Beyond the Wrist: Evaluating Wearable Optical Sensor Accuracy Against Clinical Gold Standards in Biomedical Research
This article provides a critical analysis of the accuracy and reliability of wearable optical sensors when benchmarked against established clinical gold standards.
Beyond the Wrist: Evaluating Wearable Optical Sensor Accuracy Against Clinical Gold Standards in Biomedical Research
Abstract
This article provides a critical analysis of the accuracy and reliability of wearable optical sensors when benchmarked against established clinical gold standards. Tailored for researchers, scientists, and drug development professionals, it explores the foundational technology of sensors like photoplethysmography (PPG), examines methodological challenges in data acquisition and analysis, outlines prevalent accuracy limitations and optimization strategies, and reviews validation frameworks and comparative performance metrics. The scope encompasses applications from remote patient monitoring to clinical trials, addressing both current capabilities and the path toward regulatory-grade acceptance.
The Science of Light: How Wearable Optical Sensors Work and Their Core Applications
Fundamental Principles of Photoplethysmography (PPG) and Optical Sensing
Photoplethysmography (PPG) is an optical sensing technique that measures blood volume changes in the microvascular bed of tissue. PPG functions by emitting light into the skin and measuring the amount of light reflected or transmitted to a photodetector [1]. As blood volume in the vessels changes with each cardiac cycle, light absorption varies, creating a pulsatile waveform known as the PPG signal. The increasing integration of PPG into consumer wearables has sparked critical research evaluating its accuracy against clinical-grade monitoring systems, forming a crucial thesis in modern digital health validation [1] [2].
This technology fundamentally differs from electrocardiography (ECG), which measures the heart's electrical activity directly. While ECG provides precise R-R intervals for heart rate variability (HRV) analysis, PPG estimates these intervals from peripheral blood volume changes, a metric sometimes termed pulse rate variability (PRV) [3] [4]. This distinction is central to understanding the performance characteristics and appropriate applications of PPG-based monitoring.
Fundamental Principles and Signal Acquisition
Core Operating Mechanism
The PPG system relies on a simple yet effective physical principle: the interaction of light with biological tissue. A typical PPG sensor contains a light-emitting diode (LED) that shines light (often green, though infrared and red are also used) onto the skin, and an adjacent photodetector that measures the intensity of the reflected light [1]. The resulting signal contains two primary components:
- AC Component: A pulsatile waveform synchronous with the cardiac cycle, caused by changes in arterial blood volume.
- DC Component: A relatively constant baseline related to light absorbed by non-pulsatile arterial blood, venous blood, and other tissues.
The AC component, typically representing only 1-2% of the total signal, provides the primary data for cardiovascular parameter estimation [1].
From Raw Signal to Physiological Parameters
The journey from raw PPG signal to clinically relevant metrics involves sophisticated signal processing. The raw signal is susceptible to various artifacts, particularly from motion and ambient light, requiring robust filtering algorithms. Once cleaned, the pulsatile characteristics are analyzed to extract specific features including pulse rate, pulse rate variability, and respiratory rate, with advanced algorithms further enabling detection of conditions like atrial fibrillation [5].
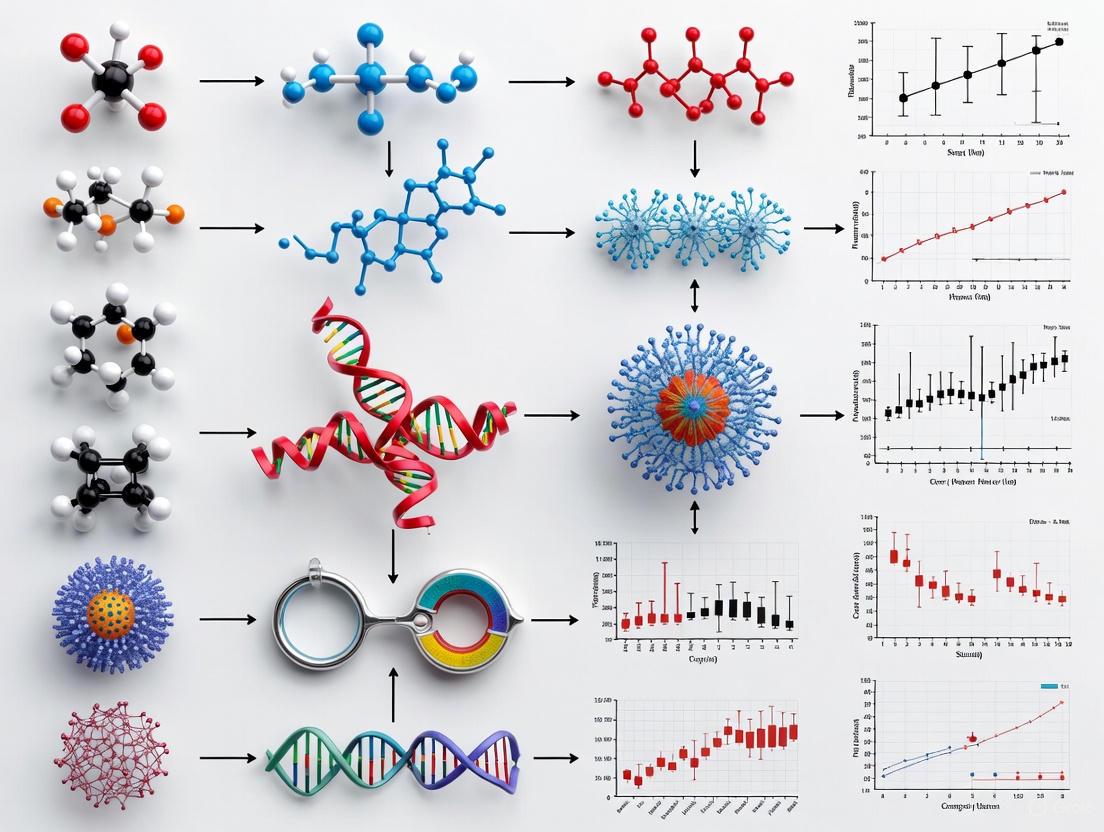
The following diagram illustrates the complete PPG signal processing workflow from acquisition to parameter extraction:
Diagram: PPG Signal Processing Workflow. The pathway illustrates the transformation of raw optical measurements into clinically useful parameters through multiple processing stages.
Quantitative Performance Comparison: PPG Versus Gold Standards
Heart Rate and Heart Rate Variability Measurement
PPG demonstrates strong performance in measuring heart rate (HR) under controlled conditions, though its accuracy is influenced by multiple factors. At rest, wearables show mean absolute errors of approximately 2 beats per minute (bpm) with correlations to ECG ranging from moderate to excellent [1]. For heart rate variability (HRV), recent comparative studies reveal more nuanced performance characteristics.
Table 1: PPG vs. ECG for Heart Rate Variability Measurement [3] [4]
| Measurement Condition | HRV Parameter | Reliability (ICC) | Mean Bias | Limits of Agreement | Clinical Interpretation |
|---|---|---|---|---|---|
| Supine Position | RMSSD | 0.955 (Excellent) | -2.1 ms | Narrow | High agreement with ECG gold standard |
| SDNN | 0.980 (Excellent) | -5.3 ms | Narrow | High agreement with ECG gold standard | |
| Seated Position | RMSSD | 0.834 (Good) | -8.1 ms | Wider | Reduced agreement in seated posture |
| SDNN | 0.921 (Excellent) | -6.2 ms | Wider | Maintained good agreement | |
| Aged >40 Years | RMSSD/SDNN | Reduced Agreement | N/A | Wider | Age impacts signal reliability |
| Female Participants | RMSSD/SDNN | Reduced Agreement | N/A | Wider | Sex influences measurement consistency |
Atrial Fibrillation Detection
For arrhythmia detection, particularly atrial fibrillation (AF), PPG-based smartwatches and ECG-based patches both show excellent diagnostic performance in meta-analyses, though with distinct strengths.
Table 2: Atrial Fibrillation Detection Accuracy [6] [7]
| Device Type | Pooled Sensitivity (%) | 95% Confidence Interval | Pooled Specificity (%) | 95% Confidence Interval | Heterogeneity (I²) |
|---|---|---|---|---|---|
| PPG Smartwatches | 97.4 | 96.5–98.3 | 96.6 | 94.9–98.3 | 3.16% (Sensitivity) 75.94% (Specificity) |
| ECG Smart Chest Patches | 96.1 | 91.3–100.8 | 97.5 | 94.7–100.2 | 94.59% (Sensitivity) 79.1% (Specificity) |
Advanced PPG algorithms have further demonstrated robust AF burden tracking capabilities, with one model showing a correlation coefficient (rₛ) of 0.8788 for AF episode duration proportion and sensitivity of 91.5% compared to Holter monitoring [5].
Specialized Population Applications
PPG validation extends to pediatric populations, where unique physiological and behavioral characteristics present distinct challenges. In a study of children with congenital heart disease or suspected arrhythmias, the Corsano CardioWatch demonstrated 84.8% accuracy for HR measurement compared to Holter monitoring, with good agreement (bias: -1.4 BPM) [8]. Accuracy was notably higher at lower heart rates (90.9% vs 79% at high HR) and declined during intense movement, highlighting the impact of activity level on measurement reliability [8].
Experimental Protocols and Methodologies
Comparative Validation Study Design
Rigorous validation of PPG performance against gold standard references follows standardized experimental protocols:
Participant Selection and Preparation
- Recruitment of healthy adults across age groups (typically 18-70 years) without known cardiovascular conditions [3] [4]
- Exclusion criteria include medications affecting cardiovascular function, smoking, and pregnancy
- Controlled for skin phototype (Fitzpatrick I-III) due to known PPG signal variation with pigmentation [3] [4]
- Stabilization period of 1 minute before formal data collection to establish baseline physiology
Device Configuration and Synchronization
- Simultaneous data collection from PPG and ECG devices with time synchronization
- PPG sensors typically worn on non-dominant arm (e.g., Polar OH1) to minimize motion artifact [3]
- ECG chest straps (e.g., Polar H10) positioned according to manufacturer specifications [3] [4]
- Raw data acquisition enabled via manufacturer SDKs for signal-level analysis
Testing Conditions and Variables
- Body position systematically varied (supine vs. seated) using standardized surfaces
- Measurement durations compared (2-minute vs. 5-minute recordings) per HRV guidelines
- Environmental controls: quiet, dark rooms to minimize sensory interference
- Instruction to participants: relax, breathe normally, keep eyes closed
Signal Processing and Data Analysis
Data Acquisition
- PPG sensors collect peak-to-peak intervals (PPI) for pulse rate variability [3]
- ECG devices record R-R intervals for heart rate variability [3] [4]
- Sampling rates typically ≥100 Hz to ensure sufficient temporal resolution
Signal Preprocessing
- Bandpass Butterworth digital filtering to remove baseline drift and high-frequency noise [5]
- Artifact detection and rejection algorithms for motion-corrupted segments
- Pulse waveform quality assessment for inclusion criteria
Statistical Comparison
- Intraclass correlation coefficients (ICC) for device reliability assessment
- Bland-Altman analysis with mean bias and limits of agreement
- Calculation of sensitivity, specificity, and accuracy metrics for arrhythmia detection
- Statistical significance threshold typically set at p < 0.05
Research Reagents and Essential Materials
Table 3: Key Research Equipment for PPG Validation Studies
| Device Category | Example Products | Primary Function | Research Application |
|---|---|---|---|
| PPG Sensors | Polar OH1, Apple Watch, Garmin wearables | Optical HR and PRV monitoring | Consumer-grade PPG validation [3] [1] |
| ECG Reference Devices | Polar H10 chest strap, Holter monitors | Gold-standard electrical heart activity recording | Validation benchmark for PPG accuracy [3] [8] |
| Medical Reference Systems | Spacelabs Healthcare Holter, 12-lead ECG | Clinical-grade cardiac monitoring | Highest accuracy reference standard [8] [5] |
| Data Acquisition Tools | Polar SDK, Elite HRV app, MATLAB | Raw signal data extraction and processing | Signal-level analysis and algorithm development [3] [5] |
| Analysis Software | HRVTool MATLAB toolbox, custom JavaScript apps | HRV parameter calculation, statistical analysis | Standardized metric extraction and comparison [3] |
Factors Influencing PPG Accuracy and Reliability
Physiological and Demographic Considerations
Multiple subject-specific factors significantly impact PPG signal quality and measurement accuracy:
Body Position: PPG demonstrates excellent reliability with ECG in the supine position (ICC = 0.955-0.980 for HRV parameters) but only good to excellent reliability in seated positions (ICC = 0.834-0.921), with wider limits of agreement [3] [4]. This degradation likely results from postural influences on pulse arrival time (PAT) and pulse transit time (PTT), which affect the timing relationship between cardiac electrical activity and peripheral pulse arrival [3].
Age and Sex: Agreement between PPG and ECG is less consistent in participants over 40 years and in females, suggesting effects of age-related vascular changes and sex-specific autonomic regulation or vascular properties [3] [4]. These demographic factors should be considered in study design and result interpretation.
Skin Properties: PPG signal quality varies with skin pigmentation, with most validation studies appropriately controlling for Fitzpatrick skin phototype [3] [9]. This factor has clinical implications, as optical sensors may overestimate oxygen saturation in darker skin tones, potentially creating health disparities [9].
Measurement Context and Environment
Activity Level: PPG accuracy is highest at rest and declines during physical activity, with wrist-worn devices particularly susceptible to motion artifacts from arm movement [8] [1]. Accuracy decreases as heart rate increases, with one pediatric study showing declines from 90.9% at low HR to 79.0% at high HR for wrist-worn PPG [8].
Recording Duration: For HRV assessment, marginal differences exist between 2-minute and 5-minute recordings in resting conditions [3]. However, shorter recordings are more vulnerable to noise and motion artifacts, particularly for PPG-based sensors [3].
Environmental Factors: Ambient light interference, temperature variations, and sensor-skin contact quality all significantly impact PPG signal integrity [1]. Controlled measurement environments are essential for high-quality data collection.
Photoplethysmography represents a compelling balance between convenience and accuracy in physiological monitoring. The technology demonstrates sufficient accuracy for many applications including basic heart rate monitoring, atrial fibrillation screening, and trend-based health assessment. However, fundamental physiological differences from electrical cardiac measurement and susceptibility to various confounders necessitate careful interpretation of results.
The choice between PPG-based wearables and clinical-grade monitoring systems ultimately depends on the specific use case. For diagnostic applications and clinical decision-making, ECG-based systems remain the gold standard. For longitudinal monitoring, trend analysis, and patient engagement, PPG-based wearables offer an unparalleled combination of convenience and capability. As algorithm development continues and validation studies expand to more diverse populations, the role of PPG in both clinical and research settings will continue to evolve, potentially narrowing but unlikely to completely eliminate the performance gap with clinical gold standards.
Accuracy of Wearable Optical Sensors vs Clinical Gold Standards Research
Wearable optical sensors, particularly those using photoplethysmography (PPG), have transitioned from consumer fitness trackers to potential tools in clinical research and healthcare monitoring. These devices offer unprecedented opportunities for continuous, longitudinal health data collection outside traditional clinical settings. For researchers and drug development professionals, understanding the accuracy and limitations of these technologies compared to established clinical gold standards is paramount. This comparison guide objectively evaluates the performance of wearable optical sensors across key biometric measurements, supported by experimental data and detailed methodologies from validation studies.
The fundamental technological divide between consumer wearables and clinical equipment lies in their measurement approaches and regulatory oversight. Medical-grade devices typically use transmittance pulse oximetry, where light passes through tissue (e.g., fingertip or earlobe), and are FDA-regulated with strict accuracy requirements. In contrast, smartwatches and fitness trackers use reflectance PPG, where light emitted into the skin is reflected back to the sensor, and generally operate without FDA oversight for wellness tracking [10].
Comparative Accuracy of Key Biometrics
Heart Rate Monitoring
Heart rate monitoring represents the most established biometric measured by wearable technologies. Research-grade validation typically compares PPG-based wearable heart rate measurements against electrocardiogram (ECG) as the gold standard.
Table 1: Heart Rate Monitoring Accuracy Across Devices and Conditions
| Device Type | Condition | Mean Absolute Error (BPM) | Reference Standard | Population | Citation |
|---|---|---|---|---|---|
| Consumer Wearables (Pooled) | At Rest | 4.6 (8.4) BPM | ECG | Sinus Rhythm | [11] |
| Consumer Wearables (Pooled) | At Rest | 7.0 (11.8) BPM | ECG | Atrial Fibrillation | [11] |
| Consumer Wearables (Pooled) | Peak Exercise | 13.8 (18.9) BPM | ECG | Sinus Rhythm | [11] |
| Consumer Wearables (Pooled) | Peak Exercise | 28.7 (23.7) BPM | ECG | Atrial Fibrillation | [11] |
| Corsano 287 Bracelet | At Rest | 94.6% accuracy within 100ms | ECG | Cardiology Patients | [12] |
| Multiple Devices | Physical Activity | 30% higher error vs. rest | ECG | All Skin Tones | [13] |
A comprehensive 2020 study systematically explored heart rate accuracy across skin tones using the Fitzpatrick scale, finding no statistically significant difference in accuracy across skin tones during various activities. However, the study revealed significant differences between devices and activity types, with absolute error during activity being 30% higher on average than during rest [13]. This has important implications for researchers designing studies involving physical activity protocols.
For patients with cardiac conditions, a validation study of the Corsano 287 bracelet demonstrated high correlation with ECG for heart rate (R = 0.991) and RR-intervals (R = 0.891), with comparable results across subgroups based on skin type, hair density, age, BMI, and gender [12].
Blood Oxygen Saturation (SpO₂)
Blood oxygen saturation represents a more challenging metric for wearable optical sensors, with significant technical and anatomical limitations affecting accuracy.
Table 2: SpO₂ Monitoring Accuracy: Wearables vs. Medical Devices
| Device | Measurement Method | Overall Accuracy | Mean Absolute Error | Gold Standard Comparison | Citation |
|---|---|---|---|---|---|
| Medical Pulse Oximeters | Transmittance | ~2% (FDA regulated) | ARMS ≤3% (required) | N/A | [10] |
| Apple Watch Series 7 | Reflectance PPG | 84.9% | 2.2% | Medical Oximeter | [10] |
| Garmin Venu 2s | Reflectance PPG | Not reported | 5.8% | Medical Oximeter | [10] |
| Withings ScanWatch | Reflectance PPG | 78.5% | Not reported | Medical Oximeter | [10] |
| Smartwatches (Pooled) | Reflectance PPG | 78.5%-84.9% | Variable | Arterial Blood Gas | [14] [10] |
A 2025 study comparing SpO₂ measurements in COPD patients found only a moderate correlation between smartwatch readings and arterial blood gas analysis (ICC: 0.502), which remains the clinical gold standard. The Bland-Altman analysis revealed a mean error of -1.79% between the smartwatch and blood gas measurements, with limits of agreement ranging from -7.43% to 4.87% [14].
Technical limitations significantly impact SpO₂ accuracy. Medical devices use transmittance oximetry through blood-perfused areas (finger, toe, earlobe), while smartwatches use reflectance PPG on the wrist where tendons and bones reduce blood perfusion and signal-to-noise ratio [10]. This fundamental anatomical limitation presents ongoing challenges for wrist-worn SpO₂ monitoring.
Atrial Fibrillation Detection
The episodic nature of atrial fibrillation makes continuous monitoring particularly valuable, and wearable technologies show promising but variable performance.
Table 3: Atrial Fibrillation Detection Accuracy
| Device Type | Sensitivity | Specificity | Number of Studies | Population | Citation |
|---|---|---|---|---|---|
| ECG Smart Chest Patches | 96.1% | 97.5% | 15 | Multiple | [6] |
| PPG Smartwatches | 97.4% | 96.6% | 15 | Multiple | [6] |
| Apple Watch | 98% | Not reported | Not specified | Compared to traditional ECG | [6] |
A 2025 systematic review and meta-analysis of 15 studies found both ECG smart chest patches and PPG-based smartwatches demonstrated excellent performance in atrial fibrillation detection. PPG smartwatches showed slightly higher sensitivity (97.4% vs. 96.1%), while ECG chest patches exhibited marginally greater specificity (97.5% vs. 96.6%) [6].
Emerging Biometrics: Hydration Monitoring
While less established than heart rate or SpO₂ monitoring, hydration tracking represents an emerging application of wearable sensor technology. A 2025 scoping review identified multiple sensor technologies being developed, including electrical, optical, thermal, microwave, and multimodal sensors. Each approach has distinct advantages and limitations [15] [16].
Experimental Protocols and Validation Methodologies
Laboratory Validation Protocols
Rigorous validation of wearable sensors requires carefully controlled laboratory protocols comparing wearable measurements against clinical gold standards.
Diagram 1: Laboratory validation workflow
A comprehensive validation protocol for patients with lung cancer includes both laboratory and free-living components. The laboratory protocol consists of structured activities: variable-time walking trials, sitting and standing tests, posture changes, and gait speed assessments. All activities are video-recorded for validation, with wearable sensor data compared against video-recorded observations [17].
Specific laboratory protocols typically include:
- Seated rest to measure baseline (4 minutes)
- Paced deep breathing (1 minute)
- Physical activity (walking to increase HR up to 50% of recommended maximum, 5 minutes)
- Seated rest (washout from physical activity, ~2 minutes)
- Typing task (1 minute) [13]
These controlled conditions allow researchers to assess device performance across different physical states and movement intensities.
Free-Living Validation Protocols
Free-living validation complements laboratory studies by assessing device performance in real-world conditions. A typical protocol involves participants wearing devices continuously for 7 days except during water-based activities. Outcome measures include step count, time spent at different physical activity intensity levels, posture, and posture changes. Agreement between devices is assessed using Bland-Altman plots, intraclass correlation analysis, and 95% limits of agreement [17].
Statistical Analysis Methods
Validation studies employ rigorous statistical methods to assess agreement between wearable sensors and gold standards:
- Bland-Altman plots visualize agreement between methods, plotting differences against averages
- Intraclass correlation coefficients (ICC) measure reliability and agreement
- Mean absolute error (MAE) quantifies average magnitude of errors
- Sensitivity and specificity calculate diagnostic accuracy for condition detection
- Mixed effects models account for repeated measures and multiple variables [14] [13] [12]
Research Reagent Solutions and Essential Materials
Table 4: Research-Grade Tools for Wearable Validation Studies
| Tool Category | Specific Examples | Research Function | Key Features |
|---|---|---|---|
| Gold Standard References | ECG Patches (Bittium Faros 180), Arterial Blood Gas Analysis, Medical-Grade Pulse Oximeters | Provide validated reference measurements for comparison | Clinical accuracy, Regulatory approval |
| Research-Grade Wearables | Empatica E4, ActivPAL3 micro, ActiGraph LEAP | High-precision research devices | Raw data access, Extensive validation |
| Consumer Wearables | Fitbit Charge 6, Apple Watch, Garmin Devices | Test consumer device accuracy | Real-world applicability, Consumer relevance |
| Signal Processing Tools | MATLAB, Python BioSPPy, R Statistical Packages | Analyze PPG signals and derive metrics | HRV analysis, Motion artifact correction |
| Validation Software | Bland-Altman plotting tools, ICC calculation packages | Statistical analysis of agreement | Standardized validation metrics |
Factors Influencing Accuracy and Research Implications
Key Variables Affecting Measurement Precision
Multiple factors significantly impact the accuracy of wearable optical sensors:
- Motion artifacts: Physical activity can increase error by 30% or more compared to rest [13]
- Cardiac rhythm: Accuracy decreases substantially during atrial fibrillation versus sinus rhythm [11]
- Device type and placement: Research-grade devices generally outperform consumer models [13]
- Sensor technology: Reflectance PPG (wearables) has inherent limitations versus transmittance oximetry (clinical devices) [10]
- Population factors: Disease-specific characteristics (e.g., lung cancer mobility impairments) affect accuracy [17]
Implications for Research and Drug Development
For researchers and drug development professionals, these findings have several important implications:
Device selection must align with research objectives - consumer wearables may suffice for general trend monitoring, while research-grade devices are preferable for clinical endpoint measurement
Study populations influence accuracy - device performance varies significantly between healthy individuals, patients with specific conditions, and those with cardiac arrhythmias
Validation is context-specific - devices should be validated for specific use cases and populations relevant to the research question
Complementary use of technologies - combining different sensor types (e.g., ECG patches with optical wearables) may provide more comprehensive monitoring
Trend analysis may be more valuable than absolute values - when absolute accuracy is limited, longitudinal trends still provide valuable insights into health status changes
Wearable optical sensors show promise for research and clinical monitoring but demonstrate variable accuracy compared to gold standard clinical methods. Heart rate monitoring is generally reliable, particularly at rest, while SpO₂ monitoring shows significant limitations. Newer applications like atrial fibrillation detection and hydration monitoring show potential but require further validation.
For researchers incorporating these technologies into studies, careful consideration of device capabilities, appropriate validation for specific use cases, and understanding of limitations are essential. As technology advances and standardization improves, wearable optical sensors are poised to play an increasingly important role in clinical research and healthcare monitoring.
In both clinical practice and biomedical research, the accuracy of physiological monitoring is paramount. "Gold standard" techniques represent the most definitive methods available for measuring a specific physiological parameter, against which all newer technologies are validated. These benchmarks, such as arterial line catheters for hemodynamic monitoring and spirometry for pulmonary function, are characterized by their well-understood operating principles, extensive validation history, and established clinical credibility. However, the rapid emergence of wearable optical sensors, particularly in clinical trials and drug development, necessitates a rigorous comparison against these reference standards. For researchers and professionals, understanding the technical basis, performance characteristics, and limitations of both traditional benchmarks and emerging technologies is essential for evaluating their appropriate application. This guide provides a structured comparison of clinical gold standards against advancing wearable alternatives, focusing on experimental methodologies for validation and the implications for data integrity in research settings.
Cardiovascular Monitoring: Arterial Lines vs. Wearable Sensors
The Invasive Hemodynamic Gold Standard
Direct arterial pressure monitoring via an indwelling arterial catheter remains the clinical gold standard for continuous blood pressure measurement, particularly in critical care and operative settings.
- Principle of Operation: A catheter is placed directly into a peripheral artery (typically radial, femoral, or brachial) and connected to a pressurized fluid-filled tubing system that transmits the arterial pressure waveform to an external electronic transducer. This transducer converts the mechanical pressure into an electrical signal, providing a real-time waveform display of systolic, diastolic, and mean arterial pressures.
- Key Metrics: The system provides direct, beat-to-beat measurement of arterial pressure with high fidelity and minimal latency. It allows for repeated arterial blood gas sampling and is considered the most accurate method for tracking rapid hemodynamic changes.
- Experimental Validation: Validation of arterial lines is inherent in their fundamental physical principle of direct hydraulic coupling to the bloodstream. Accuracy in clinical practice is maintained through routine calibration (zeroing) and dynamic response testing (fast-flush square-wave test) to ensure the system's natural frequency and damping coefficient are adequate for accurate waveform reproduction.
The Rise of Non-Invasive Wearable Optical Sensors
Wearable sensors for cardiovascular monitoring, primarily using Photoplethysmography (PPG), offer a non-invasive alternative. PPG is an optical technique that measures blood volume changes in the microvascular bed of tissue.
- Principle of Operation: A PPG sensor consists of a light-emitting diode (LED) that emits light (green, red, or near-infrared) into the skin and a photodetector (PD) that measures the amount of light reflected back. The pulsatile component of the captured signal (AC) is caused by arterial blood volume changes during the cardiac cycle, while the non-pulsatile component (DC) is influenced by venous blood, tissue, and bone. This AC component is used to extract physiological parameters like heart rate, pulse waveform, and through analysis, oxygen saturation and heart rate variability [18].
- Form Factors: PPG sensors are categorized as transmission-type (e.g., finger or ear clips), which provide higher signal-to-noise ratio (SNR), or reflection-type (e.g., wrist-worn watches/patches), which offer greater versatility for continuous, all-day monitoring despite a somewhat lower SNR [18].
- Advanced Sensor Designs: Research focuses on enhancing PPG accuracy through material and design innovations. These include developing ultra-flexible, organic photodetectors for better skin contact [18] and using multi-wavelength PPG systems combined with other sensors like ECG electrodes to create hybrid biometric capture systems. This multi-sensor fusion, as claimed by some manufacturers, addresses limitations of traditional optical sensors, such as motion artifacts and accuracy variations across different skin tones [19].
Experimental Protocol for Validation
To objectively compare the accuracy of a wearable optical sensor against the arterial line gold standard, a controlled clinical study design is required.
- Participant Cohort: Recruit a representative sample of patients already undergoing direct arterial pressure monitoring as part of their standard clinical care (e.g., in an ICU or operating room).
- Device Placement: The wearable optical sensor (e.g., a wrist-worn device or finger clip) should be applied to the patient, ensuring proper skin contact according to manufacturer guidelines. It is critical that the sensor is placed on a limb without the arterial line to avoid interference.
- Data Synchronization: Simultaneously record data from both the arterial pressure waveform and the wearable optical sensor. Precise time-synchronization of the data streams is essential for a valid beat-to-beat comparison.
- Data Analysis: For blood pressure estimation derived from PPG, comparative analysis should include:
- Bland-Altman Plots: To assess the agreement and identify any bias between the two methods across a range of pressures.
- Error Metrics: Calculation of the Mean Absolute Error (MAE) and Root Mean Square Error (RMSE) for systolic, diastolic, and mean arterial pressures.
- Clinical Accuracy: Evaluation based on standards such as the IEEE/Association for the Advancement of Medical Instrumentation (AAMI) protocol, which requires a mean error of ≤5 mmHg and a standard deviation of ≤8 mmHg.
The workflow below illustrates the key stages of this validation protocol:
Validation Protocol Workflow
Quantitative Comparison of Performance
The table below summarizes the key characteristics of these two monitoring approaches, highlighting the trade-offs between accuracy and practicality.
Table 1: Comparison of Arterial Line and Wearable Optical Sensor Technologies
| Feature | Arterial Line (Gold Standard) | Wearable Optical Sensor (PPG) |
|---|---|---|
| Invasiveness | Invasive (requires arterial access) | Non-invasive |
| Measurement Principle | Direct hydraulic coupling | Optical absorption (PPG) |
| Primary Metrics | Direct systolic, diastolic, and mean arterial pressure | Derived heart rate, pulse waveform, heart rate variability, and estimated blood pressure |
| Accuracy/Precision | High-fidelity, beat-to-beat accuracy | Varies; heart rate is generally reliable; blood pressure estimation is less accurate and requires frequent calibration [18] [19] |
| Continuity of Monitoring | Continuous, but limited to critical care settings | Continuous, enabling long-term ambulatory monitoring |
| Risk Profile | High (risk of infection, thrombosis, hemorrhage) | Very low |
| Expertise Required | High (requires trained clinician for insertion) | Low |
| Key Limitations | Cannot be used for long-term or ambulatory monitoring; high resource cost | Susceptible to motion artifacts; signal quality depends on skin perfusion and contact; accuracy can be lower in darker skin tones [18] |
Pulmonary Function: Spirometry as the Unchallenged Benchmark
Spirometry: The Definitive Test for Airflow Obstruction
Spirometry is the universally accepted gold standard for the diagnosis and monitoring of obstructive lung diseases like Chronic Obstructive Pulmonary Disease (COPD) [20]. It measures the volume and flow of air that can be inhaled and exhaled.
- Principle of Operation: A patient takes a maximal inhalation to total lung capacity, then exhales as forcefully, completely, and rapidly as possible into a spirometer. The device records the volume of air exhaled over time, generating a volume-time curve and a flow-volume loop.
- Key Metrics:
- Forced Expiratory Volume in 1 second (FEV1): The volume of air exhaled in the first second of a forced maneuver.
- Forced Vital Capacity (FVC): The total volume of air exhaled during the entire FEV maneuver.
- FEV1/FVC Ratio: This is the primary metric for diagnosing airflow obstruction. A post-bronchodilator ratio below 0.7 (or below the statistically derived Lower Limit of Normal, LLN) confirms the presence of obstruction, consistent with COPD [21] [20].
- Quality Control: Adherence to international standards (e.g., ATS/ERS guidelines) is critical. This includes technical requirements for spirometer calibration and biological checks, as well as procedural standards to ensure patient effort is maximal and reproducible.
Wearable Sensors for Remote Pulmonary Monitoring
While no wearable sensor currently replaces diagnostic spirometry, research is focused on developing continuous, remote monitoring solutions for respiratory rates and patterns.
- Acoustic Sensors: Small, wearable microphones or accelerometers placed on the chest or neck can capture respiratory sounds. Advanced signal processing algorithms can then derive respiratory rate and detect anomalies like wheezing or cough [22] [23].
- Chest Wall Movement Sensors: Respiratory Inductive Plethysmography (RIP) bands or strain sensors integrated into smart clothing can measure the expansion and contraction of the chest and abdomen, providing detailed information on breathing patterns, respiratory rate, and even tidal volume estimates [22].
- PPG-Derived Respiration: The PPG signal contains a respiratory component, as intrathoracic pressure changes during breathing modulate arterial blood flow. Algorithms can extract the Respiratory Rate (RR) from these modulations in the baseline (DC) and amplitude (AC) of the PPG signal [24] [18].
Experimental Protocol for Correlation
Validating a wearable respiratory sensor against spirometry involves assessing its ability to track changes in lung function or reliably measure respiratory rate.
- Participant Cohort: Include both healthy individuals and patients with varying degrees of COPD or asthma to test across a range of lung functions.
- Controlled Maneuvers: Data should be collected during a series of activities:
- Resting Breathing: To validate basic respiratory rate accuracy.
- Controlled Bronchoconstriction/Dilation: For example, using methacholine challenge or bronchodilator administration, with pre- and post-spirometry and continuous wearable sensor monitoring. This tests the sensor's ability to track dynamic lung function changes.
- Data Analysis:
- Respiratory Rate: Compare the wearable-derived RR with a visual count or capnography-derived RR using Bland-Altman analysis and correlation coefficients.
- Correlation with FEV1: Analyze if trends or specific features in the wearable sensor data (e.g., cough count, breathing pattern variability) correlate with changes in measured FEV1, even if the sensor cannot provide an absolute FEV1 value.
The logical relationship between the gold standard and the parameters measured by wearables is structured as follows:
Spirometry and Wearable Sensor Correlation Logic
Quantitative Comparison of Performance
The table below contrasts the definitive nature of spirometry with the emerging, surrogate capabilities of wearable sensors.
Table 2: Comparison of Spirometry and Wearable Respiratory Monitoring Technologies
| Feature | Spirometry (Gold Standard) | Wearable Respiratory Sensor |
|---|---|---|
| Measurement Principle | Direct volumetric measurement of airflow | Indirect (e.g., chest movement, sound, PPG modulation) |
| Primary Metrics | FEV1, FVC, FEV1/FVC, PEF | Respiratory rate, breathing pattern, cough frequency, activity level |
| Diagnostic Capability | Definitive for airflow obstruction | Cannot diagnose obstruction; monitors symptoms and trends |
| Nature of Test | Effort-dependent, performed in clinic | Passive and continuous, suitable for home monitoring |
| Accuracy & Standardization | Highly accurate and standardized (ATS/ERS) | Variable accuracy; lack of universal standards |
| Key Utility | Diagnosis, staging, and monitoring of COPD/Asthma | Longitudinal tracking of symptom burden and exacerbation risk [23] |
| Key Limitations | Point-measurement; requires patient effort and clinical visit | Provides surrogate measures; data may be influenced by motion and posture |
The Researcher's Toolkit: Key Reagents & Materials for Validation Studies
For researchers designing experiments to validate wearable sensors against gold standards, the following tools and methodologies are essential.
Table 3: Essential Research Reagents and Solutions for Validation Studies
| Item | Function in Validation | Example/Notes |
|---|---|---|
| Clinical-Grade Data Acquisition System | Synchronized recording of gold-standard and wearable sensor data. | Systems from ADInstruments (PowerLab) or BIOPAC; must allow for precise timestamping of all data streams. |
| Signal Processing Software | Filtering, analysis, and comparison of complex physiological waveforms. | MATLAB, Python (with SciPy/Pandas), or LabVIEW for developing custom algorithms for feature extraction (e.g., pulse wave analysis, respiratory component isolation). |
| Statistical Analysis Tools | Quantifying agreement and performance metrics. | R or Python libraries for Bland-Altman analysis, intraclass correlation coefficients (ICC), and error (MAE, RMSE) calculations. |
| Calibrated Calibration Equipment | Ensuring the reference standard is operating correctly. | Biological calibrator ("syringe simulator") for spirometers; electronic pressure calibrator for arterial line transducers. |
| Protocols for Provocation/Challenge | Testing device performance under dynamic physiological conditions. | Methacholine for bronchoconstriction; bronchodilators (e.g., albuterol) for bronchodilation; tilt-table or exercise stress-test for cardiovascular changes. |
The comparison between clinical gold standards and wearable optical sensors reveals a landscape of complementary, rather than competing, technologies. Arterial lines and spirometry remain irreplaceable for definitive diagnosis and high-acuity management due to their direct measurement principles and proven accuracy. However, their inherent limitations— invasiveness, confinement to clinical settings, and intermittent nature—create a significant opportunity for wearable sensors.
The value of wearable optical and other sensors lies in their capacity for continuous, longitudinal, and real-world data collection. For drug development professionals, this enables the capture of rich, objective datasets on patient function and symptoms in their natural environment, potentially leading to more sensitive endpoints for clinical trials [23]. For clinical researchers, these devices offer a window into disease progression and treatment response outside the narrow snapshot of a clinic visit.
The future of physiological monitoring does not pit one technology against the other but focuses on their integration. The ongoing challenge for researchers and industry professionals is to rigorously validate wearable-derived metrics against the established benchmarks, clearly define their appropriate use cases, and continue innovating to close the accuracy gap, thereby building a new, multi-layered paradigm for patient monitoring and research.
Strengths and Inherent Limitations of Surface-Level Optical Measurements
Surface-level optical measurements are pivotal in both industrial quality control and biomedical sensing. In industrial contexts, they ensure the precision of optical components, where surface imperfections can initiate laser-induced damage [25]. In the rapidly evolving field of wearable sensors, these optical techniques have been adapted for non-invasive monitoring of physiological biomarkers, such as those found in sweat [26]. However, the accuracy of these wearable optical sensors must be rigorously evaluated against clinical gold standards to validate their utility in research and drug development. This guide objectively compares the performance of prominent optical measurement technologies, detailing their inherent limitations and strengths to inform their critical application in scientific and clinical settings.
Comparative Analysis of Optical Measurement Technologies
The selection of an appropriate optical measurement technology is a trade-off between precision, speed, robustness, and application suitability. The table below summarizes the key characteristics, strengths, and limitations of five prominent optical measurement methods.
Table 1: Comparison of Key Optical Measurement Technologies
| Technology | Best For/Key Strength | Primary Limitations | Typical Accuracy/Precision |
|---|---|---|---|
| White Light Interferometry (WLI) [27] | Highest precision; smooth surfaces, roughness | Vibration-sensitive; complex shapes; steep edges | Nanometer-level measurements |
| Confocal Microscopy [27] | High resolution & excellent depth of field; 3D structures | Time-consuming for large areas; small working distances; vibration-sensitive | High resolution for fine details |
| Structured Light (Fringe Projection) [27] | Speed; measuring large areas quickly | Lower accuracy; high prep effort for non-matt surfaces; light-sensitive | Lower compared to WLI and Confocal |
| Laser Triangulation [27] | Speed and versatility on production lines | Shadowing issues with complex parts; struggles with reflective surfaces | Insufficient for tolerances in the hundredths range |
| Focus-Variation [27] | Versatility; complex surfaces and steep flanks | N/A (Technology is highlighted for its combination of accuracy and versatility) | High precision on complex topographies |
Experimental Protocols for Validation
Protocol: Validating Wearable Optical Sensors Against Gold Standards
The following methodology, adapted from studies validating wearable heart rate monitors and optical sweat sensors, provides a framework for assessing the accuracy of surface-level optical measurements in biomedical applications [8] [28].
- Objective: To validate and compare the accuracy of consumer-grade or research-grade wearable optical sensors against clinical gold-standard devices in both controlled laboratory and free-living conditions.
- Participants: A target sample size (e.g., 15-36 participants) is recruited based on the specific application, such as patients with a relevant clinical condition or healthy volunteers [28] [8].
- Devices: Participants are equipped with the optical wearable sensor(s) under investigation and the gold-standard device simultaneously.
- Procedures:
- Laboratory Protocol: Participants perform structured activities (e.g., variable-paced walking, sitting, standing) while being video-recorded for direct observation (DO) validation [28].
- Free-Living Protocol: Participants wear the devices continuously for an extended period (e.g., 24 hours to 7 days) while going about their normal daily routines [28] [8].
- Data Analysis:
- Accuracy: Defined as the percentage of sensor readings within a certain error margin (e.g., 10%) of the gold-standard values [8].
- Agreement: Assessed using Bland-Altman plots to determine bias (mean difference) and 95% limits of agreement (LoA) [28] [8].
- Statistical Measures: Calculation of sensitivity, specificity, positive predictive value, and intraclass correlation coefficients [28].
Protocol: Correlating Surface Defects with Functional Properties
This methodology, derived from research on optical components, quantifies the relationship between physical surface characteristics and performance [29].
- Objective: To systematically investigate the quantitative correlation between surface defect dimensions and a functional property, such as laser-induced absorption.
- Sample Preparation: Artificial defects with controlled dimensions (e.g., Vickers indentations) are fabricated on a sample substrate (e.g., K9 optical glass) to simulate surface imperfections [29].
- Measurement:
- Surface Defect Characterization: The dimensions of the artificial defects are measured using a high-resolution optical technique, such as differential interference contrast (DIC) microscopy [25].
- Functional Property Measurement: A corresponding functional test is performed. For example, a Surface Thermal Lensing (STL) platform is used to measure the photothermal signal and quantify absorption caused by the defects [29].
- Data Analysis: Experimental results are used to plot the functional signal (e.g., STL signal) against the defect dimension. A curve is fitted to the data to establish a quantitative correlation, verifying that increasing defect dimensions lead to heightened absorption [29].
Visualization of Technology Selection and Validation Workflow
The following diagram illustrates the logical decision-making process for selecting an optical measurement technology and the subsequent pathway for experimental validation.
Technology Selection & Validation Workflow
Essential Research Reagents and Materials
The table below details key materials and reagents used in the development and testing of advanced optical measurement systems, particularly in the context of wearable optical sweat sensors [26].
Table 2: Key Research Reagent Solutions for Optical Sensing
| Item | Function/Application | Specific Examples |
|---|---|---|
| Flexible/Stretchable Polymers [26] | Substrate for wearable sensors; provides flexibility and skin adhesion. | Polydimethylsiloxane (PDMS), Thermoplastic co-polyester elastomer (TPC). |
| Hydrogels [26] | Biocompatible matrix for sweat collection; can incorporate colorimetric reagents. | Polyvinyl alcohol (PVA)/sucrose hydrogel. |
| Colorimetric Reagents [26] | React with target biomarkers to produce a measurable color change. | Reagents for pH, glucose, chloride (Cl⁻), calcium (Ca²⁺). |
| Microfluidic Components [26] | Manage biofluid sampling; prevent contamination; enable sequential analysis. | Check valves, capillary burst valves (CBVs), suction pumps. |
| Reference Defect Standards [25] | Calibrate and quantify surface imperfection measurements. | Vickers indentations, calibrated scratch-dig standards per MIL-PRF-13830B. |
Standards for Surface Quality Specification
Quantifying surface imperfections is critical for high-precision optics. Two dominant standards govern this area:
- U.S. Standard MIL-PRF-13830B: This standard specifies surface quality using a "scratch-dig" number (e.g., 20-10). The scratch number (10, 20, 40, 60, 80) is an arbitrary indicator of scratch brightness compared to a calibrated standard, while the dig number represents the diameter of the largest pit in 1/100 mm. This method is subjective, economical, and fast, making it common for many applications. A specification of 10-5 is typically required for the most demanding laser applications [25].
- ISO 10110-7: This international standard offers a more quantitative "dimensional" method. Surface quality is expressed as
5/N x A, whereNis the number of allowed imperfections andAis the square root of the area of the maximum allowed imperfection. While more precise and objective, this method is also more time-consuming and expensive than MIL-PRF-13830B [25].
Expanding Applications in Chronic Disease Management and Remote Monitoring
The integration of wearable optical sensors into chronic disease management and remote monitoring represents a paradigm shift from episodic, facility-based care to continuous, personalized health tracking. These sensors, predominantly based on photoplethysmography (PPG) technology, utilize light to non-invasively measure physiological parameters such as heart rate, blood oxygen saturation, and potentially blood pressure [22] [24]. For researchers and drug development professionals, the critical question remains how these consumer-grade and research-grade devices perform against established clinical gold standards, particularly in complex patient populations. The expanding applications of these technologies are fueled by a growing market, projected to reach $7.2 billion by 2035, and their ability to facilitate decentralized clinical trials and remote patient monitoring (RPM) [22] [30]. This guide objectively compares the performance of leading wearable optical sensors, provides detailed experimental methodologies for their validation, and situates these findings within the broader thesis of assessing their accuracy against clinical benchmarks.
Performance Comparison: Wearable Optical Sensors vs. Clinical Gold Standards
Validation studies are essential to determine the contexts in which wearable optical sensors can provide clinically-reliable data. The following analysis compares the accuracy of several devices across different physiological metrics and patient populations.
Table 1: Accuracy Validation of Wearable Optical Sensors for Key Physiological Metrics
| Device / Sensor Type | Target Metric | Reference Gold Standard | Population | Key Performance Findings |
|---|---|---|---|---|
| Fitbit Charge 6 (Consumer-Grade) [17] [28] | Step Count, PA Intensity | Direct Observation, Video Analysis | Lung Cancer Patients (n=15 target) | Laboratory and free-living validation ongoing; results expected 2025. |
| Research-Grade Wrist-worn PPG (General) [24] | Heart Rate, Pulse Inconstancy | Clinical Pulse Oximetry, ECG | Healthy Adults | Enables estimation of pulse variability and oxygen saturation; accuracy high at normal gait. |
| Optical Sensors for BP (In Development) [22] | Blood Pressure | Auscultatory / Oscillometric BP | N/A | Under development; challenge in calibration and regulatory approval. |
| AI-Integrated Wearables (e.g., SepAl, i-CardiAx) [31] | Sepsis Prediction | Clinical SOFA Score, Diagnosis | Hospitalized Patients | Predicted sepsis onset 8.2-9.8 hours in advance. |
Table 2: Performance Limitations of Wearable Optical Sensors in Specific Contexts
| Limitation Factor | Impact on Accuracy / Performance | Supporting Evidence |
|---|---|---|
| Slow Gait Speed / Altered Mobility | Significant decrease in step count accuracy | Device accuracy decreases substantially in patients with cancer and slower walking velocities [17] [28]. |
| Skin Pigmentation | Risk of overestimating oxygen saturation (SpO₂) | PPG signals can vary with skin pigmentation, potentially missing hypoxemia in dark phototypes [31]. |
| Motion Artifacts | Signal noise and data loss | Common in free-living conditions; requires robust filtering algorithms and can lead to information overload [31]. |
Experimental Protocols for Validating Wearable Sensor Accuracy
A critical component of integrating wearable sensor data into clinical research is a rigorous and standardized validation protocol. The following section details methodologies from current studies to serve as a template for researchers.
Protocol for Laboratory and Free-Living Validation in Specific Populations
A 2025 validation study protocol for patients with lung cancer (LC) provides a comprehensive framework for assessing device accuracy in populations with impaired mobility [17] [28].
Objective: To validate and compare the accuracy of consumer-grade (Fitbit Charge 6) and research-grade (activPAL3 micro, ActiGraph LEAP) wearable activity monitors (WAMs) in patients with LC under laboratory and free-living conditions, and to establish standardized validation procedures [17] [28].
Study Design:
- Laboratory Protocol: Participants simultaneously wear all devices while performing structured activities, including:
- Free-Living Protocol: Participants wear the devices continuously for 7 days in their natural environment, removing them only for water-based activities. This assesses real-world performance and adherence [17] [28].
Primary Outcome Measures:
Statistical Analysis:
The workflow for this validation protocol is outlined below.
Framework for Clinical Predictive Algorithm Development
Beyond basic metric validation, advanced wearables integrate sensor data with AI for predictive monitoring. The protocol for developing and validating such systems involves a different workflow, as shown below [31].
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers aiming to replicate validation studies or develop new sensor applications, the following table details key materials and their functions.
Table 3: Essential Research Toolkit for Wearable Sensor Validation Studies
| Item / Solution | Category | Primary Function in Research | Example Products / Brands |
|---|---|---|---|
| Research-Grade Activity Monitors | Hardware | Provide high-fidelity, validated data on physical activity, posture, and step count; often used as a criterion measure. | ActiGraph LEAP, activPAL3 micro [17] [28] |
| Consumer-Grade Wearables | Hardware | Test the viability of low-cost, widely available devices for clinical research and remote monitoring. | Fitbit Charge 6 [17] [28] |
| Direct Observation / Video Recording System | Gold Standard | Serves as an objective, frame-by-frame reference for validating activity and posture in lab settings. | High-resolution video cameras [17] [28] |
| Validated Survey Instruments | Software | Control for confounding factors (e.g., stress, quality of life) that may influence movement patterns and device accuracy. | HRQoL, PA, and sleep surveys [17] [28] |
| FDA-Cleared Medical Devices | Gold Standard | Provide clinical-grade measurements for validating vital signs (e.g., ECG for heart rate, clinical oximeter for SpO2). | GE Healthcare's Portrait Mobile, VitalPatch [31] [32] |
| Data Analysis & Statistical Software | Software | Perform advanced statistical comparisons (Bland-Altman, ICC) and signal processing for sensor data. | R, Python, SPSS |
| AI/ML Modeling Platforms | Software | Develop and train predictive algorithms on continuous physiological data streams for early warning systems. | TensorFlow, PyTorch [31] [33] |
The expansion of wearable optical sensors into chronic disease management and remote monitoring offers unprecedented opportunities for continuous, real-world data collection in clinical research and drug development. The current evidence indicates that while these sensors show remarkable promise, particularly when integrated with AI for predictive analytics, their accuracy is not universal. Performance is contingent on the specific device, the physiological metric being measured, and the target patient population. Gait impairments, skin tone, and motion artifacts remain significant challenges to absolute accuracy.
Therefore, a cautious and validated approach is paramount. Researchers should not treat all wearable data as inherently equivalent to clinical gold standards. Instead, the future of this field lies in context-driven device selection and the implementation of standardized validation protocols, like the one detailed herein, to determine the specific boundaries of reliable use. As sensor technology and analytical algorithms continue to mature, the gap between consumer-grade wearables and clinical-grade diagnostics is expected to narrow, further solidifying their role in the next generation of clinical research and personalized medicine.
From Lab to Real World: Methodologies for Data Collection and Clinical Integration
The use of wearable optical sensors and other digital health technologies in clinical research has expanded dramatically, offering unprecedented opportunities to collect real-world mobility data outside traditional laboratory settings. However, this rapid adoption has created significant challenges for researchers and drug development professionals, primarily due to a lack of standardized protocols across studies and institutions. Heterogeneity in data acquisition protocols, sensor specifications, data formats, and analytical approaches creates substantial barriers for data sharing, reproducibility, and external validation [34] [35]. The Mobilise-D consortium, a large multi-centric study, has directly addressed these challenges by developing and implementing comprehensive procedures for standardizing the collection and processing of mobility data from wearable devices [34]. These standardized approaches are particularly crucial when validating wearable optical sensors against clinical gold standards, as they ensure that collected data is reliable, comparable, and suitable for regulatory evaluation of digital mobility outcomes (DMOs) [36]. This guide examines the protocols and insights from multi-centric studies like Mobilise-D to provide researchers with practical frameworks for standardizing data collection in their own investigations of wearable sensor accuracy.
Mobilise-D Standardization Framework: Core Components and Structure
The Mobilise-D consortium established a comprehensive framework for standardizing wearable sensor data collection across multiple clinical sites and patient populations. This framework was designed specifically to support the technical validation and clinical validation of digital mobility outcomes derived from a single wearable sensor worn on the lower back [35] [36]. The standardization procedure addresses five critical domains that are essential for ensuring data consistency and quality in multi-centric studies.
Core Standardization Domains
File Format and Data Structure: The consortium selected the .mat Matlab file format with a standardized folder structure organized by subject and recording condition (7-day, contextual, free-living, and laboratory) [35]. Each data.mat file contains wearable device and gold standard data in a consistent structure that facilitates data sharing and analysis across research groups.
Sensor Locations and Orientation Conventions: Precise specifications for sensor placement were defined, primarily focusing on a single inertial measurement unit (IMU) worn on the lower back, an ergonomically favorable position near the body's center of mass that is well-accepted by participants [37]. Standardization of sensor orientation conventions ensures consistent interpretation of sensor signals across different devices and research sites.
Measurement Units and Sampling Frequency: The protocols enforce standardized measurement units and sampling frequencies (typically 100 Hz for the primary wearable device) to enable direct comparison of data across different recording sessions and sites [35] [37].
Timing References: Implementation of synchronized timing references across all recording systems (wearable devices and gold-standard reference systems) is critical for accurate temporal alignment and validation of derived outcomes [37].
Gold Standards Integration: The framework provides detailed specifications for integrating and synchronizing data from gold-standard reference systems, such as the INDIP system (INertial modules with DIstance sensors and Pressure insoles), which combines inertial modules with distance sensors and pressure insoles for validation [37].
Multi-Cohort Study Design
The Mobilise-D approach was validated across diverse clinical populations to ensure broad applicability. The study included participants with Parkinson's Disease, Multiple Sclerosis, Proximal Femoral Fracture, Chronic Obstructive Pulmonary Disease, Congestive Heart Failure, and healthy older adults [38] [36]. This heterogeneous participant selection was intentional, designed to test the robustness of standardization protocols across different mobility impairments and walking characteristics.
Table 1: Mobilise-D Study Cohorts and Sample Sizes
| Cohort | Sample Size (Technical Validation) | Key Mobility Characteristics |
|---|---|---|
| Healthy Older Adults | 20 | Reference for normal age-related mobility |
| Parkinson's Disease | 20 | Gait impairment, bradykinesia, variability |
| Multiple Sclerosis | 20 | Fatigue-related mobility changes, ataxia |
| Proximal Femoral Fracture | 19 | Significant gait impairment, slow walking |
| Chronic Obstructive Pulmonary Disease | 17 | Exertional limitations, respiratory constraints |
| Congestive Heart Failure | 12 | Reduced exercise capacity, exertional limitations |
Quantitative Validation Results: Wearable Device Performance Across Cohorts
The Mobilise-D consortium conducted extensive validation studies to assess the accuracy of wearable-derived digital mobility outcomes against gold-standard reference systems. The validation focused on key gait parameters, including walking speed, cadence, and stride length, across different clinical populations and recording environments.
Walking Speed Estimation Accuracy
Walking speed, often termed the "6th vital sign," serves as a composite measure of walking ability and overall mobility health [38] [36]. The validation of walking speed estimation pipelines demonstrated varying accuracy across clinical cohorts and recording environments.
Table 2: Walking Speed Estimation Accuracy from Mobilise-D Validation
| Cohort | Laboratory MAE (m/s) | Laboratory MRE (%) | Real-world MAE (m/s) | Real-world MRE (%) |
|---|---|---|---|---|
| All Cohorts | 0.10 | 14.96 | 0.11 | 20.31 |
| Healthy Adults | 0.08 | Not reported | 0.09 | Not reported |
| COPD | 0.06 | Not reported | Not reported | Not reported |
| Proximal Femoral Fracture | 0.12 | Not reported | 0.11 | Not reported |
| Congestive Heart Failure | 0.12 | Not reported | Not reported | Not reported |
The data revealed that error rates were generally higher in real-world environments compared to laboratory settings, highlighting the additional challenges posed by unscripted, daily-life activities [38]. Furthermore, cohorts with more severe gait impairments (e.g., proximal femoral fracture) typically showed higher estimation errors compared to healthier cohorts.
Gait Algorithm Performance Metrics
The consortium conducted a comprehensive comparison of multiple algorithms for estimating key digital mobility outcomes, identifying optimal approaches for different clinical populations [37].
Table 3: Performance of Best Algorithms for Key Digital Mobility Outcomes
| Digital Mobility Outcome | Best Algorithm(s) | Sensitivity | Positive Predictive Value | Absolute/Relative Error |
|---|---|---|---|---|
| Gait Sequence Detection | Cohort-specific | >0.73 | >0.75 | Not applicable |
| Initial Contact Detection | Single best algorithm | >0.79 | >0.89 | Relative error <11% |
| Cadence Estimation | Cohort-specific | >0.79 | >0.89 | Relative error <8.5% |
| Stride Length Estimation | Single best algorithm | Not applicable | Not applicable | Absolute error <0.21m |
The performance of these algorithms was influenced by walking bout duration and gait speed. Shorter walking bouts and slower gait speeds (particularly below 0.5 m/s) consistently resulted in reduced algorithm performance across all cohorts and outcomes [37]. This highlights the importance of considering these factors when designing validation protocols and interpreting results from real-world monitoring.
Experimental Protocols: Laboratory and Real-World Validation
The validation of wearable optical sensors against clinical gold standards requires meticulously designed experimental protocols that assess device performance across controlled and free-living environments. The Mobilise-D approach incorporates both laboratory-based and real-world assessment components to comprehensively evaluate device accuracy [35] [37].
Laboratory Validation Protocol
The laboratory protocol employs structured activities designed to replicate a range of mobility challenges while allowing for precise measurement using gold-standard reference systems:
Structured Walking Trials: Participants perform walking tasks at various speeds, including preferred, slow, and fast walking paces, to assess accuracy across different velocity ranges [37].
Scripted Transitions: Participants execute a series of posture changes (sitting-to-standing, standing-to-sitting) and turns to evaluate algorithm performance during non-steady-state mobility [17].
Functional Tests: Standardized clinical assessments such as the Timed Up and Go (TUG) test and walking on different surfaces (slopes, stairs) are incorporated to examine device performance during functionally relevant tasks [36] [37].
Reference System Synchronization: Laboratory sessions employ synchronized gold-standard systems such as 3D motion capture systems or the INDIP multi-sensor system (inertial modules with distance sensors and pressure insoles) to provide reference values for validation [37].
Throughout laboratory sessions, activities are typically video-recorded to enable additional verification and precise timestamp alignment between the wearable device data and reference systems [17].
Real-World Validation Protocol
The real-world validation component assesses device performance during unscripted daily activities in participants' natural environments:
Extended Monitoring Period: Participants wear the wearable device (typically on the lower back) for a designated period (e.g., 2.5 hours or 7 days) while going about their usual activities [37].
Semi-Structured Tasks: Participants are asked to perform some specific tasks during the monitoring period, such as outdoor walking, navigating slopes and stairs, and moving between rooms to ensure diversity of captured activities [37].
Reference System in Real-World: The INDIP system or similar validated multi-sensor systems are used as a reference during real-world monitoring, despite the technical challenges of deploying such systems in free-living conditions [38].
Activity Logging: Participants maintain diaries to record activities, symptoms, and notable events during the monitoring period to facilitate data interpretation and alignment [39].
This dual approach—combining controlled laboratory assessment with ecologically valid real-world monitoring—provides a comprehensive framework for establishing the accuracy of wearable optical sensors across the spectrum of mobility activities encountered in daily life.
Implementation Workflow: From Data Collection to Standardized Outputs
The following diagram illustrates the comprehensive workflow for standardized data collection and processing based on the Mobilise-D approach:
Standardized Data Collection Workflow
The Scientist's Toolkit: Essential Solutions for Wearable Validation Research
Implementing robust validation protocols for wearable optical sensors requires specific technical solutions and methodological approaches. The following table details essential components derived from successful multi-centric studies:
Table 4: Essential Research Reagent Solutions for Wearable Validation Studies
| Solution/Component | Function | Example Implementations |
|---|---|---|
| Primary Wearable Device | Continuous collection of inertial measurement unit (IMU) data in real-world environments | McRoberts Dynaport MM+ (single sensor on lower back) [37] |
| Multi-Sensor Reference System | Gold-standard validation for algorithm development and accuracy assessment | INDIP System (combines inertial modules, distance sensors, and pressure insoles) [37] |
| Algorithm Validation Framework | Systematic comparison of multiple algorithms for estimating digital mobility outcomes | Ranking methodology proposed by Bonci et al. [37] |
| Data Standardization Pipeline | Harmonization of data formats, sensor orientations, and measurement units across sites | Mobilise-D MATLAB-based standardization procedure [34] [35] |
| Multi-Cohort Validation Strategy | Assessment of generalizability across diverse populations with varying mobility impairments | Inclusion of neurodegenerative, respiratory, cardiovascular, and musculoskeletal conditions [38] [36] |
The standardized protocols developed by multi-centric studies like Mobilise-D provide an essential framework for validating wearable optical sensors against clinical gold standards. The key insights from these initiatives demonstrate that robust validation requires comprehensive approaches encompassing both laboratory and real-world environments, diverse clinical populations to ensure generalizability, and standardized data processing pipelines to enable comparison across studies. The finding that algorithm performance varies significantly based on walking bout characteristics and clinical population underscores the importance of context-specific validation rather than one-size-fits-all approaches. Furthermore, the successful application of these standardized protocols across multiple disease cohorts supports their utility in drug development and clinical trial settings, particularly as the field moves toward regulatory acceptance of digital mobility outcomes. By adopting and building upon these standardized approaches, researchers can generate higher-quality, more comparable evidence regarding the accuracy of wearable optical sensors, ultimately accelerating their implementation in both clinical research and practice.
The evolution of wearable technology has ushered in a new era for biomedical research and clinical monitoring, creating a critical need to understand the relative performance of consumer-grade sensors against established clinical gold standards. Sensor integration—encompassing where sensors are placed, how they are attached, and how data from multiple sensors is combined—is a fundamental determinant of data accuracy and reliability. For researchers and drug development professionals, navigating the transition from controlled laboratory settings to free-living environments presents unique challenges. This guide objectively compares the performance of various wearable sensor integration strategies, supported by experimental data and detailed methodologies from recent validation studies, to inform their application in rigorous scientific research.
Sensor Placement, Attachment, and Their Impact on Data Quality
Strategic sensor placement and secure attachment are critical for capturing high-quality physiological signals. These factors directly influence the signal-to-noise ratio and the sensor's susceptibility to motion artifacts, which are primary sources of error in wearable data.
Common Sensor Placements and Technologies
- Wrist-Worn Placement: This is the most common form factor for consumer-grade devices (e.g., Fitbit, Garmin, Apple Watch). These devices primarily use photoplethysmography (PPG) and accelerometry. [1] While convenient, the wrist is prone to significant motion artifacts, especially during intense physical activity or fine motor tasks, which can degrade PPG signal quality. [1] [8]
- Chest-Worn Placement: Devices like the Hexoskin smart shirt incorporate sensors directly into the fabric, positioning ECG electrodes on the torso. [8] This placement provides a more stable location for cardiac electrical measurement (ECG) and is less susceptible to motion noise compared to the wrist, offering a signal closer to a clinical-grade ECG. [8]
- Neck-Worn Placement: Emerging research uses specialized neck-worn sensors like NeckSense to monitor eating behaviors by detecting jaw movements, chewing, and swallowing. This placement is chosen for its proximity to anatomical structures involved in ingestion. [40]
- Thigh-Worn Placement: Research-grade devices like the activPAL are often attached to the thigh. This placement is ideal for accurately distinguishing between sedentary postures (sitting/lying) and upright activities (standing/stepping), which is challenging for wrist-worn devices. [28]
The Influence of Attachment on Accuracy
The method of attachment is equally crucial. For optical sensors, consistent skin contact is necessary. Poor fit—either too loose or too tight—can lead to signal loss or corruption. [1] [24] As noted in a pediatric validation study, the fit of a device on a child can significantly impact measurement quality. [8] Furthermore, studies have shown that the accuracy of heart rate measurements from wrist-worn PPG sensors declines during physical activity, partly due to the motion of the device relative to the skin. [1] [8]
Table 1: Impact of Sensor Placement and Attachment on Data Quality
| Placement Location | Common Sensor Technologies | Key Advantages | Key Challenges & Impact on Accuracy |
|---|---|---|---|
| Wrist | PPG, Accelerometer | High user compliance, comfortable for long-term wear. [41] | Prone to motion artifacts; decreased HR accuracy during movement and at higher intensities. [1] [8] |
| Chest/Torso | ECG, Accelerometer, Respiration Sensors | More stable signal for cardiac and respiratory metrics; closer to clinical gold-standard placements. [8] | Less comfortable for 24/7 wear; may not be suitable for all populations. |
| Thigh | Accelerometer (high-precision) | High accuracy for classifying sedentary vs. active postures and estimating step count. [28] | Social discomfort; not ideal for capturing upper-body movement. |
| Ear | PPG, Accelerometer | Low movement artifact; useful for activity recognition. [24] | Limited surface area for multiple sensors; may not be suitable for all ear anatomies. |
Experimental Protocols for Validating Wearable Sensors
Validation studies are essential for establishing the credibility of wearable sensor data. The following are detailed methodologies from key recent studies that compare wearable performance against gold-standard references.
Protocol for Lung Cancer Population Validation
A 2025 study aims to validate the Fitbit Charge 6, ActiGraph LEAP, and activPAL3 micro in patients with lung cancer, a population often experiencing gait impairments and unique mobility challenges. [28]
- Study Design: The protocol includes both laboratory and free-living components.
- Laboratory Protocol: Participants perform structured activities, including variable-paced walking trials, sitting and standing postures, and posture changes. All activities are video-recorded for direct observation (DO), which serves as the gold standard for validation. [28]
- Free-Living Protocol: Participants wear all three devices simultaneously for 7 consecutive days in their home environment, removing them only for water-based activities. [28]
- Data Analysis: Laboratory validity is assessed by comparing wearable data to video observations. Free-living agreement between devices is evaluated using Bland-Altman plots, intraclass correlation analysis, and 95% limits of agreement. [28]
Protocol for Pediatric Heart Rate Monitoring
A 2025 study investigated the accuracy of the Corsano CardioWatch (wristband) and Hexoskin (smart shirt) in a pediatric cardiology population. [8]
- Criterion Measure: A 24-hour Holter electrocardiogram (ECG) was used as the gold-standard reference. [8]
- Procedure: Participants were equipped with the Holter ECG, CardioWatch, and Hexoskin shirt simultaneously for a 24-hour free-living period. They maintained a diary of activities and sleep times. [8]
- Accuracy Definition: Heart rate accuracy was defined as the percentage of HR values within 10% of the Holter values. Agreement was further analyzed with Bland-Altman plots to calculate bias and limits of agreement. [8]
- Factor Analysis: The study analyzed how factors like BMI, age, time of wearing, and bodily movement (via accelerometry) influenced measurement accuracy. [8]
The workflow below illustrates the core components of a robust sensor validation protocol, synthesizing elements from the cited studies.
Quantitative Performance Comparison: Consumer-Grade vs. Research-Grade vs. Gold Standards
The tables below summarize key quantitative findings from recent studies, providing a clear comparison of device performance across different populations and metrics.
Table 2: Accuracy of Heart Rate Monitoring in Different Populations
| Device (Sensor Type) | Population | Gold Standard | Key Accuracy Findings | Source |
|---|---|---|---|---|
| Corsano CardioWatch (Wrist-PPG) | Pediatric Cardiology (n=31) | Holter ECG | Mean Accuracy: 84.8% (within 10% of Holter). Bias: -1.4 BPM (95% LoA: -18.8 to 16.0 BPM). Accuracy ↓ with higher HR and movement. [8] | Formative JMIR 2025 |
| Hexoskin Shirt (Chest-ECG) | Pediatric Cardiology (n=36) | Holter ECG | Mean Accuracy: 87.4% (within 10% of Holter). Bias: -1.1 BPM (95% LoA: -19.5 to 17.4 BPM). Accuracy higher in first 12h (94.9%) vs. last 12h (80%). [8] | Formative JMIR 2025 |
| Consumer Wearables (e.g., Fitbit, Garmin) | General (Systematic Review) | ECG, Chest Straps | At rest: High accuracy (MAE ~2 BPM). During exercise: Accuracy declines, limits of agreement widen. One review found 56.5% of HR comparisons were within ±3% error. [1] | npj Cardiovasc. Health 2025 |
Table 3: Accuracy of Physical Activity and Postural Monitoring
| Device / System | Primary Sensor Type & Placement | Gold Standard | Key Accuracy Findings | Source |
|---|---|---|---|---|
| activPAL3 micro | Accelerometer (Thigh) | Direct Observation (Video) | High accuracy for measuring posture, posture changes, and step count in lab settings. Considered a criterion measure for sedentary behavior. [28] | PMC 2025 |
| ActiGraph LEAP | Accelerometer (Wrist) | Direct Observation (Video) | Research-grade device being validated against video observation in structured lab activities and free-living in a lung cancer population. [28] | PMC 2025 |
| Fitbit Charge 6 | PPG & Accelerometer (Wrist) | Direct Observation & Research-Grade Monitors | Ongoing validation for step count, time in PA intensity levels. Accuracy for step count known to decrease at slower walking speeds, relevant in impaired populations. [28] | PMC 2025 |
Multi-Sensor Fusion Strategies
Multi-sensor data fusion has emerged as a powerful solution to overcome the limitations of individual sensors, enhancing the reliability, accuracy, and robustness of health monitoring systems. [42]
Frameworks and Levels of Fusion
Fusion methodologies can be classified based on the level of abstraction at which the fusion occurs. Dasarathy's model is one widely referenced framework: [42]
- Data-In Data-Out (DAI-DAO): Fusion at the raw signal level.
- Data-In Feature-Out (DAI-FEO): Features are extracted from raw sensor data and then fused.
- Feature-In Feature-Out (FEI-FEO): Fusion of already extracted features.
- Feature-In Decision-Out (FEI-DEO): Fusion of features to reach a decision.
- Decision-In Decision-Out (DEI-DEO): Fusion of local decisions from multiple sensors. [42]
Fusion Algorithms and Applications
Different algorithmic approaches are employed depending on the fusion level and application:
- Kalman Filters: Often used for signal-level fusion (DAI-DAO) to reduce noise and improve state estimation (e.g., refining heart rate or position data). [42]
- Bayesian Networks: Useful for decision-level fusion (DEI-DEO), allowing the combination of probabilistic beliefs from different sensor sources. [42] [43]
- Machine Learning Models: Particularly adept at feature-level fusion (FEI-FEO, FEI-DEO). These models can learn complex relationships between features from multiple sensors (e.g., ECG, accelerometer, gyroscope) to detect events like arrhythmias or classify physical activities with high accuracy. [42] [24]
The following diagram illustrates the flow of data through different fusion levels, from raw sensor input to a final decision or inference.
The Researcher's Toolkit: Essential Reagents & Materials
This section details key technologies and materials used in advanced wearable sensor research, as featured in the cited experiments.
Table 4: Key Research Reagent Solutions for Wearable Sensor Studies
| Item / Technology | Function in Research | Example Use Case |
|---|---|---|
| Research-Grade Actigraphy | High-precision measurement of physical activity and sleep-wake cycles. Serves as a criterion measure for validating consumer devices. [28] [41] | ActiGraph devices used as a reference for validating Fitbit step counts in free-living conditions. [28] [41] |
| Direct Observation (Video Recording) | Provides a gold-standard ground truth for validating posture, activity type, and step count in laboratory settings. [28] | Video recording of structured lab activities (sitting, walking, standing) to validate activPAL and Fitbit data. [28] |
| Ambulatory ECG (Holter Monitor) | Gold-standard reference for validating heart rate and rhythm measurements from wearable sensors. [8] | 24-hour Holter monitoring used to assess the accuracy of Corsano CardioWatch and Hexoskin shirt HR in children. [8] |
| Multi-Sensor Fusion Platforms (e.g., mDCS) | Mobile data collection systems that integrate and synchronize data from heterogeneous sources (wearables, vendor clouds, surveys). [43] | The mDCS platform is used in preventive health projects to fuse data from direct sensors and vendor clouds (e.g., Fitbit) for centralized analysis. [43] |
| Activity-Oriented Camera (AOC) | A body-worn camera that respects privacy by triggering recording only when a specific activity (e.g., eating) occurs. [40] | Used in the HabitSense system to capture contextual eating behaviors without continuous video recording. [40] |
The Role of AI and Machine Learning in Signal Processing and Metric Estimation
The integration of wearable optical sensors into clinical research and healthcare represents a paradigm shift from reactive to predictive medicine. These devices enable continuous, non-invasive monitoring of physiological parameters, capturing subtle changes that intermittent spot checks might miss [31]. However, their value in scientific and clinical applications hinges on a fundamental question: how accurate are they? The emergence of Artificial Intelligence (AI) and Machine Learning (ML) is fundamentally reshaping how sensor data is processed and how key health metrics are estimated, bridging the gap between consumer-grade wearables and clinical gold standards. This guide objectively compares the performance of AI-enhanced sensing technologies against traditional clinical instruments, providing researchers and drug development professionals with a data-driven framework for evaluation.
AI and ML algorithms enhance wearable sensors by transforming raw, often noisy, optical signals into reliable clinical insights. They mitigate challenges like motion artifacts and signal drift through advanced signal processing and pattern recognition [31]. This capability is critical for using wearables in high-stakes environments, such as clinical trials, where data integrity is paramount. This article examines the experimental evidence validating these technologies, details the methodologies behind the comparisons, and provides a toolkit for their practical application in research.
Performance Comparison: Wearable Sensors vs. Clinical Gold Standards
Quantitative validation is essential for establishing the credibility of wearable sensors. The following tables summarize key findings from recent studies that directly compare wearable technologies and AI-driven analysis against established clinical reference systems.
Table 1: Gait Analysis Technology Comparison in Older Adults (n=20) [44]
| Gait Metric Category | Technology Assessed | Mean Absolute Error (MAE) | Pearson Correlation (r) | Agreement with Zeno Walkway |
|---|---|---|---|---|
| Macro-temporal | Foot-mounted IMUs | 0.00–6.12 | 0.92–1.00 | Highest accuracy |
| Azure Kinect Depth Camera | 0.01–6.07 | 0.68–0.98 | Close agreement | |
| Lumbar-mounted IMUs | N/A | N/A | Consistently lower agreement | |
| Micro-spatial | Foot-mounted IMUs | 0.00–6.12 | 0.92–1.00 | Highest accuracy |
| Azure Kinect Depth Camera | 0.01–6.07 | 0.68–0.98 | Close agreement | |
| Lumbar-mounted IMUs | N/A | N/A | Consistently lower agreement | |
| Spatiotemporal | Foot-mounted IMUs | 0.00–6.12 | 0.92–1.00 | Highest accuracy |
| Azure Kinect Depth Camera | 0.01–6.07 | 0.68–0.98 | Close agreement | |
| Lumbar-mounted IMuels | N/A | N/A | Consistently lower agreement |
Table 2: Accuracy of AI-Enhanced Predictive Alerts in Clinical Monitoring [31]
| Clinical Application | AI System / Metric | Key Performance Result | Lead Time Before Event |
|---|---|---|---|
| Sepsis Prediction | SepAl System | High prediction capacity | Up to 9.8 hours |
| Sepsis Prediction | i-CardiAx System | Significant prediction capability | Average of 8.2 hours |
| General Deterioration | AI + Wearable PPG & Temperature | High capacity for anticipating critical events | Up to 14-15 hours |
| Patient Severity Assessment | Deep Learning + EMR & Sensor Data | Better accuracy than SOFA score | N/A |
Table 3: Standard Model Evaluation Metrics for ML-Based Signal Processing [45] [46]
| Metric | Formula | Primary Use Case in Sensor Data |
|---|---|---|
| Precision | True Positives / (True Positives + False Positives) | Minimizing false alarms (e.g., arrhythmia detection). |
| Recall (Sensitivity) | True Positives / (True Positives + False Negatives) | Critical for not missing events (e.g., seizure detection). |
| F1 Score | 2 × (Precision × Recall) / (Precision + Recall) | Balanced view for imbalanced datasets. |
| AUC-ROC | Area Under the ROC Curve | Evaluating model's class separation capability across thresholds. |
| Mean Absolute Error (MAE) | (1/n) × Σ|Actual - Predicted| | Quantifying average error in continuous data (e.g., heart rate). |
Experimental Protocols for Technology Validation
The comparative data presented in the previous section is derived from rigorous experimental protocols designed to assess technology performance under both controlled laboratory and free-living conditions.
Protocol for Gait Analysis Validation
A 2025 study directly compared wearable inertial measurement units (IMUs) and a markerless depth camera (Azure Kinect) against the ProtoKinetics Zeno Walkway, an electronic walkway considered a clinical gold standard [44].
- Study Population: 20 older adults (mean age 70.06 ± 9.45 years) to ensure relevance to clinical populations prone to gait impairments [44].
- Experimental Design: A cross-sectional, comparative study where all sensing technologies captured data synchronously using custom hardware for precise temporal alignment. This design eliminates inter-trial variability as a confounding factor [44].
- Task Protocol: Participants performed both Single-Task and Dual-Task walking trials. The Dual-Task condition (e.g., walking while performing a cognitive task) increases cognitive load and is used to uncover subtle gait deficits that may not be apparent under simple walking conditions [44].
- Data Analysis: The study compared 11 distinct gait markers spanning macro, micro-temporal, micro-spatial, and spatiotemporal domains. Statistical analysis included Mean Absolute Error (MAE), Pearson correlation (r), and Bland-Altman analysis to assess both accuracy and agreement with the reference standard [44].
Protocol for Wearable Activity Monitor Validation in Clinical Populations
Another 2025 protocol paper outlines a comprehensive method for validating consumer-grade and research-grade activity monitors in patients with lung cancer (LC), a population with unique mobility challenges [17].
- Study Population: 15 adults diagnosed with stages 1-4 LC. Patients with cancer often experience slower walking speeds and altered movement patterns, providing a robust test of device accuracy under sub-optimal conditions [17].
- Laboratory Protocol: Participants engage in a series of structured activities while being video recorded (the gold standard for direct observation). The activities include:
- Variable-time walking trials.
- Sitting and standing tests.
- Posture changes.
- Gait speed assessments [17].
- Free-Living Protocol: Participants wear all devices (Fitbit Charge 6, activPAL3 micro, and ActiGraph LEAP) simultaneously for 7 continuous days during their normal daily life, except during water-based activities. This assesses real-world performance and adherence [17].
- Metrics and Analysis: Laboratory validity is assessed by comparing device data to video-recorded observations, calculating sensitivity, specificity, and positive predictive value. Free-living agreement between the consumer-grade device (Fitbit) and the research-grade devices is evaluated using Bland-Altman plots, intraclass correlation analysis, and 95% limits of agreement [17].
The Signaling Pathway: From Raw Sensor Data to Clinical Insight
The process of converting raw optical signals from wearables into validated clinical metrics relies on a multi-stage AI and ML pipeline. The diagram below illustrates this complex workflow.
AI-Driven Signal Processing Workflow
This workflow begins with the acquisition of the Raw Optical Signal, typically from photoplethysmography (PPG) sensors and accelerometers [24] [31]. The signal then undergoes Pre-processing, where AI-powered filters remove noise from motion artifacts and environmental interference. In the Feature Extraction stage, ML algorithms identify clinically relevant features from the cleaned signal, such as heart rate variability or specific pulse waveform characteristics. These features are fed into an ML Model (e.g., a regression model for continuous value prediction or a classifier for event detection) that generates the Estimated Clinical Metric. Finally, this output is rigorously compared against a Clinical Gold Standard in a validation step, where performance metrics like Precision, Recall, and MAE are calculated. The results from this validation can be fed back to refine the ML model, creating a continuous improvement loop [45] [46] [31].
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing validation studies or implementing wearable sensing in clinical trials, a core set of "research reagents"—both hardware and software—is essential. The following table details key solutions and their functions.
Table 4: Essential Research Reagent Solutions for Wearable Sensor Validation
| Solution / Technology | Type | Primary Function in Research & Validation |
|---|---|---|
| APDM Wearable IMUs [44] | Hardware (Sensor) | Captures high-fidelity kinematic data for gait and movement analysis; used as a benchmark against optical systems. |
| Azure Kinect Depth Camera [44] | Hardware (Sensor) | Provides markerless motion capture for spatial and temporal gait analysis in ecological settings. |
| Fitbit Charge 6 [17] | Hardware (Consumer Wearable) | Serves as a representative, widely-available consumer-grade device for validating step count, heart rate, and activity in free-living studies. |
| ActiGraph LEAP [17] | Hardware (Research Wearable) | An established research-grade activity monitor used as a criterion for validating consumer devices in specific populations. |
| activPAL3 micro [17] | Hardware (Research Wearable) | Provides validated measurements of posture, posture changes, and stepping, crucial for assessing sedentary behavior and activity. |
| Fitabase/ Fitbit API [17] | Software (Data Platform) | Enables programmatic access to minute-level data from consumer wearables for robust scientific analysis. |
| Bland-Altman Analysis [44] [17] | Statistical Method | Quantifies agreement between a new wearable technology and a gold-standard method by assessing bias and limits of agreement. |
| Confusion Matrix & ROC Analysis [45] [46] | Analytical Metric | Evaluates the performance of classification algorithms (e.g., for event detection like falls or seizures) in terms of precision, recall, and specificity. |
The integration of AI and ML is fundamentally enhancing the role of wearable optical sensors in clinical research by improving the accuracy and reliability of metric estimation. Experimental data demonstrates that properly validated systems—particularly foot-mounted IMUs and advanced depth cameras—can achieve performance levels comparable to clinical gold standards in domains like gait analysis [44]. Furthermore, AI-driven predictive models show significant promise in transforming continuous sensor data into early warnings for critical medical events, potentially hours before clinical manifestation [31].
However, the field must contend with important limitations, including sensor sensitivity to placement and patient population, potential performance degradation in individuals with dark skin phototypes, and the challenge of signal artifacts [31]. For researchers and drug development professionals, the path forward involves a context-driven selection of wearable technologies, adherence to rigorous validation protocols like those outlined in this guide, and a clear understanding of the AI metrics used to evaluate performance. By doing so, the scientific community can fully leverage these powerful tools to advance personalized medicine and improve the efficiency of clinical trials.
The emergence of digital biomarkers represents a transformative shift in clinical data collection, moving beyond traditional measurements derived from bodily fluids to quantifiable, objective data collected through digital devices [47] [48]. These consumer-generated physiological and behavioral measures are collected through connected digital tools like wearable devices, sensors, and mobile technologies to explain, influence, and predict health-related outcomes [47]. A specific and advanced category of these measures, Digital Mobility Outcomes (DMOs), refers to digitally captured characteristics of a person's mobility, such as real-world walking speed, step length, and cadence, which provide a continuous, objective readout of a patient's functional status [49] [50] [51].
The adoption of these technologies addresses a critical limitation of traditional clinical assessments, which often provide only a brief "snapshot" of a patient's capacity in a clinic setting, potentially underestimating real-world mobility impairment and lacking ecological validity [50] [51]. By enabling continuous, remote monitoring of patients in their natural environments, DMOs generate real-world evidence that offers novel insights into disease progression and treatment efficacy, complementing and sometimes surpassing conventional clinical scales [49] [52]. This is particularly valuable in chronic neurological conditions like Parkinson's disease (PD), Multiple Sclerosis (MS), and Chronic Obstructive Pulmonary Disease (COPD), where mobility is a key indicator of overall health and functional independence [49] [51].
Technological Comparison: Sensor Types and DMO Applications
Sensor Technologies Underpinning Digital Biomarkers
Wearable devices leverage a variety of sensor technologies to capture digital biomarkers, each with distinct operating principles, advantages, and applications in clinical research.
Table 1: Comparison of Wearable Sensor Technologies for Digital Biomarker Capture
| Sensor Type | Common Form Factors | Measured Parameters | Advantages | Limitations/Challenges |
|---|---|---|---|---|
| Inertial Measurement Units (IMUs) [50] [51] | Wrist-worn devices, lower-back sensors, foot-worn sensors | Gait speed, step length, cadence, posture, turn velocity | Captects real-world, continuous mobility data; Provides objective, sensitive functional measures; Established use in clinical validation consortia (e.g., Mobilise-D) | Accuracy can decrease at slower walking speeds [17]; Heterogeneity in device placement & protocols [50] |
| Electrical Sensors [15] [16] | Skin patches, smart textiles, wrist-worn devices | Skin hydration, electrodermal activity, heart rate, ECG | Ease of use and integration; Cost-effective for large-scale studies | May be less precise than optical alternatives for molecular-level insights [15] [16] |
| Optical Sensors [15] [16] | Smartwatches, finger-worn devices | Heart rate, blood oxygen saturation (SpO2), pulse wave form | Non-invasive molecular-level insights; High precision; Growing market acceptance | Signal can be susceptible to motion artifacts; Potentially higher cost |
| Multimodal Sensors [15] [16] | Advanced patches, specialized wrist devices | Combines parameters from multiple sensor types (e.g., activity + heart rate + hydration) | Improved accuracy through data fusion; More comprehensive patient phenotyping | Increased complexity in data processing and analysis; Higher device cost |
Disease-Specific Applications of DMOs
DMOs and digital biomarkers are demonstrating significant clinical utility across a spectrum of therapeutic areas, particularly in neurology and cardiology.
Table 2: Digital Biomarker and DMO Applications in Key Disease Areas
| Disease Area | Specific Condition | Measured Digital Biomarker / DMO | Clinical Utility & Context of Use |
|---|---|---|---|
| Neurology | Parkinson's Disease (PD) [50] [48] | Real-world gait speed, step length, stride time, turn duration | Differentiates PD from controls; Captures intraday symptom fluctuations & response to medication [50] [48] |
| Neurology | Multiple Sclerosis (MS) [49] [48] | Walking speed, balance metrics from smartphone-based tests (finger-tapping, walk and balance) | Characterizes symptoms and assesses disease burden for holistic quality-of-life evaluation [49] |
| Neurology | Alzheimer's Disease [48] | Subtle behavioral, cognitive, motor, and sensory changes via smartphone | Predicts disease progression from mild cognitive impairment to dementia in early stages [48] |
| Cardiovascular | Heart Failure [48] | Gait speed, physical activity, night-time toilet use, sleep quality via ambient sensors | Detects heart failure decompensation for remote monitoring and intervention [48] |
| Cardiovascular | Atrial Fibrillation [48] | Heart rhythm via optical sensors and irregular pulse algorithms | Identifies and diagnoses arrhythmia events outside clinical settings [48] |
| Oncology | Lung Cancer (LC) [17] | Step count, time spent in physical activity of different intensities, posture | Tracks debilitating disease-related symptoms (e.g., fatigue) and activity changes during treatment [17] |
Figure 1: From Sensor Data to Clinical Insight: The Workflow of Digital Mobility Outcomes in Drug Development.
Validation and Accuracy: DMOs vs. Clinical Gold Standards
Key Validation Studies and Experimental Protocols
For digital biomarkers to achieve regulatory and clinical endorsement, they must undergo rigorous technical and clinical validation to demonstrate their accuracy, reliability, and clinical meaningfulness. This involves structured experiments comparing DMOs against established clinical gold standards.
Study 1: Real-World vs. Supervised Gait Assessment in Parkinson's Disease A systematic review of real-world DMOs in PD analyzed studies comparing gait in supervised versus real-world settings [50].
- Objective: To determine if DMOs measured in real-world environments differ from those captured in supervised, clinic-based assessments [50].
- Protocol: Participants wore a single sensor on the lower back or multiple sensors on the feet and lower back. Supervised assessment consisted of structured walking tasks (e.g., 7-20 meter straight walk). Real-world assessment involved continuous monitoring over 7 days in free-living conditions [50].
- Findings: The majority of reports (5 out of 6) found that DMOs were significantly different between real-world and supervised settings. Patients typically exhibited slower walking speeds and reduced step/stride lengths in real-world conditions, demonstrating that clinical assessments can overestimate a patient's actual daily mobility performance [50].
Study 2: Validation of Wearable Activity Monitors in Lung Cancer An ongoing 2025 study protocol addresses the critical need to validate wearable devices in populations with specific mobility challenges, such as lung cancer (LC) [17].
- Objective: To validate and compare the accuracy of consumer-grade (Fitbit Charge 6) and research-grade (activPAL3 micro, ActiGraph LEAP) wearables in patients with LC under laboratory and free-living conditions [17].
- Laboratory Protocol: Participants complete structured activities (variable-time walking, sitting/standing, posture changes) while wearing all devices simultaneously. Activities are video-recorded for gold-standard validation. Outcome measures include step count and time in different physical activity intensities [17].
- Free-Living Protocol: Participants wear devices continuously for 7 days. Agreement between devices is assessed using statistical methods like Bland-Altman plots and intraclass correlation [17].
- Significance: This is the first study to establish a standardized framework for validating wearable accuracy in LC populations, where disease-related symptoms like fatigue and gait impairments can alter movement patterns and affect device performance [17].
Analytical Framework for Validation
The path to regulatory approval for DMOs requires a structured, evidence-based roadmap. The Mobilise-D consortium has developed a comprehensive framework to guide this process from initial development to regulatory submission [51].
Figure 2: Roadmap for DMO Development and Validation as exemplified by the Mobilise-D consortium [51].
The Scientist's Toolkit: Key Reagents and Solutions for DMO Research
Successfully implementing a DMO study requires careful selection of devices, software, and methodological frameworks.
Table 3: Essential Research Toolkit for DMO Studies
| Tool Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Research-Grade Wearable Sensors | activPAL3 micro, ActiGraph LEAP [17] | Provide high-fidelity data for posture, step count, and activity intensity; Considered criterion measures in validation studies. |
| Consumer-Grade Wearable Sensors | Fitbit Charge 6 [17] | Offer cost-effective, user-friendly options for large cohorts; Require rigorous validation against research-grade devices in target population. |
| Algorithm & Software Platforms | Mobilise-D validated algorithms [49], Fitbit API [17] | Open-source or commercial software to transform raw sensor data into validated DMOs; Ensure algorithms are disease- and device-agnostic where possible. |
| Clinical Outcome Assessments | MDS-UPDRS III [50], 6-minute walk test [51] | Gold-standard clinical scales used for correlation and clinical validation of DMOs to establish ecological and clinical meaning. |
| Data Management & Analysis Tools | Custom software accessing device APIs [17], Statistical packages for Bland-Altman analysis [17] | Systems for handling large volumes of continuous data, ensuring data integrity, and performing complex statistical comparisons. |
Digital Mobility Outcomes represent a paradigm shift in how mobility is quantified in clinical drug development. The evidence demonstrates that DMOs derived from wearable sensors are not merely digital equivalents of traditional endpoints, but offer superior sensitivity and ecological validity by capturing a patient's true mobility performance in their daily life [49] [50]. While challenges related to standardization, validation, and regulatory acceptance persist, concerted efforts like the Mobilise-D consortium are establishing the rigorous frameworks and evidence base needed for widespread adoption [51].
The comparison between optical and other sensor technologies reveals a trend toward multimodal systems that combine the strengths of various sensing modalities to improve accuracy and reliability [15] [16]. As the field matures, the integration of DMOs and digital biomarkers into clinical trials promises to accelerate drug development, enable more personalized treatment approaches, and ultimately lead to therapies that more effectively improve a patient's real-world functioning and quality of life [52] [48] [53].
Wearable optical sensors represent a transformative force in modern clinical monitoring, shifting healthcare from episodic, reactive measurements to continuous, proactive health assessment. These devices, predominantly using photoplethysmography (PPG) technology, illuminate the skin and measure light absorption changes to capture vital physiological data [18] [24]. Their non-invasive nature, coupled with advancements in miniaturization and battery life, has propelled their integration into clinical research and consumer health markets. This guide objectively evaluates the performance of these technologies against established clinical gold standards across three chronic disease areas, providing researchers and drug development professionals with critical, data-driven insights for their investigative work.
Fundamental Principles of Photoplethysmography (PPG)
PPG technology operates on a simple yet powerful principle: a light-emitting diode (LED) shines light onto the skin, and a photodetector (PD) measures the intensity of the light that is either transmitted through or reflected back from the tissue [18]. The resulting PPG waveform contains a wealth of physiological information. The pulsatile alternating current (AC) component reflects cardiac-synchronous changes in blood volume, while the slowly varying direct current (DC) component is related to tissue structure, average blood volume, and respiration [18]. Through sophisticated signal processing and algorithmic analysis, researchers can extract a multitude of parameters from this waveform, including heart rate, heart rate variability, oxygen saturation, respiratory rate, and more.
Research Reagent Solutions: Essential Materials for Optical Sensing Research
Table 1: Key Research Reagents and Materials for Wearable Optical Sensor Studies
| Item | Function in Research | Example Use Cases |
|---|---|---|
| Medical-Grade Reference Devices | Provides gold-standard measurements for criterion validity studies; serves as benchmark for wearable accuracy. | Polar H10 chest strap (HR, HRV) [54], Dynaport MoveMonitor (step count) [54], YSI 2300 Bioanalyzer (blood glucose) [55]. |
| Consumer/Research Wearables | Device Under Test (DUT); the technology being validated for specific clinical or research applications. | Fitbit Charge 4, HUAWEI Watch GT 3, Corsano CardioWatch, Hexoskin smart shirt [56] [54] [8]. |
| Signal Processing Algorithms | Extracts meaningful physiological features from raw PPG signals; crucial for parameter estimation. | Machine Learning models for cough sound analysis [56], proprietary algorithms for deriving RR from PPG [57]. |
| Standardized Physiological Protocols | Creates controlled conditions for testing; ensures consistent and comparable results across studies. | Pre- and post-bronchodilator spirometry [56], moderate-intensity exercise on aerobic equipment [58]. |
| Data Analysis Software | Performs statistical comparison and agreement analysis between wearable data and reference standards. | Software for calculating Intraclass Correlation Coefficient (ICC), Bland-Altman analysis, and Mean Absolute Error [56] [54] [58]. |
Case Study 1: Chronic Obstructive Pulmonary Disease (COPD) Monitoring
Experimental Protocol: Multimodal COPD Screening
A 2025 study investigated a smartwatch-based algorithm for screening ventilatory dysfunction and COPD, addressing the critical issue of underdiagnosis in China [56]. The methodology was as follows:
- Participant Recruitment: Training and validation cohorts were recruited, including patients with COPD or pulmonary dysfunctions and healthy volunteers. All participants provided informed consent [56].
- Data Collection:
- Cough Sound Recording: A smartwatch was positioned 30 cm from the subject's mouth at a 45° angle to record cough sounds after spirometry. Subjects performed forceful coughs 2-3 times following maximal inhalation [56].
- Physiological Parameter Monitoring: A smartwatch (HUAWEI Watch GT 3) captured PPG and acceleration (ACC) signals for one minute to compute Heart Rate Variability (HRV), blood oxygen saturation (SpO₂), and respiratory rate (RR) [56].
- Gold-Standard Assessment: All participants underwent pre- and post-bronchodilator spirometry using standardized equipment (Masterscreen-PFT) following ERS/ATS guidelines to measure FEV1, FVC, and FEV1/FVC ratio [56].
- Data Analysis: Machine learning algorithms extracted features from cough sounds to predict lung function. These predictions were combined with physiological data (HRV, SpO₂, RR) in a multimodal model to screen for COPD, with diagnostic performance assessed against physician diagnosis [56].
Figure 1: Workflow for the multimodal COPD screening study.
Performance Data: Wearables vs. Gold Standards in COPD
Table 2: Accuracy of Wearable-Derived Parameters in COPD Monitoring
| Parameter | Wearable Device | Reference Standard | Key Performance Metric | Result | Clinical Context |
|---|---|---|---|---|---|
| FEV1/FVC Prediction | HUAWEI Watch GT 3 (via cough sound) | Spirometry | Mean Absolute Error (MAE) | 7.4% [56] | Core diagnostic criterion for COPD (post-bronchodilator FEV1/FVC < 0.7) [56]. |
| Daily Step Count | Fitbit Charge 4 | Dynaport MoveMonitor | Intraclass Correlation (ICC) | 0.79 (COPD), 0.85 (Healthy) [54] | Measure of physical activity, often reduced in COPD. |
| Resting Heart Rate (RHR) | Fitbit Charge 4 | Polar H10 | Intraclass Correlation (ICC) | 0.80 (COPD), 0.79 (Healthy) [54] | Elevated RHR is a prognostic marker in COPD [54]. |
| Respiratory Rate (RR) | Fitbit Charge 4 | Polar H10 | Intraclass Correlation (ICC) | 0.84 (COPD), 0.77 (Healthy) [54] | Included in the new "Rome Proposal" for objective exacerbation classification [57]. |
| Oxygen Saturation (SpO₂) | Fitbit Charge 4 | Nonin WristOX2 | Intraclass Correlation (ICC) | 0.32 (COPD) [54] | Poor agreement in patients with COPD; overestimated by Fitbit [54]. |
| COPD Screening (Overall) | Multimodal Model (Cough + Physiology) | Physician Diagnosis | Accuracy / Sensitivity / Specificity | 87.82% / 86.96% / 87.73% [56] | Demonstrates potential for large-scale population screening. |
Case Study 2: Cardiovascular Health Monitoring
Experimental Protocol: Validating Heart Rate in Free-Living Conditions
A 2025 study assessed the validity of the Corsano CardioWatch bracelet and Hexoskin smart shirt for heart rate monitoring in a pediatric cardiology population, highlighting the importance of validation in specific user groups [8].
- Participants: Children (mean age 13.2 years) with an indication for 24-hour Holter monitoring, either due to congenital heart disease or suspected arrhythmias [8].
- Device Setup: Participants were equipped simultaneously with three devices:
- Gold Standard: A 3-lead Holter electrocardiogram (ECG) (Spacelabs Healthcare) [8].
- Test Device 1: Corsano CardioWatch 287-2B, a CE-medically certified wristband using reflective PPG, worn on the non-dominant wrist [8].
- Test Device 2: Hexoskin Pro shirt, a smart garment with woven electrodes capturing a single-lead ECG [8].
- Procedure: Participants underwent 24-hour monitoring in a free-living environment, maintaining a diary of activities and symptoms. They were encouraged to follow their normal daily routine but avoid showering and swimming [8].
- Data Analysis: Heart rate accuracy was defined as the percentage of wearable HR values within 10% of the Holter values. Agreement was assessed using Bland-Altman analysis. Subgroup analyses were conducted based on factors like BMI, age, time of wearing, and accelerometer-measured bodily movement [8].
Performance Data: Wearables vs. Gold Standards in Cardiology
Table 3: Accuracy of Wearable-Derived Parameters in Cardiovascular Monitoring
| Parameter | Wearable Device | Reference Standard | Key Performance Metric | Result | Clinical Context |
|---|---|---|---|---|---|
| Heart Rate (HR) - General | Corsano CardioWatch | Holter ECG | Mean Accuracy (% within 10%) | 84.8% [8] | Good overall accuracy in pediatric free-living conditions. |
| Heart Rate (HR) - General | Hexoskin Smart Shirt | Holter ECG | Mean Accuracy (% within 10%) | 87.4% [8] | Slightly higher accuracy than wrist-worn device. |
| Heart Rate (HR) - Low vs. High | Corsano CardioWatch | Holter ECG | Mean Accuracy (% within 10%) | 90.9% (Low HR) vs. 79.0% (High HR) [8] | Accuracy declines with higher heart rates. |
| Bland-Altman Agreement (HR) | Corsano CardioWatch | Holter ECG | Bias (BPM) / LoA | -1.4 BPM / -18.8 to 16.0 BPM [8] | Good agreement with minimal bias, though LoA are wide. |
| Bland-Altman Agreement (HR) | Hexoskin Smart Shirt | Holter ECG | Bias (BPM) / LoA | -1.1 BPM / -19.5 to 17.4 BPM [8] | Comparable performance to the CardioWatch. |
| Heart Rate (during exercise) | Garmin Vivosmart HR+ | Polar H7 | Mean Absolute Percentage Error (MAPE) | 3.77% (Young), 4.73% (Senior) [58] | MAPE <10% indicates acceptable accuracy during moderate exercise. |
| Heart Rate (during exercise) | Xiaomi Mi Band 2 | Polar H7 | Mean Absolute Percentage Error (MAPE) | 7.69% (Young), 6.04% (Senior) [58] | Acceptable accuracy, though generally lower than Garmin. |
Case Study 3: Metabolic Disorder Monitoring
Experimental Protocol: Non-Invasive Glucose Monitoring via PPG
A 2019 study directly compared a non-invasive glucose monitor (NIGM) using PPG optical sensors against a standard, invasive laboratory analyzer, exploring a highly sought-after application for wearable technology [55] [59].
- Participants: 200 adult participants of both sexes, aged 18-75, were recruited. Individuals with hemophilia or other serious coagulation disorders were excluded [55].
- Device and Measurement: The NIGM biosensor was placed on the right wrist of each participant for a non-invasive, indirect blood glucose measurement. The device employed PPG optical elements coupled with an optically-sensitive coating that changes its properties in the presence of specific sweat metabolites [59].
- Reference Method: In parallel, blood was drawn from the antecubital vein and glucose levels were assessed using the YSI 2300 STAT Plus Glucose and L-Lactate Laboratory Bioanalyzer, a recognized standard [55] [59].
- Protocol: Measurements were performed twice for each participant: before (anteprandial) and one hour after (postprandial) food intake, with no limitations on food type or quantity [55].
- Data Analysis: Correlation between the NIGM and YSI 2300 values was assessed using Pearson's correlation. Clinical accuracy was further evaluated using the Parkes Error Grid for Type II diabetes [55].
Figure 2: Workflow for non-invasive glucose monitor validation study.
Performance Data: Wearables vs. Gold Standards in Metabolism
Table 4: Accuracy of a Non-Invasive Optical Sensor for Glucose Monitoring
| Parameter | Wearable Device | Reference Standard | Key Performance Metric | Result | Clinical Context |
|---|---|---|---|---|---|
| Anteprandial Glucose | Non-Invasive Glucose Monitor (NIGM) | YSI 2300 Bioanalyzer | Pearson Correlation (ρ) | ρ = 0.8994, p < 0.0001 [55] | Strong correlation in fasting state. |
| Postprandial Glucose | Non-Invasive Glucose Monitor (NIGM) | YSI 2300 Bioanalyzer | Pearson Correlation (ρ) | ρ = 0.9382, p < 0.0001 [55] | Strong correlation after food intake. |
| Anteprandial Glucose | Non-Invasive Glucose Monitor (NIGM) | YSI 2300 Bioanalyzer | Mean Bias (±SD) | 3.705 ± 7.838 mg/dL [55] | Quantifies the average difference between methods. |
| Postprandial Glucose | Non-Invasive Glucose Monitor (NIGM) | YSI 2300 Bioanalyzer | Mean Bias (±SD) | 1.362 ± 10.15 mg/dL [55] | |
| Overall Accuracy | Non-Invasive Glucose Monitor (NIGM) | YSI 2300 Bioanalyzer | Mean Absolute Relative Difference (MARD) | 7.40% - 7.54% [55] | Falls at the lower end of the error range (5.6%-20.8%) for available glucometers. |
| Clinical Safety | Non-Invasive Glucose Monitor (NIGM) | YSI 2300 Bioanalyzer | Parkes Error Grid (Type II) | Majority in Zone A (no clinical risk) [55] | Indicates the device is safe for clinical use, with minimal readings in Zone B (altered clinical action). |
The presented case studies demonstrate that wearable optical sensors provide a powerful, versatile tool for monitoring chronic diseases outside traditional clinical settings. Their ability to enable continuous, unobtrusive data collection offers a significant advantage over intermittent gold-standard measurements.
However, the data reveals a critical nuance: performance is highly parameter-specific and context-dependent. While parameters like heart rate and step count generally show good to excellent agreement with reference standards [54] [8], others like oxygen saturation in COPD patients [54] and the indirect estimation of respiratory rate [57] can show poor agreement or be susceptible to overestimation. Furthermore, accuracy can be influenced by factors such as high heart rates [8], intense bodily movement [8], and skin pigmentation [18] [31].
For researchers and drug development professionals, this underscores the necessity of:
- Context-Driven Device Selection: Choosing a wearable based on the specific physiological parameter of interest and the target patient population.
- Rigorous Validation: Conducting validation studies against appropriate gold standards within the intended use context.
- Critical Data Interpretation: Understanding the limitations and potential biases of the technology, rather than treating the data as infallible.
When these conditions are met, wearable optical sensors hold immense promise for enhancing clinical research, enabling more personalized medicine, and facilitating large-scale population health screening.
Navigating the Accuracy Gap: Key Challenges and Technical Optimization Strategies
Wearable optical sensors, particularly those using photoplethysmography (PPG), are transforming clinical research and healthcare by enabling accessible, continuous, and longitudinal health monitoring outside traditional clinical settings [13] [18]. The number of chronically ill patients and health system utilization in the US is at an all-time high, driving development of low-cost, convenient, and accurate health technologies [13]. It is expected that 121 million Americans will use wearable devices, underscoring their potential to revolutionize healthcare, particularly in communities with traditionally limited access [13]. However, as these technologies are increasingly used for clinical research and digital biomarker development, understanding their accuracy and determining how measurement errors may affect research conclusions and impact healthcare decision-making becomes critically important [13].
The core principle of PPG involves using a light-emitting diode (LED) and a photodetector (PD) to measure changes in blood volume under the skin [13] [18]. The LED emits light that penetrates the skin and interacts with blood, while the PD detects the reflected or transmitted signal, which is then converted into an electrical waveform synchronized with blood flow dynamics [18]. This signal contains a slowly varying direct current (DC) component related to tissue structure and average blood volume, and a pulsatile alternating current (AC) component reflecting cardiac-induced blood volume changes [18]. Despite the technical sophistication of these devices, their accuracy faces significant challenges from three primary sources: motion artifacts, skin tone variations, and perfusion differences [13]. This review objectively compares the performance of wearable optical sensors against clinical gold standards, providing researchers, scientists, and drug development professionals with experimental data and methodological frameworks to critically evaluate these technologies for research applications.
Impact of Motion Artifacts
Motion artifacts represent one of the most significant challenges for wearable optical sensors, typically caused by displacement of the PPG sensor over the skin, changes in skin deformation, blood flow dynamics, and ambient temperature [13]. Motion can create mechanical displacements of the sensor with respect to tissue, dynamically modifying optical coupling efficiency and changing optical path lengths, thereby inducing spurious signal dynamics [60]. Even minute movements, including respiratory motions, can affect PPG signals [60].
Table 1: Impact of Motion on Heart Rate Measurement Accuracy Across Devices
| Device | Activity Condition | Mean Absolute Error (BPM) | Key Findings |
|---|---|---|---|
| Apple Watch 4 | Rest | ~5-7 BPM | Absolute error during activity was, on average, 30% higher than during rest across all devices [13] |
| Physical Activity | ~30% higher than rest | ||
| Fitbit Charge 2 | Rest | ~5-8 BPM | All devices reasonably accurate at rest but showed differences in responding to activity changes [13] |
| Physical Activity | ~30% higher than rest | ||
| Garmin Vivosmart 3 | Rest | ~5-9 BPM | Significant differences observed between devices during activity [13] |
| Physical Activity | ~30% higher than rest | ||
| Empatica E4 | Rest | ~6-9 BPM | Research-grade devices showed similar motion artifact challenges as consumer devices [13] |
| Physical Activity | ~30% higher than rest |
Advanced signal processing approaches have been developed to mitigate motion artifacts. Empirical Mode Decomposition (EMD) has demonstrated statistically significant increases in the signal-to-noise ratio (SNR) of wearable seismocardiogram (SCG) signals and improves estimation of pre-ejection period (PEP) during walking [61]. One study achieved a 23.68% increase in signal quality using deep learning models that integrate pressure channels and multiple light wavelengths to reconstruct motion-free physiological waveforms [62]. Despite these algorithmic advances, motion artifacts continue to limit the accuracy of wearable PPG devices, particularly during physical activity or cyclic wrist motions [13] [60].
Skin Tone and Optical Signal Variation
The influence of skin tone on PPG accuracy has been a topic of significant debate and investigation. Melanin, one of the key light absorbers in skin responsible for skin color, can affect light penetration and reflection characteristics [63]. Recent research has provided nuanced insights into this relationship.
Table 2: Skin Tone Impact on PPG Signal Characteristics
| Study | Participant Characteristics | Key Metrics | Findings |
|---|---|---|---|
| Bent et al. (2020) [13] | 53 individuals, equal FP distribution | Mean Absolute Error (MAE) | No statistically significant difference in accuracy across skin tones at rest or during activity |
| Ntoyanto et al. (2024) [63] | 12 individuals, CIE XYZ classification | Spectral Reflectance | Peak amplitude decreased by 90% for darker skin tones vs 70% for lighter tones; distinct patterns at 460nm/570nm |
| Shcherbina et al. [64] | Diverse cohort | Heart rate/Energy expenditure | Green light technology had larger error rates for individuals with darker skin tones, especially during exercise |
Bent et al. found no statistically significant difference in accuracy across skin tones in their comprehensive study of six wearable devices, though they noted a significant interaction between skin tone and specific devices [13]. In contrast, other research has demonstrated that darker skin tones reflect less light, with one study showing peak amplitude of reflected light signal decreased by 90% for darker skin tones compared to 70% for lighter skin tones [63]. This discrepancy highlights methodological challenges in studying skin tone effects, including appropriate skin tone classification—the Fitzpatrick Skin Type Scale commonly used has documented limitations in racial biases and weak correlation with actual skin color [64].
Reflective PPG sensors, common in commercial wearables, are generally less precise than transmission-mode PPG for detecting microvascular changes, and green illumination commonly used in reflection-mode is more strongly absorbed by melanin, potentially reducing accuracy for darker skin tones and often requiring extra calibration [18].
Perfusion Variations and Physiological Confounders
Perfusion index (PI) represents the ratio of pulsatile blood flow to static blood in tissue and is mathematically represented as the AC portion of the PPG signal as a fraction of the overall signal [60]. Physiological changes can significantly alter blood flow and volume in tissue, thereby changing the PPG signal in ways that may not reflect actual arterial pulses [60].
When a subject changes posture, the movement can partially disrupt blood flow and dynamically redistribute venous blood volume, which would be reflected in PPG measurement and could be interpreted erroneously in pulse oximetry [60]. Physiological changes can also occur without motion, such as with significant changes in ambient or skin temperature or in hydration—all factors that can impact PPG observations [60]. These perfusion-related variations present particular challenges for pulse oximetry (SpO₂) measurements, which rely on comparing light absorption of oxy-hemoglobin and deoxy-hemoglobin using a ratio of ratios (R) of perfusion indices taken using two differently colored lights [60]. The accuracy of SpO₂ depends on the ability to maintain consistent PI values, which is influenced by optical/mechanical design of the PPG probe as well as physiological conditions of the subject [60].
Experimental Protocols for Validation Studies
Comprehensive Device Validation Protocol
The study by Bent et al. provides a robust methodological framework for evaluating wearable device accuracy [13]. Their protocol involved 53 individuals (32 females, 21 males; ages 18-54) with equal distribution across the Fitzpatrick skin tone scale who completed the entire study protocol [13]. Participants wore six different wearable devices (four consumer-grade and two research-grade models) while undergoing a structured protocol:
- Seated rest (4 minutes): To measure baseline heart rate
- Paced deep breathing (1 minute): To introduce controlled physiological variation
- Physical activity (5 minutes): Walking to increase heart rate up to 50% of the recommended maximum
- Seated rest (~2 minutes): Washout from physical activity
- Typing task (1 minute): To assess device performance during fine motor movements
The protocol was performed three times per participant to test all devices, with an electrocardiogram (ECG) patch (Bittium Faros 180) worn during all three rounds as the reference standard [13]. Potential relationships between error in heart rate measurements and skin tone, activity condition, wearable device, and device category were examined using mixed effects statistical models [13].
Motion Artifact Quantification Methodology
Research by Inan et al. demonstrated approaches specifically designed to quantify and mitigate motion artifacts [61]. Their protocol involved 17 young, healthy subjects (11 males, 6 females; age: 25±4 years) performing:
- Phase 1: Walking on level ground at normal pace for 6 minutes, followed by 2 minutes of recovery
- Phase 2: Walking on a treadmill at 1.34 m/s for 5 minutes, followed by 1-2 minutes of recovery
- Phase 3: Walking on level ground at brisk pace (1.45±0.13 m/s) for 5 minutes, followed by 1 minute of recovery
All walking phases were preceded by baseline readings with subjects standing upright in a resting state for 1 minute [61]. The study used a wearable patch containing ECG and accelerometer sensors, with signals sampled at 1 kHz and synchronized with reference sensors (BNEL50 and BN-NICO wireless measurement modules) through tapping artifacts introduced at recording start and end [61]. The empirical mode decomposition (EMD) approach was applied to denoise signals and improve estimation of pre-ejection period during walking [61].
Spectral Response Analysis Across Skin Tones
Ntoyanto et al. detailed a specialized protocol for evaluating skin tone effects on optical signals [63]. Their methodology involved:
- Participant Selection: 12 individuals with even distribution of light to dark tones (6 females, 6 males; age range 20-50)
- Instrumentation: White LED (300-700nm) light source with AvaSpec 2048 Spectrometer and AS7341 spectral color sensor on flexible Kapton substrate
- Measurement Site: Inner wrist (less exposed to tanning effects), cleaned with alcohol wipes
- Control: Dark laboratory with 3D-printed housing to maintain fixed distances (1cm from skin, 1cm between source and detector)
- Skin Tone Classification: CIE XYZ color space values for objective classification rather than subjective Fitzpatrick scaling
This approach allowed for precise characterization of how different skin tones respond to varying wavelengths within the visible spectrum, identifying distinct grouping patterns according to skin tone at specific wavelengths (460nm and 570nm) [63].
Visualization of Experimental Workflows and Relationships
Comprehensive Device Validation Workflow
Error Source Analysis Framework
The Researcher's Toolkit: Essential Materials and Methods
Table 3: Research Reagent Solutions for Wearable Sensor Validation
| Category | Specific Tools | Function/Application | Key Considerations |
|---|---|---|---|
| Reference Standards | ECG (Bittium Faros 180) [13] | Gold-standard heart rate reference | Provides validation baseline for wearable accuracy assessment |
| Impedance Cardiogram (ICG) [61] | PEP measurement reference | Enables validation of mechanical cardiac function parameters | |
| Skin Tone Classification | Fitzpatrick Scale [13] | Subjective skin tone categorization | Limited by racial biases and weak color correlation [64] |
| CIE XYZ Color Space [63] | Objective color measurement | Provides quantitative, reproducible skin tone characterization | |
| Spectrocolorimeters [64] | Empirical skin color measurement | Multiple wavelength analysis for comprehensive characterization | |
| Motion Monitoring | Inertial Measurement Units [62] | Motion artifact quantification | Captures acceleration patterns for signal denoising |
| Force/Pressure Sensors [62] | Sensor-skin interface monitoring | Detects relative motion at wear site for artifact correction | |
| Signal Processing | Empirical Mode Decomposition [61] | Motion artifact reduction | Data-driven denoising approach for SCG/PPG signals |
| Deep Learning Models [62] | Waveform reconstruction | Multi-sensor fusion for motion-free signal estimation | |
| Optical Configurations | Multi-wavelength PPG [62] [63] | Spectral response analysis | Enables differentiation of absorption characteristics |
| Transmission-mode PPG [18] | High-fidelity signal acquisition | Superior SNR for validation studies | |
| Reflection-mode PPG [18] | Wearable configuration testing | Represents commercial wearable form factors |
Wearable optical sensors face significant challenges from motion artifacts, skin tone variations, and perfusion changes that impact their accuracy relative to clinical gold standards [13] [63] [60]. While recent advances in sensor technology and signal processing have improved performance, researchers must carefully consider these error sources when designing studies and interpreting data from wearable devices [61] [62].
The evidence suggests that motion artifacts remain the most significant challenge, with error rates during activity approximately 30% higher than during rest across devices [13]. Skin tone effects, while potentially significant, demonstrate complex interactions with specific device technologies and algorithms, necessitating more sophisticated evaluation methods beyond traditional Fitzpatrick classification [13] [64] [63]. Perfusion variations introduce additional physiological confounders that can affect measurement accuracy independent of device limitations [60].
For researchers and drug development professionals, these findings highlight the importance of:
- Selecting validation methodologies appropriate for specific research questions
- Implementing comprehensive testing protocols that include diverse activity states and participant characteristics
- Applying advanced signal processing techniques to mitigate common error sources
- Recognizing device-specific limitations when interpreting wearable-derived data
As wearable technologies continue to evolve and see increased use in clinical research and healthcare, understanding these fundamental error sources becomes increasingly critical for drawing valid study conclusions, combining results across studies, and making informed healthcare decisions using these devices [13]. Future research should focus on developing more robust sensor technologies, advanced algorithms capable of adapting to individual user characteristics, and standardized validation frameworks that enable direct comparison across devices and studies.
Addressing the 'Surface-Level Data' Problem with Advanced Sensor Designs
Wearable optical sensors, predominantly using photoplethysmography (PPG), are being increasingly used for clinical research and healthcare, enabling accessible, continuous, and longitudinal health monitoring [13]. The core challenge, however, lies in the transition from providing "surface-level" fitness data to achieving the accuracy required for clinical decision-making and drug development. The fundamental question is whether these consumer and research-grade devices can produce data reliable enough to stand against clinical gold standards. This guide objectively compares the performance of various wearable sensor technologies against reference methods, providing researchers with a clear framework for evaluating these tools within their own work.
Performance Comparison: Wearables vs. Gold Standards
Optical Heart Rate Sensor Accuracy
A systematic evaluation of six wearable devices (four consumer-grade, two research-grade) against ECG (Bittium Faros 180) as a reference standard revealed critical insights into their accuracy under different conditions [13].
Table 1: Mean Absolute Error (MAE) of Wearable Optical Heart Rate Sensors vs. ECG
| Device Type | MAE at Rest (bpm) | MAE During Activity (bpm) | Overall MAE (bpm) |
|---|---|---|---|
| Research-grade Device A | 8.6 (FP5) | 10.1 (FP3) | 9.5 (average) |
| Consumer-grade Device B | 10.6 (FP6) | 14.8 (FP4) | 12.9 (average) |
| Consumer-grade Device C | Data not specified | Data not specified | ~30% higher error during activity vs. rest |
The study, which included 53 participants with an equal distribution across the Fitzpatrick (FP) skin tone scale, found no statistically significant difference in accuracy across skin tones [13]. This addresses a previously held concern about the performance of PPG on darker skin. However, a significant interaction was found between device type and activity state. Absolute error during physical activity was, on average, 30% higher than during rest across all devices [13]. This highlights that motion artifact and the body's physiological response to activity remain significant challenges.
Inertial Measurement Unit (IMU) Sensor Accuracy
The accuracy of another critical sensor class—Inertial Measurement Units (IMUs) for motion tracking—was evaluated against optical motion capture (OptiTrack) as a gold standard [65]. The results demonstrate a performance gap between research-grade and consumer-grade sensors.
Table 2: Accuracy of Wrist-Worn IMU Sensors for Motion Tracking
| Sensor Device | Acceleration RMSE (m·s⁻²) | Acceleration R² | Angular Velocity RMSE (rad·s⁻¹) | Angular Velocity R² |
|---|---|---|---|---|
| Research-grade (Xsens) | 1.66 ± 0.12 | 0.78 ± 0.02 | Benchmark | Benchmark |
| Consumer-grade (Apple Watch Series 5) | 2.29 ± 0.09 | 0.56 ± 0.01 | 0.22 ± 0.02 | 0.99 ± 0.00 |
| Consumer-grade (Apple Watch Series 3) | 2.14 ± 0.09 | 0.49 ± 0.02 | 0.18 ± 0.01 | 1.00 ± 0.00 |
| Research-grade (Axivity AX3) | 4.12 ± 0.18 | 0.34 ± 0.01 | Data not specified | Data not specified |
For linear acceleration, the research-grade Xsens sensor was significantly more accurate than the consumer-grade smartwatches [65]. However, for angular velocity, the consumer-grade Apple Watches achieved remarkably high accuracy (R² ≈ 1.00), comparable to the research-grade benchmark [65]. This indicates that the suitability of a consumer-grade sensor is highly dependent on the specific kinematic parameter of interest.
Experimental Protocols for Validating Sensor Accuracy
Protocol for Optical Heart Rate Sensor Validation
The study investigating PPG accuracy used a structured protocol designed to assess sensors under various physiological states [13]:
- Reference Standard: A single-lead ECG patch (Bittium Faros 180) was used as the ground truth for heart rate.
- Participant Demographics: 53 individuals (32 female, 21 male; ages 18–54) with equal representation across all six Fitzpatrick skin tone groups.
- Test Protocol (Approx. 1 hour per participant):
- Seated Rest: 4 minutes to establish a baseline.
- Paced Deep Breathing: 1 minute to introduce minor, controlled variation.
- Physical Activity: 5 minutes of walking to increase heart rate up to 50% of the recommended maximum.
- Seated Rest: ~2 minutes for a washout period from physical activity.
- Typing Task: 1 minute to simulate low-intensity daily activity.
- Data Analysis: Mean Absolute Error (MAE) and Mean Directional Error (MDE) were calculated for each device against the synchronized ECG reference.
Protocol for Inertial Sensor Validation
The validation of IMU sensors for motion tracking involved a direct comparison with an optical gold standard in a controlled laboratory setting [65]:
- Reference Standard: Optical motion tracking system (OptiTrack).
- Sensor Mounting: All tested IMU sensors (Xsens MTw Awinda, Axivity AX3, Apple Watch Series 3 & 5) were securely mounted on the same rigid platform and on the participant's wrist to ensure simultaneous data collection under identical movements.
- Movement Tasks: Participants performed a series of naturalistic movements and functional tasks to capture a range of kinematic data.
- Data Processing: Raw accelerometer and gyroscope data were synchronized with the optical tracking data. Accuracy was quantified using Root Mean Square Error (RMSE) and the coefficient of determination (R²) for both linear acceleration and angular velocity.
Advanced Sensor Designs for Enhanced Accuracy
Beyond validating existing devices, research is focused on novel sensor designs to overcome inherent limitations. Key advancements include:
- Material Science Innovations: A 2025 study presented a breathable pressure sensor combining MXene nanosheets with a porous polyester textile [66]. This design achieved a high sensitivity of 652.1 kPa⁻¹ and a fast response/recovery time of 36 ms/20 ms, enabling precise capture of arterial pulse waveforms for cardiovascular diagnostics.
- Optical Sensor Refinement: A novel wearable sensor based on a flexible "W-shaped" microfiber structure demonstrated high sensitivity to low-pressure signals, such as the pulse [67]. When packaged with PDMS, the sensor achieved a sensitivity of 38.77 nm/N in the low-pressure range (0–0.1 N), making it suitable for detecting weak physiological signals.
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Key Research Reagent Solutions for Wearable Sensor Validation
| Item | Function / Application | Example / Specification |
|---|---|---|
| ECG Monitor | Gold-standard reference for heart rate validation. | Bittium Faros 180 [13] |
| Optical Motion Capture | Gold-standard reference for kinematic and motion tracking validation. | OptiTrack system [65] |
| Research-Grade IMU | High-accuracy benchmark for validating consumer inertial sensors. | Xsens MTw Awinda [65] |
| Fitzpatrick Skin Tone Scale | Standardized scale for ensuring participant diversity and assessing bias. | 6-point scale with equal representation [13] |
| Programmable Tilt/Motion Stage | For controlled sensor characterization and calibration. | Used with push-pull gauge for pressure testing [67] |
| PDMS (Polydimethylsiloxane) | A common polymer for encapsulating and protecting flexible sensors, enhancing sensitivity and skin contact. | SYLGARD 184 [67] |
| MXene Nanosheets | Conductive nanomaterial used in advanced flexible sensors to enhance sensitivity and detection range. | Ti₃C₂Tₓ MXene [66] |
The journey from surface-level data to clinically actionable insights relies on rigorous, standardized validation and continuous technological innovation. The data presented in this guide demonstrates that while significant progress has been made—especially in mitigating concerns about skin tone bias—challenges related to motion and device-specific performance remain. For researchers and drug development professionals, the choice of a wearable sensor must be guided by the specific physiological parameter of interest and a critical evaluation of validation data against the appropriate clinical gold standard. The emerging generation of sensors, leveraging new materials and sophisticated algorithms, holds the promise of finally closing the accuracy gap.
The adoption of commercial wearable optical sensors in scientific and drug development research is rapidly increasing, promising continuous, real-time physiological data collection in free-living conditions [68] [52]. These devices, primarily using photoplethysmography (PPG) technology, offer an attractive alternative to traditional clinical measurements confined to laboratory or hospital settings [18]. However, their integration into rigorous research is hampered by a fundamental challenge: the "black box" problem of proprietary algorithms that transform raw sensor data into actionable health metrics.
This algorithmic opacity creates significant barriers for researchers and clinicians who require fully transparent, validated, and reproducible methods. While these devices can collect data on a 24/7 basis as people go through their daily routines [52], the inability to inspect or modify the algorithms processing this data raises questions about validity, reliability, and applicability across diverse population groups [28] [18]. This guide systematically compares the performance of commercial wearable optical sensors against clinical gold standards, examines the experimental protocols for their validation, and provides frameworks for addressing algorithmic transparency in rigorous research contexts.
Performance Gap: Commercial Wearables vs. Clinical Gold Standards
Commercial wearable devices demonstrate promising but variable accuracy when benchmarked against clinical-grade monitoring systems. The table below summarizes quantitative performance data across key physiological parameters.
Table 1: Accuracy comparison between commercial wearables and clinical gold standards
| Physiological Parameter | Commercial Wearable Technology | Clinical Gold Standard | Reported Accuracy | Contextual Limitations |
|---|---|---|---|---|
| Atrial Fibrillation Detection | Smartwatch PPG algorithms [68] | Clinical ECG [2] | Sensitivity: 94.2% Specificity: 95.3% [68] | Performance varies with motion artifacts and skin tone [18] |
| Heart Rate Monitoring | Wrist-worn reflective PPG [18] | ECG/Medical-grade PPG [2] [18] | Decreases during intense physical activity [2] | Reflective PPG generally less precise than transmissive PPG for microvascular changes [18] |
| Step Counting | Wrist-worn accelerometers [2] | Direct observation/Video recording [28] | Miscounts during erratic movement or driving [2] | Accuracy substantially decreases at slower walking speeds [28] |
| Sleep Stage Classification | Consumer sleep trackers (motion, heart rate, SpO2) [2] | Polysomnography [2] | Limited accuracy for sleep stage differentiation [2] | Considered rough guide rather than clinical diagnostic [2] |
| COVID-19 Detection | Multi-parameter algorithms (heart rate, steps, sleep) [68] | PCR testing [68] | AUC: 80.2% Sensitivity: 79.5% Specificity: 76.8% [68] | Cannot distinguish from other respiratory infections [69] |
| Physical Activity Intensity | Fitbit Charge 6 [28] | Indirect calorimetry/Direct observation [28] | Ongoing validation in specialized populations [28] | Accuracy affected by movement patterns in clinical populations [28] |
The performance data reveals a consistent pattern: while commercial wearables show adequate accuracy for general wellness tracking, they demonstrate limitations in clinical and research applications, particularly in specialized populations and challenging measurement conditions.
Experimental Protocols for Validating Wearable Algorithms
Laboratory vs. Free-Living Validation Frameworks
Rigorous validation of wearable device accuracy requires multi-stage protocols conducted across both controlled laboratory and free-living environments. The V3-stage process (Verification, Analytical Validation, and Clinical Validation) provides a comprehensive framework for establishing device reliability [70].
Table 2: Key components of a comprehensive wearable validation protocol
| Protocol Component | Laboratory Setting | Free-Living Setting | Gold Standard Comparators |
|---|---|---|---|
| Participant Recruitment | Controlled demographics and health status [28] | Representative of target population [28] | Inclusion/exclusion criteria clearly defined [28] |
| Device Configuration | Simultaneous wearing of all devices [28] | Extended wear (typically 7+ days) [28] | Consistent placement and orientation [28] |
| Structured Activities | Variable-paced walking, posture changes [28] | Natural activities of daily living [68] | Video recording with time synchronization [28] |
| Data Analysis | Bland-Altman plots, Intraclass correlation [28] | Machine learning for pattern detection [68] | Statistical comparisons with reference methods [28] |
Specialized Population Considerations
Validation protocols must account for disease-specific factors that may impact measurement accuracy. For example, studies validating devices in patients with lung cancer must consider their unique mobility challenges, gait impairments, and significantly slower walking velocities that affect device performance [28]. Similar considerations apply to other clinical populations with altered movement patterns or physiology.
Wearable Device Validation Workflow: Comprehensive framework for validating commercial wearable devices against gold standards in both laboratory and free-living environments.
Technical Foundations: How Wearable Optical Sensors Work
PPG Technology and Its Limitations
Commercial wearable devices primarily utilize reflective photoplethysmography (PPG), an optical technique that measures blood volume changes in peripheral circulation [18]. A typical PPG system consists of a light-emitting diode (LED) that emits light (typically green, red, or near-infrared) into the skin and a photodetector (PD) that captures the backscattered light modulated by cardiac-induced blood volume changes [18].
The fundamental challenge with reflective PPG involves its susceptibility to motion artifacts and signal quality variability based on skin tone, sensor-skin contact, and anatomical placement [2] [18]. Green illumination, common in reflection-mode PPG, is more strongly absorbed by melanin, reducing accuracy for darker skin tones and often requiring extra calibration [18]. This has significant implications for equitable algorithm performance across diverse populations.
The Data Processing Pipeline
The transformation from raw PPG signals to physiological parameters involves multiple processing stages where algorithmic opacity becomes problematic:
- Signal Quality Assessment: Algorithms identify and exclude noisy data segments
- Feature Extraction: Key waveform characteristics are identified (pulse peaks, amplitude, etc.)
- Physiological Parameter Calculation: Heart rate, heart rate variability, respiratory rate, etc.
- Post-Processing: Smoothing, outlier removal, and data integration
At each stage, proprietary algorithms make decisions that significantly impact the final output without researcher visibility into the decision criteria or parameters.
Table 3: Essential research reagents and solutions for wearable validation studies
| Tool Category | Specific Examples | Research Function | Considerations |
|---|---|---|---|
| Reference Standard Devices | ActiGraph LEAP, activPAL3 micro [28] | Research-grade comparators for consumer devices | Require proper calibration and placement protocols |
| Data Collection Platforms | Video recording systems with time synchronization [28] | Gold-standard validation for activity classification | Must ensure participant privacy and data security |
| Statistical Analysis Tools | Bland-Altman plots, Intraclass Correlation Coefficient (ICC) [28] | Quantify agreement between wearable and reference standard | Appropriate for continuous data with adequate sample size |
| Clinical Assessment Tools | Validated survey instruments (symptom burden, quality of life) [28] | Control for confounding factors influencing movement patterns | Must be administered pre- and post-data collection |
| Algorithm Development Platforms | Open-source signal processing libraries (Python, R) | Develop transparent alternatives to proprietary algorithms | Require expertise in digital signal processing and machine learning |
Emerging Solutions: Toward Transparent Algorithmic Frameworks
Standardized Validation Protocols
The field is moving toward standardized validation frameworks specifically designed for wearable technologies. These include disease-specific validation protocols that account for unique movement patterns in clinical populations [28], and the development of comprehensive recommendation frameworks for future validation studies.
Open-Source Algorithm Initiatives
Increasing recognition of the "black box" problem has spurred development of open-source algorithmic approaches that provide full transparency into signal processing and feature extraction methods. These initiatives enable researchers to understand, modify, and validate every step of the data transformation process.
Multi-Modal Sensing Approaches
Emerging research demonstrates that combining multiple sensing modalities (electrical, optical, thermal) can improve accuracy and provide cross-validation opportunities [15]. For example, integrating PPG with electrochemical sensors creates redundant measurement pathways that can identify algorithm failures.
Algorithm Transparency Framework: Mapping the "black box" problem in wearable data processing and emerging solutions for research applications.
The algorithm transparency problem in commercial wearable devices presents significant challenges for research applications requiring rigorous validation and reproducibility. While these devices offer unprecedented opportunities for continuous physiological monitoring in naturalistic settings, their proprietary algorithms create uncertainty in data interpretation and limit scientific scrutiny.
Researchers can navigate these limitations by implementing comprehensive validation protocols that benchmark commercial devices against clinical gold standards across diverse populations and activity profiles. The development of open-source algorithmic alternatives and standardized validation frameworks promises to address current transparency gaps. As the field evolves, collaboration between device manufacturers and research communities will be essential for developing sufficiently transparent algorithmic frameworks that maintain both commercial intellectual property and scientific rigor.
For drug development professionals and clinical researchers, a cautious, validation-focused approach remains essential when incorporating commercial wearable data into regulatory decisions or clinical trial endpoints. The performance gaps identified in this guide highlight the importance of context-specific validation rather than universal acceptance of manufacturer-reported accuracy claims.
Wearable optical sensors, such as those using photoplethysmography (PPG), have emerged as powerful tools for continuous, non-invasive health monitoring in clinical research and drug development [24] [1]. These sensors leverage optical phenomena to capture physiological data by measuring light absorption and reflection in vascular tissues, providing insights into parameters like heart rate, heart rate variability, and oxygen saturation [24] [1]. However, the translation of these technologies from consumer applications to rigorous clinical research contexts necessitates a critical examination of the engineering constraints that govern their performance, particularly battery life and usability, and their subsequent impact on data quality [71] [72].
The core challenge lies in balancing the conflict between device miniaturization, limited battery capacity, and the demand for research-grade data acquisition [24] [73]. Finite battery capacity directly influences component selection, sensor duty cycling, wireless communication protocols, and onboard processing capabilities [71]. These power-saving strategies, while extending operational life, can introduce significant artifacts, noise, and biases that compromise data fidelity [72]. For researchers relying on these devices for endpoint analysis in clinical trials, understanding these constraints is paramount for evaluating the validity and reliability of collected data against established clinical gold standards [1] [70].
This guide objectively compares the performance of wearable optical sensors within the framework of these engineering limitations. It synthesizes experimental data on their accuracy, details the methodologies behind key validation studies, and provides a framework for researchers to assess the suitability of these technologies for specific clinical research applications.
Performance Comparison: Wearable Optical Sensors vs. Clinical Gold Standards
The accuracy of physiological data from wearable optical sensors is a primary concern for research applications. The following tables summarize validation data and technical specifications from comparative studies, highlighting the impact of engineering constraints on data quality.
Table 1: Accuracy of Heart Rate Monitoring from Consumer Wearables vs. Reference Standards
| Device/Sensor Type | Testing Condition | Reference Standard | Mean Absolute Error (MAE) | Correlation with Reference | Key Limitations & Data Quality Impact |
|---|---|---|---|---|---|
| PPG-based Smartwatch [1] | At Rest | ECG | ~2 beats per minute (bpm) [1] | Moderate to Excellent [1] | Susceptible to motion artifacts; requires stable fit and skin contact [24] [1] |
| PPG-based Smartwatch [1] | During Peak Exercise | ECG | Limits of Agreement widened (≥7% outliers) [1] | Reduced vs. rest | Arm movement and sweat degrade signal-to-noise ratio (SNR) [1] |
| Pulse Oximetry (Wrist) [24] | At Rest | Clinical Pulse Oximeter | Varies by manufacturer | Good | Ambient light interference can cause data loss, necessitating repeated measurements [24] |
Table 2: Impact of Engineering Constraints on Data Quality and Usability
| Engineering Constraint | Common Power-Saving Strategy | Impact on Data Quality & Usability | Evidence/Manifestation |
|---|---|---|---|
| Limited Battery Capacity [71] [73] | Duty-cycling of high-power sensors (e.g., PPG, GPS) [71] | Gaps in Data: Missed physiological events. Reduced Temporal Resolution: Inability to capture high-frequency phenomena [71]. | Optical sensors for heart rate or SpO₂ are often duty-cycled instead of running continuously [71]. |
| Wireless Data Transmission [71] | Use of Bluetooth Low Energy (BLE) vs. continuous Wi-Fi/Cellular [71] | Data Packet Loss: Can occur with low-power protocols. Processing Delays: On-device summarization vs. raw data streaming [71] [72]. | BLE allows 24/7 data streaming on a single charge but may prioritize battery life over data completeness [71]. |
| On-board Processing [71] [74] | Hierarchical sensing; low-power cores for basic analysis [71] | Algorithmic Artifacts: Proprietary algorithms may obscure raw signals. Reduced Data Transparency: Lack of access to raw waveform data for independent validation [1] [74]. | Low-power accelerometer remains on to trigger wake-up of higher-power PPG sensor only when motion is detected [71]. |
| Form Factor & Wearability [24] [73] | Miniaturization; "skin-like" flexible designs [24] | Signal Drift: Poor skin contact from rigid designs. User Non-Compliance: Bulky or uncomfortable devices are removed by users, creating data gaps [24] [75]. | Flexible, "skin-like" sensing devices improve conformity and signal stability but present battery integration challenges [24]. |
Experimental Protocols for Validating Wearable Sensor Accuracy
The following methodologies are commonly employed in rigorous experiments to quantify the performance and limitations of wearable optical sensors.
Protocol 1: Validation of Heart Rate and Pulse Rate Variability
Objective: To assess the accuracy of wearable-derived heart rate (HR) and pulse rate variability (PRV) against gold-standard electrocardiography (ECG) across various physiological states [1].
- Participant Recruitment & Setup: A cohort of participants is fitted with a 12-lead ECG or a Holter monitor for continuous ECG recording. On the contralateral wrist, the consumer-grade wearable device(s) under investigation are secured as per manufacturer guidelines [1].
- Testing Protocol: Participants undergo a multi-stage protocol:
- Resting Baseline: Seated or supine rest for 10-20 minutes to establish baseline measures [1].
- Controlled Activity: A structured activity, such as walking on a treadmill at a slow pace, to introduce low-level motion.
- Moderate-Vigorous Exercise: A graded exercise test (e.g., on a cycle ergometer or treadmill) with increasing intensity to elevate heart rate and induce significant motion and sweat [1].
- Recovery Period: Post-exercise monitoring to capture the return to baseline.
- Data Analysis:
- Heart Rate: The R-R intervals from the ECG are used to compute gold-standard HR. This is compared to the HR and pulse-to-pulse intervals from the wearable's PPG signal on a beat-to-beat or epoch-by-epoch basis. Metrics such as Mean Absolute Error (MAE), Mean Absolute Percentage Error (MAPE), and Bland-Altman limits of agreement are calculated [1].
- PRV vs. HRV: Pulse rate variability (PRV) is derived from the wearable's pulse intervals, while heart rate variability (HRV) is derived from the ECG's R-R intervals. Time-domain (e.g., SDNN, RMSSD) and frequency-domain (e.g., LF, HF power) metrics are compared between PRV and HRV to determine their equivalence and the impact of motion on PRV accuracy [1].
Protocol 2: Impact of Power Management on Signal Integrity
Objective: To evaluate how battery-driven power management strategies, such as sensor duty-cycling and signal averaging, affect the integrity and clinical utility of physiological waveforms [71] [72].
- Experimental Setup: A wearable device is configured to operate in different power modes, ranging from a "high-performance" continuous mode to various "power-saver" modes that involve intermittent sensor sampling or increased signal averaging periods.
- Stimulus and Recording: Participants perform a standardized set of movements or breathing maneuvers while data is collected simultaneously from the wearable (in its various modes) and a high-fidelity, clinical-grade reference device (e.g., medical PPG, continuous ECG).
- Data Integrity Analysis:
- Signal-to-Noise Ratio (SNR): SNR is calculated for the PPG waveform across different power modes and activity levels [24].
- Feature Detection Accuracy: The ability of the device's algorithm to accurately identify specific waveform features (e.g., pulse arrival time, diastolic peak) is compared against expert-annotated reference signals. The error rates are correlated with the active power mode.
- Polarization and Hysteresis: The impact of rapid, successive cycling (a common real-world use case) is analyzed for the introduction of reversible polarization effects in the signal, which can be mistaken for physiological trends in long-term data [72].
Visualization of Engineering Constraints and Data Quality Pathways
The following diagram illustrates the logical relationships between core engineering constraints, the mitigation strategies employed, and their ultimate impact on the data quality of wearable optical sensors.
Diagram 1: Pathway from engineering constraints to data quality impacts in wearable optical sensors.
The Scientist's Toolkit: Research Reagents and Essential Materials
For researchers designing validation studies or working with data from wearable optical sensors, understanding the key components and their functions is critical.
Table 3: Essential Materials and Reagents for Wearable Sensor Research
| Item/Category | Function in Research & Validation | Examples & Notes |
|---|---|---|
| Gold-Standard Reference Devices | Provides the ground truth against which wearable sensor data is validated for accuracy and reliability. | Clinical-grade ECG systems, medical pulse oximeters, ambulatory blood pressure monitors [1]. |
| Signal Simulators & Phantoms | Generates consistent, known physiological signals to bench-test sensor performance and algorithms in a controlled environment. | PPG waveform simulators, mechanical motion platforms to simulate arm movement. |
| Low-Power Microcontrollers (MCUs) | The core processing unit in wearables; its architecture dictates the power-performance trade-off and available sleep modes [71] [73]. | ARM Cortex-M series; selected for rich power-management features and ultra-low deep-sleep currents [71]. |
| Bluetooth Low Energy (BLE) Modules | The primary wireless communication link for most consumer wearables; its configuration directly impacts battery life and data transmission reliability [71]. | Nordic Semiconductor nRF52/nRF53 series; chosen for their optimized power profile for intermittent data transfer [71]. |
| Flexible Substrates & Conductive Inks | Enables the development of "skin-like" flexible sensors that improve wearability and signal quality by conforming to the skin [24]. | Polyimide, PET films; silver/silver-chloride conductive inks for electrodes. |
| Data Analysis Software (Open-Source) | Used for processing raw sensor data, performing signal filtering, and conducting independent statistical analysis without relying on proprietary black-box algorithms. | Python (with NumPy, SciPy, Pandas), R, MATLAB; essential for calculating HRV, SNR, and performing Bland-Altman analysis [72] [1]. |
The integration of wearable sensors into clinical and research paradigms hinges on a critical question: Can data from consumer-grade optical sensors achieve accuracy comparable to clinical gold standards? While traditional medical devices like the 12-lead electrocardiogram (ECG) and Holter monitors are benchmarks for cardiac monitoring, their bulkiness, cost, and short-term use limit continuous, real-world monitoring [39] [1]. Wearable optical sensors, primarily using photoplethysmography (PPG), offer a non-invasive, continuous alternative but face challenges from motion artifacts, skin tone, and physiological variability [1] [2]. Emerging solutions are addressing these limitations through novel hardware designs, adaptive artificial intelligence (AI) algorithms, and multi-modal sensing approaches, bridging the accuracy gap and expanding the role of wearables in digital health.
Sensor Technologies and Clinical Gold Standards
Fundamental Sensing Modalities
Wearable sensors and clinical systems operate on distinct technological principles, which fundamentally influence their accuracy and application.
Photoplethysmography (PPG) in Wearables: PPG is an optical technique used in most consumer wearables [1]. A light-emitting diode (LED) shines light onto the skin, and a photodetector measures the intensity of light reflected back from blood vessels. Pulsatile blood flow causes minor variations in light absorption, generating a pulse wave that can estimate heart rate (HR) and, through derived calculations, pulse rate variability (PRV) [1]. However, the PPG signal is a surrogate for the cardiac electrical activity and is highly susceptible to corruption from motion, ambient light, and skin perfusion [1] [2].
Clinical Gold Standards:
- Electrocardiography (ECG): This gold-standard non-invasive method measures the heart's electrical activity through electrodes placed on the body [1]. It provides a direct measurement of the cardiac cycle, from which R-R intervals are used to calculate highly accurate heart rate and heart rate variability (HRV) [39] [1].
- Holter Monitor: A portable ECG device worn for 24-72 hours, it provides a continuous, clinical-grade record of heart rhythm and is essential for diagnosing intermittent arrhythmias [39] [2].
Comparative Accuracy of Heart Rate Monitoring
The table below summarizes key validation findings comparing wearable PPG-based HR monitoring against clinical gold standards.
Table 1: Accuracy Comparison of Wearable Heart Rate Monitoring vs. Gold Standards
| Device / Study | Population | Reference Standard | Accuracy Metric | Key Findings | Contextual Factors |
|---|---|---|---|---|---|
| Corsano CardioWatch Bracelet [39] | Pediatric Cardiology (n=31, mean age 13.2y) | 24-hour Holter ECG | Mean Bias: -1.4 BPM95% LoA: -18.8 to 16.0 BPMMean Accuracy: 84.8% | Good agreement with Holter, but accuracy declined at higher heart rates and during intense bodily movement. | Accuracy was significantly higher during lower heart rates (90.9%) vs. high heart rates (79.0%). |
| Hexoskin Smart Shirt [39] | Pediatric Cardiology (n=36, mean age 13.3y) | 24-hour Holter ECG | Mean Bias: -1.1 BPM95% LoA: -19.5 to 17.4 BPMMean Accuracy: 87.4% | Good agreement with Holter. Accuracy was higher in the first 12 hours (94.9%) vs. the latter 12 (80.0%). | Accuracy declined with higher heart rates and increased bodily movement. |
| Consumer Wearables (Systematic Review) [1] | Mixed (29 studies) | ECG, Chest Straps, Pulse Oximetry | 56.5% within ±3% error | At rest, wearables are widely accurate (mean absolute error ~2 BPM). Accuracy declines during physical activity, with wider limits of agreement. | Arm movement, activity type, contact pressure, and sweat impact accuracy during exercise. |
Beyond Heart Rate: Arrhythmia Detection and HRV/PRV
The scope of validation extends beyond basic heart rate to more complex physiological measures.
Arrhythmia Detection: The Hexoskin smart shirt, which uses embedded ECG electrodes rather than PPG, demonstrated the potential for arrhythmia screening. In a blinded analysis, a pediatric cardiologist correctly classified the shirt's rhythm recordings in 86% (31/36) of cases, indicating promise for diagnostic applications beyond simple heart rate tracking [39].
HRV vs. PRV: HRV derived from ECG is a validated marker of autonomic nervous system function [1]. Wearables often report "HRV" metrics calculated from the PPG pulse wave (Pulse Rate Variability or PRV). While studies show HRV from ECG and PPG can be similar, differences exist due to the pulse arrival time, and the terms are not interchangeable [1]. Consequently, validation of wearable-derived PRV against ECG-derived HRV is an active area of research.
Experimental Protocols for Validation
Rigorous validation is critical for establishing the credibility of wearable data. The following methodology from a pediatric study exemplifies a comprehensive protocol for benchmarking wearables against a gold standard [39].
Experimental Workflow
The diagram below illustrates the step-by-step validation protocol used to assess the accuracy of wearable devices.
Key Research Reagents and Solutions
The validation of wearable technologies relies on a suite of specific devices, software, and methodological tools.
Table 2: Essential Research Toolkit for Wearable Sensor Validation
| Category | Item | Specific Examples | Function in Research |
|---|---|---|---|
| Gold Standard Reference | Holter Monitor | Spacelabs Healthcare Holter [39] | Provides the benchmark ECG data for validating heart rate and rhythm from wearables. |
| Test Wearables | PPG-based Bracelet | Corsano CardioWatch 287-2B [39] | CE-marked medical wristband using reflective PPG to measure heart rate and R-R intervals. |
| ECG-based Garment | Hexoskin Pro Shirt [39] | Smart garment with textile electrodes for single-lead ECG, heart rate, and rhythm recording. | |
| Research-Grade Activity Monitors | Tri-axial Accelerometer | Built-in in wearables, ActiGraph LEAP [39] [17] | Quantifies bodily movement (in gravitational units, g) to correlate motion with measurement accuracy. |
| Data Analysis & Algorithms | Statistical Method | Bland-Altman Analysis [39] | Calculates bias and 95% limits of agreement (LoA) to assess the level of agreement between wearable and gold standard. |
| AI/ML Model | Convolutional Neural Networks (CNNs) [70] | Used in advanced wearables to identify and correct signal errors, improving arrhythmia detection and signal quality. | |
| Participant Assessment | Patient-Reported Outcome | 5-point Likert Scale Questionnaire [39] | Quantifies user satisfaction, comfort, and adherence, which are crucial for real-world applicability. |
Emerging Solutions to Enhance Accuracy
Novel Hardware and Multi-Modal Sensing
Innovations in hardware design focus on improving signal acquisition and reducing noise.
Anatomical Diversification: Moving beyond the wrist, chest-worn sensors (e.g., Polar H10) and smart shirts (e.g., Hexoskin) offer superior signal quality due to better skin contact and proximity to the heart, demonstrating strong correlations with ECG, especially during light-to-moderate activity [76]. Other form factors include rings and in-ear sensors.
Multi-Modal Sensor Fusion: Combining multiple sensing modalities in a single device counters the limitations of any single technology. For example, integrating PPG with an accelerometer allows algorithms to identify and filter out motion artifacts [39] [77]. Emerging systems also fuse electrochemical, colorimetric, and optical sensors to track a wider range of biomarkers (e.g., glucose, lactate) alongside vital signs, providing a more holistic health picture [77] [74].
Adaptive Algorithms and Artificial Intelligence
AI and machine learning are revolutionizing data processing and interpretation in wearables.
Error Correction and Signal Enhancement: AI algorithms can identify and correct inaccuracies in collected data. For instance, machine learning models can be trained to distinguish clean PPG signals from motion-corrupted ones, ensuring the reliability of heart rate data [77].
Cross-Sensitivity Resolution: In multi-modal sensing, the measurement of one signal can be influenced by another (cross-sensitivity). AI pattern recognition models, such as deep neural networks (DNNs), are trained to isolate individual signal contributions from mixed data, leading to more accurate measurements of specific biomarkers [77].
Predictive Analytics and Personalization: Moving beyond measurement, AI can analyze continuous data streams for predictive insights. For example, ML models have been used with wearable data to predict mortality in end-of-life cancer patients with high accuracy (93%) and construct risk profiles for conditions like heart failure [74] [70]. Furthermore, AI enables the personalization of monitoring by adapting to an individual's unique physiological baseline [77] [74].
Table 3: AI Algorithms and Their Applications in Wearable Sensing
| Algorithm Type | Example Application | Impact on Accuracy & Functionality |
|---|---|---|
| Deep Neural Networks (DNNs) | Multiplex detection of single particles and molecular biomarkers [77]. | Enables high-sensitivity detection of specific analytes in complex biological fluids like sweat and saliva. |
| Convolutional Neural Networks (CNNs) | Analysis of ECG and PPG waveforms for atrial fibrillation detection [70]. | Improves the diagnostic capability for specific cardiac arrhythmias from wearable-derived signals. |
| Supervised Machine Learning | Predictive analytics for mortality and risk stratification in cancer patients [74]. | Transforms raw sensor data into clinically actionable prognostic information. |
| Reinforcement Learning | Energy-efficient routing in wireless body area sensor networks (WBSNs) [77]. | Optimizes power consumption in multi-sensor systems, enabling longer and more continuous monitoring. |
The convergence of novel hardware, multi-modal sensing, and adaptive AI algorithms is decisively narrowing the performance gap between consumer wearable optical sensors and clinical gold standards. While challenges related to motion artifacts, signal fidelity during high-intensity activity, and rigorous clinical validation remain, the trajectory of innovation is clear. Future work must focus on large-scale, diverse clinical trials, standardization of validation protocols, and the development of explainable AI to foster trust among clinicians and researchers [39] [17] [70]. As these technologies mature, they are poised to unlock a new era of personalized, predictive, and participatory medicine, transforming both clinical practice and population health research.
Benchmarks and Credibility: Validation Frameworks and Comparative Performance Analysis
The integration of wearable optical sensors into clinical research and drug development represents a significant advancement in digital health. These technologies enable continuous, remote monitoring of physiological parameters, offering a more dynamic picture of patient health than traditional, episodic measurements taken in clinical settings [78]. However, for the data from these consumer-grade devices to be considered reliable and actionable for research and regulatory decision-making, they must be rigorously validated against established clinical gold standards and navigate a complex regulatory landscape. This guide provides a comparative analysis of the performance of wearable optical sensors against clinical-grade devices, framed within the critical context of AAMI/ESH/ISO validation standards and FDA regulatory requirements.
Regulatory and Standards Framework
For a wearable optical sensor to be used in clinical research or as a medical device, it must demonstrate its accuracy and reliability through recognized standards and comply with relevant regulations.
FDA Quality System Regulation (QMSR) The U.S. Food and Drug Administration (FDA) governs medical devices under the Quality Management System Regulation (QMSR). A significant update, effective February 2, 2026, harmonizes the existing FDA Quality System (QS) Regulation with the international standard ISO 13485:2016 [79]. This rule incorporates ISO 13485 by reference, making its requirements for a comprehensive quality management system—with a strong emphasis on risk management throughout the product lifecycle—enforceable by the FDA [79]. Furthermore, for electronic records and signatures, FDA 21 CFR Part 11 defines criteria for system validation, audit trails, and access controls to ensure data integrity, security, and traceability [80].
AAMI/ESH/ISO Validation Standards The AAMI/ESH/ISO Universal Standard (ISO 81060-2) is a benchmark for validating non-invasive blood pressure measuring devices [81]. For cuffless devices, like many optical sensors, this standard is adapted. The protocol typically involves a simultaneous comparison of the test device and a reference method (e.g., auscultation) on opposite arms. Key validation criteria often include ensuring that the mean difference between the test device and the reference standard is ≤5 mmHg, with a standard deviation ≤8 mmHg [81].
Table 1: Key Regulatory and Standardization Bodies
| Body/Acronym | Full Name | Primary Role |
|---|---|---|
| FDA | U.S. Food and Drug Administration | Regulates medical devices, foods, cosmetics, and other products in the United States [80]. |
| AAMI | Association for the Advancement of Medical Instrumentation | Develops standards and recommended practices for medical devices and technology. |
| ESH | European Society of Hypertension | Provides scientific expertise and guidelines related to hypertension and BP measurement. |
| ISO | International Organization for Standardization | Develops and publishes international standards for various industries, including medical devices. |
| USP | United States Pharmacopeia | Develops public quality standards for medicines and other products [82]. |
Comparative Performance Analysis of Wearable Sensors
A growing body of research directly compares the accuracy of consumer-grade wearable sensors and research-grade prototypes against established clinical devices. The data reveals a performance spectrum highly dependent on the physiological parameter being measured, device type, and activity level.
Heart Rate Monitoring
Heart rate (HR) is one of the most commonly tracked metrics. Validation studies show that at rest and during low-intensity activities, wearable optical sensors demonstrate good to excellent agreement with clinical gold standards like electrocardiography (ECG).
- Low-Cost Prototype Validation: A study of a low-cost wearable prototype (nRF52840 MCU) showed clinically acceptable agreement with commercial devices, with Bland-Altman analysis revealing agreement thresholds of ±5–10 bpm for heart rate across different body positions (Rest, Sitting, Standing) [83].
- Consumer-Grade Wearables: A systematic review found that at rest, 56.5% of HR measurements from commercial wearables (e.g., Fitbit, Apple Watch) were within a ±3% error margin compared to reference methods like ECG [1]. Accuracy, however, decreases with higher-intensity physical activity due to motion artifacts [1] [84]. A laboratory study comparing the consumer-grade Withings Pulse HR to a research-grade chest strap (Faros Bittium 180) found good agreement at rest and slow walking (|bias| ≤ 3.1 bpm), but agreement deteriorated at higher treadmill speeds (|bias| ≤ 11.7 bpm) [84].
Blood Pressure and Oxygen Saturation
Cuffless blood pressure estimation and SpO₂ measurement are active areas of innovation for optical wearables, but they present significant validation challenges.
- Blood Pressure Trend Monitoring: The low-cost wearable prototype study demonstrated clinically acceptable agreement of ±5 mmHg for blood pressure trend (BPT) when compared to a commercial device. The study highlighted that sensor placement (finger vs. earlobe) significantly impacts stability and accuracy under different physiological conditions [83].
- Smartphone-Based BP Validation: The OptiBP smartphone application, which uses a fingertip on the camera to derive BP via photoplethysmography, successfully fulfilled modified AAMI/ESH/ISO validation requirements in a general population. The mean difference against auscultatory reference was 0.5 ± 7.7 mmHg for systolic BP and 0.4 ± 4.6 mmHg for diastolic BP [81].
- Oxygen Saturation: The same prototype study reported a clinically acceptable agreement of ±4% for SpO₂ when validated against a commercial pulse oximeter (UT-100) [83].
Body Temperature and Physical Activity
- Body Temperature: Agreement for body temperature is more variable. The low-cost wearable prototype reported a clinically acceptable agreement of ±0.5 °C [83]. In contrast, a consumer-grade Tucky thermometer showed poor agreement with a research-grade Tcore sensor during both rest and activity (|bias| ≥ 0.8°C), indicating that not all consumer devices are suitable for rigorous core temperature monitoring [84].
- Step Count and Energy Expenditure: The accuracy of step count from consumer wearables (e.g., Withings Pulse HR) decreases during structured treadmill tests, with bias increasing at higher activity levels [84]. Energy expenditure estimation is particularly challenging, with studies showing poor agreement (|bias| ≥ 1.7 MET) with the gold standard indirect calorimetry method [84].
Table 2: Summary of Wearable Sensor Accuracy vs. Clinical Standards
| Physiological Parameter | Clinical Gold Standard | Wearable Technology | Level of Agreement | Key Contextual Factors |
|---|---|---|---|---|
| Heart Rate (HR) | Electrocardiography (ECG) [1] | PPG-based Optical Sensors [83] [1] | Good at rest & low activity; declines with intensity [1] [84] | Motion artifacts, sensor contact, activity type [1] |
| Blood Pressure (BP) | Auscultation / Oscillometric Sphygmomanometer [81] | Cuffless PPG & Smartphone Apps (e.g., OptiBP) [83] [81] | Meets modified AAMI/ESH/ISO standards in controlled studies [81] | Sensor placement (finger, earlobe), body position [83] |
| Oxygen Saturation (SpO₂) | Medical Pulse Oximetry (e.g., UT-100) [83] | Reflectance PPG Sensors [83] | Clinically acceptable (±4%) [83] | Body position, peripheral perfusion [83] |
| Body Temperature | Clinical Thermometer [83] | Infrared Sensors (prototype) [83] / Consumer-grade [84] | Variable: Prototype ±0.5°C [83]; Consumer-grade poor [84] | Measurement site (skin vs. core), device quality [84] |
| Step Count | Manual Count / Video [84] | Tri-axial Accelerometry [84] | Accurate at low intensity; declines with complexity [84] | Arm movement, gait patterns [1] |
| Energy Expenditure | Indirect Calorimetry [84] | Proprietary Algorithms (HR + ACC) [84] | Poor agreement in lab studies [84] | Individual metabolic differences, algorithm limitations |
Experimental Protocols for Validation
Robust validation is not merely about the final results but hinges on a meticulously designed experimental protocol. The following methodologies are cited from key studies in the field.
Protocol for Multi-Parameter Wearable System Validation
A 2025 study provides a detailed protocol for validating a low-cost, multi-parameter wearable system [83]:
- Device Prototype: Built using an nRF52840 microcontroller, integrating PPG (MAX30102) for heart rate, SpO₂, and blood pressure trend (BPT), and an infrared sensor (MLX90614) for body temperature [83].
- Reference Devices: Compared against UT-100 pulse oximeter, G-TECH LA800 for blood pressure, and G-TECH THGTSC3 for body temperature [83].
- Participant Preparation: Ten participants were monitored over a ten-day period. Measurements were taken in three body positions (Rest, Sitting, Standing) to assess postural influences [83].
- Anatomical Configurations: The prototype was tested on two sites: the index finger (BPT-Finger) and the earlobe (BPT-Earlobe), with the reference device on the opposite hand or ear [83].
- Data Analysis: Bland-Altman analysis was used to determine the limits of agreement for each vital sign, establishing the clinically acceptable thresholds mentioned previously [83].
Protocol for Smartphone-Based BP App Validation
The validation of the OptiBP smartphone application followed a rigorous protocol based on the AAMI/ESH/ISO Universal Standard (ISO 81060-2:2018) with adaptations for a cuffless device [81]:
- Reference Method: A dual-head stethoscope was used by two independent, blinded observers with a calibrated sphygmomanometer. Observers were standardized for agreement before the study [81].
- Procedure: The study used the "opposite arm simultaneous method." After a 5-minute rest, reference BP and optical signals from the smartphone camera (via fingertip) were acquired simultaneously on opposite arms. The sides were switched after initial measurements [81].
- Data Quality Control: The protocol enforced strict exclusion criteria, including maximal observer disagreement (4 mmHg for SBP/DBP) and limits on variation between successive reference recordings (12/8 mmHg for SBP/DBP) [81].
- Participants: 91 subjects were recruited to fulfill gender, age, and BP distribution requirements of the AAMI/ESH/ISO standard. Individuals with certain cardiovascular conditions were excluded [81].
Diagram 1: AAMI/ESH/ISO Validation Workflow (Length: 87 characters)
The Scientist's Toolkit: Research Reagents and Materials
For researchers designing validation studies for wearable optical sensors, the following table details essential equipment and their functions as derived from the cited experimental protocols.
Table 3: Essential Research Materials for Wearable Sensor Validation
| Item / Reagent Solution | Function in Validation Research | Example Models / Types |
|---|---|---|
| Clinical-Grade Reference Device | Provides the "gold standard" measurement against which the wearable sensor is validated. | Thought Technology FlexComp [85], Faros Bittium 180 ECG [84], calibrated sphygmomanometer [81] |
| Wearable Sensor/Prototype | The device under test (DUT); the technology whose accuracy and reliability are being assessed. | nRF52840-based prototype [83], Empatica E4 [85], Withings Pulse HR [84] |
| Pulse Oximeter | Validates optical heart rate and SpO₂ measurements from wearables. | UT-100 pulse oximeter [83] |
| Data Acquisition & Synchronization System | Enables time-aligned collection of data from multiple devices, which is crucial for comparison. | Biograph Infinity Software [85], custom smartphone apps [85] [81] |
| Signal Processing & Analysis Software | Used for data cleaning, feature extraction, and statistical analysis (e.g., Bland-Altman plots). | Python with pyphysio package [85], custom algorithms for pulse wave analysis [81] |
| Calibration Equipment | Ensures reference devices maintain accuracy throughout the study period. | Calibration tools for sphygmomanometers [81] |
Wearable optical sensors show significant promise for decentralized health monitoring and clinical research, with studies demonstrating that properly calibrated devices can achieve clinically acceptable accuracy for parameters like heart rate, SpO₂, and blood pressure trends when validated against AAMI/ESH/ISO standards [83] [81]. However, their performance is not universal; it is highly dependent on sensor quality, anatomical placement, the physiological parameter being measured, and the user's activity level [83] [1] [84]. The evolving regulatory landscape, particularly the FDA's harmonization with ISO 13485, underscores the necessity of a robust, risk-managed quality system for any device intended for clinical or research use [79]. For researchers and developers, a thorough understanding of both the technical validation protocols and the regulatory pathways is essential for successfully translating these technologies from consumer gadgets into reliable tools for science and medicine.
Comparative Analysis of Sensor Performance for Key Metrics (e.g., VO₂max, HR, SpO₂)
Wearable optical sensors have become integral tools for health and performance monitoring in both consumer and research settings. The proliferation of devices from manufacturers like Garmin, Apple, and Fitbit has created a need for rigorous, independent validation of their accuracy against clinical gold standards. This comparative analysis synthesizes current research on the performance of wearable sensors for measuring key physiological metrics, including maximal oxygen uptake (VO₂max), heart rate (HR), and peripheral oxygen saturation (SpO₂). For researchers and drug development professionals, understanding the limitations and capabilities of these devices is crucial for their appropriate application in clinical trials and physiological monitoring.
Accuracy of VO₂max Estimation in Wearable Devices
Table 1: Validity of wearable-derived VO₂max estimates compared to laboratory gas analysis.
| Device | Population | Mean Absolute Percentage Error (MAPE) | Correlation/Concordance | Key Finding |
|---|---|---|---|---|
| Garmin fēnix 6 [86] | Apparently healthy adults (active & sedentary) | 7.05% (30s avg) | Lin's CCC = 0.73 (30s avg) | Met validation criteria (MAPE <10%, CCC >0.7) |
| Garmin Forerunner 245 [87] | All endurance athletes (moderately-to-highly trained) | 7.2% - 7.9% | ICC = 0.71 - 0.75 | Moderate agreement with criterion |
| Garmin Forerunner 245 [87] | Moderately trained athletes (VO₂max ≤ 59.8 ml/kg/min) | 2.8% - 4.1% | ICC = 0.63 - 0.66 | Good accuracy for this subgroup |
| Garmin Forerunner 245 [87] | Highly trained athletes (VO₂max > 59.8 ml/kg/min) | 9.4% - 10.4% | ICC = 0.34 - 0.41 | Systematic underestimation in elite athletes |
Accuracy of Heart Rate Monitoring in Wearable Devices
Table 2: Validity of wearable-derived heart rate measurements across conditions.
| Device Type | Condition | Mean Absolute Error (bpm) | Mean Absolute Percentage Error (MAPE) | Correlation | Key Finding |
|---|---|---|---|---|---|
| Consumer Wearables (Composite) [1] | At Rest | ~2 bpm | < 10% | Moderate to Excellent | High accuracy under resting conditions |
| Garmin & Fitbit [1] | Peak Exercise | Wider Limits of Agreement | ~7% (Garmin), ~12% (Fitbit) | - | Accuracy decreases with intensity; increased outliers |
| Consumer Wearables (Systematic Review) [1] | Across Conditions (29 studies) | - | 56.5% within ±3% error | - | Slight tendency to underestimate HR |
Accuracy of Blood Oxygen Saturation (SpO₂) Monitoring
Table 3: Validity of wearable-derived SpO₂ measurements.
| Device | Condition | Mean Absolute Percentage Error (MAPE) | Correlation/Concordance | Key Finding |
|---|---|---|---|---|
| Garmin fēnix 6 [86] | Combined (Normoxic & Hypoxic) | 4.29% | Lin's CCC = 0.10 | Failed accuracy validation; poor concordance |
| Consumer-Grade Devices [2] | Variable Conditions | Accuracy Varies | - | Affected by movement and skin tone |
Experimental Protocols for Sensor Validation
VO₂max Validation Protocol
The validation of VO₂max estimation in wearable devices typically follows a standardized two-phase protocol, as exemplified in recent studies on Garmin devices [86] [87].
Criterion Measure: Laboratory-based graded exercise test on a treadmill or cycle ergometer with breath-by-breath respiratory gas analysis using metabolic carts (e.g., ParvoMedics TrueOne 2400). VO₂max is determined as the highest average oxygen consumption over predefined timeframes (15s, 30s, 1min) [86].
Device Testing: Participants complete an outdoor run (10-15 minutes) at intensities exceeding 70% of their maximum heart rate, guided by the wearable device. The device uses proprietary algorithms incorporating heart rate (from chest strap or optical sensors), running speed, and GPS data to generate VO₂max estimates [86] [87].
Statistical Analysis: Studies employ correlation analyses (Intraclass Correlation Coefficients, Lin's Concordance Correlation Coefficient), error metrics (Mean Absolute Error, Mean Absolute Percentage Error), and equivalence testing (Bland-Altman plots) to compare device estimates with criterion measures [86] [87]. Validation criteria often pre-specify acceptable error margins (e.g., MAPE <10%, CCC >0.7) [86].
Heart Rate Validation Protocol
HR validation protocols typically compare wearable optical photoplethysmography (PPG) sensors against electrocardiography (ECG) or chest strap monitors as reference standards [88] [1].
Testing Conditions: Measurements are taken across multiple conditions: at rest, during controlled exercise at varying intensities, and during recovery. This allows assessment of accuracy across the physiological range [1].
Methodology: Simultaneous recordings from the wearable device and criterion measure are obtained during prescribed activities. The PPG sensors use green and infrared LEDs with photodetectors to measure blood volume changes at the wrist, from which pulse rate is derived [88] [1].
Analysis: Studies calculate agreement statistics, including mean absolute error, mean absolute percentage error, and limits of agreement, often stratifying results by activity type and intensity [1].
Blood Oxygen Saturation Validation Protocol
SpO₂ validation involves comparison with medical-grade pulse oximeters under various oxygen concentration conditions [86].
Testing Conditions: Participants are tested under normoxic (normal oxygen) and hypoxic conditions, the latter created using altitude simulator machines set to approximately 3657.6 meters (12,000 ft) to reduce blood oxygen levels [86].
Measurement Protocol: Simultaneous readings are taken from the wearable device and a medical-grade fingertip pulse oximeter. The wearable device is tested in different positions (e.g., posterior and anterior wrist) to assess positioning effects [86].
Analysis: Concordance correlation coefficients and mean absolute percentage error are calculated to determine agreement between the wearable and criterion device across conditions [86].
Visualizing Sensor Validation Workflows
Diagram 1: Wearable Sensor Validation Methodology. This workflow illustrates the standard protocol for validating wearable device accuracy against laboratory criterion measures.
Research Reagent Solutions
Table 4: Essential equipment and materials for wearable sensor validation research.
| Item | Function in Research | Example Models/Manufacturers |
|---|---|---|
| Metabolic Cart | Criterion measure for respiratory gas analysis during VO₂max testing | ParvoMedics TrueOne 2400 [86] |
| Medical-Grade Pulse Oximeter | Reference standard for SpO₂ validation | Roscoe Medical Fingertip Pulse Oximeter (Model: POX-ROS) [86] |
| ECG System/ Chest Strap Monitor | Gold-standard for heart rate and heart rate variability validation | POLAR H10 [89] |
| Treadmill/Ergometer | Standardized exercise protocol implementation | Technogym Excite Run 700 [89] |
| Altitude Simulator | Creates hypoxic conditions for SpO₂ validation under low oxygen | Hypoxico Everest Summit II [86] |
| Blood Lactate Analyzer | Criterion measure for lactate threshold validation | Biosen C-line (EKF) [89] |
Discussion
The collective evidence indicates that sensor performance varies significantly across different physiological metrics and population subgroups. For VO₂max estimation, devices demonstrate reasonable accuracy (MAPE ~7-8%) in general populations and moderately trained athletes [86] [87]. However, this accuracy diminishes in highly trained athletes with VO₂max values exceeding 60 ml·min⁻¹·kg⁻¹, where systematic underestimation and higher error rates (MAPE >10%) occur [87]. This limitation likely reflects algorithmic constraints in extrapolating from submaximal data to exceptional physiological capacities.
Heart rate monitoring shows the highest reliability among wearable metrics, particularly during rest and moderate-intensity exercise [1]. However, accuracy decreases during high-intensity activity, with widening limits of agreement and increased outliers [1]. This performance degradation is attributed to motion artifacts that disrupt PPG signal quality during vigorous movement [88] [1].
For SpO₂ monitoring, current wearable technology shows concerning limitations. The Garmin fēnix 6 demonstrated poor concordance with medical-grade equipment despite acceptable MAPE values, indicating systematic measurement errors that limit clinical utility [86]. This performance gap is particularly relevant for applications requiring precise oxygen saturation monitoring, such as pulmonary disease management or altitude acclimatization tracking.
The underlying technology influences these accuracy patterns. Wearables primarily utilize photoplethysmography (PPG), where light is emitted into the skin and reflected blood volume changes are detected [88] [1]. This method is susceptible to signal noise from motion, skin tone variations, and sensor placement [2] [1]. Additionally, most physiological estimates rely on proprietary algorithms that incorporate sensor data with user demographics and activity patterns, creating potential for population-specific biases [87] [90].
For researchers considering wearables in clinical trials or drug development, these findings highlight the importance of device selection based on target population and required precision. While consumer wearables offer practical advantages for continuous monitoring and large-scale data collection, their limitations necessitate caution when high measurement precision is required for decision-making.
The Role of Clinical Validation Studies in Home, Clinic, and ICU Settings
Clinical validation studies are fundamental to establishing that digital health technologies are fit-for-purpose in medical research and patient care [91]. For wearable optical sensors, these studies benchmark performance against clinical gold standards, quantifying metrics like accuracy and reliability to ensure data is trustworthy across diverse environments from controlled intensive care units (ICUs) to home settings [92] [83] [31]. This guide objectively compares the performance of various wearable devices against reference standards, detailing experimental methodologies and providing structured data to support evidence-based technology selection.
Performance Comparison of Wearable Optical Sensors vs. Clinical Gold Standards
The tables below summarize quantitative findings from clinical validation studies, comparing wearable optical sensors to established clinical gold standards across different settings and physiological parameters.
Table 1: Accuracy of a Low-Cost Wearable Sensor System vs. Commercial Devices (General Monitoring) [83]
| Vital Sign | Wearable Sensor Configuration | Reference Device | Agreement (Bland-Altman Limits) | Clinical Acceptance Threshold |
|---|---|---|---|---|
| Heart Rate (HR) | BPT-Finger & BPT-Earlobe | UT-100 Pulse Oximeter | ±5–10 bpm | Clinically Acceptable |
| Blood Oxygen Saturation (SpO₂) | BPT-Finger & BPT-Earlobe | UT-100 Pulse Oximeter | ±4% | Clinically Acceptable |
| Blood Pressure Trend (BPT) | BPT-Finger & BPT-Earlobe | G-TECH LA800 Sphygmomanometer | ±5 mmHg | Clinically Acceptable |
| Body Temperature | Arm-mounted IR Sensor | G-TECH THGTSC3 Thermometer | ±0.5 °C | Clinically Acceptable |
Table 2: Performance of Commercially Validated Wearable Patches in Clinical Settings [92] [31]
| Device Name | Key Monitored Parameters | Clinical Validation Context | Reported Performance / Utility |
|---|---|---|---|
| VitalPatch RTM | Single-lead ECG, RR, Temperature, Activity | Emergency Department (septic patients) | Detected significant vital sign changes 5.5 hours earlier than standard intermittent monitoring [92]. |
| BioButton | HR, RR, Skin Temperature, Activity | Post-operative, general ward | Designed for prolonged monitoring to identify trends and early signs of deterioration [31]. |
| Zio XT Patch Monitor | Continuous ECG (cECG) | Long-term cardiac monitoring (outpatient) | Unobtrusive, wire-free patch capable of recording heart rhythms for weeks [92]. |
Table 3: Contextual Strengths and Limitations of Wearable Devices [31]
| Clinical Setting | Device Strengths | Key Considerations and Limitations |
|---|---|---|
| ICU | High-frequency, multi-parameter monitoring; facilitates closed-loop systems and delirium detection via activity [92] [31]. | Can be obtrusive in complex patients; signal accuracy affected by patient movement and environment [31]. |
| Hospital Ward | Bridges "care blind spots" between ICU and standard wards; enables continuous monitoring for early warning scores [31]. | Accuracy varies with sensor placement; optical PPG sensors may overestimate SpO₂ in dark skin phototypes [31]. |
| Home | Enables decentralized monitoring and predictive analytics; cost-effective for large-scale use [83] [31]. | Requires robust connectivity; data integrity challenged by motion artifacts and user adherence [31]. |
Experimental Protocols for Clinical Validation
Validation of wearable optical sensors requires rigorous study designs and statistical methods to demonstrate reliability and accuracy.
Protocol 1: Validation of Vital Sign Accuracy in Controlled Conditions
This protocol assesses the core accuracy of wearable sensor readings against approved medical devices [83].
- Objective: To evaluate the accuracy of a low-cost wearable system in measuring HR, SpO₂, blood pressure trend, and body temperature across different body positions.
- Device Under Test: A prototype wearable built with an nRF52840 microcontroller, integrating PPG (MAX30102) and infrared (MLX90614) sensors [83].
- Reference Standards: UT-100 pulse oximeter (for HR, SpO₂), G-TECH LA800 sphygmomanometer (for BP), G-TECH THGTSC3 thermometer (for temperature) [83].
- Methodology:
- Participant Cohort: Enroll a representative sample of participants (e.g., n=10) across varying age, gender, and BMI [83].
- Testing Configurations: Evaluate sensor placement on two anatomical sites: finger (BPT-Finger) and earlobe (BPT-Earlobe) [83].
- Postural Conditions: Collect data in Rest, Sitting, and Standing positions to account for hemodynamic variations [83].
- Data Collection: Take simultaneous measurements with the wearable prototype and reference devices to enable direct comparison.
- Statistical Analysis: Perform Bland-Altman analysis to determine the limits of agreement between the wearable and reference devices. Compare results against pre-defined clinically acceptable thresholds [83].
Protocol 2: Assessing Reliability and Real-World Performance
This methodology evaluates the consistency and real-world utility of digital clinical measures over time [91].
- Objective: To determine the reliability (repeatability and reproducibility) of a digital clinical measure, such as physical activity derived from a wearable accelerometer.
- Device Under Test: A wearable chest patch device with a triaxial accelerometer (e.g., the AVIVO system used in heart failure trials) [91].
- Reference Standard: In the absence of a direct device comparator, reliability is assessed against the stability of the patient's clinical status.
- Methodology:
- Study Design: A repeated-measures design where data is collected from each participant over multiple periods (e.g., four 7-day periods) while their disease state is stable [91].
- Data Aggregation: Granular accelerometer data is processed into aggregate clinical measures, such as "average daily minutes of sedentary behavior" [91].
- Statistical Analysis:
- Intra-rater Reliability: Assesses consistency of the same device on the same patient under identical conditions over time (test-retest) [91].
- Inter-rater Reliability: Assesses consistency between different devices of the same model used on the same patient [91].
- Variance Component Modeling: Statistical models (e.g., mixed-effects models) partition total variance into intra-subject, inter-subject, and residual error components to calculate reliability coefficients [91].
The Scientist's Toolkit: Key Reagents and Materials for Validation Studies
Table 4: Essential Research Reagent Solutions for Sensor Validation
| Item Name | Function / Role in Validation | Example from Search Results |
|---|---|---|
| Photoplethysmography (PPG) Sensor | Measures blood volume changes to derive heart rate, SpO₂, and blood pressure trends. | MAX30102 sensor hub used in a low-cost wearable prototype [83]. |
| Electrocardiography (ECG) Patch | Provides continuous, clinical-grade recording of the heart's electrical activity for validation of cardiac parameters. | Zio XT and VitalPatch devices provide single-lead ECG data [92] [31]. |
| Inertial Measurement Unit (IMU) | Tracks patient activity, posture, and can be used for seismocardiography (SCG) to measure cardiac vibrations. | Accelerometer in the VitalPatch used for activity and SCG-derived parameters [92]. |
| Reference Gold-Standard Devices | Serves as the benchmark for validating the accuracy of the wearable device's measurements. | UT-100 pulse oximeter and G-TECH LA800 sphygmomanometer used as references [83]. |
| Statistical Analysis Software & Methods | Quantifies agreement, reliability, and measurement error between the wearable device and the gold standard. | Bland-Altman analysis for accuracy; Variance component models for reliability [83] [91]. |
Clinical validation is a multifaceted process demonstrating that wearable optical sensors are fit-for-purpose in specific clinical environments. The data shows that modern wearable devices can achieve clinically acceptable agreement with gold-standard equipment [83] and offer significant advantages in continuous monitoring and early detection of patient deterioration [92] [31]. However, their performance is not universal; factors like sensor placement, patient population, and clinical context significantly influence accuracy and utility [31]. Therefore, a one-size-fits-all approach is inadequate. Researchers and clinicians must rely on structured validation studies—employing appropriate protocols and statistical rigor—to select the right technology for the right setting, ultimately ensuring the safe and effective integration of wearable data into clinical research and decision-making.
Wearable sensors have become ubiquitous in both personal wellness and professional healthcare, creating a critical need to understand their varying levels of accuracy and appropriate applications. For researchers, scientists, and drug development professionals, distinguishing between consumer-grade and clinical-grade devices is essential for proper study design, data interpretation, and regulatory compliance. Consumer-grade wearables are mass-market devices designed primarily for personal wellness tracking and lifestyle enhancement, typically lacking comprehensive regulatory oversight [93]. In contrast, clinical-grade wearables are purpose-built for healthcare applications, featuring FDA clearance or approval, medically validated sensors, and integration into patient care plans for diagnostic or treatment purposes [93]. This analysis examines the accuracy spectrum between these device categories through experimental data, methodological protocols, and technical comparisons to guide evidence-based device selection for research and clinical applications.
The fundamental distinction between these device categories lies in their validation rigor and intended use cases. As explained by Vivalink's VP of marketing, "The medical grade devices typically will have gone through some kind of validation verification by some organizational body like FDA or CE or some other medical body like that, so you get a certain level of minimum standards of quality. Consumer devices, it's all over the place, it depends on which one you bought and where you bought it from" [94]. This validation gap directly impacts the reliability of data collected from these devices, with implications for research conclusions and healthcare decision-making.
Quantitative Accuracy Comparisons: Experimental Data
Optical Heart Rate Sensing Performance
Multiple validation studies have systematically evaluated the accuracy of optical heart rate sensing in wearable devices against clinical reference standards. The performance varies significantly based on device type, activity level, and population factors.
Table 1: Heart Rate Monitoring Accuracy Across Device Types and Conditions
| Device Category | Testing Condition | Mean Absolute Error (MAE) | Correlation with Reference | Reference Standard | Citation |
|---|---|---|---|---|---|
| Consumer Wearables (Withings Pulse HR) | Sitting, standing, slow walking (2.7 km/h) | ≤3.1 bpm | r ≥ 0.82 | Chest-worn ECG (Faros Bittium 180) | [84] |
| Consumer Wearables (Withings Pulse HR) | Higher intensity treadmill stages | ≤11.7 bpm | r ≤ 0.33 | Chest-worn ECG (Faros Bittium 180) | [84] |
| Multiple Consumer & Research Devices | Resting conditions | 9.5 bpm (average across devices) | Varies by device | ECG patch (Bittium Faros 180) | [13] |
| Multiple Consumer & Research Devices | Physical activity | 30% higher error than rest | Varies by device | ECG patch (Bittium Faros 180) | [13] |
| Garmin & Fitbit Devices | Peak exercise | ~7-12% outliers with widened limits of agreement | MAPE ≤3% at rest, worsened at peak exercise | ECG | [1] |
A comprehensive 2020 study published in npj Digital Medicine systematically explored heart rate accuracy across the complete range of skin tones using multiple wearable devices [13]. The research found that "wearable device, wearable device category, and activity condition all significantly correlated with HR measurement error, but changes in skin tone did not impact measurement error or wearable device accuracy" [13]. This study highlighted that absolute error during activity was, on average, 30% higher than during rest across all devices tested [13].
Non-Invasive Glucose Monitoring Emerging Technology
Research into completely non-invasive glucose monitoring represents a cutting-edge application of wearable optical sensors. A 2019 study in Clinical Biochemistry evaluated a non-invasive glucose monitor (NIGM) technology that "employs PPG sensors coupled with an optically-sensitive coating that changes its optochemical parameters in presence of specific compounds in sweat" [59]. The performance data showed strong correlation with reference standards in both anteprandial (ρ = 0.8994, p < 0.0001) and postprandial (ρ = 0.9382, p < 0.0001) glucose measurements [59]. The device precision was linear across the examined blood glucose range (50–350 mg/dL; r² = 0.9818) [59], demonstrating the potential for optical sensing technologies to expand into new biometric domains traditionally dominated by invasive clinical methods.
Table 2: Additional Biometric Monitoring Accuracy Comparisons
| Biometric Parameter | Consumer-Grade Accuracy | Clinical-Grade Accuracy | Key Limitations | Citation |
|---|---|---|---|---|
| Step Counting | Decreased agreement during treadmill phases (r = 0.48, bias = 17.3 steps/min at higher speeds) | Research-grade accelerometers show higher consistency | Miscounts during slow walking or erratic movements | [84] [2] |
| Energy Expenditure | Poor agreement during treadmill test (⎮r⎮ ≤ 0.29, ⎮bias⎮ ≥ 1.7 MET) | Indirect calorimetry as gold standard | Algorithmic generalizations based on limited inputs | [84] |
| Body Temperature | Poor agreement in all activity phases (r ≤ 0.53, ⎮bias⎮ ≥ 0.8°C) | Clinical thermometers with rigorous calibration | Placement variability and environmental factors | [84] |
Experimental Protocols: Validation Methodologies
Standardized Device Testing Frameworks
Research validating wearable device accuracy typically employs structured protocols comparing consumer and research-grade devices against clinical reference standards under controlled conditions. A 2025 study published in Frontiers in Physiology implemented a comprehensive protocol where participants "performed a structured protocol, consisting of six different activity phases (sitting, standing, and the first four stages of the classic Bruce treadmill test)" [84]. This approach allowed researchers to evaluate device performance across varying physiological states and activity intensities, with each variable "simultaneously tracked by consumer-grade and established research-grade devices" [84] to enable direct comparison.
The npj Digital Medicine study implemented a different but similarly rigorous protocol designed to "assess error and reliability in a total of six wearable devices (four consumer-grade and two research-grade models) over the course of approximately 1 h" [13]. Each study round included: "(1) seated rest to measure baseline (4 min), (2) paced deep breathing (1 min), (3) physical activity (walking to increase HR up to 50% of the recommended maximum; 5 min), (4) seated rest (washout from physical activity) (~2 min), and (5) a typing task (1 min)" [13]. This protocol was performed three times per study participant to test all devices, with an electrocardiogram (ECG) patch worn during all rounds as the reference standard [13].
Diagram 1: Experimental validation workflow for wearable device accuracy studies. MAE = Mean Absolute Error.
Statistical Analysis Methods for Device Validation
Researchers employ multiple statistical approaches to comprehensively evaluate wearable device accuracy. The 2025 comparative study used "Pearson's correlation r, Lin's concordance correlation coefficient (LCCC), Bland-Altman method, and mean absolute percentage error" [84] to assess agreement between consumer-grade and research-established devices. Similarly, a 2020 validation study in JMIR mHealth and uHealth determined "multiple statistical parameters including the mean absolute percentage error (MAPE), Lin concordance correlation coefficient (CCC), intraclass correlation coefficient, the Pearson product moment correlation coefficient, and the Bland-Altman coefficient" [58] to examine device performances. These multifaceted statistical approaches provide complementary insights into different aspects of device accuracy and reliability.
The Bland-Altman method is particularly valuable as it assesses agreement between two measurement techniques by calculating the mean difference between measurements (bias) and the limits of agreement [84] [58]. This approach helps identify systematic biases and determine how well measurements from consumer wearables align with clinical reference standards across the measurement range.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Equipment for Wearable Validation Studies
| Equipment Category | Specific Examples | Research Function | Key Features | |
|---|---|---|---|---|
| Reference Standard ECG | Bittium Faros 180, Polar H7 | Gold-standard heart rate measurement | High sampling rate (up to 1000 Hz), clinical-grade accuracy, continuous recording capability | [84] [13] [58] |
| Research-Grade Accelerometers | GENEActiv | Objective motion measurement | Tri-axial sensing, high sampling rates (up to 100 Hz), temperature and light recording | [84] |
| Metabolic Measurement Systems | Indirect calorimetry equipment | Energy expenditure validation | Measures oxygen consumption and carbon dioxide production for MET calculation | [84] |
| Clinical Temperature Systems | Tcore sensor with data logger | Core body temperature reference | Forehead placement, medical-grade accuracy, continuous monitoring | [84] |
| Structured Protocol Equipment | Bruce protocol treadmill test | Standardized activity intensity | Controlled increases in speed and elevation for reproducible exertion levels | [84] |
Technical Factors Influencing Accuracy Disparities
Sensor Technology and Signal Processing Foundations
The accuracy disparities between consumer-grade and clinical-grade wearables stem from fundamental differences in their technological implementation and signal processing approaches. Consumer wearables primarily utilize photoplethysmography (PPG) sensors that "work by illuminating the skin and quantifying changes in light absorption caused by expanding and contracting of blood vessels" [59]. This optical approach is susceptible to multiple interference factors including "motion artifacts, poor sensor-skin contact, or darker skin tones" [2], though recent comprehensive studies have found no statistically significant difference in accuracy across skin tones [13].
Clinical monitoring systems employ more robust sensing methodologies. For cardiac monitoring, "electrocardiograms (ECGs) measure the electrical activity of the heart via electrodes placed on the body" and "are vital for diagnosing arrhythmias, myocardial infarction, and other cardiac conditions" [2]. This electrical signal detection is inherently less susceptible to motion artifacts and skin tone variations compared to optical PPG systems [2] [1]. The difference in underlying sensing technology contributes significantly to the accuracy gap between consumer and clinical devices.
Diagram 2: Technical foundations of accuracy disparities between device categories.
Regulatory and Validation Frameworks
The regulatory landscape creates another fundamental distinction between device categories. Clinical-grade wearables "are built to meet the rigorous standards of medical accuracy, safety, and compliance" and are "regulated by authorities such as the FDA (U.S.), EMA (Europe), and other regional bodies" [2]. This regulatory oversight requires extensive validation studies, quality control in manufacturing, and proof of clinical efficacy before devices can be marketed for medical applications.
In contrast, consumer-grade devices operate under less stringent regulations, as they are "not FDA-approved: These devices are not classified as medical equipment" [93]. While some consumer wearables have obtained FDA clearance for specific functions, the majority of their biometric tracking features fall outside medical device regulations [2]. This regulatory difference translates directly to variations in validation rigor, with clinical-grade devices undergoing more comprehensive testing across diverse populations and use cases.
The spectrum of wearable device accuracy presents researchers and clinicians with complementary tools for different applications. Consumer-grade wearables offer advantages in "accessibility, it's something they're already familiar with" [94], making them suitable for population-level trends, general wellness monitoring, and promoting healthy behaviors. However, their limitations in accuracy, particularly during physical activity and for certain biometrics, necessitate caution when using them for clinical decision-making or rigorous research endpoints.
Clinical-grade devices provide the "high precision and accuracy" [2] essential for diagnostic applications, treatment monitoring, and clinical research outcomes. The expanding market for these devices reflects their growing importance in chronic disease management, remote patient monitoring, and digital biomarker development [22] [93]. Understanding the technical capabilities, validation methodologies, and appropriate applications across this accuracy spectrum enables researchers and drug development professionals to make evidence-based decisions when incorporating wearable technologies into their work.
The integration of wearable technology into clinical research and drug development represents a paradigm shift in how physiological data is collected. For years, wearable optical sensors, such as photoplethysmogram (PPG)-based smartwatches and fitness bands, have dominated the consumer and research markets for non-invasive monitoring. However, when compared to clinical gold standards, these optical technologies demonstrate significant limitations in accuracy, particularly during movement, at higher heart rates, and in diverse patient populations [39]. This accuracy gap becomes critically important when data from wearables is used for therapeutic decision-making or clinical endpoint validation in drug trials. Emerging technologies, particularly wearable ultrasound devices and advanced skin-like patches, now present compelling alternatives that may eventually serve as new benchmarks for wearable sensing accuracy. This review objectively compares the performance of these novel technologies against established optical sensors and clinical gold standards, providing researchers with experimental data and methodologies to inform their study designs.
Performance Showdown: Quantitative Comparison of Wearable Technologies
The table below summarizes key performance characteristics of optical sensors, wearable ultrasound, and skin-like patches, based on recent validation studies.
Table 1: Performance Comparison of Wearable Sensor Technologies
| Technology | Reported Accuracy vs. Gold Standard | Key Strengths | Key Limitations | Sample Experimental Context |
|---|---|---|---|---|
| Optical Sensors (PPG) | 84.8% - 87.4% within 10% of Holter ECG [39] | Non-invasive, high user comfort, strong consumer market adoption | Accuracy declines with intense movement and higher heart rates [39] | 24-hour free-living validation in pediatric cardiology patients (n=31-36) [39] |
| Wearable Ultrasound | Closely matches Arterial Line (gold standard) and blood pressure cuff [95] | Deep-tissue penetration (up to 10-15 cm [96]), unaffected by skin tone or ambient light [97] [98] | Higher power consumption, slower response vs. optical, complex form factor [97] [96] | Clinical tests on 117 subjects across activities like cycling, mental arithmetic, and postural changes [95] |
| Skin-Like Patches (Electronic) | Sensitivity up to 5.87 kPa-1, stable for >500 cycles [99] | Excellent conformability, can combine sensing with drug delivery [100] | Detection often limited to superficial layers [96] | In vivo experiments demonstrating wound healing and signal detection [99] |
Table 2: Comparative Sensor Characteristics for Different Environments
| Characteristic | Optical Sensors | Ultrasonic Sensors |
|---|---|---|
| Impact of Ambient Light/Dust | Highly affected; performance degrades [98] | Unaffected; robust performance [97] [98] |
| Detection Depth | Superficial (typically <1 cm) [96] | Deep tissue (several cm, up to 10-15 cm for wearable devices) [96] |
| Target Surface Sensitivity | Affected by color and material [97] | Unaffected by color or transparency [97] [98] |
| Typical Accuracy | High in controlled, restful conditions [39] | Lower than optical in ideal conditions, but superior in challenging/variable environments [97] |
Inside the Experiments: Methodologies for Validating Novel Technologies
Validation of a Wearable Ultrasound Patch for Blood Pressure Monitoring
A landmark study clinically validated a wearable ultrasound patch for continuous blood pressure monitoring, providing a robust protocol for device evaluation [95].
- Device Design: The postage stamp-sized patch consisted of a silicone elastomer embedded with an array of small piezoelectric transducers and stretchable copper electrodes. Key improvements over earlier prototypes included closer packing of transducers for wider coverage of smaller arteries and a backing layer to dampen redundant vibrations for clearer signals [95].
- Experimental Protocol: The validation involved 117 subjects across multiple settings:
- Controlled Activities: Seven participants wore the patch during activities such as cycling, arm/leg raising, mental arithmetic, meditating, eating, and consuming energy drinks.
- Postural Changes: A cohort of 85 subjects was tested during transitions from sitting to standing.
- Clinical Comparison: The patch was evaluated against an invasive arterial line (the clinical gold standard) in 21 patients in a cardiac catheterization lab and 4 post-surgery patients in the intensive care unit [95].
- Data Analysis: Measurements from the ultrasound patch were compared to those from a standard blood pressure cuff and the arterial line using agreement analysis, demonstrating comparable results and showcasing its potential as a non-invasive alternative [95].
Accuracy of Optical Heart Rate Sensors in Pediatric Populations
A 2025 study highlights the validation protocols and limitations of optical HR monitoring in a challenging demographic [39].
- Research Devices: The study compared the Corsano CardioWatch (a PPG-based wristband) and the Hexoskin smart shirt (with embedded ECG electrodes) against a Holter ECG (gold standard) [39].
- Participant Recruitment: 31 participants (mean age 13.2 years) were recruited from a pediatric cardiology outpatient clinic, comprising a population with congenital heart disease or suspected arrhythmias [39].
- Measurement Procedure: Participants were fitted with the Holter ECG, CardioWatch, and Hexoskin shirt simultaneously and instructed to follow their normal daily routine for 24 hours while refraining from water-based activities. They maintained a diary of activities and symptoms [39].
- Statistical Analysis: Accuracy was defined as the percentage of HR measurements within 10% of Holter values. Agreement was further assessed using Bland-Altman analysis, which plots the difference between two measures against their average. Subgroup analyses were conducted based on BMI, age, time of wearing, and accelerometry data to gauge the impact of movement [39].
The Researcher's Toolkit: Essential Components and Their Functions
The development and application of advanced wearable technologies rely on a suite of specialized materials and components.
Table 3: Key Research Reagent Solutions for Wearable Technology Development
| Item / Component | Function | Example Use Case |
|---|---|---|
| Piezoelectric Materials (PZT, PVDF) | Generate and receive ultrasound waves; convert mechanical energy to electrical signals and vice versa. | Core element in ultrasound transducers for blood pressure monitoring [95] [96]. |
| Polyurethane-Bioactive Glass (PU-BG) Ink | Provides a specialized matrix for 3D bioprinting; offers superior strength and controlled microstructure. | Used in creating dual-function skin patches for wound healing and sensing [99]. |
| Silicone Elastomer | Serves as a soft, stretchable substrate for device assembly, ensuring comfort and conformability on the skin. | Base material for the wearable ultrasound patch [95]. |
| Hydrogel-based Formulations | Facilitate passive or active transdermal drug delivery; can also be used as a coupling medium for ultrasound. | Matrix for drug reservoirs in wearable therapeutic patches [100]. |
| Stretchable Copper Electrodes | Provide flexible electrical interconnections within devices that must bend and move with the body. | Used in wearable ultrasound patches to connect piezoelectric transducers [95] [96]. |
Technological Workflows: From Signal to Diagnosis
The following diagrams illustrate the core operational and validation principles of these technologies.
Wearable Ultrasound Sensing & Validation Logic
Optical vs. Ultrasound Sensor Performance
Discussion and Future Directions
The experimental data and performance comparisons presented herein indicate that wearable ultrasound and multifunctional skin patches are poised to establish new benchmarks for non-invasive physiological monitoring. While optical sensors offer convenience and high user compliance, their susceptibility to motion artifacts and limitations with deeper tissues and diverse skin tones constrain their utility in rigorous clinical research and drug development [39] [97]. Wearable ultrasound directly addresses these limitations by providing gold-standard comparable data for deep-tissue parameters like blood pressure [95]. Concurrently, advanced skin patches are merging high-fidelity sensing with therapeutic functions, opening new avenues for closed-loop systems in personalized medicine [100] [99].
The future trajectory of this field points toward multimodal integration. Rather than a single technology dominating, the combination of optical, ultrasonic, and electronic sensors on a single flexible platform, augmented by machine learning for data fusion and artifact rejection, is likely to yield the most robust and informative monitoring systems. For researchers and drug developers, this evolving landscape underscores the importance of selecting validation protocols that reflect real-world conditions and patient diversity, ensuring that wearable-derived endpoints are both scientifically valid and clinically meaningful.
Conclusion
The journey of wearable optical sensors from fitness accessories to clinically validated tools is well underway, yet significant work remains. While these sensors offer unprecedented opportunities for continuous, real-world data collection in research and drug development, their accuracy is often context-dependent and can falter against clinical gold standards, especially for complex physiological metrics. Key takeaways include the critical need for rigorous, standardized validation protocols; the importance of transparent algorithms; and the emerging potential of hybrid systems that combine optical data with other sensing modalities like ultrasound. Future progress hinges on collaborative efforts between academia, industry, and regulators to enhance sensor technology, improve data analytics with AI, and firmly establish the role of these devices in the future of decentralized clinical trials and personalized medicine.
References
- 1. A guide to consumer-grade wearables in cardiovascular ... [https://www.nature.com/articles/s44325-025-00082-6]
- 2. Wearables vs Professional Medical Monitoring Systems [https://ccrps.org/clinical-research-blog/wearables-vs-professional-medical-monitoring-systems]
- 3. A Comparative Study Between ECG- and PPG-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473955/]
- 4. A Comparative Study Between ECG- and PPG-Based ... [https://www.mdpi.com/1424-8220/25/18/5745]
- 5. Algorithm Development and Validation - JMIR Cardio [https://cardio.jmir.org/2025/1/e78075]
- 6. Diagnostic accuracy of ECG smart chest patches versus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853970/]
- 7. Diagnostic accuracy of ECG smart chest patches versus PPG ... [https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-025-04582-2]
- 8. The Validation and Accuracy of Wearable Heart Rate Trackers ... [https://formative.jmir.org/2025/1/e70835]
- 9. Wearable Devices in Healthcare Beyond the One-Size-Fits All ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568095/]
- 10. Accuracy of SpO2 in Smartwatches vs Medical Devices [https://www.trainwithdaveoc.com/accuracy-of-spo2-in-smartwatches-vs-medical-devices]
- 11. Accuracy of Wearable Heart Rate Monitors [https://www.acc.org/Latest-in-Cardiology/Journal-Scans/2024/03/19/17/24/accuracy-of-wearable-heart]
- 12. The accuracy of heartbeat detection using ... [https://www.sciencedirect.com/science/article/pii/S0022073621001291]
- 13. Investigating sources of inaccuracy in wearable optical ... [https://www.nature.com/articles/s41746-020-0226-6]
- 14. Are Smart Watches Really Smart? Comparison of Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12085124/]
- 15. Scoping Review of Sensors, Trends, and Future Directions [https://pubmed.ncbi.nlm.nih.gov/40513095/?utm_source=SimplePie&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1DqqIY7i9Icf9J_BIwh0PRg_lq4ZdpZVa2NCCBt_Z5SBUCUY-a&fc=20220524054013&ff=20250613211938&v=2.18.0.post9+e462414]
- 16. Recent Advancements in Wearable Hydration-Monitoring ... [https://mhealth.jmir.org/2025/1/e60569]
- 17. Comparing the Accuracy of Different Wearable Activity ... [https://www.researchprotocols.org/2025/1/e70472]
- 18. State-of-the-art wearable sensors for cardiovascular health [https://www.nature.com/articles/s44325-025-00090-6]
- 19. VOSITONE Biometric Sensors vs Traditional Wearables [https://vositone.com/vositone-biometric-sensors-vs-wearables-test-2025.html]
- 20. Gold 2023: Highlights for primary care [https://www.nature.com/articles/s41533-023-00349-4]
- 21. HOW APPROPRIATE IS THE GOLD STANDARD FOR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3019348/]
- 22. Wearable Sensors Market 2025-2035: Technologies, ... [https://www.idtechex.com/en/research-report/wearable-sensors-market-2025/1051]
- 23. The Power of Wearable Sensors in Clinical Trials [https://sequenex.com/wearable-sensors-in-clinical-trials/]
- 24. Recent Advances in Wearable Optical Sensor Automation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8838083/]
- 25. Understanding Surface Quality Specifications [https://www.edmundoptics.com/knowledge-center/application-notes/lasers/understanding-surface-quality-specifications/?srsltid=AfmBOoo_HQz0F_IvJNxIRQMgvc3UQf8r-BBdy3uDUn_QEEo6-702zlc7]
- 26. Epidermal wearable optical sensors for sweat monitoring [https://www.nature.com/articles/s43246-024-00518-z]
- 27. 5 optical measuring principles at a glance [https://www.alicona.com/en/blog-posts/white-light-interferometer-3d-scan-measuring-microscope]
- 28. Comparing the Accuracy of Different Wearable Activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226780/]
- 29. Quantitative correlation between surface defect dimensions ... [https://opg.optica.org/ao/abstract.cfm?uri=ao-64-32-9731]
- 30. The State of Remote Patient Monitoring for Chronic ... [https://www.jmir.org/2025/1/e70422]
- 31. Wearable Devices in Healthcare Beyond the One-Size-Fits ... [https://www.mdpi.com/1424-8220/25/20/6472]
- 32. Remote Patient Monitoring in the United States: 2025 ... [https://intuitionlabs.ai/articles/remote-patient-monitoring-united-states-2025-landscape]
- 33. Wearable Smart Sensors Integration with AI and Machine ... [https://www.sciencedirect.com/science/article/pii/S2590137025001384]
- 34. Mobility recorded by wearable devices and gold standards [https://pubmed.ncbi.nlm.nih.gov/36658136/]
- 35. Mobility recorded by wearable devices and gold standards [https://pmc.ncbi.nlm.nih.gov/articles/PMC9852581/]
- 36. Connecting real-world digital mobility assessment to clinical ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0269615]
- 37. Assessing real-world gait with digital technology? Validation ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-023-01198-5]
- 38. Mobilise-D insights to estimate real-world walking speed in ... [https://www.nature.com/articles/s41598-024-51766-5]
- 39. The Validation and Accuracy of Wearable Heart Rate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483337/]
- 40. Wearable Sensors Could Reshape Obesity Treatment | News [https://www.mccormick.northwestern.edu/news/articles/2025/09/wearable-sensors-could-reshape-obesity-treatment/]
- 41. From wearable sensor data to digital biomarker development [https://www.nature.com/articles/s41746-024-01151-3]
- 42. A Review on Multisensor Data Fusion for Wearable Health ... [https://arxiv.org/html/2412.05895v1]
- 43. Multi-Sensor-Fusion Approach for a Data-Science-Oriented ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6800927/]
- 44. Comparison of Wearable and Depth-Sensing Technologies ... [https://pubmed.ncbi.nlm.nih.gov/40942931/]
- 45. How to Check the Accuracy of Your Machine Learning ... [https://www.deepchecks.com/how-to-check-the-accuracy-of-your-machine-learning-model/]
- 46. 9 Accuracy Metrics for ML Engineers to Evaluate AI Model [https://galileo.ai/blog/accuracy-metrics-ai-evaluation]
- 47. Digital Biomarkers in Clinical Drug Development [https://www.sciencedirect.com/science/article/abs/pii/B9780128031612000163]
- 48. Digital biomarkers: From innovation to implementation [https://www.simon-kucher.com/en/insights/digital-biomarkers-innovation-implementation]
- 49. Clario joins forces with Mobilise-D to advance Digital ... [https://clario.com/about/newsroom/clario-joins-forces-with-mobilise-d-to-advance-digital-mobility-outcomes-in-clinical-trials/]
- 50. A systematic review of real-world gait-related digital ... [https://www.nature.com/articles/s41746-025-01938-y]
- 51. A Roadmap to Inform Development, Validation and Approval ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7768123/]
- 52. Wearable Devices in Clinical Trials: Hype and Hypothesis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6032822/]
- 53. The Use of Wearables in Clinical Trials [https://www.quanticate.com/blog/wearables-in-clinical-trials]
- 54. Validity of a Consumer-Based Wearable to Measure Clinical ... [https://mhealth.jmir.org/2024/1/e56027]
- 55. Comparative accuracy of optical sensor-based wearable ... [https://pubmed.ncbi.nlm.nih.gov/30629956/]
- 56. Smartwatch-based ventilatory assessment for COPD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12444072/]
- 57. Remote patient monitoring strategies and wearable ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1236598/full]
- 58. Accuracy of Optical Heart Rate Sensing Technology in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7218601/]
- 59. Comparative accuracy of optical sensor-based wearable ... [https://www.sciencedirect.com/science/article/abs/pii/S0009912018310142]
- 60. How Common Noise and Error Sources Affect Optical ... [https://www.analog.com/en/resources/design-notes/how-common-noise-and-error-sources-affect-optical-biosensing.html]
- 61. Quantifying and Reducing Motion Artifacts in Wearable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5444999/]
- 62. Development of deep learning models for motion artifact ... [https://www.spiedigitallibrary.org/conference-proceedings-of-spie/13313/133130E/Development-of-deep-learning-models-for-motion-artifact-mitigation-in/10.1117/12.3039622.full]
- 63. Towards a Wearable Skin Tone Responsive Optical Sensor [https://www.mdpi.com/2673-4591/109/1/17]
- 64. Investigating sources of inaccuracy in wearable optical ... [https://www.nature.com/articles/s41746-021-00408-5]
- 65. Accuracy and Acceptability of Wearable Motion Tracking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7766923/]
- 66. Flexible and sensitive pressure sensor with enhanced ... [https://www.nature.com/articles/s41528-025-00469-6]
- 67. Optical smart wearable sensor for monitoring pulse ... [https://www.sciencedirect.com/science/article/abs/pii/S0927775725020461]
- 68. Real-World Accuracy of Wearable Activity Trackers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11399740/]
- 69. A Validation Study to Confirm the Accuracy of Wearable ... [https://www.mdpi.com/2079-9292/12/11/2536]
- 70. Unlocking Tomorrow's Health Care: Expanding the Clinical ... [https://www.sciencedirect.com/science/article/pii/S0828282X24005610]
- 71. How Battery Life and Power Efficiency Influence Medical ... [https://www.devicelab.com/blog/how-battery-life-and-power-efficiency-influence-medical-product-engineering/]
- 72. Battery data integrity and usability: Navigating datasets ... [https://www.frontiersin.org/journals/energy-research/articles/10.3389/fenrg.2023.1125175/full]
- 73. Wearable Devices: Battery Selection & Power ... [https://www.keytechinc.com/2020/02/wearable-devices-battery-selection-power-consumption-management/]
- 74. Artificial Intelligence-Based Wearable Sensing ... [https://www.mdpi.com/2079-6374/15/11/756]
- 75. Usability engineering in practice: developing an intervention ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9612925/]
- 76. A Systematic Review of Chest-Worn Sensors in Cardiac ... [https://www.mdpi.com/1424-8220/25/19/6049]
- 77. The Emergence of AI-Based Wearable Sensors for Digital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10708748/]
- 78. Wearable sensors enable personalized predictions of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8293303/]
- 79. QMSR: What You Need to Know about Global ... [https://aami.org/news/qmsr-what-you-need-to-know-about-global-harmonization-of-medical-device-regulations/]
- 80. FDA 21 CFR Part 11 Compliance: What You Need to Know ... [https://www.dotcompliance.com/blog/regulatory-compliance/fda-21-cfr-part-11-compliance-what-you-need-to-know-in-2025/]
- 81. Smartphone based blood pressure measurement [https://pmc.ncbi.nlm.nih.gov/articles/PMC8568326/]
- 82. Quality and Regulatory Predictability: Shaping USP ... [https://www.fda.gov/drugs/news-events-human-drugs/quality-and-regulatory-predictability-shaping-usp-standards-12112025]
- 83. Evaluating the Accuracy of Low-Cost Wearable Sensors for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299930/]
- 84. Laboratory comparison of consumer-grade and research ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11865084/]
- 85. Comparison of Wearable and Clinical Devices for ... [https://www.mdpi.com/1424-8220/20/23/6778]
- 86. Validation of Aerobic Capacity (VO2max) and Pulse ... [https://www.mdpi.com/1424-8220/25/1/275]
- 87. Validity of V̇O 2max estimates from the forerunner 245 ... [https://link.springer.com/article/10.1007/s00421-025-05923-x]
- 88. A guide to consumer-grade wearables in cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404996/]
- 89. Validity of smartwatch-derived estimates of lactate ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1621996/full]
- 90. Are Wearables Accurate? Apple Watch vs WHOOP ... [https://pnoe.com/blog/metabolic_health/wearable-accuracy-vo2-max-tracking-pnoe-review/]
- 91. Clinical Validation of Novel Digital Measures: Statistical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10425717/]
- 92. Wearable devices for patient monitoring in the intensive care ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11868008/]
- 93. Clinical-Grade vs. Consumer Wearables [https://fieldtexcases.com/blog/clinical-grade-wearables/]
- 94. Differentiating Consumer- and Medical-Grade Wearables [https://www.appliedclinicaltrialsonline.com/view/differentiating-consumer-and-medical-grade-wearables]
- 95. Researchers Develop Clinically Validated, Wearable ... [https://today.ucsd.edu/story/researchers-develop-clinically-validated-wearable-ultrasound-patch-for-continuous-blood-pressure-monitoring]
- 96. The Design and Application of Wearable Ultrasound Devices ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467586/]
- 97. Comparison between Ultrasonic Sensors and Optical ... [https://www.keyence.com/ss/products/sensor/sensorbasics/ultrasonic/comparison/]
- 98. Ultrasonic Sensors in Distance Measurement: Accuracy ... [https://www.bxuansensor.com/blog/ultrasonic-sensors-in-distance-measurement-accuracy-and-reliability789]
- 99. Advanced biomedical and electronic dual-function skin ... [https://www.sciencedirect.com/science/article/pii/S2452199X24002366]
- 100. Wearable patches for transdermal drug delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10326306/]