Biophotonics: The Complete Guide to Light-Based Technologies in Biomedicine and Drug Development
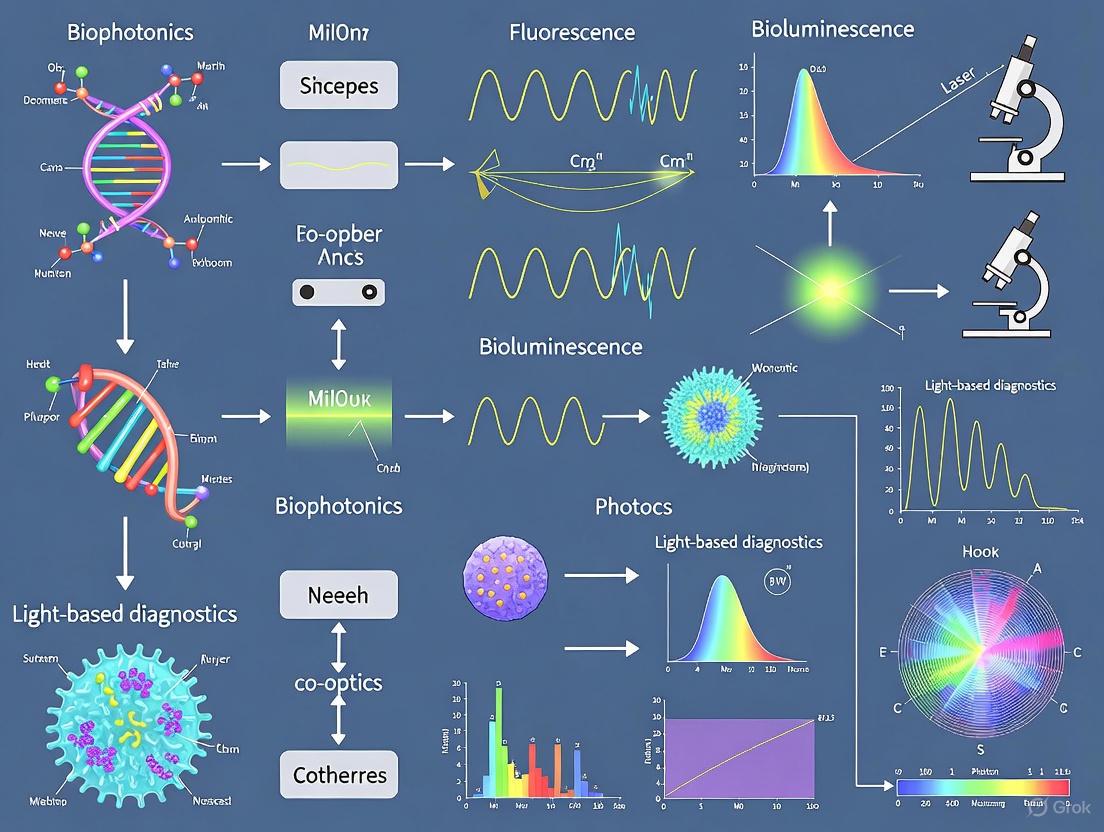
This article provides a comprehensive exploration of biophotonics, the interdisciplinary field harnessing light to analyze and manipulate biological systems.
Biophotonics: The Complete Guide to Light-Based Technologies in Biomedicine and Drug Development
Abstract
This article provides a comprehensive exploration of biophotonics, the interdisciplinary field harnessing light to analyze and manipulate biological systems. Tailored for researchers, scientists, and drug development professionals, it covers the foundational principles of light-tissue interaction, details cutting-edge methodologies from imaging to therapy, and analyzes the integration of AI and nanotechnology for optimization. The scope extends to current market trends, validation frameworks, and the transformative role of biophotonics in advancing precision medicine, non-invasive diagnostics, and targeted therapeutic applications.
Biophotonics Fundamentals: Principles of Light-Biology Interaction and Core Technologies
Biophotonics, derived from the Greek words "bios" (life) and "phos" (light), is an interdisciplinary field that represents the innovative convergence of biology, medicine, and photonics—the science and technology of generating, controlling, and detecting light [1]. This dynamic discipline employs light to analyze and manipulate biological materials, offering groundbreaking possibilities for both fundamental research and practical applications across various industries, including pharmaceuticals, biotechnology, and medicine [1]. By leveraging optical techniques, biophotonics allows scientists to capture cellular conditions and monitor dynamic processes, providing a comprehensive view of life processes at molecular, cellular, tissue, and organ levels [1].
The potential applications of biophotonics are numerous and diverse, encompassing fundamental investigations of cell processes as well as health-related applications such as diagnostics, therapy monitoring, and well-being assessment [1]. Furthermore, biophotonic technologies contribute significantly to environmental monitoring, food safety, and agricultural advancements [1]. The field stands at the forefront of scientific innovation, offering profound insights into biological and biomedical processes and paving the way for new diagnostic and therapeutic approaches that are transforming research, diagnostics, and therapy across multiple domains [1].
Core Principles and Technologies
Fundamental Light-Matter Interactions
Biophotonic techniques study the structural, functional, mechanical, biological, and chemical properties of biological materials through various light interactions, including absorption, emission, reflection, and scattering [1]. These interaction phenomena elucidate a vast array of morphological and molecular intricacies across macroscopic, microscopic, and nanoscopic resolutions [1]. The field can be broadly divided into three main technological areas:
- Bioimaging: Photonics technologies enable the characterization of biological specimens across multiple spatial scales, from the nanoscopic level—facilitating the investigation of intracellular interactions—to the microscopic and macroscopic domains, including tissues and muscle structures [1].
- Biosensing: Photonic-based approaches allow for the detection of biomolecules, such as disease-specific biomarkers, with sensitivities reaching molecular concentrations and, in principle, single-molecule resolution [1].
- Treatment and Control: Lasers and other light sources facilitate highly precise and minimally invasive surgical interventions, while bioimaging and biosensing modalities enable real-time monitoring of treatment efficacy and post-operative recovery [1].
Key Advantages of Biophotonic Technologies
The use of light in biophotonics offers several distinct advantages that make it particularly valuable for biological and medical applications:
- Non-contact measurement: Light facilitates the observation of living cells noninvasively, preserving the integrity of analyzed cells and avoiding toxic effects [1].
- Speed and instant information: Optical measurements provide rapid, real-time data, significantly reducing the time required for data interpretation and diagnosis [1].
- Sensitivity: Optical technologies allow for ultrasensitive detection, down to single molecules, which is essential for understanding fundamental biological processes [1].
- Time resolution: Optical methods enable the observation of dynamic biological processes over a range of temporal scales, from hours to ultrafast reactions [1].
Key Technological Modalities in Biophotonics
Advanced Bioimaging Techniques
Bioimaging represents one of the most developed applications of biophotonics, with numerous sophisticated modalities available for research and clinical use:
Label-free diagnostic methods include several powerful technologies. Hyperspectral imaging (HSI) and fluorescence lifetime imaging (FLIM) of endogenous fluorophores provide molecular contrast by visualizing native electronic chromophores such as hemoglobin, NADP(H), flavin, elastin, or cytochrome [1]. Second harmonic generation (SHG) and third harmonic generation (THG) visualize specific structural proteins (e.g., collagen) and phase boundaries, respectively [1]. Optical coherence tomography (OCT) provides detailed imaging of tissue architecture down to the cellular level by detecting changes in refractive index [1]. Photoacoustic imaging (PAI) combines optical absorption with ultrasonic detection for deep-tissue imaging [1]. Vibrational microspectroscopy, including infrared (IR) absorption and Raman scattering, offers molecule-specific contrast for visualizing spatial distribution of molecular markers such as proteins, lipids, or DNA [1].
Recent advances in compact high-intensity ultrashort laser sources have enabled the exploitation of nonlinear optical phenomena for biomedical imaging, resulting in significant improvements in penetration depth, optical resolution, and acquisition speed [1]. Multi-photon absorption, in particular, is valuable for microscopy applications as the simultaneous absorption of two or three photons leads to precise localization of fluorescence or harmonic generation signals [1]. Coherent Raman scattering (CRS) phenomena such as CARS (coherent anti-Stokes Raman scattering) and SRS (stimulated Raman scattering) enhance the intrinsically weak Raman signal and avoid being swamped by autofluorescence background [1].
Biosensing Platforms
Biophotonic biosensing leverages optical phenomena such as fluorescence, surface plasmon resonance (SPR), and Raman spectroscopy to enable highly sensitive, often label-free detection of biological and chemical analytes [2]. The growing emphasis on point-of-care testing (POCT) and wearable biosensing technologies for early disease detection, remote patient monitoring, and real-time health analytics has significantly driven advancement in this area [2].
Incorporating nanophotonic elements such as plasmonic nanoparticles, quantum dots, and photonic crystals has facilitated ideal biosensor performance, enabling ultrasensitive tracking of DNA, proteins, and biomarkers in small volumes [2]. These advancements support enhanced disease screening, personalized medicine, and early-stage cancer detection [2]. The rise of wearable health monitoring devices integrated with AI-driven biosensors in smartwatches, patches, and implantable sensors further exemplifies the growing application of biophotonic biosensing for continuous monitoring of glucose levels, oxygen saturation, and cardiovascular biomarkers [2].
Therapeutic Applications
Light-based therapeutic modalities represent another major application area for biophotonics. Lasers and other advanced light sources are used for facilitating highly precise and minimally invasive surgical interventions [1]. Photodynamic therapy (PDT) combines light-sensitive compounds with specific light wavelengths to selectively target and destroy abnormal cells [3]. Laser therapies are well-established in various medical specialties, including ophthalmology, dermatology, and oncology [3].
The integration of bioimaging and biosensing modalities with therapeutic applications enables real-time monitoring of treatment efficacy and post-operative recovery, creating a closed-loop system for precision medicine [1]. This convergence of diagnostic and therapeutic capabilities within a single platform represents a significant advancement in medical technology, allowing for personalized treatment approaches and improved patient outcomes.
Quantitative Market Outlook and Adoption Trends
The growing importance of biophotonics is reflected in market projections and adoption trends across various sectors and regions. The table below summarizes key quantitative data on the biophotonics market size, growth rates, and regional adoption:
Table 1: Biophotonics Market Size and Growth Projections
| Metric | 2024/2025 Value | 2034/2035 Projection | CAGR | Key Drivers |
|---|---|---|---|---|
| Global Market Size | USD 76.1 billion (2024) [3] | USD 220.1 billion (2034) [3] | 11.3% [3] | Nanotechnology, aging population, lifestyle diseases [3] |
| Alternative Market Estimate | USD 67.2 billion (2025) [2] | USD 189.3 billion (2035) [2] | 10.9% [2] | Non-invasive diagnostics, surgical visualization [2] |
| In-Vivo Segment Share | 57% (2024) [3] | Dominance through forecast period [3] | - | Optical imaging, laser diagnostics [3] |
| In-Vitro Segment Size | - | USD 89.6 billion (2034) [3] | - | Automation, AI-based analysis [3] |
| See-Through Imaging Segment | - | - | 13.7% [3] | Non-invasive, high-resolution visualization [3] |
Table 2: Regional Market Analysis and Key Characteristics
| Region/Country | Market Size | Growth Rate (CAGR) | Key Characteristics & Drivers |
|---|---|---|---|
| United States | - | - | Massive R&D investment, advanced healthcare infrastructure [3] |
| Germany | USD 3.6 billion (2024) [3] | - | Strong R&D, multiphoton microscopy, OCT adoption [3] |
| China | - | 14.1% [3] | Aggressive R&D investments, government strategic initiatives [3] |
| India | - | - | USD 8.7 billion (2034 projection) [3] |
| Japan | USD 3.3 billion (2024) [3] | - | Aging population, chronic disease prevalence [3] |
Application segments show varying growth patterns and market dynamics. The spectro molecular segment held the largest market share at USD 15.1 billion in 2024, driven by technological progress that has improved the sensitivity and accuracy of spectroscopic devices [3]. The tests and components segment dominated end-use applications with a 35.4% share in 2024, reflecting increasing demand for advanced diagnostic tools and highly reliable imaging components [3]. The medical therapeutics segment is growing at the highest rate and is expected to reach a market size of USD 83.7 billion in 2034, fueled by expansion in laser therapies, photodynamic therapy, and other light-based treatments [3].
Experimental Methodologies and Workflows
Core Experimental Workflow in Biophotonics Research
The following diagram illustrates a generalized experimental workflow for biophotonics research, highlighting the interconnected nature of various technologies and applications:
Detailed Methodologies for Key Techniques
Multiphoton Microscopy Protocol
Principle: Simultaneous absorption of two or three photons of longer wavelength (typically NIR) leads to precise localization of fluorescence or harmonic generation signals, enabling deep tissue imaging with high spatial resolution [1].
Experimental Protocol:
- Sample Preparation: Fix or maintain live biological specimens (cells, tissues, or small organisms) in appropriate mounting media compatible with optical imaging [1].
- Labeling (if required): Introduce fluorescent markers (endogenous or exogenous) that exhibit multiphoton absorption characteristics [4].
- System Setup: Configure Ti:sapphire femtosecond laser source tuned to appropriate wavelength (typically 700-1100 nm) [1]. Align laser scanning microscope system with high-sensitivity detectors (photomultiplier tubes or GaAsP detectors) [1] [2].
- Image Acquisition: Focus laser beam on sample using high-numerical-aperture objective lens. Scan beam across sample region of interest while collecting emitted fluorescence signals through non-descanned detectors [1].
- Data Collection: Acquire 3D image stacks by sequential imaging at different depths. For dynamic processes, collect time-series data at appropriate temporal resolution [1].
- Processing: Reconstruct 3D volumes from z-stacks. Apply necessary corrections for background subtraction, flat-field correction, and photon counting analysis [1].
Raman Spectroscopy and CRS Protocol
Principle: Inelastic scattering of light provides vibrational fingerprint of molecules, with CRS (CARS/SRS) enhancing weak Raman signals through coherent excitation [1].
Experimental Protocol:
- Sample Preparation: Prepare thin sections or concentrated solutions of biological material. Minimal preparation required as Raman is inherently label-free [1].
- System Setup:
- Data Acquisition:
- Spectral Processing: Remove cosmic rays, correct for background fluorescence, normalize spectra, and perform multivariate analysis for chemical mapping [1].
Optical Coherence Tomography (OCT) Protocol
Principle: Interferometric detection of backscattered light to reconstruct depth-resolved tissue microstructure with micron-scale resolution [1].
Experimental Protocol:
- Sample Preparation: Minimal preparation required. Can image tissues in vivo or ex vivo without sectioning [1].
- System Setup: Configure broadband light source (superluminescent diode or laser), Michelson interferometer with reference arm, and spectrometer-based or swept-source detection system [1].
- Data Acquisition: Scan reference arm length while detecting interference pattern. Reconstruct depth profile (A-scan) at each lateral position [1].
- Image Reconstruction: Perform Fourier transform on spectral interference patterns to reconstruct depth-resolved reflectivity profiles. Combine sequential A-scans to form 2D cross-sections (B-scans) or 3D volumes [1].
- Extension to SOCT: Acquire wavelength-dependent backscattering to determine concentration of tissue chromophores through spectroscopic OCT [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful biophotonics research requires carefully selected reagents and materials optimized for specific optical techniques. The following table details key research reagent solutions essential for experimental work in this field:
Table 3: Essential Research Reagents and Materials for Biophotonics
| Reagent/Material | Function/Application | Technical Specifications | Example Use Cases |
|---|---|---|---|
| Fluorescent Markers & Dyes | Labeling cellular structures and molecules for detection | High quantum yield, photostability, specific binding | Intracellular imaging, molecular tracking [1] |
| Monoclonal Antibodies | Specific target recognition in flow cytometry and imaging | Conjugated with fluorochromes (e.g., FITC, PE, APC) | Immune cell phenotyping, intracellular staining [5] |
| Nanoparticles | Enhanced contrast and sensing capabilities | Metallic nanoparticles, quantum dots, photonic crystals | Biosensing, signal amplification [2] [3] |
| Photosensitizers | Light-activated therapeutic agents | High singlet oxygen yield, target specificity | Photodynamic therapy, targeted cell destruction [3] |
| Intercalating Dyes | DNA/RNA staining for cell cycle analysis | Specific binding to nucleic acids, fluorescence enhancement | Cell cycle analysis, viability assessment [5] |
| Photomultiplier Tubes (PMTs) | High-sensitivity light detection | High gain, low noise, broad spectral response | Fluorescence detection, low-light imaging [2] |
| Biocompatible Optical Materials | Interfaces between light and biological tissues | Appropriate refractive index, minimal autofluorescence | Fiber optic probes, implantable sensors [2] |
Technological Integration and Emerging Frontiers
Artificial Intelligence and Machine Learning Integration
The integration of artificial intelligence (AI) and machine learning (ML) in biophotonics is transforming data interpretation and analysis. AI-driven biophotonics techniques, such as Raman spectroscopy integrated with machine learning, have demonstrated remarkable success in recent studies [3]. For example, researchers at the University of Edinburgh were able to detect early breast cancer with a 98% accuracy using a system that identified tiny chemical changes in blood tests that other methods fail to consider [3].
AI-assisted imaging analysis contributes significantly to biological data interpretation, automated lesion detection, and real-time evaluation of therapeutic effects [2]. These capabilities have broad application value and significant impact in both preclinical and clinical research settings [2]. The implementation of AI-based image reconstruction and real-time deep learning analysis is enhancing the accessibility, affordability, and automation of see-through imaging, driving sustained market growth for these solutions [2].
Nanotechnology-Enhanced Biophotonics
Nanotechnology is enabling unprecedented control over light-matter interactions at the nanoscale, significantly improving the performance of diagnostic and therapeutic tools [3]. By employing nanomaterials including metallic nanoparticles and quantum dots, biophotonic devices achieve higher sensitivity and specificity for sensing biomarkers and tissue imaging [3]. These advancements result in earlier disease detection and more specific treatments [3].
The development of nanophotonic biosensors has facilitated ideal biosensor performance, enabling ultrasensitive tracking of DNA, proteins, and biomarkers in small volumes [2]. These technologies support enhanced disease screening, personalized medicine, and early-stage cancer detection [2]. The continuous innovation in nanotechnology applications represents a significant frontier in biophotonics research and development.
Quantum Biophotonics
Emerging quantum technologies are opening new possibilities for biophotonics applications. Quantum-inspired techniques are being developed for enhanced imaging sensitivity beyond classical limits, with potential applications in super-resolution microscopy and single-molecule detection [1]. Quantum light sources and detectors may enable new modalities for biological imaging and sensing with improved signal-to-noise ratios and reduced photodamage to living samples [1].
The preservation of orbital angular momentum in scattering media, demonstrated in 2024 experiments, shows promise for new applications in biophotonics [4]. These structured light approaches may enable more efficient light penetration through turbid biological tissues and improved information encoding in optical communication with implanted devices [4].
Biophotonics stands as a cornerstone of next-generation precision medicine and the One Health approach, integrating biological research, medical applications, environmental monitoring, and agricultural advancements [1]. The field continues to evolve rapidly, driven by technological advancements in light sources, detectors, computational methods, and nanofabrication [1].
Future development will likely focus on enhancing non-invasiveness, improving spatial and temporal resolution, increasing penetration depth, and developing multi-modal platforms that combine complementary techniques [1]. The growing emphasis on point-of-care devices, wearable sensors, and affordable screening technologies will further expand the accessibility and impact of biophotonics across diverse healthcare settings and resource levels [2].
As interdisciplinary collaborations between physicists, chemists, engineers, biologists, computer scientists, medical professionals, and industry stakeholders continue to strengthen, biophotonics is poised to deliver increasingly sophisticated solutions to fundamental biological questions and pressing medical challenges [1]. The transformative potential of this field remains substantial, with ongoing innovations promising to further revolutionize how we study, diagnose, and treat biological systems across the spectrum from single molecules to entire organisms.
Biophotonics, the fusion of photonics and life sciences, leverages light to analyze and manipulate biological materials [1]. This interdisciplinary field is foundational to advancements in medical diagnostics, therapeutic applications, and fundamental biological research [1]. The core of biophotonic technologies lies in understanding how light interacts with biological tissues through the fundamental processes of absorption, emission, scattering, and reflection [6] [1]. These processes determine the propagation of light within tissue, influence the design of optical instruments, and dictate the type of biological information that can be extracted [6]. Quantitative measurement of these interactions is challenging due to the complex nature of tissue, but it is essential for developing non-invasive diagnostic tools, monitoring therapies, and guiding surgical procedures [7] [8]. This guide details the core principles, quantitative parameters, and experimental methodologies for characterizing these light-tissue interactions, providing a technical foundation for researchers and drug development professionals in the biophotonics field.
Fundamental Principles and Quantitative Parameters
When light is incident on biological tissue, it undergoes several interactions at the interface and within the tissue bulk. A portion of the light is reflected at the surface due to the mismatch in refractive index between air and tissue. The remaining light penetrates the tissue, where it may be transmitted, absorbed, or scattered in various directions [6] [9]. The specific outcome is governed by the optical properties of the tissue and the wavelength of the incident light.
Scattering Mechanisms
Scattering occurs when light is deflected from its original path by inhomogeneities within the tissue, such as organelles, collagen fibers, and other subcellular structures [6].
- Rayleigh Scattering: This occurs when light interacts with particles much smaller than the wavelength of light, such as very small cellular components [6]. The intensity of Rayleigh scattered light is proportional to the inverse fourth power of the wavelength ((I \propto \frac{1}{\lambda^4})) [6]. This wavelength dependence explains why shorter wavelengths (like blue light) scatter more effectively in tissue.
- Mie Scattering: This dominates when the particle size is comparable to or larger than the wavelength of light, such as in the case of mitochondria or nuclei [6]. Mie scattering is more uniform across wavelengths and is less wavelength-dependent than Rayleigh scattering [6].
- Multiple Scattering: In dense, thick tissues, light undergoes repeated scattering events, a phenomenon known as multiple scattering [6]. This results in diffuse light propagation, where light loses its original directionality [6]. Multiple scattering increases the effective optical path length of light within the tissue and complicates the analysis of light-tissue interactions, often requiring advanced modeling techniques like radiative transfer theory or Monte Carlo simulations [6].
Absorption and the Beer-Lambert Law
Absorption is the process by which chromophores in the tissue capture light energy, converting it into other forms of energy such as heat or chemical energy [9]. Key chromophores in biological tissues include hemoglobin (oxy- and deoxy-), melanin, water, lipids, and collagen [8]. The absorption coefficient ((μ_a)), defined as the probability of photon absorption per unit pathlength, quantifies this interaction [8]. Its typical order of magnitude is (0.1 \, \text{cm}^{-1}) in the near-infrared (NIR-I) window [8].
A fundamental model describing light attenuation in a medium is the Beer-Lambert Law: [ I = I0 e^{-\mua d} ] where (I) is the transmitted intensity, (I0) is the incident intensity, (\mua) is the absorption coefficient, and (d) is the path length through the medium [6]. While foundational, this law assumes negligible scattering and homogeneous absorption, which limits its direct accuracy in most biological tissues where scattering is significant [6].
Reflection and Transmission at Interfaces
When light encounters an interface between two media with different refractive indices (e.g., air and skin), a portion is reflected. The reflection coefficient (R) quantifies the fraction of incident light intensity that is reflected [6]. For normal incidence, it is calculated using Fresnel equations: [ R = \left( \frac{n1 - n2}{n1 + n2} \right)^2 ] where (n1) and (n2) are the refractive indices of the two media [6]. The remaining light is transmitted into the tissue. In non-absorbing media, the transmission coefficient is (T = 1 - R) [6].
Diffuse reflectance is a key concept in tissue optics. It occurs when light undergoes multiple scattering events within the tissue before re-emerging from the incident surface [6]. This diffused light carries information about the tissue's internal scattering and absorption properties and is widely used for non-invasive tissue characterization [6].
Emission Phenomena
Emission processes involve the re-radiation of light by a biological material after it has absorbed energy. A key emission phenomenon is fluorescence, where a chromophore (fluorophore) absorbs a high-energy photon and subsequently emits a lower-energy photon at a longer wavelength [7]. This "Stokes shift" allows the emitted light to be distinguished from the excitation light. Laser-Induced Fluorescence (LIF) is a powerful analytical technique that uses this principle for tissue classification and molecular analysis [7]. Other emission-based phenomena include phosphorescence and second harmonic generation (SHG) [7] [1].
Table 1: Key Parameters for Quantifying Tissue Optical Properties [6] [8]
| Parameter | Symbol | Definition | Common Units |
|---|---|---|---|
| Absorption Coefficient | (\mu_a) | Probability of photon absorption per unit pathlength | (\text{mm}^{-1}) or (\text{cm}^{-1}) |
| Scattering Coefficient | (\mu_s) | Probability of photon scattering per unit pathlength | (\text{mm}^{-1}) or (\text{cm}^{-1}) |
| Anisotropy Factor | (g) | Average cosine of the scattering angle ((⟨\cos \theta⟩)) | Unitless |
| Reduced Scattering Coefficient | (\mu_s') | (\mus' = \mus (1 - g)), represents the effective isotropic scattering | (\text{mm}^{-1}) or (\text{cm}^{-1}) |
| Refractive Index | (n) | Ratio of the speed of light in vacuum to that in the medium | Unitless |
| Effective Attenuation Coefficient | (\mu_{\text{eff}}) | (\mu{\text{eff}} = \sqrt{3\mua(\mua + \mus')}), describes attenuation in a scattering medium | (\text{mm}^{-1}) or (\text{cm}^{-1}) |
Table 2: Dominant Scattering Mechanisms and Chromophores in Biological Tissues [6] [8] [9]
| Interaction | Dominant Mechanism/Particle | Wavelength Dependence | Biological Targets/Chromophores |
|---|---|---|---|
| Rayleigh Scattering | Particles << Wavelength (e.g., small proteins) | (I \propto \frac{1}{\lambda^4}) | Very small cellular structures |
| Mie Scattering | Particles ≈ Wavelength (e.g., organelles, nuclei) | Less wavelength-dependent | Mitochondria, collagen fibers |
| Absorption in VIS | Chromophores | Varies by chromophore | Hemoglobin, Melanin |
| Absorption in NIR | Chromophores | Varies by chromophore | Water, Lipids |
| Absorption in IR | Chromophores | Varies by chromophore | Water, Hydroxyapatite |
Experimental Protocols for Measuring Optical Properties
Accurately determining the optical properties of tissues requires well-designed experiments and robust mathematical models to solve the inverse problem of relating measured light to internal properties [8].
Measurement Configurations and Instrumentation
A common setup for measuring total transmission ((T)) and diffuse reflectance ((R)) of tissue samples employs an integrating sphere coupled to a spectrometer and light source [7]. The sphere collects all light transmitted through or reflected from the sample, allowing for accurate quantification [7]. These measurements are typically performed at multiple wavelengths, for example, in the red to near-infrared spectrum (e.g., 808, 830, 980 nm) to exploit the "optical window" where tissue penetration is highest [7].
The experimental workflow can be summarized as follows:
Figure 1: Workflow for estimating tissue optical properties.
Inverse Models for Property Extraction
The measured (R) and (T) data are inputs for inverse models that compute the intrinsic optical properties.
- Kubelka-Munk (KM) Model: A widely used two-flux model that provides a simple analytical solution, directly relating (R) and (T) to the absorption ((K)) and scattering ((S)) coefficients [7]. Its simplicity is its major advantage, though it is most accurate for highly scattering and weakly absorbing samples [7].
- Inverse Adding-Doubling (IAD): This method calculates the reflectance and transmittance of a sample by iteratively adding and doubling layers until the measured values are matched, allowing for the extraction of (\mua) and (\mus) [8].
- Inverse Monte Carlo (IMC): This method uses stochastic simulations of photon transport to iteratively adjust (\mua) and (\mus) until the simulated (R) and (T) match the experimental measurements [8]. While computationally intensive, it is considered very accurate and can handle complex geometries.
- Spatial/Frequency Domain Techniques: These advanced methods analyze the spatial distribution of diffuse reflectance or the modulation and phase shift of intensity-modulated light to separate the effects of absorption and scattering [8].
Table 3: Summary of Inverse Models for Estimating Optical Properties [7] [8]
| Model/Method | Primary Inputs | Key Advantages | Key Limitations |
|---|---|---|---|
| Kubelka-Munk (KM) | R, T, sample thickness | Simple, analytical solution; fast computation | Less accurate for low-scattering or highly absorbing samples |
| Inverse Adding-Doubling (IAD) | R, T, sample thickness | High accuracy; works for a wide range of optical properties | Requires a layered geometry |
| Inverse Monte Carlo (IMC) | R, T, sample thickness | High accuracy; can model complex geometries | Computationally intensive and slow |
| Spatial/Frequency Domain | Spatially/temporally resolved reflectance | Can directly separate μa and μs' in vivo | Requires specialized source-detector hardware |
The Scientist's Toolkit: Research Reagent Solutions
Successful experimentation in biophotonics relies on a suite of essential materials and instruments. The following table details key components of a research toolkit for studying light-tissue interactions.
Table 4: Essential Research Tools for Biophotonics Experiments
| Item / Reagent | Function / Purpose |
|---|---|
| Integrating Sphere | Collects all light transmitted through or reflected from a sample, enabling accurate measurement of total diffuse reflectance (R) and transmittance (T) [7]. |
| Miniature Spectrometer | Resolves the wavelength composition of light, used for acquiring fluorescence, reflectance, and transmittance spectra [7]. |
| DPSS Lasers | (Diode-Pumped Solid-State Lasers) provide high-intensity, monochromatic light sources for excitation in techniques like LIF and for probing tissue optical properties [7]. |
| Tissue-Mimicking Phantoms | Standardized materials with known optical properties (e.g., using Intralipid for scattering, India ink for absorption) used for system calibration and validation of models [8]. |
| Digital Micrometer | Precisely measures sample thickness, a critical parameter for accurate inversion of optical properties using models like KM and IAD [7]. |
| Optical Fiber Probes | Deliver light to the sample and collect emitted or reflected light, enabling flexible experimental configurations and in-situ measurements [7]. |
| Kubelka-Munk Model | A mathematical transport model used to directly calculate absorption and scattering coefficients from measured R and T values [7]. |
Visualization of Light-Tissue Interactions and Data Analysis
Understanding the journey of light through tissue and the subsequent data analysis is crucial for interpreting experimental results. The following diagram illustrates the fundamental physical processes and the parallel workflow for analytical modeling.
Figure 2: Light-tissue interaction processes and analytical workflow.
Biophotonics, defined as the interdisciplinary fusion of light-based technologies with biology and medicine, uses the properties of photons to analyze and manipulate biological materials [1]. This field leverages the fundamental interactions between light and biological matter—including absorption, emission, reflection, and scattering—to advance our understanding of life processes at the molecular, cellular, tissue, and organ levels [1]. Among its many capabilities, three core advantages make biophotonics a transformative technology in life sciences and medical diagnostics: non-invasiveness, high sensitivity, and real-time measurement. These characteristics allow researchers and clinicians to observe biological processes in their native state, detect minute quantities of analytes, and monitor dynamic events as they unfold, thereby providing a powerful toolkit for biomedical research, drug development, and clinical diagnostics.
The non-contact nature of optical measurements allows for the observation of living cells and tissues without compromising their integrity, thereby preserving biological function and enabling longitudinal studies in vivo [1]. The sensitivity of biophotonic techniques can reach the level of single molecules, which is essential for understanding fundamental biological processes and detecting early disease biomarkers [1]. Furthermore, the speed of light enables optical technologies to provide rapid, real-time data, significantly reducing the time required for data interpretation and diagnosis [1]. This combination of attributes positions biophotonics as a cornerstone technology for next-generation precision medicine and the One Health approach, with applications spanning oncology, infectious diseases, neurology, cardiovascular health, and beyond [1].
Non-Invasiveness in Biophotonic Technologies
Fundamental Principles and Biological Interactions
The non-invasive character of biophotonics stems from the ability of light, particularly wavelengths in the near-infrared window, to penetrate biological tissues with minimal damage or disruption. This property enables researchers to probe living systems without physical contact or the need for exogenous labels in many cases, preserving the integrity of the biological specimen under investigation [1]. Label-free techniques such as optical coherence tomography (OCT), vibrational microspectroscopy (infrared and Raman scattering), and second harmonic generation (SHG) leverage inherent optical properties of tissues to generate contrast, allowing for repeated measurements over time without cumulative toxic effects [1].
Techniques based on nonlinear optical phenomena, such as multi-photon microscopy, are particularly valuable for non-invasive deep tissue imaging. The simultaneous absorption of two or three photons leads to precise localization of signal sources since such nonlinear processes only occur in an extremely small volume, thereby minimizing out-of-focus photodamage and allowing for high-resolution imaging deep within living tissues [1]. This capability has revolutionized the study of dynamic biological processes in their native context, from neural activity in the brain to immune cell trafficking in tumors.
Applications in Live-Cell and In-Vivo Imaging
Non-invasive biophotonic imaging has become indispensable for studying infectious diseases in animal models, where the same group of animals can be imaged repeatedly throughout an experiment [10]. This approach significantly refines animal models by allowing each animal to serve as its own control, reducing biological variability, and providing extremely accurate data on disease progression [10]. Furthermore, the appearance of specific photonic signals can serve as early indicators of disease outcomes, enabling humane intervention before the onset of clinical symptoms [10].
In clinical settings, non-invasive biophotonic techniques are transforming diagnostic paradigms. Optical coherence tomography (OCT) provides label-free, high-resolution optical imaging with sufficient sampling frequency for intraoperative evaluation, functioning as an "optical biopsy" that generates images comparable to histological sections without tissue removal [11]. Similarly, breath analysis using laser absorption spectroscopy and surface-enhanced Raman spectroscopy detects volatile organic compounds (VOCs) as biomarkers for diseases including tuberculosis, lung cancer, chronic obstructive pulmonary disease, and even mental disorders like schizophrenia [12]. These approaches offer completely non-invasive diagnostic avenues that could potentially replace or supplement conventional invasive procedures.
High Sensitivity of Biophotonic Methods
Technological Foundations of Sensitivity
The exceptional sensitivity of biophotonic methods arises from advanced detector technologies and sophisticated signal amplification strategies. Sensitive photon detectors based on cooled or intensified charge-coupled device (CCD) cameras can detect extremely dim light signals emitted from within living organisms [10]. These systems operate by detecting visible light that arises from either the excitation of fluorescent molecules or from enzyme-catalyzed oxidation reactions (bioluminescence), enabling researchers to observe and quantify the spatial and temporal distribution of light production from within living animals [10].
The development of biophotonic probes from natural materials and biological entities represents a significant advancement in sensitive detection. Biological lasers (biolasers), which utilize naturally derived biomaterials as part of the laser cavity and/or gain medium, can serve as highly sensitive probes for detecting biological signals at molecular, cellular, and tissue levels [13]. Compared to traditional fluorescence emission, lasing probes exhibit much narrower linewidth, stronger light intensity, higher sensitivity, and superior spectral and spatial resolution due to unique optical feedback mechanisms and threshold characteristics [13]. Similarly, nanophotonic biosensors that incorporate plasmonic nanoparticles, quantum dots, and photonic crystals enable ultrasensitive tracking of DNA, proteins, and biomarkers in minute volumes, facilitating enhanced disease screening and early-stage cancer detection [2].
Single-Molecule and Single-Cell Detection
The sensitivity of biophotonic technologies extends to the ultimate limit of detection—single molecules. Optical technologies allow for ultrasensitive detection down to single molecules, which is essential for understanding fundamental biological processes [1]. This capability has been demonstrated in techniques such as fluorescence correlation spectroscopy, surface-enhanced Raman spectroscopy, and zero-mode waveguides, enabling researchers to observe biochemical reactions and molecular interactions at previously inaccessible resolutions.
At the cellular level, biophotonic flow cytometry and imaging flow cytometry combine the statistical power of conventional flow cytometry with the detailed imagery of microscopy, allowing for high-throughput analysis and sorting of individual cells based on both phenotypic and morphological characteristics. These technologies have become indispensable tools in immunology, cancer biology, and stem cell research, where rare cell populations must be identified and isolated from complex mixtures with high precision and recovery rates.
Table 1: Quantitative Sensitivity Metrics of Selected Biophotonic Technologies
| Technology | Detection Limit | Spatial Resolution | Temporal Resolution | Key Applications |
|---|---|---|---|---|
| Single-Molecule Spectroscopy | Single molecules | <10 nm | Milliseconds | Protein folding, enzyme kinetics, molecular interactions |
| Biolasers | ~100 molecules in microcavity [13] | Diffraction-limited | Nanoseconds | Intracellular sensing, biomarker detection |
| Surface-Enhanced Raman Spectroscopy | Single molecules | ~20 nm | Seconds | VOC detection, pathogen identification [12] |
| Cooled CCD Imaging | <100 photons/sec/cm²/steradian [10] | 20-100 μm (in vivo) | Seconds to minutes | Bioluminescence imaging, infectious disease tracking [10] |
| Multiphoton Microscopy | ~100 fluorescent molecules | ~300 nm | Microseconds to seconds | Deep tissue imaging, neuronal activity |
Real-Time Measurement Capabilities
Technologies Enabling Real-Time Monitoring
Real-time measurement represents one of the most significant advantages of biophotonic technologies, stemming from the inherent speed of light and the development of high-speed detectors. Optical measurements provide rapid, real-time data, significantly reducing the time required for data interpretation and diagnosis [1]. This capability allows researchers to monitor biological processes as they unfold, rather than inferring dynamics from static snapshots. Technologies such as fluorescence lifetime imaging (FLIM), Förster resonance energy transfer (FRET), and total internal reflection fluorescence (TIRF) microscopy provide insights into molecular interactions, conformational changes, and cellular signaling events with temporal resolutions ranging from hours to ultrafast reactions [1] [14].
The integration of biophotonics with microfluidic systems has further enhanced real-time monitoring capabilities, particularly in the context of high-throughput screening and diagnostics. Lab-on-a-chip platforms incorporating optical biosensors enable continuous monitoring of cellular responses, enzyme activities, and molecular interactions with millisecond temporal resolution. These systems are particularly valuable in pharmaceutical research, where real-time assessment of compound effects on cellular models can accelerate drug discovery and reduce development costs.
Dynamic Process Monitoring in Research and Clinical Settings
In infectious disease research, real-time biophotonic imaging has transformed our understanding of host-pathogen interactions. The nondestructive nature of biophotonic imaging allows the course of an infection to be monitored by imaging the photonic signal detected from within the same group of animals over time [10]. This approach provides unprecedented accuracy in tracking disease progression, from initial colonization through dissemination and, ultimately, to resolution or lethal outcome. Importantly, real-time imaging can immediately detect errors in inoculation administration, allowing researchers to eliminate affected animals from studies—thus minimizing potential suffering and reducing flawed scientific data [10].
In clinical environments, real-time biophotonic technologies are being integrated into surgical and diagnostic workflows. Optical coherence tomography (OCT) is one of the fastest methods in terms of volume elements imaged per second, enabling real-time 3D imaging of dynamic processes [1]. This capability has established OCT as a gold standard in ophthalmology and is increasingly being applied in interventional cardiology and oncology. Similarly, rapid evidential breath analyzers based on laser absorption spectroscopy are being developed for point-of-care detection of infections and metabolic disorders, providing results in minutes rather than the hours or days required for conventional culture-based or laboratory tests [12].
Experimental Protocols and Methodologies
Protocol: Non-Invasive Biophotonic Imaging of Infection Dynamics
This protocol outlines the methodology for tracking infectious disease progression in live animal models using biophotonic imaging, based on established practices in the field [10].
Principle: Pathogens engineered to express luciferase or fluorescent proteins can be detected and quantified non-invasively in living animals using sensitive photon detectors. The light signal produced is proportional to pathogen burden, allowing for real-time monitoring of infection dynamics.
Materials:
- Bioluminescent or fluorescent pathogen strain (e.g., luxCDABE-transfected bacteria)
- Appropriate animal model (e.g., mouse)
- Cooled CCD camera system mounted in light-tight chamber
- Anesthesia system (e.g., isoflurane vaporizer)
- Depilatory cream for hair removal
- Living Image or equivalent image analysis software
- Sterile PBS for inoculum preparation
Procedure:
- Preparation of Inoculum:
- Grow bioluminescent pathogens to mid-log phase.
- Wash and resuspend in sterile PBS to desired concentration.
- Confirm luminescence using plate reader or preliminary imaging.
Animal Preparation:
- Anesthetize animal using appropriate anesthetic (e.g., 2-3% isoflurane).
- Remove hair from imaging area using depilatory cream to minimize light absorption.
- Administer pathogen via appropriate route (e.g., intranasal, intravenous, intraperitoneal).
Image Acquisition:
- Place anesthetized animal in light-tight imaging chamber.
- Maintain anesthesia throughout imaging procedure.
- Acquire series of images with varying exposure times (typically 30 seconds to 5 minutes).
- Include uninjected control animal to assess background luminescence.
- For fluorescence imaging, select appropriate excitation and emission filters.
Data Analysis:
- Use imaging software to quantify total photon flux (photons/sec/cm²/steradian) within regions of interest.
- Normalize signals to background levels from control animals.
- Generate kinetic curves of pathogen burden by repeated imaging of the same animals over time.
- Correlate bioluminescence signals with conventional metrics (e.g., colony-forming units from homogenized tissues).
Troubleshooting:
- Low signal may require increased exposure time or use of more sensitive camera.
- High background may indicate incomplete removal of hair or contamination.
- Signal saturation can be addressed by reducing exposure time or camera binning.
Protocol: Real-Time VOC Detection in Breath Samples
This protocol describes the detection of volatile organic compounds in breath for non-invasive disease diagnosis using biophotonic technologies [12].
Principle: Disease-specific volatile organic compounds present in exhaled breath can be detected and quantified using laser absorption spectroscopy or surface-enhanced Raman spectroscopy, providing a non-invasive diagnostic approach.
Materials:
- Laser absorption spectrometer or surface-enhanced Raman spectroscopy system
- Breath collection apparatus (e.g., Bio-VOC sampler)
- Nanostructured metal surfaces for SERS (e.g., gold or silver nanoparticles)
- Calibrated gas standards for target VOCs
- Data analysis software with machine learning capabilities
Procedure:
- Sample Collection:
- Instruct subject to exhale normally, then collect alveolar breath using specialized sampler.
- Transfer breath sample immediately to analysis chamber.
- For SERS analysis, preconcentrate VOCs on nanostructured surfaces.
Instrument Setup:
- For laser absorption spectroscopy: tune laser to absorption wavelength of target VOC.
- For SERS: functionalize nanostructures with selective capture agents if necessary.
- Calibrate instrument using certified gas standards at known concentrations.
Measurement:
- Direct breath sample through flow cell for laser absorption measurements.
- For SERS, expose functionalized nanoparticles to breath sample and acquire spectra.
- Perform multiple technical replicates for statistical robustness.
- Include control samples from healthy subjects for comparison.
Data Analysis:
- For laser absorption: quantify VOC concentration based on Beer-Lambert law.
- For SERS: identify characteristic Raman peaks of target VOCs.
- Apply machine learning algorithms to spectral data for pattern recognition.
- Generate classification models to distinguish disease states based on VOC profiles.
Validation:
- Compare biophotonic results with gold standard diagnostic methods.
- Assess sensitivity, specificity, and accuracy using receiver operating characteristic curves.
- Determine limit of detection and quantitative range for each target VOC.
Visualization of Biophotonic Concepts and Workflows
Technology Relationship Diagram
Diagram 1: Fundamental workflow of biophotonic systems and their core advantages. The diagram illustrates how light interacts with biological samples to generate detectable signals, with each stage enabled by specific technological advantages.
In-Vivo Infection Imaging Workflow
Diagram 2: Experimental workflow for non-invasive biophotonic imaging of infections. The process highlights how core advantages integrate at specific stages to enable longitudinal monitoring of disease progression in live animals.
Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Biophotonic Applications
| Reagent/Material | Function | Example Applications | Technical Considerations |
|---|---|---|---|
| Luciferase Enzymes | Catalyzes light-producing oxidation reactions | In vivo bioluminescence imaging, reporter gene assays | Requires substrate (e.g., D-luciferin); different luciferases vary in emission wavelength and kinetics |
| Fluorescent Proteins (GFP, RFP, etc.) | Genetic encoding of fluorescence | Cell tracking, gene expression monitoring, protein localization | Photostability, maturation time, and oligomerization state vary between variants |
| Quantum Dots | Nanocrystals with bright, tunable fluorescence | Long-term cell tracking, multiplexed detection, in vivo imaging | Potential cytotoxicity; surface coating critical for biocompatibility |
| SERS Nanoparticles | Enhances Raman scattering signals | Ultrasensitive detection, VOC profiling, multiplexed assays | Composition (Au, Ag) and morphology affect enhancement factors |
| Bioluminescent Substrates | Fuel for luciferase-mediated light production | In vivo imaging, ATP detection, cytotoxicity assays | Pharmacokinetics and bioavailability affect in vivo applications |
| Near-Infrared Dyes | Fluorescent probes with deep tissue penetration | In vivo imaging, surgical guidance, perfusion assessment | Spectral overlap with tissue autofluorescence must be considered |
| Optical Clearing Agents | Reduce light scattering in tissues | Deep tissue imaging, whole-organ microscopy | Must balance clearing efficacy with preservation of fluorescence |
| Functionalized Biosensors | Detect specific analytes or enzymatic activities | Metabolite monitoring, protease activity, pH sensing | Specificity, dynamic range, and response time are critical parameters |
The synergistic combination of non-invasiveness, high sensitivity, and real-time measurement establishes biophotonics as an indispensable technology platform for biomedical research and clinical diagnostics. These core advantages enable researchers to interrogate biological systems with minimal perturbation, detect increasingly subtle molecular signals, and observe dynamic processes as they unfold in living systems. As biophotonic technologies continue to evolve—driven by advances in laser sources, detector technologies, nanophotonics, and computational analytics—their impact will expand across diverse fields including basic research, drug discovery, clinical diagnostics, and personalized medicine. The integration of artificial intelligence with biophotonic systems promises to further enhance analytical capabilities, enabling automated interpretation of complex data and potentially uncovering novel biological insights that would otherwise remain obscured. With continuous technological innovation and growing adoption across life sciences and medicine, biophotonics is poised to remain at the forefront of scientific discovery and medical advancement for the foreseeable future.
Biophotonics, the fusion of light-based technologies with biology and medicine, is a cornerstone of 21st-century scientific innovation, revolutionizing research, diagnostics, and therapy [1]. This discipline leverages the properties of light to analyze and manipulate biological materials, enabling unprecedented precision in measuring and understanding life processes from the molecular to the organ level [1]. The core advantages of using light in biomedical applications include its capacity for non-contact measurement, which preserves the integrity of living cells; high sensitivity, allowing for detection down to single molecules; and superior time resolution, facilitating the observation of dynamic biological processes in real-time [1].
The field of biophotonics can be broadly divided into three main technological areas:
- Bioimaging: Photonics enables the characterization of biological specimens across multiple spatial scales, from nanoscopic intracellular interactions to macroscopic tissues [1].
- Biosensing: Photonic-based approaches allow for the detection of biomolecules, such as disease-specific biomarkers, with extreme sensitivity [1].
- Photonic Therapy: Lasers and other light sources facilitate highly precise and minimally invasive surgical interventions and treatments, with bioimaging and biosensing enabling real-time monitoring of efficacy [1].
Central to all these applications is the interaction between light and biological matter, primarily through processes of absorption, emission, scattering, and reflection. The choice of light source is critical, as it determines the specificity, depth, and resolution of the interaction. This guide provides an in-depth examination of the three essential light sources—Lasers, Light Emitting Diodes (LEDs), and Superluminescent Diodes (SLEDs)—that power modern biophotonics.
Fundamental Principles and Comparative Analysis
The operational principles of Lasers, LEDs, and SLEDs define their unique output characteristics and, consequently, their suitability for specific biomedical applications.
Lasers (Light Amplification by Stimulated Emission of Radiation) operate on the principle of stimulated emission [15]. They produce highly coherent, monochromatic light with a narrow spectral bandwidth and high optical power density [15]. This coherence, while beneficial for focusing light to a small spot, leads to significant speckle—a grainy interference pattern that can degrade image quality in certain imaging systems [15].
Light Emitting Diodes (LEDs) generate light through electroluminescence and spontaneous emission [15]. They are incoherent sources that emit a broad spectrum of light, resulting in low optical power density and very short coherence lengths [15] [16]. This inherent incoherence makes them immune to speckle noise.
Superluminescent Diodes (SLEDs or SLDs) bridge the gap between lasers and LEDs. They function similarly to laser diodes but are designed to suppress optical feedback, producing amplified spontaneous emission (ASE) [15] [17]. This results in a combination of laser-like properties (such as high output power and high spatial coherence) with LED-like properties (broad spectral bandwidth and low temporal coherence) [15] [17]. This unique combination minimizes speckle while maintaining high intensity, making SLEDs ideal for high-precision imaging [15].
Table 1: Fundamental Operating Principles of Lasers, LEDs, and SLEDs.
| Feature | Laser (LD) | Superluminescent Diode (SLED) | Light Emitting Diode (LED) |
|---|---|---|---|
| Operating Principle | Stimulated Emission | Amplified Spontaneous Emission (ASE) | Spontaneous Emission |
| Light Coherence | High (Coherent) | Medium (Low Temporal Coherence) | Low (Incoherent) |
| Spectral Bandwidth | Narrow (several nm or less) [16] | Medium (10-50 nm) [16] | Broad (up to ~100 nm) [16] |
| Optical Output Power | High (several hundred mW) [16] | Medium (tens of mW) | Low [15] |
| Coherence Length | Long (several dozen cm to meters) [16] | Short (~40-50 µm) [16] | Very Short (up to ~20 µm) [16] |
| Speckle Effect | High [15] | Low [15] | None |
Table 2: Summary of Key Characteristics and Biomedical Applications.
| Characteristic | Laser | SLED | LED |
|---|---|---|---|
| Spectral Nature | Narrowband, coherent | Broadband, low coherence | Broadband, incoherent |
| Power Density | High [15] | Medium [15] | Low [15] |
| Primary Biomedical Applications | Laser surgery, skin treatments, flow cytometry, DNA sequencers [15] | Optical Coherence Tomography (OCT), fiber-optic sensors [17] | Phototherapy (e.g., acne, jaundice, wound healing), photo rejuvenation [18] [19] |
| Key Advantages in Biomedicine | High precision, ability to deliver high energy for ablation and surgery | High resolution in imaging due to broadband source, reduced speckle [15] | Safety, low cost, ability to treat large areas, portability [19] |
Lasers in Biomedicine
Key Applications and Experimental Protocols
Lasers are indispensable tools in therapeutic and diagnostic applications requiring high precision and power.
- Laser Surgery and Skin Treatments: Lasers are used for highly precise and minimally invasive surgical procedures, including skin resurfacing and the treatment of various skin lesions [15] [1]. The protocol involves selecting a specific wavelength (e.g., Er:YAG for ablation) and pulse duration to match the absorption characteristics of the target tissue (e.g., water for soft tissue), thereby minimizing collateral damage to surrounding areas.
- Photodynamic Therapy (PDT) for Oncology: This treatment involves administering a photosensitizing drug (e.g., Aminolevulinic Acid - ALA or its ester, MAL) that accumulates preferentially in target cells, such as cancer cells [18]. The target area is then irradiated with a specific wavelength of laser light (e.g., red light at 633 nm for deep penetration), which activates the drug, triggering a photochemical reaction that generates cytotoxic reactive oxygen species and destroys the target cells [18]. Clinical studies have shown high efficacy, with one study reporting a 95% response rate for MAL-PDT in treating Bowen's disease [18].
- Advanced Bioimaging: Non-linear laser microscopy techniques, such as Multi-Photon Microscopy, leverage high-intensity, ultrashort-pulsed lasers (e.g., Ti:Sapphire) to enable high-resolution imaging deep within scattering biological tissues [1]. The simultaneous absorption of two or three photons provides precise spatial localization, allowing for the study of dynamic processes in live cells and tissues with minimal photodamage and out-of-focus bleaching.
Diagram 1: Laser experiment workflow.
Light-Emitting Diodes (LEDs) in Biomedicine
Key Applications and Experimental Protocols
LEDs have emerged as a safe, cost-effective, and versatile light source for a range of therapeutic applications, particularly in dermatology and regenerative medicine.
- Blue LED for Acne Treatment: Blue light (around 415 nm) is used to treat acne vulgaris through a natural photodynamic effect [18]. The protocol involves irradiating the affected skin area with blue LED light. The light is absorbed by endogenous porphyrins (mainly coproporphyrin III) produced by Propionibacterium acnes, which generates cytotoxic singlet oxygen and other free radicals, leading to bacterial destruction and a reduction in inflammation [18]. A typical clinical protocol might involve treatments twice weekly for several weeks [18].
- Red and Near-Infrared LED for Wound Healing and Photobiomodulation: Red (630-700 nm) and infrared (800-1200 nm) LEDs are used to accelerate wound healing and reduce inflammation [18]. The proposed mechanism involves the absorption of light by mitochondrial chromophores (e.g., cytochrome c oxidase), leading to increased ATP production, modulation of reactive oxygen species, and the induction of transcription factors that promote tissue repair and angiogenesis [18]. A sample experimental methodology for a rodent wound healing model would involve creating standardized wounds, followed by daily irradiation with a red LED (e.g., 670 nm) at a specific power density (e.g., 50 mW/cm²) and energy density (e.g., 4 J/cm²), with wound size measured regularly until closure [18].
- LED-based Phototherapy for Neurological and Mood Disorders: Narrow-band blue LED light has been investigated for treating Seasonal Affective Disorder (SAD) by helping to regulate circadian rhythms [19]. The treatment involves daily exposure to a blue LED light source, which influences melatonin production and serotonin levels, thereby improving mood and alertness.
Table 3: LED-Based Phototherapy Parameters for Common Applications.
| Condition | LED Wavelength | Typical Parameters | Mechanism of Action |
|---|---|---|---|
| Acne Vulgaris [18] | Blue (415 nm) | 40-50 J/cm², twice weekly | Activation of bacterial porphyrins, leading to bacterial destruction via reactive oxygen species. |
| Skin Rejuvenation & Wound Healing [18] | Red (633 nm) | 50-200 mW/cm², 1-5 J/cm², daily | Stimulation of fibroblast activity, increased collagen production, and enhanced cellular metabolism. |
| Wound Healing (Deep Tissue) [18] | Near-Infrared (830 nm) | N/A | Stimulation of circulation, angiogenesis, and growth factor production. |
| Seasonal Affective Disorder (SAD) [19] | Blue (~470 nm) | Daily exposure sessions | Regulation of circadian rhythm via suppression of melatonin and modulation of serotonin. |
Superluminescent Diodes (SLEDs) in Biomedicine
Key Applications and Experimental Protocols
SLEDs find their niche in high-resolution biomedical imaging and sensing applications where their unique combination of high spatial coherence and broad bandwidth is critical.
- Optical Coherence Tomography (OCT): This is the foremost application of SLEDs in biomedicine [17]. OCT is a non-invasive imaging technique that captures micrometer-resolution, three-dimensional images from within optical scattering media, such as biological tissue [17]. The broad bandwidth of the SLED light source directly determines the axial resolution of the system; a broader spectrum yields finer resolution [17]. The protocol involves splitting the SLED's broadband light into a sample arm and a reference arm. The light reflected from the sample and the reference mirror is recombined, and the resulting interference pattern is analyzed to construct a depth profile (A-scan). By scanning the beam across the sample, a 2D or 3D image (B-scan) is generated [17]. Frequency-domain OCT, which uses a spectrally scanning SLED source and calculates the depth scan via a Fourier transform, has dramatically improved imaging speed and is now widely established in ophthalmology for retinal imaging and in cardiology for intravascular diagnostics [1] [17].
- White-Light Interferometry for Surface Metrology: SLEDs are used as broadband sources in interferometers to measure the surface topology of materials, including biological specimens and medical implants [17]. The system works by finding the position of zero optical path difference between the sample and reference beams, which results in a localized interference fringe. This allows for highly precise, non-contact measurements of surface roughness and shape.
- Fiber-Optic Sensing: SLEDs are ideal light sources for various fiber-optic sensors, including those measuring strain, temperature, and pressure in harsh biological or environmental conditions [17]. For example, in a Fiber Bragg Grating (FBG) sensor, the broad spectrum of the SLED is used to interrogate a grating written into an optical fiber. Changes in strain or temperature shift the reflected wavelength, which can be detected and quantified [17].
Diagram 2: SLED-based OCT system.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Biophotonics Research.
| Item | Function/Application |
|---|---|
| Aminolevulinic Acid (ALA) / Methyl Aminolevulinate (MAL) | Topical photosensitizers used in Photodynamic Therapy (PDT). Metabolized in the target cells to form protoporphyrin IX, which is activated by laser or LED light to produce cytotoxic effects [18]. |
| Exogenous Porphyrins (e.g., Protoporphyrin IX) | Naturally occurring molecules in bacteria that act as endogenous photosensitizers for blue LED acne therapy [18]. |
| Cell Viability Assays (e.g., MTT Assay) | Used to quantify the therapeutic or cytotoxic effects of light-based treatments on cell cultures in vitro. |
| Specific Culture Media for P. acnes | Used to culture the bacteria for in vitro studies validating the efficacy of blue LED antimicrobial photodynamic therapy [18]. |
| Animal Models (e.g., Rodent Wound Model) | Preclinical in vivo models for studying the effects of LED photobiomodulation on wound healing, inflammation, and tissue regeneration [18]. |
| Optical Phantoms | Tissue-simulating materials with controlled optical properties (scattering and absorption coefficients) used to calibrate and validate imaging systems like OCT before use on biological samples. |
| Fibroblast Cell Lines | Commonly used in vitro models to study the effects of red and infrared LED light on collagen synthesis, proliferation, and other wound-healing pathways [18]. |
Lasers, LEDs, and Superluminescent Diodes each provide a distinct set of optical properties that make them uniquely suited for specific applications within the rapidly expanding field of biophotonics. The global biophotonics market, valued at $62.6 billion in 2024 and projected to reach $113.1 billion by 2030, is a testament to the transformative impact of these technologies on healthcare and life sciences [20]. The convergence of these light sources with artificial intelligence, novel materials, and quantum sensing promises to further redefine the boundaries of precision medicine, fundamental biological research, and the "One Health" approach, solidifying biophotonics as a cornerstone of future medical and scientific progress [1].
Biophotonics is an interdisciplinary field at the intersection of photonics and biology that involves the study of light interaction with biological matter, as well as the development and application of optical techniques for biological research and medicine [21]. This field leverages the properties of photons—particles of light—to probe, image, manipulate, and treat biological systems across scales from single molecules to entire organisms. The scope of biophotonics research is vast, encompassing fundamental studies of biological structure and function, development of novel diagnostic tools, discovery of new drugs, and creation of advanced therapeutic modalities.
Within this expansive field, three particularly promising areas have emerged: bioluminescence, biofluorescence, and biolasers. These technologies represent a continuum of sophistication in harnessing light for biological applications. Bioluminescence utilizes naturally occurring biochemical reactions to produce light without external excitation. Biofluorescence, while also endogenous, requires external light excitation for emission. Biolasers represent the most advanced frontier, incorporating biological materials or entire biological systems into laser cavities to generate coherent, highly directional light with unique properties for sensing and imaging. Together, these technologies are revolutionizing how researchers detect, monitor, and understand biological processes, offering unprecedented sensitivity, specificity, and temporal resolution for scientific discovery and therapeutic development.
Bioluminescence: Nature's Inner Light
Fundamental Principles and Mechanisms
Bioluminescence is the fascinating natural phenomenon by which living organisms produce and emit light through biochemical reactions [22]. This process occurs when the oxidation of a small-molecule luciferin is catalyysed by an enzyme luciferase to form an excited-state species that emits light [22]. Unlike fluorescence, bioluminescence does not require the absorption of sunlight or other external electromagnetic radiation to generate light, which eliminates issues with sample autofluorescence, quenching, and heating [23]. The bioluminescence reaction generally requires a luciferase enzyme, its luciferin substrate, and an oxidant (typically molecular oxygen), with some systems additionally requiring energy cofactors such as ATP [22].
The firefly (Photinus pyralis) bioluminescence system represents one of the most thoroughly characterized and widely utilized luciferase-luciferin pairs. In this system, the 62 kDa insect luciferase (FLuc) catalyses the oxidation of D-luciferin in two distinct steps: first, the carboxyl group of D-luciferin is activated through adenylation by ATP; second, the resulting luciferyl-adenylate intermediate is oxidized to form an excited-state oxyluciferin species through a dioxetanone intermediate [22]. The excited-state oxyluciferin relaxes to its ground state by emitting a photon of light, typically in the yellow-green region (peak ~560 nm) [24]. This system achieves a remarkably high quantum yield of up to 41% at optimal pH conditions [22].
Figure 1: Firefly bioluminescence mechanism involving luciferyl-adenylate intermediate formation and subsequent light emission.
Major Bioluminescent Systems and Their Characteristics
While over 30 distinct bioluminescent systems exist in nature, the luciferin-luciferase pairs of only about 11 systems have been characterized to date [22]. The most widely utilized systems in research include D-luciferin-dependent systems (from fireflies and click beetles), coelenterazine-dependent systems (from marine organisms), and bacterial bioluminescent systems [23]. Each system possesses unique characteristics that make it suitable for specific applications.
D-luciferin-dependent systems are found in various lineages of beetles including fireflies, click beetles, and railroad worms [23]. These systems typically emit light across yellow, orange, and in some cases, red wavelengths [23]. The firefly luciferase system is particularly valuable because its dependence on ATP enables its application in studies of cellular metabolism and energy status [23]. Click beetle luciferases offer additional versatility, with natural variants emitting different colors ranging from green (540 nm) to orange-red (593 nm) without modification [23].
Coelenterazine-dependent systems represent the most widespread bioluminescent system in marine ecosystems, found in organisms including the sea pansy Renilla reniformis, the copepod Gaussia princeps, and the decapod shrimp Oplophorus gracilirostris [23]. These systems do not require ATP and typically emit blue light between 450-500 nm [23]. The engineered Oplophorus luciferase (NanoLuc) represents a particularly advanced system with exceptional brightness, small size (19 kDa), and high stability, making it ideal for numerous research applications [23] [24].
Table 1: Characteristics of Major Bioluminescent Systems Used in Research
| Luciferase | Source Organism | Luciferin | Size (kDa) | Emission Maximum | Cofactors | Key Applications |
|---|---|---|---|---|---|---|
| Firefly Luciferase (FLuc) | Photinus pyralis | D-luciferin | 61 | 560 nm | ATP, Mg²⁺, O₂ | ATP sensing, in vivo imaging, reporter assays |
| Click Beetle Luciferase (CBR) | Pyrophorus plagiophthalamus | D-luciferin | 61 | 538-615 nm | ATP, Mg²⁺, O₂ | Multiplexed imaging, reporter assays |
| Renilla Luciferase (RLuc) | Renilla reniformis | Coelenterazine | 36 | 480 nm | O₂ | Dual-reporter assays, BRET |
| Gaussia Luciferase (GLuc) | Gaussia princeps | Coelenterazine | 20 | 473 nm | O₂ | Secreted reporter assays, high-throughput screening |
| NanoLuc Luciferase | Oplophorus gracilirostris | Furimazine | 19 | 460 nm | O₂ | Protein-protein interactions, high-sensitivity detection |
| Bacterial Luciferase | Photorhabdus luminescens | Fatty aldehyde | >200 | 490 nm | FMNH₂, O₂ | Bacterial labeling, continuous light production |
Research Applications and Experimental Protocols
Bioluminescence has become an indispensable tool across diverse research areas due to its exceptional sensitivity, low background, and compatibility with living systems. Key applications include gene expression reporter assays, in vivo imaging in small animal models, protein-protein interaction studies using techniques such as Bioluminescence Resonance Energy Transfer (BRET), and high-throughput drug screening [22] [24].
Protocol: Bioluminescent Reporter Gene Assay for Gene Expression Monitoring
Principle: Cells are transfected with a plasmid in which the gene of interest controls expression of a luciferase reporter. Luciferase activity directly correlates with transcriptional activity of the gene being studied [24].
Materials:
- Mammalian cells expressing luciferase reporter construct
- Appropriate luciferin substrate (D-luciferin for firefly systems, coelenterazine for marine systems)
- Cell culture medium and reagents
- Luminometer or cooled CCD camera for detection
- Lysis buffer (for endpoint assays)
- White-walled multiwell plates (to minimize cross-talk)
Procedure:
- Seed cells in multiwell plates and transfert with luciferase reporter construct
- Allow 24-48 hours for gene expression
- For endpoint assays: lyse cells with passive lysis buffer
- Add appropriate luciferin substrate to cells or lysate
- Measure light output immediately using luminometer or imaging system
- Normalize results to protein concentration or cell number
Critical Considerations:
- For firefly luciferase assays, include ATP and Mg²⁺ in assay buffer
- For live-cell kinetic measurements, use specialized media formulations that maintain cell viability while supporting bioluminescence reaction
- Consider substrate permeability when working with different luciferase systems
- For dual-reporter assays, ensure spectral separation of signals or use sequential measurement protocols
Protocol: In Vivo Bioluminescence Imaging of Tumor Growth in Mouse Models
Principle: Luciferase-expressing cells (e.g., tumor cells) are introduced into animal models. After administration of luciferin substrate, light emission is detected externally using a sensitive CCD camera, allowing non-invasive monitoring of cell proliferation and localization [24].
Materials:
- Luciferase-expressing cells (e.g., tumor cells transduced with lentiviral luciferase construct)
- Immunocompromised mice (e.g., nude or SCID mice)
- D-luciferin solution (15 mg/mL in PBS, sterile-filtered)
- Anesthesia system (isoflurane or injectable anesthetics)
- In vivo bioluminescence imaging system (e.g., IVIS Spectrum)
- Heating pad to maintain body temperature during imaging
Procedure:
- Establish tumors by injecting luciferase-expressing cells into appropriate site
- Allow tumors to establish (typically 1-4 weeks)
- Inject mice intraperitoneally with D-luciferin (150 mg/kg body weight)
- Anesthetize mice and place in imaging chamber
- Acquire images 10-20 minutes post-injection (peak signal time)
- Quantify total flux (photons/second) in region of interest
- Image repeatedly over time to monitor tumor progression
Critical Considerations:
- Optimize luciferin dose and timing for specific experimental setup
- Maintain consistent positioning and anesthesia depth between imaging sessions
- Consider substrate distribution kinetics when interpreting temporal patterns
- Account for potential effects of fur pigmentation on light attenuation
Table 2: Quantitative Performance Metrics of Common Bioluminescent Reporters
| Reporter System | Detection Sensitivity | Dynamic Range | Half-life | Quantum Yield | Molar Brightness |
|---|---|---|---|---|---|
| Firefly Luciferase | 10⁻¹⁸ - 10⁻²⁰ moles | 6-8 orders of magnitude | ~3 hours | 0.41 | High |
| Renilla Luciferase | 10⁻¹⁷ - 10⁻¹⁹ moles | 5-7 orders of magnitude | ~4 hours | 0.05-0.10 | Moderate |
| Gaussia Luciferase | 10⁻¹⁸ - 10⁻²⁰ moles | 6-8 orders of magnitude | ~6 days (secreted) | 0.10-0.15 | High |
| NanoLuc Luciferase | 10⁻¹⁹ - 10⁻²¹ moles | >7 orders of magnitude | >6 hours | ~0.30 | Very High |
Biofluorescence: Harnessing Nature's Light Absorbers
Principles and Comparison with Bioluminescence
Biofluorescence differs fundamentally from bioluminescence in its mechanism of light production. While bioluminescence generates light through biochemical reactions, fluorescence requires the absorption of external light at specific wavelengths followed by emission at longer wavelengths [25]. This process occurs when a fluorophore absorbs photons, elevating electrons to an excited state, followed by relaxation back to ground state with emission of lower-energy photons [25].
The most significant structural distinction between these phenomena lies in their requirements for external excitation. Fluorescence measurements require an external light source—typically a laser or high-intensity lamp—to excite the fluorophore, along with optical filters to separate excitation and emission light [25]. This requirement introduces several technical challenges including autofluorescence from biological samples, light scattering in turbid media, and photobleaching of fluorophores over time [25]. In contrast, bioluminescence generates its own light enzymatically, resulting in exceptionally low background and no need for external illumination [25].
Table 3: Comparison of Bioluminescence and Fluorescence Properties
| Property | Bioluminescence | Fluorescence |
|---|---|---|
| Signal Source | Enzymatic reaction (luciferase + substrate) | External excitation light |
| Background Signal | Low | Moderate to high (autofluorescence, scatter) |
| Sensitivity | High | Moderate to high |
| Photobleaching | Not applicable | Can occur |
| Multiplexing Capability | Limited | Excellent |
| Instrumentation Requirements | Luminometer | Filters, excitation source |
| Tissue Penetration Depth | Limited by signal strength | Limited by excitation penetration and autofluorescence |
| Common Applications | Reporter assays, live-cell kinetics, low-abundance targets | Imaging, flow cytometry, multiplex assays |
Fluorescent Proteins and Their Applications
The discovery and development of Green Fluorescent Protein (GFP) from the jellyfish Aequorea victoria revolutionized cell biology by enabling genetic encoding of fluorescence within living systems [26]. GFP consists of a cylindrical β-barrel structure measuring approximately 2.4 nm in diameter and 4.2 nm in height, with the actual fluorophore protected inside this structure [26]. This protective shell prevents close contact between fluorophores of neighbouring proteins, limiting intermolecular energy migration and reducing luminescence quenching even at high concentrations [26].
Enhanced GFP (eGFP) represents an optimized variant with improved light absorption characteristics. In solid-state films, eGFP demonstrates remarkable resistance to concentration quenching, with only approximately 7 dB (80%) reduction in fluorescence intensity compared to the theoretical maximum, while synthetic pyrromethene dyes show complete quenching under the same conditions [26]. This exceptional property enables eGFP to provide large optical gain (22 cm⁻¹ or 96 dB cm⁻¹) in solid-state configurations, making it suitable for laser applications [26].
Figure 2: Jablonski diagram illustrating fluorescence process with Stokes shift between absorption and emission.
Biolasers: Integrating Lasing with Biological Systems
Fundamental Principles of Biolasers
Biolasers represent the most technologically advanced frontier in biophotonics, integrating biological materials or entire biological systems into laser cavities to generate coherent light. An optofluidic bio-laser integrates biological materials into the gain medium while forming an optical cavity in a fluidic environment, either on a microfluidic chip or within a biological system [27]. The laser emission generated through this approach possesses characteristics fundamentally different from conventional fluorescence, with significantly enhanced sensitivity to specific molecular changes in the gain medium as the light-matter interaction is amplified by resonance in the cavity [27].
The fundamental components of any biolaser include: (1) a gain medium in the fluidic environment (biological or biologically-derived), (2) an optical cavity to provide feedback, and (3) a pumping mechanism to excite the gain medium [27]. The lasing threshold condition is expressed as n₁·σₑ(λ) = n₀·σₐ(λ) + γ꜀, where n₁ and n₀ are the concentrations of gain molecules in excited and ground states respectively, σₑ and σₐ are emission and absorption cross-sections, and γ꜀ is the cavity loss coefficient [27]. Below this threshold, the output comprises only weak spontaneous fluorescence, while above threshold, coherent stimulated emission builds up dramatically [27].
Cavity Designs and Integration Strategies
Various optical cavity architectures have been successfully implemented for biolaser applications, each offering distinct advantages for specific biological integration scenarios. The most common configurations include Fabry-Pérot cavities, whispering gallery mode (WGM) resonators, distributed feedback (DFB) gratings, and ring resonators [27] [28].
Whispering gallery mode (WGM) resonators represent the most prevalent architecture for biointegrated microlasers [28]. These structures confine light through continuous total internal reflection at the interface between a cylindrical or spherical resonator and the external environment [28]. WGM resonators offer extremely high-quality factors (regularly >10⁵) even at microscopic dimensions (diameters ≈1 μm), resulting in very narrow emission linewidths (generally below 0.1 nm) [28]. Their globular shape minimizes the risk of membrane puncture when internalized by cells, and their fabrication can be scaled to produce large numbers [28].
The resonance wavelengths of WGMs in a circular cavity with radius r can be approximated by 2πrnₑff ≈ mλₘ, where nₑff is the effective refractive index of the WGM with angular momentum mode number m, and λₘ is the associated resonance wavelength [28]. The spatial confinement of WGMs near the interface enables efficient excitation, while their evanescent field extends partially outside the resonator (typically <100 nm), allowing sensitive detection of refractive index changes near the resonator surface [28].
Implementation Protocols and Research Applications
Protocol: Implementation of Intracellular Microlasers for Cell Tracking
Principle: Microscopic lasers (microlasers) are internalized by cells, where their unique spectral signatures enable precise tracking of individual cells within complex populations or tissues. The significantly greater brightness and spectral narrowness of microlasers compared to fluorescent markers allows measurements in deeper tissue with greater distinguishability [28].
Materials:
- Whispering gallery mode (WGM) microresonators (typically 1-10 μm diameter)
- Mammalian cells for labeling
- Cell culture medium and reagents
- Pulsed pump laser (e.g., Q-switched solid-state laser, optical parametric oscillator)
- High-resolution hyperspectral imaging system
- Microinjection or phagocytosis protocols for resonator internalization
Procedure:
- Fabricate or source WGM microresonators with controlled size variations
- Incubate resonators with cells to facilitate internalization (phagocytosis)
- Verify internalization using microscopy
- Place labeled cells in appropriate imaging chamber
- Pump resonators with pulsed laser tuned to resonator absorption
- Collect emission spectra using hyperspectral imaging system
- Identify and track individual cells based on unique spectral signatures
Critical Considerations:
- Resonator size variations ensure unique spectral signatures for each cell
- Pump intensity must exceed lasing threshold but remain below cellular damage threshold
- Optimal pulse duration is approximately a tenth to several times the excited state lifetime of the gain molecule
- For in vivo applications, consider resonator biodegradability and long-term biocompatibility
Protocol: Biosensing Using Biointegrated Lasers
Principle: Changes in the biological environment surrounding or within the laser cavity alter its optical properties (refractive index, absorption, gain), resulting in measurable changes in laser output characteristics (threshold, intensity, spectrum) [27].
Materials:
- Optical cavity integrated with biological sample (cells, tissues, or molecules)
- Tunable pump laser system
- Spectrometer with high spectral resolution
- Microfluidic flow cell (for optofluidic implementations)
- Environmental control system (temperature, humidity, gas composition)
Procedure:
- Integrate biological sample with laser cavity (as gain medium or sensing element)
- Establish stable baseline laser operation
- Apply biochemical stimulus or environmental change
- Monitor laser output characteristics (intensity, spectrum, threshold)
- Correlate laser parameter changes with biological state changes
- Calibrate response using known standards or controls
Critical Considerations:
- Cavity Q-factor determines detection sensitivity
- Gain molecule concentrations typically range from 1 μM to 10 mM to reach threshold
- Small changes in energy transfer efficiency can produce large variations in laser output
- Environmental stability is critical for reproducible measurements
Table 4: Performance Characteristics of Different Biointegrated Laser Systems
| Laser Type | Gain Medium | Cavity Type | Threshold Energy | Emission Linewidth | Primary Applications |
|---|---|---|---|---|---|
| eGFP Solid-State Laser | Enhanced Green Fluorescent Protein | Fabry-Pérot | <100 pJ | <1 nm | Cellular sensing, environmental monitoring |
| WGM Intracellular Laser | Synthetic dyes in polymer microspheres | Whispering Gallery Mode | 10 nJ - 1 μJ | <0.1 nm | Cell tracking, intracellular sensing |
| Optofluidic Biosensor | Enzyme-activated fluorescent substrates | Distributed Feedback | 10 nJ - 100 μJ | 0.1-1 nm | Biomolecular interaction monitoring |
| FRET-based Biosensor | Donor-acceptor fluorophore pairs | Ring Resonator | 100 nJ - 10 μJ | 0.1-0.5 nm | Protein conformational changes, molecular interactions |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of bioluminescence, biofluorescence, and biolaser technologies requires specific reagents and materials optimized for each application. The following table summarizes key research solutions essential for working with these emerging biophotonic tools.
Table 5: Essential Research Reagents and Materials for Biophotonics Research
| Reagent/Material | Composition/Type | Primary Function | Example Applications |
|---|---|---|---|
| D-Luciferin | Firefly luciferase substrate | Bioluminescent substrate for ATP-dependent light production | In vivo imaging, reporter gene assays, ATP detection |
| Coelenterazine | Imidazopyrazinone-based luciferin | Bioluminescent substrate for marine luciferases | Secreted reporter assays, BRET, high-throughput screening |
| Furimazine | Synthetic coelenterazine analog | Substrate for NanoLuc luciferase | Protein-protein interactions, high-sensitivity detection |
| AkaLumine | Synthetic D-luciferin analog | Red-shifted substrate for engineered luciferases | Deep-tissue imaging, single-cell detection in vivo |
| Enhanced GFP (eGFP) | Optimized green fluorescent protein | Genetic encoded fluorescent reporter | Gene expression, protein localization, laser gain medium |
| NanoLuc Luciferase | Engineered 19 kDa luciferase | Small, bright bioluminescent reporter | Protein fusion tags, transcriptional reporting, BRET |
| Whispering Gallery Mode Resonators | Polymer or silica microspheres | High-Q optical cavities for biolasers | Intracellular sensing, cell tracking, biosensing |
| BRET Pairs | Luciferase-fluorescent protein combinations | Bioluminescence resonance energy transfer | Protein-protein interactions, molecular proximity |
| Luciferase Reporter Vectors | Plasmid constructs with luciferase genes | Genetic reporters for transcriptional activity | Pathway analysis, promoter studies, drug screening |
| Specialized Luminometers | Photon detection instruments | Sensitive detection of bioluminescent signals | Reporter assays, kinetic measurements, high-throughput screening |
The convergence of bioluminescence, biofluorescence, and biolaser technologies represents a transformative frontier in biophotonics research. Current developments point toward several promising directions, including the engineering of novel luciferase-luciferin pairs with improved brightness, red-shifted emission, and orthogonality for multiplexed applications [24] [29]. The creation of bioluminescent plants through genetic engineering demonstrates the potential for entirely new applications beyond traditional research settings [22]. Similarly, advances in biolaser technology suggest future capabilities for highly parallel cellular analysis, deep-tissue sensing, and potentially even photonic therapeutics [28].
The most ambitious frontier in this field remains the development of fully genetically encoded laser systems. While significant challenges exist—particularly regarding the energy requirements for achieving population inversion through biological pumping mechanisms—recent progress in understanding and engineering biological light production provides a foundation for future breakthroughs [28]. The demonstration of fluorescence proteins with exceptional performance in solid-state configurations suggests that evolutionary optimization of biological photonic systems may yield solutions to challenges that have limited synthetic approaches [26].
For researchers and drug development professionals, these emerging biophotonic technologies offer increasingly powerful tools for probing biological systems with unprecedented sensitivity, specificity, and temporal resolution. The continuing refinement of these technologies promises to accelerate basic research, enhance drug discovery pipelines, and ultimately enable new diagnostic and therapeutic modalities that leverage the unique properties of biological light.
Biophotonics in Action: Advanced Imaging, Biosensing, and Therapeutic Applications
Biophotonics, the convergence of light-based technologies with biology and medicine, has emerged as a transformative discipline for scientific research and medical diagnostics [1]. This field utilizes the properties of light to analyze and manipulate biological materials across multiple spatial scales, from single molecules to entire organs [1] [30]. The core advantages of biophotonic techniques include non-contact measurement, high sensitivity down to single molecules, excellent time resolution for observing dynamic processes, and the ability to provide instant information [1]. These characteristics make biophotonics indispensable for unraveling disease mechanisms, enabling early diagnosis, and developing targeted treatments [1].
Within biophotonics, high-resolution bioimaging represents a pivotal technological frontier, providing scientists with unprecedented views into biological structures and processes. Optical Coherence Tomography (OCT) and Multiphoton Microscopy stand as two prominent techniques in this domain, each with distinct physical principles and application landscapes [31] [1] [32]. OCT excels at providing cross-sectional, micron-scale images of tissue microstructure in real-time, while multiphoton microscopy offers superior resolution for deep-tissue imaging at the cellular and subcellular level [1] [32]. This whitepaper provides an in-depth technical examination of both technologies, detailing their working principles, methodological protocols, and applications within biomedical research and drug development.
Optical Coherence Tomography (OCT): Principles and Technical Evolution
Fundamental Principle and Technical Progression
OCT is a non-invasive imaging technique that generates cross-sectional images of tissue microstructure with high resolution [31] [33]. Its operation is analogous to ultrasound B-mode imaging, but it uses light instead of sound, measuring the echo time delay and intensity of backscattered or backreflected light [33]. The fundamental principle underlying all OCT implementations is low-coherence interferometry [31]. This method uses a broadband light source with a short coherence length, and an interferometer splits the light into sample and reference arms [31]. Interference occurs only when the optical path lengths of both arms are matched within the coherence length of the source, thus allowing precise depth resolution of backscattering sites within the sample [31].
The technology has evolved through several generations, summarized in Table 1, each bringing significant improvements in speed and performance.
Table 1: Technical Evolution of OCT Systems
| Parameter | Time-Domain OCT (TD-OCT) | Spectral-Domain OCT (SD-OCT) | Swept-Source OCT (SS-OCT) |
|---|---|---|---|
| Image Acquisition Method | Moving reference mirror, single photon detector [34] | Broadband source, spectrometer with line scan camera [31] [34] | Wavelength-sweeping laser, single balanced photodetector [31] [34] |
| Scanning Speed (A-scans/sec) | ~400 [34] | 20,000 - 70,000 [34] | 100,000 - 400,000 [34] |
| Axial Resolution | ~10 μm [34] | 5-7 μm [34] | ~5 μm [34] |
| Light Source Wavelength | ~810 nm [34] | 800-870 nm [34] | 1050-1060 nm [34] |
| Key Advantage | First commercial systems | Improved speed and image quality vs. TD-OCT [31] | Deeper tissue penetration without EDI; highest speed [34] |
Standard OCT Experimental Protocol
The following protocol describes a typical functional OCT experiment, such as Spectroscopic OCT (SOCT), to map hemoglobin concentration and oxygenation in vivo [35].
1. System Setup and Calibration
- Equipment: Configure a Fourier-Domain OCT system (SD-OCT or SS-OCT) [35]. For SOCT, ensure a broadband light source with sufficient bandwidth is used, as this dictates axial resolution [35].
- Calibration: Resample the detected interferogram from wavelength (λ) to a linear wavenumber (k = 2π/λ) vector to enable proper Fast Fourier Transform (FFT) processing [35].
- Animal Preparation: Anesthetize the animal (e.g., a mouse model) and position the area of interest (e.g., a dorsal window chamber for tumor studies) under the OCT objective lens. Maintain the animal's body temperature at 37°C throughout the experiment.
2. Data Acquisition
- Structural Imaging: Acquire 3D OCT volumes (comprising multiple B-scans) of the tissue region. Typical parameters: 5x5 mm field of view, 512 A-scans per B-scan, 512 B-scan positions.
- Spectral Data Acquisition: For SOCT, use the same dataset as for structural imaging but process it to extract the wavelength-dependent attenuation at each voxel [35]. This requires a high signal-to-noise ratio.
3. Data Processing and Analysis
- FFT Processing: Apply an FFT to the resampled interferometric signal at each lateral position to generate individual A-scans, revealing the depth-resolved sample structure [35].
- Spectral Analysis: Process the OCT data using algorithms like the dual-window method to compute depth-resolved spectra with simultaneously high spectral and temporal resolution [35]. This analysis reveals the wavelength-dependent attenuation of light.
- Biomarker Quantification: Calculate the concentration of hemoglobin (Hb) and hemoglobin oxygen saturation (sO₂) by fitting the extracted optical attenuation spectra to the known absorption spectra of oxy- and deoxy-hemoglobin [35].
4. Validation
- Correlate SOCT findings with gold-standard methods, such as histology of excised tissue or measurements from other optical instruments.
Research Reagent Solutions for OCT
Table 2: Key Research Reagents and Materials for OCT
| Item | Function/Description |
|---|---|
| Broadband Light Source | Provides the low-coherence light required for interferometry and defines the system's axial resolution. Examples: Superluminescent Diodes (SLDs) for SD-OCT [31]. |
| Swept-Source Laser | A rapidly tuning laser used in SS-OCT that sweeps through a range of wavelengths over time, enabling very high acquisition speeds [31] [34]. |
| Reference Mirror | A mirror in the reference arm of the interferometer that is stationary in FD-OCT systems. Its position defines the zero-delay point [31]. |
| Spectrometer (for SD-OCT) | Comprises a diffraction grating and a high-speed line scan camera to simultaneously detect all wavelengths of the interferometric signal [31]. |
| Balanced Photodetector (for SS-OCT) | A high-speed detector used in SS-OCT to sequentially measure the interferometric signal at each wavelength during a laser sweep [31] [34]. |
Multiphoton Microscopy: Principles and Applications
Fundamental Principle and Market Context
Multiphoton microscopy is a nonlinear optical technique that enables high-resolution imaging deep within scattering biological tissues. Its fundamental principle involves the near-simultaneous absorption of two or more long-wavelength, low-energy photons by a fluorophore, which collectively provide the energy equivalent to a single, higher-energy photon [1]. This nonlinear process occurs only at the focal point where photon density is highest, resulting in inherent optical sectioning without the need for a confocal pinhole, and significantly reduced photobleaching and photodamage outside the focal volume [1] [32].
The technology's value is reflected in its growing market presence. The global two-photon microscopy market is estimated at USD 1.35 billion in 2025 and is projected to reach USD 2.42 billion by 2032, exhibiting a compound annual growth rate (CAGR) of 8.7% [32]. Neuroscience is the dominant application segment, accounting for 34.3% of the market share in 2025, as it allows for the study of neural structure and function in live animals with exceptional resolution [32].
Standard Multiphoton Microscopy Experimental Protocol
This protocol outlines the key steps for in vivo two-photon imaging of neural activity in the brain of a freely moving or anesthetized mouse.
1. Animal Preparation and Surgical Procedures
- Transgenic Animal Model: Use transgenic mice expressing genetically encoded calcium indicators (e.g., GCaMP) in specific neuronal populations.
- Cranial Window Implantation: Under anesthesia, perform a craniotomy and implant a glass-sealed cranial window over the brain region of interest (e.g., somatosensory cortex) to provide optical access for long-term imaging.
- Head-Bar Fixation: Affix a custom head-bar to the skull to stabilize the animal's head under the microscope objective during imaging sessions.
2. System Setup and Configuration
- Microscope: Configure a two-photon microscope. Standalone systems are preferred for their flexibility and customization options, holding a 34.2% market share in this segment [32].
- Excitation Source: Use a mode-locked Ti:Sapphire laser or a fiber laser producing femtosecond pulses at the required wavelength (e.g., 920 nm for exciting GCaMP).
- Detection System: Equip with high-sensitivity photomultiplier tubes (PMTs) or hybrid detectors. Recent advances, such as Hamamatsu's latest PMTs, enhance detection precision for single-molecule resolution [2].
3. In Vivo Image Acquisition
- Animal Positioning: Secure the mouse with the head-bar under the objective. Maintain anesthesia if required, or use a miniature microscope for freely moving studies.
- Parameter Setting: Set laser power to the minimum necessary to achieve a good signal-to-noise ratio, minimizing tissue photodamage.
- Time-Lapse Imaging: Acquire image stacks at a high frame rate (e.g., 10-30 Hz) to capture rapid calcium transients associated with neuronal firing. The miniature FHIRM-TPM 3.0 microscope (2.6g) enables multicolor deep-brain imaging in freely moving mice [32].
4. Data Processing and Analysis
- Pre-processing: Use software for motion correction to compensate for any brain movement artifacts.
- Cell Segmentation: Apply automated algorithms (often AI-based) to identify active neurons within the field of view.
- Signal Extraction: Calculate the fluorescence change (ΔF/F) over time for each identified neuron to determine its activity trace.
- AI Integration: Leverage AI-powered platforms, like those offered by companies such as Inscopix, for automated signal extraction, behavioral correlation, and advanced visualization of neural data [32].
Research Reagent Solutions for Multiphoton Microscopy
Table 3: Key Research Reagents and Materials for Multiphoton Microscopy
| Item | Function/Description |
|---|---|
| Femtosecond Pulsed Laser | High-intensity laser source that produces ultrashort pulses necessary for efficient multiphoton excitation. Essential for deep-tissue imaging with near-IR light [1] [32]. |
| Genetically Encoded Calcium Indicators (GECIs) | Fluorescent proteins (e.g., GCaMP) expressed in specific cell types. Their fluorescence changes in response to calcium influx, allowing visualization of neuronal activity [32]. |
| High-Sensitivity Detectors (PMTs) | Photomultiplier Tubes are crucial for detecting the inherently weak fluorescence signals generated by multiphoton excitation. Advances in hybrid PMT systems improve precision [2]. |
| Miniaturized Microscope (e.g., FHIRM-TPM 3.0) | A lightweight (2.6g) two-photon microscope designed for multicolor deep-brain imaging in freely moving mice, enabling studies of naturalistic behaviors [32]. |
| AI-Powered Analysis Software | Software platforms that integrate AI algorithms for automated signal extraction, cell segmentation, and behavioral correlation, transforming the analysis of complex neural data [32]. |
Comparative Analysis and Future Outlook in Biophotonics
Technology Comparison and Complementary Roles
OCT and multiphoton microscopy occupy distinct yet complementary niches in the biophotonics toolkit. OCT is unparalleled for rapid, meso-scale structural imaging, providing volumetric data on tissue architecture in real-time. Its key strength lies in clinical translation, as evidenced by its widespread adoption in ophthalmology [31] [34]. Multiphoton microscopy, conversely, trades off imaging speed and field of view for superior resolution and molecular specificity at the cellular level, making it an indispensable tool for preclinical biological research, particularly in neuroscience [1] [32].
A significant trend is the development of functional extensions for both technologies. For OCT, this includes Spectroscopic OCT (SOCT) for quantifying chromophores like hemoglobin [35] and OCT Angiography (OCTA) for visualizing blood flow without dyes [34]. Multiphoton microscopy naturally provides molecular contrast through fluorescent indicators and can leverage techniques like fluorescence lifetime imaging (FLIM) to read out cellular microenvironment parameters such as pH or metabolic state [1].
Emerging Trends and Future Directions
The future of both OCT and multiphoton microscopy is being shaped by several convergent technological trends, with Artificial Intelligence (AI) playing a central role. AI is reshaping the market by automating complex tasks such as image reconstruction, segmentation, and feature extraction, thereby accelerating data analysis and reducing manual workload [32]. AI-driven solutions also facilitate personalization in imaging applications and enable real-time feedback during imaging sessions for superior image quality [32].
Other key trends include:
- Miniaturization: The development of devices like the 2.6g FHIRM-TPM 3.0 microscope allows for high-resolution imaging in freely behaving animals, opening new avenues for neuroscience [32].
- Multimodal Integration: Combining multiple optical contrast mechanisms (e.g., OCT with multiphoton or photoacoustic imaging) enriches information content, where the "sum is greater than the parts" [30].
- Challenges and Opportunities: Persistent challenges include the trade-off between imaging depth and resolution, data volume management, and the need for standardized protocols [30]. Ongoing research in adaptive optics, longer wavelength excitation, and intelligent data processing aims to overcome these hurdles, further solidifying the role of these technologies in the advancing field of biophotonics.
Biophotonics, the fusion of photonics and life sciences, uses light to analyze and manipulate biological materials. It has become a cornerstone for advanced molecular-level diagnostics in modern biomedical research [1]. This field leverages the interactions between light and biological matter, such as absorption, emission, and scattering, to probe cellular and molecular processes non-invasively and with high sensitivity [1]. The primary advantages of these optical techniques include non-contact measurement, rapid information acquisition, high sensitivity down to the single-molecule level, and the ability to monitor dynamic biological processes in real-time [1].
Within this domain, vibrational spectroscopy techniques, particularly Raman and Fourier-Transform Infrared (FT-IR) spectroscopy, have emerged as powerful analytical tools. They provide a unique window into the molecular composition and structure of cells, tissues, and biofluids by revealing their intrinsic chemical fingerprints without the need for labels or destructive sample preparation [36] [37]. This whitepaper provides an in-depth technical guide to these core techniques, detailing their principles, methodologies, and applications within the context of biophotonics research for drug development and clinical diagnostics.
Fundamental Principles and Comparative Analysis
Raman Spectroscopy
Raman spectroscopy is an optical technique based on the inelastic scattering of light by vibrating molecules [37]. When light interacts with a molecule, a tiny fraction of photons (approximately 1 in 10⁶) undergoes a shift in energy corresponding to the vibrational modes of the molecular bonds. This energy shift, known as the Raman effect, provides a highly specific chemical fingerprint of the sample [38] [37]. The process involves the creation of an induced dipole moment in a molecule, causing an instantaneous transition to a virtual state, which enables coupling between vibrational states and the transfer of a quantum of vibrational energy [38].
A significant challenge for traditional spontaneous Raman scattering is its intrinsically weak signal, which can result in long acquisition times for imaging applications [38]. To address this, advanced techniques such as Coherent Anti-Stokes Raman Scattering (CARS) and Stimulated Raman Scattering (SRS) have been developed. These nonlinear methods enhance the weak Raman signal and avoid being swamped by autofluorescence background, thereby enabling high-speed imaging [1].
FT-IR Spectroscopy
FT-IR spectroscopy, by contrast, measures the absorption of infrared light by molecular bonds [36]. When IR radiation interacts with a sample, chemical bonds absorb light at specific frequencies that correspond to their vibrational energies. The resulting spectrum represents the molecular composition of the sample [36]. The Fourier Transform mathematical operation is applied to the raw interferogram data to generate an IR spectrum that is rich in chemical information [36].
The primary measurement techniques in FT-IR spectroscopy are:
- Transmission: IR radiation passes directly through the sample.
- Transflection: IR radiation is transmitted through the sample, reflects off a substrate, and passes back through the sample.
- Attenuated Total Reflection (ATR): IR radiation interacts with a sample in contact with a high-refractive-index crystal, generating an evanescent wave that penetrates the sample. ATR is particularly valuable for clinical applications due to its rapid data acquisition and minimal sample preparation requirements [36].
Comparative Technical Specifications
The table below summarizes the core principles and technical attributes of Raman and FT-IR spectroscopy for direct comparison.
Table 1: Comparative Analysis of Raman and FT-IR Spectroscopy
| Parameter | Raman Spectroscopy | FT-IR Spectroscopy |
|---|---|---|
| Fundamental Principle | Inelastic scattering of light [37] | Absorption of infrared radiation [36] |
| Probed Transition | Molecular vibrations [38] | Molecular vibrations [36] |
| Typical Excitation Source | Visible or NIR lasers (e.g., 785 nm, 830 nm) [38] | Mid-infrared source (e.g., Globar) [36] |
| Key Spectral Regions | Fingerprint region (500-2000 cm⁻¹) [38] | Fingerprint region (1800-800 cm⁻¹) [36] |
| Water Interference | Low (suitable for hydrated samples) [37] | High (strong water absorption) [36] |
| Spatial Resolution | High (diffraction-limited, sub-micron) [38] | Lower (typically 10-20 µm for microspectroscopy) |
| Key Application Strength | High spatial resolution imaging; suitable for aqueous environments [38] [37] | High sensitivity for bulk biochemical analysis; rapid screening [36] |
Diagram: Fundamental Principles of Raman and FT-IR Spectroscopy
The following diagram illustrates the core physical principles and energy level transitions that differentiate Raman scattering from infrared absorption.
Experimental Protocols and Methodologies
Sample Preparation Protocols
FT-IR Spectroscopy for Tissue Analysis
ATR-FTIR is a prominent technique for tissue analysis due to its fast data acquisition and high accuracy in differentiating between normal and malignant tissues [36]. The general workflow is as follows:
- Sample Types: Analysis can be performed on fixed (e.g., Formalin-Fixed Paraffin-Embedded or FFPE), fresh, or frozen tissues [36].
- Dewaxing: For FFPE samples, dewaxing using xylol or xylene is required before spectral acquisition [36].
- Drying: As water absorbs strongly in the mid-infrared region, it is critical to remove all water from the samples. This can be achieved by air-drying or using a nitrogen flux. Previewing spectra during drying can help determine if water is fully removed [36].
- Data Acquisition: The dried tissue sample is placed in contact with the ATR crystal (commonly made of Germanium or ZnSe), and the IR spectrum is collected [36].
Table 2: Key Research Reagent Solutions for FT-IR Tissue Analysis
| Reagent/Material | Function | Technical Notes |
|---|---|---|
| Formalin (10% Neutral Buffered) | Tissue fixation | Preserves tissue structure; requires subsequent dewaxing for FFPE samples. |
| Xylol/Xylene | Dewaxing agent | Removes paraffin from FFPE sections without damaging tissue biochemistry. |
| ATR Crystal (Ge, ZnSe) | Internal Reflection Element (IRE) | Enables ATR measurement; Ge offers higher refractive index. |
| Nitrogen Gas | Sample drying | Inert atmosphere for gentle, rapid drying of fresh/frozen samples. |
Raman Spectroscopy for Biofluids and Cells
Raman spectroscopy requires minimal or no sample preparation, which is a significant advantage for clinical applications [37]. A typical protocol involves:
- Sample Loading: Biofluids (e.g., blood serum, urine) or cell suspensions are placed on a substrate such as aluminum-coated slides or CaF₂ windows, which exhibit low background Raman signal.
- Stabilization: For live-cell imaging, cells are maintained in an appropriate physiological buffer at controlled temperature and CO₂ levels.
- Data Acquisition: Using a confocal Raman microspectrometer, the laser is focused on the sample. Spectra are acquired by raster-scanning the laser beam across the specimen. To mitigate the weak signal, long wavelength sources (e.g., 785 nm or 830 nm) are often used to minimize autofluorescence [38].
Data Acquisition and Pre-processing
FT-IR Spectral Data Assessment
To ensure accurate results from FT-IR analysis, data pre-processing is essential [36]. Key steps include:
- Quality Control: Check absolute absorption, signal-to-noise ratio, and humidity effects [36].
- Pre-treatment: Apply baseline corrections to correct for sloping or varying baselines, smoothing to reduce background noise, derivation to resolve complex and overlapping bands, and vector normalization to compensate for variations in absorption caused by variable sample thickness or size [36].
Enhancing Raman Imaging Speed
The intrinsically weak signal of spontaneous Raman scattering has been a major hurdle for clinical translation [38]. Several strategies have been developed to increase imaging speed:
- Line-scanning and Multifocal Imaging: These approaches parallelize the excitation and detection process, significantly reducing acquisition times compared to single-point raster scanning [38].
- Coherent Raman Scattering (CRS): Techniques like CARS and SRS enhance the intrinsically weak Raman signal by several orders of magnitude, enabling video-rate imaging speeds suitable for in vivo applications [1].
- Multimodal Integration: Combining rapid autofluorescence imaging with Raman microspectroscopy allows for predictive segmentation. This guides the Raman system to acquire data only from points of interest, drastically reducing total measurement time. One demonstration achieved automated segmentation and imaging of nearly 800 points on a skin sample in approximately 11 minutes [38].
- Fiber Optic Probe Tracking: For surgical guidance, handheld Raman probes coupled with computer-vision tracking can generate spatial spectral maps overlaid on brightfield images in real-time, enabling tissue differentiation during procedures [38].
Diagram: Typical Experimental Workflow for Raman and FT-IR
The diagram below outlines a generalized workflow for conducting a vibrational spectroscopy study, from sample preparation to data analysis.
Applications in Biomedical Research and Diagnostics
Disease Diagnostics and Intraoperative Guidance
The high chemical specificity of Raman and FT-IR spectroscopy allows for the detection of molecular changes associated with diseases in cells, tissues, and biofluids [37].
- Cancer Detection and Grading: FT-IR spectroscopy has demonstrated significant utility in identifying molecular changes associated with various pathologies, including cancer, and can discriminate between healthy and diseased tissues based on spectral differences [36]. In a clinical study of 17 patients undergoing brain tumor surgery, intraoperative tracking of a Raman probe differentiated tissue type and glioma grade with high sensitivity and specificity, showcasing its potential for surgical guidance [38].
- Surgical Margin Delineation: Raman fiber optic probes, when combined with digital tracking, can be used to define tumor margins. In ex vivo and in vivo animal studies, this approach successfully mapped tumor tissue margins through combined Raman spectral measurements and exogenous fluorescence detection [38].
Drug Discovery and Pharmaceutical Applications
Raman spectroscopy is widely used as a non-destructive technique in drug screening. Its ability to map molecular structures using scattered light is valuable for pharmaceutical research [2]. Key applications include:
- High-Throughput Drug Screening: Raman imaging is employed to study cellular responses to drug candidates, enabling the identification of efficacious compounds based on biochemical changes within cells.
- Biomarker Discovery: The ability of these techniques to provide comprehensive molecular profiles facilitates the identification of new biochemical markers for disease, which is crucial for developing targeted therapies and personalized treatment plans [3].
Integration with Artificial Intelligence and Novel Materials
The future of Raman and FT-IR spectroscopy is closely tied to advancements in data analysis and material science. The integration of Artificial Intelligence (AI) and Machine Learning (ML) is proving transformative. AI-driven biophotonics techniques, such as Raman spectroscopy integrated with machine learning, have shown remarkable success, for example, in detecting early breast cancer with a 98% accuracy [3]. This combination is leading to the emergence of "Ramanomics," an optical omics discipline that uses advanced spectroscopy and algorithms for comprehensive biochemical analysis [39].
Furthermore, the integration of nanotechnology is enhancing the performance of diagnostic tools. The use of nanomaterials like metallic nanoparticles and quantum dots enables higher sensitivity and specificity for sensing biomarkers and tissue imaging, facilitating earlier disease detection [3]. The combination of biophotonics with nanotechnology has already led to major improvements in ultra-sensitive diagnostic tools and targeted treatments [40].
Raman and FT-IR spectroscopy represent two powerful pillars of biophotonics for molecular-level diagnostics. While FT-IR spectroscopy excels in rapid, high-sensitivity screening and bulk biochemical analysis, Raman spectroscopy offers superior spatial resolution and flexibility for imaging in aqueous environments, including live cells. Despite challenges such as the inherently weak Raman signal and the strong water absorption in FT-IR, technological advancements in coherent Raman scattering, fiber-optic probes, and AI-powered data analysis are propelling these techniques to the forefront of clinical translation.
As the biophotonics market continues its rapid growth—projected to reach \$113.1 billion by 2030—the role of Raman and FT-IR spectroscopy in shaping the future of precision medicine, drug discovery, and intraoperative diagnostics is set to expand significantly [40] [41]. Their ability to provide non-invasive, label-free, and chemically specific information makes them indispensable tools for researchers and clinicians aiming to understand and diagnose disease at the molecular level.
Biophotonics, the convergence of photonics and biological sciences, utilizes light-based technologies to address critical challenges in medicine and life sciences. This field is a key driver in modern diagnostics and therapeutic monitoring, enabling the non-invasive, highly sensitive, and real-time detection of biological interactions [42]. The global biophotonics market, projected to grow from USD 67.2 billion in 2025 to USD 189.3 billion by 2035, underscores its significant impact and rapid adoption [2]. At the heart of many advanced biophotonic tools are optical biosensors, which transduce molecular binding events into measurable optical signals. Among these, Surface Plasmon Resonance (SPR) and Fluorescence Resonance Energy Transfer (FRET) represent two powerful and complementary sensing paradigms. SPR excels in providing label-free, real-time kinetic data of biomolecular interactions, while FRET offers exceptional sensitivity for probing nanoscale distances and conformational changes within complex biological systems [43] [44]. This whitepaper provides an in-depth technical guide to these platforms, detailing their fundamental principles, current technological advancements, experimental protocols, and their pivotal role in pharmaceutical research and clinical diagnostics.
Fundamental Principles
Surface Plasmon Resonance (SPR)
SPR is a quantum optical-electronic phenomenon observed when incident polarized light, under specific conditions, couples with the collective oscillations of free electrons (known as surface plasmons) at the interface between a metal (typically gold or silver) and a dielectric medium [43] [45]. This coupling occurs at a precise resonance angle of incident light, leading to a sharp drop in the intensity of reflected light. The core sensing mechanism hinges on the fact that the resonance condition is exquisitely sensitive to the refractive index (RI) within an evanescent field, which typically extends a few hundred nanometers from the metal surface [46]. When target analytes, such as proteins or nucleic acids, bind to molecular recognition elements (e.g., antibodies, aptamers) immobilized on the sensor surface, the local RI changes, causing a measurable shift in the resonance angle, wavelength, or intensity [43] [47]. This allows for the real-time, label-free monitoring of binding events, including the determination of association and dissociation rate constants, and equilibrium affinity [45].
Fluorescence Resonance Energy Transfer (FRET)
FRET is a distance-dependent physical process whereby an excited-state donor fluorophore non-radiatively transfers its energy to a nearby acceptor fluorophore through dipole-dipole interactions [44]. For efficient FRET to occur, several conditions must be met: the emission spectrum of the donor must significantly overlap with the absorption spectrum of the acceptor, the two fluorophores must be in close proximity (typically 1-10 nm), and their transition dipoles must be favorably oriented [48] [44]. The efficiency of energy transfer is inversely proportional to the sixth power of the distance between the donor and acceptor, making FRET an exceptionally powerful "molecular ruler" [44]. In biosensing, FRET-based assays are designed such that a specific biological event—such as protease cleavage, nucleic acid hybridization, or protein-protein interaction—alters the distance between the donor and acceptor, resulting in a measurable change in the fluorescence emission intensity or lifetime of either fluorophore [48] [44].
Table 1: Core Principles of SPR and FRET Biosensing Platforms
| Feature | Surface Plasmon Resonance (SPR) | Fluorescence Resonance Energy Transfer (FRET) |
|---|---|---|
| Sensing Principle | Label-free; measures change in refractive index | Label-dependent; measures non-radiative energy transfer |
| Key Measured Parameter | Shift in resonance angle, wavelength, or intensity | Change in fluorescence intensity, lifetime, or anisotropy |
| Effective Range | Evanescent field (∼200-300 nm) | 1 - 10 nanometers |
| Primary Information | Real-time binding kinetics and affinity | Molecular proximity, conformation, and interactions |
| Typical Assay Format | Heterogeneous (surface-based) | Homogeneous (solution-based) |
Advanced Sensing Materials and Performance
The performance of SPR and FRET biosensors is profoundly enhanced by the integration of innovative nanomaterials, which boost sensitivity, specificity, and stability.
Materials for SPR Enhancement
The development of SPR sensors has moved beyond conventional thin gold films to incorporate various nanostructured materials that amplify the plasmonic signal.
- 2D Materials and Heterostructures: Materials like graphene, transition metal dichalcogenides (e.g., MoS₂, WS₂), and their heterostructures are used to enhance the electric field at the sensing interface. For instance, a heterostructure combining platinum diselenide (PtSe₂) with blue phosphorus/WS₂ (BlueP/WS₂) has been shown to achieve a theoretical sensitivity of up to 234 deg/RIU [47].
- Metal-Organic Frameworks (MOFs): Porous crystalline MOFs, such as UiO-66 and Zr-BDC, are prized for their large specific surface area, tunable porosity, and abundant functional groups. They increase probe immobilization capacity and enhance the local refractive index change, significantly improving detection sensitivity for small molecules, gases, and biomarkers [45].
- Bimetallic and Other Nanostructures: Combining metals like gold and silver or using anisotropic structures such as Au-Ag nanostars can generate "hot spots" of intense electromagnetic fields, which is particularly beneficial for techniques like surface-enhanced Raman scattering (SERS) [49].
Donor-Acceptor Pairs for FRET
The choice of fluorophores is critical for developing a highly efficient FRET system.
- Quantum Dots (QDs): Semiconductor nanocrystals (e.g., CdSe, CdTe, InP) serve as excellent donors due to their high quantum yield, photostability, and narrow, tunable emission spectra. Core-shell structures (e.g., CdSe/ZnS) further improve fluorescence efficiency [48].
- Organic Dyes: Traditional dyes like fluorescein (FAM), Cy3, Cy5, and tetramethylrhodamine (TAMRA) are widely used. However, they often suffer from photobleaching and narrow excitation spectra [48] [44].
- Carbon Dots and Nanomaterials: Carbon dots (CDs) offer excellent water solubility, modifiable surfaces, and superior biocompatibility, making them attractive for biological applications, though their broader emission spectra can be a limitation [48].
- Gold Nanoparticles (AuNPs): AuNPs are highly efficient energy acceptors/quenchers in FRET assays due to their strong plasmonic absorption, leading to sensitive "turn-on" detection when the donor is released from the AuNP surface [44].
Table 2: Advanced Materials in Biosensing Platforms
| Material Category | Example Materials | Key Functions and Advantages | Typical Sensor Application |
|---|---|---|---|
| SPR: 2D Materials | PtSe₂, BlueP/WS₂, Graphene | Electric field enhancement; high charge transfer mobility; tunable bandgap [47]. | Ultra-sensitive biodetection [47] |
| SPR: Porous Frameworks | UiO-66, Cu-TCPP, ZIF-8 | High surface area for probe loading; specific analyte adsorption/encapsulation [45]. | Gas sensing, small molecule detection [45] |
| FRET: Donors | CdSe/ZnS QDs, Carbon Dots (CDs), FAM | High quantum yield; photostability; size-tunable emission (QDs) [48] [44]. | Homogeneous immunoassays, nucleic acid detection |
| FRET: Acceptors/Quenchers | AuNPs, BHQ-1, Dabcyl, CY5 | Efficient energy acceptance/quenching; plasmonic properties (AuNPs) [44]. | Molecular beacon assays, "turn-on" sensors |
Experimental Protocols
Protocol for Fabricating an MOF-Enhanced SPR Sensor for Exosome Detection
This protocol outlines the development of a highly sensitive SPR biosensor for detecting cancer-derived exosomes, utilizing a metal-organic framework (MOF) to enhance performance [45].
1. Sensor Chip Functionalization:
- Materials: BK7 glass prism, gold target (for sputtering), Zr-MOF (e.g., UiO-66) suspension, PBS buffer (pH 7.4), aminoproyltriethoxysilane (APTES), glutaraldehyde.
- Procedure:
- Clean the BK7 glass substrate thoroughly with piranha solution (Caution: highly corrosive), followed by rinsing with ethanol and deionized water.
- Deposit a ~50 nm thin gold film onto the glass substrate using magnetron sputtering or thermal evaporation to create the conventional SPR active surface.
- Immerse the gold chip in a 1 mM ethanolic solution of APTES for 12 hours to form an amine-terminated self-assembled monolayer (SAM).
- Activate the amine groups by immersing the chip in a 2.5% glutaraldehyde solution in PBS for 2 hours.
- Finally, incubate the chip in a freshly prepared suspension of Zr-MOF nanoparticles (~1 mg/mL) for 6-12 hours, allowing the MOFs to covalently anchor to the sensor surface via Schiff base reaction. Rinse thoroughly with deionized water and dry under a nitrogen stream.
2. Probe Immobilization:
- Materials: Anti-CD63 aptamer (or antibody), EDC/NHS crosslinking reagents, ethanolamine, MES buffer.
- Procedure:
- If the MOF contains carboxylic acid groups (e.g., in its organic linkers), activate them with a mixture of EDC (400 mM) and NHS (100 mM) in MES buffer (0.1 M, pH 5.5) for 30 minutes.
- Incubate the activated sensor chip with a solution of amine-modified anti-CD63 aptamer (10-100 µg/mL in PBS) for 24 hours.
- Deactivate any remaining active esters by treating with 1 M ethanolamine (pH 8.5) for 30 minutes.
- Wash the chip with PBS to remove non-covalently bound probes. The sensor is now ready for use.
3. SPR Measurement and Exosome Detection:
- Materials: Phosphate Buffered Saline (PBS), exosome samples isolated from cell culture or biofluids, SPR instrument.
- Procedure:
- Mount the functionalized sensor chip in the SPR instrument using the Kretschmann configuration.
- Establish a stable baseline by flowing PBS over the sensor surface at a constant flow rate (e.g., 20 µL/min).
- Inject a series of exosome samples with known concentrations over the sensor surface for a fixed association time (e.g., 10-15 minutes).
- Switch back to PBS buffer flow to monitor the dissociation phase for another 10-15 minutes.
- Regenerate the sensor surface between cycles by a short injection of a mild regeneration solution (e.g., 10 mM glycine-HCl, pH 2.0) to dissociate bound exosomes without damaging the immobilized probes.
- Record the SPR angle shift (in Resonance Units, RU) as a function of time. Plot the maximum response for each concentration against the exosome concentration to generate a calibration curve.
Protocol for a FRET-based Homogeneous Immunoassay using QDs
This protocol describes a homogeneous immunoassay for detecting a target antigen using Quantum Dots (QDs) as FRET donors and gold nanoparticles (AuNPs) as acceptors [48] [44].
1. Preparation of QD-Donor and AuNP-Acceptor Conjugates:
- Materials: CdSe/ZnS core-shell QDs (emission ~605 nm), carboxylic acid-functionalized AuNPs (diameter ~5 nm), EDC/NHS, detection antibody, PBS buffer.
- Procedure:
- QD-Ab Conjugate: Activate the carboxyl groups on the QD surface with EDC/NHS. Add the detection antibody (e.g., 100 µg/mL) and allow conjugation for 2 hours under gentle shaking. Purify the QD-Ab conjugate using size-exclusion chromatography or ultrafiltration to remove unbound antibodies.
- AuNP-Ab Conjugate: Similarly, activate carboxylated AuNPs with EDC/NHS. Incubate with a second, non-competing detection antibody (or the same type) targeting the same antigen. Purify the conjugate to remove excess reagents.
2. FRET Assay Execution:
- Materials: Black-walled 96-well plate, analyte (antigen) at various concentrations, assay buffer.
- Procedure:
- In each well of the plate, mix a fixed concentration of the QD-Ab conjugate (e.g., 10 nM) and AuNP-Ab conjugate (e.g., 20 nM) in assay buffer.
- Add the antigen standard or sample to the wells. Include a negative control (no antigen).
- Incubate the plate at room temperature for 1 hour with gentle shaking. The formation of antigen-antibody complexes will bring the QDs and AuNPs into close proximity, initiating FRET.
- Excite the QDs at their absorption maximum (e.g., 350 nm) using a plate reader.
- Measure the fluorescence emission intensity of the QDs at 605 nm.
- Data Analysis: In the presence of the antigen and successful FRET, the QD fluorescence will be quenched. The degree of quenching is proportional to the antigen concentration. Calculate the FRET efficiency ( E ) using the formula: ( E = 1 - (F{DA}/FD) ) where ( F{DA} ) is the donor fluorescence intensity in the presence of the acceptor, and ( FD ) is the donor intensity in the absence of the acceptor. Plot the FRET efficiency or the quenching ratio against the analyte concentration to generate the standard curve.
Performance Metrics and Comparative Analysis
Evaluating biosensor performance requires a standardized set of metrics. Sensitivity, limit of detection (LOD), dynamic range, and assay time are critical for comparing different platforms.
Table 3: Performance Comparison of Representative SPR and FRET Biosensors
| Sensor Type & Target | Sensing Mechanism / Materials | Reported Sensitivity | Limit of Detection (LOD) | Assay Time / Real-Time | Reference |
|---|---|---|---|---|---|
| SPR: General Biomolecular Binding | Prism (BK7)/Au Film / Kretschmann | Angular shift: ~0.75 deg for 3 nm protein layer | Mass: ~0.6 pg/mm² (with 0.1 mDeg angular sensitivity) | Yes / Real-time | [46] |
| SPR: Optimized Structure | Prism (BK7)/Au/PtSe₂/BlueP/WS₂ | 234 deg/RIU (theoretical) | 4.26 × 10⁻⁶ RIU (theoretical) | Yes / Real-time | [47] |
| SPR: Exosomes | Au chip / MOF (Zr-TCPP) interface | Not Specified (N/S) | Improved vs. conventional SPR | Yes / Real-time | [45] |
| FRET: Exosomes (CD63) | FAM (Donor) / Dabcyl (Acceptor) | N/S | N/S | ~1-2 hours / End-point | [44] |
| FRET: miRNA-21 | FAM (Donor) / BHQ1 (Acceptor) | N/S | N/S | ~1-2 hours / End-point | [44] |
| FRET: Exosomes (EpCAM) | QD (Donor) / AuNP (Acceptor) | N/S | N/S | ~1-2 hours / End-point | [44] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of SPR and FRET assays relies on a suite of specialized reagents and materials.
Table 4: Essential Research Reagents and Materials
| Item Name | Function / Explanation | Example Application |
|---|---|---|
| BK7 Prism | High-refractive-index glass substrate for coupling light and exciting surface plasmons in the Kretschmann configuration [47]. | SPR sensor foundation |
| Gold Sensor Chip | ~50 nm thick gold film serves as the plasmonic active layer due to its chemical stability and strong SPR response [47] [46]. | SPR substrate |
| Carboxylated QDs | Semiconductor nanocrystals functionalized with -COOH groups for facile covalent conjugation to biomolecules via EDC/NHS chemistry [48]. | FRET donor probes |
| EDC / NHS | Crosslinking reagents that activate carboxyl groups to form stable amide bonds with primary amines on proteins or aptamers [49]. | Universal bioconjugation |
| Anti-CD63 Aptamer | A single-stranded DNA molecule that binds specifically to the CD63 tetraspanin protein, a common exosome surface marker [44] [45]. | Exosome capture and detection |
| Zr-MOF (UiO-66) | Porous crystalline material with high surface area and stability; enhances SPR response by increasing probe loading and local RI change [45]. | SPR signal amplification layer |
| BHQ-1 Quencher | A dark quencher that absorbs fluorescence energy without emitting light, leading to efficient FRET-based quenching in molecular beacons [44]. | FRET acceptor for "turn-on" assays |
| Regeneration Buffer (e.g., Glycine-HCl) | A low-pH solution that disrupts antigen-antibody bonds without permanently damaging the immobilized ligand, allowing for sensor chip re-use [45]. | SPR chip regeneration |
Schematic Workflows and Signaling Pathways
The following diagrams illustrate the core signaling mechanisms and experimental workflows for SPR and FRET biosensors.
Diagram 1: SPR Sensor Workflow. The schematic illustrates the Kretschmann configuration, where polarized light incident at angle θᵢₙc couples with surface plasmons in the thin gold film, generating an evanescent field. Analyte binding in the functionalized sensing layer alters the local refractive index, causing a measurable shift in the SPR dip (resonance angle), which is detected in real-time [43] [47] [46].
Diagram 2: FRET Mechanism. The diagram contrasts the two states of a FRET system. When donor and acceptor are far apart (>10 nm), donor excitation leads to its own emission. When brought within 1-10 nm by a biological event (e.g., binding), efficient non-radiative energy transfer occurs, resulting in acceptor emission and donor quenching [48] [44].
SPR and FRET biosensing platforms are cornerstones of modern biophotonics, each offering distinct and powerful capabilities for the drug development and research community. SPR provides an unmatched tool for the label-free, real-time analysis of biomolecular kinetics and affinity, a critical need in characterising therapeutic candidates. In parallel, FRET serves as an indispensable "molecular ruler" for probing structural changes, interactions, and localization within complex biological systems, enabling high-throughput homogeneous assays. The ongoing integration of novel materials—such as 2D heterostructures, MOFs, and advanced fluorophores—continually pushes the boundaries of sensitivity and specificity for both platforms. As these technologies evolve, becoming more miniaturized and integrated with point-of-care systems, their value in accelerating drug discovery, enabling precision medicine, and improving diagnostic outcomes will only increase. Their complementary strengths ensure that SPR and FRET will remain vital tools in the scientific arsenal for deciphering biological mechanisms and developing novel biotherapeutics.
Biophotonics, the convergence of light-based technologies with biology and medicine, is revolutionizing cancer research and treatment [1]. This discipline leverages the interactions between light and biological matter to develop non-invasive, precise tools for diagnostics, imaging, and therapeutics [1]. In oncology, two prominent biophotonic therapeutic approaches are Photodynamic Therapy (PDT) and Photothermal Therapy (PTT). Both modalities offer targeted action with minimal side effects compared to conventional therapies, representing a significant shift toward precision medicine in cancer care [50] [51].
The global biophotonics market, valued at USD 76.1 billion in 2024 and projected to reach USD 220.1 billion by 2034, reflects the growing adoption and commercial potential of these technologies [3]. This growth is driven by technological advancements, the rising prevalence of cancer, and an increasing demand for non-invasive therapeutic options [2] [3].
Photodynamic Therapy (PDT)
Mechanism of Action
PDT is a clinically established modality that uses a triad of components: a photosensitizing drug, light of a specific wavelength, and tissue oxygen [50]. The mechanism begins with the administration of a photosensitizer (PS), which preferentially accumulates in tumor tissue. Upon illumination with light of an appropriate wavelength, the PS absorbs photon energy and transitions to an excited singlet state. This excited state undergoes intersystem crossing to a longer-lived triplet state, which can then transfer energy to surrounding molecular oxygen ((O2)) [50]. This energy transfer generates reactive oxygen species (ROS), primarily singlet oxygen ((^1O2)), which exert cytotoxic effects through oxidative damage to cellular structures including lipids, proteins, and nucleic acids [50].
PDT induces tumor destruction through three interconnected mechanisms:
- Direct Cellular Damage: ROS directly damage tumor cells, triggering necrotic or apoptotic cell death pathways [50].
- Vascular Damage: PDT targets the tumor vasculature, causing vascular shutdown that disrupts oxygen and nutrient supply to the tumor [50].
- Inflammatory and Immune Response: The therapy induces a localized inflammatory reaction and can stimulate a systemic immune response against tumor antigens, contributing to long-term tumor control [50].
Clinical Applications and Photosensitizers
PDT has received regulatory approval for various cancers, particularly those in cosmetically and functionally critical areas like the skin, esophagus, lung, and cervix [50]. Its ability to be re-administered without cumulative toxicity makes it valuable for managing recurrent or unresectable tumors [50].
Table 1: Clinically Established Photosensitizers in Oncology
| Photosensitizer | Key Indications | Approval Status |
|---|---|---|
| Porfimer sodium (Photofrin) | Esophageal carcinoma, Non-small cell lung carcinoma, Barrett's esophagus | Commercially available [50] |
| Aminolevulinic acid (ALA) & its analogue MAL | Actinic keratosis, Superficial basal cell carcinoma | Approved for dermatological applications [50] |
| Temoporfin | Head and neck cancers | Under investigation in clinical trials [50] |
The global clinical pipeline includes over ten photosensitizers in various development phases, with companies like Pinnacle Biologics, Biofrontera, and Soligenix actively engaged in R&D [50]. The global cancer PDT market potential exceeds USD 6 billion, indicating significant growth and investment in this sector [50].
Experimental Protocol: In Vitro PDT Efficacy Assessment
Objective: To evaluate the cytotoxicity of a novel photosensitizer on a specific cancer cell line.
Materials:
- Photosensitizer: Compound of interest (e.g., Temoporfin derivative).
- Cell Line: Relevant cancer cell line (e.g., A549 for lung cancer).
- Light Source: Laser or LED system matched to the PS absorption peak (e.g., 630 nm red light for many PS).
- Controls: Untreated cells, light-only control, drug-only control.
- Assay Kits: Cell viability assay (e.g., MTT, CellTiter-Glo).
- ROS Detection Kit: e.g., (H_2DCFDA) assay for reactive oxygen species.
- Equipment: Cell culture facility, microplate reader, fluorescence microscope.
Methodology:
- Cell Seeding: Seed cells in a 96-well plate at a density of (5 \times 10^3) to (1 \times 10^4) cells per well and culture for 24 hours.
- PS Incubation: Prepare a dilution series of the PS in culture medium. Add these solutions to the cells and incubate in the dark for a predetermined time (e.g., 4-24 hours) to allow for cellular uptake.
- Washing & Irradiation: After incubation, wash the cells with PBS to remove extracellular PS. Add fresh PBS or medium and expose the plates to a specific light dose (e.g., 10-100 J/cm²). Precisely control light fluence rate and exposure time.
- Post-Irradiation Incubation: Replace the irradiation medium with fresh culture medium and return the plates to the incubator for a further 24-48 hours.
- Viability Assessment: Perform a cell viability assay according to the manufacturer's instructions. Measure absorbance or luminescence with a microplate reader.
- ROS Detection: In parallel experiments, after irradiation, incubate cells with the ROS detection probe. Measure fluorescence intensity at specific time points using a microplate reader or fluorescence microscope.
- Data Analysis: Calculate percentage cell viability relative to untreated controls. Use the drug-only and light-only controls to confirm that toxicity is light-dependent. Determine (IC_{50}) values and analyze ROS generation kinetics.
Diagram 1: Photodynamic Therapy (PDT) Mechanism of Action.
Photothermal Therapy (PTT)
Mechanism of Action
PTT is a hyperthermia-based treatment that utilizes photothermal agents (PTAs) to convert absorbed light energy, typically from near-infrared (NIR) lasers, into heat [51] [52]. The localized temperature increase causes irreversible damage to cancer cells through protein denaturation and membrane disruption [51]. Temperature dictates the mode of cell death: temperatures exceeding 49°C predominantly induce necrosis, while a range of 46–49°C more commonly triggers apoptosis [51]. Additionally, PTT can stimulate autophagic cell death and generate reactive oxygen species, contributing to its cytotoxic efficacy [51].
A significant advancement is the distinction between traditional PTT (≥45°C) and mild-temperature PTT (MPTT, 41–45°C) [52]. While traditional PTT is highly effective at tumor cell ablation, MPTT is less damaging to normal tissues and is increasingly recognized for its ability to modulate the tumor microenvironment and synergize with immunotherapy [52].
Photothermal Agents (PTAs) and Their Properties
The efficacy of PTT hinges on the performance of PTAs. An ideal PTA should exhibit high photothermal conversion efficiency (PCE), excellent biocompatibility, and stability [51] [52]. Their performance is influenced by size, shape, surface modifications, and absorption wavelength [51] [52]. There is growing interest in agents absorbing in the NIR-II window (1000–1500 nm) due to its deeper tissue penetration and reduced scattering compared to the NIR-I window [52].
Table 2: Classes of Photothermal Agents (PTAs) for Cancer Therapy
| PTA Category | Examples | Photothermal Conversion Efficiency (PCE) | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Inorganic PTAs | Gold Nanorods (AuNRs), Fe₃O₄ NPs, Mn-BDP Nas [52] | High (>85% for some) [52] | High PCE, tunable optics, multifunctionality [51] | Complex synthesis, potential long-term toxicity, poor biodegradability [51] [52] |
| Organic PTAs | Indocyanine Green, Aza-BODIPY, Nanocarbon Dots (CDs) [51] [53] | Variable | High biocompatibility, biodegradability, low systemic toxicity [51] | Lower photostability in some cases [53] |
| Biomaterials/Hybrids | PVA-MoS₂-R837 Hydrogel [52] | High | Synergistic effects, tunable properties | Complex fabrication and characterization [52] |
Nanocarbon dots (CDs) are an emerging class of organic PTAs attracting attention due to their good biocompatibility, tunable optical properties, and facile synthesis [53]. Research focuses on optimizing their structure and composition to enhance PCE for therapeutic applications [53].
Experimental Protocol: Evaluating PTT Efficacy In Vivo
Objective: To assess the antitumor efficacy and biodistribution of a novel PTA in a murine tumor model.
Materials:
- PTA: Nanoparticle suspension (e.g., AuNRs or Carbon Dots).
- Animal Model: Mice with subcutaneously implanted tumors (e.g., 4T1 breast cancer model).
- Light Source: NIR Laser (e.g., 808 nm or 1064 nm) with a collimator.
- Imaging System: Photoacoustic imager or fluorescence imager (if PTA is fluorescent).
- Infrared Thermal Camera: To monitor temperature changes in real-time.
- Other: Caliper for tumor measurement, reagents for histology (e.g., H&E staining).
Methodology:
- Tumor Inoculation: Inoculate mice subcutaneously with cancer cells and allow tumors to grow to a palpable size (~50-100 mm³).
- Grouping: Randomize mice into four groups: (1) PTT Group (PTA + Laser), (2) Laser-only Control, (3) PTA-only Control, and (4) Untreated Control.
- PTA Administration: Intravenously inject the PTA suspension (e.g., 100 µL at 1 mg/mL) into the PTT and PTA-only groups. The control groups receive an injection of PBS.
- Biodistribution and Imaging: At various time points post-injection (e.g., 6, 12, 24 h), use photoacoustic or fluorescence imaging to track the accumulation of the PTA in the tumor and major organs.
- Laser Irradiation: When PTA accumulation in the tumor is maximal (e.g., at 24 h), anesthetize the mice in the PTT and Laser-only groups. Irradiate the tumor area with the NIR laser at a predetermined power density (e.g., 0.5-1.0 W/cm²) for 10 minutes. Use the thermal camera to record the temperature change in the tumor every minute.
- Efficacy Monitoring: Measure tumor dimensions and body weight every 2-3 days post-treatment. Calculate tumor volume using the formula: ( V = (length \times width^2)/2 ).
- Histological Analysis: At the endpoint, euthanize the animals and harvest tumors and major organs. Process tissues for H&E staining and other immunohistochemical analyses (e.g., for apoptosis TUNEL assay, immune cell markers CD4/CD8) to evaluate treatment effects and safety.
Diagram 2: Photothermal Therapy (PTT) Pathways and Outcomes.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for PDT and PTT
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Photosensitizers (PS) | Light-activated generation of ROS for PDT. | Porfimer Sodium, Aminolevulinic Acid (ALA), Temoporfin, and novel compounds in clinical pipelines [50]. |
| Photothermal Agents (PTA) | Convert NIR light to localized heat for PTT. | Gold Nanorods (AuNRs), Carbon Nanotubes, Graphene oxides, Nanocarbon Dots (CDs), MoS₂ nanosheets [51] [52] [53]. |
| NIR Lasers | Light source for activating PTAs and some PS. | Wavelengths: NIR-I (750-1000 nm, e.g., 808 nm) and NIR-II (1000-1500 nm, 1064 nm). Key parameters: power density and pulse width [51] [52]. |
| Visible/Red Light Sources | Light source for activating most PS in PDT. | Lasers or LED systems at specific wavelengths (e.g., 630 nm, 650 nm). Require precise dosimetry (Fluence rate in mW/cm², total Fluence in J/cm²) [50]. |
| Cell Viability Assays | Quantify cytotoxicity of PDT/PTT treatments in vitro. | MTT, CellTiter-Glo Luminescent assays. |
| ROS Detection Kits | Detect and quantify reactive oxygen species generation in PDT/MPTT. | (H_2DCFDA) assay, Singlet Oxygen Sensor Green [51]. |
| Animal Tumor Models | Evaluate in vivo efficacy and biodistribution. | Subcutaneous xenograft models (e.g., 4T1, CT26); genetically engineered models. |
| In Vivo Imaging Systems | Track agent biodistribution and monitor treatment efficacy. | Photoacoustic Imaging (PAI), Fluorescence Imaging (especially NIR-II), IVIS systems [52] [3]. |
| Infrared Thermal Cameras | Monitor real-time temperature changes during PTT in vivo. | Essential for ensuring target temperature is reached and for safety monitoring [52]. |
Synergistic Approaches and Clinical Translation
Combining PTT with Immunotherapy
A leading frontier in biophotonics is the combination of therapies, particularly Immuno-Photothermal Therapy (IPTT) [52]. MPTT has been shown to remodel the tumor microenvironment by alleviating hypoxia, inducing immunogenic cell death (ICD), and promoting the release of tumor-associated antigens [52]. This converts immunologically "cold" tumors into "hot" ones, making them more susceptible to immune attack. When combined with immune checkpoint inhibitors (e.g., anti-PD-1, anti-PD-L1, anti-CTLA-4 antibodies), MPTT can synergistically enhance antitumor immunity, leading to improved outcomes in preclinical models and addressing challenges of tumor heterogeneity and immune escape [52]. For instance, a hydrogel loaded with molybdenum disulfide and the immune adjuvant R837 significantly inhibited postoperative breast cancer recurrence in a preclinical model [52].
Challenges and Future Directions
Despite their promise, the clinical translation of PDT and PTT faces several hurdles. For PTT, key challenges include the limited penetration depth of light, heterogeneous heat distribution, potential off-target toxicity of inorganic PTAs, and insufficient efficacy as a monotherapy [51] [52]. For PDT, limitations encompass prolonged patient photosensitivity, dependence on tissue oxygen levels in often hypoxic tumors, and similarly limited light penetration [50].
Future directions to overcome these challenges include:
- Development of Novel Agents: Creating PTAs/PSs with absorption in the NIR-II window for deeper penetration, and organic or biodegradable agents with improved safety profiles [51] [52] [53].
- Combinatorial Strategies: Integrating PDT/PTT with chemotherapy, radiotherapy, and especially immunotherapy to achieve synergistic effects and overcome resistance [50] [52].
- Technological Advancements: Leveraging artificial intelligence (AI) for image analysis and treatment planning, and advancing light delivery systems for greater precision and efficacy [1] [3].
- Addressing Translational Hurdles: Focusing on standardized evaluation criteria, understanding long-term biosafety and biodistribution of agents, and conducting robust clinical trials to validate efficacy [51] [53].
Diagram 3: Immuno-Photothermal Therapy (IPTT) Synergy Mechanism.
Biophotonics, defined as the interdisciplinary fusion of light-based technologies with biology and medicine, is rapidly transforming scientific research and clinical practice [1]. This field leverages the properties of light to analyze and manipulate biological materials at the molecular, cellular, and tissue levels, offering significant advantages such as non-contact measurement, high sensitivity, and minimal invasiveness [1]. Within this dynamic discipline, two powerful tools have emerged for precision interaction with biological systems: optical tweezers for micromanipulation and force measurement, and laser micro-scalpels for high-precision ablation and surgery at cellular scales. These technologies exemplify the core biophotonics areas of biosensing and treatment, enabling both fundamental investigations of life processes and advanced therapeutic applications [1]. This guide provides an in-depth technical examination of both tools, detailing their physical principles, experimental methodologies, and applications for researchers and drug development professionals.
Optical Tweezers: Principles and Applications
Fundamental Working Principles
Optical tweezers use light to manipulate microscopic objects, leveraging the momentum transfer that occurs when photons are refracted or scattered by a dielectric particle [54] [55]. A focused laser beam, typically from an infrared laser source to minimize photodamage to biological samples, creates a three-dimensional potential well that can trap particles ranging from nanometers to hundreds of micrometers in size [54] [56]. The operation relies on two primary force components:
- Gradient force: Arises from the intensity profile of the Gaussian laser beam, creating an attractive force that pulls particles toward the region of highest light intensity at the beam's center [55].
- Scattering force: Results from photon scattering at the particle surface, producing a net momentum transfer that pushes the particle along the direction of beam propagation [54] [55].
A stable optical trap is achieved when the gradient force dominates, enabling precise positioning of particles against Brownian motion with piconewton force resolution and nanometer displacement tracking [54] [56]. When a trapped particle displaces from the trap center, the restoring force follows Hooke's law (F = -kx), functioning as an "optical spring" with a characteristic stiffness [54].
Key Experimental Configurations
Table 1: Common Experimental Geometries for Optical Tweezers
| Geometry | Description | Typical Applications | Force Resolution | Displacement Resolution |
|---|---|---|---|---|
| Single-trap | One optical trap holding a microsphere | Confinement, organization, tracking movement | ~0.1 pN | ~1 nm |
| Dual-trap | Two independently controlled traps | Single-molecule stretching, molecular motor studies | ~0.01 pN | <1 nm |
| Optical Torque | Trap with rotational control | DNA supercoiling, rotary molecular motors | ~0.1 pN·nm | <0.1 rad |
| Combined fluorescence | Optical trap integrated with single-molecule fluorescence | Correlating mechanical and chemical events in biomolecules | ~1 pN | ~10 nm |
Standardized Experimental Protocol
Experiment: Measuring DNA Elasticity Using Dual-Trap Optical Tweezers
Objective: Quantify the force-extension relationship of a single DNA molecule to characterize its elastic properties.
Materials and Reagents:
- Beads: Polystyrene or silica microspheres (1-3 μm diameter)
- DNA construct: Labeled with digoxigenin on one end and biotin on the other
- Antibody coating: Anti-digoxigenin and streptavidin for functionalizing beads
- Buffer solution: Appropriate ionic strength (e.g., PBS or Tris-EDTA with oxygen scavengers)
Procedure:
- Sample preparation:
- Incubate anti-digoxigenin-coated beads with DNA construct for 15-30 minutes
- Mix with streptavidin-coated beads at optimal dilution
- Introduce sample into flow chamber mounted on microscope
Instrument setup:
- Align dual optical traps in the sample plane with ~5-10 μm separation
- Calibrate trap stiffness using power spectrum analysis of Brownian motion [56]
- Verify position detection system using known bead displacements
Molecule tethering:
- Trap one bead type in each optical trap
- Bring beads into proximity to form DNA tether
- Verify single-molecule attachment by characteristic force-extension behavior
Data acquisition:
- Move one trap position relative to the other at constant velocity (50-100 nm/s)
- Record bead positions at high bandwidth (>10 kHz)
- Convert position data to force and extension using calibration parameters
- Repeat stretching and relaxation cycles to check reproducibility
Data analysis:
- Fit force-extension data to Worm-Like Chain (WLC) model: ( F(x) = \frac{kB T}{p} \left[ \frac{1}{4}\left(1 - \frac{x}{Lc}\right)^{-2} + \frac{x}{Lc} - \frac{1}{4} \right] ) where ( p ) is persistence length and ( Lc ) is contour length
- Extract DNA elastic parameters from fit
Figure 1: Workflow for DNA elasticity measurements using dual-trap optical tweezers.
Research Reagent Solutions
Table 2: Essential Reagents for Optical Tweezers Experiments
| Reagent/Material | Function | Specific Examples | Considerations |
|---|---|---|---|
| Dielectric beads | Handles for manipulation | Polystyrene, silica spheres (0.5-3 μm) | Size uniformity, surface functionalization |
| Surface chemistry | Molecular attachment | Digoxigenin/antidigoxigenin, biotin/streptavidin | Binding strength, specificity |
| Oxygen scavengers | Reduce photodamage | Glucose oxidase/catalase, Trolox | Buffer compatibility, longevity |
| Viscosity standards | Calibration | Sucrose solutions, glycerol | Temperature control, known viscosity |
| Fluorescent tags | Combined manipulation/imaging | Cy3, Alexa Fluor dyes | Photostability, compatibility with laser traps |
Laser Micro-Scalpels: Principles and Applications
Technology Fundamentals
Laser micro-scalpels represent a class of surgical tools that use focused laser energy for high-precision ablation of biological tissues at cellular and subcellular scales [57]. Different laser types are selected based on their absorption characteristics by biological materials:
- CO₂ lasers (λ = 10.6 μm): Strongly absorbed by water in soft tissues, making them ideal for precise cutting with minimal thermal damage to surrounding areas (thermal coagulation zone as small as 50 μm) [57].
- Er:YAG lasers (λ = 2.94 μm): Also well-absorbed by water, used for delicate procedures including blood vessel repair and areas requiring small incisions [57].
- Excimer lasers (ultraviolet): Used for procedures requiring minimal thermal effects, such as corneal reshaping in ophthalmology [57].
- Fiber-delivered systems: Recent advances enable flexible delivery of laser energy through specialized fibers, allowing access to previously inaccessible anatomical regions [57] [58].
The fundamental mechanism involves photothermal ablation, where laser energy is converted to heat, rapidly vaporizing tissue water content. The precision arises from the focused beam diameter and pulse duration, which can be controlled to target specific cell types or subcellular structures.
Key Application Modalities
Table 3: Laser Micro-Scalpel Applications by Laser Type
| Laser Type | Wavelength | Primary Applications | Precision Scale | Key Advantages |
|---|---|---|---|---|
| CO₂ | 10.6 μm | Soft tissue surgery, tumor excision, oral surgery | Cellular (50 μm zone) | Minimal bleeding, reduced swelling |
| Er:YAG | 2.94 μm | Dermatology, blood vessel repair | Cellular to subcellular | Excellent water absorption, minimal penetration |
| Excimer | 193-351 nm | Corneal reshaping, precision ablation | Subcellular | Cold ablation, minimal thermal damage |
| Nd:YAG | 1.064 μm | Vascular surgery, dermatology | Cellular | Good fiber delivery, coagulation properties |
| Fiber-based | Varies | Minimally invasive surgery, spinal procedures | Cellular | Access to confined anatomical spaces |
Standardized Experimental Protocol
Experiment: Subcellular Ablation Using Pulsed Laser Micro-Scalpel
Objective: Precisely ablate specific subcellular structures while maintaining viability of surrounding cells to study wound healing or cellular mechanics.
Materials and Reagents:
- Cell culture: Appropriate cells (e.g., neurons, epithelial cells) on imaging-compatible substrates
- Fluorescent markers: Cell membrane, organelle, or viability stains
- Imaging medium: Physiologically balanced solution with pH buffering
- Calibration standards: Thin films with known absorption properties
Procedure:
- System setup and calibration:
- Align laser path through microscope objective (typically high NA, 40-100×)
- Characterize focal spot size using knife-edge method or subresolution beads
- Calibrate pulse energy with power meter at sample plane
- Establish correlation between pulse parameters and ablation crater size using calibration standards
Sample preparation and imaging:
- Plate cells at appropriate density on coverslip-bottom dishes
- Introduce fluorescent markers for target structures if needed
- Mount sample on microscope stage with environmental control (37°C, 5% CO₂)
- Identify target cells and structures using low-intensity brightfield or fluorescence imaging
Ablation protocol:
- Switch to high-speed shutter system to control exposure
- Position laser focus at target location using positioning system
- Apply single or multiple pulses with predetermined energy (typically 1-100 μJ)
- Use pulse durations of nanoseconds to microseconds for minimal thermal diffusion
- Immediately verify ablation using phase contrast or low-light fluorescence
Post-ablation analysis:
- Time-lapse imaging to document dynamic responses
- Assess cell viability using fluorescent markers (e.g., propidium iodide, calcein-AM)
- Fix cells at predetermined time points for immunostaining if needed
- Quantify wound closure rates, organelle redistribution, or molecular recruitment
Data quantification:
- Measure ablation precision (crater size vs. target size)
- Calculate collateral damage zone using viability markers
- Document cellular responses with appropriate statistical analysis
Figure 2: Experimental workflow for subcellular ablation using laser micro-scalpels.
Research Reagent Solutions
Table 4: Essential Reagents for Laser Micro-Scalpel Applications
| Reagent/Material | Function | Specific Examples | Considerations |
|---|---|---|---|
| Cell viability markers | Assess collateral damage | Calcein-AM (live), propidium iodide (dead) | Compatibility with laser wavelength |
| Organelle-specific dyes | Target identification | MitoTracker, ER-Tracker, LysoTracker | Photostability, toxicity |
| Extracellular matrix coatings | Physiological substrate | Matrigel, collagen, fibronectin | Thickness uniformity, reproducibility |
| Antibody conjugates | Post-ablation staining | Phospho-specific antibodies, structure markers | Fixation compatibility, specificity |
| Environmental control reagents | Maintain physiological conditions | HEPES buffer, CO₂-independent medium | Stability during imaging |
Integrated Applications in Biophotonics Research
The true power of biophotonics emerges when optical manipulation and ablation technologies integrate with other modalities. Combined systems such as optical tweezers with fluorescence microscopy or laser micro-scalpels with real-time imaging represent cutting-edge platforms for investigating complex biological processes [1] [55]. These integrated approaches enable researchers to not only observe but also actively intervene in biological systems with unprecedented precision.
Recent innovations include the combination of optical tweezers with single-molecule fluorescence to correlate mechanical events with molecular binding or conformational changes [56], and the integration of laser ablation with advanced imaging techniques like multiphoton microscopy for targeted intervention in thick tissues [1]. The ongoing development of multifunctional fibers that combine laser delivery, imaging guidance, and even sensing capabilities promises to further enhance the capabilities of these platforms for minimally invasive applications [58].
As these technologies continue to evolve, driven by advances in laser sources, nanofabrication, and computational methods, they will undoubtedly open new frontiers in both basic research and clinical applications. From elucidating the fundamental mechanisms of disease to enabling increasingly precise surgical interventions, optical tweezers and laser micro-scalpels exemplify the transformative potential of biophotonics in advancing human health and scientific understanding.
Biophotonics is an interdisciplinary field at the intersection of light-based technologies, biology, and medicine. It involves the generation and application of photons (light) to image, detect, and manipulate biological materials at various scales, from single molecules and cells to tissues and entire organisms [1]. The core premise of biophotonics is the interaction between light and biological matter, characterized by phenomena such as absorption, emission, reflection, and scattering [1]. This field is recognized as a cornerstone of 21st-century life sciences, driving innovations across fundamental research, medical diagnostics, therapy, and environmental monitoring [1].
The scope of biophotonics research is traditionally divided into three main technological areas:
- Bioimaging: Enables the characterization of biological specimens across spatial scales, from nanoscopic intracellular interactions to macroscopic tissue structures [1].
- Biosensing: Allows for the detection of biomolecules, such as disease-specific biomarkers, with ultra-high sensitivity down to single-molecule resolution [1].
- Treatment and Control: Utilizes lasers and other light sources for highly precise, minimally invasive surgical interventions, while also enabling real-time monitoring of therapeutic efficacy [1].
This whitepaper explores the integration of nanorobotics with these biophotonic technologies, creating a powerful synergy for revolutionizing targeted drug delivery systems.
Fundamentals of Nanorobotics for Biomedical Applications
Nanorobotics involves the design, fabrication, and control of robots at the nanoscale (1–100 nm) to perform specific tasks within biological systems [59] [60]. These nanorobots are engineered machines capable of being programmed to interact with their environment on a molecular or cellular level [59]. For drug delivery, they function as active transport vehicles, navigating through the body to deliver therapeutic payloads directly to diseased cells with unparalleled precision, thereby minimizing systemic side effects and enhancing treatment efficacy [61].
A critical challenge at the nanoscale is locomotion. Nanorobots must operate in a low Reynolds number environment where viscous forces dominate inertial forces, and Brownian motion poses a significant challenge to controlled movement [61]. To overcome this, nanorobots harvest energy from external sources or their immediate environment. The table below summarizes the primary actuation mechanisms used for nanorobotic propulsion.
Table 1: Actuation Mechanisms for Nanorobots
| Actuation Mechanism | Principle of Operation | Key Characteristics |
|---|---|---|
| Magnetic Actuation [60] [61] | External magnetic fields exert force and torque on magnetic components integrated into the nanorobot. | Precise remote control; ability to navigate in deep tissues; good biocompatibility. |
| Chemical Propulsion [61] | Asymmetric catalytic reactions (e.g., with hydrogen peroxide or gastric acid) generate propulsive force via bubble ejection or self-diffusiophoresis. | High propulsion power in specific environments; fuel dependency can limit application. |
| Acoustic Propulsion [61] | Asymmetric steady streaming is produced by ultrasonic fields, propelling the nanorobot. | Effective in various biological fluids; deep tissue penetration; no need for chemical fuels. |
| Bio-hybrid Systems [59] [61] | Integration of motile biological entities (e.g., sperm, bacteria) with synthetic nanostructures. | Leverages natural mobility and sensing capabilities; complex fabrication. |
The Convergence of Biophotonics and Nanorobotics
The integration of biophotonics and nanorobotics creates a symbiotic relationship that enhances the capabilities of both fields. Biophotonic tools provide the means to visualize, track, and control nanorobots, while nanorobots act as targeted platforms for delivering and applying photonic therapies with high spatial precision [60].
This convergence enables several advanced functions:
- Image-Guided Navigation and Tracking: Techniques like Near-Infrared II (NIR-II) fluorescence imaging offer deeper tissue penetration and higher resolution, allowing for real-time tracking of nanorobot swarms as they navigate toward a tumor [3]. Optical Coherence Tomography (OCT) provides high-speed, 3D imaging to monitor nanorobot position in dynamic environments [1].
- Optical Sensing and Control: Nanorobots can be functionalized with contrast agents or designed to respond to optical signals. For instance, nonlinear optical phenomena like multi-photon absorption can be used to trigger drug release with high spatial precision deep within tissue [1].
- Light-Activated Therapy: The combination enables advanced modalities such as photodynamic therapy (PDT), where nanorobots deliver photosensitizers directly to cancer cells. Subsequent illumination with specific light wavelengths activates these agents, generating cytotoxic reactive oxygen species that selectively kill the target cells [60].
The following diagram illustrates the integrated workflow of a nanorobotic system guided by biophotonic sensing and triggering.
Quantitative Data and Market Landscape
The field of integrated biophotonics and nanorobotics is not only scientifically promising but also experiencing significant commercial growth. The global biophotonics market, valued at USD 76.1 billion in 2024, is projected to grow at a compound annual growth rate (CAGR) of 11.3% to reach USD 220.1 billion by 2034 [3]. This growth is partly driven by the emergence of nanotechnology, which enhances the performance of diagnostic and therapeutic tools [3].
The nanorobotics sector is similarly robust, projected to grow at a CAGR of 8.3% from 2025 to 2033 [62]. Key application segments within biophotonics are expanding rapidly, as shown in the table below.
Table 2: Biophotonics Market Application Segments (Data sourced from [3])
| Application Segment | Market Size (2024) | Projected CAGR (2025-2034) | Key Drivers |
|---|---|---|---|
| Spectro Molecular | USD 15.1 Billion | Significant Growth | Demand for molecular-level diagnostics and precision medicine. |
| See-Through Imaging | Not Specified | 13.7% (Highest) | Non-invasive, high-resolution visualization for surgery and early detection. |
| Medical Therapeutics | Not Specified | Significant Growth | Expansion in laser and photodynamic therapies for oncology, dermatology. |
| In-Vivo Technologies | 57% Market Share (2024) | Continued Dominance | Advancements in optical imaging and laser diagnostics for early cancer detection. |
Detailed Experimental Protocols and Methodologies
To illustrate the practical implementation of these integrated systems, we detail two foundational protocols based on recent research.
Protocol 1: Synthesis and In Vitro Testing of Magnetically Guided Drug-Loaded Nanorobots
This protocol outlines the creation of helical nanorobots for targeted drug delivery, inspired by bacterial flagella [61].
1. Materials and Reagents:
- Silicon Dioxide (SiO₂) Substrate: For the template-assisted synthesis.
- Chrome (Cr) and Nickel (Ni): Evaporated in a glancing-angle deposition (GLAD) process to form the helical structure.
- Anticancer Drug (e.g., Doxorubicin): The therapeutic payload.
- Polymeric Coating (e.g., PLGA): To encapsulate the drug and functionalize the nanorobot surface.
- Cell Culture (e.g., HeLa cells): In vitro model for testing.
2. Fabrication Procedure: a. Template Preparation: Clean a SiO₂ substrate and prepare it for deposition. b. GLAD Evaporation: Sequentially evaporate a thin layer of Cr (for adhesion) followed by Ni at a glancing angle (e.g., 85° from normal). The substrate is rotated at a specific speed to control the pitch and diameter, forming the helical structure. c. Drug Loading: Immerse the nanorobots in a concentrated solution of the drug. Subsequently, apply a biodegradable polymeric coating via dip-coating or electrochemical deposition to seal the drug within the structure. d. Functionalization: Conjugate targeting ligands (e.g., antibodies, folic acid) to the polymer surface to enable specific binding to cancer cells.
3. In Vitro Testing and Actuation: a. Propulsion and Control: Disperse the nanorobots in a cell culture medium within a custom-built setup equipped with 3D Helmholtz coils. b. Magnetic Actuation: Apply a rotating magnetic field (1-10 mT) to actuate the nanorobots, causing them to swim along a controlled path. c. Targeting and Uptake: Steer the nanorobots toward a monolayer of target cells. Monitor the interaction and subsequent cellular internalization using time-lapse microscopy. d. Drug Release and Efficacy: Trigger drug release via the enzymatic degradation of the polymer coating or by applying a localized thermal stimulus. Quantify treatment efficacy using cell viability assays (e.g., MTT assay) and compare to control groups.
Protocol 2: Structural Characterization of Lipid Nanoparticles (LNPs) using Synchrotron Small-Angle X-ray Scattering (SEC-SAXS)
Recent research has revealed that lipid nanoparticles (LNPs), crucial nanocarriers for drugs and RNA, possess complex and varied internal structures that significantly impact their function [63]. This protocol details their comprehensive structural characterization.
1. Materials and Reagents:
- LNP Formulations: Including "gold-standard" formulations like those used in COVID-19 mRNA vaccines and Onpattro.
- Buffers: Appropriate aqueous buffers to maintain LNP integrity in solution.
2. Equipment:
- Size-Exclusion Chromatography (SEC) System: To separate LNPs by size.
- Synchrotron SAXS Facility: Such as the National Synchrotron Light Source II (NSLS-II).
- Sedimentation Velocity Analytical Ultracentrifugation (SV-AUC).
- Field-Flow Fractionation coupled to Multi-Angle Light Scattering (FFF-MALS).
3. Experimental Workflow: a. Sample Preparation: Prepare LNP samples using both microfluidic devices (for consistency) and hand-mixing via micropipettes (which can introduce functional variation). Dilute samples in a suitable buffer. b. Multi-Technique Analysis: i. SEC-SAXS: The LNPs are first separated by size via SEC. The effluent is then exposed to a high-intensity, monochromatic X-ray beam at the synchrotron facility. The resulting scattering patterns are analyzed to determine the internal structure and electron density distribution of the particles. ii. SV-AUC: LNPs are spun at high speeds (e.g., 40,000 rpm). The rate at which they sediment provides information about their density and hydrodynamic size. iii. FFF-MALS: LNPs are gently separated by size in a channel with a perpendicular flow field. The MALS detector measures the absolute size and the distribution of the nucleic acid cargo across different particle populations. c. Data Correlation: Integrate datasets from all three techniques to build a comprehensive and reliable model of the LNP population, revealing variations in shape, internal structure, and cargo packaging that are invisible to single-method analysis [63].
The following diagram visualizes this multi-technique characterization workflow.
The Scientist's Toolkit: Key Research Reagents and Materials
Successful research in this field relies on a suite of specialized materials and reagents. The table below lists essential components for developing and testing integrated nanorobotic-biophotonic systems.
Table 3: Essential Research Reagents and Materials for Nanorobotic-Biophotonic Systems
| Category / Item | Specific Examples | Function and Application |
|---|---|---|
| Nanorobot Structural Materials | ||
| ∙ Magnetic Materials | Nickel (Ni), Iron Oxide (Fe₃O₄) | Enables actuation and guidance via external magnetic fields [61]. |
| ∙ Biodegradable Polymers | Poly(lactic-co-glycolic acid) (PLGA), Chitosan | Forms the body of the nanorobot; allows for degradation and controlled drug release [64] [61]. |
| ∙ Biological Templates | DNA Origami | Provides a highly programmable, self-assembling scaffold for building complex nanostructures [59]. |
| Actuation Fuels & Components | ||
| ∙ Chemical Fuels | Hydrogen Peroxide (H₂O₂) | Serves as a propellant for catalytic micro/nanorockets in specific in vitro environments [61]. |
| ∙ Ionizable Lipids | Proprietary lipids (e.g., DLin-MC3-DMA) | A key component of Lipid Nanoparticles (LNPs) for encapsulating and delivering RNA-based therapeutics [63]. |
| Biophotonic Agents & Reagents | ||
| ∙ Fluorescent Dyes & Quantum Dots | NIR-II fluorophores, Indocyanine Green (ICG) | Provides contrast for deep-tissue imaging and real-time tracking of nanorobots [3]. |
| ∙ Photosensitizers | Porphyrin-based molecules | Used in Photodynamic Therapy (PDT); generates cytotoxic species upon light activation [60]. |
| ∙ Functionalization Ligands | Antibodies, Hyaluronic Acid, Folic Acid | Coated on nanorobot surface for active targeting of specific cell receptors (e.g., CD44, folate receptor) [64] [60]. |
| Characterization Equipment | ||
| ∙ Synchrotron X-ray Source | National Synchrotron Light Source II (NSLS-II) | Enables high-resolution structural analysis of nanoparticles via SAXS [63]. |
| ∙ Multi-Angle Light Scattering (MALS) | Wyatt Technology systems | Measures absolute size and molecular weight of nanoparticles in solution [63]. |
Challenges and Future Perspectives
Despite the considerable progress, several challenges must be addressed to advance these integrated systems from the laboratory to the clinic.
- Biocompatibility and Toxicity: Ensuring that nanorobots and their degradation byproducts are non-toxic and do not elicit adverse immune responses is paramount. Materials like magnesium-based micromotors that dissolve into benign components represent a promising path forward [61].
- Navigation in Complex Biological Environments: Precise control of nanorobots in vivo is hampered by dynamic fluid flow, biological barriers (e.g., blood-brain barrier), and the need for deep tissue imaging and control systems [60]. The integration of artificial intelligence (AI) and machine learning is emerging as a key strategy to optimize navigation paths and interpret complex biological signals in real-time [3] [60].
- Manufacturing and Scalability: Reproducible, large-scale fabrication of nanorobots with complex geometries and multiple functionalities remains a significant hurdle. Advances in 3D printing and microfluidics-assisted synthesis are critical to overcoming this challenge [62].
- Regulatory Hurdles: The path to clinical approval for such complex, multi-component systems is uncharted. Establishing clear regulatory frameworks is essential for clinical translation [62].
The future of this integrated field is exceptionally promising. Emerging trends point toward the development of intelligent, autonomous systems that can diagnose a pathological condition, deliver a therapeutic payload, and monitor the treatment response in a closed-loop manner [60]. Furthermore, the concept of swarm robotics, where large collections of simple nanorobots collectively perform complex tasks, represents a frontier that could dramatically enhance drug delivery efficacy and tissue penetration [62]. As these technologies mature, they are poised to redefine precision medicine, enabling therapies that are not only targeted but also dynamically adaptive to the patient's unique physiology.
Optimizing Biophotonic Systems: Addressing Challenges with AI and Novel Materials
Biophotonics, defined as the interdisciplinary fusion of light-based technologies with biology and medicine, uses light to analyze and manipulate biological materials across fundamental research, medical diagnostics, and therapy [1]. A core principle underpinning its application is the interaction of light with biological matter through absorption, emission, reflection, and scattering [1]. While these interactions provide a wealth of contrast mechanisms, they also present the most significant technical hurdles for deep-tissue applications: limited penetration depth and intense signal scattering.
Light scattering in biological tissues rapidly degrades image resolution and signal strength as depth increases. This limits the efficacy of many optical techniques, confining them to superficial layers. Overcoming this challenge is critical for unlocking the full potential of biophotonics in non-invasive clinical diagnostics, deep-tissue imaging, and therapeutic monitoring. This whitepaper explores the fundamental principles of these hurdles and details advanced technical strategies being deployed to overcome them, providing a guide for researchers and drug development professionals.
Fundamental Principles of Light-Tissue Interaction
The propagation of light through biological tissue is governed by its optical properties, primarily absorption and scattering. Absorption involves the conversion of light energy into other forms, such as heat or fluorescence, and is quantified by the absorption coefficient (μₐ) [1] [65]. Scattering redirects the path of photons and is described by the reduced scattering coefficient (μₛ') [66]. The cumulative effect of these phenomena leads to an exponential attenuation of light intensity as it travels through tissue.
A key metric derived from these coefficients is the Penetration Depth (δ), typically defined as the depth at which the intensity of light drops to 1/e (about 37%) of its initial value. It can be approximated as δ ≈ 1/√(3μₐ(μₐ + μₛ')) [65]. This relationship clearly shows that high absorption and scattering coefficients result in shallow penetration. Different tissue types and components—such as water, hemoglobin, and lipids—have distinct absorption profiles, making the choice of illumination wavelength a critical parameter for maximizing penetration.
Table 1: Absorption Coefficients and Penetration Depths of Select Laser Wavelengths in Oral Gingival Tissue (Ex Vivo Porcine Model)
| Laser Wavelength (nm) | Laser Type | Absorption Coefficient, α (cm⁻¹) | Penetration Depth, δ (mm) |
|---|---|---|---|
| 450 (Blue) | Diode | 26.8 | ~0.37 |
| 532 (Green) | Frequency-doubled Nd:YAG | ~20.0* | ~0.50* |
| 632 (Red) | He-Ne | ~15.0* | ~0.67* |
| 810 (Infrared) | Diode | 9.6 | ~1.04 |
| 1064 (Infrared) | Nd:YAG | ~10.5* | ~0.95* |
| 2940 (Mid-IR) | Er:YAG | 144.8 | ~0.07 |
Note: Values for 532, 632, and 1064 nm are estimates interpolated from the ranked data in [65], which lists wavelengths from most to least absorbed as: 2940 nm > 2780 nm > 450 nm > 480 nm > 532 nm > 1341 nm > 632 nm > 940 nm > 980 nm > 1064 nm > 810 nm.
The data in Table 1 illustrates a fundamental trade-off: wavelengths with very high absorption (e.g., Er:YAG at 2940 nm) are ideal for superficial, precise ablation but offer minimal penetration. Conversely, wavelengths in the near-infrared (NIR) and shortwave-infrared (SWIR) "optical window" (approximately 650-1350 nm) experience lower absorption and scattering, enabling deeper light penetration for imaging and sensing applications [1] [66].
Technical Strategies for Enhanced Penetration and Reduced Scattering
Leveraging the Optical Window and Novel Imaging Modalities
A primary strategy is to shift operations from the visible spectrum into the NIR and SWIR regions. Within this window, water and hemoglobin—the primary absorbers in tissue—have minimal absorption, allowing photons to travel further [66]. Research shows that SWIR light (900-2000 nm) offers even deeper tissue penetration (approximately 2.5–3.5 mm) compared to traditional NIR, due to reduced scattering at longer wavelengths [66].
Beyond wavelength selection, novel imaging modalities that are inherently less sensitive to scattering have been developed:
- Photoacoustic Computed Tomography (PACT): This hybrid technique harnesses the photoacoustic effect, where pulsed laser light is absorbed by tissue chromophores, generating a thermoelastic expansion that emits ultrasonic waves [67]. Since ultrasound scatters ~1000 times less than light in tissue, PACT can achieve high-resolution imaging at depths exceeding 1 cm, breaking through the optical diffusion limit [67].
- Spatial Frequency Domain Imaging (SFDI): This technique projects patterns of light (sinusoidal fringes) at different spatial frequencies onto tissue. By analyzing the demodulation of these patterns, SFDI can quantitatively map both the absorption (μₐ) and reduced scattering (μₛ') coefficients over a wide field of view [66]. This allows for the quantification of chromophores like water and lipid content at depth.
Diagram 1: Photoacoustic Computed Tomography (PACT) Workflow.
Advanced Hardware and Computational Solutions
Technological advancements are also pushing the boundaries of what is possible:
- Nonlinear Microscopy: Techniques like multiphoton microscopy rely on the simultaneous absorption of two or more long-wavelength (NIR) photons. This process only occurs at the focal point, providing inherent optical sectioning, deeper penetration, and minimal out-of-focus photobleaching [1].
- Advanced Ultrasound Detectors: In PACT, the development of all-optical ultrasonic detectors, such as Fabry-Perot interferometers and micro-ring resonators (MRRs), offers broad detection bandwidth, high sensitivity, and immunity to electromagnetic noise, improving image quality [67].
- Computational and AI-Powered Methods: The integration of Artificial Intelligence (AI) and machine learning is revolutionizing image interpretation. AI algorithms can enhance resolution, reduce noise, and accelerate the reconstruction of images from scattered signal data, enabling real-time diagnostics and extracting subtle patterns invisible to the human eye [1] [3].
Experimental Protocols for Key Techniques
Protocol: Shortwave Infrared Spatial Frequency Domain Imaging (SWIR-SFDI) for Hydration Mapping
This protocol, based on recent research, details the non-invasive quantification of tissue hydration and scattering properties [66].
1. Objective: To quantify changes in tissue water content and reduced scattering coefficient (μₛ') in ex vivo and in vivo models.
2. Materials and Reagents:
- Tissue Samples: Ex vivo porcine skin or in vivo human subject skin (e.g., dorsal hand).
- Calibration Phantom: A material with known and stable optical properties (μₐ and μₛ') for system calibration.
3. Equipment Setup:
- SWIR Light Source: LEDs at specific wavelengths (e.g., 970, 1050, 1200 nm) where water and lipids have distinct absorption features.
- Pattern Projection: A Digital Micromirror Device (DMD) to project structured illumination patterns (DC and AC spatial frequencies).
- Detection: An Indium Gallium Arsenide (InGaAs) camera sensitive to SWIR light.
- Polarizers: Crossed linear polarizers to suppress surface specular reflection.
4. Experimental Procedure:
- System Calibration: Image the calibration phantom under DC (planar) and AC (sinusoidal) illumination. Use a pre-computed Monte Carlo simulation lookup table to establish a relationship between measured pixel values and absolute diffuse reflectance [66].
- Sample Imaging: Mount the sample and acquire raw images under the same DC and AC illumination patterns.
- Data Processing:
- Demodulation: Process raw images to generate DC and AC amplitude images using phase-shifted patterns.
- Conversion to Reflectance: Apply the calibration to convert demodulated images into maps of diffuse reflectance (Rₚ).
- Property Extraction: Input Rₚ into the Monte Carlo lookup table to solve for the absorption (μₐ) and reduced scattering (μₛ') coefficients at each pixel and wavelength.
- Chromophore Calculation: Use the absorption coefficients at multiple wavelengths with known molar extinction coefficients of chromophores (e.g., water, lipid) to calculate their relative concentrations.
5. Key Application: This method has demonstrated that the reduced scattering coefficient (μₛ') can be a more sensitive indicator of small changes in tissue hydration than absorption alone, proving useful for monitoring desiccation or exercise-induced perspiration [66].
Protocol: Measuring Wavelength-Dependent Absorption in Tissue
This ex vivo protocol provides a direct method for characterizing fundamental light-tissue interactions [65].
1. Objective: To determine the absorption coefficient (α), penetration depth (δ), and thermal relaxation time (TRT) of tissue for various laser wavelengths.
2. Materials:
- Tissue Samples: Fresh, non-pigmented porcine gingival mucosa.
- Stabilization Setup: Glass slides and a custom metal stabilization device.
3. Equipment:
- Laser Systems: Multiple lasers or an Optical Parametric Oscillator (OPO) system covering wavelengths of interest (e.g., 450, 810, 1064, 2940 nm).
- Power Meter: For measuring input (Pin) and output (Pout) power.
- Thickness Gauge: Calibrated electronic micrometer.
4. Experimental Procedure:
- Sample Preparation: Mount a tissue sample of measured thickness (e.g., 1.00 mm) between two glass slides to minimize extraneous light loss.
- Laser Irradiation: Irradiate the sample with a single wavelength at a known input power (e.g., 100 mW) and spot size.
- Transmission Measurement: Measure the power transmitted through the sample-glass assembly (P_out).
- Data Analysis:
- Transmittance Calculation: Calculate transmittance as T = Pout / Pin.
- Beer-Lambert Law Application: Use the law, T = e^(-α * L), where L is the sample thickness, to compute the absorption coefficient α.
- Penetration Depth Calculation: Derive the penetration depth as δ = 1/α.
6. Key Outcome: This methodology generates foundational data, as shown in Table 1, which is critical for selecting the optimal wavelength for a specific clinical application, such as choosing a deeply penetrating 810 nm diode for photobiomodulation or a highly absorbed 2940 nm Er:YAG laser for precise ablation [65].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Advanced Biophotonics Experiments
| Item | Function / Application | Specific Example |
|---|---|---|
| Optical Parametric Oscillator (OPO) | Generates tunable, discrete laser wavelengths across visible and IR spectra for multispectral studies. | Visible-range OPO system built around a BBO crystal [65]. |
| Digital Micromirror Device (DMD) | Precisely projects structured illumination patterns (e.g., sinusoidal fringes) for quantitative imaging. | Texas Instruments LightCrafter used in SWIR-SFDI [66]. |
| InGaAs Camera | Detects light in the Shortwave Infrared (SWIR) range (900-1700 nm), enabling deep-tissue imaging. | SWIR camera used in SFDI and PACT systems [66]. |
| Fabry-Perot Interferometer / Micro-Ring Resonator (MRR) | All-optical ultrasonic detector for PACT; provides broad bandwidth and is immune to electromagnetic noise. | Used in deep-tissue PACT systems for superior acoustic detection [67]. |
| Calibration Phantom | A reference with known optical properties (μₐ, μₛ') essential for quantitative system calibration. | Used in SFDI to translate raw camera data into absolute optical properties [66]. |
| Crossed Linear Polarizers | Suppresses surface glare (specular reflection) to isolate the diffuse light signal from within the tissue. | Standard component in SFDI and other reflectance imaging setups [66]. |
Diagram 2: Strategy Selection Logic for Deep-Tissue Biophotonics.
The challenges of tissue penetration depth and signal scattering are being aggressively and creatively addressed across the field of biophotonics. By leveraging the optical properties of biological tissues in the NIR and SWIR windows, developing hybrid modalities like PACT that convert light into less-scattered ultrasound, and deploying advanced computational and hardware solutions, researchers are fundamentally overcoming these traditional barriers. The experimental protocols and tools detailed herein provide a roadmap for scientists and drug development professionals to apply these cutting-edge techniques. As these technologies continue to mature, driven by interdisciplinary collaboration and AI integration, they will further solidify biophotonics as a cornerstone of next-generation, non-invasive precision medicine and deep-tissue biological research [1].
Biophotonics, defined as the interdisciplinary fusion of light-based technologies with biology and medicine, has emerged as a transformative force in scientific research and clinical practice [1]. This field leverages the properties of photons and the systems that generate, deliver, and detect them to create advanced diagnostic, analytical, and therapeutic systems [68]. The core technological areas encompass bioimaging, biosensing, and photonic-based therapies, enabling non-contact measurement, high sensitivity, and real-time information acquisition from biological systems [1]. Despite its significant potential and rapid market growth—with projections estimating expansion from $68.4 billion in 2025 to approximately $226.18 billion by 2034—the translation of biophotonic innovations from laboratory research to commercially viable products faces substantial barriers [69] [70]. These challenges include high technology costs, regulatory complexities, and the need for specialized expertise, which collectively hinder widespread market adoption [71] [3]. This whitepaper examines these commercialization barriers within the broader context of biophotonics research and presents strategic frameworks to overcome them, specifically addressing the needs of researchers, scientists, and drug development professionals working at the intersection of light-based technologies and biological applications.
Market Landscape and Quantitative Analysis
The biophotonics market demonstrates robust growth globally, driven by increasing demand for non-invasive diagnostics, technological advancements in optical technologies, and the rising prevalence of chronic diseases [3] [69]. The market encompasses diverse applications including see-through imaging, microscopy, biosensing, spectro molecular analysis, light therapy, and inside imaging [70]. Understanding the market dynamics and growth projections is essential for contextualizing commercialization challenges and opportunities.
Table 1: Global Biophotonics Market Size Projections from Multiple Sources
| Source | Base Year/Value | Projection Year/Value | CAGR | Key Segments |
|---|---|---|---|---|
| Precedence Research [69] | 2025: $92.09B | 2034: $226.18B | 10.5% | Medical diagnostics dominates (66% share) |
| BCC Research [72] | 2024: $62.6B | 2030: $113.1B | 10.6% | Spectroscopy, optical imaging, laser technologies |
| Future Market Insights [2] | 2025: $67.2B | 2035: $189.3B | 10.9% | Medical imaging, oncology, cardiovascular diagnostics |
| Market Report Analytics [71] | 2025: $38.04B | 2033: N/A | 6.5% | Imaging technologies, chronic disease diagnostics |
| Global Insights [3] | 2024: $76.1B | 2034: $220.1B | 11.3% | In-vivo applications (57% share) |
Table 2: Biophotonics Market Analysis by Technology, Application, and Region
| Category | Subcategory | Market Share/Performance | Growth Drivers |
|---|---|---|---|
| Technology | In-Vivo | 57% market share (2024) [3] | Real-time imaging, minimally invasive procedures |
| In-Vitro | 59% market share (2024) [69] | Automation, AI integration, personalized medicine | |
| Application | Medical Imaging | Largest application area [2] | Oncology, cardiovascular diagnostics, surgical guidance |
| See-Through Imaging | Highest CAGR (13.7%) [3] | Non-invasive visualization, surgical applications | |
| Spectro Molecular | $15.1B market share (2024) [3] | Molecular-level diagnostics, precision medicine | |
| Region | North America | 38% market share (2024) [69] | Advanced healthcare infrastructure, R&D investment |
| Asia-Pacific | Fastest growing (13.54% CAGR) [69] | Healthcare modernization, rising healthcare expenditure |
Regional analysis reveals that North America currently dominates the market with a 38% share, attributed to robust research infrastructure, significant funding for medical research, and the presence of major industry players [69]. Europe maintains a substantial market share supported by stringent quality standards and research initiatives, while the Asia-Pacific region is emerging as the fastest-growing market with CAGRs exceeding 13% due to rapid industrialization, expanding healthcare infrastructure, and government-driven innovation programs [3] [69]. Germany's market was valued at $3.6 billion in 2024, reflecting Europe's strong position, while China's biophotonics market is growing at a remarkable 14.1% CAGR, positioning it as a future leader in the optoelectronics landscape [3].
Analysis of Commercialization Barriers
Economic and Cost Challenges
The development and implementation of biophotonics technologies face significant economic hurdles that impact market adoption across various sectors. The high initial investment required for biophotonics equipment creates substantial entry barriers for research institutions and clinical facilities with limited budgets [71] [3]. Advanced systems such as multiphoton microscopy, optical coherence tomography (OCT), and nonlinear coherent Raman scattering systems involve sophisticated components including ultrafast lasers, precision optical elements, and sensitive detection systems that dramatically increase manufacturing costs [1] [71]. Additionally, maintenance costs and the requirement for specialized infrastructure further contribute to the total cost of ownership, making it challenging for smaller organizations to adopt these technologies [73].
Beyond equipment expenses, the commercialization pathway requires substantial investment in regulatory compliance. The rigorous approval processes for medical devices from agencies like the FDA and EMA necessitate extensive clinical trials and documentation, with costs that can reach millions of dollars and timelines extending several years [71] [70]. This financial burden is particularly challenging for startups and academic spinoffs with limited capital reserves. Furthermore, the complexity of manufacturing biophotonic devices at scale while maintaining precision and quality control presents additional cost challenges, especially for technologies incorporating nanomaterials, custom optical components, or specialized detectors [3] [72].
Technical and Integration Complexities
Biophotonics technologies face several technical barriers that impede smooth integration into existing research and clinical workflows. A significant challenge is the limited penetration depth of optical methods in biological tissues, which restricts imaging and treatment capabilities to superficial structures or requires invasive procedures for deeper analysis [4]. While technologies such as near-infrared II (NIR-II) fluorescence imaging and adaptive optics have improved penetration and resolution, these advances often come with increased complexity and cost [3] [69].
The interpretation of biophotonic data presents another substantial barrier. Techniques such as fluorescence lifetime imaging (FLIM), spectroscopic OCT, and coherent Raman scattering generate complex datasets that require specialized expertise for accurate analysis and interpretation [1] [71]. This complexity often necessitates the involvement of highly trained personnel, creating a workforce gap that limits technology adoption [71]. Additionally, integration with existing laboratory and clinical systems remains challenging due to issues with interoperability, data standardization, and workflow compatibility. For example, incorporating advanced biophotonic capabilities into traditional diagnostic pathways or research protocols requires sophisticated interface development and validation [73].
Market Access and Adoption Barriers
Market access for biophotonics technologies is constrained by several factors beyond technical performance. The limited awareness and understanding of biophotonics benefits among potential end-users, including healthcare providers and researchers, slows adoption rates [73]. This knowledge gap is particularly pronounced in developing regions, where access to advanced technologies is further limited by infrastructure constraints, inadequate training facilities, and economic limitations [69].
The reimbursement landscape for biophotonic-based procedures and diagnostics also presents significant challenges. Establishing appropriate reimbursement codes and convincing payers of the economic value of these technologies requires extensive health economics outcomes research and real-world evidence generation [71]. This process is complicated by the rapid pace of innovation in biophotonics, which often outpaces the ability of reimbursement systems to adapt. Additionally, resistance to changing established workflows and the natural conservatism in medical practice create adoption inertia, even when biophotonic solutions demonstrate clear advantages over conventional methods [73].
Strategic Frameworks for Market Adoption
Technical Development Strategies
Overcoming the technical barriers in biophotonics commercialization requires strategic approaches to technology development and integration. The implementation of AI and machine learning algorithms for data analysis and interpretation addresses the complexity challenge by automating image analysis, enhancing diagnostic accuracy, and reducing dependency on specialized expertise [3] [69]. For example, Raman spectroscopy integrated with machine learning has demonstrated 98% accuracy in detecting early breast cancer by identifying subtle chemical changes in blood samples that conventional methods miss [3].
Device miniaturization and the development of portable, handheld systems represent another crucial strategy for expanding market access. These platforms enable point-of-care diagnostics, in-vivo monitoring in real-time, and application in resource-limited settings [2] [69]. Advances in nanophotonics, including the use of metallic nanoparticles and quantum dots, facilitate this miniaturization while enhancing sensitivity and specificity for biomarker detection [3]. Furthermore, the development of multimodal systems that combine complementary biophotonic techniques addresses limitations of individual technologies by providing comprehensive diagnostic capabilities in a single platform [73].
Collaborative Commercialization Models
Strategic partnerships across academia, industry, and healthcare institutions are essential for accelerating biophotonics commercialization. Public-private partnerships leverage complementary resources and expertise to address the high costs and risks associated with technology development [3]. For instance, the German Federal Ministry of Education and Research allocated EUR 38 million toward a national biophotonics innovation initiative, demonstrating how government funding can catalyze technological advancement and infrastructure development [2].
Industry-academia collaborations facilitate knowledge transfer and provide access to specialized facilities and expertise that would otherwise be prohibitively expensive for individual organizations. These partnerships are instrumental in driving technological advancement and shortening time-to-market for emerging diagnostic technology [3]. The integration of diagnostics and therapy ("theranostics") represents another strategic approach, creating more comprehensive solutions that deliver greater clinical value and improve reimbursement potential [3]. Additionally, cross-sector collaborations between biophotonics companies and technology firms specializing in AI, sensors, or data analytics enable the development of smarter, more connected systems that address multiple market needs simultaneously [73].
Table 3: Strategic Collaboration Models in Biophotonics Commercialization
| Collaboration Type | Key Objectives | Representative Examples | Outcomes |
|---|---|---|---|
| Public-Private Partnerships | Leverage government funding, address infrastructure gaps | German Federal Ministry initiative (€38M) [2] | Accelerated technology development, shared risk |
| Industry-Academia Collaborations | Knowledge transfer, access to specialized expertise | University of Edinburgh cancer detection research [3] | Innovative applications, validation studies |
| Cross-Sector Alliances | Integrate complementary technologies, expand capabilities | AI companies partnering with imaging device manufacturers [73] | Enhanced system capabilities, new market opportunities |
| International Consortia | Address global challenges, standardize approaches | International Congress on Biophotonics 2024 [1] | Shared standards, expanded market access |
Market-Specific Adoption Strategies
Tailored approaches for different market segments and geographic regions are essential for successful biophotonics commercialization. In established markets such as North America and Europe, strategies should focus on demonstrating superior health economic outcomes compared to existing technologies, developing comprehensive training and support programs for end-users, and working closely with regulatory bodies to streamline approval processes [3] [69]. The implementation of Olympus Corporation's confocal endomicroscopy systems at University Medical Center Hamburg-Eppendorf, which resulted in a 23% reduction in biopsy procedures, exemplifies the importance of documenting and communicating tangible clinical benefits [2].
For emerging markets in Asia-Pacific, Latin America, and Africa, different strategies are required. These include developing cost-optimized systems specifically designed for resource-constrained settings, establishing local manufacturing and distribution partnerships to reduce costs and improve market access, and implementing training programs to build local expertise [69]. The growing adoption of biophotonics technologies in China and India, linked to increasing investments in digital hospitals and public healthcare modernization, demonstrates the potential of these markets when appropriate strategies are employed [2] [3].
Across all markets, targeting specific clinical applications with clear unmet needs provides a focused pathway for initial commercialization. Oncology applications, particularly early cancer detection and surgical guidance, represent particularly promising areas due to the strong clinical value proposition and established reimbursement pathways [2] [3]. Similarly, neuroscience applications leveraging technologies such as optogenetics and in-vivo imaging are experiencing significant growth, driven by advances in brain function research [4].
Essential Research Reagent Solutions and Methodologies
The advancement of biophotonics research and development relies on specialized reagents and materials that enable precise optical interrogation of biological systems. These tools form the foundation for experimental protocols and technology development across diverse applications.
Table 4: Essential Research Reagent Solutions in Biophotonics
| Reagent/Material | Function | Application Examples | Key Characteristics |
|---|---|---|---|
| Fluorescent Probes | Molecular labeling and tracking | Cell dynamics monitoring, drug delivery tracking [4] | High quantum yield, photostability, target specificity |
| Gold Nanoparticles | Signal enhancement, contrast agents | Fluorescence enhancement in membrane studies [69] | Tunable plasmonic properties, biocompatibility |
| Quantum Dots | Bright, photostable labeling | Multiplexed detection, long-term imaging [3] | Narrow emission spectra, broad excitation |
| Lanthanide-doped Crystals | Ultra-sensitive force sensing | Photonic force microscopy [4] | Unique optical properties, precision detection |
| DNA Nanostructures | Programmable scaffolds | Nanophotonic device fabrication [4] | Molecular precision, self-assembly capability |
| Photonic Crystal Materials | Light manipulation at nanoscale | Advanced biosensing platforms [2] | Precise control of light propagation |
Experimental protocols in biophotonics require careful optimization of these reagents to ensure reliable results. For fluorescence-based techniques, key methodological considerations include probe selection based on spectral characteristics, optimization of labeling density to minimize steric hindrance while ensuring sufficient signal, and implementation of appropriate controls to account for autofluorescence and photobleaching artifacts [1]. For nanoparticle-enhanced applications, critical parameters include surface functionalization for specific targeting, size optimization for tissue penetration, and thorough biocompatibility assessment [69].
Advanced methodologies such as multiphoton microscopy require high-intensity ultrashort pulse lasers precisely tuned to specific wavelengths to enable deep tissue imaging with minimal scattering [1]. Super-resolution techniques demand specialized fluorophores with specific photoswitching characteristics and sophisticated image reconstruction algorithms. Nonlinear optical methods including second harmonic generation (SHG) and third harmonic generation (THG) rely on carefully engineered laser systems and detection pathways to visualize specific structural proteins and cellular interfaces without exogenous labeling [1].
The commercialization of biophotonics technologies, while facing significant barriers related to cost, technical complexity, and market access, presents substantial opportunities for transforming biomedical research and clinical practice. Strategic approaches that leverage collaborative models, technical innovation, and market-specific adoption pathways can effectively address these challenges. The integration of artificial intelligence and machine learning represents a particularly promising direction, enhancing both the capabilities of biophotonic systems and their accessibility to non-specialist users [3] [69]. The continuing miniaturization of devices and development of point-of-care platforms will expand applications beyond traditional laboratory and clinical settings into wearable monitoring and home-based diagnostics [2] [69].
Future advancements in biophotonics will be shaped by several key trends, including the growing integration of diagnostics and therapeutics, the development of increasingly sophisticated multimodal systems, and the expansion into non-medical applications such as environmental monitoring and food safety [69] [70]. The ongoing convergence of biophotonics with emerging fields such as quantum optics and synthetic biology will likely yield novel capabilities that further enhance the value proposition of light-based technologies. For researchers, scientists, and drug development professionals, understanding both the technical aspects of biophotonics and the strategic frameworks for overcoming commercialization barriers is essential for successfully translating innovative observations from the laboratory into practical diagnostic and therapeutic applications that address unmet medical needs [1]. As the field continues to evolve, its impact on science, medicine, and society is poised to grow significantly, making biophotonics a vital area of research and commercial development throughout the 21st century.
The Role of AI and Machine Learning in Image Analysis and Data Interpretation
The convergence of artificial intelligence (AI) and biophotonics is fundamentally transforming the landscape of biological research and precision medicine. Biophotonics, the interdisciplinary field that uses light to image, detect, and manipulate biological materials, generates vast and complex datasets. AI and machine learning (ML) have become indispensable tools for interpreting this data, enabling the extraction of subtle, clinically relevant information that often eludes conventional analysis. This whitepaper provides an in-depth technical examination of how AI and ML are applied to biophotonic data, covering core computational architectures, representative experimental protocols, and the essential tools that constitute the modern scientist's toolkit. Framed within the broader scope of biophotonics research, this review underscores how these technologies are accelerating drug development, enhancing diagnostic capabilities, and paving the way for new frontiers in personalized healthcare.
Biophotonics sits at the intersection of biology, medicine, and photonics, leveraging the properties of light to probe living systems [1]. Its core technologies are broadly categorized into:
- Bioimaging: Techniques such as optical coherence tomography (OCT), multi-photon microscopy, and hyperspectral imaging allow for the non-invasive characterization of biological specimens across spatial scales, from single molecules to entire organs [1].
- Biosensing: Photonic-based approaches like surface plasmon resonance (SPR) and Raman spectroscopy enable the highly sensitive, often label-free, detection of biomolecules and pathogens [1] [74].
- Light-Based Therapies: Lasers and other light sources are used for precise surgical intervention and photobiomodulation [1] [11].
A key advantage of biophotonic methods is their ability to perform non-contact, non-invasive measurements in real-time, preserving biological integrity and enabling dynamic studies [1]. However, these techniques, particularly modern hyperspectral and nonlinear microscopy methods, generate high-dimensional data at unprecedented rates and volumes. This deluge of complex optical data presents a significant challenge for traditional analysis, creating a critical need for sophisticated, automated interpretation tools. AI and ML have emerged as powerful solutions to this bottleneck, unlocking the full potential of biophotonic data for research and clinical applications [75] [76].
Core AI and ML Technologies in Biophotonics
Neural Networks and Deep Learning Architectures
Deep learning, a subset of ML based on artificial neural networks with multiple layers, has become the cornerstone of modern biophotonic image analysis.
- Convolutional Neural Networks (CNNs) are particularly adept at processing pixel-based data. Their architecture, featuring convolutional and pooling layers, allows them to automatically and hierarchically learn spatial features—from edges and textures in initial layers to complex morphological phenotypes in deeper layers—directly from raw images [76].
- Generative Adversarial Networks (GANs) are used to synthesize realistic biological image data, which can be invaluable for augmenting small training datasets or for simulating experiments. They are also employed in image-to-image translation tasks, such as converting label-free images into virtually stained counterparts [76].
- Transfer Learning involves taking a pre-trained model (often on a large, general image dataset) and fine-tuning it for a specific biophotonic task. This approach significantly reduces the computational resources and labeled data required to develop highly accurate models for specialized applications [76].
Key Analytical Tasks
AI models are deployed to perform several critical analytical tasks:
- Image Segmentation: AI algorithms, particularly U-Net and similar CNN variants, excel at pixel-wise classification to delineate anatomical structures, single cells, or subcellular regions of interest with high precision [76].
- Classification and Detection: ML classifiers, including Support Vector Machines (SVMs) and Random Forests, and deep learning models are used to categorize images into diagnostic classes (e.g., cancerous vs. non-cancerous) or to detect and localize specific abnormalities within an image [76].
- Pattern Recognition and Predictive Modeling: AI can identify complex, multi-scale patterns in spectral or imaging data that correlate with disease progression, treatment response, or genetic mutations. This enables predictive modeling for prognostic applications [76].
Applications in Research and Drug Development
AI-Enhanced Label-Free Phenotyping
A paradigm-shifting application is the use of AI to extract phenotypic information from label-free optical microscopy, bypassing the need for stains or fluorescent tags.
Table 1: Quantitative Outcomes of AI-Powered Label-Free Pancreatic Cancer Phenotyping
| Metric | Performance | Significance |
|---|---|---|
| Phenotype Prediction Accuracy | 89% [77] | Demonstrates high reliability in identifying disease subtypes without molecular stains. |
| Comparison to Classical Image Analysis | Classical methods failed to extract sufficient information [77] | Highlights the necessity of deep learning for this complex task. |
| Core Technology | Label-free microscopy (autofluorescence, SHG) + Deep Neural Network [77] | Provides a faster, more cost-effective alternative to expensive genetic tests. |
Experimental Protocol:
- Tissue Preparation: Human pancreatic cancer tissue specimens are sectioned onto slides without any staining or labeling.
- Spatial Transcriptomics: A baseline ground truth is established using spatial transcriptomics on the tissue, generating a high-resolution map of gene expression patterns and defining distinct disease phenotypes [77].
- Label-Free Imaging: The same tissue specimen is imaged using a multimodal label-free microscope. This typically includes:
- Natural Fluorescence Imaging: Capturing signals from endogenous fluorophores like NAD(P)H and flavins.
- Second Harmonic Generation (SHG) Microscopy: Imaging non-centrosymmetric structures such as collagen [77].
- Data Co-Registration: The label-free images are meticulously aligned with the spatial transcriptomics maps to create a paired dataset where each optical image patch is linked to a known phenotypic profile [77].
- AI Model Training: A deep neural network (e.g., a CNN) is trained on the aligned dataset. The model learns to predict the tissue phenotype based solely on the features present in the label-free microscopy images [77].
- Validation: The trained model's performance is validated on a separate, held-out test set of label-free images to quantify its accuracy.
Diagram 1: AI-powered label-free phenotyping workflow for precise disease classification.
AI-Driven Photonic Biosensors
The integration of AI is also revolutionizing photonic biosensing, leading to the development of intelligent systems like the "photonic nose" for volatile organic compound (VOC) analysis.
Experimental Protocol for an AI-Enhanced Photonic Nose:
- Sensor Design and Fabrication: An array of optical sensors is fabricated on a chip. Each sensor element is functionalized with a different coating (e.g., polymers, metal-organic frameworks) to exhibit partially overlapping selectivity to various VOCs [74].
- Data Acquisition: The sensor array is exposed to a known VOC or complex odor mixture. The optical response (e.g., wavelength shift, intensity change) from each element is recorded, creating a unique "odor fingerprint" [74].
- Dataset Curation: A large library of fingerprints is compiled for many different analytes and concentrations.
- ML Model Integration: Pattern recognition algorithms (e.g., principal component analysis for dimensionality reduction, followed by k-nearest neighbors or support vector machines for classification) are trained on the fingerprint library [74].
- Deployment and Inference: In use, the system captures the fingerprint of an unknown sample, and the trained ML model identifies and/or quantifies its components in real-time, even in complex mixtures. This can be deployed in cloud or edge-computing configurations [74].
Table 2: AI-Driven Photonic Nose Performance in Application Areas
| Application Area | Target Analytes | AI/ML Role |
|---|---|---|
| Medical Diagnostics | Volatile biomarkers for cancer, infectious diseases [74] | Identifies disease-specific VOC patterns from breath or bodily fluids for early detection. |
| Food Safety & Quality | Microbial contaminants, spoilage markers [74] | Classifies food freshness and detects contamination rapidly and non-destructively. |
| Environmental Monitoring | Air pollutants, toxins [74] | Untangles complex mixtures of environmental gases and provides quantitative analysis. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of AI in biophotonics relies on a suite of specialized materials and instruments.
Table 3: Key Research Reagent Solutions for AI-Biophotonics Experiments
| Item / Technology | Function in AI-Biophotonics Workflow |
|---|---|
| Ultrashort Pulse Lasers | High-intensity light source for non-linear microscopy techniques (e.g., multiphoton, SHG, THG), enabling deep-tissue imaging with high spatial resolution [1]. |
| Spatial Transcriptomics Kits | Provide the ground-truth gene expression data required to train AI models for label-free phenotyping studies [77]. |
| Functionalized Sensor Arrays | The core of photonic nose systems; polymer/MOF-coated waveguides or resonators that generate unique optical response patterns to vapors and analytes [74]. |
| Photomultiplier Tubes (PMTs) & Hybrid Detectors | High-sensitivity detectors capable of single-photon detection, crucial for capturing weak signals in fluorescence imaging and Raman spectroscopy [2]. |
| Raman Spectroscopy Systems | Provide detailed molecular fingerprinting data through inelastic light scattering; used in drug screening and material characterization [2]. |
The synergy between AI, machine learning, and biophotonics is creating a powerful new paradigm for scientific discovery and medical innovation. By transforming high-dimensional optical data into actionable biological insights, these technologies are making precision medicine more accessible and effective. The future will likely see a deeper integration of AI across the entire biophotonics pipeline—from guiding the acquisition of data in real-time for optimal information content to providing explainable AI diagnoses that clinicians can trust. As both fields continue to advance, their combined impact on drug development, diagnostics, and our fundamental understanding of biology is poised to grow exponentially.
Biophotonics, the interdisciplinary fusion of light-based technologies with biology and medicine, is rapidly transforming biomedical research and clinical diagnostics [1]. This field leverages the interactions between light and biological matter—including absorption, emission, reflection, and scattering—to enable non-contact measurement, high sensitivity, and real-time analysis of biological systems [1]. Within this domain, nanomaterials and quantum dots (QDs) have emerged as transformative agents that significantly enhance the sensitivity and specificity of biophotonic tools. Quantum dots are luminescent semiconductor nanocrystals with sizes typically ranging from 3 to 10 nm, exhibiting unique size-tunable optical properties due to quantum confinement effects [78] [79]. Their integration into diagnostic and imaging platforms represents a paradigm shift in our ability to detect diseases at their earliest stages and monitor biological processes with unprecedented precision, offering significant advantages over traditional organic dyes through their extraordinary brightness, photostability, and multiplexing capabilities [78] [79].
Fundamental Properties of Nanomaterials and Quantum Dots
Unique Optical Characteristics
The exceptional properties of quantum dots stem from quantum confinement effects that occur when semiconductor crystals become smaller than the Bohr exciton radius of their constituent material [78]. This phenomenon results in discrete energy levels rather than continuous bands, enabling precise tuning of optical properties. Key advantages include:
- Size-Tunable Emission: QDs can be engineered to emit wavelengths across a broad spectrum from 450 to 1600 nm by controlling their size, composition, and shape [78] [79]. For instance, CdSe QDs emit between 450-650 nm, while PbS QDs can reach near-infrared emissions of approximately 1000 nm [79].
- High Quantum Yield: Core-shell structures such as CdSe/ZnS achieve quantum yields between 50-90%, making them significantly brighter than traditional fluorescent markers [79].
- Enhanced Photostability: QDs maintain fluorescence for over 60 minutes under continuous illumination, whereas organic dyes like fluorescein experience photobleaching within seconds to minutes [79].
- Broad Absorption with Narrow Emission: The wide absorption profiles coupled with narrow, symmetric emission spectra enable simultaneous excitation of multiple QD sizes at a single wavelength while maintaining distinct emission signals [78].
Nanocomposite Integration Strategies
The incorporation of QDs into nanocomposite matrices enhances their functionality and application potential. Common integration approaches include:
- Core-Shell Architectures: Structures such as CdTe/ZnS or CdSe/CdS/ZnS improve quantum yield and reduce cytotoxicity by confining the core semiconductor material [78] [79].
- Surface Functionalization: Bioconjugation with antibodies, aptamers, peptides, or other targeting molecules enables specific binding to biomarkers of interest [78] [79]. For example, folic acid conjugation allows targeted delivery to tumor cells overexpressing folate receptors [78].
- Polymeric Encapsulation: Embedding QDs in Pluronic triblock-copolymer micelles or similar structures improves dispersibility and biocompatibility while maintaining optical properties [78].
Table 1: Comparison of Optical Properties Between Quantum Dots and Traditional Fluorophores
| Property | Quantum Dots | Traditional Organic Dyes |
|---|---|---|
| Extinction Coefficient | High (0.5-5 × 10^6 M^-1cm^-1) | Moderate (~50,000 M^-1cm^-1) |
| Quantum Yield | 50-90% (core-shell) | Typically <50% |
| Photostability | High (minutes to hours) | Low (seconds to minutes) |
| Emission Bandwidth | Narrow (20-40 nm FWHM) | Broad (50-100 nm FWHM) |
| Multiplexing Capacity | Excellent (single excitation) | Limited (multiple excitations) |
| Sensitivity Limit | Femtomolar (10^-15 M) [79] | Picomolar (10^-12 M) |
Quantitative Performance Enhancements
Sensitivity Metrics and Detection Limits
Quantum dot-infused nanocomposites (QDNCs) have demonstrated remarkable improvements in detection sensitivity, achieving femtomolar (10^-15 M) detection limits for various biomarkers [79]. This represents up to a 1000-fold enhancement compared to conventional detection methods. The high surface-to-volume ratio of nanomaterials facilitates enhanced signal amplification, while their tunable optical properties minimize background interference through precise spectral separation.
Table 2: Experimental Detection Limits Achieved with Quantum Dot-Based Platforms
| Analyte Category | Specific Target | Detection Limit | Platform Design |
|---|---|---|---|
| Cancer Biomarkers | PSA, CEA | 0.1-10 fM | QD-antibody conjugates in microarray format |
| Infectious Disease | Viral RNA/DNA | 10-100 fM | QD-oligonucleotide probes with FRET |
| Neurological Disorders | Amyloid-β peptides | 1-50 fM | QD-immunosensors with signal amplification |
| Metal Ions | Ni(II) | ~nM (10^-9 M) [80] | Functionalized QDs with specific ligands |
Specificity Enhancement Mechanisms
The specificity of QD-based detection systems is achieved through multiple engineering strategies:
- Molecular Recognition Elements: Surface functionalization with antibodies, aptamers, or peptides provides high-affinity binding to specific biomarkers [78] [79].
- Multiplexed Detection: The narrow emission spectra of QDs enable simultaneous detection of multiple targets without spectral overlap, significantly improving diagnostic accuracy [79].
- Signal-to-Noise Optimization: The minimal bleed-through between channels and reduced autofluorescence background in tissue imaging enhance the specificity of detection in complex biological environments [79].
Experimental Protocols and Methodologies
Protocol: Quantum Dot-Based Immunoassay for Protein Detection
This protocol details the procedure for detecting low-abundance proteins using QD-antibody conjugates, achieving femtomolar sensitivity [79].
Materials Required:
- Core-shell QDs (e.g., CdSe/ZnS) with appropriate emission wavelength
- Purified detection antibodies specific to target protein
- Streptavidin-coated microplates or functionalized surfaces
- Blocking buffer (1% BSA in PBS)
- Sample containing target analyte
- Biotinylated capture antibodies
- Washing buffer (PBS with 0.05% Tween-20)
- Spectrofluorometer or microarray scanner
Procedure:
- Surface Preparation: Coat microplate wells with biotinylated capture antibodies (1-10 μg/mL in carbonate buffer) and incubate overnight at 4°C.
- Blocking: Aspirate unbound antibodies and add 200 μL blocking buffer per well. Incubate for 2 hours at room temperature.
- Sample Incubation: Add 100 μL of sample or standard solution to each well. Incubate for 2 hours at 37°C with gentle shaking.
- Washing: Wash wells three times with washing buffer to remove unbound proteins.
- QD Conjugate Preparation: Mix QD-streptavidin conjugates with biotinylated detection antibodies at optimal ratio (typically 1:1 to 1:4). Incubate for 30 minutes at room temperature.
- Detection: Add 100 μL of QD-detection antibody conjugates to each well. Incubate for 1 hour at 37°C in the dark.
- Final Wash: Wash wells five times with washing buffer to remove unbound QD conjugates.
- Signal Measurement: Measure fluorescence intensity using a spectrofluorometer with excitation at 400 nm and emission at the QD-specific wavelength.
- Data Analysis: Generate standard curve using known concentrations of target protein and interpolate sample concentrations.
Critical Parameters:
- Optimize antibody:QD ratio to maximize signal while minimizing non-specific binding
- Include controls for autofluorescence and non-specific binding
- Maintain consistent washing stringency across all samples
- Protect QDs from light during all steps to prevent photodegradation
Protocol: Multiplexed Pathogen Detection Using Spectral Coding
This methodology enables simultaneous detection of multiple pathogens in a single assay through QD spectral coding [79].
Materials Required:
- Three distinct QD populations with emissions at 525, 585, and 655 nm
- Pathogen-specific antibodies or oligonucleotide probes
- Carbodiimide chemistry reagents for conjugation
- Microfluidic device or multiplex assay platform
- PBS buffer (pH 7.4)
- Spectrofluorometer with spectral unmixing capability
Procedure:
- QD Functionalization: Activate carboxylated QDs using EDC/sulfo-NHS chemistry according to manufacturer's protocol.
- Probe Conjugation: Add specific detection probes (antibodies or oligonucleotides) to activated QDs at optimized ratios. Incubate for 2 hours at room temperature.
- Purification: Remove unbound probes using size-exclusion chromatography or ultrafiltration.
- Assay Assembly: Immobilize capture probes specific to each target pathogen in designated regions of the detection platform.
- Sample Application: Introduce test sample to the platform and incubate for 1-2 hours to allow target binding.
- QD Probe Addition: Apply the mixture of QD-detection probes and incubate for 1 hour.
- Washing: Remove unbound QD probes through stringent washing.
- Spectral Imaging: Acquire fluorescence signals at multiple emission wavelengths using appropriate filter sets.
- Spectral Unmixing: Deconvolute overlapping signals using reference spectra from pure QD populations.
- Quantification: Calculate pathogen concentrations based on intensity values at each detection zone.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Quantum Dot-Based Research
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Core-Shell QDs (CdSe/ZnS, CdTe/ZnS, InP/ZnS) | Fluorescent probes with high quantum yield and stability | Cellular imaging, biosensing, multiplexed detection [78] [79] |
| Bifunctional Ligands (Mercaptounderanoic acid, PEG-phospholipids) | Surface modification for water solubility and biocompatibility | In vivo applications, reduction of cytotoxicity [78] |
| Streptavidin-QD Conjugates | Universal detection platform for biotinylated molecules | Immunoassays, nucleic acid detection, protein profiling [79] |
| QD-Labeled Antibodies | Target-specific recognition elements | Immunohistochemistry, flow cytometry, in situ hybridization [78] [79] |
| QD-Oligonucleotide Conjugates | Sequence-specific nucleic acid detection | Fluorescence in situ hybridization (FISH), gene expression analysis, pathogen detection [79] |
| Polymeric Matrices (PLGA, PEG, silica shells) | Encapsulation for enhanced stability and controlled release | Drug delivery, theranostics, in vivo imaging [78] [79] |
| Magnetic Nanocomposites (QD-Fe₃O₄ hybrids) | Combined fluorescence and magnetic properties | Cell separation, multimodal imaging, targeted delivery [79] |
Advanced Applications in Biophotonics
Diagnostic Applications
The enhanced sensitivity and specificity of QD-based platforms have enabled breakthroughs in multiple diagnostic areas:
- Cancer Diagnostics: QD-immunoassays detect circulating tumor cells and cancer biomarkers at clinically relevant concentrations, enabling early detection and monitoring of treatment response [78] [79]. For example, QD-labeled HER2 antibodies enable precise quantification of receptor expression levels in breast cancer specimens.
- Infectious Disease Detection: Multiplexed QD assays simultaneously identify multiple pathogens from minimal sample volumes, significantly reducing diagnostic turnaround time [79].
- Neurological Disorders: QD-based sensors detect amyloid-β oligomers and tau proteins associated with Alzheimer's disease at femtomolar concentrations, facilitating early intervention [79].
Imaging and Biosensing
- In Vivo Imaging: Near-infrared QDs (e.g., PbS) enable deep-tissue imaging with high spatial resolution, allowing real-time tracking of cellular processes and drug distribution [78].
- Biosensing Platforms: QD-integrated biosensors utilizing FRET mechanisms detect molecular interactions in real-time, providing insights into dynamic cellular processes [78] [79].
- Single-Molecule Tracking: The photostability of QDs enables prolonged tracking of individual molecules in living cells, revealing dynamics of cellular processes that are obscured by traditional dyes [78].
Future Perspectives and Challenges
Despite the significant advancements, several challenges remain in the widespread clinical adoption of QD-based technologies. Toxicity concerns associated with heavy metal components in conventional QDs have prompted research into alternative materials such as carbon dots, graphene QDs, and silicon QDs [80] [79]. Scalability and manufacturing consistency present additional hurdles for commercial translation. The integration of machine learning and artificial intelligence with QD-based detection systems shows promise for intelligent diagnostic platforms capable of real-time analysis and personalized medicine [79]. As these challenges are addressed, quantum dot-infused nanocomposites are poised to establish new standards for precision diagnostics, ultimately revolutionizing global healthcare through enhanced sensitivity and specificity in biophotonic applications.
Standardization and Biocompatibility in Device Design and Fabrication
The integration of biophotonic technologies—which utilize light to image, diagnose, and treat disease—into medical devices represents a frontier in modern medicine [1]. The safe and effective translation of these innovations from the laboratory to the clinic is critically dependent on a rigorous framework of standardization and biocompatibility. This whitepaper provides an in-depth examination of the core principles, regulatory requirements, and testing protocols that govern the design and fabrication of biophotonic medical devices. Framed within the broader scope of biophotonics research, this guide details the essential "Big Three" biocompatibility tests, explores the relevant international standards, and outlines a practical workflow for compliance. By synthesizing current regulatory landscapes with detailed methodological data, this document serves as a strategic resource for researchers, scientists, and drug development professionals navigating the path from innovation to clinical application.
Biophotonics, the interdisciplinary field at the convergence of photonics, biology, and medicine, is revolutionizing healthcare and life sciences. It leverages the properties of light to analyze and manipulate biological materials across multiple scales, from single molecules to entire organs [1]. Core biophotonic technologies include bioimaging (e.g., Optical Coherence Tomography (OCT), multiphoton microscopy), biosensing (e.g., surface plasmon resonance, Raman spectroscopy), and photonic-based therapies [1]. The global biophotonics market, valued at approximately $62.6 billion in 2024, is projected to grow at a compound annual growth rate (CAGR) of about 10.6%, reaching over $113 billion by 2030, underscoring its significant commercial and clinical impact [81] [72].
The defining advantages of biophotonic methods—non-contact measurement, high sensitivity, and superior time resolution—make them ideal for non-invasive diagnostics and real-time monitoring [1]. However, the integration of optical components, novel materials, and light sources into devices that interact with the human body introduces complex safety considerations. A device's biological safety, or biocompatibility, is not an intrinsic property but must be evaluated based on its intended use and the nature and duration of patient contact [82]. Standardization provides the essential framework for this evaluation, ensuring that devices are safe, perform consistently, and can gain regulatory approval across different regions. For a field as dynamic and rapidly evolving as biophotonics, adhering to these standardized pathways is not a constraint but a critical enabler of reliable and timely clinical translation.
The Regulatory and Standards Landscape
Navigating the global regulatory environment is a fundamental step in the medical device development process. Compliance with stringent international standards is mandatory for market approval and ensures patient safety.
Table 1: Key Global Regulatory Frameworks for Medical Device Biocompatibility
| Region | Regulatory Body | Primary Regulation/Standard | Key Focus |
|---|---|---|---|
| International | International Organization for Standardization (ISO) | ISO 10993 Series | Globally harmonized standards for biological evaluation of medical devices [83]. |
| United States | Food and Drug Administration (FDA) | FDA Guidance Documents (aligned with ISO 10993) | Requirements for pre-market submissions and device approval [83]. |
| European Union | European Commission | Medical Device Regulation (MDR) (EU 2017/745) | Mandatory compliance for CE marking, references ISO 10993 [83]. |
| Japan | Pharmaceuticals and Medical Devices Agency (PMDA) | PMDA Regulations (aligned with international standards) | Approval requirements for the Japanese market [83]. |
| Canada | Health Canada | Medical Devices Regulations (MDR) | Submission of biocompatibility data for device approval [83]. |
The ISO 10993 series, titled "Biological evaluation of medical devices," is the cornerstone of biocompatibility assessment [82] [83]. This series provides a framework for evaluating the potential risks a device may pose, such as cytotoxicity, irritation, and sensitization. The current standard, ISO 10993-1:2018, emphasizes a risk-based approach, moving away from a prescriptive list of tests towards a more comprehensive process of risk assessment, mitigation, and management tailored to the device's specific characteristics and intended use [82]. This requires manufacturers to develop a deep understanding of how their device design, material selection, and manufacturing processes influence biological safety.
Core Biocompatibility Testing: The "Big Three" and Methodological Detail
For nearly all medical devices, regardless of category, the initial and most critical biocompatibility assessments are the "Big Three" tests: cytotoxicity, irritation, and sensitization [83]. These tests are typically performed using device extracts, which are prepared by immersing the device or its components in extraction solvents like physiological saline or cell culture medium under specified conditions, as detailed in ISO 10993-12 [83].
Cytotoxicity Testing (ISO 10993-5)
This test evaluates the potential of a device or its extracts to cause cell death or damage.
- Objective: To assess whether the device's materials release substances that are harmful to living cells [83].
- Experimental Protocol:
- Sample Preparation: Extracts of the test device are prepared using appropriate cell culture media.
- Cell Culture: Mammalian cell lines (e.g., L929 mouse fibroblasts) are cultured and allowed to form a monolayer.
- Exposure: The device extracts are applied to the cell cultures for a defined period, typically 24 hours.
- Endpoint Assessment: Cell viability and morphological changes are evaluated. Common quantitative methods include:
- Acceptance Criteria: While ISO 10993-5 does not define strict pass/fail criteria, a cell viability of ≥70% is generally considered a positive indicator of non-cytotoxicity [83].
Sensitization Testing (ISO 10993-10)
This test assesses the potential for a device to cause an allergic reaction.
- Objective: To determine if chemicals leaching from the device can induce a hypersensitive immune response upon repeated or prolonged exposure [83].
- Experimental Protocol (Murine Local Lymph Node Assay - LLNA):
- In Vivo Model: Mice are used as the test system.
- Dosing: The test material extract is applied topically to the ears of the mice daily for three consecutive days.
- Measurement: The proliferation of lymphocytes in the draining lymph nodes is measured, typically by quantifying the incorporation of radioactive tritiated thymidine or using alternative non-radioactive markers.
- Interpretation: A significant increase in lymphocyte proliferation in the test group compared to the vehicle control group indicates a sensitizing potential.
Irritation Testing (ISO 10993-10)
This test evaluates the potential for a device to cause localized, non-specific inflammatory response at the site of contact.
- Objective: To determine if a single exposure to a device extract can cause reversible inflammatory damage to skin, eyes, or other tissues [83].
- Experimental Protocol (In Vitro Reconstructed Human Epidermis - RhE Model):
- Test System: Uses 3D, human-derived epidermal models.
- Exposure: The device extract is applied topically to the surface of the RhE model.
- Endpoint Assessment: Cell viability is measured after exposure using an MTT assay. A reduction in viability below a predetermined threshold (e.g., <50%) compared to negative controls indicates a potential for skin irritation.
Table 2: Summary of the "Big Three" Biocompatibility Tests
| Test Type | Standard | Key Objective | Common Methods | Critical Endpoints |
|---|---|---|---|---|
| Cytotoxicity | ISO 10993-5 | Assess cell damage/death | In vitro (e.g., MTT assay with L929 cells) | Cell viability, morphological changes [83] |
| Sensitization | ISO 10993-10 | Identify allergic response potential | In vivo (LLNA in mice) | Lymphocyte proliferation in lymph nodes [83] |
| Irritation | ISO 10993-10 | Evaluate localized inflammation | In vitro (Reconstructed Human Epidermis model) | Cell viability post-exposure [83] |
The following workflow diagram illustrates the strategic path for navigating the biocompatibility evaluation process, from initial planning to regulatory submission.
The Scientist's Toolkit: Key Reagents and Materials for Biocompatibility Testing
Successfully executing biocompatibility tests requires a suite of specialized reagents and materials. The following table details essential components for the core methodologies.
Table 3: Research Reagent Solutions for Core Biocompatibility Testing
| Reagent/Material | Function | Application Example |
|---|---|---|
| L929 Mouse Fibroblasts | A standardized mammalian cell line used for in vitro cytotoxicity testing. | Cultured as a monolayer and exposed to device extracts to assess effects on cell viability and morphology [83]. |
| MTT/XTT Reagents | Tetrazolium salts that are reduced by metabolically active cells to a colored formazan product. | Added to cell cultures after extract exposure; the absorbance of the dissolved formazan is measured to quantify cell viability [83]. |
| Physiological Saline | An isotonic extraction vehicle that simulates aqueous body fluids. | Used to prepare polar extracts of a device to test for leachable substances in an aqueous medium [83]. |
| Vegetable Oil | A lipophilic extraction vehicle that simulates oily body fluids. | Used to prepare non-polar extracts of a device to test for fat-soluble leachable substances [83]. |
| Reconstructed Human Epidermis (RhE) | A 3D, human-derived tissue model representing the outermost layers of human skin. | Used in place of animal testing for skin irritation assays; extracts are applied topically to assess tissue damage [83]. |
| Culture Medium (e.g., DMEM) | A nutrient-rich solution that supports the growth and maintenance of mammalian cells in vitro. | Used as both a growth medium for cell lines and as a solvent for preparing device extracts [83]. |
Within the expansive and innovative field of biophotonics, the path from a groundbreaking concept to a clinically deployed device is paved with rigorous scientific and regulatory principles. Standardization and biocompatibility are not peripheral concerns but are central to the responsible development of safe and effective biophotonic technologies. As the field continues to advance—driven by trends in miniaturization, the integration of artificial intelligence, and expansion into non-medical applications—the foundational framework provided by standards like the ISO 10993 series will remain critical [1] [69]. By embracing a proactive, risk-based approach to biocompatibility from the earliest stages of device design and fabrication, researchers and developers can mitigate risks, streamline the regulatory pathway, and ultimately fulfill the promise of biophotonics to transform healthcare and improve patient outcomes.
Biophotonics, the interdisciplinary fusion of light-based technologies with biology and medicine, is rapidly transforming research, diagnostics, and therapy [1]. This field leverages the properties of light to analyze and manipulate biological materials at the molecular, cellular, and tissue levels, offering the key advantages of non-contact measurement, high sensitivity, and real-time information [1]. At the heart of this transformation are portable and wearable biosensors—devices that represent a practical and powerful application of biophotonic principles. These tools are moving diagnostics and continuous monitoring out of specialized laboratories and into clinics, homes, and daily life. Framed within the broader scope of biophotonics research, these sensors utilize optical phenomena such as fluorescence, surface plasmon resonance (SPR), and Raman spectroscopy to achieve highly sensitive, often label-free detection of biological and chemical analytes [2]. This whitepaper provides an in-depth technical guide to the core technologies, experimental methodologies, and research tools that underpin this rapidly advancing field, offering scientists and drug development professionals a roadmap for leveraging these technologies in their work.
Technical Foundations: Core Biophotonic Principles in Biosensor Design
The operation of wearable biosensors is predicated on several key biophotonic principles that enable the detection of physiological changes and specific biomarkers.
Light-Tissue Interaction and Sensing Modalities
The fundamental mechanism involves the interaction of light with biological tissues. When near-infrared (NIR) light is used, it can penetrate biological tissue deeply because the primary tissue chromophores—oxygenated hemoglobin (HbO), deoxygenated hemoglobin (HbR), water, and lipid—have negligible absorption in the NIR "window" of 650-900 nm [84]. Biophotonic biosensors exploit various optical phenomena for detection [2]:
- Fluorescence: Measures the emission light from a fluorophore after excitation by a specific wavelength.
- Surface Plasmon Resonance (SPR): Detects changes in the refractive index on a sensor surface, often resulting from biomolecular binding events.
- Raman Spectroscopy: Uses inelastically scattered light to provide a molecular fingerprint of the analyte, often enhanced by nanophotonic structures.
From Diffuse Optics to Miniaturized Sensors
The foundational work in diffuse optical imaging demonstrated how light could be used to probe deep tissues. This technique uses a spatially distributed array of NIR light sources and detectors placed on the surface of the tissue. As photons scatter through the tissue, changes in the detected light intensity can be correlated with alterations in chromophore concentrations, providing information on physiological parameters like blood volume and oxygenation [84]. Modern wearable biosensors represent a miniaturization and specialization of these principles, often focusing on a single parameter or a small set of analytes for continuous monitoring.
Table 1: Core Biophotonic Sensing Modalities in Wearable Biosensors
| Sensing Modality | Physical Principle | Primary Applications in Wearables | Key Advantage |
|---|---|---|---|
| Fluorescence | Emission of light from excited fluorophores | Glucose monitoring, metabolite sensing, oxygen saturation | High sensitivity and specificity |
| Raman Spectroscopy | Inelastic scattering of light by molecules | Continuous glucose monitoring, biomarker detection | Provides molecular fingerprint; label-free |
| Near-Infrared (NIR) Spectroscopy | Absorption and scattering of NIR light by tissue chromophores | Hemodynamic monitoring (HbO, HbR), tissue oxygenation | Enables deep-tissue probing |
| Surface Plasmon Resonance (SPR) | Resonance oscillation of electrons at a metal-dielectric interface | Label-free detection of proteins, antibodies, and biomarkers | Real-time, kinetic binding data |
Market and Application Landscape
The integration of biophotonics into portable and wearable form factors is driving significant market growth and expanding application possibilities.
Market Trajectory and Growth Segments
The global market for biosensors in medical wearables is experiencing robust growth, projected to reach approximately $15 billion in 2025, with a compound annual growth rate (CAGR) of 5% from 2025 to 2033 [85]. This growth is fueled by the rising prevalence of chronic diseases, demand for continuous health monitoring, and advancements in sensor technology. The broader biophotonics market, valued at $62.6 billion in 2024, is expected to grow at a CAGR of 10.6% from 2025 to 2030, reaching $113.1 billion, underscoring the significant role of optical technologies in healthcare [86].
Key concentration areas for wearable biosensors include [85]:
- Glucose Monitoring: Accounts for over 40% of the market, driven by the global diabetic population.
- Cardiac Rhythm Monitoring: Holds approximately 30% of the market, focusing on heart rate, rhythm, and ECG data.
- Respiratory Monitoring: Constitutes around 15%, including monitoring of breathing patterns and oxygen saturation.
Dominant Applications in Research and Clinics
The applications of these sensors are vast and transformative. In drug development, they enable real-time, in-vivo monitoring of therapeutic response and pharmacokinetics in preclinical models, providing more nuanced data than terminal time points. For clinical researchers, they facilitate continuous, unobtrusive monitoring of patient physiology in real-world settings, generating rich datasets for understanding disease progression and treatment efficacy. In the realm of personalized medicine, wearable biosensors empower the collection of individualized baselines and dynamic responses, forming the foundation for tailored therapeutic interventions [2] [85].
Table 2: Global Market Outlook for Biophotonics and Wearable Biosensors
| Market Segment | Base Year Value (2024/2025) | Projected Value (2030/2034) | CAGR | Primary Growth Driver |
|---|---|---|---|---|
| Overall Biophotonics Market [86] [69] | $62.6 Billion (2024) | $113.1 Billion (2030) | 10.6% | Non-invasive diagnostics & chronic disease prevalence |
| Biophotonics Market (Alternate Forecast) [69] | $92.09 Billion (2025) | $226.18 Billion (2034) | 10.5% | Aging population & preventive healthcare |
| Biosensors for Medical Wearables [85] | ~$15 Billion (2025) | ~$30 Billion (2030 Est.) | 5% (2025-33) | Telehealth adoption & sensor miniaturization |
| In-Vitro Biophotonics Segment [86] | 72% of market (2024) | Dominant through 2030 | - | Demand for early disease detection & personalized medicine |
Experimental Protocols and Methodologies
This section details core experimental workflows for developing and validating wearable biophotonic biosensors, providing a reproducible guide for researchers.
Protocol: Development of a Fluorescence-Based Wearable Sensor for Metabolite Monitoring
Objective: To create a patch-based wearable sensor for continuous monitoring of a target metabolite (e.g., lactate or glucose) in interstitial fluid using fluorescence resonance energy transfer (FRET).
Materials & Reagents:
- Recognition Element: Recombinant metabolite-binding protein (e.g., glucose/galactose-binding protein).
- Fluorophores: Donor (e.g., Cy3) and acceptor (e.g., Cy5) dyes for FRET pair labeling.
- Substrate: Flexible, gas-permeable polymer (e.g., polydimethylsiloxane, PDMS).
- Optical Components: Miniature LED (wavelength matched to donor excitation) and photodetector (for acceptor emission).
- Data Acquisition: Microcontroller unit (MCU) with Bluetooth Low Energy (BLE) module.
Procedure:
- Biosensor Fabrication:
- Genetically engineer the binding protein to introduce cysteine residues at sites where conformational change occurs upon metabolite binding.
- Conjugate the donor and acceptor fluorophores to the specific cysteine residues.
- Immobilize the labeled protein within a hydrogel matrix and micropattern it onto the flexible PDMS substrate.
- Integrate the micropatterned sensing layer with the miniature LED and photodetector, and connect to the MCU.
Calibration and In-Vitro Validation:
- Expose the sensor to a series of standard solutions with known metabolite concentrations (0-30 mM) in a buffered solution (pH 7.4) at 37°C.
- Record the fluorescence intensity ratio (Acceptor Emission / Donor Emission) at each concentration.
- Generate a standard calibration curve (Ratio vs. Concentration) and fit with a logistic function.
- Assess sensor performance by calculating the limit of detection (LOD), dynamic range, and selectivity against common interferents (e.g., ascorbate, urate).
In-Vivo Testing and Data Analysis:
- Secure the sensor patch on the skin (e.g., forearm) of human subjects following institutional ethics approval.
- Initiate continuous data logging via the BLE link to a host computer.
- Have subjects undergo a controlled protocol (e.g., oral glucose tolerance test or graded exercise) to modulate metabolite levels.
- Correlate sensor readings with gold-standard measurements (e.g., blood draws analyzed with a clinical chemistry analyzer) at regular intervals to validate accuracy.
Experimental Workflow for Wearable Biosensor Development
Protocol: Validating a Wearable NIRS Device for Muscle Oxygenation
Objective: To validate the accuracy of a wearable Near-Infrared Spectroscopy (NIRS) device for monitoring muscle oxygenation (SmO₂) during exercise.
Materials & Reagents:
- Primary Device: Commercial or prototype wearable NIRS sensor.
- Reference Standard: MRI system for phosphorus magnetic resonance spectroscopy (³¹P-MRS) or a validated blood gas analyzer for invasive O₂ saturation measurement.
- Calibration Phantom: Tissue-simulating phantom with known absorption (μa) and scattering (μs) coefficients.
Procedure:
- System Characterization:
- Place the NIRS device on the calibration phantom.
- Measure the intensity of light received at the detector and use a inverse algorithm to recover the phantom's known optical properties, ensuring system accuracy.
Subject Instrumentation:
- Secure the NIRS device on the muscle of interest (e.g., vastus lateralis).
- For concurrent validation, position the subject within the MRI scanner with the NIRS device in place, or prepare for serial blood draws from the femoral vein/artery.
Protocol Execution:
- Record a 5-minute baseline at rest.
- Initiate a graded exercise protocol (e.g., on a cycle ergometer or MRI-compatible ergometer).
- Simultaneously record NIRS-derived SmO₂ and ³¹P-MRS (for phosphocreatine breakdown as a metabolic correlate) or take blood samples at defined stages of exercise.
- Continue monitoring throughout a 10-minute recovery period.
Data Analysis:
- Time-synchronize NIRS and reference data.
- Perform linear regression and Bland-Altman analysis to assess the agreement between the NIRS device and the reference standard.
- Calculate the root mean square error (RMSE) and Pearson's correlation coefficient (r) to quantify the device's performance.
The Scientist's Toolkit: Research Reagent Solutions
Successful development of biophotonic biosensors relies on a suite of specialized materials and reagents. The table below details key components and their functions.
Table 3: Essential Research Reagents and Materials for Biophotonic Biosensor Development
| Item Category | Specific Examples | Function in Research & Development |
|---|---|---|
| Recognition Elements | Genetically encoded biosensor proteins (e.g., GCaMP for calcium), Affibodies, Molecularly Imprinted Polymers (MIPs) | Provides high specificity for the target analyte; transduces binding event into a measurable optical signal. |
| Fluorophores & Labels | Quantum Dots (QDs), Near-Infrared (NIR) dyes (e.g., Cy7, IRDye800CW), Lanthanide probes | Acts as the signal generator; chosen for brightness, stability, and spectral properties to maximize penetration depth and minimize background. |
| Nanophotonic Materials | Gold nanoparticles (for SPR/LSPR), Photonic crystals, Upconverting nanoparticles | Enhances the local electromagnetic field, dramatically improving sensitivity and enabling label-free detection. |
| Biocompatible Polymers | Polydimethylsiloxane (PDMS), Polyethylene glycol (PEG) hydrogels, Ecoflex | Serves as the substrate or encapsulation matrix; ensures sensor comfort, flexibility, and stable performance on the skin. |
| Opto-electronic Components | Miniature LEDs/ Lasers, Silicon Photomultipliers (SiPMs), Avalanche Photodiodes (APDs), Micro-spectrometers | Constitutes the core hardware for generating light and detecting the resulting optical signal with high sensitivity. |
Visualization of Core Sensing Mechanisms
The following diagram illustrates the fundamental working principles of two dominant biophotonic sensing modalities employed in wearable devices.
Biophotonic Sensing Mechanisms in Wearables
Future Outlook and Strategic Research Directions
The trajectory of portable and wearable biosensors is set toward greater integration, intelligence, and fundamental material advances.
Deep Integration with AI and Data Analytics: The future lies not only in sensing but in interpreting complex data. Artificial intelligence (AI) and machine learning (ML) are being integrated to analyze massive datasets from biosensors, detect hidden patterns, provide real-time diagnostics, and even predict health events [2] [69]. This will transform raw photonic data into clinically actionable insights.
Material Science and Novel Form Factors: Research is focused on biocompatible materials, flexible and stretchable electronics, and the integration of sensors into smart fabrics [85]. This will lead to sensors that are minimally perceptible, capable of long-term implantation, and that measure a wider range of analytes directly from the skin or within the body.
The Push for Implantability and Multi-Modality: The frontier of research involves moving from wearables to implantables. These miniaturized devices aim for long-term, continuous monitoring from within the body [85]. Furthermore, the combination of multiple sensing modalities (optical, electrochemical, physical) within a single device will provide a more holistic view of an individual's physiological status, crucial for managing complex chronic diseases and advancing personalized medicine. This evolution, firmly rooted in the principles of biophotonics, will continue to dissolve the boundaries between the clinic and daily life, fundamentally reshaping biomedical research and healthcare delivery.
Validation and Impact: Clinical Translation, Market Analysis, and Future Projections
Biophotonics, the interdisciplinary fusion of light-based technologies with biology and medicine, is fundamentally transforming clinical research and practice [1]. This field leverages the interactions between light and biological matter to enable non-contact, highly sensitive, and real-time analysis of living systems, providing profound insights into disease mechanisms [1]. The core technological pillars of biophotonics—bioimaging, biosensing, and photonic-based therapies—are driving significant advancements across medical specialties by offering non-invasive diagnostics and precise therapeutic interventions [1]. The global biophotonics market, valued at $62.6 billion in 2024, reflects this transformative potential, with projections estimating growth to $113.1 billion by 2030 at a compound annual growth rate of 10.6% [87].
Clinical validation of biophotonic technologies represents a critical bridge between laboratory innovation and patient care, ensuring that these advanced optical techniques meet rigorous standards for safety, efficacy, and reliability in real-world medical settings. The expanding applications of biophotonics are particularly evident in oncology, ophthalmology, and neurology, where the ability to visualize and manipulate biological processes at the molecular and cellular levels is revolutionizing diagnostic paradigms and treatment approaches [1]. This whitepaper examines the clinical validation journey of biophotonic technologies through case studies in these three specialties, highlighting the experimental methodologies, validation metrics, and clinical evidence supporting their integration into modern healthcare.
Clinical Validation in Oncology
Oncology has emerged as a primary beneficiary of biophotonic innovations, particularly for early cancer detection and precise tumor demarcation. The clinical rationale stems from the pressing need to improve early diagnosis and treatment precision for malignancies like gastric cancer, which ranks as the fifth most common malignancy globally and represents a leading cause of cancer-related deaths [88]. Traditional endoscopic techniques and proteomic analytical methods present limitations in sensitivity and specificity that biophotonic technologies effectively address through enhanced imaging capabilities and molecular-level analysis [88].
Validated biophotonic platforms in oncology include narrow-band imaging (NBI), confocal laser endomicroscopy (CLE), Raman spectroscopy, optical coherence tomography (OCT), and fluorescence-guided surgery systems [88]. These technologies leverage distinct light-tissue interaction principles to provide complementary diagnostic information, enabling comprehensive tumor characterization from macroscopic morphology to molecular composition. The validation pathway for these technologies requires demonstrating superior performance against histopathological standards while establishing clear clinical utility in improving patient outcomes.
Case Study: Multi-Modal Biophotonics for Gastric Cancer Detection
Experimental Protocol and Methodology
A comprehensive clinical validation study evaluated multiple biophotonic technologies for early gastric cancer detection using a standardized protocol with consecutive patient enrollment [88]. The study implemented a multi-modal approach to compare the diagnostic performance of different optical techniques against the gold standard of histopathological examination.
Table 1: Biophotonic Technologies for Gastric Cancer Detection
| Technology | Principle | Sensitivity Range | Specificity Range | Key Advantages |
|---|---|---|---|---|
| Narrow Band Imaging (NBI) | Enhanced visualization of mucosal and vascular patterns | 85-92% | 80-89% | Real-time capability, easy integration with endoscopy |
| Confocal Laser Endomicroscopy (CLE) | In vivo microscopy at 1000x magnification | 90-95% | 88-94% | Cellular-level resolution, virtual histology |
| Raman Spectroscopy | Molecular fingerprinting via inelastic scattering | 87-93% | 85-91% | High molecular specificity, label-free |
| Optical Coherence Tomography (OCT) | Cross-sectional imaging using interferometry | 82-90% | 83-87% | Depth resolution (1-2 mm), architectural analysis |
| Diffuse Reflectance Spectroscopy | Analysis of tissue absorption and scattering | 80-86% | 78-85% | Quantitative tissue characterization |
The experimental workflow followed a structured approach: (1) patient preparation and standard white-light endoscopic examination; (2) targeted imaging of suspicious lesions and contralateral normal mucosa with each biophotonic modality; (3) optical biopsy acquisition from imaged areas; (4) blinded histopathological evaluation by gastrointestinal pathologists; and (5) statistical analysis comparing optical findings with histological diagnosis. The study enrolled 280 patients with suspected gastric lesions, generating 1,540 paired optical-histological datasets for analysis [88].
Figure 1: Experimental workflow for multi-modal validation of biophotonic technologies in gastric cancer detection
Key Research Reagents and Materials
Table 2: Essential Research Reagents for Oncology Biophotonics
| Reagent/Material | Function | Application in Validation Study |
|---|---|---|
| Fluorescein Sodium | Contrast agent for CLE | Intravenous administration (2.5-5.0 mL of 10% solution) for cellular and vascular enhancement |
| Methylene Blue | Topical contrast agent | 0.1-0.5% topical application for surface enhancement in NBI |
| Gold Nanoparticles | Surface-enhanced Raman scattering (SERS) substrate | Signal amplification for biomarker detection in Raman spectroscopy |
| Tissue-mimicking Phantoms | System calibration and standardization | Daily validation of imaging system performance pre-procedure |
| Reference Standards | Spectral calibration | Wavelength and intensity calibration for spectroscopic systems |
Validation Metrics and Clinical Outcomes
The clinical validation established rigorous performance metrics for each biophotonic technology. Confocal laser endomicroscopy demonstrated the highest diagnostic accuracy (94.7%) for early gastric cancer detection, with sensitivity and specificity of 95.2% and 94.1%, respectively [88]. Raman spectroscopy showed exceptional capability in identifying molecular changes associated with dysplasia and early malignancy, with characteristic spectral shifts at 855 cm⁻¹, 1003 cm⁻¹, 1155 cm⁻¹, and 1515 cm⁻¹ corresponding to protein and lipid alterations [88].
The integration of artificial intelligence with biophotonic data analysis emerged as a critical validation component, with machine learning algorithms improving diagnostic accuracy by 12-18% across all modalities compared to human interpretation alone [88]. This human-AI collaborative approach achieved negative predictive values exceeding 98%, potentially reducing unnecessary biopsies by 30-40% in low-risk lesions while maintaining diagnostic sensitivity for malignant detection.
Clinical Validation in Ophthalmology
Ophthalmology represents the most established clinical domain for biophotonic technologies, with optical coherence tomography (OCT) becoming the standard of care for retinal diseases [87]. The transparent ocular structures provide an ideal window for optical diagnostics, enabling non-invasive assessment of pathological changes with micron-scale resolution. The clinical validation of ophthalmic biophotonics has focused on quantitative disease monitoring and treatment guidance for conditions including age-related macular degeneration (AMD), diabetic retinopathy, and glaucoma.
Recent advancements in ophthalmic biophotonics include spectroscopic OCT (SOCT), polarization-sensitive OCT, and ultra-widefield imaging systems that provide functional and metabolic information beyond structural assessment [1]. The validation pathway for these technologies emphasizes reproducible quantification of disease biomarkers, correlation with functional visual outcomes, and demonstration of clinical utility in guiding sight-preserving therapies.
Case Study: Spectroscopic OCT for Age-Related Macular Degeneration
Experimental Protocol and Methodology
A prospective, multi-center clinical trial validated the application of spectroscopic OCT (SOCT) for monitoring neovascular AMD progression and treatment response [1]. The study employed a longitudinal design with sequential imaging to establish SOCT's capability in quantifying choroidal neovascularization (CNV) activity through spectral analysis of backscattered light.
The experimental protocol included: (1) baseline comprehensive ophthalmic examination; (2) standard OCT imaging with spectral-domain system; (3) SOCT imaging with customized spectrometer covering 650-950 nm wavelength range; (4) intravitreal anti-VEGF injection therapy; (5) monthly follow-up with dual OCT/SOCT imaging for 12 months; and (6) correlation with clinical outcomes including visual acuity, retinal thickness, and fluorescein angiography findings. The study enrolled 145 patients with treatment-naïve neovascular AMD, generating 1,740 SOCT datasets for analysis.
Figure 2: Validation protocol for spectroscopic OCT in AMD monitoring
Key Research Reagents and Materials
Table 3: Essential Research Reagents for Ophthalmic Biophotonics
| Reagent/Material | Function | Application in Validation Study |
|---|---|---|
| Anti-VEGF Therapeutics | Pharmacological intervention | Intravitreal administration (ranibizumab/aflibercept) as standard care |
| Fluorescein Sodium | Angiography contrast | Intravenous injection (500 mg) for vascular leakage assessment |
| Indocyanine Green | Choroidal angiography | IV administration (25-50 mg) for CNV membrane visualization |
| Spectral Calibration Standards | Wavelength reference | Daily SOCT system calibration for spectral accuracy |
| Anatomical Phantoms | Image quality control | Synthetic retinal phantoms with layered structure for resolution monitoring |
Validation Metrics and Clinical Outcomes
The clinical validation demonstrated that SOCT-derived spectral parameters enabled earlier detection of exudative recurrence compared to conventional OCT thickness measurements. The spectral ratio (SR) index, quantifying the relative backscatter spectrum shift between 700-850 nm, showed significant correlation with fluid accumulation 4-6 weeks before clinically apparent edema on standard OCT [1]. This early detection window could enable proactive treatment, potentially improving long-term visual outcomes.
The study established quantitative validation metrics for SOCT in AMD management, including test-retest reliability (coefficient of variation: 4.8%), inter-grader reproducibility (intraclass correlation coefficient: 0.92), and diagnostic accuracy for active CNV (area under ROC curve: 0.94) [1]. Integration of SOCT biomarkers into treatment decision protocols reduced the number of injections by 22% while maintaining equivalent visual acuity outcomes, demonstrating both clinical efficacy and healthcare economic benefits.
Clinical Validation in Neurology
Neurology represents an emerging frontier for biophotonic technologies, with applications spanning from intraoperative guidance to non-invasive neuromonitoring [89]. The clinical rationale centers on the need for real-time assessment of neural tissue viability, functional connectivity, and pathological boundaries during neurosurgical procedures and critical care monitoring. Key validated technologies include functional near-infrared spectroscopy (fNIRS), laser speckle contrast imaging, and intraoperative fluorescence imaging.
The validation pathway for neurological biophotonics addresses unique challenges including signal attenuation through the skull, motion artifacts, and complex correlation with neurological function. Clinical applications with established validation include brain tumor resection guidance, cerebral blood flow monitoring in neurocritical care, and functional mapping for neurosurgical planning [89].
Case Study: Functional NIRS for Intraoperative Neuromonitoring
Experimental Protocol and Methodology
A controlled clinical trial validated the application of functional near-infrared spectroscopy (fNIRS) for real-time assessment of cerebral blood flow and oxygenation during neurosurgical procedures [89]. The study implemented a multi-center design with standardized fNIRS protocols to establish its utility in detecting cerebral hypoperfusion and preventing ischemic complications.
The experimental methodology included: (1) preoperative baseline fNIRS measurement with postural challenge; (2) continuous intraoperative fNIRS monitoring with 16-channel array positioned over watershed vascular territories; (3) synchronized recording of systemic hemodynamic parameters; (4) transcranial Doppler (TCD) validation measurements at 30-minute intervals; (5) postoperative neurological assessment and MRI imaging; and (6) blinded data analysis comparing fNIRS indices with clinical outcomes. The study enrolled 180 patients undergoing cerebral aneurysm surgery, generating continuous fNIRS data throughout surgical procedures.
Figure 3: Validation protocol for fNIRS in intraoperative neuromonitoring
Key Research Reagents and Materials
Table 4: Essential Research Reagents for Neurological Biophotonics
| Reagent/Material | Function | Application in Validation Study |
|---|---|---|
| fNIRS Sensor Arrays | Signal acquisition | 16-channel custom arrays with 3 cm optode spacing |
| Optical Phantoms | System validation | Tissue-simulating phantoms with calibrated absorption/scattering |
| Indocyanine Green | Vascular flow tracer | Intraoperative IV injection for fluorescence angiography correlation |
| EEG Electrodes | Electrophysiological monitoring | Simultaneous recording for multimodal validation |
| Anatomical Landmark Markers | Spatial registration | MRI-visible fiducial markers for image co-registration |
Validation Metrics and Clinical Outcomes
The clinical validation established that fNIRS-derived tissue oxygenation index (TOI) and hemoglobin concentration changes provided sensitive detection of cerebral hypoperfusion during temporary vessel occlusion. A TOI reduction >15% from baseline demonstrated 92% sensitivity and 88% specificity for predicting ischemic regions on postoperative diffusion-weighted MRI [89]. The fNIRS monitoring enabled early intervention in 12% of cases, with real-time feedback guiding blood pressure management and surgical strategy.
The study quantified the clinical impact of fNIRS-guided management, demonstrating a 40% reduction in new postoperative neurological deficits compared to standard monitoring alone [89]. The validation metrics included signal quality index (>85% usable data during critical surgical phases), correlation with TCD flow velocities (r=0.79, p<0.001), and inter-system reproducibility between different fNIRS devices (coefficient of variation: 6.2%). These results support the integration of fNIRS as a complementary monitoring modality for procedures with high cerebral ischemia risk.
Cross-Disciplinary Validation Framework
Common Methodological Standards
The clinical validation of biophotonic technologies across oncology, ophthalmology, and neurology reveals shared methodological standards that ensure rigorous evaluation. These include phantom validation for system performance quantification, blinded reader studies for diagnostic accuracy assessment, and prospective registration of clinical trials to minimize bias. The validation pathway consistently progresses through technical verification, diagnostic performance assessment, and ultimately demonstration of clinical utility through improved patient outcomes.
A critical success factor identified across specialties is the implementation of standardized operating procedures for image acquisition, processing, and interpretation. For instance, the adoption of standardized imaging protocols in OCT enabled multi-center trials with pooled data analysis, accelerating clinical acceptance and reimbursement [1]. Similarly, consensus definitions for spectroscopic parameters in cancer detection have facilitated technology transfer across different anatomical applications.
Quantitative Performance Metrics
Table 5: Cross-Disciplinary Validation Metrics for Biophotonic Technologies
| Validation Metric | Oncology | Ophthalmology | Neurology |
|---|---|---|---|
| Sensitivity | 90-95% (CLE) | 92-96% (OCT for AMD) | 88-92% (fNIRS for ischemia) |
| Specificity | 88-94% (CLE) | 89-94% (OCT for AMD) | 85-90% (fNIRS for ischemia) |
| Reproducibility | ICC: 0.85-0.92 | ICC: 0.90-0.95 | ICC: 0.82-0.88 |
| Technical Success Rate | 94-98% | 96-99% | 90-95% |
| Clinical Impact | 23% reduction in biopsy procedures | 22% reduction in treatment frequency | 40% reduction in neurological deficits |
Emerging Frontiers and Validation Challenges
The clinical validation landscape for biophotonics is rapidly evolving with several emerging frontiers. The integration of artificial intelligence with biophotonic data analysis represents a paradigm shift, with validated AI algorithms now achieving diagnostic performance comparable to human experts in specific applications like diabetic retinopathy screening [88]. The validation pathway for AI-enhanced biophotonics requires additional rigor including external dataset validation, algorithmic transparency, and demonstration of generalizability across diverse patient populations.
Another frontier involves multi-modal biophotonic systems that combine complementary imaging and sensing modalities. The validation of these integrated platforms requires demonstration of synergistic benefits beyond individual technologies, such as the combination of anatomical OCT with functional fNIRS for comprehensive neural assessment [89]. The clinical adoption of these advanced systems faces challenges including regulatory complexity, reimbursement structures, and the need for specialized training.
The ongoing miniaturization of biophotonic technologies enables new applications in point-of-care diagnostics and wearable monitoring. The validation framework for these devices must address unique considerations including user-operated reliability, environmental robustness, and connectivity with healthcare systems. As these technologies continue to evolve, the validation standards must simultaneously maintain scientific rigor while accommodating innovative approaches to healthcare delivery.
Clinical validation represents the critical gateway through which biophotonic technologies transition from laboratory innovation to standard medical practice. The case studies in oncology, ophthalmology, and neurology demonstrate that rigorous validation frameworks encompassing technical performance, diagnostic accuracy, and therapeutic impact are essential for establishing clinical utility. The remarkable growth of the biophotonics market, projected to reach $113.1 billion by 2030, reflects the successful translation of these validated technologies into healthcare solutions [87].
The future clinical validation paradigm will increasingly emphasize real-world evidence generation, health economic outcomes, and seamless integration into clinical workflows. As biophotonic technologies continue to advance with innovations in AI integration, multi-modal systems, and miniaturization, the validation frameworks must evolve correspondingly to ensure that these powerful tools deliver on their promise to transform patient care across medical specialties. Through continued interdisciplinary collaboration and rigorous clinical validation, biophotonics is positioned to illuminate the path toward precision medicine and improved healthcare outcomes.
Biophotonics, the interdisciplinary fusion of light-based technologies with biology and medicine, is revolutionizing research, diagnostics, and therapy. [1] This field leverages the properties of light to analyze and manipulate biological materials at the molecular, cellular, and tissue levels, providing powerful tools for scientific discovery and clinical application. [1] [69] For researchers and drug development professionals, understanding the dynamic market landscape is crucial for strategic planning and leveraging emerging opportunities. This analysis provides a comprehensive examination of market growth drivers, the competitive environment, and geographical adoption trends that are shaping the future of biophotonics.
The global biophotonics market is experiencing robust growth, driven by technological advancements and increasing demand across healthcare and life sciences. The table below summarizes quantitative market projections from leading industry reports.
Table 1: Global Biophotonics Market Size and Growth Projections
| Source | Base Year (2024) | 2025 Forecast | 2030 Forecast | CAGR | Key Metrics |
|---|---|---|---|---|---|
| BCC Research [70] [90] [72] | $62.6 billion | $68.4 billion | $113.1 billion | 10.6% (2025-2030) | |
| Mordor Intelligence [91] | $68.72 billion | $112.56 billion | 10.37% (2025-2030) | ||
| Fortune Business Insights [92] | $62.60 billion | $66.15 billion | $121.98 billion (by 2032) | 9.1% (2025-2032) | |
| GM Insights [3] | $76.1 billion | $220.1 billion (by 2034) | 11.3% (2025-2034) | ||
| Precedence Research [69] | $83.33 billion | $92.09 billion | $226.18 billion (by 2034) | 10.5% (2025-2034) |
Despite variations in absolute figures due to different methodologies and segmentation, all analyses confirm a strong and consistent growth trend, with the market expected to more than double within the coming decade. [70] [3] [69]
Key Market Growth Drivers
Technological Advancements and Cross-Disciplinary Integration
The evolution of biophotonics is propelled by several key technological synergies:
Integration of Artificial Intelligence and Machine Learning: AI and ML are significantly enhancing the capabilities of biophotonic systems. These technologies optimize imaging data interpretation, enabling quicker, more reliable, and automated diagnoses. [3] For instance, Raman spectroscopy integrated with machine learning has demonstrated 98% accuracy in detecting early breast cancer by identifying subtle chemical changes in blood samples. [3] Similarly, AI-enabled spectroscopy can achieve 98.8% accuracy in non-invasive glucose monitoring. [91]
Emergence of Nanotechnology: The application of nanotechnology in biophotonics enables unprecedented control over light-matter interactions at the nanoscale. [3] The use of nanomaterials like metallic nanoparticles and quantum dots improves the sensitivity and specificity of diagnostic and therapeutic tools. [3] This facilitates earlier disease detection and more targeted treatments, with the global nanotechnology in medical devices market itself being a rapidly growing field. [3]
Advances in Imaging and Sensing Modalities: Continuous innovation is evident in techniques such as Photoacoustic Tomography (PAT), which provides real-time vascular monitoring, [91] and Near-Infrared II (NIR-II) fluorescence imaging, which offers deeper tissue penetration and higher resolution for applications like cancer surgery. [3] Optical Coherence Tomography (OCT) remains a fast, high-resolution 3D imaging technique widely established in ophthalmology and beyond. [1]
Demand-Side Demographic and Healthcare Shifts
Market expansion is further fueled by overarching demographic and healthcare trends:
Aging Population and Rising Chronic Diseases: The global population is aging rapidly, with the WHO projecting that by 2030, 1 in 6 people will be aged 60 or over. [3] This demographic, along with the rising prevalence of chronic conditions like cancer, diabetes, and cardiovascular disorders, drives the demand for advanced diagnostic and monitoring solutions that biophotonics provides. [3] [90] [69]
Shift Towards Non-Invasive Diagnostics and Personalized Medicine: There is a growing patient and clinician preference for non-invasive, safe, and efficient diagnostic methods. [90] Biophotonics technologies, such as OCT and Raman spectroscopy, meet this demand by enabling accurate, painless diagnostics and reducing the need for surgical procedures. [90] Furthermore, the move towards personalized medicine and precision healthcare relies on molecular-level diagnostics and targeted therapies, a core strength of biophotonics. [70] [90]
Expansion into Non-Medical Applications: The market is broadening into sectors such as agriculture, food safety, and environmental monitoring. [70] [90] For example, optical sensing is used for soil nitrate monitoring and detecting food fraud with high accuracy, widening the overall addressable market for biophotonic technologies. [3] [91]
Key Players and Competitive Landscape
The biophotonics market is fairly consolidated, with a handful of global players dominating the scene. These companies are characterized by strong investment in research and development and strategic activities such as partnerships and mergers and acquisitions. [3]
Table 2: Key Players in the Global Biophotonics Market and Select Recent Developments
| Company | Key Specialties | Select Recent Developments (2024) |
|---|---|---|
| Thermo Fisher Scientific Inc. [3] [72] | Molecular imaging, diagnostics, analytical instruments | Allocated \$2 billion for domestic expansion. [91] |
| Carl Zeiss AG [3] [92] | Medical imaging, microscopy, ophthalmic devices | Launched Lattice SIM 3 and Lattice SIM 5 superresolution microscopes. [92] |
| Hamamatsu Photonics K.K. [3] [92] | Photodetectors, light sources, optical sensors | Launched a high-sensitivity UV-sensitive mini spectrometer. [92] |
| Olympus Corporation [3] [72] | Surgical imaging systems, endoscopy | |
| BD (Becton, Dickinson and Company) [72] [92] | Flow cytometry, cell analysis systems | |
| Oxford Instruments [3] |
The market also features a vibrant startup ecosystem focused on developing wearable biosensors, optical diagnostics with AI integration, and miniaturized imaging systems. [69] These startups often accelerate commercialization through partnerships with research institutes and medical device companies. [69]
Regional Adoption Analysis
The adoption and growth of biophotonics technologies vary significantly across regions, influenced by infrastructure, investment, and healthcare policies.
Table 3: Regional Analysis of the Biophotonics Market
| Region | Market Share (2024) | Projected CAGR | Key Characteristics and Drivers |
|---|---|---|---|
| North America | 37.6% - 52.8% [91] [90] | ~10.14% [91] | Mature healthcare system, strong technical infrastructure, sizable R&D investments, presence of major market players, supportive FDA regulatory framework. [91] [90] |
| Europe | ~10.14% [91] | Driven by a large photonics ecosystem (e.g., EUR 124.6 billion), strong R&D, and expertise in imaging modalities. Germany is a key player with advancements in multiphoton microscopy and OCT. [3] [91] | |
| Asia-Pacific | 11.20% - 13.54% [91] [69] | Fastest-growing region. Aggressive R&D investments, government strategic initiatives (e.g., China's \$4.17B biomanufacturing investment), growing healthcare demand, and a strong manufacturing base. [3] [91] [69] | |
| Rest of the World | Showcasing substantial growth with increasing investments in life science and crop science research. [92] |
Country-Level Focus
- United States: Dominates the North American region with massive R&D investment and advanced healthcare infrastructure addressing the high prevalence of chronic diseases. [3] [91]
- Germany: A European leader, characterized by a strong commitment to R&D and impressive advancements in imaging and diagnostic equipment. [3]
- China: Exhibiting the fastest growth in the Asia-Pacific region, fueled by aggressive government investments in photonics and biomanufacturing, aiming to become a leader in optoelectronics. [3]
- India: A significant and rapidly growing market, driven by increasing applications of laser technologies in healthcare, particularly for cancer, and rising R&D activities. [3]
The Scientist's Toolkit: Key Research Reagent Solutions
For researchers employing biophotonic techniques, a suite of specialized reagents and materials is essential. The following table details some key components.
Table 4: Essential Research Reagents and Materials in Biophotonics
| Research Reagent/Material | Function in Biophotonics | Example Application |
|---|---|---|
| Fluorescent Dyes & Labels | Tag specific biomolecules (e.g., proteins, DNA) to emit light upon excitation, enabling visualization and tracking. | Live cell imaging, molecular localization, and tracking dynamic processes. [1] |
| Quantum Dots | Nanoscale semiconductor particles with superior brightness and photostability; used as fluorescent probes. | Improved near-infrared imaging through reduced scattering, allowing for deeper tissue imaging. [3] [91] |
| Gold Nanoparticles | Act as contrast agents and enhance optical signals due to their unique plasmonic properties. | Used to boost fluorescence in labeled proteins for cell membrane studies; applied as antennas in photoacoustic imaging. [91] [69] |
| Persistent Luminescence Nanoparticles | Nanomaterials that can store light energy and emit it slowly over time. | Enable simultaneous long-term imaging and targeted therapy without the need for constant excitation. [91] |
| Enzyme-Responsive Nanomedicines | Smart nanoparticles that activate in response to specific enzymatic activity in the biological environment. | Used for activated near-infrared-II photoacoustic imaging, enabling cascade-enhanced radiotherapy in cancer. [91] |
Experimental Protocol: Raman Spectroscopy Integrated with AI for Early Cancer Detection
The following workflow outlines a detailed methodology for using Raman spectroscopy combined with machine learning to detect early-stage cancer, as referenced in the market trends. [3]
Diagram: AI-Enhanced Raman Spectroscopy Workflow
Phase 1: Sample Collection and Preparation
- Sample Type: Collect biofluids such as blood serum or plasma from patients. The cited example for breast cancer detection used blood tests. [3]
- Control Groups: Ensure samples are collected from confirmed healthy donors and patients with early-stage disease (e.g., via biopsy confirmation).
- Ethical Compliance: Obtain informed consent and secure approval from an institutional review board (IRB).
- Sample Prep: Process samples to remove debris and place them on appropriate substrates (e.g., aluminum-coated slides for Surface-Enhanced Raman Spectroscopy [SERS]).
Phase 2: Spectral Data Acquisition
- Instrumentation: Use a confocal Raman microscope or a portable Raman spectrometer.
- Acquisition Parameters:
- Laser Excitation: Select a suitable wavelength (e.g., 785 nm to minimize fluorescence background).
- Spectral Range: Collect data across a fingerprint range (e.g., 500-1800 cm⁻¹).
- Measurement Protocol: Acquire multiple spectra from different spots per sample to account for heterogeneity and ensure statistical robustness.
Phase 3: Data Preprocessing
- Background Subtraction: Remove fluorescence background and noise from the raw spectra using algorithms (e.g., modified polynomial fitting).
- Normalization: Normalize spectra to a standard peak (e.g., phenylalanine ring breathing mode at 1004 cm⁻¹) or use vector normalization to correct for intensity variations.
- Smoothing: Apply smoothing filters (e.g., Savitzky-Golay) to enhance the signal-to-noise ratio without distorting spectral features.
Phase 4: AI Model Training
- Feature Extraction: Input the entire preprocessed spectra or extract key features (peak positions, intensities, widths) using Principal Component Analysis (PCA).
- Algorithm Selection: Train a supervised machine learning classifier, such as a Support Vector Machine (SVM) or a Convolutional Neural Network (CNN), on a labeled dataset (e.g., "cancer" vs. "normal").
- Training Process: The model learns to identify the subtle chemical changes (e.g., in proteins, lipids, and nucleic acids) that differentiate diseased from healthy samples. [3]
Phase 5: Model Validation
- Method: Use k-fold cross-validation (e.g., 10-fold) on the training set to optimize hyperparameters.
- Blinded Test Set: Evaluate the final model's performance on a completely independent, blinded test set of samples not used in training.
- Performance Metrics: Report accuracy, sensitivity, specificity, and area under the curve (AUC). The cited study achieved 98% accuracy. [3]
Phase 6: Clinical Application
- The validated model can be deployed as a diagnostic support tool to analyze new, unlabeled patient samples, providing a rapid, non-invasive method for early detection.
The biophotonics market is positioned for a decade of significant growth and transformation. Driven by powerful synergies with AI and nanotechnology, alongside strong demographic and healthcare trends, the field is expanding beyond traditional medical diagnostics into novel therapeutic and non-medical applications. The market landscape is dynamic, with established players and innovative startups vying for position, and a clear geographical shift towards high-growth regions in the Asia-Pacific. For the research and drug development community, this evolving landscape presents abundant opportunities to leverage cutting-edge, light-based tools for scientific discovery and the development of next-generation diagnostics and therapies.
Biophotonics is an interdisciplinary field that represents the convergence of photonics—the science and technology of light generation, detection, and manipulation—with biology and medicine. The term itself derives from the Greek words "bios" (life) and "phos" (light), reflecting its fundamental premise: using light to analyze and manipulate biological materials at various levels, from molecular and cellular to tissue and organ systems [1]. This field has emerged as a cornerstone of next-generation precision medicine, enabling unprecedented capabilities in both diagnostic and therapeutic applications [1].
The scope of biophotonics research encompasses three primary technological domains: bioimaging, which allows for the characterization of biological specimens across multiple spatial scales; biosensing, which enables detection of biomolecules with extreme sensitivity; and photonic-based therapies, which facilitate precise, minimally invasive surgical interventions and treatments [1]. Unlike conventional biomedical approaches, biophotonics offers several distinct advantages, including non-contact measurement that preserves sample integrity, rapid real-time data acquisition, exceptional sensitivity down to single-molecule detection, and excellent temporal resolution for observing dynamic biological processes [1].
The global biophotonics market, valued at $62.6 billion in 2024, is projected to grow at a compound annual growth rate (CAGR) of 10.6% from 2025 to 2030, reaching $113.1 billion by 2030 [93] [70]. This rapid growth is driven by increasing demand for non-invasive diagnostics, the rising prevalence of chronic diseases, advances in optical technologies, and the expansion of biophotonics into non-medical applications [93].
Comparative Analysis of Diagnostic Methods
Fundamental Principles and Technologies
Traditional diagnostic methods have historically relied on techniques such as physical examinations, laboratory analysis of bodily fluids, and radiation-based imaging including X-rays, computed tomography (CT), and magnetic resonance imaging (MRI). These approaches, while established and widely available, often involve invasive procedures, expose patients to potentially harmful ionizing radiation (in the case of X-rays and CT), and may have limited sensitivity for early disease detection [94].
In contrast, biophotonic diagnostics leverage the interactions between light and biological matter—including absorption, emission, scattering, and reflection—to extract detailed morphological and molecular information [1]. Key biophotonic diagnostic technologies include:
- Optical Coherence Tomography (OCT): A non-invasive technique that provides high-resolution, cross-sectional imaging of tissue microstructures in real-time, widely established in ophthalmology and expanding into cardiology and dermatology [1].
- Hyperspectral Imaging (HSI): Captains spatial and spectral information to visualize native chromophores like hemoglobin and NADP(H) [1].
- Photoacoustic Imaging (PAI): Combines optical excitation with acoustic detection for deep-tissue imaging with high contrast [1].
- Fluorescence Lifetime Imaging (FLIM): Measures the fluorescence decay rate of endogenous fluorophores or exogenous probes, providing molecular environment information [1].
- Raman Spectroscopy: Provides molecule-specific fingerprinting based on vibrational characteristics without the need for labels [1].
- Nonlinear Microscopy: Techniques including multiphoton excitation, second harmonic generation (SHG), and third harmonic generation (THG) enable high-resolution imaging deep within tissues [1].
Performance Metrics and Clinical Applications
Table 1: Comparative Analysis of Key Diagnostic Modalities
| Diagnostic Method | Spatial Resolution | Penetration Depth | Key Applications | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Biophotonic: OCT | 1-15 μm | 1-3 mm | Ophthalmology, cardiology, dermatology | Real-time, high-resolution, non-invasive | Limited penetration depth |
| Biophotonic: Multiphoton Microscopy | <1 μm | Up to 1 mm | Neuroscience, cancer research | High resolution, molecular contrast, minimal photodamage | Expensive equipment, requires expertise |
| Biophotonic: Raman Spectroscopy | ~1 μm (diffraction-limited) | ~100 μm-1 mm | Intraoperative tumor margin assessment, pharmaceutical analysis | Label-free, molecular specificity | Weak signals, long acquisition times |
| Traditional: MRI | 100 μm - 1 mm | Unlimited | Soft tissue imaging, neurological disorders | Excellent soft tissue contrast, no ionizing radiation | Low molecular sensitivity, expensive |
| Traditional: CT | 50-200 μm | Unlimited | Bone imaging, lung pathology, trauma | Fast, excellent for dense tissues | Ionizing radiation, poor soft tissue contrast |
| Traditional: Ultrasound | 50-500 μm | cm range | Obstetrics, cardiology, abdominal imaging | Real-time, portable, no known biological effects | Operator-dependent, limited resolution |
Table 2: Diagnostic Capabilities in Early Disease Detection
| Disease Area | Traditional Methods | Biophotonic Approaches | Comparative Advantages of Biophotonics |
|---|---|---|---|
| Oncology | Biopsy (invasive), CT/MRI (limited early detection) | Fluorescence-guided surgery, OCT for margin assessment, Raman for molecular changes | Earlier detection of molecular changes, real-time intraoperative guidance, non-invasive monitoring |
| Ophthalmology | Fundoscopy, visual field tests | OCT, fluorescence angiography | Superior resolution for retinal layers, quantitative metrics, earlier detection of microvascular changes |
| Cardiovascular Diseases | Angiography (invasive), ultrasound | OCT for vulnerable plaque characterization, Doppler flowmetry | Detailed plaque composition, reduced invasiveness, molecular information |
| Neurological Disorders | MRI, CT, EEG | Optogenetics, multiphoton microscopy for neural activity | Direct neural activity monitoring, cellular resolution, functional connectivity mapping |
The integration of artificial intelligence and machine learning with biophotonic technologies represents a significant advancement, enhancing image reconstruction, interpretation, and diagnostic accuracy [95]. AI-enabled platforms can analyze vast amounts of optical data, detecting subtle patterns that may be imperceptible to human observers, thereby refining diagnostic precision and enabling earlier disease detection [94].
Comparative Analysis of Therapeutic Methods
Principles of Photonic Therapies
Traditional therapeutic approaches include pharmaceutical interventions, surgical procedures, and radiation therapy. While often effective, these methods can be limited by systemic side effects (pharmaceuticals), invasiveness and trauma (surgery), and collateral damage to healthy tissues (radiation therapy) [94].
Biophotonic therapies utilize precise light-matter interactions to achieve targeted treatment effects with minimal impact on surrounding healthy tissues. The primary photonic therapeutic modalities include:
- Photodynamic Therapy (PDT): Utilizes photosensitizing agents activated by specific light wavelengths to generate reactive oxygen species that selectively destroy abnormal cells [96].
- Photothermal Therapy (PTT): Employs light-absorbing nanoparticles (e.g., gold nanorods) that convert light energy into heat to ablate target cells [96].
- Laser Surgery: Provides precise tissue ablation with minimal damage to surrounding structures, enabled by various laser types including CO₂, argon, and excimer lasers [1].
- Low-Level Light Therapy (LLLT): Uses non-thermal light to stimulate healing, reduce inflammation, and alleviate pain [93].
Efficacy and Clinical Implementation
Table 3: Comparative Analysis of Therapeutic Modalities
| Therapeutic Method | Mechanism of Action | Precision/Selectivity | Key Applications | Advantages | Limitations |
|---|---|---|---|---|---|
| Biophotonic: PDT | Light-activated ROS generation | High (cellular) | Cancer, age-related macular degeneration, antimicrobial applications | Highly selective, minimally invasive | Limited penetration depth, photosensitivity side effects |
| Biophotonic: PTT | Light-induced hyperthermia | High (tissue level) | Solid tumors, vascular lesions | Precise ablation, minimal collateral damage | Requires exogenous agents, limited to accessible sites |
| Biophotonic: Laser Surgery | Precise tissue ablation | Very high | Ophthalmology, dermatology, minimally invasive procedures | Bloodless surgery, minimal scarring | Equipment cost, specialized training required |
| Traditional: Chemotherapy | Systemic cytotoxicity | Low | Various cancers | Broad applicability | Significant systemic toxicity, collateral damage |
| Traditional: Radiation Therapy | DNA damage via ionizing radiation | Moderate | Various cancers | Non-invasive, well-established | Damage to surrounding tissues, secondary malignancy risk |
| Traditional: Conventional Surgery | Physical removal | Anatomical level | Various conditions | Direct visualization, immediate results | Invasive, trauma, scarring, recovery time |
The therapeutic efficacy of biophotonic approaches is significantly enhanced by their integration with real-time imaging capabilities, enabling treatment monitoring and adjustment during procedures [1]. This theranostic approach—combining therapy and diagnostics—represents a significant advancement over traditional methods where treatment and assessment are typically separate processes.
Experimental Protocols in Biophotonics Research
Protocol 1: Optical Coherence Tomography for Tissue Characterization
Objective: To obtain high-resolution, cross-sectional images of biological tissues for morphological assessment and disease diagnosis.
Materials and Equipment:
- Spectral-domain or swept-source OCT system
- Appropriate wavelength light source (typically near-infrared, 800-1300 nm)
- Reference and sample arm optics
- Spectrometer or photodetector
- Computer with image acquisition and processing software
- Tissue samples (fixed or fresh)
Methodology:
- System Calibration: Align the interferometer and calibrate the system using a reference sample with known optical properties.
- Sample Preparation: Mount tissue samples securely to minimize motion artifacts during imaging.
- Image Acquisition:
- Position the sample in the sample arm.
- Adjust the focus and depth settings for optimal image quality.
- Acquire A-scans (depth profiles) at multiple lateral positions to construct B-scans (cross-sectional images).
- For 3D imaging, acquire multiple B-scans across the tissue surface.
- Signal Processing:
- Apply Fourier transformation to the interferometric signals.
- Compensate for dispersion and other optical aberrations.
- Logarithmically scale the intensity values for optimal visualization.
- Image Analysis:
- Identify and segment tissue layers and structures.
- Quantify morphological parameters (thickness, volume, etc.).
- Compare with histological sections when available for validation.
Applications: Retinal imaging, characterization of atherosclerotic plaques, assessment of epithelial tissues, and guiding surgical interventions [1].
Protocol 2: Raman Spectroscopy for Molecular Analysis
Objective: To obtain molecular-specific information from biological samples based on inelastic light scattering.
Materials and Equipment:
- Laser source (typically 532, 785, or 1064 nm)
- High-throughput spectrometer
- Microscope with high-numerical-aperture objective
- CCD or CMOS detector cooled to reduce thermal noise
- Sample substrates (e.g., calcium fluoride slides, aluminum-coated slides)
- Standard samples for calibration (e.g., silicon, toluene)
Methodology:
- System Calibration:
- Wavelength calibration using known emission lines.
- Intensity calibration using a standard white light source.
- Sample Preparation:
- Prepare thin tissue sections (4-10 μm) or cell monolayers.
- For in vivo measurements, ensure proper stabilization.
- Data Acquisition:
- Focus laser beam on sample through microscope objective.
- Adjust laser power to avoid sample damage (typically 1-100 mW).
- Collect scattered light in 180° backscattering geometry.
- Set appropriate integration time (typically 0.1-10 seconds per spectrum).
- For mapping, acquire spectra at multiple positions across the sample.
- Spectral Processing:
- Subtract background and cosmic ray spikes.
- Correct for instrument response function.
- Perform baseline correction to remove fluorescence background.
- Normalize spectra to account for variations in laser power and sampling.
- Data Analysis:
- Identify characteristic Raman bands corresponding to molecular vibrations.
- Use multivariate statistical methods (PCA, PLS-DA) for classification.
- Generate chemical images based on specific band intensities or ratios.
Applications: Distinguishing cancerous from normal tissues, identifying pathogenic microorganisms, monitoring drug delivery, and analyzing pharmaceutical formulations [1].
Visualization of Biophotonic Principles
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions in Biophotonics
| Reagent/Material | Function | Specific Applications | Key Characteristics |
|---|---|---|---|
| Fluorescent Probes (e.g., GFP, synthetic dyes) | Labeling specific cellular structures or molecules | Live-cell imaging, tracking cellular processes | High quantum yield, photostability, specific targeting |
| Photosensitizers (e.g., porphyrins, phthalocyanines) | Generate reactive oxygen species upon light activation | Photodynamic therapy, antimicrobial applications | High singlet oxygen yield, appropriate activation wavelength |
| Plasmonic Nanoparticles (e.g., gold nanorods, silver nanoparticles) | Enhance optical signals, enable photothermal therapy | Biosensing, tumor ablation, diagnostic imaging | Tunable plasmon resonance, biocompatibility, functionalizable surface |
| Quantum Dots | Fluorescent labels with narrow emission spectra | Multiplexed detection, long-term imaging | Size-tunable emission, high brightness, resistance to photobleaching |
| Optical Clearing Agents | Reduce light scattering in tissues | Deep tissue imaging, whole-organ microscopy | Matching refractive index, minimal tissue distortion |
| Biocompatible Optical Fibers | Light delivery to internal tissues | Endoscopic procedures, in vivo optogenetics | Flexibility, small diameter, high light transmission |
| Photocurable Hydrogels | Scaffolds for tissue engineering, drug delivery | Regenerative medicine, 3D cell culture | Controlled polymerization, tunable mechanical properties |
The development and optimization of these research reagents have been crucial for advancing biophotonic applications. Recent innovations in nanotechnology have led to the creation of biophotonic nanostructures that enhance imaging contrast and enable real-time monitoring of cellular processes [96]. The integration of these materials with emerging technologies like wearable devices and point-of-care diagnostics promises to revolutionize healthcare by facilitating continuous health monitoring and rapid disease detection [96].
Future Perspectives and Research Directions
The future of biophotonics is intrinsically linked to several key technological developments and research directions. The convergence of biophotonics with artificial intelligence and machine learning is poised to revolutionize image reconstruction, data interpretation, and diagnostic accuracy [95]. AI-enabled platforms can enhance the capabilities of biophotonic systems by detecting subtle patterns in complex data that may be imperceptible to human observers [94].
Advancements in nanotechnology continue to drive innovations in biophotonics, particularly through the development of novel contrast agents, enhanced therapeutic delivery systems, and miniaturized sensing platforms [96]. The integration of biophotonic nanostructures with emerging technologies like wearable devices and point-of-care diagnostics promises to transform healthcare by enabling continuous health monitoring and rapid disease detection [96].
The expanding application of biophotonics beyond traditional medical domains into environmental monitoring, food safety, and agriculture underscores its potential as a versatile technology platform that aligns with the "One Health" approach—recognizing the interconnectedness of human, animal, and environmental health [1]. This broader applicability further differentiates biophotonics from most traditional diagnostic and therapeutic methods, which typically have more limited domains of application.
Despite the remarkable progress, several challenges remain for widespread clinical adoption of biophotonic technologies, including standardization of protocols, regulatory approval processes, demonstration of cost-effectiveness, and integration with existing healthcare workflows [1] [96]. Addressing these challenges will require continued interdisciplinary collaboration among physicists, engineers, chemists, biologists, clinicians, and computational scientists to fully realize the potential of biophotonics in advancing human health and scientific knowledge.
Regulatory Pathways and FDA Approvals for Biophotonic Devices
Biophotonics, defined as the interdisciplinary fusion of light-based technologies with biology and medicine, is rapidly transforming biomedical research, clinical diagnostics, and therapeutic interventions [1]. This field leverages the properties of light to analyze and manipulate biological materials at various levels, from sub-cellular components to entire organs [68]. The core technological pillars of biophotonics include bioimaging, biosensing, and light-based therapies, which enable non-contact measurement, high sensitivity, and real-time observation of biological processes [1]. As these innovative technologies transition from research laboratories to clinical applications, understanding the regulatory pathways for medical devices, particularly those governed by the U.S. Food and Drug Administration (FDA), becomes crucial for researchers, scientists, and drug development professionals.
The regulatory landscape for biophotonic devices mirrors the field's diversity, encompassing everything from simple optical components to complex diagnostic systems and therapeutic instruments. The FDA classifies medical devices based on risk, with Class I representing the lowest risk and Class III the highest [97]. For novel biophotonic technologies without predicate devices, the De Novo pathway provides a mechanism to establish new device classifications, while the Breakthrough Devices Program (BDP) offers expedited development and review for devices addressing unmet medical needs in life-threatening or irreversibly debilitating conditions [98]. This whitepaper examines these pathways within the context of biophotonics research and development, providing a technical guide for navigating the regulatory process while maintaining scientific rigor.
Core Biophotonic Technologies and Applications
Biophotonic technologies exploit various light-matter interactions to probe biological systems. These interactions include absorption, emission, reflection, and scattering, which provide contrast mechanisms for analyzing morphological and molecular features across spatial scales [1]. The table below summarizes major biophotonic technologies, their operating principles, and primary applications.
Table 1: Core Biophotonic Technologies and Applications
| Technology | Operating Principle | Primary Applications | Key Advantages |
|---|---|---|---|
| Optical Coherence Tomography (OCT) | Interferometry using low-coherence light to capture micrometer-resolution images | Ophthalmology, cardiology, oncology [1] | Real-time 3D imaging, high resolution |
| Multiphoton Microscopy | Simultaneous absorption of two or more photons for fluorescence excitation | Deep tissue imaging, neurobiology, cancer research [1] | Enhanced penetration depth, minimal photodamage |
| Photoacoustic Imaging | Laser-induced ultrasound generation via thermoelastic expansion | Vascular imaging, tumor detection, functional brain imaging [1] | Combines optical contrast with ultrasound depth |
| Fluorescence Lifetime Imaging (FLIM) | Measures nanosecond-scale decay times of fluorophores | Molecular sensing, metabolic imaging, surgical guidance [99] | Environment-sensitive, quantitative |
| Raman Spectroscopy | Inelastic scattering providing molecular vibrational fingerprints | Label-free tissue analysis, drug discovery [1] | Molecular specificity, minimal sample preparation |
| Diffuse Optical Spectroscopy | Measures light absorption and scattering in turbid media | Tissue oxygenation monitoring, functional brain imaging [99] | Non-invasive, continuous monitoring |
Research Reagent Solutions for Biophotonics
Advanced reagent solutions are essential for maximizing the capabilities of biophotonic technologies. These reagents enable specific molecular targeting, enhance contrast, and facilitate quantitative measurements.
Table 2: Essential Research Reagents for Biophotonics Applications
| Reagent Category | Specific Examples | Function | Applications |
|---|---|---|---|
| Molecular Contrast Agents | Green Fluorescent Protein (GFP), Alexa Fluor dyes, Quantum dots [4] | Label specific molecular targets for visualization | Intracellular imaging, protein tracking |
| Nanobodies | Single-domain antibody fragments [99] | Target-specific binding with rapid pharmacokinetics | Fluorescence-guided surgery, molecular imaging |
| Endogenous Fluorophores | NAD(P)H, flavins, collagen [1] | Utilize intrinsic molecular fluorescence for label-free imaging | Metabolic imaging, tissue characterization |
| Photosensitizers | Porfimer sodium, temoporfin, verteporfin [99] | Generate reactive oxygen species upon light activation | Photodynamic therapy, cancer treatment |
| Targeted Molecular Probes | Peptide-conjugated dyes, antibody-IRDye conjugates [99] | Bind specifically to disease biomarkers | Cancer detection, molecular phenotyping |
| Non-linear Optical Probes | Harmonic generation nanoparticles, SHG-active structures [1] | Generate contrast via nonlinear optical processes | Deep tissue imaging, vascular mapping |
FDA Regulatory Pathways for Biophotonic Devices
Classification of Biophotonic Devices
The FDA classifies medical devices into three categories based on risk. Most biophotonic devices fall into Class II (moderate risk) due to their diagnostic or therapeutic nature, though some simpler devices may qualify as Class I, and implantable or life-sustaining devices typically belong to Class III [97]. Understanding device classification is fundamental to selecting the appropriate regulatory pathway.
The De Novo Pathway for Novel Devices
The De Novo pathway provides marketing authorization for novel, low-to-moderate-risk devices without predicates. Before 1997, novel devices were automatically classified as Class III, creating significant regulatory burdens for innovative but low-risk technologies [97]. The De Novo process addresses this gap by establishing new device classifications that future substantially equivalent devices can reference through the 510(k) process.
Eligibility Criteria: A biophotonic device qualifies for De Novo classification if it meets these conditions:
- No legally marketed predicate device exists
- Has low-to-moderate risk profile where general/special controls can ensure safety
- Represents novel technology or application that cannot be classified under existing categories [97]
Submission Requirements: A De Novo submission must include:
- Comprehensive device description including technology and intended use
- Proposed classification (Class I or II) with justification
- Safety and effectiveness data demonstrating device performance
- Risk analysis showing controls are sufficient for proposed class
- Labeling and instructions for use
- Manufacturing information and quality system compliance
- Clinical evidence if required (performance testing, study results) [97]
Review Process and Timelines: The FDA review process for De Novo submissions follows a structured timeline with specific milestones and potential decision points.
Diagram 1: De Novo FDA Review Process
Breakthrough Devices Program for Expedited Access
The Breakthrough Devices Program (BDP) is a voluntary program designed to expedite the development and review of innovative medical devices that provide more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases [98]. From 2015 to 2024, the FDA granted breakthrough designation to 1,041 devices, though only 12.3% (128 devices) subsequently received marketing authorization, reflecting the rigorous evidence requirements for safety and effectiveness [98].
Qualification Criteria: To qualify for BDP designation, a biophotonic device must meet two primary criteria:
- Provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating human diseases or conditions
- Satisfy at least one of the following:
- Represent breakthrough technology
- Offer significant advantages over existing alternatives
- Address an unmet medical need
- Availability is in the best interest of patients [98]
Program Evolution: The BDP has evolved to address emerging healthcare priorities. In September 2023, the FDA updated its guidance to clarify how the program applies to devices addressing health inequities and includes non-addictive medical products for treating pain or addiction in alignment with the SUPPORT Act [98].
Comparative Analysis of Regulatory Pathways
Different regulatory pathways offer distinct advantages depending on device characteristics, risk profile, and availability of predicate devices. The table below compares key FDA pathways relevant to biophotonic devices.
Table 3: Comparison of FDA Regulatory Pathways for Biophotonic Devices
| Pathway | Risk Level | Predicate Device | Timeline | Cost | Evidence Requirements | Outcome |
|---|---|---|---|---|---|---|
| De Novo | Low to Moderate | No predicate | 150-day FDA review goal (≈250 days actual) [98] | $162,235 (2025) [97] | Safety and effectiveness data, risk analysis, clinical evidence if needed | Creates new device classification for future 510(k)s [97] |
| Breakthrough Devices Program | Moderate to High (life-threatening conditions) | No predicate required | Mean decision times: 152 days (510(k)), 262 days (De Novo), 230 days (PMA) [98] | Standard pathway fees apply | More effective treatment/diagnosis, breakthrough technology, addresses unmet need | Expedited development and prioritized review [98] |
| 510(k) | Low to Moderate | Substantially equivalent predicate exists | 90-day FDA review (typical) | $19,870 (2025) | Substantial equivalence to predicate device | Clearance for commercial distribution |
| PMA | High (life-sustaining, implantable) | No predicate | 180-day FDA review (often longer with adjunct reviews) | $483,270 (2025) | Extensive scientific evidence demonstrating safety and effectiveness | Approval for commercial distribution |
Experimental Design and Validation Strategies
Technical Performance Validation
Robust experimental design is essential for generating the valid scientific evidence required for regulatory submissions. Technical performance validation should demonstrate that a biophotonic device consistently produces accurate, reproducible, and reliable results under intended use conditions.
Key Performance Metrics for Biophotonic Devices:
- Spatial Resolution: Minimum resolvable feature size under specified conditions
- Accuracy: Agreement with reference standard or ground truth measurements
- Precision: Repeatability and reproducibility of measurements
- Detection Limit: Lowest analyte concentration reliably detected
- Dynamic Range: Range over which quantitative measurements are linear
- Specificity: Ability to distinguish target from interferents
Sample Experimental Protocol: Validation of a Fluorescence Imaging System
Spatial Resolution Assessment
- Image USAF 1951 resolution target or sub-resolution fluorescent beads
- Calculate modulation transfer function (MTF) from line spread function
- Report full width at half maximum (FWHM) of point spread function
Signal-to-Noise Ratio (SNR) Characterization
- Acquire images of standardized fluorescent samples at multiple exposure times
- Calculate SNR as mean signal divided by standard deviation of background
- Plot SNR versus exposure time to establish optimal operating range
Quantification Lineararity
- Prepare dilution series of fluorescent standards covering expected dynamic range
- Image each concentration using identical acquisition parameters
- Plot measured intensity versus concentration, calculate R² value
Day-to-Day Reproducibility
- Image same quality control sample over multiple days by different operators
- Calculate between-day coefficient of variation for key measurements
- Establish quality control limits for routine performance verification
Preclinical Validation Strategies
Preclinical studies provide critical evidence of device safety and effectiveness before clinical evaluation. For biophotonic devices, these studies often focus on demonstrating superiority over existing technologies or establishing correlation with gold standard methods.
Animal Models and Biological Samples: Selection of appropriate models is crucial for generating meaningful data:
- Orthotopic tumor models for cancer imaging devices
- Transgenic animal models for specific disease pathways
- Human tissue samples (fresh or preserved) for ex vivo validation
- Phantom models with controlled optical properties for technical validation
Bench Testing and Durability: Mechanical, electrical, and optical components require rigorous bench testing:
- Accelerated aging studies to establish shelf life
- Thermal cycling to validate performance under varying environmental conditions
- Mechanical endurance testing for moving parts or wearable components
- Software validation including boundary condition testing and failure mode analysis
Clinical Validation Study Design
Clinical validation provides the most compelling evidence of device effectiveness and is often required for moderate and high-risk devices. The optimal study design depends on device intended use, target population, and available comparator methods.
Table 4: Clinical Study Designs for Biophotonic Device Validation
| Study Design | Key Characteristics | Applicable Device Types | Endpoints |
|---|---|---|---|
| Prospective Cohort | Compares outcomes between users and non-users of the technology | Diagnostic, monitoring devices | Sensitivity, specificity, accuracy |
| Randomized Controlled Trial | Participants randomly assigned to intervention or control groups | Therapeutic, surgical devices | Primary efficacy, safety endpoints |
| Paired Comparison | Each participant receives both experimental and reference tests | Diagnostic imaging devices | Agreement statistics, ROC analysis |
| Single-Arm Study | All participants receive the experimental intervention | Breakthrough devices with historical controls | Objective performance criteria |
Navigating the Regulatory Submission Process
Strategic Regulatory Planning
Early and strategic regulatory planning significantly improves the efficiency and success of bringing biophotonic devices to market. The following workflow outlines key decision points in selecting an appropriate regulatory pathway based on device characteristics.
Diagram 2: Regulatory Pathway Decision Flow
Pre-Submission Engagement with FDA
The Q-Submission (Pre-Submission) Program allows developers to obtain FDA feedback on proposed regulatory strategies, clinical trial designs, and testing methodologies before formal submission [97]. This process is particularly valuable for novel biophotonic technologies where regulatory precedents may be limited.
Key Elements of Successful Pre-Submission:
- Clear Agenda: Focused list of specific questions for FDA review
- Comprehensive Background: Detailed device description, intended use, and technological features
- Proposed Approach: Specific protocols, study designs, or testing methodologies for discussion
- Supporting Data: Preliminary data justifying proposed approaches
Timeline Considerations: Pre-submission meetings should be scheduled 2-6 months before intended submission, with FDA providing written feedback approximately 21 days after the meeting [97].
Submission Preparation and Documentation
A complete regulatory submission for a biophotonic device must tell a compelling scientific story that demonstrates safety and effectiveness. Key elements include:
Administrative Elements:
- Appropriate coversheet clearly identifying submission type
- Device description including technological principles and intended use
- Proposed classification with justification
- Truthful and accurate statement disclosure
- User fee payment and form
Technical Documentation:
- Device Description: Detailed explanation of working principles, key components, and specifications
- Software Documentation: Architecture, design specifications, and verification/validation results
- Biocompatibility Evaluation: For devices contacting patients, following ISO 10993 series
- Electrical Safety and EMC: Compliance with IEC 60601-1 and IEC 60601-1-2
- Performance Testing: Comprehensive bench, preclinical, and clinical data
- Risk Management File: Following ISO 14971, identifying and mitigating potential hazards
Labeling and Instructions for Use:
- Clear, comprehensive instructions for intended users
- Limitations and contraindications explicitly stated
- Maintenance and quality control procedures
- Evidence supporting all claims and indications
Post-Market Considerations
Post-Market Surveillance
After a biophotonic device receives marketing authorization, manufacturers must implement robust post-market surveillance systems to monitor real-world performance and identify potential safety issues. The FDA may require post-market studies for certain devices to gather additional evidence about safety and effectiveness in broader populations [97].
Key components of post-market surveillance include:
- Complaint Handling System: Documenting and investigating user reports
- Adverse Event Reporting: Timely submission of mandatory reports to FDA
- Periodic Safety Updates: Comprehensive analysis of device performance
- Post-Market Clinical Follow-up: Prospective studies to answer specific safety questions
Real-World Performance Monitoring
For biophotonic devices, monitoring real-world performance provides opportunities to validate clinical utility and identify potential improvements. Key metrics include:
- Clinical Impact: How device use affects diagnostic or therapeutic decisions
- User Experience: Usability and workflow integration in clinical settings
- Long-term Reliability: Device performance over extended operational periods
- Comparative Effectiveness: Performance relative to alternative technologies
Navigating regulatory pathways for biophotonic devices requires strategic planning, robust scientific evidence, and understanding of FDA processes. The De Novo pathway and Breakthrough Devices Program offer efficient routes for novel technologies that address unmet clinical needs without existing predicates. Success depends on early regulatory engagement, comprehensive technical validation, and well-designed clinical studies that generate compelling evidence of safety and effectiveness.
As biophotonics continues to evolve with advancements in AI integration, miniaturization, and novel contrast mechanisms [1] [100], regulatory approaches will similarly adapt. Researchers and developers should monitor evolving FDA guidance, particularly regarding software as a medical device (SaMD), artificial intelligence/machine learning (AI/ML), and combination products. By integrating regulatory strategy into the development process from its earliest stages, innovators can accelerate the translation of promising biophotonic technologies from research laboratories to clinical practice, ultimately advancing patient care and diagnostic capabilities.
Biophotonics, the interdisciplinary field that leverages light-based technologies to analyze and manipulate biological materials, is increasingly recognized as a cornerstone of modern life sciences research and development (R&D) [1]. This discipline utilizes the properties of light and other forms of radiant energy to visualize, detect, and characterize biological materials at molecular, cellular, tissue, and organ levels [101]. The fundamental advantages of biophotonic techniques—including non-contact measurement, high speed and instant information delivery, exceptional sensitivity down to single-molecule detection, and excellent temporal resolution for observing dynamic biological processes—position them as transformative tools in both basic research and applied clinical settings [1]. Within pharmaceutical R&D and healthcare delivery, biophotonics provides powerful capabilities for understanding disease mechanisms, accelerating drug discovery, enabling precise diagnostics, and facilitating targeted therapies. The economic implications of these technological advantages are substantial, influencing R&D efficiency, clinical trial success rates, diagnostic accuracy, and therapeutic outcomes across the healthcare continuum.
Market Growth and Economic Trajectory of Biophotonics
The significant economic impact of biophotonics is reflected in its robust market growth, propelled by increasing adoption across medical and non-medical applications. Current market analyses project an impressive expansion trajectory, with varying estimates reflecting different segmentation methodologies but demonstrating consistent strong growth.
Table 1: Global Biophotonics Market Size and Growth Projections
| Source | 2024 Base Value (USD Billion) | 2030 Projection (USD Billion) | 2034 Projection (USD Billion) | CAGR (%) |
|---|---|---|---|---|
| BCC Research [70] [102] | 62.6 | 113.1 (by 2030) | - | 10.6 (2025-2030) |
| Precedence Research [69] | 83.33 | - | 226.18 | 10.5 (2025-2034) |
| Global Market Insights [3] | 76.1 | - | 220.1 | 11.3 (2025-2034) |
| Future Market Insights [2] | - | - | 189.3 (by 2035) | 10.9 (2025-2035) |
| IMARC Group [101] | 59.5 | - | 127.7 (by 2033) | 8.41 (2025-2033) |
This growth is primarily driven by the increasing prevalence of chronic diseases, rising demand for non-invasive diagnostics, continuous advances in optical technologies, expansion into non-medical applications, and the accelerating penetration of personalized medicine and precision healthcare [70] [69] [102]. The market exhibits distinct segmentation patterns, with medical diagnostics consistently dominating end-use applications due to the critical need for early and accurate disease detection [69] [100]. Technologically, the field is divided between in-vitro and in-vivo applications, each serving distinct roles with complementary economic value propositions.
Table 2: Biophotonics Market Analysis by Key Segments
| Segment Category | Dominant Segment | Key Statistics | Fastest-Growing Segment | Key Statistics |
|---|---|---|---|---|
| End-Use | Medical Diagnostics [69] | 66% market share (2024) [69] | Medical Therapeutics [3] | Projected to reach USD 83.7B by 2034 [3] |
| Technology | In-Vitro [69] | 59% market share (2024) [69]; 72% per BCC [100] | In-Vivo [69] | CAGR of 11% (2025-2034) [69] |
| Application | Spectromolecular [3] | USD 15.1B market value (2024) [3] | See-Through Imaging [69] [3] | CAGR of 13.7% (2025-2034) [3] |
Geographically, North America holds the largest market share (38%-52.8% in 2024), attributed to its advanced technical infrastructure, substantial R&D investments, and strong demand from healthcare and biotechnology sectors [69] [102] [100]. However, the Asia-Pacific region is anticipated to witness the most rapid growth, with countries like China and India exhibiting CAGRs exceeding 13% due to aggressive government initiatives, healthcare modernization, and expanding research capabilities [69] [3].
Key Biophotonic Technologies and Their Methodologies
The economic value and cost-effectiveness of biophotonics are realized through specific, advanced technologies that enhance R&D productivity and clinical outcomes. The following section details core methodologies, their experimental protocols, and their unique value propositions.
Raman Spectroscopy for Therapeutic Drug Monitoring
Experimental Protocol:
- Sample Collection & Preparation: Obtain biological samples (e.g., serum, plasma, urine) from patients undergoing pharmacotherapy. For antibiotics like vancomycin, collect samples at trough and peak concentrations.
- Substrate Preparation: Use appropriate substrates such as aluminum-coated glass slides or gold films for Surface-Enhanced Raman Spectroscopy (SERS) to enhance signal intensity.
- Sample Deposition: Apply a small volume (e.g., 1-10 µL) of the sample to the substrate and allow it to dry under controlled conditions.
- Instrumentation Setup: Utilize a Raman spectrometer system equipped with a laser source (e.g., 785 nm to minimize fluorescence background), a diffraction grating, and a high-sensitivity detector such as a CCD camera.
- Spectral Acquisition: Focus the laser beam on the sample. Acquire Raman spectra over a defined wavenumber range (e.g., 500-1800 cm⁻¹) with appropriate laser power and integration time to avoid sample degradation. Perform multiple acquisitions for statistical robustness.
- Data Preprocessing: Process raw spectra using algorithms for background subtraction, fluorescence correction, and normalization.
- Multivariate Analysis & Modeling: Employ machine learning techniques (e.g., principal component analysis, partial least squares regression) to build calibration models that correlate spectral features with drug concentrations. Validate the model using an independent sample set.
- Concentration Prediction: Apply the validated model to predict drug levels in unknown patient samples, enabling real-time dose adjustment [103].
The workflow for this application can be visualized as follows:
Figure 1: Raman Spectroscopy Workflow for Drug Monitoring
Near-Infrared II (NIR-II) Fluorescence Imaging for Surgical Oncology
Experimental Protocol:
- Contrast Agent Administration: Administer a targeted NIR-II fluorescent probe (e.g., IRDye 800CW, carbon nanotubes, or quantum dots) to the subject via intravenous injection. Probes can be conjugated with targeting ligands for specific tumor markers.
- Waiting Period: Allow sufficient time (typically 24-48 hours) for systemic circulation and specific binding to the target tumor tissue, followed by clearance from non-target tissues.
- Anesthesia and Preparation: Anesthetize the animal or prepare the human patient for surgery. Position the subject under the NIR-II imaging system.
- Imaging System Setup: Use a NIR-II fluorescence imaging system comprising:
- A NIR laser source (e.g., 808 nm or 980 nm).
- Appropriate excitation and emission filters.
- An InGaAs or other NIR-sensitive camera for deep-tissue signal detection.
- Intraoperative Imaging: Perform real-time imaging during the surgical procedure. Use the NIR-II signal to visualize the tumor location, margins, and any residual disease or metastatic lymph nodes.
- Image-Guided Resection: Surgically remove the primary tumor under the guidance of the NIR-II fluorescence visualization, aiming for complete resection with clear margins.
- Ex Vivo Validation: Image the resected tumor and the surgical cavity to confirm complete tumor removal. Perform histopathological analysis on the resected tissue as a gold standard validation.
- Data Analysis: Quantify tumor-to-background ratio (TBR) and signal-to-noise ratio (SNR) to assess imaging efficacy [3].
Optical Coherence Tomography (OCT) for Intracoronary Imaging
Experimental Protocol:
- Patient Preparation: Prepare the patient for coronary catheterization following standard clinical protocols.
- Catheter Insertion: Introduce an intravascular OCT catheter (e.g., a fiber-optic imaging probe) into the target coronary artery via a guiding catheter.
- Blood Clearance: Temporarily displace blood from the field of view by injecting a radiopaque contrast medium or saline flush through the guide catheter.
- Image Acquisition: Pull back the OCT catheter automatically at a defined speed (e.g., 20 mm/s) while the system emits near-infrared light and records the backscattered signals.
- Data Processing: Use interferometry to construct cross-sectional, high-resolution tomographic images of the vessel wall in real-time.
- Multimodal Integration: Co-register OCT data with complementary imaging modalities such as intravascular ultrasound (IVUS) for structural assessment and fluorescence lifetime imaging (FLIM) for biochemical plaque characterization.
- Plaque Analysis: Analyze OCT images to identify thin-cap fibroatheromas (TCFA), macrophage infiltration, intimal vasculature, and lipid core characteristics to assess plaque vulnerability.
- Therapeutic Guidance: Use the comprehensive imaging data to guide stent placement, optimize stent apposition, and assess treatment efficacy immediately post-intervention [103].
The Scientist's Toolkit: Key Research Reagent Solutions
The effective application of biophotonic technologies relies on a suite of specialized reagents and materials that enable specific and sensitive detection.
Table 3: Essential Research Reagents and Materials in Biophotonics
| Reagent/Material | Function in Biophotonics | Application Example |
|---|---|---|
| Gold Nanoparticles | Act as plasmonic nano-antennas to dramatically enhance fluorescence or Raman scattering signals via surface plasmon resonance. | Signal enhancement in Surface-Enhanced Raman Spectroscopy (SERS) for detecting low-abundance biomarkers [69]. |
| Targeted NIR-II Fluorescent Probes | Emit light in the second near-infrared window (1000-1700 nm) for deep-tissue imaging with high resolution and low background. | Real-time visualization of tumor margins and metastatic lymph nodes during cancer surgery [3]. |
| Quantum Dots | Semiconductor nanocrystals with size-tunable, bright, and photostable fluorescence properties. | Multiplexed cellular imaging and long-term tracking of biomolecules in drug discovery [3]. |
| Photomultiplier Tubes (PMTs) | Highly sensitive light detectors that amplify weak optical signals into measurable electrical currents. | Detection of low-level fluorescence and single-photon counting in advanced microscopy and flow cytometry [2]. |
| Specific Raman Reporters | Molecules with distinct Raman vibrational fingerprints used to label and track specific biological targets. | Therapeutic drug monitoring by detecting spectral shifts associated with drug-target interactions [103]. |
Cost-Effectiveness and Return on Investment Analysis
The implementation of biophotonic technologies generates substantial ROI through multiple channels, including accelerated R&D cycles, improved diagnostic accuracy, and enhanced therapeutic outcomes.
ROI in Pharmaceutical R&D and Clinical Trials
Biophotonics streamlines drug discovery and development, a process notoriously known for high costs and high failure rates. The integration of AI with techniques like Raman spectroscopy has demonstrated the potential to detect diseases such as breast cancer with up to 98% accuracy in research settings, enabling more reliable go/no-go decisions in early-stage development [3]. The non-destructive nature of techniques like Raman imaging allows for continuous monitoring of the same cell population or tissue sample over time, reducing the number of samples and animals required in preclinical studies and generating richer data from each experiment [2]. Furthermore, the ability to conduct molecular-level diagnostics and monitor therapeutic responses in real-time facilitates more precise patient stratification for clinical trials, increasing the likelihood of trial success and reducing the time and cost associated with drug development.
ROI in Clinical Diagnostics and Therapeutics
In clinical practice, biophotonics contributes to significant cost savings and improved patient outcomes by enabling minimally invasive procedures and enhancing diagnostic precision. For instance, the adoption of confocal endomicroscopy systems at the University Medical Center Hamburg-Eppendorf led to a 23% reduction in biopsy procedures in gastrointestinal diagnostics within six months, directly lowering procedural costs and associated complications [2]. The use of NIR-II imaging in oncology surgeries improves the completeness of tumor resections, which can reduce recurrence rates and the need for follow-up surgeries, thereby lowering long-term treatment costs and improving patient survival [3]. The shift towards non-invasive diagnostics reduces hospital stay durations and the use of more expensive and risky invasive procedures, contributing to overall healthcare cost containment.
Economic Value Chain and Strategic Impact
The full economic impact of biophotonics extends beyond direct cost savings, creating value across the healthcare ecosystem. The following diagram illustrates this integrated value chain:
Figure 2: Biophotonics Economic Value Chain
The high initial capital investment required for biophotonic equipment remains a challenge, particularly for smaller institutions and in developing regions [2] [3]. However, the long-term benefits—including the expansion into point-of-care and home-based monitoring devices—promise to democratize access and further improve ROI by shifting diagnostics from centralized labs to more cost-effective settings [3]. Strategic partnerships between academia, industry, and governments are crucial to sharing development costs, accelerating innovation, and maximizing the economic and clinical return on biophotonics investments [3].
Biophotonics represents a paradigm shift in life sciences R&D and clinical practice, offering a powerful combination of technological sophistication and demonstrable economic value. The field's robust market growth, driven by the demand for non-invasive, precise, and real-time analytical capabilities, underscores its fundamental role in the future of healthcare and pharmaceutical development. While challenges related to cost and accessibility persist, the continuous technological advancements, strategic collaborations, and clear evidence of improved patient outcomes and reduced healthcare costs present a compelling case for investment. As biophotonics continues to converge with AI, nanotechnology, and personalized medicine, its role as a critical enabler of cost-effective, high-return innovation in life sciences is set to expand, solidifying its position as an indispensable tool for researchers, clinicians, and drug development professionals worldwide.
Global Initiatives and Funding Landscape for Biophotonics Research
Biophotonics is an interdisciplinary field that represents the fusion of light-based technologies (photonics) with biology and medicine [1]. The term itself, derived from the Greek words "bios" (life) and "phos" (light), reflects its core focus: exploring how light interacts with biological matter [1]. This field leverages the fundamental properties of photons to image, detect, and manipulate biological materials at various scales—from single molecules and cells to tissues and entire organisms [11]. The scope of biophotonics research encompasses fundamental investigations of cellular processes, health-related applications in diagnostics and therapy, and extensions into environmental monitoring, food safety, and agriculture [1].
The significant advantage of biophotonic techniques lies in their non-contact, non-invasive nature, which allows researchers to observe living systems with minimal disruption to biological integrity [1]. Furthermore, optical measurements provide rapid, real-time data with exceptional sensitivity—in some cases, down to single-molecule detection [1]. These capabilities make biophotonics a cornerstone of 21st-century life sciences and a critical enabler of precision medicine. The field continues to evolve, embracing emerging technologies such as artificial intelligence, nanotechnology, and quantum optics to push the boundaries of what is possible in biological research and medical applications [1] [104].
Global Funding Landscape and Market Outlook
The global commitment to biophotonics research and development is reflected in substantial market growth projections and significant funding allocations across governmental and private sectors. The table below summarizes key market projections and regional initiatives that illustrate this landscape.
Table 1: Global Biophotonics Market Size and Growth Projections
| Region/Global | Market Size (Year) | Projected Market Size (Year) | CAGR | Key Funding/Initiatives |
|---|---|---|---|---|
| Global | $62.6 billion (2024) [70] | $113.1 billion (2030) [70] | 10.6% (2025-2030) [70] | |
| Global | $92.09 billion (2025) [69] | $226.18 billion (2034) [69] | 10.5% (2025-2034) [69] | |
| United States | ~$5.8 billion (2028) [105] | 8.2% (2023-2028) [105] | National Science Foundation Biophotonics Program [104]; FDA approvals for clinical imaging devices [2] | |
| Germany | €38 million national biophotonics innovation initiative (2024) [2] | |||
| South Korea | ~$2.0 billion (2028) [105] | 9.0% [105] | Government funding programs for biotech innovation [105] | |
| Brazil | ~$1.2 billion (2028) [105] | 7.5% [105] | Government initiatives for biomedical research [105] | |
| Turkey | ~$0.8 billion (2028) [105] | 7.8% [105] | Healthcare modernization initiatives [105] |
Table 2: Selected National and Regional Biophotonics Initiatives
| Country/Region | Initiative/Funding Body | Focus Areas | Recent Funding Examples |
|---|---|---|---|
| United States | National Science Foundation (NSF) Biophotonics Program | "Photonics principles, engineering and technology relevant for critical problems in medicine, biology and biotechnology" [104] | FY2020 Congressional budget allocations for biophotonics in gene therapy, immunotherapy, and Alzheimer's research [69] |
| Germany | Federal Ministry of Education and Research | Early diagnostic infrastructure [2] | €38 million national innovation initiative (2024) [2] |
| European Union | International Collaborations | Multi-disciplinary research across physics, engineering, biology, and medicine [1] | Support for initiatives like the International Congress on Biophotonics [1] |
| Japan | Corporate R&D Investment | Photon detection for cancer research [2] | Hamamatsu Photonics development of photomultiplier tubes for national cancer research centers [2] |
| Asia-Pacific | Market-Led Expansion | Clinical diagnostics and therapeutics [69] | Projected fastest growing region (13.54% CAGR) [69] |
The market growth is primarily driven by increasing demand for non-invasive diagnostics, the rising global prevalence of chronic diseases, an aging population, and ongoing technological innovations [70] [69]. The integration of artificial intelligence with biophotonic systems is creating new opportunities for enhanced diagnostic accuracy and automated analysis [69] [104]. North America currently dominates the market share, but the Asia-Pacific region is projected to experience the fastest growth, fueled by expanding healthcare infrastructure, government support, and increasing technological adoption [69] [105].
Key Research Areas and Methodologies
Biophotonics research can be broadly categorized into three interconnected areas: bioimaging, biosensing, and photonic-based therapies [1]. Each area employs distinct but often complementary methodological approaches.
Bioimaging Techniques and Protocols
Bioimaging enables the characterization of biological specimens across multiple spatial scales, from nanoscopic intracellular interactions to macroscopic tissue structures [1]. Key techniques include:
Optical Coherence Tomography (OCT) OCT is a label-free imaging technique that provides high-resolution, cross-sectional images of biological tissues by measuring backscattered light [1]. It is analogous to ultrasound, using light instead of sound waves [11].
Experimental Protocol for OCT Imaging:
- Sample Preparation: Tissue samples can be imaged in vivo or ex vivo. For in vivo human imaging, no specific preparation is typically needed beyond proper positioning.
- System Calibration: Calibrate the OCT system using a reference mirror to optimize interference signal strength.
- Image Acquisition: Direct the low-coherence near-infrared light source toward the sample. Interference patterns between light reflected from the sample and reference arm are detected by a spectrometer.
- Signal Processing: Process interferometric data using Fourier transformation to reconstruct depth-resolved reflectivity profiles (A-scans).
- Image Reconstruction: Combine multiple A-scans acquired while scanning the beam across the sample to create 2D cross-sectional images (B-scans) or 3D volumetric data.
- Analysis: Analyze morphological features in the reconstructed images. Extension to spectroscopic OCT (SOCT) can provide additional molecular contrast by analyzing wavelength-dependent backscattering [1].
Multiphoton Microscopy This technique utilizes the simultaneous absorption of two or more photons of longer wavelength (typically near-infrared) to excite fluorophores, enabling high-resolution imaging deep within scattering tissues [1].
Experimental Protocol for Multiphoton Imaging:
- Sample Preparation: Label samples with fluorescent markers or utilize endogenous fluorophores. Tissue can be live, fixed, or in thick sections.
- System Setup: Employ a mode-locked Ti:Sapphire laser producing femtosecond pulses for high peak intensity with low average power.
- Excitation: Focus excitation light through high-numerical-aperture objectives. Multiphoton absorption occurs only at the focal volume, providing inherent optical sectioning.
- Detection: Collect emitted fluorescence using non-descanned detectors in epi-configuration for improved signal collection from scattering samples.
- Image Acquisition: Scan the laser beam across the sample and collect emitted photons point-by-point to construct high-resolution images.
- Advanced Applications: Combine with fluorescence lifetime imaging (FLIM) or second harmonic generation (SHG) for additional functional and structural information [1].
Biosensing Methodologies
Biosensing applications leverage optical phenomena for sensitive detection of biomolecules, pathogens, and chemical substances [1]. Key methodologies include:
Surface Plasmon Resonance (SPR) Biosensing SPR detects changes in refractive index at a metal-dielectric interface, enabling label-free monitoring of biomolecular interactions in real-time.
Experimental Protocol for SPR Biosensing:
- Sensor Chip Functionalization: Coat a gold film with a self-assembled monolayer and immobilize capture molecules (e.g., antibodies, receptors).
- System Priming: Prime the SPR system with running buffer to establish a stable baseline.
- Sample Introduction: Inject analyte solutions over the functionalized surface at controlled flow rates.
- Binding Measurement: Monitor the change in resonance angle (or wavelength) as analytes bind to capture molecules.
- Regeneration: Remove bound analytes using regeneration solutions to prepare the surface for subsequent measurements.
- Data Analysis: Determine binding kinetics (association/dissociation rates) and affinity constants from the sensorgram data [2].
Raman Spectroscopy This technique probes molecular vibrations based on inelastic scattering of light, providing detailed chemical fingerprints of samples.
Experimental Protocol for Raman Spectroscopy:
- Sample Preparation: Minimal preparation required. Samples can be solid, liquid, or tissue sections. Avoid fluorescent contaminants that can overwhelm weak Raman signals.
- System Alignment: Calibrate the spectrometer using a silicon reference for wavelength accuracy.
- Laser Excitation: Illuminate the sample with a monochromatic laser source (typically visible or near-infrared).
- Light Collection: Collect inelastically scattered light while filtering out the dominant Rayleigh scattered component.
- Spectral Acquisition: Disperse collected light onto a CCD detector to acquire Raman spectra.
- Data Processing: Pre-process spectra (cosmic ray removal, background subtraction, normalization) before multivariate analysis for sample classification [1] [2].
Coherent Raman techniques like SRS and CARS enhance the weak Raman signal through nonlinear optical processes, enabling rapid, label-free chemical imaging of biological samples [1].
Photonic Therapeutic Approaches
Light-based therapies utilize photochemical, photothermal, or photomechanical mechanisms to treat diseases [11].
Photodynamic Therapy (PDT) Protocol
- Photosensitizer Administration: Administer photosensitizing agent systemically or topically with appropriate incubation time for target tissue accumulation.
- Light Application: Illuminate the target area with light of specific wavelength matching the photosensitizer's absorption peak.
- Oxygen Activation: The excited photosensitizer transfers energy to molecular oxygen, generating reactive oxygen species that induce cellular damage.
- Treatment Monitoring: Use imaging techniques to monitor treatment efficacy and potential side effects [11] [104].
Photobiostimulation Protocol
- Parameter Selection: Determine appropriate light parameters (wavelength, intensity, exposure time) based on target tissue and desired outcome.
- Light Delivery: Apply low-intensity laser or LED light directly to the target area.
- Treatment Regimen: Implement repeated sessions as needed based on therapeutic response [11].
Visualization of Biophotonics Research Workflows
The following diagrams illustrate key experimental workflows and logical relationships in biophotonics research.
Diagram 1: Bioimaging Workflow
Diagram 2: Biosensing Workflow
Essential Research Reagents and Materials
Successful biophotonics research requires specialized reagents and materials. The following table details key components of the "biophotonics toolkit."
Table 3: Essential Research Reagent Solutions for Biophotonics
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Fluorescent Probes & Dyes | Labeling specific cellular structures or molecules for visualization | Alexa Fluor series, GFP and variants; selected based on excitation/emission spectra matching available light sources [11] |
| Nanoparticles | Enhance contrast, enable sensing, or facilitate therapy | Gold nanoparticles (for photothermal therapy, SPR enhancement), quantum dots (bright fluorescence), upconversion nanoparticles (NIR imaging) [69] [2] |
| Antibodies & Biorecognition Elements | Target-specific molecular recognition for biosensing and imaging | Primary and secondary antibodies with optical labels; aptamers, affibodies for specific biomarker detection [11] |
| Photosensitizers | Light-activated generation of reactive oxygen species for therapy | Porphyrin-based compounds (Photofrin), chlorophyll derivatives (Foscan) with appropriate absorption characteristics [11] [104] |
| Optical Materials & Substrates | Fabrication of sensors, waveguides, and imaging components | Specialty glasses (high transmission), plasmonic metals (gold, silver), photonic crystals, optical fibers [1] [2] |
| Cell Culture Reagents | Maintain biological samples for in vitro studies | Cell lines, growth media, buffers, matrix proteins for cell adhesion in live-cell imaging studies [106] |
| Tissue Phantoms | Calibrate and validate imaging systems | Synthetic materials with controlled optical properties (scattering, absorption) mimicking biological tissues [107] |
Future Perspectives and Strategic Recommendations
The future of biophotonics research will be shaped by several converging technological trends and emerging challenges. Key areas for strategic development include:
Integration with Artificial Intelligence: Machine learning algorithms are increasingly being applied to enhance image analysis, automate feature detection, and interpret complex spectral data [1] [104]. Future research should focus on developing AI-powered biophotonic systems that can provide real-time diagnostic feedback and predictive analytics during procedures.
Miniaturization and Point-of-Care Applications: The development of compact, portable, and cost-effective biophotonic devices is essential for expanding access to advanced diagnostics in resource-limited settings [104]. Research initiatives should prioritize wearable biosensors, handheld imagers, and lab-on-a-chip platforms that can deliver clinical-grade performance outside traditional laboratory environments.
Advanced Materials and Probes: Next-generation biophotonics will benefit from novel materials with enhanced optical properties, including metamaterials, 2D materials, and multifunctional nanoparticles [1] [104]. Investment in probe development should focus on materials with improved brightness, photostability, and targeting specificity.
Multimodal Integration: Combining multiple biophotonic techniques with complementary imaging modalities (MRI, CT, ultrasound) can provide comprehensive structural, functional, and molecular information [1]. Research should focus on developing integrated platforms that seamlessly combine these capabilities for improved diagnostic accuracy.
Standardization and Clinical Translation: Overcoming barriers to clinical adoption requires standardized protocols, validated biomarkers, and demonstrated cost-effectiveness [1] [104]. Future initiatives should prioritize large-scale clinical validation studies and the development of regulatory pathways for biophotonic technologies.
Interdisciplinary Collaboration: The complexity of biophotonics research necessitates collaboration across traditional disciplinary boundaries [1] [106]. Funding agencies should promote integrated teams comprising physicists, engineers, biologists, clinicians, and data scientists to address complex biological and medical challenges.
In conclusion, the global initiatives and funding landscape for biophotonics research reflect the field's significant potential to transform healthcare, advance biological understanding, and address pressing societal challenges. Strategic investments in emerging technologies, interdisciplinary collaboration, and translational research will be essential for realizing the full potential of biophotonics in the coming decades.
Conclusion
Biophotonics stands as a cornerstone of next-generation biomedical science, seamlessly integrating with biology, AI, and nanotechnology to push the boundaries of what is possible in diagnostics and therapy. The field is poised for sustained growth, driven by the demand for non-invasive techniques and personalized medicine. Future progress hinges on overcoming commercialization challenges, fostering interdisciplinary collaboration, and continuing to innovate in areas like in-vivo imaging and intelligent biosensors. For researchers and drug development professionals, mastering biophotonics is no longer optional but essential for leading the future of precision health and therapeutic discovery.
References
- 1. Shining a Light on the Future of Biophotonics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245495/]
- 2. Biophotonics Market Demand & Growth Outlook 2025 to ... [https://www.futuremarketinsights.com/reports/global-biophotonics-market]
- 3. Biophotonics Market Size & Share Report, 2025 - 2034 [https://www.gminsights.com/industry-analysis/biophotonics-market]
- 4. Biophotonics - Latest research and news [https://www.nature.com/subjects/biophotonics]
- 5. Guidelines for the use of flow cytometry and cell sorting in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9165548/]
- 6. Light scattering, absorption, and reflection in biological media [https://fiveable.me/biophotonics/unit-2/light-scattering-absorption-reflection-biological-media/study-guide/ccOYo5Uf4iTMdTtE]
- 7. Optical Characterization of Biological Tissues Based on ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9689259/]
- 8. Tutorial on methods for estimation of optical absorption and ... [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-29/issue-6/060801/Tutorial-on-methods-for-estimation-of-optical-absorption-and-scattering/10.1117/1.JBO.29.6.060801.full]
- 9. Tissue Interactions and Biological Effects | Lasers in Dentistry [https://www.dentalcare.com/en-us/ce-courses/ce394/tissue-interactions-and-biological-effects]
- 10. Noninvasive biophotonic imaging for studies of infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3084502/]
- 11. Biomedical Applications of Biophotonics [https://www.news-medical.net/life-sciences/Biomedical-Applications-of-Biophotonics.aspx]
- 12. Detecting diseases in breath with biophotonics [https://www.aip.org/scilights/detecting-diseases-in-breath-with-biophotonics]
- 13. Biophotonic probes for bio-detection and imaging | Light [https://www.nature.com/articles/s41377-021-00561-2]
- 14. Lasers for Biophotonics & Microscopy [https://www.toptica.com/applications/biophotonics]
- 15. Lasers vs. Light Emitting Diodes (LEDs) vs.… [https://dayyphotonics.com/knowledgebase/lasers-vs-light-emitting-diodes-leds-vs-superluminescent-diodes-sleds]
- 16. Difference Between an Superluminescent Diodes (SLD) ... [https://www.inphenix.com/difference-between-sld-ld-and-led/]
- 17. Applications of the Superluminescent Diode (SLD) [https://www.inphenix.com/applications-of-the-superluminescent-diode-sld/]
- 18. Light-emitting Diodes: A Brief Review and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4479368/]
- 19. Light-emitting diodes—Their potential in biomedical ... [https://www.sciencedirect.com/science/article/abs/pii/S1364032110000547]
- 20. Biophotonics: Strategic Market and Tech Overview [https://www.bccresearch.com/pressroom/pho/biophotonics-market-was-valued-at-$626-billion-in-2024?srsltid=AfmBOoqw5nBSrHdaprFWxHJ9BB-KSCxRFWYHhx4DSWXTuQsYrH_TW1BO]
- 21. Biophotonics Research | Biophotonics Research Awards ... [https://biophotonicsresearch.com/]
- 22. Applications of bioluminescence in biotechnology and beyond [https://pubs.rsc.org/en/content/articlehtml/2021/cs/d0cs01492c]
- 23. A Comprehensive Exploration of Bioluminescence Systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10861286/]
- 24. Development and Applications of Bioluminescent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6565457/]
- 25. Bioluminescence vs. Fluorescence: Choosing the Right ... [https://www.promegaconnections.com/bioluminescence-fluorescence-choosing-the-right-assay-for-your-experiment/]
- 26. Bio-optimized energy transfer in densely packed ... [https://www.nature.com/articles/ncomms6722]
- 27. Optofluidic Bio-Lasers: Concept and Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4162132/]
- 28. Biointegrated microlasers: technologies, applications, and ... [https://opg.optica.org/optica/abstract.cfm?uri=optica-12-8-1311]
- 29. Inspired by nature: Bioluminescent systems for bioimaging ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914024012001]
- 30. Biophotonics: the big picture [https://www.spiedigitallibrary.org/journals/Journal-of-Biomedical-Optics/volume-23/issue-2/021103/Biophotonics-the-big-picture/10.1117/1.JBO.23.2.021103.full]
- 31. Optical Coherence Tomography (OCT): Principle and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK554044/]
- 32. two-photon microscopy market size and share analysis [https://www.coherentmarketinsights.com/industry-reports/two-photon-microscopy-market]
- 33. Optical Coherence Tomography: An Emerging Technology for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1531864/]
- 34. Optical Coherence Tomography [https://eyewiki.org/Optical_Coherence_Tomography]
- 35. Molecular Imaging Optical Coherence Tomography [https://robleslab.gatech.edu/absorption/]
- 36. Exploring Fourier Transform Infrared (FTIR) spectroscopy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11182784/]
- 37. From in-vitro biofluid assays to in-vivo cancer detection [https://www.sciencedirect.com/science/article/pii/S0169409X15000447]
- 38. Translational biophotonics with Raman imaging: clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8543123/]
- 39. Advances in Raman spectroscopy and imaging for ... [https://opg.optica.org/aop/abstract.cfm?uri=aop-15-2-318]
- 40. Biophotonics: Strategic Market and Tech Overview [https://www.bccresearch.com/pressroom/pho/biophotonics-market-was-valued-at-$626-billion-in-2024?srsltid=AfmBOooM68Pi6XbBzGx6moJ2kifICwpZxeKs6RUoXdYJsGRQ0iH7pdP-]
- 41. Biophotonics Technology and Global Markets Report [https://www.globenewswire.com/news-release/2025/06/03/3092930/28124/en/Biophotonics-Technology-and-Global-Markets-Report-2025-2030-Expansion-into-Non-Medical-Applications-and-Increasing-Penetration-of-Personalized-Medicine-and-Precision-Healthcare.html]
- 42. Biophotonics & lasers in medical technology [https://world-of-photonics.com/en/trade-fair/topics/biophotonics-medical-engineering/]
- 43. Advancements in surface plasmon resonance sensors for real ... [https://pubs.rsc.org/en/content/articlehtml/2025/tc/d4tc04890c]
- 44. Recent Advances in Fluorescence Resonance Energy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025574/]
- 45. Recent advances of surface plasmon resonance sensors ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914025004989]
- 46. Technical Note 102: SPR Sensitivity and Detection Limit [https://biosensingusa.com/technical-notes/technical-note-102-spr-sensitivity-detection-limit/]
- 47. An ultra-sensitive surface plasmon resonance biosensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11471480/]
- 48. Application of fluorescence resonance energy transfer in ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525004424]
- 49. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 50. Cancer Photodynamic Therapy Market Report 2025 [https://finance.yahoo.com/news/cancer-photodynamic-therapy-market-report-104900556.html]
- 51. Avenues for integrating photothermal therapy in cancer clinic [https://www.nature.com/articles/s42004-025-01705-w]
- 52. Emerging photothermal agents combined with immunotherapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540227/]
- 53. Nanocarbon dots enhancing photothermal therapy for cancer [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d5tb01971k]
- 54. Optical tweezers - Block lab [https://blocklab.stanford.edu/optical_tweezers.html]
- 55. Optical tweezers [https://www.lumicks.com/documentation/optical-tweezers]
- 56. Optical tweezers in single-molecule biophysics [https://www.nature.com/articles/s43586-021-00021-6]
- 57. Laser Scalpel - Advanced Surgical Tool for Precise ... [https://emla.info/laser-scalpel/]
- 58. Flexible fiberbotic laser scalpels: Material and fabrication ... [https://www.sciencedirect.com/science/article/pii/S2590238524000079]
- 59. Nano bio-robots: a new frontier in targeted therapeutic ... [https://www.frontiersin.org/journals/robotics-and-ai/articles/10.3389/frobt.2025.1639445/full]
- 60. Biophotonics and nanorobotics for biomedical imaging ... [https://www.sciencedirect.com/science/article/abs/pii/S1389556724000285]
- 61. Micro/Nanorobots for Biomedicine: Delivery, Surgery, Sensing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6759331/]
- 62. Nanorobots Decade Long Trends, Analysis and Forecast ... [https://www.archivemarketresearch.com/reports/nanorobots-137992]
- 63. Nanoparticle Blueprints Reveal Path to Smarter Medicines [https://www.bnl.gov/newsroom/news.php?a=222716]
- 64. Advances in Nanotechnology-Based Drug Delivery Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389492/]
- 65. Absorption, Thermal Relaxation Time, and Beam ... [https://www.mdpi.com/2304-6767/13/9/397]
- 66. Shortwave infrared spatial frequency domain imaging for ... [https://www.frontiersin.org/journals/photonics/articles/10.3389/fphot.2025.1546952/full]
- 67. Deep tissue photoacoustic imaging with light and sound [https://www.nature.com/articles/s44303-024-00048-w]
- 68. Biophotonics | Samueli School of Engineering at UC Irvine [https://engineering.uci.edu/dept/bme/research/biophotonics]
- 69. Biophotonics Market Size to Hit USD 226.18 Billion by 2034 [https://www.precedenceresearch.com/biophotonics-market]
- 70. Biophotonics Technology and Global Markets Report 2025 ... [https://finance.yahoo.com/news/biophotonics-technology-global-markets-report-140500495.html]
- 71. Exploring Barriers in Biophotonics Market: Trends and Analysis ... [https://www.marketreportanalytics.com/reports/biophotonics-310713]
- 72. Biophotonics: Lighting the Future of Life Sciences [https://blog.bccresearch.com/biophotonics-lighting-the-future-of-life-sciences]
- 73. Biophotonics Technology Market Expansion Strategies by ... [https://www.linkedin.com/pulse/biophotonics-technology-market-expansion-eortf/]
- 74. AI‑driven photonic noses: from conventional sensors to ... [https://www.nature.com/articles/s41378-025-01058-3]
- 75. Machine learning in biophotonics: progress and challenges [https://www.spiedigitallibrary.org/conference-proceedings-of-spie/12446/1244614/Machine-learning-in-biophotonics-progress-and-challenges/10.1117/12.2662811.short]
- 76. Artificial intelligence and machine learning in biophotonics [https://fiveable.me/biophotonics/unit-12/artificial-intelligence-machine-learning-biophotonics/study-guide/yq42DxRPh4ZZDCiD]
- 77. Optical microscopy combined with AI could enable new ... [https://spie.org/news/optical-microscopy-combined-with-ai-could-enable-new-avenues-in-precision-medicine]
- 78. Quantum Dots for Biophotonics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3418930/]
- 79. Quantum dot-infused nanocomposites - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr00440c?page=search]
- 80. Nanoparticles and quantum dots as emerging optical ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854524006775]
- 81. Biophotonics: Strategic Market and Tech Overview [https://www.bccresearch.com/pressroom/pho/biophotonics-market-was-valued-at-$626-billion-in-2024?srsltid=AfmBOooJ4xOrrSTqgYfJ7SEjd3Cd5K5E1GRwWAqUD9D_r8y8jBAHaBF-]
- 82. Medical Device Manufacturing and Biocompatible Materials [https://sybridge.com/biocompatible-materials-medical-device-design-manufacturing/]
- 83. The “Big Three” in biocompatibility testing of medical devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800850/]
- 84. Biophotonics techniques for structural and functional ... [https://pmc.ncbi.nlm.nih.gov/articles/mid/NIHMS611949/]
- 85. Biosensors for Medical Wearables Analysis 2025 and ... [https://www.archivemarketresearch.com/reports/biosensors-for-medical-wearables-301528]
- 86. Biophotonics: Strategic Market and Tech Overview [https://www.bccresearch.com/pressroom/pho/biophotonics-market-was-valued-at-$626-billion-in-2024?srsltid=AfmBOooms9grq9WcBd3-jKlkEYx9nYB5kklmIzMViG1JG-51rhviucYA]
- 87. Biophotonics: Strategic Market and Tech Overview [https://www.bccresearch.com/pressroom/pho/biophotonics-market-was-valued-at-$626-billion-in-2024?srsltid=AfmBOortLluN40MrMGEcMQcWpduEPSsc3xN3C7wMGs9gOOKZfblDbnXI]
- 88. Next Generation Biophotonics Technologies for Clinical ... [https://ui.adsabs.harvard.edu/abs/2025LPRv...19E1612F/abstract]
- 89. Clinical and Translational Neurophotonics 2025 [https://spie.org/Publications/Proceedings/Volume/13302]
- 90. Biophotonics: Strategic Market and Tech Overview [https://www.bccresearch.com/pressroom/pho/biophotonics-market-was-valued-at-$626-billion-in-2024?srsltid=AfmBOoqyqHzdA_uZmQk3jXTb2BMGdyvb4Wh36zlqp-jSh6iQcPiTiyLp]
- 91. Biophotonics Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/biophotonics-market]
- 92. Biophotonics Market Size, Share, Growth | Trends Report ... [https://www.fortunebusinessinsights.com/biophotonics-market-110387]
- 93. Biophotonics: Strategic Market and Tech Overview [https://www.bccresearch.com/pressroom/pho/biophotonics-market-was-valued-at-$626-billion-in-2024?srsltid=AfmBOooQZAZfGKPGQPXTrZcB9FZBDhHjcu1DgIeDFMPbdD77qTWiwxx_]
- 94. What are the 2025 Trends in Diagnostics? [https://www.hartmannyoung.com/resources/blog/what-are-the-2025-trends-in-diagnostics-/]
- 95. Bio-Optics: Design and Applications (BODA) [https://www.optica.org/events/meeting_archives/2025/bio-optics_design_and_application/]
- 96. Biophotonic (nano)structures: from fundamentals to ... [https://www.sciencedirect.com/org/science/article/pii/S2046206925019783]
- 97. FDA De Novo Pathway Explained: The Complete 2025 Guide [https://www.complizen.ai/post/de-novo-fda-pathway-complete-guide]
- 98. Regulatory landscape of accelerated approval pathways for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119601/]
- 99. Clinical and Translational Biophotonics (Translational) [https://www.optica.org/events/meeting_archives/2025/clinical_and_translational_biophotonics/]
- 100. Explore the Future of Light-Based Innovation in Healthcare ... [https://blog.bccresearch.com/explore-the-future-of-light-based-innovation-in-healthcare-and-beyond]
- 101. Global Biophotonics Market to Grow at 8.41% During 2025- ... [https://www.imarcgroup.com/global-biophotonics-market]
- 102. Biophotonics: Strategic Market and Tech Overview [https://www.bccresearch.com/pressroom/pho/biophotonics-market-was-valued-at-$626-billion-in-2024?srsltid=AfmBOoqvv95JuuYc0GGPxr93Q2xVdko3Cc--nuyO9efVnU-8XpBFao12]
- 103. BioPhotonics Conference 2025 - Photonics Media Events [https://events.photonics.com/Event.aspx?EID=40]
- 104. Grand Challenges and Opportunities in Biophotonics [https://www.frontiersin.org/journals/photonics/articles/10.3389/fphot.2021.719131/full]
- 105. Technology Market by Applications: United States Biophotonics [https://www.linkedin.com/pulse/biophotonics-technology-market-applications-united-states-tzhqf]
- 106. EXPERIMENTAL BIOPHOTONICS - Ceitec.cz [https://biophotonics.ceitec.cz/experimental-biophotonics/]
- 107. Extracting the Most Relevant Information from Bio-Photonic ... [https://www.preprints.org/manuscript/202411.2128]