Clinical Validation of Bio-Optical Cancer Diagnostics: A Roadmap for Biomarker Translation and Regulatory Success
This article provides a comprehensive framework for the clinical validation of bio-optical cancer diagnostics, tailored for researchers and drug development professionals.
Clinical Validation of Bio-Optical Cancer Diagnostics: A Roadmap for Biomarker Translation and Regulatory Success
Abstract
This article provides a comprehensive framework for the clinical validation of bio-optical cancer diagnostics, tailored for researchers and drug development professionals. It explores the foundational principles of optical technologies like genome mapping, details rigorous methodological validation protocols integrating AI and multi-omics, and addresses key troubleshooting challenges in translational workflows. Furthermore, it offers a comparative analysis against standard cytogenetic techniques, synthesizing evidence to guide robust assay development, regulatory submission, and successful clinical implementation for precision oncology.
The Foundation of Bio-Optics in Oncology: From Light-Based Imaging to Clinical Insights
Bio-optics represents the innovative convergence of photonics—the science of light generation, detection, and manipulation—with biology and medicine. This dynamic field employs light-based technologies to analyze and manipulate biological materials, creating powerful tools for research and clinical diagnostics. A core application of biophotonics is in the realm of cancer detection and characterization, where technologies like optical genome mapping (OGM) and advanced imaging systems provide unprecedented insights into genetic and cellular abnormalities. These approaches leverage the unique properties of light, including non-contact measurement, high sensitivity, and real-time data acquisition, to reveal pathological changes without invasive procedures [1]. The field is rapidly evolving beyond traditional cytogenetic techniques, offering researchers and clinicians the ability to detect structural variations in the genome and visualize tissue abnormalities with resolution that far exceeds conventional methods.
This guide provides a comprehensive comparison of optical genome mapping against established cytogenetic techniques, detailing its experimental validation, technical workflows, and growing role in cancer research. For drug development professionals and researchers, understanding the capabilities and limitations of these technologies is crucial for selecting appropriate methods for genomic analysis and clinical study design.
Optical Genome Mapping: Technology and Workflow
Fundamental Principles
Optical genome mapping is a high-resolution cytogenomic technique that enables genome-wide detection of balanced and unbalanced structural variations using ultra-high molecular weight (UHMW) DNA. Unlike sequencing-based approaches that determine nucleotide order, OGM visualizes long DNA molecules to identify structural variations based on fluorescent labeling patterns. The technology utilizes specific sequences—CTTAAG hexamer motifs—as labeling sites, creating a genome-wide density of approximately 14-17 labels per 100 kb that serves as a unique "barcode" for each genomic region [2]. These patterns allow for direct comparison against a reference genome, enabling detection of deletions, duplications, insertions, translocations, and inversions without requiring cell culture or prior knowledge of the genome's structure [3].
The resolution and detection capabilities of OGM significantly surpass traditional cytogenetic methods. While chromosomal banding analysis typically resolves abnormalities larger than 5-10 Mb, and FISH can detect variations of 60 kb-1 Mb, OGM reliably identifies structural variations down to 500 bp in size, depending on the analysis pipeline and coverage depth [3] [2]. This resolution, combined with its ability to span complex repetitive regions that challenge short-read sequencing technologies, positions OGM as a powerful tool for uncovering previously cryptic genomic rearrangements in cancer research.
Detailed Experimental Protocol
Implementing OGM requires strict adherence to specific protocols to preserve DNA integrity and ensure data quality:
DNA Extraction: Isolation of UHMW DNA is critical and utilizes a specialized paramagnetic disk-based protocol designed to minimize shearing forces. This method routinely yields DNA fragments averaging >230 kb in size, substantially longer than conventional extraction techniques [4] [2]. The process requires viable cells that cannot be previously fixed, which can be frozen for future use.
Fluorescent Labeling: Extracted DNA is fluorescently labeled at the specific CTTAAG recognition motifs. This is achieved through a covalent modification process that labels the DNA without digesting it, creating the unique pattern of fluorescent tags that serves as the barcode for subsequent analysis [3] [2].
Linearization and Imaging: Labeled DNA molecules are loaded into nanochannel arrays on silicon chips, where they become linearized. As each molecule passes through the channels, high-resolution imaging systems capture the fluorescent label patterns. Current instrumentation can generate up to 5000 Gbp of raw data per flow cell, enabling theoretical genome coverage up to 1250× [2].
Data Analysis: Specialized algorithms convert the captured images into digitalized molecule maps. These are assembled and compared to an in silico reference genome. Two primary analysis pipelines are employed:
- De novo Assembly: Typically used for germline (constitutional) analysis at >80× coverage (>400 Gbp data)
- Rare Variant Analysis (RVP): Used for somatic studies (e.g., cancer) with sensitivity down to ~5% variant allele fraction at >340× coverage (>1500 Gbp data) [2].
The entire workflow, from DNA extraction to final analysis, requires approximately four days, with the majority of time dedicated to automated imaging and computational analysis [2].
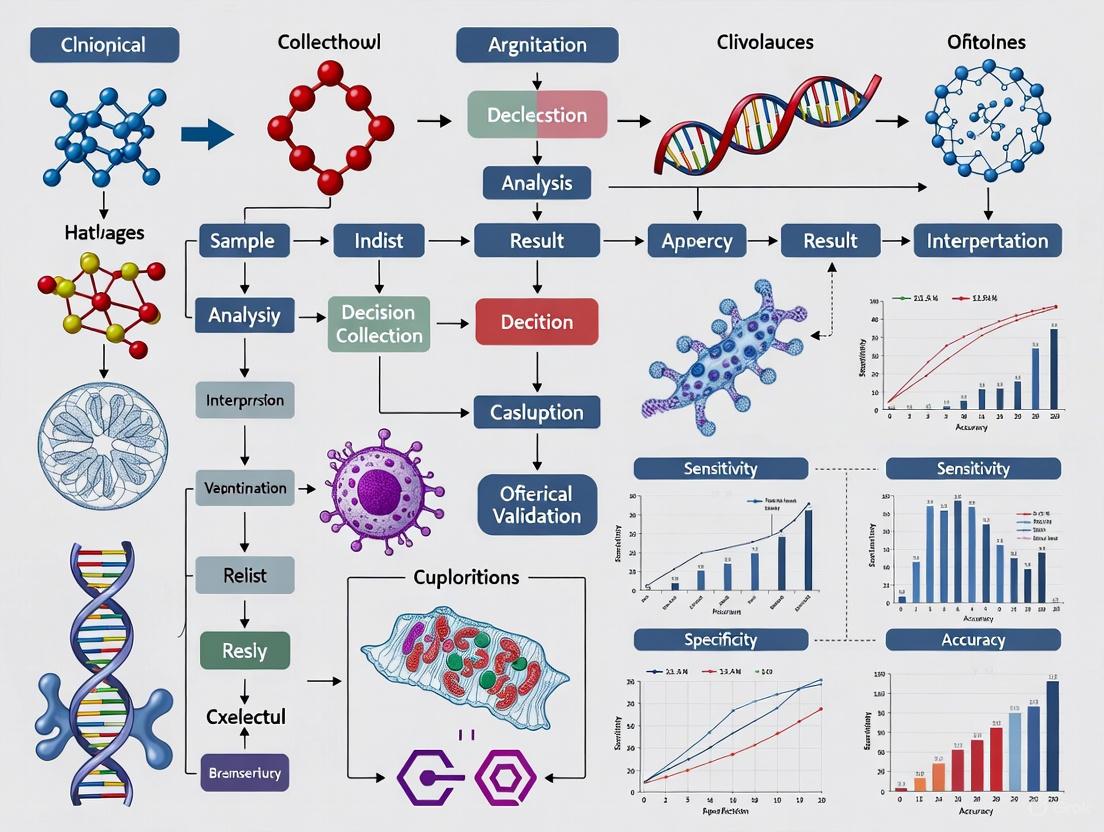
OGM Experimental Workflow: The process from sample preparation to data analysis, highlighting key steps requiring specialized reagents and equipment.
Comparative Performance Analysis
Detection Capabilities Across Cytogenetic Platforms
The selection of cytogenetic testing methodology significantly impacts the types and sizes of genomic abnormalities detectable in cancer genomics research. The table below provides a comprehensive comparison of OGM against established techniques.
Table 1: Technology Comparison for Structural Variant Detection in Cancer Genomics
| Methodology | Resolution | SV Types Detected | Limit of Detection | Genome-Wide | Balanced SV Detection | Key Limitations |
|---|---|---|---|---|---|---|
| G-Banded Chromosome Analysis | 5-10 Mb | CNV, SV | ~10% (single cell) | Yes | Limited | Poor resolution, requires cell culture |
| Fluorescence In Situ Hybridization (FISH) | 60 kb - 1 Mb | CNV, SV | ~2-5% (single cell) | Targeted only | Limited | Targeted approach, genome blind spots |
| Chromosomal Microarray (CMA) | 25 kb | CNV, AOH* | ~10-15% (bulk) | Yes | No | Cannot detect balanced rearrangements |
| Next-Generation Sequencing (NGS) | Single nucleotide | SNV, CNV, SV* | ~1-5% (bulk) | Yes* | Yes* | Complex SV detection challenging |
| Optical Genome Mapping (OGM) | 500 bp - 5 kb | CNV, SV, AOH, Repeat expansions | ~5% (bulk) | Yes | Yes | Requires UHMW DNA, not high-throughput |
AOH: Absence of Heterozygosity; *Capabilities vary by NGS approach and bioinformatic pipelines [3] [2]
OGM demonstrates particular strength in resolving complex structural variants (cxSVs), which involve multiple breakpoints and rearrangement types. Research indicates OGM can resolve interspersed duplications up to approximately 550 kb in size by obtaining multiple individual DNA molecules completely spanning the duplicated segment [4]. This capability is critical in cancer genomics, where such complex rearrangements can drive oncogenesis.
Analytical Performance and Validation Data
Clinical validation studies demonstrate OGM's robust performance characteristics. One comprehensive evaluation involving 92 sample runs (including replicates) with 59 hematological neoplasms and 10 controls reported:
- Sensitivity: 98.7%
- Specificity: 100%
- Accuracy: 99.2%
- First-pass technical success rate: 100% [5]
The study determined OGM's limit of detection to be at a 5% allele fraction for aneuploidy, translocation, interstitial deletion, and duplication, making it suitable for detecting minor clones in heterogeneous tumor samples [5]. In reproducibility assessments, OGM demonstrated excellent inter-run, intra-run, and inter-instrument consistency [5].
In a study focusing on multiple myeloma, OGM demonstrated significant clinical utility by either improving genetic diagnosis or detecting additional alterations beyond what was identified by targeted FISH analysis [6]. For hematologic malignancies, research shows OGM identifies clin relevant SVs in 34% of patients that were cytogenetically cryptic, with 17% of cases having findings that would have changed risk assessment [2].
Complementary Bio-Optical Imaging Technologies
Beyond genome mapping, other biophotonic approaches are advancing cancer detection through tissue and cellular imaging:
Hyperspectral Imaging (HSI): This technology captures data across hundreds of narrow wavelengths in addition to visible light, revealing subtle tissue differences based on unique spectral signatures. Researchers are miniaturizing HSI systems for integration with endoscopes to improve real-time detection of gastrointestinal cancers, with the goal of reducing the approximately 10% of GI cancers missed by standard endoscopy [7].
Stimulated Raman Scattering (SRS) Imaging: This label-free technique leverages Raman scattering to distinguish cancer cells from normal cells based on their vibrational characteristics. Particularly valuable for brain tumor surgery, SRS imaging can visualize lipid droplets in fresh, native condition, potentially enabling intraoperative tumor margin assessment without time-consuming histological processing [8].
PET-enabled Dual-Energy CT: This hybrid imaging innovation combines positron emission tomography (PET) with dual-energy computed tomography (CT). By using PET data to create a second, high-energy CT image, it provides enhanced tissue composition analysis alongside metabolic information, potentially improving differentiation between healthy and cancerous tissues [9].
These imaging modalities complement OGM by providing spatial context in tissues, while OGM offers comprehensive genomic structural information, together creating a multi-scale bio-optical diagnostic toolkit.
Essential Research Reagent Solutions
Implementing OGM requires specific reagents and materials designed to preserve macromolecular integrity and enable high-resolution analysis.
Table 2: Essential Research Reagents for Optical Genome Mapping
| Reagent/Material | Function | Technical Specifications | Importance for Assay Quality |
|---|---|---|---|
| Ultra-High Molecular Weight (UHMW) DNA Isolation Kit | Extracts long DNA fragments while minimizing shear | Paramagnetic disk-based purification; average fragment size >230 kb | Foundation of entire assay; shorter fragments reduce genome coverage and SV resolution |
| Direct Labeling and Staining Reagents | Fluorescently labels specific sequence motifs (CTTAAG) | Label density ~14-17 labels/100 kb; covalent binding | Creates unique "barcode" pattern for genome alignment; inconsistent labeling affects variant calling |
| Nanochannel Chips | Linearizes DNA molecules for imaging | Hundreds of thousands of parallel nanochannels | Ensures uniform molecule stretching for accurate label pattern measurement |
| Reference Genome | In silico comparison for variant detection | Species-specific assembled genome (e.g., GRCh38 for human) | Accuracy of structural variant identification depends on reference quality and completeness |
| Data Analysis Software | Identifies structural variants from raw image data | Supports de novo (germline) and rare variant (somatic) pipelines | Critical for sensitivity/specificity; requires appropriate coverage (>80× germline, >340× somatic) |
Optical genome mapping represents a significant advancement in the bio-optical diagnostics landscape, offering researchers a powerful tool for comprehensive structural variant detection. With its high resolution, ability to detect balanced and unbalanced rearrangements in a single assay, and demonstrated superior diagnostic yield compared to traditional cytogenetic methods, OGM addresses critical gaps in cancer genomics research. While the technology requires specialized reagents and bioinformatic support, its capacity to resolve complex genomic architectures provides valuable insights for tumor classification, prognostication, and therapeutic development. As the field progresses, integration of OGM with complementary bio-imaging technologies and sequencing approaches will further enhance our understanding of cancer biology and accelerate the development of targeted treatments.
Cytogenetics, the study of chromosomes and their role in human disease, has long been a cornerstone of genetic diagnostics and cancer research [10]. For over four decades, conventional karyotype analysis has provided a global assessment of chromosomal numerical and structural abnormalities, serving as a powerful view of the entire human genome [11]. However, this established technique represents what many consider a 'scientific art'—requiring extensive training, expertise, and manual interpretation that is becoming increasingly difficult to sustain as skilled cytogeneticists retire [11]. The limitations of these standard approaches have created critical unmet needs in both research and clinical diagnostics, particularly as we enter an era demanding higher resolution, greater efficiency, and more comprehensive genomic assessment.
The field has evolved through several technological revolutions, from classic G-banded karyotyping to molecular cytogenetic techniques like fluorescence in situ hybridization (FISH), and more recently to chromosomal microarrays (CMA) [10] [11]. Each advancement has addressed specific limitations while introducing new constraints. Currently, comprehensive analysis of structural variants in hematological malignancies requires a combination of multiple cytogenetic techniques, including karyotyping, FISH, and CNV microarrays [12] [13]. This multi-assay approach is labor-intensive, time-consuming, and costly, creating significant barriers to optimal patient management in oncology and other genetic fields.
This article objectively compares the performance of emerging bio-optical technologies with standard cytogenetic techniques, focusing specifically on Optical Genome Mapping (OGM) as a representative next-generation cytogenomic approach. Through examination of experimental data and validation studies, we demonstrate how these innovative methodologies are addressing the critical limitations that have long constrained conventional cytogenetic analysis.
Limitations of Standard Cytogenetic Techniques
Technical and Resolution Constraints
Conventional cytogenetic techniques face fundamental limitations that impact their diagnostic accuracy and clinical utility. Karyotype analysis, while providing a genome-wide view, has a resolution limit of approximately 5-10 megabases (Mb), preventing detection of smaller but clinically significant structural variations [10] [12]. This technique requires cell culture, which introduces selection bias and fails in 10-40% of cases due to culture failure or microbial contamination [14]. Additionally, karyotyping is labor-intensive, low-throughput, and reliant on highly trained technologists capable of interpreting complex banding patterns [11] [14].
FISH, while offering higher resolution for specific genomic regions, is inherently targeted—requiring prior knowledge of which regions to interrogate [12]. This technique cannot identify novel gene fusions or characterize unknown partner genes in translocations [12]. Furthermore, FISH is labor-intensive, and quality-assured probes are expensive, making comprehensive genome-wide assessment impractical [14]. Chromosomal microarray analysis (CMA) provides high resolution for detecting copy number variations but cannot identify balanced chromosomal rearrangements such as translocations or inversions, which are crucial drivers in many cancers [12].
Diagnostic Gaps in Clinical Practice
The limitations of standard techniques create significant diagnostic gaps in clinical practice. In cancer cytogenetics, 'phenocopies' or 'mimics' present a serious challenge—these appear under the microscope as recurrent oncogenic rearrangements but do not involve the relevant genes [11]. Studies suggest approximately 1% of rearrangements reported as recurrent oncogenic abnormalities may be these non-functional mimics, with potentially serious implications for clinical management [11].
In the analysis of products of conception (POC) for recurrent pregnancy loss, conventional karyotyping fails to provide results in 10-40% of cases due to culture failures [14]. When molecular techniques like multiplex ligation-dependent probe amplification (MLPA) are used as alternatives, they cannot characterize balanced structural rearrangements (like Robertsonian translocations) or ploidy changes, which comprise 2.46% of samples (99% confidence interval = 0.09-4.83) [14]. For mesenchymal neoplasms, cytogenetic analysis requires fresh tissue (not frozen or fixed in formalin), creating significant logistical challenges for pathologists who may prematurely place specimens in fixative [15].
Table 1: Key Limitations of Standard Cytogenetic Techniques
| Technique | Resolution Limit | Major Constraints | Failure Rate |
|---|---|---|---|
| Karyotyping | 5-10 Mb | Culture bias, subjective interpretation, labor-intensive | 10-40% [14] |
| FISH | 50-500 kb | Targeted approach only, cannot identify novel fusions | Varies by sample quality |
| CMA | Few kb | Cannot detect balanced rearrangements | 1-5% |
| MLPA | Varies by probe spacing | Cannot detect balanced rearrangements or ploidy changes | ~1% [14] |
Optical Genome Mapping: An Emerging Solution
Optical Genome Mapping (OGM) represents a paradigm shift in cytogenomic analysis, functioning as what has been termed "next-generation cytogenetics" [12]. This genome-wide technology detects both structural variants (SVs) and copy number variations (CNVs) in a single assay, overcoming the piecemeal approach required by traditional techniques [12]. OGM is based on imaging ultra-long (>150 kbp) high-molecular-weight DNA molecules that are fluorescently labeled at specific sequence motifs [12] [11].
The most common platform currently used for OGM is the Saphyr system from Bionano Genomics [12]. The workflow involves: (1) extracting ultra-high molecular weight DNA from fresh or frozen samples; (2) labeling DNA at specific sequence motifs (CTTAAG) using an enzyme (DLE-1) that achieves a label density of approximately 15 labels per 100 kb; (3) linearizing the labeled DNA molecules in nanochannel arrays; (4) imaging the genome-wide fluorescent pattern; and (5) comparing the results to a reference genome to identify structural variants [12]. Recently, Bionano introduced a direct labeling and staining (DLS) method that shows a 50x improvement in labeling contiguity compared to the DLE-1 enzyme system [12].
Two bioinformatic pipelines are used for data analysis: a rare variant pipeline (RVP) designed to identify variants at low allele frequencies (as low as 5% variant allele frequency), and a de novo assembly approach that can detect smaller SVs (approximately 500 bp) but has lower sensitivity for rare events (15-25% variant allele frequency) [12]. The system provides multiple visualization methods including Circos plots, genome browser views, and whole-genome plots that display copy number, absence of heterozygosity, and variant allele fractions [12].
Advantages Over Conventional Approaches
OGM offers several distinct advantages over the cascade of conventional diagnostic tests. It provides a more rapid, less labor-intensive approach that avoids the need for multiple techniques [12]. Where conventional approaches require a combination of karyotyping, FISH, and CMA to fully characterize genomic alterations—a process taking more than 20 days—OGM can provide comprehensive assessment in approximately one week [12].
The resolution of OGM represents a significant improvement over conventional techniques. While karyotyping has a resolution limit of about 5 Mb, OGM can detect structural variants from 500 bp up to tens of Mb, representing a 100x-20,000x improvement in resolution depending on the variant type and analysis tools used [12]. Unlike CMA, OGM can detect balanced chromosomal rearrangements including translocations and inversions [12]. Furthermore, OGM can identify novel translocations leading to gene disruption or new fusions involving genes that are important drivers of cancer pathogenesis and targeted therapy [12].
OGM is particularly powerful for characterizing complex genomic rearrangements such as chromothripsis and chromoplexy (collectively termed chromoanagenesis), which involve hundreds of genomic rearrangements caused by chromosomal shattering and random reassembly [12]. The technology can also identify additional material in marker chromosomes and define rearrangement breakpoints with precision of a few kilobases [12].
OGM Workflow: From DNA to Variant Detection
Experimental Validation and Performance Comparison
Analytical Performance in Hematological Malignancies
Multiple studies have validated OGM's performance against standard cytogenetic techniques in hematological malignancies. In a comprehensive study of 52 individuals with hematological malignancies, OGM demonstrated excellent concordance with diagnostic standard assays [13]. Samples were divided into simple (<5 aberrations, n=36) and complex (≥5 aberrations, n=16) cases, with OGM reaching an average of 283-fold genome coverage [13].
For the 36 simple cases, OGM detected all clinically reported aberrations identified through standard techniques, including deletions, insertions, inversions, aneuploidies, and translocations [13]. In the 16 complex cases, results were largely concordant between standard-of-care tests and OGM, but OGM often revealed higher complexity than previously recognized [13]. The study reported sensitivity of 100% and a positive predictive value of >80% for OGM compared to standard techniques [13].
Notably, OGM provided a more complete assessment than any single previous test and most likely reported the most accurate underlying genomic architecture for complex translocations, chromoanagenesis, and marker chromosomes [13]. The technology was particularly effective in defining rearrangements involving genes with multiple possible partners, such as KMT2A, MECOM, ETV6, NUP98, or IGHV in hematological malignancies [12]. These rearrangements are typically investigated using FISH with break-apart probes, which cannot identify the partner gene without additional targeted testing [12].
Quantitative Comparison of Technical Parameters
Table 2: Performance Comparison of Cytogenetic Techniques
| Parameter | Karyotyping | FISH | CMA | OGM |
|---|---|---|---|---|
| Resolution | 5-10 Mb [12] | 50-500 kb | Few kb [12] | 500 bp-1 Mb [12] |
| SV Detection | All types (≥5 Mb) | Targeted only | None for balanced [12] | All types [12] |
| CNV Detection | ≥5 Mb | Targeted only | Few kb [12] | >500 kb [12] |
| Turnaround Time | 7-14 days | 2-3 days | 7-14 days | ~7 days [12] |
| Success Rate | 60-90% [14] | >95% | >95% | >98% [12] |
| VAF Sensitivity | 10-20% | 5-10% | 10-20% | 5% (RVP) [12] |
Table 3: Detection Capabilities for Specific Variant Types
| Variant Type | Karyotyping | FISH | CMA | OGM |
|---|---|---|---|---|
| Aneuploidy | Yes | Targeted | Yes | Yes [12] |
| Translocations | Yes (≥5 Mb) | Targeted | No | Yes [12] |
| Inversions | Yes (≥5 Mb) | Targeted | No | Yes [12] |
| Microdeletions | No | Targeted | Yes | Yes [12] |
| Marker Chromosomes | Yes | Partial | Partial | Yes [12] |
| Ring Chromosomes | Yes | Partial | Partial | Yes [12] |
| Chromothripsis | Limited | No | Partial | Yes [12] |
| Ploidy Changes | Yes | No | Yes | Limited [12] |
Research Reagent Solutions for OGM Implementation
Successful implementation of OGM requires specific research reagents and materials optimized for the technology. The following table details essential components for establishing OGM in a research setting:
Table 4: Key Research Reagent Solutions for Optical Genome Mapping
| Reagent/Material | Function | Specification Considerations |
|---|---|---|
| Ultra-High Molecular Weight DNA Isolation Kits | Extract long DNA strands preserving molecular integrity | Minimum DNA length >150 kbp; minimize double-strand breaks |
| Sequence-Specific Labeling Enzymes | Tag specific genomic motifs for visualization | DLE-1 enzyme targets CTTAAG motifs; new DLS chemistry available |
| Fluorescent Labeling Dyes | Enable detection of labeled DNA molecules | High quantum yield; photostability; compatible with imaging system |
| Nanochannel Chips | Linearize DNA molecules for imaging | Uniform channel size; surface treatments to prevent adhesion |
| Size Standards | Calibrate molecule length measurements | DNA molecules of known length; stable under imaging conditions |
| Reference Genome Databases | Compare sample data against reference | Species-specific; regularly updated; comprehensive variant annotation |
| Bioinformatic Analysis Software | Identify, annotate, and visualize variants | User-friendly interface; clinical-grade validation; customizable filters |
Discussion: Implications for Research and Clinical Applications
The comprehensive data from validation studies demonstrates that OGM effectively addresses the critical unmet needs in conventional cytogenetic techniques. By providing a complete assessment of global genomic alterations in a single assay, OGM represents a significant advancement for both research and potential clinical applications [12] [11] [13]. The technology's ability to detect novel clinically significant structural variants suggests it will contribute to better patient classification, prognostic stratification, and therapeutic choices in hematological malignancies [12].
From a research perspective, OGM enables studies of chromoanagenesis and complex karyotypes with unprecedented resolution [12]. The technology has revealed that submicroscopic structural variants smaller than 5 Mb that overlap critical genes involved in leukemogenesis are highly under-ascertained with current testing [11]. Recent studies estimate that up to 25% of deleterious mutations in the human genome may result from structural variants [11], highlighting the importance of comprehensive detection methods.
For clinical applications, OGM shows potential to replace the multiple techniques currently required for complete cytogenetic assessment [12] [11] [13]. The technology's higher resolution and ability to detect all variant types in a single assay address the major limitations of both conventional and molecular cytogenetic techniques. However, certain limitations remain, including difficulty detecting ploidy changes, copy-number neutral loss of heterozygosity, and variants in centromeric and telomeric regions [12]. Additionally, false positive rearrangements have been reported in some studies, necessitating confirmation of clinically significant findings with orthogonal methods [12].
The future of cytogenetics lies not in abandoning classical approaches but in integrating new technologies that expand our capabilities. As one editorial eloquently stated, "Cytogenetics is a science that deals with the number, structure, and function of chromosomes within the nucleus and the role of chromosome abnormalities in human disease. While the tools we use to assess the structure and function of chromosomes may change, the study of cytogenetics retains its scope and significance" [11]. Optical Genome Mapping and other advanced genomic technologies represent the next evolution in this ongoing scientific journey, promising to unlock new discoveries in basic chromosome biology and clinical disease mechanisms.
Addressing Technical Limitations with OGM Solutions
In the field of bio-optical cancer diagnostics, establishing robust benchmarks for sensitivity, specificity, and accuracy is paramount for translating research innovations into clinically validated tools. These metrics form the foundation for evaluating diagnostic performance, guiding regulatory approval, and ultimately building clinical trust. The emergence of sophisticated technologies—from artificial intelligence (AI)-enhanced imaging to ultra-sensitive biomarker assays—has necessitated increasingly stringent performance standards to ensure reliable patient outcomes.
Diagnostic markers generally fall into three categories: diagnostic markers that identify tissue of origin or tumor subtype, prognostic markers that estimate disease outcome likelihood, and predictive markers that forecast response to specific therapies [16]. For a marker and its associated assay to be clinically useful, it must meet two critical criteria: it must be measurable by a reliable and widely available assay, and it must provide information about the disease that is meaningful to both physicians and patients [16].
This guide objectively compares the performance of contemporary diagnostic platforms, detailing their experimental protocols and establishing benchmark values essential for researchers, scientists, and drug development professionals working in cancer diagnostics.
Performance Benchmark Tables for Diagnostic Technologies
Table 1: Performance Benchmarks for AI-Based Optical Diagnostic Systems
| Technology | Clinical Application | Sensitivity | Specificity | Accuracy | AUC |
|---|---|---|---|---|---|
| AI-OCT (SVM/KNN) [17] | Diabetic Macular Edema (Binary Classification) | Not Reported | Not Reported | 92% | Not Reported |
| niceAI (XAI System) [18] | Colorectal Polyp Classification (Adenomatous vs. Hyperplastic) | 88.8% | 87.9% | 88.3% | 0.946 |
| BlurryScope [19] | Breast Cancer HER2 Scoring (Binary: 0/1+ vs. 2+/3+) | Not Reported | Not Reported | ~90% | Not Reported |
Table 2: Performance Benchmarks for Biomarker Assays
| Technology | Clinical Application | Sensitivity | Specificity | Accuracy | Key Feature |
|---|---|---|---|---|---|
| Simoa p-Tau 217 [20] | Alzheimer's Amyloid Pathology Detection | >90% | >90% | >90% | Two-cutoff approach |
| UBC Rapid Assay [21] | Bladder Cancer Detection | Variable with cutoff | Variable with cutoff | Variable with cutoff | Optimal cutoff derivation via ROC index |
Table 3: Molecular Methods in Cancer Genetics
| Technique | Key Feature | Representative Application | Detection Limit |
|---|---|---|---|
| ddPCR [22] | Quantitative detection of rare alleles | Detection of PIK3CA mutations in breast cancer | MAF < 0.1% |
| RT-PCR [22] | High sensitivity for tissue-specific genes | Detection of circulating breast cancer cells | 10 cells per 3 mL blood |
| Ultra-SEEK [22] | Multiplex detection capability | Cancer mutation panels | MAF ~0.1% |
Experimental Protocols for Benchmark Establishment
AI-Enhanced Optical Coherence Tomography (OCT)
Objective: To evaluate the performance of AI-based software against conventional clinical assessment of OCT images for diagnosing diabetic macular edema (DME) [17].
Methodology:
- Study Design: Prospective, non-randomized comparative study analyzing 700 OCT exams.
- Feature Vector: 26 features including demographic data (age, sex), eye laterality, visual acuity, and 21 quantitative OCT parameters.
- AI Models: Compared logistic regression, support vector machines (SVM), K-nearest neighbors (KNN), and decision tree models.
- Feature Engineering: Applied paraconsistent feature engineering (PFE) to isolate diagnostically relevant variables.
- Classification Scenarios: Binary (DME presence vs. absence) and multiclass (six distinct DME phenotypes).
Performance Validation: The study used specialist physician diagnosis as the reference standard. In binary classification using all features, SVM and KNN achieved 92% accuracy. When restricted to four PFE-selected features, accuracy declined modestly to 84% for logistic regression and SVM [17].
Explainable AI for Optical Diagnosis in Colonoscopy
Objective: To develop an explainable AI method (niceAI) for classifying hyperplastic and adenomatous polyps that aligns with endoscopists' decision-making processes [18].
Methodology:
- Feature Extraction: Initially identified 2,048 deep features, 93 radiomics features, and color features.
- Feature Selection: Employed multi-step selection using Spearman's correlation analysis:
- First Selection: 103 deep features and 30 radiomics features showed significant correlation (R > 0.5, p < 0.05).
- Second/Third Selection: Compared performance of deep features with NICE feature grading using R² score, identifying optimal combinations (e.g., nine deep features for surface pattern Type 1, six for Type 2).
- Model Integration: Merged selected deep features with narrow-band imaging International Colorectal Endoscopic (NICE) grading.
- Reference Standard: Histopathological diagnosis of hyperplastic versus adenomatous polyps.
Performance Validation: The system achieved an area under the curve (AUC) of 0.946, sensitivity of 0.888, specificity of 0.879, and accuracy of 0.883, meeting SODA (sensitivity > 0.8; specificity > 0.9) and PIVI 2 (negative predictive value > 0.9 for high-confidence images) benchmarks [18].
Digital Immunoassay for Plasma Biomarker Detection
Objective: To analytically and clinically validate a high-accuracy fully automated digital immunoassay for plasma phospho-Tau 217 [20].
Methodology:
- Technology: Single molecule array (Simoa) technology on HD-X instrument, a fully automated digital immunoassay analyzer.
- Assay Principle: 3-step sandwich immunoassay using anti-p-Tau 217 coated paramagnetic capture beads and biotinylated detector antibodies.
- Calibration: Peptide construct with N-terminal epitope and phosphorylated mid-region epitope, with calibrators ranging from 0.002-10.0 pg/mL.
- Study Population: 873 symptomatic individuals from two independent clinical cohorts.
- Reference Standard: Amyloid status determined by PET or cerebrospinal fluid biomarkers.
- Cutoff Strategy: Implemented a 2-cutoff approach with an intermediate "gray zone" (30.9% of samples) to maximize predictive values.
Performance Validation: The assay demonstrated >90% sensitivity, specificity, and agreement with comparator methods for samples outside the intermediate zone, meeting Alzheimer's Association recommended accuracy of ≥90% for diagnostic use [20].
Compact AI-Powered Microscopy
Objective: To develop a compact, cost-effective scanning microscope (BlurryScope) for HER2 scoring in breast cancer tissue samples [19].
Methodology:
- Imaging Approach: Continuous scanning producing motion-blurred images, interpreted by a specially trained deep neural network.
- Hardware: Compact system (35 × 35 × 35 cm, 2.26 kg) built for <$650 versus conventional scanners costing >$100,000.
- Sample Preparation: Standard HER2-stained breast cancer tissue sections.
- Classification: Four HER2 scoring categories (0, 1+, 2+, 3+) grouped into clinically actionable binary categories (0/1+ versus 2+/3+).
- Validation: Blinded experiments with 284 unique patient tissue cores with reproducibility testing.
Performance Validation: Achieved nearly 80% accuracy across four HER2 categories and approximately 90% accuracy for binary classification, with >86% reproducibility across repeated scans [19].
Diagnostic Parameter Relationships and Cutoff Optimization
Diagram 1: Diagnostic metric relationships as cutoff changes. PPV: Positive Predictive Value; NPV: Negative Predictive Value; FN: False Negative; FP: False Positive.
The relationship between sensitivity and specificity represents a fundamental trade-off in diagnostic test design. As the cutoff value for test positivity increases, sensitivity typically decreases while specificity increases [21]. This inverse relationship necessitates careful optimization based on clinical context.
Traditional ROC curve analysis plotting sensitivity versus (1-specificity) has been supplemented with newer approaches that provide more comprehensive diagnostic profiling. Recent methodologies include:
- Multi-Parameter ROC Curves: Integrating accuracy, precision, and predictive values alongside sensitivity and specificity [21].
- Cutoff-Index Diagrams: Enabling visualization of optimal cutoffs that balance multiple diagnostic parameters simultaneously [21].
- Two-Cutoff Approach: Implementing dual thresholds to create "rule-out" and "rule-in" zones with high confidence, acknowledging an intermediate "gray zone" where diagnostic certainty is lower [20].
For clinical decision-making, predictive values (PPV and NPV) often provide more actionable information than sensitivity and specificity alone, as they incorporate disease prevalence and provide the probability of disease given a test result [21].
Research Reagent Solutions for Diagnostic Development
Table 4: Essential Research Reagents and Materials for Diagnostic Development
| Reagent/Material | Function | Example Application |
|---|---|---|
| Paramagnetic Capture Beads [20] | Immobilize target molecules for detection | Simoa p-Tau 217 assay |
| Biotinylated Detector Antibodies [20] | Bind to captured analyte for signal generation | Digital immunoassays |
| Streptavidin-β-galactosidase (SβG) Conjugate [20] | Enzyme label for signal amplification | Simoa technology |
| Resorufin β-D-galactopyranoside (RGP) [20] | Fluorogenic substrate for enzymatic signal detection | Digital immunoassays |
| Purified Peptide Constructs [20] | Calibrator material for assay standardization | p-Tau 217 assay calibration |
| Heterophilic Blockers [20] | Prevent interference from heterophilic antibodies | Immunoassay reliability |
| LabelEncoder (Scikit-learn) [17] | Encode categorical variables for machine learning | AI-OCT data preprocessing |
Establishing robust benchmarks for sensitivity, specificity, and accuracy remains crucial for advancing bio-optical cancer diagnostics from research tools to clinically validated solutions. The technologies examined demonstrate that while high performance is achievable across diverse platforms, the optimal approach depends heavily on the specific clinical context and application requirements.
The evolving landscape of cancer diagnostics shows a clear trend toward multi-parameter assessment, AI-enhanced interpretation, and careful cutoff optimization to maximize clinical utility. By adhering to rigorous validation standards and transparent reporting of performance metrics, researchers can accelerate the translation of innovative diagnostic technologies into tools that meaningfully impact patient care.
The Expanding Role of AI in Enhancing Bio-Optical Image Analysis and Data Interpretation
The integration of artificial intelligence (AI) with bio-optical imaging is fundamentally transforming oncology research and diagnostic validation. This synergy is addressing one of the most significant challenges in modern cancer care: the accurate and reproducible interpretation of complex biological images to guide therapeutic decisions. Bio-optical imaging—encompassing techniques from digital pathology to in vivo imaging—generates vast, information-rich datasets. AI algorithms, particularly deep learning and multimodal systems, are now unlocking nuanced patterns within this data that often elude human observation, thereby accelerating the path to clinical validation of novel cancer diagnostics [23] [24]. This evolution is critical for advancing precision oncology, as it enables the connection of visual morphological patterns with underlying molecular pathways and clinical outcomes.
The field is rapidly progressing from providing basic assistance to pathologists toward powering autonomous diagnostic systems and discovering novel biomarkers. By 2025, AI is no longer a speculative technology but an inseparable component of the biotech research process, converting previously impossible analytical tasks into routine procedures [25]. This review objectively compares the current performance of leading AI technologies enhancing bio-optical image analysis, detailing their experimental validation within the critical context of clinical cancer diagnostics.
Comparative Analysis of AI-Enhanced Bio-Optical Technologies
The performance of AI in bio-optical analysis can be evaluated across several key domains, including diagnostic precision, prognostic stratification, and molecular phenotype prediction. The table below summarizes quantitative data from recent studies and validated commercial tools, providing a direct comparison of their capabilities.
Table 1: Performance Comparison of AI Technologies in Bio-Optical Image Analysis for Oncology
| Technology / Tool | Cancer Type | Primary Function | Performance Metrics | Key Experimental Findings |
|---|---|---|---|---|
| Mindpeak HER2 AI Assist [26] | Breast Cancer | HER2-low/ultralow scoring on IHC slides | Diagnostic agreement: 86.4% (vs. 73.5% without AI) [26] | Misclassification of HER2-null cases decreased by 65% in a 6-center study. [26] |
| CAPAI Biomarker [26] | Stage III Colon Cancer | Risk stratification from H&E slides | 3-year recurrence: 35% (High-risk) vs. 9% (Low-risk) [26] | Identified high-risk ctDNA-negative patients for intensified monitoring. [26] |
| Stanford Spatial AI Model [26] | Non-Small Cell Lung Cancer (NSCLC) | Predicts immunotherapy outcome | Hazard Ratio (PFS): 5.46 [26] | Outperformed PD-L1 scoring alone (HR=1.67) by analyzing tumor microenvironment interactions. [26] |
| Artera Multimodal AI (MMAI) [26] | Prostate Cancer | Predicts metastasis post-prostatectomy | 10-year metastasis risk: 18% (High-risk) vs. 3% (Low-risk) [26] | Combined H&E image features with clinical variables (age, PSA, Gleason grade). [26] |
| MIA:BLC-FGFR Algorithm [26] | Bladder Cancer | Predicts FGFR status from H&E slides | AUC: 80-86% [26] | Offers a rapid, tissue-efficient alternative to molecular testing for trial enrollment. [26] |
| Digital PATH Project Tools [27] | Breast Cancer | Quantify HER2 expression | High agreement with experts for strong expression; greater variability in low/HER2-low cases. [27] | Analysis of 1,100 samples highlighted the need for standardized validation in low-expression ranges. [27] |
| Prov-GigaPath, Owkin Models [28] | Various Cancers | Foundation models for cancer detection & biomarker discovery | Outperforms human experts in specific tasks (e.g., mammogram interpretation). [28] | DeepHRD tool detects HRD characteristics with 3x more accuracy than some genomic tests. [28] |
Key Performance Insights from Comparative Data
The comparative data reveals several critical trends. First, AI tools consistently enhance diagnostic precision and agreement among pathologists, particularly in challenging, subjective tasks like scoring HER2-low breast cancer [26]. Second, AI models extracting spatial and morphological features from standard H&E slides demonstrate powerful prognostic value, stratifying patient risk beyond traditional biomarkers like ctDNA or PD-L1 [26]. Finally, the ability of AI to predict molecular alterations (e.g., FGFR status) from routine histology presents a paradigm shift, potentially making advanced genomic profiling more accessible and cost-effective [26].
Experimental Protocols for AI Tool Validation
The rigorous validation of AI tools is paramount for their acceptance in clinical research. The following section details the methodologies underpinning key experiments cited in this review, providing a framework for evaluating new technologies.
Protocol 1: Validation of AI for Biomarker Scoring (HER2)
This protocol is based on the international multi-center study that validated the Mindpeak AI tool for HER2 scoring [26].
- Objective: To evaluate the accuracy and concordance of pathologists, with and without AI assistance, in digitally scoring HER2 IHC levels, including the challenging HER2-low and ultralow categories.
- Sample Preparation:
- Tissue Source: Archived breast cancer tumor samples.
- Staining: Serial sections are stained with Hematoxylin and Eosin (H&E) and anti-HER2 IHC according to standard clinical laboratory protocols.
- Digitization: All stained slides are scanned using a high-throughput whole-slide scanner to create digital whole-slide images (WSIs).
- AI Analysis:
- The AI algorithm is trained on a large dataset of HER2-labeled WSIs.
- For the validation study, the AI processes the IHC WSIs to generate an initial HER2 score (0, 1+, 2+, 3+).
- Pathologist Assessment:
- A cohort of pathologists from multiple international academic centers independently scores the same set of WSIs.
- The same pathologists then re-score the WSIs with the assistance of the AI's output.
- Outcome Measures:
- Diagnostic Agreement: The inter-observer agreement rate among pathologists with and without AI assistance.
- Misclassification Rate: The rate of incorrect classification, particularly for HER2-null cases that should not receive targeted therapy.
Protocol 2: Development of a Spatial Biomarker for Immunotherapy
This protocol outlines the methodology used by Stanford researchers to develop an AI model for predicting outcomes of immune checkpoint inhibitor therapy in NSCLC [26].
- Objective: To identify and quantify features within the tumor microenvironment (TME) on H&E slides that predict progression-free survival (PFS) in patients treated with immunotherapy.
- Sample Preparation:
- Tissue Source: H&E-stained biopsy slides from NSCLC patients before treatment with immunotherapy.
- Digitization: Slides are scanned to create WSIs.
- AI Training & Feature Extraction:
- The AI model, based on a deep learning architecture, is trained to identify and segment different cell types (tumor cells, fibroblasts, T-cells, neutrophils) and tissue structures.
- The model analyzes the spatial relationships and interactions between these components (e.g., proximity of T-cells to tumor cells).
- A model comprising five key spatial features is constructed.
- Data Integration & Statistical Analysis:
- The AI-generated spatial biomarker score is correlated with clinical outcome data (PFS).
- The predictive power of the AI model is compared against standard-of-care biomarkers like PD-L1 tumor proportion score using hazard ratios from survival analysis.
Table 2: Essential Research Reagent Solutions for AI-Enhanced Bio-Optical Analysis
| Reagent / Material | Primary Function in Workflow | Specific Application Example |
|---|---|---|
| H&E Staining Kits | Provides standard morphological context on tissue sections. | Basis for all diagnostic and AI-based risk stratification models (e.g., CAPAI, Stanford spatial model). [26] |
| IHC Assays & Antibodies | Enables visualization of specific protein biomarkers (e.g., HER2, PD-L1). | Gold standard for validating AI-predicted protein expression levels. [26] |
| Bioluminescent/Fluorescent Reporters | Allows non-invasive, real-time tracking of biological processes in vivo. | Used in preclinical optical imaging for studying drug efficacy and disease progression in animal models. [29] |
| Next-Generation Sequencing (NGS) Kits | Provides genomic ground truth data (e.g., mutations, HRD status). | Used to validate AI models that predict genomic alterations from histology images (e.g., DeepHRD, MIA:BLC-FGFR). [28] [26] |
| Digital Whole-Slide Scanners | Converts physical glass slides into high-resolution digital images for AI analysis. | Foundational hardware for all digital pathology workflows; critical for image quality and subsequent AI accuracy. [27] |
Visualizing AI Workflows in Cancer Diagnostics
The integration of AI into bio-optical analysis follows structured workflows. The diagram below illustrates a generalized pipeline for developing and validating an AI model for cancer diagnosis and prognosis.
Foundation models are becoming a core architectural component in modern AI systems for digital pathology. The diagram below details how these pre-trained models are fine-tuned for specific diagnostic tasks.
Future Directions and Challenges
Despite the promising advances, the clinical validation and deployment of AI-powered bio-optical diagnostics face several hurdles. A significant challenge is the "black box" nature of some complex AI models, where the reasoning behind a decision is not transparent, raising concerns for clinical adoption [24]. Ensuring data privacy, navigating regulatory frameworks for software as a medical device, and guaranteeing generalizability across diverse patient populations and imaging equipment are active areas of focus [27] [23] [24]. Furthermore, the initial high cost of advanced imaging systems and a shortage of skilled personnel for operation and data analysis can limit uptake, particularly in smaller institutions and emerging markets [29].
Future development will likely focus on multimodal AI that seamlessly integrates histology, genomics, and clinical data for a holistic patient profile [24] [26]. The use of federated learning—training algorithms across multiple institutions without sharing patient data—is a promising approach to overcome data privacy and scarcity issues [23]. Finally, the push for standardized regulatory science, as exemplified by the Friends of Cancer Research Digital PATH Project, is critical for establishing benchmarks and ensuring that these powerful tools are validated with the same rigor as traditional diagnostics [27]. As these technologies mature, they hold the undeniable potential to make cancer diagnostics more precise, accessible, and profoundly impactful on patient outcomes.
Building a Validated Assay: Methodologies and Integrated Applications in Clinical Workflows
The clinical validation of bio-optical cancer diagnostics represents a complex multidisciplinary challenge, requiring a structured approach to ensure analytical robustness and clinical relevance. Strategic validation frameworks provide the necessary scaffolding to navigate this complexity, integrating analytical measurements, orthogonal verification methods, and rigorous clinical utility assessment. Within oncology research and drug development, these frameworks enable researchers and scientists to transform innovative diagnostic concepts into clinically validated tools that can reliably inform patient management decisions. The convergence of advanced optical technologies with artificial intelligence has further accelerated the need for sophisticated validation strategies that can keep pace with diagnostic innovation while meeting regulatory standards.
The fundamental purpose of validation in this context is to assure the safety and efficacy of medicinal products and diagnostic tools in clinical settings [30]. This process hinges on the comprehensive evaluation of Critical Quality Attributes (CQAs)—properties of a biotherapeutic or diagnostic sample that indicate its general stability and quality, which may be connected to product efficacy [30]. For bio-optical cancer diagnostics, these attributes typically include analytical sensitivity, specificity, reproducibility, and clinical performance metrics that must be thoroughly characterized throughout development and manufacturing. The strategic frameworks guiding this characterization employ a hierarchical approach that moves from basic analytical validation through orthogonal verification and ultimately to assessment of clinical utility, creating a robust chain of evidence that supports diagnostic adoption.
Comparative Framework for Strategic Validation
Analytical Validation Frameworks
Analytical validation establishes that a diagnostic test reliably measures what it claims to measure, forming the foundational layer of the validation pyramid. For bio-optical cancer diagnostics, this involves demonstrating performance characteristics such as accuracy, precision, sensitivity, specificity, and reproducibility under controlled conditions. The Balanced Scorecard (BSC) framework offers a structured approach to analytical validation by balancing multiple perspectives—including internal process quality, learning and growth in methodological refinements, and stakeholder requirements—through cause-and-effect logic that connects improvement goals with performance indicators and action plans [31]. This framework ensures that analytical validation activities remain aligned with broader strategic objectives rather than occurring in isolation.
The Objectives and Key Results (OKR) framework provides a more agile complement to BSC for managing analytical validation, particularly useful for focusing teams on specific, inspirational goals with quarterly review cycles that maintain momentum in development projects [31]. For the highly structured environment of diagnostic validation, the Hoshin Kanri framework emphasizes continuous improvement through its Plan-Do-Check-Act cycle and promotes strategic alignment through "Catchball" discussions that ensure all team members understand and contribute to validation objectives [31]. When selecting an analytical validation framework, researchers must consider factors such as the diagnostic's development stage, organizational structure, and regulatory requirements, as each framework offers distinct advantages for different contexts.
Table 1: Comparison of Strategic Frameworks for Analytical Validation
| Framework | Primary Focus | Key Components | Application in Bio-Optical Diagnostics | Advantages |
|---|---|---|---|---|
| Balanced Scorecard (BSC) | Strategy execution with balanced perspective | Strategy maps, four perspectives (internal, learning & growth, customer, stakeholders), cause-effect logic, leading/lagging indicators | Connects analytical performance goals with clinical outcomes through measurable indicators | Comprehensive strategic alignment, strong cause-effect documentation |
| OKR | Agile goal setting for specific challenges | Objectives (inspirational goals), Key Results (measurable outcomes), quarterly cycles | Rapid iteration on specific analytical parameters during development | Lightweight, adaptable, promotes focus and alignment on critical goals |
| Hoshin Kanri | Strategy deployment through continuous improvement | Plan-Do-Check-Act cycle, Catchball process, X-matrix for strategic priorities | Systematic approach to improving analytical methods and processes | Emphasizes learning and adaptation, strong alignment through discussion |
| OGSM Model | Strategic planning with one-page overview | Objectives, Goals, Strategies, Measures structured document | Clear documentation of analytical validation strategy and progress | Simplicity and clarity, easy communication across teams |
| Results-Based Management | Cause-effect logic for outcome achievement | Inputs, Activities, Outputs, Outcomes, Impact hierarchy with quantification | Tracking analytical validation activities through to clinical impact | Strong focus on measurable outcomes and impact demonstration |
Orthogonal Verification Frameworks
Orthogonal verification represents a critical strategic layer in diagnostic validation, employing methodologies based on different physicochemical or biological principles to assess the same attributes, thereby providing independent data to support quality assessments [30]. The fundamental principle of orthogonality in analytical science acknowledges that each measurement technique introduces specific biases or systematic errors due to its operating principles, making confirmation through independent methods essential for robust validation [32] [30]. For bio-optical cancer diagnostics, this typically involves employing multiple measurement techniques that probe the same critical quality attributes through different physical mechanisms, such as combining label-free optical methods with fluorescence-based detection or correlating optical measurements with non-optical techniques like mass spectrometry.
The strategic implementation of orthogonal methods follows a structured framework that begins with identifying Critical Quality Attributes (CQAs) most relevant to clinical performance, then selecting appropriate orthogonal technique pairs that measure the same CQAs through different principles [30]. For example, in assessing subvisible particles in diagnostic reagents—a key quality attribute—researchers might employ both Flow Imaging Microscopy (FIM) and Light Obscuration (LO), as both measure particle count and size but use digital imaging versus light blocking principles respectively [30]. This orthogonal approach is particularly valuable when the primary technique is qualitative or when the CQA is dynamic and cannot be completely mapped by a single method [32]. The regulatory emphasis on orthogonal approaches reflects their importance in providing unambiguous demonstration of biosimilarity in pharmaceutical development, a principle that extends directly to bio-optical diagnostics validation [32].
Table 2: Orthogonal Technique Pairs for Bio-Optical Diagnostic Validation
| Critical Quality Attribute | Primary Optical Method | Orthogonal Verification Method | Measurement Principle Difference | Application Context |
|---|---|---|---|---|
| Particle Concentration & Size | Flow Imaging Microscopy (FIM) | Light Obscuration (LO) | Digital imaging vs. light blocking | Subvisible particle analysis in diagnostic reagents [30] |
| Protein Aggregation | Dynamic Light Scattering (DLS) | Analytical Ultracentrifugation (AUC) | Brownian motion vs. sedimentation velocity | Stability of protein-based recognition elements [32] |
| Nanoparticle Morphology | Scanning Electron Microscopy (SEM) | Atomic Force Microscopy (AFM) | Electron interaction vs. physical probing | Characterization of optical contrast agents [33] |
| Molecular Structure | Circular Dichroism (CD) | Nuclear Magnetic Resonance (NMR) | Optical activity vs. magnetic properties | Confirmation of biorecognition element structure |
| Surface Properties | Surface Plasmon Resonance (SPR) | X-ray Photoelectron Spectroscopy (XPS) | Refractive index changes vs. electron emission | Functionalization of optical biosensors |
Clinical Utility Assessment Frameworks
Clinical utility assessment forms the capstone of the validation pyramid, evaluating whether a diagnostic test provides information that leads to improved patient outcomes, better survival rates, or more efficient healthcare delivery. For bio-optical cancer diagnostics, this involves generating evidence that the diagnostic meaningfully impacts clinical decision-making, treatment selection, or patient management in real-world settings. The McKinsey Three Horizons framework offers a strategic approach to planning and validating clinical utility by categorizing innovation according to three time frames: current core applications (now), emerging applications in the comfort zone (near-term future), and potentially disruptive future applications (future) [31]. This framework helps diagnostic developers allocate appropriate validation resources across their development pipeline while maintaining focus on both immediate and long-term clinical utility.
Artificial intelligence integration in bio-optical cancer diagnostics has expanded the scope of clinical utility assessment, requiring frameworks that can validate both the optical technology and the algorithmic components. Recent advances in deep learning have demonstrated remarkable potential in addressing previously insurmountable challenges in cancer detection and diagnosis [34]. For instance, convolutional neural networks (CNNs) applied to optical imaging data have shown performance comparable or superior to human experts in tasks such as tumor detection, segmentation, and grading [34]. The validation of these AI-enhanced diagnostics requires specialized frameworks that assess not only traditional clinical performance metrics but also algorithmic robustness, generalizability across diverse populations, and integration into clinical workflows.
Table 3: Clinical Performance of AI-Enhanced Bio-Optical Cancer Diagnostics
| Cancer Type | Optical Modality | AI System | Dataset Size | Sensitivity | Specificity | AUC | Evidence Level |
|---|---|---|---|---|---|---|---|
| Colorectal Cancer | Colonoscopy | CRCNet | 464,105 images from 12,179 patients (training) | 91.3% (AI) vs. 83.8% (human) | 85.3% (AI) | 0.882 (95% CI: 0.828-0.931) | Retrospective multicohort diagnostic study with external validation [34] |
| Breast Cancer | 2D Mammography | Ensemble of three DL models | 25,856 women (UK) 3,097 women (US) | +2.7% vs. first reader (UK) +9.4% vs. radiologists (US) | +1.2% vs. first reader (UK) +5.7% vs. radiologists (US) | 0.889 (UK) 0.8107 (US) | Diagnostic case-control study with comparison to radiologists [34] |
| Colorectal Cancer | Colonoscopy/Histopathology | Real-time image recognition system | 118 lesions from 41 patients | 95.9% (neoplastic lesion detection) | 93.3% (nonneoplastic identification) | Not Reported | Prospective diagnostic accuracy study with blinded gold standard [34] |
Experimental Protocols for Validation Studies
Protocol for Analytical Validation of Bio-Optical Assays
A robust analytical validation protocol for bio-optical cancer diagnostics must systematically address multiple performance characteristics using standardized methodologies. The following protocol outlines a comprehensive approach:
Accuracy Assessment: Compare diagnostic results from the bio-optical assay against a gold standard reference method using clinically characterized specimens spanning the assay's intended use population. Calculate percent agreement, sensitivity, specificity, and overall accuracy with 95% confidence intervals. For quantitative assays, use linear regression and Bland-Altman analysis to assess systematic and proportional bias.
Precision Evaluation: Conduct within-run, between-run, and between-operator precision studies following Clinical and Laboratory Standards Institute (CLSI) EP05-A3 guidelines. Test at least two levels of controls (normal and pathological ranges) with 20 replicates per level for within-run precision, and duplicate measurements over 10 days for between-run precision. Calculate coefficients of variation (CV) with acceptance criteria typically <15% for biomarker assays.
Linearity and Reportable Range: Prepare a series of samples with analyte concentrations spanning the claimed measuring range, typically through serial dilution of high-concentration samples. Test each dilution in triplicate and plot observed versus expected values. Establish the reportable range as the interval over which linearity, precision, and accuracy claims are met.
Limit of Detection (LOD) and Limit of Quantitation (LOQ): Determine LOD using at least 20 replicates of blank (analyte-free) samples and low-concentration samples near the expected detection limit. Calculate LOD as mean blank value + 3 standard deviations. Establish LOQ as the lowest concentration that can be measured with ≤20% CV while maintaining stated accuracy requirements.
Interference and Cross-Reactivity Testing: Evaluate potential interferents including hemoglobin, lipids, bilirubin, common medications, and structurally similar compounds that might cross-react. Spike interferents at clinically relevant concentrations and assess recovery against non-spiked controls.
Protocol for Orthogonal Verification Studies
Orthogonal verification requires careful experimental design to ensure methods truly provide independent assessment of the same attributes:
Orthogonal Technique Selection: Identify technique pairs that measure the same Critical Quality Attributes (CQAs) but employ fundamentally different measurement principles [30]. For example, combine flow imaging microscopy (measurement principle: digital imaging of particles) with light obscuration (measurement principle: light blocking by particles) for subvisible particle analysis [30].
Sample Preparation for Orthogonal Analysis: Use identical sample aliquots for both primary and orthogonal methods to eliminate preparation variability. Ensure sample stability throughout the testing window and document handling conditions.
Comparative Testing Protocol: Analyze a minimum of 3-5 lots of samples representing expected variation in manufacturing or clinical use. For each lot, perform triplicate measurements using both primary and orthogonal methods in randomized order to avoid sequence effects.
Data Correlation Analysis: Assess agreement between methods using appropriate statistical approaches based on data type. For continuous data, use Pearson or Spearman correlation, Deming regression, and concordance correlation coefficients. For categorical data, calculate percent agreement and Cohen's kappa.
Bias Assessment and Resolution: Systematically identify and document discrepancies between orthogonal methods. Investigate technical reasons for discrepancies related to methodological biases, such as differential sensitivity to particle translucency in particle counting methods [30]. Establish acceptance criteria for orthogonal agreement prior to testing.
Protocol for Clinical Utility Assessment
Clinical utility assessment requires multidimensional evaluation of real-world performance and impact:
Diagnostic Performance Study: Conduct a prospective, blinded validation study comparing the bio-optical diagnostic against the clinical reference standard in the intended use population. Pre-specify primary endpoints (sensitivity, specificity, AUC), secondary endpoints (PPV, NPV, likelihood ratios), and statistical power calculations. Include diverse patient subgroups to assess generalizability.
Clinical Impact Assessment: Design studies evaluating how diagnostic results influence clinical decision-making, such as treatment selection, additional testing, or referral patterns. Use methods including surveys, interviews, and observation of clinical workflows before and after diagnostic implementation.
Health Outcomes Analysis: For diagnostics claiming improved patient outcomes, collect data on relevant endpoints such as time to diagnosis, treatment response rates, progression-free survival, or overall survival. Adjust for potential confounders using multivariate statistical methods.
Economic Evaluation: Perform cost-effectiveness analysis comparing the bio-optical diagnostic against current standard of care. Include direct medical costs, indirect costs, and quality-adjusted life years (QALYs) where appropriate. Conduct sensitivity analyses to assess robustness of conclusions to parameter uncertainty.
Visualization of Strategic Validation Workflows
Integrated Validation Strategy Diagram
Validation Strategy Workflow: This diagram illustrates the integrated sequential approach to bio-optical diagnostic validation, moving from analytical validation through orthogonal verification to clinical utility assessment.
Orthogonal Method Selection Algorithm
Orthogonal Method Selection: This decision algorithm outlines the process for selecting appropriate orthogonal methods based on measurement principles, dynamic ranges, and validation status.
Research Reagent Solutions for Validation Studies
The successful implementation of strategic validation frameworks requires specific research reagents and materials carefully selected for their intended functions in analytical, orthogonal, and clinical utility assessment.
Table 4: Essential Research Reagents for Bio-Optical Diagnostic Validation
| Reagent/Material | Function in Validation | Specific Application Examples | Quality Requirements |
|---|---|---|---|
| Characterized Reference Materials | Serve as gold standard for accuracy assessment and calibration | Certified tumor markers, cell line derivatives with known mutation status | Traceable to international standards, certificate of analysis with documented uncertainty |
| Multiplex Quality Controls | Monitor assay precision across multiple analytes and concentrations | Commercial serum/plasma controls with predetermined values for oncology biomarkers | Defined acceptability ranges, stability documentation, commutable with patient samples |
| Interference Testing Panels | Evaluate assay susceptibility to common interferents | Hemolyzed, icteric, and lipemic samples; common medication panels | Clinically relevant interference concentrations, standardized preparation protocols |
| Stability Testing Materials | Assess reagent and sample stability under various conditions | Temperature-controlled storage systems, light exposure chambers | Environmental monitoring capability, standardized challenge conditions |
| Orthogonal Method Kits | Provide independent measurement of same analytes | ELISA kits for protein biomarkers when primary method is optical immunoassay | Different methodological principle, validated performance characteristics |
| Clinical Sample Panels | Validate diagnostic performance in intended use population | Well-characterized specimens with reference method results and clinical outcomes | IRB-approved collection protocols, comprehensive clinical annotation, appropriate storage conditions |
Strategic validation frameworks provide an essential structured approach for establishing the analytical robustness and clinical utility of bio-optical cancer diagnostics. By integrating analytical validation, orthogonal verification, and clinical utility assessment within a cohesive strategy, researchers and drug development professionals can systematically address the complex challenges of diagnostic validation while meeting regulatory standards. The comparative framework analysis presented in this guide demonstrates that no single approach fits all scenarios—rather, the selection of specific frameworks must align with the diagnostic's development stage, technological complexity, and intended clinical application.
The accelerating integration of artificial intelligence with bio-optical technologies necessitates continued evolution of these validation frameworks, particularly in addressing novel challenges related to algorithmic validation and clinical generalizability. Furthermore, the established principle of orthogonality from biotherapeutic development offers valuable guidance for bio-optical diagnostics, emphasizing the importance of independent methodological verification to overcome technique-specific biases and limitations. As the field advances, these strategic frameworks will play an increasingly critical role in translating technological innovations into clinically validated tools that reliably improve cancer patient outcomes.
Integrated multi-omic approaches represent a paradigm shift in biomedical research, moving beyond single-layer molecular analysis to a comprehensive systems biology perspective. By combining DNA sequencing (genomics), RNA sequencing (transcriptomics), and various forms of optical imaging, researchers can now capture complementary information across multiple biological layers—from genetic blueprint to functional activity and spatial organization [35] [36]. This integration is particularly transformative in oncology, where complex molecular interactions and tissue-level manifestations must be correlated to understand disease mechanisms, identify biomarkers, and develop targeted therapies [37] [36].
The clinical validation of bio-optical cancer diagnostics depends on this multi-modal approach, as it enables researchers to trace the flow of biological information from DNA variations through RNA expression to protein function and metabolic activity, while simultaneously capturing structural and compositional changes through imaging [38] [39]. This guide objectively compares the performance, requirements, and applications of different integration methodologies, providing researchers with experimental protocols and analytical frameworks for implementing these powerful approaches in cancer research.
Multi-Omic Integration Methodologies: A Comparative Analysis
Conceptual Frameworks for Data Integration
Multi-omics data integration strategies can be categorized into distinct conceptual frameworks, each with specific strengths, limitations, and optimal use cases. The table below compares the primary integration approaches used in contemporary research.
Table 1: Comparison of Multi-Omics Data Integration Approaches
| Integration Type | Description | Advantages | Limitations | Best Applications |
|---|---|---|---|---|
| Horizontal Integration | Combining multiple datasets of the same omics type from different batches or sources [38] | Standardizes data across platforms; reduces batch effects | Limited to single omics layer; cannot capture cross-omics interactions | Merging genomic datasets from multiple sequencing centers; cross-study transcriptomic comparisons |
| Vertical Integration | Combining diverse omics datasets (genomics, transcriptomics, proteomics) from the same samples [38] | Captures complementary biological information; enables systems-level analysis | Complex statistical integration; requires careful normalization | Identifying biomarkers across molecular layers; mapping information flow from DNA to RNA to protein |
| Concatenation-Based | Early integration by merging features from different omics into a single matrix [40] [37] | Simple implementation; preserves all feature relationships | Creates high-dimensional data; requires strong normalization; sensitive to outliers | Small datasets with similar feature scales; when computational resources are limited |
| Transformation-Based | Converting each omics dataset into a simplified representation before integration [40] [37] | Reduces dimensionality; handles different data types effectively | May lose biologically relevant variance; complex interpretation | Large-scale multi-omics studies; integration of disparate data types (e.g., sequences and images) |
| Model-Based | Using statistical models to integrate omics layers while preserving their structures [40] | Accounts for data structure; robust to noise | Computationally intensive; complex implementation | Studies with clear biological priors; causal inference analysis |
| Graph-Based | Representing multi-omics data as networks with nodes and edges [37] | Captures complex relationships; incorporates biological prior knowledge | Requires specialized expertise; computationally intensive | Mapping molecular interactions; identifying network perturbations in disease |
Performance Benchmarking of Integration Methods
Recent comprehensive evaluations have assessed various integration methods for key performance metrics in cancer subtyping and biomarker discovery. The benchmarking results provide critical guidance for method selection based on research objectives.
Table 2: Performance Benchmarking of Multi-Omics Integration Methods for Cancer Subtyping
| Method | Category | Clustering Accuracy | Clinical Significance | Robustness | Computational Efficiency | Recommended Omics Combinations |
|---|---|---|---|---|---|---|
| Similarity Network Fusion (SNF) | Network-based | High | High | Medium | Medium | mRNA + miRNA + DNA methylation |
| iClusterBayes | Statistics-based | High | High | High | Low | mRNA + DNA methylation + copy number variation |
| MOFA+ | Transformation-based | Medium-High | Medium-High | High | Medium | Any combination with >2 omics types |
| LRAcluster | Statistics-based | Medium | Medium | Medium | High | mRNA + miRNA |
| Pattern Fusion Analysis (PFA) | Network-based | Medium-High | Medium | Medium | Medium | mRNA + protein expression |
| Subtype-GAN | Deep Learning | High | Medium | Low | Low | All major omics types combined |
Key Insights from Performance Evaluation: Contrary to intuitive expectations, incorporating more omics data types does not always improve performance. Some integration methods perform better with specific combinations—for example, mRNA expression with DNA methylation data often yields more clinically relevant cancer subtypes than simply adding more data types [40]. The optimal combination depends on both the biological context and the specific integration method employed.
Experimental Protocols for Multi-Omic Profiling
The Quartet Project Protocol for Multi-Omic Reference Materials
The Quartet Project provides a robust framework for quality control and data integration in multi-omics studies, using reference materials from immortalized cell lines of a family quartet (parents and monozygotic twin daughters) [38].
Protocol Overview:
Reference Material Preparation: Simultaneous establishment of DNA, RNA, protein, and metabolite reference materials from the same B-lymphoblastoid cell lines, with large batch production (>1,000 vials each) to ensure consistency [38].
Cross-Platform Profiling: Analysis of reference materials across multiple technology platforms:
- 7 DNA sequencing platforms
- 1 DNA methylation platform
- 2 RNA-seq platforms
- 2 miRNA-seq platforms
- 9 LC-MS/MS-based proteomics platforms
- 5 LC-MS/MS-based metabolomics platforms [38]
Ratio-Based Profiling Implementation:
- Scale absolute feature values of study samples relative to a concurrently measured common reference sample
- Calculate ratios on a feature-by-feature basis (e.g., D5/D6, F7/D6, M8/D6)
- Apply these ratios to eliminate systematic biases across batches and platforms [38]
Quality Control Metrics:
- Horizontal Integration QC: Mendelian concordance rate for genomic variants; signal-to-noise ratio for quantitative omics
- Vertical Integration QC: Sample classification accuracy (4 individuals; 3 genetic clusters); central dogma consistency (DNA→RNA→protein) [38]
Integrated Optical and Sequencing Analysis Protocol
This protocol details the methodology for correlating optical imaging data with DNA and RNA sequencing information, enabling spatial contextualization of molecular profiles.
Experimental Workflow:
Sample Preparation and Multi-Modal Data Collection:
Optical Imaging Acquisition:
- Structural Imaging: Implement Optical Coherence Tomography (OCT) for tissue architecture
- Molecular Imaging: Apply hyperspectral imaging, spectroscopic OCT, or scattering-based light sheet microscopy [41] [42] [39]
- Cellular Resolution: Utilize confocal or light sheet microscopy with automated image analysis algorithms [42] [39]
Data Processing and Alignment:
- Sequencing Data: Standard processing, quality control, and feature quantification
- Imaging Data: Process using automated image analysis algorithms; extract quantitative features (texture, morphology, intensity)
- Spatial Alignment: Register imaging and sequencing data using reference landmarks or computational alignment methods [37]
Integrated Analysis:
- Correlation Analysis: Identify associations between genetic variants and imaging phenotypes
- Network Construction: Build molecular-interaction networks incorporating imaging features
- Graph Machine Learning: Implement graph neural networks to model complex relationships across data types [37]
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of integrated multi-omic approaches requires specific reagents, reference materials, and computational tools. The following table details essential components for these studies.
Table 3: Research Reagent Solutions for Multi-Omic Studies
| Category | Specific Product/Resource | Application | Key Features | Validation Requirements |
|---|---|---|---|---|
| Reference Materials | Quartet Project Reference Materials (DNA, RNA, protein, metabolites) [38] | Quality control across multi-omics platforms | Built-in truth from pedigree relationships; approved as National Reference Materials | Mendelian consistency; signal-to-noise ratio; central dogma compliance |
| DNA Sequencing | Whole genome sequencing platforms (Illumina, PacBio, Oxford Nanopore) [35] | Comprehensive genomic variant detection | Short-read and long-read technologies; structural variant identification | Concordance with benchmark variants; sensitivity/specificity metrics |
| RNA Sequencing | RNA-Seq platforms; single-cell RNA-Seq solutions [36] | Transcriptome quantification; alternative splicing; novel isoform detection | Strand-specific; broad dynamic range; low input requirements | Correlation with qPCR; detection of known isoforms |
| Optical Imaging | Spectroscopic OCT systems; light sheet microscopes; hyperspectral imaging [41] [42] [39] | Tissue structure visualization; molecular contrast; cellular resolution | Cellular-level resolution; molecular specificity; real-time capability | Resolution targets; correlation with histology; reproducibility |
| Data Integration Tools | Graph neural networks (PyTorch Geometric, Deep Graph Library) [37] | Multi-omics network analysis; relationship modeling | Heterogeneous graph support; message-passing architectures | Benchmarking on reference datasets; biological plausibility of networks |
| Analysis Platforms | Multi-omics integration software (SNF, iClusterBayes, MOFA+) [40] | Joint analysis of multiple omics datasets | Specific integration strategies; visualization capabilities | Reproduction of known biological relationships; clinical relevance |
Clinical Applications in Cancer Diagnostics
Cancer Subtyping and Classification
Multi-omics approaches have demonstrated superior performance in identifying molecularly distinct cancer subtypes compared to single-omics approaches. In comprehensive evaluations across nine cancer types, integrated analysis of genomics, epigenomics, transcriptomics, and proteomics data revealed subtypes with significant differences in clinical outcomes, including overall survival and treatment response [40]. These molecular subtypes often transcend traditional histopathological classifications, providing insights into underlying biological mechanisms and potential therapeutic vulnerabilities.
The combination of DNA sequencing with optical imaging has been particularly valuable in connecting genetic alterations with their morphological consequences. For example, in colorectal cancer, specific mutational profiles have been correlated with distinct glandular structures and tumor microenvironment features visible through advanced imaging [37] [36]. These correlations enable more precise classification and potentially guide treatment selection.
Early Detection and Diagnostic Imaging
Novel optical imaging technologies are enhancing early cancer detection by revealing subcellular changes that precede macroscopic tumor formation. Light sheet microscopy techniques, for instance, can identify precancerous lesions in epithelial tissues with cellular-level resolution, enabling non-invasive screening for anal, cervical, and oral cancers [42]. When these imaging biomarkers are correlated with DNA methylation markers or transcriptomic signatures detected in liquid biopsies, they create powerful composite biomarkers for early detection.
Advanced optical methods like spectroscopic OCT extract additional functional information from tissue by analyzing wavelength-dependent scattering properties. These scattering patterns can distinguish subtle changes in tissue microstructure and composition, providing a "digital staining" approach that complements molecular profiling [41]. The integration of these optical biomarkers with genomic and transcriptomic data creates multi-dimensional diagnostic models with improved sensitivity and specificity.
AI-Enhanced Integration for Clinical Decision-Making
Recent advances in artificial intelligence are enabling more sophisticated integration of multi-omics data for clinical applications. Autonomous AI agents equipped with specialized tools for genomic analysis, image interpretation, and literature mining have demonstrated remarkable accuracy in complex clinical decision-making tasks [43]. In one validation study, an AI agent integrating GPT-4 with vision transformers for histopathology analysis and specialized oncology databases reached correct clinical conclusions in 91.0% of cases, significantly outperforming the base language model alone (30.3% accuracy) [43].
These systems exemplify the power of tool-enhanced integration, where each data type is processed by specialized analytical modules before being synthesized into a comprehensive clinical assessment. The AI agent successfully chained multiple tool calls—for example, using MedSAM for tumor segmentation on imaging data, calculating progression metrics, querying knowledge bases for mutation significance, and retrieving relevant literature—to formulate personalized treatment recommendations [43]. This approach mirrors the interdisciplinary collaboration required for effective multi-omics research in clinical oncology.
Analytical Framework for Multi-Omic Data Integration
Graph Machine Learning for Multi-Omic Data
Graph-based approaches provide a powerful framework for representing and analyzing complex relationships in integrated multi-omics datasets. In this paradigm, different molecular entities (genes, proteins, metabolites) are represented as nodes, while their relationships (interactions, correlations) are represented as edges [37]. This network representation naturally accommodates diverse data types and incorporates prior biological knowledge from existing databases.
Implementation Workflow:
Graph Construction:
- Create nodes for each molecular feature across omics layers
- Establish edges based on known interactions (e.g., protein-protein interactions) or statistical correlations
- Incorporate imaging features as specialized nodes with connections to relevant molecular entities
Graph Neural Network Processing:
- Implement message-passing algorithms to propagate information across the network
- Learn node embeddings that capture both features and network context
- Apply attention mechanisms to weight the importance of different relationships [37]
Downstream Applications:
- Node classification for biomarker identification
- Graph classification for patient stratification
- Link prediction for discovering novel relationships
Quantitative Performance Metrics
Rigorous quality assessment is essential for validating integrated multi-omics approaches. The Quartet Project has established specific metrics for this purpose [38]:
Horizontal Integration Metrics:
- Mendelian Concordance Rate: Proportion of genetic variants consistent with Mendelian inheritance patterns in family-based designs
- Signal-to-Noise Ratio (SNR): Ratio of biological signal strength to technical variability in quantitative omics data
Vertical Integration Metrics:
- Sample Classification Accuracy: Ability to correctly cluster samples based on known biological relationships (e.g., genetic relatedness)
- Central Dogma Consistency: Strength of correlation between DNA variants, RNA expression, and protein abundance for the same genes
Clinical Relevance Metrics:
- Subtype Clinical Significance: Association of identified subtypes with clinical outcomes (survival, treatment response)
- Biomarker Reproducibility: Consistency of identified biomarkers across independent datasets and technological platforms
These metrics provide a comprehensive framework for evaluating the success of multi-omics integration, addressing both technical performance and biological validity.
The choice between fresh-frozen (FF) and formalin-fixed paraffin-embedded (FFPE) tissue preservation represents a critical crossroads in cancer diagnostics and research. These two methodologies offer distinct advantages and limitations that directly impact downstream analytical outcomes, particularly in the evolving field of bio-optical cancer diagnostics. As precision medicine advances, with the global biomarkers market projected to grow from $62.39 billion in 2025 to over $104.15 billion by the early 2030s, understanding these sample considerations becomes increasingly vital for researchers, scientists, and drug development professionals [44]. This guide provides a comprehensive, data-driven comparison of FF and FFPE tissues, framing their performance characteristics within the context of clinical validation for optical-based diagnostic technologies.
Fundamental Preservation Methodologies
The divergence between FF and FFPE tissues begins at the moment of sample collection, with each method employing fundamentally different physical and chemical principles to halt tissue degradation.
Fresh-Frozen Preservation relies on rapid thermal immobilization of biological activity. Tissues are typically snap-frozen in liquid nitrogen or cooled to -80°C in ultra-low freezers. This process essentially pauses cellular metabolism and halts enzymatic degradation, preserving biomolecules in their native state. The rapid cooling minimizes ice crystal formation that can damage cellular structures, particularly when optimized protocols are followed [45] [46]. The primary goal is to maintain molecular integrity for subsequent analyses.
FFPE Preservation utilizes a chemical fixation process followed by embedding in a solid matrix. Tissue samples are immersed in formalin (a formaldehyde solution), which creates covalent cross-links between proteins, effectively stabilizing tissue architecture and preventing decomposition. Following fixation, tissues undergo dehydration through alcohol gradients, are cleared with xylene, and are infiltrated with and embedded in paraffin wax to create stable blocks that can be sectioned for microscopic analysis [45] [47]. This method excels at preserving morphological details but introduces chemical modifications to biomolecules.
The following diagram illustrates the key decision points and technical considerations in selecting and processing biospecimens for cancer research:
Comparative Performance in Molecular Analyses
Biomolecular Integrity and Analytical Suitability
The preservation method profoundly influences the quantity, quality, and analytical suitability of biomolecules extracted from tissue specimens, with significant implications for research outcomes and diagnostic accuracy.
Nucleic Acid Preservation: Fresh-frozen tissues maintain DNA and RNA in a largely intact, undegraded state, making them the "gold standard" for sensitive molecular analyses. Nucleic acids from FF tissues exhibit minimal fragmentation and chemical modification, enabling successful applications in next-generation sequencing (NGS), whole-genome sequencing, and gene expression profiling [45]. In contrast, FFPE processing causes substantial nucleic acid fragmentation and introduces formalin-induced chemical modifications that can complicate molecular analyses. While DNA and RNA can be extracted from FFPE tissues, they often require specialized protocols and may yield lower-quality data with potential artifacts [45] [47].
Protein and Lipid Preservation: FF tissues preserve proteins in their native conformation, maintaining enzymatic activity and antigenicity crucial for proteomics studies, enzyme assays, and certain immunohistochemistry applications. Lipids are also generally well-preserved in frozen specimens [45]. FFPE tissues suffer from protein cross-linking due to formalin fixation, which can alter native protein conformation and lead to loss of enzymatic activity. While many antigens can still be detected through IHC after antigen retrieval techniques, some epitopes are irrevocably masked or denatured. Lipids are often dissolved or altered during the dehydration and paraffin embedding process [45].
Experimental Data: Whole-Genome Sequencing Performance
A 2025 study directly compared WGS outcomes from 50 matched pairs of cryopreserved (CP, a type of fresh-frozen) and FFPE tumor samples across multiple cancer types, providing robust quantitative data on molecular performance differences [48].
Presequencing Metrics: The study demonstrated significantly superior DNA quality from cryopreserved tissues across all measured parameters. CP tissues yielded seven times higher gDNA concentration (85.2 ng/µL vs. 12.5 ng/µL, p < 0.001) and substantially higher DNA Integrity Number (8.4 vs. 4.7, p < 0.001). After library preparation, CP tissues maintained higher DNA library concentrations (340.0 ng/µL vs. 137.8 ng/µL, p < 0.001) and larger fragment sizes (644.6 bp vs. 444.1 bp, p < 0.001) [48].
Sequencing Performance: The quality advantages of CP tissues translated directly into superior sequencing metrics. CP samples achieved higher mean read depth (54.2× vs. 34.6×, p < 0.001) and demonstrated better variant calling accuracy. Notably, FFPE samples exhibited higher tumor mutation burden (13.7 vs. 6.4 mutations/Mb) and lower concordance with CP in variant calls (43.5% overlap), suggesting that FFPE processing may introduce sequencing artifacts that inflate mutation calls. CP samples also detected more structural variants and enabled improved identification of oncogenic driver mutations [48].
Table 1: Comparative Performance in Whole-Genome Sequencing (50 Matched Pairs)
| Performance Metric | Cryopreserved Tissue | FFPE Tissue | P-value |
|---|---|---|---|
| gDNA Concentration (ng/µL) | 85.2 | 12.5 | <0.001 |
| DNA Integrity Number (DIN) | 8.4 | 4.7 | <0.001 |
| Library Concentration (ng/µL) | 340.0 | 137.8 | <0.001 |
| Library Fragment Size (bp) | 644.6 | 444.1 | <0.001 |
| Mean Read Depth | 54.2× | 34.6× | <0.001 |
| Tumor Mutation Burden (mutations/Mb) | 6.4 | 13.7 | Not reported |
| Variant Call Concordance | Reference | 43.5% overlap | Not applicable |
Morphological and Microenvironment Preservation
While FFPE tissues demonstrate limitations in molecular analyses, they excel in morphological preservation, providing exceptional cellular and tissue architecture details that remain the gold standard for pathological diagnosis [45]. The formalin fixation and paraffin embedding process preserves tissue morphology with exceptional clarity, allowing pathologists to identify subtle cellular features, tissue organization patterns, and disease characteristics under conventional microscopy [45] [49].
Frozen tissues can suffer from morphological artifacts due to ice crystal formation during the freezing process, making detailed histological examination more challenging compared to FFPE. However, advances in cryosectioning and staining techniques have improved the histological quality achievable with frozen sections [45].
For tumor microenvironment studies, FFPE tissues maintain architectural relationships between different cell types and tissue components, which is valuable for understanding spatial organization in cancer biology. Recent research has demonstrated that perfusion-based bioreactor systems can successfully culture both fresh and slow-frozen ovarian cancer tissues, maintaining not only cancer cell viability but also key microenvironment components including cancer-associated fibroblasts, endothelial cells, and immune cells [50].
Applications in Bio-Optical Cancer Diagnostics
Advanced Imaging and Super-Resolution Microscopy
The emergence of super-resolution microscopy (SRM) techniques has created new opportunities for extracting nanoscale information from archived FFPE tissues, bridging the gap between conventional microscopy and electron microscopy.
SRM Modalities for FFPE Tissues: Multiple SRM approaches have been successfully applied to FFPE specimens, including Structured Illumination Microscopy (SIM), Stimulated Emission Depletion (STED) microscopy, Single-Molecule Localization Microscopy (SMLM), and Fluorescence Fluctuation-based SRM [49]. These techniques overcome the diffraction limit of conventional light microscopy (approximately 250 nm), enabling visualization of subcellular structures that were previously only accessible through electron microscopy. This is particularly valuable for examining tight junctions, synapses, foot processes, microvilli brush-borders, and other ultrastructural features relevant to cancer diagnostics [49].
Implementation Considerations: SRM typically uses standard immunofluorescence staining protocols already common in pathology laboratories, reducing implementation barriers. The same SRM instrument can typically operate in conventional diffraction-limited mode for large field-of-view scanning and switch to super-resolution modality for regions of interest, streamlining clinical workflows [49]. While frozen tissues can also be used for SRM, the superior morphological preservation of FFPE specimens often makes them preferable for correlative studies linking nanoscale findings to established histopathological features.
Biomarker Discovery and Validation
Both FF and FFPE tissues play complementary roles in biomarker discovery, validation, and implementation, with their relative advantages aligning with different phases of the development pipeline.
Fresh-Frozen for Discovery: The high quality of biomolecules preserved in FF tissues makes them ideal for initial biomarker discovery phases, particularly for genomic, transcriptomic, and proteomic profiling. The integrity of nucleic acids from frozen tissues enables more comprehensive and accurate characterization of molecular alterations in cancer, supporting the identification of candidate biomarkers [45] [48]. Frozen tissues also permit functional studies, including cell culture and drug sensitivity testing, which are impossible with FFPE material [45].
FFPE for Validation and Translation: The extensive archives of FFPE tissues with associated clinical follow-up information make them invaluable for validating biomarkers across large patient cohorts. Researchers can quickly access samples with known outcomes to assess the clinical utility of candidate biomarkers [47]. The ability to conduct retrospective studies on well-annotated FFPE cohorts significantly accelerates biomarker validation and clinical translation. Furthermore, the stability of FFPE blocks at room temperature simplifies multi-center studies and regulatory submissions [45] [47].
Table 2: Application-Based Selection Guide for Tissue Preservation Methods
| Research Application | Recommended Method | Key Considerations |
|---|---|---|
| Whole Genome/Exome Sequencing | Fresh-Frozen | Superior DNA quality and variant calling accuracy [48] |
| RNA Sequencing & Transcriptomics | Fresh-Frozen | Preserved RNA integrity with minimal fragmentation [45] |
| Proteomics & Enzyme Activity Studies | Fresh-Frozen | Native protein conformation and retained enzymatic activity [45] |
| Routine Histopathology & Diagnosis | FFPE | Excellent morphological preservation for microscopic evaluation [45] |
| Immunohistochemistry (IHC) | FFPE (with caveats) | Widely established, though some epitopes may be damaged [45] |
| Super-Resolution Microscopy | FFPE preferred | Compatibility with standard protocols and morphological correlation [49] |
| Biomarker Discovery | Fresh-Frozen | Optimal biomolecule quality for novel target identification [45] |
| Biomarker Validation | FFPE | Access to large retrospective cohorts with clinical outcomes [47] |
| Long-term Biobanking | Context-dependent | FFPE: Room temperature stability; FF: Requires ultra-cold storage [45] |
| Functional & Viability Studies | Fresh-Frozen | Potential retention of cell viability for culture assays [45] |
The Scientist's Toolkit: Research Reagent Solutions
Selecting appropriate reagents and methodologies is crucial for optimizing results with either preservation method. The following table details essential solutions for working with FF and FFPE tissues.
Table 3: Essential Research Reagents and Solutions for Tissue Analysis
| Reagent/Solution | Primary Function | Application Context |
|---|---|---|
| RNA Stabilization Solutions | Preserve RNA integrity during freezing process | Fresh-Frozen: Prevents degradation during sample processing |
| Cryoprotective Agents | Minimize ice crystal formation | Fresh-Frozen: Improves cellular structure preservation |
| Antigen Retrieval Buffers | Reverse formalin-induced cross-linking | FFPE: Restores antigen accessibility for IHC and IF |
| DNA/RNA FFPE Extraction Kits | Optimized nucleic acid isolation | FFPE: Specialized protocols for cross-linked, fragmented biomolecules |
| Library Preparation Kits | NGS library construction from suboptimal samples | FFPE: Designed for fragmented DNA/RNA; Fresh-Frozen: Standard kits suitable |
| Hydrogel-Based Expansion Reagents | Physical tissue expansion for improved resolution | Expansion Microscopy: Enables nanoscale imaging on conventional microscopes [49] |
| Tissue Digestion Enzymes | Dissociate tissue for single-cell analyses | Both Methods: Enzyme selection and conditions vary by preservation method |
Methodological Protocols
Optimal Fresh-Frozen Tissue Processing
Sample Acquisition and Freezing: Collect tissue samples promptly after excision, minimizing ischemic time. For snap-freezing, place tissue in optimal cutting temperature (OCT) compound or directly submerge in liquid nitrogen. Use pre-cooled isopentane as an intermediate coolant for larger specimens to prevent cracking. Document sample orientation for future sectioning [45] [46].
Storage and Management: Store frozen tissues at -80°C or in liquid nitrogen vapor phase (-150°C to -196°C) for long-term preservation. Implement robust monitoring systems for temperature stability and power backup. Maintain detailed inventory records with freeze dates to track storage duration, as studies indicate gDNA concentration may decrease in samples stored beyond three years [48] [46].
Nucleic Acid Extraction: Use standard phenol-chloroform or column-based extraction methods. For RNA work, employ RNase-free conditions and include DNase treatment if needed. Assess nucleic acid quality using spectrophotometry, fluorometry, and fragment analysis (e.g., DNA Integrity Number, RNA Integrity Number) [48].
Optimized FFPE Tissue Processing
Fixation Protocol: Immerse tissues in 10% neutral buffered formalin within 30 minutes of excision. Maintain a tissue:fixative ratio of 1:10. Optimize fixation time based on tissue size (typically 24-48 hours for most specimens); prolonged fixation increases cross-linking and biomolecule degradation [47].
Embedding and Sectioning: Process fixed tissues through graded alcohols (70%-100%) for dehydration, followed by xylene clearing and paraffin infiltration. Use tissue processors for consistency. Section blocks at 2-5μm thickness using a microtome, float sections in a water bath at 40-45°C, and mount on charged slides [45] [47].
Nucleic Acid Extraction from FFPE: Use proteinase K digestion for extended periods (up to 72 hours) to reverse cross-links. Employ specialized FFPE DNA/RNA extraction kits with dedicated buffers. Include steps to remove paraffin and reverse formalin-induced modifications. Quantify yield and quality using methods appropriate for fragmented nucleic acids [47].
Super-Resolution Microscopy of FFPE Tissues
Sample Preparation: Section FFPE blocks at 2-5μm thickness. After deparaffinization and rehydration, perform antigen retrieval using heat-induced or enzymatic methods. Optimize antibody concentrations for sparse labeling, particularly for single-molecule localization microscopy [49].
Imaging and Analysis: Select appropriate SRM modality based on resolution requirements and equipment availability. For STED, use high-intensity depletion lasers; for SMLM, optimize blinking buffer composition. Process acquired data with appropriate reconstruction algorithms. Correlate super-resolution findings with conventional histology from adjacent sections [49].
The choice between fresh-frozen and FFPE tissue preservation is not a matter of identifying a universally superior option, but rather of matching preservation methodology to research objectives and practical constraints. Fresh-frozen tissues provide unparalleled biomolecular integrity for genomics, transcriptomics, and functional studies, while FFPE specimens offer exceptional morphological preservation, clinical relevance, and accessibility for large-scale validation studies. In the context of bio-optical cancer diagnostics, FFPE tissues are experiencing a renaissance through advanced applications like super-resolution microscopy, which extracts nanoscale information from these archived resources. The optimal approach often involves leveraging both preservation methods complementarily—using fresh-frozen tissues for discovery phases and FFPE collections for validation and translation. As biomarker science evolves with artificial intelligence and multi-omics integration, understanding these fundamental sample considerations remains essential for advancing cancer diagnostics and therapeutic development.
Bioinformatics Pipelines for Robust Data Analysis, Alignment, and Quality Control
In the field of clinical bio-optical cancer diagnostics research, the reliability of experimental findings is fundamentally dependent on the computational frameworks used for data analysis. Bioinformatics pipelines provide the essential structure for transforming raw, complex datasets into actionable biological insights. For researchers, scientists, and drug development professionals, selecting the appropriate pipeline framework is a critical decision that impacts the reproducibility, accuracy, and clinical translatability of research outcomes. This guide offers a comparative analysis of prominent bioinformatics pipeline frameworks, supported by experimental data and detailed methodologies, to inform selection decisions within the specific context of validating optical biosensors and label-free cancer diagnostic technologies.
Comparative Analysis of Bioinformatics Pipeline Frameworks
The landscape of workflow management systems is diverse, with each framework embodying a distinct philosophy toward data analysis, execution, and infrastructure management. The table below summarizes the core characteristics of five prominent frameworks.
Table 1: Technical Comparison of Bioinformatics Pipeline Frameworks
| Framework | Primary Language | Execution Model | Key Strength | Typical Use Case | Deployment |
|---|---|---|---|---|---|
| Nextflow | DSL (Groovy-based) | Dataflow channels with processes [51] | Reproducibility & hybrid execution [51] | Reproducible genomics pipelines [51] | HPC / Cloud [51] |
| Flyte | Python (Typed) | Typed, versioned DAGs on Kubernetes [51] | Type safety & versioning [51] | ML & bioinformatics pipelines [51] | Kubernetes [51] |
| Prefect | Python | Dynamic runtime task graphs [51] | Developer experience & observability [51] | Developer-friendly orchestration [51] | Cloud / Local [51] |
| Apache Airflow | Python | Static DAG scheduler [51] | Enterprise readiness & ecosystem [51] | Enterprise data workflows [51] | K8s / VM [51] |
| Snakemake | Python | Rule-based dataflow execution [52] | Readability & compatibility with HPC [52] | Academic research & data analysis [52] | HPC / Cloud [52] |
Among these, Nextflow has demonstrated significant growth in adoption, becoming a major driver in the adoption of bioinformatics workflow management systems [52]. Its dataflow model, which connects isolated processes via immutable channels, naturally supports reproducibility—a non-negotiable requirement in clinical research. Furthermore, its ability to seamlessly operate across high-performance computing (HPC), cloud, and local environments provides the flexibility needed in collaborative research settings [51].
Frameworks like Snakemake are also widely adopted in academic and research contexts due to their intuitive Python-based syntax and strong support for HPC schedulers [52]. In contrast, Airflow, with its static DAG model, is better suited for scheduled, predictable enterprise data workflows rather than the iterative, exploratory analysis common in research [51].
Performance Comparison of Analytical Tools and Assemblers
The choice of specific analytical tools within a pipeline can drastically affect results. This is particularly true for areas like metagenomic analysis and variant calling, where tool performance is critical for accurate diagnostics.
Assembler Performance in Viral Metagenomics
A 2025 study compared the performance of four different assemblers—MEGAHIT, rnaSPAdes, rnaviralSPAdes, and coronaSPAdes—in analyzing metagenomic sequencing data from nosocomial respiratory virus outbreaks [53]. The performance was evaluated based on the size of the largest contig produced and the percentage of the viral genome covered when aligned to a reference.
Table 2: Comparison of Assembler Performance in Viral Metagenomic Analysis [53]
| Assembler | Performance in Viral Outbreak Analysis | Key Metric |
|---|---|---|
| MEGAHIT | Standard performance | Largest contig size, genome alignment % |
| rnaSPAdes | Standard performance | Largest contig size, genome alignment % |
| rnaviralSPAdes | Standard performance | Largest contig size, genome alignment % |
| coronaSPAdes | Outperformed others for coronaviruses | Generated more complete data, higher viral genome coverage |
The study concluded that coronaSPAdes significantly outperformed the other pipelines for analyzing seasonal coronaviruses, generating more complete data and covering a higher percentage of the viral genome [53]. Achieving a higher percentage of the viral genome sequence is crucial for detailed characterization during an outbreak, where viral strains may differ by only a few genetic changes. This level of sensitivity is directly analogous to the requirements for detecting rare cancer biomarkers using bio-optical sensors.
Essential Tools for Data Quality Control
Robust quality control (QC) is the foundation of any reliable bioinformatics analysis. The "garbage in, garbage out" principle is acutely relevant in clinical diagnostics, where data errors can have direct consequences on patient outcomes [54]. Standardized QC tools are used at various stages of the pipeline to assess and ensure data integrity.
Table 3: Essential Bioinformatics Tools for Data Quality Control
| Tool | Function | Application in Pipeline |
|---|---|---|
| FastQC | Quality assessment of sequencing data [55] [56] | Initial QC of raw reads |
| Trimmomatic | Trimming of adapter sequences and low-quality bases [55] | Read preprocessing |
| MultiQC | Aggregates QC reports from multiple tools into a single report [55] | Summary and visualization of QC metrics |
| SAMtools | Processing and analysis of alignment files [55] | Post-alignment QC |
| Picard | Removes duplicate reads and other QC tasks [55] | Post-alignment QC |
| Qualimap | Generates alignment quality metrics and visualizations [54] | Post-alignment QC |
| GATK | Best practices for variant calling and quality score recalibration [54] | Variant discovery and filtering |
Experimental Protocols for Pipeline Validation
Implementing a pipeline requires more than just stringing tools together; it requires a rigorous methodology to ensure the entire workflow is robust and validated. The following protocol outlines key steps for validating a bioinformatics pipeline for cancer genomic data, incorporating lessons from metagenomic studies.
Detailed Protocol for Pipeline Validation
Objective: To validate a bioinformatics pipeline for the analysis of sequencing data from cancer diagnostics research, ensuring the reliability and reproducibility of variant calls and expression profiles.
Sample Preparation and Data Generation:
- Sample Source: Use well-characterized cell lines or patient-derived samples (e.g., from liquid biopsies) relevant to the cancer type under investigation [57].
- Spike-in Controls: Introduce synthetic oligonucleotides or DNA from a distinct organism at known concentrations to later assess sensitivity and specificity computationally [54].
- Sequencing: Perform next-generation sequencing (e.g., whole-genome, whole-exome, or RNA-seq) on an Illumina, PacBio, or Oxford Nanopore platform, following manufacturer protocols [58]. Document the library preparation kit and sequencing parameters meticulously.
Bioinformatics Analysis:
- Quality Control (QC): Run FastQC on raw FASTQ files to assess base quality, GC content, and adapter contamination. Use Trimmomatic to trim low-quality bases and adapter sequences based on QC results [55].
- Alignment: Align cleaned reads to a reference genome (e.g., GRCh38) using a splice-aware aligner like STAR for RNA-seq data or BWA for DNA-seq data [55].
- Post-Alignment QC: Use SAMtools to sort and index BAM files. Generate metrics for alignment rate, coverage depth, and uniformity using Qualimap. Mark or remove PCR duplicates using Picard [54].
- Variant Calling & Expression Quantification: Execute variant calling with GATK best practices for DNA-seq data, or quantify gene expression (e.g., with featureCounts) for RNA-seq data [54].
Validation and Verification:
- Cross-Tool Verification: Compare variant calls from two different callers (e.g., GATK and FreeBayes) to assess consensus [54].
- Experimental Validation: Select a subset of identified genetic variants (e.g., SNPs, fusions) for confirmation using an orthogonal method like Sanger sequencing or digital PCR [58].
- Reference Standard Comparison: If available, process a commercial reference standard with known variants (e.g., from Genome in a Bottle Consortium) through the entire pipeline to calculate accuracy, precision, and recall metrics [56].
Workflow Visualization of a Standardized Pipeline
The following diagram illustrates the logical flow and key quality control checkpoints of a robust bioinformatics pipeline, from raw data to validated results.
Diagram 1: Bioinformatics Pipeline with QC Checkpoints
The Scientist's Toolkit: Essential Research Reagent Solutions
The wet-lab reagents and materials used to generate samples are as critical as the computational tools. The quality of data entering the pipeline is contingent on the quality and appropriateness of these reagents.
Table 4: Essential Research Reagents for Bioinformatics-Grade Data Generation
| Reagent / Material | Function | Considerations for Clinical Diagnostics |
|---|---|---|
| Reference Standards | Well-characterized samples with known variants for pipeline validation [56]. | Essential for demonstrating analytical accuracy for regulatory compliance. |
| Nucleic Acid Extraction Kits | Isolate DNA/RNA from samples (tissue, blood, liquid biopsy) [58]. | Purity, yield, and integrity (e.g., RIN) directly impact sequencing library complexity. |
| Liquid Biopsy Collection Tubes | Stabilize circulating tumor cells (CTCs) and cell-free DNA in blood samples [57]. | Preserves analyte integrity, minimizing pre-analytical variability. |
| Library Preparation Kits | Prepare sequencing libraries from nucleic acids [53]. | Choice affects GC bias, duplicate rates, and coverage uniformity. |
| Spike-in Controls | Synthetic molecules added to samples to monitor technical performance [54]. | Allows for quality control and can help normalize for technical batch effects. |
| Optical Biosensor Chips | Nanostructured surfaces (e.g., photonic crystals) for label-free biomarker detection [59]. | Surface chemistry and nanomaterial properties dictate sensitivity and specificity. |
The choice of a bioinformatics pipeline is a strategic decision that underpins the validity of clinical diagnostics research. As demonstrated, frameworks like Nextflow offer a robust balance of reproducibility and flexibility, while specialized assemblers and QC tools are critical for generating accurate results. The integration of standardized experimental protocols, rigorous quality control checkpoints, and high-quality research reagents creates a synergistic system for producing reliable, clinically actionable data. For researchers in bio-optical cancer diagnostics, adopting these comprehensive practices is a necessary step toward translating innovative diagnostic technologies from the research lab into the clinical setting.
Clinical Application Across Hematologic and Solid Tumor Neoplasms
Diagnostic Foundations and Clinical Characterization
The diagnostic and clinical management of hematologic malignancies and solid tumors is fundamentally guided by their distinct origins and physical presentations. Hematologic malignancies originate from blood-forming tissues and are characterized by their diffuse, systemic nature, often precluding surgical intervention [60]. In contrast, solid tumors arise from specific organs or tissues, forming discrete masses that are frequently amenable to surgical resection [60]. This fundamental anatomical distinction directly shapes diagnostic strategies, treatment modalities, and clinical trial designs across oncology.
Epidemiologically, these cancer categories demonstrate different age distribution patterns. While solid tumors more commonly affect middle-aged to older populations, hematologic malignancies represent the most common cancers in children, though specific types like acute myeloid leukemia predominantly affect older adults [60]. The research landscape also reflects important disparities; despite hematological malignancies accounting for only approximately 6.2% of cancer deaths, they constituted 26% of malignancy-focused research articles in major clinical journals from 1995-2004, indicating substantial research interest relative to disease prevalence [61].
Table 1: Fundamental Diagnostic and Classification Approaches
| Diagnostic Characteristic | Hematologic Malignancies | Solid Tumors |
|---|---|---|
| Primary Diagnostic Methods | Peripheral blood smear, bone marrow biopsy, flow cytometry, cytogenetics [62] | Imaging (CT, MRI), tissue biopsy, histopathological examination [63] |
| Classification Basis | WHO classification based on cell lineage, genetic alterations, and immunophenotype [62] | Histological type, organ of origin, TNM staging, molecular profiling [64] |
| Common Genetic Alterations | Translocations (e.g., BCR-ABL, PML-RARA), mutations (FLT3, NPM1, IDH1/2) [62] | Point mutations (KRAS, BRAF, EGFR), copy number alterations, gene fusions (NTRK, ALK) [64] [65] |
| Key Specimen Types | Peripheral blood, bone marrow aspirate, lymph nodes [62] | Formalin-fixed paraffin-embedded (FFPE) tissue, liquid biopsy [66] [63] |
Figure 1: Diagnostic Workflow Comparison Between Hematologic and Solid Tumor Neoplasms
Molecular Profiling Technologies and Clinical Applications
Molecular profiling technologies have revolutionized diagnostic precision and therapeutic decision-making across both hematologic and solid tumor malignancies, albeit with technology platforms tailored to specific clinical needs. Comprehensive genomic profiling represents the cornerstone of modern oncology, enabling biomarker-driven treatment selection.
Next-generation sequencing (NGS) platforms form the technological backbone for comprehensive molecular characterization. The MI Cancer Seek assay exemplifies advanced profiling capabilities, utilizing whole exome sequencing (WES) and whole transcriptome sequencing (WTS) from minimal FFPE tissue input to detect single nucleotide variants, insertions/deletions, microsatellite instability, and tumor mutational burden across 228 genes [66]. This approach provides simultaneous RNA and DNA extraction, reducing tissue requirements and potential delays compared to individual testing processes [66].
Table 2: Advanced Molecular Profiling Technologies and Applications
| Technology Platform | Key Applications in Hematologic Malignancies | Key Applications in Solid Tumors | Clinical Utility |
|---|---|---|---|
| Whole Exome Sequencing (WES) | Identification of mutations in RUNX1, FLT3-ITD, NPM1, IDH1/2 in AML [62] | Comprehensive mutation profiling across 228+ genes (e.g., KRAS, BRAF, EGFR) [66] [64] | Therapeutic target identification, clinical trial eligibility |
| Whole Transcriptome Sequencing (WTS) | Detection of fusion transcripts (BCR-ABL1, PML-RARA, RUNX1-RUNX1T1) [62] | Gene expression profiling, fusion detection (NTRK, ALK, RET), tumor microenvironment analysis [66] | Diagnosis, prognostication, immunotherapy response prediction |
| Liquid Biopsy (ctDNA) | Minimal residual disease monitoring, early relapse detection [67] | Early detection, therapy selection, resistance monitoring, tumor heterogeneity assessment [63] | Non-invasive monitoring, guiding intervention decisions |
| Digital PCR | FLT3-ITD allelic ratio quantification, low-frequency mutation detection [62] | BRAF V600E mutation detection, quantitative biomarker assessment [63] | High-sensitivity mutation detection for low tumor burden |
The emergence of tissue-agnostic biomarkers represents a paradigm shift in precision oncology, bridging the historical divide between hematologic and solid tumor classifications. Targets including BRAFV600E mutations, IDH1/2 mutations, ALK, FGFR, and NTRK fusions, and microsatellite instability demonstrate therapeutic relevance across both cancer categories [65]. This convergence underscores that molecular drivers transcend traditional histological classifications, enabling biomarker-driven treatment strategies regardless of tissue origin.
Research Methodologies and Experimental Design
Research approaches for hematologic and solid tumor malignancies reflect their distinct disease biologies and clinical manifestations, with variations in specimen acquisition, model systems, and clinical trial designs.
Specimen acquisition differs substantially between these cancer categories. Hematologic malignancy research typically utilizes peripheral blood, bone marrow aspirates, or cerebrospinal fluid, which often contain malignant cells in liquid suspension [61]. Solid tumor research primarily relies on image-guided tissue biopsies or surgical resection specimens, increasingly supplemented by liquid biopsy approaches that analyze circulating tumor DNA, circulating tumor cells, or extracellular vesicles [63]. The relative ease of specimen procurement for hematologic malignancies partially explains the higher proportion of basic research publications (12% vs. 4.1%) compared to solid tumors [61].
Liquid biopsy technologies have particularly transformed solid tumor research and clinical management through non-invasive serial monitoring capabilities. These approaches analyze circulating tumor DNA (ctDNA), which accounts for only 0.1%-10% of total circulating cell-free DNA but provides high sensitivity for tumor detection [63]. Technological advances including droplet digital PCR and ultra-sensitive whole-genome sequencing assays have improved detection limits, enabling minimal residual disease monitoring in traditionally challenging low-shedding cancers [67].
Table 3: Experimental Models and Research Applications
| Research Model | Hematologic Malignancy Applications | Solid Tumor Applications | Key Limitations |
|---|---|---|---|
| Patient-Derived Xenografts (PDX) | Leukemia/lymphoma dissemination studies, stem cell biology | Tumor-stroma interactions, metastasis studies, drug penetration | Engraftment efficiency, cost, time |
| Cell Line Models | Established leukemia/lymphoma lines (e.g., HL-60, K562) | 2D/3D culture systems, organoid models | Genetic drift, limited microenvironment |
| Genetic Engineering Models | Transgenic mice (e.g., BCR-ABL, PML-RARA) | Genetically engineered mouse models (GEMMs) | Incomplete disease recapitulation |
| Liquid Biopsy Models | Circulating tumor cell isolation, ctDNA analysis | ctDNA methylation studies, extracellular vesicle analysis | Sensitivity in early-stage disease |
Figure 2: Specimen Collection and Analysis Workflow in Cancer Research
Clinical Trial Methodologies and Supportive Care Considerations
Clinical trial designs and supportive care approaches demonstrate significant variation between hematologic and solid tumor malignancies, reflecting their distinct disease courses, treatment modalities, and complication profiles.
Trial design characteristics differ between these cancer categories. Hematologic malignancy trials show a higher proportion of non-randomized clinical trials (11% vs. 3.4%) compared to solid tumors [61]. This may reflect the sensitivity of certain hematologic malignancies to novel agents and their frequent position as first candidates for newly developed anticancer drugs [61]. Solid tumor trials more commonly feature randomized designs, particularly in advanced disease settings where standard-of-care comparisons are more established [61].
Supportive care terminology and implementation also demonstrate notable variations. Hematologic malignancy guidelines are significantly more likely to use the term "supportive care" (94% vs. 59%) and describe it as management of cancer-related complications (73% vs. 9%) compared to solid tumor guidelines [68]. Conversely, solid tumor guidelines more frequently mention "best supportive care" (78% vs. 43%), typically in advanced disease settings where active anticancer treatment is no longer pursued [68].
Essential Research Reagent Solutions
- Nucleic Acid Extraction Kits: Specialized reagents for DNA/RNA extraction from diverse specimen types including FFPE tissue, peripheral blood, and bone marrow aspirates. Enable high-quality nucleic acid recovery from challenging, limited specimens [66] [64].
- Multiplex PCR Master Mixes: Optimized enzymatic formulations for simultaneous amplification of multiple genomic targets from minimal input material. Critical for NGS library preparation and targeted sequencing panels [62] [64].
- ctDNA Enrichment Reagents: Specialized solutions for selective isolation and stabilization of circulating tumor DNA from plasma samples. Include fragment size-based selection methods to enhance signal-to-noise ratio in liquid biopsy applications [63].
- Flow Cytometry Antibody Panels: Comprehensive fluorescent antibody combinations for immunophenotyping hematopoietic cells. Enable detection of lineage-specific markers, differentiation patterns, and minimal residual disease in hematologic malignancies [62].
- IHC Staining Kits: Automated immunohistochemistry reagents for protein expression analysis in tissue sections. Include antigen retrieval solutions and detection systems optimized for FFPE tissue [64].
- Cryopreservation Media: Specialized formulations for maintaining viability of primary patient samples including malignant cells, stem cells, and tumor-infiltrating lymphocytes. Enable creation of biobanks for longitudinal studies [60].
Emerging Technologies and Future Directions
The oncology landscape is rapidly evolving with several disruptive technologies demonstrating transformative potential across both hematologic and solid tumor malignancies.
Artificial intelligence platforms are advancing diagnostic precision and biomarker quantification. Recent applications demonstrate superior sensitivity in immunohistochemistry scoring, particularly for identifying HER2-low and ultra-low breast cancers, and enhanced accuracy in biomarker assessment including TROP2 [67]. AI algorithms are also expanding across the drug development continuum, from target discovery and clinical trial design to diagnostic applications and patient care optimization [67].
Multi-cancer detection (MCD) tests represent a paradigm shift in cancer screening, analyzing cancer-related biological signatures in blood including DNA fragments, methylation patterns, RNA, and proteins [67]. These tests utilize machine learning algorithms to predict tissue of origin, with clinical utility dependent on achieving critical balances between high specificity to minimize false positives and sufficient sensitivity for early-stage disease detection [67].
Cell and gene therapies are demonstrating remarkable expansion from hematologic to solid tumor applications. TCR therapies including afami-cel (targeting MAGE-A4) and lete-cel (targeting NY-ESO-1) show promising activity in synovial sarcoma and myxoid round-cell liposarcoma [67]. Similarly, tumor-infiltrating lymphocyte therapy lifileucel has gained FDA approval for metastatic melanoma [67]. Emerging natural killer (NK) cell therapies offer promising off-the-shelf alternatives with faster production timelines and potentially improved toxicity profiles compared to traditional gene therapies [67].
The continued convergence of molecular profiling technologies, combined with innovative therapeutic modalities and advanced computational analytics, promises to further bridge the historical divide between hematologic and solid tumor malignancies, ultimately enabling more precise, effective, and patient-specific cancer care.
Navigating the Translational Gap: Troubleshooting Common Validation Hurdles
Overcoming Preclinical-Clinical Divide with Human-Relevant Models (PDX, Organoids)
A significant translational gap remains a major roadblock in oncology drug development, with less than 1% of published cancer biomarkers ultimately entering clinical practice [69]. This failure stems largely from the poor predictive power of traditional preclinical models, such as conventional cell lines and animal models, which suffer from genetic drift and cannot fully replicate human disease heterogeneity and the tumor microenvironment (TME) [70] [69]. Consequently, drug responses observed in these models frequently fail to predict clinical outcomes, leading to costly late-stage trial failures and delays in delivering effective treatments to patients.
To bridge this divide, the field has increasingly adopted more human-relevant models, primarily patient-derived xenografts (PDX) and patient-derived organoids (PDOs). These models preserve key characteristics of original patient tumors, including genetic profiles, histopathological features, and intratumoral heterogeneity, enabling more predictive preclinical research [71] [72]. This guide provides a comparative analysis of PDX and PDO models, detailing their established capabilities, limitations, and roles in advancing clinically translatable research, with a specific focus on their application in validating bio-optical cancer diagnostics.
Model Comparison: PDX vs. Organoids
Patient-derived models offer complementary strengths. The table below provides a systematic comparison of their core characteristics.
Table 1: Fundamental Characteristics of PDX and PDO Models
| Characteristic | Patient-Derived Organoids (PDOs) | Patient-Derived Xenograft (PDX) Models |
|---|---|---|
| Model Type | Ex vivo 3D cell culture | In vivo animal model |
| Patient Recapitulation | Yes | Yes |
| Tumor Microenvironment | Limited or none (can be added via co-culture) | Yes (murine stroma) |
| Maintenance of Immune Response | No | No (requires humanized mice) |
| Scalability | High (amenable to HTS) | Medium |
| Establishment Time | Relatively fast (weeks) | Generally slow (months) |
| Cost | Relatively low | High |
| Genetic/Histologic Stability | High in culture [73] | High through passages [72] |
Quantitative Correlation with Clinical Response
The ultimate validation of a preclinical model is its ability to predict patient outcomes. Both PDX and PDO models have demonstrated significant correlation with clinical drug response.
Table 2: Documented Predictive Performance of Human-Relevant Models
| Model Type | Cancer Type | Reported Correlation with Clinical Response | Key Evidence |
|---|---|---|---|
| PDX-derived Organoids (PXO) | Pancreatic Ductal Adenocarcinoma (PDAC) | Specific relationship between organoid drug dose response (AUC) and in vivo tumor growth, irrespective of drug [70]. | Recapitulated in vivo glycan landscape and drug response of matched PDX [70]. |
| PDOs | Various Gastrointestinal Cancers | 100% sensitivity, 93% specificity in predicting patient response to chemotherapy or targeted therapy [71]. | A living biobank of PDOs accurately forecasted patient responses in a clinical setting [71]. |
| PDOs | Oesophageal Adenocarcinoma (EAC) | Drug sensitivity of PDOs consistent with patient molecular status and chemoresistance [71]. | EAC PDO with ERBB2 amplification responded to mubritinib, while wild-type organoids did not [71]. |
| PDX | Colorectal Cancer | Biological equivalency (>90% correlation) in drug response between matched PDX and organoids [73]. | PDXOs serve as effective surrogates for high-throughput screens, maintaining clinical relevance [73]. |
Experimental Workflows and Protocols
Establishing and Utilizing a PDX-Organoid Platform
The integrated use of PDX models and organoids derived from them (PDXOs) creates a powerful platform for sequential in vitro and in vivo validation. The workflow below outlines this process.
Key Methodological Details
PDX-derived Organoid (PXO) Culture (WNT-free conditions): This protocol is critical for maintaining in vivo-like differentiation and drug response [70].
- Tissue Processing: Minced PDX tumor tissue is subjected to enzymatic digestion (e.g., collagenase) to create a single-cell suspension or small clusters.
- Matrix Embedding: The cell suspension is mixed with a basement membrane extract (e.g., Matrigel) and plated to form a 3D support scaffold.
- Culture Medium: Cells are fed with a specialized Pancreatic Tumor Organoid Medium (PTOM), which is serum-free and lacks exogenous WNT ligands. Growth factors such as EGF, Noggin, and R-spondin are typically included to support stem cell expansion and organoid growth [70].
- Drug Screening: Established organoids are dissociated and re-embedded in matrix in multi-well plates. Compounds are added at varying doses, and viability is assessed after several days using assays like CellTiter-Glo.
Orthotopic PDX Model with Advanced Imaging: This protocol enhances the clinical relevance of PDX models [74].
- Implantation: Tumor cells or tissue fragments are implanted into the organ-specific site of the original tumor (e.g., pancreas) in immunodeficient mice, using high-frequency ultrasound for guidance to ensure precision.
- Longitudinal Monitoring: Tumor growth and metastasis are tracked in real-time using non-invasive imaging techniques such as:
- High-frequency ultrasound for precise 2D and 3D measurement of tumor volume.
- Bioluminescence imaging (BLI) to monitor tumor burden and metastatic spread in real-time.
- Therapeutic Intervention: Once tumors are established, mice are randomized into treatment and control groups. Drug efficacy is evaluated based on tumor growth inhibition and metastasis reduction.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these models relies on a specific set of reagents and tools.
Table 3: Essential Reagents and Tools for PDX and PDO Research
| Reagent/Tool | Function | Example Application |
|---|---|---|
| Basement Membrane Extract (Matrigel) | Provides a 3D extracellular matrix scaffold for organoid growth. | Used to embed dissociated tumor cells for PDO and PXO formation [70]. |
| Specialized Media Formulations | Provides lineage-specific growth factors and signals. | WNT-free PTOM medium maintains in vivo differentiation; other media may include WNT3A, R-spondin, Noggin [70] [71]. |
| Immunodeficient Mice | Host for PDX models, allowing engraftment of human tissue. | Used to propagate patient tumors in vivo for PDX generation and subsequent therapy testing [71] [72]. |
| Enzymatic Dissociation Kits | Liberates viable cells from tumor tissues for culture. | Contains collagenase and other enzymes to process solid tumor samples into single-cell suspensions for organoid culture [70]. |
| High-Frequency Ultrasound Imager | Guides orthotopic implantation and measures deep tumor volumes. | Enables precise implantation into organ-specific sites and allows non-invasive, longitudinal tracking of tumor growth in orthotopic PDX models [74]. |
PDX and PDO models are not mutually exclusive but are powerfully complementary. The integrated workflow, where high-throughput drug screening in patient-relevant PDOs is followed by targeted validation in clinically predictive PDX models, offers a rational and efficient path to de-risking drug development. By faithfully capturing patient-specific disease biology, these human-relevant models are proving indispensable for bridging the preclinical-clinical divide, ultimately accelerating the delivery of effective therapies to cancer patients.
Addressing Tumor Heterogeneity and Limits of Detection in Complex Samples
Tumor heterogeneity presents a formidable challenge in oncology, complicating diagnosis, prognostication, and therapeutic intervention [75]. This variability manifests at multiple levels—within individual tumors (intratumoral), between different tumors in the same patient (intertumoral), and across different patients with histologically similar cancers (interpatient) [75]. The clinical consequence of this diversity is significant differential treatment response among patients, driving the need for advanced diagnostic approaches that can navigate this complexity [75].
Concurrently, the limits of detection in complex biological samples constrain our ability to characterize rare cell populations and subtle molecular alterations that drive cancer progression and therapy resistance. Next-generation technologies—including single-cell sequencing, spatial transcriptomics, liquid biopsy, and artificial intelligence—are now pushing these boundaries, enabling unprecedented resolution into the multidimensional complexity of cancer [75].
This comparison guide objectively evaluates leading technological approaches and platforms addressing these dual challenges, providing researchers and drug development professionals with experimental data and methodological frameworks to advance precision oncology.
Technological Approaches for Deconvoluting Tumor Heterogeneity
Comprehensive Molecular Profiling Platforms
Table 1: Comparison of Comprehensive Molecular Profiling Approaches
| Platform/Technology | Primary Analytical Targets | Key Strengths | Detection Limitations | Reported Performance Metrics |
|---|---|---|---|---|
| MI Cancer Seek (Caris) [66] | Whole exome (WES), whole transcriptome (WTS), SNVs, indels, MSI, TMB, CNA | Simultaneous RNA/DNA extraction from minimal tissue; FDA-approved CDx claims | Tissue input requirements; limited to predefined 228-gene panel | Positive/negative agreement: 97-100% vs. other FDA-approved assays |
| Single-cell RNA-seq Atlas [76] | Transcriptomes of 5 cell types simultaneously; 70 cell subtypes | Identifies spatially co-localized immune hubs; associates with ICB response | Loss of spatial context in standard protocol; dissociation bias | 611,750 high-quality cells; 1,358 avg. genes/cell; 9 cancer types |
| Heterogeneity-optimized ML Framework [77] | 7 clinical/molecular features (TMB, NLR, BMI, etc.) | Addresses multimodal distribution violation of unimodal assumptions | Requires large training cohorts; complex implementation | Accuracy gain: ≥1.24% vs. 11 baseline methods; validated in external cohort |
| Multi-cancer Early Detection (MCED) [78] | Circulating tumor DNA (ctDNA) methylation, fragmentation | Non-invasive; broad cancer type coverage | Limited sensitivity for early-stage cancers; false positives | Under investigation; not yet approved for clinical use |
Spatial Resolution Technologies
Table 2: Spatial Technologies for Tumor Microenvironment Analysis
| Technology Approach | Resolution Capability | Heterogeneity Insights | Sample Requirements | Key Findings |
|---|---|---|---|---|
| Integrated scRNA-seq + Spatial Transcriptomics [79] | Single-cell (RNA-seq); spot-based (spatial) | Reveals region-specific cell distribution; tumor-grade associations | Fresh frozen or FFPE tissue sections | High-grade tumors show greater tumor cell density; intermediate-grade has higher immune content |
| Spatial Characterization of TME Hubs [76] | Identification of spatially co-localized subtypes | Two TME hubs: TLS-like and PD1+/PD-L1+ immune-regulatory cells | 230 treatment-naive samples across 9 cancer types | Hub abundance associates with early and long-term ICB response |
| Spatial CNV Inference + Cell-type Deconvolution [79] | Tumor/non-tumor classification with spatial context | Distinguishes tumor and immune-enriched zones across grades | 9 BRCA samples with H&E staining | SCGB2A2+ neoplastic cells enriched in low-grade tumors with distinct spatial localization |
Experimental Protocols and Methodologies
Pan-Cancer Single-Cell Atlas Construction
Experimental Protocol (adapted from Lodi et al. [76]):
- Sample Collection: 230 tissue samples from 160 patients across 9 cancer types (BC, CC, CRC, GBM, HNSCC, HCC, HGSOC, MEL, NSCLC), predominantly treatment-naïve.
- Tissue Processing: Standardized dissociation protocol into single-cell suspension, with majority (61.3%) subjected to 5'-scRNA-seq (10× Genomics).
- Quality Control: 611,750 high-quality cells retained with mean detection of 1,358 genes/cell.
- Cell Type Identification: Analysis per cancer type for cancer/epithelial cells, endothelial cells, fibroblasts, and immune populations (DCs, macrophages/monocytes, mast cells, B cells, NK cells, T cells).
- Dissociation Bias Assessment: Comparison of cell type fractions between scRNA-seq and bulk RNA-seq deconvolution from 25 samples across 4 cancer types.
- Batch Effect Correction: Harmony algorithm applied to correct for 5' vs. 3' scRNA-seq batch effects, with LISI scores confirming correction.
- Subclustering Analysis: 70 pan-cancer single-cell subtypes identified based on marker genes and published signatures.
Heterogeneity-Optimized Machine Learning Framework
Experimental Protocol (adapted from Scientific Reports 2025 [77]):
- Data Source: Pan-cancer cohort of 1,479 ICB-treated patients across 16 cancer types from Chowell et al. [77].
- Response Classification: RECIST v1.1 criteria with responders (n=409; complete/partial response) and non-responders (n=1,070; stable/progressive disease).
- Feature Processing:
- Dichotomous features (sex, prior chemotherapy) directly encoded as 0/1
- Ordinal variables (disease stage, ECOG score) assigned integer values
- Nominal variables (cancer type, drug class) one-hot encoded
- Continuous features (TMB, FCNA, MSI) log10(x+1) transformed and z-scored
- Heterogeneity Testing: Multimodal distribution analysis using Mann-Whitney U test (continuous) and Fisher's exact test (categorical).
- Clustering: K-means clustering (K=2) identified hot-tumor and cold-tumor subgroups, validated by silhouette analysis and elbow method.
- Predictive Modeling: SVM developed for hot-tumor subtype; Random Forest for cold-tumor subtype using 7 heterogeneity-associated biomarkers.
- Validation: External validation using independent metastatic melanoma cohort (Liu et al. [77]).
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Tumor Heterogeneity Studies
| Reagent/Platform Category | Specific Examples | Primary Function | Considerations for Complex Samples |
|---|---|---|---|
| Single-cell RNA-seq Platforms | 10x Genomics (5'/3') | High-throughput single-cell transcriptomics | Dissociation bias assessment critical; cell viability impacts recovery |
| Spatial Transcriptomics | InferCNV, CARD deconvolution | Spatial mapping of cell types with CNV inference | Resolution limits (spot-based); integration with scRNA-seq required |
| Liquid Biopsy Assays | MCED tests (under development) | Non-invasive cancer detection via ctDNA | Sensitivity limitations for early-stage disease; false positives |
| Multimodal Integration Tools | Harmony batch correction | Integrates datasets while removing technical variance | Algorithm choice affects biological signal preservation |
| AI/ML Analytical Frameworks | Heterogeneity-optimized SVM/RF | Models multimodal distributions in patient data | Requires large training cohorts; complex implementation |
| Molecular Profiling Panels | MI Cancer Seek (228 genes) | Comprehensive SNV, indel, MSI, TMB assessment | Tissue input requirements; coverage limitations |
Discussion and Future Directions
The evolving landscape of tumor heterogeneity research reveals several critical trends. Artificial intelligence and automation are playing increasingly transformative roles, with AI demonstrating superior sensitivity in immunohistochemistry scoring and enabling image-based biomarkers that identify previously undetectable patterns [80]. The integration of single-cell and spatial technologies provides unprecedented insight into the spatial organization of tumor ecosystems, revealing clinically relevant structures such as tertiary lymphoid structures and immune-reactive hubs that correlate with immunotherapy response [76] [79].
Liquid biopsy technologies continue to advance, with multi-cancer early detection tests showing potential to revolutionize cancer screening, though they currently face sensitivity limitations for early-stage disease and have not yet received regulatory approval for clinical use [78]. The validation of comprehensive profiling assays like MI Cancer Seek demonstrates the feasibility of combining whole exome and whole transcriptome sequencing from minimal tissue inputs, addressing practical constraints in clinical implementation [66].
Future advancements will likely focus on multi-omic integration at single-cell resolution, improved sensitivity for detecting rare cell populations and early-stage malignancies, and standardized computational frameworks for reconciling the multimodal distributions inherent in heterogeneous cancer populations. These technologies collectively push the boundaries of detection in complex samples, enabling researchers and clinicians to navigate the challenges of tumor heterogeneity with increasing precision and clinical utility.
In the field of bio-optical cancer diagnostics, the integrity of research data and the success of clinical translation are fundamentally dependent on effectively managing pre-analytical variables. These factors, which encompass all processes from sample collection to analysis, introduce significant technical variability that can compromise assay performance and lead to erroneous conclusions. It has been estimated that pre-analytical variables account for up to 75% of laboratory errors in diagnostic processes, highlighting their profound impact on data reliability [81] [82]. For researchers and drug development professionals, understanding and mitigating these variables is not merely a quality control measure but a fundamental requirement for generating clinically valid and reproducible results.
The challenge is particularly acute in oncology, where biomarkers such as circulating tumor DNA, proteins, and RNA transcripts are highly susceptible to degradation and alteration under suboptimal pre-analytical conditions [83]. As advocated in ICH Q14 and USP <1220>, continued verification of critical method attributes linked to bias and precision is essential throughout the analytical method lifecycle [84]. This article provides a comprehensive comparison of how different bio-analytical approaches perform under various pre-analytical challenges, offering experimental data and methodologies to strengthen assay robustness in cancer research.
Understanding Pre-analytical Variables and Their Impacts
Pre-analytical variables encompass all activities and conditions occurring prior to the actual analytical testing of a sample [83]. In the context of cancer diagnostics, these variables can be systematically categorized to better understand and control their effects:
- Sample Collection Variables: Including sampling methods (surgical, biopsy, cytological), collection apparatus (tube type, anticoagulants), and patient-related factors (anesthesia, sampling site) [85] [82].
- Sample Processing Variables: encompassing processing delays, centrifugation protocols, temperature conditions, and tumor sample heterogeneity [83] [85].
- Sample Storage and Transportation Variables: Including storage temperature, duration, freeze-thaw cycles, shipping conditions, and preservation methods (FFPE vs. fresh-frozen) [83] [85].
- Analytical Preparation Variables: covering RNA/DNA quantity and quality, library preparation kits, amplification methods, and laboratory site variations [85].
The practical implications of these variables are substantial. For instance, one study demonstrated that the choice of blood sampling site in mice significantly affected measured plasma insulin concentrations, with retrobulbar sinus sampling yielding consistently lower values compared to tail vein sampling under identical conditions [82]. Similarly, the duration between sample aspiration and preservation has been shown to dramatically impact RNA integrity, with delays of 24-48 hours causing expression changes in thousands of genes [85]. These examples underscore why assays that perform well under controlled laboratory conditions often exhibit unexpected variability when deployed in clinical settings with diverse pre-analytical workflows [83].
Comparative Analysis of Assay Robustness to Pre-analytical Variability
Different analytical approaches exhibit varying levels of resilience to pre-analytical challenges. The following comparison examines three primary methodological frameworks used in cancer diagnostics, with particular focus on their robustness to pre-analytical variability.
Quantitative Comparison of Method Performance
Table 1: Comparative robustness of diagnostic approaches to pre-analytical variables
| Analytical Approach | Impact of Sample Heterogeneity | Impact of Processing Delays | Impact of Preservation Methods | Data Type Generated |
|---|---|---|---|---|
| Absolute Expression Analysis | High sensitivity: 5,707 genes showed ≥2-fold change with low tumor cellularity (73%-14% vs 93%-74%) [85] | High sensitivity: 2,113-2,970 genes showed ≥2-fold change with 24-48 hour delays [85] | High sensitivity: Significant expression differences between FFPE vs fresh-frozen samples [85] | Continuous numerical measurements relative to calibrators |
| Relative Expression Ordering (REO) | High robustness: 89.24% consistency score maintained despite tumor cellularity variations; increased to 92.46% after excluding 10% of closest-expressed gene pairs [85] | High robustness: 85.63%-88.94% consistency scores maintained despite 24-48 hour processing delays [85] | High robustness: Maintained consistent REO patterns despite preservation method differences [85] | Binary comparisons of gene expression ranks within individual samples |
| AI-Based Histopathology Models | Variable performance: Affected by training data diversity and stain normalization techniques [86] | Limited data; potentially significant impact depending on biomarker stability | Performance variations between FFPE and fresh tissue processing [86] | Classification outputs (e.g., malignant vs. non-malignant, cancer subtypes) |
Key Findings and Performance Insights
The comparative data reveal several critical patterns:
Absolute Expression Quantification demonstrates high sensitivity to pre-analytical variables, with thousands of genes showing significant expression changes (≥2-fold) in response to suboptimal conditions. This approach provides precise quantitative measurements but requires stringent control over pre-analytical factors [85].
Relative Expression Ordering (REO) exhibits remarkable robustness across multiple pre-analytical challenges. Despite substantial changes in absolute expression values, the relative ordering of gene pairs remains largely consistent (76%-82% consistency in multivariable analyses) [85]. This approach maintains analytical performance even with variations in tumor cellularity, processing delays, and preservation methods, making it particularly valuable for samples collected in diverse clinical settings.
AI-Based Digital Pathology Models show variable robustness depending on their training and validation approaches. Models validated on technically diverse datasets (incorporating different scanners, stains, and preservation methods) generally demonstrate better real-world performance [86]. External validation remains a significant challenge, with only approximately 10% of AI pathology models undergoing proper external validation [86].
Table 2: Impact of specific pre-analytical variables on gene expression measurements
| Pre-analytical Variable | Effect on Absolute Expression | Effect on REO Consistency | Recommended Mitigation Strategy |
|---|---|---|---|
| Sampling Method (Biopsy vs Surgical) | 3,286 genes with ≥2-fold change [85] | >86% consistency maintained; increased to 89.90% after excluding 10% closest-expressed gene pairs [85] | Standardize sampling protocols; account for method in analysis |
| Tumor Cellularity (Low vs High) | 5,707 genes with ≥2-fold change [85] | 89.24% consistency maintained; increased to 92.46% after filtering [85] | Document cellularity percentages; establish minimum thresholds |
| Processing Delays (24-48 hours) | 2,113-2,970 genes with ≥2-fold change [85] | 85.63%-88.94% consistency maintained [85] | Implement strict processing windows; use stabilizing preservatives |
| Multi-variable Effects (Combined variables) | Thousands of genes with ≥2-fold change [85] | 76% consistency maintained in multi-variable analysis [85] | Implement comprehensive quality control systems |
Experimental Protocols for Assessing Pre-analytical Variability
Robust evaluation of pre-analytical variables requires systematic experimental approaches. The following protocols provide methodologies for quantifying the impact of these variables on assay performance.
Controlled Comparative Biospecimen Studies
Objective: To directly quantify the impact of specific pre-analytical variables on assay performance metrics [83].
Methodology:
- Collect biospecimens from the same patients under different pre-analytical conditions (immediate vs. delayed processing, different storage temperatures, alternative collection tubes)
- Process all samples through identical analytical workflows
- Compare results between matched sample pairs to isolate pre-analytical effects
Key Measurements:
- For absolute quantification: Percentage of genes/proteins with significant expression changes (≥2-fold)
- For REO analysis: Consistency scores of gene pair orderings between paired samples
- For AI models: Changes in classification accuracy, sensitivity, and specificity
Data Interpretation: Calculate consistency scores using the formula: CS = N/(N+M), where N represents the number of gene pairs with consistent REO patterns and M represents contradictory pairs between paired samples [85]. This approach enables quantitative assessment of pre-analytical impacts on assay robustness.
Multi-variable Robustness Assessment
Objective: To evaluate combined effects of multiple pre-analytical variables reflecting real-world conditions [85].
Methodology:
- Design experiments that simultaneously vary multiple pre-analytical factors (e.g., sampling method, processing delay, storage condition)
- Utilize factorial experimental designs to efficiently explore variable interactions
- Compare case samples (exposed to multiple suboptimal conditions) against control samples (optimally processed) from the same donors
Analysis Approach:
- Quantify both absolute expression changes and REO consistency
- Statistically compare the proportion of differentially expressed genes versus reversed gene pairs
- Calculate the proportion of reversal gene pairs among all pairs involving differentially expressed genes
Visualizing Pre-analytical Workflows and Robustness Strategies
Effective management of pre-analytical variability requires clear understanding of sample journeys and critical control points. The following diagrams illustrate key workflows and strategic approaches.
Pre-analytical Phase Workflow
Diagram 1: Pre-analytical workflow in cancer diagnostics
REO Robustness Concept
Diagram 2: REO robustness concept under pre-analytical variability
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful management of pre-analytical variability requires appropriate selection of research reagents and materials. The following toolkit highlights critical solutions for robust cancer diagnostics research.
Table 3: Essential research reagents for managing pre-analytical variability
| Reagent/Material | Function | Selection Considerations | Impact on Pre-analytical Variability |
|---|---|---|---|
| Specialized Collection Tubes (e.g., Streck, PreAnalytiX) | Stabilize specific biomarkers during collection and transport | Compatibility with target biomarkers (e.g., DNA, RNA, proteins); stability profile; cost considerations [83] | High impact: Can significantly extend processing windows and preserve biomarker integrity |
| RNA/DNA Stabilization Buffers | Prevent nucleic acid degradation during processing delays | Processing delay tolerance; compatibility with downstream applications; storage requirements [85] | Critical for transcriptomic studies: Reduces degradation-related artifacts in expression profiling |
| Multiplex Immunoassay Kits | Simultaneous measurement of multiple protein biomarkers | Validation data for rodent samples; matrix compatibility; performance characteristics [82] | Medium-high impact: Proper validation reduces analytical variability in protein biomarker studies |
| Standardized Library Preparation Kits | Consistent NGS library construction across samples | Performance with degraded samples; input requirements; reproducibility between batches [85] | Medium impact: Standardization reduces technical variability in sequencing-based assays |
| Quality Control Assays (e.g., RNA Integrity Number) | Assess sample quality pre-analysis | Correlation with downstream assay performance; sample requirements; throughput [85] | Essential for all studies: Enables objective sample quality assessment and inclusion/exclusion decisions |
The management of pre-analytical variables represents a critical challenge in the clinical validation of bio-optical cancer diagnostics. The comparative data presented in this analysis demonstrates that while absolute quantification methods provide precise measurements, they show high sensitivity to pre-analytical variations. In contrast, REO-based approaches exhibit remarkable robustness across multiple pre-analytical challenges, maintaining consistent performance even with variations in tumor cellularity, processing delays, and preservation methods [85]. AI-based digital pathology models show promise but require rigorous external validation on technically diverse datasets to ensure real-world applicability [86].
For researchers and drug development professionals, strategic assay selection should be guided by the anticipated pre-analytical conditions of the target clinical setting. In environments with limited standardization capabilities, REO-based approaches may offer more reliable performance. Regardless of the chosen methodology, comprehensive pre-analytical validation using controlled comparative studies remains essential for generating clinically meaningful data [83]. By systematically addressing pre-analytical variability through appropriate reagent selection, protocol standardization, and robust analytical design, the cancer research community can accelerate the development of reliable diagnostic tools that perform consistently across diverse clinical environments.
Bridging the Technical-Clinical Divide in AI Validation and Interpretation
The integration of Artificial Intelligence (AI) into bio-optical cancer diagnostics presents a paradigm shift for early detection and characterization of diseases like cervical cancer. However, a significant chasm often exists between technically proficient AI models and their reliable, clinically validated application. For researchers, scientists, and drug development professionals, bridging this technical-clinical divide is paramount. Robust validation frameworks ensure that AI-driven interpretations of optical data—such as multispectral imaging for quantifying tissue oxygen saturation—are not only computationally sound but also clinically actionable, safe, and effective [87] [88]. This guide provides a structured approach for the objective comparison of AI validation tools and methodologies, framed within the critical context of clinical translation for bio-optical cancer diagnostics.
Comparative Analysis of AI Validation Approaches
A systematic approach to AI model validation is essential for establishing trust in predictive outputs. The following table compares core validation methodologies, highlighting their clinical relevance.
Table 1: Comparison of AI Model Validation Approaches
| Validation Approach | Core Principle | Clinical Analogy | Best Suited For | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Hold-Out Validation | Single split of data into training, validation, and test sets. | Initial pilot study with a distinct patient cohort for final testing. | Large, stable datasets with high event rates. | Simple, fast, and computationally efficient. | Estimates of performance can be highly variable based on a single data split. |
| Cross-Validation (e.g., k-Fold) | Data is partitioned into 'k' folds; model is trained and validated 'k' times, each time with a different fold as the test set. | Multi-site clinical trial to ensure model generalizability across different patient populations. | Medium-sized datasets or models requiring hyperparameter tuning. | Provides a more robust and stable estimate of model performance; maximizes data use. | Computationally intensive; can be problematic for temporal or correlated data. |
| Time-Series Validation | Data is split chronologically, with past data used for training and future data for testing. | Validating a prognostic model on patients enrolled after the initial training cohort. | Any predictive task involving temporal data, such as disease progression. | Realistically simulates model deployment in a clinical setting; prevents data leakage from the future. | Requires substantial historical data; cannot use future data to predict the past. |
| A/B Testing | Comparing the performance of a new model (B) against the current standard (A) in a live, randomized controlled environment. | Comparing a new AI-assisted diagnostic probe against standard colposcopy in a clinical workflow. | Validating the real-world impact of a new model before full-scale deployment. | Provides the highest level of evidence for clinical efficacy and utility. | Complex to set up ethically and technically; requires a live clinical environment. |
Selecting the appropriate validation strategy is the first step. The subsequent critical phase is defining what success looks like through a balanced set of metrics that align with both technical and clinical goals [89].
Defining Success: A Multi-Dimensional Metric Framework
A clinically validated AI model must be evaluated beyond simple accuracy. A multi-faceted metric framework ensures the model is robust, fair, and impactful.
Table 2: Key Performance Metrics for Clinical AI Validation
| Metric Category | Specific Metric | Technical Definition | Clinical Interpretation & Importance |
|---|---|---|---|
| Performance & Accuracy | Precision (Positive Predictive Value) | (True Positives) / (True Positives + False Positives) | The probability that a positive AI finding (e.g., "precancerous lesion") is correct. High precision minimizes unnecessary biopsies or treatments. |
| Recall (Sensitivity) | (True Positives) / (True Positives + False Negatives) | The model's ability to identify all actual disease cases. High recall is critical for screening applications to avoid missing cancers. | |
| F1-Score | 2 * (Precision * Recall) / (Precision + Recall) | The harmonic mean of precision and recall, providing a single score to balance the two when their relative importance is equal. | |
| Robustness & Fairness | Fairness/Bias Metrics (e.g., Equalized Odds) | Measures of performance disparity across different demographic subgroups (e.g., age, ethnicity). | Ensures the model performs equitably for all patient populations, preventing the amplification of healthcare disparities. |
| Confusion Matrix | A table showing counts of True Positives, False Positives, True Negatives, and False Negatives. | Provides a complete picture of where the model succeeds and fails, allowing clinicians to understand its error profile. | |
| Clinical Utility | Specificity | (True Negatives) / (True Negatives + False Positives) | The probability that a negative finding is truly negative. High specificity helps correctly reassure healthy patients. |
Case Study: Clinical Validation of a Bio-Optical Imaging Probe
To ground these concepts, consider the development and validation of "GynoSight v2.0," a portable multispectral transvaginal imaging probe designed for the early detection of precancerous cervical lesions [87]. This case study exemplifies a direct bridge between technical innovation and clinical validation.
Experimental Protocol for Probe Validation
The clinical validation of GynoSight v2.0 involved a direct comparison against a standard colposcope, with a focus on quantitative, objective metrics [87].
- Objective: To compare the illumination performance (shadowing effect) and analytical capability of GynoSight v2.0 against a standard colposcope.
- Patient Cohort: Imaging was performed on a cohort of patients, with the same cervical areas imaged by both devices.
- Primary Quantitative Endpoints:
- Mean Pixel Intensity (MPI): The average intensity of all pixels, where a higher value indicates better overall illumination [87].
- Shadow Area Percentage (SAP): The percentage of image pixels below a set intensity threshold, quantifying the proportion of the image obscured by shadow [87]. A lower SAP is superior.
- Entropy: A measure of randomness and texture in the image; can be affected by uneven illumination [87].
- Contrast-to-Noise Ratio (CNR): The ability to distinguish a region of interest from the background [87].
- Relative Oxygen Saturation (OS) Mapping: A key biomarker for cancer, calculated from multispectral images using a Discrete Fourier Transform-based registration technique [87].
- Results: The study found that GynoSight v2.0 images demonstrated less shadowing (inferred from MPI and SAP metrics) and provided better illumination than traditional colposcopy, thereby aiding in more reliable diagnosis. Furthermore, its ability to generate relative OS maps provided a functional biomarker not available with standard imaging [87].
Diagram 1: Probe validation workflow.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key components used in the development and validation of advanced bio-optical devices like GynoSight v2.0, illustrating the bridge between engineering and clinical application [87].
Table 3: Essential Research Toolkit for Bio-Optical Diagnostic Development
| Item / Reagent | Technical Function | Clinical / Research Relevance |
|---|---|---|
| Multispectral LEDs (e.g., 450nm, 545nm, 610nm, White) | Provides illumination at specific wavelengths to probe different tissue properties (e.g., hemoglobin absorption). | Enables the calculation of functional biomarkers, such as relative oxygen saturation, which is altered in cancerous tissues due to increased vascularity [87]. |
| Raspberry Pi 5 Module | A single-board computer serving as the central control unit for image capture, processing, and display. | Facilitates the creation of a portable, cost-effective, and standalone imaging system, crucial for deployment in resource-constrained settings [87]. |
| Biocompatible Probe Sleeve (e.g., MED-WHT 10) | A disposable, medical-grade sheath that covers the probe tip. | Ensures patient safety by preventing contamination and enabling sterilization between uses, a mandatory requirement for clinical translation [87]. |
| 5-Megapixel Camera Module | Captures high-resolution images of the cervix through the central aperture of the probe. | Provides the raw data necessary for detailed visual inspection and computational analysis. Higher resolution can improve the detection of subtle morphological changes [87]. |
| Discrete Fourier Transform (DFT) Registration Algorithm | A computational method to align multispectral images that may have shifted due to motion between exposures. | Critical for accurate biomarker calculation. Misaligned images lead to erroneous oxygen saturation values, compromising clinical validity [87]. |
A Framework for Continuous Clinical Validation
Validation is not a one-time event but a continuous process throughout the AI model lifecycle. Deployed models are susceptible to model drift (where the model's performance degrades over time) and data drift (where the statistical properties of the input data change), necessitating ongoing monitoring [89]. Establishing a MLOps pipeline with continuous validation protocols—including automated performance dashboards, drift detection algorithms, and scheduled re-validation with new clinical data—is essential for maintaining model efficacy and safety in a real-world clinical environment [89].
Diagram 2: Continuous validation lifecycle.
Bridging the technical-clinical divide in AI validation is a rigorous, multi-stage process that demands more than just algorithmic excellence. It requires a holistic framework encompassing robust experimental design, the selection of clinically meaningful metrics, transparent comparison methodologies, and a commitment to continuous monitoring. By adhering to structured validation guides—such as the TRIPOD+AI statement for reporting [88] or employing specialized validation platforms [89]—researchers and drug developers can ensure that their innovative bio-optical cancer diagnostics are not only technically sophisticated but also reliable, equitable, and ultimately, capable of improving patient outcomes. The future of cancer diagnostics lies in the seamless integration of advanced optics and AI, grounded in uncompromising clinical validation.
Strategic Use of Biobanks vs. Prospective Trials for Efficient Evidence Generation
In the field of bio-optical cancer diagnostics, generating robust clinical evidence is paramount for regulatory approval and clinical adoption. The strategic choice between utilizing existing biobanks and conducting prospective clinical trials represents a critical juncture in the development pathway. This guide provides an objective comparison of these two approaches, detailing their respective advantages, limitations, and optimal applications to help researchers and drug development professionals efficiently build compelling evidence for their diagnostic technologies.
Biobanks are organized collections of biological samples and associated data stored for research purposes [90]. They provide access to diverse, annotated biospecimens crucial for early-stage assay development. In contrast, prospective trials involve the active collection of samples and data according to a specific research protocol, typically from participants recruited for the study [91]. For oncology diagnostics, particularly those leveraging bio-optical technologies, the decision between these paths is not merely methodological but strategic, impacting development timelines, costs, and the ultimate credibility of the evidence generated [92].
The emergence of rigorous regulatory standards, including the FDA's Final Rule on Laboratory Developed Tests (LVDs) and the EU's In Vitro Diagnostic Regulation (IVDR), has increased the evidence burden for diagnostic developers [92]. Simultaneously, payers increasingly demand proof of real-world clinical utility—evidence that a test meaningfully impacts patient management or outcomes [92]. Understanding how biobanks and prospective trials contribute to meeting these demands is essential for efficient diagnostic development.
Strategic Comparison: Biobanks vs. Prospective Trials
The following table summarizes the core characteristics of each approach, highlighting their strategic profiles for evidence generation in cancer diagnostics.
Table 1: Strategic Comparison of Biobanks and Prospective Trials
| Feature | Biobanks | Prospective Trials |
|---|---|---|
| Primary Purpose | Accelerate early development, biomarker discovery, and feasibility testing [92] | Generate pivotal evidence for regulatory approval and clinical utility [92] |
| Typical Study Designs | Retrospective case-control; cross-sectional [92] | Prospective cohort; interventional; pragmatic trials [93] [94] |
| Sample Quality & Control | Variable; depends on historical collection and storage protocols [91] | High; controlled collection conditions under standardized protocols [91] |
| Clinical Context of Data | Often limited; may lack full longitudinal outcomes [92] | High; rich, protocol-specified clinical data with follow-up [92] |
| Time Requirements | Rapid access to samples [92] [91] | Lengthy process due to recruitment and follow-up [92] [91] |
| Cost Implications | Cost-effective for early-stage work [92] [91] | High upfront investment [92] [91] |
| Ideal Use Cases | Analytical validation, signal detection, rare cancer feasibility [92] | Pivotal clinical validation, demonstration of clinical utility [92] |
Advantages and Limitations in Practice
Biobanks offer significant advantages in accessibility and speed. Researchers can rapidly obtain samples representing diverse cancers, including rare types that would be difficult to collect prospectively [92]. This is invaluable for analytical validation and early biomarker discovery. However, a key limitation is spectrum bias. For instance, biobanks often underrepresent early-stage (Stage I/II) or asymptomatic cancers, which are critical for validating early detection assays [92]. Furthermore, pre-analytical variability in sample handling and storage can introduce artifacts, particularly sensitive for bio-optical analyses [92].
Prospective trials, while resource-intensive, generate evidence that is inherently more robust for regulatory and payer submissions. They demonstrate how a test performs in its intended-use population and setting, providing data on real-world usability and clinical impact [92]. The PATHFINDER 2 study for GRAIL's Galleri test is a prime example. This large, prospective study demonstrated the test's ability to increase cancer detection more than seven-fold when added to standard screenings, with a promising positive predictive value of 61.6% [93].
Performance Data from Key Studies
Recent landmark studies highlight the type of performance data generated by both approaches and their role in the evidence hierarchy.
Table 2: Performance Data from Recent Oncology Diagnostic Studies
| Study (Test) | Design | Key Performance Metrics | Role in Evidence Generation |
|---|---|---|---|
| ALTUS (OncoGuard Liver) | Prospective, head-to-head trial vs. ultrasound [95] | Early-stage HCC sensitivity: 77% (Test) vs. 36% (Ultrasound); Specificity: 82% [95] | Pivotal validation for regulatory submission; demonstrated superior clinical performance versus standard of care. |
| PATHFINDER 2 (Galleri MCED) | Prospective, interventional study [93] | Cancer Signal Detection Rate: 0.93%; Positive Predictive Value: 61.6%; Specificity: 99.6% [93] | Registrational study to support premarket approval; assessed clinical use and diagnostic pathways. |
| UK Biobank Research | Retrospective analysis of a large population cohort [96] | Used to develop/validate risk models; revealed a 10% lower overall cancer incidence in biobank vs. general population, indicating "healthy volunteer" bias [96] | Model development and calibration; revealed inherent selection biases that must be accounted for in retrospective validations. |
| Freenome Hybrid Strategy | Hybrid (Biobank + Prospective) [92] | Biobank: >80% sensitivity in feasibility; Prospective (PREEMPT CRC): 79.2% sensitivity at 91.5% specificity for regulatory submission [92] | Exemplifies using biobanks for early feasibility and prospectives for pivotal validation in a complementary strategy. |
Experimental Protocols for Diagnostic Validation
The journey from assay development to validated diagnostic requires a sequence of structured experiments. The methodologies below are adapted from successful studies of blood-based tests.
Protocol 1: Retrospective Biobank Study for Assay Feasibility
This protocol is designed for initial analytical and clinical feasibility testing using banked samples.
- Objective: To assess the initial clinical performance (sensitivity/specificity) of a bio-optical assay for detecting a specific cancer signal against a control group.
- Sample Selection:
- Case Group: Select banked samples (e.g., plasma) from patients with a confirmed diagnosis of the target cancer(s). Annotation should include cancer type, stage, histology, and age.
- Control Group: Select banked samples from individuals without a cancer diagnosis (healthy controls) or those with non-malignant conditions (disease controls), matched for factors like age and sex.
- Source: Biobanks like TCGA, BBMRI-ERIC, or UK Biobank, which offer annotated samples [92] [97].
- Blinding: Samples should be de-identified and randomized before analysis. The analytical team should be blinded to the case/control status.
- Bio-optical Analysis: Process samples using the standardized diagnostic assay protocol. This may involve isolating optical signals (e.g., from fluorescently labeled biomarkers) and analyzing them with a predefined algorithm.
- Data Analysis: Compare the assay's output (e.g., positive/negative signal) against the ground truth diagnosis to calculate sensitivity, specificity, and area under the curve (AUC).
Protocol 2: Prospective Trial for Pivotal Clinical Validation
This protocol outlines a prospective study design suitable for regulatory submissions.
- Objective: To validate the clinical performance and utility of the diagnostic test in an intended-use population.
- Study Population: Recruit participants based on the test's intended use (e.g., asymptomatic individuals aged 50+ for an early detection test) [93] [94]. Obtain informed consent.
- Sample Collection & Processing: Collect fresh biospecimens (e.g., blood draws) from all participants at baseline using a standardized, validated kit and protocol to minimize pre-analytical variability [92].
- Reference Standard & Follow-up: Participants with a positive test result undergo a predefined diagnostic workup based on the test's "cancer signal origin" prediction [93]. All participants are followed for a set period (e.g., 12 months) via cancer registries or medical records to identify interval cancers in test-negative individuals [93].
- Outcome Measures:
- Primary Endpoints: Sensitivity (overall and by stage), specificity, and Positive Predictive Value (PPV).
- Secondary Endpoints: Accuracy of cancer signal origin prediction, time to diagnostic resolution, and types of procedures required for workup [93].
Workflow and Decision Pathway
The following diagram illustrates the strategic decision-making process for integrating biobanks and prospective trials into an efficient evidence generation pathway.
Strategic Evidence Generation Pathway
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of the experimental protocols requires a suite of reliable reagents and tools. The following table details essential components for bio-optical cancer diagnostic research.
Table 3: Key Research Reagent Solutions for Diagnostic Validation
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Matched FFPE Tissue & Plasma Sets | Validate liquid biopsy performance against traditional histopathology as a ground truth [92]. | Critical for concordance studies; available from biobanks like BBMRI-ERIC and NCI [92]. |
| Cell-Free DNA (cfDNA) Preservation Tubes | Stabilize nucleated blood cells immediately after draw to prevent genomic DNA contamination and preserve cfDNA profile [95]. | Essential for prospective trials to ensure pre-analytical consistency for liquid biopsy and optical analysis. |
| Target-Specific Bio-optical Probes | Bind to target biomarkers (e.g., methylated DNA, proteins) to generate a measurable optical signal [95]. | The core reagent of the test; requires high specificity and affinity to minimize background noise. |
| PCR Master Mixes & Reagents | Amplify target genomic regions for detection, as used in Exact Sciences' proprietary PCR technology [95]. | Must be optimized for multiplexing and work with bisulfite-converted DNA for methylation-based assays. |
| Automated Nucleic Acid Extraction Systems | Isulate high-purity, consistent yields of cfDNA from plasma samples [98]. | Automation reduces human error and increases throughput for large-scale studies. |
| Barcoded Sample Storage Tubes | Enable secure, traceable long-term sample storage at ultra-low temperatures [98]. | Integral to biobank and trial sample management; links physical sample to digital clinical data. |
| Multi-omic Assay Kits | Allow for simultaneous analysis of different analyte classes (e.g., DNA methylation, protein markers) from a single sample [95] [93]. | Key for developing high-sensitivity, multi-analyte tests like Galleri and OncoGuard Liver. |
The strategic use of biobanks and prospective trials is not an "either/or" decision but a "both/and" progression in the development lifecycle of bio-optical cancer diagnostics. Biobanks provide the foundational evidence needed for rapid, cost-effective assay refinement and feasibility testing, while prospective trials deliver the definitive evidence of clinical validity and utility required by regulators, payers, and clinicians.
The most successful diagnostic developers, as exemplified by companies like Freenome and Exact Sciences, adopt a hybrid development model [92] [95]. They leverage biobanks to de-risk early development and then commit to the necessary investment in prospective trials to generate high-quality, real-world data. This balanced approach efficiently accelerates innovation while ultimately ensuring that new diagnostics meet the high evidence standards necessary to achieve commercial success and, most importantly, improve patient outcomes in oncology.
Demonstrating Clinical Utility: Comparative Performance and Regulatory Pathways
The genetic characterization of cancers, particularly hematologic malignancies, is fundamental to accurate diagnosis, risk stratification, and therapeutic decision-making [99] [3]. For decades, the standard-of-care (SoC) cytogenetic workflow has relied on a multi-assay approach, primarily involving the combination of chromosome banding analysis (karyotyping), fluorescence in situ hybridization (FISH), and chromosomal microarray analysis (CMA) [100] [101]. While effective, this multi-modal approach is labor-intensive, time-consuming, and has inherent limitations in resolution and genome-wide scope [3] [100]. There is a growing need for more efficient and comprehensive technologies that can streamline diagnostic workflows while improving the detection of clinically significant genetic aberrations.
This guide objectively compares the performance of two newer genomic technologies—Optical Genome Mapping (OGM) and Targeted RNA Sequencing (RNA-Seq)—against traditional SoC methods and against each other. By examining recent head-to-head studies, we provide a data-driven resource to help researchers and clinicians understand the relative strengths and applications of these powerful tools in cytogenomic analysis.
To interpret comparative study data, it is essential to understand the fundamental principles and standard protocols for each technology.
Optical Genome Mapping (OGM)
- Principle: OGM utilizes ultra-high molecular weight (UHMW) DNA for the genome-wide detection of structural variants (SVs) and copy number variations (CNVs). It linearizes fluorescently labeled DNA molecules within nanochannels to image label patterns, which are then assembled and compared to a reference genome [3] [100].
- Standard Protocol (as cited):
- DNA Extraction: Fresh blood, bone marrow, or tissue samples are used to isolate UHMW DNA.
- Labeling: DNA is labeled with a proprietary enzyme (DLE-1) that targets a specific sequence motif (CTTAAG), creating a unique fluorescent barcode pattern.
- Imaging: Labeled DNA is linearized and imaged using the Saphyr instrument (Bionano Genomics).
- Data Analysis: Bioinformatic pipelines (Bionano Solve) assemble the data de novo and call SVs and CNVs by comparing the sample's label pattern to a reference genome (GRCh38) [99] [101]. Quality criteria often include a map rate >60% and effective genome coverage >300x [101].
Targeted RNA Sequencing (RNA-Seq)
- Principle: This method uses next-generation sequencing (NGS) to detect gene fusions and chimeric transcripts from expressed RNA. Targeted panels use gene-specific primers to enrich for sequences of clinical interest.
- Standard Protocol (as cited):
- RNA Extraction: RNA is isolated from peripheral blood or bone marrow aspirates.
- Library Preparation: The Archer FusionPlex or similar anchored multiplex PCR (AMP) chemistry is used for target enrichment. This method uses gene-specific primers to capture known and novel fusion partners.
- Sequencing: Amplified libraries are sequenced on an Illumina platform.
- Data Analysis: Sequencing reads are aligned to a reference genome (GRCh37/hg19), and fusion transcripts are identified using specialized software (e.g., Archer Analysis) [99].
Standard-of-Care (SoC) Methods
- Karyotyping: The microscopic analysis of G-banded chromosomes from metaphase cells, capable of detecting genome-wide numerical and large structural abnormalities (>5-10 Mb) but requires cell culture [100].
- FISH: A targeted molecular cytogenetic technique that uses fluorescent probes to detect specific genetic aberrations, such as gene rearrangements or aneuploidy, without the need for cell culture [100].
- CMA: A microarray-based technique that provides genome-wide detection of CNVs and copy-neutral loss of heterozygosity (CN-LOH) but cannot detect balanced SVs [102] [100].
The following diagram illustrates the foundational workflow for OGM, one of the key emerging technologies discussed.
Diagram 1: Optical Genome Mapping (OGM) Workflow. The process begins with the extraction of Ultra-High Molecular Weight (UHMW) DNA, which is fluorescently labeled at specific sequence motifs, linearized, and imaged to generate a genome-wide map of label patterns for structural variant and copy number variant analysis [3] [100].
Head-to-Head Performance in Acute Leukemia
A landmark 2025 study directly compared a 108-gene targeted RNA-Seq panel and OGM in 467 acute leukemia cases, providing robust, quantitative data on their performance [99].
The study found that OGM and/or RNA-Seq revealed at least one gene rearrangement or fusion in 43.6% of cases (206/467). A Tier 1 aberration (clinically relevant for diagnosis, prognosis, or therapy) was observed in 31.5% of cases (147/467) [99].
Overall Concordance: Among the 234 gene/rearrangement fusions detected, the two methods were concordant for 175 (74.7%). However, concordance varied significantly by leukemia subtype, as detailed below [99].
Table 1: Concordance and Unique Detection Rates of OGM and RNA-Seq in 467 Acute Leukemia Cases [99]
| Leukemia Type | Number of Cases | Concordance Rate | Uniquely Detected by OGM | Uniquely Detected by RNA-Seq |
|---|---|---|---|---|
| B-ALL | 89 | 80.2% | Information Not Specified | Information Not Specified |
| AML | 360 | Information Not Specified | Information Not Specified | Information Not Specified |
| T-ALL | 12 | 41.7% | Information Not Specified | Information Not Specified |
| All Types (Aggregate) | 467 | 74.7% | 37/234 (15.8%) | 22/234 (9.4%) |
Technology-Specific Strengths and Weaknesses
The study provided clear evidence of the complementary nature of these technologies, with each excelling in different areas [99].
- OGM Superiority in Enhancer-Hijacking Events: OGM was particularly effective at detecting enhancer-hijacking lesions (e.g., involving MECOM, BCL11B, and IGH genes), which often do not produce fusion transcripts. The concordance for these specific events was markedly low at 20.6%, as many were missed by RNA-Seq [99].
- RNA-Seq Superiority in Fusion Transcript Detection: Conversely, targeted RNA-Seq slightly outperformed OGM for detecting some fusions arising from intrachromosomal deletions. In these cases, OGM sometimes labeled the event as a simple deletion rather than a rearrangement leading to a fusion [99].
OGM vs. Standard-of-Care in Pediatric ALL
A 2025 study of 60 pediatric ALL (pALL) patients benchmarked OGM against SoC methods (karyotyping and FISH), providing further insight into the limitations of traditional workflows [101].
Diagnostic Yield and Resolution
The study demonstrated OGM's superior resolution and diagnostic capabilities as a standalone test [101].
- OGM detected a higher percentage of chromosomal gains and losses (51.7% vs. 35% with SoC).
- OGM was significantly better at identifying gene fusions (56.7% vs. 30% with SoC, p = 0.0057).
- Crucially, OGM was able to resolve 15% of cases that were non-informative with SoC techniques [101].
Comprehensive Workflow Analysis
The study concluded that combining dMLPA and RNA-seq was the most effective approach, achieving precise classification in 95% of cases. However, OGM as a standalone test identified clinically relevant alterations in 90% of cases, a substantial improvement over the 46.7% achieved by SoC techniques alone [101]. This highlights the limitation of traditional methods and the value of comprehensive genomic approaches.
Table 2: Comparison of Genomic Analysis Techniques [99] [3] [100]
| Feature | Karyotyping | FISH | CMA | OGM | Targeted RNA-Seq |
|---|---|---|---|---|---|
| Genome-Wide Coverage | Yes | No (Targeted) | Yes | Yes | Targeted (Gene Panel) |
| Resolution | 5-10 Mb | ~100 kb | 25-40 kb | 500 bp - 70 kb* | Single Nucleotide |
| Detects Balanced SVs | Yes (Large) | Yes (Targeted) | No | Yes | Yes (as transcripts) |
| Detects CNVs | Yes (Large) | Yes (Targeted) | Yes | Yes | Indirectly |
| Detects Gene Fusions | Indirectly | Yes (Targeted) | No | Yes (DNA level) | Yes (RNA level) |
| Cell Culture Required | Yes | No | No | No | No |
| Key Strength | Single-cell context, ploidy | High sensitivity for targeted aberrations | Gold standard for CNVs | Comprehensive SV/CNV detection | Direct fusion transcript identification |
*Resolution depends on variant type and analysis pipeline [3].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these technologies relies on a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for Cytogenomic Analysis
| Reagent / Solution | Function | Example Use Case |
|---|---|---|
| Ultra-High Molecular Weight (UHMW) DNA Kits | Isolation of long, intact DNA strands essential for OGM analysis. | Bionano Prep SP Blood & Cell Culture DNA Isolation Kit for generating high-quality DNA from patient samples [100]. |
| DLE-1 Labeling Enzyme | Fluorescently labels specific DNA sequence motifs (CTTAAG) for OGM. | Bionano Prep DLS Labeling Kit used to create the unique fluorescent barcode pattern for DNA molecule imaging [100] [101]. |
| Anchored Multiplex PCR (AMP) Kits | Target enrichment for RNA-Seq to detect known and novel fusion partners. | Archer FusionPlex kits used in the 108-gene panel study to prepare libraries for sequencing [99]. |
| Stranded Total RNA Library Prep Kits | Preparation of sequencing libraries for whole-transcriptome or RNA-Seq analysis. | Illumina TruSeq Stranded Total RNA Kit used in pALL study to convert RNA into sequencer-ready form [101]. |
| Bioinformatic Analysis Suites | Software for alignment, variant calling, and interpretation of NGS and OGM data. | Bionano Access/Solve for OGM [99] [101]; Archer Analysis for fusion detection [99]; Ion Reporter for t-NGS [101]. |
Consensus Recommendations and Clinical Validation
The growing body of evidence has led to formal recommendations from expert consortia. The International Consortium for Optical Genome Mapping (ICOGM) published recommendations in 2025, stating that OGM is recommended as a first-line cytogenetic tool in place of conventional karyotyping and FISH for several hematologic malignancies, including AML, MDS, B-ALL, T-ALL, and pediatric leukemias [103]. This recommendation is driven by OGM's ability to identify cryptic fusions, avoid the need for large FISH panels, and provide unbiased detection for improved risk stratification [103].
Furthermore, a 2022 clinical validation study of OGM for hematological neoplasms demonstrated robust performance, with an analytical sensitivity of 98.7%, specificity of 100%, and accuracy of 99.2%, determining a limit of detection at a 5% allele fraction [104]. This level of analytical validation provides confidence in the reliability of OGM data for both research and clinical applications.
The head-to-head evidence clearly demonstrates that newer genomic technologies are overcoming the significant limitations of traditional cytogenetic methods.
- OGM provides a comprehensive, genome-wide view of structural variations, excelling where SoC methods fail, particularly in detecting cryptic rearrangements and complex karyotypes with a single, unified assay [99] [101] [103].
- Targeted RNA-Seq remains the superior method for the definitive identification of expressed gene fusion transcripts, especially those arising from complex intrachromosomal rearrangements [99].
Rather than being mutually exclusive, OGM and targeted RNA-Seq are highly complementary. The most comprehensive cytogenomic analysis for complex diseases like acute leukemia is achieved through their synergistic use. This multi-technology approach provides a more complete molecular picture, ultimately enhancing diagnosis, risk stratification, and informing targeted treatment decisions for patients [99]. As the field moves forward, integrating these technologies into streamlined diagnostic workflows represents the new frontier in precision oncology.
The field of cancer diagnostics is increasingly moving toward integrated bio-optical testing platforms that combine multiple optical sensing modalities to provide comprehensive metabolic and vascular characterization of tumors. These systems represent a significant advancement over single-modality tools by enabling simultaneous quantification of multiple metabolic parameters, vascular oxygenation, and tumor microenvironment dynamics in vivo. The clinical validation of these platforms rests on their demonstrated ability to capture highly diverse metabolic phenotypes in cancer models, providing a systems-level view of cell metabolism that is essential for understanding critical biomedical problems [105]. The value proposition of these integrated systems extends beyond improved diagnostic accuracy to encompass significant gains in workflow efficiency and cost-effectiveness, particularly through their point-of-care, easy-to-use design philosophy that enables rapid characterizations of biological tissue metabolism without requiring specialized sample preparation or complex operational expertise [105].
Integrated bio-optical tests fill a crucial technological gap in cancer research and clinical oncology by enabling the quantification of glycolysis, mitochondrial function, and vascular microenvironment together in vivo—a capability that remains challenging with conventional tools like Seahorse assays, metabolomics, immunohistochemistry, PET, or MRSI, each of which has practical and scientific limitations [105]. The portability and cost-effectiveness of these platforms further maximize access to biomedical research across laboratories, breaking the limitations of conventional equipment that is typically housed in core facilities, requires transporting samples to designated locations, and demands significant operational expertise [105]. This review provides a comprehensive comparison of integrated bio-optical testing platforms, focusing on their cost and workflow efficiency advantages through directly comparable experimental data and standardized performance metrics relevant to researchers, scientists, and drug development professionals.
Comparative Performance Analysis of Bio-Optical Platforms
Technical Performance Metrics
Integrated bio-optical systems demonstrate variable performance across critical technical parameters that directly impact their research utility and application suitability. The comparative data below, compiled from recent peer-reviewed studies and technology validations, highlights key metrics for platform evaluation.
Table 1: Comparative Technical Performance of Bio-Optical Platforms
| Platform/Technology | Key Measured Parameters | Spatial Resolution | Temporal Resolution | Target Applications | Validation Status |
|---|---|---|---|---|---|
| PEERS Optical Spectroscopy [105] | Tissue vascular saturation (StO₂), total hemoglobin concentration [THB], glucose uptake (via 2-NBDG), mitochondrial membrane potential (via TMRE) | Fiber probe with source-detector distances: 1.5mm (Channel 1), 3.0mm (Channel 2) | Rapid, point-of-care measurements | In vivo metabolic characterizations of head and neck tumors with different radiation sensitivities | Validated on tissue-mimicking phantoms, human subjects, and in vivo animal models |
| Multisensor Optical System [106] | Functional states of microcirculatory tissue systems using 18 photodiode-sensitive elements | Array of 18 photodiodes with selective sensitivity | Multidimensional data mining techniques | Identification and analysis of functional states of complex multicomponent biological tissues and fluids | Experimental studies with human participants |
| Portable Optical Biosensors [107] | Various cancer biomarkers via surface plasmon resonance (SPR), fluorescence, interferometry | Varies by specific technology (nanomaterial-based) | Real-time monitoring capabilities | Point-of-care cancer biomarker detection | Research stage with advancements in sensitivity and specificity |
| OCT Angiography (OCTA) [108] | Microvascular pathologies, capillary dropout, neovascularization | Capillary-level resolution | Functional vascular imaging added to structural OCT | Diabetic retinopathy, age-related macular degeneration, glaucoma | Clinical use with quantitative features serving as biomarkers |
Cost and Workflow Efficiency Metrics
Workflow efficiency and operational economics present compelling value propositions for integrated bio-optical platforms, particularly when compared to established diagnostic technologies and centralized testing approaches.
Table 2: Workflow Efficiency and Economic Comparison
| Parameter | Integrated Bio-Optical Platforms | Conventional Tools (IHC, PET, MRSI) | Liquid Biopsy Assays |
|---|---|---|---|
| Equipment Cost Footprint | Low-cost footprint designed for accessibility [105] | High capital investment, core facility requirements [105] | Variable (moderate to high) |
| Operational Requirements | Easy-to-use, minimal sample preparation, no transport needed [105] | Specialized sample preparation, expertise-dependent, transport to designated locations [105] | Specialized laboratory processing required |
| Measurement Speed | Rapid, point-of-care measurements [105] | Time-consuming procedures [105] | Moderate (includes processing time) |
| Multiplexing Capability | Simultaneous quantification of multiple metabolic and vascular parameters [105] | Typically single-parameter or sequential measurements | Multi-analyte detection possible |
| Regulatory Status | Research use, validation in progress [105] | Clinically established with regulatory approvals | Increasing FDA approvals (e.g., Roche Elecsys pTau181) [109] |
| Personnel Expertise Required | Easy-to-use algorithms reduce expertise dependency [105] | Expertise-dependent with complicated data processing [105] | Specialized technical expertise |
Experimental Protocols and Methodologies
The PEERS Optical Spectroscopy Platform Protocol
The Portable, Easy-to-use, Easy-to-access, Rapid, Systematic (PEERS) optical spectroscopy platform represents a seminal implementation of integrated bio-optical testing with robust clinical validation. The experimental methodology encompasses the following standardized protocol [105]:
System Configuration: The platform incorporates a high-power white LED source with 450-nm and 550-nm bandpass filters for fluorescence excitation of 2-NBDG (glucose uptake probe) and TMRE (mitochondrial membrane potential probe) respectively. A neutral density filter protects the spectrometer during diffuse reflectance measurements. The custom-designed fiber optics probe features two groups of source-detector distances (1.5mm and 3.0mm) to enable tumor-sensitive metabolic characterizations [105].
Measurement Procedure: The platform performs sequential measurements through an optical switch that directs signals from two collection channels to a compact spectrometer. For fluorescence measurements, long-pass filters (515nm for 2-NBDG, 575nm for TMRE) remove excitation light, while no filter is used for diffuse reflectance collection. The entire integrated system is packaged into a small cart for point-of-care measurements [105].
Data Processing Algorithms: The platform employs both Monte Carlo inversion models and novel ratio-metric analytical methods for spectral data processing. The diffuse reflectance MC inversion model fits measured spectra to simulated spectra until sum of squares error is minimized, while fluorescence MC inversion extracts intrinsic fluorescence using absorption and scattering information from reflectance data. For rapid quantification, ratio-metric methods using specific wavelength ratios (e.g., 584nm/545nm for [THB]) provide simplified analytical approaches [105].
Validation Methods: Platform validation follows a rigorous three-stage process: (1) tissue-mimicking phantom studies to establish baseline accuracy, (2) human subject pilot tests for clinical feasibility, and (3) in vivo animal studies capturing diverse metabolic phenotypes of head and neck tumors with different radiation sensitivities [105].
Multisensor Optical System with Data Mining Protocol
An alternative integrated approach employs multisensor optical systems combined with advanced data mining techniques for biomedical diagnostics [106]:
System Architecture: This methodology utilizes a compact optical multisensor system featuring an array of 18 photodiode-sensitive elements with selective sensitivity to optical radiation across visible and infrared ranges (410-940nm). This multi-wavelength approach enables comprehensive tissue characterization [106].
Data Processing Methodology: The system applies multidimensional data mining techniques, specifically principal component analysis and cluster analysis algorithms, to process optical signals and identify hidden patterns in functional states of microcirculatory tissue systems. This approach enables ranking of optical spectroscopy signals based on multiple parameters simultaneously [106].
Application Workflow: The methodology involves: (1) multisensor data acquisition across multiple wavelengths, (2) preprocessing of large volumes of optical signals using data mining techniques, (3) multidimensional analysis to extract features characterizing biological tissue states, and (4) visualization of ranked subject data to reveal hidden patterns in tissue functional states [106].
Visualizing Integrated Bio-Optical Testing Workflows
Optical Sensing Principle and Metabolic Parameter Quantification
Integrated Experimental and Data Processing Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Integrated bio-optical testing requires specialized reagents and materials that enable precise metabolic and vascular measurements. The following table details essential research reagent solutions for implementing these platforms in cancer research and drug development contexts.
Table 3: Essential Research Reagent Solutions for Bio-Optical Cancer Diagnostics
| Reagent/Material | Function | Application Context | Key Characteristics |
|---|---|---|---|
| 2-NBDG (2-[N-(7-nitrobenz-2-oxa-1,3-diazol-4-yl)amino]-2-deoxy-d-glucose) | Fluorescent glucose analog for quantifying glycolysis via glucose uptake [105] | In vivo measurement of tissue glycolysis in animal models | Measures glucose uptake analogous to clinically accepted FDG-PET imaging [105] |
| TMRE (Tetramethylrhodamine ethyl ester) | Mitochondrial membrane potential probe for studying OXPHOS [105] | In vivo quantification of mitochondrial function | Utilized extensively to measure MMP to study oxidative phosphorylation [105] |
| Noble Metal Nanoparticles (Gold/Silver) | Enhance sensitivity in surface plasmon resonance (SPR) sensors [107] | Label-free detection of nucleic acids, proteins, and carbohydrates | Functionalized plasmonic nanomaterials enable ultra-sensitive detection of specific bioanalytes [107] |
| Quantum Dots & 2D Nanomaterials | Fluorescence-based sensors with high sensitivity and multiplexing capabilities [107] | Detection of various cancer biomarkers | Offer high sensitivity and multiplexing capabilities in fluorescence-based sensors [107] |
| Photonic Crystals | Create sensitive and selective optical biosensors by manipulating light at nanoscale [107] | Development of advanced optical biosensors | Manipulate and control light at the nanoscale to create sensitive and selective optical biosensors [107] |
| Optical Fiber Probes | Light delivery and collection for spectroscopic measurements [105] | In vivo measurements on biological tissues | Custom-designed with specific source-detector distances (e.g., 1.5mm, 3.0mm) for tumor-sensitive characterizations [105] |
| Microfluidic Platforms | Ensure biocompatibility and precise microfabrication for biosensors [107] | Point-of-care diagnostic devices | Ensure biocompatibility and precise microfabrication in biosensor development [107] |
Integrated bio-optical testing platforms represent a transformative approach in cancer diagnostics, offering compelling value through enhanced workflow efficiency and cost-effectiveness without compromising analytical performance. The clinical validation of these systems, as demonstrated in studies capturing diverse metabolic phenotypes of head and neck tumors with different radiation sensitivities, establishes their robustness for research and potential clinical applications [105]. The integration of multiple optical sensing modalities within portable, easy-to-use platforms addresses critical limitations of conventional diagnostic tools while providing unprecedented insights into tumor metabolism and vascular microenvironment.
Future developments in this field will likely focus on several key areas: increased automation through AI integration, enhanced digital connectivity for seamless data integration into healthcare systems, further miniaturization of components, and expansion of multiplexing capabilities to simultaneously quantify additional biomarkers [105] [107]. The emerging trend toward combining optical biosensors with artificial intelligence for data analysis promises to further improve diagnostic precision and support personalized cancer treatment approaches [110]. Additionally, advancements in materials science, particularly in plasmonic nanomaterials, photonic crystals, and surface functionalization techniques, will continue to enhance the sensitivity and specificity of these platforms [107].
For researchers, scientists, and drug development professionals, integrated bio-optical tests offer a valuable toolset that balances technical sophistication with practical usability. As these technologies continue to evolve and undergo further clinical validation, they are poised to significantly impact cancer research workflows and potentially transform clinical diagnostic paradigms through their unique combination of comprehensive metabolic assessment, point-of-care operation, and cost-efficient implementation.
For developers of bio-optical cancer diagnostics, navigating the complex landscape of regulatory compliance and payer expectations represents a critical pathway to clinical adoption and commercial success. The regulatory frameworks of the U.S. Food and Drug Administration (FDA) and the European Union's In Vitro Diagnostic Regulation (IVDR) share the common goal of ensuring device safety and efficacy, yet they diverge significantly in their approaches, requirements, and evidentiary expectations [111] [112]. Simultaneously, payers are increasingly demanding robust clinical and economic validation to support coverage and reimbursement decisions. This guide provides a structured comparison of FDA and IVDR compliance pathways, with a specific focus on bio-optical cancer diagnostics, to help researchers and developers build comprehensive evidence generation strategies that satisfy both regulatory and payer requirements.
Regulatory Framework Comparison: FDA vs. IVDR
Classification Systems and Regulatory Pathways
The FDA and IVDR employ distinct risk-based classification systems that directly influence the regulatory pathway and evidence requirements for bio-optical cancer diagnostics [111] [112] [113].
Table 1: FDA and IVDR Classification Systems and Regulatory Pathways
| Aspect | U.S. FDA | EU IVDR |
|---|---|---|
| Classification System | Class I (low risk), Class II (moderate risk), Class III (high risk) [111] | Class A (lowest risk), B, C, D (highest risk) [111] [113] |
| Basis for Classification | Risk to patient and intended use [112] | Risk to public health and patient outcomes [113] |
| Notified Body Involvement | Not applicable | Required for most classes (80-90% of IVDs) [111] [112] |
| Premarket Pathways | 510(k), De Novo, PMA [114] | Technical documentation review by Notified Body [111] |
| Quality System Requirement | 21 CFR Part 820 (transitioning to alignment with ISO 13485 via QMSR) [115] [112] | ISO 13485:2016 (mandatory) [112] [116] |
The classification difference is particularly important for bio-optical cancer diagnostics, as many previously self-certified tests now require Notified Body involvement under IVDR [111]. Under FDA regulations, many cancer diagnostics would typically fall into Class II or III, while under IVDR, they often classify as Class C or D, requiring the highest level of scrutiny [111].
Clinical Evidence and Performance Evaluation Requirements
Both regulatory frameworks require demonstration of analytical and clinical performance, but with differing emphasis and structure throughout the device lifecycle [111] [112] [113].
Table 2: Comparison of Clinical Evidence Requirements
| Evidence Component | U.S. FDA | EU IVDR |
|---|---|---|
| Clinical Evidence Basis | Verification and validation studies to support safety and performance [111] | Performance Evaluation Reports (PERs) covering scientific validity, analytical and clinical performance [111] [117] |
| Evidence Continuity | Typically assessed during premarket review [112] | Ongoing requirement throughout product lifecycle [112] |
| Post-Market Evidence | Reactive system focusing on adverse events [111] | Structured Post-Market Performance Follow-up (PMPF) required [111] [113] |
| Reporting Format | No formal report structure specified [111] | Periodic Safety Update Reports (PSURs) for Class C & D devices [111] [113] |
For bio-optical cancer diagnostics, the IVDR's emphasis on continuous clinical evaluation and structured post-market surveillance represents a significant shift from the previous IVDD framework and differs from the FDA's more focused premarket approach [111] [112].
Analytical Performance Studies: Methodologies and Protocols
Core Analytical Parameters for Bio-optical Cancer Diagnostics
Robust analytical performance studies form the foundation for both FDA and IVDR submissions of bio-optical cancer diagnostics. The IVDR specifically requires demonstration of several key parameters, many of which align with FDA expectations [117].
Table 3: Essential Analytical Performance Parameters and Methodologies
| Parameter | Definition | Standard Methodology | Bio-optical Application |
|---|---|---|---|
| Analytical Sensitivity | Ability to detect the presence of a target marker [117] | Limit of Detection (LoD) studies using dilution series [117] | Determine minimum detectable analyte concentration using optical signals |
| Analytical Specificity | Ability to recognize only the target marker [117] | Interference testing with potentially cross-reactive substances [117] | Assess optical interference from sample matrix or similar biomarkers |
| Precision | Closeness of agreement between independent test results [117] | Repeatability and reproducibility studies across multiple lots, operators, and days [117] | Evaluate consistency of optical readouts across measurement conditions |
| Trueness | Agreement between average measurement value and accepted reference value [117] | Method comparison with reference standard [117] | Compare bio-optical measurements with gold standard pathological assessment |
| Measuring Range | Range where the IVD demonstrates suitable analytical performance [117] | Linearity studies across analyte concentrations [117] | Establish quantitative range for optical signal correlation with analyte concentration |
Experimental Protocol for Analytical Performance Studies
A comprehensive analytical validation protocol for bio-optical cancer diagnostics should incorporate the following elements, which satisfy both FDA and IVDR expectations when properly documented [117]:
Sample Preparation and Matrix Considerations:
- Use real-world clinical samples that represent the intended use population
- Evaluate matrix effects across different sample types relevant to the diagnostic's intended use
- Account for pre-analytical variables including sample collection, anticoagulants, and storage conditions
- Include contrived samples when rare biomarkers or specific concentrations are needed
Study Design and Statistical Analysis:
- Develop a statistical analysis plan before study initiation with pre-defined acceptance criteria
- Employ appropriate sample sizes to ensure adequate statistical power
- Use established guidelines (CLSI, ISO) to strengthen technical documentation
- Implement risk-based approaches to prioritize critical performance parameters
Reference Materials and Standards:
- Utilize internationally recognized reference materials when available
- Develop and validate in-house reference materials with thorough characterization for novel biomarkers
- Document rationale and approach for any homemade reference materials
Clinical Validation Frameworks for Bio-optical Cancer Diagnostics
Integrating Artificial Intelligence and Computational Pathology
Bio-optical cancer diagnostics increasingly incorporate artificial intelligence (AI) components, particularly for image analysis and pattern recognition in computational pathology. Both FDA and EU regulators have established specific frameworks for these technologies [34] [118].
For AI-based diagnostic tools, external validation using diverse, real-world datasets is crucial for demonstrating generalizability [86]. Recent studies of AI pathology models for lung cancer diagnosis reveal that performance can vary significantly when tested on external datasets, with common methodological challenges including:
- Small and/or non-representative datasets that don't reflect clinical population diversity
- Retrospective study designs that may not predict real-world performance
- Technical diversity limitations in imaging equipment, tissue processing protocols, and staining variations
The EU AI Act, which becomes mandatory in 2026, classifies AI components in medical devices as high-risk, requiring additional conformity assessment integrated with MDR/IVDR processes [115] [118].
Clinical Performance Study Design Considerations
Well-designed clinical performance studies for bio-optical cancer diagnostics should address several key considerations to satisfy both regulatory and payer requirements:
Patient Cohort Selection:
- Enroll participants representing the intended use population with appropriate demographic and clinical characteristics
- Include disease spectrum representation spanning the diagnostic's clinical application
- Consider multi-center recruitment to enhance generalizability
Reference Standard Implementation:
- Employ clinically accepted reference standards (e.g., histopathology, clinical follow-up)
- Ensure blinded assessment between index test and reference standard
- Document reference standard limitations and their potential impact on performance estimates
Outcome Measures and Endpoints:
- Define primary endpoints addressing both regulatory requirements and payer-relevant outcomes
- Include clinical utility measures beyond analytical accuracy (e.g., impact on treatment decisions, patient outcomes)
- Consider health economic endpoints relevant to payer coverage decisions
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Research Reagents and Materials for Bio-optical Cancer Diagnostic Development
| Reagent/Material | Function | Application in Bio-optical Diagnostics |
|---|---|---|
| Optical Contrast Agents | Enhance specific signal detection from target biomarkers [34] | Improve sensitivity for low-abundance cancer markers in optical imaging |
| Reference Standard Materials | Provide benchmark for analytical accuracy [117] | Establish trueness and calibration for quantitative optical measurements |
| Stable Control Materials | Monitor assay performance across multiple runs [117] | Quality control for optical platform consistency and reproducibility |
| Matrix Diversification Panels | Assess interference from sample variations [117] | Evaluate impact of different sample types on optical signal generation |
| Biomarker Reference Panels | Validate assay specificity and cross-reactivity [117] | Confirm optical assay specificity against related biomarkers and isoforms |
Strategic Implementation for Global Market Access
Integrated Quality Management Systems
Developing an integrated Quality Management System (QMS) that satisfies both FDA and IVDR requirements is essential for efficient global market access. Key considerations include:
- Align QMS with ISO 13485:2016 requirements, which is mandatory under IVDR and increasingly recognized by FDA through the Quality Management System Regulation (QMSR) [112] [116]
- Implement risk management processes according to ISO 14971:2019, which notified bodies consider state of the art despite not yet being harmonized [111]
- Establish performance evaluation procedures that address IVDR requirements for scientific validity, analytical performance, and clinical performance [116]
The deadline for implementing an IVDR-compliant QMS was May 26, 2025, for Class D devices, with staggered deadlines for other classes [116].
Post-Market Surveillance and Real-World Evidence Generation
Post-market evidence generation strategies should address both regulatory requirements and payer evidence needs:
IVDR-Specific Requirements:
- Implement Post-Market Performance Follow-up (PMPF) plans to proactively collect ongoing performance data [111]
- Prepare Periodic Safety Update Reports (PSURs) for Class C and D devices [111] [113]
- Utilize EUDAMED for regulatory reporting and device tracking [112]
Payer-Focused Evidence Generation:
- Collect real-world clinical utility data demonstrating impact on patient management and outcomes
- Generate health economic evidence supporting cost-effectiveness and resource utilization
- Document comparative effectiveness against existing diagnostic approaches
Successfully navigating both FDA and IVDR regulatory pathways while simultaneously addressing payer evidence requirements demands a strategically integrated approach from the earliest stages of bio-optical cancer diagnostic development. By understanding the distinct yet complementary requirements of these frameworks, researchers can design comprehensive development plans that efficiently generate evidence satisfying multiple stakeholders. The increasing harmonization in quality system requirements, combined with thoughtful planning of clinical validation studies, enables developers to accelerate global market access while building the robust evidence base needed for favorable coverage and reimbursement decisions.
Real-World Evidence and Prospective Clinical Trial Designs for Pivotal Validation
In the field of bio-optical cancer diagnostics, demonstrating conclusive clinical utility requires robust pivotal validation. Researchers and developers must navigate between traditional prospective clinical trials and the increasingly prominent real-world evidence (RWE). While prospective trials, particularly randomized controlled trials (RCTs), remain the recognized gold standard for establishing efficacy, RWE derived from real-world data (RWD) offers complementary insights into effectiveness in routine clinical practice [119]. This guide objectively compares these approaches, detailing their methodologies, applications, and synergistic potential to inform evidence generation strategies for novel diagnostic technologies.
Comparative Frameworks: RWE vs. Prospective Trials
The table below summarizes the core characteristics of these two validation paradigms.
Table 1: Core Characteristics of RWE and Prospective Clinical Trials
| Feature | Real-World Evidence (RWE) | Prospective Clinical Trials |
|---|---|---|
| Primary Objective | Describe effectiveness, safety, and clinical utility in heterogeneous, routine practice populations [119]. | Establish efficacy and safety under controlled, ideal conditions [119]. |
| Typical Design | Observational (e.g., cohort, case-control), analysis of pre-existing data [119]. | Experimental (e.g., randomized controlled trial), prospectively designed [119]. |
| Data Collection | Retrospective or prospective collection of routine clinical data (EHRs, registries, claims) [120]. | Prospective, protocol-driven collection with rigorous data verification [119]. |
| Patient Population | Broad and heterogeneous, reflecting clinical practice; includes underrepresented groups [119]. | Highly selected based on strict eligibility criteria; often excludes complex patients [119]. |
| Key Strength | Generalizability to real-world settings; efficiency for studying rare cancers or long-term outcomes [121] [119]. | High internal validity through controlled conditions and randomization to minimize bias [121]. |
| Key Limitation | Potential for confounding and bias due to lack of randomization [119] [122]. | Limited generalizability (external validity) due to selective patient populations [119]. |
The choice between these methodologies is not always mutually exclusive. A methods flowchart has been proposed to guide researchers from a well-defined scientific question to the most suitable analytical approach, considering multiple feasibility aspects related to comparative effectiveness research (CER) [121]. This tool aims to standardize methods and ensure rigorous, consistent research quality [121].
Methodological Deep Dive: Experimental Protocols
Protocol 1: Generating RWE from Integrated Clinicogenomic Data
This protocol, based on the MSK-CHORD study, details the creation of a high-quality RWD resource for cancer outcome prediction [120].
- Data Acquisition and Sourcing: Gather multimodal data from electronic health records (EHRs), including unstructured text (radiology/pathology reports, clinical notes), structured medication records, tumour registry data, demographic data, and genomic sequencing data [120].
- Natural Language Processing (NLP) Annotation:
- Model Training: Train and validate transformer-based NLP models using manually curated datasets (e.g., the Project GENIE BPC dataset) to annotate features from free-text reports [120].
- Key Annotations: Extract features such as cancer progression, tumour sites, prior outside treatment, and receptor status (e.g., HER2) from radiology reports and clinician notes [120].
- Validation: Validate model performance against manually curated labels using metrics like area under the curve (AUC), precision, and recall. Performance should exceed AUC >0.9 and precision/recall >0.78 [120].
- Data Integration and Harmonization: Combine NLP-derived features with structured treatment, survival, demographic, and genomic data to create a unified, clinicogenomic dataset (e.g., MSK-CHORD) [120].
- Outcome Prediction Modeling: Leverage the harmonized dataset to train machine learning models (e.g., for overall survival prediction). Models incorporating NLP-derived features, such as sites of disease, have been shown to outperform those based on genomic data or stage alone [120].
Protocol 2: Designing a Pivotal Prospective Clinical Trial
This protocol outlines the core design considerations for a prospective trial intended to serve as pivotal evidence for a bio-optical diagnostic.
- Define Primary Objective and Endpoints: Clearly state the primary objective (e.g., to demonstrate superior sensitivity and specificity of the new diagnostic versus a standard-of-care comparator). Define primary and secondary endpoints (e.g., accuracy metrics, safety, clinical utility outcomes).
- Select Study Population and Eligibility Criteria: Define the patient population with specific inclusion and exclusion criteria. While necessary for internal validity, carefully consider the trade-off with future generalizability [119].
- Choose Study Design:
- Randomized Controlled Trial (RCT): The gold standard for interventional studies. Patients are randomly assigned to diagnostic-guided strategies to eliminate confounding bias [121] [119].
- Single-Arm Trial: May be used when a RCT is not feasible, particularly in rare cancers. Outcomes are often compared to an external control from historical RWD [121]. Such externally controlled trials are recognized as a form of RWE generation [121].
- Blinding: Implement blinding where possible (e.g., pathologists interpreting outcomes should be blinded to the diagnostic arm assignment) to reduce assessment bias.
- Statistical Analysis Plan: Pre-specify the statistical analysis, including the primary analysis population (e.g., intention-to-diagnose), methods for calculating accuracy metrics with confidence intervals, and hypothesis testing framework.
Visualizing the Clinical Validation Pathway
The following diagram illustrates the complementary roles and integration points of RWE and prospective trials throughout the development lifecycle of a cancer diagnostic.
The Scientist's Toolkit: Key Research Reagents and Materials
Successfully executing the protocols above requires a suite of reliable data and analytical tools. The table below lists essential "research reagents" for this field.
Table 2: Essential Reagents and Tools for Diagnostic Validation Research
| Tool/Reagent | Primary Function | Application Examples |
|---|---|---|
| Structured Clinical Data | Provides baseline treatment, demographic, and outcome information. | Medication records, tumour registry data (e.g., cancer stage, histology) [120]. |
| Unstructured Clinical Text | Contains rich, detailed patient narratives and findings. | Radiology reports, pathology reports, clinician progress notes [120]. |
| Natural Language Processing (NLP) Models | Automates the extraction and structuring of information from clinical text. | Identifying sites of metastasis, cancer progression, or receptor status from reports [120]. |
| Tumour Genomic Data | Provides molecular characterization of cancers. | Targeted sequencing assays (e.g., MSK-IMPACT) to link genomic variants to outcomes [120]. |
| Harmonized Real-World Datasets | Pre-integrated, high-quality datasets for analysis. | Resources like MSK-CHORD, which combine clinical, genomic, and NLP-derived features [120]. |
| External Control Arms | Serves as a historical comparator for single-arm trials. | Real-world cohorts of patients receiving standard-of-care treatment [121]. |
The validation of bio-optical cancer diagnostics is strengthened by a strategic combination of prospective clinical trials and RWE. Prospective trials provide the high-integrity evidence of efficacy required for initial regulatory and HTA approvals [121] [119]. RWE, when generated with rigorous methodologies like automated NLP and data integration, extends this understanding by demonstrating real-world effectiveness, validating results in broader populations, and providing contextual control groups [120] [119]. Despite challenges, particularly regarding the inconsistent acceptability of RWE among HTA bodies [122], the synergistic use of both paradigms creates a comprehensive evidence package that accelerates the development and adoption of robust cancer diagnostics.
The field of oncology is witnessing a transformative convergence of diagnostic and therapeutic technologies. Bio-optics and radiopharmaceuticals represent two distinct yet increasingly complementary modalities advancing cancer care. Bio-optics utilizes light-based technologies for imaging, analysis, and manipulation of biological samples and systems, enabling non-invasive detection and monitoring of cancer [123]. Meanwhile, radiopharmaceutical therapy (RPT) has reemerged as a targeted anticancer approach that delivers radioactive isotopes directly to tumor cells, combining precision targeting with systemic treatment capabilities [124]. This guide objectively compares the performance characteristics, experimental methodologies, and clinical applications of these evolving technologies, providing researchers and drug development professionals with a comprehensive framework for understanding their respective positions in the oncology landscape.
The growing significance of both fields is reflected in their market trajectories and clinical adoption. The bio-optics market was valued at $2.03 billion in 2024 and is projected to reach $3.31 billion by 2032, demonstrating a compound annual growth rate of 6.3% [123]. Similarly, radiopharmaceuticals have gained substantial attention with US sales projected to reach $2 billion in 2025, driven by clinical successes such as Pluvicto ([177Lu]Lu-PSMA-617) for metastatic castration-resistant prostate cancer and Lutathera for neuroendocrine tumors [124]. This parallel growth underscores their expanding roles in precision oncology.
Technology Comparison: Fundamental Principles and Performance Characteristics
Bio-optics and radiopharmaceuticals operate on fundamentally different physical principles, leading to distinct performance characteristics and clinical applications. The following comparison outlines their core technological differences and performance metrics.
Table 1: Fundamental Technology Comparison Between Bio-Optics and Radiopharmaceuticals
| Characteristic | Bio-Optics | Radiopharmaceuticals |
|---|---|---|
| Physical Principle | Light-matter interaction (absorption, scattering, fluorescence) | Radioactive decay (α, β, γ, or conversion electron emission) |
| Primary Applications | Imaging, analysis, manipulation of biological samples | Targeted diagnosis and therapy of cancer |
| Spatial Resolution | Cellular to subcellular (μm scale) [125] | Tissue to organ level (mm scale) [126] |
| Penetration Depth | Limited (superficial tumors or endoscopic access) [127] | Whole-body systemic distribution [124] |
| Molecular Targeting | Indirect (biomechanical properties, spectral signatures) [125] | Direct (receptor-ligand binding, antigen-antibody) [128] |
| Quantitative Output | Biomechanical properties, chemical composition [125] | Target expression levels, radiation dose [129] |
| Therapeutic Capability | Limited (primarily diagnostic) [123] | High (direct tumor cell killing) [126] |
Bio-optics technologies encompass a diverse range of devices including optical coherence tomography (OCT), microscopy systems, spectroscopy devices, and optical biosensors [123]. These technologies excel in providing high-resolution morphological and functional information without ionizing radiation. Recent advancements in techniques like Brillouin microscopy enable non-contact, label-free assessment of the biomechanical properties of cells and tissues, which is significant as cancer mechanically alters its microenvironment [125]. This mechanobiological profiling capability provides a unique window into disease states that complements molecular information.
Radiopharmaceuticals consist of three key elements: a radioactive isotope, a targeting molecule (antibody, peptide, or small molecule), and often a chelator that links them [124]. They function through target-specific delivery of radiation, with different isotopes selected based on their emission properties. Beta-emitters like Lutetium-177 penetrate several millimeters, making them suitable for larger tumors, while alpha-emitters like Actinium-225 deliver high-energy radiation over very short distances (a few cell diameters), ideal for small clusters of cancer cells or micrometastases [124]. This precise targeting enables destruction of cancer cells while potentially sparing healthy tissues.
Table 2: Clinical and Research Application Profiles
| Application Domain | Bio-Optics | Radiopharmaceuticals |
|---|---|---|
| Early Cancer Detection | High potential (especially point-of-care) [123] | Limited (requires sufficient target expression) |
| Tumor Delineation | Excellent for superficial tumors [127] | Whole-body systemic assessment [126] |
| Treatment Monitoring | Real-time biomechanical/chemical changes [125] | Functional response via target expression [130] |
| Therapeutic Intervention | Limited (primarily diagnostic/sensing) | High (direct tumor cytotoxicity) [124] |
| Metastasis Detection | Limited to accessible sites | Comprehensive (systemic circulation) [126] |
| Patient Stratification | Emerging (biomechanical phenotypes) [125] | Established (target expression via imaging) [128] |
Experimental Protocols and Methodologies
Radiopharmaceutical Development and Validation
Radiopharmaceutical development follows a rigorous multi-step validation process to ensure specificity, selectivity, and deliverability against tumors [128]. The development pipeline encompasses target selection, radiochemistry optimization, preclinical evaluation, and clinical translation.
Step 1: Target Antigen Validation - Initial validation begins with immunohistochemistry (IHC) assessment of the intended antigen target on formalin-fixed paraffin-embedded (FFPE) tissues. Tissue microarrays (TMAs) containing hundreds of tissue cores from both cancerous and normal tissues provide a comprehensive platform for evaluating target specificity. Positive controls (antigen-expressing cells) and negative controls (antigen knockout cells) are essential for establishing assay specificity [128].
Step 2: Preclinical in vitro and in vivo Evaluation - Comprehensive preclinical testing utilizes various cancer models. Cell lines provide initial target validation and efficacy screening. More complex models include patient-derived organoids (PDOs) that preserve tumor heterogeneity, cell line-derived xenografts (CDXs) in immunocompromised mice for in vivo studies, and patient-derived xenografts (PDXs) that more closely maintain the original tumor's complexity [124]. Orthotopic models, where tumors are implanted in their original tissue site, best mimic the natural tumor microenvironment and metastatic behavior [124].
Step 3: Radiolabeling and Quality Control - The radiolabeling process involves attaching a radioactive isotope to the targeting molecule using chelating agents like DOTA or DfO [124]. Quality control is critical and employs both radio-thin-layer chromatography (radio-TLC) and high-performance liquid chromatography (HPLC). HPLC is particularly essential for identifying radiolysis products that may not be detected by TLC but can significantly impact binding affinity and treatment efficacy [129].
Step 4: Biodistribution and Dosimetry Studies - Preclinical biodistribution studies track how the radiopharmaceutical disperses, accumulates, and clears from the body. Dosimetry quantifies radiation absorbed by tumors and healthy tissues to optimize the therapeutic index. Imaging readouts using positron emission tomography (PET) or single-photon emission computed tomography (SPECT) enable real-time visualization of drug distribution and tumor targeting [124].
Bio-Optics Experimental Workflows
Bio-optics methodologies employ diverse optical techniques for cancer detection, each with specific experimental protocols and applications.
Optical Coherence Tomography (OCT) - OCT is a non-invasive imaging technique that uses light waves to capture high-resolution, cross-sectional images of biological tissues in real-time. It has gained significant prominence in ophthalmology, cardiology, dermatology, and oncology, enabling visualization of tissue microstructures at a cellular and subcellular level [123]. The technique provides valuable insights into tissue morphology, composition, and pathology without ionizing radiation.
Brillouin Microscopy Protocol - This label-free technique measures the viscoelastic properties of cells and tissues through spontaneous Brillouin light scattering [125]. The experimental workflow involves:
- Sample Preparation - Cells, tissues, or organoids are prepared with appropriate physiological buffers. Fixation may alter mechanical properties, so live samples are preferred.
- Instrument Setup - A focused laser beam is directed toward the sample through a high-numerical-aperture objective. The backscattered light is collected through the same objective.
- Spectral Analysis - The inelastically scattered light is analyzed using a high-contrast VIPA-based spectrometer or Fabry-Perot interferometer to detect the small frequency shifts caused by interaction with intrinsic thermal phonons in the material.
- Data Interpretation - The Brillouin frequency shift (ΩB) is proportional to the longitudinal elastic modulus, while the Brillouin linewidth (ΓB) relates to viscosity. These parameters serve as mechanical biomarkers to distinguish cancerous from healthy tissues [125].
Raman Spectroscopy for Cancer Detection - Raman spectroscopy provides detailed molecular information about biological samples based on inelastic scattering of monochromatic light. When combined with artificial intelligence, it has demonstrated 98% effectiveness in identifying stage 1a breast cancer using blood plasma samples [131]. The technique can distinguish between different breast cancer subtypes with over 90% accuracy, offering a non-invasive alternative to traditional biopsies.
Research Reagent Solutions and Essential Materials
Successful implementation of both bio-optics and radiopharmaceutical research requires specific reagents and materials. The following table outlines essential components for experimental workflows in both fields.
Table 3: Essential Research Reagents and Materials
| Category | Specific Reagents/Materials | Function/Application | Field |
|---|---|---|---|
| Targeting Vectors | PSMA-I&T, BAY2315493 antibody, somatostatin analogs | Specific delivery to cancer cell targets | Radiopharmaceuticals |
| Radionuclides | Lutetium-177, Actinium-225, Tin-117m, Gallium-68 | Therapeutic radiation emission or imaging | Radiopharmaceuticals |
| Chelators | DOTA, DfO | Secure binding of radionuclides to targeting molecules | Radiopharmaceuticals |
| Quencher Solutions | Gentisic acid, ascorbate | Prevent radiolysis during storage and administration | Radiopharmaceuticals |
| Chromatography | Radio-TLC plates, RP-18 HPLC columns | Quality control and purity assessment | Radiopharmaceuticals |
| Optical Components | High-NA objectives, VIPA spectrometers, lasers | Enable high-resolution optical measurements | Bio-Optics |
| SERS Substrates | Silver nanowires, gold nanoparticles | Enhance Raman signals for sensitive detection | Bio-Optics |
| AI/ML Algorithms | Support vector machines, neural networks | Analyze spectral/mechanical data for classification | Bio-Optics |
| Preclinical Models | PDX, CDX, organoids, 3D culture systems | Provide biologically relevant testing platforms | Both |
Comparative Performance Data and Clinical Validation
Technical Performance Metrics
Direct comparison of technical performance metrics reveals complementary strengths between bio-optics and radiopharmaceutical approaches.
Table 4: Quantitative Performance Comparison
| Performance Metric | Bio-Optics | Radiopharmaceuticals | Notes/Context |
|---|---|---|---|
| Early Detection Sensitivity | 98% (Raman/AI for breast cancer) [131] | N/A (requires established tumors) | Bio-optics excels in detecting molecular changes before macroscopic tumor formation |
| Tumor Subtype Discrimination | >90% accuracy (4 breast cancer subtypes) [131] | Dependent on target expression heterogeneity | Bio-optics identifies biochemical/mechanical patterns beyond molecular targets |
| Spatial Resolution | Submicron (Brillouin microscopy) [125] | Millimeter (clinical PET/SPECT) | Resolution difference reflects different application scales |
| Treatment Response Assessment | Days (mechanical property changes) [125] | Weeks (tumor size reduction on imaging) | Bio-optics can detect early treatment-induced changes before morphological alterations |
| Therapeutic Efficacy | 25-50% (various RPTs in advanced cancers) [128] [124] | N/A (primarily diagnostic) | Radiopharmaceuticals show significant efficacy even in treatment-resistant cases |
| Target Specificity | Indirect (mechanochemical properties) | Direct (molecular target engagement) | Different specificity paradigms: phenotypic vs molecular |
Clinical Validation Status
The clinical validation pathways and current status differ significantly between these technologies, reflecting their distinct developmental stages and applications.
Radiopharmaceuticals have established clinical validation with FDA-approved agents including Pluvicto ([177Lu]Lu-PSMA-617) for metastatic castration-resistant prostate cancer and Lutathera for neuroendocrine tumors [124]. The validation framework for radiopharmaceuticals follows a structured four-step process: (1) target antigen immunohistochemistry, (2) in vitro and in vivo preclinical experiments, (3) animal biodistribution and dosimetry studies, and (4) first-in-human microdose biodistribution studies [128]. This comprehensive pathway ensures that therapeutic radiopharmaceuticals demonstrate specificity, selectivity, and deliverability against tumors in patient subgroups likely to benefit from treatment.
Bio-optics technologies are primarily in the translational research phase, with varying levels of clinical validation across different techniques. Optical coherence tomography (OCT) has the most established clinical role, particularly in ophthalmology and cardiology, with growing applications in cancer diagnostics [123]. Brillouin microscopy remains primarily a research tool but shows consistent ability to biomechanically delineate between healthy and cancerous cells, organoids, and tissues across multiple cancer types [125]. The most clinically advanced bio-optics applications for cancer detection combine Raman spectroscopy with artificial intelligence, demonstrating 98% effectiveness in identifying stage 1a breast cancer through blood plasma analysis [131]. This approach is moving toward clinical implementation as a non-invasive alternative to traditional diagnostic methods.
Integration Potential and Future Directions
The future oncology landscape will likely leverage both technologies in complementary roles rather than as competing modalities. Several convergent trends suggest promising integration potential:
Theranostic Applications - The radiotheranostic paradigm combines diagnostic and therapeutic radiopharmaceuticals targeting the same biomarker, enabling patient stratification, treatment planning, and response assessment [126]. Bio-optics could enhance this approach by providing additional mechanistic insights through non-invasive monitoring of treatment-induced changes in the tumor microenvironment.
Artificial Intelligence Integration - Both fields increasingly incorporate AI for data analysis and interpretation. For radiopharmaceuticals, AI tools are advancing earlier detection of occult lymph node metastases that may be missed by current diagnostic techniques [130]. In bio-optics, AI algorithms analyze spectral data from techniques like Raman spectroscopy to classify cancer subtypes with high accuracy [131]. Continued AI development will enhance the analytical capabilities of both technologies.
Mechanistic Complementarity - The technologies provide fundamentally different but complementary information: radiopharmaceuticals offer quantitative data on target expression and biodistribution, while bio-optics provides insights into resulting biomechanical and biochemical changes in the tumor microenvironment [125]. Combined approaches could yield more comprehensive understanding of tumor biology and treatment response.
Technical Innovation Convergence - Technical advances in both fields show parallel development trajectories. Radiopharmaceutical research focuses on novel targets, optimized radiochemistry, and combination therapies [132], while bio-optics advances include improved resolution, speed, and integration of multiple optical modalities [127]. These parallel innovations will continue to expand their respective applications in cancer research and clinical management.
In conclusion, bio-optics and radiopharmaceuticals represent distinct but complementary technologies in the evolving oncology landscape. Radiopharmaceuticals offer well-established therapeutic capabilities with precise molecular targeting, while bio-optics provides high-resolution diagnostic information with sensitivity to early biomechanical and biochemical changes. Their integration offers promising pathways for advancing precision oncology through multimodal assessment of tumor biology and treatment response.
Conclusion
The clinical validation of bio-optical cancer diagnostics represents a paradigm shift towards more precise and comprehensive cytogenomic analysis. Success hinges on a multi-faceted strategy that integrates robust technical performance with demonstrable clinical utility, as evidenced by superior detection of complex genomic alterations compared to standard methods. Future progress will be driven by the maturation of AI-driven analytics, the standardization of multi-omic validation frameworks, and the generation of rigorous prospective evidence. For researchers and developers, adhering to these outlined principles is crucial for bridging the translational gap, securing regulatory approval, and ultimately delivering on the promise of personalized cancer care, positioning bio-optics as a potential first-tier test in the oncologic arsenal.
References
- 1. Shining a Light on the Future of Biophotonics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245495/]
- 2. Optical Genome Mapping: A 'Tool' with Significant Potential ... [https://www.cap.org/member-resources/articles/optical-genome-mapping-a-tool-with-significant-potential-from-discovery-to-diagnostics]
- 3. Optical Genome Mapping: A New Tool for Cytogenomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385997/]
- 4. Exploring the size limits of Bionano optical genome mapping ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01571-0]
- 5. Clinical Validation and Diagnostic Utility of Optical Genome ... [https://www.sciencedirect.com/science/article/pii/S1525157822002902]
- 6. Validation and Clinical Utility in the Cytogenetic Diagnosis ... [https://pubmed.ncbi.nlm.nih.gov/40974307/]
- 7. Researchers Develop New Imaging Tool for Earlier Cancer ... [https://news.utdallas.edu/health-medicine/advanced-micro-imaging-device-cancer-detection-2025/]
- 8. Cancer detection gets a boost from new technology [https://www.binghamton.edu/news/story/5827/cancerdetection]
- 9. New hybrid imaging breakthrough could transform ... [https://health.ucdavis.edu/news/headlines/new-hybrid-imaging-breakthrough-could-transform-detection-of-cancer-and-other-diseases/2025/08]
- 10. Cytogenetics - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/cytogenetics]
- 11. Cytogenetics Is a Science, Not a Technique! Why Optical Genome Mapping Is So Important to Clinical Genetic Laboratories - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10670395/]
- 12. Feasibility of Optical Genome Mapping in Cytogenetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10252312/]
- 13. Next-generation cytogenetics: Comprehensive assessment ... [https://www.sciencedirect.com/science/article/pii/S0002929721002238]
- 14. A comparison of molecular and cytogenetic techniques for the diagnosis of pregnancy loss | Genetics in Medicine [https://www.nature.com/articles/gim920118]
- 15. Advantages and limitations of cytogenetic, molecular cytogenetic, and molecular diagnostic testing in mesenchymal neoplasms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2778709/]
- 16. Diagnostics Research and Development Resources - NCI [https://dctd.cancer.gov/research/research-areas/cancer-diagnosis-research/diagnostic-research-development]
- 17. A Comparative Study Between Clinical Optical Coherence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452668/]
- 18. A novel approach to overcome black box of AI for optical ... [https://www.nature.com/articles/s41598-025-04770-2]
- 19. UCLA Researchers Unveil “BlurryScope”: A Compact, AI ... [https://cnsi.ucla.edu/august-17-2025-ucla-researchers-unveil-blurryscope-a-compact-ai-powered-microscope-for-rapid-cancer-scoring/]
- 20. Analytical and clinical validation of a high accuracy fully ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1568971/full]
- 21. Interrelationships Among Sensitivity, Precision, Accuracy ... [https://www.mdpi.com/2075-4418/15/4/410]
- 22. Molecular methods in cancer diagnostics: a short review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11100444/]
- 23. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 24. Unlocking the potential: multimodal AI in biotechnology ... [https://www.nature.com/articles/s41746-025-01992-6]
- 25. How AI Will Impact the Biotech Industry In 2025 [https://biotechbreakthroughawards.com/how-ai-will-impact-the-biotech-industry-in-2025/]
- 26. Digital Pathology and AI Highlights from ASCO 2025 [https://proscia.com/digital-pathology-and-ai-highlights-from-asco-2025/]
- 27. Diagnostics World - Comparison of AI Digital Pathology ... [https://friendsofcancerresearch.org/news/diagnostics-world-comparison-of-ai-digital-pathology-tools-finds-means-to-measure-performance/]
- 28. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 29. Optical Preclinical Imaging Market Growth Statistics - 2035 [https://www.factmr.com/report/optical-preclinical-imaging-market]
- 30. The role of orthogonal and complementary analytical ... [https://www.news-medical.net/whitepaper/20240718/Enhancing-biotherapeutic-research-The-role-of-orthogonal-and-complementary-analytical-techniques.aspx]
- 31. Comparison of Strategic Planning Frameworks [https://bscdesigner.com/strategic-frameworks-comparison.htm]
- 32. Analytical Similarity Assessment of Biosimilars - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8865741/]
- 33. Orthogonal and complementary measurements of ... [https://www.sciencedirect.com/science/article/pii/S016836592200863X]
- 34. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 35. Integrative Multi-Omics Approaches for Identifying and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11855028/]
- 36. Multi-omics approaches to disease | Genome Biology | Full Text [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-017-1215-1]
- 37. Graph machine learning for integrated multi-omics analysis [https://www.nature.com/articles/s41416-024-02706-7]
- 38. Multi-omics data integration using ratio-based quantitative ... [https://www.nature.com/articles/s41587-023-01934-1]
- 39. Biomedical Applications of Translational Optical Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC8587670/]
- 40. Evaluation and comparison of multi-omics data integration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8384175/]
- 41. Comparison of different metrics for analysis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3862158/]
- 42. Researcher developing noninvasive imaging for anal cancer ... [https://cancercenter.arizona.edu/news/2025/09/researcher-developing-noninvasive-imaging-anal-cancer-screening]
- 43. Development and validation of an autonomous artificial ... [https://www.nature.com/articles/s43018-025-00991-6]
- 44. Biomarkers in 2025: From Liquid Biopsy to AI-Driven ... [https://www.barchart.com/story/news/35377423/biomarkers-in-2025-from-liquid-biopsy-to-ai-driven-discovery-what-business-leaders-must-know]
- 45. How is Cryopreserved Tissue Different from Standard ... [https://specicare.com/how-is-cryopreserved-tissue-different-from-standard-tumor-preservation-ffpe/]
- 46. Fresh frozen vs FFPE samples for next-generation ... [https://www.lexogen.com/blog/fresh-frozen-vs-ffpe-samples-for-next-generation-sequencing-studies/]
- 47. Biomedical analysis of formalin-fixed, paraffin-embedded ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708518304059]
- 48. Cryopreserved Tissue Biospecimens Offer Superior Quality ... [https://www.mdpi.com/1422-0067/26/22/11038]
- 49. Optical super-resolution histology of formalin-fixed paraffin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589544/]
- 50. Perfusion-based ex vivo culture of frozen ovarian cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12102267/]
- 51. A Comparative Review of Bioinformatics Pipeline Frameworks ... [https://www.tracer.cloud/resources/bioinformatics-pipeline-frameworks-2025]
- 52. Empowering bioinformatics communities with Nextflow and nf ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03673-9]
- 53. Comparison of bioinformatic pipelines for analysis of viral ... [https://pubmed.ncbi.nlm.nih.gov/41046678/]
- 54. Garbage In, Garbage Out: Dealing with Data Errors ... [https://blog.omni-inc.com/blog/garbage-in-garbage-out-dealing-with-data-errors-bioinformatics]
- 55. Bioinformatics Pipeline For Data Quality Control [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-for-data-quality-control]
- 56. What Is Data Quality Assurance in Bioinformatics? [https://ranchobiosciences.com/2025/04/bioinformatics-and-quality-assurance-data/]
- 57. Label-Free Cancer Detection Methods Based on Biophysical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562235/]
- 58. A Comprehensive Review of Bioinformatics Tools for Genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11353282/]
- 59. Advancing cancer diagnostics through multifaceted optical ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X2401419X]
- 60. Tackling the Complex Challenges of Hard-to-Treat Blood ... [https://www.pfizer.com/news/articles/tackling_the_complex_challenges_of_hard_to_treat_blood_cancers]
- 61. Difference between hematological malignancy and Solid ... [https://www.nature.com/articles/2404369]
- 62. Diagnosis and classification of hematologic malignancies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5533199/]
- 63. Advances in early detection methods for solid tumors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9998680/]
- 64. Genetics and Solid Tumor Diagnostic Testing [https://dlmp.uw.edu/test-guide/view/genetics_solid_tumors]
- 65. If it is a solid tumor target, then it may be a hematologic ... [https://www.sciencedirect.com/science/article/pii/S2666634024004446]
- 66. Press Release [https://www.carislifesciences.com/about/news-and-media/caris-life-sciences-demonstrates-scientific-rigor-with-clinical-validation-of-fda-approved-mi-cancer-seek/]
- 67. ASCO 2025 Highlights [https://www.diaceutics.com/articles/asco-2025-highlights]
- 68. Differences between solid tumor and hematologic malignancy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8641046/]
- 69. Bridging the Gap: Translating Preclinical Biomarkers to ... [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 70. PDX-derived organoids model in vivo drug response and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7710298/]
- 71. Promising preclinical patient-derived organoid (PDO ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10702130/]
- 72. Patient-derived xenograft models: Current status ... [https://www.sciencedirect.com/science/article/pii/S2352304225000091]
- 73. PDOs, PDXOs, PDOXs or PDXs? Selecting the Best Model ... [https://blog.crownbio.com/pdos-pdxos-pdoxs-or-pdxs-selecting-the-best-model-to-progress-your-patient-centric-research]
- 74. Orthotopic Models with Advanced Imaging [https://www.crownbio.com/model-systems/in-vivo/orthotopic-and-bioluminescent-models]
- 75. Heterogeneity in Cancer [https://www.mdpi.com/2072-6694/17/3/441]
- 76. Decoding tumor heterogeneity: A spatially informed pan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629804/]
- 77. Heterogeneity-optimized method for predicting immune ... [https://www.nature.com/articles/s41598-025-17718-3]
- 78. Review Liquid biopsy-based multi-cancer early detection [https://www.sciencedirect.com/science/article/pii/S2095927325006565]
- 79. Machine learning analysis reveals tumor heterogeneity ... [https://www.nature.com/articles/s41746-025-01967-7]
- 80. Experts See 17 Laboratory Trends Dominating 2025 [https://clpmag.com/diagnostic-technologies/experts-see-17-laboratory-trends-dominating-2025/]
- 81. Expert Pre-Analytical Work Processing - Sampled [https://sampled.com/the-critical-role-of-pre-analytical-work/]
- 82. Control of (pre)-analytical aspects in immunoassay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5881432/]
- 83. Why Pre-Analytical Variables Can Make or Break Your Assay [https://mtgroupbio.com/the-hidden-challenge-in-assay-development-why-pre-analytical-variables-can-make-or-break-your-assay/]
- 84. A practical approach to estimate analytical method ... [https://www.sciencedirect.com/science/article/pii/S0731708524003844]
- 85. Exploring the influence of pre-analytical variables on gene ... [https://www.nature.com/articles/s41598-025-88756-0]
- 86. Systematic scoping review of external validation studies ... [https://www.nature.com/articles/s41698-025-00940-7]
- 87. Development and clinical validation of a ... [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-30/issue-10/106002/Development-and-clinical-validation-of-a-clinically-translatable-non-chip/10.1117/1.JBO.30.10.106002.full]
- 88. Rethinking the scientific method in the age of AI [https://www.nature.com/articles/s44222-025-00386-3]
- 89. A Step-by-Step Guide to Effective AI Model Validation [https://galileo.ai/blog/ai-model-validation]
- 90. Cancer oriented biobanks: A comprehensive review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6047884/]
- 91. Banked Biospecimens vs. Prospective Collection [https://sanguinebio.com/researchers/banked-biospecimens-vs-prospective-biospecimen-collection-evaluating-pros-and-cons-for-scientific-research/?srsltid=AfmBOooeG3QeH-CqOQvdM3Ce9wsYvI37FZopxFifErsSvgXKurWgAFq2]
- 92. Building Evidence in Oncology Diagnostics: Strategic Use ... [https://www.lindushealth.com/blog/building-evidence-in-oncology-diagnostics-strategic-use-of-biobanks-and-clinical-trials]
- 93. GRAIL PATHFINDER 2 Results Show Galleri® Multi ... [https://grail.com/press-releases/grail-pathfinder-2-results-show-galleri-multi-cancer-early-detection-blood-test-increased-cancer-detection-more-than-seven-fold-when-added-to-uspstf-a-and-b-recommended-screenings/]
- 94. Fred Hutch leads new Vanguard Study for Cancer ... [https://www.fredhutch.org/en/news/releases/2025/07/vanguard-study-launch.html]
- 95. Exact Sciences Announces Breakthrough Results from ... [https://www.exactsciences.com/newsroom/press-releases/exact-sciences-announces-breakthrough-results-from-landmark-study]
- 96. Cancer incidence inconsistency between UK Biobank ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11948887/]
- 97. UK Biobank: a globally important resource for cancer ... [https://www.nature.com/articles/s41416-022-02053-5]
- 98. Comprehensive biobanking strategy with clinical impact at ... [https://www.sciencedirect.com/science/article/pii/S1874391925000697]
- 99. Comparative Analysis of Targeted RNA-Seq and Optical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608001/]
- 100. Integration of Newer Genomic Technologies into Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193535/]
- 101. Benchmarking standard-of-care and emerging genomic ... [https://www.nature.com/articles/s41416-025-03204-0]
- 102. Comprehensive performance comparison of high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5402652/]
- 103. International Consortium for Optical Genome Mapping ... [https://ir.bionano.com/news-releases/news-release-details/international-consortium-optical-genome-mapping-publishes-expert]
- 104. Clinical Validation and Diagnostic Utility of Optical Genome ... [https://pubmed.ncbi.nlm.nih.gov/36265723/]
- 105. Point-of-care optical spectroscopy platform and ratio-metric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11687633/]
- 106. Analysis of data from biomedical multisensor optical systems [https://opg.optica.org/jot/abstract.cfm?uri=jot-91-7-509]
- 107. Advances and challenges in portable optical biosensors for ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993624001225]
- 108. Advances in optical coherence tomography: Celebrating its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456903/]
- 109. Liquid Biopsy | October Round-Up 2025 [https://www.decibio.com/insights/liquid-biopsy-october-round-up-2025]
- 110. Deep Learning Applications in Clinical Cancer Detection [https://www.sciencedirect.com/science/article/pii/S2949761225000604]
- 111. A Comparison of IVDR to FDA IVD Regulatory Submission Requirements | RQM+ [https://www.rqmplus.com/blog/a-comparison-of-ivdr-to-fda-ivd-regulatory-submission-requirements/]
- 112. How Do You Comply with EU MDR/IVDR vs. U.S. FDA ... [https://avendium.com/2025/10/31/how-do-you-comply-with-eu-mdr-ivdr-vs-u-s-fda-regulations/]
- 113. IVDs – A Comparison of Requirements between the US and EU [https://blog.pqegroup.com/medical-device/ivds-a-comparison-of-requirements-between-the-us-and-eu]
- 114. Overview of IVD Regulation [https://www.fda.gov/medical-devices/ivd-regulatory-assistance/overview-ivd-regulation]
- 115. The 5 Major Regulatory Focus Areas For Medical Device Compliance In 2025 [https://www.meddeviceonline.com/doc/the-major-regulatory-focus-areas-for-medical-device-compliance-in-2025-0001]
- 116. Adapting your QMS to IVDR requirements until May 2025: what manufacturers need to know | Blog | Pure Global [https://www.pureglobal.com/blog-posts/adapting-your-qms-to-ivdr-requirements-until-may-2025-what-manufacturers-need-to-know]
- 117. Breaking Down Analytical Performance Studies under IVDR [https://www.abingdonhealth.com/breaking-down-analytical-performance-studies-under-ivdr/]
- 118. AMDM 2025: Shaping the Future of IVD Regulation [https://beaufortcro.com/blog/ivd-regulatory-update-2025/]
- 119. Real‐World Evidence in Oncology - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC7216461/]
- 120. Automated real-world data integration improves cancer ... [https://www.nature.com/articles/s41586-024-08167-5]
- 121. Advancing the role of real-world evidence in comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11609978/]
- 122. A Review and Comparative Case Study Analysis of Real- ... [https://www.sciencedirect.com/science/article/pii/S1098301524028596]
- 123. Bio Optics Market: Global Technology Analysis and Forecast [https://www.maximizemarketresearch.com/market-report/bio-optics-market/189394/]
- 124. The Evolving Role of Radiation in Targeted Cancer Therapy [https://blog.crownbio.com/radiopharmaceuticals-the-evolving-role-of-radiation-in-targeted-cancer-therapy]
- 125. Brillouin microscopy in cancer research: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530143/]
- 126. Radiopharmaceuticals and their applications in medicine [https://www.nature.com/articles/s41392-024-02041-6]
- 127. Wearable bioelectronics for cancer theranostics [https://www.nature.com/articles/s41378-025-01048-5]
- 128. Radiopharmaceutical Validation for Clinical Use - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7966985/]
- 129. Radiolabeling and quality control of therapeutic ... [https://ejnmmipharmchem.springeropen.com/articles/10.1186/s41181-022-00181-0]
- 130. MD Anderson experts highlight top trends ahead of 2025 ... [https://www.mdanderson.org/newsroom/research-newsroom/md-anderson-experts-highlight-top-trends-ahead-of-2025-astro-mee.h00-159779601.html]
- 131. World Cancer Day 2025: AI Analysis of Biological Samples ... [https://www.reddie.co.uk/2025/02/04/ai-analysis-of-biological-samples-for-cancer-diagnosis/]
- 132. Radiopharmaceuticals Reshaping Oncology Trials [https://www.medpace.com/blog/snmmi-2025-highlights-radiopharmaceuticals-reshaping-oncology-trials/]