Bio-Optics 2025: A Comprehensive Guide to Design, Applications, and Future Trends in Biomedical Light Technologies
This article provides researchers, scientists, and drug development professionals with a current and in-depth exploration of bio-optics, the field leveraging light-based technologies for biological and medical applications.
Bio-Optics 2025: A Comprehensive Guide to Design, Applications, and Future Trends in Biomedical Light Technologies
Abstract
This article provides researchers, scientists, and drug development professionals with a current and in-depth exploration of bio-optics, the field leveraging light-based technologies for biological and medical applications. It covers foundational principles, core technologies like Optical Coherence Tomography (OCT) and Raman spectroscopy, and their transformative applications in cancer diagnostics, infectious disease detection, and minimally invasive surgery. The content also addresses key optimization strategies, the integration of artificial intelligence (AI), and provides a comparative analysis of emerging technologies and market trends to guide research and development decisions in this rapidly advancing field.
The Principles and Expanding Scope of Bio-Optics
Bio-optics and biophotonics represent a dynamic interdisciplinary frontier that merges the principles of optics and photonics with biology and medicine. This field utilizes light-based technologies to analyze, detect, and manipulate biological materials, driving innovations across medical diagnostics, therapeutics, and fundamental research [1]. While the terms are often used interchangeably, biophotonics broadly encompasses the interaction of light with biological matter, including the development of tools for imaging, sensing, and therapy [2] [3]. In contrast, bio-optics often refers more specifically to the design and application of optical instruments and systems for solving biological problems, a focus reflected in specialized conferences like the Optica Bio-Optics: Design and Application (BODA) meeting [4]. The core of this discipline lies in understanding fundamental light-biological matter interactions—such as absorption, emission, fluorescence, and scattering—and leveraging this knowledge to develop technologies that provide high spatial and temporal resolution for observing biological processes in real-time [2] [5]. This technical guide outlines the core principles, advantages, and methodologies of bio-optics and biophotonics, framed within the context of advanced design and application research.
Core Concepts and Fundamental Interactions
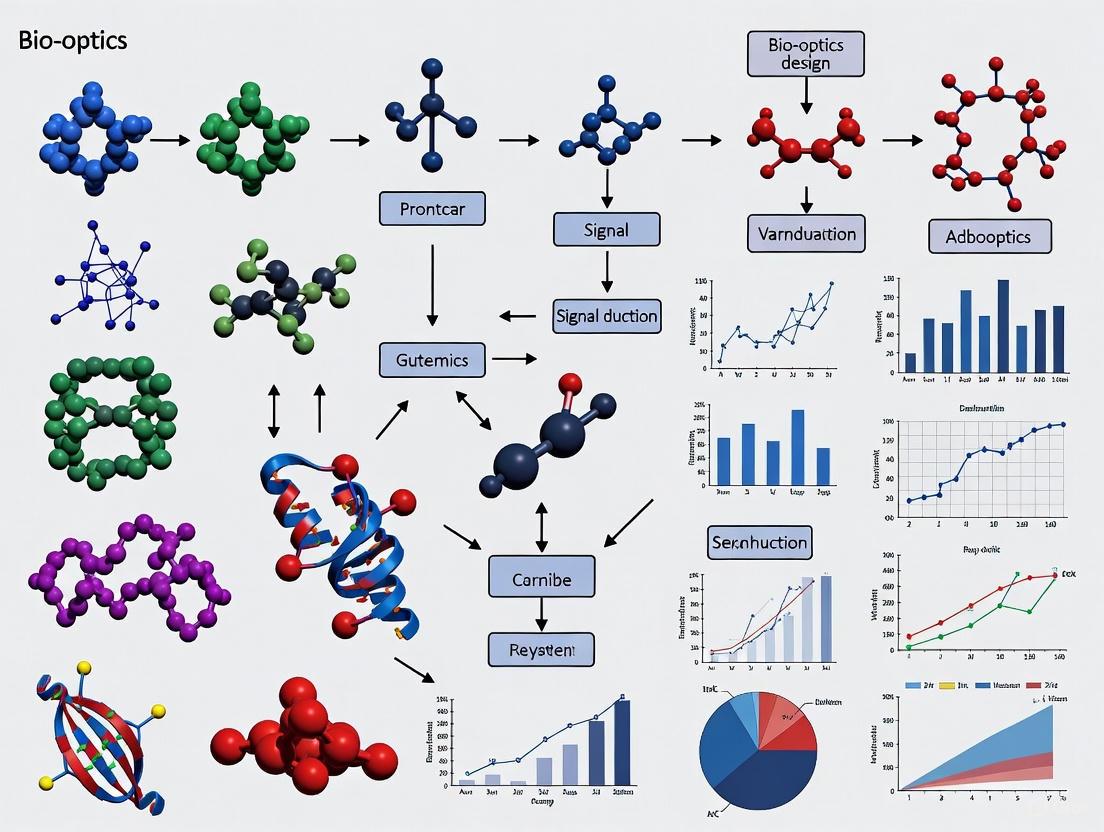
The theoretical foundation of biophotonics rests on the interactions between photons and biological components, ranging from single molecules to entire tissues. The following diagram illustrates the primary physical phenomena that occur when light interacts with biological matter.
Light-Biology Interaction Mechanisms
Absorption and Emission: When biological molecules absorb photons, they enter an excited state. Upon returning to ground state, they may emit light through processes like fluorescence or phosphorescence [5]. This principle is harnessed in fluorescence microscopy, where specific fluorophores are used to label and visualize cellular components, enabling the study of dynamic processes in living cells.
Scattering: Light can be elastically scattered (Rayleigh scattering) or inelastically scattered (Raman scattering) by biological tissues. Optical Coherence Tomography (OCT) leverages back-scattered light to generate high-resolution, cross-sectional images of tissue morphology in real-time, making it invaluable in ophthalmology and cardiology [6] [7].
Surface Plasmon Resonance (SPR): This label-free biosensing technique detects changes in the refractive index near a metal surface, allowing researchers to monitor biomolecular interactions—such as antigen-antibody binding—in real-time without the need for fluorescent labeling [5].
Key Advantages and Technological Benefits
Biophotonic technologies offer significant advantages over conventional methods in biological research and clinical practice, which can be summarized in the following table.
Table 1: Key Advantages of Biophotonic Technologies
| Advantage | Technical Description | Primary Applications |
|---|---|---|
| Non-Invasiveness & High Resolution | Enables visualization of biological structures and processes in vivo without causing damage, with resolutions down to the cellular and molecular level [2] [7]. | Real-time cellular imaging, in vivo functional brain mapping, tumor microenvironment studies [7]. |
| Minimally Invasive Therapeutics | Replaces conventional surgery through endoscopic delivery of light via flexible optical fibers, reducing patient pain and recovery time [3]. | Laser endoscopic surgery, photodynamic therapy (PDT), intraluminal calculi removal [3]. |
| Precision and Specificity | Allows for targeted interaction with specific tissues or molecules through control of light parameters like wavelength and intensity [3] [1]. | Laser tissue processing (incision, coagulation), selective tumor excision, optogenetics [3]. |
| Rapid, Real-Time Analysis | Provides immediate feedback and monitoring of biological processes, enabling rapid diagnostics and dynamic study of cellular functions [2] [7]. | Point-of-care biosensing, surgical guidance, monitoring of cellular dynamics and drug responses [7]. |
These advantages collectively contribute to the transformative impact of biophotonics. The technology facilitates a reduction in treatment times, minimizes surgical trauma and blood loss through high-temperature laser incision that seals small blood vessels, and provides unparalleled precision for both diagnostic and therapeutic interventions [3]. The integration of optical fibers allows light to be delivered to previously inaccessible areas of the body through natural openings or small incisions, fundamentally changing surgical approaches [3] [6].
Essential Optical Components and Research Tools
The advancement of biophotonics relies on a suite of core optical components that enable the generation, manipulation, and detection of light for biological applications. The table below details these essential tools and their functions within the researcher's toolkit.
Table 2: Essential Optical Components in Biophotonics Research
| Optical Component | Primary Function | Specific Research Applications |
|---|---|---|
| Lasers | Emit high-intensity, coherent light at specific wavelengths and intensities [6] [1]. | Tissue ablation, coagulation, cell manipulation, optical tweezers, flow cytometry [3] [6]. |
| Imaging Systems | Visualize and observe cellular and tissue structures and functions [6] [1]. | Confocal microscopy, multiphoton microscopy, super-resolution imaging, optical coherence tomography [6] [5]. |
| Fiber Optics | Deliver light precisely into tissues and enable light transmission within living organisms [6] [1]. | Endoscopic imaging and surgery, light delivery in photodynamic therapy, in vivo sensing [3] [6]. |
| Spectrometers | Analyze the wavelength and intensity of light [6] [1]. | Measuring fluorescence and absorption spectra, Raman spectroscopy, characterizing biological samples [6]. |
Customization of these optical systems is a critical trend, allowing researchers to optimize parameters such as resolution, wavelength, and power for specific experimental needs. This customization enhances performance, provides greater experimental flexibility and control, and improves cost-efficiency by eliminating unnecessary features [1]. For instance, custom-designed imaging systems can be developed to provide high resolution within specific wavelength ranges crucial for particular fluorescence markers.
Detailed Experimental Protocols
Protocol: In Vitro Cell Imaging Using Fluorescence Microscopy
Fluorescence microscopy is a cornerstone technique for visualizing the localization and dynamics of specific molecules within cells.
Table 3: Key Reagent Solutions for Fluorescence Microscopy
| Reagent/Material | Function | Example Specifics |
|---|---|---|
| Fluorescent Dyes or Proteins | Bind to or are expressed by cellular targets to provide contrast. | GFP (Genetic Encoding), FITC (Antibody Conjugation), Hoechst stains (Nuclear DNA) [5]. |
| Cell Culture Media & Buffers | Maintain cell viability and provide a physiological environment during imaging. | Phenol-free medium (to reduce background fluorescence), PBS for washing [5]. |
| Fixation and Permeabilization Agents | Preserve cell structure and enable dye access to intracellular targets (for fixed cells). | Paraformaldehyde (fixation), Triton X-100 (permeabilization) [5]. |
| Mounting Medium | Preserve samples under coverslips for high-resolution imaging. | Antifading agents to reduce photobleaching [5]. |
Methodology:
- Sample Preparation: Culture cells on sterile, glass-bottomed dishes. For fixed cell imaging, treat cells with a fixative (e.g., 4% paraformaldehyde) followed by a permeabilization agent if labeling internal targets. Incubate with specific primary antibodies and then with fluorescently-labeled secondary antibodies. For live-cell imaging, use cells expressing genetically encoded fluorescent proteins like GFP.
- Microscope Setup: Configure the fluorescence microscope (widefield, confocal, or multiphoton). Select appropriate excitation and emission filters matched to the spectral properties of the fluorophores used. For confocal microscopy, set the pinhole aperture to optimize optical sectioning and signal-to-noise ratio.
- Image Acquisition: Illuminate the sample with the specific excitation wavelength. The emitted light from the fluorophores is captured by a high-sensitivity detector (e.g., PMT or CCD camera). For live imaging, control environmental factors (temperature, CO₂). Minimize light exposure to prevent phototoxicity and photobleaching.
- Image Analysis: Use software to process acquired images for tasks like colocalization analysis, fluorescence resonance energy transfer (FRET) to monitor molecular interactions, or fluorescence recovery after photobleaching (FRAP) to study protein mobility [5].
Protocol: In Vivo Tumor Imaging and Photodynamic Therapy (PDT)
PDT is a clinically approved biophotonic therapy that combines light, a photosensitizer, and tissue oxygen to selectively destroy target cells [3]. The workflow is complex, integrating pharmacokinetics, light delivery, and therapeutic action, as shown in the following diagram.
Methodology:
- Photosensitizer Administration: A light-sensitive chemical (photosensitizer) is administered to the patient intravenously or topically. The photosensitizer is designed to be preferentially absorbed and retained by rapidly dividing tumor cells compared to healthy tissue [3].
- Drug-Tissue Interval: A specific time interval (ranging from hours to days) is allowed for the photosensitizer to clear from normal tissues and accumulate in the target tumor tissue.
- Light Application: The target tumor is irradiated with light of a specific wavelength (typically in the near-infrared range for deeper tissue penetration) that corresponds to the absorption peak of the photosensitizer. This light can be delivered via optical fibers or specialized light sources [3] [6].
- Therapeutic Action: The activated photosensitizer interacts with molecular oxygen in the tissue, generating reactive oxygen species (ROS), such as singlet oxygen. These highly cytotoxic species induce oxidative damage to cellular components, leading to targeted cancer cell death, vascular damage within the tumor, and an associated inflammatory response [3].
Future Outlook and Emerging Trends
The field of bio-optics and biophotonics is poised for significant evolution, driven by several converging technological trends. A major growth area is the development of miniaturized and portable devices, including handheld imaging probes and wearable biosensors, which facilitate point-of-care diagnostics and continuous health monitoring [2] [7]. The integration of Artificial Intelligence (AI) and Machine Learning (ML) is revolutionizing data analysis, enhancing image reconstruction, automated lesion detection, and the interpretation of complex biological data, thereby improving diagnostic accuracy and speed [2] [4] [8].
Furthermore, the fusion of biophotonics with nanotechnology is leading to the creation of novel biophotonic nanostructures and nanophotonic biosensors. These advancements enable ultrasensitive tracking of biomarkers and pathogens, opening new avenues for early-stage disease detection and personalized medicine [7] [9]. Research is also advancing novel therapeutic applications, such as optogenetics for precise neural stimulation and the use of NIR phototherapy for wound healing and tissue repair [3] [7]. Despite the promising outlook, the field must overcome challenges related to high equipment costs, the need for specialized training, limited optical penetration depth in tissues, and the complexities of regulatory approval and clinical translation [7] [9]. Ongoing research and interdisciplinary collaboration are crucial to addressing these hurdles and fully realizing the potential of biophotonics in advancing healthcare and biological research.
This document serves as an in-depth technical guide to the fundamental principles of light-matter interactions, framed within the context of bio-optics design and application research. Biophotonics—the interdisciplinary fusion of light-based technologies with biology and medicine—is rapidly transforming scientific research, diagnostics, and therapy [10]. At its core, biophotonics involves the use of light to analyze and manipulate biological materials, providing a powerful tool for understanding and influencing life processes at the molecular, cellular, tissue, and organ levels [10]. The field leverages key optical phenomena, including absorption, emission, scattering, and reflection, to enable groundbreaking applications in bioimaging, biosensing, and photonic-based therapies [10]. This whitepaper provides researchers, scientists, and drug development professionals with a detailed examination of these core interactions, their quantitative descriptors, associated experimental methodologies, and the essential reagents and materials required for their investigation in a biological context.
Fundamental Interactions and Quantitative Parameters
When a photon interacts with an atom or molecule, three primary outcomes are possible: elastic scattering, inelastic interaction, or absorption with energy dissipation [11]. The following sections detail these phenomena and their quantitative measures, which are critical for designing bio-optical instruments.
Absorption
Absorption occurs when a photon is absorbed by a molecule, causing an electron to move from its ground state to a higher, excited state [11]. The excited state could be virtual or a quantum level permitted for the molecule, depending on the photon's energy and the difference between the molecular energy levels [11]. At a microscopic scale, absorption is described by the polarizability (P) of the media in response to the optical field (E) via the electrical susceptibility (χ) [11]. Macroscopically, absorption manifests as attenuation of light intensity, governed by the Beer-Lambert law [11]. The absorption coefficient (μₐ) is a key parameter that depends on the wavelength of light and the complex-valued refractive index at the incident wavelength [11].
Emission
Emission processes involve the release of energy as photons when excited electrons relax to lower energy states. A key emission phenomenon is fluorescence, which occurs when an absorbing electron relaxes from its excited state and releases energy as a photon [11]. During the nanosecond-scale excited state, some energy dissipates through vibrational relaxation, resulting in the emitted photon having a longer wavelength than the absorbed photon—a phenomenon known as the Stokes shift [11]. The time lag between excitation and emission is the fluorescence lifetime, which exhibits a temporal profile of exponential decay [11]. Fluorophores possess unique absorption and emission spectra and fluorescence lifetimes that are generally dependent on their chemistry and can be altered by their environment [11].
Scattering
Scattering refers to any interaction that changes the trajectory of light and is responsible for phenomena such as the twinkling of stars and the turbidity of milk [11]. Scattering can be elastic, where the excitation and emission wavelengths are identical, or inelastic [11]. The scattering coefficient (μₛ) is often combined with the absorption coefficient in modified versions of the Beer-Lambert law [11]. Scattering mechanisms are categorized based on particle size relative to the wavelength of light, with three primary types being Rayleigh scattering (particle size ≤ wavelength), Mie scattering (particle size 1-10× wavelength), and geometric scattering (particle size >> wavelength) [11]. For Mie scattering by particles typically 1-10 times the wavelength of light, over 90% of the light is forward scattered and 1-5% is back-scattered [11].
Reflection
Reflection is a fundamental light-matter interaction where light bounces off a surface or interface between two media. In the context of biophotonics, reflection is often considered alongside scattering phenomena, as both involve changes in light direction without alteration of its energy [11]. Reflection plays a crucial role in various bio-optical techniques, particularly in surface-based imaging and sensing applications where light interacts with tissue interfaces or sensor surfaces.
Table 1: Key Parameters for Light-Matter Interactions in Bio-optics
| Interaction Type | Governing Law/Principle | Key Quantitative Parameter(s) | Biological Application Examples |
|---|---|---|---|
| Absorption | Beer-Lambert Law | Absorption Coefficient (μₐ) | Measuring chromophore concentration (e.g., hemoglobin, melanin) [11] |
| Emission | Exponential decay kinetics | Fluorescence Lifetime, Quantum Yield | FRET imaging, cellular environment sensing, molecular tracking [11] |
| Scattering | Mie, Rayleigh theories | Scattering Coefficient (μₛ), Anisotropy (g) | Optical coherence tomography, tissue characterization [11] [10] |
| Reflection | Fresnel Equations | Reflectance, Refractive Index | Surface topography imaging, ellipsometry-based biosensing [11] |
Experimental Methodologies and Protocols
This section provides detailed methodologies for measuring and characterizing the fundamental light-matter interactions discussed previously, with a focus on techniques relevant to bio-optics research.
Protocol 1: Measuring Absorption Spectra of Biological Chromophores
Objective: To determine the absorption characteristics and concentration of biological chromophores (e.g., hemoglobin, NADH, melanin) in solution or tissue samples.
Materials Required:
- UV-Vis spectrophotometer with cuvette holder or integrating sphere for turbid samples
- Quartz cuvettes (for UV transmission)
- Phosphate-buffered saline (PBS) or appropriate buffer
- Standard solutions of target chromophores for calibration
- Biological samples (tissue homogenates, cell lysates, or purified chromophore solutions)
Procedure:
- Sample Preparation:
- For solution measurements, dilute samples in appropriate buffer to achieve optical densities between 0.1 and 1.0 for optimal measurement accuracy.
- For turbid samples (tissue sections, cell suspensions), use an integrating sphere attachment to account for both absorption and scattering contributions.
Instrument Calibration:
- Perform baseline correction with blank buffer solution.
- Measure absorption spectra of standard solutions to create a calibration curve.
Data Acquisition:
- Set spectrophotometer to scan from 250 nm to 800 nm or the relevant spectral range.
- Record absorption spectra of all samples, averaging multiple scans to improve signal-to-noise ratio.
Data Analysis:
- Apply Beer-Lambert law: A = ε × c × l, where A is absorbance, ε is molar absorptivity, c is concentration, and l is path length.
- For turbid samples, use modified Beer-Lambert law incorporating scattering correction factors.
Expected Outcomes: Absorption spectra showing characteristic peaks for target chromophores, enabling quantification of concentration and purity assessment.
Protocol 2: Time-Resolved Fluorescence Spectroscopy
Objective: To measure fluorescence lifetimes and characterize molecular environments and interactions in biological systems.
Materials Required:
- Time-correlated single photon counting (TCSPC) system or streak camera system
- Pulsed laser source (wavelength matched to fluorophore excitation)
- Fluorophore-labeled biomolecules (proteins, nucleic acids)
- Reference fluorophore with known lifetime for instrument response calibration
- Temperature-controlled sample chamber
Procedure:
- System Setup:
- Align excitation and emission pathways, ensuring proper collection optics and filters.
- Measure instrument response function using a reference scatterer or fluorophore with known lifetime.
Sample Preparation:
- Prepare fluorophore-labeled biomolecules in appropriate physiological buffer.
- Degas samples if necessary to reduce oxygen quenching effects.
Data Acquisition:
- Set appropriate laser power and acquisition time to avoid photobleaching and pile-up effects.
- Collect fluorescence decay curves at multiple emission wavelengths if performing lifetime-resolved measurements.
Data Analysis:
- Fit decay curves to single or multi-exponential models: I(t) = Σαᵢexp(-t/τᵢ), where τᵢ are lifetime components and αᵢ are their amplitudes.
- Calculate average lifetime: <τ> = Σαᵢτᵢ² / Σαᵢτᵢ
Expected Outcomes: Fluorescence lifetime values that provide information about local environment, molecular interactions, and conformational changes of biomolecules.
Protocol 3: Quantifying Light Scattering in Biological Tissues
Objective: To characterize scattering properties of biological tissues for optical tomography and spectroscopy applications.
Materials Required:
- Integrating sphere spectrophotometer
- Tissue samples (fresh or preserved) of controlled thickness
- Index-matching fluids
- Thin-sectioning microtome
- Calibrated reflectance standards
Procedure:
- Sample Preparation:
- Prepare tissue sections of known thickness (typically 100-500 μm) using a microtome.
- Mount samples between glass slides with index-matching fluid if necessary.
System Calibration:
- Calibrate integrating sphere using reflectance standards with known reflectance values.
- Measure baseline with no sample.
Data Acquisition:
- Measure total transmission (T), collimated transmission (T꜀), and reflectance (R) of tissue samples.
- Perform measurements at multiple wavelengths relevant to application (typically 400-1000 nm).
Data Analysis:
- Use inverse adding-doubling method to extract absorption (μₐ) and reduced scattering (μₛ') coefficients from T and R measurements.
- Calculate anisotropy factor (g) from collimated and total transmission measurements.
Expected Outcomes: Wavelength-dependent absorption and scattering coefficients that inform light transport models for tissue optics applications.
Diagram 1: Tissue scattering measurement workflow
Research Reagent Solutions and Essential Materials
Successful investigation of light-matter interactions in biological systems requires specific reagents and materials. The following table details key components of the "Researcher's Toolkit" for bio-optics experiments.
Table 2: Essential Research Reagents and Materials for Bio-optics Investigations
| Category | Specific Examples | Function/Application | Key Characteristics |
|---|---|---|---|
| Biological Chromophores | Hemoglobin, NADH, FAD, Melanin | Endogenous absorbers; natural contrast agents in label-free imaging [10] | Characteristic absorption spectra; concentration-dependent contrast |
| Exogenous Fluorophores | GFP, RFP; Alexa Fluor dyes; ICG | Fluorescent labeling for molecular tracking and environment sensing [11] | High quantum yield; photostability; specific excitation/emission profiles |
| Quantum Dots | CdSe/ZnS core-shell nanoparticles | Photostable fluorescent probes for long-term imaging and multiplexing | Size-tunable emission; broad absorption; narrow emission spectra |
| Scattering Phantoms | Polystyrene microspheres; TiO₂ suspensions | Calibration standards for optical instruments; tissue simulating phantoms | Well-defined size distribution; known scattering properties |
| Nonlinear Crystals | BBO, KTP crystals | Frequency conversion for multiphoton microscopy (SHG, THG) [10] | High nonlinear coefficients; appropriate phase-matching properties |
| Optical Clearing Agents | FocusClear, ScaleS | Reduce scattering in tissue for improved imaging depth | Refractive index matching; tissue compatibility |
| Biosensor Constructs | FRET-based molecular tension sensors; GECIs | Reporting specific molecular activities or ionic concentrations | Specific targeting; dynamic response to biochemical changes |
Advanced Technical Considerations in Bio-optics
Modern biophotonics research extends beyond basic interactions to leverage advanced phenomena and computational approaches for enhanced biological insight.
Linear vs. Nonlinear Interactions
Recent advances in the development of compact and easy-to-operate high-intensity ultrashort laser sources have enabled the exploitation of nonlinear optical phenomena for biomedical imaging, resulting in significant improvements in penetration depth, optical resolution, and acquisition speed [10]. In linear interactions, the response of the material is proportional to the incident light field, whereas nonlinear interactions depend on higher powers of the electric field strength and enable phenomena such as multiphoton absorption, second harmonic generation (SHG), and third harmonic generation (THG) [10]. Multi-photon imaging using near IR (NIR) femtosecond lasers provides high penetration depths, allowing the study of biological tissue with high spatial resolution and good contrast not only on the surface but also deep within the tissue [10].
Molecular Specificity and Contrast Mechanisms
The contrast mechanisms underlying biophotonic methods can be highly molecule-specific in the case of IR absorption and Raman scattering [10]. These techniques can visualize native electronic chromophores such as hemoglobin, NADP(H), flavin, elastin, or cytochrome by absorption (hyperspectral imaging or photoacoustic imaging) or emission (autofluorescence or fluorescence label imaging) [10]. Specific structural proteins (e.g., collagen) can be visualized by SHG, while changes in refractive index are detected by optical coherence tomography (OCT) and phase boundaries by THG [10]. Molecular contrast is highest when spectroscopic data are acquired, as in hyperspectral imaging, fluorescence lifetime imaging (FLIM), spontaneous or coherent Raman spectroscopy, or IR absorption spectroscopy [10].
Diagram 2: Electronic transitions in light-matter interactions
The Role of Artificial Intelligence in Biophotonics
In the recent decade, machine learning (ML) and artificial intelligence (AI) have played an increasingly transformative role in biophotonics by enhancing data analysis, interpretation, and optimization of complex imaging and sensing [4]. AI approaches are being applied to improve image reconstruction, interpret complex biological patterns, and even optimize optical design itself [4]. These computational methods are particularly valuable for extracting meaningful biological information from the complex datasets generated by techniques such as hyperspectral imaging, OCT, and Raman spectroscopy, where traditional analysis methods may be insufficient for fully leveraging the rich information content.
The fundamental light-matter interactions of absorption, emission, scattering, and reflection form the foundation upon which modern bio-optics and biophotonics are built. Understanding these core principles at both quantitative and mechanistic levels enables researchers to design increasingly sophisticated instruments for biological discovery and medical application. As the field continues to evolve through integration with artificial intelligence, novel materials, and quantum approaches, these basic interactions will remain central to extracting meaningful biological information from light. The methodologies and resources detailed in this technical guide provide a foundation for researchers to investigate and apply these principles in their own work, contributing to the advancement of bio-optics design and application research with potential impacts across basic science, clinical diagnostics, and therapeutic development.
Bio-optics and its closely related field, biophotonics, represent the convergence of light-based technologies with biological and medical sciences. This discipline utilizes light to image, analyze, and manipulate biological materials, driving advancements in research, diagnostics, and therapeutics [10]. The market for these technologies is experiencing significant global growth, fueled by the increasing demand for non-invasive diagnostic tools, minimally invasive surgical procedures, and advanced research applications in drug discovery and life sciences [12] [13] [14]. This whitepaper provides a comprehensive analysis of the market landscape, detailing projected growth rates, key drivers, dominant sectors, and the essential methodologies and tools that underpin this dynamic field. Aimed at researchers, scientists, and drug development professionals, it frames this commercial and technological landscape within the broader context of bio-optics design and application research.
The global market for bio-optics and biophotonics is on a strong growth trajectory, though reported valuations vary depending on the specific definition and scope of the market segments. The table below summarizes key quantitative projections from recent analyses.
Table 1: Global Market Size and Growth Projections for Bio-optics and Biophotonics
| Market Segment | Base Year & Value (USD) | Projected Year & Value (USD) | CAGR | Source & Notes |
|---|---|---|---|---|
| Bio-optics | 2024: 2.03 Billion [12] | 2032: 3.31 Billion [12] | 6.3% (2025-2032) [12] | "Bio Optics Market" report [12] |
| Bio-optics | 2022: 1.2 Billion [15] | 2031: 2.1 Billion [15] | 6.0% (2023-2031) [15] | "Bio-optics Market" report [15] |
| Biophotonics | 2024: 76.1 Billion [13] | 2034: 220.1 Billion [13] | 11.3% (2025-2034) [13] | "Biophotonics Market" report [13] |
| Biophotonics | 2024: 62.6 Billion [14] | 2030: 113.1 Billion [14] | 10.6% (2025-2030) [14] | BCC Research report [14] |
The disparity in market values between "bio-optics" and "biophotonics" reports suggests that the latter may encompass a broader range of light-based technologies in life sciences. Despite different baselines, both sectors demonstrate robust growth, with CAGRs consistently exceeding 6% and reaching over 11% for the biophotonics segment [12] [13] [14]. Regionally, North America, particularly the United States, holds the dominant market share, attributed to its advanced healthcare infrastructure, significant R&D investments, and the presence of leading industry players [12] [13] [14]. Europe is also a major market, with Germany and the UK being key contributors, while the Asia-Pacific region, led by China and India, is expected to witness the fastest growth [13] [15].
Key Market Growth Drivers
The expansion of the bio-optics market is propelled by several interconnected factors:
- Demand for Non-Invasive Diagnostics and Minimally Invasive Surgeries: There is a strong clinical and patient preference for procedures that reduce discomfort, risk, and recovery time. Bio-optics technologies, such as Optical Coherence Tomography (OCT) and advanced endoscopy, are crucial for guiding and monitoring these procedures, thereby boosting market growth [12] [15] [14].
- Rising Prevalence of Chronic Diseases and Aging Populations: The increasing global burden of chronic conditions such as cancer, cardiovascular diseases, and diabetes is driving the need for advanced diagnostic and therapeutic tools. Furthermore, the aging global population, which is more susceptible to these conditions, creates a sustained demand for these technologies [13] [15].
- Technological Advancements and Convergence: Continuous innovation in optical technologies, including the development of novel fluorescent probes, super-resolution microscopy, and portable devices, is expanding the capabilities and applications of bio-optics. The integration of Artificial Intelligence (AI) and machine learning for image analysis and data interpretation is enabling quicker, more reliable diagnoses and is a key trend shaping the market [10] [13] [15].
- Expansion into Point-of-Care and Personalized Medicine: There is a growing emphasis on decentralizing healthcare and bringing diagnostics closer to patients. Portable and handheld bio-optics devices facilitate point-of-care testing, while the capabilities of these technologies for molecular-level analysis align perfectly with the trend towards personalized and precision medicine [12] [13] [14].
Dominant Market Sectors and Applications
The bio-optics market can be segmented by technology, device, and application, with certain segments demonstrating clear dominance.
By Technology and Device
Table 2: Dominant Segments by Technology and Device
| Segment Category | Dominant Segment | Key Applications and Notes |
|---|---|---|
| Technology | Raman Spectroscopy [12] | Provides detailed molecular information for studying cell and tissue composition, identifying disease biomarkers, and monitoring drug interactions without extensive sample preparation. |
| Device | Optical Coherence Tomography (OCT) [12] | A non-invasive imaging technique that captures high-resolution, cross-sectional images of biological tissues in real-time. It is well-established in ophthalmology and expanding into cardiology, dermatology, and oncology. |
| Imaging Modality | See-Through Imaging [13] [7] | This segment, which includes techniques like OCT, is growing at the highest CAGR. It provides non-invasive, high-resolution visualization of internal anatomical structures, crucial for early disease detection and surgical guidance. |
By Application
The most prominent application sector for bio-optics is medical diagnostics, with cancer diagnostics representing the largest sub-segment [12] [16] [14]. Bio-optics technologies are indispensable in the fight against cancer, enabling early detection, accurate staging, and personalized treatment planning. Techniques like OCT, fluorescence imaging, and Raman spectroscopy are used to detect and characterize cancer cells, assess tumor margins, and monitor treatment responses [12]. The detection of infectious diseases is another critical application area, where optical biosensors and advanced imaging offer rapid and sensitive pathogen detection, a need highlighted by the COVID-19 pandemic [16] [7].
Core Experimental Methodologies in Bio-optics
For researchers designing and applying bio-optics tools, understanding core methodologies is essential. Below are detailed protocols for three key techniques.
Optical Coherence Tomography (OCT) for Tissue Imaging
OCT is a label-free technique that uses interferometry to generate high-resolution, cross-sectional images of scattering biological tissues [10].
Experimental Protocol:
- Sample Preparation: Tissue samples (e.g., retinal, arterial, or skin) can be imaged in vivo or ex vivo. For in vivo human imaging, such as in ophthalmology, no physical preparation is needed. For ex vivo studies, tissues are typically fixed and stored in appropriate buffers to preserve morphology.
- System Setup: A broadband low-coherence light source (e.g., a super-luminescent diode) is split into a reference arm and a sample arm via a beamsplitter.
- Data Acquisition: Light backscattered from the sample and reflected from the reference mirror recombines at the detector, creating an interferometric signal. This signal is digitized as a function of optical wavelength.
- Image Processing: The digitized interferogram is processed via a Fourier transform to reconstruct the depth-resolved reflectivity profile (A-scan). Multiple A-scans are acquired by scanning the beam across the sample to build a 2D cross-sectional image (B-scan).
- Analysis: The resulting B-scan image reveals tissue microstructure, allowing for the identification of layers, abnormalities, or specific morphological features based on differences in optical scattering.
Raman Spectroscopy for Molecular Analysis
Raman spectroscopy probes the vibrational state of molecules, providing a highly specific chemical fingerprint of a sample based on inelastic scattering of light [12] [10].
Experimental Protocol:
- Sample Preparation: Biological samples (cells, tissues, biofluids) can be analyzed with minimal preparation, often requiring no labels or stains. Cells may be cultured on suitable substrates, and tissues are typically sectioned.
- System Setup: A monochromatic laser source is focused onto the sample through a microscope objective. A spectrometer equipped with a sensitive CCD detector is used to collect the scattered light.
- Data Acquisition: The Raman scattered light is collected and its spectrum is dispersed. The intrinsic weakness of the Raman signal is a key challenge. This can be overcome by using nonlinear coherent Raman scattering (CRS) phenomena like CARS or SRS, which enhance the signal [10].
- Spectral Processing: Acquired spectra are processed to remove background fluorescence and noise, and may be normalized for comparative analysis.
- Analysis: The resulting spectrum shows peaks corresponding to specific molecular vibrations. Multivariate statistical analysis or machine learning algorithms can be applied to identify biochemical differences between sample groups (e.g., healthy vs. diseased tissue) [13].
Fluorescence Imaging for Cellular and Molecular Visualization
This technique uses the property of fluorescence to visualize the spatial distribution of specific molecules or ions within cells and tissues [12] [10].
Experimental Protocol:
- Sample Preparation and Labeling:
- Option A (Labeled): Introduce exogenous fluorescent probes, such as organic dyes or antibodies conjugated to fluorophores, that target specific structures (e.g., actin, nuclei) or biomarkers.
- Option B (Label-free): Utilize endogenous fluorophores (e.g., NAD(P)H, flavins) for autofluorescence imaging [10].
- Option C (Genetically Encoded): Transfert cells with genes encoding fluorescent proteins (e.g., GFP, RFP) fused to proteins of interest.
- System Setup: An epifluorescence or confocal microscope is used, equipped with a light source for excitation (e.g., laser, LED), a set of optical filters (excitation, emission, dichroic), and a high-sensitivity detector.
- Data Acquisition: The sample is illuminated with light at the excitation wavelength. The emitted fluorescence light, at a longer wavelength, is collected through the objective and filtered to block excitation light before being detected.
- Image Processing: Background subtraction, flat-field correction, and deconvolution algorithms may be applied to improve image quality and resolution.
- Analysis: Images are analyzed to determine the localization, concentration, and dynamics of the target molecules. Techniques like FRET (Förster Resonance Energy Transfer) can be used to monitor molecular interactions.
Diagram 1: Fluorescence imaging workflow.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful bio-optics experiments rely on a suite of specialized reagents and materials. The following table details key components of the researcher's toolkit.
Table 3: Key Research Reagent Solutions in Bio-optics
| Item | Function/Application | Specific Examples & Notes |
|---|---|---|
| Fluorescent Probes & Dyes | To label and visualize specific biological structures, ions, or molecules. | Organic dyes (e.g., Cyanine, Alexa Fluor), cell-permeant dyes for organelles, ion indicators (e.g., Ca²⁺ dyes). |
| Genetically Encoded Fluorescent Proteins | To tag and track proteins in live cells via genetic engineering. | Green Fluorescent Protein (GFP), Red Fluorescent Protein (RFP) [12]. Enable long-term live-cell imaging. |
| Antibodies (Conjugated) | For highly specific immunolabeling of target antigens in fixed cells/tissues. | Antibodies conjugated to fluorophores for immunofluorescence microscopy. |
| Nanoparticles and Quantum Dots | Act as contrast agents or sensors, often offering superior brightness and photostability. | Metallic nanoparticles, quantum dots [13]. Used in biosensing and super-resolution imaging. |
| Biosensors (Optical) | Detect the presence or concentration of a biological analyte by converting a biological response into an optical signal. | Utilize principles like surface plasmon resonance (SPR) or FRET for label-free detection of biomolecules [7]. |
| Live Cell Imaging Media | To maintain cell viability and function during prolonged imaging on a microscope stage. | Phenol-red free formulations (to reduce background), with buffers to maintain pH. |
Diagram 2: Biophotonic biosensor operating logic.
The bio-optics and biophotonics market is positioned for sustained, robust growth, driven by relentless technological innovation and critical unmet needs in healthcare and life sciences. Key sectors such as cancer diagnostics, powered by technologies like OCT and Raman spectroscopy, will continue to dominate and evolve. For researchers and drug development professionals, mastering the core experimental protocols—from foundational fluorescence imaging to advanced label-free techniques—is essential for leveraging the full potential of this field. The ongoing integration of AI, the development of novel reagents and nanomaterials, and the push toward point-of-care applications will undoubtedly shape the next generation of bio-optics design and research, solidifying its role as a cornerstone of modern precision medicine.
Biophotonics, the interdisciplinary fusion of light-based technologies with biology and medicine, has emerged as a transformative force in 21st-century science and healthcare [10]. This field, derived from the Greek words "bios" (life) and "phos" (light), focuses on understanding how light interacts with biological matter to advance fundamental research, diagnostics, and therapeutic interventions [10]. The core technology areas of bioimaging, biosensing, and photonic therapies represent the foundational pillars of biophotonics, enabling unprecedented capabilities for analyzing and manipulating biological systems from the molecular to organism level. These technologies leverage key advantages of light, including non-contact measurement, rapid information acquisition, exceptional sensitivity down to single-molecule detection, and high temporal resolution for observing dynamic biological processes [10].
The integration of these core areas is driving innovation across numerous domains, from pharmaceutical development and clinical medicine to environmental monitoring and agriculture [10]. This technical guide provides an in-depth examination of each core technology area, focusing on their operating principles, current applications, methodological protocols, and future directions within the broader context of bio-optics design and application research. As the field continues to evolve through convergence with artificial intelligence, novel materials, and quantum technologies, bioimaging, biosensing, and photonic therapies are poised to become increasingly central to precision medicine and the One Health approach [10].
Bioimaging Technologies and Methodologies
Fundamental Principles and Modalities
Bioimaging encompasses a diverse suite of photonic technologies that enable the characterization of biological specimens across multiple spatial scales, from nanoscopic investigation of intracellular interactions to macroscopic imaging of tissues and organ systems [10]. These techniques are fundamentally based on the interaction of light with biological matter through processes of absorption, emission, scattering, and reflection, which elucidate morphological and molecular details across resolution scales [10]. The most representative label-free biophotonic diagnostic methods include hyperspectral imaging (HSI), fluorescence lifetime imaging (FLIM), second and third harmonic generation (SHG, THG), optical coherence tomography (OCT), diffuse remission spectroscopy (DRS), photoacoustic imaging (PAI), and vibrational microspectroscopy (IR absorption and Raman scattering) [10].
A critical distinction in bioimaging technologies lies between linear and nonlinear light-matter interaction phenomena. Recent advances in compact high-intensity ultrashort laser sources have enabled the exploitation of nonlinear optical phenomena for biomedical imaging, resulting in significant improvements in penetration depth, optical resolution, and acquisition speed [10]. Multi-photon absorption, for instance, provides precise localization of fluorescence or harmonic generation signals since such nonlinear processes occur only in extremely small volumes, offering superior imaging capabilities deep within biological tissues [10].
Table 1: Major Bioimaging Technologies and Their Characteristics
| Imaging Technology | Spatial Resolution | Penetration Depth | Key Applications | Contrast Mechanism |
|---|---|---|---|---|
| Optical Coherence Tomography (OCT) | 1-15 μm | 1-2 mm | Ophthalmology, tissue morphology | Refractive index changes |
| Multi-Photon Microscopy | 0.2-0.8 μm | 0.5-1 mm | Deep tissue cellular imaging | Nonlinear excitation |
| Photoacoustic Imaging (PAI) | 20-200 μm | 2-5 cm | Vascular imaging, oncology | Light absorption → ultrasound |
| Fluorescence Lifetime Imaging (FLIM) | 0.3-1 μm | Single cell to tissue | Metabolic monitoring, molecular environment | Fluorescence decay rates |
| Coherent Raman Scattering (CRS) | 0.3-0.5 μm | 0.2-0.5 mm | Label-free molecular imaging | Molecular vibrations |
Experimental Protocol: Multi-Modal Imaging of Tissue Structures
Objective: To characterize tissue morphology and molecular composition using a combined OCT and SHG imaging approach for distinguishing pathological from healthy tissues.
Materials and Equipment:
- Spectral-domain OCT system with near-infrared light source (center wavelength ~1300 nm)
- Femtosecond laser system tuned for SHG imaging (typical wavelength ~800 nm)
- High-numerical aperture objectives suitable for both OCT and nonlinear microscopy
- Precision motorized sample stage for co-registered imaging
- Biological specimens (tissue sections or in vivo preparations)
- Data acquisition and processing workstation with specialized software
Procedure:
- System Calibration: Align OCT and SHG optical paths to ensure precise spatial registration between modalities. Adjust laser power levels to ensure biological safety thresholds are maintained, especially for in vivo applications.
Sample Preparation: For ex vivo imaging, prepare tissue sections of appropriate thickness (typically 100-500 μm) and mount using compatible media. For in vivo imaging, properly position the subject and stabilize the region of interest.
OCT Data Acquisition: Acquire volumetric OCT datasets by scanning the reference arm while recording interferometric signals from the sample. Typical acquisition parameters: 512 × 512 A-scans per volume, with scan depth adjusted to encompass the full sample thickness.
SHG Data Acquisition: Following OCT acquisition, switch to SHG imaging mode without moving the sample. Using the femtosecond laser, acquire SHG images by detecting emitted light at exactly half the excitation wavelength (400 nm for 800 nm excitation). Collagen-rich structures will generate strong SHG signals.
Multi-Modal Data Registration: Use fiduciary markers or intrinsic tissue features to precisely align OCT and SHG datasets. Apply appropriate transformation matrices to ensure pixel-level correspondence between modalities.
Image Analysis and Interpretation:
- Segment OCT images to identify tissue layers and structural boundaries
- Quantify SHG signal intensity and distribution to assess collagen density and organization
- Correlate structural features from OCT with molecular information from SHG
- Generate composite visualization that overlays SHG data on OCT structural maps
Troubleshooting Notes:
- Poor SHG signal may indicate suboptimal laser alignment or insufficient collagen content
- Motion artifacts in in vivo OCT can be mitigated by faster scanning or respiratory gating
- Incomplete registration between modalities may require additional control points or landmark-based alignment
Multi-Modal Bioimaging Workflow
Research Reagent Solutions for Bioimaging
Table 2: Essential Research Reagents for Advanced Bioimaging
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Genetically Encoded Fluorescent Proteins (e.g., GFP, RFP) | Labeling specific cellular structures or proteins | Live-cell tracking, protein localization studies |
| Synthetic Fluorophores (e.g., Alexa Fluor, Cy dyes) | High-intensity labeling with broad spectral range | Multi-color imaging, super-resolution microscopy |
| Quantum Dots | Photostable nanoparticles for long-term imaging | Single-particle tracking, multiplexed detection |
| Environment-Sensitive Dyes | Report on local physicochemical conditions | pH sensing, membrane potential measurements |
| Tissue Clearing Reagents | Render tissues transparent for deep imaging | Light-sheet microscopy, whole-organ imaging |
| Nonlinear Optical Crystals | Frequency conversion for harmonic generation | Calibration standards for SHG/THG microscopy |
Biosensing Systems and Applications
Biosensor Fundamentals and Classification
Biosensors are analytical devices that combine a biological sensing element with a transducer to detect specific analytes, ranging from small molecules to macromolecular complexes [17]. These systems function by integrating a sensor module that detects intracellular or environmental signals with an actuator module that drives a measurable or functional response [17]. The global biosensors market is projected to grow from USD 34.51 billion in 2025 to USD 54.37 billion by 2030, at a compound annual growth rate (CAGR) of 9.5%, reflecting their expanding applications across healthcare, environmental monitoring, and industrial biotechnology [18].
Biosensors are characterized by several key performance metrics: (1) dynamic range, representing the span between minimal and maximal detectable signals; (2) operating range, defining the concentration window for optimal performance; (3) response time, indicating the speed of reaction to analyte changes; and (4) signal-to-noise ratio, determining the clarity and reliability of the output signal [17]. These parameters collectively determine the suitability of biosensors for specific applications, from real-time metabolic monitoring to high-throughput screening in industrial biotechnology.
Biosensors are broadly categorized into wearable and non-wearable formats, with wearable biosensors emerging as the most commercially successful segment [18]. These include sensor patches and embedded devices integrated into larger medical or wearable hardware systems such as smartwatches, fitness bands, ECG patches, and implantable monitors [18]. Wearable biosensors are particularly valuable for continuous, multi-parametric health monitoring and chronic disease management, with form factors ranging from wristwear to bodywear including adhesive patches, smart garments, and headbands [18].
Table 3: Biosensing Technologies by Detection Mechanism
| Biosensor Category | Sensing Principle | Response Characteristics | Advantages | Example Applications |
|---|---|---|---|---|
| Electrochemical | Measures electrical changes from biochemical reactions | High sensitivity, moderate response time | Low cost, portability, ease of miniaturization | Glucose monitoring, pathogen detection |
| Optical | Detects changes in light properties | High sensitivity, multiplexing capability | Superior sensitivity, non-invasive detection | Oncology, infectious disease detection |
| Piezoelectric | Measures mass/pressure changes on crystal surface | Label-free detection, high mass sensitivity | Detects minute physical interactions | Environmental sensing, gas detection |
| Thermal | Detects temperature changes from reactions | Specialized response profiles | Specific to thermal signatures | Specialized lab analytics |
| Nanomechanical | Uses cantilever sensors at nanoscale | Extreme sensitivity to molecular interactions | Single-molecule detection potential | Early disease detection, personalized medicine |
Experimental Protocol: Developing Transcription Factor-Based Biosensors
Objective: To engineer a transcription factor (TF)-based whole-cell biosensor for quantitative monitoring of bioactive compounds in microbial systems.
Materials and Equipment:
- Microbial chassis (e.g., E. coli, Pseudomonas putida)
- Plasmid vectors with modular cloning sites
- Target transcription factor (e.g., TtgR from P. putida)
- Reporter gene (e.g., egfp, mCherry)
- Microplate reader with fluorescence detection capability
- Flow cytometer for single-cell analysis
- Target analyte compounds for testing
- Cell culture equipment and media
Procedure:
- Genetic Construct Design:
- Clone the transcription factor gene (e.g., ttgR) under a constitutive promoter
- Place the reporter gene (egfp) under control of the TF-regulated promoter (e.g., PttgABC)
- Include appropriate selection markers and origins of replication
Biosensor Assembly and Transformation:
- Assemble genetic constructs using standard molecular biology techniques (e.g., Gibson assembly, Golden Gate cloning)
- Transform constructs into appropriate microbial host
- Verify correct assembly by colony PCR and sequencing
Biosensor Characterization:
- Culture biosensor strains in appropriate media to mid-log phase
- Expose to a concentration gradient of target analyte (e.g., 0 μM to 1000 μM)
- Incubate for predetermined time (typically 4-8 hours)
- Measure fluorescence output using plate reader or flow cytometer
- Normalize fluorescence to cell density (OD600)
Dose-Response Analysis:
- Plot fluorescence intensity against analyte concentration
- Fit data to appropriate model (e.g., Hill equation) to determine dynamic range, sensitivity, and EC50
- Calculate response threshold (lowest detectable concentration) and saturation point
Specificity and Cross-Reactivity Testing:
- Expose biosensor to structural analogs of target compound
- Assess response to identify potential cross-reactivities
- For non-responders, consider engineering TF binding pocket for improved specificity
Performance Optimization:
- Fine-tune expression levels by modifying promoter strength, ribosome binding sites, or plasmid copy number
- Address trade-offs between dynamic range and response threshold as needed
- Implement directed evolution strategies if necessary to enhance sensitivity or specificity
Applications in Metabolic Engineering:
- Dynamic regulation of synthetic metabolic pathways
- High-throughput screening of strain libraries
- Real-time monitoring of metabolite production in bioreactors
Transcription Factor Biosensor Mechanism
Research Reagent Solutions for Biosensing
Table 4: Essential Research Reagents for Biosensor Development
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Transcription Factors | Natural sensing elements for specific metabolites | Metabolite biosensors, regulatory circuits |
| Riboswitches | RNA-based sensing elements | Real-time metabolic regulation, compound detection |
| Fluorescent Reporter Proteins | Generate measurable optical signals | Quantitative biosensor output measurement |
| Toehold Switches | Programmable RNA sensors | Nucleic acid detection, logic-gated control |
| Two-Component Systems | Signal transduction from extracellular cues | Environmental sensing, intercellular communication |
| Enzyme-Based Sensors | Catalytic detection of specific substrates | Specific molecular detection with signal amplification |
Photonic Therapies and Treatment Modalities
Principles of Light-Based Therapies
Photonic therapies encompass a range of light-based treatment modalities that leverage the interactions between light and biological tissues for therapeutic purposes [10]. These approaches include laser surgery, photodynamic therapy, low-level light therapy, and photobiomodulation, each with distinct mechanisms of action and clinical applications [10]. The fundamental principle underlying photonic therapies is the selective absorption of light by specific tissue components or photosensitizing agents, leading to localized therapeutic effects while minimizing damage to surrounding healthy tissues.
Lasers and other advanced light sources enable highly precise and minimally invasive surgical interventions, with applications ranging from ophthalmology and dermatology to oncology and neurosurgery [10]. The efficacy of these treatments is often monitored in real-time using complementary bioimaging and biosensing modalities, creating integrated therapeutic platforms that combine diagnosis and treatment in a single workflow [10]. Recent advances in photonic therapies include the development of targeted approaches that respond to specific molecular biomarkers, enabling personalized treatment strategies with improved therapeutic outcomes and reduced side effects.
Experimental Protocol: Fluorescence-Guided Surgery with Nanobodies
Objective: To implement fluorescence-guided surgery using targeted nanobodies and fluorescence lifetime imaging (FLIM) for enhanced tumor specificity and reduced background signal.
Materials and Equipment:
- Targeted nanobody-fluorophore conjugates (e.g., anti-EGFR nanobody with IRDye 800CW)
- Surgical microscope with fluorescence imaging capability
- Fluorescence lifetime imaging (FLIM) system
- Animal model with appropriate tumor xenografts
- Anesthesia equipment and monitoring systems
- Image processing software with FLIM analysis capabilities
Procedure:
- Probe Preparation and Characterization:
- Conjugate selected nanobodies with appropriate fluorophores
- Purify conjugates using size exclusion chromatography
- Characterize labeling efficiency and binding specificity using flow cytometry or ELISA
- Determine optimal imaging time window through pharmacokinetic studies
Preoperative Planning:
- Establish baseline imaging of surgical area using white light and fluorescence
- Identify potential areas of concern based on preoperative imaging
- Determine surgical approach that maximizes visualization of fluorescent signals
Administration of Targeted Agent:
- Administer nanobody-fluorophore conjugate via appropriate route (typically intravenous)
- Allow sufficient time for agent distribution and target binding (typically 2-48 hours depending on agent)
- Clear unbound agent from circulation to reduce background signal
Intraoperative Imaging and FLIM:
- Perform surgery under standard white light illumination
- Switch to fluorescence mode to identify target-positive tissues
- Acquire FLIM data to distinguish specific binding from non-specific signal based on fluorescence lifetime differences
- Use real-time image overlay to guide surgical margins and identify potential metastatic deposits
Tissue Validation:
- Collect excised tissues for histopathological analysis
- Correlate fluorescence signals with histological findings
- Assess margin status using both conventional pathology and fluorescence imaging
Data Analysis and Interpretation:
- Quantify fluorescence intensity in target versus non-target tissues
- Analyze fluorescence lifetime distributions to differentiate specific from non-specific binding
- Calculate target-to-background ratios for quantitative assessment of imaging performance
Advantages of Nanobody-Based Approaches:
- Rapid pharmacokinetics leading to higher target-to-background ratios
- Superior tissue penetration compared to full antibodies
- Potential for same-day imaging and surgery
- Reduced immunogenicity
Fluorescence-Guided Surgical Workflow
Research Reagent Solutions for Photonic Therapies
Table 5: Essential Research Reagents for Photonic Therapies
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Photosensitizers | Light-activated compounds for therapy | Photodynamic therapy, antimicrobial applications |
| Targeted Nanobodies | Small antigen-binding domains for precision targeting | Fluorescence-guided surgery, molecular imaging |
| Biocompatible Fluorophores | Light-emitting molecules for visualization | Surgical guidance, treatment monitoring |
| Light-Activated Ion Channels | Optogenetic control of cellular activity | Neuromodulation, cardiac pacing |
| Thermoplastic Polymers | Materials for light-based fabrication | Medical device manufacturing, surgical guides |
| Light-Activated Drugs | Therapeutic compounds with photolabile protecting groups | Spatiotemporally controlled drug release |
Integrated Systems and Future Directions
Convergence of Bioimaging, Biosensing, and Therapies
The most significant advances in bio-optics are emerging from integrated systems that combine bioimaging, biosensing, and photonic therapies into unified platforms [10]. These integrated approaches enable closed-loop systems where sensing informs treatment, and imaging guides intervention, creating responsive therapeutic systems with unprecedented precision. For example, intraoperative imaging systems can now combine multiple modalities like OCT, fluorescence imaging, and photoacoustic imaging to provide comprehensive tissue characterization during surgical procedures, while integrated biosensors monitor physiological parameters in real-time to guide therapeutic decisions [10].
The convergence of these technologies is particularly evident in emerging applications such as theranostics (combined therapy and diagnostics), where a single agent serves both diagnostic and therapeutic functions [10]. Photoactivatable agents, for instance, can be visualized using fluorescence imaging to confirm target engagement before light activation initiates therapeutic action. This approach minimizes off-target effects and enables personalized treatment dosing based on real-time assessment of drug distribution and target expression [10].
Enabling Technologies and Future Outlook
Several enabling technologies are driving the future integration of bioimaging, biosensing, and photonic therapies. Artificial intelligence and machine learning are playing an increasingly transformative role by enhancing data analysis, interpretation, and optimization of complex imaging and sensing data [4] [10]. These computational approaches enable real-time decision support, automated image interpretation, and optimization of optical systems for specific applications [4].
Novel materials, including nanomaterials, metamaterials, and stimuli-responsive polymers, are expanding the capabilities of bio-optical systems through enhanced contrast, improved targeting, and responsive functionality [10]. Quantum technologies, including quantum sensing and imaging, promise unprecedented sensitivity for detecting biological signals at the fundamental physical limits [10]. These advances are complemented by progress in miniaturization and wearable technologies, making sophisticated bio-optical systems increasingly accessible for point-of-care applications and continuous health monitoring [18].
The future of bio-optics will see increased emphasis on multimodal integration, where complementary technologies are combined to overcome individual limitations and provide more comprehensive biological information [10]. Clinical translation will be accelerated through improved standardization, validation protocols, and regulatory frameworks that ensure the safety and efficacy of these advanced bio-optical systems [10]. As these trends converge, bioimaging, biosensing, and photonic therapies will become increasingly central to precision medicine, enabling personalized approaches to diagnosis, monitoring, and treatment across a wide spectrum of diseases and health conditions.
Core Technologies and Their Transformative Applications in Biomedicine
Optical imaging modalities have revolutionized biomedical research and diagnostic medicine by enabling non-invasive, high-resolution visualization of biological tissues. Among these, Optical Coherence Tomography (OCT) and Multiphoton Microscopy (MPM) represent two powerful technologies that operate on fundamentally different physical principles while offering complementary capabilities. OCT leverages low-coherence interferometry to provide cross-sectional structural information, while MPM utilizes nonlinear optical processes to achieve high-resolution molecular imaging. The integration of these modalities addresses the critical trade-offs between imaging depth, resolution, and molecular specificity that have historically limited individual optical techniques. This technical guide examines the core principles, current advancements, and synergistic applications of OCT and MPM, with particular emphasis on their growing importance in preclinical research and drug development workflows where comprehensive structural and functional assessment is required.
Fundamental Principles and Technical Specifications
Optical Coherence Tomography: Theory and Evolution
OCT operates on the principle of low-coherence interferometry to perform optical sectioning within scattering tissues. The technology measures backscattered light from internal tissue structures by comparing it with light from a reference arm, generating cross-sectional images with micron-scale resolution. The evolution of OCT has progressed through several generations, each offering distinct advantages. Time-Domain OCT (TD-OCT) utilizes a moving reference mirror and was the first commercially available implementation, providing basic imaging capability but limited by slower acquisition speeds (approximately 400 A-scans/second) and lower resolution (8-10 µm axial resolution) [19]. The development of Spectral-Domain OCT (SD-OCT) dramatically improved performance by replacing the moving reference with a stationary spectrometer, enabling significantly faster acquisition rates (20,000-52,000 A-scans/second) and improved axial resolution (5-7 µm) [19]. The current state-of-the-art, Swept-Source OCT (SS-OCT), employs a wavelength-swept laser and photodetector to achieve even faster scanning rates (100,000-236,000 A-scans/second) with enhanced penetration depth, making it particularly suitable for imaging deeper ocular structures and anterior segment visualization [19].
Table 1: Technical Comparison of OCT Modalities
| Parameter | TD-OCT | SD-OCT | SS-OCT |
|---|---|---|---|
| Light Source | Broadband light source with moving reference mirror | Broadband light with spectrometer detection | Tunable laser swept across wavelengths |
| Axial Resolution | 8-10 µm | 5-7 µm | ~11 µm |
| Scan Rate | 400 A-scans/s | 20,000-52,000 A-scans/s | 100,000-236,000 A-scans/s |
| Key Advantages | Lower cost | High resolution, widely available | Superior depth penetration, faster imaging |
| Primary Limitations | Slow acquisition, motion artifacts | Limited depth penetration | Higher cost, limited availability |
Multiphoton Microscopy: Physical Foundations and Advancements
Multiphoton microscopy encompasses both two-photon and three-photon excitation processes that rely on the near-simultaneous absorption of multiple photons to excite fluorescent molecules. The probability of multiphoton absorption depends on the square (for two-photon) or cube (for three-photon) of the instantaneous light intensity, confining excitation to a small focal volume without the need for a detection pinhole. This inherent optical sectioning capability, combined with the use of longer excitation wavelengths (typically in the near-infrared range), enables deep tissue imaging with reduced phototoxicity compared to confocal microscopy [20]. Two-photon microscopy typically employs excitation wavelengths of 680-1050 nm for imaging conventional fluorophores, while three-photon microscopy utilizes longer wavelengths (1300-1700 nm) to access greater penetration depths in highly scattering tissues like the brain [20].
Recent advancements in MPM have focused on extending imaging depth through optimized wavelength selection. The effective attenuation coefficient in biological tissues reaches a minimum at approximately 1.7 µm, making this wavelength ideal for three-photon excitation of red fluorophores [20]. Additionally, the development of adaptive excitation sources and pulse-on-demand systems has improved signal strength by concentrating illumination only on regions of interest, thereby increasing permissible pulse energy at the focus while maintaining safe average power levels [20]. The integration of adaptive optics has demonstrated approximately 10× signal increase for neuronal imaging and up to 30× enhancement for finer dendritic structures by correcting for tissue-induced aberrations [20].
Table 2: Performance Characteristics of Multiphoton Modalities
| Parameter | Confocal Microscopy | Two-Photon Microscopy | Three-Photon Microscopy |
|---|---|---|---|
| Excitation Mechanism | Single-photon absorption | Simultaneous two-photon absorption | Simultaneous three-photon absorption |
| Excitation Wavelength | Visible/UV | NIR (680-1050 nm) | Longer NIR (1300-1700 nm) |
| Penetration Depth | Shallow (100-200 µm) | Moderate (500-800 µm) | Deep (up to 1.5 mm) |
| Resolution | High (lateral: 0.2 µm, axial: 0.5 µm) | Slightly lower than confocal | Similar to two-photon |
| Background Signal | High without pinhole | Minimal, inherent sectioning | Minimal, improved sectioning |
| Photodamage | High in deep tissue | Reduced outside focal plane | Further reduced outside focus |
Methodologies and Experimental Protocols
Integrated OCT-MPM System for Cochlear Imaging
A representative multimodal imaging platform combines spectral-domain OCT with two-photon microscopy for investigating mechanotransduction in the mammalian cochlea. This system addresses the challenge of rapid switching between optical configurations with different numerical apertures (ranging from 0.13 to 0.8) required to capture both cellular (<10 µm) and structural (>200 µm) details [21].
System Configuration:
- Light Sources: The integrated system incorporates a custom SD-OCT engine alongside a femtosecond laser for two-photon excitation.
- Beam Conditioning: Two tunable liquid lenses form a beam expander that dynamically adjusts beam diameter at the back aperture of each objective, optimizing light throughput and maintaining high signal-to-noise ratio across all objectives [21].
- Automation: Optical adjustments are automated to facilitate seamless imaging across spatial scales, enabling high-precision vibration and fluorescence imaging in a single experimental session.
Experimental Protocol:
- Sample Preparation: Excised murine cochlea samples or living murine models are positioned using a high-precision stage.
- Multimodal Data Acquisition:
- TPM is first used to locate fluorescent outer hair cells through the round window membrane.
- OCT vibrometry measurements are performed concurrently to assess tissue mechanics.
- Functional Assessment: Cochlear structures including hair cells, basilar membrane, and reticular lamina are analyzed for phase relationships in response to acoustic stimuli (e.g., 70 kHz at 90 dB SPL) [21].
Key Findings: The integrated system demonstrated that all measured cochlear structures moved in phase in response to high-frequency stimulation, consistent with expected cochlear mechanics [21].
Combined MPM/OCT for Refractive Index and Thickness Characterization
This methodology enables noninvasive characterization of refractive index (RI) and thickness distribution in biological tissues through the synergistic combination of multiphoton microscopy and OCT.
Theoretical Basis: OCT measures optical pathlength (Lp), which represents the product of physical thickness (t) and refractive index (n): Lp = t × n [22]. Multimodal imaging resolves this ambiguity by providing independent measurements of optical pathlength (from OCT) and physical thickness (from MPM), allowing calculation of RI as n = Lp/t.
Experimental Workflow:
- Sample Preparation: Fresh tissue samples (e.g., fish cornea) are mounted without chemical fixation or sectioning.
- Co-registered Imaging:
- OCT cross-sectional images are acquired to determine optical pathlength.
- 3D MPM images (TPEF and SHG) are successively captured at the identical sample location to determine physical thickness.
- Data Analysis:
- Tissue layers are distinguished based on biochemical contrasts from MPM (cellular features via TPEF, collagen via SHG).
- For each identified layer, physical thickness is derived from MPM data while optical pathlength is obtained from OCT.
- Layer-specific RI is calculated as the ratio of optical pathlength to physical thickness.
Validation: The method demonstrated precision within ~1% error compared to reference values when tested on standard samples (water, air, immersion oil, cover glass) [22]. Application to fish cornea identified three distinct layers with RIs of ~1.446-1.448 (epithelium), 1.345-1.372 (stroma I), and 1.392-1.436 (stroma II), correlating with their tissue compositions [22].
Integrated Optoacoustic and Two-Photon Microscopy for Neuroimaging
This protocol details the integration of optical-resolution optoacoustic microscopy (OAM) with two-photon microscopy for functional neuroimaging in murine models, enabling comprehensive analysis of neurovascular coupling.
System Configuration:
- Light Sources: Separate nanosecond and femtosecond laser sources for OAM and TPM, respectively.
- Data Acquisition: Custom LabVIEW code manages semi-simultaneous acquisition, capturing alternating frames from OAM and TPM subsystems at different time points [23].
- Spatial Resolution: The TPM subsystem achieves 400 nm lateral and 6.85 µm axial resolution, while OAM achieves 670 nm lateral and 4.01 µm axial resolution [23].
Experimental Protocol:
- Animal Preparation:
- C57BL/6 mice are injected with adeno-associated virus (AAV) for neuronal labeling.
- A 3-mm diameter cranial window is created over the primary somatosensory cortex.
- A head plate is attached to the skull using cyanoacrylate glue and dental cement.
- In Vivo Imaging:
- Mice are anesthetized with ketamine (25 mg/kg) and xylazine (1.25 mg/kg).
- Physiological parameters (body temperature, oxygen saturation) are continuously monitored.
- Medical ultrasonic gel is applied to ensure efficient coupling of ultrasound waves.
- Data Acquisition:
- Z-stacks (330 × 300 µm² FOV) up to 350 µm depth are acquired semi-simultaneously.
- Vascular networks are imaged at 90 µm depth across an 800 × 800 µm² lateral FOV with OAM.
- Neuronal structures are captured concurrently via TPM at matching depth planes.
Functional Analysis: The system captures spontaneous vasodilation and vasoconstriction dynamics in cortical vessels, with diameter changes monitored over time to investigate neurovascular coupling mechanisms [23].
Advanced Applications and Current Research
Ophthalmic Imaging and Accessibility Innovations
OCT has established itself as the clinical standard for retinal disease diagnosis and management, with recent innovations focusing on improving accessibility. Traditional OCT systems require trained technicians and are confined to clinical settings, creating barriers for elderly, rural, and frequently monitored patients [19]. The development of portable, community-based systems like the SightSync OCT addresses these limitations through a compact design (6 × 6 mm resolution, 80,000 A-scans/s) that enables technician-free operation with secure data transfer capabilities [19]. This innovation expands screening possibilities for vision-threatening conditions like age-related macular degeneration (affecting approximately 196 million people globally in 2020) and diabetic retinopathy (affecting 103.12 million adults worldwide) [19].
Multimodal platforms such as the Silverstone system integrate RGB imaging with OCT, fluorescein angiography, indocyanine green angiography, and autofluorescence. The addition of blue wavelength in RGB imaging provides enhanced visualization of whitish features like fibrosis and inflammation, while peripheral OCT capability enables examination of previously inaccessible retinal lesions [24]. These integrated systems eliminate the need to move patients between different imaging devices, significantly improving clinical workflow efficiency.
Deep Tissue and In Vivo Functional Imaging
Multiphoton microscopy continues to extend its capabilities for deep tissue imaging, with three-photon microscopy now enabling visualization of neuronal activity at depths exceeding 1 mm in the mouse brain with ~10 Hz temporal resolution [20]. Recent advances have demonstrated mouse brain vasculature imaging at depths greater than 2 mm, while maintaining single-cell spatial resolution [20]. Furthermore, imaging through the intact mouse or adult zebrafish skull is now achievable, minimizing surgical intervention and enabling more natural experimental conditions.
The development of multicolor single-wavelength excitation at 1.34 µm has simplified three-photon imaging by enabling simultaneous "conventional" three-photon excitation of green fluorophores and "high-energy" three-photon excitation of red fluorophores [20]. This approach leverages three-photon higher-energy excited state excitation of red fluorophores, with measurements revealing enhanced blue-shifted cross-sections (sometimes exceeding 10× the three-photon cross-section at the energy-scaled one-photon excitation peak) due to resonance enhancement [20].
Novel Biomedical Applications
OCT and MPM are expanding into diverse biomedical applications beyond their traditional domains. Reproductive biology has benefited from OCT imaging of fallopian tube dynamics, where 4D OCT imaging in mouse models revealed that the oviduct functions as a "leaky peristaltic pump" to transport preimplantation embryos [25]. This mechanism involves contraction waves originating in the ampulla and propagating through the isthmus, with relaxation at earlier contraction sites pulling fluid back to create bidirectional embryo movement [25]. These insights provide foundational understanding for investigating infertility and ectopic pregnancy.
In cancer diagnostics, second harmonic generation (SHG) imaging has demonstrated capability to differentiate between normal and cancerous thyroid tissue through quantitative analysis of collagen organization. Specific metrics like forward-backward ratio variance and mean Collagen Area Fraction show statistically significant differences (p⪅0.001) between tissue types, offering promise for improved diagnostic accuracy [26].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Multimodal Imaging Studies
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Adeno-Associated Virus (AAV) | Neuronal labeling for in vivo two-photon imaging | AAV vectors expressing fluorescent proteins (e.g., GFP) under neuronal promoters [23] |
| Femtosecond Laser Sources | Multiphoton excitation for deep tissue imaging | Er:doped fiber lasers (80 MHz), Yb-pumped NOPA systems (1.3 µJ pulses at 1.3 µm) [20] |
| Tunable Liquid Lenses | Dynamic beam adjustment in multimodal systems | Commercially available electrowetting or elastomer-based lenses for rapid focal length adjustment [21] |
| Fluorescent Microspheres | System resolution characterization | 0.2-µm diameter FluoSpheres for point spread function measurement [23] |
| Medical Ultrasonic Gel | Acoustic coupling in optoacoustic microscopy | Commercial ultrasound transmission gels transparent to excitation lasers and fluorescence [23] |
| NAD(P)H and FAD | Endogenous metabolic contrast for FLIM | Natural coenzymes imaged via two-photon fluorescence lifetime microscopy [26] |
| Cranial Window Materials | Surgical preparation for chronic brain imaging | Cyanoacrylate glue, dental cement, 3-mm glass coverslips for murine cortical imaging [23] |
Future Directions and Emerging Technologies
The convergence of OCT and MPM with computational methods represents the next frontier in bio-optical imaging. Artificial intelligence is being increasingly integrated into OCT technology, with deep learning algorithms demonstrating remarkable capabilities in automated image analysis. Hybrid convolutional and recurrent neural networks (CNN-RNN) have achieved an area under the curve (AUC) of 0.94 for detecting diabetic macular edema, while specialized algorithms for segmenting pathological features in neovascular age-related macular degeneration show AUC values ranging from 0.932 to 0.990 for various fluid compartments [19]. These AI-driven tools not only improve diagnostic consistency but also enable large-scale screening initiatives through reduced interpretation time.
Advancements in fluorescence lifetime imaging microscopy (FLIM) coupled with multiphoton excitation are expanding metabolic imaging capabilities. Simultaneous two-photon excitation of NAD(P)H and FAD through wavelength mixing enables multiparametric metabolic imaging in dynamic biological systems with minimal phototoxicity [26]. This approach has been successfully applied to longitudinal studies of stem cell differentiation and embryo development, revealing the richness and complexity of metabolic processes in intact tissues [26].
Technical developments in compact and portable systems are increasing accessibility to advanced imaging technologies. The development of a briefcase OCT system weighing only 9 kg and costing approximately $8,000 demonstrates the potential for point-of-care applications in primary care centers and low-resource settings [27]. Similarly, ultracompact femtosecond fiber lasers are enabling nonlinear imaging and 3D lithography in more accessible formats, with applications demonstrated in live, beating heart tissue organoids [26].
The continued synergy between OCT and MPM technologies promises to further dissolve the traditional boundaries between structural and molecular imaging, providing researchers and clinicians with increasingly comprehensive tools for understanding biological systems and developing novel therapeutic interventions.
Raman spectroscopy has emerged as a pivotal analytical tool within the field of bio-optics, offering a unique synergy of speed, sensitivity, and non-destructivity for molecular profiling. This technique is revolutionizing biopharmaceutical development and biomedical research by providing detailed molecular "fingerprints" without extensive sample preparation. The integration of Raman spectroscopy into bio-optics design addresses critical challenges in analyzing complex biological systems and pharmaceutical formulations, enabling real-time monitoring and quality control in both research and clinical applications [28] [29]. Its ability to provide quantitative insights into molecular structure, composition, and interactions makes it particularly valuable for drug development professionals seeking to optimize processes and ensure product integrity.
Fundamental Principles of Raman Spectroscopy
Raman spectroscopy hinges on inelastic light scattering by molecules. When a monochromatic laser beam (typically in the visible or near-infrared range) interacts with a sample, most photons scatter elastically (Rayleigh scattering). However, a small fraction (approximately 1 in 10⁷ photons) undergoes inelastic scattering (Raman scattering), resulting in a shift in photon energy that corresponds to the molecules' vibrational modes [29].
These vibrational modes generate unique "spectral fingerprints" that provide detailed information about molecular structure, symmetry, chemical bonds, and molecular environment. Unlike infrared spectroscopy, Raman spectroscopy exhibits low sensitivity to water, rendering it particularly advantageous for analyzing aqueous biological samples without extensive sample preparation [29]. The Raman effect was discovered by physicist C.V. Raman and relies on the interaction between laser light and molecular vibrations, providing a powerful method for non-destructive molecular analysis [28].
Technical Workflow
The basic instrumentation involves:
- A monochromatic laser source (typically 785 nm for biological samples to minimize fluorescence)
- A spectrograph that disperses the scattered light according to wavelength
- A high-sensitivity detector, such as a charge-coupled device (CCD) or electron-multiplying charge-coupled device (EMCCD) [29]
After spectral acquisition, data processing involves baseline correction, noise reduction using advanced algorithms, and spectral normalization to facilitate quantitative analysis and comparison [28] [29].
Advanced Spectral Processing Methodologies
The accurate interpretation of Raman spectral data requires sophisticated processing algorithms to mitigate noise and fluorescence interference, which are particularly challenging in complex biological and pharmaceutical samples.
Table 1: Key Spectral Processing Algorithms and Their Applications
| Algorithm | Primary Function | Application Context | Key Parameters |
|---|---|---|---|
| airPLS (adaptive iteratively reweighted penalized least squares) | Background subtraction and noise reduction | Effective for liquid formulations with minimal fluorescence interference [28] | Iterative weighting with penalty factor |
| Hybrid Peak-Valley Interpolation | Fluorescence background correction | Complex samples with strong fluorescence (gels, solid formulations) [28] | Local peak-valley identification with PCHIP interpolation |
| Savitzky-Golay Smoothing | Spectral smoothing and noise reduction | General signal preprocessing for biological samples [29] | Polynomial order, window size |
| Density Functional Theory (DFT) | Theoretical spectrum prediction | Validation of experimental results via quantum mechanical calculations [28] | Computational modeling of molecular vibrations |
Experimental Protocol: Multi-Algorithm Spectral Processing
For complex pharmaceutical formulations with significant fluorescence interference, the following integrated protocol has demonstrated success:
Initial Acquisition: Collect raw spectra using a 785 nm excitation wavelength with 4-second acquisition time per sample [28]
Primary Processing: Apply the airPLS algorithm for baseline correction and initial noise reduction using the following MATLAB/Python pseudocode:
Fluorescence Correction: For samples with persistent fluorescence:
- Identify local spectral peaks and valleys using derivative spectroscopy
- Apply piecewise cubic Hermite interpolating polynomial (PCHIP) interpolation between valleys
- Subtract the interpolated baseline from the airPLS-corrected spectrum [28]
Validation: Compare processed experimental spectra with DFT-simulated theoretical predictions to verify detection accuracy of target molecules [28]
This method has successfully identified active ingredients (antipyrine, paracetamol, and lidocaine) in diverse drug formulations (liquid, solid, and gel) with an average response time of just 4 seconds per test and a signal-to-noise ratio reaching 800:1 [28].
Research Reagent Solutions and Essential Materials
Table 2: Key Research Reagents and Materials for Raman Spectroscopy in Pharmaceutical Applications
| Material/Reagent | Function | Application Example |
|---|---|---|
| Gold Nanoparticles | SERS substrate for signal enhancement | Trace contaminant detection; engineered with precise size/shape control [29] |
| Custom Plasmonic Nanostructures | Create "hot spots" for electromagnetic enhancement | Improve SERS signal reproducibility (<10% RSD across substrates) [29] |
| Temperature-Controlled Stage | Precise thermal management for stability studies | Protein denaturation studies with ±1°C precision [29] |
| Fiber-Optic Raman Probes | In situ monitoring in bioreactors | Real-time cell culture metabolite tracking [29] |
| Microfluidic Chips with SERS Substrates | Automated sample handling | High-throughput analysis of trace contaminants (μL sample volumes) [29] |
| Specialized Excipients (sucrose, polysorbate 80) | Protein stabilization in formulations | Excipient interaction mapping via spectral changes [29] |
Applications in Drug Development and Biopharmaceutical Manufacturing
Protein Structure and Stability Analysis
Raman spectroscopy provides deep, quantifiable insights into protein secondary and tertiary structure crucial for biological product stability. Advanced algorithms enable identification of subtle shifts in peak positions and intensity ratios that correlate with specific structural elements:
Experimental Protocol: Temperature-Dependent Stability Studies
Sample Preparation: Prepare monoclonal antibody formulations with varying excipient concentrations (e.g., sucrose 0-10% w/v, polysorbate 80 0-0.1% w/v)
Spectral Acquisition:
- Use temperature-controlled stage with ±1°C precision
- Acquire spectra at 5°C increments from 25°C to 85°C
- Monitor specific Raman bands: amide I (1600-1700 cm⁻¹), amide III (1230-1300 cm⁻¹), and disulfide bonds (500-550 cm⁻¹)
Data Analysis:
- Apply curve fitting using Gaussian/Lorentzian functions for spectral deconvolution
- Calculate intensity ratios of deconvoluted bands associated with different structural elements
- Determine melting temperature by sigmoidal fitting of intensity changes [29]
Case Study: A biopharmaceutical company developing a novel monoclonal antibody discovered aggregation issues during long-term storage. Using Raman spectroscopy with temperature-dependent studies and spectral deconvolution of the amide I band, they identified a specific disulfide bond with vibrational frequency shifts preceding aggregation. By monitoring intensity ratios of deconvoluted bands, the team quantitatively determined the optimal storage temperature (-20°C), extending product shelf life by six months (50% improvement). The analysis was completed in two days per formulation condition, significantly faster than traditional stability assays requiring several weeks [29].
Precision Cell Culture Media Optimization
Raman spectroscopy enables real-time, quantifiable monitoring of cellular metabolism and critical quality attributes (CQAs) in bioprocessing:
Experimental Protocol: Bioreactor Monitoring
System Setup: Integrate fiber-optic Raman probes with bioreactors using industrial communication protocols
Model Development:
- Acquire Raman spectra every 15 minutes throughout cell culture process
- Collect parallel off-line measurements: viable cell density, metabolite concentrations, product titer, glycosylation patterns
- Apply partial least squares (PLS) regression to establish correlations between spectral features and process parameters
Implementation:
- Develop control algorithms based on validated PLS models (typically R² > 0.95)
- Automate feeding strategies based on real-time metabolite monitoring (e.g., glucose, glutamate)
- Maintain critical parameters within ±10% of target concentrations [29]
Real-World Example: A contract manufacturing organization implemented in situ Raman spectroscopy for real-time monitoring of a fed-batch mAb production process. By continuously monitoring lactate and glutamate levels using a validated PLS model (R² > 0.97, RMSEP < 3 mM), process engineers identified critical feeding points where nutrient depletion limited cell growth and affected glycosylation. Implementing automated feedback controls increased average product titer by 25% (from 2 g/L to 2.5 g/L) and reduced standard deviations of CQAs by 15% [29].
Trace-Contaminant Detection with SERS
Surface-Enhanced Raman Spectroscopy (SERS) dramatically enhances sensitivity for detecting low-concentration analytes:
Experimental Protocol: SERS-Based Contaminant Screening
Substrate Preparation:
- Engineer custom gold nanoparticles with controlled size, shape, and surface chemistry
- Characterize using TEM and DLS to ensure uniformity
- Immobilize nanoparticles on microfluidic chips
Method Validation:
- Establish calibration curves with spiked samples
- Determine limit of detection (LoD) and limit of quantification (LoQ)
- Assess reproducibility across multiple substrates (<10% RSD)
Sample Analysis:
- Inject microliter-volume samples through microfluidic system
- Acquire SERS spectra with 10-30 second integration time
- Quantify contaminants using pre-established multivariate models [29]
Quantified Benefit: A quality-control laboratory reduced average analysis time per batch from four hours using conventional HPLC-MS to <10 minutes using SERS microfluidics. The method achieved an LoD of 10 ppb for specific leachable impurities (compared to 25 ppb with HPLC-MS) and saved an estimated $50,000 annually in reagent costs [29].
Workflow Visualization
Raman Spectroscopy Experimental Workflow
SERS Signal Enhancement Mechanism
Future Perspectives and Integration with Bio-Optics
The trajectory of Raman spectroscopy points toward increased integration with computational methods and biomedical optical systems. Key emerging trends include:
AI and Advanced Chemometrics: Machine learning algorithms are transforming Raman data analysis, achieving >98% classification accuracy for identifying product quality deviations and R² > 0.98 for predicting critical quality attributes. The integration of Raman spectral data with other process data (temperature, pH, dissolved oxygen) using data-fusion techniques enables comprehensive multivariate process models [29].
Standardization and Regulatory Acceptance: Industry consortia and regulatory bodies are developing comprehensive guidelines for Raman spectroscopy applications in biopharmaceutical manufacturing, focusing on method validation, spectral-library development, and data integrity to ensure robust regulatory acceptance [29].
Integration with Digital Twins: Combining real-time Raman spectroscopy data with sophisticated digital-twin models provides dynamic virtual representations of manufacturing processes, enabling advanced predictive modeling and virtual process optimization [29].
Bio-Optics Synergies: Raman spectroscopy aligns with broader bio-optics applications discussed at leading conferences, including ophthalmic imaging, biochips and optofluidics, nanophotonics for biomedicine, and machine learning for image reconstruction and interpretation [4]. These integrations highlight the growing role of Raman spectroscopy within the comprehensive bio-optics design and application ecosystem, particularly for biomedical optical technologies in life sciences and clinical research.
As Raman spectroscopy continues to evolve, its synergy with other bio-optical technologies will undoubtedly unlock new capabilities for molecular profiling, ultimately accelerating drug development and enhancing our understanding of complex biological systems.
Bio-optics, which involves the application of optical principles to biological studies, has been revolutionized by advances in fluorescence imaging. This field sits at the intersection of biology, physics, and engineering, driving innovations that enable researchers to visualize biological processes with unprecedented clarity. Within this domain, two areas showing particularly rapid advancement are the development of novel fluorescent probes and the refinement of Fluorescence Lifetime Imaging Microscopy (FLIM). These technologies are transforming our understanding of cellular processes and disease mechanisms, offering researchers and drug development professionals powerful tools for diagnostic and therapeutic applications. The global fluorescence microscopy market, valued at $968.5 million in 2024 and projected to reach $1.3 billion by 2029, reflects the significant investment and growth in these technologies [30].
The evolution from traditional intensity-based fluorescence imaging to lifetime-based techniques represents a paradigm shift in biological imaging. While conventional fluorescence microscopy relies primarily on signal intensity, FLIM exploits the nanosecond-scale decay characteristics of fluorophores, providing information independent of concentration, excitation intensity, or photon scattering [31]. This additional dimension of fluorescence information helps researchers unveil functional and mechanistic information about biological systems, making it particularly valuable for studying protein interactions, cellular metabolism, and disease biomarkers. When combined with specially designed fluorescent probes that respond to specific biological triggers, FLIM enables precise monitoring of pathological processes in live cells and tissues.
Novel Fluorescent Probes for Biomedical Applications
Design Principles and Signaling Mechanisms
Modern fluorescent probes have evolved significantly from simple labeling molecules to sophisticated biosensors that respond to specific biochemical environments or analytes. Contemporary probe design incorporates several strategic approaches to maximize signal-to-noise ratios and biological relevance. Aggregation-induced emission (AIE) probes display minimal background signal and selectively light up upon binding to specific targets like protein aggregates [32]. Photoinduced electron transfer (PET) mechanisms effectively quench fluorescence until the probe interacts with its target analyte, creating a "turn-on" response that minimizes background interference [33]. Intramolecular charge transfer (ICT) systems utilize donor-π-acceptor structures that create large Stokes shifts, reducing self-quenching and improving signal detection [33]. Environment-sensitive probes that exhibit fluorescence enhancement in specific hydrophobic or hydrophilic microenvironments enable localization to specific cellular compartments such as lipid droplets [34].
The strategic incorporation of specific recognition groups allows probes to respond to particular biomarkers. For instance, ester bonds can serve as cleavage sites for specific enzymes or analytes like hydrogen sulfide (H2S), which acts as a nucleophile to break the bond and release a fluorescent signal [33]. The selection of fluorophores with appropriate quantum yields, photostability, and biocompatibility is crucial for prolonged imaging sessions, particularly in live-cell applications where phototoxicity and photobleaching must be minimized [30].
Representative Probe Designs and Applications
Table 1: Characteristics of Novel Fluorescent Probes
| Probe Name | Target | Detection Mechanism | Emission Peak | Detection Limit | Application |
|---|---|---|---|---|---|
| Probe-1 [33] | H2S | Ester bond cleavage by nucleophilic attack | 603 nm | Not specified | Tumor imaging |
| mRA [32] | Amyloid-β aggregates | Aggregation-induced emission | 510-750 nm | 0.12 μg/mL | Alzheimer's diagnosis |
| BZMN & BZID [34] | Lipid droplets | Environment-sensitive turn-on | Not specified | High signal-to-noise ratio | Atherosclerosis research |
Probe-1 for Hydrogen Sulfide Detection: This benzochromene-based probe features a D-π-A structure with benzopyrylium as an electron-donating group and 7-hydroxy-1-indanone as an electron-accepting group with ICT effects. The acryloyl group serves as both a quenching moiety via PET and a recognition element through its ester bond. When H2S cleaves this ester bond, fluorescence enhances at 603 nm within 3 minutes, enabling rapid detection of this gasotransmitter that is overexpressed in many tumor tissues [33].
Triphenylamine Rhodamine-3-Acetic Acid (mRA) for Alzheimer's Diagnosis: This aggregation-induced emission probe specifically binds with high affinity to Aβ aggregates, with a detection limit of 0.12 μg/mL. Molecular docking studies confirm significant binding affinity toward the Aβ peptide at N/C-terminal regions with binding energy of -6.5 kcal/mol. The binding process is spontaneous, driven by enthalpy and favored by entropy, with hydrogen bonding identified as a dominant interaction force [32].
BZMN and BZID for Lipid Droplet Imaging: These probes feature large Stokes shifts, excellent biocompatibility, and superior photostability. They demonstrate extremely low fluorescence in aqueous solution and significantly enhanced fluorescence in lipid environments, creating high signal-to-noise ratios crucial for precise visualization of lipid droplets in cellular and mouse atherosclerosis models [34].
Experimental Protocols for Probe Validation
Validation of H2S Probe-1: To explore the optimal testing system, researchers evaluated Probe-1's response to H2S in several common solvents, finding highest fluorescence intensity in DMSO due to aggregation-induced restrictions on intramolecular rotation and vibration. For biological applications, they selected a DMSO:PBS = 1:99 (v/v) system. The probe (10 μM) was incubated with various concentrations of H2S (0-200 μM) in PBS (pH 7.4) containing 1% DMSO at 37°C. Fluorescence intensity was measured at 603 nm with excitation at 475 nm, with scans taken every 30 seconds for 10 minutes to establish reaction kinetics. Selectivity was assessed by challenging the probe with various biologically relevant analytes including reactive oxygen species, amino acids, and metal ions [33].
Characterization of mRA Binding to Aβ Aggregates: Fluorescence spectroscopy determined binding affinity of mRA with Aβ protein. The probe (2.5 μM) was incubated with varying Aβ concentrations (0-300 μg/mL) in PBS buffer (pH 7.4) for 15 minutes at 25°C under dim light to prevent photo-oxidation. Emission spectra were recorded from 510-750 nm with excitation at 475 nm, using 5 nm excitation and 10 nm emission slit widths with 1 cm path length. The limit of detection was calculated using the formula LOD = 3.3σ/S, where σ is the standard deviation of the blank signal and S is the slope of the calibration plot. Circular dichroism studies confirmed structural alterations upon binding, and molecular docking studies identified specific binding sites [32].
Fluorescence Lifetime Imaging (FLIM) Methodologies
Fundamental Principles and Technical Advances
Fluorescence lifetime refers to the average time a fluorophore remains in its excited state before returning to the ground state, typically occurring on the nanosecond scale. Unlike intensity-based measurements, fluorescence lifetime is independent of fluorophore concentration, excitation light intensity, and photobleaching, making it a more robust parameter for quantitative biological imaging [31]. FLIM translates the duration of excited states of fluorophores into lifetime information as an additional source of contrast in biological samples, offering the possibility to separate fluorophores with similar excitation spectra but different lifetimes [35].
Recent technical advances have significantly expanded FLIM applications in biological research. Phasor analysis approaches simplify lifetime data interpretation by transforming complex decay curves into graphical representations that facilitate component separation without requiring prior knowledge of the system [35]. Multiplexing applications use lifetime differences to distinguish multiple fluorophores in the same sample, overcoming spectral overlap limitations in conventional fluorescence microscopy [31]. STED super-resolution integration combines FLIM with stimulated emission depletion microscopy to achieve nanoscale resolution while maintaining lifetime information (tauSTED) [31]. Open-source analysis tools like the napari-flim-phasor-plotter enable accessible data handling and workflow implementation for FLIM data of different formats [35].
FLIM Experimental Workflows and Applications
Protein-Protein Interaction Studies: FLIM-FRET (Förster Resonance Energy Transfer) is a powerful technique for monitoring protein-protein interactions in live cells. When two proteins interact and their associated fluorophores come within close proximity (typically <10 nm), energy transfer occurs, resulting in a measurable decrease in the fluorescence lifetime of the donor fluorophore. This approach provides quantitative information about interaction dynamics without the need for absolute concentration measurements [31].
Metabolic Imaging: FLIM of endogenous fluorophores like NAD(P)H and FAD enables label-free metabolic imaging. Different metabolic states produce characteristic lifetime changes in these cofactors, allowing researchers to monitor metabolic shifts in response to pharmacological treatments or disease states without exogenous labeling [31] [35].
Multiplexing in Live-Cell Imaging: A recent fluorescence lifetime separation approach for FLIM live-cell imaging demonstrates the distinction of highly spectrally overlapping fluorophores like mCherry and mKate2. This enables distinctive tracking of tagged proteins in six-dimensional datasets to investigate processes like cell division in developing early embryos of model systems like Caenorhabditis elegans [35].
Background and Autofluorescence Separation: FLIM can separate fluorescence of tagged proteins of interest from masking natural autofluorescence in tissue samples and animal models. This is particularly valuable in complex biological samples where autofluorescence often interferes with conventional intensity-based measurements [31] [35].
Detailed FLIM Experimental Protocol
FLIM Phasor Separation for Live-Cell Imaging: For distinguishing highly spectrally overlapping fluorophores, researchers used Caenorhabditis elegans as a model system. Samples expressing fluorescently tagged proteins were mounted on appropriate imaging chambers. FLIM data was acquired using a confocal microscope equipped with time-correlated single photon counting (TCSPC) capabilities. Excitation was performed using a 560 nm pulsed laser at 40 MHz repetition rate, with emission collected through appropriate bandpass filters. Acquisition continued until sufficient photons were collected for reliable lifetime calculation (typically 100-1000 photons per pixel). Data was processed using phasor analysis implemented in the napari-flim-phasor-plotter, an open-source plugin that facilitates conversion, visualization, analysis and reuse of FLIM data of different formats. Lifetime separation was achieved by identifying distinct clusters in the phasor plot corresponding to different fluorophores or environmental conditions [35].
FLIM-FRET for Protein-Protein Interactions: Cells expressing donor and acceptor fusion proteins were plated on glass-bottom dishes and imaged in appropriate culture medium. FLIM data was acquired using a confocal microscope with TCSPC module. Donor fluorophores were excited using a pulsed laser (e.g., 470 nm for EGFP), and emission was collected through a bandpass filter. The fluorescence decay was fitted to a multi-exponential model, and the average lifetime was calculated for each pixel. FRET efficiency was determined by comparing the lifetime of the donor in the presence and absence of the acceptor using the formula: E = 1 - (τDA/τD), where τDA is the donor lifetime in the presence of acceptor and τD is the donor lifetime alone [31].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Fluorescence Imaging
| Category | Specific Examples | Function/Application | Key Characteristics |
|---|---|---|---|
| Fluorescent Probes | Probe-1 [33], mRA [32], BZMN/BZID [34] | Target-specific detection and imaging | High selectivity, large Stokes shifts, low background fluorescence |
| Microscopy Systems | STELLARIS (Leica) [31], Systems by Bruker, Nikon, Olympus, Zeiss [30] | Image acquisition and data collection | FLIM capability, spectral detection, high sensitivity detectors |
| Analysis Software | napari-flim-phasor-plotter [35], Commercial FLIM analysis packages | Data processing and lifetime calculation | Phasor analysis, lifetime fitting, component separation |
| Biological Models | Cell lines, C. elegans [35], Mouse models [33] [34] | Experimental biological systems | Relevance to human disease, genetic tractability, imaging accessibility |
The implementation of advanced fluorescence imaging requires careful selection of instruments, probes, and analytical tools. Modern fluorescence microscopes for FLIM applications typically incorporate time-correlated single photon counting (TCSPC) capabilities, high-sensitivity detectors, and tunable laser systems for flexible excitation [30]. The choice of fluorescent probes depends on specific application requirements, with considerations including brightness, photostability, lifetime characteristics, and compatibility with biological systems [33] [34] [32].
Sample preparation protocols vary depending on the biological model and specific research question. For live-cell imaging, maintaining cell viability is paramount, requiring careful control of temperature, CO₂, and humidity during imaging sessions [30]. For model organisms like C. elegans, appropriate mounting techniques and anesthesia methods are necessary to minimize motion artifacts while preserving physiological function [35].
Data analysis represents a critical component of the FLIM workflow. The emergence of open-source analysis tools like the napari-flim-phasor-plotter has made sophisticated lifetime analysis more accessible to researchers without specialized expertise in photophysics [35]. These tools facilitate the implementation of phasor analysis, which provides a graphical representation of lifetime data that can be more intuitively interpreted than traditional multi-exponential fitting approaches.
The evolution of fluorescence imaging continues to accelerate, driven by synergistic advances in probe design, instrumentation, and computational analysis. Several emerging trends are likely to shape future developments in this field. The integration of artificial intelligence and machine learning with fluorescence lifetime analysis is already showing promise for automated cell classification and subcellular structure identification [30] [31]. The ongoing development of novel fluorescent probes with larger Stokes shifts, improved photostability, and higher target specificity will expand the applications of both conventional fluorescence imaging and FLIM [33] [34] [32]. Advancements in super-resolution FLIM techniques like tauSTED are pushing the boundaries of spatial resolution while maintaining valuable lifetime information [31]. The increasing accessibility of FLIM through user-friendly instrumentation and open-source software is democratizing this powerful technology, making it available to a broader range of researchers [35].
In conclusion, the combination of novel fluorescent probes and FLIM technologies represents a powerful toolkit for researchers and drug development professionals working in the field of bio-optics. These technologies provide unprecedented capabilities for visualizing and quantifying biological processes in live cells and tissues, offering insights that were previously inaccessible. As these technologies continue to evolve and become more widely adopted, they will undoubtedly accelerate both basic biological discovery and the development of novel diagnostic and therapeutic approaches for human disease. The framing of these advances within the broader context of bio-optics design and application highlights the interdisciplinary nature of this progress, requiring collaboration across physics, chemistry, biology, and engineering to fully realize the potential of these innovative imaging technologies.
Bio-optics, the application of light-based technologies for the imaging, analysis, and manipulation of biological systems, has emerged as a transformative force in modern medicine. This field represents a synergistic convergence of optical physics, engineering, and biological science, creating powerful tools that bridge technological innovation and clinical application. The fundamental premise of bio-optics involves leveraging the interactions between light and biological tissues to extract diagnostic information or enable therapeutic interventions with exceptional precision and minimal invasiveness.
The clinical significance of bio-optics continues to expand, driven by technological advancements and growing healthcare needs. The global bio-optics market, valued at approximately $2.03 billion in 2024, reflects this importance and is projected to grow at a compound annual growth rate (CAGR) of 6.3% through 2032 [12]. Within the United States, this growth is even more pronounced, with the market anticipated to advance at a CAGR of 9.46% from 2026-2033, reaching $22.62 billion by 2033 [36]. This remarkable expansion is fueled by increasing adoption across healthcare diagnostics, surgical procedures, and research applications, particularly in cancer diagnostics, infectious disease detection, and microsurgery.
The integration of bio-optics with artificial intelligence (AI) and machine learning (ML) represents a paradigm shift in diagnostic and therapeutic capabilities. AI-enhanced optical systems can now identify biological alterations and abnormal cellular growth with precision that often surpasses human capability [37]. Similarly, the emergence of wearable bioelectronics with optical sensing capabilities is creating new opportunities for continuous monitoring and point-of-care diagnostics, particularly in resource-limited settings [38] [39]. These developments position bio-optics as a critical enabler of personalized medicine, precision diagnostics, and minimally invasive interventions.
Key Application Areas: Technological Foundations and Principles
Cancer Diagnostics
Optical technologies have revolutionized cancer diagnostics by enabling non-invasive detection, precise characterization, and real-time monitoring of malignant tissues. The biological basis for optical cancer diagnostics leverages the fundamental differences in how healthy and cancerous tissues interact with light, including variations in absorption, scattering, fluorescence, and Raman spectra [39].
Table 1: Bio-Optic Technologies in Cancer Diagnostics
| Technology | Operating Principle | Key Applications | Spatial Resolution | Penetration Depth |
|---|---|---|---|---|
| Optical Coherence Tomography (OCT) | Interferometry with low-coherence light | Tissue microstructure imaging, tumor margin assessment | 1-15 μm | 1-3 mm |
| Fluorescence Imaging | Detection of emitted light from fluorescent probes or tissues | Cancer biomarker detection, tumor visualization, surgical guidance | 10-100 μm | 0.5-2 mm |
| Raman Spectroscopy | Inelastic scattering providing molecular fingerprint | Biochemical composition analysis, cancer typing | 1-10 μm | 0.1-0.5 mm |
| Diffuse Optical Tomography | Near-infrared light propagation through tissue | Deep tissue oxygenation monitoring, tumor metabolism | 5-10 mm | Several centimeters |
| Optical Biosensors | Light-biomarker interaction causing detectable signal changes | Liquid biopsy, circulating tumor cell detection | N/A (solution-based) | N/A |
Advanced optical methods are particularly valuable for detecting novel biomarkers like extracellular vesicles (EVs), which are released in significantly greater quantities by tumor cells compared to healthy cells [40]. Techniques exploiting EV size, optical properties, and surface protein markers offer promising frontiers in non-invasive cancer diagnostics. Furthermore, the integration of AI with optical imaging has enabled automated analysis of complex optical data, identifying subtle patterns indicative of early-stage malignancies that might escape human detection [37].
Experimental Protocol: Fluorescence-Guided Cancer Margin Assessment
Tracer Administration: Administer tumor-specific fluorescent tracer (e.g., folate-FITC conjugate, indocyanine green) intravenously 24 hours before procedure [41].
Imaging Setup: Configure fluorescence imaging system with appropriate excitation (e.g., 750-800 nm for ICG) and emission filters (e.g., 820-870 nm for ICG).
Intraoperative Imaging: Position imaging system 15-20 cm above surgical field with consistent illumination intensity.
Signal Acquisition: Capture both white light and fluorescence images simultaneously using dual-channel imaging detector.
Quantitative Analysis: Calculate tumor-to-background ratio (TBR) using dedicated software: TBR = Mean fluorescence intensity of tumor region / Mean fluorescence intensity of adjacent normal tissue.
Histological Validation: Correlate optical findings with standard histopathology of biopsied samples.
Infectious Disease Detection
Bio-optics has dramatically transformed infectious disease diagnostics by enabling rapid, sensitive pathogen detection at the point of care. The urgent need for timely diagnosis is particularly critical in infectious diseases, where delayed results can lead to ongoing transmission and worsened patient outcomes [38]. Optical technologies address this need by providing rapid results that enable early, targeted therapy while reducing unnecessary antibiotic use.
Table 2: Bio-Optic Technologies in Infectious Disease Detection
| Technology | Pathogen Types | Detection Time | Sensitivity | Multiplexing Capability |
|---|---|---|---|---|
| Label-free Surface-Enhanced Raman Spectroscopy (SERS) | Bacteria, Viruses | 10-30 minutes | Single bacterium level | Moderate (3-5 targets) |
| Optical Biosensors | Viruses, Bacteria, Parasites | 5-15 minutes | ~100 CFU/mL | High (10+ targets) |
| Fluorescence Microscopy | Malaria parasites, Bacteria | 15-60 minutes | ~100 parasites/μL | Low (1-2 targets) |
| Digital Fluorescence Microscopy | Bloodborne pathogens | 10-20 minutes | Varies by pathogen | Moderate (2-4 targets) |
| Cherenkov Luminescence Imaging | Deep tissue infections | 30-60 minutes | N/A | Low |
The application of computer vision to read microscope slides significantly enhances accessibility in resource-limited settings where expert microbiologists may be scarce [38]. Similarly, portable fluorescence imaging systems enable rapid malaria diagnosis through hemozoin detection without the need for extensive laboratory infrastructure [42]. Advancements in optical biosensor technology have enabled detection of pathogen-specific biomarkers, including proteins, nucleic acids, and entire microbial cells, with sensitivity comparable to conventional culture methods but with dramatically reduced turnaround times.
Experimental Protocol: SERS-Based Pathogen Detection
Sample Preparation: Mix 10 μL of clinical sample (blood, urine, or saliva) with 90 μL of phosphate-buffered saline (PBS) and centrifuge at 5000 rpm for 5 minutes.
Substrate Preparation: Fabricate or acquire SERS-active substrate (silver or gold nanoparticles on silicon/silica).
Sample Loading: Apply 5-10 μL of processed sample to SERS substrate and allow to dry for 2-5 minutes under ambient conditions.
Spectral Acquisition: Position substrate under Raman microscope with 785 nm laser excitation at 10-50 mW power. Collect spectra with 1-5 second integration time.
Data Processing: Preprocess spectra with smoothing, baseline correction, and vector normalization.
Classification: Input processed spectra into machine learning classifier (e.g., support vector machine, random forest) trained on reference pathogen spectra.
Result Interpretation: Compare classification confidence scores against predetermined threshold (typically >85%) for pathogen identification.
Microsurgery
Optical technologies have revolutionized microsurgical procedures by enhancing visualization, enabling precise tissue differentiation, and facilitating real-time feedback. Fluorescence-guided surgery represents a particularly significant advancement, allowing surgeons to distinguish critical structures and pathological tissues with exceptional precision [4]. The integration of advanced optical systems with robotic surgical platforms has further enhanced surgical precision beyond human physical limitations.
Optical coherence tomography (OCT) provides cross-sectional tissue imaging at near-histological resolution, enabling real-time assessment of tissue layers during delicate procedures. This capability is particularly valuable in ophthalmic surgery, neurosurgery, and vascular procedures where millimeter-scale precision is critical [12]. Similarly, laser-based surgical systems enable extremely precise tissue ablation, cutting, and coagulation with minimal damage to surrounding healthy tissues.
The emerging field of optogenetics is creating unprecedented capabilities for precise control of cellular functions using light, opening new possibilities for targeted therapeutic interventions. While primarily in research stages, optogenetic approaches show promise for modulating neural circuits, controlling cardiac function, and regulating cellular signaling pathways with temporal and spatial precision unattainable with pharmaceutical interventions.
Experimental Protocol: Optical Phantom Validation for Surgical Systems
Phantom Design: Create tissue-mimicking phantoms with optical properties (absorption coefficient μa, reduced scattering coefficient μs') matching target tissues.
Material Preparation: Prepare base material (e.g., polydimethylsiloxane, polyurethane, or hydrogel) and incorporate titanium dioxide (scattering agent) and ink (absorbing agent) at precisely controlled concentrations.
Fluorescent Inclusion: Embed fluorescent targets (e.g., infrared dyes, quantum dots) with known concentrations to simulate labeled tumors or critical structures.
System Calibration: Calibrate fluorescence imaging system using phantoms with known optical properties and fluorophore concentrations.
Performance Metrics: Quantify system spatial resolution, sensitivity, uniformity, and linearity across expected dynamic range.
Clinical Validation: Compare phantom results with preclinical animal models and initial clinical experience to establish correlation.
Advanced Integrative Technologies
Artificial Intelligence and Machine Learning in Bio-Optics
The integration of artificial intelligence with bio-optical systems has created a paradigm shift in diagnostic and therapeutic capabilities. AI algorithms, particularly deep learning networks, can identify subtle patterns in optical data that may escape human detection [37]. In cancer diagnostics, AI-enhanced optical systems can automatically track tumor volumes over time, simultaneously monitor multiple lesions, and link phenotypic nuances to genotypes by comparing data with vast tumor databases [37].
Natural language processing (NLP), another AI specialization, bridges human language with machine interpretation, transforming unstructured data like clinical notes and diagnostic reports into discrete data elements [37]. This capability facilitates the construction of complex databases and tumor registries that recursively strengthen analytical models, enabling more precise correlations between optical findings and clinical outcomes.
The application of AI in fluorescence imaging and optical coherence tomography has significantly improved image reconstruction, interpretation, and even optical system design [4]. Machine learning approaches can reduce noise in optical signals, enhance resolution beyond physical limitations, and automatically classify tissues based on their optical signatures, providing real-time decision support to clinicians.
Wearable Bioelectronics and Point-of-Care Devices
Wearable bioelectronics represent a transformative development in bio-optics, enabling continuous physiological monitoring outside traditional clinical settings. These devices typically integrate optical sensors, electronic components, and wireless communication modules on flexible, biocompatible substrates [39]. Their inherently flexible, lightweight, and financially affordable nature provides better patient compliance while enabling painless, low-burden monitoring experiences.
Optical sensing modalities in wearable devices include photoplethysmography for cardiovascular monitoring, fluorescence-based chemical sensing, and reflectance spectroscopy for tissue oxygenation assessment [39]. These technologies are particularly valuable for cancer monitoring, where they can track dynamic biomarkers that reflect real-time biological changes in malignancies, providing a window into tumor dynamics and therapeutic response [39].
Point-of-care bio-optics technologies are revolutionizing healthcare delivery in resource-limited settings. Portable optical coherence tomography systems, handheld microscopes, and compact fluorescence imaging devices enable diagnostic capabilities previously restricted to centralized laboratories [38] [12]. The integration of these devices with telemedicine platforms further expands their impact, allowing remote imaging and consultation that enhances access to specialized healthcare services.
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Materials in Bio-Optics
| Category | Specific Examples | Research Applications | Key Functional Properties |
|---|---|---|---|
| Fluorescent Probes | Indocyanine green, FITC, Quantum dots, GFP | Tumor labeling, cellular imaging, vascular flow assessment | Excitation/emission spectra, quantum yield, photostability |
| Nanoparticles | Gold nanorods, Silica nanoparticles, Carbon dots | Contrast enhancement, targeted drug delivery, thermal therapy | Surface plasmon resonance, biocompatibility, surface functionalization |
| Optical Phantoms | PDMS-based phantoms, Polyurethane phantoms, Hydrogel phantoms | System calibration, performance validation, comparative studies | Tissue-mimicking optical properties, stability, reproducibility |
| Biosensors | Surface plasmon resonance chips, Optical fiber sensors, Photonic crystals | Biomarker detection, kinetic binding studies, continuous monitoring | Sensitivity, specificity, response time, regeneration capability |
| Contrast Agents | Methylene blue, Evans blue, Targeted molecular agents | Tissue demarcation, functional imaging, specific target visualization | Extinction coefficient, binding affinity, clearance profile |
Future Perspectives and Challenges
The future development of bio-optics faces several significant challenges that must be addressed to fully realize its potential. Regulatory hurdles and compliance requirements pose substantial constraints on the development and commercialization of bio-optics technologies [12]. The rigorous approval processes, which involve extensive testing, safety evaluations, and clinical trials, can be time-consuming and costly, potentially delaying market entry and innovation.
Technical challenges include the need for standardized validation methods and reference materials to ensure reliability and comparability across different platforms and institutions [41]. Issues of reproducibility and standardization are particularly relevant for quantitative optical techniques, where variations in instrumentation, protocols, and data analysis can significantly impact results.
Data security and patient privacy concerns emerge as bio-optics technologies increasingly incorporate digital connectivity and cloud-based data analysis [36]. Ensuring the security of sensitive medical optical data requires robust cybersecurity measures and compliance frameworks that balance accessibility with protection.
Despite these challenges, the future of bio-optics appears exceptionally promising. The continuous convergence with emerging fields such as nanotechnology, synthetic biology, and quantum optics is expected to yield new capabilities with profound implications for medicine and biology. The development of increasingly miniaturized and cost-effective systems will further expand access to advanced diagnostic and therapeutic options, ultimately democratizing precision medicine.
The integration of bio-optics with artificial intelligence will continue to advance, creating increasingly sophisticated systems capable of autonomous operation and complex decision-making. These developments will further blur the boundaries between diagnostic and therapeutic applications, enabling closed-loop systems that can detect pathological conditions and immediately initiate appropriate optical interventions, representing the ultimate realization of bio-optics as a transformative force in medicine.
Optical biosensors have emerged as a transformative class of point-of-care diagnostic (POCD) devices, offering sensitive, specific, and rapid detection of diseases [43]. These analytical devices combine a biological sensing element with an optical transducer to detect and quantify specific analytes, producing easy-to-read, real-time signals such as color changes or light emission [44]. The significance of these sensors in modern healthcare stems from their ability to provide rapid diagnostic results at or near the patient's location, enabling immediate clinical decision-making that can significantly enhance patient outcomes [45]. This technological approach addresses critical limitations of traditional laboratory-based diagnostics, which often involve lengthy turnaround times that can delay treatment initiation [45].
The fundamental architecture of a biosensor comprises three key components: a bioreceptor to sense specific biological interactions, a transducer that converts this recognition into a measurable signal, and a signal processor that outputs the detectable reading [46] [44]. Optical biosensors specifically utilize optical transduction mechanisms, exploiting light-molecule interactions to generate signals corresponding to analyte concentration [44]. Their advantages include high specificity and sensitivity, miniaturization capability for portable devices, cost-effectiveness, and in many cases, label-free and real-time detection capabilities [46] [45]. The non-invasive nature of many optical detection methods further enhances patient comfort and safety, making them particularly suitable for repeated monitoring and point-of-care applications [44].
Classification and Working Principles of Optical Biosensors
Optical biosensing technologies employ diverse physical phenomena based on fundamental light emission or light-matter interactions [46]. The following section provides a technical overview of the predominant optical biosensor types being developed for point-of-care applications.
Fluorescence-Based Biosensors
Fluorescence biosensors operate on the principle that electromagnetic radiation is absorbed by fluorophores or fluorescently labeled molecules, causing energy conversion into fluorescence emission [46] [47]. These systems typically include an excitation light source (LEDs or lasers), fluorophore molecules labeling target biomolecules, and a photodetector that records fluorescence intensity and spectrum [47]. Advanced fluorescence techniques include Förster resonance energy transfer (FRET), fluorescence lifetime imaging (FLIM), fluorescence correlation spectroscopy (FCS), and monitoring changes in fluorescence intensity [46] [47]. Fluorescence-based biosensors offer exceptionally high sensitivity, with detection limits often reaching nanomolar to picomolar concentrations, making them suitable for detecting low-abundance biomarkers [48].
Surface-Enhanced Raman Scattering (SERS) Biosensors
SERS biosensors exploit the enhancement of normally weak Raman scattering when analyte molecules adsorb onto specially prepared metal surfaces [46] [47]. This enhancement arises through two primary mechanisms: an electromagnetic enhancement from localized surface plasmon resonance (LSPR) in noble metal nanoparticles, and a chemical enhancement involving charge transfer between analyte molecules and the metal surface [47]. The electromagnetic mechanism typically contributes significantly more to signal enhancement, with factors reaching 10⁶-10⁸ compared to normal Raman scattering [47]. SERS provides molecular fingerprint information, enabling highly specific identification of analytes, and has recently evolved from single-point detection to multiplexed bioimaging applications using SERS tags [47].
Photonic Crystal (PC) and Guided Mode Resonance (GMR) Biosensors
Photonic crystal biosensors utilize periodic dielectric structures that create optical resonant modes or photonic bandgaps sensitive to refractive index changes on their surfaces [46] [47]. These sensors feature extremely narrow bandwidths (<1 nm) and high reflectivity (≈95-100%), enabling detection of small molecules, virus particles, DNA microarrays, and live cells [47]. Guided Mode Resonance (GMR) biosensors operate on a similar principle, where resonant modes are excited in an optical waveguide layer coupled with a diffraction element [47]. The resulting resonance peaks exhibit high sensitivity to surrounding refractive index changes, with recent demonstrations achieving phase shift detection corresponding to refractive index changes as small as 3.43 × 10⁻⁷ [47].
Plasmon-Based Biosensors
Surface Plasmon Resonance (SPR) biosensors and Localized Surface Plasmon Resonance (LSPR) biosensors utilize the resonant oscillation of conduction electrons at metal-dielectric interfaces when excited by incident light [46] [47]. SPR occurs on continuous metallic films and typically requires prism couplers, while LSPR utilizes metallic nanoparticles and can be directly excited by light [47]. These label-free techniques enable real-time monitoring of biomolecular interactions, with SPR providing exceptional sensitivity for binding kinetics studies and LSPR offering simpler instrumentation suitable for point-of-care applications [45] [48]. The confined electromagnetic fields near metal surfaces significantly enhance sensitivity by strengthening light-molecule interactions [47].
Table 1: Comparative Analysis of Optical Biosensing Technologies
| Technology | Detection Principle | Sensitivity | Multiplexing Capability | Key Advantages |
|---|---|---|---|---|
| Fluorescence | Light emission from excited fluorophores | High (nanomolar to picomolar) | Moderate to High | Extremely sensitive, multiple parameters via different fluorophores |
| SERS | Enhanced Raman scattering at metal surfaces | Very High (single molecule possible) | High | Molecular fingerprinting, minimal sample preparation |
| SPR/LSPR | Refractive index change at metal interface | High (picogram levels) | Moderate | Label-free, real-time kinetics monitoring |
| Photonic Crystal | Resonance shift from refractive index change | High | Moderate to High | Label-free, high Q-factor, scalable fabrication |
| GMR | Guided mode resonance in waveguide structures | Very High (Δn ~10⁻⁷) | Moderate | Extreme sensitivity, compact size |
Advanced Materials and Integration Platforms
The performance of optical biosensors is intrinsically linked to the materials employed in their fabrication [45]. Recent advancements have focused on developing novel nanomaterials and integration strategies to enhance sensitivity, specificity, and point-of-care applicability.
Functional Materials for Enhanced Biosensing
Plasmonic nanomaterials including gold and silver nanoparticles, nanostars, and nanorods enable ultra-sensitive detection through enhanced electromagnetic fields [45]. These materials functionalized with specific biorecognition elements can detect viruses, toxins, drugs, antibodies, and tumor markers at clinically relevant concentrations [45]. Photonic crystals with precisely engineered periodic structures manipulate light at the nanoscale, creating highly sensitive and selective detection environments [45]. Quantum dots and two-dimensional nanomaterials such as graphene and transition metal dichalcogenides provide exceptional fluorescence properties and high surface-to-volume ratios for biomarker detection [45]. Additionally, surface functionalization techniques utilizing self-assembled monolayers (SAMs) and biocompatible polymers create stable and selective sensing interfaces that maintain biorecognition element functionality [45].
Microfluidic Integration and Lab-on-a-Chip Platforms
Integration with microfluidic channels represents a critical advancement for point-care optical biosensors [46] [47]. These lab-on-a-chip platforms combine several laboratory functions into a single device, enabling fluid handling, sample preparation, and detection on a miniature scale [47]. Microfluidic integration provides multiple advantages including reduced sample and reagent volumes, faster analysis times due to shortened diffusion paths, higher accuracy and sensitivity through simultaneous multi-parameter monitoring, and automation of complex assay procedures [46] [47]. Furthermore, microfluidic systems can incorporate additional functionalities such as electrical control and signal readout monolithically in a single semiconductor chip, making them ideal for point-of-care testing [47].
Portable Form Factors and Wearable Biosensors
The miniaturization of optical components has enabled the development of portable handheld readers and smartphone-based biosensing platforms that bring laboratory-quality detection to point-of-care settings [45] [48]. These systems leverage the computational power, imaging capabilities, and connectivity of smartphones to provide quantitative results in resource-limited environments [48]. Emerging wearable optical biosensors offer continuous, non-invasive monitoring of physiological parameters and biomarkers through skin-interfaced platforms [45]. These devices typically employ flexible substrates and low-power optical sources to enable long-term health monitoring, creating new opportunities for personalized medicine and remote patient monitoring [45].
Experimental Methodologies and Protocols
The development and implementation of optical biosensors for point-of-care applications require standardized methodologies to ensure reliability, reproducibility, and clinical validity.
Sensor Fabrication and Functionalization
Substrate preparation begins with thorough cleaning of transducer surfaces (e.g., glass, silicon, or plastic) using oxygen plasma or piranha solution to remove organic contaminants and enhance hydrophilicity [45]. For plasmonic sensors, metal film deposition (typically 50nm gold) employs electron-beam evaporation or sputtering with a chromium or titanium adhesion layer (2-5nm) [45] [47]. Nanostructure fabrication utilizes bottom-up chemical synthesis of nanoparticles or top-down approaches including nanoimprint lithography and electron-beam lithography for precise pattern definition [45]. Surface functionalization involves creating self-assembled monolayers (SAMs) of alkanethiols on gold surfaces or silanization on oxide surfaces, followed by immobilization of biorecognition elements (antibodies, aptamers, enzymes) via EDC-NHS chemistry or other covalent coupling strategies [45]. Quality control at each stage employs characterization techniques such as atomic force microscopy, scanning electron microscopy, and spectroscopic ellipsometry to verify surface morphology, film thickness, and functional group presence [45].
Assay Implementation and Signal Detection
Sample introduction typically employs microfluidic systems with controlled flow rates (1-100 μL/min) to deliver analyte solutions to the sensing region while minimizing non-specific binding [45]. For label-free detection platforms, baseline establishment occurs with a running buffer solution before analyte injection, monitoring the stable signal reference [47]. Specific binding measurement records signal changes (wavelength shift, intensity change, or phase difference) during analyte injection over 5-15 minutes, followed by buffer washing to remove unbound molecules [47]. For labeled assays, incubation and washing steps follow specific time sequences (typically 10-30 minutes incubation) with precise wash buffers to remove unbound labels while retaining specific complexes [48]. Signal acquisition utilizes appropriate optical components (LEDs/lasers for excitation, spectrometers/cameras for detection) with optimized integration times and signal-to-noise enhancement strategies such as lock-in amplification or spectral averaging [45] [48].
Diagram 1: Operational workflow of optical biosensors showing key stages from sample introduction to data output
Data Analysis and Validation Protocols
Signal processing employs digital filtering (Savitzky-Golay, wavelet transform) to reduce noise while preserving meaningful signal components [43]. Quantitative analysis utilizes calibration curves generated from standard solutions with known analyte concentrations, typically spanning 3-5 orders of magnitude to establish dynamic range [45]. For multiplexed detection, signal deconvolution algorithms separate overlapping signals from different detection zones or spectral signatures [43]. Validation procedures include assessment of limit of detection (LOD) calculated as 3×standard deviation of blank signals divided by the calibration curve slope, and limit of quantification (LOQ) calculated as 10×standard deviation of blank signals [45]. Cross-reactivity evaluation tests structurally similar compounds to establish assay specificity, while recovery studies (80-120% recovery) validate accuracy in complex matrices like serum or whole blood [45]. Quality control incorporates internal standards and control samples in each assay run to monitor performance and reproducibility [45].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and implementation of optical biosensors require carefully selected reagents and materials optimized for specific sensing platforms and applications.
Table 2: Essential Research Reagents and Materials for Optical Biosensor Development
| Category | Specific Examples | Function and Application |
|---|---|---|
| Biorecognition Elements | Antibodies, aptamers, enzymes, DNAzymes, molecularly imprinted polymers | Target capture and specificity; antibodies provide high affinity, aptamers offer stability |
| Plasmonic Materials | Gold and silver nanoparticles, nanorods, nanostars | Signal enhancement via localized surface plasmon resonance |
| Fluorescent Labels | Quantum dots, organic dyes, fluorescent proteins, upconversion nanoparticles | Signal generation; quantum dots offer brightness and photostability |
| Substrate Materials | Glass, silicon, PDMS, PMMA, nitrocellulose | Sensor platform; PDMS for microfluidics, nitrocellulose for lateral flow assays |
| Surface Chemistry Reagents | SAMs (alkanethiols, silanes), EDC/NHS, biotin-streptavidin | Immobilization of biorecognition elements; EDC/NHS for covalent bonding |
| Signal Amplification Systems | Enzyme-polymers, metal-enhanced fluorescence, catalytic nanomaterials | Enhanced sensitivity; enzyme-polymers for catalytic signal amplification |
Emerging Trends and Future Research Directions
The field of optical biosensors for point-of-care applications is rapidly evolving, driven by several transformative technological trends that promise to enhance capabilities and expand applications.
Artificial Intelligence and Machine Learning Integration
The integration of AI algorithms, particularly machine learning and deep learning, is revolutionizing optical biosensing by enabling enhanced analytical performance through intelligent signal processing, pattern recognition, and automated decision-making [43]. These approaches significantly improve signal-to-noise ratios, enable accurate classification of complex spectral data, and facilitate multivariate analysis of multiplexed detection platforms [43]. AI-enhanced biosensors can automatically compensate for environmental variations, identify subtle pattern changes indicative of specific diseases, and provide real-time diagnostic interpretations without expert intervention [43] [4]. The combination of AI with optical biosensors is particularly powerful for processing high-dimensional data from imaging-based biosensors and extracting meaningful biological information from complex samples [4].
Internet of Things (IoT) and Cloud Connectivity
The convergence of optical biosensors with Internet of Things (IoT) technologies and cloud computing enables decentralized healthcare monitoring and real-time data sharing with healthcare providers [43]. Connected biosensing platforms facilitate continuous remote patient monitoring, automated data logging, and centralized analysis of population health trends [43] [49]. These systems typically feature wireless communication capabilities (Bluetooth, Wi-Fi, or cellular) that transmit sensor data to cloud-based analytics platforms for specialized processing, long-term storage, and healthcare system integration [43]. This connectivity framework supports the development of comprehensive digital health ecosystems where point-of-care diagnostic data directly informs clinical decision-making and therapeutic interventions [49].
Multiplexed Detection and Personalized Medicine
Advanced optical biosensors increasingly incorporate multiplexing capabilities that simultaneously detect multiple biomarkers in a single assay [45]. This parallel analysis provides comprehensive diagnostic information that enables more accurate disease stratification, treatment selection, and therapeutic monitoring [45]. Multiplexed biosensing platforms are particularly valuable for infectious disease differentiation, cancer biomarker panels, and chronic disease management where multiple parameters must be tracked over time [45]. The trend toward personalized medicine leverages these multiplexed biosensors to generate individual biomarker profiles that guide tailored therapeutic interventions based on unique patient physiology and disease characteristics [45].
Diagram 2: Emerging technology trends in optical biosensors and their impact on healthcare delivery
Challenges and Implementation Considerations
Despite significant advancements, several technical and practical challenges must be addressed to fully realize the potential of optical biosensors in point-of-care diagnostics.
Technical and Clinical Validation Challenges
A primary obstacle involves miniaturization without performance compromise, particularly maintaining sensitivity and signal-to-noise ratios in compact, portable formats [45]. Integration complexity presents another significant challenge, as combining optical components, fluidic systems, and electronic controls into a seamless, robust platform requires sophisticated engineering solutions [43]. Sample matrix effects from complex biological fluids (blood, saliva, urine) can interfere with optical measurements through autofluorescence, light scattering, or non-specific binding, necessitating effective sample preparation methodologies [45]. Additionally, clinical validation demands extensive testing across diverse patient populations to establish diagnostic accuracy, clinical sensitivity, specificity, and reproducibility that meet regulatory standards [43] [45]. These validation studies must demonstrate performance comparable to established laboratory methods while operating in more variable point-of-care environments [45].
Regulatory and Commercialization Hurdles
The path to commercialization for optical point-of-care biosensors involves navigating regulatory approval processes that vary across geographic regions but generally require rigorous demonstration of safety, efficacy, and manufacturing quality [45]. Manufacturing scalability must be addressed to transition from laboratory prototypes to mass-produced devices with consistent performance characteristics, often requiring adaptation of fabrication methods for high-volume production [45]. Cost-effectiveness remains crucial for widespread adoption, particularly in resource-limited settings, necessitating careful balance between performance and affordability [45]. Additionally, data privacy and security concerns emerge with connected biosensing platforms that handle sensitive health information, requiring robust cybersecurity measures and compliance with health data protection regulations [43]. Successful commercialization strategies must address this complex interplay of technical, regulatory, and economic factors to deliver viable diagnostic solutions to healthcare markets [45].
Optical biosensors represent a rapidly advancing field with transformative potential for point-of-care diagnostics. These technologies offer sophisticated solutions for rapid, sensitive, and specific detection of clinically relevant biomarkers in formats suitable for decentralized healthcare settings. Current research focuses on enhancing performance through novel materials, integration with microfluidics, implementation of artificial intelligence, and development of connected health platforms. While significant challenges remain in standardization, validation, and commercialization, the continuing convergence of optical engineering, nanotechnology, biotechnology, and data science promises to address these limitations and expand the capabilities of point-of-care diagnostic systems. The ongoing evolution of optical biosensors is poised to dramatically impact healthcare delivery by enabling earlier disease detection, personalized treatment approaches, and improved health monitoring outcomes across diverse clinical and community settings.
Overcoming Design and Implementation Challenges in Bio-Optic Systems
The field of bio-optics, which involves the application of light-based technologies to biological and medical challenges, is fundamentally constrained by three interdependent technical limitations: spatial resolution, penetration depth, and acquisition speed. These parameters are locked in a delicate balance; optimizing one often comes at the expense of another. For instance, achieving high spatial resolution typically requires high-numerical-aperture optics, which severely limits the field of view and penetration depth due to light scattering in biological tissues. Conversely, techniques that image deep within tissue often sacrifice resolution and speed. Similarly, increasing imaging speed can compromise signal-to-noise ratio and resolution. For researchers and drug development professionals, navigating these trade-offs is a central challenge in experimental design. This whitepaper, framed within a broader thesis on bio-optics design and application, provides a comprehensive analysis of these core limitations. It explores the fundamental physical constraints, surveys current advanced technological solutions that push these boundaries, and details specific experimental methodologies. The objective is to equip practitioners with the knowledge to select appropriate modalities and implement protocols that best address their specific research requirements, from fundamental cellular studies to in vivo preclinical applications.
Fundamental Trade-offs and Physical Limits
The performance of any bio-optical imaging system is governed by the fundamental physics of light-matter interaction. A deep understanding of these underlying principles is essential for making informed decisions about system design and application.
The Trilemma of Optical Imaging
The core challenge in bio-optics is often described as a trilemma between resolution, depth, and speed. Spatial resolution defines the smallest distinguishable detail in an image and is fundamentally limited by the diffraction of light, as described by Abbe's limit. In practice, for standard diffraction-limited microscopy, this translates to a lateral resolution of approximately 200-300 nm. Penetration depth is limited by the scattering and absorption of light by biological tissues. Scattering events deflect photons from their original path, blurring the image and reducing signal intensity as depth increases. Absorption by molecules like hemoglobin and water converts light energy to heat, further attenuating the signal. The effective penetration depth is the point at which the signal-to-noise ratio becomes too low for useful image formation. Acquisition speed is constrained by the need to collect sufficient photons to form an image with adequate contrast and the mechanical or electronic scanning limitations of the system. In vivo functional imaging presents a particularly stringent requirement for speed, as it must capture dynamic physiological processes, such as blood flow or neural activity, on millisecond timescales.
Table 1: Fundamental Limits and Their Impact on Bio-optical Imaging
| Technical Parameter | Fundamental Physical Limit | Primary Constraining Factors in Biology | Typical Range in Conventional Systems |
|---|---|---|---|
| Spatial Resolution | Diffraction Limit (~λ/2NA) | Numerical Aperture (NA) of objective, optical aberrations, scattering | 200 nm - 1 µm (lateral) |
| Penetration Depth | Light Transport Mean Free Path (lt') | Tissue scattering (µs) & absorption (µa) coefficients, wavelength | 0.5 - 1 mm (in scattering tissue) |
| Acquisition Speed | Signal-to-Noise Ratio (SNR) & Scanning Mechanism | Laser power (photobleaching/phototoxicity), detector sensitivity, scanning mechanism | Milliseconds to seconds per frame |
Visualizing the Core Technical Trade-off
The following diagram illustrates the fundamental and often competing relationships between the three core technical parameters in bio-optics. No single modality can simultaneously maximize all three; technological choices inevitably involve prioritizing certain parameters over others.
Figure 1: The Core Technical Trilemma in Bio-optics. Achieving high performance in one parameter often negatively impacts the others, creating a fundamental design challenge.
Advanced Solutions and Modality Comparisons
Innovative optical techniques have been developed to circumvent these classical limitations. The following section details state-of-the-art technologies, highlighting how they redefine the possible combinations of resolution, depth, and speed.
Overcoming the Penetration Depth Barrier
Several modalities have made significant strides in imaging deeper into scattering biological tissues.
Photoacoustic Imaging (PAI) is a hybrid modality that elegantly bypasses the optical scattering limit. It leverages the photoacoustic effect, where pulsed laser light is absorbed by chromophores (e.g., hemoglobin, melanin), generating a transient thermoelastic expansion that emits ultrasonic waves. Since ultrasound scatters ~1000 times less than light in tissue, these waves can be detected at depth to form an image with optical absorption contrast but ultrasonic resolution [50]. PAI systems are categorized as:
- Optical-Resolution PAM (OR-PAM): Uses a tightly focused optical beam, providing high lateral resolution (~λ, sub-micron) but limited to depths of about 1 mm [50].
- Acoustic-Resolution PAM (AR-PAM): Relies on acoustic focusing, allowing deeper imaging (up to several cm) beyond the optical diffusion limit, albeit with lower resolution [50].
- Photoacoustic Computed Tomography (PACT): Uses unfocused light and an array of ultrasonic detectors to reconstruct images from multiple angles, enabling deep-tissue imaging with a large field of view [50].
Multi-photon Microscopy (MPM), primarily two-photon excitation, uses near-infrared (NIR) pulsed lasers to nonlinearly excite fluorescence only at the focal point. The use of longer, less-scattering wavelengths and the confined excitation volume significantly enhance penetration depth (up to 1 mm in brain tissue) and reduce out-of-focus photobleaching. An integrated system combining optoacoustic microscopy and two-photon microscopy has demonstrated visualization of capillaries with submicron resolution to 140 µm depth and neurons beyond 300 µm depth, providing complementary neurovascular information [23].
Mesoscale Imaging techniques aim to bridge the gap between cellular and organ-level investigations. They strive to achieve a high space-bandwidth product—a large field of view while maintaining high resolution—though they must constantly balance this against scattering, aberrations, phototoxicity, and acquisition speed [51].
Pushing the Boundaries of Spatial Resolution
While diffraction poses a hard limit for classical optics, several methods have been developed to achieve super-resolution.
Stimulated Emission Depletion (STED) microscopy is a deterministic super-resolution technique that uses a donut-shaped depletion beam to de-excite fluorophores at the periphery of the excitation focus, effectively reducing the point-spread function to a sub-diffraction region.
Quantum Imaging techniques exploit non-classical properties of light to enhance imaging capabilities. For example, Quantum Optical Coherence Tomography (QOCT) uses entangled photon pairs to provide superior axial resolution and dispersion cancellation compared to classical OCT, effectively doubling the resolution [52]. N00N state-based imaging utilizes quantum entanglement to achieve super-resolved interference fringes, enabling phase sensitivity and resolution beyond the classical diffraction limit [52].
Enhancing Acquisition Speed for Functional Imaging
Capturing fast biological dynamics requires exceptionally high imaging speeds.
Compressed Sensing and Computational Imaging methods break the link between data acquisition and image formation. By leveraging prior knowledge about image sparsity, these techniques can reconstruct images from highly undersampled data, drastically reducing the number of measurements needed and thus increasing acquisition speed.
Wide-field Imaging Techniques such as light-sheet fluorescence microscopy (LSFM) illuminate only a thin plane within the specimen, enabling rapid acquisition of an entire 2D plane without scanning. This dramatically increases volumetric acquisition speed while reducing light dose.
Advanced Camera Technologies are also pivotal. The development of cameras with ultra-high frame rates, such as those capable of trillions of frames per second, enables the capture of previously unobservable ultrafast phenomena like light propagation [53].
Table 2: Performance Comparison of Advanced Bio-optical Imaging Modalities
| Imaging Modality | Mechanism of Contrast | Max Lateral Resolution | Max Penetration Depth | Key Advantage | Primary Limitation |
|---|---|---|---|---|---|
| Two-Photon Microscopy (TPM) [23] | Nonlinear Fluorescence | ~400 nm | ~1 mm (in mouse cortex) | Deep tissue, cellular resolution | Requires exogenous labels (typically) |
| Optical-Resolution PAM (OR-PAM) [50] | Optical Absorption | ~670 nm | ~1.2 mm | Label-free hemodynamic imaging | Limited to superficial structures |
| Acoustic-Resolution PAM (AR-PAM) [50] | Optical Absorption | Tens of µm | Several cm | Deep tissue with optical contrast | Lower resolution than OR-PAM |
| Integrated OAM/TPM [23] | Absorption & Fluorescence | OAM: ~670 nm | OAM: 140 µm (capillaries) | Multimodal, co-registered data | System complexity |
| TPM: ~400 nm | TPM: >300 µm (neurons) | ||||
| Quantum OCT (QOCT) [52] | Quantum Interference | 2x Classical OCT | Similar to OCT | Dispersion cancellation, enhanced resolution | Technically complex, low light |
Detailed Experimental Protocol: Integrated OAM and TPM
To illustrate how these technologies are implemented in practice, this section details a specific experimental protocol for dual-modal functional neuroimaging, as described in a recent study [23]. This protocol showcases the practical considerations for achieving high resolution, sufficient depth, and adequate speed for studying neurovascular coupling.
System Configuration and Workflow
The integrated system combines optical-resolution optoacoustic microscopy (OAM) and two-photon microscopy (TPM) for in vivo imaging of the mouse cortex. The system utilizes two separate laser sources: a nanosecond-pulsed laser for OAM and a femtosecond-pulsed laser for TPM. The beams are combined and directed to a shared objective lens. A custom data acquisition system (e.g., using LabVIEW) controls the laser triggering, scanning mirrors, and data recording. A critical feature is the semi-simultaneous acquisition protocol, where the system alternates between acquiring OAM and TPM frames at the same focal plane before moving to the next Z-plane. This minimizes temporal discrepancies and motion artifacts, ensuring robust spatiotemporal co-registration of the multimodal datasets [23].
Figure 2: Experimental Workflow for Integrated OAM and TPM Neuroimaging. This protocol ensures spatially and temporally aligned multimodal data acquisition for studying neurovascular coupling.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs the key reagents and materials required to execute the integrated OAM/TPM experiment described above.
Table 3: Essential Research Reagents and Materials for Integrated OAM/TPM Neuroimaging
| Item Name | Specifications / Example | Critical Function in the Experiment |
|---|---|---|
| Nanosecond Pulsed Laser | Wavelength: 532 nm, Pulse duration: ns | Generates photoacoustic waves in OAM by exciting optical absorption in hemoglobin. |
| Femtosecond Pulsed Laser | Wavelength: 920 nm, Pulse duration: fs | Enables two-photon excitation of fluorescent labels in TPM. |
| High-NA Objective Lens | e.g., 20x, Water Immersion | Focuses excitation light and collects emitted signals for both modalities. |
| Ultrasonic Detector | High-frequency, single-element | Detects photoacoustic waves generated in the OAM modality. |
| Photomultiplier Tube (PMT) | High-sensitivity, GaAsP preferred | Detects faint fluorescence photons emitted in the TPM modality. |
| Adeno-Associated Virus (AAV) | e.g., AAV-hSyn-GCaMP | Genetically encodes fluorescent indicators in neurons for TPM visualization. |
| Medical Ultrasonic Gel | Acoustically transparent, optically clear | Couples ultrasound waves between sample and detector for OAM. |
| Head Plate & Dental Cement | Custom-designed, titanium | Provides stable head fixation for in vivo mouse brain imaging, reducing motion. |
The field of bio-optics continues to evolve rapidly, with several emerging technologies poised to further redefine the limits of resolution, depth, and speed. Quantum imaging is emerging as a transformative approach, applying nonclassical properties of light such as entanglement and squeezing to overcome fundamental limits of classical techniques. These methods promise superior spatial resolution, enhanced signal-to-noise ratios, and reduced radiation dose for potentially safer and more precise imaging of delicate biological samples [52]. The integration of artificial intelligence (AI) and machine learning is another powerful trend. AI is not only accelerating data processing and image analysis but is also being used for hardware control, image reconstruction in undersampled data, and even the prediction of optimal imaging parameters [10] [49]. Finally, the drive for miniaturization and wearability is pushing the development of compact, robust optical systems for decentralized and continuous health monitoring, moving bio-optical tools from the laboratory into clinical and point-of-care settings [49].
In conclusion, the technical limitations of resolution, penetration depth, and acquisition speed remain central challenges in bio-optics. However, as detailed in this whitepaper, a rich and evolving toolkit of advanced modalities—from photoacoustic and multi-photon imaging to quantum and computational techniques—provides powerful strategies to navigate these trade-offs. The successful application of these technologies, as demonstrated in the detailed experimental protocol for neuroimaging, hinges on a deep understanding of their underlying principles and a careful, purpose-driven design. For researchers and drug development professionals, staying abreast of these advancements is crucial for leveraging the full potential of optical methods to drive discovery and translate innovation into practice.
Navigating Regulatory Hurdles and Compliance for Clinical Translation
The successful translation of bio-optical technologies from the laboratory to the clinic is a critical pathway for advancing modern healthcare. Bio-optics—which encompasses the design and application of optical technologies for biology and medicine—is a rapidly evolving field. Conferences like Bio-Optics: Design and Application (BODA) highlight cutting-edge developments, from novel biomedical optical technology and ophthalmic imaging to instruments and systems for clinical imaging [4]. These technologies, which include everything from complex imaging systems to patient-used diagnostic devices, must navigate a complex global regulatory landscape to achieve clinical adoption and market access. This guide provides researchers and drug development professionals with a detailed framework for overcoming the primary regulatory and compliance hurdles in the clinical translation of bio-optical technologies, ensuring patient safety, data integrity, and successful market entry.
Foundational Regulatory Frameworks
Navigating the regulatory environment requires a solid understanding of the major global regulations and the specific linguistic demands they impose on clinical evidence and documentation.
Global Regulatory Bodies and Key Regulations
| Regulatory Body/Regulation | Region | Core Focus for Clinical Translation | Key Document Requirements |
|---|---|---|---|
| European Medical Device Regulation (MDR) [54] | European Union | Safety, performance, post-market monitoring, traceability | Instructions for Use (IFUs), Summary of Safety and Clinical Performance (SSCP), Technical Documentation |
| EU Clinical Trials Regulation (EU CTR) [55] | European Union | Harmonized submission & transparency for clinical trials | Clinical Trial Application (CTA) documents, patient-facing materials via Clinical Trials Information System (CTIS) |
| U.S. Food and Drug Administration (FDA) [55] | United States | Safety, efficacy, and data integrity for submissions | Investigational Device Exemption (IDE), Pre-market Approval (PMA), 510(k), clinical study reports |
| ICH Good Clinical Practice (GCP) E6(R3) [56] | International | Ethical & scientific quality in trial design/conduct/data reporting | Clinical trial protocols, Informed Consent Forms (ICFs), SOPs, ensuring patient comprehension |
The Critical Role of Language and Translation
Regulatory compliance is intrinsically linked to clear, accurate, and accessible language. Key concepts include:
- Meaningful Access: A legal standard under ACA Section 1557 in the U.S., requiring healthcare providers to take reasonable steps to ensure Limited English Proficiency (LEP) patients receive language assistance, making it a crucial consideration for patient-facing technologies and clinical trials [57].
- Linguistic Validation: A formal methodology for ensuring translated patient-facing materials (e.g., Informed Consent Forms, patient-reported outcome questionnaires) are conceptually equivalent and comprehensible to the target population. This process often involves forward translation, back-translation, reconciliation, and cognitive debriefing [55].
- Qualified Personnel: Regulations explicitly forbid relying on untrained bilingual staff, family members, or unverified machine translation for critical documents. Work must be performed by translators and interpreters who are fluent in medical terminology and adhere to confidentiality standards [57].
Key Compliance Requirements and Methodologies
Essential Documents Requiring translation
Virtually every component of a clinical trial and device submission requires meticulous translation [55]:
- Informed Consent Forms (ICFs) & eConsent interfaces
- Patient-Reported Outcome (PRO) questionnaires
- Investigator's Brochure and Clinical Trial Protocols
- Instructions for Use (IFUs) for medical devices [54]
- Adverse event reporting instructions
- Regulatory submission documents for agencies like the FDA and EMA
- Recruitment materials and site training materials
Seven Vital Translation Requirements
The following requirements are critical for maintaining compliance, data integrity, and patient safety [55].
- Engage Qualified Medical Translators: Use translators with demonstrable experience in clinical terminology and trial documents. Partnering with a Language Service Provider (LSP) certified to standards like ISO 17100 and ISO 13485 (for medical devices) ensures adherence to quality management systems [54] [55].
- Maintain Clear Source-Language Control: Designate a single approved master document for all translations. Maintain a detailed change log to ensure traceability and prevent conflicting versions across clinical sites, which can cause significant regulatory issues during inspections [55].
- Implement Linguistic Validation & Cognitive Debriefing: For ICFs and PROs, perform formal linguistic validation. This multi-step process tests participant comprehension to ensure scores and consent are meaningful and comparable across different populations [55].
- Execute Cultural Adaptation: Adjust idioms, examples, units, and culturally sensitive references rather than translating literally. This reduces confusion, improves recruitment and retention, and ensures questions measure the same scientific construct in different cultures [55].
- Adhere to Regulatory & Ethics Compliance: Identify regional regulatory and ethics committee (IRB/EC) rules early. Some jurisdictions require specific documents to be translated for submission, and these must be integrated into project timelines to avoid delays in site activation [55].
- Conduct Independent Linguistic Review: Utilize back-translation or two independent linguistic reviews to identify subtle shifts in meaning for critical materials like ePRO items or key regulatory text [55].
- Ensure Quality Assurance and Audit Trail: Implement robust QA steps, including bilingual editing and final reviewer sign-off. Maintain auditable records of all translators, reviewer comments, version histories, and approval dates to demonstrate compliance during regulatory audits [55].
Experimental and Validation Protocols
Protocol 1: Linguistic Validation for Patient-Reported Outcome (PRO) Measures
- Objective: To ensure a PRO instrument is conceptually equivalent across different languages and cultures, thereby guaranteeing the validity of collected data.
- Methodology:
- Forward Translation: Two independent, qualified translators produce initial target language versions.
- Reconciliation: A third translator or reviewer compares the two versions to create a single reconciled translation.
- Back-Translation: A blind translator, unfamiliar with the original source, translates the reconciled version back into the source language.
- Review and Harmonization: An expert committee (clinicians, linguists, the translators) reviews the back-translation against the original, identifies discrepancies, and finalizes the translation.
- Cognitive Debriefing: The finalized translation is tested with a sample of the target population (typically 5-10 participants). Participants are interviewed to assess their understanding of each item and response option.
- Finalization: Based on cognitive debriefing feedback, the translation is finalized and proofread [55].
Protocol 2: Change Management for Updated Instructions for Use (IFUs)
- Objective: To ensure all language versions of an IFU are synchronized promptly after a change to the source document, as required by MDR [54].
- Methodology:
- Change Trigger: A change is made to the source IFU (e.g., updated safety information).
- Impact Assessment: Determine which language versions are affected.
- Translation Update: The updated text is sent to qualified translators working with a Translation Memory (TM) system to ensure consistency with previous translations.
- Quality Assurance: The updated translation undergoes bilingual review and technical verification.
- Regulatory Review & Approval: The updated translation is submitted for internal approval and, if necessary, to a Notified Body.
- Controlled Deployment: The new IFU is distributed according to a controlled plan, and obsolete versions are recalled from the field [54].
Implementation Strategies and Technology Solutions
Integrating Translation into the Quality Management System (QMS)
Treating translation as an afterthought is a common pitfall. MDR mandates traceability, quality control, and documentation management as integral parts of the product lifecycle. Therefore, translation processes must be embedded within your QMS. Disconnected workflows risk outdated content, loss of version control, and missed regulatory reviews [54]. Systematically track version updates, approvals, and language coverage within your QMS framework.
A Risk-Based Approach to Technology and AI
Artificial Intelligence (AI) and Machine Translation (MT) can streamline workflows but require careful validation.
- AI-Assisted Translation under MDR: MDR does not prohibit AI-assisted translations, but the manufacturer remains legally responsible for the final product's accuracy and compliance. Sole reliance on AI without human oversight is high-risk [54].
- Hybrid Workflow: A compliant strategy uses AI for initial drafts or quality checks (e.g., verifying the inclusion of MDR-required elements) but mandates rigorous Human Post-Editing (HPE) by a qualified medical translator for all critical documents [54]. This is also mandated by ACA Section 1557 for vital healthcare content [57].
- Technology Tools: The following table compares solutions used in GCP-compliant translation workflows [58].
Research Reagent Solutions: GCP Translation Tools
| Tool / Solution Type | Primary Function | Key Considerations for Clinical Translation |
|---|---|---|
| Specialized AI Platforms (e.g., X-doc.ai) [58] | AI-driven translation tailored for clinical/regulatory documents. | High accuracy (e.g., 99% claimed); built for GCP; enterprise security (SOC 2, ISO 27001). Ideal for protocols, ICFs, submissions. |
| Computer-Assisted Translation (CAT) Tools (e.g., SDL Trados Studio, Smartcat) [58] | Workbench for human translators with Translation Memory (TM) & Terminology Management. | Ensures consistency via TM; essential for enforcing approved terminology; quality is dependent on human linguist skill. |
| Neural Machine Translation with Post-Editing (NMT with MTPE) [58] | General MT engines (e.g., DeepL Pro) for draft generation, followed by human correction. | High-speed for high-volume content; high risk of critical errors if used alone; mandatory for rigorous MTPE for GCP use. |
| Linguistic Validation & QA Tools (e.g., Xbench) [58] | Supports the quality assurance methodology for checking translations. | Catches subtle errors; essential for high-risk documents like ICFs; time and resource-intensive. |
Workflow Visualization
The following diagram illustrates the integrated workflow for managing compliant clinical translations, from initial risk assessment to final audit-ready documentation.
Diagram 1: Clinical Translation Compliance Workflow. This chart outlines the decision pathway for translating clinical content, emphasizing risk-based approaches and integration with Quality Management Systems (QMS).
For bio-optics researchers and developers, navigating the intricate web of regulatory and translation compliance is not merely a final administrative step but a foundational component of the clinical translation process. Success hinges on a proactive strategy that integrates qualified expertise, robust processes, and appropriate technology from the earliest stages of development. By adhering to global regulations like MDR and ICH GCP, implementing rigorous validation protocols, and leveraging a risk-based approach to translation management, research teams can effectively mitigate hurdles. This disciplined approach accelerates the journey of innovative bio-optical technologies from the laboratory bench to the patient's bedside, ensuring safety, efficacy, and global market access.
Strategies for Cost Management and Improving Market Adoption
The field of bio-optics, which encompasses technologies utilizing light to image, analyze, and manipulate biological systems, faces significant challenges in cost management and market adoption despite its substantial growth potential. The global bio-optics market is projected to reach $18.26 billion by 2035, growing at a CAGR of 4.18%, while the broader biophotonics market is expected to grow at a more rapid CAGR of 10.20% to reach $145.64 billion by 2033 [59] [60]. Key barriers include high equipment costs, stringent regulatory requirements, technical complexity, and workforce training limitations [36] [12] [7]. This whitepaper provides comprehensive strategies to address these challenges through technological innovation, strategic partnerships, and market-focused product development, specifically targeting researchers, scientists, and drug development professionals working at the intersection of optical technology and biological applications.
Market Landscape and Economic Context
Understanding the market dynamics and economic pressures is essential for developing effective cost management and adoption strategies. The bio-optics market demonstrates varying growth patterns across different segments and geographic regions, influenced by local industry dynamics, regulatory frameworks, and technological adoption rates [36].
Table 1: Bio-optics and Biophotonics Market Outlook
| Market Segment | 2024-2025 Market Size | 2032-2033 Projected Size | CAGR | Primary Growth Drivers |
|---|---|---|---|---|
| United States Bio-optics | $13.15 billion (2025) [36] | $22.62 billion (2033) [36] | 9.46% [36] | Healthcare diagnostics, minimally invasive surgeries, aging population [36] |
| Global Bio-optics | $11.64 billion (2024) [59] | $18.26 billion (2035) [59] | 4.18% [59] | Non-invasive diagnostic tools, biological research, pharmaceutical applications [59] |
| Global Biophotonics | $67.09-67.2 billion (2025) [7] [60] | $145.64-189.3 billion (2033-2035) [7] [60] | 10.20-10.9% [7] [60] | Rising chronic diseases, precision medicine, non-invasive diagnostics [7] [60] [61] |
The market segmentation reveals distinct opportunities and challenges across different applications and technologies. Clinical diagnostics represents the largest application segment, while pharmaceutical applications show the most rapid growth potential [59]. From a technology perspective, fluorescence imaging currently dominates the market, but laser scanning microscopy is emerging as the fastest-growing segment [59].
Regional Market Variations
Significant regional variations impact cost structures and adoption strategies:
North America: Maintains market leadership with 37.30% revenue share in biophotonics, driven by technological infrastructure, high R&D spending, and established healthcare systems [60]. The U.S. market specifically benefits from strong regulatory frameworks and a high concentration of biophotonics companies [36] [60].
Europe: Characterized by stringent quality standards and sustainability goals, with Germany leading in medical device manufacturing and innovation [36] [60]. The UK demonstrates strong biomedical research integration within its healthcare system [12].
Asia-Pacific: Emerging as the fastest-growing region (CAGR of 10.85% for biophotonics), driven by rapid industrialization, government-supported innovation programs, and expanding healthcare infrastructure [36] [60]. China's market expansion is particularly notable due to government support for medical device innovation [60].
Latin America and MEA: Experiencing gradual market progression with improving economic conditions and growing awareness of advanced diagnostic solutions [36] [60].
Cost Management Strategies
Effective cost management in bio-optics requires a multifaceted approach addressing development, manufacturing, and implementation phases. The high costs associated with advanced bio-optic devices (often exceeding acquisition capabilities of smaller healthcare facilities) represent a significant barrier to market penetration [36] [12].
Technology Optimization Approaches
Diagram: Cost Management Strategic Framework
Modular System Architecture
Developing bio-optic systems with modular components enables significant cost reduction through several mechanisms:
Component Standardization: Implementing standardized optical interfaces, detector systems, and illumination sources across multiple product lines reduces manufacturing complexity and inventory costs. Research indicates that modular fluorescence imaging systems can reduce development costs by 30-40% compared to fully integrated proprietary systems [1].
Scalable Configurations: Offering base systems with tiered capability options allows customers to purchase appropriate functionality for their current needs while maintaining upgrade paths. This approach particularly benefits research laboratories and academic institutions with budget constraints [59].
Customized Optical Solutions: As demonstrated by Avantier and other leading providers, customized imaging systems and lasers optimized for specific applications eliminate unnecessary features while enhancing performance parameters critical to the application, improving overall cost efficiency [1].
Open-Source Platform Development
The adoption of open-source frameworks for data analysis, instrument control, and image processing significantly reduces software development costs while accelerating innovation:
Collaborative Development Models: Establishing consortium-based development of core processing algorithms and software infrastructure distributes R&D costs across multiple institutions. The Bio-Optics: Design and Application (BODA) conference series has highlighted successful implementations of this approach for optical coherence tomography and multiphoton microscopy platforms [4] [42].
Standardized Data Formats: Implementing community-developed data standards improves interoperability and reduces integration costs. Initiatives such as the Open Bio-Optics Data Format (OBODF) enable sharing of analysis tools and processing pipelines across institutions [42].
Miniaturization and Portable Designs
Miniaturization strategies address cost barriers while expanding application possibilities:
Point-of-Care Devices: Compact, portable bio-optic devices for point-of-care applications reduce costs by 30-50% compared to traditional laboratory systems while expanding market reach to primary care settings and resource-limited environments [12] [7]. The development of smartphone-based fluorescence readers has demonstrated particularly rapid growth, projected at 42% in 2024 [60].
Integrated Optofluidic Systems: Combining microfluidics with optical detection systems creates lab-on-a-chip platforms that minimize reagent consumption and reduce overall system costs while maintaining high sensitivity [4] [1].
Strategic Partnership Models
Collaborative approaches distribute costs and accelerate development cycles:
Academic-Industry Partnerships: Structured collaborations with research institutions provide access to cutting-edge innovations while sharing R&D expenses. These partnerships have been shown to reduce individual company development costs by 25-35% while decreasing time-to-market by 30-40% [36] [7].
Pre-Competitive Consortia: Multi-company collaborations focused on developing foundational technologies and addressing standardized regulatory frameworks distribute fundamental research costs while establishing industry standards. Examples include the Biophotonics Consortium organized through the Wellman Center for Photomedicine [4].
Supplier Integration: Early involvement of component suppliers in the design process optimizes specifications for cost-effective manufacturing without compromising performance. This approach is particularly valuable for specialized optical elements and detector systems [1].
Market Adoption Enhancement
Improving market adoption requires addressing both technical and ecosystem barriers, including regulatory challenges, technical complexity, and limited awareness among healthcare professionals [36] [12].
Regulatory Strategy Optimization
Navigating regulatory requirements efficiently is critical for timely market entry:
Diagram: Regulatory Pathway Optimization
Early Regulatory Engagement: Proactive consultation with regulatory agencies (FDA, EMA, etc.) during the development phase identifies potential approval challenges early, reducing delays. The FDA's 2024 approval of four new biophotonic imaging devices for clinical cancer screening demonstrated the value of early agency engagement [7].
Streamlined Clinical Validation: Designing focused clinical studies that address specific regulatory requirements while collecting real-world performance data. The implementation of optical coherence tomography (OCT) systems in ophthalmology provides a successful template for efficient clinical validation [12] [7].
Quality Management Systems: Implementing robust quality systems from initial development through manufacturing reduces regulatory review times. Adherence to ISO standards and Good Manufacturing Practices (GMP) is essential for efficient regulatory compliance [12].
Educational and Training Initiatives
Addressing the expertise gap through comprehensive education programs:
Structured Training Programs: Developing tiered training programs for healthcare professionals, researchers, and technical staff improves operational competence and confidence in bio-optic technologies. Programs combining online modules with hands-on workshops have demonstrated 45% improvement in proper device utilization [36] [59].
Clinical Implementation Support: Providing comprehensive implementation resources including protocol development, clinical workflow integration, and ongoing technical support. The University Medical Center Hamburg-Eppendorf's implementation of confocal endomicroscopy systems demonstrated how structured support resulted in a 23% reduction in biopsy procedures over six months [7].
Academic Curriculum Development: Partnering with universities to integrate bio-optics principles and applications into biomedical engineering, biology, and medical curricula builds future workforce capability. The incorporation of bio-optics modules in over 40 leading universities has accelerated adoption in research settings [36] [62].
Demonstration of Clinical and Economic Value
Clearly establishing the clinical utility and economic value of bio-optic technologies:
Health Economic Studies: Conducting rigorous analyses of cost-effectiveness, operational efficiency improvements, and patient outcome enhancements. Studies have shown that minimally invasive biophotonic procedures reduce hospital stays by 30-50% and cut complication rates by approximately 40% compared to traditional surgery [60].
Real-World Evidence Generation: Implementing structured post-market surveillance and outcomes tracking to demonstrate clinical utility in diverse practice settings. The growing database of clinical outcomes using OCT for cancer margin assessment provides compelling evidence for adoption [12] [7].
Value-Based Positioning: Aligning technology positioning with healthcare system priorities including value-based care, patient satisfaction, and operational efficiency. Highlighting applications in personalized medicine and precision diagnostics resonates with evolving healthcare delivery models [36] [60].
Experimental Protocols and Technical Implementation
Successful cost management and adoption strategies require solid technical foundations and optimized experimental approaches.
Key Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for Bio-optics Applications
| Reagent/Material | Function | Application Examples | Cost Optimization Strategies |
|---|---|---|---|
| Fluorescent Probes & Labels | Molecular targeting and contrast enhancement | Cellular imaging, molecular tracking, diagnostic assays | Bulk purchasing agreements, centralized labeling cores, extended stability studies [12] [1] |
| Genetically Encoded Fluorescent Proteins | Intracellular expression and localization | Live-cell imaging, protein trafficking, gene expression | Open-source protein engineering, modular vector systems, shared repository resources [4] [1] |
| Surface Plasmon Resonance Materials | Label-free biomolecular interaction analysis | Binding kinetics, concentration measurements, biomolecular characterization | Reusable sensor chips, regeneration protocols, high-throughput formatting [7] [60] |
| Raman Spectroscopy Enhancements | Signal amplification for molecular fingerprinting | Tissue analysis, drug distribution studies, metabolic profiling | Substrate recycling, optimized nanoparticle synthesis, collaborative material development [12] [7] |
| Optical Coherence Tomography Contrast Agents | Enhanced scattering properties for structural imaging | Tissue microstructure, disease morphology, surgical guidance | Multi-purpose formulations, concentration optimization, simplified synthesis protocols [12] [42] |
| Biocompatible Optical Materials | Light transmission in biological environments | Fiber optics, implantable sensors, wearable devices | Material standardization, bulk manufacturing, alternative material development [1] [60] |
Optimized Experimental Workflows
Implementing standardized, efficient experimental protocols ensures reproducibility while managing costs:
Diagram: Experimental Workflow Optimization
Standardized Imaging Protocol for Cost-Effective Reproducibility
Protocol: Multi-modal Imaging for Tissue Characterization
This protocol optimizes resource utilization while maintaining data quality for tissue characterization applications:
Sample Preparation Phase (Time: 2-4 hours, Cost: $$)
- Implement standardized fixation and embedding protocols to minimize reagent costs while ensuring optical compatibility
- Utilize reference standards for calibration and quality control (commercially available or internally developed)
- Employ multi-purpose staining protocols compatible with multiple imaging modalities
Optical Configuration Phase (Time: 30-60 minutes, Cost: $)
- Establish standardized system calibration procedures using certified reference materials
- Implement automated alignment and quality verification routines
- Utilize modular optical components to optimize configuration for specific applications
Data Acquisition Phase (Time: variable, Cost: $$-$$$)
- Implement adaptive acquisition protocols that focus resources on relevant regions or signals
- Utilize multi-modal data collection to maximize information from single samples
- Establish standardized metadata capture for reproducible experimental conditions
Processing and Analysis Phase (Time: 1-4 hours, Cost: $)
- Deploy open-source analysis platforms (ImageJ, Fiji, etc.) with customized macros for specific applications
- Implement automated processing pipelines to reduce manual intervention and improve consistency
- Utilize cloud-based computing resources for computationally intensive analyses
This structured approach has demonstrated 40% reduction in repeat experiments due to improved reproducibility and 25% decrease in reagent costs through optimized utilization [42] [1].
Future Outlook and Strategic Recommendations
The bio-optics field continues to evolve rapidly, with several emerging trends creating new opportunities for cost management and adoption enhancement.
Emerging Technology Integration
Artificial Intelligence and Machine Learning: Integration of AI/ML for image analysis, system optimization, and automated interpretation addresses expertise limitations while improving performance. The BODA 2025 conference highlights multiple sessions focused on "Machine Learning for Image Reconstruction, Interpretation and Optical Design" [4]. AI-assisted imaging analysis enhances biological data interpretation, automated lesion detection, and real-time evaluation of therapeutic effects [7].
Hybrid Technology Platforms: Combining multiple optical modalities with complementary strengths creates systems with broader applications while distributing development costs across multiple market segments [42] [59].
Wearable and Continuous Monitoring: Miniaturized bio-optic systems for continuous physiological monitoring represent a growing market segment with particular potential for chronic disease management [7] [60].
Strategic Implementation Recommendations
Based on comprehensive analysis of market dynamics and technology trends, the following strategic recommendations provide a roadmap for effective cost management and accelerated market adoption:
Prioritize Modular Design Principles: Implement modular system architectures that enable cost-effective customization and upgrading, particularly for core imaging platforms used across multiple applications [1] [59].
Develop Structured Partnership Networks: Establish formal collaboration frameworks with academic institutions, clinical research centers, and complementary technology providers to distribute development costs and accelerate validation [36] [7].
Implement Tiered Product Strategies: Offer product portfolios with graduated capabilities and price points to address diverse market segments from basic research to advanced clinical applications [12] [59].
Invest in Education Infrastructure: Allocate resources to develop comprehensive training programs, user support resources, and implementation tools to overcome expertise barriers [36] [59].
Engage Regulatory Authorities Early: Establish proactive relationships with regulatory agencies and participate in standards development to streamline approval processes [12] [7].
Demonstrate Economic Value: Conduct rigorous health economic studies and real-world evidence generation to document clinical utility and economic benefits [7] [60].
By implementing these strategies, stakeholders in the bio-optics ecosystem can effectively address the dual challenges of cost management and market adoption, positioning themselves for success in this rapidly evolving field.
The field of bio-optics, which focuses on the development and application of optical technologies for life sciences and clinical research, is undergoing a profound transformation driven by artificial intelligence (AI) and machine learning (ML). These computational technologies are addressing core challenges in biomedical optical imaging, from enhancing image quality and accelerating acquisition to enabling novel analytical capabilities. In the context of bio-optics design and application, AI is not merely an incremental improvement but a paradigm shift, moving beyond traditional signal processing to create more intelligent, adaptive, and efficient imaging systems [4]. This evolution is critical for advancing research in biology, biotechnology, and drug development, where extracting meaningful information from complex, noisy biological data is paramount.
The integration of AI is particularly timely, coinciding with the development of advanced imaging hardware. For instance, the emergence of total-body and long-axial field-of-view PET scanners provides increased sensitivity and larger coverage [63]. However, these systems generate vast, complex datasets that benefit immensely from AI-driven reconstruction and analysis methods to fully realize their potential for faster, lower-dose imaging. This synergy between cutting-edge hardware and sophisticated software is defining the next generation of bio-optical tools, enabling researchers and drug development professionals to uncover insights that were previously inaccessible.
Core AI Methodologies in Image Processing
AI and ML encompass a range of techniques tailored to specific problems in image reconstruction and analysis. Understanding these core methodologies is essential for appreciating their applications in bio-optics.
Convolutional Neural Networks (CNNs) for Feature Recognition
Convolutional Neural Networks (CNNs) are a cornerstone of image analysis, designed to process pixel data with a grid-like topology. Their architecture is exceptionally adept at learning spatial hierarchies of features, from simple edges and textures in initial layers to complex, object-specific patterns in deeper layers. A prime application in bio-optics is the analysis of Diffuse in-vivo Flow Cytometry (DiFC) data. Researchers have developed a CNN that leverages the shapes of signal peaks to more accurately distinguish real cellular events (like circulating tumor cells) from artifacts in mice, outperforming previous amplitude-based methods [64]. This demonstrates a key advantage of CNNs: their ability to learn and utilize complex, non-intuitive features in optical data for superior classification.
Generative AI and Synthetic Data
Generative AI models represent a powerful frontier, capable of creating new, synthetic data that closely mirrors real-world data. In medical imaging, this is leveraged to generate derivative synthetic datasets that can augment and diversify research resources [65]. The applications are multifaceted:
- Augmenting Rare Disease Datasets: By generating synthetic images of rare conditions, these models help build robust training sets for diagnostic algorithms that would otherwise be hampered by data scarcity.
- Privacy Preservation: Synthetic data can be used to facilitate multi-center collaborations without sharing sensitive patient information.
- Enhancing Resolution: Techniques like AI-driven super-resolution allow for the enhancement of image detail beyond the physical limits of the optical system, improving lesion detectability [63].
Multimodal AI for Integrated Analysis
Multimodal Language Models (MLMs) are advanced systems that can process and correlate information from different data types, or "modalities"—such as genomic sequences, chemical structures, clinical notes, and medical images [66]. This approach overcomes the limitations of traditional, siloed analysis. In drug discovery, for example, MLMs can simultaneously explore genetic sequences, images of tissue samples from optical microscopes, and clinical data to identify more robust therapeutic targets and predict patient responses with greater accuracy [66]. This holistic, data-integration capability is crucial for tackling complex biological problems and accelerating the development of new therapies.
Quantitative Analysis of AI Applications
The impact of AI and ML in bio-optics can be measured through key performance metrics. The following table summarizes the quantitative benefits across different application areas.
Table 1: Performance Metrics of AI/ML in Bio-Optics Applications
| Application Area | AI Technique | Key Improvement | Quantitative / Qualitative Impact |
|---|---|---|---|
| Drug Discovery | Generative AI & Multimodal Models | Accelerated early-stage R&D | Compression of discovery/preclinical phase from ~5 years to under 2 years in some cases [67] |
| Lead Optimization | AI-Driven Design | Efficiency in Compound Synthesis | 70% faster design cycles; 10x fewer synthesized compounds required [67] |
| In-vivo Flow Cytometry | Convolutional Neural Network (CNN) | Event Classification Accuracy | Improved distinction of real events from artifacts based on peak shapes vs. amplitude [64] |
| PET Imaging | AI-Guided Reconstruction | Image Quality & Acquisition | Enables faster, lower-dose imaging via super-resolution and motion compensation [63] |
| Spatial Biology | AI-Powered Image Analysis | Workflow Reproducibility | Enables automated, scalable analysis for high-throughput imaging [68] |
Experimental Protocols for AI-Enhanced Bio-Optics
Protocol: AI-Assisted Analysis of Diffuse in-vivo Flow Cytometry Data
This protocol details the methodology for using a CNN to analyze DiFC data, as cited in recent research [64].
1. Objective: To develop and validate a convolutional neural network (CNN) for analyzing Diffuse in-vivo Flow Cytometry (DiFC) data to better distinguish real cellular events (e.g., circulating tumor cells) from artifacts in anesthetized or awake mice.
2. Materials and Equipment:
- DiFC Instrumentation: A system for in-vivo flow cytometry, including lasers, detectors, and data acquisition hardware.
- Animal Model: Mice (anesthetized or awake) with introduced fluorescently-labeled cells.
- Data Acquisition System: Software for recording raw time-series optical data.
- Computing Hardware: A computer with a sufficient GPU (Graphics Processing Unit) for training and running deep learning models.
- Software Frameworks: Python with deep learning libraries such as TensorFlow or PyTorch.
3. Procedure:
- Step 1: Data Collection. Acquire raw DiFC signal data from mice. The data consists of a time-series of fluorescence intensity measurements.
- Step 2: Data Labeling and Pre-processing. Manually label segments of the data to create a ground-truth dataset, identifying peaks corresponding to true cellular events versus artifacts. Normalize the amplitude of the signals and segment the time-series data into windows centered on candidate peaks.
- Step 3: Model Architecture Design. Design a CNN architecture suitable for 1D signal processing. This typically includes:
- Input layer for the 1D signal window.
- Convolutional layers with ReLU activation to extract features.
- Pooling layers (e.g., max pooling) for down-sampling.
- Fully connected layers at the end for classification.
- Output layer with a softmax activation for binary classification (e.g., "real event" vs. "artifact").
- Step 4: Model Training. Split the labeled dataset into training, validation, and test sets. Train the CNN on the training set, using the validation set to monitor for overfitting and tune hyperparameters. The loss function is typically binary cross-entropy, optimized with an algorithm like Adam.
- Step 5: Model Validation. Evaluate the final model on the held-out test set. Compare its performance (e.g., using metrics like accuracy, precision, recall, and F1-score) against the traditional amplitude-based thresholding method.
- Step 6: Deployment. Integrate the trained model into the DiFC data analysis pipeline to automatically classify new, unseen data.
4. Analysis and Interpretation: The key innovation lies in the CNN's ability to learn from the entire shape of the signal peak, rather than relying solely on a simple amplitude threshold. This allows the model to capture subtle, complex patterns that are indicative of a true biological event, leading to a significant reduction in false positives and false negatives.
Protocol: AI-Guided Reconstruction for PET/CT Imaging
This protocol outlines the application of AI in enhancing PET image reconstruction, leveraging advancements in scanner technology [63].
1. Objective: To utilize artificial intelligence for enhancing PET image reconstruction and resolution, enabling rapid processing, improved quantification, and lower-dose imaging, particularly in conjunction with modern total-body and long-axial field-of-view scanners.
2. Materials and Equipment:
- Imaging System: A PET/CT scanner, preferably with a long-axial field-of-view.
- Radiotracer: A clinically relevant PET radiotracer.
- Computing Infrastructure: High-performance computing resources with GPUs.
- Software: Access to AI-enabled image reconstruction software (commercial or research-grade).
3. Procedure:
- Step 1: Data Acquisition. Acquire PET raw sinogram data and CT-based attenuation correction data from a patient or subject.
- Step 2: Traditional Reconstruction (Baseline). Reconstruct the images using a conventional method, such as Ordered-Subsets Expectation Maximization (OSEM), to establish a baseline for comparison.
- Step 3: AI-Driven Reconstruction.
- Input: The raw sinogram data and/or the initially reconstructed images from Step 2 are fed into a pre-trained deep learning model.
- Processing: The AI model (often a CNN or a Generative Adversarial Network) applies a suite of enhancements. These can include:
- Denoising: Suppressing statistical noise inherent in low-count data.
- Super-Resolution: Enhancing the spatial resolution of the image.
- Positron Range Correction: Correcting for the blurring caused by the distance a positron travels before annihilation.
- Motion Compensation: Correcting for patient respiratory or involuntary motion during the scan.
- Output: The model generates a final, enhanced image with improved signal-to-noise ratio and clarity.
- Step 4: Quantitative Analysis. Perform quantitative analysis on both the baseline and AI-reconstructed images. Key metrics include Standardized Uptake Value (SUV), signal-to-noise ratio (SNR) in regions of interest, and target-to-background ratios.
4. Analysis and Interpretation: The AI-guided reconstruction aims to produce images with superior lesion detectability and image quality compared to traditional methods. This allows for either a reduction in radiotracer dose (reducing patient radiation exposure) or a shortening of the scan duration, while maintaining diagnostic quality. The model's training on high-quality datasets enables it to effectively predict and correct for various physical degradations in the imaging process [63].
Visualization of Workflows and Signaling Pathways
AI-Enhanced Bio-Optics Data Analysis Workflow
The following diagram illustrates a generalized, integrated workflow for AI-enhanced image reconstruction and analysis in bio-optics, synthesizing concepts from the cited research.
AI Model Training & Validation Pathway
This diagram details the critical pathway for developing and validating the AI models used in the analysis workflow above.
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of AI in bio-optics relies on a combination of specialized hardware, software, and biological materials. The following table details key components of this experimental toolkit.
Table 2: Essential Research Reagents and Materials for AI-Enhanced Bio-Optics
| Item Name | Function / Application | Relevant Example |
|---|---|---|
| Long-Axial Field-of-View PET/CT Scanner | Provides high-sensitivity, large-coverage imaging data that serves as input for AI reconstruction algorithms. | Used for acquiring the raw data enhanced by AI-driven super-resolution and motion compensation [63]. |
| Diffuse in-vivo Flow Cytometry (DiFC) | An optical technique for detecting and analyzing rare cells (e.g., circulating tumor cells) in live animals. | Generates the time-series signal data analyzed by the custom CNN to distinguish real events from artifacts [64]. |
| ZEISS Axioscan 7 | An automated microscope for high-throughput spatial biology imaging. | Used in automated workflows; its output is analyzed by AI (e.g., Mindpeak software) for reproducible, scalable data [68]. |
| Fluorescently-Labeled Probes | Molecules that bind to specific cellular targets (e.g., folate receptors) to enable optical detection. | Used to label circulating tumor cells for detection and analysis in DiFC experiments [64]. |
| Pre-trained AI Models & Software | Software packages containing algorithms for image reconstruction, denoising, and feature extraction. | Includes tools for AI-guided PET reconstruction [63] and AI-powered image analysis in spatial biology [68]. |
| High-Performance Computing (HPC) Cluster | Computing infrastructure with GPUs for training complex AI models and processing large datasets. | Essential for running the computationally intensive tasks of model training and inference on large image sets. |
The field of bio-optics is undergoing a transformative shift toward miniaturization, driven by the convergence of optical engineering, materials science, and artificial intelligence. This paradigm shift enables the development of portable and wearable devices that extend biomedical sensing and imaging from traditional laboratory settings to point-of-care diagnostics, continuous health monitoring, and personalized medicine. Bio-optics, which encompasses the application of light-based technologies to biological and medical sciences, now prioritizes the creation of compact, efficient, and user-friendly devices that maintain the precision of their benchtop counterparts [69]. The global bio-optics market, valued at approximately USD 20.5 billion in 2024, reflects this trend, with projections estimating growth to USD 34.8 billion by 2033 at a compound annual growth rate (CAGR) of 6.7% [69].
This technical guide examines the core principles, technologies, and methodologies underpinning the design of miniaturized bio-optic devices. Framed within broader research on bio-optics design and application, this review addresses the critical challenges and innovative solutions that are reshaping how researchers and clinicians monitor physiological status, detect diseases, and therapeutic interventions. The movement toward miniaturization is not merely a technical curiosity but a fundamental evolution that enhances healthcare accessibility, enables real-time physiological monitoring, and supports the growing demand for decentralized clinical trials and remote patient management [70] [71].
Market Dynamics and Growth Projections
The accelerating adoption of miniaturized bio-optic technologies is reflected in robust market growth trajectories across multiple segments. The broader biophotonics market, within which portable and wearable devices represent a rapidly expanding segment, is projected to grow from $68.4 billion in 2025 to $113.1 billion by 2030, at a CAGR of 10.6% [72]. This growth is fueled by increasing demand for non-invasive diagnostics, the rising prevalence of chronic diseases, and technological advancements in optical technologies [72] [7].
Table 1: Global Market Projections for Bio-Optics and Related Technologies
| Market Segment | 2024/2025 Value (USD Billion) | 2030/2035 Projection (USD Billion) | CAGR (%) | Primary Growth Drivers |
|---|---|---|---|---|
| Bio-Optics Market | 20.5 (2024) [69] | 34.8 (2033) [69] | 6.7 [69] | Demand for portable diagnostics, agricultural biotechnology, environmental monitoring |
| Biophotonics Market | 68.4 (2025) [72] | 113.1 (2030) [72] | 10.6 [72] | Non-invasive medical diagnostics, light therapy, see-through imaging, biosensing |
| Wearable Sensors Market | N/A | 7.2 (2035) [71] | ~5 (2025-2035) [71] | Remote patient monitoring, decentralized clinical trials, consumer wellness |
Regional analysis reveals that North America currently dominates the bio-optics market with an estimated 35% share, followed by Europe (28%) and Asia-Pacific (27%) [69]. The Asia-Pacific region is expected to exhibit the fastest growth rate due to expanding healthcare infrastructure, increasing government initiatives, and growing investments in digital health technologies [69]. The wearable sensors market, a key segment for miniaturized bio-optics, is forecast to reach $7.2 billion by 2035, driven by integration into digital health platforms, extended reality systems, and non-invasive diagnostics [71].
Key Technological Innovations in Device Miniaturization
Materials and Fabrication Advances
Miniaturized bio-optic devices leverage innovative materials and fabrication techniques to achieve reduced footprint while maintaining high performance. Gallium nitride (GaN) semiconductors are revolutionizing power electronics by providing energy-efficient and highly durable components for portable systems [73]. The wider band gap in GaN enables more powerful and efficient power conversion than traditional silicon, which is crucial for battery-operated wearable devices [73].
Biocompatible materials represent another critical innovation area, particularly for wearables and implantables. The use of biocompatible metals and polymers ensures that devices can safely interface with the human body while minimizing adverse reactions [73] [70]. Flexible substrates such as polydimethylsiloxane (PDMS) enable the development of conformable skin patches that maintain comfortable contact with the curvilinear surfaces of the body while housing optical components [70]. For implantable applications, materials with enhanced biocompatibility profiles reduce fibrotic responses and extend functional lifetime within the biological environment.
Advanced manufacturing techniques including custom molding services, micro-electro-mechanical systems (MEMS) fabrication, and 3D printing of micro-optics facilitate the production of complex miniaturized components [73] [4]. For instance, 3D printing of glass micro-optics is emerging as a promising approach for shaping precision optical systems for biomedical applications, allowing for rapid prototyping and customization of optical elements at reduced scales [4].
Optical Sensing Modalities
Miniaturization has been particularly impactful for optical sensing modalities, enabling their integration into wearable and portable platforms. Optical biosensors utilizing principles such as fluorescence, surface plasmon resonance (SPR), and Raman spectroscopy provide highly sensitive, label-free detection of biological and chemical analytes [7]. The incorporation of plasmonic nanoparticles, typically made from gold or silver, allows for concentration and guidance of light, enhancing signal strength and detection accuracy even at trace analyte concentrations [73].
Quantum dots — nanometer-scale semiconductor particles that control wavelengths of light based on their size and composition — enable devices to spot chemicals in very small concentrations due to their tunable optical properties and high extinction coefficients [73]. These nanomaterials are being integrated into wearable sensors for monitoring various biomarkers through colorimetric or fluorometric detection methods.
Spectroscopic techniques have also benefited from miniaturization trends. Near-infrared spectroscopy enables non-invasive assessment of tissues and fluids deep beneath the skin surface, eliminating the need for invasive sampling procedures [73]. The integration of microfluidics with spectroscopy creates lab-on-a-chip platforms that rapidly process trace quantities of fluids, bringing critical laboratory components to the sample rather than requiring sample transport to centralized labs [73].
Energy Efficiency and Power Management
Power constraints represent a significant challenge for miniaturized bio-optic devices, driving innovations in energy harvesting and management. Spectral analysis methods increasingly rely on efficient lighting solutions such as LEDs to achieve effective illumination with minimal energy expenditure [73]. Advanced power management circuits optimize the duty cycling of optical components, extending battery life while maintaining necessary measurement frequency.
Energy harvesting from physiological processes (motion, heat gradients) or ambient sources (light, radio frequency) is emerging as a promising approach for powering wearable bio-optic devices, potentially eliminating the need for battery replacement in long-term monitoring scenarios. The development of ultra-low power sensors, such as flexible piezo-resistive sensors consuming as little as 3 nanowatts for cardiovascular monitoring, demonstrates the potential for extended operation without frequent recharging [70].
Data Processing and Artificial Intelligence
The miniaturization of bio-optic devices generates substantial data streams that require sophisticated processing capabilities. Artificial intelligence (AI) and machine learning (ML) are transforming how miniaturized devices handle data analysis, enabling real-time interpretation of complex optical signals at the point of sensing [73] [74]. AI algorithms enhance diagnostic accuracy by identifying subtle patterns and anomalies that traditional methods might miss, facilitating earlier disease detection and personalized treatment plans [74].
Edge computing approaches bring processing capabilities directly to wearable devices, reducing latency and bandwidth requirements for data transmission. This enables real-time analysis and decision-making without constant connectivity to cloud resources [73]. For instance, AI-powered systems for early disease detection can analyze medical images such as X-rays, MRIs, and CT scans directly on portable devices, identifying patterns and abnormalities that might be missed by the human eye [75]. The integration of AI with biophotonics promotes the development of smart instruments capable of adaptive control and personalized feedback based on individual physiological responses.
Design Protocols for Miniaturized Bio-Optic Devices
Wearable Skin Patch for Multi-Parameter Monitoring
Table 2: Research Reagent Solutions for Wearable Skin Patch Development
| Component | Function | Technical Specifications |
|---|---|---|
| Flexible Piezo-Resistive Sensors (FPS) | Detection of epidermal pulse waves for blood pressure measurement | Ultra-low power (3 nW), high stability for subliminal physiological change detection [70] |
| Epidermal ECG Electrodes | Simultaneous electrocardiogram monitoring | Flexible, dry electrodes with stable skin contact [70] |
| Potentiometric Ion Sensors | Sodium ion detection in sweat | Polyvinyl chloride membrane with electrochemically deposited PEDOT layer [70] |
| Amperometric Lactate Sensor | Lactate measurement in sweat | Enzyme-doped copolymer membrane with outer polyurethane layer for selectivity [70] |
| PDMS Microfluidic Sampling | Non-invasive sampling of interstitial fluids | Thermal ablation technology for biomolecule access without invasive extraction [70] |
| Flexible Piezoelectric Membranes | Pulse wave detection | Perforated polyimide membranes with high chemical resistance and flexibility [70] |
Experimental Protocol: Development of a Multi-Parameter Monitoring Skin Patch
Objective: To design and validate a flexible, stamp-sized wearable patch (25 mm × 15 mm × 72 mm) for simultaneous monitoring of cardiovascular signals (blood pressure, ECG) and biomarkers in sweat (sodium ions, lactate).
Methodology:
Substrate Fabrication:
- Utilize a multi-layered integrated structure to reduce skin contact areas to approximately 1/125th of conventional sensors.
- Select polydimethylsiloxane (PDMS) as the primary substrate material for its flexibility, biocompatibility, and optical properties.
- Implement micro-manufacturing processes to create microfluidic channels for sweat transport and analysis.
Sensor Integration:
- Develop a ferro-electric film with special electrodes and flexible electrical circuitry for simultaneous ECG and ballistocardiogram (BCG) measurements on the human chest.
- Integrate a flexible piezo-resistive sensor (FPS) optimized through parametric modeling to ensure highly stable surface pulse signal detection.
- Incorporate epidermal-ECG sensors synchronized with the FPS for pulse transit time (PTT) calculation for cuffless blood pressure monitoring.
- Deposit a polyvinyl chloride membrane in the internal layer of electrochemically deposited Poly(3,4-ethylenedioxythiophene) (PEDOT) for potentiometric sodium ion sensing.
- Create a pH sensing layer using high-sensitivity iridium oxide (IrOx) membrane.
- Dope enzymes at the end of a copolymer membrane with outer layers of polyurethane for selective lactate detection in the presence of various analytes.
Data Processing and Validation:
- Implement signal processing algorithms for real-time calculation of pulse transit time and conversion to blood pressure values.
- Validate device performance against gold standard measurements (cuff-based blood pressure, laboratory sweat analysis) across diverse physiological states (rest, post-exercise).
- Conduct wearability studies to assess comfort, adhesion stability, and signal reliability during daily activities.
This protocol demonstrates the integration of multiple optical and electrochemical sensing modalities within a miniaturized, flexible form factor for comprehensive physiological monitoring [70].
Miniaturized Optical Coherence Tomography System
Experimental Protocol: Development of a Handheld OCT Scanner
Objective: To create a portable, handheld optical coherence tomography system for point-of-care dermatological and cardiovascular imaging.
Methodology:
Optical Design:
- Implement a spectral-domain OCT configuration using a miniature spectrometer and broadband light source.
- Utilize MEMS-based scanning mirrors to reduce the size of the beam steering mechanism.
- Employ single-mode optical fibers to deliver light to the sample arm, maintaining flexibility in the imaging probe.
Miniaturization Strategies:
- Replace traditional bulk optics with miniaturized alternatives, including 3D-printed glass micro-optics for beam shaping and focusing.
- Implement a custom ASIC (Application-Specific Integrated Circuit) for data acquisition and processing to reduce electronic footprint.
- Design a compact housing using lightweight polymers with ergonomic considerations for handheld operation.
Image Processing:
- Develop optimized algorithms for real-time image reconstruction on embedded processors.
- Incorporate AI-based image analysis for automated feature detection and diagnostic support.
- Implement compression techniques for efficient data storage and transmission.
Validation:
- Compare imaging performance with benchtop OCT systems using standardized phantoms.
- Conduct clinical validation studies for specific applications (skin cancer screening, coronary artery assessment).
- Evaluate usability in point-of-care settings by non-specialist operators.
This approach to OCT miniaturization enables the transition of a powerful laboratory imaging technique to bedside, operating room, and primary care settings [4] [7].
Imaging and Analysis Workflows
The integration of miniaturized bio-optic devices into research and clinical practice requires standardized workflows for data acquisition, processing, and interpretation. The following diagram illustrates a generalized workflow for a wearable bio-optic monitoring system:
This workflow highlights the seamless integration of hardware and software components in modern miniaturized bio-optic systems, emphasizing the role of AI/ML in transforming raw optical signals into clinically actionable information.
Future Perspectives and Research Directions
The field of miniaturized bio-optic devices continues to evolve rapidly, with several emerging trends shaping its future trajectory. Multi-modal integration represents a significant frontier, combining multiple optical sensing modalities (e.g., fluorescence, Raman spectroscopy, OCT) within a single miniaturized platform to provide comprehensive physiological assessment [74]. This approach leverages the complementary strengths of different optical techniques while maintaining a compact form factor.
Advanced biocompatibility and longevity remain critical challenges, particularly for implantable bio-optic devices. Research continues into novel encapsulation materials, biofouling-resistant coatings, and compliant interfaces that maintain optimal performance throughout extended implantation periods. The development of biodegradable optical components represents a promising direction for temporary monitoring applications, eliminating the need for extraction procedures.
The integration of quantum technologies with bio-optics opens new possibilities for ultra-sensitive detection. Recent demonstrations of protein-based spin qubits encoded in the metastable triplet state of fluorescent proteins show promise for quantum-enhanced biological sensing with coherence times rivaling traditional solid-state systems [4]. These genetically encodable quantum sensors could revolutionize cellular-scale imaging and detection.
Regulatory frameworks and standardization will play an increasingly important role as miniaturized bio-optic devices transition from research prototypes to clinically approved tools. The recent FDA approvals of several biophotonic imaging devices for clinical cancer screening indicate growing regulatory acceptance of these technologies [7]. Standardized validation protocols and performance metrics will be essential for widespread clinical adoption.
Finally, the convergence of miniaturized bio-optics with therapeutics creates opportunities for closed-loop systems that not only monitor physiological status but also deliver targeted interventions. Light-based neural modulation, optogenetic therapies, and photodynamic treatments represent promising avenues where diagnostic and therapeutic capabilities are unified within miniaturized implantable or wearable platforms.
The miniaturization of bio-optic devices represents a paradigm shift in biomedical sensing and imaging, enabling transition from laboratory-based equipment to portable, wearable, and implantable platforms. This transformation is driven by innovations in materials science, optical engineering, artificial intelligence, and power management, which collectively address the challenges of reducing device footprint while maintaining performance. The robust market growth projections for bio-optics and wearable sensors reflect the increasing adoption of these technologies across healthcare, research, and consumer wellness applications.
For researchers, scientists, and drug development professionals, understanding the principles and methodologies underlying miniaturized bio-optic device design is increasingly essential. The protocols and workflows presented in this guide provide a foundation for developing next-generation portable and wearable bio-optic systems that offer unprecedented capabilities for continuous monitoring, point-of-care diagnostics, and personalized medicine. As the field continues to evolve, the integration of advanced computational methods, novel materials, and quantum-enhanced detection will further expand the possibilities for miniaturized bio-optics to transform biomedical research and clinical practice.
Evaluating Performance, Market Leaders, and Future-Proof Technologies
Bio-optics, the application of light-based technologies to analyze and manipulate biological systems, has become a cornerstone of modern life sciences and medical research [10]. This interdisciplinary field, often used interchangeably with biophotonics, leverages the interactions between light and biological matter to enable advancements in imaging, diagnostics, and therapy [12] [10]. For researchers and drug development professionals, understanding the distinct strengths and limitations of available bio-optic technologies is crucial for selecting the appropriate tool for specific experimental or clinical needs. This whitepaper provides a comparative analysis of core bio-optic technologies, framed within the context of bio-optics design and application research, to inform strategic decision-making in research and development.
Core Bio-Optic Technologies and Comparative Analysis
Bio-optic technologies can be broadly categorized into imaging, sensing, and therapeutic systems. Their performance varies significantly based on underlying principles, such as the use of labels, interaction mechanisms (e.g., absorption, emission, scattering), and the type of information they provide (e.g., structural, molecular, functional) [10].
Table 1: Comparative Analysis of Major Bio-Optic Imaging Technologies
| Technology | Working Principle | Key Strengths | Major Limitations | Primary Applications in Research |
|---|---|---|---|---|
| Optical Coherence Tomography (OCT) | Interferometry to capture backscattered light [10] | High-resolution, real-time 3D imaging; non-invasive; deep tissue penetration [12] [10] | Limited molecular specificity; contrast often based on refractive index [10] | Ophthalmology [12] [10], cardiology, dermatology, oncology [12] |
| Multiphoton Microscopy | Simultaneous absorption of two or more photons for excitation [10] | High spatial resolution; reduced photobleaching & phototoxicity; deep tissue imaging [10] | High cost of ultrafast lasers; system complexity [10] | Deep-tissue cellular and subcellular imaging [10] |
| Fluorescence Imaging | Detection of light emitted from fluorophores after excitation [12] [10] | High sensitivity and specificity; molecular contrast; versatile (e.g., FLIM, FRET) [12] [10] | Often requires exogenous labels; photobleaching; limited penetration depth [10] | Cell biology, protein interaction studies (FRET) [76], cancer research [12] |
| Photoacoustic Imaging (PAI) | Absorption of light by chromophores generates ultrasonic waves [10] [77] | Combines optical contrast with ultrasonic depth resolution; label-free visualization of chromophores [10] | Can be expensive (e.g., clinical units >$500,000) [77] | Vascular imaging, real-time stroke assessment, oncology [77] |
Table 2: Comparative Analysis of Major Bio-Optic Sensing and Biosensing Technologies
| Technology | Working Principle | Key Strengths | Major Limitations | Primary Applications in Research |
|---|---|---|---|---|
| Surface Plasmon Resonance (SPR) | Measures refractive index change near a metal surface [76] | Label-free, real-time kinetics of biomolecular interactions; high sensitivity [76] | Bulk refractive index sensitivity can cause interference; requires specialized chips [76] | Drug discovery, biomarker detection, protein-protein interactions [76] |
| Raman Spectroscopy | Analyzes inelastic scattering of light for molecular fingerprinting [12] [10] | Label-free; highly specific molecular information; minimal sample preparation [12] | Intrinsically weak signal [10]; can be enhanced with substrates (SERS) [77] | Studying cell/tissue composition, identifying disease biomarkers [12] |
| Fiber-Optic Biosensors | Uses optical fibers to transmit light; biological interaction modulates light properties [76] | Suitability for remote sensing and miniaturization; potential for point-of-care use [76] | Susceptible to environmental interference; design complexity for multi-analyte sensing [76] | In-vivo monitoring, environmental sensing [78] |
| CRISPR-based Optical Biosensors | Cas enzyme's trans-cleavage activity releases fluorescent signal upon target recognition [76] | Extremely high sensitivity (attomolar range) [76]; high specificity; short assay time [76] | Primarily for nucleic acid detection; relatively new technology with evolving protocols [76] | Rapid, point-of-care diagnostics for infectious diseases [76] |
Emerging Trends and Technological Convergence
The convergence of bio-optics with other technological fields is creating powerful new capabilities for research and diagnostics.
Integration with Artificial Intelligence (AI)
Machine learning and deep learning algorithms are revolutionizing optical biosensors and imaging systems by enhancing analytical performance [79] [74]. AI integration improves signal processing, enables intelligent pattern recognition, and facilitates automated, real-time decision-making [79]. For instance, AI-enabled spectroscopy has demonstrated 98.8% accuracy in non-invasive glucose monitoring, and machine learning enhances Surface-Enhanced Raman Spectroscopy (SERS) for cancer detection [77]. This synergy is pushing the boundaries of sensitivity, specificity, and multiplexing capabilities in bio-optic devices [79].
Miniaturization and Point-of-Care Applications
There is a significant trend toward the miniaturization of bio-optic devices to enable point-of-care diagnostics and monitoring [12] [79]. This includes the development of handheld imaging devices, portable spectroscopy systems, and wearable biosensors [12]. These technologies facilitate rapid, accurate diagnostics outside traditional laboratories, empowering real-time analysis in remote settings and supporting the growing trends of home healthcare and self-monitoring [12] [74]. The integration of these portable devices with telemedicine platforms further expands access to specialized healthcare services [12].
Experimental Protocols and Methodologies
To ensure reproducibility and provide a practical guide for researchers, this section outlines detailed protocols for key applications of bio-optic technologies.
Protocol: Detection of Neurodegenerative Disease Biomarkers using Fluorescence-Based SIMOA
Application: Ultra-sensitive, quantitative detection of protein biomarkers (e.g., Amyloid-beta, Tau) for Alzheimer's disease in cerebrospinal fluid or blood plasma [76].
Principle: This digital immunoassay technology uses paramagnetic beads to capture and isolate single protein molecules in femtoliter-sized wells, enabling digital counting and detection at femtomolar concentrations [76].
Workflow:
- Sample Preparation: Dilute patient CSF or plasma sample in a specific assay buffer. Prepare paramagnetic beads coated with capture antibodies specific to the target biomarker (e.g., anti-Tau antibody).
- Antigen Capture and Labeling: Incubate the sample with the functionalized beads and a biotinylated detection antibody to form a sandwich complex. Follow with incubation with an enzyme label (e.g., Streptavidin-β-Galactosidase).
- Bead Sealing and Signal Generation: Isolate and resuspend the beads. Mix them with a fluorescent substrate and load the mixture onto a SIMOA disc containing microwells. The system then seals each well with oil, statistically ensuring one bead per well. The enzyme on the bead converts the substrate into a fluorescent product within each sealed well.
- Imaging and Data Analysis: Use an integrated fluorescence microscope to image the wells. Software counts the number of fluorescent wells (positive for the protein) versus the total number of wells to provide an absolute digital count of the target protein molecules, allowing for precise quantification [76].
SIMOA Digital Detection Workflow
Protocol: AI-Enhanced Surface Plasmon Resonance (SPR) for Drug Binding Kinetics
Application: Label-free, real-time analysis of biomolecular interactions, such as the binding kinetics between a drug candidate and its protein target.
Principle: SPR detects changes in the refractive index on a sensor chip surface, which occur when a binding event increases the mass on the surface [76]. AI algorithms are applied to the sensorgram data to improve the accuracy of kinetic parameter estimation and correct for bulk refractive index effects or non-specific binding [79].
Workflow:
- System and Sensor Chip Preparation: Prime the SPR instrument with running buffer. Dock a sensor chip coated with a dextran matrix (e.g., CM5 chip). Activate the surface using standard amine-coupling chemistry.
- Ligand Immobilization: Dilute the purified protein target (ligand) in a low-salt buffer. Inject it over the activated chip surface to covalently immobilize it. Deactivate any remaining active groups.
- Analyte Binding and AI-Enhanced Data Acquisition: Dilute the drug candidate (analyte) in running buffer at a minimum of five different concentrations. Inject the analyte solutions over both the ligand surface and a reference flow cell. The SPR instrument records the association and dissociation phases in real-time.
- Data Processing and Model Fitting: Subtract the reference cell sensorgram to correct for bulk effects. Apply a machine learning-augmented fitting algorithm to the corrected data. The AI model, trained on diverse binding datasets, identifies the optimal kinetic model (e.g., 1:1 Langmuir binding) and calculates the association rate (ka), dissociation rate (kd), and equilibrium dissociation constant (KD) with high precision [79] [76].
AI-Enhanced SPR Kinetic Analysis
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of bio-optic technologies relies on a suite of specialized reagents and materials. The following table details key components for setting up and conducting experiments.
Table 3: Key Research Reagent Solutions for Bio-Optic Applications
| Reagent/Material | Function/Description | Example Applications |
|---|---|---|
| Genetically Encoded Fluorescent Proteins (e.g., GFP, RFP) | Enable visualization of specific proteins and dynamics in live cells without the need for external labeling [12]. | Live-cell imaging, tracking protein localization and expression [12]. |
| CRISPR-Cas Proteins & Guide RNA (gRNA) | The core components of CRISPR-based biosensors; gRNA provides specificity, and Cas proteins (e.g., Cas12, Cas13) provide signal amplification via trans-cleavage activity [76]. | Ultrasensitive nucleic acid detection for pathogen identification or genetic biomarkers [76]. |
| Functionalized Paramagnetic Beads | Micron-sized beads coated with antibodies or other capture molecules for immunomagnetic separation and concentration of analytes [76]. | Sample preparation for SIMOA and other bead-based digital assays [76]. |
| SPR Sensor Chips (e.g., Gold Film with Dextran Matrix) | The solid support where ligand immobilization occurs; the gold film enables plasmon excitation, and the matrix provides a surface for covalent coupling [76]. | Real-time, label-free interaction analysis (e.g., antibody-antigen, drug-receptor) [76]. |
| Surface-Enhanced Raman Scattering (SERS) Substrates | Nanostructured metallic surfaces (e.g., gold or silver nanoparticles) that dramatically enhance the weak Raman signal, enabling single-molecule detection [77] [80]. | Boosting sensitivity in Raman spectroscopy for biomarker detection and chemical analysis [77]. |
| Near-Infrared (NIR) Fluorophores | Fluorescent dyes excited by NIR light, which penetrates tissue more deeply and has lower autofluorescence background than visible light [77]. | In vivo imaging, deep-tissue microscopy, and photoacoustic imaging [77]. |
The landscape of bio-optic technologies offers a diverse and powerful toolkit for researchers and drug development professionals. As this comparative analysis demonstrates, the choice between imaging and sensing technologies—from the structural clarity of OCT to the molecular specificity of Raman spectroscopy and the ultra-sensitivity of CRISPR-based biosensors—must be guided by the specific experimental question, considering inherent trade-offs between resolution, sensitivity, invasiveness, and cost. The ongoing convergence with AI and the push toward miniaturization are poised to further overcome current limitations, enhancing the role of bio-optics as an indispensable component in the advancement of life sciences and precision medicine.
Bio-optics, the convergence of biological science with optical technologies, is fundamentally transforming modern healthcare, research, and diagnostic applications. This field leverages the interactions between light and biological matter to enable non-invasive imaging, precise molecular detection, and advanced therapeutic strategies. As we move through 2025, the bio-optics sector is characterized by rapid innovation, driven by established industry giants and agile emerging startups. These entities are pushing the boundaries of what is possible in precision medicine, diagnostic accuracy, and therapeutic development. For researchers, scientists, and drug development professionals, understanding the key players, their core technologies, and the experimental methodologies that underpin their innovations is crucial for navigating this dynamic landscape. This whitepaper provides a structured analysis of the sector, detailing the contributions of market leaders in optical components, specialists in medical imaging, and innovators in biological therapeutics and diagnostics, thereby offering a comprehensive resource for those engaged in bio-optics design and application research.
Established Industry Leaders in Optical Components
Long-standing corporations form the backbone of the bio-optics industry, providing the fundamental components and systems that enable advanced research and clinical applications. These companies are recognized for their extensive product portfolios, deep technical expertise, and global reach.
Hamamatsu Photonics
Hamamatsu Photonics is a pivotal player in the development and manufacture of core photodetection technologies for life sciences. The company's products are integral to systems requiring high-sensitivity light detection, such as flow cytometers and spectrometers. A key innovation announced for 2025 is the Hypereon, a new hybrid photosensor designed specifically for flow cytometry applications. It promises to enhance sensitivity and precision in cytometric detection, pushing the boundaries of research capabilities [81]. Beyond this, Hamamatsu offers a versatile range of spectroscopy products, including mini-spectrometers and FTIR engines, which facilitate precise light analysis from UV to NIR ranges for applications in environmental monitoring, quality control, and process analysis [82]. Their comprehensive portfolio also includes:
- Avalanche Photodiode (APD) Modules: Known for high-sensitivity detection of low-light signals, offering fast response and low noise [81].
- Multi-pixel Photon Counter (MPPC): Features high photon detection efficiency, ideal for analyzing rare events and dim fluorescence signals [81].
- SPAD Modules: Deliver single-photon precision with a digital output, suited for time-resolved fluorescence and applications requiring precise timing [81].
Additional Key Component Suppliers
The ecosystem of established optical component suppliers is diverse, supporting a wide array of bio-optics applications through specialized expertise.
- Carl Zeiss Meditec AG: A recognized pioneer in biomedical optics, particularly in Optical Coherence Tomography (OCT). The company leads the industry with high-performance imaging systems that combine spectral domain and swept-source technologies for high-resolution, cross-sectional imaging in ophthalmology and microsurgery [83].
- Topcon Corporation: Renowned for its robust OCT platforms tailored for diverse clinical applications, with a focus on rapid image acquisition and accessible, portable solutions for point-of-care diagnostics [83].
- Avantes: Specializes in high-end fibre-optic spectroscopy systems for measurements in the ultra-violet, visible, and near-infrared wavelengths. Their products range from small-form-factor instruments to high-sensitivity systems for demanding applications [82].
- Horiba Scientific: Offers a wide array of spectroscopy products, including high-quality spectrometers, monochromators, and systems for Raman spectroscopy, fluorescence spectroscopy, and spectroscopic ellipsometry [82].
- Teledyne Princeton Instruments: Designs and manufactures high-performance cameras (CCD, sCMOS, ICCD, EMCCD) and spectrographs for scientific research and industrial imaging, known for high sensitivity and low read noise [82].
Table 1: Established Leaders in Optical Components and Systems
| Company | Core Specialty | Example Product/Technology | Primary Application |
|---|---|---|---|
| Hamamatsu Photonics | Photodetection & Spectroscopy | Hypereon Hybrid Photosensor, Mini-spectrometers [81] [82] | Flow Cytometry, Light Analysis |
| Carl Zeiss Meditec AG | Medical Imaging | Spectral Domain OCT Systems [83] | Ophthalmology, Microsurgery |
| Topcon Corporation | Medical Imaging | Portable OCT Platforms [83] | Point-of-Care Diagnostics |
| Avantes | Spectroscopy | Fibre-optic Spectrometers (CompactLine, SensLine) [82] | UV-Vis-NIR Spectral Measurements |
| Horiba Scientific | Spectroscopy | Raman Spectrometers, Spectrographs [82] | Molecular Analysis, Material Science |
| Teledyne Princeton Instruments | Scientific Imaging | High-performance CCD & sCMOS Cameras [82] | Low-Light Imaging, Spectroscopy |
Specialized Innovators in Biomedical Imaging and Sensing
Beyond the broad-component suppliers, a class of companies has emerged with a sharp focus on applying optical principles to solve specific challenges in biomedical imaging and sensing. These innovators often develop integrated systems or specialized materials that are critical for advancing research and clinical practice.
OCT Imaging Specialists
Optical Coherence Tomography (OCT) is a non-invasive imaging technique that provides high-resolution, cross-sectional images of biological tissues. The OCT market is forecasted to grow from USD 2.18 billion in 2025 to USD 3.32 billion by 2030, driven by demand for advanced diagnostic solutions [83]. Key innovators in this space include:
- Heidelberg Engineering GmbH: Excels in delivering high-definition OCT systems renowned for exceptional image quality, robust data management, and interoperability. Their systems are widely adopted in both clinical and research settings for advances in biomarker identification and personalized healthcare [83].
- Optovue, Inc.: Acknowledged for transforming OCT accessibility through ultra-high speed and swept-source platforms. Their systems provide comprehensive anterior and posterior segment imaging capabilities with real-time, quantitative analytics for ophthalmic care [83].
- Santec Corporation: Distinguished as a strategic supplier of advanced swept-source modules and precision optical components. Their expertise in wavelength agility and light source coherence underpins the development of next-generation OCT platforms capable of higher imaging depths and speeds [83].
Standardization and Phantom Technology
The reliability and accuracy of biomedical optical sensing depend heavily on calibration and standardization. QUEL Imaging addresses this critical need as a leader in biomedical optical characterization tools. The company is the only North American supplier of tissue-equivalent optical phantoms—reference targets that mimic the optical properties of human tissue [84]. In a significant November 2025 announcement, QUEL Imaging acquired specialized time-of-flight (ToF) optical characterization equipment and assets from the Institut National d'Optique (INO). This transfer strengthens QUEL's OptiBlox platform and its capability to provide standardized, reproducible optical characterization from ultraviolet (UV) through short-wave infrared (SWIR) [84]. This ensures that researchers and device manufacturers can validate and calibrate their optical sensing technologies against a known benchmark, which is essential for clinical translation.
Emerging Companies and Startups in Biotech and Bio-optics
The bio-optics landscape is continually refreshed by emerging companies that leverage cutting-edge technologies to address unmet needs in diagnostics and therapeutics. These startups often operate at the intersection of biology, optics, and data science, pioneering novel approaches.
AI-Driven Drug Discovery and Diagnostics
Several emerging companies are harnessing artificial intelligence to accelerate discovery and enhance diagnostic precision.
- BillionToOne: A precision diagnostics company that utilizes its proprietary Quantitative Counting Template (QCT) technology to count DNA molecules at single-molecule resolution. This technology powers their UNITY Fetal Risk Screen, a non-invasive prenatal test that assesses fetal risk for numerous severe genetic conditions from a maternal blood sample. The company also offers liquid biopsy tests for oncology, helping to personalize and monitor cancer treatment [85].
- Insilico Medicine: A clinical-stage biotechnology company that uses a generative AI-powered platform (Pharma.AI) for end-to-end drug discovery and development. Their platform integrates biology, chemistry, and clinical development with deep learning models to design precise molecular compounds and discover new targets, with a focus on oncology, fibrosis, and immunology [85].
- Sumatrix Biotech: This startup combines artificial intelligence with advanced computational biology to accelerate the drug discovery process. Their AI algorithms analyze complex biological data to uncover novel drug candidates, with a particular focus on treatments for rare genetic disorders and oncology [86].
Novel Therapeutic Platforms
Other startups are building innovative platforms for next-generation therapies.
- Nurix Therapeutics: A clinical-stage biopharmaceutical company developing degrader-based medicines that harness the cell's natural protein degradation machinery (the ubiquitin-proteasome system). Their fully AI-driven discovery engine is focused on creating therapies for cancer and inflammatory diseases that are untreatable with traditional approaches [85].
- Crinetics Pharmaceuticals: Dedicated to developing oral, nonpeptide therapies for rare endocrine diseases and related tumors. Their pipeline includes investigational treatments for conditions like acromegaly and Cushing's disease, aiming to provide meaningful new options for patients [85].
- Hera Biotech: Focuses on addressing the invasive and time-consuming diagnosis of endometriosis. The company is developing innovative gene-based diagnostic tools that use genomic biomarkers and single-cell microfluidic analysis to identify the condition at its earliest stages, enabling personalized treatment plans [86].
Table 2: Emerging Innovators in Biotech and Bio-optics
| Company | Technology Focus | Key Innovation | Primary Application |
|---|---|---|---|
| BillionToOne | Precision Diagnostics | Quantitative Counting Template (QCT) [85] | Non-invasive Prenatal Screening, Liquid Biopsy |
| Insilico Medicine | AI-Driven Drug Discovery | Generative AI Platform (Pharma.AI) [85] | Novel Drug Target Identification & Design |
| Nurix Therapeutics | Targeted Protein Degradation | Degrader-based Medicines [85] | Oncology, Inflammatory Diseases |
| Crinetics Pharmaceuticals | Endocrinology Therapeutics | Oral, Nonpeptide Therapies [85] | Rare Endocrine Diseases & Tumors |
| Hera Biotech | Diagnostic Tools | Gene-based Diagnostics & Microfluidics [86] | Endometriosis Diagnosis & Treatment |
| MxT Biotech | Manufacturing Technology | Microfluidic Gene Therapy Production [86] | Scalable Gene Therapy Manufacturing |
Experimental Protocols in Bio-optics Research
Robust and reproducible experimental methodologies are the foundation of innovation in bio-optics. The following protocols detail common and advanced procedures in the field.
Protocol: Time-of-Flight Optical Characterization of Tissue Phantoms
This methodology, recognized as a gold standard in peer-reviewed publications and central to QUEL Imaging's recent asset acquisition, is used to quantitatively measure the optical properties of materials [84].
1. Principle: Time-of-Flight (ToF) spectroscopy characterizes how light propagates through a scattering medium, like tissue. A short pulse of light is injected into the sample. The temporal distribution of transmitted photons is measured, which reveals key optical properties—namely the absorption coefficient (μa) and the reduced scattering coefficient (μs').
2. Materials and Reagents:
- Tissue-Equivalent Phantom: The sample under test (e.g., QUEL Imaging OptiBlox or legacy INO Biomimic phantom) [84].
- Pulsed Light Source: A laser diode or supercontinuum laser capable of generating picosecond or femtosecond pulses.
- High-Speed Detector: A photomultiplier tube (PMT) or single-photon avalanche diode (SPAD) with a timing resolution of <100 ps.
- Time-Correlated Single Photon Counting (TCSPC) Module: Electronics to record the arrival time of individual photons relative to the laser pulse.
- Calibration Standards: Phantoms with known optical properties for system validation.
3. Procedure: a. System Calibration: Measure the instrument response function (IRF) by placing a reflective material in the sample position or using a phantom with known, very low scattering. b. Sample Mounting: Position the tissue phantom securely between the light source and the detector, ensuring proper optical alignment. c. Data Acquisition: Emit the pulsed light source and use the TCSPC module to record the temporal point spread function (TPSF)—the histogram of photon arrival times. d. Data Analysis: Fit the measured TPSF to a solution of the light diffusion equation using an iterative algorithm. This fitting process extracts the numerical values of μa and μs' for the phantom at the specific wavelength used.
4. Applications: This technique is critical for validating and calibrating any optical device used in medicine, such as those for fluorescence-guided surgery or near-infrared spectroscopy, ensuring their measurements are accurate and comparable across devices and studies [84].
Protocol: Hypereon Photodetector Performance Characterization in Flow Cytometry
This protocol outlines the key experiments to validate the performance of a new photodetector, such as the Hypereon hybrid photosensor, for use in a flow cytometry system [81].
1. Principle: To evaluate the detector's sensitivity, signal-to-noise ratio (SNR), and dynamic range by measuring its response to fluorescently labeled cells or standardized beads under controlled conditions.
2. Materials and Reagents:
- Flow Cytometer Setup: equipped with the Hypereon photodetector and standard lasers (e.g., 488 nm, 640 nm).
- Fluorescent Calibration Beads: A set of beads with known, stable fluorescence intensities across a range of brightness.
- Labeled Cell Sample: e.g., Jurkat cells stained with a titration series of a fluorescent antibody (e.g., CD3-PE).
- Buffer: Phosphate Buffered Saline (PBS).
3. Procedure: a. Dark Current Measurement: Block all light to the detector and record the output signal over time to determine the baseline noise (dark count). b. Sensitivity and Detection Limit: Run the dimmest fluorescent beads and a negative control (unstained beads). Record the fluorescence signal. The detection limit is defined as the signal intensity that produces an SNR greater than 3. c. Linearity and Dynamic Range: Run a series of calibration beads with increasing fluorescence intensity. Plot the measured signal output against the expected intensity to verify linearity and identify the upper limit of the dynamic range. d. Spectral Characterization: Use different fluorescent dyes (e.g., FITC, PE, APC) excited by appropriate lasers to measure the detector's photon detection efficiency across its operational wavelength range. e. Biological Sample Analysis: Compare the resolution of dim and bright populations in the stained cell sample against data acquired with a conventional photomultiplier tube (PMT) or avalanche photodiode (APD).
4. Data Analysis: Key performance metrics include:
- Signal-to-Noise Ratio (SNR):
(Mean Signal - Mean Background) / Standard Deviation of Background - Resolution Index: The ability to distinguish between dim and bright populations, often calculated using the
(Mean Bright - Mean Dim) / (√(SD_Bright² + SD_Dim²))formula.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimentation in bio-optics relies on a suite of specialized reagents and materials. The following table details key items referenced in the protocols and company technologies.
Table 3: Essential Research Reagents and Materials for Bio-optics Experiments
| Item Name | Function/Brief Explanation | Example Use Case |
|---|---|---|
| Tissue-Equivalent Optical Phantoms (QUEL OptiBlox) | Mimics the optical properties (scattering, absorption) of human tissue; serves as a calibration standard [84]. | Device calibration for fluorescence-guided surgery systems. |
| Fluorescent Calibration Beads | Polystyrene beads embedded with precise amounts of fluorophore; provide a stable signal for instrument calibration [81]. | Determining the sensitivity and linearity of a flow cytometer's detector. |
| Time-Correlated Single Photon Counting (TCSPC) Module | Electronics that measure the time between a laser pulse and the detection of a single photon with high precision [82]. | Time-of-Flight spectroscopy for quantifying tissue optical properties. |
| Hybrid Photodetector (e.g., Hypereon) | A photosensor combining the advantages of PMTs and APDs for high sensitivity and fast response in flow cytometry [81]. | Detecting dim fluorescence signals from rare cell populations. |
| Specific Fluorescent Antibodies | Antibodies conjugated to fluorophores; bind to specific cell surface or intracellular targets for detection. | Staining cells for analysis by fluorescence-activated cell sorting (FACS). |
| Pulsed Laser Source | A laser that emits light in short, defined pulses (picosecond to nanosecond duration). | Providing the excitation pulse for time-resolved fluorescence or ToF measurements. |
Technology and Workflow Visualization
The following diagrams, generated using Graphviz DOT language, illustrate the core logical relationships between key bio-optics technologies and a standard experimental workflow for detector characterization.
Bio-optics Technology Ecosystem Map
Photodetector Characterization Workflow
The bio-optics industry in 2025 is a vibrant and critical engine for progress in life sciences and medicine. The landscape is healthily balanced between the sustained innovation of established giants like Hamamatsu Photonics and Carl Zeiss Meditec, who provide the foundational technologies, and the disruptive potential of emerging players like BillionToOne and QUEL Imaging, who apply these technologies in novel ways to solve specific diagnostic and standardization challenges. The strategic acquisition of INO's assets by QUEL Imaging underscores a mature focus on standardization and reproducibility, which is essential for the clinical translation of optical technologies [84]. Looking forward, the sector's trajectory points toward greater integration of artificial intelligence and machine learning at all stages, from target discovery and experimental design to data analysis [87] [88]. Furthermore, the industry is likely to see continued consolidation through mergers and acquisitions as companies strive to build comprehensive, end-to-end solutions. For researchers and drug development professionals, staying abreast of these players, their technologies, and the underlying methodologies is not merely an academic exercise but a strategic necessity for leveraging the full power of light-based technologies to advance human health.
Bio-optics represents a multidisciplinary field that combines optical technologies with biological sciences to develop advanced methods for medical diagnostics, therapeutic applications, and biological research [89]. This field focuses on utilizing light-based technologies to visualize, analyze, and manipulate biological structures, often at the cellular or molecular level, enabling non-invasive, precise, and real-time analysis [69] [89]. The global bio-optics market has witnessed significant growth in recent years thanks to advancements in optical technologies, increasing research and development activities in the life sciences, and rising demand for minimally invasive medical procedures [12]. This whitepaper provides an in-depth analysis of regional market leadership patterns across North America, Europe, and Asia-Pacific, framed within the context of bio-optics design and application research for scientific and drug development professionals.
The scope of bio-optics encompasses a wide range of products and applications, including microscopy systems, spectroscopy devices, optical coherence tomography systems, biophotonics tools, and optical sensors [12]. Applications across healthcare, pharmaceutical research, environmental monitoring, and agriculture define the market's breadth, with each application driving innovation and demand based on specific end-use needs [69]. The continuous growth of biomedical research and life sciences has significantly benefited the bio-optics market, with optical techniques being widely used in areas such as cell biology, neuroscience, genetics, and drug discovery [12].
Regional Market Analysis
Quantitative Regional Market Assessment
Table 1: Global Bio-Optics Market Regional Breakdown
| Region | Market Share (2024) | Market Size (2024) | Projected CAGR | Key Growth Drivers |
|---|---|---|---|---|
| North America | 35-38% [69] [90] | $1.1 Billion (application market) [69] | 6.7% [69] [91] | Advanced healthcare infrastructure, high R&D expenditure, early technology adoption [69] [91] |
| Europe | 28% [69] | $900 Million (application market) [69] | 6.3% [12] | Strong pharmaceutical & life sciences sectors, regulatory support, research collaborations [69] [12] |
| Asia-Pacific | 27% [69] | $850 Million (application market) [69] | 13.54% [90] | Healthcare infrastructure investments, rising healthcare awareness, government initiatives [69] [91] |
| Rest of World | ~10% [69] | $350 Million (application market) [69] | Varies | Emerging investments in healthcare technology [69] |
Table 2: Market Segmentation Analysis by Application and Technology
| Segment Category | Leading Segment | Market Position | Key Applications |
|---|---|---|---|
| Application | Cancer Diagnostics [12] [89] | Dominant segment [12] [89] | Early detection, tumor margin assessment, treatment monitoring [12] |
| Device | Optical Coherence Tomography [12] | Dominant segment [12] | Ophthalmology, cardiology, dermatology, oncology [12] |
| Technology | Raman Spectroscopy [12] | Dominant segment [12] | Molecular analysis, disease biomarker identification, drug interaction monitoring [12] |
| End-user | Hospitals [89] | Major segment [89] | Cancer detection, microsurgery, infection identification, blood oxygen monitoring [89] |
North American Market Leadership
North America maintains its position as the dominant region in the global bio-optics market, accounting for approximately 35-38% of the global share [69] [90]. This leadership stems from several structural advantages, including advanced healthcare infrastructure, high R&D expenditure, and early adoption of innovative medical technologies [69] [91]. The United States represents the largest market within the region, driven by robust healthcare spending that reached $4.5 trillion in 2022, approximately $13,493 per capita [89]. The presence of leading research institutions, technology firms, and substantial government funding through agencies like the NIH and NSF further accelerates bio-optics innovation and adoption in the region [90].
The aging population in North America represents a significant driver for bio-optics market growth, with increasing demand for healthcare solutions that can diagnose and manage chronic diseases more effectively [92]. Bio-optics plays a crucial role in enabling early disease detection and management, particularly in applications such as cancer diagnostics, where optical imaging technologies provide real-time, high-resolution tissue imaging for early identification of malignant cells [89]. The region's leadership is also reinforced by strategic collaborations between academia and industry, as well as the presence of major market players focusing on innovations in optical imaging systems, biosensors, and diagnostic platforms [89].
European Market Strengths
Europe holds the second-largest share of the global bio-optics market at approximately 28% [69], with particular strength in the medical diagnostics segment [12]. The region's market is characterized by strong healthcare policies, widespread adoption of innovative medical technologies, and extensive collaborations between research institutions and healthcare providers [69] [91]. The European market benefits from stringent environmental regulations that drive demand for bio-optic solutions in environmental monitoring applications, alongside well-established pharmaceutical and life sciences sectors that invest heavily in research and development [12].
The United Kingdom stands out as a particularly dominant country within the European bio-optics landscape, with a thriving biomedical research community and renowned universities driving advancements in bio-optics technologies [12]. The UK's National Health Service (NHS) has integrated bio-optics technologies into its diagnostic and treatment protocols, contributing to their widespread adoption [12]. The country's focus on precision medicine and personalized healthcare further drives the demand for advanced bio-optics technologies, positioning the UK as a key innovation hub within the European market [12].
Asia-Pacific Growth Trajectory
The Asia-Pacific region represents the fastest-growing market for bio-optics technologies, with a projected CAGR of 13.54% from 2025 to 2034 [90]. This remarkable growth trajectory is fueled by expanding healthcare access, increasing government initiatives, growing healthcare awareness, and rising environmental concerns [69] [91]. The region's bio-optics market was valued at approximately $850 million in 2024 [69], with expectations for continued expansion as healthcare infrastructure develops and adoption of advanced medical technologies increases.
Countries like China, Japan, and India are making significant investments in healthcare infrastructure and biotechnology sectors, driving demand for bio-optics solutions [91] [92]. China has particularly made remarkable strides in bio-optic research and development, with rapid adoption of technologies like optical coherence tomography in ophthalmology and dermatology [92]. The growing geriatric population in the region also contributes to market expansion, as aging demographics increase demand for diagnostic and therapeutic solutions that address age-related health challenges [90].
Growth Drivers and Market Opportunities
Key Growth Drivers
Technological Advancements: Continuous innovations in optics, nanotechnology, and artificial intelligence are propelling the bio-optic market forward [92]. These innovations improve the resolution, accuracy, and efficiency of bio-optic devices, driving demand across healthcare, diagnostics, and environmental monitoring [92]. Advancements in fluorescence imaging techniques have been particularly transformative, with novel fluorescent probes exhibiting improved brightness, photostability, and specificity for targeting specific biomarkers or cellular structures [12].
Demand for Non-Invasive Diagnostics: Growing preference for non-invasive diagnostic tools represents a significant market driver, with patients and healthcare providers increasingly seeking safer, more comfortable alternatives to traditional invasive procedures [89] [92]. This trend fosters the growth of bio-optic technologies such as optical coherence tomography, photoacoustic imaging, and wearable biosensors [92]. The non-invasive nature of these technologies enhances patient comfort, accelerates recovery, and reduces healthcare risks [89].
Aging Population Demographics: The global aging population is increasing demand for healthcare solutions that can effectively diagnose and manage chronic diseases [92]. With the global aging population expected to reach 2.1 billion by 2050, a substantial market is developing for biophotonics applications in age-related diseases [90]. Bio-optics plays a crucial role in enabling early detection and management of conditions prevalent in older demographics [92].
Environmental Monitoring Requirements: Rising concerns about environmental sustainability are boosting demand for bio-optic sensors in environmental monitoring applications [92]. Governments and industries worldwide are seeking innovative solutions to track pollutants and protect ecosystems, creating new opportunities for bio-optic technologies [69] [92]. Optical sensors are increasingly deployed for detecting pollutants and ensuring ecosystem health, supporting regulatory compliance and sustainability initiatives [69].
Emerging Opportunities
Point-of-Care Applications: The growing emphasis on point-of-care applications represents a significant opportunity for bio-optics market expansion [12]. Bio-optics technologies enable rapid and accurate diagnostics at the point of care, particularly valuable in remote or resource-limited settings where access to centralized laboratories is limited [12]. Portable and robust bio-optics devices provide essential diagnostic capabilities, enabling healthcare professionals to make informed decisions without delays [12].
Wearable Bio-Optic Devices: The rise of wearable bio-optic devices has enabled continuous monitoring of physiological parameters like glucose levels, heart rate, and oxygen saturation [92]. These devices are becoming critical in managing chronic conditions, particularly in diabetes and cardiovascular diseases, by providing real-time data to both patients and healthcare providers [92]. The integration of bio-optics with telemedicine platforms further enhances remote monitoring capabilities [12].
AI and Machine Learning Integration: The combination of artificial intelligence with bio-optic technologies is creating new opportunities for enhanced diagnostic accuracy and speed [92]. AI algorithms can process data from bio-optic devices to identify patterns that might be missed by human analysis, particularly in imaging diagnostics where AI enhances the ability to detect and diagnose conditions like cancer, cardiovascular diseases, and neurological disorders [92].
Precision Agriculture Applications: Bio-optics is finding expanding applications in agriculture, where optical sensors monitor crop health, soil conditions, and detect pests [92]. This opportunity is expected to grow as farmers adopt precision agriculture techniques to improve crop yield, reduce waste, and increase sustainability [92]. The push toward precision farming and sustainable crop management represents a significant growth avenue for bio-optics technologies [69].
Experimental Protocols in Bio-Optics Research
Fluorescence Imaging Experimental Protocol
Table 3: Research Reagent Solutions for Fluorescence Imaging
| Reagent/Equipment | Function | Application Example |
|---|---|---|
| Genetically Encoded Fluorescent Proteins | Enable visualization of specific proteins within live cells | Tracking protein localization and dynamics [12] |
| Novel Fluorescent Probes | Target specific biomarkers with improved brightness and photostability | Cancer cell identification and tumor boundary visualization [12] |
| High-resolution Fluorescence Microscopy | Provides detailed imaging of cellular and molecular structures | Studying neuronal activity via calcium imaging [12] |
| Multiphoton Microscopy | Enables deeper tissue imaging with reduced phototoxicity | In vivo imaging of tissue structures [90] |
| Optical Filters and Improved Detectors | Enhance image quality, sensitivity, and resolution | Signal detection and noise reduction [12] |
Methodology: Fluorescence imaging protocols begin with sample preparation and labeling using appropriate fluorescent probes or genetically encoded fluorescent proteins [12]. For cellular imaging, cells are cultured under optimal conditions and transfected with plasmids encoding fluorescent proteins if necessary. Tissues may require sectioning and staining with fluorescent antibodies or dyes. The imaging process involves configuring the fluorescence microscope with appropriate excitation and emission filters matched to the fluorophores used [12]. Laser power and detection sensitivity must be optimized to maximize signal-to-noise ratio while minimizing photobleaching and phototoxicity. For time-lapse imaging, environmental control maintaining temperature, humidity, and CO2 levels is essential [12]. Image acquisition parameters including exposure time, z-stack intervals, and time intervals between frames are set based on experimental requirements. Post-acquisition processing may include background subtraction, contrast enhancement, and quantitative analysis of fluorescence intensity, localization, or dynamics [12].
Optical Coherence Tomography Experimental Protocol
Methodology: Optical Coherence Tomography (OCT) protocols begin with sample preparation appropriate for the application. For clinical ophthalmology, this may involve pupil dilation; for tissue imaging, samples may require mounting in stabilizing media [12]. The OCT system is calibrated according to manufacturer specifications, ensuring proper alignment of reference and sample arms. Scanning parameters are set based on sample type and resolution requirements, including scan depth, area, and density [12]. For in vivo imaging, motion stabilization techniques may be necessary. Image acquisition involves capturing cross-sectional slices or volumetric data sets, with real-time monitoring to ensure quality. Post-processing typically includes noise reduction, segmentation of tissue layers or structures, and quantitative analysis of morphological features [12]. In advanced applications, functional OCT techniques may measure blood flow, polarization properties, or spectroscopic features [12].
Raman Spectroscopy Experimental Protocol
Methodology: Raman spectroscopy protocols begin with sample preparation that minimizes fluorescence interference and preserves native state [12]. Solid samples may require no preparation, while liquids might need containment in appropriate cuvettes. The Raman system is calibrated using a standard reference material such as silicon to verify wavenumber accuracy and system performance [12]. Laser power and integration time are optimized to achieve sufficient signal-to-noise ratio while avoiding sample damage. Spectral acquisition involves collecting scattered light from the sample illuminated with monochromatic laser light, with multiple accumulations often used to improve signal quality [12]. Post-processing steps typically include cosmic ray removal, background subtraction, and normalization. Multivariate analysis techniques such as principal component analysis (PCA) may be employed for complex biological samples to identify spectral patterns corresponding to different molecular compositions [12].
Market Challenges and Restraints
Despite the promising growth trajectory, the bio-optics market faces several significant challenges that could impact regional development and technology adoption:
Regulatory Hurdles: Regulatory challenges, particularly in healthcare applications, can delay the approval and commercialization of bio-optics technologies [92]. The complexity of meeting safety and efficacy standards across different regions can slow the introduction of new products to the market [12] [92]. Bio-optics technologies, especially those used in medical applications, are subject to rigorous regulatory approval processes involving extensive testing, safety evaluations, and clinical trials to ensure efficacy, safety, and quality [12].
High Development Costs: Developing cutting-edge bio-optics devices requires significant investment in research and development, which can be a barrier for many companies, especially startups [92]. High costs associated with prototyping, testing, and manufacturing can limit market entry and innovation [92]. The substantial financial resources required for equipment and training further compound these challenges, particularly in cost-sensitive markets [90].
Limited Accessibility in Developing Regions: Limited accessibility in developing regions serves as a significant restraint for the bio-optics market, hindering its widespread adoption and potential impact on healthcare [90]. In these regions, inadequate infrastructure, including lack of reliable power sources and limited healthcare facilities, poses challenges for integrating advanced bio-optics technologies [90]. Economic constraints also limit financial resources available for healthcare investments, making it difficult for institutions to afford necessary equipment and training [90].
Market Adoption Barriers: Despite technological advancements, widespread adoption of bio-optics devices in clinical settings and consumer healthcare can be slow due to factors such as cost, training requirements, and skepticism about new technologies [92]. The need for specialized expertise to operate sophisticated bio-optics equipment and interpret results creates additional adoption barriers, particularly in resource-limited settings [90].
Future Outlook and Regional Projections
The future of the bio-optics market appears highly promising, with expected growth driven by the integration of advanced photonic technologies and artificial intelligence, leading to smarter diagnostic and analytical tools [69]. Emerging opportunities include wearable bio-optical sensors, point-of-care diagnostics, and personalized medicine applications [69]. Over the next 5 to 10 years, expanding applications in telemedicine, environmental sustainability, and agricultural efficiency are poised to significantly contribute to market expansion globally [69].
North America is expected to maintain its leadership position through the forecast period, supported by continuous technological innovation, strong R&D infrastructure, and high healthcare expenditure [92]. The region's focus on personalized medicine and early disease detection will continue to drive demand for advanced bio-optics solutions [89]. Europe will likely maintain its strong market position, bolstered by supportive regulatory frameworks and cross-border research collaborations [69] [12]. The Asia-Pacific region is projected to experience the most rapid growth, potentially reshaping global market shares as healthcare infrastructure develops and technology adoption accelerates [90] [92].
The competitive landscape is expected to intensify as companies focus on developing innovative products with enhanced resolution, improved precision, and non-invasive capabilities [89]. Key areas of innovation, including optical coherence tomography, fluorescence imaging, and biosensors, will be crucial for maintaining competitive advantage [89]. Companies that establish strong distribution networks, particularly in emerging markets, will be strategically positioned to expand their market presence [89]. Additionally, access to international markets and forming strong partnerships with hospitals, research labs, and pharmaceutical companies will be essential for success in this dynamic sector [89].
The global bio-optics market demonstrates distinct regional leadership patterns, with North America currently dominating, Europe maintaining a strong position with specific technological strengths, and Asia-Pacific exhibiting remarkable growth potential. Each region contributes uniquely to the advancement of bio-optics technologies, driven by regional capabilities, infrastructure, and strategic priorities. The continued expansion of the bio-optics market will depend on overcoming existing challenges related to regulation, cost, and accessibility, while capitalizing on emerging opportunities in point-of-care diagnostics, wearable devices, and AI integration.
For researchers, scientists, and drug development professionals, understanding these regional dynamics is crucial for strategic planning, collaboration formation, and technology development. The ongoing innovation in bio-optics design and applications promises to significantly impact healthcare outcomes, research capabilities, and environmental monitoring efforts worldwide. As regional markets evolve, the global bio-optics landscape will likely become more integrated, with cross-regional collaborations and knowledge exchange accelerating technological advancements and market growth.
Bio-optics, the field dedicated to the development and application of optical technologies for biological and medical purposes, has become a cornerstone of modern clinical research and therapeutic development. This field integrates advanced optical imaging, sensing, and data analysis to provide non-invasive, quantitative assessments of disease progression and treatment efficacy. The transition of bio-optics from an observational tool to a quantitative measurement technique has empowered researchers to validate clinical impact with unprecedented precision [93]. This whitepaper examines case studies in ophthalmology and oncology to demonstrate how bio-optics technologies are driving innovation in clinical validation, supporting drug development, and ultimately improving patient care through rigorous, data-driven approaches.
The fundamental principle underlying quantitative bio-optics is that microscopy and imaging produce more than just visual representations; they contain meaningful measurements that can provide critical insights into biological processes [93]. Proper quantification requires careful planning and decision-making at every step of the experimental workflow, from sample preparation through image acquisition, analysis, and data interpretation. This interconnectedness demands a "reverse workflow" approach where desired endpoints inform necessary experimental steps and controls [93]. The following case studies illustrate how this methodology is applied in real-world clinical contexts to validate therapeutic efficacy and safety profiles.
Ophthalmology Case Study: Home OCT for Neovascular AMD Monitoring
Clinical Context and Validation Challenge
Neovascular age-related macular degeneration (nAMD) requires frequent monitoring via optical coherence tomography (OCT) to detect fluid changes that guide treatment decisions. The clinical validation challenge was to determine whether home-based OCT (HOCT) could provide reliable fluid detection comparable to in-office OCT (IO-OCT), thereby potentially reducing treatment burden and improving patient outcomes through more frequent monitoring [94]. This validation was essential for establishing HOCT as a viable tool for decentralized clinical trials and remote patient management.
The pivotal trial aimed to validate the usability and visualization performance of the Notal Home OCT system. The study design addressed key clinical questions: Could patients successfully self-operate the device? Could the collected images provide clinically actionable data? And could the system accurately identify the presence or absence of fluid—the key biomarker for treatment decisions in nAMD? This validation was conducted under the framework of a prospective, multicenter study approved by an institutional review board and conducted in accordance with the Declaration of Helsinki [94].
Experimental Protocol and Methodology
The "Home OCT Fluid Visualization Agreement Study" employed a rigorous methodological approach to validate the home OCT system. The study enrolled patients with nAMD who were trained to perform self-operations of the HOCT device at home. Participants performed daily scans, which were transmitted to the Notal Vision Monitoring Center (NVMC) for processing and review by a reading center (RC) [94].
The core validation methodology included:
- Device and Setting: The Notal Home OCT system was used by patients in their home environment, with scans transmitted to the NVMC for processing.
- Comparator: In-office OCT images were acquired using commercial spectral-domain OCT systems (Heidelberg Spectralis or Zeiss Cirrus).
- Image Analysis: Both HOCT and IO-OCT images were evaluated by a reading center for the presence of intraretinal hyporeflective spaces (IRO), subretinal hyporeflective spaces (SRO), and total retinal hyporeflective spaces (TRO).
- Statistical Measures: The primary endpoints were positive percent agreement (PPA) and negative percent agreement (NPA) for fluid detection between HOCT and IO-OCT, calculated with confidence intervals using a bootstrap method [94].
The study utilized a modified visualization analysis population (mVAP) that included all qualified HOCT scans with a manufacturer signal quality index (MSI) of ≥25. This quality threshold ensured that only technically adequate images were included in the primary analysis, a critical methodological consideration for validating remote imaging systems [94].
Quantitative Results and Clinical Implications
The home OCT pivotal trial generated substantial quantitative data validating its clinical utility. The results demonstrated that home OCT provides reliable detection of retinal fluid compared to in-office OCT, supporting its use for monitoring nAMD patients in decentralized settings.
Table 1: Home OCT Fluid Detection Agreement with In-Office OCT
| Fluid Type | Positive Percent Agreement (PPA) | Negative Percent Agreement (NPA) | Overall Agreement |
|---|---|---|---|
| Any Fluid | 90.2% (95% CI: 86.6-93.0) | 89.4% (95% CI: 86.9-91.6) | 89.7% (95% CI: 87.7-91.5) |
| Intraretinal Fluid (IRO) | 75.6% (95% CI: 68.3-81.7) | 96.4% (95% CI: 94.9-97.6) | 93.0% (95% CI: 91.1-94.6) |
| Subretinal Fluid (SRO) | 83.3% (95% CI: 77.0-88.3) | 94.4% (95% CI: 92.4-96.0) | 91.7% (95% CI: 89.6-93.4) |
Source: Adapted from Ophthalmology Science, 2025 [94]
These results validated the home OCT system as a clinically viable tool for monitoring nAMD patients. The high agreement rates across different fluid types demonstrated that the technology could effectively identify the key biomarkers that guide anti-VEGF treatment decisions in nAMD. This capability enables more frequent monitoring of disease activity without requiring clinic visits, potentially allowing for earlier detection of fluid recurrence and more personalized treatment approaches [94].
The clinical implications of these findings are substantial. First, they support the use of home monitoring for nAMD in both clinical practice and decentralized clinical trials. Second, the technology addresses the significant treatment burden associated with frequent monitoring visits, potentially improving patient quality of life. Third, the continuous stream of data enables a more dynamic understanding of individual patient disease activity patterns, paving the way for truly personalized treatment regimens based on individual patient needs rather than fixed dosing schedules.
Research Reagent Solutions for OCT Validation
Table 2: Key Research Reagents and Materials for OCT Clinical Validation
| Reagent/Material | Function in Validation | Application Specifics |
|---|---|---|
| Spectral-Domain OCT Systems | Reference standard for image comparison | Heidelberg Spectralis or Zeiss Cirrus systems used for in-office imaging |
| Manufacturer Signal Quality Index (MSI) | Quality threshold for image inclusion | MSI ≥25 required for primary analysis to ensure technical adequacy |
| Hyporeflective Space Classification | Standardized fluid categorization | Enables consistent identification of IRO, SRO, and TRO across imaging platforms |
| Bootstrap Statistical Method | Robust agreement analysis | Provides confidence intervals for PPA and NPA estimates through resampling |
Ophthalmology Case Study: Deep Learning-Based OCT for Skin Pathology
Clinical Context and Validation Challenge
Recent advancements in cellular-resolution optical coherence tomography (OCT) have created opportunities for high-resolution, non-invasive clinical diagnosis of skin pathologies. The clinical validation challenge was to develop and validate a deep learning-based approach for quantitative analysis of in vivo human skin layers and keratinocyte nuclei from OCT images, enabling standardized metrics for clinical assessment of skin structures [95]. This technology addresses a critical need in dermatology for non-invasive diagnostic tools that can provide cellular-level information without requiring tissue biopsy.
The segmentation of skin layers and cellular structures presents significant technical challenges due to the complexity and variability of biological tissues. Traditional computer vision algorithms often struggle to adapt to this diversity, requiring time-consuming adjustments for color filters and feature extractors [95]. The validation goal was to demonstrate that deep learning models could overcome these limitations and provide accurate, reproducible measurements of skin morphology that align with established clinical findings.
Experimental Protocol and Methodology
The study employed a sophisticated methodological approach to develop and validate the deep learning-based segmentation model for OCT images of human skin. The protocol integrated advanced imaging technology with state-of-the-art computational approaches to achieve cellular-level segmentation.
The experimental methodology included:
- Imaging System: A Mirau-based full-field OCT (FF-OCT) system manufactured by Apollo Medical Optics (Model# S100) with an axial resolution of 1.00 µm and lateral resolution of 1.35 µm was used for image acquisition.
- Dataset Composition: 305 B-scan OCT images were obtained from in vivo healthy human skin across diverse anatomical regions (leg, face, arm, back) from 139 total patients.
- Image Pre-processing: Images were resized to 1000 × 800 pixels for uniform resolution (0.5 µm/pixel), with contrast and luminance normalization applied. Cropping was implemented to focus on relevant tissue regions while excluding artifacts.
- Annotation Protocol: Annotations for keratinocytes and skin layers were provided by experts with biology and medicine backgrounds using an electronic pen and refined with an active contour model. Separate groups handled annotation and model training to prevent bias.
- Model Architecture: A U-Net architecture enhanced with deep supervision was implemented as the foundational framework. The model incorporated a deeply supervised learning objective function to handle the significant size difference between nuclei and skin layers, with separate consideration of global (skin layers) and local (nuclei) features [95].
The model's performance was evaluated using 5-fold cross-validation, with the Dice coefficient serving as the primary accuracy metric. This rigorous validation approach ensured that the model's performance could be generalized across different patients and skin regions.
Quantitative Results and Clinical Implications
The deep learning-based segmentation approach generated highly accurate quantitative measurements of skin structures, demonstrating strong correlation with established clinical knowledge of human skin morphology.
Table 3: Quantitative Measurements of Human Skin Structures via Deep Learning OCT Segmentation
| Skin Structure | Measured Value | Clinical Reference Range | Segmentation Accuracy |
|---|---|---|---|
| Stratum Corneum Thickness | 22.71 ± 17.20 µm | Aligns with clinical findings | Dice coefficient >85% across all structures |
| Epidermis Thickness | 66.44 ± 11.61 µm | ~50-150 µm in normal skin | Consistent performance across skin regions |
| Keratinocyte Nuclei Area | 17.21 ± 9.33 µm² | Matches histological expectations | Accurate nuclear boundary identification |
Source: Adapted from Biomedical Optics Express, 2025 [95]
The model achieved a Dice coefficient of 85.82% through 5-fold cross-validation, demonstrating high accuracy in joint segmentation for the stratum corneum, epidermis, dermis, and cell nuclei [95]. These results validated the approach as a clinically viable method for non-invasive skin analysis. The measurements obtained closely aligned with previously reported research on human skin structures, supporting the biological relevance of the quantitative outputs.
The clinical implications of this validation extend to multiple dermatological applications. The technology enables non-invasive, quantitative assessment of skin layers and cellular features that serve as essential benchmarks for prognosticating and predicting conditions like actinic keratosis, Bowen's disease, and basal cell carcinoma [95]. By providing reproducible measurements of skin morphology, the approach facilitates objective monitoring of disease progression and treatment response without requiring repeated biopsies. This capability is particularly valuable for long-term management of chronic skin conditions and for clinical trials evaluating new dermatological therapies.
Research Reagent Solutions for Skin OCT Analysis
Table 4: Essential Research Materials for Deep Learning-Based OCT Skin Segmentation
| Reagent/Material | Function in Validation | Application Specifics |
|---|---|---|
| Full-Field OCT System | High-resolution image acquisition | Apollo Medical Optics S100 with 1.00 µm axial and 1.35 µm lateral resolution |
| Electronic Pen Input | Precise annotation capability | Enables accurate boundary delineation for training data creation |
| Active Contour Model | Annotation refinement | Improves boundary accuracy through algorithmic optimization |
| U-Net Architecture | Deep learning framework | Base model for segmentation with encoder-decoder structure and skip connections |
| Deep Supervision | Training optimization | Handles size disparity between nuclei and skin layers in segmentation |
Experimental Design and Workflow Visualization
Quantitative Bioimaging Experimental Framework
The validation approaches in both ophthalmology case studies exemplify the principles of rigorous quantitative bioimaging experimentation. As outlined in the biologist's guide to quantitative bioimaging, these experiments require careful planning and decision-making at every stage, from sample preparation through image acquisition, analysis, and data interpretation [93]. The interconnectedness of these steps necessitates a holistic approach where decisions at one stage affect what is possible at others.
A critical principle in quantitative bioimaging is beginning with the end in mind—employing a "reverse workflow" in which the desired end result informs the necessary experimental steps and controls [93]. This approach was evident in both ophthalmology case studies, where the clinical need (remote monitoring of nAMD and non-invasive skin diagnosis) drove the technical development and validation strategy. This framework ensures that the resulting data and measurements effectively address the biological or clinical question being investigated.
Bio-optics Clinical Validation Workflow
Cross-Disciplinary Methodological Considerations
The validation of bio-optics technologies for clinical application requires addressing several cross-disciplinary methodological considerations that span both ophthalmology and oncology applications. These considerations ensure that the resulting data meets the rigorous standards required for clinical decision-making and therapeutic development.
Sample Preparation and Standardization In quantitative bioimaging, optimal sample preparation is fundamental to controlling for optical aberrations and enabling accurate measurements. For clinical applications, this translates to standardized imaging protocols that account for patient variability, positioning differences, and anatomical considerations. Both case studies implemented rigorous quality control measures—the home OCT study used a manufacturer signal quality index (MSI) threshold of ≥25, while the skin OCT study employed systematic pre-processing including resizing, contrast normalization, and cropping to eliminate artifacts [94] [95].
Image Acquisition Optimization The selection of appropriate image acquisition parameters is critical for generating quantitatively reliable data. This includes choosing appropriate spatial and temporal resolution, field of view, and signal-to-noise ratio based on the specific clinical question. The home OCT study balanced resolution with practical considerations for patient self-operation, while the skin OCT study utilized full-field OCT with cellular-level resolution (1.00 µm axial, 1.35 µm lateral) to capture the necessary detail for nuclear segmentation [94] [95].
Analytical Validation Framework Both case studies employed robust statistical approaches to validate their quantitative measurements. The home OCT study used positive and negative percent agreement with confidence intervals calculated via bootstrap methods, while the skin OCT study employed 5-fold cross-validation with the Dice coefficient as the primary accuracy metric [94] [95]. These approaches provide rigorous frameworks for establishing the technical performance of bio-optics technologies before their implementation in clinical decision-making.
The case studies presented in this whitepaper demonstrate the powerful role of bio-optics in validating clinical impact across medical specialties. The home OCT system for nAMD monitoring and the deep learning-based OCT for skin pathology both exemplify how advanced optical technologies, coupled with rigorous validation methodologies, can provide quantitative, clinically actionable data that addresses real-world healthcare challenges. These approaches enable more frequent monitoring, earlier detection of disease changes, and objective assessment of treatment response—capabilities that directly impact patient outcomes.
Future developments in bio-optics will likely focus on increasing integration with artificial intelligence and machine learning, enhancing portability and accessibility, and expanding multi-modal imaging approaches. The incorporation of AI is already evident in both case studies, from the deep learning segmentation of skin structures to the automated quality assessment of home OCT images [94] [95]. As these technologies mature, we can anticipate increased validation of bio-optics for decentralized clinical trials and remote patient monitoring, potentially transforming how healthcare is delivered across both ophthalmology and oncology.
The continued advancement of bio-optics as a quantitative discipline requires ongoing attention to methodological rigor, standardization, and validation against clinically relevant endpoints. By maintaining these standards while pursuing technological innovation, the field will continue to provide powerful tools for validating clinical impact and improving patient care across medical specialties.
Bio-optics, defined as the fusion of light-based technologies with biology and medicine, is rapidly transforming research, diagnostics, and therapy [10]. This field leverages the interaction of light with biological matter—through processes such as absorption, emission, and scattering—to enable non-contact, sensitive, and rapid characterization of biological systems [10]. Within this discipline, quantum dots (QDs) have emerged as a cornerstone nanomaterial. These are nanoscale semiconductor particles, typically between 1–20 nm, whose excitons are confined in all three spatial dimensions, leading to discrete energy levels and exceptional optical properties [96] [97]. Their high brightness, narrow and symmetric fluorescence emission, tunable photoluminescence based on size, and excellent photostability make them superior to traditional organic fluorophores for many bio-optical applications [96] [97]. The evolution of QDs has expanded from traditional cadmium-based semiconductors to include more biocompatible variants such as carbon quantum dots (CQDs) and green carbon dots (GCDs), which are synthesized sustainably from renewable biomass and align with the principles of green chemistry [98] [99]. The integration of these novel materials with artificial intelligence (AI) is forging a new paradigm in bio-optics design, enabling intelligent, data-driven systems for advanced healthcare solutions [99].
Table 1: Fundamental Properties and Advantages of Quantum Dots in Bio-Optics
| Property | Description | Advantage in Bio-Optics |
|---|---|---|
| Size-Tunable Emission | Bandgap energy inversely related to QD size; smaller dots emit higher energy (blue), larger dots emit lower energy (red) light [96]. | Enables multiplexed imaging and color-coded diagnostics with a single excitation source [100] [97]. |
| High Quantum Yield & Brightness | High efficiency in converting absorbed light into emitted light; core-shell structures (e.g., CdSe@ZnS) can further enhance yield [97]. | Allows for highly sensitive detection of low-abundance biomarkers and real-time tracking of biological processes [97]. |
| Broad Absorption & Narrow Emission | Can be excited by a wide range of wavelengths but emit light in a very narrow, symmetric band [96]. | Reduces background noise and crosstalk in complex biological samples, improving signal-to-noise ratio [96]. |
| Excellent Photostability | Resistant to photobleaching under prolonged illumination compared to organic dyes [100]. | Facilitates long-term, real-time imaging and monitoring of dynamic cellular events [100]. |
| Ease of Functionalization | Surface can be modified with organic/inorganic ligands, polymers, and biomolecules [98] [97]. | Permits targeting to specific cells (e.g., tumors), enhances biocompatibility, and enables integration into drug delivery systems [98]. |
AI-Driven Synthesis and Design of Novel Quantum Dots
The synthesis of quantum dots, particularly for precise biomedical applications, is a complex, multivariate process. Traditional optimization relying on empirical, trial-and-error methods is resource-intensive and struggles with reproducibility and scalability [99] [97]. The integration of Artificial Intelligence (AI), specifically machine learning (ML) and deep learning (DL), is revolutionizing this domain by establishing a computational–experimental feedback loop. AI models can predict optimal synthesis parameters—such as precursor type, temperature, reaction time, and pH—to produce QDs with targeted properties like specific fluorescence intensity, quantum yield, and particle size [99]. This data-driven approach can potentially reduce experimental iterations by over 80%, minimizing material consumption, energy use, and chemical waste, thereby aligning with the sustainability ethos of green carbon dots [99].
A key advancement in synthesis is the use of microfluidic technology, which provides precise control over reaction conditions compared to traditional batch reactors [97]. When combined with additive manufacturing (3D printing), this allows for the creation of sophisticated, custom-designed microreactors for scalable and cost-effective QD production [96]. AI algorithms can be integrated with these microfluidic systems for in-situ monitoring and real-time parameter adjustment, creating a closed-loop optimization framework that ensures high reproducibility and quality [99] [97].
Figure 1: AI-driven closed-loop workflow for the optimized synthesis of quantum dots, integrating predictive modeling, automated microfluidic reactors, and real-time analysis.
Table 2: AI and Microfluidic Applications in QD Synthesis
| AI/Microfluidic Technology | Function | Impact on QD Development |
|---|---|---|
| Supervised Machine Learning | Predicts material properties (quantum yield, cytotoxicity) from labeled synthesis data [99]. | Accelerates the design of QDs with predefined optical and biological characteristics. |
| Deep Learning (CNNs) | Analyzes photoluminescence spectra and microscopy images for high-resolution classification [99]. | Enables real-time quality control and anomaly detection during synthesis. |
| Additive-Manufactured Microfluidics | 3D-printed microreactors for precise fluid dynamics and parameter control [96]. | Overcomes limitations of traditional methods, enabling scalable, reproducible QD production. |
| Active Learning & Reinforcement | Guides experimental design by selecting the most informative next experiments [99]. | Drastically reduces the number of experiments needed, promoting sustainable discovery. |
Experimental Protocols and Research Toolkit
Protocol: Microfluidic Synthesis of Carbon Quantum Dots
This protocol details the synthesis of CQDs using a continuous-flow microfluidic reactor, ensuring superior control and reproducibility compared to batch methods [97].
- Precursor Preparation: Prepare an aqueous solution of small organic molecules (e.g., citric acid) or natural biomass extract (e.g., chitosan) as the carbon source. A second solution containing a passivating agent (e.g., polyethyleneimine) may be prepared separately [98] [97].
- Microreactor Setup: Prime a commercially available or additively-manufactured microfluidic chip. Use syringe pumps to independently control the flow rates of the precursor solutions into the chip's inlets [96] [97].
- Reaction and Hydrothermal Synthesis: Guide the mixed precursors through a microchannel configured as a heated reactor. Maintain a precise, elevated temperature (e.g., 180–250 °C) and pressure to facilitate the carbonization and passivation reactions. The residence time is controlled by adjusting the total flow rate and the length of the heated channel [97].
- Product Collection and Purification: Collect the crude CQD solution from the outlet. Purify the product by dialysis against deionized water or using size-exclusion chromatography to remove unreacted precursors and byproducts [98].
- Characterization: Analyze the synthesized CQDs using transmission electron microscopy (TEM) for size and morphology, UV-Vis and photoluminescence spectroscopy for optical properties, and Fourier-transform infrared spectroscopy (FTIR) for surface chemistry [98] [97].
Protocol: AI-Enhanced Analysis of QD-Based Protein Aggregation
This protocol employs QDs as fluorescent probes to study protein aggregation, a key process in neurodegenerative diseases, with AI-powered image analysis [100].
- Sample Preparation: Incubate the target protein (e.g., tau, amylin) under conditions that promote aggregation (specific pH, temperature, and time). Include experimental wells with potential aggregation inhibitors (e.g., rosmarinic acid) [100].
- QD Staining: Add functionalized QDs to the protein samples. The QDs bind non-specifically to the protein aggregates, providing high-contrast fluorescence labeling [100].
- Image Acquisition: Use fluorescence microscopy to capture 2D and 3D images of the QD-labeled aggregates over time. Confocal laser microscopy is used for high-resolution 3D structural analysis [100].
- AI-Based Image Analysis: Process the acquired images using a pre-trained deep learning model, such as a Convolutional Neural Network (CNN). The model is trained to identify, segment, and quantify aggregate features—such as size, density, distribution, and morphology—from the fluorescence signals [99] [100].
- Data Correlation and Inhibition Analysis: Correlate the AI-quantified aggregation metrics (e.g., standard deviation of aggregate distribution) with incubation time and inhibitor concentration. Calculate the half-maximal effective concentration (EC₅₀) of inhibitors from the dose-response data generated by the AI analysis [100].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for QD-Based Biomedical Research
| Reagent / Material | Function | Application Example |
|---|---|---|
| Cadmium-Free QDs (InP, Si, CQDs) | Fluorescent nanoprobes with low cytotoxicity [97]. | Safe in vivo bioimaging and biosensing [100] [97]. |
| Green Carbon Dots (GCDs) | Sustainably synthesized from biomass; biocompatible and fluorescent [99]. | Eco-friendly platform for drug delivery and diagnostic imaging [99]. |
| Functionalization Ligands | Modify QD surface with COOH, NH₂, or biotin for conjugation with biomolecules [98] [97]. | Targeted drug delivery to cancer cells; biosensor development [98]. |
| Microfluidic Chip | Miniaturized reactor for continuous, controlled QD synthesis [96] [97]. | Reproducible, high-throughput production of high-quality QDs. |
| Rosmarinic Acid | Model polyphenol compound with protein anti-aggregation activity [100]. | Inhibitor control in studies of amylin or tau protein aggregation [100]. |
Applications in Bio-Imaging, Diagnostics, and Therapeutics
The convergence of QDs and AI is creating powerful applications across the core areas of biophotonics: bioimaging, biosensing, and therapy [10].
In bioimaging, QDs are invaluable probes. Their size-tunable and narrow emission is ideal for multiplexed imaging, where different colored QDs can track multiple cellular targets simultaneously [100]. Near-infrared (NIR) emitting QDs (e.g., InAs) allow for deep-tissue imaging with minimal absorption and scattering, providing critical visual guidance during surgical procedures, such as tumor resection [100] [97]. Furthermore, the integration of DL models significantly enhances the analytical precision of these imaging platforms, enabling automated, real-time segmentation and analysis of complex biological structures from QD-derived images [99].
In diagnostics and biosensing, QDs form the basis of highly sensitive detection platforms.当他们与微流体芯片结合时,可以创建用于检测疾病生物标志物的芯片实验室设备 [97]. AI further boosts the capabilities of these platforms by interpreting complex sensor data, improving diagnostic sensitivity and specificity, and enabling the discovery of novel biomarker patterns [99].
In therapeutics, carbon-based QDs show significant promise in drug and gene delivery. Their rich surface chemistry allows for easy loading of therapeutic molecules, and their fluorescence enables real-time tracking of delivery vehicles [98] [99]. AI is instrumental in optimizing these nanocarriers by modeling drug-QD interactions and predicting release kinetics, paving the way for intelligent, stimuli-responsive delivery systems [99]. Additionally, QDs serve as effective agents for photothermal (PTT) and photodynamic therapy (PDT), where they convert absorbed light energy to heat or generate reactive oxygen species to destroy cancer cells [98].
Figure 2: The convergence of quantum dots and AI across key biomedical applications, creating a feedback loop for enhanced performance and intelligent design.
Challenges and Future Directions in Bio-Optics Integration
Despite the considerable promise, the path to the widespread clinical adoption of QD-based technologies is fraught with challenges. A primary constraint is the potential cytotoxicity of heavy-metal QDs (e.g., CdSe), which necessitates the development of robust core-shell structures or a full transition to safer alternatives like silicon, indium phosphide, or carbon dots [97]. Furthermore, the reproducibility and scalability of high-quality QD synthesis remain significant hurdles, even with advanced microfluidic approaches [96].
The integration of AI also faces its own set of limitations. The efficacy of AI models is heavily dependent on access to large, high-quality, and standardized datasets, which are currently scarce in QD research due to heterogeneous synthesis protocols and reporting [99]. There is also a critical need for explainable AI (XAI) frameworks to improve the interpretability of model predictions, especially for safety-critical applications like drug delivery [99].
Looking forward, the field is moving towards the concept of "Quantum Biophotonics," which explores the intersection of quantum technologies with biological systems [10]. The synergy between quantum computing and AI holds potential to address complex optimization problems in material design and to analyze biological data with unprecedented speed [101]. For successful clinical translation, future efforts must prioritize standardization of synthesis and characterization protocols, establish community-wide data-sharing practices, and navigate the necessary regulatory pathways for the approval of AI-enhanced nanomedicines [99] [10]. Addressing these challenges will solidify the role of intelligent QDs as a cornerstone of next-generation bio-optics and precision medicine.
Conclusion
Bio-optics stands as a cornerstone of modern biomedical research and clinical practice, driven by continuous technological refinement and the powerful integration of AI. The field is moving decisively towards miniaturized, point-of-care devices and non-invasive diagnostics, expanding its impact from personalized medicine to environmental monitoring. For researchers and drug development professionals, success will depend on navigating the regulatory landscape, leveraging cross-disciplinary collaborations, and adopting the synergistic potential of AI with optical technologies. The future of bio-optics is bright, promising not only enhanced diagnostic precision and therapeutic efficacy but also a fundamental shift towards more accessible and proactive healthcare solutions on a global scale.
References
- 1. Biophotonics: Optics and Biological Systems [https://avantierinc.com/resources/application-note/biophotonics-optics-and-biological-systems/]
- 2. What is Biophotonics Technology? Uses, How It Works & Top... [https://www.linkedin.com/pulse/what-biophotonics-technology-uses-how-works-fq4nc/]
- 3. Clinical Biophotonics [https://www.news-medical.net/life-sciences/Clinical-Biophotonics.aspx]
- 4. Bio-Optics: Design and Applications (BODA) [https://www.optica.org/events/meeting_archives/2025/bio-optics_design_and_application/]
- 5. Fundamentals of biophotonics - BIO -443 - EPFL [https://edu.epfl.ch/coursebook/fr/fundamentals-of-biophotonics-BIO-443]
- 6. : Biophotonics and Biological Systems - Shanghai Optics ... Optics [https://www.shanghai-optics.com/about-us/resources/technical-articles/biophotonics-optics-and-biological-systems/]
- 7. Biophotonics Market Demand & Growth Outlook 2025 to ... [https://www.futuremarketinsights.com/reports/global-biophotonics-market]
- 8. Shining a Light on the Future of Biophotonics [https://pubmed.ncbi.nlm.nih.gov/40364668/]
- 9. Biophotonic (nano)structures: from fundamentals to ... [https://pubs.rsc.org/en/content/articlelanding/2025/ra/d5ra03288a]
- 10. Shining a Light on the Future of Biophotonics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12245495/]
- 11. Light-Matter Interactions | Biophotonics Imaging Laboratory [https://biophotonics.illinois.edu/imaging-technology/light-matter-interactions]
- 12. Bio Optics Market: Global Technology Analysis and Forecast [https://www.maximizemarketresearch.com/market-report/bio-optics-market/189394/]
- 13. Biophotonics Market Size & Share Report, 2025 - 2034 [https://www.gminsights.com/industry-analysis/biophotonics-market]
- 14. Biophotonics: Strategic Market and Tech Overview [https://www.bccresearch.com/pressroom/pho/biophotonics-market-was-valued-at-$626-billion-in-2024?srsltid=AfmBOoqFTYwYNI8hqnS7G1klHIxBiTfJYYVl26Cw39WHdwnAI5od5tHV]
- 15. Bio-optics Market Latest Trends with Future Insights by 2031 [https://www.manchesterprofessionals.co.uk/article/business-management/93294/bio-optics-market-latest-trends-with-future-insights-by-2031]
- 16. Bio-optics Market's Growth Catalysts [https://www.datainsightsmarket.com/reports/bio-optics-182105]
- 17. Challenges and Opportunities in Smart Biosensing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455640/]
- 18. Biosensors Market 2025 To 2030 : Future, Product, ... [https://www.linkedin.com/pulse/biosensors-market-2025-2030-future-product-wearables-p-virkhe-xtmqf]
- 19. Recent Optical Coherence Tomography (OCT) Innovations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12108957/]
- 20. Deep Multiphoton Imaging [https://www.optica-opn.org/home/articles/volume_36/april_2025/features/deep_multiphoton_imaging/]
- 21. Multimodal microscope for optical coherence microscopy ... [https://pubmed.ncbi.nlm.nih.gov/41111488/]
- 22. Characterizing refractive index and thickness of biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3539195/]
- 23. Integrated two-photon and optoacoustic microscopy for ... [https://www.nature.com/articles/s41598-025-07819-4]
- 24. AAO 2025: The value of RGB imaging in OCT [https://www.ophthalmologytimes.com/view/aao-2025-the-value-of-rgb-imaging-in-oct]
- 25. Researchers use OCT imaging to uncover how the ... [https://www.optica.org/about/newsroom/news_releases/2025/researchers_use_oct_imaging_to_uncover_how_the_fallopian_tube_transports_embryos/]
- 26. Multiphoton Microscopy in the Biomedical Sciences XXV [https://spie.org/Publications/Proceedings/Volume/13324]
- 27. OCT system development | Biophotonics Imaging Laboratory [https://biophotonics.illinois.edu/research/optical-coherence-imaging/oct-system-dev]
- 28. New Raman Spectroscopy Method Boosts Drug ... [https://www.spectroscopyonline.com/view/new-raman-spectroscopy-method-boosts-drug-component-detection-accuracy-and-speed]
- 29. Streamlining Development with Raman Spectroscopy [https://www.bioprocessintl.com/product-characterization/streamlining-biopharmaceutical-development-and-manufacturing-a-detailed-exploration-of-raman-spectroscopy]
- 30. Fluorescence Microscopy Market Report 2025, with Major ... [https://www.businesswire.com/news/home/20250225931500/en/Fluorescence-Microscopy-Market-Report-2025-with-Major-Players-Bruker-Nikon-Olympus-Zeiss-Oxford-Instruments-and-Etaluma---ResearchAndMarkets.com]
- 31. Fluorescence imaging beyond intensity [https://www.embl.org/about/info/course-and-conference-office/events/lef25-01/]
- 32. A novel fluorescent probe, triphenylamine rhodamine-3- ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1653063/full]
- 33. Novel fluorescent probes constructed on the basis of ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267025011869]
- 34. Novel fluorescent probes with high signal-to-noise ratios ... [https://pubs.rsc.org/en/content/articlelanding/2025/ay/d5ay01401h]
- 35. A fluorescence lifetime separation approach for FLIM live- ... [https://pubmed.ncbi.nlm.nih.gov/41025451/]
- 36. United States Bio-Optics Market Latest Report [https://www.linkedin.com/pulse/united-states-bio-optics-market-latest-report-emerging-ktr7f/]
- 37. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 38. Artificial intelligence and machine learning in infectious ... [https://www.sciencedirect.com/science/article/pii/S0026265X25031509]
- 39. Wearable bioelectronics for cancer theranostics [https://www.nature.com/articles/s41378-025-01048-5]
- 40. Technologies for Quantifying the Particle Concentration of ... [https://pubmed.ncbi.nlm.nih.gov/41251186/]
- 41. Optica webinar: Optical phantoms for fluorescence guided ... [https://ncibt.ucdavis.edu/events/optica-webinar-optical-phantoms-fluorescence-guided-surgery-practical-insights-and]
- 42. Introduction to the bio-optics: design and application - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4679263/]
- 43. Emerging trends in AI-integrated optical biosensors for ... [https://pubs.rsc.org/en/content/articlelanding/2025/cc/d5cc04899k]
- 44. Advances in optical biosensors: Technologies and trends ... [https://pubmed.ncbi.nlm.nih.gov/41033727/]
- 45. Advances and challenges in portable optical biosensors for ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993624001225]
- 46. Review of Integrated Optical Biosensors for Point-of-Care ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7766912/]
- 47. Review of Integrated Optical Biosensors for Point-of-Care ... [https://www.mdpi.com/2079-6374/10/12/209]
- 48. Electrochemical vs. Optical Biosensors for Point-of-Care ... [https://www.mdpi.com/2227-9040/11/10/546]
- 49. About Optica Biophotonics Congress [https://www.optica.org/events/congress/biophotonics_congress/about/]
- 50. Advancements in photoacoustic detection techniques for ... [https://www.nature.com/articles/s44384-025-00005-w]
- 51. Intravital mesoscale optical imaging: challenges, ... [https://www.biophysics-reports.org/article/doi/10.52601/bpr.2025.250015]
- 52. Quantum Optical Techniques for Biomedical Imaging [https://arxiv.org/html/2511.03935v1]
- 53. Media - Caltech Optical Imaging Laboratory [https://coilab.caltech.edu/media]
- 54. MDR-compliant IFU translations: five common pitfalls to ... [https://novalins.com/mdr-compliant-ifu-translations-five-common-pitfalls-to-avoid-in-2025/]
- 55. 7 Vital Translation Requirements for Clinical Trials [https://www.conversis.com/insights/translation-requirements-for-clinical-trials]
- 56. 10 Clinical Trial Regulatory Changes Coming in 2025 [https://en.ennov.com/blog/clinical-blog/trial-regulatory-changes-coming-2025/]
- 57. ACA Language Access rules for 2025 - Part 1 [https://phrase.com/blog/posts/aca-section-1557-language-access-2025-guide/]
- 58. The Best Good Clinical Practice (GCP) Translator 2025 [https://x-doc.ai/articles/en/the-best-good-clinical-practice-gcp-translator]
- 59. Bio-Optics Market Size, Share, Growth & Forecast Report ... [https://www.marketresearchfuture.com/reports/bio-optics-market-38820]
- 60. Biophotonics Market Size, Share, Trends & Growth Report ... [https://www.snsinsider.com/reports/biophotonics-market-8492]
- 61. Biophotonics Market Forecast 2025-2032: Non-Invasive [https://www.openpr.com/news/3958756/biophotonics-market-forecast-2025-2032-non-invasive]
- 62. Journal of Bio-optics [https://www.sciltp.com/journals/jbo]
- 63. Artificial Intelligence-Guided PET Image Reconstruction ... [https://pubmed.ncbi.nlm.nih.gov/40858423/]
- 64. Machine Learning Approach for Signal Processing in ... [https://opg.optica.org/abstract.cfm?uri=BODA-2025-DTu3A.2]
- 65. Exploring the potential of generative artificial intelligence in ... [https://www.sciencedirect.com/science/article/pii/S258975002500072X]
- 66. From siloed data to breakthroughs: multimodal AI in drug ... [https://www.drugtargetreview.com/article/160597/from-siloed-data-to-breakthroughs-multimodal-ai-in-drug-discovery/]
- 67. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 68. Advanced workflow automation and scalable image ... [https://www.zeiss.com/microscopy/en/about-us/newsroom/press-releases/2025/partnership-concept-life-sciences.html]
- 69. Bio-optics Market By Application 2025 [https://www.linkedin.com/pulse/bio-optics-market-application-2025-green-leaf-solution-pro-7ljdf/]
- 70. State of the Art in Smart Portable, Wearable, Ingestible and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9185336/]
- 71. Wearable Sensors Market 2025-2035: Technologies, ... [https://www.idtechex.com/en/research-report/wearable-sensors-market-2025/1051]
- 72. Biophotonics Technology and Global Markets Report 2025 ... [https://finance.yahoo.com/news/biophotonics-technology-global-markets-report-140500495.html]
- 73. Miniaturized Photonic Devices Trends For Wearables And ... [https://www.photonicsonline.com/doc/miniaturized-photonic-devices-trends-for-wearables-and-medical-diagnostics-0001]
- 74. Biophotonics Technology Market 2025–2033: Strategic ... [https://www.linkedin.com/pulse/biophotonics-technology-market-20252033-strategic-insights-9mn3c/]
- 75. Top Wellness Device Trends Revolutionizing Your Health ... [https://ajprotech.com/blog/articles/smart-wellness-medical-devices-trends-transforming-health.html]
- 76. Optical biosensors for diagnosing neurodegenerative ... [https://www.nature.com/articles/s44328-025-00040-3]
- 77. Biophotonics Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/biophotonics-market]
- 78. Global Optical Bio Sensors Market Competitive Landscape ... [https://www.statsndata.org/report/optical-bio-sensors-market-172078]
- 79. Emerging trends in AI-integrated optical biosensors for point ... [https://pubs.rsc.org/en/content/articlehtml/2025/cc/d5cc04899k]
- 80. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 81. CYTO 2025 [https://www.hamamatsu.com/us/en/news/events/2025/CYTO-2025.html]
- 82. The latest spectroscopy products for 2025 [https://www.electrooptics.com/article/latest-spectroscopy-products-2025]
- 83. Top 7 Optical Coherence Tomography Companies to ... [https://www.researchandmarkets.com/articles/key-companies-in-optical-coherence-tomography?srsltid=AfmBOooj5R8SEqv9LomCJ9QQvolV5As256L9308Et2MHqFJTmGvM5GuF]
- 84. QUEL Imaging and INO Announce Technology Transfer to ... [https://www.wboy.com/business/press-releases/cision/20251118NE26921/quel-imaging-and-ino-announce-technology-transfer-to-advance-biomedical-optics]
- 85. The Top 25 Biotech and Life Sciences Companies of 2025 [https://thehealthcaretechnologyreport.com/the-top-25-biotech-and-life-sciences-companies-of-2025/]
- 86. Emerging Biotech Startups to Watch Out For in 2025 [https://www.mrlcg.com/resources/blog/emerging-biotech-startups-to-watch-out-for-in-2025/]
- 87. Top Bio-optics Companies & How to Compare Them (2025) [https://www.linkedin.com/pulse/top-bio-optics-companies-how-compare-them-2025-alphavista-research-vfbme/]
- 88. Top Bio-optics Companies & How to Compare Them (2026) [https://www.linkedin.com/pulse/top-bio-optics-companies-how-compare-them-2026-jl4cf/]
- 89. Bio-optics Market Size, Share, Growth Forecast 2032 [https://www.analystviewmarketinsights.com/reports/report-highlight-bio-optics-market]
- 90. Biophotonics Market Size to Hit USD 226.18 Billion by 2034 [https://www.precedenceresearch.com/biophotonics-market]
- 91. Bio-optics Market Trends: Reginal Size Share Analysis for ... [https://www.linkedin.com/pulse/bio-optics-market-trends-reginal-size-share-analysis-2031-kw7gf/]
- 92. Bio-optic Market Report: Trends, Forecast and Competitive ... [https://www.researchandmarkets.com/reports/6167978/bio-optic-market-report-trends-forecast?srsltid=AfmBOoo1oTq8xIhedIo957pBDwnwErtXMSV_7_5kbKsYvqxWsPjvkyTh]
- 93. A biologist's guide to planning and performing quantitative ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3002167]
- 94. Pivotal Trial Validating Usability and Visualization ... [https://www.sciencedirect.com/science/article/pii/S2666914525000703]
- 95. Quantitative assessment of in vivo nuclei and layers of ... [https://opg.optica.org/boe/abstract.cfm?uri=boe-16-4-1528]
- 96. Redefining Quantum Dot Synthesis with Additive- ... [https://www.mdpi.com/2571-8800/8/2/18]
- 97. Microfluidic synthesis of quantum dots and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9417800/]
- 98. Biomedical application of carbon quantum dots: A review [https://www.sciencedirect.com/science/article/pii/S2667056924000889]
- 99. Green carbon dots in the era of AI: sustainable synthesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12614371/]
- 100. Quantum Dots for Biomedical Applications - Special Issue [https://www.mdpi.com/journal/ijms/special_issues/Z93EGW809E]
- 101. Integrating artificial intelligence and quantum computing [https://www.sciencedirect.com/science/article/pii/S266630742500035X]