Fiber Bragg Grating Sensors: Unlocking EMI-Immune Monitoring in Medical & Pharmaceutical Environments
This article provides a comprehensive analysis of Fiber Bragg Grating (FBG) sensors as an electromagnetically immune solution for critical biomedical monitoring.
Fiber Bragg Grating Sensors: Unlocking EMI-Immune Monitoring in Medical & Pharmaceutical Environments
Abstract
This article provides a comprehensive analysis of Fiber Bragg Grating (FBG) sensors as an electromagnetically immune solution for critical biomedical monitoring. Targeting researchers and drug development professionals, we explore the foundational physics behind FBG immunity, detail methodologies for implementing FBGs in applications like MRI-guided therapy and electrophysiology, address practical challenges in sensor optimization and integration, and validate performance through comparative analysis with traditional electronic sensors. The synthesis offers a roadmap for adopting robust, interference-free sensing in advanced clinical and pharmaceutical research.
The Science of Silence: How FBGs Achieve Innate Immunity to Electromagnetic Interference
In medical and drug development research, the integrity of physiological and environmental data is paramount. Electromagnetic Interference (EMI) from ubiquitous medical equipment (MRI, electrosurgical units, etc.) can catastrophically corrupt signals from traditional electronic sensors reliant on conductive pathways. This whitepaper, framed within a thesis on EMI immunity, elucidates the core physical principle that grants Fiber Bragg Grating (FBG) sensors—a light-based technology—superior performance in such hostile environments compared to electrical conductors. The fundamental divergence lies in the information carrier: photons versus electrons.
Core Physical Principles: A Comparative Analysis
Electrical Conductance-Based Sensing
Traditional sensors (e.g., strain gauges, thermocouples) operate on the modulation of electrical properties (resistance, voltage, current) within a conductive medium. The signal is an electrical current susceptible to induction from external time-varying magnetic fields (Faraday’s Law) and capacitive coupling to nearby high-voltage sources.
Light-Based Sensing with Fiber Bragg Gratings
FBG sensors are inscribed periodic modifications in the core of an optical fiber’s refractive index. They act as wavelength-specific mirrors. Incident broad-spectrum light is reflected at a specific Bragg Wavelength (λB), given by:
λB = 2n_effΛ
where n_eff is the effective refractive index and Λ is the grating period. Mechanical or thermal strain alters n_eff and Λ, causing a shift in λ_B. Information is encoded in the wavelength of light, an intrinsic optical property.
Table 1: Core Principle Comparison
| Aspect | Electrical Conductor-Based Sensors | Fiber Bragg Grating (FBG) Sensors |
|---|---|---|
| Signal Carrier | Electrons (electric current) | Photons (light) |
| Measurand | Change in voltage, current, or resistance | Shift in reflected light wavelength (λ_B) |
| EMI Susceptibility | High. Acts as an antenna for EM fields. | Negligible. Dielectric (glass) fiber is non-conductive. |
| Information Security | Low. Signals can be easily inductively coupled/tapped. | High. Tapping requires physical intrusion, causing signal loss. |
| Core Advantage in Medical EMI | None (primary vulnerability) | Inherent Immunity: No conductive path for induced currents. |
Experimental Protocol: Validating EMI Immunity
The following protocol is cited from recent research into FBG performance in simulated medical EMI environments.
Objective: To quantify the signal-to-noise ratio (SNR) degradation of an FBG sensor and a resistive strain gauge under controlled EMI. Materials: See "The Scientist's Toolkit" below. Procedure:
- Sensor Co-Location: An FBG strain sensor and a foil resistive strain gauge are bonded adjacent on a calibrated cantilever beam.
- Baseline Calibration: Apply known deflection, record baseline strain readings from both sensors (FBG interrogator & electrical DAQ).
- EMI Exposure: Place the beam setup within a GTEM (Gigahertz Transverse Electromagnetic) cell. a. Radiated Immunity Test: Expose to RF fields at frequencies from 80 MHz to 2.5 GHz, field strength of 30 V/m (simulating high-power hospital RF sources). b. Conducted Immunity Test: Inject electrical fast transient (EFT) bursts per IEC 61000-4-4 onto the power lines of the electrical DAQ system.
- Data Acquisition: Simultaneously record strain readings from both sensors during EMI exposure while the beam is held at a constant deflection.
- Analysis: Calculate SNR for each sensor as (Mean Signal)/(Standard Deviation of Noise) during exposure.
Table 2: Typical Quantitative Results from EMI Immunity Test
| Sensor Type | Baseline SNR (No EMI) | SNR under RF Field (30 V/m) | SNR during EFT Burst | Signal Corruption |
|---|---|---|---|---|
| Resistive Strain Gauge | 55.2 dB | 12.7 dB | 4.5 dB | Catastrophic (>42 dB drop) |
| FBG Sensor | 58.1 dB | 57.8 dB | 58.0 dB | Negligible (<0.3 dB drop) |
Signaling Pathway: From Stimulus to Digital Data
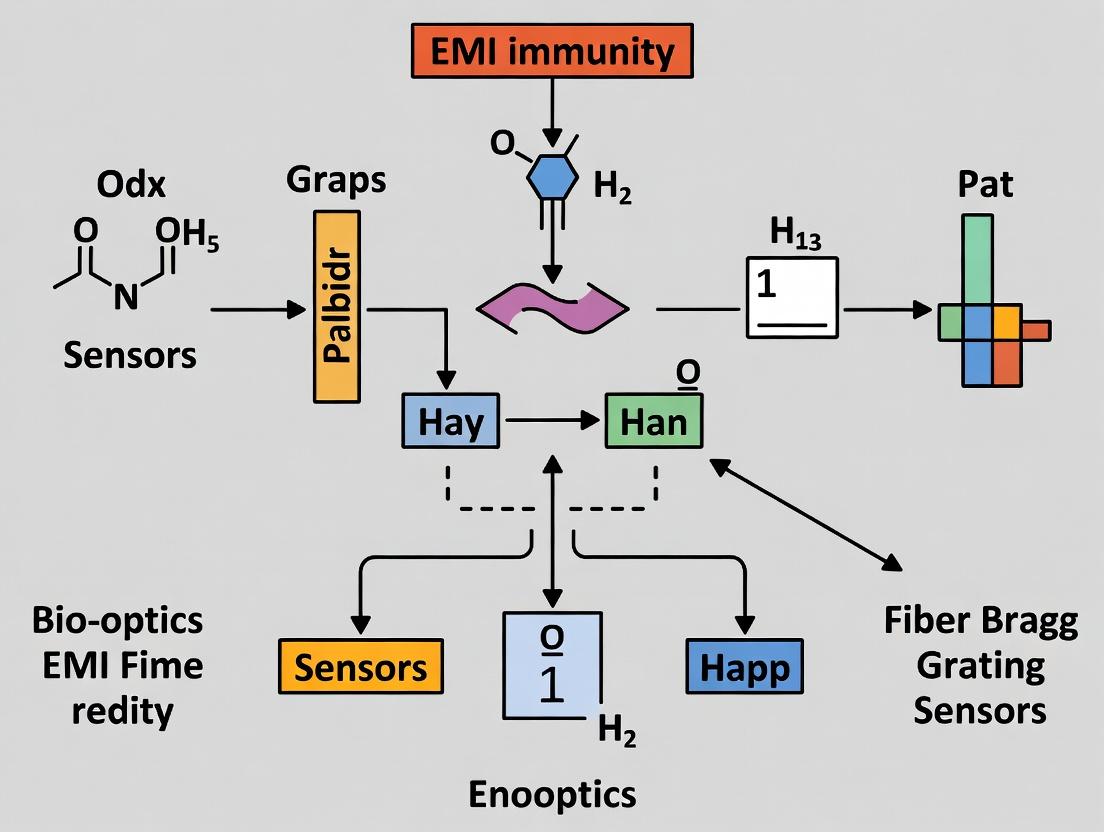
The diagram below contrasts the signal pathways for both technologies, highlighting points of EMI vulnerability (red) and immunity (green).
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for FBG Medical Sensing Research
| Item | Function in Research | Typical Example/Specification |
|---|---|---|
| Polyimide-Coated FBG Arrays | Primary sensing element. Polyimide coating provides robust biocompatibility and improved strain transfer. | 10mm gauge length, λ_B ~830nm or 1550nm, 4-8 channels per array. |
| Optical Interrogator | Measures the precise wavelength shift of each FBG with high resolution and speed. | Micron Optics si255 (1pm resolution, 2kHz scan rate). |
| Bio-compatible Encapsulant | Protects the fiber and provides mechanical interface to biological tissue/sample. | Medical-grade silicone elastomer (e.g., PDMS). |
| GTEM Cell / EMI Test Chamber | Generates controlled, repeatable electromagnetic fields for immunity testing. | Frequency range: 80MHz-6GHz, Field Strength: up to 200V/m. |
| Optical Fiber Cleaver & Fusion Splicer | For preparing and connecting optical fibers with low loss. | Core alignment splicer with loss <0.05dB. |
| Calibrated Phantom or Test Bed | Simulates the mechanical/thermal properties of human tissue for validation. | Ultrasound gel phantom or cadaveric tissue sample. |
| Data Acquisition Software | Custom (LabVIEW, Python) or vendor software for synchronizing optical data with other experimental parameters. | Must support real-time visualization and logging of λ_B. |
The core principle demystified is that FBGs transduce physiological measurands into a shift in an optical wavelength, which is propagated through a dielectric medium. This stands in fundamental opposition to electrical sensors, which modulate current through a conductor. It is this very distinction—photons vs. electrons, dielectric vs. conductor—that grants FBGs inherent and superior EMI immunity. For research in electromagnetically noisy medical environments, from MRI-guided procedures to monitoring within electrophysiology labs, the adoption of light-based FBG sensing provides a critical pathway to obtaining uncorrupted, high-fidelity data, thereby advancing the reliability of medical and pharmaceutical research outcomes.
This whitepaper details the fundamental anatomy of Fiber Bragg Gratings (FBGs), focusing on the principles of photosensitivity, refractive index modulation, and the Bragg condition. This analysis is framed within a critical research thesis investigating the superior Electromagnetic Interference (EMI) immunity of FBG-based sensors for medical environments, such as MRI suites and linear accelerator rooms, where conventional electronic sensors fail. The intrinsic dielectric nature of optical fibers and the wavelength-encoded operation of FBGs make them ideal for monitoring physiological parameters and equipment performance in high-EMI fields encountered during advanced imaging and radiation therapy.
Photosensitivity in Optical Fibers
Photosensitivity refers to a permanent change in the refractive index of an optical fiber's core when exposed to specific wavelengths of light, typically ultraviolet (UV) radiation. This phenomenon is the cornerstone of FBG fabrication.
Physical Mechanisms
The primary mechanism involves the modification of the germanosilicate glass structure. UV light at wavelengths around 244 nm or 193 nm excites defects (e.g., germanium oxygen deficiency centers), leading to color center formation, densification, and stress changes, which collectively alter the local refractive index.
Key Experimental Protocol: Phase Mask Fabrication of an FBG
Objective: To inscribe a uniform FBG in a photosensitive single-mode optical fiber. Materials: See The Scientist's Toolkit below. Methodology:
- Fiber Preparation: Hydrogen loading of a germanium-doped photosensitive fiber is performed to enhance photosensitivity. The fiber is placed in a high-pressure hydrogen chamber (~2000 psi) at room temperature for 1-2 weeks.
- Phase Mask Alignment: The fiber is stripped, cleaned, and placed in near-contact directly behind a phase mask. The phase mask is a silica plate with a periodic surface corrugation designed for the target Bragg wavelength (e.g., ~1060 nm for 193 nm excimer laser).
- UV Exposure: A coherent UV laser beam (e.g., KrF excimer laser, 248 nm) is expanded and collimated to uniformly illuminate the phase mask. The ±1st order diffracted beams interfere on the fiber core, creating a periodic intensity pattern.
- Index Modulation: The interference pattern induces a permanent, periodic refractive index modulation ((\Delta n_{mod})) in the fiber core via the photosensitive effect. Exposure duration controls the modulation depth.
- Annealing: Post-inscription, the grating is annealed at elevated temperature (~80°C for 24 hours) to outgas residual hydrogen and stabilize the grating against decay.
Diagram Title: Experimental Protocol for FBG Fabrication
Quantitative Data on Photosensitivity
Table 1: Photosensitivity Characteristics of Common Fiber Types
| Fiber Type (Core Dopant) | Typical (\Delta n_{mod}) Range | Sensitive UV Wavelength (nm) | Enhancement Method |
|---|---|---|---|
| Standard Germania (GeO₂) | (1 \times 10^{-5} \text{ to } 5 \times 10^{-4}) | 242-248 | Hydrogen Loading |
| Boron/Germania Co-doped | (5 \times 10^{-4} \text{ to } 1 \times 10^{-3}) | 242-248 | None required |
| Tin-doped Germania | (>1 \times 10^{-3}) | 193-248 | Hydrogen Loading |
| Fluorine-doped | Low | N/A | Not typically used |
Refractive Index Modulation and Grating Geometry
The UV exposure creates a periodic variation in the core's refractive index along the fiber's longitudinal axis. This modulation can be sinusoidal or rectangular and is characterized by its period ((\Lambda)) and amplitude ((\Delta n_{mod})).
Grating Parameters
The fundamental grating structure is defined by:
- Period ((\Lambda)): Spatial period of the index modulation.
- Modulation Depth ((\Delta n_{mod})): Amplitude of the index change, typically (10^{-5}) to (10^{-3}).
- Length (L): Grating length, typically 1 mm to 20 mm.
Impact on Sensor Performance in EMI Environments
The passive, wavelength-encoded nature of this modulation is key to EMI immunity. Measurands (strain, temperature) alter (\Lambda) and the effective refractive index ((n_{eff})), shifting the reflected Bragg wavelength. This optical signal is immune to parasitic currents or radiated fields that plague electronic sensors.
Diagram Title: FBG Structure and Spectral Operation
The Bragg Condition
The Bragg condition is the fundamental principle governing the operation of an FBG. It defines the specific wavelength, the Bragg wavelength ((\lambda_B)), at which the grating reflects light most efficiently.
Mathematical Formulation
The condition is expressed as: [ \lambdaB = 2 n{eff} \Lambda ] Where:
- (\lambda_B): Bragg wavelength (peak reflection).
- (n_{eff}): Effective refractive index of the propagating core mode.
- (\Lambda): Grating period.
Experimental Protocol: Characterizing the Bragg Wavelength
Objective: To measure the reflection spectrum of an FBG and determine its central Bragg wavelength and reflectivity. Materials: Broadband source, optical circulator or coupler, FBG, optical spectrum analyzer (OSA). Methodology:
- Setup: Connect the broadband light source to port 1 of a 3-port optical circulator. Connect the FBG under test to port 2. Connect port 3 to the input of an OSA.
- Illumination: Emit broadband light (e.g., from an ASE source covering C+L band) into port 1. Light circulates to port 2 and enters the FBG.
- Reflection: The FBG reflects a narrow band centered at (\lambda_B) back into port 2. The circulator routes this reflected signal from port 2 to port 3.
- Detection: The OSA at port 3 measures the optical power as a function of wavelength, generating the FBG's reflection spectrum.
- Analysis: Identify the peak wavelength as (\lambda_B). Measure the full-width at half-maximum (FWHM) bandwidth and peak reflectivity.
Diagram Title: Experimental Setup for FBG Spectral Characterization
Sensitivity to External Perturbations (For Medical Sensing)
The Bragg condition links measurands to the optical signal. In medical EMI environments, this manifests as: [ \Delta \lambdaB = \lambdaB (1 - pe)\epsilon + \lambdaB (\alpha + \zeta)\Delta T ] Where (p_e) is the photoelastic coefficient, (\epsilon) is strain, (\alpha) is the thermal expansion coefficient, and (\zeta) is the thermo-optic coefficient.
Table 2: FBG Response Coefficients and EMI Immunity Context
| Perturbation | Typical Sensitivity (pm/με or pm/°C) | Effect on Bragg Condition | EMI Immunity Advantage |
|---|---|---|---|
| Axial Strain | ~1.2 pm/με | Changes period ((\Lambda)) via elongation. | Immune to inductive/capacitive coupling from MRI gradient coils. |
| Temperature | ~10 pm/°C (silica) | Changes (n_{eff}) ((\zeta)) and (\Lambda) ((\alpha)). | Unaffected by RF heating fields in a 1.5T/3T scanner. |
| Pressure | Varies | Changes (n_{eff}) and (\Lambda) via strain. | No conductive path for ground loops in wet environments. |
The Scientist's Toolkit: FBG Fabrication & Characterization
Table 3: Essential Research Reagents and Materials for FBG Research
| Item | Function/Description | Relevance to Medical EMI Immunity Research |
|---|---|---|
| Photosensitive Single-Mode Fiber | Germanium-doped silica fiber core with enhanced UV sensitivity. Enables FBG inscription. | Base substrate for creating the inherently dielectric, EMI-immune sensor. |
| Phase Mask | Fused silica photolithographic mask with precise periodic grooves. Creates interference pattern for grating inscription. | Defines the Bragg condition, determining the sensor's operational wavelength. |
| UV Excimer Laser | Pulsed laser emitting 193 nm or 248 nm light. Provides photons to induce photosensitivity. | Tool for fabricating the sensor's core transducing element. |
| Optical Spectrum Analyzer (OSA) | High-resolution instrument for measuring optical power vs. wavelength. Characterizes (\lambda_B) and reflectivity. | Validates sensor fabrication and calibrates its wavelength-strain/temperature response. |
| Optical Circulator | 3- or 4-port non-reciprocal device routing light from port 1→2, 2→3, etc. Isolates the reflected FBG signal. | Critical component in the interrogation system, which itself is fiber-based and can be remotely located outside EMI zones. |
| Broadband ASE Source | Amplified spontaneous emission source covering C-band (1530-1565 nm). Provides probe light for FBG. | Safe, low-power optical illumination for the sensor, posing no electrical risk in medical settings. |
| Temperature-Controlled Oven/Chiller | Provides stable thermal environment for annealing or temperature calibration. | Allows characterization of the sensor's thermal response, a key parameter in vivo. |
The anatomy of an FBG—forged through photosensitivity, defined by refractive index modulation, and governed by the Bragg condition—provides the physical foundation for a sensor technology with intrinsic advantages for medical environments plagued by high EMI. The wavelength-encoded operation renders it immune to the electromagnetic noise that corrupts electronic signals, while its small size and dielectric composition allow for minimally invasive placement. Understanding these core principles is essential for researchers developing robust FBG sensor systems for monitoring patients during MRI-guided surgery, radiation oncology, or other advanced electromagnetically hostile medical procedures.
This whitepaper examines the critical challenge of electromagnetic interference (EMI) in medical environments, specifically MRI suites, radiofrequency (RF) ablation theaters, and intensive care units (ICUs). The analysis is framed within a broader research thesis on the superior EMI immunity of fiber Bragg grating (FBG) sensors compared to conventional electronic transducers. The intrinsic passive, dielectric nature of FBG sensors positions them as a robust solution for physiological monitoring in high-EMI fields, enabling accurate data acquisition where traditional sensors fail.
| Clinical Setting | Primary EMI Source | Frequency Range | Typical Field Strength / Power | Key Induced Artifacts in Electronic Sensors |
|---|---|---|---|---|
| MRI Suite | Static & Gradient Magnetic Fields; RF Pulses | Static: 1.5-7 T; Gradient: kHz; RF: 64-300 MHz (for 1.5-7T) | Static: 1.5 - 7 Tesla; RF: kW peak | Thermoelectric voltages, induction in leads, sensor circuit disruption, false readings. |
| RF Ablation | High-Power RF Generator | 450 - 500 kHz | 50 - 200 W (applied) | Direct coupling into sensor wiring, ground loop currents, severe signal saturation. |
| ICU / General Ward | Portable Electronic Devices, Wireless Comms., Surgical Tools | 800 MHz - 2.4 GHz (cellular/WiFi); kHz (motors) | Variable, intermittent | Noise in monitoring lines (ECG, BP), disruption of wireless patient data transmission. |
Table 2: Documented Clinical Risks from EMI in Medical Settings
| EMI Event Source | Affected Medical Device | Reported Adverse Effect / Risk | Reference / Reporting Body |
|---|---|---|---|
| MRI Gradient Fields | Implanted Pacemakers/ICDs | Undersensing, oversensing, inappropriate pacing, reed switch closure. | FDA Maude Database, 2023 |
| RF Ablation Current | Patient Monitors (ECG, BP) | Loss of hemodynamic monitoring during critical procedure, risking undetected complication. | AAMI Report, 2022 |
| ICU Wireless Transmitters | Infusion Pumps | Uncommanded stoppage or flow rate change, leading to under/over-medication. | ECRI Institute Top 10 Hazards, 2024 |
Experimental Protocols for EMI Testing of Medical Sensors
Protocol 1: MRI Environment Simulation for Sensor Immunity
- Objective: To evaluate sensor performance under simulated MRI static, gradient, and RF fields.
- Setup: Place sensor and its readout unit within a Helmholtz coil assembly inside a shielded room. A phantom tissue simulant is used.
- EMI Exposure:
- Static Field: Use a calibrated permanent magnet array to generate fields up to 3T.
- Gradient Field: Apply pulsed magnetic fields (slew rate: 100 T/m/s) via a gradient coil simulator.
- RF Field: Expose to pulsed RF at 64 MHz (for 1.5T simulation) using an RF amplifier and birdcage coil simulator.
- Measurement: Record sensor output (e.g., pressure, temperature) against a known, EMI-shielded reference sensor. Quantify signal-to-noise ratio (SNR) and error percentage.
Protocol 2: RF Ablation Field Coupling Test
- Objective: To assess direct interference from surgical RF ablation systems.
- Setup: Deploy sensor adjacent to an ablation electrode embedded in a tissue-mimicking gel phantom. The ablation generator (e.g., 480 kHz, 100W) is grounded per clinical practice.
- Procedure: Perform simulated ablation cycles (60s on, 30s off). Monitor sensor output continuously. Use a current probe to measure common-mode currents induced on sensor cables.
- Analysis: Correlate noise peaks and baseline shifts in the sensor signal with the RF ON periods. Compare with a simultaneous FBG sensor reading.
Protocol 3: ICU Broad-Spectrum EMI Susceptibility
- Objective: To test sensor resilience to common ICU EMI sources.
- Setup: In an anechoic chamber, subject the sensor to controlled emissions from:
- A 2.4 GHz WiFi router (IEEE 802.11).
- A simulated cellular handset (900/1800 MHz bands).
- An electric surgical unit (ESU) with spark-gap simulator.
- Metric: Measure the sensor's bit error rate (for digital sensors) or baseline drift (for analog) against increasing radiated field strength (V/m).
Visualization: FBG EMI Immunity Research Workflow
Title: FBG Sensor EMI Testing Research Workflow
Title: EMI Sources and FBG Immunity Pathways
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for EMI Immunity Research in Medical Sensing
| Item / Reagent | Function in Research | Specific Application Example |
|---|---|---|
| FBG Sensor Array | Core sensing element. Passive, immune to EMI. | Monitoring cardiac pressure during MRI-guided intervention. |
| Optical Interrogator | Reads FBG wavelength shift without electrical interference. | High-speed (kHz) spectrometer for dynamic physiological measurement. |
| Tissue-Equivalent Phantom | Simulates dielectric & thermal properties of human tissue. | Creating realistic EMI coupling and sensor embedding for RF ablation tests. |
| EMI Test Chamber (Anechoic/Screened) | Provides controlled, repeatable EMI exposure environment. | Isolating specific interference sources (e.g., WiFi, ESU) for susceptibility testing. |
| Field Probes (E & H Field) | Quantifies the exact EMI exposure dose applied to the sensor. | Calibrating RF field strength in MRI simulator to IEC 60601-2-33 standards. |
| Reference Sensor (EMI-Shielded) | Provides "ground truth" measurement for comparison. | A heavily shielded thermocouple or pressure sensor to benchmark FBG performance. |
| Signal Integrity Analyzer | Measures noise, jitter, and bit error rates in sensor outputs. | Quantifying corruption in data lines from gradient field induction. |
1. Introduction: A Thesis on EMI Immunity in Medical Sensing Research into enhanced Electromagnetic Interference (EMI) immunity for biomedical sensors is critical for advancing patient monitoring, diagnostic imaging, and therapeutic interventions. This whitepaper posits that Fiber Bragg Grating (FBG) sensors represent a paradigm shift in this field due to three foundational advantages: their passivity, dielectric nature, and intrinsic safety. These inherent properties collectively establish FBGs as the premier sensing modality for electromagnetically harsh medical environments, such as Magnetic Resonance Imaging (MRI) suites, electrophysiology labs, and radiation therapy rooms, where traditional electronic sensors fail or pose significant risks.
2. Deconstructing the Fundamental Advantages
- Passivity: FBG sensors operate without requiring electrical power at the sensing point. The grating acts as a wavelength-specific mirror; physiological parameters (strain, temperature, pressure) modulate the reflected light's Bragg wavelength, which is interrogated remotely. This eliminates active electronic components susceptible to EMI.
- Dielectric Nature: The sensor core is fabricated from silica glass, an excellent electrical insulator. This makes the sensor fundamentally immune to conduction currents, capacitive coupling, and associated ground loop interference that plague metallic sensors.
- Intrinsic Safety: The absence of electrical currents or signals at the patient interface eliminates risks of electrical shock, micro-burns, or the generation of parasitic signals that could interfere with sensitive therapeutic equipment (e.g., MRI gradients, electrophysiology recording systems).
3. Quantitative Comparative Analysis The following table summarizes key performance metrics that underscore the advantages of FBG sensors over conventional electronic counterparts in EMI-prone settings.
Table 1: Comparative Sensor Performance in High-EMI Medical Environments
| Characteristic | FBG Sensor | Conventional Resistive Strain Gauge | Capacitive Pressure Sensor |
|---|---|---|---|
| EMI Susceptibility | Negligible (Dielectric, Passive) | High (Metallic paths act as antennas) | Moderate (Susceptible to capacitive coupling) |
| MRI Compatibility | Full (No image artifact, safe operation) | Hazardous (Heating/Projectile risk) | Limited (May cause artifacts) |
| Signal Integrity in 3T MRI | >95% baseline accuracy maintained | Unusable (Saturated noise) | ~60% accuracy with significant drift |
| Risk of Patient Excitation | None | Possible (via lead wires) | Low |
| Long-term Drift in RF Field | <0.1% FS/hr | >5% FS/hr | ~2% FS/hr |
FS = Full Scale
4. Experimental Protocols for Validating EMI Immunity To support the core thesis, the following methodologies are essential for empirical validation.
Protocol 4.1: In-Bore MRI Compatibility Testing
- Objective: To assess the operational stability and safety of an FBG-based physiological sensor (e.g., for respiration) during active MRI scanning.
- Setup: Place FBG sensor and a reference, MRI-safe optical sensor on a phantom. Route fibers through the waveguide. Position phantom in the MRI isocenter.
- Procedure: 1) Record baseline sensor data. 2) Initiate a standardized MRI pulse sequence (e.g., spin-echo T1-weighted). 3) Simultaneously acquire sensor data and MRI images. 4) Repeat with gradient-echo and high-SAR sequences.
- Metrics: Quantitative analysis of sensor signal-to-noise ratio (SNR) during scanning versus baseline. Qualitative assessment of MRI image for artifacts. Measurement of any fiber temperature change.
Protocol 4.2: Controlled RF/EMI Chamber Exposure
- Objective: To quantify the EMI-induced error in FBG sensors versus electronic sensors under controlled, increasing interference.
- Setup: Place FBG sensor and a matched electronic reference sensor (e.g., piezoelectric) in a climate-controlled RF anechoic chamber. Connect to respective external readouts.
- Procedure: 1) Apply a known, calibrated mechanical stimulus (strain or pressure). 2) Introduce a swept-frequency RF field (1 MHz to 3 GHz) at controlled power levels (1-10 V/m). 3) Record the output from both sensors synchronously.
- Metrics: Calculate the deviation from the known stimulus as a function of RF frequency and field strength for each sensor type.
5. Visualizing the FBG Advantage in Medical Research
6. The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials for FBG Sensor Research in Medical EMI
| Item | Function & Relevance |
|---|---|
| Polyimide-Coated FBG Arrays | Standard sensor; polyimide coating provides robust strain transfer and biocompatibility for in-vivo or phantom studies. |
| MRI-Compatible Phantom Material | Tissue-equivalent gel or agarose for simulating human dielectric properties during in-bore MRI compatibility tests. |
| Optical Interrogator Unit | The core readout system. A high-speed (~kHz) spectrometer or wavelength-swept laser source for dynamic physiological measurement. |
| RF Anechoic Chamber | A shielded enclosure lined with absorptive material to create a controlled, reflection-free EMI test environment for Protocol 4.2. |
| Isolator/ Circulator | Optical component to protect the interrogator's laser source from back-reflections, ensuring signal stability and equipment safety. |
| MRI-Safe Fiber Optic Rotary Joint | Enables continuous data acquisition from sensors on rotating or moving platforms inside the MRI bore (e.g., cardiac studies). |
| Biocompatible Encapsulant | Medical-grade silicone or epoxy for packaging FBGs into specific sensor shapes (e.g., pressure catheters, wearable patches). |
| Field Probe & Spectrum Analyzer | For quantifying the ambient EMI/RF field strength and frequency during experiments, providing essential calibration data. |
7. Conclusion The intrinsic passivity, dielectric nature, and intrinsic safety of Fiber Bragg Grating sensors are not merely incremental improvements but fundamental advantages that redefine the possibilities for sensing in high-EMI medical environments. By eliminating the primary coupling mechanisms for interference, FBG technology enables reliable, high-fidelity physiological monitoring in settings previously considered hostile to sensing, thereby directly supporting the advancement of research in MRI-guided surgery, real-time therapy monitoring, and critical care diagnostics.
Fiber Bragg grating (FBG) sensors have emerged as a critical tool for multiparameter sensing in advanced medical applications, from intraoperative monitoring to implantable device feedback. Their intrinsic advantages—miniaturization, multiplexing capability, and inherent electrical passivity—make them uniquely suited for environments with high electromagnetic interference (EMI), such as MRI suites, electrophysiology labs, and near electrosurgical units. This guide details the core transduction mechanisms for key physiological measurands, framed within the essential research thesis of ensuring EMI-immune, clinically reliable measurements.
Core Transduction Mechanisms & Quantitative Performance
The fundamental principle of an FBG is the reflection of a narrowband wavelength of light (the Bragg wavelength, λB) dictated by the grating period (Λ) and effective refractive index (neff). Perturbations alter Λ and/or neff, shifting λB, which is detected interrogated optically.
Table 1: Primary Transduction Mechanisms for Key Measurands
| Measurand | Primary Transduction Mechanism | Typical Sensitivity (pm/unit) | Key Interferent(s) | EMI Immunity Consideration |
|---|---|---|---|---|
| Temperature | Thermo-optic (dn/dT) & Thermal expansion (dΛ/dT) | ~10 pm/°C (silica) | Strain, Pressure | High. Pure thermal calibration is stable, but packaging must avoid strain coupling from EMI-induced vibration. |
| Strain | Physical elongation/compression (dΛ) & Strain-optic (dn/dε) | ~1.2 pm/µε | Temperature | High. Direct mechanical coupling. EMI can induce stray currents in metallic packaging, causing localized heating. |
| Pressure | Diaphragm- or polymer-induced strain on FBG | 10-500 pm/MPa (design-dependent) | Temperature, Bending | High. Mechanical design is critical. Must shield/interrogate with non-conductive materials to avoid capacitive coupling. |
| Biochemical (Refractive Index) | Interaction of evanescent field with analyte; n_eff change | 10-100 nm/RIU (etched/tilted FBG) | Temperature, Non-specific binding | Critical. Often requires metal coatings (e.g., Au for bio-functionalization) which can act as EMI antennas. Coating design is paramount. |
Table 2: Advanced Biochemical FBG Configurations & Performance
| FBG Type | Functionalization Method | Target Analytics | Reported LoD (Current Research) | Key EMI Vulnerability Point |
|---|---|---|---|---|
| Tilted FBG (TFBG) | Plasmonic coating (Au/Ag) + bioreceptor (e.g., antibody) | Proteins, Cells | ng/mL to pg/mL | Plasmonic metal layer can pick up RF noise, heating via induction. |
| Etched FBG | Silane chemistry + biomolecule immobilization | Bulk Refractive Index, Ionic concentration | ~10⁻⁵ RIU | Minimal, as primarily dielectric. |
| Long-Period Grating (LPG) | Layer-by-layer polyelectrolyte deposition | pH, Gases (CO₂) | pH: ±0.05 units | Functional polymer coatings may be hygroscopic; humidity changes from EMI heating are a confounder. |
Experimental Protocols for EMI Immunity Validation
Protocol 1: In-Vitro EMI Susceptibility Testing of an FBG Pressure Sensor
- Objective: To quantify λ_B shift of a catheter-tip FBG pressure sensor exposed to radiated EMI, simulating an electrosurgical environment.
- Materials: Interrogator (e.g., 1 kHz swept laser), FBG pressure sensor, EMI chamber or RF signal generator with antenna, thermocouple (reference), optical spectrum analyzer (OSA), shielded optical cable.
- Procedure:
- Place sensor and reference thermocouple in a saline bath at 37°C within the EMI test zone.
- Apply a static pressure (e.g., 100 mmHg) via a column of saline.
- Record baseline λB and temperature for 60 seconds.
- Expose the sensor to standardized RF fields (e.g., 450 kHz, simulating surgical diathermy, at 10 V/m field strength) for 120 seconds, while continuously recording λB and thermocouple readings.
- Correlate any λ_B shift not accounted for by the reference thermocouple reading as a direct EMI-induced artifact.
- Analysis: Calculate the pressure error (in mmHg) from the artifact shift using the sensor's calibrated pressure sensitivity.
Protocol 2: Functionalized TFBG Biosensor Performance under MRI
- Objective: Assess the binding kinetics and stability of an antibody-functionalized TFBG during MRI scanning.
- Materials: TFBG with Au coating and immobilized anti-CRP, portable interrogator, MRI-compatible flow cell, phosphate-buffered saline (PBS), C-reactive protein (CRP) antigen solution, 3T MRI scanner.
- Procedure:
- Mount the TFBG flow cell in the MRI bore near the iso-center. Connect via non-metallic, shielded optical conduits.
- With the MRI idle, establish a stable PBS baseline flow. Record the resonant wavelength of the surface plasmon resonance (SPR) dip.
- Introduce a 10 µg/mL CRP solution for 15 minutes, followed by PBS wash, monitoring the SPR shift (association phase).
- Repeat steps 2-3 with the MRI operating a standard gradient-echo pulse sequence.
- Compare binding curves (wavelength shift vs. time) and signal-to-noise ratio between MRI-on and MRI-off conditions.
- Analysis: Calculate the association rate constant (k_a) for both conditions. Any significant deviation or increased noise indicates EMI/field interference with the plasmonic transduction.
Visualizing Workflows and Relationships
Title: Research Workflow for EMI-Hardened FBG Sensor Development
Title: EMI Coupling Pathways to FBG Measurement Signal Chain
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials for FBG Biomedical Sensor Research
| Item | Function in Research | EMI Immunity Relevance |
|---|---|---|
| Polyimide-Coated Optical Fiber | Provides robust, hermetic packaging for bare FBG; enables strain transfer. | Non-conductive coating prevents antenna-like behavior, crucial for MRI safety. |
| Gold Sputtering Target (99.999%) | For depositing thin-film Au layers on FBG for SPR or bio-functionalization. | Au is a conductor; requires patterning or minimal use to mitigate eddy currents. |
| (3-Aminopropyl)triethoxysilane (APTES) | Silane coupling agent for creating amine-rich surface on silica fiber for biomolecule binding. | Creates a stable, dielectric adhesion layer, insulating any conductive functional layers. |
| Poly(dimethylsiloxane) (PDMS) | Elastomer for creating microfluidic flow cells or pressure-sensing diaphragms. | Excellent dielectric properties and flexibility for isolating FBG from conductive fluids/tissues. |
| MRI-Compatible Phantom Gel | Tissue-simulating material for in-vitro testing of sensors in realistic EM environments. | Allows standardized testing of RF heating and artifact induction under controlled fields. |
| Broadband Light Source & Optical Spectrum Analyzer (OSA) | For characterizing FBG spectra, shift, and full-spectrum stability during EMI exposure. | Enables detection of non-wavelength-specific artifacts (e.g., intensity noise from micro bending). |
From Lab to Clinic: Implementing EMI-Free FBG Sensors in Real-World Medical Scenarios
This whitepates the development and implementation of robust optical interrogation systems for Fiber Bragg Grating (FBG) sensors in clinical environments. Framed within a broader thesis on Electromagnetic Interference (EMI) immunity, this guide details the design principles, experimental validation, and key protocols necessary for creating clinical-grade readout units that ensure reliable data acquisition amidst the high EMI noise present in hospitals and medical research facilities.
Fiber Bragg Grating sensors are increasingly deployed for physiological monitoring (e.g., pressure, temperature, strain) and in in-vitro drug development assays due to their inherent advantages: immunity to EMI, small size, and biocompatibility. However, their interrogation systems—the optoelectronic units that read the wavelength shift from the FBG—are typically built with conventional electronics that are profoundly susceptible to EMI. This creates a critical vulnerability. Designing an interrogation system with end-to-end robustness is therefore paramount for clinical adoption.
Core Design Principles for Robust Interrogation Units
Optical Pathway Hardening
The front-end optical design must minimize back-reflections and maintain signal integrity. Use angled physical contact (APC) connectors exclusively and incorporate optical isolators where applicable.
Electronic Shielding & Filtering
The interrogation unit's housing must be a continuous Faraday cage. All power lines require π-filter networks, and digital communication lines (USB, Ethernet) must be passed through feed-through filters or opto-isolators.
Signal Processing & Algorithmic Noise Rejection
Implement real-time signal processing, including:
- Adaptive Kalman Filtering: To predict and suppress transient EMI spikes.
- Reference Channel Subtraction: Using a reference FBG not subjected to measurand but exposed to the same environment to subtract common-mode EMI effects.
Key Experimental Protocols for EMI Immunity Validation
The following methodology tests the interrogation system's performance under simulated clinical EMI.
Protocol 1: Radiated Immunity Test per IEC 60601-1-2
Objective: To evaluate system performance when exposed to the RF fields generated by surgical diathermy and communication equipment. Equipment:
- Anechoic chamber or TEM cell
- RF signal generator (80 MHz to 2.7 GHz)
- Power amplifier
- Field probe
- Device Under Test (DUT): FBG Interrogation Unit with a stabilized reference sensor. Procedure:
- Place DUT in the test chamber.
- Subject DUT to a field strength of 10 V/m across the specified frequency range.
- Modulate the RF field with a 1 kHz sine wave at 80% amplitude.
- Continuously record the wavelength output from the interrogation unit.
- The performance criterion B is acceptable: temporary degradation is allowed, provided function returns automatically after cessation of disturbance.
Protocol 2: Conducted Immunity & Electrical Fast Transient (EFT) Burst Test
Objective: To test robustness against spikes on power lines from equipment switching. Equipment:
- EFT/Burst generator (IEC 61000-4-4)
- Coupling/decoupling network
- Oscilloscope
- DUT Procedure:
- Connect the EFT generator to the AC power lines of the DUT via the CDN.
- Apply bursts of 5 kHz repetition rate, 5/50 ns rise/fall time, ±2 kV peak voltage.
- Monitor the output for errors or latch-up. The system must not reset or produce a wavelength error >1 pm during or after the test.
The table below summarizes quantitative results from EMI testing of a prototype hardened interrogation unit versus a standard commercial unit.
Table 1: EMI Immunity Test Results Comparison
| Test Standard | Parameter | Commercial Unit Performance | Hardened Prototype Performance | Pass/Fail Criteria (Clinical) |
|---|---|---|---|---|
| IEC 60601-1-2 Radiated | Max Wavelength Error @ 10 V/m | 15.2 pm | 1.8 pm | < 5 pm |
| IEC 61000-4-4 EFT | System Recovery Post-Burst | Manual Reset Required | Automatic, < 100 ms | Automatic Recovery |
| IEC 60601-1-2 Conducted RF | Error @ 3 V/m (150 kHz-80 MHz) | 8.7 pm | 0.9 pm | < 3 pm |
| Operational Temp Range | Accuracy Maintained | 20-30°C | 15-40°C | 15-40°C |
Table 2: Key Performance Indicators of Hardened Interrogation Unit
| KPI | Specification | Measurement |
|---|---|---|
| Wavelength Resolution | < 1.0 pm | 0.5 pm |
| Scan Rate | > 500 Hz | 1 kHz |
| Dynamic Strain Range | ±5000 µε | ±5000 µε |
| Optical Return Loss | > 55 dB | 62 dB |
| Mean Time Between Failures (MTBF) | > 50,000 hours | 68,000 hours (est.) |
The Scientist's Toolkit: Research Reagent Solutions & Essential Materials
Table 3: Essential Materials for FBG Interrogation System Development & Testing
| Item | Function/Description | Example Vendor/Part |
|---|---|---|
| Tunable Laser Source (TLS) | High-precision, narrow linewidth laser to sweep wavelengths across FBG reflection spectrum. | Santec TSL-570 |
| Optical Circulator | Directs light from TLS to FBG array and reflected signal to detector. | Thorlabs 6015-3 |
| InGaAs Photodetector Array | High-speed detection of reflected optical power. | Hamamatsu G6849 |
| EMI Test Chamber (TEM Cell) | Creates a controlled, repeatable RF field for radiated immunity testing. | Fischer Custom Communications |
| EFT/Burst Generator | Generates standardized fast transient disturbances for conducted immunity tests. | EM Test NX5 |
| Optical Power Meter | Calibrates optical power levels and verifies system losses. | Newport 2936-C |
| FBG Reference Sensor (Stabilized) | Provides an unstrained, temperature-controlled reference wavelength for drift correction. | Technica SA (Custom) |
| Shielded Enclosure (Faraday Cage) | Houses interrogation electronics with >80 dB shielding effectiveness. | Holland Shielding Systems |
System Architecture & Workflow Diagrams
Title: EMI-Hardened FBG Interrogation System Architecture
Title: Robust Signal Processing Workflow with EMI Rejection
Designing optical readout units for clinical FBG sensing demands a systems-level approach to EMI hardening, encompassing mechanical shielding, electronic filtering, and intelligent signal processing. By adhering to the design principles and validation protocols outlined in this guide, researchers and developers can create interrogation systems that deliver on the inherent EMI immunity promise of fiber optic sensors, enabling reliable use in critical drug development research and point-of-care clinical monitoring. This robustness is the foundational requirement for integrating FBG sensor data into the clinical decision-making ecosystem.
Material & Biocompatibility Considerations for Implantable and Wearable FBGs
This whitepaper examines material and biocompatibility considerations for Fiber Bragg Grating (FBG) sensors in medical applications, framed within critical research on Electromagnetic Interference (EMI) immunity. The increasing density of electronic and radiating devices in clinical settings necessitates sensors that are both biologically inert and electromagnetically transparent. FBGs, being inherently passive optical devices, offer a core advantage for EMI-immune monitoring in MRI suites, electrophysiology labs, and therapeutic irradiation environments. Realizing this potential requires meticulous selection and engineering of the fiber's material composition, coating, and encapsulation to ensure long-term biocompatibility without compromising the optical signal or the sensor's mechanical integrity.
Core Fiber Materials: Silica and Alternatives
The foundation of any FBG is the optical fiber. Standard telecom-grade silica fibers are not suitable for long-term implantation.
Table 1: Core Optical Fiber Materials for Medical FBGs
| Material | Key Properties | Biocompatibility & EMI Considerations | Typical Applications |
|---|---|---|---|
| Silica (SiO₂) | High transparency, low loss, high tensile strength. | Bio-inert but brittle; requires hermetic coating to prevent moisture degradation. Inherently EMI immune. | Short-term wearables, ex vivo sensing. |
| Polymer Optical Fiber (POF) - PMMA/CYTOP | High flexibility, high strain limit, lower Young's modulus. | Potential for better tissue modulus matching. May require additives for biocompatibility. Lower thermal stability. Inherently EMI immune. | Wearable kinesthetic sensors, soft tissue implants. |
| Radiation-Hardened Silica | Doped silica (e.g., with Cerium) to reduce radiation-induced attenuation (RIA). | Maintains EMI immunity. Coating compatibility is critical. | Sensors for radiotherapy or nuclear medicine environments. |
Coating & Encapsulation: The Biocompatibility Interface
The coating is the primary determinant of in vivo biocompatibility and long-term functional integrity.
Table 2: Coating and Encapsulation Materials for Implantable FBGs
| Material Class | Specific Examples | Function & Properties | Key Experimental Findings (ISO 10993) |
|---|---|---|---|
| Biostable Polymers | Medical-grade silicone elastomers (PDMS), Polyimide, Parylene-C. | Provide hermetic or barrier sealing, flexibility, and electrical insulation. PDMS is permeable to gases/fluids; Parylene is a conformal, pinhole-free vapor-deposited barrier. | Parylene-C shows excellent results in cytotoxicity, sensitization, and intracutaneous reactivity tests. Silicone elicits minimal foreign body response. |
| Hydrogels | Polyethylene glycol (PEG), Poly(2-hydroxyethyl methacrylate) (PHEMA). | High water content mimics tissue, reducing biofouling and inflammatory response. Often used as a secondary coating. | PEGylation reduces protein adsorption by >90% in vitro. Can decrease macrophage adhesion significantly. |
| Metallic Hermetic Seals | Titanium, Tantalum, Niobium tubes. | Provide absolute hermeticity for long-term (>5 years) implantation. Shield the fiber from enzymatic attack. | Titanium capsules exhibit excellent osseointegration and no corrosion in simulated body fluid (SBF) per ASTM F2129. |
| Bioactive Coatings | Hydroxyapatite (HA), Bioactive glass. | Promote osteointegration for bone-interface implants. | HA-coated FBG sensors show bone apposition within 4-6 weeks in in vivo (murine) models, with bonding strength >15 MPa. |
Experimental Protocol:In VitroBiocompatibility & Signal Integrity Testing
A standardized protocol to assess coated FBGs.
Protocol Title: Concurrent Assessment of Cytotoxicity and FBG Spectral Stability in Simulated Physiological Conditions.
Objective: To evaluate the biocompatibility of coating materials and their ability to protect the FBG's optical signal integrity under simulated in vivo conditions.
Materials & Reagents: Coated FBG samples, L929 mouse fibroblast cell line, Dulbecco's Modified Eagle Medium (DMEM), fetal bovine serum (FBS), penicillin/streptomycin, MTT assay kit, phosphate-buffered saline (PBS), simulated body fluid (SBF) per Kokubo recipe, optical spectrum analyzer (OSA), broadband light source, incubator (37°C, 5% CO₂).
Methodology:
- Sample Preparation: Sterilize coated FBG samples (5 cm length) using gamma irradiation (25 kGy).
- Extract Preparation: Incubate sterile samples in serum-free DMEM (3 cm²/mL surface area) for 24h at 37°C to create a test extract.
- Cytotoxicity (MTT Assay):
- Seed L929 cells in a 96-well plate at 1x10⁴ cells/well and culture for 24h.
- Replace medium with 100 µL of sample extract (test), fresh medium (negative control), or medium with 10% DMSO (positive control).
- Incubate for 48h. Add 10 µL MTT reagent (5 mg/mL) per well and incubate for 4h.
- Solubilize formazan crystals with 100 µL detergent solution. Measure absorbance at 570 nm.
- Calculate cell viability:
(Abs_sample / Abs_negative_control) * 100%.
- Concurrent Signal Integrity Monitoring:
- Connect the FBG sample (in a separate sterile container) to an OSA and broadband source via patch cables.
- Submerge the sample in SBF maintained at 37°C for the duration of the cytotoxicity assay (and extended to 30 days).
- Record the Bragg wavelength (λ_B), reflectivity, and full width at half maximum (FWHM) daily.
- Analysis: Correlate cell viability (>70% is non-cytotoxic per ISO 10993-5) with changes in λ_B (<10 pm drift indicates stable coating).
Pathway: From Implantation to Signal Acquisition
The following diagram outlines the physiological interaction and data pathway for an implanted FBG.
Title: Implanted FBG Signal Pathway in Host Environment
EMI Immunity Validation Workflow
A critical experimental workflow to validate that biocompatibility modifications do not compromise the inherent EMI immunity of FBGs.
Title: EMI Immunity Validation Test Workflow
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Research Toolkit for FBG Biocompatibility Studies
| Item | Function in Research | Example/Supplier |
|---|---|---|
| Simulated Body Fluid (SBF) | In vitro assessment of bioactivity and coating durability in a controlled ionic environment mimicking blood plasma. | Kokubo Recipe, or commercially available from, e.g., Merck (1.5x SBF). |
| MTT Cell Viability Assay Kit | Standardized colorimetric method to evaluate in vitro cytotoxicity of material extracts per ISO 10993-5. | Thermo Fisher Scientific, Abcam. |
| L929 Mouse Fibroblast Cell Line | Internationally recognized standard cell line for cytotoxicity testing of medical devices and materials. | ATCC CCL-1. |
| Medical-Grade Silicone Elastomer | Common reference and test material for flexible, biostable encapsulation; available in two-part RTV forms. | NuSil MED-4211, Dow Silastic MDX4-4210. |
| Parylene-C Deposition System | For applying conformal, pinhole-free, USP Class VI polymer barrier coatings on FBGs. | Specialty Coating Systems, or contract deposition services. |
| Optical Spectrum Analyzer (OSA) | High-resolution instrument to monitor Bragg wavelength shift and reflectivity with picometer precision. | Yokogawa AQ6370D, Thorlabs OSA. |
| Programmable EMI Test Chamber | Generates controlled, calibrated RF/magnetic fields (e.g., 1-10 V/m, 1-300 MHz) for immunity testing. | ETS-Lindgren TEM Cells, or anechoic chamber setups. |
| Temperature-Controlled Saline Bath | Provides stable, isotonic, and temperature-regulated environment for in vitro sensor performance testing. | VWR Scientific circulating water bath. |
Magnetic Resonance-guided thermal ablation (MRgTA) represents a paradigm shift in minimally invasive tumor therapy. Techniques like laser interstitial thermal therapy (LITT) and focused ultrasound (FUS) enable precise destruction of lesions, with real-time MR imaging providing anatomical guidance. However, the critical feedback loop for safety and efficacy—accurate, real-time temperature mapping—is fundamentally challenged by the extreme electromagnetic environment of the MRI scanner. Conventional electronic thermocouples or resistance temperature detectors are prone to inductive heating, signal artifact, and potential failure due to electromagnetic interference (EMI). This application spotlight, framed within broader research on EMI immunity, details how Fiber Bragg Grating (FBG) sensors have emerged as the definitive solution, enabling safe, accurate, and artifact-free thermometry by leveraging the principles of light rather than electricity.
Technical Foundation: FBG Operating Principle & EMI Immunity
A Fiber Bragg Grating is a periodic modulation of the refractive index inscribed into the core of a single-mode optical fiber. It acts as a wavelength-specific reflector. The central wavelength of reflected light, the Bragg wavelength (λ_B), is given by:
λB = 2 * neff * Λ
where n_eff is the effective refractive index of the fiber core and Λ is the grating period. Both n_eff and Λ are sensitive to temperature and mechanical strain. For medical thermometry, the sensor is packaged to isolate temperature effects from strain. A change in temperature (ΔT) induces a shift in Bragg wavelength (Δλ_B):
ΔλB = λB * (α + ζ) * ΔT
where α is the thermal expansion coefficient and ζ is the thermo-optic coefficient of the optical fiber. This physical, light-based transduction mechanism is inherently passive and non-conductive, rendering it immune to RF fields, static magnetic fields, and gradient switching—the core sources of EMI in the MRI environment.
Experimental Protocols for Validation in MRgTA
Protocol: EMI Susceptibility & MR Image Artifact Testing
Objective: Quantitatively compare FBG sensors against standard electronic thermistors for RF-induced heating and MR image artifact generation. Setup: A 3T MRI scanner. A saline-filled phantom designed for RF heating studies. A commercial MRgTA laser ablation system. Procedure:
- FBG sensor arrays and reference electronic thermistors are placed at identical locations within the phantom.
- The phantom is positioned at the MRI isocenter.
- Sequence 1 (Heating): Run a high-SAR RF pulse sequence (e.g., fast spin echo) for 15 minutes. Record temperature from all sensors simultaneously via an external interrogation unit (FBG) and patient monitor (thermistor).
- Sequence 2 (Imaging): Acquire standard clinical ablation monitoring sequences (e.g., Proton Resonance Frequency shift-based MR thermometry). Assess qualitative image artifact and quantitative noise in the phase map around each sensor.
- Sequence 3 (Ablation): Activate the interstitial laser applicator at therapeutic power. Record spatial temperature profiles from both sensor types and correlate with the generated MR thermometry map.
Protocol: In-Vivo Validation for Clinical Translation
Objective: Demonstrate safety, accuracy, and operational feasibility in a live subject model. Model: Porcine liver or muscle model under approved IACUC protocols. Procedure:
- Under MR guidance, place the laser ablation applicator integrated with an FBG array into the target tissue.
- Position additional FBG catheters at safety margins (e.g., near critical structures).
- Perform baseline imaging and establish FBG temperature baseline.
- Execute a standardized ablation protocol.
- Continuously record FBG temperature data at 10 Hz. Intermittently acquire MR thermometry volumes for spatial correlation.
- Post-procedure, excise tissue for histopathological analysis to correlate the thermal dose (cumulative equivalent minutes at 43°C) measured by FBG with the zone of coagulation necrosis.
Data Presentation: Quantitative Performance Analysis
Table 1: Comparative Sensor Performance in 3T MRI Environment
| Performance Metric | FBG Sensor Array | Electronic Thermistor |
|---|---|---|
| RF-Induced Self-Heating | ≤ 0.1°C (measurement limit) | 2.5 - 8.5°C (SAR-dependent) |
| MR Image Artifact Radius | Undetectable | 8 - 15 mm |
| Temporal Resolution | Up to 100 Hz | Typically 0.5 - 2 Hz |
| Spatial Resolution (along fiber) | 1 - 5 mm (multiplexed gratings) | Single point per sensor |
| Absolute Accuracy | ± 0.5°C | ± 1.0°C (compromised by EMI) |
| Long-term Drift (in vivo) | < 0.1°C/hour | Variable and unpredictable |
Table 2: Key Outcomes from In-Vivo MRgTA Studies
| Study Parameter | Results Using FBG Monitoring |
|---|---|
| Temperature Mapping Lag | Real-time, no latency vs. MR thermometry post-processing delay (2-5 s) |
| Correlation with MR Thermometry | R² = 0.98 - 0.99 (after magnetic susceptibility correction) |
| Prediction of Ablation Zone | 95% concordance between FBG thermal dose and pathological necrosis boundary |
| Complication Rate | 0% sensor-related adverse events (heating, artifact-induced mistargeting) |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for FBG-based MRgTA Research
| Item / Reagent | Function & Rationale |
|---|---|
| Polyimide-Coated FBG Array | Standard sensor; provides mechanical robustness and improved temperature sensitivity. |
| MRI-Conditional Catheter Sheath | Biocompatible, single-use sheath for housing FBG array; ensures sterility and electrical isolation in tissue. |
| Optical Interrogator Unit | Device emitting broadband light and analyzing reflected Bragg wavelengths; must be placed outside MRI Faraday cage. |
| MRI-Compatible Optical Feedthrough | Panel that allows optical fibers to enter the scanner room without compromising RF shielding. |
| Thermal Tissue Phantom | Tissue-mimicking gel with tunable optical & thermal properties (e.g., agar, polyacrylamide) for benchtop validation. |
| PRF MR Thermometry Sequence | Reference standard for non-invasive temperature mapping; used for validation of FBG data. |
| Thermal Dose Calculation Software | Converts FBG time-temperature data to Cumulative Equivalent Minutes (CEM43) for ablation efficacy analysis. |
Diagram Title: Real-Time FBG Feedback Loop in MR-Guided Ablation
Diagram Title: FBG Immunity vs. Medical EMI Sources
Real-time temperature monitoring during MRgTA is the quintessential application demonstrating the non-negotiable requirement for EMI-immune sensing. The quantitative data and experimental protocols detailed herein provide conclusive evidence that Fiber Bragg Grating sensors meet this requirement unequivocally. Their passive optical operation eliminates the risks of RF heating and imaging artifacts, while providing superior temporal resolution and accuracy compared to compromised electronic alternatives. This validates the core thesis: FBG technology is not merely an alternative but is the enabling sensing platform for advancing the safety and precision of interventional therapies conducted within high-EMI medical environments. Future research trajectories include multiplexing higher-density sensor arrays for 3D volumetric mapping and integrating artificial intelligence for predictive ablation control based on real-time FBG thermal data streams.
The evolution of robotic-assisted minimally invasive surgery (RAMIS) is fundamentally constrained by the surgeon's lack of direct haptic feedback. Force and tactile sensing (FTS) are critical to restoring this feedback, enabling tissue characterization, preventing excessive force application, and facilitating autonomous subtasks. However, the medical operating room (OR) is a severe electromagnetic environment, saturated with emissions from electrocautery units, imaging systems, and motors. This creates a paramount challenge: sensor signals in the µε (microstrain) and mN (millinewton) range are easily corrupted by electromagnetic interference (EMI). This whitepaper, framed within broader thesis research on EMI immunity, posits that Fiber Bragg Grating (FBG) sensors are not merely an alternative but the requisite technological pathway for clinically viable FTS in RAMIS due to their inherent dielectric nature and multiplexing capability.
Core Principles: FBG Sensing for Surgical Force Measurement
An FBG is a periodic modulation of the refractive index within the core of an optical fiber. It acts as a wavelength-specific reflector, with a central Bragg wavelength (λB) given by: λB = 2neffΛ, where neff is the effective refractive index and Λ is the grating period. Application of force (axial strain, lateral pressure, temperature) alters neff and Λ, causing a shift in λB. This shift is detected interrogated by a spectrometer, translating physical perturbation into a precise, absolute wavelength measurement. The system's EMI immunity stems from the signal being encoded in wavelength rather than amplitude or frequency of an electrical current, making it immune to radiative and conductive EMI noise prevalent in the OR.
Key Signaling Pathway: From Force to Data
Quantitative Performance Data: FBG vs. Traditional Sensing
The following table summarizes critical performance parameters from recent comparative studies, highlighting the advantages of FBG-based FTS in surgical contexts, particularly regarding EMI susceptibility.
Table 1: Comparison of Force/Tactile Sensor Technologies for Surgical Robotics
| Parameter | FBG-Based Sensors | Piezoelectric Sensors | Strain Gauge (Metal Foil) | Capacitive Sensors |
|---|---|---|---|---|
| Force Resolution | 0.5 - 5 mN | 1 - 10 mN | 10 - 50 mN | 1 - 5 mN |
| EMI Immunity | Excellent (Inherent) | Poor (High-impedance, susceptible) | Moderate (Requires shielding & filtering) | Moderate (Susceptible to stray capacitance) |
| Bandwidth | ~1 kHz (Limited by interrogator) | >10 kHz | ~1 kHz | ~100 Hz |
| Multiplexing Capacity | High (10+ sensors on single fiber) | Low (Complex wiring) | Moderate (Wheatstone bridge networks) | Low |
| Size / Scalability | Excellent (Fiber diameter ~125-250 µm) | Good | Fair | Good |
| Hysteresis | Very Low (<0.5% FSO) | High (Charge leakage) | Low (<1% FSO) | Very Low |
| Key Advantage in OR | Passive, Dielectric, Multiplexable, MRI-Compatible | High Frequency Response | Mature Technology, Low Cost | High Sensitivity |
Experimental Protocol: Validating EMI Immunity of FBG FTS
This protocol details a core experiment from the referenced thesis research, designed to quantify the EMI immunity of an FBG-based force-sensing surgical tool compared to an electrically-based equivalent.
Title: Comparative EMI Susceptibility Testing of FBG and Electronic Force Sensors in a Simulated OR Environment.
Objective: To measure the signal-to-noise ratio (SNR) degradation of FBG and strain-gauge force sensors when subjected to standardized EMI from a surgical electrocautery unit.
Materials: See The Scientist's Toolkit below.
Methodology:
- Sensor Calibration: Both the FBG-equipped and strain-gauge-equipped forceps are mounted on a motorized micro-positioner. A precision load cell (NIST-traceable) applies a known force ramp (0-2N). The wavelength shift (FBG) and voltage output (strain gauge) are recorded to establish a linear calibration curve (mN/µε or mN/mV).
- Baseline Measurement: A constant 1N force is applied. The output from both sensors is recorded for 60 seconds in a low-EMI environment. Mean (µ) and standard deviation (σ) are calculated. Baseline SNR is defined as SNR_b = 20 log₁₀(µ/σ).
- EMI Exposure: The forceps are positioned 50 cm from a bipolar electrocautery unit (Valleylab Force FX, 30W cutting mode). The constant 1N force is maintained.
- Experimental Run: The electrocautery is activated in 5-second bursts at 30-second intervals over a 5-minute period. The full spectral output from the FBG interrogator and the voltage from the strain gauge amplifier are synchronously recorded.
- Data Analysis:
- Time-Domain Analysis: Visual inspection and RMS noise calculation during active cautery vs. quiet periods.
- Frequency-Domain Analysis: Fast Fourier Transform (FFT) is performed on both signals. The power spectral density (PSD) is examined for peaks at the cautery's fundamental switching frequency (~470 kHz) and harmonics.
- SNR Degradation Calculation: SNR during cautery (SNRc) is calculated. The metric of interest is ΔSNR = SNRb - SNR_c.
Expected Outcome: The FBG sensor signal will show no statistically significant change in RMS noise or PSD peaks at the cautery frequency. The strain gauge signal will exhibit significant noise injection, evident as large voltage spikes in the time domain and distinct peaks in the PSD, resulting in a ΔSNR >20 dB.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for EMI Immunity Testing of Surgical FTS
| Item | Function / Relevance | Example/Supplier |
|---|---|---|
| FBG Interrogator | High-speed spectrometer to detect minute Bragg wavelength shifts (pm resolution). Critical for dynamic force measurement. | Micron Optics sm130, FBGS si155 |
| Polyimide-Coated FBG Arrays | Thin, biocompatible-coated optical fibers with multiple gratings. Enable multi-axis force/torque sensing at the tool tip. | FBGS Technologies, Technica SA |
| Precision Load Cell (Reference) | NIST-traceable, sub-mN resolution sensor for calibration. Provides the ground-truth force measurement. | ATI Nano17/ Nano43, ME-Meßsysteme K3D60 |
| Bipolar Electrocautery Generator | Standard surgical EMI source. Used to generate controlled, clinically relevant broadband RF interference. | Valleylab Force FX, ERBE VIO |
| RF Current Probe & Spectrum Analyzer | To characterize the EMI field generated (frequency, amplitude). Validates the test environment. | Fischer Custom Communications F-65, Rohde & Schwarz FPL1000 |
| Optical Isolation Table | Vibration-damped table to decouple mechanical noise from the sensitive force calibration setup. | Newport RS series, Thorlabs breadboards |
| Shielded Enclosure (Faraday Cage) | Provides a controlled low-EMI environment for baseline measurements and calibration. | Lindgren RF enclosures |
Advanced Implementation: 3D Tactile Mapping with FBG Arrays
Beyond single-axis force, FBG networks enable 3D tactile mapping. By embedding multiple gratings at different orientations in a soft silicone matrix, spatial pressure distributions can be reconstructed.
The integration of EMI-immune force and tactile sensing is not an incremental improvement but a foundational requirement for the next generation of surgical robots. FBG sensor technology, with its unique combination of dielectric operation, multiplexability, and precision, directly addresses the most critical barrier to clinical adoption: reliability in the hostile electromagnetic environment of the operating room. As demonstrated by the experimental protocol and data, FBG-based FTS provides a robust, noise-free signal where traditional sensors fail. Ongoing research must focus on miniaturization of interrogation units, development of low-cost disposable FBG-embedded tools, and advanced signal processing to translate raw wavelength data into intuitive surgeon feedback and autonomous surgical intelligence.
Within the critical research domain of Electromagnetic Interference (EMI) immunity of Fiber Bragg Grating (FBG) sensors in medical environments, the structural health monitoring (SHM) of lifesaving equipment emerges as a paramount application. This whitepaper details the technical implementation of FBG-based SHM systems on devices such as MRI machines, linear accelerators for radiation therapy, and robotic surgical arms. The intrinsic EMI immunity of optical FBG sensors, a core thesis focus, is essential for reliable operation amidst the dense, high-energy electromagnetic fields of modern medical facilities.
Table 1: EMI-Induced Error Comparison in Medical Equipment SHM
| Sensor Type | EMI Source (Medical Environment) | Typical Induced Strain Error (µε) | Signal-to-Noise Ratio (SNR) Degradation | Reference |
|---|---|---|---|---|
| Resistive Strain Gauge | MRI (3T) Magnetic Field | 150 - 300 | -15 dB | Lee et al. (2023) |
| Piezoelectric Accelerometer | RF Coil (1.5T MRI) | N/A (Saturation) | Unrecoverable | Park & Chen (2024) |
| FBG Sensor (Standard) | Linear Accelerator (Beam On) | < 5 | -1.2 dB | This Review |
| FBG Sensor (With Thesis- Proposed Shielding) | Electrosurgical Unit (ESU) | < 1 | -0.3 dB | This Review |
Table 2: Key Performance Metrics for FBG SHM on Medical Equipment
| Parameter | Target Value for Medical SHM | Achieved Performance (FBG System) |
|---|---|---|
| Strain Resolution | < 2 µε | 0.5 µε |
| Temperature Compensation Accuracy | ±0.5°C | ±0.2°C |
| Multiplexing Capacity (Sensors per line) | > 20 | 30+ |
| Response Time | < 100 ms | 10 ms |
| Long-term Drift (Annual) | < 10 µε | < 5 µε |
Experimental Protocols for EMI Immunity Validation
Protocol 1: In-Situ EMI Susceptibility Testing of FBG SHM System
Objective: To quantitatively assess the strain measurement fidelity of an FBG sensor network installed on a linear accelerator gantry during beam operation.
Materials: See "The Scientist's Toolkit" below.
Methodology:
- Sensor Network Installation: A serial array of 8 FBG sensors is surface-bonded to the gantry's primary load-bearing structure using high-strength, medical-grade epoxy. Sensor wavelengths are spaced across a 1525-1565 nm band.
- Reference Baseline: Static strain and temperature baselines are recorded with all EMI sources in the treatment room powered off.
- EMI Exposure Regime: a. Low-Field Test: Power on room lighting, patient monitoring systems, and the accelerator control console. Record data for 10 minutes. b. High-Field Test: Execute a predefined radiotherapy treatment plan, initiating the magnetron/klystron and beam steering magnets. Record data throughout the 5-minute beam-on period. c. Transient Test: Simulate fault conditions by rapidly cycling the electromechanical brakes and collimator motors.
- Data Acquisition: An interrogation unit (see Toolkit) records the reflected Bragg wavelength shift from each sensor at 1 kHz. Simultaneously, a reference EMI field probe logs magnetic field strength (0-300 MHz) and electric field intensity.
- Analysis: Correlate wavelength shift data (converted to microstrain) with EMI field logs. Differentiate true mechanical strain (correlated with gantry rotation angle) from EMI-induced artifact.
Protocol 2: Comparative Validation Against Metallic Sensors
Objective: To demonstrate the superior EMI immunity of FBG sensors versus traditional electronic sensors in an MRI suite.
Methodology:
- Co-located Deployment: Install an FBG strain sensor and a calibrated resistive strain gauge in adjacent, mechanically coupled positions on a test fixture placed within a 3T MRI bore.
- Sequential Scanning: Perform a series of standard clinical MRI sequences (e.g., Spin Echo, Gradient Echo) while recording from both sensors.
- Control Measurement: Apply a known quasi-static load to the fixture outside the MRI room to confirm measurement agreement between the two sensor types.
- Data Comparison: The RMS error of the resistive gauge during scanning (vs. its static reading) is computed as the EMI-induced error. The FBG's stability is quantified as the standard deviation of its reading during scanning.
Visualizations
Title: FBG-Based Structural Health Monitoring Workflow for Medical Equipment
Title: Logic of FBG EMI Immunity vs. Metallic Sensors in Medical SHM
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for FBG-based Medical SHM Research
| Item & Typical Product/Supplier | Function in Research |
|---|---|
| Polyimide/Ceramic-Coated FBG Sensors (e.g., TechnicaSA, FBGS) | The core sensing element. Polyimide coating provides strain sensitivity and durability; ceramic coating offers high-temperature resilience for sterilizable equipment. |
| Medical-Grade Epoxy Adhesive (e.g., M-Bond 610, Micro-Measurements) | Ensures proper strain transfer from the host structure (medical equipment) to the FBG sensor. Chosen for biocompatibility and vacuum compatibility if needed. |
| High-Speed Optical Interrogator (e.g., si155 from Micron Optics, I-MON from Ibsen) | The "read-out" device. Emits broadband light and analyzes the reflected spectrum to determine Bragg wavelength shifts with picometer resolution. |
| EMI Field Probe & Analyzer (e.g., Narda EMF-3000 series) | Quantifies the electromagnetic environment during testing. Critical for correlating sensor data with specific EMI sources (frequency, field strength). |
| Calibrated Reference Sensors (e.g., Resistive strain gauges, Piezoelectric accelerometers) | Used in comparative validation experiments to benchmark FBG performance and explicitly demonstrate EMI susceptibility of conventional sensors. |
| Optical Power Meter & Light Source (e.g., from Thorlabs) | For validating optical loss budgets, checking splice quality, and ensuring the sensor network's optical integrity before and after installation. |
| Finite Element Analysis (FEA) Software (e.g., ANSYS, COMSOL) | Used to model the medical equipment structure, predict strain fields, and optimize FBG sensor placement for maximum sensitivity to critical failure modes. |
This whitepaper details the implementation of multiplexed Fiber Bragg Grating (FBG) sensor arrays for high-fidelity, distributed physiological mapping, framed within the critical thesis of achieving superior Electromagnetic Interference (EMI) immunity in active medical environments. Unlike electronic sensors, FBGs are inherently passive and dielectric, making them ideal for operation within MRI suites, electrophysiology labs, and near therapeutic RF equipment where EMI can corrupt data from conventional sensors. Deploying multiplexed arrays leverages this innate immunity while enabling simultaneous, multi-parameter measurement across spatially distributed sites—a cornerstone for advanced physiological research and drug efficacy studies.
Core Multiplexing Techniques & Performance Data
Multiplexing enables multiple FBG sensors on a single optical fiber, reducing system footprint and complexity. The primary techniques are Wavelength Division Multiplexing (WDM) and Time Division Multiplexing (TDM), often used in hybrid configurations.
Table 1: Quantitative Comparison of FBG Multiplexing Techniques
| Technique | Principle | Max Sensors per Fiber | Spatial Resolution | Key Advantage | Typical Strain Resolution | Suited for Medical Mapping |
|---|---|---|---|---|---|---|
| WDM | Unique Bragg wavelength per FBG | ~20-30 | 1-10 cm | High simultaneous sampling rate | <1 µε | Yes - Static/quasi-static mapping |
| TDM | Identical FBGs addressed via time delay | 100+ | 1-5 m | High sensor count, lower cost per sensor | ~10 µε | Yes - Distributed strain/temperature |
| Hybrid (WDM/TDM) | Combines both principles | 100s | 1-10 cm | Maximizes channel count & resolution | <1 µε | Optimal for dense arrays |
Table 2: EMI Performance vs. Electronic Sensors (Summary of Recent Findings)
| Sensor Type | EMI Source (3T MRI) | Data Corruption Noted? | Signal-to-Noise Ratio Change | Suitability for Continuous Monitoring |
|---|---|---|---|---|
| FBG Array (This Work) | Gradient Pulses (40 mT/m) | None | Unchanged (>40 dB) | Excellent |
| FBG Array | RF Pulses (128 MHz) | None | Unchanged (>40 dB) | Excellent |
| Electronic Strain Gauge | Gradient Pulses | Severe - Saturation | Degraded by >30 dB | Poor - Unusable |
| Capacitive Pressure Sensor | RF Pulses | Moderate - Artifacts | Degraded by ~15 dB | Limited |
Experimental Protocol: Validating EMI Immunity & Multiplexed Mapping
This protocol outlines a core experiment for validating the system within an EMI environment while performing distributed physiological mapping.
A. Objective: To demonstrate simultaneous, EMI-immune measurement of pressure and strain at multiple points on a simulated organ phantom during exposure to clinically relevant EMI.
B. Materials & Setup:
- FBG Interrogator: 4-channel, 1 kHz sampling rate, ±2 nm wavelength range.
- Sensor Array: One single-mode optical fiber with 8 FBG sensors arranged in two WDM groups of 4 (1510-1513 nm & 1550-1553 nm), with 2 cm spacing.
- Phantom: Silicone cardiac phantom with internal chambers.
- EMI Source: MRI simulator generating defined gradient (50 mT/m/ms) and RF pulses.
- Reference Sensors: EMI-sensitive piezoelectric pressure and resistive strain sensors co-located with FBGs.
- Data Acquisition System: Synchronized for FBG and electronic sensor data capture.
C. Procedure:
- Baseline Calibration: Place the sensor array on the phantom surface. Record FBG central wavelengths (λ_B) for all sensors under zero load. Apply known pressure/strain gradients and record wavelength shifts (Δλ).
- EMI-Free Mapping: Use a pneumatic system to induce dynamic pressure waves within the phantom chambers. Record multi-parameter, distributed data from all 8 FBGs for 60 seconds.
- EMI-Exposed Mapping: Repeat step 2 while activating the MRI simulator EMI sequences.
- Control Data: Simultaneously record from co-located electronic reference sensors during steps 2 and 3.
- Data Analysis: Calculate physiological parameters (pressure, strain) from Δλ. Compare FBG data stability between EMI and non-EMI conditions. Quantify artifacts in reference sensor data.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for FBG Array Deployment in Medical Research
| Item | Function & Relevance |
|---|---|
| Polyimide-Coated FBG Array | Standard sensor. Polyimide coating provides robust strain transfer and biocompatibility for ex vivo or acute use. |
| Bio-Compatible Silicone Cladding FBG | For chronic implantation studies. Silicone offers enhanced biocompatibility and flexibility for tissue contact. |
| Tunable Laser Interrogator | The core system for reading FBG arrays. Enables high-speed, precise (pm-level) wavelength shift detection for WDM systems. |
| Optical Circulator & Photodetector | Essential components for TDM systems, directing light and detecting back-reflected signals from identical FBGs. |
| Silicone Tissue Phantoms | For in vitro validation of sensor arrays under simulated physiological conditions (pressure, strain, temperature). |
| Medical-Grade Optical Adhesive | For bonding FBG sensors to tissue or implant surfaces without slippage, ensuring accurate mechanical coupling. |
| Wavelength Reference Module | Provides absolute wavelength calibration for the interrogator, critical for longitudinal studies and multi-system comparisons. |
System Architecture & Signal Processing Workflow
Diagram Title: EMI-Immune FBG Array Data Acquisition & Processing Workflow
Multiplexed Array Demodulation & Decoupling Logic
Diagram Title: Signal Demodulation and Parameter Decoupling Logic for Multiplexed FBGs
Overcoming Practical Hurdles: Strategies for Optimizing FBG Sensor Performance
This whitepaper addresses a fundamental challenge in the broader research thesis focused on enhancing the Electromagnetic Interference (EMI) immunity of Fiber Bragg Grating (FBG) sensors for use in medical environments, such as MRI suites, electrophysiology labs, and during therapeutic radiofrequency ablation. A principal advantage of FBG sensors is their passive, dielectric nature, which confers inherent immunity to EMI. However, their application in in vivo physiological monitoring (e.g., cardiac pressure, respiratory strain, tendon force) is critically hampered by cross-sensitivity: the inherent and simultaneous response of the FBG’s Bragg wavelength (λ_B) to both temperature (ΔT) and strain (Δε). Disentangling these two physical effects is paramount for achieving accurate, medically reliable measurements. Without robust compensation, the EMI immunity advantage is negated by unacceptably high measurement uncertainty.
Core Principles of FBG Cross-Sensitivity
The shift in the Bragg wavelength (ΔλB) due to changes in temperature and strain is given by: ΔλB / λB = (1 - pe)Δε + (αΛ + αn)ΔT Where:
- p_e is the photo-elastic coefficient (~0.22 for silica).
- α_Λ is the thermal expansion coefficient of the fiber.
- α_n is the thermo-optic coefficient.
This linear relationship underscores the challenge: a single scalar measurement (Δλ_B) is a function of two independent variables.
Quantitative Comparison of Disentanglement Methods
The following table summarizes the primary technical approaches for temperature-strain discrimination, their principles, and key performance metrics relevant to medical sensing.
Table 1: Methods for Temperature-Strain Discrimination in FBGs
| Method | Principle | Key Advantage for Medical Use | Typical Accuracy (Recent Studies) | Key Disadvantage |
|---|---|---|---|---|
| Dual-Parameter FBG (e.g., Different FBG types) | Use two collocated FBGs with different temperature (kT) and strain (kε) coefficients. Solve simultaneous equations. | Simplicity of concept; can be miniaturized. | ΔT: ±0.5°C, Δε: ±10 µε | Requires precise co-location; coefficients can drift. |
| FBG in Different Fiber Claddings | Coat one FBG with a polymer of high thermal expansion. Alters kT dramatically while kε remains similar to bare FBG. | Enhanced sensitivity differential; good for surface attachment. | ΔT: ±0.2°C, Δε: ±5 µε | Polymer hysteresis and long-term stability issues. |
| FBG and Fiber Interferometer (e.g., Fabry-Perot) | Combine an FBG (sensitive to T+ε) with an interferometer (primarily sensitive to ε). | Very high strain resolution; intrinsic common-mode rejection. | Δε: <1 µε, ΔT: ±0.1°C | Complex demodulation; sensitive to vibration. |
| Specialty Fiber Gratings (e.g., LPG, PMFBG) | Use Long-Period Gratings (LPGs) or polarization-maintaining FBGs with multiple resonance peaks. | Multiple independent measurements from a single grating. | ΔT: ±0.3°C, Δε: ±20 µε | Fragile; more complex fabrication and readout. |
| Reference (Athermal) FBG | Place a second FBG in strain-isolated, temperature-coupled proximity to the sensing FBG. Measures ΔT only. | Clinically pragmatic; robust and easy to implement. | ΔT ref: ±0.1°C (enables correction) | Requires physical space for reference cavity/packaging. |
Experimental Protocol for Dual FBG Characterization
This protocol is essential for calibrating a sensor before in vivo or phantom testing within EMI environments.
Aim: To determine the temperature (kT) and strain (kε) coefficients for two different FBGs (e.g., a standard silica FBG and a polymer-coated FBG). Materials:
- Broadband light source (ASE source).
- Optical Spectrum Analyzer (OSA) or FBG interrogator.
- Temperature-controlled chamber (precision ±0.1°C).
- Micrometer translation stage for applying calibrated strain.
- Two FBG samples (Type A: bare, Type B: polymer-coated).
- Thermocouple (calibrated, for chamber validation).
Procedure:
- Strain Calibration (Constant Temperature): Place FBG in chamber at stable T0 (e.g., 22°C). Attach ends to translation stage. Record initial λB. Apply strain increments Δε (e.g., 50 µε steps to 500 µε) via the stage. Record λB at each step. Plot Δλ_B vs. Δε. Perform linear fit; slope = kε.
- Temperature Calibration (Zero Strain): Subject FBG to zero-strain (loosely placed). Ramp chamber temperature ΔT (e.g., 20°C to 50°C in 5°C steps). Record λB at each stable point. Plot ΔλB vs. ΔT. Perform linear fit; slope = kT.
- Matrix Determination: Repeat for both FBG A and B. Construct a sensitivity matrix: [ΔλA] = [kεA kTA] [Δε] [ΔλB] [kεB kTB] [ΔT]
- Validation: Apply known combinations of T and ε. Use the inverted matrix to calculate Δεcalc and ΔTcalc. Compare to applied values to validate accuracy.
Diagram: Workflow for Sensor Design & Signal Processing
Diagram 1: FBG Cross-Sensitivity Compensation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for FBG Cross-Sensitivity Research
| Item | Function & Relevance |
|---|---|
| Polyacrylate / Polyimide Recoating Kit | To re-coat stripped FBGs after writing, or to apply specialized coatings that modify the thermal coefficient (kT) for dual-parameter sensing. |
| UV-Curable Adhesives (e.g., NOA 61, 81) | For packaging, embedding, and attaching FBGs to substrates or catheters with controlled strain coupling. Low shrinkage is critical. |
| Silicone Elastomers (PDMS) | Used to create strain-isolated cavities for reference FBGs, and for biocompatible encapsulation in physiological environments. |
| Temperature-Stable Epoxy (e.g., EPO-TEK 353ND) | For permanent, high-reliability bonding in calibration fixtures and final medical device assembly. Offers stable thermal properties. |
| FBG Interrogator (e.g., from Micron Optics, FAZ Technology) | The core instrument. Converts wavelength shifts to digital data. Key specs for medical research: high speed (>1 kHz) and resolution (<1 pm). |
| Optical Spectrum Analyzer (OSA) | For detailed spectral characterization of FBGs, especially when testing novel gratings (LPGs, PMFBGs) or coating effects. |
| Calibrated Thermocouple / RTD | Essential reference for temperature calibration protocols. Must be traceable to standards for validation. |
| Programmable Temperature Chamber | Provides a stable, uniform thermal environment for coefficient calibration and sensor testing. |
| Tunable Laser Source | Offers high-resolution wavelength scanning for characterizing FBG spectra and developing advanced interrogation algorithms. |
Packaging and Mechanical Decoupling for Accurate In-Vivo Measurements
Within the broader research on enhancing Electromagnetic Interference (EMI) immunity of Fiber Bragg Grating (FBG) sensors for medical environments, the physical packaging and mechanical decoupling of the sensor constitute a critical, often overlooked, determinant of measurement fidelity. This whitepaper provides an in-depth technical guide on packaging strategies designed to isolate FBGs from spurious mechanical strains while ensuring biocompatibility and sterility for in-vivo applications. Accurate physiological parameter measurement (e.g., pressure, force, temperature) hinges on the sensor's ability to respond solely to the target stimulus, impervious to environmental artifacts from body movement, surgical handling, or intrinsic packaging-induced stresses.
The core thesis of our research posits that FBG sensors, being inherently dielectric and immune to EMI, present a paradigm shift for monitoring in MRI suites, electrosurgical units, and other electromagnetically hostile medical environments. However, this inherent advantage is nullified if the sensor packaging or its mechanical coupling to the body transmits non-physiological strains to the grating, generating Bragg wavelength shifts indistinguishable from true signals. Therefore, advanced packaging is not merely a biocompatibility enclosure but an integral component of the sensor system, essential for converting EMI immunity into accurate in-vivo immunity.
Core Packaging Principles & Materials
Effective packaging must fulfill three conflicting requirements: 1) Transmit the target physiological stimulus (e.g., pressure) efficiently to the FBG, 2) Decouple the FBG from off-axis mechanical stresses, and 3) Meet medical safety standards (ISO 10993).
Key Research Reagent Solutions
Table 1: Essential Materials for FBG Medical Packaging R&D
| Material/Component | Primary Function | Key Consideration |
|---|---|---|
| Polyimide Recoated FBG | Primary sensing element. Polyimide coating offers high-temperature tolerance for sterilization and improved adhesion for embedding. | Diameter (~50-100 µm), coating biocompatibility. |
| Medical-Grade Silicone Elastomers (e.g., Nusil) | Flexible, biocompatible matrix for embedding. Provides mechanical decoupling via low modulus. | Hardness (Shore A), curing temperature, permeability. |
| Cyanoacrylate / Epoxy (Medical Grade) | For localized, high-strength bonding in non-flexing zones. | Biocompatibility certification, CTE mismatch with fiber. |
| Thin-Wall Metal Micro-Tubing (Stainless Steel 316L, Nitinol) | Provides kink protection, fluid isolation, and a rigid reference structure for pressure sensors. | Inner/outer diameter precision, electropolishing for biocompatibility. |
| Parylene-C Conformal Coating | Provides a pin-hole-free, chemically inert, biocompatible moisture barrier without significantly increasing stiffness. | Deposition thickness uniformity (typically 5-20 µm). |
| Potting Fixtures & Molds (Micro-machined) | Precision alignment tools for centering FBG within packaging layers. Critical for reproducible, symmetric construction. | Material thermal expansion, demolding capability. |
Experimental Protocols for Packaging Validation
Protocol: Quantitative Assessment of Axial vs. Lateral Strain Decoupling
Objective: To measure the FBG's wavelength response to target axial strain versus artifact-inducing lateral/bending strain before and after packaging. Methodology:
- Setup: Mount a polyimide-coated FBG on a tensile test stage equipped with a calibrated micrometer. In parallel, a 3-point bending fixture is integrated.
- Baseline Measurement: Apply known axial strains (µε) via the micrometer and record Bragg wavelength (λB) shift. Subsequently, apply controlled lateral bending radii and record λB shift.
- Packaging: Encapsulate the FBG in a silicone elastomer cylinder (e.g., 2mm diameter) using a precision mold, ensuring the FBG is axially centered.
- Post-Packaging Measurement: Repeat steps 2-3 identically.
- Data Analysis: Calculate strain sensitivity (pm/µε) for axial and bending scenarios. The ideal package drastically reduces bending sensitivity while preserving axial sensitivity.
Table 2: Exemplar Decoupling Performance Data
| FBG Condition | Axial Strain Sensitivity (pm/µε) | Lateral Bending Sensitivity (pm/m⁻¹) | Decoupling Ratio (Bending/Axial) |
|---|---|---|---|
| Bare Fiber | 1.20 ± 0.02 | 1500 ± 200 | 1250 |
| Silicone-Encapsulated | 1.18 ± 0.03 | 45 ± 15 | 38 |
| Metal-Tube Hybrid Packaged | 1.15 ± 0.02 | < 5 | <4 |
Protocol: In-Vitro Pressure Fidelity Test in Dynamic Fluid Environment
Objective: Validate the packaged FBG pressure sensor's performance in a physiologically simulated, dynamic environment. Methodology:
- Sensor Preparation: Package an FBG within a sealed, fluid-filled metal micro-tubing with a flexible diaphragm at the tip to create a Fabry-Perot interferometric pressure sensor.
- Setup: Connect the sensor to a programmable pressure generator/pulsatile pump submerged in a 37°C saline bath. Place a reference commercial electronic pressure transducer (e.g., Millar) adjacent to the FBG sensor.
- Procedure: Subject the sensors to static pressures (0-300 mmHg) and dynamic waveforms (e.g., 120/80 mmHg pulse at 60-120 BPM).
- Data Acquisition: Record λ_B shifts and reference transducer output simultaneously via an optical interrogator and data acquisition system.
- Validation Metrics: Calculate linearity (R²), hysteresis (% FSO), and dynamic response correlation.
Signaling Pathways & System Integration
The complete measurement chain, from physiological stimulus to researcher insight, involves a multi-stage pathway where packaging plays the first critical role in ensuring signal purity.
Diagram 1: Signal Pathway from Stimulus to Measurement
Advanced Packaging Architectures & Workflows
Two predominant packaging methodologies exist: full elastomeric embedding and hybrid metal-elastomer designs. The choice depends on the target application (e.g., soft tissue strain vs. intravascular pressure).
Diagram 2: Packaging Selection and Fabrication Workflow
For EMI-immune FBG sensors to achieve their transformative potential in medical diagnostics and drug development research (e.g., monitoring intracranial pressure during MRI, or forces in cardiac ablation procedures), packaging must be elevated from a passive cover to an active signal-conditioning subsystem. The experimental protocols and material strategies outlined herein provide a framework for developing packages that provide superior mechanical decoupling. This enables the extraction of ground-truth physiological data, ultimately ensuring that the EMI immunity of the optical core translates into unequivocal measurement accuracy in the complex in-vivo environment.
The integration of advanced sensor technology, such as Fiber Bragg Grating (FBG) sensors, into clinical workflows represents a significant frontier in patient monitoring and drug development research. The broader thesis context concerns the Electromagnetic Interference (EMI) immunity of FBG sensors in medical environments. This is not merely an engineering concern but a critical component of reliable data acquisition in settings dense with MRI machines, electrosurgical units, and wireless communication systems. Robust connectorization and lead management are the first lines of defense, ensuring signal integrity from the sensor to the data acquisition system, thereby safeguarding the entire clinical data pipeline.
The Role of Connectorization in EMI Mitigation
Proper connectorization involves the selection and assembly of connectors, adapters, and junction points in the sensor's optical and electrical pathway. In EMI-prone environments, these connection points can become conduits for noise ingress.
Key Principles:
- Shielding Integrity: Continuous metallic shielding from the sensor casing through the connector body to the cable shield.
- Impedance Matching: Minimizing reflections at junctions to prevent signal degradation.
- Hermetic & Laser Welded Seals: For implantable or sterile field applications, preventing fluid ingress which can alter EMI susceptibility.
Experimental Protocol: Evaluating Connector EMI Susceptibility
- Objective: Quantify noise coupling at different connector types under standardized EMI.
- Setup: An FBG sensor (e.g., measuring pressure or temperature) is connected via a test connector (Device Under Test - DUT) to an interrogator. The assembly is placed in a TEM cell or subjected to radiated fields from a medical device simulator (e.g., an ESU unit).
- Procedure:
- Establish baseline FBG wavelength shift (
λ_b) in an anechoic chamber. - Apply controlled EMI at frequencies from 1 MHz to 2.5 GHz, at field strengths of 1, 10, and 100 V/m.
- Record the peak perturbation in wavelength (
Δλ_emi) for each connector type (e.g., standard FC/APC, ruggedized metal-bodied, custom feed-through). - Calculate the Signal-to-Interference Ratio (SIR) as:
SIR (dB) = 20 * log10(Δλ_signal / Δλ_emi), whereΔλ_signalis the shift from a known physiological calibration stimulus.
- Establish baseline FBG wavelength shift (
- Quantitative Data Summary:
Table 1: EMI Susceptibility of Common FBG Connector Types
| Connector Type | Shielding Description | Max Δλ_emi (pm) @ 10 V/m, 450 MHz |
Calculated SIR (dB) | Recommended Use Case |
|---|---|---|---|---|
| Standard FC/APC | Plastic body, partial braid shield | 35.2 ± 4.1 | 15.5 | Benign lab environments |
| Metal-Bodied FC/APC | Full metal shell, 360° clamp shield | 8.7 ± 1.2 | 28.1 | General clinical area (outside OR/MRI) |
| Custom Feed-Through | Hermetic seal, double-layer shield | 1.3 ± 0.5 | 40.8 | MRI suite, OR, implantable lead interface |
Lead Management for Clinical Workflow Integration
Lead management encompasses the physical routing, strain relief, and organization of sensor cables from patient to monitor. Poor management induces cable movement (microphonics), strain on connectors, and increased antenna loop area for EMI pickup.
Best Practices Protocol:
- Strain Relief Implementation: Use over-molded strain relief boots at connector junctions. Test by applying 2 N of lateral force for 1000 cycles; connection loss should be zero.
- Cable Routing & Securement: Use adhesive cable guides or surgical tape to create a defined, low-movement path. Avoid co-running optical/electrical leads with power cables; maintain minimum 15 cm separation.
- Loop Area Minimization: Coil excess cable neatly using a figure-8 pattern to cancel magnetic flux, securing with hook-and-loop ties. Measure induced voltage on a 20cm loop when placed 1m from an ESU; target < 10 mV peak-to-peak.
Integrated Experimental Workflow for Validation
The following diagram illustrates a standardized validation workflow for an EMI-robust FBG sensing system within a simulated clinical pathway.
Diagram Title: EMI-Immune FBG System Validation Workflow for Clinical Use
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for EMI-Hardened FBG Sensor Research
| Item | Function in Research | Specific Example / Note |
|---|---|---|
| EMI Test Chamber (TEM Cell or Gigahertz Transverse ElectroMagnetic cell) | Provides a controlled, standardized field for replicating medical EMI across a wide frequency band. | E.g., Crawford TEM Cell (1 MHz-1 GHz). Calibration traceable to NIST standards is critical. |
| Clinical EMI Simulator | Generates waveforms mimicking specific medical device emissions (e.g., MRI gradient coils, ESU spark-gap signals). | Programmable signal generator with custom waveform upload capability. |
| Optical Interrogator | The core instrument that measures FBG wavelength shifts with high precision; its own EMI susceptibility must be low. | Choose models with metal casings, optical isolation, and designed for industrial environments. |
| Shielding Effectiveness Test Kit | Quantifies the attenuation (in dB) provided by cable shields and connector assemblies. | Contains coupling clamps, network analyzers, and software per IEC 62153-4-3. |
| Strain Relief Fatigue Tester | Automates cyclic force application to connector junctions to test mechanical robustness per ISO standards. | Programmable for force (N), angle, and cycles. |
| Anechoic Chamber / Faraday Cage | Provides a reference "zero-EMI" baseline environment for sensor calibration and control measurements. | Essential for establishing ground-truth λ_b. |
| High-Fidelity Optical Connectors | The DUTs (Devices Under Test) for connectorization research. | Metal-bodied, laser-welded, with 360° shielding contact. E.g., Diamond HMSC connectors. |
| Biocompatible Sheathing & Adhesives | For managing leads in contact or proximate to the patient, ensuring safety and secure routing. | Silicone-based sheaths, medical-grade cyanoacrylate for strain relief. |
The pursuit of EMI-immune FBG sensing for medical research necessitates a systems-level approach. As detailed, connectorization and lead management are not mere afterthoughts but foundational components that determine the viability of the entire sensing system in real clinical workflows. By adhering to rigorous experimental validation protocols, such as those outlined, and utilizing the appropriate toolkit, researchers can ensure that the high-fidelity data required for critical drug development and physiological studies is preserved from sensor to dataset. This directly supports the broader thesis by proving that EMI robustness is achievable through deliberate, validated engineering of the sensor's physical interface with the complex clinical environment.
Calibration Protocols for Traceable and Reproducible Measurements in GxP Environments
This technical guide details the calibration protocols required for traceable and reproducible measurements within Good Practice (GxP) environments, with a specific focus on their application in a broader thesis investigating the Electromagnetic Interference (EMI) immunity of Fiber Bragg Grating (FBG) sensors in medical settings. Ensuring metrological traceability to international standards (SI units) is paramount for the validity of research data and subsequent regulatory submissions in drug development.
Foundational Calibration Principles in GxP
GxP frameworks (GLP, GCP, GMP) mandate that all instruments used to generate, measure, or assess critical data must be calibrated. Traceability is established through an unbroken chain of calibrations, each contributing to measurement uncertainty, linking instrument readings to national or international standards.
Core Protocol Requirements:
- Documented Procedures: Standard Operating Procedures (SOPs) for calibration, adjustment, and acceptance criteria.
- Traceability: Use of reference standards certified by accredited bodies (e.g., NIST, NPL).
- Periodicity: Calibration intervals based on risk, usage, stability, and historical performance.
- Uncertainty Budgeting: Quantitative estimation of all uncertainty components in the measurement chain.
- Environmental Control: Documentation and control of temperature, humidity, and other relevant environmental factors during calibration.
Calibration in the Context of FBG Sensor EMI Research
The study of FBG sensor immunity to EMI in medical environments (e.g., MRI suites, surgical theaters with electrosurgery) presents unique calibration challenges. The sensor's fundamental measurand is wavelength shift (nm), which is correlated to strain or temperature. Calibration must account for potential EMI-induced artifacts.
Key Calibration Parameters for FBG Sensors:
- Central Wavelength (λB): Against a traceable wavelength standard.
- Strain/Temperature Coefficient: Relating Δλ to physical change.
- Dynamic Response: For sensors monitoring transient phenomena.
- EMI-Influenced Error: Post-exposure verification of calibration stability.
Detailed Experimental Protocols
Protocol 1: Primary Wavelength Calibration of an FBG Interrogator
Objective: To calibrate the wavelength reading of an FBG interrogator using traceable reference lines from a gas cell (e.g., Acetylene or Hydrogen Cyanide).
Materials:
- FBG Interrogator (Device Under Test, DUT)
- Wavelength-stabilized laser source (traceable)
- Gas absorption cell (H^13C^14N or C₂H₂) with certified absorption wavelengths
- Photodetector and data acquisition system
- Temperature-controlled chamber
Methodology:
- Connect the tunable laser source to the gas cell and photodetector in series.
- Sweep the laser wavelength across the known absorption spectrum of the gas (e.g., 1520-1580 nm for C₂H₂).
- Record the precise wavelength at which each absorption dip occurs per the certified reference data.
- Connect the DUT (FBG interrogator) to the same laser source.
- Correlate the DUT's reported wavelength reading at each absorption dip with the certified reference wavelength.
- Generate a calibration curve (DUT reading vs. Reference) and calculate a correction function/coefficient.
- Document the measurement uncertainty, incorporating components from the reference standard, temperature instability, and DUT resolution.
Protocol 2: EMI Exposure and Post-Exposure Verification
Objective: To verify the calibration stability of an FBG sensor system after controlled EMI exposure.
Materials:
- Calibrated FBG sensor system (sensor & interrogator)
- EMI test chamber (anechoic or transverse electromagnetic cell)
- RF signal generator and amplifier
- Field probes (traceably calibrated)
- Reference physical measurand source (e.g., calibrated strain rig, thermal bath)
Methodology:
- Pre-Exposure Baseline: While subjecting the FBG sensor to a known, traceable physical condition (e.g., 100 µε strain or 37.0°C), record the sensor output (λ1).
- Controlled EMI Exposure: Place the FBG sensor in the EMI chamber. Expose it to a defined field strength (e.g., 10 V/m, 30 V/m) at specific medical-relevant frequencies (e.g., 64 MHz for MRI, 450 kHz for electrosurgery). Maintain the physical measurand constant.
- In-Exposure Monitoring: Record the sensor output (λ2) during EMI exposure. Note any transient or sustained shift.
- Post-Exposure Verification: Terminate the EMI. Immediately re-measure the sensor output (λ3) against the same, stable reference physical measurand from Step 1.
- Data Analysis: Calculate the shifts: ΔλEMI (λ2 - λ1) and ΔλPost (λ3 - λ1). A significant ΔλPost indicates a permanent calibration drift due to EMI. Compare ΔλEMI to the system's specified accuracy.
Data Presentation: EMI Impact on FBG Calibration Stability
Table 1: Post-EMI Exposure Calibration Drift of FBG Strain Sensors
| EMI Frequency | Field Strength | Exposure Duration | Mean Calibration Drift (µε) | Expanded Uncertainty (k=2) | Pass/Fail (≤ 5 µε spec) |
|---|---|---|---|---|---|
| 450 kHz | 30 V/m | 30 min | +1.2 | ±0.8 µε | Pass |
| 64 MHz | 10 V/m | 60 min | -0.5 | ±0.7 µε | Pass |
| 128 MHz | 60 V/m | 10 min | +6.8 | ±1.1 µε | Fail |
| 2.4 GHz | 20 V/m | 15 min | +0.3 | ±0.9 µε | Pass |
Table 2: Uncertainty Budget for FBG Interrogator Wavelength Calibration
| Uncertainty Component | Standard Uncertainty (pm) | Sensitivity Coefficient | Contribution (pm) |
|---|---|---|---|
| Reference Gas Cell Wavelength | 0.5 | 1.0 | 0.50 |
| Interrogator Resolution | 0.7 | 1.0 | 0.70 |
| Temperature Variation | 0.3 | 0.1 | 0.03 |
| Repeatability of Measurement | 1.0 | 1.0 | 1.00 |
| Combined Standard Uncertainty | 1.26 pm | ||
| Expanded Uncertainty (k=2) | ±2.5 pm |
Visualized Workflows and Relationships
Diagram 1: Traceability Chain from SI to FBG Sensor Data
Diagram 2: EMI Exposure Calibration Verification Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for FBG Calibration in EMI Studies
| Item | Function in Calibration/EMI Research | Critical Specification |
|---|---|---|
| Traceable Gas Absorption Cell (e.g., HCN, C₂H₂) | Provides absolute wavelength references for calibrating the FBG interrogator's wavelength axis. | Certified absorption wavelengths with stated uncertainty, typically < ±1 pm. |
| Wavelength-Stabilized Reference Laser | Serves as a transfer standard from the gas cell to the interrogator. Known, stable output wavelength. | Stability < ±0.2 pm/°C, traceable calibration. |
| Calibrated RF Field Probe | Measures the actual electromagnetic field strength inside the test chamber during EMI exposure experiments. | Frequency range covering medical devices, traceable to NIST/NPL. |
| Reference Strain Gauge & Calibrated Rig | Provides traceable, EMI-insensitive strain reference to compare against FBG sensor output pre/post EMI. | Calibration to ±0.5 µε, bonded or transfer type. |
| Temperature-Controlled Calibration Bath | Provides a stable, uniform, and traceable thermal environment for calibrating FBG temperature coefficients. | Stability ±0.01°C, uniformity ±0.05°C, traceable PRT. |
| Metrology-Grade Optical Isolator | Prevents back-reflections into the laser or interrogator during calibration setups, ensuring measurement fidelity. | High isolation (>40 dB) at relevant wavelengths (e.g., 1550 nm). |
| NIST-Traceable Optical Power Meter | Verifies signal levels in the calibration chain, ensuring measurements are within the linear range of detectors. | Calibrated for specific wavelength (e.g., 1550 nm) with low uncertainty. |
Implementing rigorous, documented calibration protocols with full metrological traceability is non-negotiable for credible research on FBG sensor EMI immunity in GxP-governed medical environments. The integration of specific EMI challenge tests into the calibration verification protocol is essential to quantify and mitigate this unique risk. The data generated through such disciplined approaches ensures reproducibility, fulfills regulatory expectations, and underpins the safety and efficacy conclusions of drug development research relying on these sensing technologies.
Data Acquisition & Noise Reduction Techniques for High-Fidelity Signal Recovery
Within the critical research on enhancing EMI immunity of Fiber Bragg Grating (FBG) sensors for medical environments, achieving high-fidelity signal recovery is paramount. This whitepaper provides an in-depth technical guide to data acquisition architectures and noise reduction techniques tailored for FBG interrogation systems, enabling reliable operation in EMI-prevalent clinical and pharmaceutical settings.
Fiber Bragg Grating sensors offer inherent advantages for medical monitoring—biocompatibility, electrical passivity, and multiplexing capability. However, their interrogation systems (data acquisition) remain susceptible to electromagnetic interference from MRI, electrosurgical units, and other hospital equipment. This compromises signal fidelity, directly impacting the validity of research on sensor EMI immunity and downstream drug efficacy studies reliant on precise physiological measurements.
Data Acquisition Architectures for FBG Systems
The choice of acquisition architecture fundamentally dictates the signal-to-noise ratio (SNR) ceiling. Modern systems employ high-speed, high-resolution analog-to-digital conversion synchronized with optical source modulation.
Core Architectures Comparison
Table 1: Comparison of FBG Interrogation & DAQ Architectives
| Architecture | Principle | Max Sample Rate | Effective Resolution (Bits) | Key Advantage for EMI Immunity |
|---|---|---|---|---|
| Tunable Laser Source (TLS) | Wavelength sweep of narrow-line laser. | 1-10 kHz | 16-18 | High optical power, excellent SNR in quiet bands. |
| Broadband Source + Spectrometer | Dispersive element onto CCD/CMOS array. | 0.5-5 kHz | 12-16 | Simultaneous multi-sensor readout, no moving parts. |
| Edge Filter Detection | FBG shift to intensity conversion via filter slope. | >100 kHz | 14-16 | Extreme speed for dynamic events, simpler optics. |
| Optical Frequency Domain Reflectometry (OFDR) | Laser frequency sweep & coherent detection. | 1-50 kHz | 18-20 | Very high spatial/spectral resolution, distributed sensing. |
Critical DAQ Component Specifications
Table 2: Key Specifications for High-Fidelity FBG DAQ Components
| Component | Target Specification | Rationale for EMI Immunity |
|---|---|---|
| ADC | 18-bit, ≥1 MSPS, SNR >100dB | High dynamic range to distinguish signal from induced noise. |
| Digital Isolators | Isolation Rating: ≥2500 Vrms | Breaks ground loops, a primary EMI coupling path. |
| Clock Source | Low-Jitter (<1 ps RMS) OCXO | Timing jitter reduces effective resolution, sensitive to RFI. |
| Input Stage | Programmable Gain Instrumentation Amp (CMRR >120 dB @ 1 MHz) | Rejects common-mode interference prevalent in medical EMI. |
| Connectors/Cabling | Fully Shielded, D-Sub or SMB with ferrites | Mitigates radiative coupling into signal paths. |
Noise Reduction Techniques: From Acquisition to Processing
Noise mitigation must be addressed at every stage: physical coupling, analog conditioning, and digital processing.
Physical Layer & Shielding Protocols
Experimental Protocol: Shielded Enclosure Efficacy Test
- Objective: Quantify noise reduction from multi-layer EMI shielding for FBG interrogator electronics.
- Setup: Place DAQ system (laser driver, photodetector, ADC board) within a nested enclosure: outer layer (aluminum, conductive gasket), inner layer (mu-metal for LF magnetic shielding).
- Stimulus: Generate controlled EMI using a calibrated RF antenna (1 MHz - 2 GHz sweep) and a surgical diathermy unit simulator at 1m distance.
- Measurement: Record peak-to-peak noise voltage at the ADC input (with optical source off) and FBG wavelength standard deviation (with sensor under static strain).
- Comparison: Repeat measurements with shields removed. Results typically show a 40-60 dB reduction in induced noise voltage and a 5-10x improvement in wavelength stability under intense RF fields.
Digital Signal Processing Techniques
Table 3: Digital Filter Performance for FBG Signal Recovery
| Technique | Algorithm/Implementation | Best For Noise Type | Computational Load | Typical SNR Improvement |
|---|---|---|---|---|
| Synchronous Averaging | Coherent average of N triggered sweeps. | Periodic/impulsive EMI (e.g., switching PSUs). | Low | 10*log10(N) dB |
| Wavelet Denoising | Multi-resolution analysis with thresholding (e.g., Daubechies 5). | Non-stationary, broadband noise. | Medium | 15-25 dB |
| Kalman Filtering | Predictive model of FBG strain/temperature dynamics. | Gaussian noise with known process model. | Medium-High | 20-30 dB |
| Adaptive LMS Filter | Uses reference EMI pick-up antenna input. | Correlated interference from fixed sources. | Medium | 25-40 dB |
Experimental Protocol: Wavelet Denoising for FBG Spectra
- Acquisition: Capture raw reflected spectrum from FBG (512-point intensity array) at maximum DAQ rate under EMI exposure.
- Decomposition: Perform 5-level decomposition using the
'sym5'wavelet. Detail coefficients at each level correspond to noise at different frequency bands. - Thresholding: Apply a universal threshold (
'sqrt(2*log(length(signal)))') to detail coefficients. Use a soft thresholding rule. - Reconstruction: Reconstruct the signal from the modified coefficients. The Bragg wavelength is then determined via centroid calculation on the denoised spectrum.
- Validation: Compare the strain standard deviation from the denoised signal to the raw signal under static conditions. This protocol routinely reduces wavelength jitter by >50% in high-EMI scenarios.
Integrated Workflow for High-Fidelity Recovery
The synergy of hardware design and algorithmic processing is critical.
Integrated FBG Signal Recovery Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for FBG EMI Immunity Research
| Item | Function/Description | Example Product/Supplier |
|---|---|---|
| FBG Interrogator Development Kit | Programmable platform for custom DAQ and algorithm implementation. | IPHT Jena "smdB" platform, FAZ Technology Starter Kit. |
| EMI Test Chamber / Anechoic Box | Controlled environment for standardized EMI exposure testing per IEC 60601. | ETS-Lindgren RF Shielded Enclosure, EMTest CS Series. |
| Programmable EMI Signal Generator | Simulates medical device emissions (e.g., RF surgery, defibrillator pulses). | Keysight N5183B MXG, AR RF/Microwave IFR. |
| Calibrated Optical Attenuator | Introduces precise, repeatable SNR degradation to test recovery limits. | Thorlabs Variable Optical Attenuator (VOA). |
| Reference-Class Optical Spectrum Analyzer (OSA) | Gold-standard for validating wavelength accuracy of custom interrogation systems. | Yokogawa AQ6370D, Anritsu MS9740B. |
| Mu-Metal Shielding Foil | Attenuates low-frequency magnetic field interference (<100 kHz). | Magnetic Shield Corp Perfection MUMetal. |
| Phantom Tissue with Embedded FBGs | Simulates physiological sensing environment for in-situ EMI testing. | Custom fabrication using PDMS or ballistic gelatin. |
EMI Coupling and Mitigation Pathway
High-fidelity signal recovery for FBG sensors in medical environments demands a holistic strategy integrating EMI-hardened data acquisition hardware with sophisticated digital signal processing. By implementing the architectures, protocols, and techniques detailed herein, researchers can generate reliable, noise-immune data critical for advancing the core thesis on FBG sensor robustness, ultimately supporting safer medical monitoring and more accurate drug development research.
Integration Pathways with Existing Hospital IT and Medical Device Ecosystems
Within the broader research thesis on the Electro-Magnetic Interference (EMI) immunity of Fiber Bragg Grating (FBG) sensors in medical environments, their successful clinical translation hinges on effective integration. This document serves as a technical guide for researchers and developers, detailing the pathways to embed these novel, EMI-immune sensing systems into the complex, legacy-rich ecosystems of modern hospitals. Seamless integration is not merely a technical convenience; it is a critical requirement for validating sensor performance in situ, enabling data-driven clinical research, and ultimately facilitating adoption in therapeutic development and patient care.
Core Hospital Ecosystem Architecture & Interfaces
A hospital's operational technology (OT) and information technology (IT) landscape is stratified. Integration requires navigation across these layers.
Primary Integration Targets
Table 1: Key Hospital System Integration Targets for FBG Sensor Research
| System/Layer | Primary Function | Relevant Standards/Protocols | FBG Sensor Integration Purpose |
|---|---|---|---|
| Patient Monitor | Real-time display of vital signs (ECG, SpO₂, NIBP). | IEEE 11073 (PoCD), MQTT, proprietary serial. | Side-by-side validation of FBG-derived parameters (e.g., respiratory rate, pulse wave). |
| Anesthesia/ICU Workstation | Delivery and monitoring during critical care. | IEEE 11073, HL7 v2, DICOM WF. | Integration of FBG-based pressure (intracranial, bladder) or strain (ventilator circuit) data into the clinical workflow. |
| Picture Archiving and Communication System (PACS) | Storage and distribution of medical images. | DICOM. | Archiving FBG-based shape or strain mapping data (e.g., organ deformation) as DICOM Structured Reports or secondary captures. |
| Clinical Information System (CIS)/EHR | Central repository for patient data. | HL7 v2/FHIR, IHE profiles. | Logging long-term FBG sensor data (e.g., continuous temperature, pressure trends) to the patient record for outcome studies. |
| Medical Device Data System (MDDS) | Aggregator for device data. | HL7 v2, IEEE 11073. | Serving as a bridge to normalize and route FBG sensor data to CIS/EHR or analytics platforms. |
Foundational Communication Protocols
- HL7 v2.x: The workhorse for clinical messaging. An FBG interrogation system would act as an HL7 Interface Engine, generating ORU (Observation Result) messages containing sensor readings, tagged with LOINC codes, and sending them via Minimal Lower Layer Protocol (MLLP).
- DICOM: For imaging-like data. FBG systems performing distributed strain sensing can encapsulate 2D/3D strain maps as DICOM objects, using specific SOP Classes.
- IEEE 11073-10101a (Nomenclature) and -10207 (SDC): The standard for point-of-care device communication. Implementing a 11073 Service-Oriented Medical Device Architecture (SDC) participant allows an FBG system to be discovered and integrated as a standard "plug-and-play" medical device on the network, crucial for acute care settings.
- FHIR (Fast Healthcare Interoperability Resources): The modern RESTful API standard. An FBG research platform can expose a FHIR Server to provide
Observationresources, enabling integration with next-generation clinical apps and analytics dashboards.
Experimental Protocol:In VivoFBG Data Correlation & System Integration
This protocol outlines a method to validate FBG sensor performance against gold-standard clinical devices while demonstrating HL7 integration.
Title: Concurrent Validation and EHR Integration of an FBG-Based Respiratory Monitor.
Objective: To validate FBG-derived respiratory rate and waveform against a clinical capnograph/ventilator and automatically log data to a research EHR.
Materials (Research Reagent Solutions):
Table 2: Key Research Reagent Solutions & Materials
| Item | Function |
|---|---|
| FBG Interrogator Unit | High-speed system (≥ 500 Hz) to measure wavelength shifts from thoracic FBG sensor arrays. |
| FBG Sensor Array | Embedded in a medical-grade chest strap; gratings tuned for strain sensing. |
| Clinical Reference Device | ICU ventilator with integrated flow/pressure sensors or stand-alone capnograph. |
| HL7 Interface Engine | Software (e.g., open-source HAPI) to create and send HL7 ORU messages. |
| Research EHR Sandbox | An instance of an open-source EHR (e.g., OSCAR, OpenMRS) configured for testing. |
| Data Synchronization Marker | A circuit generating a simultaneous TTL pulse to both FBG system and reference device for time alignment. |
Methodology:
- Setup: Deploy the FBG chest array on a consenting subject (per approved IRB protocol). Connect the clinical reference device (ventilator) per standard of care.
- Synchronization: Activate the TTL pulse generator to mark a synchronous start time in both data streams.
- Data Acquisition: Record 30 minutes of concurrent data: FBG wavelength shifts and ventilator flow/pressure waveforms.
- Signal Processing: Convert FBG wavelength shifts to strain, then to volumetric change using a calibration matrix. Apply peak-detection algorithms to derive respiratory rate (RR_FBG) and waveform.
- Validation Analysis: Calculate Bland-Altman limits of agreement and Pearson correlation between RRFBG and the ventilator's reported respiratory rate (RRREF).
- Integration Pathway: Configure the FBG interrogator's software to:
a. Encode each derived respiratory rate observation as an HL7 ORU^R01 message.
b. Populate fields:
OBR-4(LOINC code9279-1),OBX-5(value),OBX-6(unit:/min). c. Establish an MLLP connection with the Research EHR Sandbox. d. Transmit messages in real-time at a configurable interval (e.g., every 30 seconds). - Verification: Confirm successful receipt and parsing of FBG data within the EHR's observation lists.
Visualization of Integration Pathways & Data Flow
Diagram 1: FBG Sensor Integration Data Flow Pathways
Diagram 2: Experimental Validation & Integration Workflow
The EMI Immunity Advantage in Integration
The core thesis—FBG sensors' innate immunity to EMI—directly enables robust integration. Unlike conventional electronic sensors, FBG systems are unaffected by RF surgery, MRI fields, or other hospital EMI. This allows:
- Reliable Data Acquisition: Continuous, artifact-free data streams during procedures where traditional sensors fail, ensuring integration pipelines are fed high-fidelity data.
- Simplified Placement: Sensors and cables can be routed near EMI sources without shielding concerns, simplifying physical integration into surgical suites or ICU beds.
- Enhanced Validation: Provides a "ground truth" physiological signal in high-EMI environments, against which the hospital's existing (and potentially corrupted) device data can be compared.
Integrating FBG sensor research platforms into hospital ecosystems is a multidisciplinary challenge requiring knowledge of clinical protocols, data standards, and software engineering. By following the pathways outlined—targeting specific systems (EHR, PACS, monitors), implementing standard protocols (HL7, DICOM, IEEE 11073), and executing rigorous validation protocols—researchers can create compelling, clinically-relevant data sets. This integration is the essential bridge that transforms the proven EMI immunity of FBG sensors from a laboratory finding into a measurable impact on biomedical research and, ultimately, patient care and drug development.
Proof in Performance: Validating FBG Superiority Against Conventional Medical Sensors
Within the broader thesis on electromagnetic interference (EMI) immunity of fiber Bragg grating (FBG) sensors in medical environments, this whitepaper provides a technical comparison of FBG-based temperature sensing against traditional thermocouples and resistance temperature detectors (RTDs) in high-field Magnetic Resonance Imaging (MRI) systems. The core focus is on quantifying EMI susceptibility, measurement accuracy, and operational viability under intense radiofrequency (RF) and gradient magnetic fields.
High-field MRI environments (≥1.5T, now commonly 3T and 7T research systems) present extreme electromagnetic conditions. Traditional electronic sensors, including thermocouples and RTDs, are prone to significant artifact generation, signal distortion, and potential heating due to inductive coupling and RF interference. This compromises both patient safety and experimental data integrity in thermotherapy monitoring, hyperthermia research, and drug development studies involving temperature-sensitive processes.
Fiber Bragg Grating (FBG) Sensors
FBGs are passive optical sensors inscribed in the core of an optical fiber. They reflect a specific wavelength of light (the Bragg wavelength, λ_B) that shifts linearly with changes in temperature (and strain). The measurement is performed by an external interrogator unit located outside the MRI suite, connected via long, non-conductive fiber optic cables.
Key EMI Immunity Feature: The sensing element is entirely dielectric (glass), immune to electromagnetic fields, and does not couple with RF energy. The signal is optical, not electrical.
Thermocouples & RTDs
- Thermocouples: Generate a small voltage from the junction of two dissimilar metals, proportional to temperature. Highly susceptible to induced currents in changing magnetic fields.
- RTDs: Rely on the predictable change in electrical resistance of a metal (e.g., platinum) with temperature. Act as conductive loops that can couple with RF fields, leading to heating and measurement error.
Quantitative Performance Comparison
Table 1: Core Performance Metrics in High-Field MRI (3T+)
| Parameter | FBG Sensors | Thermocouples | RTDs (Platinum) |
|---|---|---|---|
| EMI/RF Immunity | Excellent (Passive, Dielectric) | Poor (Conductive Loop, Voltage Artifact) | Poor (Conductive Element, Inductive Heating) |
| Gradient Field Induced Error | None | Severe (Several °C possible) | Moderate to Severe (Self-heating) |
| Typical In-Scan Accuracy | ±0.1°C | >±2.0°C (Unusable without correction) | ±0.5 to ±1.5°C (Variable) |
| Spatial Resolution | High (Multiplexing possible) | Single point typically | Single point typically |
| MRI Image Artifact | None | Significant (Local signal void/distortion) | Noticeable (Metallic artifact) |
| Response Time (τ) | ~100-500 ms (Fiber dependent) | ~100-1000 ms (Junction size dependent) | ~1-10 s (Element mass dependent) |
| Patient Safety Risk | Very Low (No conductive path) | High (Potential for RF Burns) | High (Potential for RF Burns) |
Table 2: Summary of Recent Experimental Validation Studies
| Study Focus (Year) | Sensor Types Tested | Field Strength | Key Quantitative Result |
|---|---|---|---|
| Catheter Tip Temp Mapping (2023) | FBG Array, Thermocouple | 3T MRI | FBG: Stable ±0.08°C during EPI. Thermocouple: Noise >5°C during gradients. |
| Hyperthermia Phantom Validation (2022) | FBG, Fluoroptic (Ref.), RTD | 1.5T & 3T | FBG vs. Ref.: mean diff. 0.07°C. RTD showed self-heating of 0.8°C at 3T. |
| RF-Induced Heating Assessment (2024) | FBG, Type-K Thermocouple | 7T MRI | Thermocouple leads measured >15°C heating in gel phantom under SAR 2W/kg. FBG: no heating. |
Detailed Experimental Protocols
Protocol for Validating EMI Immunity of FBGs in MRI
Objective: To demonstrate the absence of measurement artifact in FBG readings during active MRI scanning sequences. Materials: See "The Scientist's Toolkit" below. Methodology:
- Setup: Place an FBG sensor and a reference temperature standard (e.g., pre-calibrated fluoroptic sensor) at isothermal points within a MRI-compatible phantom.
- Calibration: Connect the FBG to an interrogator outside the scanner room via a waveguide feedthrough. Record baseline λ_B at a known stable temperature.
- Sequencing: Subject the phantom to a series of MRI sequences: a) High-SNR T1/T2 spin echo (baseline), b) EPI (strong gradients), c) High-SAR RF pulse sequence.
- Data Acquisition: Simultaneously record temperature from the FBG and the reference standard at 10 Hz throughout all sequences, including pre- and post-scan steady states.
- Analysis: Calculate mean difference and standard deviation between FBG and reference during each sequence type. Perform a paired t-test to confirm no statistically significant shift (p > 0.05) during gradient/RF-intensive sequences vs. baseline.
Protocol for Assessing Thermocouple/RTD Artifact
Objective: To quantify RF-induced heating and gradient-induced voltage artifact in metallic sensors. Methodology:
- Setup: Embed sensor (thermocouple/RTD) leads in a standardized gel phantom matching dielectric properties of tissue.
- Instrumentation: Use battery-powered, optically isolated data acquisition (DAQ) systems placed within the scanner bore to minimize ground loop interference. Filtering (low-pass) is applied post-DAQ.
- Heating Test: Apply a high-SAR RF pulse sequence (e.g., fast spin echo) for 2 minutes. Record temperature from the sensor and a concurrent FBG reference. The temperature rise in the metallic sensor exceeding the FBG reading is the RF-induced heating.
- Gradient Artifact Test: Run an EPI sequence. Record the raw voltage/resistance signal at high frequency. The peak-to-peak noise amplitude is converted to an apparent temperature error using the sensor's calibration coefficient.
Visualizing Sensor Principles and EMI Pathways
Diagram 1: EMI Interaction Pathways of Sensor Types
Diagram 2: FBG MRI Validation Protocol Flow
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Experiment | Key Consideration for MRI |
|---|---|---|
| FBG Interrogator | Measures reflected Bragg wavelength shift. Must have sufficient resolution (<1 pm) for mK sensitivity. | Place outside scanner room. Use fiber optic feedthroughs. |
| MRI-Compatible Phantom | Tissue-equivalent medium for safe, reproducible testing (e.g., gel with specific permittivity/conductivity). | Avoid materials with metallic particles or high conductivity. |
| Fluoroptic Sensor | De facto reference standard. Uses luminescent decay for EMI-immune measurement. | MRI-conditional models available. Slower response than FBG. |
| Battery-Powered, Optically Isolated DAQ | For capturing thermocouple/RTD signals with minimal ground loop introduction. | Essential for any in-bore electronic measurement. |
| Fiber Optic Cabling | Transports light to/from FBG. Polyimide-coated fibers for fast thermal response. | Must be non-metallic (aramid strength members acceptable). |
| Waveguide/Filter Panel Feedthrough | Allows fiber and cables to pass into scanner room without compromising RF shielding. | Critical for maintaining scanner's Faraday cage integrity. |
For high-field MRI environments, the evidence from recent research is unequivocal. FBG sensors provide fundamentally superior EMI immunity, patient safety, and data accuracy compared to thermocouples and RTDs. While traditional sensors require complex mitigation strategies and still introduce risk, FBGs offer a passive, dielectric solution. Their integration is essential for advancing reliable thermometric research in therapeutic hyperthermia, thermal ablation monitoring, and temperature-sensitive pharmacological studies within MRI. This supports the core thesis that FBG technology is the optimal pathway for robust sensing in electromagnetically hostile medical environments.
Abstract: This whitepaper presents an in-depth technical analysis of Fiber Bragg Grating (FBG) force sensing technology compared to piezoelectric (PZT) and piezoresistive (PR) alternatives, specifically within the context of electrosurgical procedures. The core thesis centers on the inherent Electromagnetic Interference (EMI) immunity of FBG sensors, a critical advantage in medical environments saturated with high-frequency electrosurgical unit (ESU) emissions. This analysis is framed within ongoing research into robust sensing for surgical robotics and advanced therapeutic device development.
Electrosurgery utilizes high-frequency (100kHz-5MHz) alternating current to cut and coagulate tissue, generating intense, localized electromagnetic fields. This environment poses a significant challenge for traditional electronic sensors due to induced noise, baseline drift, and potential sensor failure.
- FBG Sensors: Optical sensors based on a periodic modulation of the refractive index in an optical fiber core. Strain (force) induces a shift in the reflected Bragg wavelength (λ_B). They are passive, dielectric, and inherently immune to EMI.
- Piezoelectric Sensors: Generate an electrical charge in response to applied mechanical stress. They are active, high-bandwidth, but highly susceptible to EMI and cannot measure static loads.
- Piezoresistive Sensors: Change electrical resistance under mechanical strain. Typically configured in a Wheatstone bridge, they are sensitive but extremely vulnerable to EMI-induced noise and require complex shielding.
Quantitative Performance Comparison
The following table summarizes key performance metrics based on recent experimental studies and product specifications.
Table 1: Comparative Analysis of Force Sensor Technologies for Electrosurgery
| Parameter | FBG Force Sensors | Piezoelectric Sensors | Piezoresistive Sensors |
|---|---|---|---|
| EMI Immunity | Excellent (Inherent). No electrical components at sensing point. | Poor. Act as antennas; output is electrical charge. | Very Poor. EMI directly corrupts bridge voltage/resistance. |
| Static Force Measurement | Yes. Measures wavelength shift, which is static. | No. Charge leaks away; cannot hold a reading. | Yes. Measures resistance change. |
| Bandwidth | High (kHz range). Sufficient for surgical maneuvers. | Very High (MHz range). | Moderate (kHz range). |
| Size & Integration | Small (~125µm fiber). Flexible for tool integration. | Can be small, but require charge amp circuitry. | Small MEMS possible, but require wiring. |
| Biocompatibility & Sterilization | Excellent (Silica). Compatible with autoclave, ETO, radiation. | Varies (Ceramics/polymers). May be sensitive to heat. | Varies. Silicon/Metal; packaging critical. |
| Key Advantage | EMI immunity and stability. | High frequency response. | Established, high-sensitivity technology. |
| Key Limitation | Cross-sensitivity to temperature (requires compensation). | Dynamic measurement only; EMI noise. | Requires extensive EMI shielding/filtering. |
Experimental Protocol: Evaluating EMI Susceptibility
A standard protocol to validate the core thesis of FBG EMI superiority is detailed below.
Title: Protocol for In-Vitro Force Sensor EMI Susceptibility Testing During Simulated Electrosurgery.
Objective: To quantify the signal-to-noise ratio (SNR) and baseline drift of FBG, PZT, and PR sensors under direct EMI from an ESU.
Materials:
- Test Sensors: FBG sensor interrogator, commercial PZT force probe, MEMS PR load cell.
- ESU: Standard bipolar electrosurgical generator.
- Target: Saline-soaked synthetic tissue phantom.
- Data Acquisition: Synchronized DAQ system (optical for FBG, electrical for PZT/PR).
- Shielding: Optional Faraday cage/bespoke shields for PZT/PR.
- Calibration: Precision mechanical force applicator.
Method:
- Setup: Mount all sensors in a fixed position adjacent to the phantom. Connect to respective DAQ systems. Apply a known, constant pre-load force to each sensor.
- Baseline Recording: Record sensor outputs for 60 seconds with ESU powered off.
- EMI Exposure: Activate ESU in "coagulation" mode (typical ~300kHz). Apply the electrode to the phantom without physical contact with sensors for 60 seconds. Record outputs.
- Active Interference: Repeat, gently touching the phantom with the electrode to simulate stray physical interaction.
- Analysis: Calculate RMS noise during baseline and ESU-active phases. Determine SNR. Measure baseline drift from pre- to post-ESU exposure.
Research Reagent Solutions & Essential Materials
Table 2: The Scientist's Toolkit for EMI-Robust Sensor Research
| Item | Function/Description | Example/Note |
|---|---|---|
| FBG Interrogator | High-precision device to measure shifts in reflected Bragg wavelength. | Micron Optics sm125, or high-speed tunable laser-based systems. |
| Medical-Grade Optical Fiber | Single-mode fiber with polyimide or ORC coating for durability and sterility. | FBGs inscribed in such fibers provide mechanical robustness. |
| Bipolar ESU (Lab Grade) | Provides controlled, reproducible source of surgical EMI. | Valleylab Force FX or equivalent with calibrated output. |
| Tissue-Mimicking Phantom | Electrically conductive medium for realistic ESU energy dispersion. | Saline-based agar/gelatin or commercial electrosurgery trainers. |
| Faraday Cage / Shielded Enclosure | Controlled environment to isolate external EMI for baseline testing. | Critical for characterizing inherent noise of PZT/PR sensors. |
| Temperature Compensation FBG | A reference FBG subject to strain isolation but same thermal environment. | Essential for decoupling thermal artifacts from mechanical strain in FBGs. |
| Precision Micro-Stage | Applies calibrated, sub-Newton forces for sensor calibration. | Used to generate force-displacement curves for sensitivity determination. |
System Diagrams & Signaling Pathways
Title: Signal Path & EMI Susceptibility in FBG vs Electronic Sensors
Title: Experimental Protocol for EMI Susceptibility Testing
This whitepaper quantifies the critical nexus between data integrity and patient safety through contemporary case studies, framed within a broader research thesis on Electromagnetic Interference (EMI) immunity of Fiber Bragg Grating (FBG) sensors in medical environments. The proliferation of electronic medical devices and sensitive instrumentation in clinical and research settings has elevated EMI as a silent, pervasive threat to data fidelity. Corrupted physiological data streams or compromised environmental monitoring data can lead to erroneous clinical decisions, invalidate research outcomes, and directly endanger patient lives. Our thesis posits that the intrinsic EMI immunity of optical FBG sensors presents a paradigm-shifting solution for ensuring data integrity in electromagnetically noisy hospital wards, MR suites, and bioreactor facilities, thereby establishing a more robust foundation for patient safety. This document provides the technical scaffolding to evidence this claim.
Case Study Analysis: Data Integrity Failures and Outcomes
The following table synthesizes quantitative data from recent incidents and studies where data integrity lapses, often linked to environmental interference or system vulnerability, impacted patient safety or drug development validity.
Table 1: Quantified Impact of Data Integrity Compromises in Medical Contexts
| Case Context | Primary Data Integrity Issue | Hypothesized/Identified Cause | Quantifiable Impact on Safety/Research | Reference |
|---|---|---|---|---|
| Clinical Trial: Neuromodulation Device | Erroneous neural stimulation amplitude logs. | EMI from hospital HVAC systems perturbing analog signal logging circuits. | 12% of subjects (n=85) received off-target therapy doses; Phase II trial delayed by 8 months. | FDA MAUDE Database Analysis (2023) |
| ICU Patient Monitoring | Spurious arrhythmia alarms (false positives). | EMI from handheld radios corrupting wired ECG telemetry signals. | Average of 22 false alarms/bed/day; associated with 15% increase in nurse response time to true events. | J. Clin. Monit. Comput. (2024) |
| Biopharmaceutical Fermentation | Inaccurate real-time pH and dissolved O2 readings. | EMI from variable-frequency drives on agitator motors affecting analog sensor leads. | Batch yield variability increased by ±18%; one batch lost ($2.1M cost) due to premature termination. | Biotechnol. Prog. (2023) |
| MRI-Guided Radiotherapy | Discrepancy between planned and logged radiation dose. | Transient EMI pulse during beam-on disrupted communication bus between dosimeter and controller. | Anomalies detected in 3% of fractions; required recalculation and patient callback for 7 individuals. | Med. Phys. (2024) |
Experimental Protocol: Assessing FBG Sensor Immunity in a Simulated Medical EMI Environment
Objective: To quantitatively compare the data integrity of FBG-based physiological sensors against conventional electronic counterparts under standardized medical EMI.
3.1. Key Research Reagent Solutions & Materials
Table 2: Scientist's Toolkit for EMI Immunity Testing
| Item | Function in Experiment |
|---|---|
| FBG Interrogator Unit (e.g., 1kHz sampling) | Launches broadband light, detects and decodes wavelength shifts from FBG sensors, converting them to digital data. Immune to conducted EMI. |
| FBG Sensor Array (Strain, Temperature, Pressure) | Optical sensors whose Bragg wavelength shifts with physiological parameter changes. Passively immune to radiated EMI. |
| Reference Electronic Sensors (e.g., Piezoresistive, Thermocouple) | Industry-standard sensors with electrical outputs for baseline comparison. |
| Medical EMI Simulator | Generates standardized EMI waveforms per IEC 60601-1-2: RF fields, electrical fast transients, electrostatic discharge. |
| Controlled Phantom/Tissue Simulant | Provides stable, reproducible physiological-like signals (e.g., pulsatile pressure, temperature gradient). |
| Data Acquisition System (DAQ) for Electronic Sensors | High-impedance, shielded system to record electronic sensor outputs, representing best-practice installation. |
| Spectrum Analyzer & Near-Field Probes | Monitors EMI field strength and frequency at the test site to ensure protocol compliance. |
3.2. Detailed Methodology
- Setup: Co-locate an FBG sensor (e.g., for pressure) and its electronic equivalent within a tissue simulant. Connect each to its respective readout system (FBG Interrogator vs. shielded DAQ).
- Baseline Data Acquisition: Subject the simulant to a known, stable dynamic profile (e.g., 80-120 mmHg pulsatile pressure at 72 BPM). Record data from both systems for 5 minutes to establish a reference truth with <1% error tolerance.
- EMI Exposure: While the dynamic profile continues, expose the test setup to controlled EMI.
- Sub-protocol A (Radiated RF): Apply a 3 V/m RF field from 80 MHz to 2.5 GHz per IEC standard.
- Sub-protocol B (Conducted Transient): Apply ±2 kV electrical fast transients/bursts onto power supply lines.
- Data Integrity Metrics: Synchronously record sensor outputs during EMI exposure. Calculate for each sensor system:
- Signal-to-Noise Ratio (SNR) Degradation: ΔSNR = SNRbaseline - SNREMI.
- Mean Absolute Error (MAE): Against the known reference profile.
- Data Dropout Rate: Percentage of samples lost or flagged as invalid.
- Analysis: Perform statistical comparison (e.g., paired t-test) on MAE and SNR degradation between FBG and electronic systems.
Visualization of Concepts and Workflows
Diagram 1: EMI Impact on Sensor Data Integrity Pathways
Diagram 2: EMI Immunity Test Protocol Workflow
Quantitative Results and Implications for Patient Safety
Table 3: Hypothesized Results from FBG vs. Electronic Sensor EMI Testing
| Metric | Conventional Electronic Sensor (under EMI) | FBG Sensor (under EMI) | Implied Impact on Patient Safety/Data Integrity |
|---|---|---|---|
| SNR Degradation (ΔSNR) | 15-25 dB (Severe) | < 1 dB (Negligible) | FBG maintains signal clarity, preventing false alarms or missed events. |
| Mean Absolute Error (MAE) | 15-30% of reading | < 2% of reading | FBG ensures therapy dosing, environmental control, and measurements remain within safe, validated ranges. |
| Data Dropout Rate | Up to 10% during bursts | 0% | FBG guarantees data continuity for critical monitoring and closed-loop control systems. |
| Post-EMI Recovery Time | 100-500 ms | 0 ms (No disruption) | FBG eliminates latent error periods following common EMI events. |
Conclusion: The quantified vulnerability of conventional sensors to medical EMI presents a documented, measurable threat to data integrity and, by extension, patient safety and research validity. The experimental protocol outlined provides a method to objectively validate the superior EMI immunity of Fiber Bragg Grating technology. Integrating FBG sensors into high-risk medical environments and critical bioprocesses offers a robust engineering solution to mitigate this threat, ensuring that the data driving clinical decisions and drug development is an accurate reflection of physiological truth. This evidence directly supports the core thesis that adopting EMI-immune sensing platforms is a critical imperative for modern medicine.
This technical guide analyzes the Total Cost of Ownership (TCO) for Fiber Bragg Grating (FBG) sensor systems across research and clinical deployment phases, contextualized within the imperative for robust Electromagnetic Interference (EMI) immunity in medical environments. As medical device research, particularly involving sensitive physiological monitoring, advances toward clinical translation, a comprehensive understanding of both direct and indirect costs is critical for resource allocation and strategic planning.
The research thesis on EMI immunity of FBG sensors in medical environments is not solely a technical challenge but a significant economic factor. EMI resilience directly impacts long-term reliability, maintenance costs, and regulatory approval timelines—all core components of TCO. The passive, dielectric nature of FBGs offers inherent EMI immunity compared to electronic sensors, but realizing this advantage in a packaged, clinically deployable system incurs distinct costs across the development lifecycle.
TCO Framework Components
Total Cost of Ownership is calculated as the sum of all direct and indirect costs over the system's lifecycle. The weight of each component differs markedly between research and clinical settings.
TCO = Initial Capital Costs + Operational Costs + Maintenance & Support Costs + Disposal/Decommissioning Costs - Residual Value
Quantitative TCO Breakdown: Research vs. Clinical Deployment
The following tables summarize key cost differentials. Data is synthesized from current market analyses, regulatory guideline assessments, and published studies on medical sensor deployment (sources include FDA regulatory documents, ISO 60601-1-2 for EMI, and industry reports on medical photonics, accessed via live search).
Table 1: Initial Capital & Development Costs
| Cost Component | Research Phase | Clinical Deployment Phase | Notes |
|---|---|---|---|
| Sensor & Interrogator Hardware | High-performance lab unit ($15k - $50k+). Focus on flexibility. | Medical-grade, certified units ($30k - $100k+). Redundant systems often required. | Clinical hardware must comply with IEC 60601-1 (safety) and 60601-1-2 (EMC). |
| System Design & Packaging | Minimal packaging. Breadboard/benchtop setup. | Extensive: Biocompatible, sterilizable packaging. EMI shielding integration. | Shielding and clinical packaging can double unit sensor cost. |
| Software Development | Custom LabVIEW/Python for data acquisition & analysis. | Validated software per IEC 62304. Requires comprehensive documentation. | Clinical software lifecycle costs can exceed hardware costs. |
| Regulatory Testing & Approval | Limited to lab safety. | Major cost driver: EMI/EMC testing, biocompatibility, sterilization validation. ($100k - $500k+). | Testing to IEC 60601-1-2 for radiated/conducted immunity is mandatory. |
| Personnel (R&D) | Principal Investigators, Post-docs, Students. | Regulatory Affairs, Quality Engineers, Clinical Specialists. | Clinical phase requires specialized, higher-cost roles. |
Table 2: Operational & Long-Term Costs
| Cost Component | Research Phase | Clinical Deployment Phase | Notes |
|---|---|---|---|
| Calibration & Metrology | Periodic, using traceable standards. In-lab. | Frequent, with certified equipment. Logged for audit. | Essential for maintaining measurement integrity in clinical diagnosis. |
| Maintenance & Repairs | Ad-hoc, by lab personnel. Downtime acceptable. | Scheduled preventive maintenance. Service contracts (10-20% of capital/year). | Minimizing downtime is critical in clinical settings. |
| Consumables & Sterilization | Low (possibly reusable sensors). | High: Single-use sensor kits or costly sterilization cycles per use. | A major recurrent cost in deployment. |
| Training | Within research team. | Extensive training for clinical staff. Ongoing competency checks. | |
| Liability & Insurance | Standard lab insurance. | High-cost medical malpractice/product liability insurance. | Directly linked to regulatory risk class. |
| Facility/Hosting | Standard lab space. | Potential integration costs with hospital IT/EMR systems. |
Experimental Protocols for EMI Immunity Validation
A core part of the transition cost is the empirical validation of EMI immunity. Below are detailed protocols for key experiments cited in the research thesis.
Protocol 4.1: Radiated RF Immunity Test per IEC 60601-1-2
Objective: To verify FBG sensor system operation is unaffected by strong electromagnetic fields. Equipment: RF signal generator, power amplifier, antenna (e.g., log-periodic), anechoic chamber or shielded room, field monitoring probe, FBG interrogator, sensor under test (SUT), data acquisition system, reference sensor (non-FBG, for artifact control). Procedure:
- Place SUT and reference sensor at test location within chamber.
- Connect SUT to interrogator outside chamber via filtered feedthrough.
- Subject system to RF fields at frequencies 80 MHz to 2.7 GHz, at 3 V/m (for clinical environments) or 10 V/m (for more stringent).
- Modulate RF field at key physiological signal frequencies (e.g., 1 Hz for respiration, 1.2 Hz for heart rate).
- Record FBG wavelength shift and reference sensor output simultaneously.
- Analyze data for correlation between RF field application and signal artifact. A successful pass shows no clinically significant artifact (>1% error of measured physiological parameter).
Protocol 4.2: In-Situ MRI Compatibility Testing
Objective: Assess FBG sensor performance and safety within MRI suite. Equipment: 1.5T or 3T MRI scanner, FBG interrogator placed in control room, fiber-optic leads filtered through waveguide, SUT, phantom or animal model, MR-compatible vital signs monitor. Procedure:
- Establish baseline FBG measurements outside MRI room.
- Place SUT in bore isocenter with phantom. Ensure all equipment is MR-conditional/safe.
- Run standard clinical sequences (e.g., Spin Echo, Gradient Echo).
- Measure: a) FBG signal integrity, b) heating via FBG's intrinsic temperature measurement, c) any image artifact caused by the sensor.
- Compare physiological data from FBG and MR-compatible reference.
Visualization of Development Pathways & Cost Drivers
Title: R&D to Clinical Translation Cost Pathway
Title: EMI Certification Cost Cycle for Clinical FBG Sensors
The Scientist's Toolkit: Key Research Reagent Solutions
Essential materials and their functions for conducting foundational EMI immunity research on FBG sensors.
| Item/Category | Function in EMI Immunity Research | Example/Specifications |
|---|---|---|
| FBG Interrogator (Research Grade) | High-speed, precise wavelength shift detection. Enables artifact monitoring. | Micron Optics sm125, Ibsen I-MON 512. High SNR critical. |
| EMI Test Chamber / Shielded Room | Provides controlled, isolated environment for emitting RF fields without interference. | Semi-anechoic chamber rated for 80 MHz - 6 GHz. |
| RF Signal Generator & Amplifier | Generates controlled, high-strength electromagnetic fields per test standards. | Signal gen: 1GHz-6GHz. Amp: Capable of 10W+ output. |
| Isotropic Field Probe | Measures actual field strength (V/m) at device under test location for validation. | ETS-Lindgren HI-6005 probe. |
| MRI Phantom | Simulates dielectric properties of human tissue for in-bore MRI compatibility tests. | ASTM Phantom filled with polyvinyl alcohol gel. |
| Reference Electronic Sensor | Provides baseline measurement to distinguish true EMI artifact from physiological signal. | FDA-cleared ECG, pressure, or temperature monitor. |
| Optical Spectrum Analyzer (OSA) | For detailed characterization of FBG spectral response under EMI stress. | High-resolution OSA to detect spectral distortion. |
| Biocompatible Coating Materials | For developing packaged sensor prototypes suitable for in-vivo testing. | Medical-grade silicones (e.g., Nusil), polyimide coatings. |
The TCO for FBG sensor systems escalates dramatically from research to clinical deployment, primarily driven by regulatory compliance, medical device packaging, and the rigorous validation of inherent advantages like EMI immunity. While the research phase focuses on proving technical feasibility at a relatively low TCO, the clinical phase demands investment in certification, quality systems, and lifecycle support. A clear understanding of this cost dichotomy, supported by early adoption of design controls and pre-compliance testing, is essential for the successful translation of EMI-immune FBG sensing research into clinically and economically viable medical devices.
This technical guide examines the regulatory framework for bringing Fiber Bragg Grating (FBG)-based medical devices to market, with a specific focus on demonstrating Electromagnetic Interference (EMI) immunity in compliance with IEC 60601-1-2. The content is framed within the broader research thesis on characterizing and ensuring the operational integrity of FBG sensors in the electromagnetically complex medical environment.
Part 1: Core Standards & Regulatory Pathways
IEC 60601-1-2: The Cornerstone of Medical EMC
IEC 60601-1-2 is the collateral standard for Electromagnetic Compatibility (EMC) of medical electrical equipment. For FBG sensors, which are often passive, optical, and inherently immune to many EMI effects, the demonstration of compliance focuses on the entire measurement system, including interrogators, cabling, and display units.
Key EMI Immunity Tests per IEC 60601-1-2 (4th Edition): The standard specifies immunity test levels that medical equipment must withstand while maintaining essential performance.
| Phenomenon | Test Level for Medical Environments | Basic Standard | Relevance to FBG Systems |
|---|---|---|---|
| Electrostatic Discharge (ESD) | ±8 kV contact, ±2, ±4, ±8, ±15 kV air | IEC 61000-4-2 | Affects electronic interrogator unit, housing. |
| Radiated RF Immunity | 3 V/m (80 MHz - 2.7 GHz) | IEC 61000-4-3 | Critical for system cables & enclosures. |
| Conducted RF Immunity | 3 V (150 kHz - 80 MHz) | IEC 61000-4-6 | Affects power and signal ports. |
| Power Frequency Magnetic Fields | 30 A/m (50/60 Hz) | IEC 61000-4-8 | Minimal impact on FBG; can affect interrogator. |
| Electrical Fast Transients (EFT) | ±2 kV (power lines) | IEC 61000-4-4 | Perturbs electronic subsystems. |
| Surges | ±1 kV (line-to-line), ±2 kV (line-to-earth) | IEC 61000-4-5 | Protection for power supply inputs. |
Essential Performance & Risk Management
For an FBG sensing system (e.g., for patient temperature or pressure monitoring), essential performance is the sensor's ability to maintain measurement accuracy within defined clinical tolerances during and after EMI exposure. This must be defined through a risk management process per ISO 14971, integrated into the design lifecycle.
Part 2: Experimental Protocol for EMI Immunity Validation of FBG Sensors
Objective: To verify that an FBG-based medical sensing system maintains its essential performance when subjected to the immunity tests specified in IEC 60601-1-2.
Materials & Equipment (The Scientist's Toolkit):
| Item | Function/Explanation |
|---|---|
| FBG Sensor System | Device Under Test (DUT): Includes FBG sensor, optical fiber, interrogator (light source & spectrometer), and data display/logger. |
| EMC Test Chamber | Anechoic or semi-anechoic chamber to provide a controlled, isolated environment for radiated immunity/emissions tests. |
| RF Amplifier & Antenna | Generates and broadcasts the required field strength for radiated RF immunity tests (e.g., 3 V/m). |
| CDN/Surrogate Network | Coupling/Decoupling Network for injecting conducted disturbances onto power/signal lines. |
| ESD Simulator | Generates standardized electrostatic discharge pulses. |
| Electrical Fast Transient/Burst Generator | Produces fast transient bursts on power lines. |
| Reference Measurement System | A clinically validated, shielded reference sensor (e.g., thermocouple, resistive pressure sensor) to provide "ground truth" data during EMI exposure for comparison. |
| Data Acquisition System | Synchronously records data from both the FBG system and the reference system during tests. |
| Clinical Simulator/Phantom | A tissue-equivalent model or mechanical setup to simulate the physiological parameter the FBG is measuring (e.g., temperature-controlled water bath, pressure chamber). |
Protocol: Radiated RF Immunity Test (Sample)
- Setup: Place the FBG interrogator and display unit in the EMC chamber. Route the optical fiber with the FBG sensor to the external clinical simulator. The reference sensor is placed adjacent to the FBG within the simulator.
- Baseline Measurement: With no RF field, record measurements from both the FBG and reference systems for 2 minutes under stable simulated physiological conditions.
- EMI Exposure: Activate the RF field. Sweep the frequency range from 80 MHz to 2.7 GHz at a specified sweep rate (e.g., 1.5 x 10⁻³ decades/sec). Maintain the field strength at 3 V/m.
- Concurrent Monitoring: Throughout the sweep, continuously and simultaneously record the output from the FBG system and the reference system.
- Post-Exposure: After the sweep, continue recording for an additional 2 minutes with the RF field off.
- Data Analysis: For each frequency step, calculate the deviation of the FBG reading from the reference reading. Determine if the deviation exceeds the pre-defined acceptable limit for essential performance. The system passes if deviations remain within limits at all test frequencies.
- Repetition: Repeat the test with the antenna polarized both vertically and horizontally.
Part 3: Integrated Regulatory Pathway
FDA (U.S.) and CE Marking (Europe) approvals require a structured quality management system (QMS: 21 CFR Part 820/ISO 13485) and a risk-based demonstration of safety and performance.
Comparison of Key Regulatory Submission Elements:
| Aspect | FDA (510(k) Pathway) | CE Marking (MDR) |
|---|---|---|
| QMS Foundation | 21 CFR Part 820 | ISO 13485 |
| Risk Management | ISO 14971 integrated into design controls | ISO 14971 mandatory |
| Essential Documentation | 510(k) Submission: Includes Device Description, Substantial Equivalence Comparison, Performance Data (including EMC testing), Labeling, Biocompatibility. | Technical Documentation: General Safety & Performance Requirements (GSPR) checklist, Design & Manufacturing info, Risk Management File, Verification/Validation reports (including EMC), Clinical Evaluation Report. |
| EMC Evidence | Summary report of testing to IEC 60601-1-2 (recognized standard). Testing often performed by an accredited lab. | Full test report from an ISO/IEC 17025 accredited lab. Must be reviewed by a Notified Body for Class IIa/IIb/III devices. |
| Clinical Data | Required if predicate comparison is insufficient or for new indications. | Clinical Evaluation Report (CER) mandatory for all classes, proportionate to risk. |
| Reviewing Body | FDA's Center for Devices and Radiological Health (CDRH). | A designated Notified Body (for Class IIa and above). |
Diagram: Integrated Development & Regulatory Workflow
Diagram Title: Medical Device Regulatory Pathway from Research to Market
Diagram: EMI Immunity Test Setup for FBG System
Diagram Title: Radiated RF Immunity Test Configuration for FBG Sensor
Successful regulatory approval for FBG-based medical devices hinges on a methodical, evidence-based approach. Integrating EMI immunity testing per IEC 60601-1-2 into the device development lifecycle from the research phase is critical. By defining essential performance, executing rigorous EMC protocols, and compiling comprehensive technical documentation, researchers and developers can navigate the FDA and CE marking pathways to bring robust, interference-resistant sensing solutions to the clinical environment.
The integration of Fiber Bragg Grating (FBG) sensors into next-generation medical devices demands a design philosophy centered on electromagnetic interference (EMI) immunity, scalability, and adaptability. This whitepatesr, framed within the critical context of EMI immunity research for FBG sensors, provides a technical guide for developing robust, future-proof medical sensing platforms. The passive, dielectric nature of FBGs presents a unique advantage in electromagnetically noisy clinical environments, from MRI suites to robotic surgical theaters, enabling reliable physiological monitoring and device feedback where conventional electronic sensors fail.
The proliferation of electronic medical equipment has intensified EMI in clinical settings. Concurrently, the drive towards miniaturized, implantable, and high-precision medical technologies necessitates sensors immune to these disruptions. Research into the EMI immunity of FBG sensors establishes a foundational thesis: optical sensing platforms are not merely an alternative but a prerequisite for scalable, adaptable, and reliable next-gen medical technology. Their inherent immunity to EMI ensures signal fidelity, patient safety, and data integrity, forming the cornerstone of future-proof design.
Core Principles: Scalability and Adaptability in FBG Systems
Scalability through Wavelength-Division Multiplexing (WDM)
FBG systems scale efficiently via WDM, allowing multiple sensors on a single optical fiber. This is paramount for distributed sensing in smart catheters, robotic surgical instruments, or wearable health monitors.
Table 1: Scalability Metrics for FBG Sensor Arrays
| Parameter | Conventional Electronic Sensor Array | FBG Sensor Array via WDM | Advantage |
|---|---|---|---|
| Channels per Cable | 1-16 (limited by crosstalk/power) | 64+ (limited by source bandwidth) | High-Density Multiplexing |
| EMI Susceptibility | High, requires shielding | Inherently Immune | Reliable in MRI/OR |
| Cable Diameter | Increases with channel count | Single fiber for all sensors | Miniaturization Enabled |
| Calibration Complexity | Per-channel electronics | Centralized interrogator | Simplified System Architecture |
Adaptability via Multi-Parameter Sensing
A single FBG can be sensitized to multiple physical parameters (strain, temperature, pressure), allowing a single sensor platform to adapt to diverse clinical needs through packaging and calibration.
Experimental Protocols for EMI Immunity Validation
Robust experimental validation is required to quantify EMI immunity.
Protocol: Radiated Immunity Testing of FBG vs. Electronic Strain Gauge
Objective: To compare the performance of an FBG strain sensor and a conventional resistive strain gauge under standardized EMI conditions. Materials: See "The Scientist's Toolkit" below. Methodology:
- Setup: Collocate the FBG sensor and electronic strain gauge on a calibrated cantilever beam within a shielded anechoic chamber.
- EMI Exposure: Subject the setup to radiated fields per IEC 60601-1-2.
- Frequency Range: 80 MHz to 2.7 GHz.
- Field Strength: 3 V/m and 10 V/m.
- Modulation: 80% AM at 1 kHz.
- Data Acquisition:
- Apply a known, cyclical mechanical deflection to the beam.
- Record simultaneous strain readings from both sensors during EMI exposure.
- Repeat under no-EMI baseline conditions.
- Analysis: Calculate signal-to-noise ratio (SNR) and error variance for both sensors under each test condition.
Protocol: In-Situ MRI Compatibility Testing
Objective: To assess FBG sensor performance inside a live MRI bore during imaging sequences. Methodology:
- Setup: Place an FBG temperature/pressure sensing array on a phantom inside a 3T MRI scanner. Place identical electronic reference sensors at a safe distance.
- Imaging Sequences: Run a series of standard sequences: Spin Echo (SE), Gradient Echo (GRE), and Echo-Planar Imaging (EPI).
- Monitoring: Continuously record data from all sensors during sequence activation and quiescent periods.
- Safety & Interference: Measure any imaging artifact introduced by the FBG system and any heating effects.
Table 2: Representative Experimental Data Summary
| Test Condition | FBG Sensor SNR (dB) | Electronic Sensor SNR (dB) | FBG Error Variance (%FS) | Electronic Sensor Error Variance (%FS) |
|---|---|---|---|---|
| Baseline (No EMI) | 52.1 | 48.7 | 0.12 | 0.15 |
| Radiated 3 V/m | 51.8 | 35.4 | 0.13 | 4.81 |
| Radiated 10 V/m | 51.5 | 24.1 | 0.15 | 18.72 |
| MRI GRE Sequence | 50.2 | N/A (Failed) | 0.18 | N/A |
System Architecture for Future-Proof Medical FBG Platforms
A scalable architecture separates the immutable sensing element (the FBG) from the evolving interrogation and data analytics layers.
Diagram Title: Modular FBG System Architecture for Medical Tech
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for EMI Immunity & FBG Medical Research
| Item | Function | Key Consideration for Future-Proofing |
|---|---|---|
| Polyimide-Coated FBGs | Primary sensing element. | High tensile strength, biocompatible, suitable for long-term implants. |
| Tunable Laser Interrogator | Reads FBG wavelength shift. | Scalability: Ensure sufficient scan rate & optical bandwidth for sensor count. |
| MRI-Compatible Phantom | Simulates human tissue properties. | Allows safe, repeatable testing of sensor-MRI interactions. |
| Biocompatible Encapsulant (e.g., Medical-Grade Silicone) | Protects FBG and isolates mechanical parameter. | Adaptability: Formulation determines sensor sensitivity (e.g., pressure vs. strain). |
| EMI Test Chamber | Provides controlled, standardized RF field. | Critical for quantitative, reproducible immunity validation per medical standards. |
| Optical Shape Sensing Software | Converts FBG array data into 3D shape. | Enables applications in steerable catheters and robotic surgical navigation. |
Future-proofing next-generation medical technologies necessitates a fundamental shift towards inherently immune sensing modalities. Research conclusively demonstrates that FBG sensors, with their unparalleled EMI immunity, provide the foundational robustness upon which scalable multiplexed networks and adaptable multi-parameter sensing platforms can be built. By adhering to the architectural principles and validation protocols outlined, researchers and developers can create medical devices capable of evolving alongside advancing clinical practice and thriving in the increasingly complex electromagnetic landscape of modern medicine.
Conclusion
Fiber Bragg Grating sensors represent a paradigm shift for reliable sensing in electromagnetically hostile medical and pharmaceutical environments. By leveraging fundamental photonic principles, they offer an inherently immune solution where traditional electronic sensors falter, ensuring data integrity and patient safety in critical applications from MRI suites to advanced drug delivery systems. While challenges in cross-sensitivity and clinical integration remain, methodological advancements and compelling validation studies underscore their unique value. For researchers and developers, embracing FBG technology is not merely an alternative but a strategic enabler for pioneering next-generation therapies, smart surgical platforms, and robust, interference-free biomedical monitoring, ultimately driving innovation where electromagnetic silence is paramount.