, biomaterials expertise, regulatory knowledge) and professional skills (e.g., cross-disciplinary communication, project management) against target role requirements [67].
Market Alignment Assessment: Evaluate target fields using growth projections, funding trends, and technological adoption curves. Emerging fields like neurotechnology and digital health show particularly strong growth trajectories [6].
Work Environment Preference Mapping: Identify personal preferences across key dimensions including structure, autonomy, collaboration style, and innovation pace. Academic settings typically offer greater autonomy while industry provides more structured collaboration [116].
Strategic Networking Protocol: Develop intentional connections across target environments through professional associations (e.g., Optica), conferences, and informational interviews to gain insider perspectives on workplace culture and advancement pathways [121].
Experiential Learning Implementation: Pursue targeted experiences (internships, fellowships, project collaborations) in environments of interest to develop relevant skills and validate career direction preferences before making full transitions.
Adaptation Strategies for Career Transitions
Successful navigation between traditional and emerging paths requires specific adaptation strategies:
For Academic to Industry Transitions: Develop fluency in business terminology, product development cycles, and regulatory frameworks. Highlight transferable skills in problem-solving, data analysis, and project management from academic research experience [116].
For Industry to Entrepreneurship Transitions: Cultivate investor networks, develop minimum viable product (MVP) development skills, and leverage industry experience to identify unmet market needs. Resources like the Optica Startup and Entrepreneurship Meeting provide practical entrepreneurship training [121].
Cross-Disciplinary Mobility: Intentionally develop "T-shaped" expertise with depth in one technical area complemented by breadth across related fields. This profile is particularly valuable in emerging areas like AI-driven healthcare solutions that integrate multiple domains [67].
The biomedical engineering and optics research landscapes present both enduring opportunities in traditional pathways and exciting possibilities in emerging fields. Traditional roles in clinical engineering, regulatory affairs, and academic research continue to offer stable, meaningful careers addressing fundamental healthcare needs. Simultaneously, emerging pathways in neurotechnology, computational biomedicine, and digital health create new frontiers for innovation and impact. The most successful researchers and drug development professionals will be those who strategically develop complementary technical and professional skills, maintain awareness of evolving work environment trends, and implement deliberate career planning processes. By understanding the structural, cultural, and operational differences between pathway options, technical professionals can make informed decisions that align their capabilities and aspirations with opportunities for maximum professional fulfillment and contribution to advancing human health.
The global technological landscape is undergoing a rapid transformation, driven by convergent advances in artificial intelligence, connectivity, and digitalization. This analysis examines demand patterns across four critical sectors—telecommunications, healthcare, defense, and consumer electronics—with specific focus on implications for careers in biomedical engineering and optics research. These fields are increasingly intersecting, creating new opportunities for professionals working at the nexus of photonics, medical technology, and advanced computing. Understanding these industry dynamics provides valuable insight for researchers, scientists, and drug development professionals navigating evolving career pathways and research directions.
Telecommunications Industry Analysis
The global telecommunications industry demonstrates steady growth amid evolving technological paradigms. With revenues reaching approximately $1.53 trillion in 2024, the sector is positioned for transformation driven by generative AI, 5G monetization, and emerging 6G standards [122]. The industry faces the dual challenge of sustaining core connectivity services while investing in next-generation infrastructure, with capital expenditures increasingly directed toward AI-enabled networks and fiber expansion.
Table: Global Telecommunications Market Indicators (2024-2028)
| Indicator | 2024 Value | Projected CAGR (2024-2028) | Key Insights |
|---|---|---|---|
| Total Service Revenue | $1.14 trillion (2023) | 2.9% | Expected to reach $1.3 trillion by 2028 [123] |
| Mobile Internet Users | 4.6 billion (2023) | ~2% annually | Projected to reach 5 billion by end of 2025 [122] |
| 5G Subscriptions | 1.79 billion (2023) | 33.2% | Projected to reach 7.51 billion by 2028 [123] |
| Fixed Wireless Access (FWA) | Growing segment | 18.3% | Expected to reach 99 million subscriptions by 2028 [123] |
Key Growth Areas and Technologies
Generative AI Integration: Telecommunications companies are implementing generative AI to optimize operations and create new services. Use cases include AI-powered network management, customer service automation, and "cognitive network operations centers" that function as smart copilots for engineers [123]. The AI-RAN Alliance represents a significant initiative exploring AI integration into radio access networks, potentially shaping 6G development [122].
5G Monetization and B2B Applications: While 5G adoption accelerates, monetization strategies are evolving beyond consumer connectivity. Fixed Wireless Access (FWA) has emerged as the fastest-growing broadband technology, while private 5G networks for industrial applications (manufacturing, energy, ports) represent a niche growth area [123]. Telecommunications providers are increasingly pursuing verticalization strategies—developing industry-specific solutions for sectors including healthcare, manufacturing, and defense [123].
Network Infrastructure Evolution: As the industry approaches 6G development, focus is shifting toward making future networks more profitable than 5G has proven. Investment priorities include long-haul fiber networks (sometimes built to support "sovereign AI" requirements), AI-native architecture, and open network interfaces [122]. Big tech players are projected to spend over $100 billion on network capex between 2024-2030, representing 5-10% of their total capex [122].
Implications for Biomedical Engineering and Optics Research
The telecommunications evolution creates multiple intersections with biomedical engineering and optics. High-speed, low-latency 5G and future 6G networks enable real-time remote patient monitoring and telemedicine applications [124]. Photonics technologies are fundamental to the fiber optic infrastructure underpinning these advanced networks. The growing emphasis on AI-RAN integration creates opportunities for biomedical engineers with expertise in edge computing architectures relevant to distributed medical device networks.
Diagram: Telecommunications-Biomedical Convergence Areas. This diagram illustrates the interconnections between advanced telecommunications infrastructure and biomedical applications, highlighting opportunities for optics and engineering professionals.
Healthcare Industry Analysis
Digital Transformation and Market Dynamics
The global healthcare industry is accelerating digital transformation initiatives, with over 70% of health system executives prioritizing operational efficiencies and productivity gains in 2025 [125]. Healthcare organizations face constrained budgets, staff shortages, and clinician burnout while implementing new technologies and adapting to changing consumer expectations. Digital transformation represents the issue most likely to impact global health systems, with approximately 90% of healthcare executives expecting accelerated use of digital technologies in 2025 [125].
Table: Healthcare Digital Transformation Impact Metrics
| Technology Area | Adoption Status | Key Impact Metrics | Implementation Challenges |
|---|---|---|---|
| Telehealth Services | Widespread adoption post-COVID | 84% reduction in specialist wait times; 92% decrease in travel burden for rural patients; $42 billion in annual savings [124] | Digital equity concerns; reimbursement policies; integration with clinical workflows |
| Generative AI | Early adoption phase | 40% of organizations report significant-to-moderate ROI; 37% say it's too early to know [125] | Data quality and bias; regulatory uncertainty; "hallucination" risks |
| Wearable Health Monitoring | Rapid consumer adoption | 63% fewer hospital readmissions; 82% patient satisfaction rates [124] | Data privacy; device accuracy; EHR integration |
| Precision Medicine | Growing in specialized areas | Particularly impactful in oncology for targeting specific genetic mutations [124] | Affordability; equitable access; integration into clinical workflows |
Technology Adoption and Implementation
Generative AI in Healthcare: Healthcare organizations are developing use cases for generative AI, with focus on administrative process automation and clinical support applications. Autonomous "agentic AI" systems show promise for automating multi-step processes like patient referrals, appointment scheduling, and data entry [125]. On the clinical side, AI applications for medical imaging analysis represent more than three-quarters of AI-based devices authorized by the FDA [125].
Telehealth and Remote Monitoring: Telehealth has transitioned from temporary solution to permanent care delivery model, with Congress extending Medicare telehealth coverage [124]. Wearable health technologies are creating new paradigms for chronic disease management and preventive care through continuous physiological monitoring. These technologies support a shift from reactive treatment to proactive, data-informed care models [124].
Workforce Challenges and Technology Integration: The global healthcare workforce shortage is expected to continue, with the World Health Organization projecting a shortfall of 10 million health care workers by 2030 [125]. Technology implementation aims to alleviate burnout by reducing administrative burdens—research indicates that 15-28% of nurses' work comprises low-value tasks, while doctors in intensive care units may spend only 15-30% of their time with patients [125]. Digital tools potentially free up 13-21% of nurses' time (240-400 hours annually per nurse) [125].
Implications for Biomedical Engineering and Optics Research
Biomedical engineers are positioned to develop integrated solutions that bridge technological capabilities with clinical needs. The expansion of wearable health monitoring creates opportunities for engineers with expertise in biosensors, photonics-based measurements, and data analytics [124] [105]. Optics researchers can contribute to advances in medical imaging, endoscopic systems, and lab-on-a-chip diagnostic technologies. The growing emphasis on precision medicine drives demand for engineering talent capable of developing targeted therapeutic devices and personalized monitoring solutions.
Defense Industry Analysis
Market Priorities and Technological Advancements
The aerospace and defense (A&D) industry is experiencing transformation driven by AI integration, supply chain resilience initiatives, and evolving procurement models. Commercial aerospace continues growth with rising fleet utilization, while defense priorities shift toward enhancing mission readiness and accelerating deployment of AI-enabled systems [126]. "Speed to field" has emerged as a unifying metric across defense portfolios, with emphasis on rapid capability deployment.
Table: Defense Technology Investment Priorities
| Technology Domain | Key Applications | Spending Projections | Implementation Status |
|---|---|---|---|
| AI and Agentic AI | Modeling/simulation; operator assistants; command/control; autonomous mission planning | US A&D AI spending to reach $5.8B by 2029 (3.5x 2025 levels) [126] | Early adoption; pilot programs; scaling challenges |
| Digital Sustainment | Predictive maintenance; condition-based monitoring; inventory optimization | Global commercial MRO demand growing at 3.2% CAGR (2026-2035) [126] | Transition from analytics to embedded workflows |
| Autonomous Systems | Collaborative combat aircraft; unmanned aerial systems; hypersonic weapons | Increasing investment priority across defense budgets | Rapid prototyping; "build-first" models emerging |
| Advanced Procurement | Commercial Solutions Openings; Other Transaction Authority | Shift toward non-traditional suppliers | Compressing acquisition timelines |
Technology Implementation Trends
AI and Autonomous Systems: AI is becoming a foundational capability across defense missions, with applications including modeling/simulation, operator assistants, and command/control systems [126]. The U.S. Department of Defense has awarded contracts to multiple AI companies to accelerate adoption in critical mission areas [126]. Agentic AI—software capable of completing complex tasks with minimal human supervision—is progressing from pilot projects to scaled deployments, with the Deloitte "From vision to value" report estimating that 36% of tasks in industrial products manufacturing could benefit from human-AI collaboration [126].
Aftermarket and Sustainment Innovation: Aftermarket services remain a resilient revenue stream, with engine maintenance, repair, and overhaul (MRO) as the dominant driver [126]. Technology integration focuses on AI-enabled inspection systems, predictive health monitoring, and condition-based maintenance models. The convergence of aftermarket offerings into end-to-end service portfolios (parts supply, repair, engineering modifications, training, and digital support) represents a significant trend [126].
Supply Chain and Procurement Transformation: Defense supply chains face persistent pressures from material shortages, skilled labor constraints, and geopolitical disruptions [126]. Acquisition reforms are transforming competition mechanics, emphasizing speed, commercial solutions, and expanded vendor access. Emerging procurement pathways like Commercial Solutions Openings and Other Transaction Authority aim to attract non-traditional suppliers and compress development timelines [126].
Implications for Biomedical Engineering and Optics Research
Defense priorities create multiple crossover opportunities for biomedical and optics professionals. Photonics technologies are essential for sensing, surveillance, communications, and directed energy applications [127]. Biomedical engineers contribute to human-system integration, warfighter performance monitoring, and field medical technologies. The defense emphasis on rapid prototyping and commercial technology adoption potentially accelerates the transition of biomedical innovations from research to deployment.
Consumer Electronics Industry Analysis
The global consumer electronics market demonstrates robust growth, with revenue reaching $1.00 trillion in 2025 and projected compound annual growth rate (CAGR) of 2.81% through 2030 [128]. Alternative projections suggest potentially higher growth trajectories, with the market expanding at 7.8% CAGR through 2032 to reach $1.46 trillion in 2025 [129]. The telephony segment represents the largest category, with market volume of $504.08 billion in 2025 [128].
Table: Consumer Electronics Market Segmentation (2025)
| Market Segment | 2025 Revenue | Growth Drivers | Key Players |
|---|---|---|---|
| Telephony | $504.08B | 5G adoption; emerging market expansion; premiumization | Apple, Samsung, Huawei [128] |
| TV, Radio & Multimedia | Significant segment | High-quality immersive experiences; content accessibility | Sony, LG, Samsung [128] |
| Computing | Established segment | Hybrid work models; gaming; productivity needs | HP, Dell, Apple [128] |
| Wearables | Growing segment | Health/fitness tracking; convenience features | Apple, Fitbit, Garmin [129] |
| Gaming Equipment | Expanding segment | Esports popularity; VR/AR integration | Sony, Microsoft, Nintendo [128] |
Key Trends and Consumer Behaviors
Health and Fitness Integration: Wearable health technologies represent a significant growth category, with devices evolving from fitness tracking to medically-relevant monitoring [129]. Consumer electronics are increasingly incorporating health monitoring capabilities, creating convergence between consumer technology and healthcare applications. These devices support the shift toward proactive, data-informed health management [124] [105].
AI-Powered Personalization: Consumer expectations increasingly include personalized experiences across all touchpoints, with 71% of consumers expecting brands to personalize every interaction [129]. Electronics manufacturers are responding with AI-driven product recommendations, customized user interfaces, and adaptive functionality. This trend extends to B2B channels, where self-serve platforms with personalized content are becoming standard [129].
Distribution and Commerce Transformation: Consumer electronics purchasing journeys are predominantly digital, with 72% of consumers "almost always" starting their search for electronic devices online [129]. Social commerce is growing rapidly, particularly through TikTok Shop, with projected sales of $85.6 billion in 2025 [129]. Despite digital channel dominance, physical retail maintains importance for product testing, with 44% of electronics shoppers preferring to physically interact with devices before purchase [129].
Implications for Biomedical Engineering and Optics Research
The consumer electronics sector offers significant opportunities for biomedical engineers and optics researchers. The integration of health monitoring capabilities into consumer devices creates demand for expertise in miniaturized sensors, signal processing, and physiological measurement [105]. Optics professionals contribute to displays, cameras, optical sensors, and emerging applications in augmented and virtual reality. The consumer electronics emphasis on miniaturization, power efficiency, and manufacturing scalability drives innovation that often transfers to medical device development.
Cross-Industry Convergence and Research Implications
Interdisciplinary Technology Trends
Several technologies demonstrate significant cross-industry impact, creating opportunities for researchers with interdisciplinary expertise:
Artificial Intelligence and Machine Learning: AI adoption accelerates across all four sectors, from telecommunications network optimization and healthcare diagnostics to defense autonomous systems and consumer electronics personalization. The emergence of "agentic AI" capable of completing complex tasks with minimal human supervision represents a significant advancement [125] [126].
Advanced Sensing and Imaging: Photonics-based sensing technologies enable applications ranging from medical diagnostics and environmental monitoring to defense surveillance and consumer device interfaces. Research opportunities exist in miniaturization, multi-modal sensing, and computational imaging techniques.
Connectivity and Distributed Computing: 5G/6G communications, edge computing, and cloud infrastructure create foundations for distributed intelligence systems across industries. These capabilities enable real-time remote monitoring, telemedicine, autonomous operations, and seamless consumer experiences.
Experimental Methodology for Cross-Domain Technology Assessment
Evaluating emerging technologies across multiple domains requires structured assessment frameworks. The following methodology provides a systematic approach for researchers investigating cross-industry applications:
Phase 1: Technology Characterization
- Define core technical parameters and performance metrics
- Identify technology readiness level (TRL) and implementation requirements
- Map dependency relationships with complementary technologies
Phase 2: Application Mapping
- Identify potential use cases across telecommunications, healthcare, defense, and consumer electronics
- Assess implementation requirements and adaptation needs for each domain
- Evaluate regulatory, security, and interoperability considerations
Phase 3: Impact Assessment
- Analyze potential market size and adoption timelines for each application
- Evaluate technical barriers and research requirements
- Assess workforce implications and skill requirements
Phase 4: Research Prioritization
- Identify high-impact research opportunities addressing multiple domains
- Develop interdisciplinary collaboration models
- Establish performance metrics and evaluation criteria
Diagram: Cross-Domain Technology Assessment Methodology. This workflow illustrates a structured approach for evaluating emerging technologies across multiple industries, highlighting interdisciplinary application opportunities.
Research Reagent Solutions for Cross-Industry Innovation
Table: Essential Research Tools and Platforms for Interdisciplinary Technology Development
| Research Area | Key Tools/Platforms | Application Examples | Industry Relevance |
|---|---|---|---|
| AI/ML Development | TensorFlow, PyTorch, scikit-learn | Predictive maintenance algorithms; diagnostic support systems; personalized recommendations | Healthcare, Defense, Consumer Electronics, Telecommunications |
| Sensor Integration | IoT platforms (AWS IoT, Azure IoT); embedded systems | Remote monitoring; environmental sensing; user interface systems | Healthcare, Defense, Consumer Electronics |
| Signal Processing | MATLAB, LabVIEW, Python SciPy | Biomedical signal analysis; communications protocols; image processing | Healthcare, Telecommunications, Defense |
| Optical Simulation | Zemax, Code V, FRED | Medical imaging systems; display technologies; optical communications | Healthcare, Consumer Electronics, Telecommunications |
| Prototyping Platforms | Arduino, Raspberry Pi, custom FPGA | Proof-of-concept development; rapid iteration; field testing | All sectors |
| Data Analytics | Tableau, R, Python Pandas | Performance analysis; user behavior analytics; operational optimization | All sectors |
The analysis of telecommunications, healthcare, defense, and consumer electronics reveals significant convergence around AI, connectivity, sensing, and digitalization technologies. For professionals in biomedical engineering and optics research, these trends create expanding opportunities at industry intersections. The growing emphasis on health technologies within consumer electronics, the defense sector's focus on human-performance monitoring, and telecommunications infrastructure enabling distributed healthcare all represent areas for interdisciplinary innovation.
Successful navigation of this evolving landscape requires both technical specialization and cross-domain awareness. Researchers should consider developing T-shaped expertise—deep knowledge in core capabilities coupled with broad understanding of adjacent applications. The increasing pace of technological change underscores the importance of continuous learning and adaptive research strategies. By understanding these industry dynamics and convergence patterns, biomedical engineers and optics researchers can better position themselves for impact across multiple domains, contributing to solutions that address complex challenges at the nexus of technology, health, and human performance.
For researchers, scientists, and drug development professionals, the rapid evolution of technology makes long-term career planning both essential and challenging. The fields of biomedical engineering and optics research are at the epicenter of healthcare and technological innovation, experiencing transformative growth driven by interdisciplinary convergence. Framing career development within these specific disciplines requires a strategic understanding of emerging sub-specialties, required skill sets, and the experimental methodologies pushing the boundaries of current research. This guide provides a technical framework for assessing career viability through analysis of high-growth areas, detailed experimental protocols, and visualization of innovation pathways that are defining the future of these integrated fields. By adopting a proactive approach to skill development and specialization, professionals can position themselves at the forefront of developments that are reshaping medicine, biology, and technology.
High-Growth Areas in Biomedical Engineering and Optics
Biomedical Engineering Specializations
Biomedical engineering stands as a critical discipline at the intersection of healthcare and technology, with its practitioners developing solutions that significantly improve human health and advance medical research [4]. The field offers numerous specialization pathways, each with distinct technical requirements and career trajectories.
Table 1: High-Growth Biomedical Engineering Specializations
| Specialization Area | Key Technical Focus | Projected Growth & Market Data | Representative Job Roles |
|---|---|---|---|
| Medical Device Design & Development | Surgical robotics, wearable diagnostics, AI-driven devices | Medical device design demand expected to increase by 12% over the next decade [5] | Product Design Engineer, R&D Engineer, Quality Assurance Engineer [5] |
| Tissue Engineering & Regenerative Medicine | Biomaterials, stem cells, 3D bioprinting, artificial organs | High demand for alternatives to organ transplants with long waitlists and rejection issues [4] | Research Scientist, Bioprocess Engineer, Clinical Trials Manager [5] |
| Biomechanics & Rehabilitation Engineering | Prosthetics, exoskeletons, advanced mobility aids, orthopedic devices | Growing focus on inclusivity and quality of life driving innovation [4] | Prosthetics/Orthotics Designer, Rehabilitation Engineer, Sports Biomechanist [5] |
| Biomedical Imaging & AI Analytics | MRI/CT/ultrasound enhancement, machine learning for image analysis, 3D imaging, augmented reality | Applications transforming medical procedures and surgeries through advanced visualization [4] | Imaging Systems Engineer, Machine Learning Engineer, Clinical Imaging Specialist [5] |
| Neural Engineering | Brain-computer interfaces (BCIs), neuroprosthetics, deep brain stimulation | Transformative potential for Parkinson's, epilepsy, and paralysis treatments [4] | Neuroprosthetics Engineer, BCI Developer, Neuroengineering Researcher [5] |
| Bioinformatics & Health Data Analytics | Genomic data analysis, predictive healthcare, machine learning/AI for patient outcomes | Rapid growth field leveraging big data in healthcare [4] | Bioinformatics Analyst, Computational Biologist, Healthcare Data Scientist [5] |
The integration of artificial intelligence and machine learning across biomedical engineering specializations represents a particularly powerful trend. Over 75% of surveyed life science companies have implemented some form of AI in the last two years, underscoring the demand for data scientists and AI-skilled professionals in biotech teams [107]. This digital transformation is creating entirely new job roles and increasing cross-sector competition for talent with hybrid expertise.
Optics and Photonics Research Applications
Photonics and optics research are experiencing strong growth, with research and development (R&D) and manufacturing roles driving the highest demand [127]. The first half of 2025 saw over 330 R&D vacancies in the photonics sector alone, highlighting innovation as the core of competitiveness [127].
Table 2: Optics and Photonics Growth Areas
| Research Domain | Technical Applications | Industry Demand & Job Trends | Intersection with Biomedical Fields |
|---|---|---|---|
| Integrated Photonics | Optical computing, high-capacity networks, semiconductor-based optical circuits | Driving breakthroughs in telecommunications; pursued by industry giants (Intel, IBM) [130] | Lab-on-a-chip diagnostics, miniaturized medical sensors, portable imaging devices |
| Quantum Optics | Quantum key distribution (QKD), quantum computing solutions | Rapid transition from theoretical exploration to tangible applications; high demand for skilled professionals [130] | Quantum-enhanced imaging, secure medical data transmission, fundamental biological research tools |
| Advanced Imaging Techniques | Multi-spectral imaging, 3D imaging, precision visualization | Indispensable across healthcare and manufacturing; enhances diagnostic techniques [130] | Improved early detection, treatment outcome monitoring, surgical guidance systems |
| AI-ML Integration in Optics | AI-driven image analysis, precision data processing, automated interpretation | Germany led demand with almost 50 software engineer offers in photonics [127] | Optimized complex diagnostic processes, enhanced speed and accuracy in medical imaging |
| Biophotonics | Medical diagnostics, therapeutic applications, clinical instrumentation | Strong alignment with biomedical device sector; convergence point for interdisciplinary research | Optical coherence tomography, photodynamic therapy, laser surgery, fluorescence imaging |
The geographical distribution of opportunities in photonics shows clear hubs of innovation, with Germany emerging as the main European hub (nearly 900 positions in H1 2025), while the United States continues to lead globally (685 vacancies in same period) [127]. France and the Netherlands have consolidated their roles as secondary but essential hubs, each with just over 300 vacancies [127]. This distribution demonstrates the dual dominance of Europe and North America in attracting and creating talent in the sector.
Experimental Protocols in Integrated Research Fields
Development of a Biomedical Imaging System with AI Analytics
The integration of advanced optics with machine learning represents a cutting-edge methodology in medical diagnostics. This protocol outlines the development of an AI-enhanced biomedical imaging system for early disease detection.
Objective: To design, validate, and implement a biomedical imaging system that combines multi-spectral imaging hardware with machine learning algorithms to improve diagnostic accuracy for early-stage pathologies.
Materials and Research Reagent Solutions:
Table 3: Essential Research Materials and Reagents
| Item/Category | Specification | Function/Application |
|---|---|---|
| Optical Components | High-resolution CCD/CMOS sensors, precision lenses, multi-spectral light sources | Image acquisition hardware foundation for capturing detailed biological data |
| Tissue Phantoms | Hydrogel-based with controlled optical properties (scattering, absorption) | System calibration and validation against known standards |
| Cell Cultures | Human epithelial cell lines (normal and pathological phenotypes) | Biological testing substrates for system validation |
| Contrast Agents | Fluorescent dyes (ICG, fluorescein), targeted molecular probes | Enhancement of specific biological structures or molecular targets |
| Computational Resources | GPU-accelerated workstations, cloud computing access | Training and implementation of complex machine learning models |
| Software Libraries | Python with OpenCV, TensorFlow/PyTorch, specialized imaging toolkits | Image processing, algorithm development, and data analysis |
Methodology:
System Architecture Design:
- Configure multi-spectral imaging hardware capable of capturing data across visible and near-infrared spectra (400-900nm)
- Integrate high-sensitivity detectors with precision optical components to maximize signal-to-noise ratio
- Establish computational pipeline for real-time image processing and analysis
Data Acquisition Protocol:
- Acquire imaging data from calibrated tissue phantoms to establish baseline performance metrics
- Collect comprehensive image datasets from cell cultures and tissue samples representing normal and pathological states
- Implement standardized lighting, positioning, and calibration procedures to ensure data consistency
Algorithm Development and Training:
- Preprocess raw image data to correct for instrumental artifacts and enhance relevant features
- Develop convolutional neural network (CNN) architectures specifically optimized for medical image analysis
- Train models using annotated datasets, employing transfer learning where appropriate to enhance efficiency
- Validate model performance against independent test sets and clinician annotations
System Integration and Validation:
- Integrate trained models into the imaging system software for real-time analysis capabilities
- Conduct rigorous testing using blinded samples to determine diagnostic sensitivity and specificity
- Compare system performance against conventional diagnostic methods and expert assessment
This methodology highlights the interdisciplinary approach required for modern biomedical research, combining precision optical engineering with advanced computational analytics. The integration of AI does not merely automate existing processes but creates fundamentally new capabilities in diagnostic medicine [4] [130].
Advanced Biomaterials Development for Optical Sensing
The convergence of biomaterials engineering with optical technologies enables novel sensing modalities for medical applications.
Objective: To design, synthesize, and characterize biocompatible material systems with tailored optical properties for implantable sensing applications.
Materials and Methodology:
Polymer Synthesis and Functionalization:
- Synthesize base polymer matrices (e.g., PEG-based hydrogels, silicone elastomers) with controlled mechanical properties
- Incorporate optical functional elements (fluorescent reporters, plasmonic nanoparticles, photonic crystals)
- Modify surface chemistry to enhance biocompatibility and reduce fouling in biological environments
Optical Characterization:
- Quantify reflectance, transmission, and fluorescence properties using spectrophotometry
- Assess stability of optical signals under simulated physiological conditions
- Evaluate response dynamics to target analytes (glucose, oxygen, specific biomarkers)
Biological Compatibility Assessment:
- Conduct in vitro cytotoxicity testing using standardized assays (MTT, Live/Dead)
- Perform accelerated aging studies to determine functional longevity
- Validate performance in ex vivo tissue models and eventually in vivo models
The development of such integrated systems requires expertise spanning material science, optics, and biology, representing the cross-functional nature of modern biomedical research [4] [5].
Essential Skills and Career Development Pathways
Technical and Cross-Functional Competencies
Future-proofing a career in these rapidly evolving fields requires a strategic combination of technical specialization and adaptable human skills. Employers expect 39% of key skills required in the job market will change by 2030, representing significant disruption that professionals must anticipate [131].
Technical competencies experiencing rapid growth in importance include:
- AI and Big Data Analytics: Topping the list of growing skill requirements, with particular application in medical image analysis, genomic data interpretation, and predictive healthcare [131]
- Integrated Photonics Design: Understanding of semiconductor-based optical circuits for medical devices and diagnostic equipment [130]
- Biomaterial Synthesis and Characterization: Expertise in developing biocompatible materials with tailored optical and functional properties [4] [5]
- Regulatory Knowledge: Understanding of FDA/CE regulations for medical devices, with certifications such as Regulatory Affairs Certification (RAC) providing competitive advantage [5]
The World Economic Forum specifically identifies AI and big data as the top-growing skills in importance, followed by networks and cybersecurity and technological literacy [131]. These technical capabilities must be complemented with strong human skills that enable professionals to adapt to changing environments and lead interdisciplinary teams.
Critical cross-functional competencies include:
- Creative Thinking and Analytical Thinking: Ranked among the top skills needed to thrive in evolving job markets [131]
- Resilience, Flexibility, and Agility: Essential for navigating the boom-bust cycles common in research-intensive fields [131] [107]
- Cross-Functional Leadership: The ability to guide people across roles and disciplines without formal authority [132]
- Digital Communication and Persuasion: The capacity to explain complex technical concepts to diverse stakeholders [132]
Career Development Framework
A strategic approach to career development in biomedical engineering and optics research involves multiple dimensions of professional growth. The following diagram illustrates the integrated pathway for building a future-proof career in these interdisciplinary fields:
Career Development Pathway
Professionals can demonstrate expertise through multiple complementary approaches:
- Advanced Education: Pursuing master's or PhD programs focused on emerging specializations [5]
- Certifications and Training: Obtaining credentials such as Certified Clinical Engineer (CCE) or Regulatory Affairs Certification (RAC) [5]
- Practical Application: Building portfolios through internships, research projects, and industry collaborations [5]
- Knowledge Dissemination: Publishing research in academic journals and presenting at conferences [5]
- Professional Engagement: Joining organizations like the Biomedical Engineering Society (BMES) or optical engineering societies [5]
The early development of AI strategy and implementation skills creates particular advantage, as companies seek professionals who can bridge the gap between technology and measurable business or research outcomes [132]. Similarly, intentional professional brand building through platforms like LinkedIn can draw opportunities to professionals rather than requiring them to constantly pursue new positions [132].
The long-term viability of careers in biomedical engineering and optics research hinges on strategic positioning at the intersection of multiple high-growth domains. Professionals who develop deep technical specialization while maintaining adaptable, cross-functional competencies will be best equipped to navigate the evolving landscape. The integration of AI and machine learning across these fields is not a temporary trend but a fundamental transformation that will define the next decade of innovation. Similarly, the convergence of biological and optical technologies continues to create novel research directions and applications. By focusing on the experimental methodologies, technical skills, and career development pathways outlined in this guide, researchers, scientists, and drug development professionals can future-proof their careers while contributing to meaningful advances in healthcare and technology. The most successful professionals will be those who embrace continuous learning, interdisciplinary collaboration, and the translation of fundamental research into practical solutions for pressing human challenges.
Conclusion
The integration of biomedical engineering and optics represents one of the most promising frontiers in healthcare technology, driven by advancements in AI integration, photonic technologies, and sustainable practices. Professionals in this field can expect rewarding careers addressing complex medical challenges through innovative devices and systems. Future directions will likely focus on personalized medicine through enhanced imaging, AI-driven diagnostics, sophisticated biomaterials, and sustainable manufacturing practices. Success requires continuous adaptation to technological changes, proactive skill development, and strategic navigation of regulatory landscapes. For researchers and scientists, this convergence offers unprecedented opportunities to lead transformative developments that will define the next generation of medical breakthroughs and patient care innovations.
References
- 1. Optical Manipulation and Its Applications (OMA) [https://www.optica.org/events/meeting_archives/2025/optical_manipulation_and_its_applications/]
- 2. Synergy between photonics and biological approaches—A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575004/]
- 3. Ophthalmic drug discovery and development using artificial ... [https://www.nature.com/articles/s41746-025-01954-y]
- 4. Top Career Paths in Biomedical Engineering (2025) [https://biomedevices.com/top-career-paths-in-biomedical-engineering-2025-why-this-discipline-is-the-future/]
- 5. Biomedical Engineering Specialization Options for 2025 [https://research.com/careers/biomedical-engineering-specialization-options]
- 6. 10 Excellent Biomedical Engineering Career Opportunities [https://ep.jhu.edu/news/10-excellent-biomedical-engineering-career-opportunities/]
- 7. Developing Drugs for Optical Imaging January 2025 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/developing-drugs-optical-imaging]
- 8. Developing Drugs for Optical Imaging; Draft Guidance ... [https://www.federalregister.gov/documents/2025/01/08/2025-00213/developing-drugs-for-optical-imaging-draft-guidance-for-industry-availability]
- 9. 2025 Synergy Program - UBC - SBME [https://bme.ubc.ca/2025-synergy-program/]
- 10. Career Paths | Biomedical Engineering [https://bme.osu.edu/biomedical-engineering-undergraduate-program/career-paths]
- 11. Biomedical Engineering Careers: Research to Medical Devices [https://online-engineering.case.edu/blog/exploring-biomedical-engineering-careers]
- 12. Choosing Your Niche: Specializations Within Biomedical ... [https://online-engineering.case.edu/blog/choosing-your-niche-specializations-within-biomedical-engineering]
- 13. AOG at European Conferences on Biomedical ... - Research at Kent [https://research.kent.ac.uk/applied-optics/2025/07/09/aog-at-european-conferences-on-biomedical-optics-22-26-june-2025-munchen-germany/]
- 14. Navigating Biomedical Engineering Careers: A 2024 Guide [https://und.edu/blog/biomedical-engineering-careers.html]
- 15. Specializations | Biomedical Engineering [https://bme.ucdavis.edu/undergraduate/specializations]
- 16. A quantitative analysis of the use of anonymization in ... [https://www.nature.com/articles/s41746-025-01644-9]
- 17. Early Career Professionals [https://www.optica.org/get_involved/earlycareer/]
- 18. Optics Jobs - SPIE Career Center [https://spie.org/career-center/advice--tools/optics-jobs]
- 19. Photonics Market Size, Share, Forecast | Growth Analysis ... [https://www.fortunebusinessinsights.com/photonics-market-106525]
- 20. US Photonics Market Trends and Company Analysis ... [https://finance.yahoo.com/news/us-photonics-market-trends-company-082500084.html]
- 21. Photonics Market Size & Trends 2025-2035 [https://www.futuremarketinsights.com/reports/photonics-market]
- 22. Silicon Photonics Market Size to Hit USD 28.75 Billion ... [https://www.precedenceresearch.com/silicon-photonics-market]
- 23. Medical Device Industry Facts, Trends and Statistics 2025 [https://arterexmedical.com/medical-device-industry-statistics/]
- 24. Medical Device Market Growth Outlook: 2025–2030 [https://www.medicalmicromolding.com/medical-device-market-growth-outlook-2025-2030/]
- 25. What is Biomedical Engineering: Career Paths, Skills & ... [https://research.com/careers/what-is-biomedical-engineering-career-paths-skills-and-salary]
- 26. Continued strength for the photonics industry [https://spie.org/news/photonics-focus/mayjune-2025/continuing-strength-for-photonics-industry]
- 27. Trend Overview 2025: Key Developments in Biomedical Science & Research [https://biomedgrid.com/fulltext/volume25/trend-overview-2025-key-developments-in-biomedical-science-research.003320.php]
- 28. Innovations in Biomedical Engineering: Advancements Transforming Healthcare [https://online-engineering.case.edu/blog/innovations-in-biomedical-engineering]
- 29. Best Global Universities for Optics [https://www.usnews.com/education/best-global-universities/optics]
- 30. 2025 Best Optics/Optical Sciences Schools [https://www.collegefactual.com/majors/physical-sciences/physics/optics-optical-sciences/rankings/top-ranked/]
- 31. Best Optics/Optical Sciences colleges in the US 2025 [https://www.universities.com/programs/optics-optical-sciences-degrees]
- 32. October 2025: Sue Halligan | Biomedical Engineering [https://www.bme.columbia.edu/october-2025-sue-halligan]
- 33. How to Become a Biomedical Engineer? [https://und.edu/blog/how-to-become-a-biomedical-engineer.html]
- 34. Fundamentals of Optics Learning Track [https://innovationspace.ansys.com/courses/learning-track/fundamentals-of-optics/]
- 35. Best Online Optics Courses and Programs [https://www.edx.org/learn/optics]
- 36. Bachelor's Degrees in Bioengineering [https://seas.harvard.edu/bioengineering/bachelors-degrees-bioengineering]
- 37. Biomedical engineering degree overview [https://www.careerexplorer.com/degrees/biomedical-engineering-degree/]
- 38. What to Look for in a Biomedical Engineering Degree | CWRU [https://online-engineering.case.edu/blog/what-to-look-for-in-biomedical-engineering-degree]
- 39. Which classes are best for biomedical engineering? [https://uiowa.edu/explore/biomedical-engineering-degree/which-classes-are-best-for-biomedical-engineering]
- 40. A Survey on Optical Coherence Tomography—Technology ... [https://www.mdpi.com/2306-5354/12/1/65]
- 41. Optical Coherence Tomography (OCT): Principle and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK554044/]
- 42. Comparative Study of CT and MRI in the Early Detection ... [https://healthcare-bulletin.co.uk/article/comparative-study-of-ct-and-mri-in-the-early-detection-and-staging-of-hepatocellular-carcinoma-a-prospective-diagnostic-accuracy-cohort-study-3217/]
- 43. ARVO 2025 Highlights: Advances in Ophthalmology Trials [https://tfscro.com/resources/arvo-2025-highlights-driving-innovation-in-ophthalmic-drug-development/]
- 44. What Can You Do with a Biomedical Engineering Degree? [https://ep.jhu.edu/news/what-can-you-do-with-a-biomedical-engineering-degree/]
- 45. Advancements in biodegradable implants: evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577823/]
- 46. Biomaterials Market Trends, Share and Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/biomaterials-market]
- 47. Tissue Engineering: The Future is Here [https://www.bme.jhu.edu/news-events/news/tissue-engineering-the-future-is-here/]
- 48. Next-Generation Biomaterials for Load-Bearing Tissue ... [https://www.mdpi.com/2079-4983/16/7/232]
- 49. Biomaterials in Medicine: Current Trends and Future ... [https://www.sciencepublishinggroup.com/article/10.11648/j.ijbmr.20251301.13]
- 50. Materials science breakthroughs 2025: Trends to watch [https://www.cas.org/resources/cas-insights/materials-science-trends-2025]
- 51. Applying to the Summer Institute in Biomedical Optics [https://hst.mit.edu/applying-hst/applying-summer-institute-biomedical-optics]
- 52. Research Optical Engineer - Butte Lab - Department of ... [https://careers.cshs.org/job/los-angeles/research-optical-engineer-butte-lab-department-of-neurosurgery/252/76430755696]
- 53. Surgical Lasers Industry Eyes $27.9 Billion Opportunity by [https://www.globenewswire.com/news-release/2025/01/16/3010564/28124/en/Surgical-Lasers-Industry-Eyes-27-9-Billion-Opportunity-by-2035-Tripling-in-Size-Solid-State-Laser-Systems-Dominate-the-Market-While-Diode-Lasers-Experience-Explosive-Growth.html]
- 54. Surgical Laser System in the Real World: 5 Uses You'll ... [https://www.linkedin.com/pulse/surgical-laser-system-real-world-5-uses-youll-actually-kupgc]
- 55. UI scholars find laser technology could make surgeries safer [https://engineering.uiowa.edu/news-all/2025/11/ui-scholars-find-laser-technology-could-make-surgeries-safer]
- 56. prosthetics [https://www.media.mit.edu/research/?filter=everything&tag=prosthetics]
- 57. Next-Gen Prosthetic Arms: The Most Anticipated ... [https://www.robobionics.in/blog/next-gen-prosthetic-arms-the-most-anticipated-innovations-of-2025-2030/]
- 58. The Best Assistive Tech Gadgets in 2025: Enhancing ... [https://thinkbeyondthechair.org/the-best-assistive-tech-gadgets-in-2025-enhancing-independence-through-innovation/]
- 59. Pediatric Prosthetic Advancements: Top Innovations in 2025 [https://www.hortonsoandp.com/pediatric-prosthetic-advancements-whats-new-in-2025/]
- 60. Laser-based engineering strategies for biomedical and ... [https://www.sciencedirect.com/science/article/pii/S0927796X25002001]
- 61. Emerging Trends in Laser Technology for 2025 [https://lttcorp.com/laser-technology-trend/]
- 62. Therapeutics in the 2025 Pipeline [https://modernod.com/topics/contact-lenses/therapeutics-in-the-2025-pipeline/38957/]
- 63. Functional Optical Imaging Laboratory (FOIL) [https://foil.northwestern.edu/]
- 64. Researchers demonstrate precise optical clock signal ... [https://www.optica.org/about/newsroom/news_releases/2025/researchers_demonstrate_precise_optical_clock_signal_transmission_via_multicore_fiber/]
- 65. 10 Skills Biomedical Engineers Need to Stay Competitive [https://graduate.northeastern.edu/knowledge-hub/biomedical-engineer-skills/]
- 66. 5 skills you need to become a photonics engineer [https://www.siliconrepublic.com/advice/photonics-engineer-skills]
- 67. Biomedical Engineer Skills in 2025 (Top + Most ... [https://www.tealhq.com/skills/biomedical-engineer]
- 68. Shining a Light on the Future of Biophotonics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245495/]
- 69. Universities can do more to prepare the biomedical ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324925008114]
- 70. The Photonics Skills Gap Threatens Innovation in Quantum ... [https://www.azooptics.com/Article.aspx?ArticleID=2825]
- 71. Solving the optics technician shortage starts with education [https://spie.org/news/photonics-focus/sept-oct-2025/solving-optics-technician-shortage]
- 72. A Future-Focused Lens to Equipping Biomedical ... [https://link.springer.com/article/10.1007/s43683-025-00186-6]
- 73. Biomedical Engineer Education Requirements in 2025 [https://www.tealhq.com/education/biomedical-engineer]
- 74. Photonics Skills Gap Threatens Innovation in Quantum and ... [https://www.aimphotonics.com/news/photonics-skills-gap-threatens-innovation-in-quantum-and-ai]
- 75. Quality Management System Regulation: Final Rule [https://www.fda.gov/medical-devices/quality-system-qs-regulationmedical-device-current-good-manufacturing-practices-cgmp/quality-management-system-regulation-final-rule-amending-quality-system-regulation-frequently-asked]
- 76. Quality Management System Information for Certain ... [https://www.federalregister.gov/documents/2025/11/17/2025-19947/quality-management-system-information-for-certain-premarket-submission-reviews-draft-guidance-for]
- 77. QMS Information for Certain PMA Reviews Draft Guidance [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/quality-management-system-information-certain-premarket-submission-reviews]
- 78. Novel Drug for Approvals | 2025 FDA [https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2025]
- 79. : Full List of 28 New Therapies - GreyB FDA Drug Approvals 2025 [https://www.greyb.com/blog/fda-drug-approvals-2025/]
- 80. How will FDA changes reshape drug in approval and beyond? 2025 [https://cen.acs.org/pharmaceuticals/drug-development/FDA-changes-reshape-drug-approval/103/web/2025/05]
- 81. Engineer Positions at FDA [https://www.fda.gov/about-fda/career-descriptions/engineer-positions-fda]
- 82. Engineering Careers at CDER [https://www.fda.gov/about-fda/jobs-center-drug-evaluation-and-research-cder/engineering-careers-cder]
- 83. Biomedical Engineering Cost Analysis [https://www.spendedge.com/casestudy/biomedical-engineering-cost-model/]
- 84. What Does 2025 Hold for Optical Components? [https://www.uqgoptics.com/what-does-2025-hold-for-optical-components/]
- 85. 'Controlled Evolution' Dramatically Boosts pDNA Production ... [https://news.ncsu.edu/2025/08/boosting-pdna-production/]
- 86. Coherent Optics in 2025: Scaling Speed, Efficiency and ... [https://www.cablelabs.com/blog/coherent-optics-in-2025-scaling-speed-efficiency-and-reliability]
- 87. Optics & Photonics Innovations - November 2025 [https://www.techbriefs.com/component/content/article/54249-doc-9796]
- 88. Best Biomedical Engineering Courses & Certificates [2025] [https://www.coursera.org/courses?query=biomedical%20engineering]
- 89. Best Certifications for Biomedical Engineers in 2025 ( ... [https://www.tealhq.com/certifications/biomedical-engineer]
- 90. Certified Biomedical Equipment Technician (CBET) [https://aami.org/certifications/cbet/]
- 91. 2025 Session Tracks [https://www.bmes.org/2025/annualmeeting/session-tracks]
- 92. Biomedical Engineering Accelerated MS | UW-Madison PDC [https://pdc.wisc.edu/degrees/biomedical-eng-accelerated-program-ms/]
- 93. Graduate Program Overview [https://www.bme.utah.edu/graduate-program-overview/]
- 94. Dual Degree Program: Biomedical Engineering combined ... [https://catalog.colostate.edu/general-catalog/colleges/engineering/biomedical-chemical-engineering/electrical-lasers-optical-concentration-dual-degree-program/]
- 95. Best Optics Courses & Certificates [ 2025 ] | Coursera Learn Online [https://www.coursera.org/courses?query=optics]
- 96. BMES Launches 2025 Mentorship Program for Members [https://www.bmes.org/news/bmes-launches-2025-mentorship-program-for-members]
- 97. Student Chapter Mentor Matchup [https://member.bmes.org/student-chapter-mentorship]
- 98. Mentor Match [https://www.optica.org/get_involved/students/student_chapters/student_chapter_benefits/mentor_match/]
- 99. IEEE Strategic Plan & OFC 2025 Highlights [https://ieeephotonics.org/news/celebrating-excellence-in-photonics-ieee-strategic-plan-ofc-2025-highlights/]
- 100. 2025 Program | FIO - Frontiers in Optics [https://www.frontiersinoptics.com/program]
- 101. Optica Startup Meeting 2025 [https://circleoptics.com/optica-startup-meeting-2025/]
- 102. Empowering Tomorrow's Innovators: Mentoring in ... [https://www.linkedin.com/pulse/empowering-tomorrows-innovators-mentoring-biomedical-dan-storey-8eiwe]
- 103. 2025 Fellows [https://www.optica.org/get_involved/awards_and_honors/fellow_members/elected_fellows/2025_fellows/]
- 104. Biomedical Engineering: Salary, Outlook, & Description [https://www.mckissock.com/blog/professional-engineering/biomedical-engineering-salary-outlook-and-description/]
- 105. Biomedical Engineering Careers in 2025: Opportunities, ... [https://www.linkedin.com/pulse/biomedical-engineering-careers-2025-opportunities-growth-sagar-hedau-g0osf]
- 106. U.S. Life Sciences Talent Trends 2025 [https://www.cbre.com/insights/reports/us-life-sciences-talent-trends-2025]
- 107. US Biotech Job Market: 2025 Trends, Data & Analysis [https://intuitionlabs.ai/articles/us-biotech-job-market-2025]
- 108. Optical Measurement Market Outlook 2025-2034 [https://www.researchandmarkets.com/reports/6185858/optical-measurement-market-outlook-market?srsltid=AfmBOoqu76ow-qcyJmOecL3itaf-5FYa1Kllpk37NyGjf7M2TqBgOBIt]
- 109. Optical Interconnect Market Share & Size Analysis [https://www.nextmsc.com/report/optical-interconnect-market-se3569]
- 110. Biomedical Engineer Salary Guide for 2025 [https://research.com/careers/biomedical-engineer-salary-guide]
- 111. Biomedical Engineer Salary in 2025 | PayScale [https://www.payscale.com/research/US/Job=Biomedical_Engineer/Salary]
- 112. Biomedical Engineering Salary in 2024 [https://und.edu/blog/biomedical-engineering-salary.html]
- 113. Optical Engineer Salary in 2025 [https://www.payscale.com/research/US/Job=Optical_Engineer/Salary]
- 114. Quantum Optics Researcher Salaries [https://www.quantumjobs.us/salaries/quantum-optics-researcher]
- 115. Bioengineer and Biomedical Engineer Salaries [https://www.patenteducationseries.com/career-insights/bioengineer-and-biomedical-engineer-salaries.html]
- 116. Be A Research Scientist In Industry (Not Academia) [https://cheekyscientist.com/why-its-better-to-be-research-scientist-in-industry-than-in-academia/]
- 117. Career Opportunities | Biomedical Engineering [https://bme.engr.uky.edu/academics-0/undergraduate/career-opportunities]
- 118. Is Biomedical Engineering Hard? Challenges & Career ... [https://und.edu/blog/is-biomedical-engineering-hard.html]
- 119. Future of Work Trends 2025: Strategic Insights for CHROs [https://www.gartner.com/en/articles/future-of-work-trends]
- 120. The Future of Work: Trends and Insights for 2025 [https://www.imd.org/blog/learning-and-development/future-of-work/]
- 121. Optica Startup and Entrepreneurship Meeting [https://www.optica.org/events/topical_meetings/startup_and_entrepreneurship_program/]
- 122. 2025 global telecommunications outlook [https://www.deloitte.com/us/en/insights/industry/technology/technology-media-telecom-outlooks/telecommunications-industry-outlook-2025.html]
- 123. Perspectives from the Global Telecom Outlook 2024-2028 [https://www.pwc.com/gx/en/industries/tmt/telecom-outlook-perspectives.html]
- 124. Health Care Industry Trends to Watch in 2025 [https://www.publicpolicy.cornell.edu/masters-blog/health-care-industry-trends-to-watch-in-2025/]
- 125. 2025 global health care outlook | Deloitte Insights [https://www.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-global-health-care-executive-outlook.html]
- 126. 2026 Aerospace and Defense Industry Outlook [https://www.deloitte.com/us/en/insights/industry/aerospace-defense/aerospace-and-defense-industry-outlook.html]
- 127. First Semester 2025 Photonics Industry Jobs Report [https://epic-photonics.com/news-media/first-semester-2025-photonics-job-market-report/]
- 128. Consumer Electronics - Worldwide | Statista Market Forecast [https://www.statista.com/outlook/cmo/consumer-electronics/worldwide?srsltid=AfmBOorpWApxPYi-WmweSkMqtLgsxQZFM3cju36zsLjt6grfWhIhAoFj]
- 129. Consumer Electronics Trends 2025: Market Growth, AI & ... [https://www.shopify.com/enterprise/blog/consumer-electronic-trends]
- 130. The Optics Landscape Opportunities and Predictions [https://opticsjobs.com/the-optics-landscape-opportunities-and-predictions/]
- 131. Future of Jobs Report 2025: The jobs of the future [https://www.weforum.org/stories/2025/01/future-of-jobs-report-2025-jobs-of-the-future-and-the-skills-you-need-to-get-them/]
- 132. 4 High-Income Skills To Future-Proof Your Career In 2025 [https://www.forbes.com/sites/sarahhernholm/2025/09/05/4-high-income-skills-to-future-proof-your-career-in-2025/]