Bio-Optics vs. Traditional Imaging: A Comparative Analysis for Biomedical Research and Drug Development
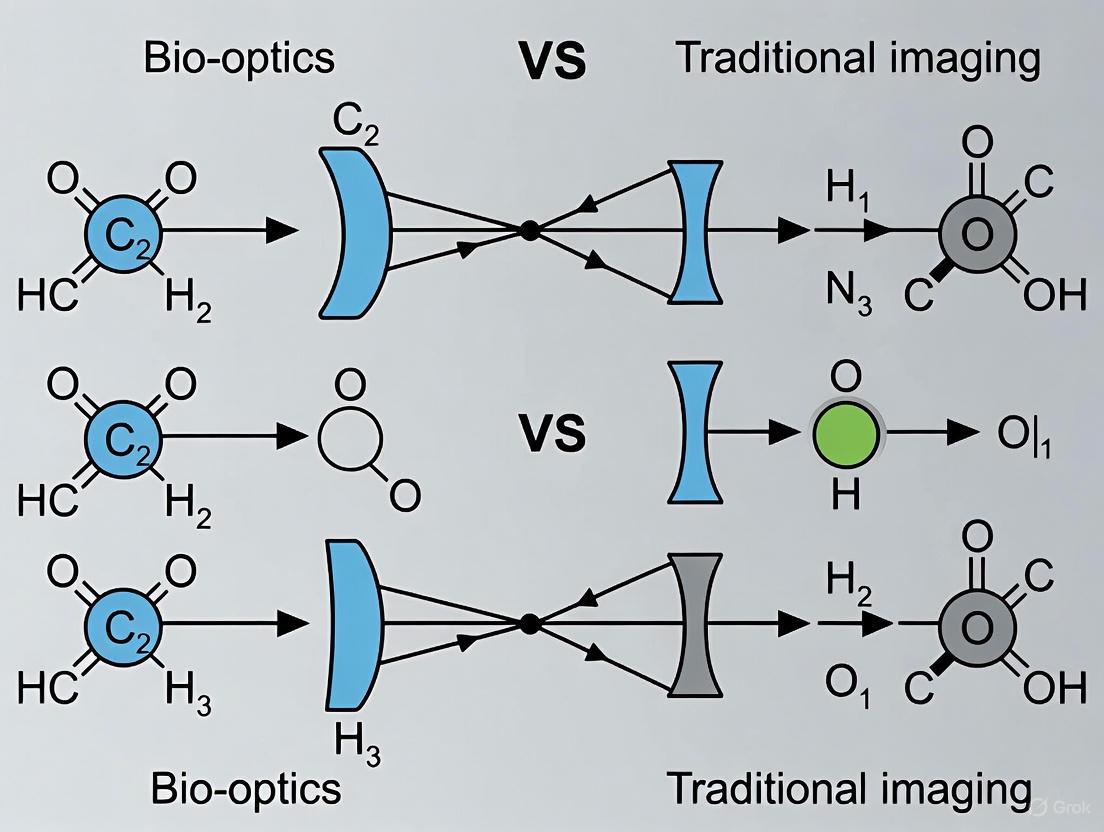
This article provides a comprehensive comparison between bio-optics—the convergence of light-based technologies with biology—and traditional imaging modalities for an audience of researchers, scientists, and drug development professionals.
Bio-Optics vs. Traditional Imaging: A Comparative Analysis for Biomedical Research and Drug Development
Abstract
This article provides a comprehensive comparison between bio-optics—the convergence of light-based technologies with biology—and traditional imaging modalities for an audience of researchers, scientists, and drug development professionals. It explores the foundational principles of bio-optics, including its core advantages of non-invasiveness, high sensitivity, and molecular specificity. The scope covers key methodological advancements such as super-resolution microscopy, photoacoustic imaging, and optical coherence tomography, alongside their applications in cancer diagnostics, neuroscience, and therapeutic monitoring. The analysis also addresses critical challenges related to standardization, data management, and clinical translation, culminating in a direct performance comparison with established techniques like MRI and CT. The synthesis aims to guide the strategic adoption of these transformative technologies in biomedical research and clinical practice.
The Principles of Bio-Optics: Unveiling the Power of Light in Biology
Bio-optics and biophotonics represent the interdisciplinary fusion of biological sciences with optical and photonic technologies. This convergence is transforming research, diagnostics, and therapy across life sciences and medicine. Biophotonics specifically denotes the combination of biology and photonics, where photonics is the science and technology of generation, manipulation, and detection of photons—the quantum units of light [1]. It can be described as the "development and application of optical techniques, particularly imaging, to the study of biological molecules, cells and tissue" [1]. The term encompasses all techniques dealing with the interaction between biological items—biomolecular, cells, tissues, organisms, and biomaterials—and photons, including their emission, detection, absorption, reflection, modification, and creation [1]. The field leverages the unique properties of light to analyze and manipulate biological materials, thereby offering new opportunities for precision measurements in fundamental and applied research, medical diagnostics, and treatment [2].
A key differentiation exists between applications that use light primarily to transfer energy, such as therapy and surgery, and those that use light to excite matter and transfer information back to the operator, such as diagnostics. The term biophotonics most frequently refers to the latter [1]. The field is recognized as a key technology of the 21st century, playing a crucial role in addressing significant societal challenges and driving advancements in life sciences, communication, and production [2]. The primary advantages of using light in biophotonics include its capability for non-contact measurement, which preserves the integrity of living cells; high speed providing real-time data; exceptional sensitivity down to single molecules; and excellent time resolution for observing dynamic biological processes across a wide range of temporal scales [2].
Core Technologies and Methodologies
The field of biophotonics can be divided into three main technological areas: bioimaging, biosensing, and photonic-based therapies. These areas often work in parallel, offering synergistic potential [2].
Key Biophotonic Imaging and Sensing Technologies
Table 1: Core Biophotonic Imaging and Sensing Technologies
| Technology | Core Principle | Primary Applications | Key Advantage |
|---|---|---|---|
| Optical Coherence Tomography (OCT) | Interferometry to measure backscattered light [2] | Ophthalmology, real-time 3D tissue imaging [1] [2] | High imaging speed; detailed tissue architecture [2] |
| Multi-Photon Microscopy | Simultaneous absorption of two/three photons for precise localization of fluorescence [2] | Deep tissue imaging with high spatial resolution [2] | Superior penetration depth and optical resolution [2] |
| Coherent Raman Scattering (CARS/SRS) | Nonlinear optical phenomena enhancing weak Raman signals [2] | Molecular-specific tissue imaging without autofluorescence [2] | High molecular selectivity and imaging speed [2] |
| Photoacoustic Imaging (PAI) | Combination of laser-induced ultrasound waves [2] | Deep tissue and vascular imaging [1] [2] | Superior deep tissue imaging of hemoglobin/oxygen saturation [1] |
| Fluorescence Lifetime Imaging (FLIM) | Measuring fluorescence decay times of endogenous fluorophores [2] | Tumor specificity, reducing non-specific signals [3] [2] | Provides biological insights beyond conventional fluorescence [3] |
| Optical Tweezers | Using light's momentum to exert forces on microscopic particles [1] | Manipulating atoms, DNA, bacteria, viruses, and nanoparticles [1] | Non-contact organizing, sorting, and tracking of cells [1] |
Photonic Therapeutic Modalities
Table 2: Core Photonic-Based Therapeutic Techniques
| Technique | Mechanism of Action | Applications | Benefits and Limitations |
|---|---|---|---|
| Photodynamic Therapy (PT) | Uses photosensitizing chemicals and oxygen to induce a cellular reaction to light [1] | Killing cancer cells, treating acne, reducing scarring, antimicrobial [1] | Minimal long-term side effects; limited to surfaces/organs exposed to light [1] |
| Photothermal Therapy | Uses nanoparticles to convert light (700-1000 nm) into heat, destroying surrounding cells [1] | Treating deep-seated cancers [1] | Can target deep tissues; few long-term side effects [1] |
| Low-Level Laser Therapy (LLLT) | Applying low-power lasers for tissue repair [1] | Reducing inflammation, chronic joint pain, potential for brain injuries [1] | Non-invasive; efficacy is sometimes controversial [1] |
| Laser Micro-Scalpel | Combining fluorescence microscopy with a femtosecond laser to excise single cells [1] | Delicate surgeries (e.g., eyes, vocal cords) [1] | Removes diseased cells without disturbing healthy surrounding cells [1] |
Biophotonics vs. Traditional Imaging Techniques
Biophotonic techniques offer distinct advantages over traditional medical imaging modalities, particularly in terms of resolution, molecular specificity, and the absence of ionizing radiation.
Comparative Analysis of Imaging Modalities
Table 3: Biophotonic Techniques vs. Traditional Imaging Modalities
| Imaging Technique | Physical Principle | Spatial Resolution | Penetration Depth | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| Multi-Photon Microscopy [2] | Non-linear absorption of NIR photons | Sub-micrometer | Up to ~1 mm in tissue | High resolution deep-tissue imaging, molecular specificity | Limited penetration compared to MRI/CT |
| Optical Coherence Tomography (OCT) [2] | Low-coherence interferometry | 1-10 µm | 1-2 mm in tissue | Real-time, high-speed cellular-level resolution | Limited to superficial tissues |
| Magnetic Resonance Imaging (MRI) [4] | Magnetic fields and radio waves | 10-100 µm (clinical) | Whole body | Excellent soft-tissue contrast, no ionizing radiation | Long scan times, high cost, incompatible with metal implants |
| Computed Tomography (CT) [4] | X-ray absorption | 50-200 µm (clinical) | Whole body | Rapid imaging, excellent for bones and lungs | Uses ionizing radiation, poor soft-tissue contrast |
| Ultrasound (US) [4] | Reflection of sound waves | 50-500 µm | Organ-specific | Real-time imaging, no radiation, portable | Operator-dependent, limited penetration in obese patients |
| Positron Emission Tomography (PET) [4] | Detection of gamma rays from radiopharmaceuticals | 1-2 mm (clinical) | Whole body | High sensitivity to metabolic activity | Poor spatial resolution, uses ionizing radiation |
A paradigm shift enabled by biophotonics is the move from static anatomical assessment to dynamic, functional, and molecular imaging. Techniques like hyperspectral imaging and FLIM provide molecular contrast by visualizing native electronic chromophores such as hemoglobin, NADP(H), and flavins [2]. This allows for the unraveling of disease mechanisms, enabling prevention, early diagnosis, and targeted or personalized treatment [2]. Furthermore, biophotonic techniques often provide label-free diagnostics, exploiting intrinsic optical properties of tissues without the need for exogenous dyes, which is a significant advantage for in vivo applications [2].
Detailed Experimental Protocols in Biophotonics
Protocol: Fluorescence-Guided Surgery with Nanobodies and FLIM
This protocol leverages the rapid pharmacokinetics of Nanobodies and the analytical power of Fluorescence Lifetime Imaging for precise tumor delineation [3].
Objective: To intraoperatively distinguish tumor margins from healthy tissue using targeted Nanobody agents and FLIM.
Materials:
- Targeted Nanobody: Fluorescently labeled single-domain antibody fragments for rapid, specific tumor targeting [3].
- FLIM-Capable Imaging System: A surgical microscope or endoscope equipped with time-resolved fluorescence detection capabilities [3].
- Excitation Laser: Pulsed laser source tuned to the fluorophore's excitation wavelength.
- Control Tracer: A non-specific fluorescent tracer for comparison.
Procedure:
- Tracer Administration: Systemically administer the fluorescently labeled Nanobody to the subject prior to or during surgery.
- Waiting Period: Allow a circulation time for the Nanobody to accumulate in the target tissue and clear from the bloodstream (typically rapid due to small size).
- Intraoperative Imaging:
- Excite the surgical field with the pulsed laser source.
- Acquire fluorescence intensity images using a standard camera to identify general fluorescent regions.
- FLIM Data Acquisition:
- For regions of interest identified in step 3, acquire time-resolved fluorescence data.
- Measure the fluorescence decay curve for each pixel in the image.
- Data Analysis:
- Fit the decay curves to extract the fluorescence lifetime (τ) at every pixel.
- Generate a false-color FLIM map where color represents the lifetime value.
- Tissue Discrimination:
- Correlate the lifetime values with tissue type. Specific molecular environments in tumor versus healthy tissue will result in distinct lifetime signatures, independent of tracer concentration.
- Use this FLIM map to guide the complete resection of tumor tissue while preserving healthy tissue.
Workflow Diagram: Nanobody FLIM for Surgical Guidance
Protocol: Stimulated Raman Scattering (SRS) Microscopy for Label-Free Histology
This protocol uses the nonlinear optical phenomenon of SRS to generate virtual histology images without tissue staining or processing [2].
Objective: To achieve label-free, molecular-specific imaging of fresh or processed tissue sections with high chemical contrast.
Materials:
- SRS Microscope: A system featuring two synchronized pulsed lasers (pump and Stokes) focused onto the sample.
- Photodetector: A high-sensitivity detector for measuring the intensity modulation of one of the beams.
- Lock-in Amplifier: To extract the weak SRS signal from the background.
- Tissue Sample: Fresh, frozen, or fixed tissue section (label-free).
Procedure:
- Laser Setup:
- Tune the frequency difference (ωpump - ωStokes) to match a specific molecular vibrational frequency (e.g., CH₂ stretch at ~2845 cm⁻¹ for lipids).
- Sample Preparation:
- Mount the tissue section on a standard microscope slide. No staining, dehydration, or coverslipping is strictly required.
- Beam Modulation and Overlap:
- Intensively overlap the pump and Stokes beams at the sample.
- Modulate the intensity of one beam (e.g., the Stokes beam) at a high frequency (MHz).
- Signal Detection:
- Detect the pump beam after it passes through the sample.
- The SRS effect will cause a slight intensity change of the pump beam at the modulation frequency.
- Use the lock-in amplifier to detect this minute intensity change, which is proportional to the concentration of the target molecule.
- Image Generation:
- Raster-scan the beams across the sample.
- Record the lock-in amplifier output at each pixel to construct the SRS image.
- Switch the laser frequencies to target different chemical bonds (e.g., from lipids to proteins) for multi-color chemical imaging.
Workflow Diagram: SRS Microscopy for Label-Free Imaging
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimentation in biophotonics relies on a suite of specialized reagents and optical components.
Table 4: Essential Research Reagents and Materials for Biophotonics
| Item | Function/Description | Example Application |
|---|---|---|
| Fluorescent Proteins (e.g., GFP, mCherry) [1] [5] | Genetically encodable, biocompatible gain media or biomarkers. | Biolasers [1], intracellular biosensing and tracking. |
| Indocyanine Green (ICG) [2] [6] | FDA-approved near-infrared fluorescent dye. | Fluorescence-guided surgery, photoacoustic imaging, assessing blood flow [6]. |
| Nanobodies [3] | Small, single-domain antibody fragments for rapid targeting. | Tumor-specific imaging agents in fluorescence-guided surgery [3]. |
| Noble Metal Nanoparticles (e.g., Gold Nanorods) [1] | Strong light absorbers and scatterers, convertible to heat. | Contrast agents for imaging, mediators for photothermal therapy [1]. |
| Biocompatible Gain Media [5] | Natural dyes (e.g., riboflavin) or proteins that amplify light. | Forming the active laser medium within biological environments (biolasers) [5]. |
| Femtosecond Pulsed Lasers [1] [2] | High-intensity, ultrashort pulsed light sources. | Pump source for multi-photon microscopy and laser micro-scalpels [1] [2]. |
| Optical Fibers [1] [7] | Flexible waveguides for light delivery and collection. | Endoscopic probes, light delivery deep within tissues for sensing or therapy [1]. |
| Spectrometers [7] | Instruments for measuring wavelength and intensity of light. | Analysis of fluorescence and absorption spectra from samples [7]. |
Future Directions and Enabling Technologies
The future of biophotonics is being shaped by several key enabling technologies. Artificial Intelligence (AI) and Machine Learning (ML) are playing an increasingly transformative role by enhancing data analysis, interpretation, and optimization of complex imaging and sensing [3] [2]. AI is being leveraged for tasks ranging from image reconstruction and interpretation to optical design itself [3]. However, the "black box" nature of some complex AI models poses challenges for transparency and explainability in medical decision-making, an issue being addressed by emerging regulations like the European Union's AI Act [8].
Novel Materials, particularly biophotonic probes derived from biological entities like viruses and cells, are being developed to create seamless interfaces between optical and biological worlds [5]. These probes offer high biocompatibility, biodegradability, and the unique ability to serve simultaneously as optical devices and diagnostic specimens [5]. Furthermore, Quantum Biophotonics is an emerging frontier, with research demonstrating optically addressable protein-based spin qubits in fluorescent proteins, which have coherence times rivaling NV centers in nanodiamonds but are genetically encodable and roughly ten times smaller [3]. The global biophotonics market, valued at $62.6 billion in 2024 and projected to reach $113.1 billion by 2030, reflects the vigorous commercial and technological momentum of this field [9].
The field of bio-optics represents the innovative convergence of biology, medicine, and photonics, employing light to analyze and manipulate biological materials [2]. This interdisciplinary fusion has transformed research, diagnostics, and therapy across various domains, offering significant advantages over traditional imaging techniques such as X-ray computed tomography (CT), positron emission tomography (PET), and magnetic resonance imaging (MRI) [2] [10]. Unlike ionizing radiation-based methods, bio-optical techniques utilize the interactions between light and biological matter—specifically absorption, emission, scattering, and reflection—to generate contrast and provide information about biological systems non-invasively and with high sensitivity [2] [11].
The fundamental principle underlying bio-optics is that when light encounters biological tissue, it undergoes various physical interactions that can be measured and interpreted to reveal structural, functional, and molecular information [2] [11]. These interactions form the basis for a wide array of bio-optical technologies that enable visualization of biological processes across multiple spatial scales, from single molecules to entire organs [2]. This technical guide provides an in-depth examination of these core interaction phenomena, framed within the context of a broader thesis comparing bio-optics with traditional imaging techniques for researchers, scientists, and drug development professionals.
Fundamental Principles of Light-Tissue Interactions
Photon Transport in Biological Tissue
When light propagates through biological tissues, it undergoes a series of photophysical interactions including absorption, scattering, and reflection [12] [11]. The trajectory of individual photons is determined by the optical properties of the tissue, which vary depending on molecular composition, structural organization, and physiological state [11]. These interactions are not mutually exclusive; rather, they occur simultaneously, with their relative predominance depending on the optical properties of the tissue at specific wavelengths [2].
The key advantage of utilizing these light-tissue interactions for imaging lies in their ability to provide non-contact measurement, enabling observation of living cells without compromising their integrity [2]. Additionally, optical measurements offer exceptional speed for real-time data acquisition, ultrasensitive detection capabilities down to single molecules, and excellent time resolution for observing dynamic biological processes across various temporal scales [2].
Core Interaction Phenomena
The four primary phenomena governing light-tissue interactions are:
- Absorption: Process where light energy is transferred to molecular chromophores, causing electronic transitions [2]
- Emission: Process where excited molecules return to ground state, releasing energy as photons [11]
- Scattering: Redirection of light caused by interactions with microscopic variations in refractive index [2] [12]
- Reflection: Return of light from tissue interfaces due to differences in refractive indices [2]
These interaction phenomena are distinguished by their capacity to elucidate a vast array of morphological and molecular intricacies across a spectrum of size scales, encompassing macroscopic, microscopic, and nanoscopic resolutions [2].
Figure 1: Fundamental light-tissue interactions and their applications in bio-optical imaging techniques.
Quantitative Analysis of Interaction Phenomena
Performance Metrics Across Modalities
The effectiveness of bio-optical imaging techniques depends critically on how they leverage the core interaction phenomena. Different modalities optimize for specific interactions to achieve desired performance characteristics including penetration depth, resolution, and molecular specificity.
Table 1: Performance comparison of bio-optical imaging modalities based on core interaction phenomena
| Imaging Modality | Primary Interaction | Penetration Depth | Spatial Resolution | Key Applications |
|---|---|---|---|---|
| Optical Coherence Tomography (OCT) | Scattering, Reflection | 1-3 mm [2] | 1-15 μm [2] | Ophthalmology, tissue morphology [2] [13] |
| Multi-photon Microscopy | Absorption, Emission | ~1 mm [2] | <1 μm [2] | Deep tissue cellular imaging [2] |
| Photoacoustic Imaging | Absorption | Several cm [10] | 10-200 μm [10] | Vascular imaging, oxygen saturation [10] |
| Diffuse Optical Tomography | Scattering | Several cm [11] | 5-10 mm [11] | Breast cancer imaging, brain functional imaging [11] |
| NIR-II Fluorescence Imaging | Emission, Absorption | Millimeters to centimeters [12] | High spatiotemporal resolution [12] | Tumor imaging, vascular imaging, surgical navigation [12] |
| Raman Spectroscopy | Scattering | Surface/subsurface [2] | Molecular fingerprinting [2] [14] | Biochemical analysis, disease biomarkers [2] [14] |
Wavelength-Dependent Interactions
The nature and efficiency of light-tissue interactions vary significantly with wavelength, creating distinct optical windows for biomedical applications.
Table 2: Wavelength-dependent characteristics of light-tissue interactions
| Spectral Region | Wavelength Range | Primary Interactions | Tissue Effects | Representative Applications |
|---|---|---|---|---|
| Ultraviolet (UV) | 200-400 nm | Strong absorption, scattering | Photodamage, limited penetration | Surface fluorescence, microscopy [11] |
| Visible | 400-700 nm | Moderate absorption and scattering | Good contrast, moderate penetration | Color imaging, oximetry [12] [11] |
| Near-infrared I (NIR-I) | 700-1000 nm | Reduced scattering, low absorption | Deep penetration | Optical coherence tomography, diffuse tomography [12] |
| Near-infrared II (NIR-II) | 1000-1700 nm | Minimal scattering and absorption | Maximum penetration | Deep tissue imaging, biosensing [12] |
Experimental Methodologies
Protocol 1: NIR-II Fluorescence Bioimaging
Principle: Utilizing fluorophores emitting in the second near-infrared window (1000-1700 nm) where tissue absorption and scattering coefficients are significantly reduced, enabling enhanced penetration depth and spatiotemporal resolution [12].
Materials:
- NIR-II fluorophore (quantum dots, single-walled carbon nanotubes, rare-earth-doped nanoparticles, conjugated polymers, or organic dyes) [12]
- NIR-compatible excitation source (tunable laser system)
- InGaAs or other NIR-II sensitive detector
- Animal model or tissue sample
- Anesthesia system (for in vivo studies)
- Data acquisition and processing software
Procedure:
- Administer NIR-II fluorophore via intravenous injection (for in vivo) or add to media (for in vitro)
- Allow appropriate circulation/uptake time (typically 1-24 hours depending on application)
- Anesthetize animal if performing in vivo imaging
- Set excitation wavelength according to fluorophore absorption maximum (typically 808 nm for many NIR-II probes)
- Acquire time-series images using NIR-II detector
- Process images to remove background autofluorescence
- Quantify signal intensity in regions of interest
- Perform biodistribution analysis if required
Key Parameters:
- Excitation power density: <100 mW/cm² for in vivo to prevent tissue damage
- Acquisition frame rate: Adjust based on phenomenon of interest (seconds to minutes)
- Spectral filters: Optimized for specific emission ranges within NIR-II window
- Image analysis: Include flat-field correction, background subtraction, and spectral unmixing if multiple probes used
Protocol 2: Photoacoustic Imaging
Principle: Combines optical excitation with acoustic detection based on the photoacoustic effect, where chromophores absorb pulsed light, undergo thermoelastic expansion, and generate ultrasound waves that reflect optical absorption properties [10].
Materials:
- Pulsed laser source (Nd:YAG, OPO, or diode laser) with nanosecond pulse width
- Ultrasound transducer (single-element for microscopy, array for tomography)
- Data acquisition system with high-speed digitizer
- Scanning system (for microscopy implementations)
- Image reconstruction software
- Animal model or tissue sample
Procedure:
- Position sample or animal in imaging chamber
- Adjust laser parameters: wavelength (according to chromophore absorption), pulse energy, repetition rate
- Align ultrasound transducer with respect to illumination spot
- Acquire photoacoustic signals following each laser pulse
- Scan transducer or sample if using single-element detection
- Reconstruct images using appropriate algorithm (delay-and-sum, time-reversal, or model-based)
- Process images to extract quantitative parameters (oxygen saturation, chromophore concentration)
Key Parameters:
- Laser wavelength: Selected based on target chromophore (e.g., 532 nm for hemoglobin, 750-900 nm for contrast agents)
- Pulse duration: Typically 1-100 ns to satisfy stress confinement
- Ultrasound transducer frequency: Trade-off between resolution and depth (1-100 MHz)
- Reconstruction algorithm: Chosen based on system geometry and signal-to-noise requirements
Protocol 3: Adaptive Optics Ophthalmoscopy
Principle: Corrects ocular aberrations in real-time using wavefront sensing and deformable mirrors, enabling diffraction-limited imaging of retinal structures at cellular resolution [13].
Materials:
- Adaptive optics system with wavefront sensor (Shack-Hartmann)
- Deformable mirror
- Multi-modal imaging system (confocal scanning laser ophthalmoscopy, fluorescence, OCT)
- Light sources for imaging and wavefront sensing
- Computer for real-time control and image acquisition
- Human subject or animal model
Procedure:
- Align subject's eye with optical system
- Measure wavefront aberrations using wavefront sensor
- Compute correction signals using control algorithm
- Apply correction via deformable mirror
- Verify correction quality by measuring residual aberrations
- Acquire high-resolution retinal images using various contrast mechanisms (reflectance, fluorescence, multiphoton)
- Process images to correct for residual distortions and enhance signal-to-noise ratio
Key Parameters:
- Wavefront sensor sampling: Sufficient to capture higher-order aberrations
- Correction rate: Typically 10-100 Hz to track dynamic aberrations
- Imaging wavelength: Selected based on target structures (e.g., 790 nm for photoreceptors, 550 nm for blood vessels)
- Power levels: Maintained within safe retinal exposure limits
Figure 2: Generalized workflow for bio-optical imaging experiments, highlighting key stages from sample preparation to quantitative analysis.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of bio-optical imaging requires specialized reagents and materials designed to enhance, quantify, or modulate light-tissue interactions.
Table 3: Essential research reagents and materials for bio-optical investigations
| Reagent/Material | Composition/Type | Primary Function | Application Examples |
|---|---|---|---|
| NIR-II Fluorophores | Organic dyes, quantum dots, single-walled carbon nanotubes, rare-earth nanoparticles [12] | Emission signal generation in 1000-1700 nm range for deep tissue imaging | Tumor imaging, vascular mapping, surgical navigation [12] |
| Genetically Encoded Fluorescent Proteins | Green/red fluorescent proteins (GFP, RFP) and their variants [11] | Labeling specific proteins or cells for visualization in live specimens | Protein localization, cell tracking, gene expression studies [11] |
| Target-Specific Molecular Probes | Antibodies, peptides, or small molecules conjugated to fluorophores [11] | Binding to specific biomarkers for molecular imaging | Cancer biomarker detection, inflammation imaging [11] |
| Gold Nanoparticles | Spherical, rod-shaped, or nanostructured gold particles [11] | Enhancing optical contrast through scattering and absorption | Photoacoustic imaging, biosensing, thermal therapy [11] |
| Environmental-Responsive Probes | Fluorophores with sensing moieties for pH, ions, or metabolites [11] | Reporting on subcellular microenvironment changes | Metabolic activity monitoring, organelle-specific sensing [11] |
| Adaptive Optics Components | Wavefront sensors, deformable mirrors, control algorithms [13] | Correcting optical aberrations in real-time | High-resolution retinal imaging, deep tissue microscopy [13] |
Comparative Analysis: Bio-Optics vs. Traditional Imaging
Technical Advantages of Bio-Optical Methods
Bio-optical imaging techniques offer several distinct advantages over traditional imaging modalities:
Non-ionizing Nature: Unlike X-ray CT and PET, bio-optical methods utilize non-ionizing radiation, enabling repeated imaging sessions without cumulative radiation exposure [11] [10]. This is particularly advantageous for longitudinal studies, pediatric applications, and monitoring treatment response.
Molecular Sensitivity: Optical techniques can detect specific molecular targets through endogenous contrast or targeted agents with high specificity [2] [11]. Traditional anatomical imaging modalities like CT and MRI primarily provide structural information and often require contrast agents for functional assessment.
Real-time Capabilities: The high speed of optical measurements enables real-time monitoring of dynamic biological processes [2]. This temporal resolution exceeds that of most traditional modalities, facilitating studies of physiological processes, drug delivery, and surgical guidance.
Cost-effectiveness and Accessibility: Bio-optical systems are generally more compact and affordable than MRI, CT, or PET scanners, making them more accessible for research and clinical applications [10].
Limitations and Complementary Role
Despite these advantages, bio-optical imaging faces certain limitations:
Penetration Depth: Light scattering in biological tissue fundamentally limits penetration depth to a few centimeters, whereas CT, MRI, and PET can image the entire body [12] [10]. This restricts bio-optical methods to superficial structures, small animals, or intraoperative applications.
Quantification Challenges: Light attenuation and scattering complicate quantitative measurements compared to more established modalities like CT, where attenuation coefficients directly relate to material density.
Clinical Translation Barriers: While numerous bio-optical techniques have proven invaluable in research, regulatory approval and clinical adoption have been slower than for traditional modalities, particularly for novel contrast agents [12] [14].
The future of biomedical imaging lies not in replacement but in complementarity, with hybrid approaches combining the strengths of multiple modalities. For instance, photoacoustic imaging merges optical contrast with ultrasound resolution, effectively addressing the depth limitation of pure optical methods [10].
Emerging Frontiers and Future Directions
Integration with Artificial Intelligence
Machine learning and artificial intelligence are transforming bio-optical imaging through enhanced image reconstruction, interpretation, and optical design [2] [3]. AI algorithms can extract subtle patterns from optical data that are imperceptible to human observers, enabling earlier disease detection and more precise quantification. The integration of AI is particularly valuable for resolving the inverse problem in diffuse optical tomography and for analyzing complex data from hyperspectral imaging techniques [2].
Novel Materials and Contrast Mechanisms
The development of advanced contrast agents represents a vibrant research frontier. Second near-infrared window (NIR-II) fluorophores continue to evolve with improvements in quantum yield, biocompatibility, and targeting specificity [12]. Stimuli-responsive probes that alter their optical properties in response to specific biomarkers enable sensing of physiological parameters with high spatiotemporal resolution [11]. Additionally, nanomaterials with tailored optical properties are expanding the capabilities of bio-optical techniques for both diagnostic and therapeutic applications.
Clinical Translation and Commercial Outlook
The biophotonics market is projected to grow significantly, with estimates exceeding $100 billion by 2032, reflecting increasing clinical adoption and technological advancement [15]. Key growth areas include point-of-care diagnostics, minimally invasive surgical guidance, and therapeutic monitoring. Optical coherence tomography has already established strong clinical utility in ophthalmology, while other techniques like photoacoustic imaging and diffuse optical tomography are progressing toward broader clinical implementation [14] [10].
The core interaction phenomena of absorption, emission, scattering, and reflection form the physical foundation for bio-optical imaging techniques that are revolutionizing biomedical research and clinical practice. These light-tissue interactions enable non-invasive visualization of biological structures and processes across multiple spatial and temporal scales, with advantages in molecular sensitivity, safety, and cost-effectiveness compared to traditional imaging modalities. While penetration depth limitations present challenges for certain applications, ongoing advancements in instrumentation, contrast agent design, and computational methods continue to expand the capabilities and applications of bio-optical imaging. For researchers, scientists, and drug development professionals, understanding these fundamental principles and their implementation is essential for leveraging the full potential of bio-optics in scientific discovery and translational medicine.
Bio-optics, the interdisciplinary fusion of light-based technologies with biology and medicine, is fundamentally transforming biomedical research and clinical diagnostics [2]. This technical guide examines the core advantages that establish bio-optical methods as superior to traditional imaging and analytical techniques across numerous applications. The convergence of advanced photonic technologies with biology has enabled a new generation of tools that operate without damaging samples, deliver results in real-time, and detect individual molecules with extraordinary precision [16] [2]. These capabilities are reshaping experimental approaches in basic research and accelerating translational applications in drug development, clinical diagnostics, and therapeutic monitoring [17]. This whitepaper provides an in-depth technical analysis of these advantages, supported by current experimental data and methodologies, framed within the broader context of bio-optics versus traditional imaging techniques research.
Core Technical Advantages: A Comparative Analysis
Non-Invasiveness: Preserving Native Biological States
Non-invasive measurement stands as a foundational advantage of bio-optical techniques, enabling observation of living cells and biological processes without compromising sample integrity or inducing toxic effects [2]. Unlike conventional methods that often require fixation, staining, or physical disruption of samples, optical measurements facilitate the longitudinal study of dynamic processes in their native states.
- Mechanism of Action: Bio-optical techniques leverage various forms of light-matter interaction—including absorption, emission, reflection, and scattering—to extract biological information without physical contact or destructive sampling [2]. This non-contact approach preserves the viability of cells and tissues, enabling repeated observations over time.
- Comparative Advantage: Traditional histological methods require tissue fixation, sectioning, and staining, processes that permanently alter samples and prevent longitudinal studies. In contrast, techniques like optical coherence tomography (OCT) and adaptive optics ophthalmoscopy provide detailed structural information while maintaining full sample viability [13].
- Experimental Evidence: Research on retinal organoids and explants demonstrates how fully automated OCT systems enable non-invasive, high-throughput 3D imaging and quantification of tissue architecture for drug discovery applications, eliminating the need for destructive histology methods [13]. Similarly, adaptive optics technologies correct optical imperfections in the eye to visualize individual retinal cells, including photoreceptors, microglia, and blood vessels, in living subjects without biopsy [13].
Speed and Real-Time Capability: Instantaneous Biological Insights
The speed and instant information delivery capability of optical measurements represents a transformative advantage, providing rapid, real-time data that significantly reduces the time required for data interpretation and diagnosis [2].
- Technical Foundation: The inherent speed of light enables temporal resolution ranging from hours for slow biological processes to ultrafast reactions, capturing dynamic molecular and cellular events inaccessible to conventional methods [2].
- Implementation Examples: Optical coherence tomography (OCT) stands as one of the fastest methods in terms of volume elements (voxels) imaged per second, enabling real-time 3D imaging of dynamic processes that has established its clinical utility in ophthalmology [2]. Advanced microfluidic platforms integrated with optical detection achieve response times as low as seven milliseconds with 100% success rates in automated object detection [13].
- Impact on Research and Diagnostics: This temporal resolution enables researchers to monitor cellular processes, molecular interactions, and therapeutic responses as they occur, transforming our understanding of biological dynamics and accelerating diagnostic procedures [18]. For drug development professionals, this capability provides real-time insights into compound effects during screening campaigns, dramatically reducing development timelines.
Single-Molecule Sensitivity: Ultimate Detection Limits
The ability to achieve single-molecule sensitivity represents perhaps the most significant technical advancement enabled by bio-optical methods, revealing heterogeneities and transient states invisible to conventional ensemble measurements [19].
- Fundamental Principles: Label-free single-molecule detection techniques exploit intrinsic molecular properties—particularly scattering and refractive index changes—to achieve detection at the ultimate sensitivity limit [19]. For biomolecules in aqueous environments, the inherently low refractive index contrast creates weak scattering signals that modern photonic sensors overcome through interference, plasmonic enhancement, and optical resonance phenomena [19].
- Quantitative Performance: Next-generation photonic sensors now enable detection at attomolar (10⁻¹⁸ M) and even zeptomolar (10⁻²¹ M) levels, surpassing the sensitivity limits of conventional fluorescence-based methods [16]. Techniques like interferometric scattering microscopy (iSCAT) can detect single proteins in the tens of kilodalton range, functioning as an optical analog of mass spectrometry for precise mass profiling and real-time tracking of molecular transport [19].
- Methodological Advancements: Plasmonic sensors based on individual metal nanoparticles provide confined modes with significantly smaller probing volumes than traditional surface plasmon resonance (SPR), enabling true single-molecule resolution for biomolecular interaction analysis [19]. Nanofluidic scattering microscopy (NSM) employs nanochannels to container freely diffusing molecules, enabling stable signal detection throughout the imaging process for both molecular mass and diffusivity measurements [19].
Table 1: Quantitative Comparison of Bio-Optical Techniques Enabling Single-Molecule Sensitivity
| Technique | Detection Principle | Sensitivity Limit | Temporal Resolution | Key Applications |
|---|---|---|---|---|
| iSCAT | Interference between scattered and reference light | Single proteins (~10s kDa) [19] | Millisecond to second [19] | Mass profiling, molecular transport, interaction studies [19] |
| Plasmonic Nanosensors | Refractometric detection via resonance shift | Single biomolecule binding events [19] | Real-time monitoring [19] | Biomolecular interaction analysis, affinity determination [19] |
| Nanofluidic Scattering | Interference with channel-scattered reference | Single proteins (comparable to iSCAT) [19] | Stable during diffusion [19] | Mass and diffusivity measurements [19] |
| WGM Resonators | Resonance shift from binding-induced refractive index change | Attomolar to zeptomolar [16] | Real-time [16] | Cancer diagnostics, viral identification, pollutant sensing [16] |
Experimental Protocols: Methodologies for High-Sensitivity Detection
Protocol: Interferometric Scattering (iSCAT) for Single-Protein Detection
Principle: iSCAT detects biomolecules through interference between light scattered by the analyte and a reference wave reflected from a substrate interface [19]. The interference term in the detected intensity (2|Er||Es|cosϕ) becomes the dominant signal for subwavelength particles, enabling detection of single proteins with masses in the kilodalton range [19].
Experimental Workflow:
- Substrate Preparation: Use coverslips with controlled refractive index and thickness, typically cleaned and functionalized for specific binding applications.
- Optical Configuration: Employ epi-illumination with laser sources (typically 405-660 nm), high-numerical-aperture objectives (NA 1.2-1.5), and fast scientific CMOS or EMCCD cameras [19].
- Reference Wave Management: Optimize the reference wave intensity relative to the scattering signal to maximize contrast while minimizing background fluctuations.
- Sample Application: Introduce protein solutions at appropriate concentrations (pM-nM range) to enable single-molecule binding events to the functionalized surface.
- Image Acquisition: Record video-rate sequences (50-1000 frames/s) to capture binding and diffusion events.
- Data Analysis: Apply background subtraction algorithms and analyze interference contrast, which scales linearly with protein mass, enabling quantitative mass determination at the single-molecule level [19].
Critical Considerations: Detection sensitivity depends strongly on phase stability, restricting optimal detection to surface-bound or near-surface molecules. Rapid phase fluctuations from axial diffusion of molecules in solution can average out the signal [19].
Protocol: Plasmonic Nanoparticle Sensing for Biomolecular Interactions
Principle: Single metal nanoparticles support localized surface plasmon resonances (LSPRs) that shift in response to local refractive index changes caused by biomolecules binding to their surfaces [19].
Experimental Workflow:
- Nanoparticle Fabrication: Synthesize or commercially source monodisperse gold or silver nanoparticles (typically 20-100 nm diameter) and immobilize on functionalized substrates.
- Surface Functionalization: Modify nanoparticle surfaces with capture molecules (antibodies, DNA oligonucleotides, etc.) specific to the target analyte.
- Optical Setup: Implement dark-field microscopy, photothermal imaging, or total internal reflection scattering to monitor individual nanoparticles with high signal-to-noise ratio.
- Spectral Monitoring: Track resonance wavelength shifts of single nanoparticles in real-time using spectrophotometric detection or scattering-based approaches.
- Binding Kinetics: Introduce analyte solutions and monitor resonance shifts versus time to extract binding kinetics and affinity constants.
- Data Analysis: Fit binding curves to appropriate kinetic models (Langmuir, etc.) to determine association and dissociation rate constants [19].
Critical Considerations: The small surface area of individual nanoparticles (a 50 nm particle accommodates ~100 proteins) enables true single-molecule detection but requires careful statistical analysis of multiple nanoparticles to account for heterogeneity [19].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Advanced Bio-Optical Experiments
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Functionalized Coverslips | Provides substrate for biomolecule immobilization with controlled refractive properties | iSCAT, TIRF, single-molecule tracking [19] |
| Plasmonic Nanoparticles | Enhances optical signals via localized surface plasmon resonance | Single-particle sensing, enhanced spectroscopy [19] |
| DNA Nanostructures | Precisely positions molecules and functions on nanoscale | Modular single-molecule sensors, nanodevice assembly [20] |
| Fluorescent Proteins (GFP, RFP) | Genetically encoded labels for specific protein visualization | Live-cell imaging, protein localization and dynamics [14] |
| Raman Tags | Provides distinct vibrational signatures for multiplexed detection | Raman spectroscopy, chemical imaging of cellular components [14] |
| Microfluidic Chips | Enables precise environmental control and high-throughput screening | Organoid imaging, single-cell analysis, drug screening [18] |
| Advanced Fluorophores | Bright, photostable labels for prolonged single-molecule tracking | Super-resolution microscopy, single-molecule fluorescence [20] |
Technical Challenges and Emerging Solutions
Despite these significant advantages, bio-optical methods face several technical challenges that active research is addressing:
- Noise Suppression: Weak single-molecule signals require sophisticated noise reduction strategies. Solutions include computational approaches (machine learning denoising), lock-in detection methods, and plasmonic enhancement to boost signal-to-noise ratios [16] [18].
- Fabrication Complexity: Nanophotonic structures enabling single-molecule detection often involve complex fabrication. Emerging solutions include DNA nanotechnology for self-assembled structures [20] and improved nanofabrication protocols [16].
- Bio-Compatibility: Maintaining biological function while achieving sufficient optical contrast remains challenging. Label-free methods address this by eliminating exogenous probes, while advanced functionalization strategies improve biocompatibility of interfaces [16] [19].
- Data Interpretation: The complexity of bio-optical data requires advanced analysis tools. Machine learning and artificial intelligence are increasingly deployed for image analysis, feature extraction, and data interpretation [2] [18].
Bio-optical technologies have established a new paradigm for biological investigation and clinical diagnostics through their fundamental advantages in non-invasiveness, speed, and single-molecule sensitivity. These capabilities are driving transformative applications across biomedical research, drug development, and clinical practice. The continued advancement of photonic sensors, combined with emerging enhancements from artificial intelligence, hybrid sensor architectures, and miniaturization for point-of-care applications, promises to further accelerate the adoption of these technologies [16] [2]. As these methodologies mature, they are poised to redefine the standards for biological measurement and therapeutic monitoring, enabling unprecedented insights into cellular and molecular processes that underlie health and disease. For researchers and drug development professionals, understanding and leveraging these advantages is essential for driving the next generation of biomedical innovations.
The field of biomedical science is experiencing a fundamental transformation driven by the convergence of optical technologies, nanomaterials science, and artificial intelligence. This paradigm shift from traditional imaging techniques to integrated bio-optics platforms addresses critical limitations in conventional modalities like MRI, CT, and PET, which often involve ionizing radiation, limited spatial-temporal resolution, complex infrastructure requirements, and high costs [21]. Bio-optical approaches leverage the unique properties of light-matter interactions at micro and nanoscales to enable non-invasive, high-resolution, and multi-parametric assessment of biological systems with unprecedented sensitivity and specificity. These core technology pillars—bioimaging, biosensing, and photonic therapies—are converging toward unified platforms that provide comprehensive diagnostic and therapeutic capabilities, ultimately advancing personalized medicine through enhanced molecular-level precision, real-time monitoring, and minimally invasive interventions.
Core Technology Pillar I: Advanced Bioimaging
Advanced bioimaging technologies represent the foundational pillar of modern bio-optics, enabling visualization of biological structures and processes across multiple scales from single molecules to entire organisms.
Photoacoustic Imaging (PAI)
Photoacoustic imaging elegantly bridges optical contrast and acoustic resolution, overcoming the traditional depth limitations of pure optical microscopy. This hybrid modality operates on the photoacoustic effect, where short laser pulses illuminate chromophores in tissue, causing rapid thermoelastic expansion and generating ultrasonic waves that convey optical absorption properties with acoustic resolution [10]. The initial pressure of the photoacoustic wave is determined by the equation: p₀ = ΓηthμaF, where Γ is the Grüneisen parameter, ηth is the photothermal conversion efficiency, μa is the optical absorption coefficient, and F is the optical fluence [10].
PAI systems employ various detection technologies categorized into ultrasonic transducers and optical sensing methods. Conventional piezoelectric transducers using materials like PVDF, PZT, and PMN-PT can be configured as single-element detectors for high-resolution microscopy (PAM) or multi-element arrays for computed tomography (PACT) [10]. Recent advancements include piezoelectric micromachined ultrasonic transducers (PMUTs) and capacitive micromachined ultrasound transducers (CMUTs) that combine MEMS technology with conventional approaches, offering improved performance with customizable sizes and shapes [10].
Diagram 1: Photoacoustic imaging workflow. The process begins with pulsed laser excitation, leading to ultrasound generation via the photoacoustic effect, followed by detection and computational reconstruction.
Near-Infrared-II (NIR-II) Imaging
The discovery of the second near-infrared window (NIR-II, 1000-1700 nm) represents a breakthrough in deep-tissue optical imaging. NIR-II technology provides unprecedented tissue penetration depth, low photon scattering, and negligible autofluorescence compared to traditional visible-light and NIR-I fluorescence imaging [21]. This capability dramatically improves sensitivity and specificity for biological sensing and imaging applications, enabling dynamic tracking of cell distribution and fate in deep tissues and organs with high spatial-temporal resolution and improved signal-to-noise ratio [21].
NIR-II imaging employs various contrast agents including quantum dots (QDs), semiconducting polymer dots (Pdots), rare-earth-doped nanoparticles, and small-molecular organic fluorophores [21]. Key parameters for optimal performance include cellular labeling brightness, chemostability, photostability, biocompatibility, and functionalization capabilities for targeted imaging.
Hybrid Imaging Platforms
The integration of multiple imaging modalities creates synergistic platforms that overcome individual limitations. A groundbreaking development from UC Davis combines PET and dual-energy CT in a novel configuration called PET-enabled Dual-Energy CT [22]. This approach uses PET scan data to create a second, high-energy CT image, enabling dual-energy imaging that provides detailed tissue composition information without new hardware or additional radiation exposure [22]. This hybrid technique enhances cancer detection, improves bone marrow scanning, and provides new insights into cardiovascular risk assessment, potentially implementable on existing PET/CT scanners without expensive equipment upgrades [22].
Table 1: Performance Comparison of Bio-optical Imaging Modalities Versus Traditional Techniques
| Imaging Modality | Spatial Resolution | Penetration Depth | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| NIR-II Imaging | 10-50 μm | 5-10 mm | Low autofluorescence, high spatio-temporal resolution | Limited clinical translation of contrast agents |
| Photoacoustic Imaging | 20-200 μm | 2-5 cm | Combines optical contrast with ultrasound resolution | Limited by optical absorption properties |
| PET-enabled DECT | 0.5-1 mm | Whole body | Provides metabolic and compositional data | Requires radiotracers, higher cost |
| MRI | 0.1-1 mm | Whole body | Excellent soft tissue contrast | Low temporal resolution, high cost |
| CT | 0.2-0.5 mm | Whole body | Fast acquisition, excellent bone imaging | Ionizing radiation, poor soft tissue contrast |
| Fluorescence (NIR-I) | 5-20 μm | 1-2 mm | High sensitivity, real-time imaging | Limited penetration, autofluorescence |
Core Technology Pillar II: Biosensing and Diagnostics
Biosensing technologies have evolved from simple analyte detection to sophisticated systems integrating nanophotonics, molecular recognition, and artificial intelligence for comprehensive diagnostic applications.
Nanophotonic Biosensing
Nanophotonics—the manipulation of light at the nanometer scale—enables control of optical fields beyond diffraction limits through phenomena like near-field coupling, photonic bandgap (PBG) effects, and localized surface plasmon resonance (LSPR) [23]. These capabilities allow nanostructures to confine and manipulate light with high precision, creating powerful biomedical tools for diagnosis and monitoring.
Surface Plasmon Resonance (SPR) arises when incident light couples with free electrons at a metal-dielectric interface, producing resonance exquisitely sensitive to changes in the local refractive index [23]. Modern SPR platforms integrate advanced computational modeling using Finite-Difference Time-Domain (FDTD) and Finite Element Method (FEM) simulations to optimize sensor geometry and material selection for enhanced performance [23].
Plasmonic nanoparticles, particularly gold (AuNPs) and silver (AgNPs), sustain LSPR and generate localized electromagnetic fields that amplify optical signals in their immediate vicinity [23]. These nanoparticles enable surface-enhanced Raman spectroscopy (SERS), plasmon-enhanced fluorescence, and photothermal imaging. Anisotropic structures like nanorods and nanostars exhibit resonances in the near-infrared region, penetrating biological tissues for deep-tissue imaging and targeted therapies [23].
Elemental Imaging and Analysis
Elemental bioimaging techniques provide crucial information about tissue composition for clinical diagnostics and research. Modern methods including laser ablation inductively coupled plasma mass spectrometry (LA-ICP-MS), laser-induced breakdown spectroscopy (LIBS), X-ray fluorescence (XRF), and electron microscopy methods (SEM/TEM-EDS) enable mapping of elemental distributions in biological samples [24]. These techniques are revolutionizing areas from oncology to neurology by detecting pathogens, monitoring therapy safety, determining intracellular processes, and assessing the necessity for implant revision [24].
Critical parameters ensuring measurement quality include selectivity, detection limits, linearity, and precision, though challenges remain in standardization, calibration materials, and accuracy assessment for trace elements [24].
Integrated Diagnostic Systems
The convergence of multiple technologies creates diagnostic systems with enhanced capabilities. A prime example is a dual-mode optical imaging system developed by researchers at Saint-Étienne University Hospital and Paris-Saclay University, which combines line-field confocal optical coherence tomography (LC-OCT) with confocal Raman microspectroscopy [25]. This system captures high-resolution cellular-level images while simultaneously analyzing chemical composition, achieving 95% classification accuracy for basal cell carcinoma in clinical testing on over 330 skin cancer samples [25]. The integration of artificial intelligence for pattern recognition further enhances diagnostic reliability by distinguishing cancerous tissues based on their chemical signatures [25].
Diagram 2: Integrated biosensing pathway. Nanophotonic probes interact with biological samples, transducing molecular recognition events into optical signals enhanced by AI analysis.
Core Technology Pillar III: Photonic Therapies
Photonic therapies harness light-matter interactions for precise, targeted treatment modalities with minimal invasiveness and reduced side effects compared to conventional approaches.
Photothermal Therapy (PTT)
Photothermal therapy utilizes light-absorbing nanoparticles to generate localized heat under external illumination. Recent advances include size-regulated antimony nanoparticles that precisely adjust localized surface plasmon resonance to match therapeutic laser wavelengths, enhancing both photothermal and photodynamic effects [26]. These semimetallic nanomaterials demonstrate high photothermal conversion efficiencies while maintaining biocompatibility, offering promising alternatives to traditional noble metal nanoparticles [26].
Gold nanorods (AuNRs) represent another advanced platform, converting NIR (850 nm) light into thermal energy with high efficiency. Their anisotropic structure enables resonance tuning to tissue-transparent near-infrared wavelengths, facilitating deeper tissue penetration for ablation of malignant cells while sparing surrounding healthy tissue [23].
Photodynamic Therapy (PDT)
Photodynamic therapy combines photosensitizing agents with specific wavelength light to generate reactive oxygen species that selectively destroy target cells. The integration of nanotechnology has addressed traditional limitations in photosensitizer delivery, specificity, and efficacy. Advanced platforms include two-dimensional materials, quantum dots, and self-assembled nanostructures with tunable optical, electrical, and biochemical properties [26]. These materials act as transducers, amplifying biological recognition events into measurable signals, or as therapeutic agents delivering payloads with spatial and temporal precision [26].
Image-Guided Interventions
The combination of diagnostic and therapeutic capabilities creates theranostic platforms that enable real-time treatment monitoring and adjustment. Nanomaterials with responsiveness to multiple stimuli—pH, temperature, light, or enzymatic activity—create opportunities for systems where detection and treatment are seamlessly linked [26]. This integration is particularly valuable in oncology, where precise tumor delineation and targeted ablation significantly improve treatment outcomes while reducing collateral damage to healthy tissues.
Experimental Protocols and Methodologies
Protocol: Dual-Mode Optical Imaging for Skin Cancer Diagnosis
This protocol outlines the methodology for combining line-field confocal optical coherence tomography (LC-OCT) and confocal Raman microspectroscopy based on clinical validation studies [25].
Sample Preparation:
- Obtain fresh biopsy samples or perform in vivo measurements on suspected skin lesions
- Clean the area with saline solution to remove surface contaminants
- For ex vivo samples, mount in optimal cutting temperature (OCT) compound without chemical fixation
Instrument Setup:
- Configure LC-OCT system with superluminescent diode source (central wavelength ~830 nm)
- Align confocal Raman microspectroscopy system with 785 nm laser excitation
- Calbrate both systems using standardized reflectance phantoms and Raman standards
Data Acquisition:
- Acquire LC-OCT images of suspicious regions with field of view of ~1.2 × 0.8 mm
- Collect high-resolution depth-resolved images down to ~500 μm penetration
- Perform Raman spectral mapping on regions identified as abnormal by LC-OCT
- Collect 1,300-1,500 spectra per sample with integration times of 1-5 seconds
Data Analysis:
- Preprocess Raman spectra with smoothing, baseline correction, and vector normalization
- Apply principal component analysis (PCA) for dimensionality reduction
- Train support vector machine (SVM) classifier with cross-validation
- Correlate molecular features from Raman with structural features from LC-OCT
Protocol: NIR-II Cell Tracking in Live Animals
This protocol details procedures for in vivo cell tracking using NIR-II fluorescence imaging based on established methodologies [21].
Cell Labeling:
- Culture target cells (e.g., stem cells, immune cells) in standard conditions
- Incubate with NIR-II contrast agent (e.g., rare-earth-doped nanoparticles, quantum dots) for 4-24 hours
- Remove excess label through multiple washing steps with phosphate-buffered saline (PBS)
- Verify labeling efficiency and cell viability using flow cytometry and trypan blue exclusion
Animal Preparation:
- Anesthetize animal using isoflurane or ketamine/xylazine based on institutional guidelines
- Position animal in imaging chamber with temperature maintenance at 37°C
- Administer cells via appropriate route (intravenous, intramuscular, etc.)
Imaging Acquisition:
- Set up NIR-II imaging system with 808 nm or 980 nm laser excitation
- Configure InGaAs camera with appropriate filters for NIR-II detection (1000-1700 nm)
- Acquire time-series images at predetermined intervals (e.g., 0, 6, 24, 48 hours)
- Include control animals receiving unlabeled cells for background subtraction
Image Processing:
- Apply flat-field correction to account for uneven illumination
- Subtract autofluorescence background using control images
- Quantify signal intensity in regions of interest (ROIs)
- Reconstruct 3D distributions using tomographic approaches when applicable
Table 2: Research Reagent Solutions for Bio-optics Applications
| Reagent Category | Specific Examples | Key Functions | Application Notes |
|---|---|---|---|
| Plasmonic Nanoparticles | Gold nanorods, silver nanostars, antimony nanoparticles | Photothermal conversion, signal enhancement for SERS | Size and shape dictate resonance wavelength; surface chemistry affects targeting |
| NIR-II Contrast Agents | Rare-earth-doped nanoparticles, single-walled carbon nanotubes, quantum dots | Deep-tissue fluorescence imaging | Emission tails beyond 1000 nm reduce scattering; functionalization enables specific targeting |
| Photoacoustic Contrast Agents | Indocyanine green derivatives, methylene blue, gold nanocages | Enhanced optical absorption for PA signal generation | Biocompatibility and clearance profiles crucial for clinical translation |
| Gene Editing Components | CRISPR-Cas systems, guide RNA, repair templates | Precision genetic modification | Can be integrated with optical readouts for real-time monitoring of editing efficiency |
| Surface Chemistry Reagents | PEG linkers, thiol compounds, biotin-avidin systems | Nanoparticle functionalization and stabilization | Reduce non-specific binding; improve circulation half-life; enable targeting moiety attachment |
The Scientist's Toolkit: Research Reagent Solutions
The advancement of bio-optics technologies relies on specialized research reagents and materials that enable precise manipulation of light-matter interactions at biological interfaces.
Nanoparticle Superstructures represent emerging platforms that combine nanoparticle assembly with photonic biosensing capabilities. These superstructures exhibit collective properties not present in individual nanoparticles, enabling enhanced sensitivity in detection systems integrated with deep learning algorithms for spectroscopy analysis [27].
CRISPR-Based Biosensing Platforms harness gene editing technology for diagnostic applications, capable of detecting specific nucleic acid sequences with single-base resolution. When integrated with optical or electrochemical readouts, these platforms achieve rapid, label-free detection of genetic disorders, viral mutations, and minimal residual disease, shifting diagnostics from centralized laboratories toward portable, decentralized applications [26].
Advanced Optical Materials including high-speed electro-optic modulators based on thin-film lithium niobate architectures achieve over 110 GHz bandwidth with low driving voltage, demonstrating how photonic devices originally conceived for telecommunications can be adapted for real-time biosignal processing in high-throughput genetic analysis and rapid pathogen detection [26].
The convergence of bioimaging, biosensing, and photonic therapies establishes a transformative framework for next-generation medical diagnostics and interventions. Several emerging trends will define the future trajectory of these core technology pillars.
Intelligent Adaptive Platforms will increasingly integrate artificial intelligence with biosensing and imaging to enable diagnostics that learn from each patient's data, refining both detection thresholds and therapeutic strategies in real time [26]. Advances in wearable and implantable biosensors will provide continuous molecular monitoring, adding a crucial temporal dimension to diagnostic assessments [26].
Materials Innovation will focus on smart nanomaterials that respond dynamically to disease-associated cues—releasing drugs, altering optical signatures, or modulating gene expression—bringing the field closer to closed-loop therapeutic systems [26]. The development of semimetallic and biodegradable nanoparticles will address limitations of traditional noble metal nanoparticles in terms of biocompatibility, clearance, and clinical translation.
Clinical Translation Pathways will require evolving regulatory frameworks to keep pace with these rapidly converging technologies, ensuring both safety and timely access to innovation [23]. Multifunctional platforms that combine diagnostic and therapeutic capabilities present unique regulatory challenges that must be addressed through coordinated solutions engaging academic researchers, industry partners, and regulatory bodies [23].
The integration of bio-optics technologies represents more than incremental improvement—it constitutes a fundamental shift toward precision medicine. By continuing to bridge molecular specificity, nanoscale functionality, and photonic precision, the scientific community can create diagnostic and therapeutic systems that are not only powerful but also accessible, adaptable, and truly transformative for patient care across global healthcare systems.
The field of biomedical imaging is undergoing a foundational transformation, moving beyond direct visual interpretation of images to a paradigm where computational extraction of latent information is paramount. This shift from qualitative "what you see" to quantitative "what computers reveal" is redefining the capabilities of optical technologies in biological research and drug development. Bio-optics, the science of generating and using light to interrogate biological systems, now increasingly relies on computational methods to transcend traditional physical limitations of imaging systems [2]. Where conventional imaging techniques once provided primarily morphological information, modern bio-optical systems coupled with advanced computation can reveal molecular composition, dynamic physiological processes, and functional interactions within living systems—all with unprecedented spatial and temporal resolution [28] [29].
This transition is driven by the recognition that biological systems operate across multiple spatial and temporal scales, and comprehending their complexity requires analytical approaches that extend beyond human visual perception. Computational interpretation enables researchers to convert optical signals into rich, multidimensional datasets, extracting biomarkers and functional parameters that are invisible to the naked eye [2] [30]. This technical guide explores the core technologies, methodologies, and analytical frameworks powering this information-driven shift, providing researchers and drug development professionals with both theoretical foundations and practical protocols for implementation.
Core Bio-Optical Technologies and Computational Integration
Advanced Imaging Modalities: Capabilities and Limitations
The information-driven shift leverages both established and emerging bio-optical technologies, each generating unique data types requiring specialized computational interpretation methods.
Table 1: Technical Specifications of Core Bio-Optical Imaging Modalities
| Technology | Spatial Resolution | Penetration Depth | Key Contrast Mechanisms | Primary Applications in Research |
|---|---|---|---|---|
| Optical Coherence Tomography (OCT) | 1-15 μm | 1-3 mm | Backscattering, polarization, flow | Ophthalmology [28], cardiology [28], oncology [28] |
| Photoacoustic Tomography (PAT) | 10-500 μm | 1-5 cm | Optical absorption | Vascular imaging [28], cancer detection [28], brain imaging [28] |
| Multiphoton Microscopy | 0.3-1.0 μm | 0.5-1 mm | Two-photon excitation fluorescence, SHG, THG | Deep tissue cellular imaging [2] [31], neuronal activity [2] |
| Bioluminescence Imaging (BLI) | 1-5 mm | Several cm | Luciferase-luciferin reaction | Cell tracking [31], gene expression monitoring [31], tumor growth [31] |
| Fluorescence Imaging (FLI) | 1-100 μm | 1-2 mm | Exogenous/endogenous fluorescence | Molecular targeting [31] [30], intraoperative guidance [31] |
| Raman Spectroscopy | 0.5-10 μm | 0.1-1 mm | Molecular vibrational signatures | Label-free molecular analysis [2] [14], cancer diagnostics [14] |
Optical Coherence Tomography (OCT) exemplifies the computational evolution in bio-optics. While conventional OCT provides structural information based on backscattered light, advanced computational techniques have enabled functional extensions including OCT angiography (OCTA), which uses moving-induced decorrelation of interference signals to image microvasculature without exogenous contrast agents [28]. Similarly, polarization-sensitive OCT (PS-OCT) computes birefringence properties to image fibrous tissues like collagen, while optical coherence elastography (OCE) calculates tissue mechanical properties by measuring displacement induced by applied pressure [28]. Each extension relies on sophisticated computational extraction of specific signal features that are not directly visible in raw OCT images.
Photoacoustic Tomography (PAT) represents a hybrid approach where optical energy absorption generates ultrasonic waves that are computationally reconstructed into images [28]. This combination provides optical contrast at ultrasonic resolution, overcoming the traditional depth limitation of pure optical microscopy. PAT's computational backbone lies in the inverse reconstruction algorithms that convert time-resolved acoustic detection into spatially resolved optical absorption maps, enabling visualization of hemoglobin concentration, oxygen saturation, and contrast agent distribution in deep tissues [28] [30].
The Space-Bandwidth Product Challenge and Computational Solutions
A fundamental limitation in conventional optical imaging is the space-bandwidth product (SBP), which defines the number of resolvable points in an image [32]. High-resolution imaging traditionally requires sacrificing field of view, while wide-field imaging compromises resolution. Computational approaches are overcoming this physical constraint through several innovative strategies:
- Spatial-domain methods capture multiple images to scale up the SBP, including array microscopy and multiscale optical imaging that tile the sample space [32].
- Frequency-domain methods augment SBP through Fourier ptychography and structured illumination microscopy, synthesizing high-resolution information from multiple low-resolution acquisitions [32].
- Wavefront-engineering methods utilize hardware- or computation-based approaches to correct lens aberrations across large fields of view [32].
These approaches collectively enable gigapixel-scale bioimaging, providing both cellular resolution and centimeter-scale fields of view—an impossibility with conventional optics alone [32]. The information capacity (N) of such systems can be quantified as N = SBP · log₂(1 + SNR), highlighting how both spatial information and signal-to-noise ratio contribute to overall system performance [32].
Computational Frameworks and Artificial Intelligence Integration
From Images to Quantitative Biomarkers
The computational interpretation of bio-optical data extends beyond image formation to the extraction of quantitative biomarkers with clinical and research significance. In OCT angiography, computational analysis transforms raw interference data into detailed vascular maps through decorrelation analysis of sequential B-scans [28]. Quantitative parameters then extracted from these maps include vessel density, foveal avascular zone area, vessel perimeter index, and branching coefficients—all providing objective measures of vascular health and pathology [28].
Similarly, in fluorescence and bioluminescence imaging, computational methods overcome limitations of these techniques through photon diffusion modeling and scatter correction algorithms to improve quantitative accuracy [31]. For bioluminescence imaging, which suffers from significant photon attenuation in tissue, 3D reconstruction algorithms incorporate optical properties of tissues to localize signal sources more accurately [31].
Table 2: Computational Methods for Quantitative Bio-Optical Analysis
| Analytical Challenge | Computational Solution | Output Parameters | Application Example |
|---|---|---|---|
| Vascular Quantification | OCTA decorrelation analysis | Vessel density, tortuosity, FAZ metrics | Diabetic retinopathy progression [28] |
| Molecular Specificity | Spectral unmixing algorithms | Concentration maps of chromophores | Oxygen saturation mapping [28] |
| Deep Tissue Localization | Photon migration models | 3D source reconstruction | Cancer metastasis tracking [31] |
| Multi-scale Integration | Image registration and fusion | Correlated structural-functional maps | Whole-brain imaging with cellular resolution [32] |
| Dynamic Process Analysis | Time-series computational analysis | Kinetic parameters, flow velocities | Neuronal activity monitoring [2] |
Artificial Intelligence and Machine Learning Applications
Artificial intelligence (AI) and machine learning (ML) have dramatically accelerated the information extraction capabilities of bio-optical technologies. These approaches are transforming every aspect of the imaging pipeline from acquisition to interpretation:
- Image Enhancement and Reconstruction: Deep learning models can reduce noise, enhance resolution, and accelerate image acquisition by reconstructing high-quality images from undersampled or low-quality data [2].
- Feature Identification and Segmentation: Convolutional neural networks automatically identify and segment biological structures in complex images, enabling high-throughput morphological analysis [2] [33].
- Predictive Modeling: ML algorithms correlate optical signatures with clinical outcomes or treatment responses, creating predictive biomarkers from complex, multidimensional optical data [2] [34].
In drug development, AI-powered analysis of bio-optical data is accelerating target validation and compound screening. The integration of cellular thermal shift assays (CETSA) with optical detection methods allows researchers to confirm direct target engagement of drug candidates in biologically relevant environments [35]. AI algorithms then analyze these complex datasets to quantify drug-target interactions, providing critical insights for lead optimization [35] [34].
Experimental Protocols and Methodologies
Protocol: Quantitative OCT Angiography for Microvascular Analysis
This protocol details the acquisition and computational analysis of OCTA data for quantitative assessment of microvascular networks, particularly in retinal and dermal applications.
Research Reagent Solutions and Essential Materials:
- Spectral-Domain OCT System: Provides high-speed, high-resolution cross-sectional imaging with stable phase information [28].
- Image Processing Software: Custom algorithms for motion correction, decorrelation calculation, and vessel segmentation [28].
- Computational Framework: Software environment for quantitative parameter extraction and statistical analysis [28].
Methodology:
- System Calibration: Ensure proper alignment of spectrometer-based SD-OCT system. Verify phase stability using a stationary mirror sample.
- Data Acquisition: Acquire repeated B-scans (typically 3-5) at the same retinal position. Implement high-speed scanning (≥70,000 A-scans/second) to minimize motion artifacts between consecutive B-scans.
- Motion Correction: Apply computational motion correction algorithms based on strip-based registration and histogram-based merging to eliminate tissue motion artifacts.
- Decorrelation Calculation: Compute decorrelation between consecutive B-scans using the formula: D = 1 - (I₁·I₂)/((I₁² + I₂²)/2), where I₁ and I₂ represent intensity values from sequential B-scans.
- Projection-Resolved Processing: Apply specialized algorithms to distinguish flowing elements at different depths, preserving the 3D vascular architecture.
- Vessel Segmentation: Use adaptive thresholding and machine learning-based classification to distinguish vascular elements from noise and static tissue.
- Parameter Quantification: Extract quantitative metrics including:
- Vessel density: Total length or area of perfused vasculature per unit area
- Fractal dimension: Complexity metric of vascular branching pattern
- Foveal avascular zone (FAZ) area: Quantify the central avascular region
- Vessel diameter index: Measure average vessel caliber
Computational Considerations: Implement batch processing for cohort studies with quality control metrics including signal strength index and motion artifact grading.
Protocol: Multiphoton Microscopy for Deep Tissue Cellular Imaging
This protocol describes the implementation of multiphoton microscopy for high-resolution imaging in scattering tissues, with computational analysis of cellular dynamics and tissue architecture.
Research Reagent Solutions and Essential Materials:
- Femtosecond Pulsed Laser: Titanium-sapphire laser system tuned to appropriate wavelength (typically 700-1100 nm) [2].
- High-Sensitivity Detectors: Non-descanned detectors optimized for emission wavelengths [2].
- Fluorescent Probes: Genetically encoded calcium indicators, cell tracers, or vital dyes specific to structures of interest [31].
Methodology:
- System Optimization: Align laser path and verify pulse width at sample plane. Calibrate laser power to balance signal-to-noise ratio with sample viability.
- Sample Preparation: For in vivo imaging, utilize surgical window chambers or cranial windows as appropriate. For ex vivo imaging, maintain physiological conditions.
- Three-Dimensional Data Acquisition: Acquire z-stacks with optimal step size (typically 1-5 μm) based on objective lens characteristics and scattering properties.
- Motion Stabilization: Implement real-time motion correction algorithms or post-acquisition image registration to compensate for tissue movement.
- Signal Extraction and Analysis:
- For calcium imaging, compute ΔF/F₀ where F₀ is baseline fluorescence
- Apply source separation algorithms (e.g., non-negative matrix factorization) to identify individual cells
- Extract temporal dynamics of identified regions of interest
- Morphological Analysis: Apply segmentation algorithms to identify cellular boundaries and quantify morphological parameters.
- Second Harmonic Generation (SHG) Analysis: For collagen imaging, compute alignment indices and fiber orientation distributions from SHG signals.
Advanced Computational Extensions: Implement 3D reconstruction and visualization for tissue architecture analysis. Apply machine learning classifiers for automated cell type identification based on morphological and dynamic features.
Visualization of Experimental Workflows and Data Relationships
Bio-Optical Data Processing Pipeline
Diagram 1: Bio-optical data processing workflow
Multi-Modal Imaging Integration Framework
Diagram 2: Multi-modal imaging integration
Implementation in Drug Development and Biomedical Research
Applications in Target Validation and Therapeutic Efficacy
The computational interpretation of bio-optical data provides critical insights throughout the drug development pipeline. In target validation, techniques like OCT and multiphoton microscopy enable non-invasive, longitudinal monitoring of disease progression and treatment response in animal models, generating rich datasets for evaluating target relevance [31]. For example, in oncology research, computational analysis of tumor vascular morphology and function through OCTA provides early biomarkers of treatment efficacy [28] [31].
In therapeutic efficacy assessment, the quantitative nature of computationally enhanced bio-optics enables precise measurement of treatment effects. Bioluminescence imaging with computational 3D reconstruction allows researchers to track cell populations over time, monitoring disease progression or regenerative processes [31]. The high sensitivity of BLI (detection of 100-1000 cells) combined with computational background suppression enables early detection of treatment response before morphological changes become apparent [31].
Technical Challenges and Implementation Barriers
Despite its promise, the implementation of computationally enhanced bio-optics faces several significant challenges:
- Data Management and Processing: High-SBP imaging generates massive datasets requiring substantial computational resources and efficient data management strategies [32].
- Algorithm Validation: Computational methods require rigorous validation against ground truth data to ensure biological relevance rather than algorithmic artifacts.
- Standardization and Reproducibility: Variability in acquisition parameters and processing algorithms complicates cross-study comparisons and multi-center trials [29].
- Regulatory Considerations: For clinical applications, computational approaches must meet regulatory standards for reliability and reproducibility, particularly for AI-based algorithms [29] [14].
The biophotonics industry is addressing these challenges through development of standardized data formats, open-source processing pipelines, and validation frameworks for computational methods [33].
Future Perspectives and Emerging Trends
The convergence of bio-optics with computational science continues to accelerate, with several emerging trends shaping future capabilities:
- Integration of AI and Machine Learning: AI is becoming embedded throughout the bio-optical pipeline, from optimized acquisition strategies to automated interpretation and prediction [2] [33].
- High-Throughput Computational Imaging: Advances in high-SBP imaging are enabling new applications in screening and phenotypic analysis where both high content and high throughput are required [32].
- Miniaturized and Portable Systems: Computational advances are enabling smaller, more affordable systems suitable for point-of-care applications and decentralized clinical trials [33] [14].
- Multi-Modal Data Integration: Computational frameworks are increasingly capable of integrating diverse optical data with other modalities (genomic, proteomic, clinical) to create comprehensive biological models [31] [30].
The global bio-optics market, valued at $2.03 billion in 2024 and projected to reach $3.31 billion by 2032, reflects the growing adoption of these computationally enhanced technologies across research and clinical applications [14]. This growth is particularly strong in medical diagnostics, where optical coherence tomography and Raman spectroscopy dominate application segments [14].
The transformation from direct visual interpretation to computational extraction represents a fundamental shift in how we derive biological insight from optical technologies. This paradigm enables researchers to move beyond structural assessment to functional and molecular characterization, revealing patterns and relationships that are inaccessible to human observation alone. For drug development professionals, these advances provide powerful tools for target validation, efficacy assessment, and treatment personalization. As computational methods continue to evolve in sophistication and integration with bio-optical technologies, they will undoubtedly unlock new dimensions of biological understanding and therapeutic innovation.
Advanced Bio-Optical Modalities and Their Transformative Applications
The diffraction limit of light, a physical barrier described by Ernst Abbe in 1873, has historically constrained traditional optical microscopy to a resolution of approximately 200-300 nanometers laterally and 500-800 nanometers axially, preventing the visualization of key subcellular structures and molecular processes [36]. Bio-optics, the interdisciplinary fusion of light-based technologies with biology and medicine, has overcome this fundamental limitation through the development of super-resolution microscopy (SRM) techniques [2]. These advancements have effectively narrowed the resolution gap between fluorescence microscopy and electron microscopy, enabling biological discovery at the nanoscale level and transforming approaches to drug development and diagnostic applications [36].
Unlike traditional imaging techniques that offer limited resolution regardless of magnification, super-resolution microscopy employs sophisticated optical strategies, specialized fluorophores, and computational reconstruction to achieve spatial resolution in the 10-150 nanometer range [36]. This technical whitepaper provides an in-depth examination of current super-resolution microscopy techniques, their operational principles, experimental requirements, and applications within biomedical research and drug development, with a specific focus on their advantages within the broader context of bio-optical innovation.
Core Super-Resolution Modalities: Principles and Trade-offs
Technical Foundations of Major SRM Techniques
Super-resolution microscopy encompasses several distinct technological approaches, each with unique mechanisms for overcoming the diffraction limit. Structured Illumination Microscopy (SIM) uses patterned illumination to generate moiré interference that encodes extended-resolution information, which is computationally extracted to reconstruct images with up to two-fold improvement in both lateral and axial resolution [36]. Stimulated Emission Depletion (STED) microscopy employs a doughnut-shaped depletion beam superimposed upon a confocal scanning laser beam to manipulate the point spread function (PSF), effectively squeezing the fluorescence emission volume to achieve resolution typically around 50 nanometers [37] [36].
Single-Molecule Localization Microscopy (SMLM) techniques, including PALM (Photoactivated Localization Microscopy) and STORM (Stochastic Optical Reconstruction Microscopy), rely on the temporal separation of stochastic fluorescence emissions from photoswitchable fluorophores [37]. By activating only a sparse subset of molecules at a time, their precise positions can be determined through centroid fitting, with thousands of frames combined to create a composite super-resolution image with localization precision of 10-20 nanometers [36]. Pixel reassignment methods (e.g., AiryScan, SoRA) represent a fourth category, extending confocal microscopy through detection path engineering and computational processing to achieve a moderate ∼1.4-fold resolution improvement [36].
Table 1: Comparison of Major Super-Resolution Microscopy Techniques
| Technique | Resolution (Lateral) | Live-Cell Capability | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| STED | ~50 nm (tunable) | Yes (with limitations) | No post-processing; direct imaging | High photodamage; complex alignment |
| SIM | 90-130 nm | Yes (2D-SIM: high; 3D-SIM: intermediate) | Fast; multi-color imaging (3-4 colors) | Susceptible to artifacts; high aberration sensitivity |
| SMLM (PALM/STORM) | ≥2× localization precision (10-20 nm) | Limited (fixed cells primarily) | Highest resolution; molecular counting | Very slow; high dye restrictions; complex sample prep |
| Pixel Reassignment (AiryScan, etc.) | 140-180 nm | Yes (low to high depending on configuration) | Easy implementation; works with standard dyes | Moderate resolution improvement |
Emerging Techniques and Innovations
Recent advancements continue to push the boundaries of super-resolution imaging. Super-resolution panoramic integration (SPI), introduced in 2025, represents a significant innovation that enables instantaneous generation of sub-diffraction images concurrently with high-throughput screening [38]. SPI leverages multifocal optical rescaling, high-content sample sweeping, and synchronized line-scan readout while preserving minimal post-processing and compatibility with conventional epi-fluorescence settings [38]. This technique achieves twofold resolution enhancement with unperturbed streaming throughput, acquiring up to 1.84 mm²/s (typically containing 5,000-10,000 cells/s) while maintaining approximately 120 nm resolution, making it particularly suitable for large-scale diagnostic applications and population-level biological analysis [38].
Other emerging approaches include MINFLUX, which combines elements of single-molecule localization with targeted excitation to achieve ultra-high precision down to 1-5 nanometers, and expansion microscopy, which physically enlarges biological specimens before imaging to achieve effective super-resolution on conventional microscopes [36]. The integration of machine learning and artificial intelligence for image reconstruction, interpretation, and optical design represents another frontier, enabling enhanced resolution with reduced photon damage and faster processing times [3] [18].
Table 2: Performance Characteristics of Super-Resolution Techniques
| Parameter | STED | SIM | SMLM | SPI (Emerging) |
|---|---|---|---|---|
| Temporal Resolution | Variable (low for cell-sized FOVs) | High (2D-SIM); Intermediate (3D-SIM) | Very low (fixed cells) | High (continuous streaming) |
| Photodamage | High (tunable with resolution) | Low to Intermediate | Very high (dSTORM) | Low (compatible with live cells) |
| Multi-color Capacity | 2-3 colors | 3-4 colors | 2 to multiple colors | Demonstrated with multiple labels |
| Throughput | Low | Intermediate | Very low | Very high (up to 1.84 mm²/s) |
| Sample Preparation Complexity | Intermediate | Low | High | Low |
Experimental Implementation and Workflows
Sample Preparation and Labeling Strategies
Successful super-resolution imaging requires meticulous attention to sample preparation, particularly for techniques with high dye restrictions such as SMLM. For fixed cell preparations, careful consideration of fixation methods is crucial - paraformaldehyde (typically 2-4% in PBS) is preferred over alcohols for better preservation of ultrastructure, with possible supplementation with low concentrations (0.1-0.5%) of glutaraldehyde for improved structural integrity, though this may increase autofluorescence requiring subsequent treatment with sodium borohydride [39].
The selection of appropriate fluorophores and labeling strategies is technique-dependent. For STED microscopy, bright, photostable dyes such as ATTO 590, ATTO 647N, or Abberior STAR dyes are recommended due to their high saturation intensity [36]. SMLM techniques require photoswitchable or photoactivatable fluorophores, with Alexa Fluor 647 being the most common for dSTORM, typically used in specialized blinking buffers containing primary thiols (e.g., β-mercaptoethylamine) and oxygen scavenging systems (e.g., glucose oxidase-catalase) to promote stochastic blinking [39] [36]. For live-cell compatible techniques like SPI or SIM, genetically encoded fluorescent proteins (e.g., GFP, RFP) or cell-permeable dyes can be utilized, with attention to minimizing phototoxic effects during extended imaging [38].
Protocol for High-Throughput Super-Resolution Imaging of Blood Smears Using SPI
The following detailed protocol, adapted from recent work on Super-resolution Panoramic Integration (SPI) microscopy, demonstrates the application of super-resolution techniques for high-content cellular analysis [38]:
Sample Preparation:
- Prepare peripheral blood smears on high-precision glass coverslips (No. 1.5 thickness).
- Label with wheat germ agglutinin (WGA) conjugates for membrane staining (5-10 µg/mL in PBS for 15 minutes at room temperature).
- Rinse gently with phosphate-buffered saline (PBS) and mount with appropriate imaging medium.
SPI System Configuration:
- Utilize an epi-fluorescence microscope (e.g., Nikon Eclipse Ti2-U) equipped with a 100×, 1.45 NA oil immersion objective.
- Configure concentrically aligned microlens arrays in both illumination and detection paths.
- Implement synchronized time-delay integration (TDI) sensor with line-scan readout rates exceeding 10 kHz.
- Set sample sweeping speed to achieve throughput of 9250 μm²/s.
Image Acquisition:
- Continuously introduce samples through the field of view with modest sweeping motion.
- Acquire raw data via instant TDI readout, producing initial sub-diffraction-limited resolution (~152 nm FWHM).
- For enhanced resolution, apply non-iterative rapid Wiener-Butterworth (WB) deconvolution, achieving final resolution of ~116 nm.
- Maintain consistent illumination intensity and detector gain throughout acquisition.
Data Analysis:
- Process acquired images for cellular segmentation and classification.
- Perform population analysis on >80,000 cells, identifying RBCs (93.1%), platelets (6.8%), and WBC subpopulations (neutrophils 49.3%, lymphocytes 38.8%, monocytes 11.9%).
- Generate quantitative morphological metrics for comparative analysis.
This protocol enables continuous super-resolution streaming with unperturbed high throughput, typically acquiring 5000-10,000 cells per second across a 2 mm × 2 mm area in approximately 60 seconds [38].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Super-Resolution Microscopy
| Reagent/Material | Function | Example Applications | Technical Notes |
|---|---|---|---|
| High-Precision Coverslips (No. 1.5) | Optimal optical performance | All super-resolution techniques | Thickness tolerance ±5 µm; required for oil immersion |
| Photoswitchable Fluorophores (Alexa Fluor 647) | Stochastic blinking for SMLM | dSTORM, PALM | Used with specialized blinking buffers |
| Genetically Encoded FPs (rsEGFP2, mEos) | Protein-specific labeling | Live-cell PALM | Photoconvertible or photoswitchable variants |
| STED-Compatible Dyes (ATTO 590, Abberior STAR) | High photostability for depletion | STED microscopy | High saturation intensity required |
| Oxygen Scavenging Systems (glucose oxidase) | Reduce photobleaching | SMLM, live-cell imaging | Extends fluorophore longevity |
| Primary Thiols (β-mercaptoethylamine) | Promote blinking in SMLM | dSTORM | Concentration optimization required |
| Mounting Media (Prolong Diamond, Mowiol) | Sample preservation and index matching | Fixed sample imaging | Refractive index matched to immersion oil |
Applications in Biomedical Research and Drug Development
Cellular and Subcellular Imaging
Super-resolution microscopy has revolutionized the visualization of subcellular structures that were previously inaccessible with traditional diffraction-limited microscopy. Applications include:
- Visualization of cytoskeletal elements including actin filaments, intermediate filaments, and microtubules with sufficient resolution to distinguish individual filaments and their organizational patterns [37].
- Mapping of organelle ultrastructure including mitochondrial cristae, endoplasmic reticulum organization, and nuclear pore complexes, providing insights into their functional states in health and disease [38].
- Analysis of protein-protein interactions and molecular clustering at the nanoscale, particularly in signaling complexes and membrane receptor organizations, with colocalization analysis at tens-of-nanometers precision [37].
Recent work with SPI microscopy has demonstrated particular utility for imaging diverse biological specimens including β-tubulin networks, mitochondrial organizations, and peroxisome distributions, achieving consistent two-fold resolution enhancement (~120 nm) while maintaining high throughput capabilities suitable for population-level analysis [38].
Drug Discovery and Development Applications
In pharmaceutical research, super-resolution techniques are increasingly employed throughout the drug development pipeline:
- Target identification and validation through nanoscale localization of drug targets within cellular compartments and examination of their spatial relationships with signaling machinery.
- Mechanism of action studies by visualizing drug-induced changes to subcellular structures and molecular complexes at unprecedented resolution.
- Therapeutic efficacy assessment in disease models, such as monitoring structural preservation in neurodegenerative models or analyzing tumor microenvironment changes in response to chemotherapeutic agents.
The high-throughput capabilities of techniques like SPI microscopy enable drug screening applications, as demonstrated by its use in analyzing morphological features of snowflake yeast clusters across evolutionary timepoints, revealing progressive cellular elongation with average aspect ratios increasing from ~1.30 (ancestors) to ~3.28 over 1000 transfers [38]. Such quantitative morphological analysis at population scale provides robust datasets for evaluating compound effects in screening campaigns.
Clinical Diagnostic and Translational Applications
Super-resolution microscopy is finding increasing application in clinical and diagnostic contexts:
- Hematological analysis as demonstrated by SPI imaging of peripheral blood smears, enabling differentiation of white blood cell subtypes (lymphocytes, neutrophils, monocytes) based on detailed membrane and cytoplasmic features at sub-diffraction resolution [38].
- Ophthalmic applications through adaptive optics ophthalmoscopy, which corrects imperfections in the eye's optics to achieve cellular-resolution imaging of retinal structures, including photoreceptors, microglia, and blood vessels, for monitoring disease progression and treatment response [13].
- Cancer diagnostics utilizing techniques like optical coherence tomography (OCT) and fluorescence imaging for detection and characterization of cancer cells, assessment of tumor margins, and monitoring treatment responses [14] [13].
The integration of fully automated OCT systems with computer vision algorithms and deep learning represents a particularly promising direction for high-throughput tissue screening in clinical research applications, enabling non-invasive, real-time monitoring of 3D tissue structures with detection success rates of 100% and rapid response times [13].
Implementation Considerations and Future Directions
Technical and Practical Implementation Factors
Implementing super-resolution microscopy requires careful consideration of multiple technical factors:
- Cost considerations: Super-resolution systems represent significant investments, ranging from $250,000 to over $1 million, with additional costs for service contracts, sample preparation stations, and supporting infrastructure [37].
- Infrastructure requirements: Laboratories must account for vibration isolation, temperature control, and low-light environments, with additional requirements for live-cell imaging such as CO₂ and humidity control [37].
- Expertise and training: These systems require extensive training for proper operation, with dedicated personnel often necessary for imaging, analysis, and maintenance, particularly in core facility settings [36].
- Data management: Super-resolution techniques, particularly SMLM methods, generate substantial datasets (>10,000 raw images for a single SMLM acquisition) requiring significant storage capacity and computational resources for processing and analysis [36].
Leasing arrangements present an alternative acquisition strategy for many laboratories, offering lower upfront costs, built-in support services, and upgrade flexibility that may be particularly advantageous for startup labs or core facilities testing demand for super-resolution capabilities [37].
Emerging Trends and Future Outlook
The field of super-resolution microscopy continues to evolve rapidly, with several emerging trends shaping its future development:
- Integration of machine learning and AI for enhanced image reconstruction, interpretation, and optical design, potentially enabling improved resolution with reduced photon exposure and faster processing times [3] [18].
- Miniaturization and portability of super-resolution systems for point-of-care applications, with developments in handheld imaging devices and portable spectroscopy systems enabling diagnostic capabilities outside traditional laboratory settings [14].
- Multimodal integration combining super-resolution microscopy with complementary techniques such as spatial transcriptomics, mass spectrometry, and electron microscopy for correlative analysis across multiple resolution scales and molecular modalities [38].
- Expansion of live-cell applications through reduced phototoxicity approaches, faster acquisition speeds, and improved fluorescent probes, enabling dynamic observation of cellular processes at the nanoscale over extended time periods [38] [36].
The continued innovation in super-resolution technologies, exemplified by developments such as SPI microscopy, ensures that bio-optics will remain at the forefront of biomedical research, providing methodological pathways for elucidating fundamental biological systems and advancing translational applications in diagnostics and therapeutic development [38]. As these technologies become more accessible and user-friendly, their integration into standard research and clinical workflows will further expand their impact across the life sciences and medical fields.
Photoacoustic imaging (PAI) emerges as a transformative hybrid modality within the bio-optics landscape, uniquely bridging optical contrast and acoustic resolution. This whitepaper delineates the core principles, technological advancements, and methodological protocols of PAI, framing it as a superior solution for researchers and drug development professionals seeking integrated structural and functional insight. By synergizing the high sensitivity of optical imaging with the deep-tissue penetration of ultrasound, PAI addresses critical limitations of traditional modalities, enabling non-invasive, high-resolution visualization of physiological processes. This guide provides a comprehensive technical overview, detailing system configurations, quantitative capabilities, and experimental workflows, thereby establishing PAI as a cornerstone technology in modern biomedical research and therapeutic development.
The field of biomedical imaging is characterized by a fundamental trade-off: optical techniques offer exquisite molecular contrast but suffer from limited penetration depth due to light scattering, while traditional radiological methods like CT and MRI provide deep anatomical views but often lack specific functional or molecular information [10]. Biophotonics, the interdisciplinary fusion of light-based technologies with biology and medicine, is rapidly transforming research and diagnostics by leveraging light to analyze and manipulate biological materials [2]. Within this innovative ecosystem, photoacoustic imaging (PAI) occupies a critical niche as a hybrid modality that effectively breaks the penetration-depth barrier of conventional optical microscopy.
PAI operates on the photoacoustic effect, where pulsed laser light is absorbed by endogenous chromophores (e.g., hemoglobin, melanin, lipids), generating a transient thermoelastic expansion that emits broadband ultrasonic waves [10] [40]. These waves, unscathed by optical scattering, are detected at the tissue surface and reconstructed to map the original optical absorption distribution with acoustic resolution. This core principle allows PAI to deliver high-contrast images of vascular morphology, tissue metabolism, and molecular targets at depths unreachable by purely optical methods [40]. Its capacity for label-free functional imaging—quantifying parameters like oxygen saturation (sO₂) and total hemoglobin concentration—positions it as an unrivaled tool for longitudinal studies in preclinical research and a promising modality for clinical diagnostics, particularly in oncology, neurology, and vascular diseases [40] [2]. As a bio-optics technology, PAI exemplifies key advantages such as non-contact measurement, high sensitivity, and the capacity for real-time, dynamic observation of biological processes [2].
Technical Foundations and System Configurations
Core Physical Principles
The initial pressure ((p0)) of the photoacoustic wave, which forms the basis of the image contrast, is governed by the following equation [10]: $${p}{0}=\Gamma {\eta }{th}{\mu }{a}F$$ Here, (\Gamma) is the Grüneisen parameter, a dimensionless constant representing the thermoelastic conversion efficiency of the tissue; ({\eta }{th}) is the photothermal conversion efficiency; ({\mu }{a}) is the optical absorption coefficient of the target chromophore; and (F) is the local optical fluence [10]. This equation highlights that PA signal intensity is directly proportional to the concentration of optical absorbers, enabling quantitative imaging of biomolecules such as hemoglobin.
The spatial resolution in PAI is system-dependent. In photoacoustic microscopy (PAM), the lateral resolution ((RL)) is determined by the focusing capability of either light or sound, while the axial resolution ((RA)) is governed by the bandwidth of the ultrasonic detector [10]: $$\begin{array}{c}{R}{L,{AR}}=0.71\frac{{v}{A}}{N{A}{A}\,\cdot\, {f}{c}},\,\quad{R}{L,{OR}}=0.51\frac{{\lambda }{O}}{N{A}{O}}\ {R}{A}=0.88\frac{{v}{A}}{\Delta {f}{A}}\end{array}$$ where ({v}{A}) is the speed of sound, (N{A}{A}) and (N{A}{O}) are the acoustic and optical numerical apertures, ({f}{c}) is the center frequency of the transducer, ({\lambda }{O}) is the optical wavelength, and (\Delta {f}{A}) is the bandwidth of the detected ultrasound signal [10].
Detection Technologies and System Architectures
PAI systems are primarily categorized based on their detection technology and image formation method. The choice of detector directly impacts bandwidth, sensitivity, and field of view.
- Ultrasonic Transducers: The most common detection method, which can be further divided into:
- Piezoelectric Transducers (PZT, PVDF, PMN-PT): Convert mechanical pressure into electrical signals via the piezoelectric effect. These can be configured as single elements for high-resolution microscopy or multi-element arrays for rapid tomographic imaging [10].
- Advanced MEMS Transducers: Including Piezoelectric Micromachined Ultrasonic Transducers (PMUTs) and Capacitive Micromachined Ultrasonic Transducers (CMUTs), which offer advantages in miniaturization, integration, and bandwidth [10].
- Optical Sensing: A contact-free alternative that detects ultrasound-induced changes in an optical interferometer.
The two primary system architectures are:
- Photoacoustic Microscopy (PAM): Employs a focused single-element transducer to achieve high spatial resolution (sub-micrometer to sub-millimeter) at shallow to moderate depths. It is subdivided into:
- Optical-Resolution PAM (OR-PAM): Lateral resolution is determined by a tightly focused laser spot, enabling sub-cellular imaging but limited to depths of about one optical transport mean free path (~1 mm in skin) [10] [41].
- Acoustic-Resolution PAM (AR-PAM): Lateral resolution is determined by the acoustic focus, allowing for deeper imaging (a few millimeters) beyond the optical diffusion limit [10].
- Photoacoustic Computed Tomography (PACT): Utilizes an array of ultrasonic detectors to capture signals from a large area simultaneously. Volumetric images are reconstructed using algorithms like delay-and-sum, time-reversal, or model-based approaches, providing a larger field of view and faster acquisition for deep-tissue imaging [10] [40].
Comparative Analysis with Traditional Imaging Modalities
The following table summarizes how PAI compares to established imaging techniques, underscoring its unique value proposition within the bio-optics arsenal.
Table 1: Quantitative Comparison of PAI with Traditional Imaging Modalities [40]
| Modality | Ionizing Radiation | Contrast Agent | Imaging Depth | Spatial Resolution | Temporal Resolution | Key Limitation for Biomedical Research |
|---|---|---|---|---|---|---|
| Photoacoustic Imaging (PAI) | No | Label-free (optional) | < 7 cm | 1 μm – 1 mm | ms – s | Limited whole-body imaging depth |
| Computed Tomography (CTA) | Yes | Iodine-based | Whole body | 0.5 – 1 mm | ms | Limited soft-tissue contrast, radiation dose |
| Magnetic Resonance Angiography (MRA) | No | Gadolinium-based (optional) | Whole body | 0.5 – 1 mm | s | Metal artifacts, high cost/complexity |
| Positron Emission Tomography (PET) | Yes | Radiolabeled tracers | Whole body | 4 – 5 mm | s – min | Poor spatial resolution, cannot delineate anatomy |
| Ultrasound (US) | No | Microbubbles (optional) | < 15 cm | 0.1 – 3 mm | ms – s | Low contrast for microvasculature, operator-dependent |
| Laser Speckle Contrast Imaging (LSCI) | No | Label-free | < 2 mm | 10 – 100 μm | ms – s | Cannot image deep vessels |
Advanced Techniques and Experimental Protocols
Key Research Reagent Solutions
Successful PAI experimentation relies on a suite of specialized reagents and materials. The following table details essential components of the "Scientist's Toolkit" for PAI.
Table 2: Essential Research Reagent Solutions for Photoacoustic Imaging
| Item | Function & Application in PAI |
|---|---|
| Tunable Pulsed Laser (e.g., OPO Lasers) | Provides short-pulse, wavelength-tunable light for exciting specific chromophores, enabling spectroscopic analysis for sO₂ and molecular imaging [10] [40]. |
| High-Frequency US Transducer (e.g., PZT, PMUT) | Detects the generated broadband ultrasound waves; center frequency and bandwidth directly determine spatial resolution [10] [41]. |
| Endogenous Chromophores (e.g., Hemoglobin, Melanin) | Native contrast agents for label-free imaging of vasculature, oxygen metabolism, and pigmented tissues [10] [40]. |
| Exogenous Contrast Agents (e.g., ICG, SWCNTs) | Synthetic dyes or nanoparticles that enhance contrast for specific molecular targets (e.g., integrins, proteases) or improve signal in weakly absorbing regions [40]. |
| Spectral Unmixing Algorithms | Computational tools that decompose mixed PA signals acquired at multiple wavelengths to quantify the concentration of individual chromophores [40] [42]. |
| Deep Learning Models (e.g., FRDGAN) | AI-based networks for image reconstruction, denoising, and super-resolution, significantly improving image quality and acquisition speed [41]. |
Protocol for High-Resolution Vascular Imaging and Quantification
This protocol outlines the procedure for in vivo imaging of mouse cerebral vasculature using OR-PAM, followed by deep learning-enhanced reconstruction, as adapted from recent literature [41].
Objective: To acquire high-resolution, quantitative maps of cerebral vasculature and oxygen saturation in a live mouse model.
Materials and Equipment:
- Tunable pulsed laser system (e.g., Nd:YAG/OPO) with a high pulse repetition rate (≥ kHz).
- Optical-resolution PAM system with a high-frequency ultrasonic transducer (e.g., 50-500 MHz).
- Anesthesia system (e.g., isoflurane vaporizer).
- Stereotaxic frame for head fixation.
- Physiological monitoring unit (e.g., for body temperature and ECG).
- Data acquisition (DAQ) system with high-speed digitizer.
- Computer with deep learning reconstruction software (e.g., FRDGAN model) [41].
Procedure:
Animal Preparation:
- Anesthetize the mouse using a recommended anesthetic (e.g., 1.5-2% isoflurane in oxygen).
- Secure the animal in a stereotaxic frame. Maintain body temperature at 37°C using a heating pad.
- Perform a craniotomy if required by the study protocol to reduce skull-induced signal attenuation.
- Apply ultrasound gel to the scalp or exposed skull to ensure acoustic coupling.
System Calibration and Setup:
- Calibrate the laser system. Select appropriate wavelengths (e.g., 570 nm and 578 nm for isosbestic points, 576 nm for sO₂ calculation) based on the absorption spectra of oxy- and deoxy-hemoglobin.
- Focus the laser beam and align the ultrasonic transducer confocally with the optical focus.
- Set the DAQ parameters (e.g., sampling rate, averaging) to optimize the signal-to-noise ratio.
Data Acquisition:
- Define the region of interest (ROI) over the cerebral cortex.
- Initiate a raster scan of the ROI. The laser pulse repetition rate and scanning step size will determine the acquisition time and spatial sampling density. For faster acquisition, a down-sampled (sparse) scan can be performed [41].
- Acquire PA data (A-lines) at each scanning point and at all pre-selected wavelengths.
Image Reconstruction and Processing:
- Basic Reconstruction: Apply a standard reconstruction algorithm (e.g., delay-and-sum) to the raw data to form a 2D or 3D image of the vasculature.
- Deep Learning Enhancement (for sparse data): Input the down-sampled, low-resolution image into a pre-trained FRDGAN model. The generator network, incorporating Fast Residual Dense Blocks (FRDB) and depth-wise separable convolutions, will output a high-quality, super-resolved image [41].
- Functional Quantification:
- Perform spectral unmixing on the multi-wavelength data to separate the contributions of oxy-hemoglobin (HbO₂) and deoxy-hemoglobin (HbR).
- Calculate oxygen saturation using the formula:
sO₂ = [HbO₂] / ([HbO₂] + [HbR]) * 100%. - Generate false-color sO₂ maps overlaid on the structural vascular image.
Validation and Analysis:
- Quantify image quality using metrics like Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM) when comparing reconstructed images to a ground truth [41].
- Analyze vascular parameters such as vessel diameter, density, and branching pattern from the structural image.
- Correlate sO₂ values with physiological states or experimental interventions.
Workflow Visualization
The following diagram illustrates the integrated experimental and computational workflow for high-resolution PAI, from data acquisition to quantitative analysis.
Diagram 1: PAI Experimental Workflow
Frontier Innovations and Clinical Translation
Technological Advancements
Recent innovations are rapidly expanding the capabilities and applications of PAI:
- High-Speed Volumetric Imaging: Systems employing single-shot volumetric imaging with ergodic relays can achieve real-time 3D imaging at up to 1 kHz volume rates, enabling the capture of rapid hemodynamic dynamics during occlusion and reperfusion [40].
- Large-Scale Synthetic Aperture Arrays: These systems expand the field of view and resolution for PACT, facilitating comprehensive imaging of larger anatomical structures such as the human breast or limb [40].
- Quantitative PAI (qPAI): Advanced algorithms are being developed to correct for the wavelength-dependent light fluence attenuation within tissue, enabling accurate, absolute quantification of chromophore concentrations rather than relative measurements. One approach uses known chromophores as internal fluence markers [42].
- All-Optical Scanners: Systems based on Fabry-Perot polymer film sensors allow for parallel detection without a coupling medium, providing superior sensitivity and bandwidth for detailed vascular imaging in clinical settings like the human foot [40].
Application in Peripheral Arterial Disease (PAD)
PAI demonstrates significant clinical potential in vascular diseases. In Peripheral Arterial Disease (PAD), it offers functional insights into microvascular health that complement traditional anatomical imaging. Emerging PAI techniques can visualize corkscrew-shaped collaterals, distinguish venous and arterial compartments, and quantify dynamic perfusion changes during physiological challenges, providing a powerful tool for diagnosis and monitoring therapeutic response [40]. The diagram below outlines the clinical value proposition of PAI in this context.
Diagram 2: PAI Clinical Value in PAD
Photoacoustic imaging stands as a paradigm-shifting technology within the bio-optics domain, effectively overcoming the historical limitations of pure optical and acoustic methods. Its capacity to deliver simultaneous high-resolution structural and functional information non-invasively and without ionizing radiation makes it an indispensable tool for biomedical researchers and drug developers. The ongoing integration of advanced detectors, high-speed acquisition schemes, and artificial intelligence promises to further solidify its role. As validation through large-scale studies progresses, PAI is poised to transition from a powerful research instrument to a central modality in precision medicine, enabling deeper insights into disease mechanisms and more effective evaluation of novel therapeutics.
Optical Coherence Tomography (OCT) has emerged as a transformative imaging technology in the biomedical field, providing non-invasive, high-resolution, cross-sectional imaging of biological tissues. Since its introduction in the early 1990s, OCT has revolutionized clinical diagnostics and biomedical research by enabling real-time, in-situ visualization of tissue microstructure with micrometer-scale resolution [43] [44]. The fundamental principle of OCT relies on low-coherence interferometry, typically using near-infrared light, to measure backscattered or backreflected light from tissue structures [45]. This technology fills a critical niche between high-resolution but shallow-depth optical microscopy and deep-penetrating but lower-resolution imaging modalities like ultrasound, MRI, and CT [44].
The significance of OCT in the context of bio-optics research lies in its unique ability to perform "optical biopsy" – providing detailed histological information without the need for tissue excision [44] [46]. This capability has positioned OCT as a powerful alternative to traditional imaging techniques, particularly in delicate tissues and organs where non-invasiveness is paramount. While ophthalmology remains the most established clinical application, OCT technology continues to expand into other medical fields, including oncology, cardiology, dermatology, and endoscopic procedures [47] [43] [46]. The evolution from time-domain to Fourier-domain OCT systems has dramatically improved imaging speeds and resolutions, enabling real-time visualization and functional extensions that provide insights into tissue physiology, composition, and pathology [45] [48].
Technical Foundations of OCT
Basic Principles and Imaging Mechanisms
OCT operates on the principle of low-coherence interferometry, analogous to ultrasound B-mode imaging but using light instead of sound waves [44]. The core system typically employs a Michelson interferometer configuration with a broadband light source split into two paths: a reference arm with a known path length and a sample arm directed toward the tissue of interest [45]. Backscattered light from the sample interferes with light from the reference arm only when the optical path lengths match within the coherence length of the source. By scanning the reference mirror or using Fourier-domain techniques, depth-resolved information (A-scans) is obtained, with multiple A-scans combined to form two-dimensional cross-sectional images (B-scans) [48] [44].
The axial resolution of OCT is determined by the coherence length of the light source and is inversely proportional to its bandwidth, as defined by the equation: Δz = (2ln2/π) · (λ²/Δλ), where λ is the central wavelength and Δλ is the spectral bandwidth [44]. This relationship highlights a fundamental advantage of optical techniques – utilizing broad bandwidth sources enables ultrahigh axial resolution in the 1-15 μm range, significantly superior to clinical ultrasound (100-200 μm) [44]. Transverse resolution, conversely, is determined by the focusing optics and is governed by standard diffraction limitations similar to conventional microscopy [44].
Evolution of OCT Technologies
OCT technology has evolved through three distinct generations, each offering significant improvements in imaging capabilities (Table 1).
Table 1: Comparison of OCT Technology Generations
| Feature | TD-OCT (Time-Domain) | SD-OCT (Spectral-Domain) | SS-OCT (Swept-Source) |
|---|---|---|---|
| Commercial Availability | 1996 [45] | 2006 [45] | 2012 [45] |
| Principle of Operation | Moving reference mirror measures different depth reflections sequentially [45] | Spectrometer analyzes interference spectrum via Fourier transform [45] | Tunable laser sweeps wavelengths; single photodetector captures interference [45] [48] |
| Central Wavelength | 810 nm [45] | 840 nm [45] | 1050-1080 nm [45] |
| Axial Resolution | 8-10 μm [45] [48] | 5-7 μm [45] [48] | 5.3-11 μm [45] [48] |
| Scan Speed | 400 A-scans/second [45] | 20,000-52,000 A-scans/second [45] | 100,000-236,000 A-scans/second [45] [48] |
| Key Advantages | Lower cost [48] | High resolution, fast, widely available [48] | Best depth penetration, reduced sensitivity roll-off [48] |
| Primary Limitations | Slow acquisition, motion artifacts [48] | Limited depth penetration [48] | Costly, limited availability [48] |
Time-Domain OCT (TD-OCT), the first generation, utilized a moving reference mirror to measure reflection times from different tissue depths. While revolutionary, its slow scanning speeds (400 A-scans/second) limited clinical utility [45]. The advent of Fourier-Domain techniques, including Spectral-Domain OCT (SD-OCT) and Swept-Source OCT (SS-OCT), marked a paradigm shift by eliminating moving parts and dramatically improving scan speeds and sensitivity [45] [48]. SD-OCT employs a broadband light source with a spectrometer to detect interference patterns, while SS-OCT uses a wavelength-swept laser and photodetector [48]. These advancements enabled real-time, high-resolution imaging critical for clinical applications.
Functional Extensions of OCT
Beyond structural imaging, several functional OCT extensions have been developed to extract additional biochemical and physiological information:
- Doppler OCT: Combines Doppler flowmetry with OCT to visualize blood vessels and measure blood flow velocity without contrast agents [44].
- OCT Angiography (OCTA): Uses motion contrast from flowing blood cells to generate detailed microvasculature maps, valuable for assessing retinal diseases and tumor vascularization [49] [48].
- Polarization-Sensitive OCT (PS-OCT): Detects birefringence in tissues like collagen and muscle fibers by measuring polarization state changes [44].
- Dynamic OCT: Analyzes signal fluctuations to extract information about metabolic activity and cellular dynamics [46].
These functional extensions significantly enhance the diagnostic capability of OCT beyond mere structural assessment, providing insights into tissue physiology, composition, and function.
OCT in Ophthalmology: Applications and Protocols
Retinal Imaging and Disease Management
Ophthalmology represents the most established clinical application of OCT, where it has become the standard of care for diagnosing and managing retinal diseases [45] [46]. The transparent ocular media allows optimal light penetration, making the retina particularly suitable for OCT imaging. In retinal diagnostics, OCT provides high-resolution cross-sectional images of retinal layers, enabling precise assessment of morphological changes associated with various pathologies [45] [48].
Table 2: OCT Applications in Ophthalmology
| Clinical Application | OCT Findings | Clinical Utility |
|---|---|---|
| Age-related Macular Degeneration (AMD) | Drusen, retinal pigment epithelium changes, intraretinal/subretinal fluid, choroidal neovascularization [48] | Diagnosis, treatment planning, and monitoring of anti-VEGF therapy response |
| Diabetic Retinopathy | Macular edema, retinal thickening, vitreomacular traction, microvascular changes [48] | Detection of clinically significant macular edema guiding treatment decisions |
| Glaucoma | Retinal nerve fiber layer (RNFL) thinning, optic nerve head structural changes [45] [49] | Early detection and monitoring of disease progression |
| Retinopathy of Prematurity (ROP) | Retinal vascularization extent, plus disease, tractional changes [50] | Objective quantification of disease severity and progression |
| Macular Holes & Epiretinal Membranes | Vitreomacular interface abnormalities, structural defects [45] | Surgical planning and postoperative assessment |
Experimental Protocol: Retinal OCT Imaging
For researchers implementing retinal OCT imaging, the following standardized protocol ensures consistent, high-quality results:
Sample Preparation:
- Dilate pupils using tropicamide 0.5% and phenylephrine 2.5% to ensure adequate field of view
- Position subject comfortably with proper chin and forehead rest to minimize motion artifacts
- Instruct subject to maintain fixation on internal target to stabilize gaze
Image Acquisition:
- Select appropriate scan pattern based on clinical question (e.g., radial, circular, or 3D cube scans)
- For macular assessment: Use 6mm radial line scan or 20°×20° 3D volume scan
- For glaucoma evaluation: Implement circular peripapillary scan around optic nerve head
- Adjust signal strength optimally (typically >7/10) while remaining within safe exposure limits
- Acquire multiple scans and utilize eye-tracking when available to enhance signal-to-noise ratio
Image Analysis:
- Assess image quality based on signal strength indicator and absence of artifacts
- Utilize automated segmentation software for retinal layer thickness measurements
- Compare quantitative parameters (RNFL thickness, total retinal thickness) with normative databases
- Perform longitudinal analysis by comparing with previous scans using follow-up mode
Quality Control:
- Ensure proper calibration of device according to manufacturer specifications
- Exclude images with significant motion artifacts or poor signal quality from analysis
- Maintain consistent scan protocols across longitudinal studies
This protocol has been validated in multiple clinical studies and provides reliable, reproducible results for both clinical and research applications [45] [49].
OCT in Oncology: Emerging Applications
Cancer Detection and Characterization
While ophthalmology remains the primary domain for clinical OCT applications, oncology represents a rapidly expanding frontier. OCT's high resolution enables visualization of architectural changes associated with early carcinogenesis, providing valuable diagnostic information without the need for biopsy in certain scenarios [43] [46]. The concept of "optical biopsy" is particularly valuable in tissues where conventional biopsy carries significant risk or in situations requiring repeated assessment.
In dermatologic oncology, OCT can non-invasively differentiate between benign and malignant skin lesions based on architectural disorganization and loss of normal stratification [43] [46]. Similarly, in endoscopic applications, OCT can identify dysplasia in Barrett's esophagus and early neoplasia in the gastrointestinal tract with high accuracy [43]. Intraoperative OCT has also shown promise in defining tumor margins during surgical resection, particularly in neurosurgery where distinguishing tumor from healthy tissue is challenging [43].
Experimental Protocol: Tumor Margin Assessment
The following protocol outlines the methodology for using OCT in tumor margin assessment, particularly relevant for intraoperative guidance:
Sample Preparation:
- For ex vivo tissue: Embed in optimal cutting temperature compound and section if correlative histology planned
- For in vivo imaging: Clean area of interest to remove debris or blood that may interfere with imaging
- Position OCT probe perpendicular to tissue surface at appropriate working distance
Image Acquisition:
- Select SS-OCT system for enhanced penetration in scattering tissues
- Set scan parameters to 3D volume acquisition with 500 × 500 A-scans over 4mm × 4mm area
- Use longer wavelength (1300nm) for improved penetration in highly scattering tissues
- Acquire reference images from normal adjacent tissue for comparison
- For intraoperative use, utilize sterile probe cover while maintaining optical clarity
Image Analysis:
- Evaluate architectural features: loss of layered structure, increased optical scattering, heterogeneous signal patterns
- Quantify optical parameters: attenuation coefficient, backscattering intensity
- Utilize automated classification algorithms when available to standardize interpretation
- Correlate with histopathological findings when possible to validate observations
Validation Methods:
- Process imaged tissue for standard histology (H&E staining)
- Register OCT images with corresponding histological sections
- Calculate diagnostic sensitivity and specificity using histology as gold standard
- Assess inter-observer agreement for qualitative OCT interpretation
This methodology has been successfully applied in studies of breast cancer margins, skin cancer detection, and gastrointestinal neoplasia [43].
Comparative Analysis: OCT vs Traditional Imaging
The positioning of OCT within the landscape of biomedical imaging techniques highlights its unique value proposition compared to established modalities (Table 3).
Table 3: OCT Compared to Other Imaging Modalities
| Imaging Modality | Resolution | Penetration Depth | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| OCT | 1-15 μm [44] | 1-3 mm [51] [44] | High resolution, real-time imaging, no ionizing radiation | Limited penetration depth |
| Magnetic Resonance Imaging (MRI) | 25-100 μm [44] | Unlimited [44] | Excellent soft tissue contrast, whole-body imaging | Low resolution, high cost, limited availability |
| Computed Tomography (CT) | 50-200 μm [44] | Unlimited [44] | Fast acquisition, excellent for bony structures | Ionizing radiation, poor soft tissue contrast |
| Ultrasound | 50-500 μm [44] | cm-range [44] | Real-time, portable, low cost | Lower resolution, operator dependent |
| Confocal Microscopy | 0.2-1 μm [44] | 0.2-0.5 mm [44] | Very high resolution | Very limited penetration, requires contact |
OCT occupies a unique niche with its combination of micron-scale resolution and millimeter-scale penetration, effectively bridging the gap between conventional microscopy and macroscopic imaging techniques. Unlike histology, which provides superior resolution but requires tissue excision and processing, OCT enables non-destructive, in-situ evaluation of tissue microstructure [44]. This advantage is particularly valuable for longitudinal studies and intraoperative guidance where real-time information is critical.
Advanced Innovations and Future Directions
Technological Advancements
Recent innovations in OCT technology continue to expand its capabilities and applications:
- Long-Range OCT: Novel akinetic all-semiconductor lasers with ultra-narrow instantaneous linewidths enable imaging ranges up to 53 meters while maintaining high resolution, opening possibilities for industrial and remote sensing applications [47].
- Portable and Community-Based Systems: Devices like the SightSync OCT feature technician-free operation with secure data transfer, potentially revolutionizing screening programs in underserved areas [48].
- Ultra-Widefield OCT: Systems capable of capturing peripheral retinal pathology are enhancing assessment of conditions like retinopathy of prematurity and diabetic retinopathy [50].
- Enhanced Resolution: Improvements in light source technology continue to push resolution boundaries, with some research systems achieving subcellular resolution [44].
Artificial Intelligence Integration
The integration of artificial intelligence (AI) with OCT represents one of the most significant advancements, addressing key challenges in image interpretation and analysis:
- Automated Segmentation: Deep learning algorithms enable precise identification and quantification of retinal layers, pathological features, and structural abnormalities [48].
- Disease Classification: Convolutional neural networks can distinguish between disease stages with high accuracy, achieving area under curve (AUC) values of 0.94 for diabetic macular edema detection [48].
- Predictive Analytics: AI models can predict disease progression and treatment response based on longitudinal OCT data [48].
- Image Enhancement: Machine learning techniques reduce noise and artifacts, improving diagnostic quality especially in challenging imaging situations [48].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for OCT Studies
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Swept-Source Laser | Light source for SS-OCT systems | Akinetic all-semiconductor laser, 1050-1300nm wavelength, 50kHz-400kHz sweep rate [47] |
| Spectrometer | Detection component for SD-OCT systems | High-speed line-scan camera, broad spectral range matching light source [45] |
| Reference Mirror | Critical component for interferometry | Precision movable mirror (TD-OCT) or fixed mirror (FD-OCT) with controlled path length [45] |
| Balanced Photodetector | Interference signal detection | InGaAs photodiodes, DC to 400MHz bandwidth, <5 pW/√Hz noise-equivalent power [47] |
| Galvanometer Scanners | Beam steering for transverse scanning | Dual-axis mirrors, precise angular control for raster scanning patterns [47] |
| Optical Fibers | Light delivery in sample and reference arms | Single-mode fibers maintaining polarization, appropriate for wavelength range [45] |
| MATLAB Scripts | Custom image processing and analysis | Automated segmentation, quantitative parameter extraction, motion correction [49] |
| AI/ML Algorithms | Automated image classification and analysis | ResNet, CNN-RNN hybrid models for pathology detection and segmentation [48] |
Optical Coherence Tomography represents a paradigm shift in high-resolution biomedical imaging, effectively bridging the gap between conventional microscopy and macroscopic imaging techniques. Its non-invasive nature, capability for real-time imaging, and continuous technological advancements have established OCT as an indispensable tool in ophthalmology and a promising modality in oncology. The evolution from time-domain to Fourier-domain systems has dramatically improved imaging speeds and resolutions, while functional extensions like OCT angiography and polarization-sensitive OCT provide complementary physiological information.
The integration of artificial intelligence with OCT imaging is poised to revolutionize diagnostic capabilities, enabling automated analysis, enhanced detection sensitivity, and predictive analytics. Combined with innovations in portability and accessibility, these advancements promise to expand OCT's impact beyond traditional clinical settings into community-based screening and point-of-care applications. As OCT technology continues to evolve, its role in both basic research and clinical practice will undoubtedly expand, solidifying its position as a cornerstone of modern biomedical imaging within the broader context of bio-optics research.
Raman spectroscopy has emerged as a powerful analytical technique in the bio-optics landscape, offering distinct advantages over traditional imaging modalities for molecular fingerprinting. Unlike conventional biomedical imaging techniques that primarily provide structural information, Raman spectroscopy delivers detailed molecular composition data by probing the vibrational states of molecules through inelastic light scattering [52]. This capability for non-destructive, label-free chemical analysis positions Raman technology as a transformative tool in biological research and drug development, particularly where understanding biochemical composition at the molecular level is paramount.
The bio-optics field has witnessed significant growth, with the global market valued at $2.03 billion in 2024 and projected to reach $3.31 billion by 2032, reflecting a compound annual growth rate (CAGR) of 6.3% [14]. Within this expanding market, Raman spectroscopy has established itself as a dominant technology, especially in life sciences applications where its non-destructive nature, minimal sample preparation requirements, and ability to analyze samples in various states (solid, liquid, or gas) provide significant advantages over traditional analytical methods [53]. The Raman spectroscopy technology market itself is projected to grow at a CAGR of 8% from 2025 to 2032, underscoring its increasing adoption across multiple sectors [53].
When evaluated against traditional biomedical imaging techniques, Raman spectroscopy addresses several limitations inherent in conventional approaches. While established modalities like Computed Tomography Angiography (CTA), Magnetic Resonance Imaging (MRI), and Positron Emission Tomography (PET) excel at providing anatomical localization and structural information, they typically cannot directly determine chemical composition, often involve radioactivity (in the case of CTA and PET), and may have insufficient spatial resolution for molecular-level analysis [52]. In contrast, Raman techniques provide molecular specificity without ionizing radiation, with theoretical spatial resolution limits of 200-500 nm [52], enabling researchers to investigate biochemical processes at the subcellular level.
Theoretical Fundamentals
Principles of Raman Scattering
Raman spectroscopy is founded on the inelastic scattering of monochromatic light, typically from a laser source, when it interacts with molecular vibrations or other excitations in a system [53]. The fundamental principle involves energy transfer between incident photons and sample molecules, resulting in scattered photons with frequencies different from the incident light. This energy shift provides a characteristic molecular fingerprint that is unique to the specific molecular bonds and symmetry [52].
The Raman effect occurs when photons collide with matter, with most undergoing elastic scattering (Rayleigh scattering) where the scattered light frequency remains identical to the incident light [52]. A small fraction of photons (approximately 1 in 10^6 to 10^9) undergo inelastic collisions, producing Raman scattering with shifted frequencies [54]. Two types of Raman scattering exist: Stokes scattering, where the scattered photon has lower energy than the incident photon, and anti-Stokes scattering, where the scattered photon has higher energy [52]. The Stokes lines are typically more intense than anti-Stokes lines because molecules are more populated at the ground vibrational level at ordinary temperatures [55]. The frequency difference between incident and scattered light, known as the Raman shift, is proportional to the energy difference between initial and final molecular states and is measured in wavenumbers (cm⁻¹) [52].
The entire process can be understood through both quantum mechanical and classical theoretical frameworks. According to quantum theory, Raman scattering involves transitions between quantized energy levels through virtual states [55]. Classical theory describes the phenomenon through the induction of a dipole moment via interaction between molecular charges and an external electric field, leading to molecular polarization [55].
Coherent Raman Scattering Mechanisms
Coherent Raman Spectroscopy (CRS) encompasses advanced techniques including Coherent Anti-Stokes Raman Scattering (CARS) and Stimulated Raman Scattering (SRS) that overcome the inherent weakness of spontaneous Raman scattering through nonlinear optical processes involving multiple light beams [52]. These techniques employ laser fields to coherently drive molecular vibrations, significantly enhancing the Raman signal intensity.
In CARS, a pump beam (frequency ωp) and a Stokes beam (frequency ωS) interact with the sample to generate a coherent anti-Stokes signal at frequency 2ωp - ωS when the frequency difference (ωp - ωS) matches a molecular vibration [52]. This process produces a signal that is several orders of magnitude stronger than spontaneous Raman scattering, enabling faster imaging speeds and reduced data acquisition times. The CARS signal is generated in a directional beam, facilitating efficient signal collection.
SRS relies on the stimulated Raman effect, where the simultaneous presence of pump and Stokes beams modifies the Raman scattering probability [52]. This manifests as a measurable intensity loss in the pump beam (Stimulated Raman Loss) or gain in the Stokes beam (Stimulated Raman Gain). Unlike CARS, SRS spectra are free from non-resonant background interference and directly resemble spontaneous Raman lineshapes, simplifying spectral interpretation.
The following diagram illustrates the fundamental energy level diagrams and scattering processes for both spontaneous and coherent Raman techniques:
Figure 1: Energy level diagrams comparing spontaneous Raman scattering and coherent Raman processes (CARS/SRS)
Technical Comparison with Traditional Imaging Techniques
Performance Metrics Analysis
The comparative advantages of Raman techniques over traditional biomedical imaging methods become evident when analyzing key performance metrics across multiple dimensions. The following table summarizes the quantitative and qualitative differences:
Table 1: Comparison of Raman spectroscopy with traditional biomedical imaging techniques
| Technique | Spatial Resolution | Molecular Specificity | Radiation Exposure | Key Limitations | Primary Applications in Bio-optics |
|---|---|---|---|---|---|
| Raman Spectroscopy | 200-500 nm (theoretical) [52] | High (direct chemical composition analysis) [52] | None [52] | Weak signal intensity, fluorescence interference [52] | Cellular analysis, plaque composition, drug distribution [52] |
| CARS/SRS | ~250-400 nm [52] | High with reduced non-resonant background (SRS) [52] | None [52] | Complex instrumentation, higher cost [52] | Real-time tissue imaging, lipid metabolism studies [52] |
| MRI | 100 μm - 1 mm [52] | Low (requires contrast agents) [52] | None (magnetic fields) [52] | Poor molecular specificity, expensive [52] | Anatomical imaging, soft tissue contrast [52] |
| CTA | 500 μm - 1 mm [52] | Low (structural information only) [52] | X-ray radiation [52] | Radioactivity, cannot detect chemical composition [52] | Vascular imaging, aneurysm detection [52] |
| PET | 1-2 mm [52] | Moderate (with radioactive tracers) [52] | Radioactive tracers [52] | Radiation exposure, requires tracers [52] | Metabolic activity, tumor detection [52] |
| OCT | 1-15 μm [52] | Low (structural information) [52] | None [52] | Limited penetration depth, poor molecular specificity [52] | Retinal imaging, endoscopic procedures [52] |
Bio-optics Market Positioning
The growing adoption of Raman spectroscopy within the bio-optics sector is reflected in market analysis data. Raman technology dominates the spectroscopy segment of the bio-optics market, which is projected to grow from USD 2.03 billion in 2024 to USD 3.31 billion by 2032, at a CAGR of 6.3% [14]. Several key factors drive this growth trajectory:
Application Diversity: Raman spectroscopy spans multiple domains including life sciences (cellular analysis and disease diagnosis), materials science (material properties and phase identification), carbon materials (graphene and nanotubes characterization), and semiconductors (strain analysis and defect characterization) [53]. The life sciences segment represents the fastest-growing application area, driven by advancements in diagnostics and personalized medicine [53].
Technology Integration: The integration of artificial intelligence and machine learning with Raman spectroscopy has significantly enhanced data analysis capabilities, improving accuracy and facilitating real-time decision-making across various applications [53] [56]. Deep learning approaches have demonstrated particular utility in spectral preprocessing, classification, and quantitative prediction tasks [56].
Miniaturization Trend: Advances in micro-optics and sensor technology have led to the development of portable and handheld Raman devices, expanding applications for on-site analysis in clinical, pharmaceutical, and environmental settings [53].
Regional market dynamics further highlight the global adoption of Raman technologies, with Europe currently dominating the bio-optics market, followed by North America and the Asia-Pacific region, the latter representing a significant growth opportunity driven by rapid industrialization and increasing healthcare investments [53] [14].
Advanced Raman Techniques and Methodologies
Signal Enhancement Strategies
The inherent weakness of the Raman scattering effect has driven the development of several enhancement strategies to improve signal-to-noise ratios and detection sensitivity:
Surface-Enhanced Raman Spectroscopy (SERS) utilizes nanostructured metallic surfaces (typically gold or silver) to amplify Raman signals through plasmonic effects, enabling detection of analytes at extremely low concentrations [53] [55]. The enhancement mechanisms involve both electromagnetic effects (local field enhancement) and chemical effects (charge transfer). SERS has demonstrated particular utility in forensic trace analysis, enabling identification of minute quantities of substances such as drugs, explosives, and biochemical agents [55].
Tip-Enhanced Raman Spectroscopy (TERS) combines scanning probe microscopy with Raman spectroscopy to achieve nanoscale spatial resolution, overcoming the diffraction limit of conventional Raman systems [53]. By using a metallicized scanning probe tip to locally enhance the electromagnetic field, TERS can provide chemical information with spatial resolution below 10 nm, making it invaluable for characterizing nanomaterials and biological systems at the molecular level.
Spatially Offset Raman Spectroscopy (SORS) enables subsurface chemical analysis by collecting Raman spectra at different distances from the excitation point, allowing depth profiling of turbid samples such as biological tissues [55]. This technique has shown promise for non-invasive medical diagnostics, including bone disease detection and cancer margin assessment during surgery.
Experimental Design Considerations
Effective implementation of Raman spectroscopy requires careful consideration of several experimental parameters:
Laser Excitation Wavelength Selection represents a critical design choice that significantly influences spectral quality. Shorter excitation wavelengths (e.g., 532 nm) provide stronger Raman signals due to the ν⁴ dependence of scattering efficiency but are more prone to fluorescence interference, which can overwhelm the Raman signal [54]. Longer wavelengths (e.g., 785 nm or 1064 nm) reduce fluorescence but yield weaker Raman signals, often requiring more sensitive detectors [54]. The optimal excitation wavelength must be determined empirically based on the sample properties.
Spatial Resolution Optimization in micro-Raman systems follows diffraction-limited optics principles. The theoretical spatial resolution (p) and Airy disk diameter (D_Airy) can be calculated as:
- D_Airy = 1.22 × λ / NA
- p = 0.61 × λ / NA where λ is the excitation wavelength and NA is the numerical aperture of the objective [54]. For example, using 532 nm excitation with a 0.9 NA objective yields a theoretical spatial resolution of approximately 360 nm, while 785 nm excitation with the same objective provides about 530 nm resolution [54].
Sample Preparation Methodologies vary significantly based on sample type and analytical goals. For biological samples, careful preparation is essential to preserve native biochemical states while minimizing interfering signals. Common approaches include:
- Minimal Processing: Direct analysis of native tissues or cells to avoid artificial alterations [52]
- Substrate Optimization: Selection of low-fluorescence substrates such as calcium fluoride or optimized glass slides [54]
- Environmental Control: Maintenance of physiological conditions (temperature, humidity, pH) for live cell analysis [52]
The following workflow diagram illustrates a generalized experimental protocol for Raman spectroscopic analysis:
Figure 2: Generalized workflow for Raman spectroscopy experimental protocols
Research Reagent Solutions and Essential Materials
Successful implementation of Raman spectroscopy in biological research requires specific reagents and materials optimized for vibrational spectroscopy. The following table details essential components for Raman-based experiments:
Table 2: Essential research reagents and materials for Raman spectroscopy applications
| Category | Specific Materials/Reagents | Function/Purpose | Application Examples |
|---|---|---|---|
| Laser Sources | Argon ion lasers (488, 514 nm), Diode-pumped solid-state lasers (532, 785 nm), Ti:Sapphire lasers (tunable) [55] | Monochromatic excitation source for Raman scattering | Cellular imaging, material characterization |
| SERS Substrates | Gold/silver nanoparticles, Nanostructured metal surfaces, Polymer-embedded nanoparticles [55] | Signal enhancement via plasmonic effects | Trace detection, single-molecule spectroscopy |
| Reference Standards | Silicon wafer (520.7 cm⁻¹ peak), Toluene, Cyclohexane [54] | Instrument calibration and wavelength verification | Spectral calibration, system validation |
| Sample Substrates | Calcium fluoride slides, Low-fluorescence glass, Aluminum-coated slides [54] | Sample support with minimal background interference | Tissue sections, cell cultures |
| Nanoparticles for TERS | Gold-coated AFM tips, Silver nanowires [53] | Nanoscale spatial resolution enhancement | Single-cell analysis, nanomaterial characterization |
| Chemometric Tools | Principal Component Analysis (PCA), Partial Least Squares Discriminant Analysis (PLS-DA), Support Vector Machines (SVM) [55] | Multivariate data analysis and pattern recognition | Disease classification, spectral interpretation |
Applications in Biomedical Research and Drug Development
Cardiovascular Disease Diagnostics
Raman spectroscopy has demonstrated significant potential in cardiovascular disease research, particularly in the analysis of atherosclerotic plaques. Traditional imaging modalities like CTA and IVUS can locate plaque and observe blood vessel structure but cannot accurately determine the chemical composition of lesions [52]. Raman techniques precisely detect plaque composition, enabling differentiation between stable and vulnerable plaques based on lipid core size, collagen content, and inflammatory cell infiltration [52]. This molecular fingerprinting capability provides crucial information for assessing plaque rupture risk and guiding therapeutic interventions.
The label-free nature of Raman spectroscopy facilitates real-time monitoring of disease progression and treatment response without requiring contrast agents or radioactive tracers [52]. This advantage is particularly valuable in tracking the efficacy of lipid-lowering therapies and evaluating stent integration with vascular tissue. Furthermore, Raman systems can be integrated with endoscopic platforms for in situ analysis during minimally invasive procedures, potentially revolutionizing cardiovascular diagnostics and interventional guidance.
Pharmaceutical Applications
In drug development, Raman spectroscopy serves as a powerful tool for multiple aspects of the pharmaceutical pipeline. A prominent application involves accelerating the development of complex medicinal products, including the assessment of cutaneous pharmacokinetics and determination of topical drug bioavailability and bioequivalence [57]. These applications leverage Raman's non-destructive nature to monitor drug permeation through skin layers and quantify active pharmaceutical ingredient concentrations in various tissue compartments.
Additional pharmaceutical applications include:
- Formulation Analysis: Characterization of polymorphic forms, monitoring of solid-state transformations, and quantification of drug-excipient interactions [53]
- Process Analytical Technology: Real-time monitoring of manufacturing processes such as blending, granulation, and coating to ensure product quality [53]
- Drug Delivery Systems: Evaluation of drug release profiles from nanocarriers and implantable devices through molecular fingerprinting [57]
The integration of deep learning algorithms with Raman spectroscopy has further enhanced pharmaceutical applications by enabling automated spectral analysis, prediction of formulation properties, and real-time quality control decision-making [56].
Cancer Diagnostics and Research
Raman spectroscopy has emerged as a valuable tool in oncology, with the cancer diagnostics segment dominating the bio-optics application market [14]. The technology's ability to provide molecular-level information without exogenous labels makes it ideal for identifying cancer biomarkers, characterizing tumor margins, and monitoring treatment responses at the biochemical level.
Specific oncological applications include:
- Intraoperative Margin Assessment: Differentiation between cancerous and healthy tissue during surgical procedures through rapid spectral acquisition and machine learning classification [14]
- Cellular Analysis: Identification of metabolic changes associated with oncogenic transformation and therapeutic resistance mechanisms [56]
- Therapeutic Monitoring: Tracking drug distribution within tumor tissues and assessing treatment efficacy through molecular fingerprint evolution [57]
The non-destructive nature of Raman analysis enables longitudinal studies of the same cells or tissue samples, providing insights into dynamic biological processes and enabling more predictive in vitro models for drug screening [56].
Future Perspectives and Emerging Trends
The field of Raman spectroscopy continues to evolve rapidly, driven by technological innovations and expanding application domains. Several emerging trends are positioned to shape future developments:
Artificial Intelligence Integration: Deep learning approaches are revolutionizing Raman spectral analysis by overcoming limitations of traditional chemometric techniques [56]. Convolutional neural networks (CNNs) have demonstrated superior performance in classification tasks, often outperforming traditional methods that rely on manually preprocessed spectra [56]. The ongoing development of specialized neural network architectures for spectral analysis will further enhance accuracy, reduce computational demands, and improve model interpretability.
Multimodal Imaging Platforms: Integration of Raman spectroscopy with complementary imaging modalities represents a growing trend in advanced bio-optics. Combining Raman with techniques like optical coherence tomography, multiphoton microscopy, or mass spectrometry provides correlated structural, chemical, and molecular information from the same sample [3]. These hybrid systems offer comprehensive sample characterization while leveraging the respective strengths of each technology.
Miniaturization and Point-of-Care Applications: The development of portable and handheld Raman devices is expanding applications beyond traditional laboratory settings [53]. Field-deployable systems enable environmental monitoring, food safety testing, and clinical diagnostics in resource-limited settings. The growing emphasis on point-of-care applications aligns with broader healthcare trends toward decentralized testing and personalized medicine [14].
Advanced Computational Methods: Emerging computational approaches address longstanding challenges in Raman spectroscopy, including model transfer between instruments, standardization of preprocessing protocols, and interpretation of complex biological spectra [56]. Physics-informed neural networks and other hybrid models that incorporate domain knowledge with data-driven learning show particular promise for improving analytical robustness across diverse sample types and experimental conditions.
As these trends converge, Raman spectroscopy is poised to become an increasingly indispensable tool in the bio-optics arsenal, offering unprecedented capabilities for molecular fingerprinting across fundamental research, translational medicine, and clinical diagnostics.
The evolution of optical microscopy from a rudimentary observational tool into a powerful bioanalytical platform represents a paradigm shift in biological research. Dynamic live-cell imaging stands as an essential pillar in modern science, offering unprecedented insights into cellular processes, yet it confronts fundamental limitations imposed by traditional imaging techniques. Bio-optics approaches, specifically light-sheet fluorescence microscopy (LSFM) and multi-photon microscopy, have emerged as transformative solutions that overcome the critical trade-offs between spatial resolution, temporal resolution, sample health, and imaging depth that plague conventional methods [58] [59]. This technical guide examines the core principles, current implementations, and experimental protocols of these advanced modalities, framing them within the broader thesis that bio-optics provides superior alternatives to traditional imaging for investigating dynamic biological systems.
The limitations of traditional laser scanning confocal microscopy are particularly pronounced in live-cell imaging. Conventional techniques illuminate the entire sample during acquisition, generating substantial out-of-focus light that causes phototoxicity and photobleaching – effects highly nonlinear to excitation intensity that compromise sample viability and data quality [58]. Furthermore, the point-scanning approach of confocal systems creates a fundamental speed barrier for volumetric imaging, while scattering and absorption in biological tissues restrict practical imaging depth to superficial layers [58] [60]. These constraints have driven the development of bio-optics solutions that fundamentally reengineer the relationship between illumination and detection.
Technical Foundations and Comparative Advantages
Light-Sheet Fluorescence Microscopy (LSFM)
Core Principle and Mechanism
Light-sheet microscopy operates on an elegant orthogonal separation of illumination and detection paths. Unlike traditional epi-fluorescence techniques where excitation and detection occur through the same objective, LSFM utilizes a dedicated illumination objective to launch a thin sheet of laser light that selectively excites fluorophores only within the focal plane of a detection system positioned at a 90-degree angle [58] [61]. This optical arrangement provides intrinsic 3D optical sectioning without the need for physical apertures or computational optical sectioning, thereby eliminating out-of-focus blur while dramatically reducing light exposure to the sample [61].
The fundamental advantage of this architecture lies in its dramatically improved spatial duty cycle – the proportion of time fluorophores are excited during exposure. Because LSFM illuminates an entire plane simultaneously rather than point-scanning, it achieves similar signals with orders of magnitude lower laser powers than point-scanning confocal microscopes [58]. This efficiency translates directly to reduced photobleaching and phototoxicity, enabling extended time-lapse observations of delicate biological processes from embryogenesis to neural dynamics over hours or days [58] [61].
Implementation Variants
Modern LSFM implementations have diversified to address specific biological challenges. Selective Plane Illumination Microscopy (SPIM), the original LSFM configuration, typically employs one or two static or scanned light-sheets from the side [61]. Lattice Light-Sheet Microscopy utilizes optically engineered Bessel or Airy beams to create thinner sheets with extended depth of focus, enabling high-resolution imaging with minimal scattering [58]. Open-Top Light-Sheet systems permit imaging of large, cleared tissues from multiple angles while accommodating additional experimental apparatus [58]. Recent innovations include two-photon light-sheet systems that combine the gentle optical sectioning of light-sheet illumination with the superior penetration of multi-photon excitation [62].
Multi-Photon Microscopy
Multi-photon microscopy operates on a fundamentally different excitation principle than single-photon techniques. In n-photon excitation, n photons (each with approximately 1/n the energy required for single-photon excitation) arrive simultaneously at a fluorophore, combining their energies to promote electron transition to an excited state [60]. This nonlinear process occurs with significant probability only at the focal volume where photon density is highest, creating intrinsic 3D resolution without the need for a detection pinhole [60].
The practical implementation of this principle requires ultrafast pulsed lasers (typically femtosecond pulse widths) that deliver high peak powers with moderate average power to enable efficient nonlinear excitation while avoiding thermal damage to biological samples [60]. Two-photon excitation of visible-light-emitting fluorophores typically uses near-infrared (NIR) wavelengths (700-1100 nm), while three-photon imaging extends further into the NIR spectrum (1300-1700 nm) for even greater penetration [60].
Advantages for Deep-Tissue Imaging
The longer excitation wavelengths employed in multi-photon microscopy provide critical advantages for deep-tissue imaging. Biological tissues scatter shorter wavelengths more strongly, so NIR light penetrates more deeply with less scattering [60]. Additionally, the nonlinear excitation confinement means that emitted fluorescence – even when scattered – can be unequivocally assigned to its origin point within the scan volume, unlike in confocal microscopy where scattered signal is rejected by the pinhole [60].
Recent advances have pushed the depth limits of multi-photon imaging through three-photon microscopy. By operating at local minima in the effective attenuation coefficient of biological tissues (approximately 1.3 μm and 1.7 μm for mouse brain), three-photon systems can image at depths exceeding 1 mm while maintaining single-cell resolution [60]. The higher-order nonlinearity of three-photon excitation also provides superior signal-to-background ratio (SBR) in scattering environments compared to two-photon approaches, though at the expense of signal strength due to the higher-order process [60].
Quantitative Performance Comparison
Technical Specifications Across Modalities
Table 1: Comparative technical specifications of live-cell imaging modalities
| Parameter | Confocal Microscopy | Light-Sheet Microscopy | Multi-Photon Microscopy |
|---|---|---|---|
| Excitation Mechanism | Single-photon | Single- or multi-photon | Multi-photon (typically 2P/3P) |
| Illumination-Detection Geometry | Co-axial through same objective | Orthogonal separation | Co-axial through same objective |
| Typical Excitation Wavelengths | 400-600 nm | 400-600 nm (1P); 700-1300 nm (2P) | 700-1300 nm (2P); 1300-1700 nm (3P) |
| Penetration Depth | <100 μm | 100-500 μm (1P); up to 1 mm (2P) | 500 μm-1.5 mm (2P); >1.5 mm (3P) |
| Photobleaching/Phototoxicity | High | 10-100x reduction vs confocal [61] | 5-10x reduction in focal plane |
| Volumetric Acquisition Speed | Slow (seconds-minutes) | Fast (milliseconds-seconds) [58] | Moderate (seconds) |
| Spatial Resolution | High (lateral: ~250 nm; axial: ~800 nm) | High (lateral: ~250 nm; axial: ~500 nm) [61] | Moderate (lateral: ~400 nm; axial: ~1.5 μm) |
| Primary Limitations | Photodamage, slow volumetric imaging | Scattering in opaque tissues, sample mounting | Cost, system complexity, lower resolution |
Performance in Key Biological Applications
Table 2: Application-specific performance metrics
| Application | Optimal Modality | Key Performance Metrics | Notable Achievements |
|---|---|---|---|
| Long-term Developmental Biology | Light-sheet microscopy | Days of continuous imaging with minimal phototoxicity [58] | Embryogenesis tracking over 24+ hours [58] |
| Fast Volumetric Calcium Imaging | High-speed light-sheet | 10-100 Hz volumetric rate for neural activity [62] | Whole-brain zebrafish imaging at 1 Hz [62] |
| Deep-Tissue Neuroscience | Three-photon microscopy | >1 mm depth with single-cell resolution [60] | Hippocampal imaging through intact mouse skull [60] |
| Subcellular Resolution in Live Cells | Lattice light-sheet | ~140 nm lateral resolution with minimal damage [58] | Organelle dynamics over hours [58] |
| Large Cleared Tissues | Open-top light-sheet | cm-scale samples with μm resolution in minutes [61] | Whole mouse brain at subcellular resolution [61] |
Experimental Protocols and Methodologies
Implementation of Two-Photon Light-Sheet Microscopy
Recent open-source designs have democratized access to advanced imaging modalities. The following protocol describes the transformation of a conventional brightfield microscope into a versatile one- and two-photon light-sheet system, adapted from an open-source publication [62]:
System Configuration and Assembly
- Microscope Platform: Begin with a commercial upright electrophysiology microscope (e.g., Scientifica) with motorized Z-stage for focus control.
- Light-Sheet Module: Construct a compact light-sheet formation unit (6 × 9 × 10 cm³) comprising two objectives in a one-to-one telescope configuration, with a galvanometric mirror at the back focal plane of the second objective for digital sheet scanning.
- Laser Delivery: Implement a custom negative curvature hollow-core photonic crystal fiber (HC-NCF) with 30 μm core diameter for broadband transmission (400-535 nm and 700-1500 nm bands) enabling both single-photon and two-photon operation through the same fiber.
- Alignment Protocol: Perform two primary alignments: (1) coarse positioning of the galvanometric mirror at 45° with fine-tuning via controller offset to center the beam into the second objective, and (2) adjustment of fiber-to-collimating objective distance to ensure proper beam collimation.
Sample Preparation and Mounting
- Biological Sample: Express pan-neuronal calcium indicator (e.g., GCaMP6f) in larval zebrafish (5-7 days post-fertilization).
- Sample Immobilization: Embed specimens in 1.5-2% low-melting-point agarose within fluorinated ethylene propylene (FEP) tubing or glass capillaries.
- Mounting Configuration: Position sample at the intersection of illumination and detection paths, ensuring unobstructed optical access for both objectives.
Image Acquisition Parameters
- One-Photon Mode: Use 488 nm continuous-wave laser at 1-10 μW/μm² power density with scientific CMOS camera exposure times of 10-50 ms.
- Two-Photon Mode: Employ femtosecond laser (e.g., 920 nm for GCaMP6f) at 10-50 mW average power with pulse widths of <100 fs at 80 MHz repetition rate.
- Volumetric Imaging: Acquire Z-stacks through sample volume using synchronized stage translation or objective piezo positioning at 0.5-5 Hz volume rates.
Three-Photon Microscopy for Deep-Tissue Imaging
This protocol details the implementation of three-photon microscopy for imaging neuronal activity in deep brain structures through the intact mouse skull [60]:
- Laser System: Implement a noncollinear optical parametric amplifier (NOPA) pumped by a frequency-doubled Yb-doped fiber MOPA system producing >1 μJ pulses at 1.3 μm or 1.7 μm wavelengths with >1 MHz repetition rates.
- Pulse Compensation: Apply external dispersion compensation to maintain <70 fs pulse widths at the sample plane.
- Wavelength Selection: Use 1.3 μm excitation for conventional three-photon imaging of green fluorophores (e.g., GFP, GCaMP) or 1.7 μm for red fluorophores (e.g., RFP, tdTomato).
Optical Path Configuration
- Beam Delivery: Employ high-numerical-aperture objectives (NA 0.8-1.0) with optimized transmission in NIR wavelengths.
- Detection Path: Implement non-descanned detectors with appropriate spectral filters (e.g., 525/50 nm bandpass for green, 595/50 nm for red emission).
- Adaptive Optics: Incorporate deformable mirrors for wavefront correction using sensorless or guide-star-based approaches to compensate for tissue-induced aberrations.
In Vivo Imaging Preparation
- Animal Preparation: Use adult mice (6-12 weeks) expressing calcium indicators in targeted brain regions under appropriate anesthetic or awake head-fixed conditions.
- Cranial Window: Perform thinned-skull or glass-reinforced cranial window surgery for long-term optical access.
- Motion Stabilization: Implement real-time motion correction algorithms or physical stabilization to minimize movement artifacts during functional imaging.
Functional Imaging Acquisition
- Imaging Parameters: Set appropriate field of view (300-500 μm) with 512×512-1024×1024 pixel resolution at 5-15 Hz frame rates.
- Excitation Power: Adjust power to 20-80 mW at sample depending on depth, using higher powers for deeper structures while monitoring for potential thermal effects.
- Neuronal Activity Recording: Acquire continuous time-series data during stimulus presentation or spontaneous activity periods, with typical durations of 30-120 minutes.
Essential Research Reagent Solutions
Table 3: Critical reagents and materials for advanced live-cell imaging
| Reagent/Material | Function/Application | Specifications | Implementation Notes |
|---|---|---|---|
| Genetically Encoded Calcium Indicators (e.g., GCaMP6f, jGCaMP7) | Monitoring neuronal activity dynamics | High signal-to-noise ratio, appropriate kinetics | AAV delivery for stable expression; 2P/3P excitation optimized variants [62] [60] |
| Tissue Clearing Reagents (e.g., CUBIC, iDISCO, CLARITY) | Rendering tissues transparent for light-sheet imaging | Refractive index matching, macromolecule preservation | Compatibility with endogenous fluorescence; minimal tissue distortion [61] |
| Hollow-Core Negative Curvature Fibers | Broadband laser delivery for multimodal systems | 30 μm core diameter; 400-1500 nm transmission bands | Low dispersion (<300 dB/km); high damage threshold [62] |
| Ultrafast Laser Sources | Multi-photon excitation | >1 μJ pulse energy; 1 MHz repetition rate; wavelength tunability | NOPA systems for 1.3-1.7 μm; Ti:Sapphire for 700-1000 nm [60] |
| Immobilization Matrices (e.g., low-melt agarose, FEP tubing) | Sample stabilization during live imaging | Optimal refractive index; biocompatibility | Rapid temperature-controlled gelling; gas-permeable for oxygenation [62] |
| Environmental Control Systems | Maintaining physiological conditions | Temperature (37°C), CO₂ (5%), humidity regulation | Integration with microscope stage; rapid recovery after sample mounting [59] |
Integrated Workflow for Multimodal Imaging
Future Directions and Emerging Innovations
The convergence of light-sheet and multi-photon technologies represents a particularly promising direction for bio-optics. Recent open-source designs for two-photon light-sheet microscopy demonstrate the feasibility of systems that combine the gentle optical sectioning of light-sheet illumination with the superior penetration of multi-photon excitation [62]. These hybrid systems address traditional limitations of light-sheet microscopy in scattering tissues while maintaining high volumetric acquisition speeds.
Emerging technological developments are poised to further advance these imaging modalities. Adaptive excitation systems that illuminate only regions of interest enable higher signal-to-noise ratios while minimizing total light exposure [60]. Artificial intelligence-powered image analysis facilitates automated segmentation, tracking, and restoration processes that transform large datasets into quantitative biological insights [59]. The development of miniaturized systems makes advanced imaging accessible for diverse laboratory settings and applications [61] [62].
As these technologies continue to evolve, they reinforce the central thesis that bio-optics approaches provide fundamentally superior solutions for dynamic live-cell imaging compared to traditional methods. Through their optimized use of light, innovative optical geometries, and integration with computational methods, light-sheet and multi-photon microscopy have transformed our ability to visualize and quantify biological processes in living systems across spatial and temporal scales previously inaccessible to researchers.
The field of bio-optics represents a transformative convergence of light-based technologies with biology and medicine, offering groundbreaking possibilities for both fundamental research and practical applications. Unlike traditional imaging techniques, which primarily serve observational roles, bio-optics enables active intervention and manipulation of biological systems at multiple scales—from single molecules to entire organisms. Optical manipulation technologies exemplify this paradigm shift, moving beyond mere observation to enable precise, non-contact control over biological processes. These techniques leverage the fundamental momentum carried by photons to exert mechanical forces on microscopic objects, providing researchers with tools capable of probing cellular mechanics, molecular interactions, and neural circuitry with unprecedented precision.
The distinctive advantage of optical manipulation within the bio-optics landscape lies in its non-invasive character and capacity for quantitative force measurement. Whereas traditional imaging techniques like brightfield microscopy or standard fluorescence imaging provide structural information, optical manipulation technologies add functional dimensionality—allowing scientists not only to see biological processes but to interact with them mechanically. This capability has proven particularly valuable in biophysical studies, drug discovery, and neuroscience, where the mechanical properties of cells and the activation of specific neural pathways can be critically important. The integration of optical manipulation with advanced imaging modalities creates a powerful synergistic platform for investigating dynamic biological systems in their native states, without the need for physical contact that might perturb delicate processes [2].
Technical Foundations of Optical Manipulation
Physical Principles and Force Generation
Optical manipulation techniques are fundamentally based on the momentum transfer that occurs when photons interact with matter. When light encounters a dielectric object such as a biological cell or microscopic bead, its path is altered through processes of reflection, refraction, and absorption. According to Newton's third law, this change in light direction results in an equal and opposite force being applied to the object. The total optical force ((F)) on a microscopic particle can be derived from Maxwell's stress tensor formalism and is mathematically represented as:
[ \langle F \rangle = \langle \oint_s \overset{\leftrightarrow}{T} dS \rangle ]
where (\overset{\leftrightarrow}{T}) is the Maxwell stress tensor and the integral is taken over a surface enclosing the particle [63]. In practical experimental systems, three primary optical forces dominate:
- Gradient force: Arises from intensity variations in the optical field and pulls particles toward regions of highest intensity when they have a higher refractive index than their surrounding medium.
- Scattering force: Results from photon reflection and absorption, pushing particles along the direction of light propagation.
- Absorption force: Occurs when light is absorbed by the particle, typically leading to heating effects and radiation pressure.
Three-dimensional trapping is achieved when the gradient force overcomes the scattering and absorption forces, creating a stable potential well that can confine particles against Brownian motion and other external disturbances [64]. The effectiveness of optical trapping depends on numerous factors including laser wavelength, beam profile, particle size and composition, and the refractive index contrast between the particle and its medium.
Key Optical Manipulation Modalities
Table 1: Comparison of Major Optical Manipulation Technologies
| Technique | Working Principle | Force Resolution | Spatial Resolution | Primary Biological Applications |
|---|---|---|---|---|
| Optical Tweezers | Highly focused laser beam creates intensity gradient | 0.1-100 pN [64] | Sub-nanometer [64] | Single molecule biophysics, cellular mechanics, molecular motors [65] |
| Optogenetics | Light-sensitive ion channels/opsins control neural activity | N/A (electrophysiological) | Single-cell (with targeting) | Neural circuit mapping, neuronal dynamics, behavior control [64] |
| Optical Fiber Tweezers | Tapered or lensed fibers create trapping fields | pN range [63] | Micrometer scale | Microsphere manipulation, cell sorting, integrated microfluidics [63] |
| Holographic Optical Tweezers | Computer-generated holograms shape laser beam | Similar to optical tweezers | Dependent on optical system | Multi-particle manipulation, complex assembly, tissue-level studies [65] |
| Plasmonic Tweezers | Surface plasmons create enhanced near-fields | Higher than conventional tweezers | Nanoscale | Nanoparticle manipulation, single molecule studies [65] |
Table 2: Recommended Laser Parameters for Biological Applications
| Application Domain | Optimal Wavelength Range | Typical Power | Considerations |
|---|---|---|---|
| Single Molecule Biophysics | 750-1100 nm [64] | 0.1-1 W | Minimize absorption in aqueous environments; avoid DNA/protein damage |
| Cellular Manipulation | 980-1064 nm [64] | 10-1000 mW | Balance trapping efficiency with cell viability; monitor heating effects |
| Neural Stimulation (Optogenetics) | Varies by opsin (e.g., 460-630 nm) | 1-100 mW/mm² | Match opsin activation spectra; minimize tissue scattering |
| In-tissue Manipulation | 750-1300 nm (biological window) [64] | Higher due to scattering | Use adaptive optics to compensate for tissue-induced aberrations |
Experimental Protocols and Methodologies
Protocol: Optical Trapping of Microspheres Using Axicon Lensed Fiber
This protocol details the experimental procedure for trapping polystyrene microspheres using an axicon lensed fiber (ALF), based on combined numerical and experimental investigation [63].
Research Reagent Solutions and Materials
Table 3: Essential Materials for ALF Optical Trapping
| Item | Specifications | Function/Purpose |
|---|---|---|
| Axicon Lensed Fiber | Taper outline: (y = \pm x/a), where a=0.5, 1, or 2; refractive index: 1.47; diameter: 20 μm [63] | Creates focused Bessel beam for optical trapping |
| Polystyrene Microspheres | Diameter: 8 μm; refractive index: 1.58 [63] | Model system for trapping experiments and calibration |
| Microfluidic Channel | PDMS or glass-based flow cell | Confines sample and enables fluid flow for force calibration |
| Aqueous Medium | Deionized water or buffer (refractive index: 1.33) [63] | Matching biological environment with controlled refractive index |
| Laser Source | Wavelength: 900-1500 nm; Gaussian beam profile with beam waist: 4 μm [63] | Provides trapping laser beam with appropriate parameters |
| Numerical Simulation Software | Finite-difference time-domain (FDTD) method implementation | Models optical force distribution and optimizes fiber design |
Step-by-Step Procedure
Fabricate axicon lensed fiber according to desired taper equation (y = \pm x/a), where parameter (a) controls taper length and angle. For (a = 0.5), the tapered length is 5 μm with a tapered angle of 127°; for (a = 1), length is 10 μm with 90° angle; for (a = 2), length is 20 μm with 63° angle [63].
Numerical analysis using FDTD:
- Build a 2D model with perfectly matched layer boundary conditions
- Set mesh grid of 0.1 μm globally with refined grid of 0.02 μm near fiber tip
- Calculate electrical and magnetic field distributions
- Compute optical forces using Maxwell stress tensor formalism
Experimental setup assembly:
- Align ALF within microfluidic channel
- Introduce polystyrene microsphere suspension (8 μm diameter) at controlled density
- Position microscope objective for observation and tracking
Optical trapping execution:
- Launch laser light at selected wavelength (900-1500 nm) through ALF
- Monitor formation of Bessel beam trapping field
- Observe and record microsphere trapping events via high-speed camera
Force calibration:
- Apply controlled fluid flow of known velocity
- Measure displacement of trapped microsphere from trap center
- Calculate optical force using Stokes' drag formula: (F = 6\pi\eta rv), where (\eta) is viscosity, (r) is microsphere radius, and (v) is flow velocity [63]
Validation:
- Compare experimental force measurements with numerical predictions
- Optimize fiber geometry and wavelength parameters for specific applications
Protocol: Optical Tweezers in Single Molecule Neuroscience
This protocol outlines the application of optical tweezers for investigating single molecule processes in neuroscience, particularly for studying neuronal dynamics and molecular mechanics [64].
Research Reagent Solutions and Materials
Table 4: Essential Materials for Single Molecule Neuroscience Studies
| Item | Specifications | Function/Purpose |
|---|---|---|
| Optical Tweezers System | High numerical aperture objective (NA≥1.2), NIR laser (980-1064 nm), position detection system [64] | Creates optical trap with sub-nanometer position resolution |
| Functionalized Microspheres | Polystyrene or silica, 0.5-2 μm diameter, surface-coated with specific binding groups | Serves as handles for attaching biomolecules while minimizing direct laser exposure |
| Neuronal Preparations | Cultured neurons, brain slices, or in vivo models | Biological systems for studying neuronal processes |
| Molecular Probes | Fluorescent tags, quantum dots, or functionalized ligands | Enable specific targeting and visualization of neuronal components |
| Buffer Solutions | Physiological ionic strength, oxygen scavengers, energy regeneration systems | Maintain biological activity and reduce photodamage during extended measurements |
Step-by-Step Procedure
System calibration:
- Align optical tweezers with high numerical aperture objective
- Calibrate trap stiffness using power spectrum analysis of Brownian motion or Stokes' drag method
- Verify position detection system using known displacements
Sample preparation:
- Functionalize microspheres with appropriate binding chemistry (e.g., streptavidin-biotin)
- Attach molecules of interest (e.g., membrane receptors, motor proteins) to functionalized beads
- Introduce prepared complexes to neuronal preparation
Attachment and manipulation:
- Trap functionalized bead with optical tweezers
- Position bead near target neuronal structure (e.g., growth cone, synapse)
- Form specific molecular attachments by controlled contact
Mechanical measurements:
- Apply controlled forces (0.1-100 pN range) while measuring molecular displacement
- Record force-extension relationships to determine mechanical properties
- Monitor dynamic processes (folding, unfolding, binding) under varying load conditions
Data analysis:
- Convert position signals to force measurements using calibrated trap stiffness
- Apply statistical mechanics models to extract energy landscapes
- Correlate mechanical measurements with neuronal function or dysfunction
Comparative Analysis: Bio-Optics vs Traditional Imaging Techniques
The integration of optical manipulation technologies represents a significant advancement over traditional imaging techniques in biological research. While conventional microscopy methods provide essential structural information, they lack the capacity for active intervention and mechanical interrogation that optical manipulation offers.
Table 5: Bio-Optics vs Traditional Imaging Approaches
| Characteristic | Optical Manipulation (Bio-Optics) | Traditional Imaging |
|---|---|---|
| Interaction Capability | Active manipulation and mechanical intervention | Passive observation only |
| Information Obtained | Structural, functional, and mechanical properties | Primarily structural information |
| Force Sensitivity | 0.1-100 pN range [64] | Not applicable |
| Temporal Resolution | Microsecond to second timescales for dynamics | Limited by camera frame rates |
| Sample Perturbation | Minimal non-contact interaction | Potential phototoxicity and photobleaching |
| Quantitative Output | Direct force and displacement measurements | Qualitative or semi-quantitative intensity data |
| Technical Complexity | High (requires precise alignment and calibration) | Moderate (more accessible implementation) |
The distinctive advantages of optical manipulation technologies within the bio-optics paradigm include their non-contact nature, which preserves sample integrity; versatility across scales from single molecules to cells; and quantitative precision in force and displacement measurements. These capabilities enable researchers to address fundamental biological questions that are inaccessible through traditional imaging alone, such as the mechanical forces governing cell division, protein folding pathways, neuronal growth cone dynamics, and the mechanical properties of individual molecular bonds [64] [2].
Traditional imaging techniques remain essential for contextualizing optical manipulation experiments, often serving as the observational framework within which targeted manipulations occur. The most powerful modern approaches combine high-resolution imaging with precise optical manipulation, creating integrated platforms that enable researchers to both observe and interact with biological systems in real time.
Emerging Applications and Future Directions
Optical manipulation technologies continue to evolve and expand into new application domains. In neuroscience, optical tweezers have been increasingly used for studies of molecules and neuronal dynamics, as well as for the study of model organisms as a whole [64]. Recent advances have enabled researchers to investigate the physical properties and intrinsic forces of neurons, their axonal navigation preferences and regeneration processes, and some of the fundamental dynamics around their function. The combination of optical tweezers with other modern optical tools has created remarkable opportunities for manipulating complex objects, mechanically altering surfaces, and controlling dynamics in neuronal systems.
In the broader field of biophotonics, optical manipulation technologies are converging with artificial intelligence, novel materials, and quantum approaches to create next-generation tools for precision medicine [2]. These developments are extending the capabilities of optical manipulation in several key directions:
- Hybrid trapping systems that combine optical tweezers with other manipulation modalities (e.g., acoustic trapping, optical nanofibers) for enhanced control over complex particles [66]
- Computational advances including machine learning-assisted wavefront shaping and inverse design of plasmonic nanotweezers for optimized performance [65]
- Miniaturization and integration of optical manipulation systems with microfluidics and lab-on-a-chip platforms for high-throughput applications [65] [63]
- Quantum biophotonics approaches that exploit quantum properties of light to achieve unprecedented sensitivity in force detection and manipulation [2]
The ongoing development of optical manipulation technologies ensures their expanding role in biological research, clinical applications, and pharmaceutical development. As these tools become more sophisticated and accessible, they will continue to transform our ability to interrogate and manipulate biological systems across scales from single molecules to functional tissues.
Navigating Challenges in Quantitative Bio-Optical Imaging
The field of bio-optics, defined as the interdisciplinary fusion of light-based technologies with biology and medicine, is rapidly transforming biomedical research and drug development [2]. This revolution is driven by advanced biophotonic techniques such as non-linear microscopy, optical coherence tomography (OCT), and coherent Raman scattering (CRS) imaging, which enable unprecedented investigation of biological specimens across multiple spatial scales, from the nanoscopic to the macroscopic level [2]. Unlike traditional broad-spectrum microscopy, these modalities generate rich, multi-parametric data with superior chemical specificity, penetration depth, and optical resolution.
However, these advancements come with a significant challenge: a massive data deluge. A single multi-photon fluorescence lifetime imaging (FLIM) experiment can easily generate terabytes of high-dimensional data, encompassing spatial, temporal, and spectral information. This article provides a comprehensive technical guide for managing and analyzing these complex image datasets, framing solutions within the specific context of bio-optics research to empower scientists and drug development professionals in harnessing the full potential of their data.
Bio-optics vs. Traditional Imaging: A Quantitative Comparison
The transition from traditional to advanced bio-optics imaging necessitates a paradigm shift in data management strategies. The following table summarizes the key differences that contribute to the data deluge.
Table 1: Data Output Comparison: Bio-optics vs. Traditional Imaging Techniques
| Imaging Characteristic | Traditional Widefield Microscopy | Advanced Bio-optics Imaging (e.g., OCT, Multi-photon) |
|---|---|---|
| Typical Data Volume per Experiment | Megabytes (MB) to low Gigabytes (GB) | Hundreds of Gigabytes (GB) to Terabytes (TB) |
| Dimensionality | 2D (x, y) or 3D (x, y, z) | 5D+ (x, y, z, channel, time, spectrum, lifetime) |
| Temporal Resolution | Low to medium (seconds-minutes) | High (milliseconds-seconds) for dynamic processes |
| Spectral Bands | Often 3-4 fluorescence channels | Hyperspectral (dozens to hundreds of bands) |
| Primary Data Management Challenge | Storage and basic organization | Ingestion, normalization, and scalable analysis |
Bio-optics techniques offer significant advantages that directly drive data complexity. These include non-contact measurement, which preserves cell integrity; high sensitivity, allowing for ultrasensitive detection down to single molecules; and excellent time resolution for observing dynamic biological processes [2]. Techniques like spectroscopic OCT (SOCT) capture the spectral content of backscattered light, while hyperspectral imaging (HSI) and FLIM add vast spectroscopic dimensions to each pixel in an image [2]. Managing this data effectively requires a robust, modern pipeline.
A Scalable Data Management Pipeline for Bio-optics
The following workflow diagram outlines the core stages of a scalable data management system designed to handle bio-optics data, from acquisition to actionable insight.
Pipeline Stage Protocols
Stage 1: Ingestion and Provenance Capture The initial stage involves transferring data from bio-optics instruments to a central system. Best practice mandates capturing critical provenance metadata at the point of ingestion [67]. This includes:
- Source IDs: A unique identifier for the microscope or instrument.
- Capture Timestamps: Precise time of image acquisition.
- Content Hashes/Checksums: Cryptographic hashes (e.g., SHA-256) to verify data integrity and enable deduplication, preventing storage of identical datasets from repeated experiments.
- Acquisition Parameters: As key-value pairs (e.g., laser power, exposure time, objective lens).
Protocol: Implement event-driven ingestion for real-time transfer post-acquisition or bulk parallel pipelines for backfilling historical data. All metadata should be written to an immutable log.
Stage 2: Normalization and Format Conversion Raw data from various vendor systems often comes in proprietary formats. This stage converts data into durable, analyzable artifacts to ensure long-term usability [67].
- Conversion to Standard Formats: Convert images to community-standard, open file formats like OME-TIFF, which robustly embed multidimensional metadata.
- OCR and Parsing: Apply Optical Character Recognition (OCR) to extract textual information from image annotations and use layout-aware parsers to recover data from embedded tables.
Protocol: Store the original file alongside the derived, normalized artifacts. Version the derived outputs and store their checksums to enable reprocessing when analytical models are updated.
Stage 3: AI-Driven Understanding and Enrichment This is the core analytical stage where raw images are transformed into quantifiable, searchable data.
- Computer Vision Tasks: Apply pre-trained or custom-trained models for object detection (e.g., identifying cells), instance segmentation (delineating boundaries), and classification (categorizing phenotypes) [68].
- Feature Extraction: Generate numerical embeddings (dense vector representations) for each image or region of interest using deep learning models. These embeddings power semantic search and similarity analysis.
- Metadata Generation: Produce confidence scores for every automated extraction and link identified entities (e.g., a specific cell type) to canonical records.
Stage 4: Organization and Indexing for Retrieval Processed data must be organized for efficient access. This involves mapping data to a business or research taxonomy and implementing a dual-search strategy [67].
- Taxonomy Mapping: Tag images with terms from a controlled vocabulary or ontology (e.g., Cell Ontology, Gene Ontology).
- Dual-Search Indexing: Build both a traditional keyword inverted index for fast filtering (e.g., "all images from 2025 containing 'mitochondria'") and a vector database for semantic similarity search (e.g., "find cells morphologically similar to this query cell").
- Storage Tiering: Use cost-effective object storage (e.g., Amazon S3, Azure Blob) with lifecycle policies to automatically move older data to cooler tiers, controlling costs [67].
Quantitative Analysis of Large-Scale Image Data
With data managed in a structured pipeline, researchers can apply robust quantitative analysis methods. The goal is to systematically study the data to discover patterns, trends, and connections that guide scientific choices [69].
Core Quantitative Methodologies
Table 2: Quantitative Data Analysis Methods for Bio-optics Imagery
| Method Category | Description | Application in Bio-optics Research |
|---|---|---|
| Descriptive Statistics | Summarizes the main characteristics of a dataset [69]. | Calculating the mean cell area, standard deviation of fluorescence intensity, or distribution of organelle counts across thousands of cells. |
| Inferential Statistics | Makes inferences about a population based on a sample, using hypothesis testing [69]. | Using a T-test to determine if the difference in protein expression levels between a treated and control group is statistically significant. |
| Regression Analysis | Models the relationship between a dependent variable and one or more independent variables [70]. | Understanding how drug dosage (independent variable) predicts changes in tumor spheroid growth (dependent variable) in 3D culture models. |
| Cluster Analysis | Identifies natural groupings or segments in data without pre-defined categories [70]. | Discovering novel sub-populations of cells based on high-dimensional morphological features extracted by a deep learning model. |
| Time Series Analysis | Analyzes data points collected sequentially over time to identify trends and patterns [70]. | Tracking the dynamic change in calcium flux in neurons in response to a stimulus, or modeling long-term cell migration trajectories. |
Experimental Protocol: A Quantitative Analysis Workflow
The following protocol details a typical workflow for analyzing a high-content screen of drug compounds.
Aim: To identify compounds that induce a specific phenotypic change (e.g., altered mitochondrial morphology) in a cell model.
Step 1: Feature Extraction
- Acquire 3D fluorescence images (e.g., using a multi-photon microscope) for each well of the screening plate.
- Use a pre-trained instance segmentation model (e.g., from Ultralytics YOLO or Cellpose) to identify individual cells and sub-cellular structures like mitochondria [68].
- For each segmented object, extract hundreds of morphological, intensity, and texture features (e.g., area, eccentricity, total intensity, Haralick features).
Step 2: Data Cleaning and Normalization
- Handle missing data, often by imputation or case deletion.
- Identify and treat outliers that may skew analysis (e.g., dead cells or segmentation artifacts).
- Apply normalization (e.g., Z-score normalization per plate) to correct for technical variation between experimental batches.
Step 3: Dimensionality Reduction and Clustering
- Apply Principal Component Analysis (PCA) to reduce the feature space and visualize high-dimensional data in 2D/3D plots.
- Perform cluster analysis (e.g., K-means) on the normalized features to group cells with similar phenotypic profiles.
Step 4: Statistical Testing and Inference
- For each compound treatment, aggregate single-cell data to well-level statistics (e.g., mean per feature).
- Use Analysis of Variance (ANOVA) to test if any compound treatment induces a significant change in the phenotypic profile compared to the control group [69].
- For significant hits, apply post-hoc tests to confirm the effect size and calculate false discovery rates (FDR) to account for multiple comparisons.
Step 5: Predictive Modeling
- Use significant hits as a labeled training set to build a machine learning classifier (e.g., a Random Forest or Support Vector Machine).
- This model can now be deployed to rank or classify new compounds based on their likelihood to induce the target phenotype.
The Scientist's Toolkit: Essential Research Reagents and Materials
Success in managing and analyzing bio-optics data relies on a combination of computational tools, data resources, and AI models.
Table 3: Essential Research Tools for Bio-optics Data Science
| Tool Category / Name | Function | Relevance to Bio-optics |
|---|---|---|
| Python & Key Libraries | A general-purpose programming language. Libraries like NumPy, Pandas, and Scikit-learn form the foundation for data manipulation and machine learning [69]. | The primary environment for building custom analysis scripts, from basic image feature calculation to complex deep learning pipelines. |
| R Statistical Software | An open-source environment for statistical computing and graphics [69]. | Excellent for in-depth statistical analysis, hypothesis testing, and generating publication-quality plots of quantitative results. |
| Ultralytics YOLO | A state-of-the-art framework for real-time object detection and segmentation [68]. | Used to train or fine-tune models to automatically detect and segment specific cells or sub-cellular structures in large image datasets. |
| COCO Dataset | A large-scale dataset for object detection, segmentation, and captioning [68]. | Serves as a source of pre-trained models that can be fine-tuned for biological tasks, and as a benchmark for evaluating model performance. |
| ImageNet Dataset | A large dataset with millions of labeled images for object classification [68]. | Provides foundational models for transfer learning, significantly improving performance on bio-optics tasks even with limited labeled data. |
| Cloud Platforms (AWS, GCP, Azure) | Provide scalable computing, storage, and AI services [67]. | Essential for elastically scaling compute resources for model training and providing the storage backbone for petabyte-scale bio-optics data lakes. |
| Unstructured Data Management Tools | Platforms like Numerous automate file labeling, entity tagging, and metadata extraction at ingestion [67]. | Critical for automating the initial stages of the data pipeline, applying AI to classify incoming images and populate metadata fields for governance. |
The data deluge from advanced bio-optics imaging is a formidable challenge, but also an unparalleled opportunity. By implementing a structured data management pipeline and leveraging modern quantitative analysis and AI methods, researchers can transition from being overwhelmed by data to being empowered by it. This integrated approach enables the extraction of deep, quantitative insights from complex biological systems, ultimately accelerating the pace of discovery in basic research and therapeutic development. The future of bio-optics is inextricably linked to our ability to manage and interpret the data it generates, turning the deluge into a wellspring of scientific insight.
The rapid advancement of biomedical optical imaging has established it as a cornerstone of modern biological research and drug development, enabling the investigation of living systems at scales ranging from single molecules to whole organisms [71]. However, this technological sophistication introduces a critical challenge: ensuring that the intricate images and data produced can be understood, verified, and replicated by the scientific community. The field of bio-optics, which utilizes light-based tools to interrogate biological systems, faces a unique set of reproducibility hurdles not always as prevalent in traditional imaging techniques like MRI or CT scanning. Where traditional methods often rely on more standardized clinical protocols, bio-optical methods boast a multitude of modalities (e.g., confocal, multiphoton, light-sheet, super-resolution) and a vast parameter space that includes intensity, wavelength, polarization, coherence, and timing [71]. This very flexibility, which makes light such a powerful investigational tool, also creates a labyrinth of variables that must be meticulously documented to ensure that results are reliable and reproducible.
The consequences of inadequate reporting are significant. A recent analysis revealed that a mere 17% of research articles pass a test for the minimal information required to reproduce microscopy experiments [72]. This "reproducibility crisis" undermines the scientific process, hindering the translation of basic research into reliable clinical applications and effective therapeutics [73]. Addressing this requires a concerted focus on three pillars: standardization of methods reporting, rigorous quality control of instruments and images, and comprehensive metadata capture. This guide details the practical strategies and tools that researchers, scientists, and drug development professionals can employ to embed reproducibility into the very foundation of their bio-optical research.
Standardization in Bio-Optical Imaging
Standardization provides the common language necessary for scientists to communicate their methods unambiguously. Community-driven initiatives have developed clear guidelines and specifications to ensure that all critical information about an experiment is captured and reported.
Community-Driven Reporting Guidelines
International consortia such as QUAREP-LiMi (Quality Assessment and Reproducibility for Instruments & Images in Light Microscopy) have developed tiered checklists to guide researchers in publishing their work [73]. These guidelines break down the reporting requirements into three levels:
- Minimal: The essential requirements for reproducible images, such as indicating the origin of any insets and citing each step of an established image-analysis workflow.
- Recommended: Practices that significantly bolster image comprehensibility, including providing intensity scales for grayscale and color images.
- Ideal: Top-tier best practices, such as annotating image details like pixel size and exposure time, or providing a screen recording for a new image-analysis workflow [73].
A reproducible imaging protocol should comprehensively cover four main areas [74]:
- Sample Preparation: Details on tissue/cell culture, staining procedures, optical grade of the coverslip, and mounting media.
- Microscope Configuration: The type of stand, stage, illumination, detector, filters, objective, and immersion medium.
- Image Acquisition Settings: Exposure/dwell time, final magnification, pixel size, time intervals, laser power, and the number of z-planes.
- Image Analysis Workflow: All processing steps, segmentation methods, software used (with versions), and details of the computing hardware for large datasets.
Tools for Automated Metadata Capture
The complexity of modern microscopes makes manual recording of all settings prone to error. Fortunately, software tools now exist to automate this process. A key development is the 4DN-BINA-OME model, a community-driven microscopy metadata specification that builds on the Open Microscopy Environment (OME) data model [72]. This model scales with experimental complexity, ensuring essential information is captured without overburdening scientists.
To put these specifications into practice, tools like MethodsJ2 have been created. This open-source software, which runs in the popular ImageJ/Fiji platform, automates the generation of methods text for publication [72]. Its workflow involves:
- Using the companion Micro-Meta App to create a standardized
.JSONfile containing all metadata for a specific microscope. - Automatically extracting metadata from the image file itself using OME BioFormats.
- Guiding the user to enter experimental and sample-specific metadata (e.g., cell type, dyes).
- Validating the consolidated metadata and automatically generating a draft methods text for the research paper [72].
This integration of community standards with user-friendly software is a critical step toward making comprehensive reporting a routine part of the bio-optics workflow.
Quality Control for Reproducible Results
Quality control (QC) is the practice of maintaining and verifying the performance of both the optical instruments and the biological preparations to ensure data consistency and reliability over time.
Instrument Quality Control
In the realm of bio-optics, precision is paramount, and the quality of components like lenses and sensors is foundational [75]. Regular performance monitoring of microscopes is essential. This includes measuring key parameters such as illumination intensity, laser power stability, and camera noise. The use of reference standards, such as fluorescent beads with known emission characteristics, allows researchers to periodically assess and document critical performance metrics like spatial resolution, channel registration, and illumination uniformity [72].
Table 1: Key Research Reagents and Materials for QC and Sample Preparation
| Item | Function in Bio-Optics Research |
|---|---|
| High-NA Plan-Apochromatic Objective | Provides high-resolution, aberration-free imaging, crucial for precise data [76]. |
| Fluorescent Beads (e.g., Tetraspeck) | Serve as calibration standards for resolution, colocalization, and channel registration [72]. |
| Biocompatible Gain Materials (e.g., GFP, ICG) | Enable the creation of cell- or tissue-based biolasers for highly sensitive biosensing within biological systems [5]. |
| Refractive Index Matching Solutions | Used in optical clearing to reduce light scattering, enabling deeper imaging in 3D samples [77]. |
| Optical Clearing Reagents (e.g., CUBIC, ScaleA2) | Chemically equilibrate RI throughout a 3D sample to increase transparency [77]. |
Quality Assessment of 3D Samples and Optical Clearing
The shift toward more physiologically relevant 3D cell cultures, such as spheroids, introduces significant QC challenges. Light scattering within these dense samples limits penetration and contrast, making it difficult to visualize individual cells in deeper layers [77]. Optical clearing protocols have been developed to overcome this by equilibrating the refractive index throughout the sample. However, with numerous clearing protocols available (e.g., ClearT2, CUBIC, ScaleA2, Sucrose), a major open issue has been the lack of a gold-standard metric to evaluate their efficacy.
A recent study addressed this by benchmarking seven no-reference sharpness metrics against evaluations from ten microscopy experts. The study created a large 3D light-sheet dataset of 90 spheroids cleared with five different protocols and found that intensity variance was the only metric that strongly correlated with human expert assessment [77]. This makes intensity variance a suitable quantitative metric, or a potential gold standard, for deciding on the most effective optical clearing protocol for a given experiment. These metrics have been implemented in an open-source ImageJ/Fiji plugin named Spheroid Quality Measurement (SQM) for community use [77].
Table 2: Quantitative Metrics for Evaluating Optical Clearing Protocols
| Metric | Description | Correlation with Human Evaluation |
|---|---|---|
| Intensity Variance | Measures the spread of pixel intensity values; sharper images tend to have higher variance. | Strong correlation; identified as a potential gold standard [77]. |
| Laplacian Variance | Calculates the variance of the image after applying a Laplacian filter, which highlights edges. | Weak or inconsistent correlation [77]. |
| Gradient Magnitude Variance | Assesses sharpness based on the variance of the gradient magnitude across the image. | Weak or inconsistent correlation [77]. |
| Histogram Entropy | Measures the randomness in the image's intensity distribution. | Weak or inconsistent correlation [77]. |
| Frequency Threshold | Evaluates the high-frequency content in the image's Fourier transform. | Weak or inconsistent correlation [77]. |
Experimental Protocols for Reproducible Bio-Optics
Detailed Protocol: Assessing Optical Clearing Efficacy
The following methodology outlines the process for quantitatively evaluating different optical clearing protocols to achieve single-cell resolution in 3D multicellular spheroids, as validated in recent literature [77].
Objective: To identify the most effective optical clearing protocol for a specific 3D cell culture model by quantitatively comparing image quality post-clearing.
Materials:
- Biological Models: 3D multicellular spheroids (e.g., from T-47D, 5-8F, or Huh-7D12 cell lines).
- Clearing Reagents: Prepare solutions for protocols under investigation (e.g., ClearT, ClearT2, CUBIC, ScaleA2, Sucrose).
- Imaging Instrument: Light-sheet fluorescence microscope (LSFM), chosen for its high speed, low photobleaching, and suitability for large spheroids up to 500 µm [77].
- Analysis Software: ImageJ/Fiji with the Spheroid Quality Measurement (SQM) plugin [77].
Procedure:
- Spheroid Generation and Staining: Generate mono-culture spheroids using a standardized method (e.g., hanging drop or ultra-low attachment plates). Fluorescently stain the spheroids to enable visualization.
- Clearing Treatment: Divide the spheroids into experimental groups. Treat each group with a different optical clearing protocol, following the published specifications for each method precisely. Include an uncleared group as a control.
- Image Acquisition: Image all spheroids (cleared and uncleared) using identical LSFM settings. Ensure consistent laser power, exposure time, detection parameters, and z-step size across all samples to allow for direct comparison.
- Quality Metric Calculation: For each acquired 3D image stack, run the SQM plugin in ImageJ/Fiji. The plugin will calculate the seven sharpness metrics (including intensity variance) for each optical section.
- Data Analysis and Protocol Selection:
- Calculate the average intensity variance value for each spheroid.
- Compare the average intensity variance values across the different clearing protocol groups.
- The protocol that yields the highest average intensity variance value is quantitatively the most effective at reducing light scattering and producing sharper images for that specific cell line.
Detailed Protocol: Reporting a Published Microscopy Experiment
To meet minimal reproducibility standards, the following workflow, leveraging the MethodsJ2 tool, should be followed when preparing microscopy data for publication [72].
Objective: To capture and report all necessary microscopy metadata to allow for the experiment to be understood and replicated.
Materials:
- The image data to be published.
- Access to the microscope used for the experiment.
- ImageJ/Fiji software with the MethodsJ2 script.
- Micro-Meta App (web-based or standalone).
Procedure:
- Pre-Acquisition Microscope Profiling: Before the experiment, use the Micro-Meta App on a computer connected to the microscope. Follow the step-by-step guide to enter all relevant hardware information (e.g., microscope stand, objectives, light sources, detectors, filters) and save the resulting
Microscope.JSONfile. - Image Acquisition: Perform the experiment, ensuring that the image acquisition software itself records as many settings (e.g., pixel size, exposure time, laser power) as possible into the image file metadata.
- Methods Draft Generation:
- Open your image file in ImageJ/Fiji and run the MethodsJ2 script.
- The script will automatically extract metadata from the image file.
- Select the corresponding
Microscope.JSONfile when prompted. - Input the requested sample and experimental details (e.g., cell type, fluorescent dyes/blotches).
- MethodsJ2 will guide you through validating the consolidated metadata.
- Upon completion, the software will automatically generate a draft methods text and copy it to your clipboard.
- Final Review and Submission: Paste the draft text into your manuscript and review it carefully. It is the researcher's responsibility to ensure the accuracy and completeness of the final text before publication [72].
Ensuring reproducibility in bio-optics is not a solitary task but a shared responsibility across the entire scientific ecosystem. Experimental scientists must diligently apply the standardized protocols and QC measures outlined here. Imaging scientists and core facility managers play a crucial educational role and are responsible for instrument calibration. Microscope manufacturers are urged to integrate community metadata standards directly into their software, automating and simplifying the reporting process. Finally, scientific publishers and reviewers must enforce these community-developed guidelines to ensure a minimum standard of reporting is met in every published paper [72] [73].
By adopting these practices—leveraging standardized reporting guidelines, implementing quantitative quality control, and utilizing automated metadata tools—the field of bio-optics can solidify its foundation of reliability. This will accelerate the translation of groundbreaking optical research from the bench to the bedside, ultimately fulfilling the promise of advanced theranostics and improving patient outcomes [71].
The pursuit of non-invasive, high-resolution imaging in biological sciences is fundamentally constrained by three interconnected physical phenomena: light scattering, absorption, and phototoxicity. These properties of biological tissues directly limit the penetration depth and fidelity of optical imaging techniques, while the very light used for illumination can perturb or damage living systems. While traditional imaging modalities like magnetic resonance imaging (MRI) and computed tomography (CT) penetrate deeply, they lack the molecular specificity and resolution required for many cellular and functional studies. Bio-optical techniques bridge this gap by offering unparalleled resolution and contrast, but their effectiveness is ultimately governed by how well they overcome these physical limits. This whitepaper examines the core challenges and the innovative optical strategies being developed to address them, providing a framework for researchers and drug development professionals to select and optimize imaging methodologies for advanced biomedical applications.
Fundamental Photon-Tissue Interactions and Imaging Modalities
The interaction between light and biological tissue is the foundation of all bio-optical imaging. When photons encounter tissue, they can be absorbed, scattered, or transmitted. The specific utilization of these interactions defines the capabilities and limitations of each imaging modality.
- Absorption-Based Techniques: These methods rely on the absorption of light by endogenous chromophores. Photoacoustic imaging (PAI) is a prominent example, where the absorption of pulsed laser light by molecules like hemoglobin generates a thermoelastic expansion, producing ultrasound waves that are detected to form an image. PAI leverages the fact that ultrasound scatters less than light in tissues, enabling deeper penetration while retaining optical absorption contrast [78].
- Emission-Based Techniques: These techniques detect light emitted from intrinsic fluorophores following excitation. Two-photon fluorescence (TPF) and fluorescence lifetime imaging microscopy (FLIM) exploit endogenous fluorophores such as nicotinamide adenine dinucleotide (NADH) and flavin adenine dinucleotide (FAD) to assess cellular energy metabolism. The non-linear excitation in TPF confines the excitation volume, reducing out-of-focus light and enabling deeper tissue imaging [78].
- Scattering-Based Techniques: This category uses the scattering properties of light. Optical coherence tomography (OCT) is an interferometric method that detects back-scattered light to provide high-resolution, cross-sectional images of tissue morphology. It is widely used in ophthalmology and dermatology but remains limited by scattering in deeper tissue layers [78]. Second harmonic generation (SHG) is a non-linear scattering process that generates light at half the wavelength of the excitation light and is highly sensitive to non-centrosymmetric structures like collagen [78].
Table 1: Core Label-Free Optical Imaging Modalities and Their Contrast Mechanisms
| Imaging Modality | Primary Contrast Mechanism | Key Applications | Main Strengths |
|---|---|---|---|
| Photoacoustic Imaging (PAI) | Light Absorption | Vasculature, Oxygen Saturation, Melanin | Deep penetration (cm), spectroscopic unmixing [78] |
| Two-Photon Fluorescence (TPF) | Native Fluorescence | Cellular Metabolism (via NADH/FAD) | Confined excitation, reduced photobleaching [78] |
| Optical Coherence Tomography (OCT) | Back-Scattering | Tissue Morphology, Ophthalmic Imaging | High-speed, high-resolution volumetric imaging [79] [78] |
| Second Harmonic Generation (SHG) | Nonlinear Scattering | Collagen, Microtubules | Highly specific to non-centrosymmetric structures [78] |
| Interferometric Scattering (iSCAT) | Interference & Scattering | Single-protein detection, Virus tracking | Label-free, single-molecule sensitivity [19] |
Diagram 1: Photon-Tissue Interactions and Resulting Modalities.
Quantitative Analysis of Penetration Depth
A critical parameter in any imaging technique is its penetration depth, which is influenced by the optical properties of the tissue and the configuration of the imaging system. Understanding these relationships is key to experimental design.
Source-Detector Distance Dependence in NIRS
In Near-Infrared Spectroscopy (NIRS), the depth of penetration is directly related to the distance between the light source and the photodetector (SDS). A 2025 experimental study using porcine kidney models quantified this relationship, providing empirical data that aligns with theoretical models [80]. The study found that both the maximum depth and mean depth of penetration increase with a larger SDS. Specifically, a linear relationship was derived between the SDS and the maximum depth, while the mean depth was found to be proportional to the square root of the SDS [80].
Table 2: Experimentally Derived Penetration Depth Relationships in Porcine Kidney (NIRS) [80]
| Source-Detector Distance (SDS) | Relationship to Maximum Depth | Relationship to Mean Depth |
|---|---|---|
| 16 mm to 40 mm | Linear Increase | Proportional to √(SDS) |
Enhancing Depth with Optical Clearing Agents (OCAs)
Scattering remains the primary barrier to depth. Optical clearing agents (OCAs) reduce scattering by matching the refractive index (RI) of different tissue components. A novel approach uses strongly absorbing dye molecules (e.g., tartrazine, 4-aminoantipyrine) approved as food additives. According to the Lorentz oscillator model and Kramers-Kronig relations, these dyes increase the RI of aqueous tissue components, thereby reducing RI mismatch and decreasing scattering. Topical application of these dyes on mouse skin significantly enhanced the penetration depth of OCT, allowing visualization of sub-surface structures like blood vessels that were previously obscured [79].
Mitigating Phototoxicity in Live Samples
Phototoxicity—the light-induced damage to living cells—is a major constraint in longitudinal and live-cell imaging. It is primarily caused by high-intensity illumination and the generation of reactive oxygen species.
Recent studies demonstrate that not all optical modalities pose the same risk. For instance, a 2025 investigation into the genotoxic impact of broadband infrared radiation used in OCT on porcine and human sperm found no observable effect on sperm parameters or DNA integrity following irradiation. The sperm retained their functionality, including the ability to penetrate cumulus cells, indicating that OCT imaging can be non-phototoxic for certain sensitive biological systems [81].
Strategies to minimize phototoxicity include:
- Using Modalities with Lower Energy Requirements: Optical coherence tomography, which relies on interferometry of back-scattered light, often uses power levels that do not induce significant damage [81].
- Optical Sectioning with Off-Axis Illumination: Techniques like light sheet fluorescence microscopy (LSFM) illuminate only the focal plane being imaged. This dramatically reduces the total light dose delivered to the sample compared to wide-field or confocal microscopy, thereby minimizing phototoxicity and enabling long-term imaging of delicate processes like embryonic development [82].
- Employing Longer Wavelengths: Light in the near-infrared (NIR) window (650-1350 nm) experiences less scattering and absorption in tissue, reducing the energy required for imaging and the associated phototoxic effects [80].
Diagram 2: Optical Techniques and Associated Phototoxicity.
Advanced Optical Sectioning for Scattering Mitigation
Optical sectioning is the ability of a microscope to isolate in-focus light from out-of-focus background, which is crucial for imaging thick, scattering samples. The performance of different sectioning methods can be quantitatively assessed by their axial response to a thin fluorescent sheet [82].
Table 3: Comparison of Optical Sectioning Modalities and Their Characteristics [82]
| Technique | Illumination/Detection Scheme | Optical Sectioning Strength | Imaging Speed | Best For |
|---|---|---|---|---|
| Confocal | Coaxial; point scanning with pinhole | High | Low | Fixed cells, high-contrast imaging |
| Two-Photon | Coaxial; non-linear intra-focal excitation | High | Medium | Deep tissue, live imaging |
| Light Sheet | Off-axis; plane illumination | Medium | Very High | Large samples, long-term live imaging |
| Structured Illumination (SIM) | Coaxial; patterned illumination | Medium | Medium-High | Sub-diffraction resolution |
| Line Illumination Modulation (LiMo) | Off-axis; line scanning | Medium-High | High | Thick tissues, organ-level imaging |
These techniques are broadly categorized by the spatial relationship between illumination and detection:
- Coaxial Imaging: The illumination and detection paths are co-aligned (e.g., confocal, two-photon, SIM). They achieve sectioning through physical pinholes, non-linear excitation, or computational processing of patterned illumination [82].
- Off-Axis Imaging: The illumination and detection paths are separated (e.g., light sheet, LiMo). This geometric separation naturally rejects out-of-focus light, offering superior sectioning strength and often higher speeds with lower phototoxicity [82].
Experimental Protocols and Reagent Solutions
Protocol: Quantifying NIRS Penetration Depth in Ex Vivo Tissue
This protocol is adapted from a study that experimentally measured photon penetration depth in porcine kidney [80].
Objective: To derive the cumulative distribution function (CDF) of re-emitted photon penetration depth at different source-detector distances (SDS).
Materials:
- Fresh porcine kidney tissue, trimmed to a uniform thickness >15 mm.
- Continuous-wave NIRS sensors (e.g., PortaLite, Artinis Medical Systems).
- Custom fixture to hold the sensor and tissue stably.
- A thin, absorbent black blade and a mechanism for making precise, incremental cuts (e.g., feeler gauges to control depth).
Procedure:
- Setup: Place the NIRS sensor in the custom fixture and position the tissue sample on top, ensuring full contact with the sensor surface.
- Baseline Measurement: Record the optical intensity (DAQ value) from the photodetector for the intact tissue.
- Incremental Cutting: Make a perpendicular cut between the source and detector at the midpoint for the shortest SDS (e.g., 8 mm for a 16 mm SDS).
- Photon Blocking Measurement:
a. Insert the black blade into the cut to block light transmission. Record the DAQ value once stable.
b. Remove the blade and record a calibration DAQ value.
c. Calculate the fraction of unblocked light as:
(Blocked DAQ Value) / (Calibration DAQ Value). - Repetition: Repeat steps 3 and 4, deepening the cut in small increments. For each cut, the fraction of unblocked light corresponds to the portion of photons that penetrated deeper than the cut depth.
- Data Analysis: Plot the fraction of unblocked light against cut depth to generate the CDF for penetration depth. Repeat the entire experiment for different SDSs (e.g., 16, 21, 26, 30, 35, 40 mm).
Protocol: Enhancing OCT Penetration with Absorbing Dyes
This protocol describes the topical application of absorbing dyes for in vivo enhancement of OCT imaging depth [79].
Objective: To improve the penetration depth of OCT in skin using topical applications of tartrazine or 4-aminoantipyrine.
Materials:
- Dye Gel Compound: 30-38% (w/w) tartrazine or 4-aminoantipyrine dissolved in 1X PBS, mixed with low-melting-point agarose (final concentration 10 mg/mL) to form a stable gel.
- Animal model (e.g., mouse).
- OCT imaging system (e.g., commercial SD-OCT).
- Hair removal cream (e.g., Nair), isopropyl alcohol, cotton applicators.
Procedure:
- Animal Preparation: Anesthetize the animal. Shave and treat the abdominal skin with a depilatory cream for 5 minutes to remove remaining fur. Clean the area with isopropyl alcohol.
- Baseline Imaging: Acquate OCT B-scans of the untreated skin.
- Dye Application: a. Massage a thin topical coating of the dye-pumice gel mixture onto the skin for 10 minutes. b. Wipe away pumice particles and apply the pure dye gel for 3-5 minutes until maximum tissue transparency is visually observed.
- Post-Treatment Imaging: Acquire OCT B-scans in the same region as the baseline.
- Analysis: Quantify the improvement in penetration depth by measuring the depth at which the signal attenuates to a predefined threshold (e.g., noise floor) in both pre- and post-treatment images.
The Scientist's Toolkit: Key Reagent Solutions
Table 4: Essential Reagents for Advanced Bio-Optical Experiments
| Reagent / Material | Function | Example Application |
|---|---|---|
| Tartrazine / 4-Amino-antipyrine | Optical Clearing Agent (OCA) | Topical application to reduce scattering and enhance penetration depth for OCT and PAM in skin [79]. |
| Porcine Kidney Tissue | Ex Vivo Biological Tissue Model | Provides a readily accessible, optically uniform medium for experimental validation of photon penetration depth (NIRS) [80]. |
| Low-Melting-Point Agarose | Gel Matrix for Topical Application | Enables the formation of a stable, applicable gel for in vivo delivery of optical clearing dyes [79]. |
| NADH & FAD | Endogenous Fluorophores | Serve as natural contrast agents for label-free metabolic imaging using TPF and FLIM [78]. |
| Nanofluidic Channels | Physical Sample Constraint | Used in Nanofluidic Scattering Microscopy (NSM) to minimize axial displacement of freely diffusing molecules for stable interferometric detection [19]. |
The field of bio-optics is dynamically evolving to overcome the fundamental physical limits of scattering, phototoxicity, and penetration depth. The synergy between novel optical concepts—such as off-axis sectioning and interferometric detection—and biochemical approaches, including safe optical clearing agents, is pushing the boundaries of what is possible. The translation of these technologies is accelerating, with OCT becoming a clinical standard in ophthalmology, optoacoustic imaging advancing toward clinical use for visualizing vasculature and metabolism, and adaptive optics beginning to enable single-cell resolution in the living eye [13] [83] [78]. Future progress will be driven by the integration of deep learning for image reconstruction and analysis, the continued development of wearable optoacoustic devices, and the refinement of multi-modal systems that combine the strengths of individual techniques. For researchers and drug development professionals, this expanding toolkit offers powerful means to non-invasively probe structure and function from the single-molecule to the whole-organ level, paving the way for new discoveries in basic biology and transformative advances in therapeutics.
The Role of AI and Machine Learning in Image Reconstruction and Analysis
The convergence of artificial intelligence (AI) and biophotonics is fundamentally reshaping the landscape of medical imaging. This whitepaper explores the transformative role of AI and machine learning (ML) in image reconstruction and analysis, framing these advancements within the context of bio-optics versus traditional imaging techniques. Bio-optics, defined by its use of light to interact with biological matter, offers non-contact, high-speed, and highly sensitive imaging capabilities [2]. AI-driven enhancements are now unlocking the full potential of these modalities—such as optical coherence tomography (OCT) and photoacoustic imaging—enabling super-resolution reconstruction, quantitative analysis, and accelerated diagnostic pathways. This technical guide details the core algorithms, provides experimental protocols for key applications, and visualizes the workflows that are setting new benchmarks for image quality and analytical depth in biomedical research and drug development.
Bio-optics, or biophotonics, represents the interdisciplinary fusion of light-based technologies with biology and medicine [2]. Its core advantage lies in the ability to perform non-contact, non-invasive measurements at high speeds and with exceptional sensitivity, allowing for the observation of dynamic biological processes without damaging samples [2]. Key biophotonic technologies include bioimaging (e.g., OCT, hyperspectral imaging), biosensing, and photonic-based therapies [2].
However, the intrinsic physical limitations of optical systems, such as light scattering, diffraction, and the trade-off between resolution and penetration depth, have historically constrained their performance. AI and ML are now overcoming these barriers. Techniques like deep learning (DL) are being integrated directly into image reconstruction pipelines, moving beyond traditional filtered back-projection or analytic methods to produce higher-quality images from less data [84] [85]. Furthermore, ML models excel at extracting subtle, quantitative features from bio-optical images for automated classification and predictive modeling, tasks that are challenging and time-consuming for human operators. This synergy is creating a new paradigm where bio-optical systems, supercharged by AI, are providing unprecedented insights into biological structures and disease pathologies, thereby accelerating drug discovery and development [86].
Core AI and Machine Learning Techniques in Image Processing
The application of AI in image reconstruction and analysis leverages a suite of sophisticated algorithms, each suited to specific tasks. The table below summarizes the key algorithms and their primary applications in this domain.
Table 1: Key Machine Learning Algorithms for Image Reconstruction and Analysis
| Algorithm Category | Example Algorithms | Key Applications in Imaging | Strengths |
|---|---|---|---|
| Supervised Learning | Convolutional Neural Networks (CNNs), Support Vector Machines (SVMs) [87] | Image classification, semantic segmentation, noise reduction [88] [89] | High accuracy in pattern recognition; excels with spatial data. |
| Unsupervised Learning | K-means, Convolutional Autoencoders (CAE) [87] [89] | Image clustering, anomaly detection, data compression [89] | Discovers hidden patterns without labeled data. |
| Ensemble Methods | Random Forest, Gradient Boosting [87] | Feature selection, predictive model building from image features | Reduces overfitting; robust performance. |
| Generative Models | Generative Adversarial Networks (GANs), Variational Autoencoders (VAEs) [90] | Super-resolution reconstruction, data augmentation, synthetic image generation [90] | Generates new data; enhances image resolution and quality. |
Deep Learning Architectures
- Convolutional Neural Networks (CNNs): CNNs are the workhorse for image analysis tasks. Their hierarchical structure, with convolutional and pooling layers, allows them to automatically and adaptively learn spatial hierarchies of features from low-level edges to high-level semantic concepts [88]. This makes them ideal for image classification, where they can, for instance, categorize skin lesions from dermoscopic images [90], or filter social media images for relevant content [89].
- Generative Adversarial Networks (GANs): GANs consist of two competing neural networks: a generator that creates images and a discriminator that evaluates them [90]. This adversarial training process results in highly realistic image generation. In bio-optics, they are pivotal for super-resolution (SR) reconstruction, where a low-resolution (LR) input image is transformed into a high-resolution (HR) output, revealing intricate textures and features essential for early diagnosis, as demonstrated in melanoma detection [90].
- Convolutional Autoencoders (CAEs): Autoencoders learn efficient codings of unlabeled data. The convolutional variant, CAE, has shown superior performance in tasks like image denoising and anomaly detection, often outperforming CNNs in clustering and reconstructing clean images from noisy data, as seen in social media image analysis for urban ecology [89].
AI-Enhanced Bio-optics vs. Traditional Imaging Modalities
The integration of AI creates a significant performance gap between advanced bio-optical techniques and traditional imaging methods. AI-enhanced bio-optics offers superior resolution, quantitative capability, and functional insight, often in a non-invasive manner.
Table 2: Comparative Analysis: AI-Enhanced Bio-optics vs. Traditional Imaging
| Imaging Characteristic | AI-Enhanced Bio-optics | Traditional Imaging (e.g., CT, MRI, US) |
|---|---|---|
| Spatial Resolution | Micrometer to sub-micrometer scale (e.g., OCT, Super-resolution Microscopy) [2] [91] | Millimeter to sub-millimeter scale |
| Key Strengths | High sensitivity, non-invasiveness, molecular contrast, real-time speed [2] | Excellent deep-tissue penetration, well-established clinical protocols |
| Role of AI | Integral to image formation (reconstruction), resolution enhancement, and quantitative analysis [84] [90] | Primarily applied post-hoc for image analysis, segmentation, and computer-aided detection (CADe) |
| Impact of AI | Enables novel capabilities (e.g., super-resolution, virtual staining) [90], reduces acquisition time & cost [84] | Improves diagnostic accuracy and workflow efficiency; does not fundamentally change data acquisition physics |
| Example Application | MELIIGAN for early melanoma diagnosis from dermoscopy [90]; AI-guided PET reconstruction for lesion detectability [84] | AI-based volumetry of tumors in CT scans; automated stroke detection in MRI |
This comparative framework can be visualized as a flowchart, illustrating the fundamental differences in how AI is integrated and the resulting outputs of each paradigm.
Figure 1: AI Integration Pathways in Bio-optics vs. Traditional Imaging. This diagram illustrates the fundamental difference in how AI is applied: as an integral part of the image formation process in bio-optics versus a post-processing step in traditional imaging.
Experimental Protocols and Methodologies
Protocol 1: Super-Resolution Reconstruction for Early Skin Cancer Diagnosis
This protocol is based on the development of MELIIGAN, a novel framework for reconstructing super-resolution images from dermoscopic images to reveal fine-grained features of intermediate skin lesions [90].
- Objective: To reconstruct a high-resolution (HR) image (I{SR}) from a low-resolution (LR) input (I{LR}) for the expedited diagnosis of early-stage melanoma [90].
- Materials:
- Dermoscope: For acquiring initial low-resolution skin lesion images.
- Benchmark Dataset: A curated set of dermatological images with labels (e.g., benign, malignant, intermediate).
- Computational Hardware: High-performance GPU(s) for training deep learning models.
- Methodology:
- Data Preprocessing: Resize all images to uniform dimensions (e.g., 224x224 pixels). Normalize pixel values to a [0,1] range. Apply data augmentation techniques including rotation, flipping, and brightness adjustment to increase dataset diversity and robustness [90].
- Model Architecture (MELIIGAN):
- Generator Network: Utilizes stacked residual blocks to handle larger scaling factors and enable the reconstruction of fine-grained details. The network learns the mapping from (I{LR}) to (I{SR}).
- Discriminator Network: Differentiates between the generated (I{SR}) and real high-resolution (I{HR}) images, forcing the generator to produce more realistic outputs.
- Loss Function Optimization: A hybrid loss function is employed, combining:
- Adversarial Loss: From the discriminator to ensure perceptual realism.
- Charbonnier Loss: A robust substitute for Mean Square Error (MSE), which is less sensitive to outliers and improves edge preservation. A Total Variation (TV) regularization term is added to suppress noise [90].
- Model Training & Evaluation:
- The dataset is split into training, validation, and test sets.
- The model is trained until the generator and discriminator reach a Nash equilibrium.
- Performance is evaluated using Peak Signal-to-Noise Ratio (PSNR) and Structural Similarity Index (SSIM). The proposed MELIIGAN achieved a PSNR of 40.12 dB and an SSIM of 0.946, outperforming other state-of-the-art methods [90].
The workflow for this protocol is methodically structured as follows:
Figure 2: Workflow for Super-Resolution Image Reconstruction using MELIIGAN. The process involves a generative network creating SR images and a discriminator network providing adversarial feedback to improve perceptual quality.
Protocol 2: AI-Assisted Model-Guided Reconstruction for Photoacoustic Computed Tomography (PACT)
This protocol outlines a hybrid approach that integrates physical model-based reconstruction with AI, as applied to PACT, a bio-optical modality that combines light and sound [85].
- Objective: To develop computationally efficient and high-fidelity image reconstruction methods for PACT by incorporating AI-assisted model-guided techniques [85].
- Materials:
- PACT Scanner: System for acquiring initial photoacoustic signal data.
- Neural Field Representations: A technique to represent images as continuous functions approximated by a neural network.
- Methodology:
- Data Acquisition: Collect raw time-series sensor data from the PACT system.
- Hybrid Reconstruction Framework:
- Physical Model Incorporation: The known physics of photoacoustic wave propagation is embedded directly into the reconstruction algorithm's loss function. This ensures the solution is consistent with the measured data.
- AI Assistance: Neural field representations are used to represent the image. This approach can better represent complex tissues and can be trained with novel learning algorithms to efficiently find an optimal solution that satisfies both the data consistency (physics) and any learned priors (AI) [85].
- Validation: The reconstructed images are compared against those generated by purely model-based methods (e.g., filtered back-projection) and purely data-driven deep learning methods in terms of quantitative metrics like contrast-to-noise ratio (CNR) and resolution.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key solutions and technologies central to conducting experiments in AI-driven bio-optical image reconstruction and analysis.
Table 3: Essential Research Reagents and Solutions for AI-Enhanced Bio-optics
| Item Name | Function/Brief Explanation | Example Use Case |
|---|---|---|
| Long-Axial Field-of-View PET/CT Scanner | Enables high-sensitivity, large-coverage, fast, and low-dose imaging, providing rich data for AI reconstruction [84]. | Total-body dynamic imaging for pharmacokinetic studies [84]. |
| Generative Adversarial Network (GAN) Framework | A deep learning architecture for generative tasks, crucial for super-resolution and synthetic data generation [90]. | MELIIGAN for reconstructing high-res skin lesion images [90]. |
| Convolutional Neural Network (CNN) Model | The standard deep learning model for image classification and feature extraction [88] [89]. | Automated classification of urban wild space images from social media [89]. |
| Optical Coherence Tomography (OCT) System | A non-invasive bio-optical imaging technology that uses light to capture micrometer-resolution, cross-sectional images of biological tissues [2] [91]. | Retinal layer segmentation for diagnosing age-related macular degeneration [91]. |
| AI-Assisted Model-Guided Reconstruction Software | Specialized software that integrates physical models of image formation with learned neural priors for superior reconstruction [85]. | Hybrid reconstruction for Photoacoustic Computed Tomography (PACT) [85]. |
| Benchmarked Medical Image Dataset | A curated, labeled dataset of medical images essential for training and validating supervised ML models [90]. | Training and testing the MELIIGAN model for skin cancer diagnosis [90]. |
The fusion of AI with bio-optics is poised for rapid advancement. Key future trends include the rise of self-supervised learning to reduce dependency on large, labeled datasets, the integration of attention mechanisms to improve model focus on relevant image regions [88], and the development of more sophisticated hybrid physics-AI models that are more interpretable and data-efficient [85]. Furthermore, the field will see greater integration of multi-modal data, where AI correlates insights from bio-optical images with genomic, proteomic, and clinical data to provide a holistic view of disease biology, a critical need in drug development [86].
In conclusion, AI and machine learning are not merely incremental improvements but are foundational to the next generation of bio-optical imaging. They are transforming image reconstruction from a simple inversion problem to a knowledge-driven process of information synthesis. This transformation enhances the intrinsic advantages of bio-optics—non-invasiveness, speed, and sensitivity—making it an indispensable tool for researchers and drug development professionals aiming to unravel complex biological processes and deliver precision medicine.
Regulatory Hurdles and the Path to Clinical Translation
Bio-optics, the interdisciplinary fusion of light-based technologies with biology and medicine, is rapidly transforming biomedical research and offers significant advantages over traditional imaging techniques [2]. This field leverages the interactions of light with biological matter to enable non-contact, non-invasive measurement with exceptional sensitivity and speed, providing instant information on dynamic biological processes [2]. Unlike traditional imaging methods like conventional MRI or CT scans, bio-optics technologies can visualize tissue microstructure at the cellular and subcellular level without invasive procedures or ionizing radiation [13] [91].
However, the transition of these innovative technologies from research laboratories to clinical applications faces substantial regulatory challenges. The very advantages that make bio-optics revolutionary—their technological complexity, novel operating principles, and application in sensitive diagnostic and therapeutic roles—also create significant hurdles in the regulatory pathway. This whitepaper examines these regulatory challenges in the context of the evolving 2025 landscape and provides a strategic framework for successful clinical translation, with specific emphasis on navigating the U.S. Food and Drug Administration (FDA) requirements.
The Evolving Regulatory Landscape in 2025
Current Regulatory Framework and Recent Changes
The regulatory environment for bio-optics technologies in 2025 is characterized by significant transitions and increased complexity. Several key developments are shaping the regulatory pathway for these innovative technologies:
ICH E6(R3) Finalization: The updated Good Clinical Practice guideline emphasizes proportionate, risk-based quality management, data integrity across all modalities, and clear sponsor-investigator oversight. Risk-based quality management (RBQM) must now be integrated across the entire study lifecycle rather than being applied仅仅 to monitoring activities [92].
EU Clinical Trials Regulation (CTR): As of January 31, 2025, all EU trials must operate under the centralized CTIS portal, requiring more public transparency, stricter timelines, and reduced tolerance for procedural inefficiencies [92].
FDA Workforce Changes: Recent staffing reductions at the FDA may introduce new challenges, including longer review timelines for Biologics License Applications (BLAs), New Drug Applications (NDAs), and Investigational New Drug (IND) applications. With fewer staff available, companies may experience delays in receiving feedback on study protocols, regulatory submissions, or trial design considerations [93].
The regulatory priorities may also shift with political changes. As one industry expert notes: "Regulatory priorities might shift—an administration focused on deregulation could speed up approval pathways, which might bring new opportunities but could also raise concerns about cutting corners" [94].
Specific Regulatory Challenges for Bio-Optics Technologies
Bio-optics technologies face particular regulatory hurdles that distinguish them from conventional medical devices and imaging systems:
Stringent Regulatory Frameworks: Optical imaging systems employed in medical diagnostics face rigorous regulatory frameworks aimed at ensuring patient safety, product efficacy, and clinical reliability. In the United States, these systems must secure FDA approval, which may involve Pre-Market Approval (PMA) or clearance via the 510(k) process, requiring extensive clinical testing, documentation, and safety and performance evaluations that can span several years [91].
Classification Complexities: Many bio-optics technologies fall into ambiguous regulatory categories, potentially being classified as combination products or facing uncertainty regarding their regulatory pathway. This is particularly challenging for novel applications that don't fit neatly into existing classification frameworks [93].
Ethical and Privacy Considerations: Bio-optics technologies often involve the collection and analysis of sensitive biological and medical data, raising ethical concerns and privacy considerations. Ensuring patient privacy, data protection, and informed consent adds complexity and cost to the development and deployment of bio-optics solutions [14].
Table 1: Key Regulatory Challenges for Bio-Optics Technologies
| Challenge Category | Specific Issues | Impact on Development Timeline |
|---|---|---|
| Approval Process | PMA vs. 510(k) determination, extensive clinical data requirements | Can add 2-4 years to development cycle |
| Technical Standards | Lack of established standards for novel technologies, validation requirements | Additional 6-12 months for testing and validation |
| Data and Evidence | Clinical performance data, comparative effectiveness, real-world evidence | 1-2 years for evidence generation |
| Quality Systems | Good Manufacturing Practices (GMP), ISO certifications, quality management | Ongoing requirements throughout lifecycle |
| Global Harmonization | Differing requirements across regions, regulatory disparities in global studies | Additional 6-18 months for multi-regional approvals |
Strategic Framework for Clinical Translation
Preclinical Validation and Technical Optimization
Robust preclinical validation is essential for establishing the scientific and technical foundation required for regulatory approval. For bio-optics technologies, this involves demonstrating superior performance compared to existing standards and establishing safety profiles.
Key Performance Metrics for Bio-Optics Technologies: Bio-optics technologies must demonstrate clear advantages over traditional imaging methods. For instance, Adaptive Optics Ophthalmoscopy corrects imperfections in the eye's optics, enabling visualization of individual cells that are not visible with conventional clinical instruments [13]. Similarly, Optical Coherence Tomography (OCT) provides micrometer-scale resolution, enabling early diagnosis and effective management of retinal conditions [91].
Table 2: Quantitative Performance Comparison: Bio-Optics vs. Traditional Imaging
| Performance Parameter | Bio-Optics Technology | Traditional Imaging | Advantage Factor |
|---|---|---|---|
| Spatial Resolution | 1-10 micrometers (OCT, AOSLO) [13] [91] | 100-500 micrometers (MRI, CT) | 10-100x improvement |
| Temporal Resolution | Milliseconds to seconds (real-time imaging) [2] | Seconds to minutes | Up to 100x faster |
| Molecular Sensitivity | Single molecule detection (fluorescence imaging) [2] | Limited to macroscopic contrast | Several orders of magnitude |
| Tissue Penetration | 1-3 mm (multiphoton microscopy) [2] | Unlimited (CT, MRI) | Limited but cellular level |
| Clinical Throughput | 100% detection success with automated systems [13] | Variable, often manual operation | Significant improvement |
Figure 1: Clinical Translation Pathway for Bio-Optics Technologies
Protocol Design and Methodological Standardization
Well-defined experimental protocols and standardized methodologies are critical for generating reproducible data that meets regulatory standards. The following detailed protocol for validation of bio-optics imaging systems provides a template for researchers:
Comprehensive Validation Protocol for Bio-Optics Imaging Systems
Objective: To establish performance characteristics, accuracy, and reproducibility of [Bio-Optics Technology Name] for [specific clinical application].
Materials and Reagents:
- [Technology Name] imaging system
- Calibration phantoms with known optical properties
- Biological samples (cell cultures, tissue specimens)
- Reference standard method (e.g., histology, established imaging modality)
- Data analysis software with version control
Procedure:
System Calibration
- Perform daily calibration using standardized phantoms
- Verify illumination intensity, detector sensitivity, and spatial alignment
- Document all calibration parameters and any deviations
Spatial Resolution Assessment
- Image USAF 1951 resolution target or similar standardized test pattern
- Measure modulation transfer function (MTF) at three field positions
- Compare against manufacturer specifications and predicate devices
Contrast-to-Noise Measurement
- Image phantoms with varying contrast levels
- Calculate contrast-to-noise ratio (CNR) using standardized regions of interest
- Establish minimum detectable contrast for the system
Repeatability and Reproducibility Testing
- Acquire repeated measurements of stable phantoms (n=10) within one session
- Perform measurements across multiple days (n=5) with recalibration
- Calculate intra-session and inter-session coefficients of variation
Biological Validation
- Image well-characterized biological samples with known properties
- Compare results with reference standard method using Bland-Altman analysis
- Establish concordance metrics and limits of agreement
Stability Testing
- Monitor system performance parameters over extended period (≥8 hours)
- Document environmental conditions (temperature, humidity)
- Establish stability thresholds for clinical operation
Data Analysis:
- Apply predetermined statistical methods for performance characterization
- Use version-controlled algorithms for quantitative measurements
- Implement blinded analysis where applicable to reduce bias
Acceptance Criteria:
- Spatial resolution within [X]% of specification
- CNR greater than established threshold for clinical utility
- Intra-class correlation coefficient ≥0.9 for repeatability measurements
- Concordance with reference standard within clinically acceptable limits
Essential Research Reagent Solutions
Successful translation of bio-optics technologies requires carefully selected reagents and materials that ensure reproducibility, reliability, and regulatory compliance.
Table 3: Essential Research Reagent Solutions for Bio-Optics Development
| Reagent/Material | Function | Technical Specifications | Regulatory Considerations |
|---|---|---|---|
| Standardized Calibration Phantoms | System performance validation | Traceable to national standards, stable optical properties | Documentation of traceability and stability data |
| Fluorescent Probes and Dyes | Molecular contrast enhancement | High quantum yield, photostability, specific binding | FDA-approved or analogous regulatory status |
| Genetically Encoded Fluorescent Proteins | Intracellular biosensing and labeling | Brightness, photostability, minimal oligomerization | Compliance with gene therapy regulations if applicable |
| Optical Coherence Tomography Phantoms | OCT system validation | Controlled scattering properties, stable microstructure | Validation against clinical endpoints |
| Tissue Mimicking Materials | System performance testing | Biologically relevant optical properties, stability | Documentation of composition and manufacturing process |
| Reference Standard Materials | Method comparison and validation | Well-characterized, established clinical utility | Recognition by regulatory bodies as appropriate comparator |
| Quality Control Assays | Lot-to-lot consistency verification | Validated methods, established acceptance criteria | Inclusion in regulatory submission as part of quality system |
Regulatory Strategy and Submission Framework
Proactive Regulatory Engagement
In the evolving regulatory landscape of 2025, proactive engagement with regulatory agencies is essential for successful translation of bio-optics technologies. Several strategic approaches can facilitate this process:
Early and Frequent Communication: Proactively engage FDA reviewers early in the development process to clarify expectations and minimize unexpected regulatory hurdles. Participate in FDA advisory meetings and industry collaborations to stay informed about evolving policies and staffing changes [93].
Pre-submission Meetings: Utilize pre-submission meetings to obtain feedback on proposed validation strategies, clinical trial designs, and data requirements. These meetings are particularly valuable for novel bio-optics technologies that don't fit established regulatory pathways.
Q-Submission Program: Engage with the FDA's Q-Submission program for feedback on proposed development plans, particularly for novel technologies that may combine diagnostic and therapeutic functions.
The importance of early regulatory engagement cannot be overstated. As noted by regulatory experts, "Sponsors should anticipate potential shifts in regulatory timelines and engagement strategies, adjusting their development plans accordingly" [93].
Comprehensive Documentation Strategies
Robust documentation is fundamental to successful regulatory submissions for bio-optics technologies. Key elements include:
Technical Documentation: Comprehensive system specifications, design history files, and manufacturing controls that demonstrate consistent production of safe and effective devices.
Performance Validation Data: Well-controlled studies establishing analytical performance characteristics, including precision, accuracy, sensitivity, specificity, and reproducibility across the intended use population.
Clinical Validation Evidence: Data from clinical studies demonstrating clinical validity and utility, including comparison to appropriate reference standards and evidence of improved patient outcomes where applicable.
Risk Management Files: Systematic identification, analysis, and control of risks associated with device use, including mitigation strategies and residual risk assessment.
Human Factors Engineering: Validation of usability and human factors engineering processes, particularly for complex bio-optics systems requiring operator interpretation.
Figure 2: Regulatory Submission Framework
Clinical Evidence Generation
Generating robust clinical evidence is paramount for regulatory approval of bio-optics technologies. Key considerations include:
Clinical Trial Design: Innovative trial designs such as adaptive trials, umbrella trials, and platform trials are increasingly important in the current regulatory environment. As one industry expert notes: "I think we will see a resurgence of adaptive trials such as umbrella and platform trials" [94].
Diversity Requirements: Recent guidance from regulatory agencies emphasizes the importance of diverse population enrollment in clinical trials. "2025 seems poised for transformative progress in diversifying clinical trials. To overcome challenges in meeting these diversity goals, sponsors will increasingly need to explore unconventional recruitment avenues" [94].
Endpoint Selection: Carefully selected endpoints that demonstrate clinical utility are essential. For bio-optics technologies, this may include comparison to clinical reference standards, assessment of impact on clinical decision-making, or demonstration of improved patient outcomes.
Real-World Evidence: Incorporating real-world evidence (RWE) and real-world data (RWD) can complement traditional clinical trial data and provide insights into device performance in routine clinical practice.
The clinical translation of bio-optics technologies presents unique regulatory challenges that require strategic planning, robust technical validation, and proactive regulatory engagement. The evolving regulatory landscape in 2025, characterized by updated guidelines, workforce changes, and increasing complexity, demands sophisticated approaches to technology development and regulatory submission.
Successful translation of bio-optics technologies requires balancing innovation with regulatory compliance, demonstrating clear advantages over existing technologies while meeting stringent safety and efficacy standards. By implementing the frameworks and strategies outlined in this whitepaper—including comprehensive preclinical validation, methodological standardization, strategic regulatory engagement, and robust clinical evidence generation—researchers and developers can navigate the complex pathway from laboratory innovation to clinical implementation.
As the field continues to advance, with emerging applications in areas such as cancer diagnostics, point-of-care testing, and minimally invasive procedures, the regulatory framework will likewise continue to evolve. Maintaining flexibility, engaging proactively with regulatory agencies, and prioritizing patient safety and clinical utility will remain essential principles for successful clinical translation of bio-optics technologies.
Bio-Optics vs. Traditional Imaging: A Performance and Application Benchmark
Medical imaging is often synonymous with radiological techniques in the conventional narrative. However, optical imaging technologies represent a distinct and vast field characterized by a highly fragmented distribution across medical specialties, from dermatology and ophthalmology to surgery and family medicine [95]. This whitepaper establishes a direct comparison framework for evaluating bio-optical imaging techniques against traditional radiological methods, focusing on the core parameters of resolution, penetration depth, contrast mechanism, and cost. The global technology revenue valuation for biomedical optical tools is approximately $128 billion USD/year, surpassing the valuation of radiological tools at $48 billion USD/year [95]. Despite this market dominance, optical device research receives significantly less NIH funding ($3.6 billion/year) compared to radiological tools ($8.5 billion/year), indicating a substantial opportunity for accelerated innovation [95]. This analysis is framed within a broader thesis that optical imaging, while less centralized than radiology, provides a cornerstone for next-generation precision medicine through its unique capacity for molecular contrast, real-time functional assessment, and non-ionizing operation [2] [31].
Core Comparison Tables: Performance and Economic Metrics
The following tables provide a consolidated, quantitative comparison of major imaging modalities based on the four key parameters.
Table 1: Technical Performance Comparison of Imaging Modalities
| Modality | Resolution (Spatial) | Penetration Depth | Primary Contrast Mechanism |
|---|---|---|---|
| Optical Coherence Tomography (OCT) | 1 - 10 µm [2] | 1 - 2 mm [2] | Refractive index, scattering [2] |
| Multi-Photon Microscopy | < 1 µm [2] | Up to 1 mm [2] | Fluorescence, SHG/THG [2] |
| Photoacoustic Imaging | 10 - 100 µm [83] | Several cm [83] | Light absorption by chromophores [83] |
| Diffuse Optical Tomography (DOT) | 5 - 10 mm [96] | > 5 cm [96] | Hemoglobin concentration, oxygen saturation [96] |
| NIR-II Fluorescence Imaging | ~10 - 100 µm [21] | 5 - 10 mm [21] | Targeted fluorescent probes [21] |
| MRI | 100 µm - 1 mm [31] | Unlimited (whole body) | Proton density, T1/T2 relaxation [31] |
| CT | 50 - 200 µm [31] | Unlimited (whole body) | X-ray attenuation (electron density) [31] |
| PET | 1 - 2 mm [31] | Unlimited (whole body) | Distribution of radiotracers [31] |
| Ultrasound | 50 - 500 µm [31] | Several cm | Acoustic impedance [31] |
SHG/THG: Second/Third Harmonic Generation. NIR-II: Second Near-Infrared Window (1000-1700 nm).
Table 2: Economic and Operational Comparison
| Modality | System Cost (Approx.) | Operational Cost | Key Applications in Research | Ionizing Radiation |
|---|---|---|---|---|
| OCT | Medium [95] | Low | Ophthalmology, dermatology, cardiology [2] | No |
| Photoacoustic Imaging | $200K - $900K [97] | Medium | Oncology, neuroimaging, vasculature imaging [83] [97] | No |
| NIR-II Imaging | Medium-High [21] | Medium (probes) | Cell tracking, deep-tissue vascular imaging [21] | No |
| MRI | Very High [95] | Very High | Soft tissue anatomy, functional brain imaging [31] | No |
| CT | High [95] | Medium | Bone imaging, lung tissue, angiography [31] | Yes |
| PET | Very High [31] | High (radiotracers) | Metabolic activity, receptor studies [31] | Yes |
| Ultrasound | Low [95] [31] | Low | Real-time imaging, obstetrics, cardiology [31] | No |
Technical Breakdown of Core Parameters
Resolution and Penetration: The Fundamental Trade-Off
A fundamental trade-off in biomedical imaging exists between spatial resolution and penetration depth due to light-tissue interactions [2]. Techniques based on ballistic photons (e.g., OCT, multi-photon microscopy) achieve high resolution (sub-micron to 10 µm) but are limited to superficial depths (1-2 mm) because of intense scattering [2]. Photoacoustic imaging uniquely bypasses this limitation by converting absorbed light into ultrasonic waves, which scatter much less than light in tissue. This "hybrid" approach enables high resolution (10-100 µm) at depths of several centimeters [83]. For whole-body imaging, radiological techniques like MRI and CT provide unlimited penetration but with lower inherent spatial resolution (100 µm and above) [31]. Emerging optical technologies like NIR-II fluorescence imaging (1000-1700 nm) reduce scattering and autofluorescence, improving penetration depth to 5-10 mm with micron-scale resolution, making them ideal for preclinical cell tracking studies [21].
Contrast Mechanisms: Molecular versus Anatomical
Contrast mechanisms define the biological information an image provides.
- Bio-optical Contrast: Primarily derives from molecular interactions. This includes absorption by endogenous chromophores (e.g., hemoglobin, melanin, lipids) [83], fluorescence from targeted probes or proteins [96] [31], and Raman scattering providing molecular vibrational fingerprints [2]. This enables visualization of specific metabolic processes, gene expression, and protein-protein interactions.
- Radiological Contrast: Largely based on bulk physical or anatomical properties. CT measures X-ray attenuation (electron density), while MRI contrasts proton density and relaxation times in different tissue environments [31]. PET and SPECT are exceptions, offering molecular insight through radiotracers, but require ionizing radiation and have lower spatial resolution [31].
Cost Analysis: Acquisition, Operation, and Translation
Cost is a multi-faceted parameter. Optical systems like standard microscopy and ultrasound are generally low-cost and widely accessible [95] [31]. Advanced optical systems (e.g., photoacoustic, non-linear microscopes) and radiological systems (MRI, CT, PET) reside in the high-cost category (>$200,000) [95] [97]. Operational costs diverge significantly: optical imaging often involves recurring costs for fluorescent probes or dyes [96] [21], whereas radiology faces high maintenance costs and, for nuclear medicine, expensive radiotracers [31]. A critical economic advantage of optical techniques is their lack of ionizing radiation, permitting repeated, longitudinal studies in preclinical research without cumulative toxicity, thereby reducing the number of animals needed and improving data quality [31].
Experimental Protocols for Validated Imaging
Protocol: In Vivo Cell Tracking using NIR-II Fluorescence
Objective: To non-invasively track the biodistribution and migration of administered therapeutic cells (e.g., stem cells, immune cells) in a live animal model over time [21].
Cell Labeling (Ex Vivo):
- Isolate and culture the cells of interest (e.g., mesenchymal stem cells, T-cells).
- Incubate the cells with a NIR-II fluorescent contrast agent (e.g., rare-earth-doped nanoparticles, semiconducting polymer dots, or small-molecule organic fluorophores) at a predefined optimal concentration and duration [21].
- Wash the cells thoroughly with PBS to remove any unincorporated contrast agents.
- Validate labeling efficiency and cell viability using an in vitro assay (e.g., flow cytometry, trypan blue exclusion).
Animal Preparation:
- Anesthetize the mouse or rat using an approved anesthetic regimen (e.g., isoflurane).
- Administer the labeled cells via the desired route (e.g., intravenous injection for systemic distribution, local implantation).
Image Acquisition:
- Place the animal in the NIR-II fluorescence imaging system, maintaining anesthesia.
- Set the excitation laser to the appropriate wavelength and use a cooled InGaAs camera for signal detection with a long-pass filter (>1000 nm) [21].
- Acquire sequential images over time (e.g., 1 hour, 24 hours, 7 days post-injection) from multiple views.
Data Analysis:
- Use region-of-interest (ROI) analysis to quantify the fluorescence signal intensity in target organs (e.g., liver, spleen, tumor) and background tissue.
- Calculate the signal-to-noise ratio to assess image clarity.
- Co-register fluorescence images with a white-light photograph or a structural scan (e.g., X-ray) for anatomical context.
Protocol: Multiparametric Tissue Analysis using Photoacoustic Imaging
Objective: To simultaneously visualize tissue microvasculature, oxygen saturation, and lipid distribution in a tumor model [83].
System Calibration:
- Power on the multispectral optoacoustic tomography system and allow the laser to stabilize.
- Perform a system check using a reference absorber (e.g., carbon nanotube suspension) to ensure proper signal generation and detection.
Animal Setup:
- Anesthetize the tumor-bearing mouse and secure it in the imaging chamber.
- Apply ultrasound gel to the skin over the region of interest to ensure acoustic coupling.
- Maintain the animal's body temperature at 37°C using a heating pad.
Multispectral Data Acquisition:
- Acquire optoacoustic images at multiple wavelengths (e.g., 750, 800, 850, 900 nm) across the spectral range of interest. This wavelength tuning is crucial for spectral unmixing [83].
- The system will detect the laser-induced ultrasound waves and reconstruct them into a 3D image dataset for each wavelength.
Spectral Unmixing and Quantification:
- Import the multiwavelength image dataset into the analysis software.
- Apply a spectral unmixing algorithm based on the known absorption spectra of key chromophores:
- Oxy-hemoglobin (HbO2)
- Deoxy-hemoglobin (HbR)
- Lipids
- The algorithm will generate separate, coregistered images showing the spatial distribution and concentration of each chromophore.
- Calculate the oxygen saturation (sO2) map using the formula: sO2 = HbO2 / (HbO2 + HbR).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for Bio-Optical Imaging
| Reagent / Material | Function in Experiment |
|---|---|
| D-Luciferin | Substrate for firefly luciferase in bioluminescence imaging; oxidation reaction produces light, enabling tracking of cell viability and gene expression [31]. |
| NIR-II Fluorophores | Fluorescent probes (e.g., quantum dots, polymer dots) that emit in the second near-infrared window; enable deep-tissue imaging with high contrast for cell tracking and vascular imaging [21]. |
| Targeted Fluorescent Probes | Probes conjugated with antibodies, peptides, or other targeting moieties; bind specifically to biomarkers on cells or in the extracellular matrix, providing molecularly specific contrast [96]. |
| Gold Nanoparticles | Serve as contrast agents for photoacoustic imaging due to their strong and tunable light absorption; can be functionalized for targeted imaging or photothermal therapy [96]. |
| Genetically Encoded Fluorophores | Fluorescent proteins (e.g., GFP, RFP) expressed by transfected cells; allow for long-term, non-diluting labeling of specific cell populations in vivo [31]. |
Visualizing Experimental Workflows and Interactions
Workflow for In Vivo Cell Tracking
Diagram Title: In Vivo Cell Tracking Workflow
Core Principle of Photoacoustic Imaging
Diagram Title: Photoacoustic Imaging Principle
The choice between bio-optical imaging and magnetic resonance imaging (MRI) represents a fundamental consideration in biomedical research and drug development. These modalities offer complementary strengths based on their distinct physical principles: bio-optics leverages photon-tissue interactions to achieve high molecular specificity, while MRI utilizes nuclear magnetic resonance to provide exceptional anatomical depth and resolution. This technical analysis examines their contrast mechanisms, functional imaging capabilities, and practical implementation requirements to guide researchers in selecting appropriate imaging strategies for specific applications. The evolving landscape of both technologies shows promising convergence through multimodal approaches and artificial intelligence enhancement, creating new opportunities for advanced biomedical investigation. [98] [78]
Fundamental Contrast Mechanisms
Bio-Optical Imaging Principles
Bio-optical imaging techniques generate contrast through various photon-tissue interactions, primarily leveraging absorption, emission, and scattering phenomena. These interactions provide molecular specificity by exploiting the unique optical properties of biological components. [78]
Absorption-based techniques rely on light absorption by endogenous chromophores. Photoacoustic imaging (PAI) exemplifies this approach, where absorbed light generates thermal expansion that produces ultrasound waves. This enables deep-tissue visualization of hemoglobin oxygenation, glucose concentrations, and other metabolically important absorbers with spatial resolution that surpasses purely optical techniques. [78]
Emission-based methods primarily utilize photoluminescence, where photons excite molecules that subsequently emit lower-energy photons upon relaxation. Two-photon fluorescence (TPF) and fluorescence lifetime imaging microscopy (FLIM) exploit intrinsic fluorophores like nicotinamide adenine dinucleotide (NADH) and flavin adenine dinucleotide (FAD) to assess cellular energy metabolism without exogenous labels. [78]
Scattering-based approaches include nonlinear techniques like second harmonic generation (SHG), which detects non-centrosymmetric structures such as collagen fibers, and elastic scattering methods like optical coherence tomography (OCT) that provide structural information based on tissue refractive properties. [78]
Magnetic Resonance Imaging Principles
MRI contrast derives from the magnetic properties of atomic nuclei, primarily hydrogen protons in water and fat molecules, when placed in strong magnetic fields. The signal is influenced by multiple tissue-specific parameters that can be weighted through pulse sequence design. [99] [100]
Conventional contrast mechanisms in clinical MRI include T1-weighting (longitudinal relaxation), T2-weighting (transverse relaxation), and proton density. These relative weightings provide excellent soft-tissue differentiation but offer limited quantitative biological information. [100]
Quantitative MRI (qMRI) techniques measure physical tissue parameters with defined units, including T1/T2 relaxation times (ms), proton density (%), diffusion metrics (mm²/s), magnetic susceptibility (ppm), and perfusion parameters (mL/100g/min). These quantitative biomarkers provide objective measures of tissue properties for tracking disease progression and treatment response. [100]
Functional MRI (fMRI) primarily utilizes the blood oxygen level-dependent (BOLD) contrast, which detects changes in blood oxygenation related to neural activity. This weak hemodynamic response is measured using T2*-weighted gradient echo planar imaging sequences with high temporal resolution. [101]
Table 1: Fundamental Contrast Mechanisms in Bio-Optics and MRI
| Imaging Modality | Primary Contrast Mechanism | Physical Basis | Key Measurable Parameters |
|---|---|---|---|
| Bio-Optical Imaging | Photon-tissue interactions | Light absorption, emission, scattering | Hemoglobin concentration & oxygenation, NADH/FAD fluorescence, collagen density |
| MRI | Nuclear magnetic resonance | Precession of hydrogen nuclei in magnetic fields | T1/T2 relaxation times, proton density, diffusion coefficients, magnetic susceptibility |
| Functional MRI | Hemodynamic response | Blood oxygen level-dependent (BOLD) contrast | Signal changes related to deoxyhemoglobin concentration |
Functional and Metabolic Imaging Capabilities
Bio-Optical Functional Imaging
Optical techniques excel at visualizing metabolic activities at cellular and tissue levels through label-free methods that exploit endogenous contrast. [78]
Diffuse optical imaging techniques like near-infrared spectroscopy (NIRS) and diffuse optical tomography (DOT) measure hemodynamic changes by quantifying oxygenated hemoglobin (HbO) and deoxygenated hemoglobin (HbR) concentrations based on their distinct absorption spectra in the near-infrared window. This enables functional brain imaging and monitoring of tissue oxygenation with temporal resolution sufficient to track physiological processes. [99]
Metabolic flux imaging utilizes autofluorescence of metabolic coenzymes NADH and FAD to assess cellular energy metabolism. Fluorescence lifetime imaging (FLIM) provides additional information about protein binding and cellular microenvironment changes that alter fluorescence decay kinetics. These approaches offer real-time monitoring of metabolic responses to pharmacological interventions or disease progression. [78]
Molecular imaging applications have been enhanced by targeted fluorescent probes, including nanobodies and affibodies, which enable specific detection of disease biomarkers. When combined with techniques like fluorescence lifetime imaging, these probes improve tumor specificity and reduce background signal in image-guided surgery applications. [3] [99]
MRI Functional and Metabolic Imaging
MRI provides complementary functional information with greater penetration depth but generally lower molecular specificity compared to optical methods.
fMRI and brain activation mapping detects weak transient signals resulting from neurovascular coupling, where neuronal activity triggers localized increases in blood flow and oxygenation. Advanced preclinical fMRI systems operating at ultrahigh fields (7T-18T) provide sufficient functional contrast-to-noise ratio (fCNR) to map neural circuits with high spatial and temporal resolution, enabling studies of brain function under physiological conditions. [101]
Perfusion and permeability quantification techniques including dynamic susceptibility contrast (DSC) and dynamic contrast-enhanced (DCE) MRI measure parameters like cerebral blood volume (rCBV) and contrast transfer coefficient (Ktrans) to characterize tumor angiogenesis and blood-brain barrier integrity. These quantitative biomarkers are valuable for glioma grading and monitoring treatment response. [100]
Diffusion-based microstructural imaging measures water mobility restrictions in tissue environments, providing metrics like apparent diffusion coefficient (ADC) and fractional anisotropy (FA) that are sensitive to cellular density and white matter integrity. These techniques are particularly valuable for stroke assessment and tracking demyelination in multiple sclerosis. [100]
Table 2: Functional and Metabolic Imaging Capabilities
| Parameter | Bio-Optical Methods | MRI Methods |
|---|---|---|
| Temporal Resolution | Milliseconds to seconds [99] | Seconds to minutes [101] |
| Spatial Resolution | Micrometers to millimeters [78] | Millimeters to hundreds of micrometers [101] |
| Penetration Depth | ~1-3 mm (microscopy), up to several cm (diffuse optics) [99] [78] | Unlimited (whole body) [100] |
| Key Metabolic Targets | NADH/FAD, hemoglobin oxygenation, glucose [78] | Cerebral blood flow, oxygen extraction, pH (via specialized techniques) [101] |
| Molecular Specificity | High (endogenous chromophores, targeted probes) [78] | Moderate to low (primarily physiological contrasts) [100] |
Technical Implementation and Methodologies
Bio-Optical Imaging Systems and Protocols
Bio-optical imaging instrumentation varies significantly based on the specific technique and application requirements:
Diffuse optical imaging systems incorporate three essential components: near-infrared light sources (laser diodes or LEDs), detectors (avalanche photodiodes, silicon photodiodes, or CCDs), and electronics for signal processing. These systems implement three primary measurement schemes: continuous-wave (measures light attenuation only), frequency-domain (modulates light intensity to separate absorption and scattering), and time-domain (uses short light pulses to measure photon time-of-flight). [99]
Advanced microscopy platforms for metabolic imaging typically include pulsed lasers for multiphoton excitation, high-sensitivity detectors (photomultiplier tubes or avalanche photodiodes), and scanning systems for volumetric imaging. Fluorescence lifetime imaging requires additional time-correlated single photon counting electronics to measure nanosecond-scale fluorescence decays. [78]
Image reconstruction in tomography approaches uses mathematical models of light propagation in tissue, implemented through finite element methods, Monte Carlo simulations, or analytical solutions to the diffusion equation. These computationally intensive algorithms convert measured light intensities into spatial maps of absorption and scattering coefficients. [99]
MRI System Requirements and Protocol Optimization
MRI hardware and acquisition parameters significantly impact image quality and quantitative accuracy:
Magnet field strength directly influences signal-to-noise ratio (SNR), with preclinical systems ranging from 3T to 18T. Ultrahigh fields (≥7T) provide supra-linear gains in functional contrast-to-noise ratio for BOLD fMRI, enabling higher spatial resolution for mapping small animal brains. [101]
Gradient performance determines spatial and temporal resolution capabilities, with modern preclinical scanners achieving gradient strengths of 400-1000 mT/m and slew rates of 1000-9000 T/m/s. These high-performance gradients enable rapid switching for echo planar imaging (EPI) sequences used in fMRI, though they generate substantial acoustic noise that may require animal habituation. [101]
Radiofrequency coil design critically impacts SNR, with specialized coils including multi-channel arrays, implantable coils, and cryogenically-cooled coils providing significant sensitivity improvements. Customized coils also enable integration with complementary techniques like optogenetics or electrophysiology through strategic coil design. [101]
Protocol optimization for fMRI requires careful parameter selection including echo time (TE), repetition time (TR), spatial resolution, and parallel imaging factors to balance SNR, temporal stability, and physiological noise. Animal handling and physiological monitoring are equally critical, with specialized cradles providing precise head fixation, anesthetic delivery, and vital sign monitoring to maintain stable physiological conditions during acquisitions. [101]
Experimental Design and Research Applications
Representative Experimental Workflows
Diagram 1: Generalized Preclinical Imaging Workflow. This workflow outlines common steps for both bio-optical and MRI experiments, with modality-specific variations at each stage.
Table 3: Essential Research Tools for Bio-Optical and MRI Imaging
| Tool Category | Specific Examples | Function/Application |
|---|---|---|
| Contrast Agents | Coordination clusters (multi-nuclear Gd3+, Mn2+, Fe3+), gadolinium complexes [102] | Enhanced relaxation rates for MRI contrast |
| Molecular Probes | Targeted fluorescent nanobodies, affibodies, NADH/FAD autofluorescence [3] [99] [78] | Specific molecular target detection in optical imaging |
| Hardware Components | Cryogenic RF coils, implantable detectors, high-performance gradients [101] | Signal-to-noise ratio improvement in MRI |
| Image Reconstruction | AI-based reconstruction (Deep Resolve), model-based deep learning, physics-informed neural networks [103] [104] | Accelerated acquisition, improved image quality |
| Quality Control | Image quality metrics (SSIM, MSE, BRISQUE), phantom testing [103] | Performance monitoring and standardization |
Emerging Trends and Future Directions
The convergence of bio-optical and MRI technologies is creating new opportunities in biomedical imaging. Multimodal approaches combining PET/MRI, PET/fluorescent, and optoacoustic/MRI are being actively developed to leverage complementary strengths of each modality. [105]
Artificial intelligence is transforming both image acquisition and analysis. AI-based reconstruction techniques like Deep Resolve accelerate MRI acquisitions while maintaining image quality, enabling resource-efficient protocols. [103] Similarly, deep learning methods are being applied to optical image reconstruction from undersampled data and automated analysis tasks. [104]
Quantitative imaging biomarker development is advancing toward clinical translation, with consensus efforts focusing on standardization, multiparametric integration, and clinical validation. [100] For bio-optics, technological innovations including wavefront engineering and optical clearing techniques are addressing traditional depth limitations. [78]
Miniaturization and portability trends are enabling new applications, with bio-optical approaches leading in developing compact, cost-effective imaging devices suitable for point-of-care applications and longitudinal monitoring. [98]
Bio-optical imaging and MRI offer complementary capabilities for functional and metabolic imaging in biomedical research. Bio-optical techniques provide superior molecular specificity and temporal resolution for surface and small-animal imaging, while MRI offers unparalleled depth penetration and whole-organ coverage. The choice between these modalities depends on specific research questions, with multimodal approaches increasingly providing comprehensive biological insights. Continuing technological advancements in both fields promise to enhance spatial and temporal resolution, molecular sensitivity, and clinical translation, further solidifying their roles as indispensable tools in biomedical research and drug development.
Medical imaging stands as a cornerstone of modern biomedical research and clinical diagnostics, with bio-optics and computed tomography/X-ray (CT/X-ray) representing two fundamentally different technological approaches. The critical distinction between these modalities lies in their interaction with biological matter: CT and X-ray utilize ionizing radiation that possesses sufficient energy to eject electrons from atoms, potentially damaging cellular components [106]. In contrast, bio-optics employs non-ionizing radiation from the visible light and near-infrared spectrum, which lacks the energy to ionize atoms but can induce electronic excitation for imaging and stimulation purposes [106]. This fundamental physical difference establishes divergent safety profiles that significantly impact their application in basic research, drug development, and clinical translation.
The safety considerations for these imaging classes extend beyond initial physical interaction to encompass complex biological consequences. Ionizing radiation operates through direct DNA damage and indirect oxidative stress generation via water radiolysis, creating complex molecular lesions including double-strand breaks and oxidative base modifications [106]. Bio-optical techniques, while generally considered safer due to their non-ionizing nature, can still induce photothermal effects and photochemical reactions at high intensities that require careful management [106]. For research scientists and drug development professionals, understanding these mechanistic differences is essential for selecting appropriate imaging modalities that align with experimental requirements while minimizing biological perturbation, particularly in longitudinal studies where cumulative effects become significant.
Physical Mechanisms and Biological Interactions
Ionizing Radiation: CT and X-Ray
Ionizing radiation used in CT and X-ray imaging interacts with biological tissues through discrete energy deposition events that can directly and indirectly damage cellular components. The primary interaction mechanisms include photoelectric absorption and Compton scattering, both resulting in electron ejection and subsequent ionization cascades [106]. These physical processes deposit energy in tissue through localized events classified as spurs (≤100 eV, ~4 nm diameter), blobs (100-500 eV, ~7 nm diameter), and short tracks (>500 eV) based on energy transfer magnitude [106]. The probabilistic nature of these interactions means that energy deposition is heterogeneous at microscopic levels, creating complex patterns of molecular damage.
The biological impact of ionizing radiation manifests primarily through DNA damage, with double-strand breaks representing the most lethal lesion type [106]. When ionizing radiation traverses cellular structures, it can directly damage DNA through energy deposition or indirectly through water radiolysis that generates reactive oxygen species (ROS), particularly hydroxyl radicals (.OH) [106]. These radicals subsequently attack DNA bases, producing lesions such as 8-hydroxyguanine and thymine glycol, and causing both single and double-strand breaks [106]. The relative biological effectiveness (RBE) of radiation depends on its linear energy transfer (LET), with high-LET radiation (alpha particles, neutrons) causing more complex, difficult-to-repair damage compared to low-LET radiation (X-rays, gamma rays) [106]. Beyond DNA damage, ionizing radiation induces RNA strand breaks, disrupts three-dimensional genome organization by altering topologically associating domains (TADs), and triggers cellular senescence, mutations, or apoptosis through complex signaling pathways [106] [107].
Non-Ionizing Radiation: Bio-Optics
Bio-optical techniques utilize non-ionizing radiation spanning ultraviolet (UV), visible light, and infrared spectra, with energies insufficient to eject electrons but capable of electronic excitation [106]. The primary interactions include light absorption by specific chromophores, fluorescence emission, and scattering phenomena that provide contrast mechanisms for imaging. Unlike ionizing radiation, non-ionizing radiation primarily induces molecular excitement rather than ionization, though UV light approaching the ionization threshold can still disrupt chemical bonds through non-ionizing photochemical reactions, particularly in DNA molecules [106].
Advanced bio-optical techniques like optogenetics exemplify the precise biological control possible with non-ionizing radiation. In this approach, microbial opsins or engineered photoreceptors are genetically expressed in specific cell populations, enabling light-controlled modulation of cellular activity with millisecond precision [108]. The safety considerations for bio-optics shift from stochastic DNA damage to photothermal effects (tissue heating from light absorption), photochemical damage (particularly with UV light), and photobleaching of fluorescent molecules [106]. Thermal effects become significant with high-intensity applications, especially in infrared and microwave ranges where water absorption converts electromagnetic energy to heat [106]. For instance, microwave radiation can induce both thermal effects (tissue heating) and purported non-thermal effects whose biological significance remains under investigation [106].
Table 1: Fundamental Characteristics of Ionizing versus Non-Ionizing Imaging Modalities
| Characteristic | CT/X-Ray (Ionizing) | Bio-Optics (Non-Ionizing) |
|---|---|---|
| Energy Range | High-energy (X-rays: ~120-140 keV for CT) | Lower energy (Visible light: 1.65-3.26 eV) |
| Primary Interactions | Photoelectric effect, Compton scattering | Absorption, fluorescence, scattering |
| Molecular Targets | DNA (direct damage), Water (indirect via radiolysis) | Specific chromophores, engineered photoreceptors |
| Biological Effects | DNA strand breaks, oxidative damage, carcinogenesis | Photothermal effects, photochemical reactions |
| Cumulative Effects | Significant (dose accumulation) | Generally minimal with proper parameters |
| Safety Measures | ALARA principle, dose monitoring, shielding | Power density limits, exposure duration control |
Quantitative Safety and Dose Comparisons
Radiation exposure from medical imaging represents a critical consideration for research subjects and clinical translation. Effective dose, measured in millisieverts (mSv), enables comparison of radiation risk across different imaging procedures by accounting for tissue-specific radiosensitivity [109]. Natural background radiation provides a useful reference, with the average person in the U.S. receiving approximately 3 mSv per year from natural sources [109]. Diagnostic CT procedures vary significantly in their radiation output, with abdominal CT delivering approximately 7.7 mSv (equivalent to 2.6 years of natural background radiation) and CT colonography delivering 6 mSv (2 years of background radiation) [109]. Notably, repeated studies with contrast material can effectively double these doses, while specialized protocols like lung cancer screening CT utilize lower doses (1.5 mSv) optimized for specific diagnostic tasks [109].
Technological advancements have substantially reduced CT radiation doses without compromising image quality. A 2025 study demonstrated that replacing decade-old CT scanners with new models significantly reduced radiation dose metrics—CT dose index (CTDI) and dose length product (DLP)—while maintaining objective image quality measures like signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) [107]. This improvement reflects evolving detector technology, image reconstruction algorithms, and automated exposure control systems. In stark contrast, bio-optical techniques involve no ionizing radiation exposure, with safety considerations focusing instead on light intensity, duration, and wavelength-specific biological effects [106]. Optical techniques like visible light imaging typically pose minimal risk at diagnostic intensity levels, though therapeutic applications like photodynamic therapy intentionally induce localized photochemical reactions for therapeutic benefit.
Table 2: Radiation Dose Comparison for Common Imaging Procedures in Adults
| Procedure | Approximate Effective Dose (mSv) | Comparable Natural Background Exposure |
|---|---|---|
| Chest X-ray | 0.1 mSv | 10 days |
| Dental X-ray | 0.005 mSv | 1 day |
| CT - Brain | 1.6 mSv | 7 months |
| CT - Chest | 6.1 mSv | 2 years |
| CT - Abdomen/Pelvis | 7.7 mSv | 2.6 years |
| Cardiac CT Angiography | 8.7 mSv | 3 years |
| PET/CT (Whole body) | 22.7 mSv | 7.6 years |
| Bio-optics/Optogenetics | 0 mSv | 0 days |
Experimental Methodologies and Research Applications
CT/X-Ray in Research: Protocol for Dose-Reduced Oncological Imaging
The ongoing optimization of CT protocols for research purposes balances image quality requirements with radiation safety principles. A representative methodology from recent literature demonstrates approaches for validating dose-reduced protocols in oncological imaging:
Objectives: Primary: Determine whether new-model CT scanners reduce radiation dose while maintaining diagnostic image quality. Secondary: Compare objective image quality metrics between scanner generations [107].
Subject Selection: Retrospective inclusion of 14,601 chest and abdominal CT phases from oncologic patients, comparing scans from older scanners (SOMATOM Definition Edge, Brilliance iCT) versus new models (SOMATOM X.ceed, X.cite) [107].
Dose Metrics Extraction: CT dose index (CTDIvol) and dose-length product (DLP) extracted for each acquisition phase (unenhanced, arterial, portal venous, delayed) using commercial dose management software (Radimetrics, Bayer) [107].
Image Quality Evaluation: Random selection of 120 examinations (60 per scanner group) for objective quality assessment. Circular regions of interest placed in abdominal aorta, right hepatic lobe, and paraspinal muscles at L1 level. Signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) calculated using standardized formulas:
- SNRorgan = HUorgan / SD_organ
- CNRorgan = (HUorgan - HUmuscle) / √(SDorgan² + SD_muscle²) [107]
Statistical Analysis: Non-parametric Wilcoxon-Mann-Whitney tests comparing dose metrics and image quality parameters between scanner groups, with significance threshold of p < 0.05 [107].
Results: Significant reductions in CTDI and DLP with new scanners across most phases, with no significant difference in SNR at liver or aorta levels, and improved CNR at aortic level, demonstrating maintained diagnostic quality despite dose reduction [107].
Bio-Optical Experimental Protocol: Optogenetic Control for Neuro-Robotic Systems
Bio-optical methodologies enable precise manipulation and monitoring of biological processes, as exemplified by this optogenetic framework for neural control:
Aim: Utilize optogenetically controlled in vitro neural networks with FORCE learning algorithm to achieve obstacle avoidance in neuro-robotic systems [108].
System Setup: Development of an all-optical biological reservoir computing framework integrating optogenetic stimulation and calcium imaging for simultaneous precise regulation and recording of neuronal activities [108].
Optogenetic Stimulation: Genetic expression of light-sensitive ion channels (e.g., Channelrhodopsin-2) in cultured neural networks, enabling millisecond-timescale neuronal activation via specific light wavelengths (typically 470 nm blue light).
Neural Activity Monitoring: Real-time recording of network dynamics using genetically-encoded calcium indicators (e.g., GCaMP), which fluoresce upon calcium influx during action potentials, providing optical readout of neuronal spiking.
Closed-Loop Control Implementation: Integration with FORCE (First-Order Reduced and Controlled Error) learning algorithm, creating continuous feedback between recorded neural activity and optogenetic stimulation patterns to guide virtual car through obstacle avoidance tasks [108].
Performance Metrics: Tracking of obstacle avoidance success rate throughout training period, with system achieving >95% success rate using minimal output signals from just 15 neurons after approximately 150 seconds of training [108].
Validation: Demonstration of significantly improved obstacle avoidance success rates with optogenetic stimulation compared to control conditions, highlighting the capability of bio-optical systems for precise biological computation [108].
Signaling Pathways and Experimental Workflows
Ionizing Radiation-Induced DNA Damage Response Pathway
Figure 1: Ionizing Radiation DNA Damage Pathway
Bio-Optical Control Experimental Workflow
Figure 2: Bio-Optical Control Experimental Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Imaging Studies
| Reagent/Material | Function | Application Context |
|---|---|---|
| Genetically-Encoded Calcium Indicators (e.g., GCaMP) | Fluorescent calcium sensing for neuronal activity monitoring | Bio-optics: Real-time recording of network dynamics in optogenetic experiments [108] |
| Channelrhodopsin-2 (ChR2) | Light-gated ion channel for neuronal activation | Bio-optics: Precise millisecond-timescale control of specific cell populations [108] |
| Iodinated Contrast Agents | Enhanced tissue contrast for vascular and structural imaging | CT/X-ray: Improved visualization of vasculature and tissue perfusion in oncological studies [107] |
| Phospho-H2AX Antibodies | Immunofluorescence detection of DNA double-strand breaks | CT/X-ray: Quantification of radiation-induced DNA damage in experimental models [106] |
| Reactive Oxygen Species (ROS) Detection Probes | Fluorescent detection of oxidative stress | CT/X-ray: Measurement of indirect radiation damage in biological samples [106] |
| FORCE Learning Algorithm | Adaptive control system for neural decoding | Bio-optics: Closed-loop processing of neural activity for neuro-robotic control tasks [108] |
| 3D Cell Culture Matrices | Support for in vitro neural network development | Bio-optics: Physiologically relevant environments for neural tissue engineering [108] |
| Dose Calibration Phantoms | Standardized measurement of radiation output | CT/X-ray: Quality assurance and protocol optimization for imaging systems [107] |
The choice between bio-optics and CT/X-ray imaging in research contexts involves balancing multiple considerations beyond basic safety profiles. CT and X-ray technologies provide exceptional anatomical resolution and deep-tissue penetration capabilities, with ongoing advancements significantly reducing radiation exposure while maintaining diagnostic quality [107]. These modalities remain indispensable for structural assessment, particularly in oncological research where precise tumor characterization and treatment response monitoring are paramount [110] [107]. The adherence to ALARA (As Low As Reasonably Achievable) principles, combined with technological innovations like AI-based reconstruction and spectral imaging, continues to optimize the risk-benefit ratio for these ionizing modalities [109].
Bio-optical techniques offer complementary advantages in functional imaging and precise perturbation capabilities, enabling researchers to not only observe but actively manipulate biological processes with exceptional cellular specificity and temporal precision [108]. The non-ionizing nature of these approaches facilitates longitudinal studies without cumulative dose concerns, while optogenetic methods provide unprecedented control over specific cellular populations and signaling pathways [108]. For drug development professionals, bio-optical platforms enable high-throughput screening and detailed mechanistic studies of therapeutic candidates in physiologically relevant model systems.
Future directions in medical imaging research will likely emphasize multi-modal integration, combining the structural precision of advanced CT with the functional and molecular capabilities of bio-optical techniques. Emerging fields like radiopharmaceutical theranostics, which combine imaging isotopes with targeted therapeutic compounds, exemplify this convergent approach [110]. Similarly, the development of digital twin technology promises to create comprehensive patient-specific models that integrate multimodal imaging data to predict treatment responsiveness and optimize therapeutic interventions [110]. For researchers and drug development professionals, understanding the complementary strengths, limitations, and safety considerations of both ionizing and non-ionizing imaging modalities remains essential for designing robust experimental paradigms and translating findings into clinical applications.
The evolution of biomedical imaging has been marked by a continuous pursuit of greater resolution and deeper molecular insight. In this landscape, bio-optics and ultrasound represent two fundamental technological approaches with distinct physical principles and capabilities. Bio-optics utilizes light to interrogate biological systems, enabling exceptional resolution and molecular specificity through light-matter interactions [2]. Ultrasound employs high-frequency sound waves, providing excellent soft tissue penetration and real-time functional imaging [111] [112]. This whitepaper provides a technical comparison of these modalities, focusing on their respective strengths in resolution and molecular specificity for research and drug development applications. We examine core technologies, present quantitative performance comparisons, detail experimental methodologies, and explore emerging hybrid approaches that combine advantages of both fields.
Fundamental Principles and Technical Comparison
Core Imaging Principles
Bio-optics encompasses technologies that generate, control, and detect photons for biological interrogation. Imaging relies on phenomena including absorption, emission (fluorescence, bioluminescence), reflection, and scattering of light by biological tissues [2]. Key advantages include non-contact measurement, high speed providing real-time data, sensitivity down to single molecules, and excellent temporal resolution for observing dynamic processes [2]. Techniques range from microscopic (super-resolution microscopy, multi-photon imaging) to macroscopic (diffuse optical tomography) applications.
Ultrasound imaging operates on the pulse-echo principle, where transmitted high-frequency sound waves (1-20 MHz) reflect off tissue interfaces and are detected to construct structural images. Acoustic impedance differences between tissues generate contrast, while Doppler effects enable blood flow measurement [111]. Key advantages include deep tissue penetration (centimeters), real-time imaging capability, portability, and absence of ionizing radiation [111] [112].
Quantitative Performance Comparison
Table 1: Technical comparison of representative bio-optical and ultrasound imaging modalities
| Parameter | Optical Microscopy | Photoacoustic Imaging | High-Frequency Ultrasound | Clinical Ultrasound |
|---|---|---|---|---|
| Spatial Resolution | 1 nm (super-res) - 1 μm (confocal) [2] | 1-50 μm [113] [112] | 20-100 μm [111] | 100-500 μm [111] |
| Penetration Depth | 1 μm - 1 mm [2] | 1-5 cm [112] | 1-3 cm [111] | 5-20 cm [112] |
| Molecular Specificity | Excellent (multiple contrast mechanisms) [2] [11] | Good (optical absorption) [11] [112] | Limited (mainly structural) [111] | Limited (mainly structural) [111] |
| Temporal Resolution | Milliseconds - seconds [2] | Seconds - minutes [113] | Milliseconds (real-time) [111] | Milliseconds (real-time) [111] |
| Key Contrast Mechanisms | Fluorescence, scattering, absorption, Raman shifts [2] | Optical absorption [113] [112] | Acoustic impedance [111] | Acoustic impedance, Doppler shift [111] |
Table 2: Comparison of molecular imaging capabilities
| Aspect | Bio-optics | Ultrasound |
|---|---|---|
| Native Molecular Contrast | Multiple mechanisms (fluorescence, Raman, absorption) [2] [11] | Minimal (requires contrast agents) [111] |
| Contrast Agent Types | Fluorescent probes, nanoparticles, genetically-encoded markers [11] | Microbubbles, nanodroplets, acoustic nanophores [111] |
| Targeting Specificity | Single biomarker level possible [11] | Vascular targets (with targeted microbubbles) [111] |
| Multiplexing Capacity | High (multiple spectral channels) [2] [11] | Low (limited frequency coding) [111] |
| Quantification Capability | Excellent (linear responses common) [11] | Moderate (non-linear acoustic responses) [111] |
Experimental Protocols and Methodologies
Protocol: Fluorescence Molecular Tomography (FMT) for Deep-Tissue Imaging
Principle: FMT reconstructs 3D fluorescence distribution in scattering media using photon propagation models and boundary measurements [11].
Procedure:
- Agent Administration: Inject 2 nmol of near-infrared fluorescent probe (e.g., Cy5.5, ICG) intravenously via tail vein (mouse models) [11].
- Excitation Setup: Illuminate subject with laser diodes (670 nm, 750 nm) at multiple source positions using raster scanning pattern.
- Signal Detection: Capture emitted light (>780 nm) using cooled CCD camera with time-gated detection to reject early photons.
- Image Reconstruction: Apply iterative algebraic reconstruction algorithm with diffusion approximation model for photon migration.
- Quantification: Convert fluorescence intensity to probe concentration using calibration phantom with known dye concentrations.
- Validation: Correlate with ex vivo fluorescence imaging of excised tissues and HPLC analysis of probe concentration.
Applications: Tumor receptor quantification, protease activity monitoring, cell trafficking studies [11].
Protocol: Ultrasound Molecular Imaging with Targeted Microbubbles
Principle: Gas-filled microbubbles functionalized with targeting ligands accumulate at disease sites, enhancing ultrasound signals [111].
Procedure:
- Contrast Agent Preparation: Prepare phospholipid-shelled microbubbles (1-5 μm diameter) conjugated with targeting ligands (e.g., antibodies, peptides).
- Administration: Inject 5×10⁷ microbubbles per kg body weight via slow intravenous bolus injection.
- Imaging Acquisition: Acquire non-destructive contrast-enhanced ultrasound images at mechanical index <0.2 using linear array transducer (5-15 MHz).
- Binding Phase: Allow 5-10 minutes circulation for targeted microbubble adhesion to molecular markers.
- Destruction-Replenishment: Apply high-power ultrasound pulses (mechanical index >0.8) to destroy bubbles in field of view, then monitor fresh bubble inflow.
- Signal Analysis: Quantify adherent microbubble signal by subtracting post-destruction signal from pre-destruction signal.
Applications: Angiogenesis imaging, inflammation assessment, thrombus detection [111].
Visualization of Core Technologies
Diagram 1: Bio-optics interaction mechanisms (44 characters)
Diagram 2: Photoacoustic hybrid principle (38 characters)
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for bio-optics and ultrasound imaging
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Fluorescent Probes (e.g., Cyanine dyes, GFP variants) | Target-specific labeling for optical imaging [11] | Cellular tracking, receptor quantification, molecular activity sensing [11] |
| NIR-II Fluorophores | Deep-tissue imaging with reduced scattering [11] | Intravital microscopy, whole-body imaging [11] |
| Genetically-Encoded Calcium Indicators (GECIs) | Neural activity monitoring [114] | Optogenetics, functional brain imaging [114] |
| Microbubbles (1-5 μm diameter) | Ultrasound contrast agents for vascular imaging [111] | Perfusion assessment, molecular imaging of endothelial targets [111] |
| Targeted Nanoparticles (gold, silica) | Enhanced contrast for photoacoustic imaging [11] [113] | Molecular photoacoustic imaging, therapeutic monitoring [11] [113] |
| Opsins (Channelrhodopsins, Halorhodopsins) | Optogenetic control of cellular activity [114] | Neural circuit manipulation, cardiac pacing [114] |
| Agarose Tissue Phantoms | System calibration and validation [11] | Performance quantification, comparison across imaging systems [11] |
Emerging Technologies and Future Directions
Hybrid Imaging Platforms
The convergence of bio-optics and ultrasound has created powerful hybrid technologies. Photoacoustic imaging (PAI) combines optical contrast with ultrasound resolution, overcoming the traditional depth-resolution tradeoff of pure optical methods [113] [112]. PAI leverages optical absorption of pulsed laser light by tissue chromophores, generating thermoelastic expansion that produces broadband ultrasound waves detectable at depth [113]. This enables high-resolution visualization of hemoglobin, lipids, and contrast agents several centimeters deep—addressing a critical limitation of conventional bio-optics [112].
Clinical Translation and Niche Applications
While ultrasound maintains dominance in applications requiring real-time imaging and deep penetration, bio-optics excels in molecular specificity. Photoacoustic imaging is finding clinical niches in dermatology (visualizing melanomas), cardiovascular imaging (vulnerable plaque detection), and oncology (tumor hypoxia mapping) [112]. These applications leverage its unique ability to combine structural, functional, and molecular information [113] [112].
Technology Advancement Trends
Bio-optics continues to evolve toward higher resolution (super-resolution microscopy breaking the diffraction limit) and greater depth (improved tomographic reconstruction algorithms) [2]. Ultrasound development focuses on higher frequency transducers for improved resolution and novel contrast mechanisms [111]. Both fields are increasingly incorporating artificial intelligence for image reconstruction, enhancement, and interpretation [2] [115]. The integration of these complementary technologies promises to further expand capabilities for biological discovery and therapeutic development.
The field of medical imaging is witnessing a transformative shift with the emergence of bio-optics as a formidable complement and alternative to traditional radiological techniques. Bio-optics, defined as the application of light-based technologies for imaging, analysis, and manipulation of biological samples, has revolutionized diagnostic medicine by providing non-invasive, high-resolution visualization of tissue microstructures in real-time [14] [116]. This whitepaper examines the market dynamics and technological advancements propelling the dominance of bio-optics, with particular emphasis on its application in cancer diagnostics and the pivotal role of Optical Coherence Tomography (OCT). The global bio-optics market, valued at USD 2.03 Billion in 2024, is projected to grow at a compound annual growth rate (CAGR) of 6.3% from 2025 to 2032, reaching nearly USD 3.31 Billion [14]. This growth trajectory underscores the increasing reliance on optical technologies within life sciences research, clinical diagnostics, and therapeutic interventions, positioning bio-optics as an indispensable tool for researchers, scientists, and drug development professionals seeking enhanced precision in pathological assessment and therapeutic monitoring.
Global Market Size and Growth Trajectory
The bio-optics market demonstrates robust expansion driven by technological innovations, increasing research and development activities in life sciences, and growing demand for minimally invasive medical procedures. Market analysis reveals consistent upward trends across all segments, with particularly strong performance in diagnostic applications.
Table 1: Global Bio-Optics Market Projections
| Metric | 2024 Value | 2032 Projection | CAGR (2025-2032) |
|---|---|---|---|
| Total Market Size | USD 2.03 Billion | USD 3.31 Billion | 6.3% |
| Cancer Diagnostics Segment | Dominant Position | Continued Dominance | Expected to Exceed Market Average |
| OCT Device Segment | Dominant Position | Continued Dominance | Expected to Exceed Market Average |
Source: [14]
Application and Technology Segment Dominance
Market segmentation analysis reveals clear patterns of technology adoption and application preference among research and clinical users:
By Device: The Optical Coherence Tomography (OCT) segment dominated the market in 2024 and is expected to maintain leadership throughout the forecast period. OCT's non-invasive imaging capabilities, providing high-resolution, cross-sectional images of biological tissues in real time, have established it as a preferred technology across ophthalmology, cardiology, dermatology, and oncology [14].
By Application: The cancer diagnostics segment dominated the market in 2024 and is projected to continue its dominance. Bio-optics technologies play a crucial role in cancer diagnostics by providing non-invasive imaging and analysis of cancerous tissues, enabling detection and characterization of cancer cells, assessment of tumor margins, and monitoring of treatment responses [14].
By Technology: Raman spectroscopy led the market in 2024, with its powerful analytical capabilities for providing detailed molecular information about biological samples without extensive sample preparation. Its non-destructive nature, high specificity, and ability to analyze samples in their native state make it a dominant technology in the bio-optics market [14].
Comparative Analysis: Bio-Optics vs. Traditional Imaging
Technological Advantage of Optical Systems
Bio-optics offers distinct advantages over traditional radiological imaging modalities, particularly in resolution, safety profile, and functional imaging capabilities.
Table 2: Bio-Optics vs. Traditional Radiological Imaging
| Parameter | Bio-Optics (OCT) | Traditional Radiology (MRI/CT) |
|---|---|---|
| Resolution | Micrometer-scale (typically ~10 μm axial resolution) [117] | Millimeter-scale (MRI), sub-millimeter (CT) |
| Penetration Depth | Few millimeters (1-3 mm typically) [117] | Whole-body capability |
| Radiation Risk | None (uses near-infrared light) [116] [117] | Ionizing radiation (CT), strong magnetic fields (MRI) |
| Imaging Speed | Real-time to seconds (depending on volume) | Minutes to tens of minutes |
| Molecular Contrast | Native contrast from tissue scattering; enhanced with nanoparticles [117] | Primarily anatomical; requires contrast agents for functional data |
| Cost Profile | Lower operational costs | High acquisition and maintenance costs |
Market Impact and Physician Adoption
The global technology revenue valuation of biomedical optical tools reached $128 billion USD/year, significantly surpassing the $48 billion USD/year valuation of radiological tools [95]. This market dominance reflects the widespread integration of optical technologies across medical specialties. Approximately 66% of all physicians utilize optical systems on a nearly daily basis, making optical technology the largest single technology utilized by physicians, compared to approximately 4% of physicians who primarily utilize radiological tools [95].
Technical Deep Dive: Optical Coherence Tomography in Oncology
OCT Working Principle and Technical Evolution
Optical Coherence Tomography functions as a non-contact imaging technique based on low-coherence interferometry to create 3D volumetric images of biological tissues [117]. The underlying principle employs a Michelson-type interferometer where a light beam is split into reference and sample paths; the recombination of reflected beams generates interference patterns that are reconstructed into depth-resolved images [117]. Technological evolution has progressed from time-domain OCT (TD-OCT) to spectral-domain OCT (SD-OCT) and swept-source OCT (SS-OCT), with each generation offering improvements in acquisition speed, sensitivity, and imaging depth [117].
Figure 1: OCT Imaging Principle Workflow
Experimental Protocol for OCT in Cancer Diagnostics
Standardized methodologies have been established for utilizing OCT in cancer diagnostics across various tissue types. The following protocol outlines the key steps for implementing OCT in tumor characterization and margin assessment:
Sample Preparation: For ex vivo imaging, tissue specimens should be fresh or appropriately preserved in phosphate-buffered saline to maintain optical properties. Minimal manipulation is required as OCT typically requires no staining or sectioning [117].
System Calibration: Perform daily calibration using a reference standard with known scattering properties. Verify axial and lateral resolution using standardized phantoms containing embedded microspheres or resolution targets [117].
Image Acquisition:
- Position the sample perpendicular to the imaging beam
- Set appropriate scanning parameters (typically 5-20 μm resolution, 1-3 mm depth)
- Acquire multiple B-scans (cross-sectional) in a raster pattern to generate 3D volumes
- For in vivo imaging, utilize approved probe designs with sterile barriers [118]
Image Analysis:
- Quantitative assessment of backscattering intensity
- Measurement of epithelial layer thickness and integrity
- Identification of architectural disorganization
- Detection of irregular glandular patterns
- Assessment of border effacement between tissue layers [117]
Validation: Correlate OCT findings with histopathological assessment (hematoxylin and eosin staining) as the gold standard. Calculate sensitivity, specificity, and accuracy metrics through blinded reader studies [117].
Research Reagent Solutions for OCT
Table 3: Essential Research Reagents and Materials for OCT Imaging
| Reagent/Material | Function | Application Example |
|---|---|---|
| Gold Nanoparticles | Enhance optical scattering and contrast; functionalize with targeting ligands for molecular imaging | Tumor-specific biomarker detection [117] |
| Superparamagnetic Iron Oxide Nanoparticles | Provide contrast through altered scattering properties; enable multimodal imaging | Lymph node metastasis detection [117] |
| Tissue-Mimicking Phantoms | System calibration and validation; quantitative performance monitoring | Resolution verification and intensity standardization [117] |
| Index-Matching Gels | Reduce surface reflection artifacts; improve signal penetration | Skin and mucosal imaging [118] |
| Targeted Fluorescent Probes | Enable multimodal imaging when combined with OCT; molecular specificity | Intraoperative tumor margin delineation [14] |
Cancer Diagnostics: The Dominant Application Segment
Diagnostic Workflow and Pathway Analysis
In clinical oncology, OCT enables real-time visualization of tissue microstructures, providing critical diagnostic information without the need for invasive biopsy in certain cases. The integration of OCT into cancer diagnostic pathways has demonstrated significant improvements in early detection accuracy and procedural efficiency.
Figure 2: OCT Cancer Diagnostic Pathway
Clinical Performance Metrics
OCT has demonstrated significant diagnostic capabilities across various cancer types:
Dermatological Cancers: OCT enables differentiation of basal cell carcinoma, squamous cell carcinoma, and melanoma through characteristic architectural patterns with sensitivity of ~85% and specificity above 90% in differentiating malignant from benign lymphatic tissue [117].
Gastrointestinal Cancers: In colorectal and esophageal cancer screening, OCT detects submucosal abnormalities with higher sensitivity than traditional white-light endoscopy, providing detailed visualization of epithelial and subepithelial structures [117].
Surgical Guidance: Intraoperative OCT has shown approximately 80% agreement with histology in tumor margin detection in oral cancer, enabling real-time assessment without requiring frozen section analysis [117].
Technological Innovations and Future Directions
Artificial Intelligence Integration in OCT
The integration of Artificial Intelligence (AI), particularly through machine learning (ML) and deep learning (DL) algorithms, has significantly advanced OCT capabilities in cancer diagnostics. AI-driven OCT systems can extract complex patterns and biomarkers from imaging data that may be imperceptible to the human eye, thereby enhancing diagnostic precision [118]. Convolutional neural networks (CNNs) have demonstrated remarkable efficacy in classifying OCT images to identify normal versus cancerous tissue, enabling earlier cancer detection with improved accuracy [118] [119].
Figure 3: AI-Enhanced OCT Analysis Pipeline
Nanoparticle-Enhanced OCT Imaging
The integration of nanoparticles has emerged as a transformative approach to overcome OCT's limitations in molecular contrast. Gold nanoparticles and superparamagnetic iron oxide nanoparticles have demonstrated significant potential in enhancing OCT's diagnostic accuracy through improved optical scattering and targeted biomarker detection [117]. These engineered contrast agents specifically accumulate in tumor tissues through enhanced permeability and retention effects or via targeted ligand-receptor interactions, providing molecular specificity to OCT's structural imaging capabilities [117].
Multimodal Imaging Platforms
Future developments focus on integrating OCT with complementary imaging modalities to create comprehensive diagnostic systems. Hybrid platforms combining OCT with ultrasound, MRI, or positron emission tomography (PET) offer synergistic advantages by combining OCT's high-resolution surface and near-surface imaging with deeper penetration capabilities of other modalities [117]. These systems enable correlation of microscopic tissue architecture with metabolic information and whole-organ or whole-body imaging, particularly valuable for surgical guidance and treatment monitoring in oncology [117].
The bio-optics market continues to demonstrate robust growth and technological advancement, with Optical Coherence Tomography establishing itself as a cornerstone technology in cancer diagnostics. OCT's unique value proposition lies in its ability to provide non-invasive, high-resolution tissue characterization in real-time, addressing critical needs in early cancer detection, biopsy guidance, and surgical margin assessment. The integration of artificial intelligence and nanoparticle contrast agents represents the next frontier in enhancing OCT's diagnostic capabilities, potentially enabling molecular-level tissue characterization without the need for invasive procedures. For researchers, scientists, and drug development professionals, these advancements offer unprecedented opportunities to refine diagnostic paradigms, accelerate therapeutic development, and ultimately improve patient outcomes through precision medicine approaches. As the field continues to evolve, OCT and related bio-optics technologies are poised to become increasingly indispensable tools in the ongoing effort to combat cancer through early detection and targeted intervention.
The integration of bio-optics with multi-modal imaging platforms represents a paradigm shift in biomedical research and clinical diagnostics. This whitepaper examines how light-based technologies are synergistically combining with other imaging modalities to overcome the limitations of traditional single-mode systems. By leveraging the complementary strengths of diverse imaging techniques, these integrated platforms provide unprecedented insights into biological structures and processes across multiple spatial and temporal scales. This technical guide explores the core technologies, experimental protocols, and applications of these platforms, with a specific focus on their transformative potential in drug development and clinical diagnostics. We highlight how bio-optics enhances traditional imaging through superior resolution, molecular specificity, and functional imaging capabilities, ultimately enabling more comprehensive understanding of complex biological systems.
Bio-optics, defined as the interdisciplinary fusion of light-based technologies with biology and medicine, employs light to analyze and manipulate biological materials for precision measurements in fundamental and applied research [2]. This dynamic discipline leverages various forms of light-matter interactions, including absorption, emission, reflection, and scattering, to investigate biological systems from molecular to organismal levels. The core areas of biophotonics encompass bioimaging, biosensing, and photonic-based therapies, which can operate independently or in parallel for enhanced functionality [2].
Multi-modal imaging refers to the integration of two or more imaging techniques or modalities to examine the same subject, with images registered in both space and time [120]. This approach systematically combines complementary biological and clinical data sources such as genomics, medical imaging, electronic health records, and wearable device outputs to provide a multidimensional perspective of patient health [121]. Conceptualized broadly, multi-modal bioimaging involves combining strengths of different imaging approaches to overcome limitations of individual techniques, providing more holistic understanding of investigated samples [122].
The synergy between bio-optics and other imaging modalities emerges from their complementary capabilities. While traditional imaging techniques like MRI, CT, and PET provide excellent anatomical or functional information at macroscopic scales, bio-optical methods offer superior resolution, molecular specificity, and functional imaging capabilities at microscopic levels. This integration enables researchers and clinicians to bridge the gap between structure and function, offering means to image the entire biological repertoire scaling from single molecules to organs [122].
Core Bio-Optical Technologies in Multi-Modal Systems
Key Bio-Optical Imaging Modalities
Bio-optical imaging encompasses several powerful technologies that provide unique insights into biological systems. These modalities exploit various light-matter interactions to reveal different aspects of cellular and tissue structure, composition, and function.
Table 1: Key Label-Free Bio-Optical Imaging Modalities and Their Characteristics
| Modality | Contrast Mechanism | Spatial Resolution | Penetration Depth | Primary Applications |
|---|---|---|---|---|
| Multiphoton Fluorescence (MPF) | Absorption and emission of endogenous fluorophores (NADH, FAD) | Submicron | ~1 mm (depending on tissue) | Cellular metabolism, tissue viability [123] |
| Second Harmonic Generation (SHG) | Non-centrosymmetric structures | Submicron | ~0.5-1 mm | Collagen, myosin, tubulin imaging [123] |
| Stimulated Raman Scattering (SRS) | Molecular vibrational transitions | Submicron | ~0.3-0.5 mm | Chemical bond mapping, molecular composition [123] |
| Optical Coherence Tomography (OCT) | Refractive index variations | 1-10 μm | 1-2 mm | Tissue microarchitecture, ophthalmology [2] |
| Photoacoustic Imaging (PAI) | Light absorption and ultrasound emission | 10-100 μm | Several cm | Hemoglobin, chromophore mapping [2] |
Advantages of Bio-Optical Methods
Bio-optical techniques offer several distinct advantages over traditional imaging approaches that make them particularly valuable for integration into multi-modal platforms:
- Non-contact measurement: The utilization of light facilitates observation of living cells noninvasively, preserving sample integrity without toxic effects [2].
- Speed and instant information: Optical measurements provide rapid, real-time data, significantly reducing interpretation and diagnosis time [2].
- High sensitivity: Optical technologies allow ultrasensitive detection down to single molecules, essential for understanding fundamental biological processes [2].
- Excellent time resolution: Optical methods enable observation of dynamic biological processes across temporal scales, from hours to ultrafast reactions [2].
- Molecular specificity: Techniques like Raman spectroscopy and hyperspectral imaging provide detailed chemical information about samples without exogenous labels [2].
The integration of these bio-optical methods into multi-modal platforms creates systems where the whole is greater than the sum of its parts, enabling comprehensive investigation of complex biological phenomena.
Integration Approaches and System Architectures
Direct vs. Indirect Correlative Imaging
Multi-modal bioimaging approaches generally fall into two broad categories: direct correlative and indirect methods, each with distinct advantages and implementation considerations.
Direct correlative multimodal bioimaging involves using two or more imaging techniques simultaneously (as in hybrid hardware-fused imaging platforms) or sequentially to capture complementary information about the same biological sample and region of interest [122]. This approach is valuable for understanding relationships between different cellular or tissue structures and functions. Examples include correlative light electron microscopy (CLEM), where data is acquired sequentially on the same sample, or PET/MRI scanners, where images are acquired simultaneously on one multimodal instrument [122].
Indirect multimodal bioimaging uses different imaging modalities to study the same biological sample type, but not necessarily at the same time or region within that sample [122]. This approach is useful when synchronizing modalities is challenging, or when each modality must be acquired independently due to technical constraints (e.g., sensitivity issues or need for moving samples between equipment). Data integration is established post-acquisition through computational or analytical techniques.
Integrated Bio-Optical Platform Architecture
Advanced multi-modal platforms now integrate multiple bio-optical techniques into unified systems. One such platform combines multiphoton fluorescence (MPF), second harmonic generation (SHG), and stimulated Raman scattering (SRS) modalities into a single instrument [123]. This integration enables acquisition of multifaceted information from the same localization within cells, tissues, organs, or even bodies, facilitating detailed exploration of intricate relationships between cellular metabolism, extracellular matrix structure, and molecular composition.
The experimental workflow for such integrated systems can be visualized as follows:
This multi-modality approach is increasingly favored over single-modality imaging because it provides a broader range of measurements while mitigating limitations associated with individual techniques [123]. As previously discussed, MPF measures endogenous fluorescence to reflect metabolic changes, SHG can image non-centrosymmetric structures such as collagen, and SRS predominantly detects proteins and lipids based on their vibrational signatures.
Experimental Protocols and Methodologies
Protocol for Multimodal MPF-SHG-SRS Imaging
The following detailed protocol outlines the implementation of a multimodal imaging platform that integrates MPF, SHG, and SRS for biomedical research applications [123]:
System Setup and Calibration
- Laser Warm-up: Power on the laser system and wait approximately 15-20 minutes for stabilization.
- Component Activation: Power on control units and monitors in the specified sequence: Control box → Touch panel controller → AC adapter for main laser remote → AC adapter for sub laser remote.
- Detection System: Power on the Si photodiode detector and lock-in amplifier.
- Beam Configuration: Set up the laser system with a pump beam tunable from 780 nm to 990 nm, 5-6 ps pulse width, and 80 MHz repetition rate. The Stokes laser beam should have a fixed wavelength of 1,031 nm with a 6 ps pulse and 80 MHz repetition rate.
- Alignment: Ensure both pump and Stokes beams are at low power (at least 20 mW) to be visible on the alignment plate. Place an alignment plate in the optical path and adjust beam positioning.
Sample Preparation and Imaging
- Sample Mounting: Secure samples appropriately for the specific experiment (e.g., cell cultures, tissue sections, or live specimens).
- Parameter Optimization: Adjust laser power, detector gain, and scanning parameters based on sample properties to maximize signal-to-noise ratio while minimizing photodamage.
- Sequential Acquisition: Collect MPF, SHG, and SRS images from the same region of interest. The integrated system enables instantaneous coregistration without position adjustments, device switching, or post-analysis alignment [123].
- Data Validation: Verify image quality and coregistration accuracy before proceeding with full experimental acquisition.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of multimodal bio-optical imaging requires specific reagents and materials tailored to each modality:
Table 2: Essential Research Reagents for Multimodal Bio-Optical Imaging
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Heavy Water (D₂O) | Enables metabolic tracking via SRS | Incorporates carbon-deuterium bonds for quantitative measurement of protein synthesis and lipogenesis [123] |
| Alignment Plate | Laser beam alignment and system calibration | Critical for precise optical alignment before sample imaging [123] |
| NADH/FAD Standards | Reference for MPF redox measurements | Enables quantification of optical redox ratios reflecting cellular oxidative state [123] |
| Collagen Reference Samples | SHG signal validation | Provides positive control for SHG imaging of non-centrosymmetric structures [123] |
| Multimodal Contrast Agents | Enhanced visibility across modalities | Probes must cross imaging disciplines and retain properties for tracking proteins/contrast agents/cells in vivo [122] |
Applications in Research and Drug Development
Oncology and Tumor Microenvironment Characterization
Multimodal integration of bio-optics has emerged as a transformative approach in cancer research and oncology, enabling more precise tumor characterization and personalized treatment plans [121]. The integration of multimodal data in cancer care represents one of the most promising advancements in modern oncology, with several key applications:
Enhanced Tumor Characterization: Combining pathological images and omics data through multimodal integration enables accurate prediction of breast cancer subtypes [121]. Dedicated feature extractors capture deep features from pathological images using convolutional neural networks, while genomic and other omics data are processed through deep neural networks. These multimodal features integrate through fusion models to achieve precise prediction of molecular subtypes.
Tumor Microenvironment (TME) Analysis: Advancements in technologies such as single-cell and spatial approaches provide fine-grained resolution of TME, significantly enhancing understanding of cellular interactions at both single-cell and spatial dimensions [121]. Using multimodal features extracted from single-cell and spatial transcriptomics reveals immunotherapy-relevant non-squamous NSCLC TME heterogeneity [121].
Treatment Response Prediction: Multi-modal models can predict responses to targeted therapies using multimodal radiology, pathology, and clinical information. For instance, one model demonstrated accurate prediction of anti-human epidermal growth factor receptor 2 therapy response with an area under the curve (AUC) of 0.91 [121].
Ophthalmology and Neurodegenerative Diseases
In ophthalmology, multimodal integration through combination of genetic and imaging data facilitates early diagnosis of retinal diseases [121]. Optical coherence tomography (OCT) is currently one of the fastest methods in terms of volume elements imaged per second, enabling real-time 3D imaging of dynamic processes, and is already widely established in ophthalmology [2].
For neurodegenerative diseases, multimodal approaches combining bio-optics with other imaging modalities provide insights into disease mechanisms and potential therapeutic interventions. These integrated approaches are particularly valuable for tracking disease progression and treatment response in conditions where anatomical and functional changes occur across different spatial and temporal scales.
Drug Discovery and Development
Artificial intelligence-driven multi-modal ocular biomarkers may improve treatment monitoring and support personalized medicine in ophthalmic drug development [124]. Integrating AI shortens development timelines, enhances efficiency, reduces costs, and increases the success rate of new drugs [124]. Specific applications include:
- Target Identification: AI-powered platforms like PandaOmics integrate gene expression, proteomics, and text-based knowledge graphs to systematically identify and rank potential drug targets [124].
- Computer-Aided Drug Design (CADD): Structure-based drug design leverages 3D structures of biological targets identified through methods like AlphaFold to identify drug candidates [124].
- Molecular Docking and Dynamics: AI-powered docking approaches predict binding affinity and orientation of millions of potential drug molecules more efficiently than traditional methods [124].
Current Challenges and Future Directions
Technical and Implementation Challenges
Despite the significant promise of integrated bio-optics and multi-modal imaging, several substantial challenges remain:
Data Standardization and Integration: Multi-modal analysis typically includes two main steps, co-registration and data-fusion [122]. Co-registration aligns different modalities to a common coordinate space, enabling mapping of spatial regions and/or their derived readouts from one modality to another. Challenges include differences in spatial resolution, field-of-view size, tissue morphological deformations due to sample preparations, and imaging artifacts [122].
Hardware Integration: The co-location of instruments is often necessary for direct correlative imaging, which is rarely feasible as instruments are rarely located in the same facility [122]. Combined platforms across different domains are highly challenging, though some successful examples exist, including combined optical projection tomography and light sheet microscopy, and coupling of quantitative fluorescence endoscopy with MRI [122].
Multimodal Contrast Agents: An important issue in both direct and indirect multimodal imaging is the development of multimodal contrast agents [122]. Such probes need to cross imaging disciplines and retain their properties to track proteins/contrast agents/cells in vivo and be preserved for onward analysis using complementary approaches. While such probes are being developed, they still represent a technical challenge.
Future Directions and Emerging Opportunities
The future of integrated bio-optics and multi-modal imaging platforms lies in several key technological and methodological advancements:
Artificial Intelligence Integration: By 2025, bio-optics solutions are expected to become more integrated with AI and machine learning, enhancing diagnostic accuracy and automation [125]. AI-driven approaches are increasingly being applied to multimodal imaging data, improving image registration, feature extraction, and diagnostic accuracy [120].
Expanded Disease Applications: The future of multimodal integration includes expanded disease applications, such as neurological and otolaryngological diseases, and the trend toward large-scale multimodal models, which enhance accuracy [121].
Advanced Computational Methods: Development of more sophisticated AI algorithms and data fusion techniques will enhance the ability to analyze and interpret complex multimodal data [121]. This includes advanced computational methods for image co-registration and analysis, which will be essential for handling increasingly complex multimodal datasets.
The integration of bio-optics with multi-modal imaging platforms represents a cornerstone of next-generation precision medicine, offering transformative potential for both research and clinical applications [2]. As these technologies continue to evolve and overcome existing challenges, they will undoubtedly revolutionize our understanding of biological systems and enhance our ability to diagnose and treat complex diseases.
Conclusion
The comparative analysis unequivocally positions bio-optics as a transformative force in biomedical research and drug development, not merely as a replacement for traditional imaging but as a complementary suite of tools that offers unparalleled molecular specificity, non-invasiveness, and real-time functional insight. While challenges in data standardization, quantification, and clinical integration remain, the trajectory is clear. The convergence of bio-optics with artificial intelligence, novel materials, and quantum sensing is poised to further revolutionize the field. For researchers and drug development professionals, the strategic adoption of these technologies will be critical for driving the next wave of discoveries in precision medicine, from unraveling complex cellular dynamics to accelerating the development of targeted therapeutics. The future lies in leveraging the unique strengths of each modality within an integrated, quantitative, and data-driven framework.
References
- 1. Biophotonics [https://en.wikipedia.org/wiki/Biophotonics]
- 2. Shining a Light on the Future of Biophotonics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245495/]
- 3. Bio-Optics: Design and Applications (BODA) [https://www.optica.org/events/meeting_archives/2025/bio-optics_design_and_application/]
- 4. Exploring 5 Healthcare Imaging Techniques: Uses and ... [https://www.techtarget.com/pharmalifesciences/feature/Exploring-5-Healthcare-Imaging-Techniques-Uses-and-Limitations]
- 5. Biophotonic probes for bio-detection and imaging | Light [https://www.nature.com/articles/s41377-021-00561-2]
- 6. Biophotonics - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/biophotonics]
- 7. Biophotonics: Optics and Biological Systems [https://avantierinc.com/resources/application-note/biophotonics-optics-and-biological-systems/]
- 8. Predictive techniques in medical imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12218343/]
- 9. Biophotonics: Lighting the Future of Life Sciences [https://blog.bccresearch.com/biophotonics-lighting-the-future-of-life-sciences]
- 10. Advancements in photoacoustic detection techniques for ... [https://www.nature.com/articles/s44384-025-00005-w]
- 11. Advances in Optical Contrast Agents for Medical Imaging [https://www.mdpi.com/2313-433X/11/3/87]
- 12. Advanced second near-infrared fluorophores for ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525007167]
- 13. The Role of Advanced Imaging Technologies in the Future ... [https://eyeandear.org/2025/01/the-role-of-advanced-imaging-technologies-in-the-future-of-eye-care/]
- 14. Bio Optics Market: Global Technology Analysis and Forecast [https://www.maximizemarketresearch.com/market-report/bio-optics-market/189394/]
- 15. The Key Trends Fueling Biophotonics Market Growth from ... [https://www.linkedin.com/pulse/key-trends-fueling-biophotonics-market-growth-from-2025-2032-y58je]
- 16. Next-generation photonic sensors for single-molecule ... [https://www.sciencedirect.com/science/article/pii/S2709472325000486]
- 17. Biophotonics Market Demand & Growth Outlook 2025 to ... [https://www.futuremarketinsights.com/reports/global-biophotonics-market]
- 18. Review Integrative functional optical imaging approaches ... [https://www.sciencedirect.com/science/article/pii/S0006349525005946]
- 19. Label-free single-molecule optical detection | npj Biosensing [https://www.nature.com/articles/s44328-025-00048-9]
- 20. Single Molecule Sensing - MPI for Medical Research [https://www.mr.mpg.de/14599619/single-molecule-sensing]
- 21. Advanced optical imaging technology in the near infrared ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854524005241]
- 22. New hybrid imaging breakthrough could transform ... [https://health.ucdavis.edu/news/headlines/new-hybrid-imaging-breakthrough-could-transform-detection-of-cancer-and-other-diseases/2025/08]
- 23. Nanophotonics in Molecular Imaging and Biomedicine [https://link.springer.com/article/10.1007/s11307-025-02061-w]
- 24. Modern Bioimaging Techniques for Elemental Tissue ... [https://www.mdpi.com/1420-3049/30/13/2864]
- 25. Dual-mode optical imaging system offers new noninvasive ... [https://ecancer.org/en/news/26830-dual-mode-optical-imaging-system-offers-new-noninvasive-approach-to-skin-cancer-diagnosis]
- 26. Editorial: Synergistic Advances in Gene Technology ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1685142/abstract]
- 27. Photonic Biosensors based on Nanoparticle Superstructures [https://www.sciencedirect.com/science/article/pii/S2667325825004947]
- 28. Biomedical optical imaging technology and applications: From basic research toward clinical diagnosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7370594/]
- 29. Challenges and opportunities in clinical translation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5838403/]
- 30. Optical Imaging Technique - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/optical-imaging-technique]
- 31. Optical imaging in biomedical research: guidelines and practical insights | Health Nanotechnology | Full Text [https://healthnanotechnology.biomedcentral.com/articles/10.1186/s44301-025-00004-6]
- 32. Review of bio-optical imaging systems with a high space-bandwidth product - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8849623/]
- 33. Bio photonics Industry 2025-2033 Market Analysis [https://www.datainsightsmarket.com/reports/bio-photonics-industry-11664]
- 34. Artificial Intelligence in Drug & Biological Product Development [https://ctti-clinicaltrials.org/2025-ai-in-drug-biological-product-development/]
- 35. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 36. Resolution in super-resolution microscopy – facts, artifacts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12148039/]
- 37. Investing in Super-Resolution Microscopy [https://www.excedr.com/blog/investing-in-super-resolution-microscopy]
- 38. Real-time, high-throughput super-resolution microscopy ... [https://www.nature.com/articles/s41467-025-64368-0]
- 39. Super-resolution imaging protocols [https://www.nature.com/collections/jgedbdedaa]
- 40. Emerging Photoacoustic Imaging Techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394336/]
- 41. High resolution photoacoustic vascular image reconstruction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12000740/]
- 42. Quantitative photoacoustic imaging using known ... [https://www.sciencedirect.com/science/article/pii/S2213597924000909]
- 43. A Survey on Optical Coherence Tomography—Technology ... [https://www.mdpi.com/2306-5354/12/1/65]
- 44. Optical Coherence Tomography for Three-Dimensional ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2021.744346/full]
- 45. Optical Coherence Tomography (OCT): A Brief Look at the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10744394/]
- 46. Optical coherence tomography—current technology and ... [https://orbit.dtu.dk/en/publications/optical-coherence-tomographycurrent-technology-and-applications-i/]
- 47. High-resolution long-range swept-source OCT for ... [https://opg.optica.org/optica/abstract.cfm?uri=optica-12-8-1144]
- 48. Recent Optical Coherence Tomography (OCT) Innovations ... [https://www.mdpi.com/2306-5354/12/5/441]
- 49. Quantitative evaluation of OCT angiography images in healthy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11226596/]
- 50. Optical-coherence tomography derived quantitative ... [https://www.sciencedirect.com/science/article/pii/S2666914525002106]
- 51. The Rise of Optical Coherent Tomography in Intracoronary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12415738/]
- 52. Discussion on the comparison of Raman spectroscopy and ... [https://link.springer.com/article/10.1007/s10103-025-04315-z]
- 53. Global Raman Spectroscopy Technology Market Study (2025 [https://www.linkedin.com/pulse/global-raman-spectroscopy-technology-market-study-2025-muifc]
- 54. Selecting an Excitation Wavelength for Raman Spectroscopy [https://www.spectroscopyonline.com/view/selecting-excitation-wavelength-raman-spectroscopy]
- 55. A systematic review on the analysis of trace materials via ... [https://www.sciencedirect.com/science/article/abs/pii/S0379073825002476]
- 56. Advances in deep learning-based applications for Raman ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25000463]
- 57. Raman spectroscopy as a tool to accelerate development ... [https://www.sciencedirect.com/science/article/pii/S0168365925008028]
- 58. Light-sheets and smart microscopy, an exciting future is ... [https://www.nature.com/articles/s42003-023-04857-4]
- 59. Advances in Microscopy and Imaging: Enhancing Live Cell ... [https://www.labmanager.com/advances-in-microscopy-and-imaging-enhancing-live-cell-capabilities-with-new-technology-and-software-33746]
- 60. Deep Multiphoton Imaging [https://www.optica-opn.org/home/articles/volume_36/april_2025/features/deep_multiphoton_imaging/]
- 61. Light Sheet Microscopy [https://www.mbfbioscience.com/light-sheet-microscopy]
- 62. A versatile and open source design for one and two photon ... [https://www.nature.com/articles/s41598-025-03107-3]
- 63. Numerical and Experimental Investigation on the Optical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7918515/]
- 64. Optical Tweezers Exploring Neuroscience - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7732537/]
- 65. Optical Manipulation and Its Applications (OMA) [https://www.optica.org/events/meeting_archives/2025/optical_manipulation_and_its_applications/]
- 66. Optical Manipulation and Structured Materials Conference ... [https://spie.org/Publications/Proceedings/Volume/13703]
- 67. 5 Unstructured Data Management Tools to Use in 2025 [https://numerous.ai/blog/unstructured-data-management-tools]
- 68. Exploring the best computer vision datasets in 2025 [https://www.ultralytics.com/blog/exploring-the-best-computer-vision-datasets-in-2025]
- 69. Quantitative Data Analysis. A Complete Guide [2025] [https://www.6sigma.us/six-sigma-in-focus/quantitative-data-analysis/]
- 70. A Practical Guide to Quantitative Data Analysis Methods ... [https://www.looppanel.com/blog/quantitative-data-analysis-methods]
- 71. Biomedical Applications of Translational Optical Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC8587670/]
- 72. MethodsJ2: A Software Tool to Capture Metadata and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9488561/]
- 73. Community-developed guidelines for publishing images ... [https://www.rockefeller.edu/news/34834-community-developed-guidelines-for-publishing-images-help-address-reproducibility-problem-in-science/]
- 74. Reporting reproducible imaging protocols [https://www.sciencedirect.com/science/article/pii/S2666166722009194]
- 75. Best Practices for Quality Control in Optical Components [https://www.uqgoptics.com/best-practices-for-quality-control-in-optical-components/]
- 76. BioOptics - Light Microscopy [https://www.maxperutzlabs.ac.at/research/facilities/biooptics-light-microscopy]
- 77. A quantitative metric for the comparative evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7907228/]
- 78. Light and metabolism: label-free optical imaging of ... [https://opg.optica.org/boe/abstract.cfm?uri=boe-16-9-3770]
- 79. Enhanced penetration depth in optical coherence ... [https://opg.optica.org/optica/abstract.cfm?uri=optica-12-1-24]
- 80. Towards accurate penetration depth estimation in near- ... [https://opg.optica.org/boe/abstract.cfm?uri=boe-16-12-5161]
- 81. Investigating phototoxicity of optical coherence tomography ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648325003827]
- 82. Optical sectioning methods in three-dimensional bioimaging [https://www.nature.com/articles/s41377-024-01677-x]
- 83. Advances in Optoacoustic Imaging [https://www.nature.com/collections/hbhcfdicee]
- 84. Artificial Intelligence-Guided PET Image Reconstruction ... [https://pubmed.ncbi.nlm.nih.gov/40858423/]
- 85. AI-assisted Model-Guided Image Reconstruction Methods with ... [https://www.aps.anl.gov/APS-Events/2025-06-17/ai-assisted-model-guided-image-reconstruction-methods-with-application-to]
- 86. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 87. 10 Machine Learning Algorithms to Know in 2025 [https://www.coursera.org/articles/machine-learning-algorithms]
- 88. Machine Learning Image Classification Guide 2025 [https://encord.com/blog/machine-learning-image-classification-guide/]
- 89. Leveraging machine learning techniques for image ... [https://www.nature.com/articles/s41598-025-06731-1]
- 90. A promising AI based super resolution image ... [https://www.nature.com/articles/s41598-025-89693-8]
- 91. Optical Imaging Technologies Market Size 2025-2029 [https://www.technavio.com/report/optical-imaging-technologies-market-industry-analysis]
- 92. Clinical Research in 2025: Key Shifts, Challenges, and ... [https://blog.cloudbyz.com/resources/clinical-research-in-2025-key-shifts-challenges-and-whats-next]
- 93. Navigating Regulatory Uncertainty: Adapting to FDA ... [https://www.allucent.com/resources/blog/navigating-regulatory-uncertainty-fda-changes-2025]
- 94. The biggest challenges clinical trials will face in 2025 [https://www.clinicaltrialsarena.com/features/clinical-trials-challenges-expect-2025/]
- 95. Perspective on the optics of medical imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10541334/]
- 96. Advances in Optical Contrast Agents for Medical Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC11942650/]
- 97. Photoacoustic Imaging Market: $80M to $105M Growth ... [https://finance.yahoo.com/news/photoacoustic-imaging-market-80m-105m-123000819.html]
- 98. Medical Imaging Devices and Optical Technology [https://www.medicaldevice-network.com/buyers-guide/medical-imaging-technology/]
- 99. Biophotonics techniques for structural and functional ... [https://pmc.ncbi.nlm.nih.gov/articles/mid/NIHMS611949/]
- 100. Quantitative MRI in Neuroimaging: A Review of Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562573/]
- 101. Advanced preclinical functional magnetic resonance ... [https://www.nature.com/articles/s44303-025-00085-z]
- 102. Coordination clusters as emerging magnetic resonance ... [https://www.sciencedirect.com/science/article/pii/S2950584425000220]
- 103. Quantitative image quality metrics enable resource-efficient ... [https://link.springer.com/article/10.1007/s10334-025-01253-3]
- 104. Quantitative Bio-Imaging Lab [https://qbioimaging.github.io/]
- 105. Molecular Probes and Imaging Agents [https://www.nibib.nih.gov/programs/molecular-imaging]
- 106. Multiple radiations and its effect on biological system [https://pmc.ncbi.nlm.nih.gov/articles/PMC11995768/]
- 107. Radiation Dose Reduction in Cancer Imaging with New- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12153870/]
- 108. Volume 30 Issue 10 | Journal of Biomedical Optics [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-30/issue-10]
- 109. Radiation Dose from X-Ray and CT Exams [https://www.radiologyinfo.org/en/info/safety-xray]
- 110. Top 7 Trends in Imaging Clinical Trials for 2025 [https://www.qmenta.com/blog/top-trends-in-imaging-clinical-trials-for-2025]
- 111. Comparison of optical biometry versus ultrasound biometry in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12240281/]
- 112. Defining the clinical niche for photoacoustic imaging [https://www.nature.com/articles/s44222-025-00284-8]
- 113. A comprehensive review of high-performance ... [https://www.sciencedirect.com/science/article/pii/S221359792500062X]
- 114. Roadmap for direct and indirect translation of optogenetics ... [https://www.nature.com/articles/s41593-025-02097-9]
- 115. Global Bio-imaging Market Size & YoY Growth Rate, 2025- ... [https://www.coherentmarketinsights.com/industry-reports/global-bio-imaging-market]
- 116. Bioimaging: Evolution, Significance, and Deficit - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9541884/]
- 117. OCT in Oncology and Precision Medicine: From Nanoparticles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189282/]
- 118. Artificial intelligence in advancing optical coherence ... [https://www.sciencedirect.com/science/article/abs/pii/S074879832500616X]
- 119. Artificial intelligence in advancing optical coherence ... [https://pubmed.ncbi.nlm.nih.gov/40839924/]
- 120. Multimodal Imaging | Integration, Techniques & Applications [https://collectiveminds.health/articles/multimodal-imaging-complete-guide-to-integration-applications]
- 121. Multimodal Integration in Health Care - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370271/]
- 122. Multimodal bioimaging across disciplines and scales [https://www.nature.com/articles/s44303-024-00010-w]
- 123. Multimodal Optical Imaging Platform for Studying Cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626104/]
- 124. Ophthalmic drug discovery and development using artificial ... [https://www.nature.com/articles/s41746-025-01954-y]
- 125. Top Bio-optics Companies & How to Compare Them (2025) [https://www.linkedin.com/pulse/top-bio-optics-companies-how-compare-them-2025-alphavista-research-vfbme/]