AI-Enhanced Optical Coherence Tomography: Revolutionizing Cancer Diagnostics and Surgical Oncology
This article comprehensively reviews the transformative role of Optical Coherence Tomography (OCT) in oncology, a field increasingly augmented by artificial intelligence.
AI-Enhanced Optical Coherence Tomography: Revolutionizing Cancer Diagnostics and Surgical Oncology
Abstract
This article comprehensively reviews the transformative role of Optical Coherence Tomography (OCT) in oncology, a field increasingly augmented by artificial intelligence. OCT provides non-invasive, high-resolution, real-time imaging of tissue microstructures, enabling early cancer detection, precise surgical guidance, and treatment monitoring. We explore the foundational principles of OCT and its functional extensions like angiography and elastography. The article details its methodological applications across various cancers—including skin, oral, breast, and gastrointestinal—and critically examines the integration of machine learning for automated image analysis. A thorough validation against histological standards is presented, alongside a discussion of current technical limitations and optimization strategies. This resource is tailored for researchers, scientists, and drug development professionals engaged in advancing cancer diagnostics and therapeutic interventions.
The Principles and Scope of OCT in Oncology: From Basic Science to Clinical Discovery
Low-coherence interferometry (LCI) is a non-contact optical sensing technology that serves as the foundational operating principle for Optical Coherence Tomography (OCT). In oncology, OCT leverages LCI to provide high-resolution, cross-sectional, and three-dimensional imaging of tissue microanatomy in situ and in real-time, offering tremendous value for cancer detection, diagnosis, and guided intervention [1] [2]. The technique functions by directing a beam of broadband, low-coherence light at a sample. The light reflected from sub-surface tissue structures is then combined with light that has traveled a known reference path, generating an interference pattern only when the optical path lengths of the two beams match to within the coherence length of the light source [1]. This interferometric gating enables depth-resolved measurements with micrometer-scale axial resolution, typically ranging from 1 to 15 micrometers in biological tissues [3]. This level of resolution is critical in oncology for identifying architectural disorganization, abnormal cell morphologies, and other hallmarks of early cancer that are not visible on gross examination.
Core Principles and System Architectures
The fundamental operating principle of LCI is based on the wave nature of light. In an interferometer, light is split into two paths: one illuminating the sample and the other reflecting from a reference mirror. When the beams recombine, interference fringes are detected only if the path length difference is shorter than the coherence length of the light source. This short coherence length, characteristic of broadband light sources like superluminescent diodes (SLDs) or supercontinuum lasers, provides the fine axial sectioning capability [1] [4]. By scanning the reference mirror length (in time-domain systems) or by analyzing the spectrum of the interference pattern (in frequency-domain systems), the precise depth of light scattering points within the sample can be determined, generating a depth profile known as an A-scan [1].
Key LCI System Architectures
Two main types of low-coherence interferometers are employed, differing in their implementation and performance characteristics.
Table 1: Comparison of LCI System Architectures
| Feature | Time-Domain (TD) LCI | Frequency-Domain (FD) with Swept Source |
|---|---|---|
| Light Source | Super-luminescent Diode (SLD) [1] | Fast-Sweeping Laser [1] |
| Reference Arm | Scanning Mirror [1] | Fixed Mirror [1] |
| Operating Principle | Mechanical scanning of reference mirror path length to find interference signal [1] | Fourier transformation of captured interference spectrum to obtain depth information [1] |
| Scanning Speed | Up to a few kHz [1] | 20 kHz and higher [1] |
| Key Advantages | Robust; immune to saturation; consistent sensitivity with depth [1] | High and very high scanning speeds [1] |
| Key Limitations | Lower scanning speed compared to FD [1] | Loses sensitivity with increased scanning depth [1] |
Both LCI architectures are immune to air perturbation and know the absolute distance to the sample surface upon initialization without needing to count fringes, unlike laser interferometers [1].
Visualization of LCI System Architectures
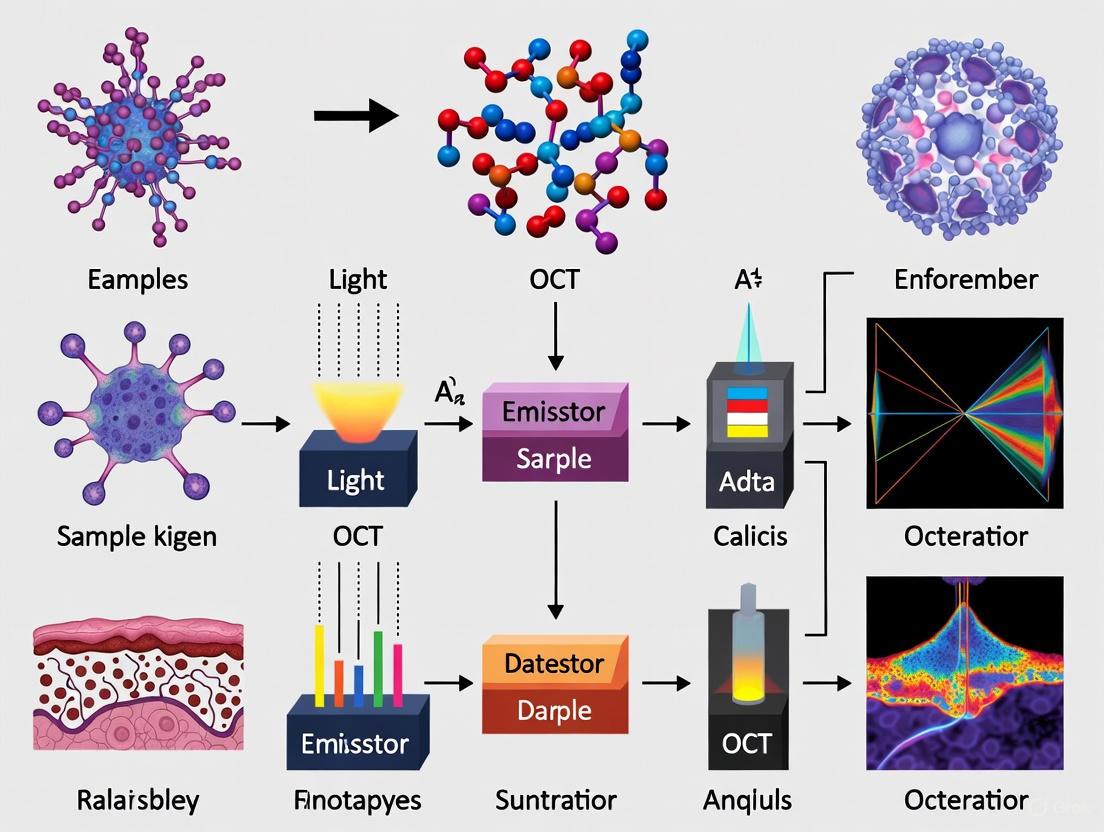
The following diagrams illustrate the core components and signal pathways for the two primary LCI system types.
Diagram 1: Time-Domain LCI System Schematic
Diagram 2: Frequency-Domain Swept-Source LCI Schematic
Quantitative Performance Metrics
The performance of an LCI system is characterized by several key parameters that directly impact its imaging capabilities and suitability for specific applications in cancer research.
Table 2: Key Performance Metrics for LCI/OCT Systems
| Performance Parameter | Typical Value or Requirement | Impact on Imaging & Application |
|---|---|---|
| Axial Resolution | 1 – 15 µm [3] | Determines the ability to resolve thin tissue layers and cellular structures; critical for identifying early dysplasia. |
| Lateral Resolution | 5 – 25 µm [3] | Dictated by the numerical aperture (NA) of the focusing optics; defines the smallest resolvable transverse feature. |
| Imaging Depth | 1 – 2 mm in most tissues [2] [5] | Limits the depth within scattering tissues (e.g., epithelial linings) that can be effectively probed. |
| Scanning Speed | Time-Domain: Few kHzFrequency-Domain: 20 kHz+ [1] | Determines acquisition time for 2D/3D datasets; high speed reduces motion artifacts in in vivo imaging. |
| Optical Path Length Difference | < 1 µm across the system [3] | Requires wavefront-optimized optics to maintain interference signal quality and measurement precision. |
| Profilometry Resolution | Can achieve nanometer-scale (e.g., 26.4 nm repeatability) [4] | Enables ultra-precise measurements of surface topography and thin film thicknesses in industrial and lab settings. |
Achieving micron-scale resolution requires meticulous control of the system's optical components. Axial resolution is inversely proportional to the bandwidth of the light source; a broader bandwidth yields finer resolution. For instance, an ultra-high-resolution retinal OCT system operating at a center wavelength of 840 nm with a 100 nm bandwidth can achieve an axial resolution of approximately 3 µm in tissue [3]. Lateral resolution, conversely, is determined by the focusing optics and is independent of the coherence length. It is governed by the same principles as in conventional microscopy, where a higher numerical aperture (NA) provides a tighter focus and better lateral resolution, albeit with a reduced depth of field [3].
Experimental Protocols for Cancer Diagnostic Applications
The application of LCI/OCT in cancer diagnostics requires standardized protocols to ensure consistent, reliable, and interpretable data. The following section details a generalized protocol for acquiring and analyzing OCT data in the context of oral cancer diagnostics, a model that can be adapted for other epithelial cancers.
Protocol: Site-Targeted OCT for Evaluation of Oral Potentially Malignant Disorders (OPMDs)
This protocol is adapted from a clinical study demonstrating high diagnostic accuracy for oral leukoplakia (OL), oral lichen planus (OLP), and oral squamous cell carcinoma (OSCC) [6].
A. Sample Preparation and Registration
- Patient Selection and Positioning: Enroll patients clinically diagnosed with OPMDs or OSCC. Position the patient comfortably to minimize motion artifacts during imaging.
- Target Site Identification: Perform a conventional clinical oral examination to identify the target lesion and specific sites for evaluation.
- Punch Scrapel-Site Registration: Gently mark the target imaging site using a punch scalpel to create a superficial, site-coded registration point. This critical step ensures precise co-registration between the OCT scan and the subsequent biopsy site, significantly enhancing diagnostic accuracy [6].
B. OCT Data Acquisition
- System Calibration: Prior to imaging, calibrate the OCT system according to manufacturer specifications. Ensure the light source output and detector sensitivity are stable.
- Probe Positioning: Align the imaging probe (e.g., a handheld scanner or endoscopic probe) perpendicular to the tissue surface at the registered target site. Maintain a consistent working distance.
- Image Acquisition Parameters:
- Scan Type: Acquire 3D volumetric scans by obtaining a series of consecutive, parallel B-scans (cross-sectional images).
- Scan Density: A typical dataset may comprise 100-120 B-scans per volume, with each B-scan consisting of 512 A-scans [6].
- Field of View: Adjust to cover the entire lesion and a margin of normal-appearing tissue (e.g., a 5x5 mm or 10x10 mm area).
- Data Storage: Save the raw interferometric data and processed images in an uncompressed format for subsequent analysis.
C. Data Analysis and Interpretation
- Blinded Review: OCT scans are analyzed by independent, blinded observers trained in OCT image interpretation.
- Qualitative Morphological Assessment: Evaluate the OCT B-scans for key pathological features, including:
- Epithelial Thickening: Loss of the normal, stratified epithelial layer uniformity.
- Disruption of Layering: Alteration or loss of the clearly defined boundary between the epithelium and the underlying lamina propria.
- Increased and Anarchic Backscattering: Changes in the optical scattering properties within the tissue, indicating nuclear pleomorphism, increased nuclear-to-cytoplasmic ratio, and disorganized tissue microarchitecture [2].
- Diagnostic Classification: Based on the assessed features, render an OCT-based diagnosis (e.g., "normal," "OPMD," or "OSCC") for the target site.
- Validation: Compare the OCT-based diagnosis with the gold standard of histopathology from the site-targeted biopsy. Calculate diagnostic performance metrics including sensitivity, specificity, and accuracy [6].
Diagram 3: Workflow for Site-Targeted OCT Diagnosis
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of LCI/OCT in a research setting, particularly for preclinical oncology studies, relies on a suite of essential reagents, materials, and equipment.
Table 3: Essential Research Toolkit for Preclinical OCT Imaging
| Category / Item | Specification / Example | Function in LCI/OCT Research |
|---|---|---|
| Broadband Light Source | Superluminescent Diode (SLD); Ti:Sapphire Laser (λ=830 nm, Δλ=45 nm) [1] [7] | Provides the low-coherence, high-power illumination required for micrometer-scale axial resolution. |
| Interferometer Core | Mach-Zehnder or Michelson configuration; Fiber-optic couplers [1] [7] | Splits light into sample and reference paths and recombines them to generate the interference signal. |
| Reference Arm Optics | Scanning mirror (TD-OCT); Fixed mirror (FD-OCT) [1] | Provides the known reference path length against which the sample arm is compared. |
| Sample Arm Optics | Galvanometer scanners; Scanning lenses (NA ~0.1, WFE <0.02λ) [3] | Directs and focuses the light onto the sample and scans the beam to form 2D/3D images. |
| Detection Subsystem | Spectrometer (SD-OCT); Dual-balanced detector (SS-/TD-OCT) [1] [7] | Measures the resulting interference pattern with high sensitivity and speed. |
| Animal Models | Mammary fat pad window models; Brain window models; Subcutaneous tumor models [5] | Provides optical access to deep tissues for longitudinal imaging of tumor development and response. |
| Image Analysis Software | Custom deep learning algorithms for segmentation (e.g., of RPE loss) [8] | Enables automated, quantitative analysis of OCT datasets (e.g., tumor volume, layer thickness). |
| Tissue Phantoms | Polydimethylsiloxane (PDMS) with embedded scatterers [7] | Used for system calibration, resolution validation, and algorithm development. |
Low-coherence interferometry provides the fundamental physical principles that enable optical coherence tomography to perform non-invasive, high-resolution, depth-resolved imaging. The precise interplay between broadband light sources, interferometric detection, and high-precision optics is paramount to achieving the micrometer-scale resolution necessary to discern the subtle morphological changes associated with early-stage neoplasia. As detailed in these application notes and protocols, the rigorous implementation of LCI, from system selection and calibration to standardized imaging and analysis procedures, is essential for generating reliable and actionable data in cancer research. The continued evolution of LCI technology, including faster scanning speeds, improved resolution, and advanced analytical algorithms, promises to further solidify its role as a powerful tool for preclinical research and its translation into clinical oncology diagnostics.
Optical coherence tomography (OCT) has emerged as a transformative imaging modality in biomedical research and clinical diagnostics, particularly in oncology. As a non-invasive technique that generates high-resolution, cross-sectional images of tissue microstructure in near-real time, OCT provides capabilities intermediate between ultrasound and confocal microscopy. The technology functions as an "optical biopsy," enabling researchers to visualize architectural morphology at resolutions of 1-15 μm with penetration depths of 1-3 mm in scattering tissues [9]. For cancer diagnostics, this capability allows for identification of malignant changes in epithelial tissues, assessment of tumor margins, and guidance for precision interventions without the need for physical tissue removal [10] [11].
The diagnostic value of OCT stems from its ability to differentiate tissue types based on their intrinsic optical properties. Cancerous tissues typically exhibit altered scattering properties, architectural disruption, and changes in layering compared to normal tissues. These differences are readily visualized in OCT images and show strong correlation with histological findings [11]. In pulmonary oncology, for instance, OCT can distinguish normal bronchial layers (epithelium, lamina propria, smooth muscle, cartilage) from tumor areas that display unevenly distributed high backscattering with loss of normal layer structure [11]. Similar differentiations have been demonstrated in skin, digestive, and other organ systems [12].
OCT system configurations have evolved to meet diverse research needs across anatomical sites. This article details the three primary configurations—benchtop, endoscopic, and needle-based probes—with specific application notes and experimental protocols tailored for cancer research applications.
Benchtop OCT Systems
System Configuration and Technical Specifications
Benchtop OCT systems represent the foundational configuration for laboratory research, providing maximum flexibility for system optimization and method development. These systems typically employ free-beam optics with galvo-scanners for beam steering and are ideal for ex vivo tissue imaging, technical validation studies, and development of novel contrast mechanisms.
The core components of a benchtop OCT system include a broadband light source, interferometer (typically Michelson), reference arm, sample arm with scanning optics, spectrometer (in spectral-domain systems), and detection electronics. Key performance parameters include axial resolution (governed by source bandwidth), lateral resolution (determined by focusing optics), imaging depth (dependent on source central wavelength), and acquisition speed [13].
Table 1: Technical Specifications of Representative Benchtop OCT Systems
| Parameter | Time-Domain OCT | Spectral-Domain OCT | Swept-Source OCT |
|---|---|---|---|
| Light Source Wavelength | 1314 nm [13] | 855 nm [13] | 1319 nm [13] |
| Bandwidth (FWHM) | 53 nm [13] | 56 nm [13] | 100 nm [13] |
| Axial Resolution | 14 μm [13] | 6 μm [13] | 7.7 μm [13] |
| Lateral Resolution | 6.6 μm [13] | 7.9 μm [13] | 12 μm [13] |
| Scanning Rate | Varies with reference arm translation | Typically higher than TD-OCT | 50-100 kHz [11] |
| Max Scan Range | Arbitrary [13] | 2.4 × 0.5 mm [13] | 8.3 × 6.7 mm [13] |
| Signal-to-Noise Ratio | Moderate | Improved compared to TD-OCT [9] | Highest among configurations [9] |
Application Notes for Cancer Research
Benchtop systems excel in applications requiring the highest possible image quality and stability. In cancer research, they are particularly valuable for:
- Tumor margin assessment: Imaging of excised tissue specimens to identify malignant regions with high resolution comparable to histology [12].
- Therapeutic monitoring: Longitudinal studies of tumor response to therapeutic interventions in animal models.
- Algorithm development: Training and validation of machine learning approaches for automated cancer detection.
- Multi-modal integration: Combination with complementary techniques like fluorescence microscopy or spectroscopy.
A significant advantage of benchtop systems is their adaptability for specialized applications. For instance, researchers have demonstrated feasible en face optical coherence microscopy using a low-cost OCT engine integrated with a commercially available inverted microscope [14]. Such configurations enable high-resolution cellular imaging valuable for fundamental cancer biology studies.
Experimental Protocol: System Performance Validation
Purpose: To quantitatively characterize benchtop OCT system performance using standardized phantoms prior to cancer imaging studies.
Materials:
- PSF phantom containing sub-resolution particles (260-nm gold nanoshells, 400-nm iron oxide particles, or 1.5-μm silica particles) [13]
- Tissue-simulating phantoms with known optical properties
- Specimen mounting apparatus
- Computer with image analysis software (e.g., MATLAB, ImageJ)
Procedure:
- System Calibration:
- Align optical components using a model eye or equivalent for retinal systems or a flat mirror for free-space systems.
- Adjust reference arm length to position zero-delay line appropriately for the sample type.
Resolution Measurement:
- Image PSF phantom at multiple locations throughout field of view.
- Identify individual particle signals and measure full-width at half-maximum (FWHM) in three dimensions.
- Calculate mean and standard deviation of axial and lateral resolutions across the imaging volume.
Signal Uniformity Assessment:
- Acquire 3D image dataset of particle phantom.
- Measure intensity of individual particles at varying depths and lateral positions.
- Generate intensity uniformity maps to identify system aberrations.
Sensitivity Roll-off:
- Image a highly reflective surface at multiple depth positions.
- Plot signal intensity versus depth to characterize sensitivity decrease with depth.
Documentation:
- Record all measured parameters for system qualification.
- Compare with manufacturer specifications and establish baseline performance metrics.
Quality Control: Repeat validation quarterly or following any system modification. Typical performance thresholds: <10% variation in resolution across field of view, <3 dB signal variation over central 70% of imaging depth.
Endoscopic OCT Configurations
System Design and Technical Considerations
Endoscopic OCT (E-OCT) enables access to internal organs and hollow anatomical structures for cancer detection in locations such as the gastrointestinal tract, respiratory system, and genitourinary tract. E-OCT probes can be broadly classified as side-viewing or forward-viewing designs, with scanning implemented via proximal or distal mechanisms [10].
Side-viewing probes typically employ a rotating deflector (prism or mirror) to generate circumferential scans ideal for surveying luminal organs. These can be implemented via proximal rotation of the entire fiber assembly or using distal micro-motors. Forward-viewing probes are better suited for visualizing structures ahead of the probe, such as at airway branches or during surgical guidance, and often use MEMS mirrors or fiber scanning mechanisms [15] [10].
Table 2: Comparison of Endoscopic OCT Probe Configurations
| Parameter | Proximal-Scanning Side-Viewing | Distal-Scanning Side-Viewing | Forward-Viewing |
|---|---|---|---|
| Minimum Probe Diameter | ~0.5 mm [10] | ~1.5 mm [10] | Typically 2-3 mm [15] |
| Rigid Length | ~1.0 cm [10] | ~2.0 cm [10] | Varies with design |
| Maximum Speed | ~200 rps [10] | ~4000 rps [10] | Limited by scanning mechanism |
| Imaging Area | Large (with pullback) [10] | Large (with pullback) [10] | Limited field of view [15] |
| Fiber Stress-induced Distortion | Moderate [10] | Less [10] | Minimal |
| Cost | Low (often disposable) [10] | High (with micromotor) [10] | Moderate to high |
Distal-end optics for E-OCT typically incorporate a single-mode fiber, glass rod spacer, GRIN lens, and optional beam deflector. The GRIN lens parameters and spacer length are tuned to achieve desired lateral resolution and working distance within strict size constraints [10]. Recent advances include the use of double-clad fibers that enable simultaneous OCT and fluorescence imaging [15].
Application Notes for Cancer Research
Endoscopic OCT has demonstrated particular value in oncology for:
- Early cancer detection in high-risk epithelia: Identification of dysplasia and early carcinoma in Barrett's esophagus, inflammatory bowel disease, and bronchial pre-neoplasia [10] [11].
- Guidance for precision biopsy: Targeting suspicious regions for tissue sampling, significantly improving diagnostic yield over random biopsy [9] [11].
- Therapeutic monitoring: Assessing response to endoscopic therapies such as ablation or resection.
- Intraoperative margin assessment: Defining tumor boundaries during endoscopic resection procedures.
In pulmonary oncology, Endobronchial OCT (EB-OCT) has shown capability to differentiate normal airway architecture from tumor regions based on disruption of layered structure and increased, heterogeneous backscattering [11]. The technique provides high-resolution (10-20 μm) images that correlate well with histology, enabling real-time assessment of bronchial lesions without tissue removal.
Experimental Protocol: Endobronchial OCT for Lung Cancer Detection
Purpose: To obtain high-quality OCT images of bronchial mucosa and subepithelial structures for detection of neoplastic changes.
Materials:
- OCT-compatible bronchoscope (working channel ≥1.2 mm)
- EB-OCT system with probe (typical parameters: wavelength 1255-1355 nm, scan rate ≥50 kHz, detection depth 0.3-1.5 mm) [11]
- Navigation system (e.g., electromagnetic or virtual bronchoscopy)
- Sterile sheath for OCT probe
Procedure:
- Pre-procedure Planning:
- Acquire HRCT within 24 hours prior to procedure.
- Reconstruct 3D bronchial tree and plan navigation path to target lesion.
- Identify optimal registration points for navigation system.
Patient Preparation:
- Administer local anesthesia via nebulized 2% lidocaine.
- Consider conscious sedation based on patient factors and procedure duration.
Bronchoscopic Navigation:
- Insert bronchoscope transnasally and advance to tertiary bronchi of target lobe.
- Register real-time position with pre-procedure 3D model using navigation system.
OCT Image Acquisition:
- Insert OCT probe through working channel until it reaches target bronchus.
- Instruct patient to hold breath at full inspiration to minimize motion artifact.
- Initiate automated pullback with rotational scanning.
- Acquire multiple datasets (3-5 repetitions) to ensure adequate quality.
- Maintain gentle contact between probe and airway wall for stability.
Image Analysis:
- Measure lumen diameter, lumen area, and airway wall thickness.
- Assess architectural features: epithelial layer integrity, submucosal gland patterns, cartilage structure.
- Identify abnormalities: disruption of layered structure, increased heterogeneous backscattering, altered glandular architecture.
Interpretation Notes: Normal bronchi demonstrate distinct, continuous layers: epithelium, lamina propria, smooth muscle, and cartilage. Tumors typically show loss of layered structure with uneven backscattering and invasion beyond the cartilage layer [11].
Diagram 1: EB-OCT Procedural Workflow for Lung Cancer Detection
Needle-Based OCT Probes
System Design and Technical Considerations
Needle-based OCT probes represent the smallest form factor, enabling integration with biopsy needles for interstitial imaging during percutaneous procedures. These systems typically range from 20-30 gauge in diameter and employ various scanning mechanisms, including rotating cores, distal micromotors, or manually scanned single-fiber designs.
A significant innovation in this category is the single-fiber OCT (sfOCT) system, which eliminates distal optics and scanning components entirely. In this configuration, a bare optical fiber serves as both the sample and reference arm in a common-path interferometer, with the fiber tip itself providing the reference reflection [12]. Lateral scanning is achieved through manual movement of the fiber across the tissue surface, with sophisticated algorithms correcting for motion artifacts.
Table 3: Needle-Based OCT Probe Specifications
| Parameter | Rotating Needle Probe | MEMS-Based Needle Probe | Single-Fiber OCT Probe |
|---|---|---|---|
| Typical Diameter | 27-30 gauge | 20-25 gauge | 20 gauge [12] |
| Scanning Mechanism | Rotating fiber core with proximal motor | Distal MEMS mirror | Manual scanning with motion correction [12] |
| Lateral Resolution | 15-30 μm | 10-20 μm | Not specified |
| Field of View | Circumferential (360°) | Sector or circumferential | Unlimited manual scanning range [12] |
| Key Advantages | Comprehensive circumferential imaging | High scanning speed, programmable patterns | Extreme miniaturization, cost-effectiveness [12] |
| Limitations | Potential non-uniform rotation distortion | Complex fabrication, higher cost | Requires motion tracking algorithms [12] |
The manual scanning approach in sfOCT systems presents unique challenges in image reconstruction due to non-uniform probe velocity. This limitation is addressed through speckle decorrelation analysis, which quantifies lateral displacement between adjacent A-scans by calculating cross-correlation coefficients and uses this information to resample data at regular spatial intervals [12].
Application Notes for Cancer Research
Needle-based OCT probes offer unique capabilities for cancer research applications:
- Core biopsy guidance: Real-time assessment of tissue at the needle tip prior to acquisition, ensuring sampling of viable tumor regions.
- Margin assessment in confined spaces: Imaging of tumor boundaries in anatomically constrained locations where conventional probes cannot access.
- Intraoperative delineation of tumor margins: Precise identification of cancer boundaries during minimally invasive procedures.
In dermatologic oncology, sfOCT has demonstrated capability to identify normal skin morphology and differentiate features of basal cell carcinoma and squamous cell carcinoma with qualitative correlation to histopathology [12]. The system's ability to quantify disruption of the dermo-epidermal junction pattern provides an objective biomarker for tumor presence.
Experimental Protocol: Single-Fiber OCT for Skin Cancer Margin Delineation
Purpose: To delineate non-melanoma skin cancer margins using manually scanned sfOCT for guidance of Mohs micrographic surgery.
Materials:
- sfOCT system with 1060 nm swept-source engine [12]
- Single-fiber probe with 20-gauge needle integration [12]
- GPU-accelerated processing workstation
- Sterile probe sheath or disinfectant
Procedure:
- System Setup:
- Calibrate common-path interferometer using a reference surface at typical working distance.
- Configure real-time processing parameters: speckle window size, correlation threshold, resampling interval.
Probe Motion Training:
- Instruct operator on proper scanning technique: consistent speed, maintained contact, perpendicular orientation.
- Practice on tissue phantoms to achieve uniform scanning velocity.
Image Acquisition:
- Position probe at region of interest with gentle tissue contact.
- Manually scan across lesion in linear passes with slight overlap.
- Maintain consistent pressure using integrated rubber cap to minimize tissue deformation.
- Acquire data from entire lesion and apparent margins.
Real-time Processing:
- Compute cross-correlation between sequential A-scans: ρᵢ = (Sᵢ - ⟨Sᵢ⟩)(Sᵢ₊₁ - ⟨Sᵢ₊₁⟩)/(σᵢσᵢ₊₁)
- Calculate lateral displacement: δxᵢ = w₀√(ln(1/ρᵢ))
- Determine accumulated lateral displacement: δxₙ = Σδxᵢ
- Resample A-scans when δxₙ reaches predetermined spatial interval (e.g., 10 μm)
Image Interpretation:
- Identify normal skin architecture: stratified epidermis, intact dermo-epidermal junction, homogeneous dermal reflectivity.
- Recognize tumor features: disrupted layering, dark nodular structures (BCC), keratin pearls (SCC), increased heterogeneous scattering.
- Mark tumor boundaries on skin surface based on OCT findings.
Validation: Compare OCT-determined margins with histologic findings from Mohs surgery stages. Calculate sensitivity, specificity, and concordance rates.
Diagram 2: Single-Fiber OCT Image Processing Workflow
Research Reagent Solutions
Table 4: Essential Research Reagents for OCT Cancer Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| PSF Phantoms (260-nm gold nanoshells, 400-nm iron oxide particles, 1.5-μm silica particles) [13] | System resolution quantification | Enables standardized performance comparison across systems and laboratories |
| Tissue-Simulating Phantoms | Image quality assessment | Should mimic optical properties of target tissues; useful for validation studies |
| Double-Clad Fiber [15] | Simultaneous OCT and fluorescence imaging | Enables multi-modal imaging for enhanced molecular specificity |
| GRIN Lens Assemblies [10] | Miniaturized focusing optics | Critical for endoscopic and needle-based probe designs |
| Common-Path Interferometer Components [12] | Simplified system architecture | Eliminates need for separate reference arm; ideal for miniaturized systems |
| Speckle Decorrelation Algorithms [15] [12] | Motion tracking and correction | Essential for manual scanning approaches; enables distortion-free imaging |
The strategic selection of OCT system configuration is paramount for successful cancer research applications across diverse anatomical sites. Benchtop systems provide unparalleled performance for fundamental studies and algorithm development, endoscopic configurations enable access to internal organs for early detection and guidance, and needle-based probes offer minimally invasive options for interstitial imaging and biopsy guidance.
Future directions in OCT technology development include further miniaturization of probe architectures, increased imaging speeds for comprehensive volumetric assessment, integration with complementary modalities such as fluorescence and spectroscopy, and implementation of artificial intelligence for real-time image interpretation. These advances will continue to enhance OCT's role as a powerful tool in the cancer researcher's arsenal, providing non-destructive, high-resolution imaging capabilities that bridge the gap between macroscopic clinical imaging and microscopic histology.
As OCT technology evolves, standardization of performance assessment using validated phantoms and protocols will be essential for comparing results across studies and translating findings into clinical practice. The configurations and methodologies detailed herein provide a foundation for rigorous cancer research applications across the spectrum of anatomical sites and cancer types.
Optical Coherence Tomography (OCT) has emerged as a transformative medical imaging technology in oncological research and diagnostic applications. Initially developed for ophthalmology, OCT is a non-invasive, non-contact imaging technique based on low-coherence interferometry to create high-resolution, three-dimensional volumetric images of biological tissues in real-time [16]. The fundamental principle operates on a Michelson-type interferometer employing a low-coherence light source where the light beam splits into two paths—directed toward the sample and a reference mirror. The recombination of reflected beams generates an interference pattern only when optical path lengths match within the short coherence length of the source, enabling depth-resolved imaging at micrometer-scale resolution [16]. This capability provides significant advantages over other imaging modalities; ultrasound typically offers resolution around 200 μm, while MRI delivers excellent soft-tissue contrast but with lower spatial resolution. Furthermore, OCT does not require ionizing radiation, making it safer for repeated use [16].
In oncology, OCT's value stems from its ability to visualize tissue microstructures for early cancer detection, biopsy guidance, and treatment monitoring. The technology has demonstrated particular promise in detecting epithelial cancers such as skin, oral, and gastrointestinal cancers by allowing real-time imaging of superficial layers through non-invasive procedures [17]. However, traditional OCT primarily provides structural information, which sometimes results in low contrast between morphological features in cancerous versus benign breast tissue, for example [18]. This limitation has driven the development of advanced functional extensions that leverage specific contrast mechanisms to interpret microstructural, viability, and angiographic signatures of tumors. These innovations include polarization-sensitive OCT (PS-OCT) for detecting collagen organization through birefringence, dynamic OCT (d-OCT) for visualizing tissue viability via intrinsic motility, and OCT angiography (OCTA) for mapping microvascular networks [19] [18] [20]. The integration of these contrast mechanisms with artificial intelligence is further advancing OCT's capabilities, enabling automated analysis of complex patterns and biomarkers imperceptible to the human eye [17].
Quantitative Biomarkers of Cancer Angiogenesis
The formation of new blood vessels, or angiogenesis, represents a critical hallmark of cancer progression, enabling tumors to exceed a few millimeters in diameter by supplying essential oxygen and nutrients [21]. In breast cancer, the microvessels in malignant tumors differ structurally from those in normal tissues or benign tumors. Malignant tumors typically exhibit leaky, tortuous, irregular microvessels often oriented toward the lesion center, triggered by hypoxic conditions that stimulate vascular endothelial growth factor (VEGF) secretion [22] [21]. In contrast, benign tumors generally contain regularly shaped, non-tortuous vessels circumferentially oriented around the tumor [22]. These distinct vascular patterns provide a foundation for quantitative biomarkers that can objectively differentiate malignant from benign lesions.
Recent research has established novel orientation-based quantitative biomarkers derived from contrast-free ultrasound microvasculature imaging, though these principles apply similarly to OCT angiography. These biomarkers computationally analyze microvessel orientation patterns in both polar and Cartesian coordinates, derived from histogram, gradient angle, angle of penetration, and penetration factor metrics [22]. Table 1 summarizes key quantitative biomarkers for angiogenesis assessment.
Table 1: Quantitative Biomarkers for Tumor Angiogenesis Assessment
| Biomarker Category | Specific Biomarker | Description | Malignant Signature | Performance Metrics |
|---|---|---|---|---|
| Vessel Orientation | Angle-Based Penetration Density (APD) | Ratio of penetrating microvessels' area to total microvessel area | Increased penetrating vessels | AUC: 0.91 (95% CI: 0.86, 0.97) [22] |
| Vessel Orientation | Penetration to Circumferential Density (PCD) | Density ratio between penetrating and circumferential vessels | Higher penetration-to-circumferential ratio | - |
| Spatial Distribution | Polar Coordinate Histogram Features | Vessel distribution patterns in polar coordinates | Irregular, radial orientation | - |
| Spatial Distribution | Polar Gradient Angle | Directional patterns of microvessels | Gradient toward lesion center | - |
| Clinical Integration | BI-RADS + Orientation Biomarkers | Combined assessment with standard classification | - | AUC: 0.97 (95% CI: 0.91, 1.00) [22] |
The clinical performance of these orientation-based biomarkers is substantial, with an area under the receiver operating characteristic curve (AUC) of 0.91 (95% CI: 0.86, 0.97) for differentiating malignant from benign breast masses. When combined with the standard Breast Imaging Reporting and Data System (BI-RADS) score, the AUC improves to 0.97 (95% CI: 0.91, 1.00), demonstrating the significant complementary value of quantitative angiographic assessment [22].
The biological mechanisms driving these distinct vascular patterns involve complex interactions within the tumor microenvironment. Hypoxia in solid tumors triggers hypoxia-inducible factor 1 (HIF-1) activation, stimulating cancer cells to secrete VEGFA and other pro-angiogenic factors that promote endothelial cell proliferation, migration, and new vessel formation [21]. In primary breast cancers, the median partial pressure of oxygen is significantly lower (10 mm Hg) compared to normal breast tissue (65 mm Hg), creating strong drivers for aberrant angiogenesis [21]. The newly formed microvasculature in malignant tumors becomes disorganized and leaky, further exacerbating hypoxia and creating a vicious cycle that promotes tumor progression and metastasis.
Experimental Protocols for Contrast Mechanism Analysis
Protocol 1: Microvascular Imaging and Orientation Analysis
This protocol details the methodology for quantifying microvessel orientation biomarkers using high-definition microvasculature imaging, adapted for OCT angiography applications.
Research Reagent Solutions:
- Contrast-Free Imaging Solution: Physiological saline or optical clearing agents (e.g., glycerol solutions) for maintaining tissue hydration and optical properties during ex vivo imaging [18]
- Tissue Stabilization Matrix: Agarose or similar substrates for specimen immobilization during extended image acquisition
- Histology Validation Kit: 10% neutral-buffered formalin for fixation, paraffin for embedding, hematoxylin and eosin (H&E) for staining [18]
Procedure:
- Sample Preparation:
- For ex vivo specimens, excise fresh tissue samples (approximately 30 × 20 × 5 mm³) containing both malignant and benign regions confirmed by pathological assessment [18].
- Hydrate specimens with saline and compress against an imaging window to minimize surface topology variation and avoid bulk tissue motion during acquisition.
Image Acquisition:
- Acquire wide-field OCT images by stitching multiple partially overlapping sub-volumes in a grid pattern to construct a mosaiced image (e.g., ∼28 × 28 × 3.5 mm³) [18].
- For localized microvasculature assessment, select a region of interest (3 × 3 mm²) for high-resolution OCTA imaging with optimized spatial sampling rates.
Vessel Segmentation:
- Apply connected component analysis to identify microvessel segments, considering horizontal, vertical, and diagonal adjacency in 8 possible directions [22].
- Perform skeletonization using morphological thinning algorithms to achieve single-pixel-wide vessel representations while preserving structure.
Orientation Quantification:
- Categorize vessels as small (skeleton length < 50 pixels) or large, with only large vessels used for orientation classification due to directional measurement reliability [22].
- For Cartesian coordinate features:
- Calculate Angle-Based Penetration Density (APD) by determining the angle between the tangent to the ROI boundary and the microvessel direction, classifying vessels as penetrating (angle between 45°-135°) or circumferential [22].
- Compute Penetration to Circumferential Density (PCD) by identifying vessels approaching the central ROI (scaled to 70% of original size) and calculating penetration length as the absolute difference between distances from vessel skeleton start and end points to the ROI center [22].
- For polar coordinate features:
- Calculate histogram distribution of vessel orientations relative to lesion centroid.
- Compute gradient angles to determine directional patterns.
Validation:
- Process imaged specimens for standard histology (fixation, embedding, sectioning, H&E staining) [18].
- Perform co-registration between OCTA images and histology slides with pathologist annotation of tissue types for validation.
Figure 1: Microvessel Orientation Analysis Workflow
Protocol 2: Dynamic OCT for Tissue Viability Assessment
This protocol describes the acquisition and processing of 3-D dynamic OCT (d-OCT) images to assess tissue viability through intrinsic motility contrast.
Research Reagent Solutions:
- Tissue Viability Maintenance Solution: Oxygenated physiological buffer (e.g., Krebs-Ringer solution) for ex vivo specimen maintenance during motility imaging [18]
- Motion Stabilization Platform: Vibration-damping optical tables with temperature control to minimize external vibrations
- Multimodal Validation Agents: Fluorescent viability markers (e.g., calcein-AM) for correlative assessment of tissue activity
Procedure:
- System Configuration:
- Utilize a spectral-domain OCT (SD-OCT) system with central wavelength of 1300 nm and 200 nm bandwidth for optimal penetration and resolution [18].
- Employ an objective lens providing full-width-half-maximum (FWHM) lateral resolution of approximately 7.2 μm, balancing resolution with acquisition speed and depth of field.
Acquisition Parameter Optimization:
- Determine optimal trade-off between spatial resolution, temporal resolution, and acquisition time through pilot acquisitions.
- For 3-D d-OCT, acquire multiple repeated B-scans at each spatial location (e.g., 5-10 repetitions) to capture temporal signal variations [18].
Signal Processing:
- Apply Fourier power spectral analysis to transpose time-series intensity variance data into frequency domain [18].
- Implement multiple visualization methods:
- RGB Method: Sum spectral power within three frequency ranges at each pixel, with relative power determining corresponding channel intensity in red-green-blue image [18].
- HSV Method: Map statistical metrics from frequency distribution to channels in hue-saturation-value image [18].
- Phase Variance Imaging: Utilize phase-sensitive detection for higher sensitivity to tissue motion [18].
Contrast Quantification:
- Calculate contrast-to-noise ratio between malignant and benign tissue regions.
- Compare d-OCT contrast with conventional OCT intensity images.
Validation:
- Acquire consecutive d-OCT and compression optical coherence elastography (OCE) images to provide complementary contrast mechanisms [18].
- Process tissue for co-registered histology with pathologist annotation of tissue types.
Table 2 summarizes the acquisition parameters for dynamic OCT imaging.
Table 2: Dynamic OCT Acquisition Parameters for Tissue Viability
| Parameter | Pilot Acquisition | Optimized 3-D Acquisition | Description |
|---|---|---|---|
| Lateral Range | 3 mm | 3 × 3 mm² | Field of view for dynamic analysis |
| Image Size | 1000 × 1024 pixels | Variable based on sampling | Spatial pixels (x × z) |
| Pixel Size | 3 × 3.4 μm² | 10 × 10 × 3.5 μm³ | Voxel dimensions |
| Temporal Sampling | 2000 B-scans at same location | 5-10 repetitions per location | Number of repeated measurements |
| Central Wavelength | 1300 nm | 1300 nm | OCT system central wavelength |
| Bandwidth | 200 nm | 200 nm | 3-dB bandwidth of source |
Protocol 3: Polarization-Sensitive OCT for Collagen Mapping
This protocol outlines the methodology for enhanced polarization contrast imaging using PS-OCT to visualize collagen organization through birefringence signatures.
Research Reagent Solutions:
- Polarization Calibration Standards: Quarter-wave plates and polarizers for system calibration
- Collagen Reference Samples: Rat tail tendon or similar highly birefringent reference materials for validation
- Optical Clearing Agents: Glycerol, fructose solutions, or other clearing agents to reduce scattering for improved polarization maintenance
Procedure:
- System Calibration:
- Configure PS-OCT system with polarization diversity detection.
- Calibrate using known polarization standards to ensure accurate Mueller matrix measurement.
Data Acquisition:
- Acquire depth-resolved polarization images using multiple input polarization states.
- Measure full Mueller matrix elements for each voxel in the imaging volume.
Polarization Parameter Calculation:
Contrast Enhancement:
- Apply depolarization mechanism to enhance polarization contrast of multiple parameters simultaneously.
- Integrate combined non-depolarizing images into combined depolarizing image to form enhanced contrast visualization.
Validation:
- Compare PS-OCT results with histology stained for collagen (e.g., Masson's trichrome, picrosirius red).
- Perform correlation analysis between birefringence patterns and collagen density/organization.
Integrated Diagnostic Framework and Clinical Translation
The integration of multiple contrast mechanisms within a unified diagnostic framework significantly enhances the capability for cancer detection and characterization. Figure 2 illustrates how microstructural, viability, and angiographic signatures can be combined within a comprehensive diagnostic workflow for breast cancer assessment.
Figure 2: Multi-Contrast Diagnostic Integration Workflow
The clinical translation of these advanced contrast mechanisms is actively progressing, particularly in oncology applications. OCT has demonstrated promising performance in intraoperative margin assessment during breast-conserving surgery, where it can potentially reduce the 20-30% re-excision rate currently required due to positive margins [18]. The integration of artificial intelligence with OCT imaging further enhances diagnostic capabilities by automating complex image analysis and extracting subtle patterns imperceptible to human observers [17]. AI-driven OCT systems can classify tissue as normal versus cancerous with high accuracy, enabling real-time decision support during surgical procedures [17].
Future perspectives for advancing contrast mechanisms in cancer imaging include the development of nanoparticle-enhanced OCT approaches. Gold and superparamagnetic iron oxide nanoparticles have demonstrated potential for increasing OCT's diagnostic accuracy through enhanced optical scattering and targeted biomarker detection [16]. Additionally, the combination of OCT with other imaging modalities, such as photoacoustic imaging (PAI), creates complementary contrast mechanisms that provide comprehensive assessment of tumor hemodynamics, metabolic microstructure, and vascular networks [23]. These technological advances, coupled with standardized protocols for quantitative biomarker assessment, position OCT as an increasingly powerful tool for cancer detection, characterization, and treatment monitoring in both research and clinical settings.
Optical Coherence Tomography (OCT) has transformed from a high-resolution structural imaging technique into a powerful multimodal platform capable of revealing tissue physiology, biomechanics, and molecular composition. This evolution is particularly significant for cancer diagnostics research, where functional OCT extensions provide non-invasive means to visualize tumor microenvironment, vascular abnormalities, and tissue stiffness alterations. The integration of elastography, angiography, and spectroscopic extensions has positioned OCT as an invaluable tool for researchers and drug development professionals seeking to understand tumor mechanics, neovascularization, and metabolic changes at cellular resolution. These functional modalities now enable real-time assessment of tissue properties that serve as critical biomarkers in oncology, offering insights that extend far beyond conventional histological analysis.
Functional OCT Techniques: Principles and Biomedical Applications
Functional OCT technologies extract complementary information from biological tissues by analyzing additional properties of light beyond simple backscattering. These advancements have significantly expanded OCT's utility in cancer research, particularly for characterizing tumor microenvironment and treatment response.
Table 1: Functional OCT Modalities and Their Applications in Cancer Research
| Technique | Measured Parameters | Key Applications in Oncology | Resolution | Penetration Depth |
|---|---|---|---|---|
| OCT Angiography (OCTA) | Blood flow, microvascular density, vessel morphology | Tumor angiogenesis, therapy monitoring, vascular abnormalities [24] [25] | 1-15 μm [25] | 1-2 mm [25] [26] |
| Optical Coherence Elastography (OCE) | Tissue stiffness, Young's modulus, biomechanical properties | Tumor margin detection, tissue fibrosis, treatment response [27] [28] | Micrometer-level [25] | 1-2 mm [26] |
| Polarization-Sensitive OCT (PS-OCT) | Birefringence, polarization properties | Collagen organization, fibrous cap characterization [29] | 10-15 μm axial [29] | 1-3 mm [29] |
| Spectroscopic OCT | Spectral attenuation, wavelength-dependent scattering | Tissue oxygenation, metabolic changes [24] | N/A | N/A |
| Visible Light OCT | Optical attenuation, oximetry | Retinal oximetry, metabolic imaging [24] | Higher than standard OCT [24] | Reduced vs. infrared OCT [24] |
| Optoretinography (ORG) | Stimulus-evoked intrinsic optical signals | Photoreceptor function, retinal degeneration [24] | Cellular level [24] | N/A |
OCT Angiography (OCTA)
OCTA visualizes microvascular networks by detecting blood flow-induced signal variations in sequential OCT scans. Unlike fluorescence angiography requiring exogenous contrast agents, OCTA provides label-free, depth-resolved vascular imaging with capillary-level resolution [25]. This capability is particularly valuable for monitoring tumor angiogenesis—a hallmark of cancer progression characterized by abnormal vessel morphology, increased density, and altered perfusion [24]. OCTA algorithms primarily utilize Doppler variance and amplitude decorrelation to generate high-resolution vasculature maps, enabling quantification of vascular biomarkers including vessel density, perfusion, and fractal dimension [25].
In oncological applications, OCTA enables longitudinal monitoring of anti-angiogenic therapy response without repeated biopsies. Research demonstrates its efficacy in detecting microvascular changes preceding tumor structural alterations, providing an early indicator of treatment efficacy [30]. The technology's high spatial resolution (1-15μm) facilitates visualization of pathological vessel patterns characteristic of malignancies, including tortuosity, dilation, and chaotic architecture [25].
Optical Coherence Elastography (OCE)
OCE maps tissue mechanical properties by measuring deformation responses to applied force, providing insights into tissue microstructure and composition. Malignant transformation is frequently accompanied by extracellular matrix remodeling and changes in tissue stiffness, which OCE detects with micrometer-scale spatial resolution and nanometer-scale displacement sensitivity [25] [28].
Wave-based OCE techniques measure shear wave propagation speed, which correlates with tissue Young's modulus—a critical parameter distinguishing pathological from healthy tissues [28]. Recent studies demonstrate OCE's capability to detect stiffness alterations in corneal tissue resulting from prolonged intraocular pressure elevation, highlighting its sensitivity to biomechanical changes in disease states [28]. In oncology, OCE shows promise for intraoperative tumor margin assessment, potentially reducing positive margin rates in cancer surgery. The technology's ability to provide real-time, non-contact stiffness measurements makes it particularly suitable for guiding surgical interventions and monitoring tissue remodeling during therapy [27].
Polarization-Sensitive and Spectroscopic OCT Extensions
Polarization-sensitive OCT (PS-OCT) enhances tissue contrast by detecting birefringence properties related to organized structural proteins like collagen. In coronary applications, PS-OCT has identified birefringence signals corresponding to cholesterol crystals and collagen-rich regions within plaques [29]. This capability is transferable to oncology, where collagen remodeling in tumor microenvironment serves as a significant diagnostic marker.
Spectroscopic OCT analyzes wavelength-dependent scattering properties to infer tissue composition, while visible light OCT enables retinal oximetry by measuring spectral absorption characteristics of oxygenated and deoxygenated hemoglobin [24]. These approaches provide access to functional metabolic information, potentially revealing hypoxia—a key feature of aggressive tumors associated with treatment resistance.
Experimental Protocols and Methodologies
Multimodal OCT for Liver Regeneration Assessment
The protocol below, adapted from liver regeneration studies, demonstrates how combined OCT modalities can comprehensively characterize tissue remodeling relevant to cancer research [27].
Objective: To quantitatively monitor microstructural, microcirculatory, and biomechanical alterations during tissue regeneration and repair processes.
Materials:
- Spectral-domain OCT system (central wavelength: 1.3 µm, axial resolution: ~15 µm, lateral resolution: ~20 µm in air)
- Animal model (e.g., Wistar rats for partial hepatectomy study)
- Custom software for attenuation coefficient calculation and OCTA processing
- Histological processing equipment for validation
Procedure:
- System Calibration: Verify axial (15 µm) and lateral (20 µm) resolution using resolution target. Set laser power to approximately 2 mW at tissue surface.
- Data Acquisition:
- Acquire 3D data (4 × 4 × 1.5 mm) with acquisition time of 26 seconds at 20,000 A-scans/second
- For OCTA: Capture sequential B-scans at same position for decorrelation analysis
- For attenuation mapping: Ensure sufficient signal-to-noise ratio throughout depth
- For OCE: Implement phase-stabilized acquisition for nanoscale displacement detection
- OCTA Processing:
- Apply displacement compensation algorithm to correct for breathing and cardiac motion artifacts [27]
- Compute intensity decorrelation or phase variance between consecutive B-scans
- Generate 2D en-face angiograms using maximum intensity projection
- Quantify vessel density and diameter distribution
- Attenuation Coefficient Calculation:
- Apply depth-resolved algorithm to calculate attenuation coefficient from ~50 µm to ~600 µm below tissue surface [27]
- Generate 2D color-coded maps of attenuation distribution
- Calculate mean attenuation values for entire tissue region
- OCE Analysis:
- Induce mechanical waves using controlled excitation (e.g., air-pulse, acoustic radiation force)
- Track wave propagation using phase-sensitive OCT detection
- Calculate wave velocity through linear regression of space-time maps
- Derive Young's modulus using appropriate mechanical models
- Validation: Correlate OCT findings with histological analysis (H&E, trichrome stains) and biochemical markers (AST, ALT levels) [27]
Data Analysis: Compare vascular density, attenuation coefficients, and stiffness values at different time points (e.g., day 0, 3, and 7 post-intervention). Statistical analysis should include appropriate multiple comparisons corrections.
Wave-Based OCE for Corneal Stiffness Assessment
This protocol details wave-based OCE methodology for detecting tissue stiffness changes, with applications in detecting pathological tissue alterations in cancer research [28].
Objective: To quantify stiffness changes in tissue resulting from pathological remodeling using wave-based optical coherence elastography.
Materials:
- Phase-sensitive OCT system (central wavelength: 840 nm, axial resolution: ~9.7 µm, lateral resolution: ~6.2 µm)
- Piezoelectric actuator with blunt needle tip
- Function generator and amplifier
- Animal preparation equipment (anesthesia, speculum)
Procedure:
- Subject Preparation:
- Anesthetize subject following approved protocols (e.g., ketamine/xylazine combination)
- Position subject using bite bar and secure eyelids with speculum
- Maintain hydration with periodic saline application
- Measure baseline IOP using tonometer
- System Setup:
- Position blunt needle attached to piezoelectric actuator at temporal limbus
- Set needle contact angle at approximately 45° to tissue surface
- Configure M-B-mode imaging at 50 kHz camera rate
- Wave Excitation and Detection:
- Generate sinusoidal signals at multiple frequencies (1, 3, and 5 kHz) using function generator
- Amplify signal using piezoelectric amplifier
- Acquire M-B-mode data: 1000 A-lines (20 ms) at each of 500 spatial lateral points
- Repeat for each excitation frequency
- Wave Speed Calculation:
- Extract phase difference between sequential A-scans to compute axial particle velocity
- Reconstruct space-time maps of wave propagation
- Apply linear regression to determine wave speed at each frequency
- Calculate Young's modulus using appropriate viscoelastic models
Data Analysis: Compare wave speeds between experimental and control conditions using statistical tests (e.g., t-test with significance threshold of p<0.01). Correlate stiffness measurements with histological evidence of tissue remodeling.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Materials for Functional OCT Studies
| Item | Specifications | Function/Application | Example Use Cases |
|---|---|---|---|
| Spectral-Domain OCT System | Central wavelength: 1.3 µm or 840 nm; Axial resolution: 9-15 µm; Imaging speed: 20,000-50,000 A-scans/sec | High-resolution structural and functional imaging | Liver regeneration monitoring [27], corneal biomechanics [28] |
| Phase-Sensitive OCT Platform | Displacement sensitivity: <1 nm; Phase stability: high | Detection of nanoscale tissue displacements for elastography | Wave-based OCE [28] |
| Piezoelectric Actuator | Frequency range: 1-5 kHz; Suitable amplification | Controlled mechanical excitation for elastography | Shear wave generation in OCE [28] |
| Animal Disease Models | Species-appropriate (e.g., Wistar rats, Macaca mulatta) | Modeling human disease pathophysiology | Partial hepatectomy model [27], experimental glaucoma [28] |
| Function Generator | Multiple waveform output; Frequency precision | Generating excitation signals for mechanical actuation | Wave-based OCE [28] |
| Motion Compensation Algorithms | Phase difference compensation; Speckle tracking | Artifact reduction in OCTA and OCE | Microvascular imaging in presence of tissue motion [27] |
| Polarization-Sensitive OCT Components | Polarization-maintaining optics; Polarization diversity detection | Birefringence contrast imaging | Collagen organization assessment [29] |
| Attenuation Coefficient Algorithm | Depth-resolved method [27] | Quantifying tissue optical properties | Differentiating tissue types based on scattering properties [27] |
Data Analysis and Interpretation
Quantitative Analysis of Functional OCT Data
Functional OCT generates multidimensional datasets requiring specialized analytical approaches. OCTA data analysis typically involves vessel segmentation, skeletonization, and morphometric parameter extraction including vessel density, diameter, tortuosity, and branching patterns [24]. In cancer research, particular attention should be paid to heterogeneous vascular patterns and abnormal vessel morphologies characteristic of tumor angiogenesis.
OCE data interpretation requires understanding of mechanical models relating measured wave speeds to tissue viscoelastic properties. The shear wave speed is directly related to tissue stiffness through the relationship: ( v = \sqrt{\frac{E}{3\rho}} ) for incompressible materials, where ( E ) is Young's modulus and ( \rho ) is tissue density [28]. Stiffness alterations in cancer may manifest as focal increases at tumor cores or peripheral changes at invasion fronts.
Attenuation coefficient mapping provides quantitative measures of tissue scattering properties, which correlate with structural alterations in disease states. In liver regeneration studies, attenuation coefficients increased by the third day post-resection before trending toward normal values, reflecting tissue remodeling processes [27]. Similar approaches can detect structural disorganization in malignancies.
Integration with Artificial Intelligence
AI and deep learning are transforming functional OCT analysis by enabling automated segmentation, classification, and prediction tasks. Convolutional neural networks can identify subtle patterns in OCT data that may elude conventional analysis, potentially improving early cancer detection and classification accuracy [30]. AI-driven platforms are particularly valuable for analyzing the complex datasets generated by multimodal OCT, integrating structural, vascular, and mechanical information for comprehensive tissue characterization [29].
Visualizing Functional OCT Workflows
Functional OCT extensions have fundamentally transformed the capabilities of optical imaging in cancer research. The integration of angiography, elastography, and spectroscopic techniques provides a multidimensional perspective on tumor pathophysiology, enabling non-invasive assessment of critical hallmarks of cancer including angiogenesis, tissue mechanics, and metabolic alterations. These technologies offer unprecedented opportunities for longitudinal monitoring of disease progression and treatment response in preclinical models, potentially accelerating therapeutic development. As functional OCT continues to evolve with advancements in artificial intelligence, multimodal integration, and novel contrast mechanisms, its role in cancer diagnostics research will expand, providing researchers and drug development professionals with powerful tools to visualize and quantify the complex tumor microenvironment.
Optical Coherence Tomography (OCT) represents a cornerstone imaging technology in biomedical research and clinical diagnostics, offering non-invasive, high-resolution, cross-sectional imaging of biological tissues. The fundamental principle of OCT relies on low-coherence interferometry to measure backscattered light from tissue microstructures, generating volumetric images with micrometer-scale resolution. In the specific context of cancer diagnostics research, OCT's ability to provide real-time, label-free optical biopsies has positioned it as a valuable tool for identifying pathological alterations in tissue morphology. However, the optimization of OCT systems necessitates careful consideration of the intrinsic trade-offs between three critical parameters: spatial resolution, penetration depth, and imaging speed. These interdependent factors directly influence image quality, diagnostic capability, and practical applicability in both preclinical and clinical settings.
The pursuit of higher resolution in OCT imaging inevitably conflicts with the need for sufficient penetration depth to visualize clinically relevant tissue structures. This technical challenge is particularly pronounced in oncology applications, where the identification of early neoplastic changes often requires cellular-level resolution at depths sufficient to assess subepithelial morphology. Furthermore, the transition from preclinical validation to clinical translation introduces additional constraints regarding imaging speed, patient comfort, and safety standards. This application note provides a detailed technical framework for understanding and navigating these trade-offs, offering specific protocols and performance specifications tailored to cancer diagnostics research.
Fundamental Technical Principles and Trade-offs
The Resolution-Penetration Relationship
In OCT system design, resolution and penetration depth are governed by distinct yet interconnected physical principles. Axial resolution, the ability to distinguish features along the beam's axis, is determined solely by the coherence length of the light source and is mathematically expressed as Δz = (2ln2/π)⋅(λ²/Δλ), where λ is the center wavelength and Δλ is the spectral bandwidth. Consequently, achieving ultrahigh axial resolution (< 2 µm) requires broadband light sources with bandwidths exceeding 150 nm in the visible spectrum or 250 nm in near-infrared regions [31]. For example, Visible Light OCT (VIS-OCT) systems utilizing shorter wavelengths (500-650 nm) achieve superior axial resolutions of approximately 1.0-1.7 µm compared to the 5-10 µm typical of conventional near-infrared OCT (NIR-OCT) systems [31].
Lateral resolution, determined by the focusing properties of the optical system, follows the conventional rules of Gaussian beam optics. The lateral spot size is given by Δx = (4λ/π)⋅(f/D), where f is the focal length and D is the beam diameter. High lateral resolution necessitates large numerical apertures (NA), which inherently reduce the depth of focus (DOF). This creates a fundamental constraint where systems optimized for high lateral resolution suffer from limited usable imaging range, requiring mechanical refocusing or computational solutions to maintain resolution throughout the imaging depth [32].
Penetration depth in OCT is primarily limited by optical scattering and absorption in biological tissues. Scattering increases exponentially as wavelength decreases, making visible light OCT (VIS-OCT) suitable for superficial imaging (e.g., retina, skin epidermis), while near-infrared light (NIR-OCT around 1300 nm) provides deeper penetration (1-2 mm in most tissues) due to reduced scattering and absorption in the "optical window" of biological tissues [33] [34]. This wavelength-dependent attenuation directly establishes the core trade-off: shorter wavelengths enable higher resolution but shallower penetration, while longer wavelengths provide deeper penetration at the expense of resolution.
Advanced Techniques for Performance Enhancement
Recent technological innovations have sought to overcome these inherent limitations through novel approaches. Chromatic OCT leverages pronounced chromatic focal shifts in high-numerical-aperture optics to extend the depth of focus while maintaining high isotropic resolution of 2-3 µm. This system utilizes a broad bandwidth source (650-950 nm) and specialized processing algorithms to achieve up to a sevenfold DOF extension compared to conventional high-resolution OCT systems [32]. Similarly, Bessel beam illumination techniques can extend the focal range but often introduce sidelobe artifacts and signal-to-noise ratio (SNR) penalties inversely proportional to the square of the DOF gain [32].
Dynamic contrast OCT (DyC-OCT) represents an alternative approach that extracts additional functional information from signal fluctuations rather than relying solely on structural backscattering. By analyzing temporal variations in OCT signals caused by intracellular motions and metabolic activity, DyC-OCT enhances image contrast for cellular and subcellular features without requiring exogenous contrast agents [35]. This method effectively improves the visualization of cellular morphology despite resolution limitations, making it particularly valuable for live cell imaging and viability assessment in cancer research.
Table 1: Key Performance Trade-offs in OCT System Design
| Parameter | High-Resolution Configuration | High-Penetration Configuration | Balanced Clinical Configuration |
|---|---|---|---|
| Wavelength Range | Visible (500-650 nm) [31] | NIR (1300 nm) [34] | Broadband NIR (1000-1300 nm) |
| Axial Resolution | 1.0-1.7 µm [31] | 8-12 µm [34] | 3-5 µm |
| Lateral Resolution | 2-4 µm (high NA) [32] | 15-25 µm (low NA) [34] | 8-12 µm |
| Penetration Depth | 0.3-0.5 mm [31] | 1.5-2.0 mm [34] | 1.0-1.5 mm |
| Typical Applications | Retinal layers [31], cellular imaging [35] | Anterior eye [34], dermatology | Intracoronary imaging [36], endoscopic |
Technical Specifications Across OCT Modalities
Comparative Performance Analysis
The implementation of OCT technology has evolved into several distinct modalities, each with characteristic performance profiles suited to specific applications in cancer research. Spectral-Domain OCT (SD-OCT) utilizes a broadband light source and spectrometer-based detection, offering superior sensitivity and signal-to-noise ratio for rapid imaging. Modern SD-OCT systems achieve axial resolutions of 1-3 µm with A-scan rates exceeding 100 kHz, making them ideal for high-resolution anatomical imaging of layered structures [33] [35]. Swept-Source OCT (SS-OCT) employs a wavelength-tunable laser and photodetector, enabling higher imaging speeds (up to 400 kHz) and longer imaging ranges (> 10 mm) while maintaining resolutions of 8-12 µm [34]. This makes SS-OCT particularly suitable for comprehensive volumetric imaging of larger tissue structures.
Emerging implementations continue to push performance boundaries. Visible Light OCT (VIS-OCT) exemplifies the high-resolution approach, achieving 1.7 µm axial resolution by operating at shorter wavelengths (585 nm center) [31]. This ultrahigh resolution enables visualization of fine retinal structures including sub-banding in the photoreceptor layers and individual capillary networks. Conversely, long-range SS-OCT systems designed for anterior eye imaging demonstrate the deep-penetration approach, offering 15.5 mm imaging range with 12.2 µm axial resolution at 1310 nm wavelength [34]. This extended range enables simultaneous visualization of both anterior and posterior corneal surfaces, along with detailed assessment of iris and lens structures.
Table 2: Performance Specifications of OCT Modalities for Cancer Research
| OCT Modality | Axial Resolution (µm) | Lateral Resolution (µm) | Imaging Depth (mm) | A-Scan Rate | Key Applications in Oncology |
|---|---|---|---|---|---|
| SD-OCT | 1-3 [35] | 4-15 [37] | 1.0-1.5 [35] | Up to 100 kHz | Superficial epithelial imaging, cellular dynamics [35] |
| SS-OCT | 8-12 [34] | 15-25 [34] | 2.0-4.0 [34] | 100-400 kHz | Volumetric tumor mapping, angiography |
| VIS-OCT | 1.0-1.7 [31] | 2-4 [31] | 0.3-0.5 [31] | 24-125 kHz | Retinal metabolism, microvascular oximetry [31] |
| FF-OCT | ~1.0 [35] | ~1.0 [35] | 0.2-0.3 [35] | Limited by camera frame rate | Live cell imaging, organoid assessment [35] |
| Chromatic OCT | 2-3 [32] | 2-3 [32] | 0.7-1.0 [32] | Standard SD-OCT rates | High-resolution deep tissue imaging [32] |
Impact of Light Source Selection
The light source fundamentally determines OCT system capabilities, with center wavelength and bandwidth dictating both resolution and penetration characteristics. Superluminescent diodes (SLDs) provide compact, cost-effective solutions with moderate bandwidths (50-100 nm) suitable for general-purpose OCT systems. Supercontinuum lasers offer extremely broad bandwidths (>200 nm) enabling ultrahigh resolution (<2 µm) but introduce challenges with relative intensity noise that requires balanced detection schemes [31]. Vertical-cavity surface-emitting lasers (VCSELs) utilized in SS-OCT systems provide narrow linewidths with rapid tuning capabilities, enabling long imaging ranges with minimal sensitivity roll-off [34].
The recent development of broadband cyan-green SLD sources for VIS-OCT represents a significant advancement toward reducing system complexity while maintaining >95% shot-noise-limited performance [31]. Similarly, second harmonic generation approaches using periodically poled lithium niobate crystals enable conversion of commercial NIR swept sources to the visible range, offering a promising route toward high-speed, deep-penetration visible-light imaging [31]. These source innovations continue to expand the available parameter space for OCT system designers, enabling more specialized implementations for specific cancer diagnostic applications.
Experimental Protocols for Cancer Imaging Applications
Protocol 1: Dynamic Contrast OCT for Live Cell Imaging
Purpose: To visualize cellular morphology and monitor changes in cellular activity/viability in 3D tumor spheroids or cancer cell cultures without exogenous labels.
Principle: DyC-OCT analyzes temporal fluctuations in OCT signals caused by intracellular motions and metabolic activities. These fluctuations provide enhanced contrast for cellular structures, enabling label-free visualization of subcellular features [35].
Materials and Equipment:
- Spectral-domain or swept-source OCT system with high spatial resolution (<5 µm)
- Stable environmental chamber maintaining 37°C and 5% CO₂
- Cancer cell lines or patient-derived organoids
- Matrigel or extracellular matrix substitute for 3D cultures
- Custom sample holders compatible with OCT imaging
Procedure:
- Sample Preparation:
- Embed cancer cells in Matrigel (1:1 ratio) in glass-bottom culture dishes.
- Culture for 3-7 days to form 3D spheroids or organoids.
- Replace culture medium with fresh pre-warmed medium before imaging.
System Configuration:
- Set OCT system to high-resolution mode (axial resolution <5 µm).
- Configure for repeated B-scans at the same location (M-B mode).
- Set B-scan rate to at least 2x the frequency of cellular dynamics being measured (typically 1-10 Hz).
- Adjust incident power to 5-10 mW to ensure safety for live cells.
Data Acquisition:
- Acquire 50-100 repeated B-scans at each location for STD and OCDS analysis.
- For PSD analysis, acquire 200+ repeated B-scans to ensure frequency resolution.
- For 3D DyC-OCT, acquire repeated volumetric scans (5-10 volumes).
- Total acquisition time per location should not exceed 5 minutes to maintain cell viability.
Signal Processing:
- STD Algorithm: Calculate temporal standard deviation of intensity fluctuations for each pixel to highlight regions of high dynamic activity.
- OCDS Analysis: Compute temporal autocorrelation function for each pixel and extract decay constant to quantify speed of intracellular dynamics.
- PSD Analysis: Perform fast Fourier transform on temporal fluctuations and integrate power within specific frequency bands (0.8-4 Hz for slow dynamics, 4-20 Hz for fast dynamics).
Image Interpretation:
- Overlay DyC-OCT colormaps on structural OCT images for co-registered visualization.
- Interpret high-dynamic regions as areas of viable, metabolically active cells.
- Correlate specific fluctuation frequencies with different cellular processes (organelle transport, membrane fluctuations).
Troubleshooting:
- Poor contrast may result from insufficient frame rate; increase B-scan repetition rate.
- Excessive photodamage manifests as gradual reduction then cessation of dynamics; reduce incident power.
- Motion artifacts can be minimized by mechanical stabilization of sample chamber.
Protocol 2: High-Resolution Vascular Imaging and Oximetry
Purpose: To characterize tumor microvasculature and quantify hemoglobin oxygen saturation (sO₂) for assessment of tumor hypoxia.
Principle: VIS-OCT leverages the strong optical absorption of hemoglobin in the visible range to enable spectroscopic oximetry while utilizing ultrahigh resolution to resolve microvascular networks [31].
Materials and Equipment:
- VIS-OCT system with center wavelength 500-650 nm and axial resolution <2 µm
- Balanced detection system to minimize relative intensity noise
- Rodent window chamber models or translucent tumor models
- Image processing workstation with custom oximetry algorithms
Procedure:
- System Calibration:
- Characterize wavelength-dependent system response using calibrated reflectance standards.
- Validate spectroscopic detection with phantoms containing known hemoglobin oxygen saturation.
- Optimize reference arm power to achieve shot-noise-limited detection.
In Vivo Imaging:
- Anesthetize animal and stabilize tissue region of interest.
- Position animal for OCT imaging with tumor region accessible to probe beam.
- Acquire 3D OCT volumes (500 x 500 x 1024 pixels) over tumor region.
- For angiography, acquire repeated B-scans (5 repeats) at each location.
Data Processing:
- Angiogram Generation: Compute speckle variance or phase variance between repeated B-scans to extract vascular network.
- Extinction Coefficient Calculation: For each vessel segment, determine attenuation coefficient at multiple wavelengths (560 nm and 585 nm).
- sO₂ Calculation: Apply modified Beer-Lambert law using known extinction coefficients of oxy- and deoxy-hemoglobin: sO₂ = (εHb·μa^λ2 - εHb·μa^λ1) / (μa^λ2·(εHbO - εHb) - μa^λ1·(εHbO - εHb)) where εHb and εHbO are extinction coefficients, and μ_a is absorption coefficient.
Data Analysis:
- Segment vascular network into arterioles, venules, and capillaries based on diameter and flow characteristics.
- Quantify vascular density, vessel diameter distribution, and tortuosity.
- Map sO₂ values across vascular network to identify hypoxic regions.
- Correlate vascular parameters with histological findings when possible.
Validation:
- Compare OCT oximetry readings with simultaneous measurements using fiber-optic probes.
- Validate microvascular morphology with confocal or two-photon microscopy post-mortem.
- Correlate hypoxic regions with immunohistochemical markers (pimonidazole, HIF-1α).
Visualization of Technical Trade-offs and Workflows
Technical Interdependencies in OCT System Design
Experimental Workflow Selection Framework
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Materials for OCT in Cancer Research
| Category | Specific Items | Function/Application | Technical Notes |
|---|---|---|---|
| Cell Culture | Matrigel, Collagen I, Organoid media | 3D tumor spheroid formation, tumor microenvironment modeling | Optimal matrix concentration varies by cell type; maintain pH stability during imaging |
| Contrast Agents | Gold nanoparticles, Magnetic microparticles [35] | Enhanced scattering for specific targeting, molecular contrast | Functionalize surfaces with targeting ligands; optimize concentration for SNR improvement |
| Tissue Phantoms | Titanium dioxide, Silicone elastomers, Intralipid [38] | System calibration, resolution validation, protocol optimization | Adjust scattering coefficients to match tissue type (μs' = 0.5-2.0 mm⁻¹) |
| Immobilization | Agarose, Custom tissue holders, Medical adhesive | Motion stabilization during in vivo imaging | Ensure biocompatibility; minimize pressure-induced tissue deformation |
| Optical Components | Balanced detectors, Dispersion compensation optics [31] | System optimization, artifact reduction | Essential for ultrahigh-resolution systems; requires precise alignment |
| Calibration Standards | US Air Force resolution target, Spectralon reflectance standards | Spatial and spectral calibration | Regular validation maintains measurement accuracy |
The strategic balancing of penetration depth and resolution parameters in OCT system design remains a critical consideration for advancing cancer diagnostics research. As demonstrated through the technical specifications and experimental protocols outlined in this application note, optimal OCT configuration is inherently application-dependent, requiring researchers to make informed decisions based on specific biological questions and experimental constraints. The ongoing development of novel OCT methodologies, including chromatic OCT with extended depth-of-focus and dynamic contrast OCT for enhanced cellular visualization, continues to expand the technological landscape available to cancer researchers.
Future directions in OCT technology development point toward increasingly sophisticated approaches for overcoming traditional performance trade-offs. Computational imaging techniques, including inverse scattering algorithms and machine learning-based image reconstruction, show promise for extracting additional information from detected signals while minimizing hardware limitations. Similarly, the integration of multi-modal imaging approaches combining OCT with complementary techniques such as fluorescence microscopy or Raman spectroscopy offers opportunities for correlative structural and molecular assessment. These advancements, coupled with continued innovation in light source technology and detection schemes, will further establish OCT as an indispensable tool in the cancer researcher's arsenal, ultimately contributing to improved diagnostic capabilities and therapeutic monitoring in oncology.
OCT in Action: Methodologies for Cancer Detection, Diagnosis, and Guided Therapy
Optical biopsy represents a paradigm shift in cancer diagnostics, enabling non-invasive, real-time detection of pre-cancerous and early malignant changes in epithelial tissues. Unlike traditional histopathology, which requires physical tissue removal and processing, optical biopsy techniques utilize light-tissue interactions to provide immediate microscopic information of tissue microstructure. These technologies are particularly vital for examining epithelial tissues, the origin of approximately 85% of all cancers [39]. Among these technologies, Optical Coherence Tomography (OCT) has emerged as a cornerstone modality, providing cross-sectional images of biological tissues with resolutions approaching the cellular level (typically 1-10 μm) without the need for contrast agents or ionizing radiation [40] [35]. The fundamental principle underlying OCT is low-coherence interferometry, which measures the backscattered or reflected light from tissue microstructures to generate depth-resolved images [40].
The clinical significance of optical biopsy lies in its potential to address critical diagnostic challenges. Traditional biopsy procedures suffer from sampling errors, with studies indicating that 25-50% of early esophageal cancers are missed during initial endoscopic surveillance [41]. Optical biopsy technologies can guide physical biopsy to suspicious areas, significantly improving detection rates. Furthermore, the real-time feedback provided by these systems enables immediate clinical decision-making during diagnostic and therapeutic procedures. Advanced forms of OCT, including Dynamic Contrast OCT (DyC-OCT) [35], OCT angiography (OCTA) [42], and vibrational OCT (VOCT) [43], now provide functional information beyond structural imaging, revealing metabolic activity, microvascular changes, and tissue biomechanics that correlate with early neoplastic transformation.
Table 1: Comparison of Major Optical Biopsy Technologies
| Technology | Resolution | Penetration Depth | Key Applications | Strengths |
|---|---|---|---|---|
| Optical Coherence Tomography (OCT) | 1-10 μm [40] [35] | 1-2 mm [40] | Retina, skin, GI tract, oral mucosa [42] [41] [40] | High-resolution cross-sectional imaging, real-time capability |
| Frequency-Domain Angle-Resolved Low Coherence Interferometry (fa/LCI) | Subcellular [39] | Epithelial layer [39] | Esophagus, colon, lung [39] | Detects nuclear morphology changes, single-cell sensitivity |
| Dynamic Contrast OCT (DyC-OCT) | 1-10 μm [35] | 1-2 mm [35] | Live cell imaging, tissue viability assessment [35] | Visualizes cellular dynamics and metabolic activity |
| Vibrational OCT (VOCT) | 1-10 μm [43] | 1-2 mm [43] | Skin cancer, squamous cell carcinoma [43] | Assesses tissue biomechanical properties |
Key Optical Coherence Tomography Methodologies
Structural OCT for Epithelial Layer Analysis
Structural OCT serves as the foundation for optical biopsy by providing detailed cross-sectional images of epithelial tissues. In normal epithelial tissues, OCT reveals distinct, well-organized layers including the keratinized layer (KL), stratified epithelial layer (SEL), basement membrane (BM), and lamina propria (LP) [41]. The transition to precancerous states is characterized by specific structural alterations: epithelial thickening, disruption of the basement membrane, and loss of normal layer architecture [41]. In squamous cell carcinoma, OCT images demonstrate reduced reflection in the green channel and loss of hyporeflective regions corresponding to architectural disintegration at the cellular level [43].
The diagnostic capability of structural OCT has been quantitatively validated in oral carcinogenesis. A recent cross-sectional study implementing targeted biopsy-based OCT protocols demonstrated exceptional diagnostic performance for oral squamous cell carcinoma (OSCC) with 98.57% sensitivity and 100% specificity after target site registration [41]. Similarly, for oral leukoplakia (OL) and oral lichen planus (OLP), OCT achieved sensitivities and specificities exceeding 97% [41]. These performance metrics highlight OCT's capability to differentiate between various stages of epithelial transformation, from benign disorders to invasive carcinoma.
Dynamic Contrast OCT (DyC-OCT) for Cellular Dynamics
DyC-OCT represents a significant advancement in functional imaging by leveraging temporal fluctuations in OCT signals to generate contrast based on cellular dynamics [35]. This label-free technique captures intracellular motions and metabolic activities by analyzing signal fluctuations from repeated scans at the same location. The core principle is that living cells exhibit continuous dynamic processes including metabolic activity, organelle movement, and membrane fluctuations that alter optical scattering properties [35]. These inherent motions create a characteristic "dynamic fingerprint" that distinguishes viable cells from non-viable tissue or artifacts.
Several algorithmic approaches have been developed to extract dynamic information from OCT signal fluctuations:
- Standard Deviation (STD) Analysis: Measures the amplitude of OCT signal fluctuations, highlighting regions of high metabolic activity [35]. This method requires approximately 10 repeated frames and provides robust contrast enhancement for cellular visualization.
- OCT Correlation Decay Speed (OCDS): Quantifies the speed of dynamic motions by analyzing the temporal decorrelation function of OCT signals [35]. This approach differentiates between slow and rapid cellular dynamics, providing additional functional information.
- Power Spectral Density (PSD) Analysis: Utilizes Fast Fourier Transform to analyze fluctuation frequencies, offering comprehensive insights into tissue dynamics across multiple frequency bands [35]. This method typically requires over 100 repeated scans but provides the most detailed dynamic profiling.
DyC-OCT has demonstrated particular utility in live cell imaging and tissue viability assessment. Experimental studies have shown that DyC-OCT can effectively monitor cellular responses to therapeutic interventions, track viability in 3D tissue models, and visualize individual cells within complex tissue architectures without exogenous labels [35].
Vibrational OCT (VOCT) for Biomechanical Properties
VOCT combines conventional OCT imaging with controlled mechanical stimulation to assess tissue biomechanical properties, which are increasingly recognized as important biomarkers in carcinogenesis [43]. This technique applies sound frequencies in the range of 50-80 Hz to target cellular components and 100-120 Hz for collagen evaluation [43]. The resulting tissue displacements are measured by analyzing phase changes in the reflected OCT signals, generating mechanovibrational spectra that reveal the resonant frequencies of different tissue components.
In squamous cell carcinoma, VOCT has identified distinctive biomechanical signatures characterized by altered resonant frequencies in cancerous regions compared to normal adjacent tissue [43]. These mechanical changes correlate with histopathological features including disorganized collagen architecture, keratin accumulation, and loss of tissue elasticity. The application of resonant frequencies specifically targets cancer-associated fibroblasts (CAFs) and transformed keratinocytes, providing a novel approach to identify microenvironmental changes associated with early malignant transformation [43].
Quantitative Diagnostic Parameters and Performance
The diagnostic utility of optical biopsy technologies depends on quantitative parameters derived from optical signatures. These parameters provide objective metrics for distinguishing between normal, precancerous, and cancerous epithelial tissues.
Table 2: Quantitative OCT Parameters for Epithelial Tissue Classification
| Tissue Type | OCT Parameter | Normal Range | Abnormal Range | Diagnostic Significance |
|---|---|---|---|---|
| Normal Epithelium | Epithelial thickness | Site-dependent [41] | Increased thickness [41] | Basal layer hyperplasia |
| Basement membrane integrity | Continuous, well-defined [41] | Disrupted or indistinct [41] | Early invasion | |
| Signal intensity gradient | Consistent layer pattern [41] | Disorganized pattern [41] | Architectural disruption | |
| Dysplastic Epithelium | Nuclear size distribution | Consistent size [39] | Irregular, enlarged [39] | Nuclear pleomorphism |
| Nuclear-to-cytoplasmic ratio | Lower ratio [39] | Increased ratio [39] | Cellular atypia | |
| Subcellular heterogeneity | Uniform scattering [35] | Increased heterogeneity [35] | Early transformation | |
| Squamous Cell Carcinoma | Green channel intensity | Higher in normal [43] | Reduced intensity [43] | Cellular content changes |
| Resonant frequency | Normal skin profile [43] | Altered frequency [43] | Tissue stiffness changes | |
| Keratin accumulation | Minimal [43] | Significant [43] | Tumor differentiation |
The diagnostic performance of OCT-based optical biopsy has been rigorously evaluated across various epithelial tissues. In gastroenterology applications, fa/LCI demonstrated 100% sensitivity for detecting precancerous changes in Barrett's esophagus epithelium [39]. For oral cavity lesions, targeted OCT protocols achieved near-perfect differentiation of oral squamous cell carcinoma with 98.57% sensitivity and 100% specificity [41]. These performance metrics approach and sometimes exceed those of conventional histopathology, particularly when functional OCT techniques are combined with structural assessment.
Experimental Protocols and Methodologies
Protocol 1: Targeted OCT with Site Registration for Oral Lesions
This protocol outlines a standardized approach for OCT imaging of oral potentially malignant disorders (OPMDs) and oral squamous cell carcinoma (OSCC), ensuring precise correlation between optical images and histopathology [41].
Sample Preparation and Mounting
- Obtain informed consent and institutional review board approval following ethical guidelines.
- Perform comprehensive conventional oral examination (COE) to document lesion characteristics.
- Acquire digital photographs of each lesion using a standardized imaging system (e.g., Nikon D7200 Camera with AF-S DX 105 mm F2.8G Lens and R1C1 dual flash).
- Code each lesion site according to NIH/SEER ICD-0-3.2 topographical classification (C02.0-C02.2 for mobile tongue, C03.0-C03.1 for upper/lower gum, C06.0 for cheek mucosa).
OCT Image Acquisition
- Utilize a Swept-source Fourier-Domain OCT system (e.g., OCT SS-OCT VivoSight) with central wavelength of 1305 ± 15 nm.
- Set axial resolution to <10 μm and lateral resolution to <7.5 μm with maximum scan width of 6 mm × 6 mm.
- Acquire "EnFace" scans with default width of 6 mm with 120 slices (50 μm slicing step) for total scan duration of 12 seconds.
- Perform preliminary OCT assessment on the most clinically suggestive area of each lesion.
- Acquire 120 OCT scans per lesion, then select 10 most representative scans based on image definition and tissue stratification clarity.
Site Registration and Histological Correlation
- Mark the OCT imaging area with surgical ink or gentle surface ablation.
- Perform punch biopsy precisely at the registered imaging site.
- Process biopsy specimens using standard histological preparation with H&E staining.
- Correlate OCT findings with histopathological diagnosis by blinded, experienced pathologists.
Image Analysis
- Analyze OCT scans for characteristic features of OL, OLP, and OSCC using validated parameters.
- Evaluate keratinized layer thickness, epithelial layer organization, basement membrane integrity, and lamina propria density.
- For OSCC, identify specific features including epithelial thickening, basement membrane disruption, and altered signal intensity.
Protocol 2: DyC-OCT for Live Cell Imaging and Viability Assessment
This protocol details the application of DyC-OCT for non-invasive monitoring of cellular dynamics and viability in epithelial tissue models [35].
System Configuration
- Select appropriate OCT modality based on resolution requirements:
- Full-field OCT (FF-OCT): For highest resolution (~1 μm) imaging of thin samples (<300 μm)
- Spectral-domain OCT (SD-OCT): For balanced resolution (~1-2 μm) and penetration (~1 mm) in layered tissues
- Swept-source OCT (SS-OCT): For high-speed imaging of thick samples with lower resolution (~10 μm)
- Ensure system frame rate exceeds twice the frequency of target dynamics (Nyquist criterion).
- For metabolic activity imaging, implement high-speed acquisition capable of capturing rapid fluctuations.
Sample Preparation
- Culture epithelial cells or tissue explants in appropriate media under standard conditions.
- For 3D models (organoids, spheroids), maintain in matrigel or similar extracellular matrix substitute.
- Mount samples in imaging chambers compatible with OCT systems.
- For viability assessment, include control samples with known viability status.
Data Acquisition
- Acquire repeated B-scans or volumetric scans at the same location.
- For STD and OCDS analysis: Acquire minimum of 10 repeated frames.
- For PSD analysis: Acquire minimum of 100 repeated frames for adequate frequency resolution.
- Maintain stable environmental conditions (temperature, CO₂, humidity) throughout acquisition.
Signal Processing and Dynamic Contrast Extraction
- Reconstruct OCT intensity images from raw interferometric data.
- Apply logarithmic transformation to B-frame data for analysis.
- Implement appropriate dynamic analysis algorithm:
- STD Analysis: Compute temporal standard deviation of each pixel across repeated frames.
- OCDS Analysis: Calculate temporal autocorrelation function and fit with exponential decay model.
- PSD Analysis: Perform FFT on temporal signals and integrate power within specific frequency bands.
- Generate color-coded DyC-OCT maps overlayed on structural OCT images.
Interpretation and Quantification
- Identify regions of high dynamic activity corresponding to viable cells.
- Compare dynamic patterns between experimental conditions and controls.
- For viability assessment, correlate signal fluctuation amplitude with metabolic activity markers.
- Quantify dynamic parameters (STD values, OCDS rates, PSD integrals) for statistical analysis.
Protocol 3: Vibrational OCT for Biomechanical Property Assessment
This protocol describes the integration of mechanical stimulation with OCT imaging to assess tissue biomechanical properties in epithelial lesions [43].
System Configuration
- Modify commercial OCT system (e.g., Lumedica OQ Labscope 2.0) by adding a 2-inch diameter speaker placed approximately 2 inches from the tissue surface.
- Integrate sound generation system capable of producing sinusoidal waves at 55 dB with frequency range of 50-260 Hz.
- Synchronize sound wave application with OCT image acquisition along the axis of the light beam.
- Implement software for controlled frequency sweeps and displacement measurement.
Sample Handling
- For in vivo measurements: Position probe perpendicular to tissue surface with minimal contact pressure.
- For ex vivo measurements: Mount excised tissue samples in physiological solution to maintain hydration.
- Ensure proper stabilization to eliminate external vibrations.
Data Acquisition
- Apply sound frequencies across the diagnostic spectrum:
- 50-80 Hz: Target cellular components and cancer-associated fibroblasts
- 100-120 Hz: Evaluate collagen properties
- 130-150 Hz: Assess blood vessels
- 180-260 Hz: Characterize fibrotic tissue
- Collect single raw image data for displacement calculation from A-line data.
- Acquire mechanovibrational spectra by plotting displacement amplitude against applied frequency.
Data Processing
- Process raw data using MATLAB or similar computational software.
- Calculate weighted displacement measurements from line data at single points based on lesion location.
- Filter reflected light to isolate in-phase (elastic) component with sound input signal.
- Generate displacement spectra identifying resonant frequencies of tissue components.
Image Analysis
- Analyze standard OCT images for structural features.
- Process gray scale OCT images through RGB subchannel decomposition:
- Green channel: Cellular content representation
- Blue channel: Collagen information
- Red channel: General tissue architecture
- Generate pixel intensity versus depth plots for quantitative comparison.
- Correlate vibrational data with structural findings.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of optical biopsy protocols requires specific research tools and materials. The following table details essential components for establishing OCT-based epithelial tissue analysis.
Table 3: Essential Research Materials for Optical Biopsy Studies
| Category | Item | Specifications | Application/Function |
|---|---|---|---|
| Imaging Systems | Swept-source OCT system | Central wavelength 1305±15nm, axial resolution <10μm [41] | High-resolution cross-sectional imaging |
| Spectral-domain OCT system | Central wavelength 840nm, frame rate 13,000 fps [43] | High-speed cellular imaging | |
| Full-field OCT system | Isotropic resolution ~1μm [35] | Ultra-high resolution cellular imaging | |
| Sample Preparation | Cell culture media | Organoid-specific (e.g., STEMCELL protocols) [35] | Maintain tissue viability during imaging |
| Extracellular matrix | Matrigel or similar substitutes [35] | 3D tissue model support | |
| Imaging chambers | Compatible with OCT systems [35] | Sample mounting and stabilization | |
| Analysis Tools | MATLAB software | With image processing toolbox [43] [44] | Data processing and algorithm implementation |
| ImageJ/Fiji | With custom plugins [43] | Image analysis and visualization | |
| GLCM texture analysis | 100×100 texture maps [44] | Quantitative texture feature extraction | |
| Computational Resources | Vision Transformer models | DINOv2 architecture [44] | Feature extraction and classification |
| Convolutional Neural Networks | Custom architectures [44] | Image analysis and pattern recognition | |
| Adversarial discriminator networks | Patient-specific bias mitigation [44] | Improved generalizability |
Emerging Applications and Future Directions
The application of optical biopsy technologies continues to expand with emerging clinical and research applications. In neurosurgical oncology, OCT-based systems have demonstrated exceptional capability to distinguish cancerous from noncancerous brain tissue with 98.6% accuracy using advanced machine learning classification [44]. This intraoperative guidance application highlights the potential for real-time surgical margin assessment. For systemic disease monitoring, OCT angiography has revealed correlations between retinal microvascular changes and cardiovascular risk, with studies showing decreased superficial capillary plexus vessel density (SCP-VD) in patients with acute coronary syndrome [42].
The integration of artificial intelligence with optical biopsy represents perhaps the most promising future direction. Vision transformer models combined with convolutional neural networks have achieved unprecedented classification performance by leveraging both global contextual features and local texture patterns [44]. These approaches effectively mitigate patient-specific bias through adversarial discrimination networks, forcing models to learn generalizable cancer-indicative features rather than individual patient characteristics [44]. Further advancements in automated diagnostic algorithms will likely focus on standardized imaging protocols and interoperable data formats to enable multicenter validation studies [41].
Emerging technical innovations continue to address current limitations in optical biopsy. Ultra-high speed OCT systems are enabling comprehensive 4D imaging (3D space + time) for capturing rapid dynamic processes [35]. Multimodal approaches combining OCT with complementary techniques like Raman spectroscopy and fluorescence imaging provide correlated structural and molecular information [45]. These technological advances, coupled with robust validation studies, position optical biopsy as an increasingly essential tool for early cancer detection in epithelial tissues.
Accurate assessment of tumor margins during cancer surgery is a critical determinant of patient prognosis. In breast-conserving surgery (BCS), which has become the standard treatment for early-stage breast cancer, positive resection margins (where cancer cells are found at the edge of the excised tissue) occur in 20-30% of cases, necessitating repeat surgeries in 20-70% of patients [46] [47]. Re-excision procedures significantly increase patient trauma, healthcare costs, and delay adjuvant therapies [46] [48]. The fundamental challenge stems from the lack of real-time, intraoperative tools for microscopic margin evaluation; traditional histopathology, the gold standard, requires days for processing and cannot guide surgical decision-making in the operating room [47].
Optical Coherence Tomography (OCT) has emerged as a powerful, real-time imaging technology capable of addressing this clinical need. OCT functions as the optical analogue to ultrasound, utilizing near-infrared light to generate high-resolution, cross-sectional images of tissue microstructure in real-time [49]. It provides a non-destructive, label-free method for visualizing tissue morphology up to 1-2 mm beneath the surface, a depth scale directly relevant to the definitions of "close" (e.g., tumor cells within 1-2 mm) and "positive" (ink on tumor cells) margins [49] [50]. This application note details the implementation of OCT for intraoperative margin assessment, providing validated protocols and analytical frameworks tailored for research and clinical translation.
Basic OCT Principles
OCT is based on low-coherence interferometry to measure back-reflected and back-scattered light from biological tissues. A system typically employs a broadband light source (e.g., centered at 1310 nm), and the interference pattern between light from a reference arm and the sample arm is used to construct depth-resolved profiles (A-scans) [49] [17]. Multiple A-scans are combined to create two-dimensional cross-sections (B-scans), which can then be assembled into three-dimensional volumes [47]. Key performance parameters include:
- Axial Resolution: 5-15 µm, enabling visualization of cellular and sub-cellular structures.
- Penetration Depth: 1-2 mm in breast tissue, sufficient to assess margin status.
- Imaging Speed: Thousands of A-scans per second, enabling rapid assessment of large tissue areas [49] [17].
The primary contrast mechanism in standard OCT (intensity-based OCT) is the variation in optical scattering properties between tissue types. For example, highly scattering tumor cells and fibrous stroma appear bright, while the large, lipid-filled adipocytes that dominate normal breast tissue appear dark [49].
Advanced OCT Techniques
To overcome the challenge of sometimes low contrast in breast tissue, several functional extensions of OCT have been developed:
Dynamic OCT (d-OCT): This technique leverages intrinsic tissue motion (e.g., from cellular metabolism or blood flow) as a contrast mechanism. By acquiring multiple repeated B-scans at the same location and analyzing the temporal variations in the OCT signal (either intensity or phase), d-OCT generates maps of tissue dynamics. This method has been shown to provide consistently higher contrast between malignant and benign breast tissues compared to intensity-based OCT alone, potentially due to increased metabolic activity and collagen remodeling in cancerous regions [50].
AI-Enhanced OCT: The integration of Artificial Intelligence, particularly deep learning and convolutional neural networks (CNNs), is revolutionizing OCT image analysis. AI algorithms can be trained to automatically classify tissue as normal or cancerous with high sensitivity and specificity, reducing operator dependency and interpretation time. AI-assistance is pivotal for translating OCT into the clinical workflow, offering real-time decision support to surgeons [30] [17] [47].
The diagnostic performance of OCT for margin assessment has been rigorously evaluated. A recent meta-analysis reported pooled sensitivity of 91% and specificity of 88%, with a pooled area under the curve (AUC) of 0.94, confirming its high accuracy [47]. The following tables summarize key performance metrics and compare OCT against other margin assessment technologies.
Table 1: Diagnostic Performance of OCT in Breast Cancer Margin Assessment
| Cancer Type | Sensitivity | Specificity | Remarks | Source |
|---|---|---|---|---|
| Invasive Ductal Carcinoma (IDC) | 100% | 82% | Feasibility study (n=20 margins) | [49] |
| Overall Breast Cancer (Meta-Analysis) | 91% | 88% | Pooled data from multiple studies | [47] |
| AI-Enhanced OCT | Significant Improvement | Significant Improvement | Superior to OCT alone | [47] |
Table 2: Comparison of Intraoperative Margin Assessment Techniques
| Technique | Principle | Advantages | Limitations | Reported Performance (Sens/Spec) |
|---|---|---|---|---|
| OCT | Optical scattering / interferometry | Real-time, high resolution, 1-2 mm depth | Limited penetration, contrast can be low | 91% / 88% [47] |
| Specimen PET-CT | Metabolic activity & anatomy | High sensitivity for IDC | Requires radioactive tracer ([18F]FDG) | 91% / 86% (for IDC) [51] |
| Frozen Section Analysis (FSA) | Microscopy of frozen tissue | High specificity | Time-consuming (~20-30 min), sampling error | 73% / 98% [49] |
| Touch Prep Cytology | Surface cell microscopy | Assesses entire surface area | No sub-surface info, cells must detach | 75% / 83% [49] |
| Specimen Radiography | X-ray absorption | Good for microcalcifications | Poor for diffuse masses | 49% / 73% [49] |
| Stereoscopic Optical Palpation (SOP) | Tissue stiffness mapping | Fast, cost-effective, simple | Surface stress measurement only | 82% / 84% [48] |
Experimental Protocols
This section provides a detailed methodology for implementing OCT for intraoperative margin assessment, from specimen handling to image interpretation.
Protocol 1: Basic OCT Margin Assessment for Breast-Conserving Surgery
This protocol is adapted from foundational clinical feasibility studies [49] and is suitable for initial validation in a research setting.
A. Specimen Preparation and Handling
- Immediate Transfer: Transport the freshly excised lumpectomy specimen from the operating room to the imaging suite promptly.
- Hydration: Maintain tissue hydration by periodically applying physiological saline (0.9% NaCl) to prevent imaging artifacts from tissue desiccation.
- Orientation and Inking: Prior to OCT imaging, orient the specimen according to standard surgical practice (e.g., using sutures or clips). The corresponding surface should be marked with colored ink to allow precise correlation between OCT images and histology.
- Imaging Setup: Place the specimen with the margin of interest facing the OCT objective lens. Ensure stable positioning to minimize motion artifacts. A compression window can be used to flatten the tissue surface and minimize topology variations [50].
B. OCT Image Acquisition
- System Calibration: Calibrate the OCT system according to the manufacturer's instructions. A typical spectral-domain OCT system may use a 1310 nm central wavelength light source with a 100 nm bandwidth, yielding an axial resolution of ~5.9 µm in tissue [49].
- Parameter Setting:
- Power: Set the sample arm power to a safe level (e.g., <5 mW) to avoid tissue damage.
- Scan Area: Define a grid that covers the region of interest on the specimen margin. A typical scan may cover a 10 mm x 10 mm area.
- Scan Density: Acquire images with sufficient density (e.g., 500-1000 A-scans per B-scan) to resolve morphological features.
- Data Collection: Acquire 3D-OCT volumes from all inked margins of the specimen. Ensure that image data is saved with filenames that encode the specimen orientation and location.
C. Image Analysis and Interpretation
- Qualitative Assessment: Trained readers evaluate OCT images for characteristic features of tumor tissue:
- Normal Breast Tissue: Dominated by large, dark, oval structures (adipocytes) with low signal heterogeneity.
- Tumor Tissue: Appears as a region of highly scattering tissue with a heterogeneous pattern. The organized architecture of normal breast structures is disrupted [49].
- Margin Classification: Based on the presence or absence of tumor features at the inked surface, classify the margin as:
- Negative: No tumor features within the imaging depth (1-2 mm).
- Close: Tumor features present within 1-2 mm of the surface, but not at the surface.
- Positive: Tumor features present at the specimen surface.
D. Validation with Histopathology
- Tissue Processing: After OCT imaging, place the specimen in 10% neutral-buffered formalin for fixation (minimum 24-48 hours).
- Sectioning and Staining: Process the specimen through standard paraffin embedding. Section the tissue at the locations co-registered with the OCT scans and stain with Hematoxylin and Eosin (H&E).
- Pathologist's Annotation: A certified pathologist should examine the H&E slides and annotate regions of cancer, benign tissue, and their distances from the margin.
- Co-registration and Data Analysis: Correlate OCT images with the corresponding histology slides. Calculate diagnostic performance metrics (sensitivity, specificity, accuracy) by comparing OCT-based margin calls with the histopathological gold standard.
Protocol 2: Dynamic OCT (d-OCT) for Enhanced Contrast
This protocol builds on the basic method by incorporating dynamic contrast, as described in recent technical advances [50].
A. Sample Preparation
- Follow steps in Protocol 1, Section A. For d-OCT, minimizing bulk tissue motion is critical. Compressing the specimen against an imaging window is highly recommended.
B. d-OCT Data Acquisition
- System Requirements: Use a Fourier-domain OCT system capable of high-speed, repeated scanning at a single location.
- Acquisition Parameters:
- Temporal Sampling: Acquire multiple repeated B-scans (e.g., 100-200) at each lateral location. The number of repetitions is a trade-off between motion contrast quality and total acquisition time.
- Temporal Resolution: Ensure the B-scan frame rate is sufficiently high (e.g., tens of Hz) to capture relevant tissue dynamics.
- Volume Acquisition: Perform this repeated scanning across a 3D grid to construct a 4D dataset (x, z, time).
C. Dynamic Signal Processing
- Time-Series Analysis: For each pixel in the 3D volume, a time-series of the complex OCT signal (intensity and phase) is obtained.
- Analysis Method Selection:
- Fourier Power Spectral Analysis: Transform the time-series into the frequency domain. The power in different frequency bands can be color-coded (e.g., using an RGB method) to visualize different dynamic components [50].
- Variance Analysis: Compute the temporal variance of the OCT signal (intensity or phase) to create a "dynamic" image where brightness corresponds to the degree of signal fluctuation.
- Image Visualization: Overlay the dynamic contrast image onto the standard OCT intensity image using a color map to provide complementary structural and functional information.
D. Interpretation of d-OCT Images
- Malignant Tissue: Typically exhibits higher and more heterogeneous dynamic signal compared to benign fibrous stroma and adipose tissue, likely due to different microenvironments and cellular densities [50].
Workflow Visualization
The following diagram illustrates the integrated experimental and clinical workflow for intraoperative OCT margin assessment.
Integrated Workflow for Intraoperative OCT Margin Assessment.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for OCT Margin Assessment Research
| Item | Specification / Example | Primary Function in Protocol |
|---|---|---|
| Spectral-Domain OCT System | e.g., Telesto 320 (Thorlabs); EX1301 (Michelson Diagnostics) | Core imaging hardware. Key specs: 1300 nm source, >5 µm axial resolution, kHz A-scan rate. |
| Broadband Light Source | Superluminescent Diode (SLD), ~1300 nm center, >90 nm bandwidth | Provides low-coherence light for high axial resolution. |
| Objective Lens | Achromatic lens, e.g., 60 mm focal length (LSM03, Thorlabs) | Focuses light onto the sample; determines lateral resolution and depth-of-field. |
| Line Scan Camera (InGaAs) | e.g., SU1024LE (Sensors Unlimited) | High-speed detection of interferometric signal in spectrometer. |
| Physiological Saline | 0.9% Sodium Chloride (NaCl), sterile | Hydrates excised tissue to prevent desiccation artifacts during imaging. |
| Histology Inks | Multi-colored tissue marking dyes (e.g., Davidson Marking System) | Specimen orientation and margin identification for co-registration. |
| Tissue Fixative | 10% Neutral Buffered Formalin | Fixes tissue post-imaging for standard histopathological processing. |
| H&E Staining Kit | Hematoxylin and Eosin solutions | Standard histological stain for validation of OCT findings. |
| AI/ML Software Platform | e.g., Python with TensorFlow/PyTorch; MATLAB | For developing custom CNNs for automated OCT image classification. |
OCT represents a transformative technology for intraoperative tumor margin assessment, offering the potential to significantly reduce re-excision rates and improve patient outcomes in oncologic surgery. Its core strengths lie in its real-time imaging capability, high resolution, and practical penetration depth. The integration of functional extensions like d-OCT and, most importantly, artificial intelligence, is rapidly advancing its diagnostic accuracy and operational utility. The protocols and data outlined in this application note provide a foundation for researchers and drug development professionals to further validate, optimize, and integrate this promising technology into the surgical workflow, ultimately guiding surgeons toward achieving complete cancer excision in a single procedure.
Application Notes: Optical Coherence Tomography for Cancer Diagnostics
Optical Coherence Tomography (OCT) has emerged as a transformative, high-resolution, non-invasive imaging technology for real-time in vivo cancer diagnostics. By utilizing low-coherence near-infrared light, OCT generates cross-sectional, micrometer-scale structural images of biological tissues, functioning as an "optical biopsy" [52] [26]. Its primary clinical value lies in its ability to visualize tissue microarchitecture without the need for physical excision, enabling immediate diagnostic assessment and guiding subsequent therapeutic interventions [53] [52]. This is particularly valuable for the early detection and characterization of epithelial cancers, which account for approximately 85% of all cancers [26].
The application of OCT in oncology focuses on three primary diagnostic pillars: detection, typing, and subtyping of malignant lesions. OCT facilitates the differentiation between major non-melanoma skin cancers, such as Basal Cell Carcinoma (BCC) and Cutaneous Squamous Cell Carcinoma (cSCC), by identifying their distinct morphological features in vivo [53] [54]. Furthermore, it enables the sub-classification of BCCs into superficial, nodular, and aggressive (micronodular, infiltrative) variants, which is critical for determining the most appropriate management strategy [55] [53]. The integration of artificial intelligence (AI), particularly deep learning algorithms, is advancing the field by enhancing the precision of OCT image interpretation for disease classification and margin detection [30] [52].
Table 1: Diagnostic Performance of OCT for Basal Cell Carcinoma (BCC)
| Diagnostic Metric | Performance Value | Context / Subtype |
|---|---|---|
| Overall Sensitivity | 96.8% | Facial BCC Detection [53] |
| Overall Specificity | 98.2% | Facial BCC Detection [53] |
| Overall Accuracy | 97.5% | Facial BCC Detection [53] |
| Area Under Curve (AUC) | 0.97 | Facial BCC Detection [53] |
| Subtyping Sensitivity | 93.1% | Superficial BCC [53] |
| Subtyping Sensitivity | 92.1% | Nodular BCC [53] |
| Subtyping Sensitivity | 89.3% | Micronodular BCC [53] |
| Subtyping Sensitivity | 90.0% | Infiltrative BCC [53] |
Table 2: Key OCT Diagnostic Features for Cancer Typing and Subtyping
| Cancer Type / Subtype | Characteristic OCT Features | Clinical Utility |
|---|---|---|
| Basal Cell Carcinoma (BCC) | Hyporeflective tumor nests and bundles, dark silhouettes, peritumoral clefting [53] | Distinguishing BCC from other skin malignancies. |
| Superficial BCC | Small, hyporeflective nests attached to the epidermis, confined to the upper dermis [53] | Guiding non-surgical topical therapies. |
| Nodular BCC | Large, well-circumscribed, round to oval hyporeflective nests in the dermis [55] [53] | Confirming diagnosis for surgical excision. |
| Infiltrative BCC | Thin, elongated, irregular hyporeflective strands infiltrating the dermis [53] | Identifying aggressive growth for wider excision. |
| Squamous Cell Carcinoma (SCC) | Altered epithelial architecture, disruption of layering, bright (hyperreflective) regions [54] | Differentiating SCC from BCC and benign lesions. |
Experimental Protocols
Protocol 1: Preoperative OCT for BCC Diagnosis and Subtyping
This protocol outlines the procedure for using OCT to non-invasively diagnose and subtype basal cell carcinomas prior to surgical intervention, based on a prospective diagnostic accuracy study [53].
2.1.1 Materials and Equipment
- VivoSight OCT system (or equivalent high-resolution dermatological OCT scanner)
- Computer workstation with OCT acquisition and analysis software
- Disposable probe covers or appropriate sterilization materials
- Ultrasound gel or similar immersion medium (if required by the device)
- Patient data management system for image archiving
2.1.2 Step-by-Step Procedure
- Patient Preparation and Positioning: Position the patient to ensure stability and easy access to the lesion. Cleanse the lesion and surrounding skin with alcohol to remove any oils or debris that might interfere with imaging. Ensure the area is dry before proceeding.
- System Calibration and Setup: Power on the OCT system and allow it to initialize. Perform any required system calibrations according to the manufacturer's instructions. Mount the sterile probe cover onto the imaging handpiece.
- Lesion Scanning:
- Gently place the OCT probe perpendicular to the skin surface, directly over the target lesion. Use a minimal amount of immersion fluid if needed to optimize optical coupling.
- Acquire comprehensive scans in a systematic raster pattern to cover the entire lesion and a 5 mm peripheral margin of clinically normal-appearing skin [53].
- Ensure imaging captures the epidermis, dermo-epidermal junction, and papillary dermis at a minimum. Acquire both cross-sectional (B-scans) and en face (C-scan) images.
- Maintain probe contact without applying significant pressure that could deform the underlying tissue architecture.
- Image Analysis and Interpretation:
- Review the acquired image stacks in real-time for quality and completeness.
- Identify key diagnostic features for BCC: hyporeflective tumor nests, dark silhouettes, and peritumoral clefting [53].
- Subtype the BCC based on nest morphology and distribution:
- Superficial BCC: Small nests connected to the epidermis.
- Nodular BCC: Large, well-defined round-to-oval nests in the dermis.
- Infiltrative/Micronodular BCC: Thin, elongated strands or small, sparse nests.
- Data Documentation and Reporting: Save all images and scans in the patient's electronic record. Generate a report detailing the presence/absence of BCC, the determined subtype, and measurements of tumor depth and lateral extent.
Protocol 2: Intraoperative Margin Assessment for Carcinomas
This protocol describes the use of OCT for real-time evaluation of resection margins during cancer surgery, helping to ensure complete tumor removal [52].
2.2.1 Materials and Equipment
- Portable or handheld OCT system suitable for intraoperative use
- Sterile surgical drapes for the device
- Biocompatible optical coupling gel
- Specimen mounting plate (for ex-vivo specimen scanning)
- Access to histopathology lab for standard frozen section correlation (if applicable)
2.2.2 Step-by-Step Procedure
- Pre-scanning Baseline: Before resection, use the OCT system to scan the visible tumor and establish a baseline of its architectural features in vivo.
- Tumor Resection: Perform the standard surgical resection of the primary tumor mass as planned.
- Margins Assessment:
- In Vivo Approach: Scan the surgical wound bed, focusing on the edges and deep margin. Systematically image the entire cavity surface to check for residual tumor islands [52].
- Ex Vivo Approach: Alternatively, place the freshly excised specimen on a mounting plate. Orient it and systematically scan all peripheral and deep margins of the specimen.
- Real-time Image Interpretation:
- Analyze the OCT images at the margins for the presence of residual hyporeflective nests (BCC) or disorganized, hyperreflective epithelial structures (SCC).
- Compare the architecture of the margin tissue to the baseline tumor scan and known features of normal skin.
- The goal is to identify any microscopic tumor extension that is not visibly apparent.
- Guided Re-excision: If OCT analysis suggests positive or close margins, mark the corresponding area in the wound bed. Proceed with a targeted re-excision of the specific involved area. Re-scan the new margin to confirm completeness of removal before closing the wound.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for OCT Cancer Diagnostics Research
| Item Name | Function / Application | Example / Specification |
|---|---|---|
| High-Resolution OCT Scanner | Core imaging device for in vivo tissue microarchitecture visualization. | VivoSight (Michelson Diagnostics) or VivaScope 1500 (Caliber ID) systems [55] [53]. |
| AI/Deep Learning Software | Automated image analysis for classification, segmentation, and margin detection. | Convolutional Neural Networks (CNNs) for OCT image analysis [30]. |
| Immersion Fluid | Optical coupling medium to minimize surface reflection and enhance image quality. | Ultrasound gel or specialized optical gel [53]. |
| Histopathology Consumables | Gold standard validation of OCT findings via tissue processing and staining. | 10% Buffered Formalin, Paraffin, H&E Stains [53] [54]. |
| RGB Subchannel Analysis Tool | Quantitative image analysis technique to decompose OCT signals for tissue characterization. | Software to separate green (cellular), blue (collagen), and red (high-intensity) channels [54]. |
Advanced optical imaging technologies are revolutionizing the monitoring of dynamic tumor responses to established cancer therapies. Optical coherence tomography (OCT) has emerged as a pivotal non-invasive modality for real-time, high-resolution imaging of tumor microstructural and microvascular changes during treatment [17] [56]. This Application Note details specialized protocols integrating OCT and complementary imaging technologies to quantify therapeutic efficacy across radiotherapy, chemotherapy, and photodynamic therapy (PDT). The procedures are framed within a comprehensive optical coherence tomography for cancer diagnostics research framework, providing researchers and drug development professionals with standardized methodologies for longitudinal tumor response assessment.
OCT in Radiotherapy Response Monitoring
Application Note
Radiotherapy induces complex structural and vascular changes in tumor tissue that can be quantitatively tracked using OCT. Line-field confocal optical coherence tomography (LC-OCT) enables detailed assessment of post-radiotherapy skin alterations, identification of residual tumor cells, and detection of recurrence without invasive biopsies [57]. Enhanced Depth Imaging (EDI) and Swept-Source OCT (SS-OCT) provide superior visualization of deep ocular structures, facilitating monitoring of radiation-induced complications such as capillary dropout and foveal avascular zone enlargement in ocular oncology [58].
Protocol: Longitudinal Monitoring of Radiation-Induced Vascular Changes
Purpose: To quantitatively monitor radiation-induced microvascular alterations in tumor tissue using OCT angiography (OCTA).
Materials & Equipment:
- Swept-source OCT system with angiography function
- Animal tumor model (e.g., murine xenograft)
- Radiation therapy system
- Image analysis software (e.g., MATLAB, FIJI/ImageJ)
Procedure:
- Pre-treatment Baseline Imaging: Anesthetize subject and acquire baseline OCTA scans (3×3 mm or 6×6 mm) of the target tumor region.
- Radiation Administration: Deliver prescribed radiation dose (e.g., 2-8 Gy) to tumor region using clinical radiotherapy system.
- Post-treatment Imaging Schedule: Acquire OCTA scans at 24h, 72h, 1 week, 2 weeks, and 4 weeks post-radiation using identical scan parameters to baseline.
- Image Analysis:
- Calculate vessel density (%) using automated thresholding and binarization algorithms
- Quantify foveal avascular zone (FAZ) area using manual or semi-automated segmentation
- Assess capillary dropout areas through inter-scan difference analysis
- Data Interpretation: Compare longitudinal vascular metrics to baseline; significant reduction in vessel density indicates positive vascular response to radiotherapy.
Research Reagent Solutions
Table: Essential Reagents for Radiotherapy Monitoring Studies
| Reagent/Equipment | Function | Application Example |
|---|---|---|
| Swept-Source OCT System | High-speed, deep-penetration imaging | Monitoring choroidal melanoma response to plaque brachytherapy [58] |
| Line-Field Confocal OCT (LC-OCT) | Cellular-level resolution imaging of skin | Detecting residual basal cell carcinoma post-radiotherapy [57] |
| Murine Xenograft Tumor Models | Preclinical therapeutic testing | Evaluating radiation dose response in patient-derived tumors [59] |
| Vessel Density Analysis Software | Quantification of vascular changes | Measuring radiation-induced capillary dropout in retinal vasculature [58] |
OCT in Chemotherapy Response Assessment
Application Note
OCT provides non-invasive, real-time monitoring of tumor response to chemotherapeutic agents through serial assessment of structural and functional changes. Nanoparticle-enhanced OCT improves visualization of tumor vasculature and drug distribution, while polarization-sensitive OCT detects subtle changes in tissue birefringence associated with early treatment response [56]. The integration of artificial intelligence with OCT imaging enables automated detection of chemotherapeutic response patterns that may be imperceptible to human observers [17].
Protocol: Nanoparticle-Enhanced OCT for Chemotherapy Monitoring
Purpose: To utilize gold nanoparticles as contrast agents for enhanced visualization of tumor vasculature and drug delivery during chemotherapy.
Materials & Equipment:
- Spectral-domain or swept-source OCT system
- Gold nanoshells or nanoparticles (50-150 nm)
- Chemotherapeutic agent (e.g., cisplatin, doxorubicin)
- Tumor-bearing animal model
- NIR fluorescent tags (optional)
Procedure:
- Nanoparticle Preparation: Synthesize or procure gold nanoparticles (∼100 nm) with surface modifications for tumor targeting.
- Agent Administration: Co-administer chemotherapy agent and gold nanoparticles intravenously via tail vein injection.
- Image Acquisition:
- Acquire pre-contrast OCT images of tumor region
- Perform serial OCT imaging at 5 min, 15 min, 30 min, 1h, 2h, 4h, and 24h post-injection
- Maintain consistent scan parameters and positioning across timepoints
- Image Analysis:
- Calculate contrast-to-noise ratio (CNR) in tumor vs. normal tissue
- Measure nanoparticle accumulation kinetics in tumor region
- Correlate nanoparticle distribution with therapeutic response
- Validation: Harvest tumors for histopathological correlation of OCT findings.
OCT in Photodynamic Therapy Monitoring
Application Note
Photodynamic therapy response is highly dependent on oxygen availability, requiring real-time monitoring of tumor oxygenation and vascular dynamics. Photoacoustic imaging (PAI) integrated with OCT provides complementary information on blood oxygen saturation (StO₂) and vascular morphology during PDT [59]. Low-dose PDT (L-PDT) promotes vascular E-selectin expression, enhancing CD8+ T-cell infiltration and improving tumor control, which can be monitored via OCT angiography [60].
Protocol: Real-Time Oxygenation Mapping During PDT
Purpose: To monitor heterogeneous tumor blood oxygenation dynamics during photodynamic therapy using integrated US-PAI and OCT.
Materials & Equipment:
- Combined US-PAI and OCT imaging system
- Photosensitizer (e.g., Benzoporphyrin derivative, BPD)
- PDT light delivery system
- Animal tumor model (e.g., FaDu head and neck cancer model)
- Hypoxia marker (e.g., Pimonidazole)
Procedure:
- Pre-treatment Setup:
- Anesthetize tumor-bearing subject
- Administer photosensitizer (e.g., 400 μg/kg Visudyne intravenously)
- Position integrated US-PAI/OCT transducer and PDT light delivery fibers
- Baseline Imaging: Acquire co-registered US-PAI StO₂ maps and OCT structural images
- PDT Administration: Deliver PDT light (e.g., 50 mW/cm², 10 J/cm²) while continuously monitoring with US-PAI/OCT
- Real-time Monitoring:
- Track spatial and temporal changes in StO₂ during light irradiation
- Identify regions of rapid oxygen consumption and reoxygenation
- Document vascular shutdown events
- Post-treatment Analysis:
- Correlate StO₂ dynamics with treatment outcome
- Map heterogeneous oxygen utilization across tumor regions
- Validate with immunohistochemistry for hypoxia and vascular markers
Table: OCT and PAI Parameters for Therapy Response Monitoring
| Therapy | Imaging Modality | Key Parameters | Response Indicators | Reference |
|---|---|---|---|---|
| Radiotherapy | OCT Angiography | Vessel density (%), FAZ area (mm²) | Capillary dropout >25%, FAZ enlargement >15% | [58] [57] |
| Chemotherapy | Nanoparticle-enhanced OCT | Contrast-to-noise ratio, Accumulation kinetics | Reduced CNR in responders, Altered kinetics | [17] [56] |
| Photodynamic Therapy | US-PAI/OCT | StO₂ (%), Oxygen consumption rate | StO₂ decrease >30% during PDT, Reoxygenation patterns | [59] |
| Immunotherapy | OCTA + Molecular Imaging | CD8+ T-cell infiltration, E-selectin expression | Increased vascular E-selectin, Enhanced T-cell recruitment | [60] |
Advanced Integration: AI-Enhanced OCT Analysis
Application Note
Artificial intelligence (AI) algorithms, particularly deep learning networks, significantly enhance OCT data analysis by automating tumor response assessment and identifying subtle patterns indicative of treatment efficacy [17]. Convolutional neural networks (CNNs) can classify OCT images to distinguish responding from non-responding tumors with reported accuracy exceeding 99% in validation datasets [61]. AI-powered OCT systems enable real-time intraoperative feedback and precise tumor margin delineation.
Protocol: AI-Assisted OCT Analysis for Treatment Response Classification
Purpose: To implement deep learning algorithms for automated classification of tumor response to therapy using OCT imaging data.
Materials & Equipment:
- OCT image dataset (pre- and post-treatment)
- Deep learning framework (e.g., TensorFlow, PyTorch)
- High-performance computing workstation with GPU
- Pre-trained CNN architectures (EfficientNet, ResNet)
Procedure:
- Dataset Preparation:
- Curate labeled OCT dataset with response classifications (responder/non-responder)
- Apply data augmentation (rotation, flipping, brightness adjustment)
- Split data into training (70%), validation (15%), and test (15%) sets
- Model Training:
- Initialize with pre-trained CNN weights (ImageNet)
- Fine-tune final layers on OCT dataset
- Optimize hyperparameters using validation set performance
- Model Validation:
- Evaluate on held-out test set
- Calculate performance metrics (accuracy, sensitivity, specificity, AUC)
- Implement cross-validation for robustness assessment
- Clinical Implementation:
- Integrate optimized model into clinical workflow
- Provide real-time response predictions during OCT imaging
- Continuously update model with new data
Research Reagent Solutions
Table: Advanced Imaging and Analysis Tools
| Technology | Function | Specifications/Applications |
|---|---|---|
| AI-OCT Integration | Automated tumor response classification | EfficientNet/ResNet architectures >99% accuracy in validation datasets [61] |
| PS-OCT (Polarization-Sensitive OCT) | Detection of tissue birefringence changes | Identifying early treatment-induced collagen remodeling [56] |
| Combined US-PAI/OCT | Simultaneous structural and oxygenation imaging | Real-time StO₂ monitoring during PDT [59] |
| Nanoparticle Contrast Agents | Enhanced vascular visualization | Gold nanoshells (50-150 nm) for improved OCT contrast [56] |
The integration of advanced OCT technologies with complementary imaging modalities provides powerful tools for monitoring dynamic tumor responses to radiotherapy, chemotherapy, and photodynamic therapy. The protocols detailed in this Application Note enable researchers to quantitatively assess therapeutic efficacy through microstructural and microvascular changes, oxygenation dynamics, and cellular infiltration patterns. The addition of AI-enhanced analysis further strengthens the capability to detect subtle response patterns and predict treatment outcomes. These standardized methodologies support the ongoing advancement of optical coherence tomography for cancer diagnostics research, facilitating more precise and personalized cancer therapy monitoring.
Optical Coherence Tomography (OCT) has emerged as an indispensable medical imaging technology, providing high-resolution, cross-sectional images of biological tissues at the micrometer scale in real-time and without invasive procedures [17]. The integration of Artificial Intelligence (AI), particularly through deep learning, is now revolutionizing OCT capabilities, transforming it from a diagnostic imaging tool into an intelligent system for automated analysis in oncology [17] [30]. This transformation addresses critical limitations in traditional OCT interpretation, including the complexity of image analysis, inter-observer variability, and the substantial time required for expert review [17].
AI-augmented OCT systems leverage convolutional neural networks (CNNs) and other deep learning architectures to extract complex patterns and biomarkers from imaging data that may be imperceptible to the human eye [17]. This capability is particularly valuable in oncology, where early detection and precise margin delineation are critical for successful cancer treatment [17] [62]. The synergy between AI and OCT enables faster, more accurate, and more consistent diagnoses while potentially reducing the need for invasive procedures like biopsies [17] [30].
AI-OCT Applications in Oncology: Quantitative Performance
Research demonstrates the effective application of AI-enhanced OCT across various cancer types. The table below summarizes key quantitative findings from recent studies.
Table 1: Performance Metrics of AI-OCT Systems in Cancer Diagnostics
| Cancer Type | AI Application | Key Performance Metrics | Reference |
|---|---|---|---|
| Skin Cancer (Nonmelanoma) | Classification of basal cell carcinoma and squamous cell carcinoma using dual-mode OCT and Raman spectroscopy | 95% accuracy for BCC; 92% accuracy when both cancer types included | [62] |
| Epithelial Cancers (e.g., oral, gastrointestinal) | AI-driven detection and classification of cancerous tissues | High-resolution imaging of superficial layers for early cancer identification | [17] |
| Surgical Oncology | Real-time tumor margin delineation using AI-OCT systems | Enabled surgeons to pinpoint tumor margins to decrease residual malignant tissue | [17] |
| Dermatological Cancers | Detection of basal cell carcinoma, squamous cell carcinoma, and melanoma through structural abnormalities | Non-invasive examination minimizing unnecessary biopsy procedures | [17] |
Experimental Protocols for AI-OCT in Cancer Diagnostics
Protocol 1: Automated Classification of Skin Cancer Lesions
This protocol outlines the procedure for using AI-OCT to distinguish between different types of nonmelanoma skin cancers, specifically basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
Materials and Equipment:
- Line-field confocal OCT (LC-OCT) system
- Confocal Raman microspectroscopy attachment
- AI processing unit with deep learning capabilities
- Database for storing OCT images and chemical spectra
Procedure:
- Image Acquisition: Position the LC-OCT probe over the suspicious skin lesion to capture high-resolution, cellular-level images of the skin tissue [62].
- Targeted Spectroscopy: Apply confocal Raman microspectroscopy to gather chemical spectra from specific areas identified as suspicious in the OCT images [62].
- Data Collection: Compile over 1,300 chemical spectra from more than 330 skin cancer samples to create a robust training dataset [62].
- AI Model Training: Train a deep learning model to recognize patterns associated with cancerous tissues using both structural (OCT) and chemical (Raman) data [62].
- Validation: Test the AI model on new, unseen data to evaluate its classification accuracy for BCC and SCC [62].
Expected Outcomes: The AI model should achieve approximately 95% accuracy for BCC classification and 92% accuracy when classifying both BCC and SCC, leveraging distinct chemical differences between cancer types [62].
Protocol 2: Automated Segmentation of Retinal Layers for Cancer-Associated Retinopathy
While primarily used in ophthalmology, this protocol has relevance for detecting cancer-associated retinopathy, where retinal changes may signal systemic malignancies.
Materials and Equipment:
- Spectral-domain OCT or Swept-source OCT system
- Computing workstation with adequate processing power
- Implementation of improved Canny operator algorithm
- Ground truth manual segmentations for validation
Procedure:
- Image Acquisition: Obtain cross-sectional OCT images of the retina centered at the macula [63].
- Image Enhancement:
- Apply denoising filters to reduce noise interference
- Calculate gradient maps using adjusted convolution kernels
- Perform non-maximum suppression to thin edges [63]
- Boundary Search:
- Select multiple gradient peak points as seed points
- Search for retinal boundaries and superimpose obtained boundaries
- Convert the number of superposed boundaries into probabilities [63]
- Boundary Selection:
- Apply double threshold method to select and connect edges
- Identify eleven distinct retinal boundaries without A-lines alignment [63]
- Validation: Compare automated segmentation results with manual segmentation by ophthalmologists, expecting average differences of 2-6 microns for healthy subjects and 3-10 microns for patients with pathology [63].
Expected Outcomes: The algorithm should achieve 98% "perfect segmentation" and "good segmentation" in healthy subjects and 94% in patients with retinal pathology, providing reliable boundary detection despite vascular shadows or noise interference [63].
Protocol 3: Biomarker Discovery for Neovascularization Detection
This protocol focuses on identifying vascular biomarkers for cancer detection using OCT angiography (OCTA), particularly for detecting neovascularization associated with diabetic retinopathy and age-related macular degeneration, with applications in oncology angiogenesis research.
Materials and Equipment:
- OCTA system with split-spectrum amplitude-decorrelation angiography (SSADA) algorithm
- Ultra-wide-field OCTA capability (optional)
- Automated quantification software for vascular parameters
- Database for longitudinal tracking of vascular changes
Procedure:
- OCTA Image Acquisition: Acquire volumetric OCTA data of the region of interest using standardized scan patterns (3mm²-12mm²) [64] [65].
- Image Segmentation: Segment the resulting image into four zones: superficial retinal plexus, deep retinal plexus, outer retina, and choriocapillaris (for ophthalmic applications) [65].
- Neovascularization Detection:
- Quantitative Analysis:
- AI-Enhanced Classification: Implement deep learning models, particularly CNNs, to classify neovascularization and distinguish true NV from mimics like IRMA and microaneurysms [64].
Expected Outcomes: Reliable detection of neovascularization patterns that serve as biomarkers for disease progression, with OCTA demonstrating high detection rates across vascular layers [64].
Workflow Visualization
Diagram 1: AI-OCT Integrated Workflow. This diagram illustrates the comprehensive pipeline from image acquisition to clinical decision support, highlighting the three primary AI analysis pathways.
Diagram 2: Deep Learning Feature Extraction. This diagram shows how CNNs process OCT images to extract diverse features for tissue classification and margin delineation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Materials for AI-OCT Development
| Item | Function/Application | Specifications |
|---|---|---|
| SD-OCT System | Spectral-domain OCT imaging for standard resolution applications | Center wavelength ~840 nm, spectrometer detector [65] |
| SS-OCT System | Swept-source OCT for enhanced imaging depth and speed | Center wavelength ~1050 nm, single photodiode detector [65] |
| Line-Field Confocal OCT | High-resolution cellular-level skin imaging | Combines confocal microscopy with OCT for dermatology [62] |
| OCT Angiography Module | Vascular imaging without dye injection | Uses SSADA algorithm for motion contrast [67] |
| Raman Microspectroscopy | Chemical composition analysis | Combined with OCT for dual-mode structural and chemical imaging [62] |
| CNN Software Framework | Deep learning implementation for image analysis | TensorFlow, PyTorch, or specialized medical imaging platforms |
| Annotation Software | Manual segmentation for training data generation | Supports precise boundary marking for retinal layers or tumors |
| High-Performance Computing | Processing large OCT datasets and AI training | GPU-accelerated workstations for efficient model development |
Future Perspectives
The future of AI-augmented OCT in oncology includes several promising directions. Full-field OCT (FF-OCT) technology will enable dynamic cell imaging with excellent resolution for detecting minor pathological cell alterations [17]. Visible light OCT represents another advancement, shifting the operating wavelength to allow high-resolution structural imaging along with retinal oximetry, measuring blood oxygen saturation down to the capillary level [24]. This enables noninvasive assessment of tissue metabolism, with vast implications for early cancer detection [24].
Multimodal imaging approaches that combine OCT with complementary techniques like photoacoustic imaging, optical coherence elastography, and confocal Raman microspectroscopy will provide more comprehensive tissue characterization [66] [62]. These integrated systems capture both structural and molecular information, offering new insights into cancer development and behavior [62].
Explainable AI will become increasingly important as these systems move toward clinical implementation, helping build trust in AI decisions among clinicians [17]. Future research must also address challenges related to model optimization, dataset biases, and seamless integration into clinical workflows to realize the full potential of AI-OCT in cancer diagnostics [30].
Overcoming Clinical Hurdles: Technical Limitations and Optimization Strategies for OCT
The penetration depth of optical coherence tomography (OCT), typically limited to 1-2 millimeters in biological tissues, represents a fundamental constraint for its application in cancer diagnostics and deeper tissue interrogation. This limitation arises primarily from the scattering and absorption of light within tissue, which degrades signal quality at greater depths [68]. In the context of oncology, where tumors often reside beneath the surface, this constraint can hinder early detection and comprehensive characterization. This Application Note details current engineered and computational strategies designed to overcome this barrier, thereby expanding OCT's utility for researchers and drug development professionals working in cancer diagnostics.
Technical Strategies for Enhanced Penetration
Multiple technical approaches have been developed to enhance OCT's imaging depth. The following table summarizes the core principles, key features, and primary applications of three prominent strategies.
Table 1: Technical Strategies for Enhancing OCT Penetration Depth
| Strategy | Core Principle | Key Features | Reported Performance | Relevance to Cancer Diagnostics |
|---|---|---|---|---|
| Chromatic OCT [32] | Leverages a broad bandwidth light source and high-NA optics with a pronounced chromatic focal shift to extend depth of focus. | - Isotropic resolution of 2-3 µm- Sevenfold DOF extension vs. conventional OCT- Novel noise-gating algorithm suppresses artifacts | DOF of ~475 µm (vs. 53.1 µm in conventional OCT); Enhanced SNR via noise gating | High-resolution imaging of deep tumor margins and microvascular structures. |
| Visible-light OCT (vis-OCT) [69] | Uses shorter wavelengths in the visible spectrum (535–700 nm) to achieve superior resolution and leverage hemoglobin absorption. | - Axial resolution of ~0.6 µm in tissue- Enables spectroscopic analysis (e.g., oximetry)- Enhanced superficial contrast | Axial resolution <1 µm; Improved contrast for superficial microvasculature | Early detection of superficial cancers (e.g., skin, oral) and metabolic imaging. |
| Optical Clearing Agents (OCAs) [68] | Topical application of agents to reduce refractive index mismatch between tissue components, reducing scattering. | - Use of FDA-approved absorbing dyes (e.g., Tartrazine, 4-Amino-antipyrine)- Reversible and suitable for in vivo use | "Significantly improved" penetration depth in mouse skin models | Improving imaging of skin cancers and assessment of tumor margins in vivo. |
Experimental Protocol: Enhancing Penetration with Optical Clearing Agents
The following protocol details the methodology for using absorbing dyes as OCAs to enhance OCT penetration depth in vivo, based on a study using mouse abdominal skin [68].
Research Reagent Solutions
Table 2: Essential Materials for OCA-Enhanced OCT Imaging
| Item | Specification/Function |
|---|---|
| Absorbing Dye | Tartrazine (428 nm peak) or 4-Amino-antipyrine (380 nm peak). Reduces scattering by increasing the refractive index of aqueous tissue components [68]. |
| Agarose | Low melting temperature. Used as a gel matrix for topical dye application. |
| Phosphate Buffered Saline (PBS) | 1X solution. Solvent for dissolving dye powder. |
| Animal Model | Pigmented (e.g., C57BL/6) and non-pigmented (e.g., CD-1) mice. Allows evaluation of efficacy across skin types. |
| OCT Imaging System | Commercial or custom system (e.g., spectral-domain OCT at 840 nm center wavelength). |
Step-by-Step Procedure
- Animal Preparation: Anesthetize the mouse using an approved protocol (e.g., 5% isoflurane with oxygen). Shave the abdominal area and apply a depilatory cream (e.g., Nair) for 5 minutes to remove remaining fur. Thoroughly clean the area with isopropyl alcohol pads [68].
- Dye-Gel Preparation:
- Dissolve the dye powder in 1X PBS to achieve a high concentration (e.g., 38% w/w for 4-Amino-antipyrine or 30% w/w for Tartrazine).
- Pre-heat the dye solution in an 80°C water bath.
- Combine the pre-heated dye solution with low-melting-temperature agarose to reach a final agarose concentration of 10 mg/mL.
- Remove the solution from the bath and cool it in a 4°C refrigerator for approximately 10 minutes until it forms a stable gel [68].
- Topical Dye Application:
- Optionally, mix the dye gel with fine pumice particles to create a mild abrasive paste.
- Apply a thin coating of the gel (or paste) to the prepared skin and massage gently with a cotton tip applicator for 10 minutes, or until the skin color changes.
- If paste was used, wipe away the pumice particles. Apply the pure dye gel for an additional 3-5 minutes until maximum tissue transparency is visually achieved [68].
- OCT Image Acquisition: Perform OCT imaging of the treated area using standard B-scan acquisition protocols. Ensure system parameters (e.g., wavelength, power, A-scan rate) are documented.
- Post-Imaging Care: After imaging, gently rinse the skin with warm saline or water until the skin returns to its normal color. Apply an antibiotic ointment (e.g., Neosporin) to prevent infection [68].
Workflow Visualization
Computational & AI-Driven Approaches
Beyond hardware and chemical methods, computational strategies play a crucial role in extracting more information from the detected signal, effectively enhancing usable penetration.
- Noise-Gating Algorithms: The Chromatic Gating (ChG) algorithm developed for chromatic OCT acts as a depth-dependent spectral filter. By applying a Gaussian window that shifts according to the frequency of harmonics, it selectively uses in-focus wavenumber regions for image reconstruction. This suppresses system-inherent noise, sidelobe artifacts, and multiple scattering effects, leading to a significant enhancement in the signal-to-noise ratio (SNR) at depth [32].
- Artificial Intelligence (AI): Deep learning models are being applied to improve OCT image quality and interpretation. AI can enhance image resolution, reduce noise, and assist in segmenting features at deeper layers that may be challenging to visualize with conventional processing. These models can also help classify pathological conditions by identifying complex, sub-visual patterns in OCT data, which is particularly valuable for cancer diagnostics [17].
The penetration depth limitation of OCT is being successfully addressed through a multi-faceted arsenal of strategies. Technical innovations like chromatic OCT and vis-OCT push the boundaries of resolution and depth of focus, while the use of optical clearing agents provides a practical method for enhancing depth in accessible tissues. Furthermore, advanced computational algorithms and AI work to maximize the information extracted from every photon detected. For researchers in cancer diagnostics, the integration of these strategies enables deeper, higher-resolution, and more informative tissue interrogation, positioning OCT as an increasingly powerful tool for early detection and study of cancer.
Optical Coherence Tomography (OCT) provides high-resolution, cross-sectional, and non-invasive imaging based on the back-scattering of near-infrared light, enabling real-time visualization of tissue microanatomy. Its application in cancer diagnostics, particularly for oral squamous cell carcinoma (OSCC) and oral potentially malignant disorders (OPMDs), shows significant promise for improving early detection and guiding surgical resections. However, the transition of OCT from a research tool to a reliable clinical modality faces substantial hurdles. The inherent operator dependency of image acquisition and the lack of standardized methodologies for image interpretation compromise the reproducibility of findings, creating critical barriers to its widespread adoption and validation in oncology research and drug development.
Quantitative Data on Standardization Challenges
Table 1: Key Challenges in OCT Standardization and Reproducibility
| Challenge Category | Specific Issue | Quantitative/Qualitative Impact | Primary Source |
|---|---|---|---|
| Interpretation Heterogeneity | Lack of standardized nomenclature and annotation | Consensus reached for only 31 of 45 initial terms for anterior-segment OCT structures; absence of consensus for less accessible areas [70]. | APOSTEL-AS Panel Consensus [70] |
| Operator Dependency | Manual interpretation and analysis | Time-consuming; susceptible to intra-observer and inter-observer variability [71]. | Garg et al. [71] |
| Algorithm & Sample Variability | Impact of sample preparation on AI diagnostics | Machine learning algorithms for resection margins are "significantly affected by sample extension and preparation" [72]. | Critical Review on OCT [72] |
| Reproducibility of AI Software | Variation in plaque composition measurements | Good inter-catheter and intra-software correlation demonstrated; absolute mean differences for various plaque characteristics were small (e.g., -0.02% to 0.12%) [71]. | Garg et al. [71] |
Experimental Protocols for Assessing Reproducibility
This section outlines a detailed protocol, modeled on a coronary atherosclerosis study [71], for evaluating the reproducibility of an automated AI-OCT analysis software in a cancer context.
Protocol: Reproducibility Assessment of AI-OCT Software for Tissue Characterization
1. Objective: To determine the inter-catheter and intra-software reproducibility of an automated AI-OCT software for quantifying tissue characteristics (e.g., dysplasia, carcinoma) in a longitudinal study design.
2. Materials and Reagents:
- OCT Imaging System: A spectral-domain (SD-OCT) or swept-source (SS-OCT) system suitable for the target tissue (e.g., oral mucosa).
- OCT Catheters/Probes: At least two different models of OCT imaging catheters or probes compatible with the system.
- AI-OCT Analysis Software: The automated software to be validated (e.g., software for delineating dysplastic regions, tumor borders, or specific tissue microstructures).
- Sample Cohort: Human or animal model tissue samples with confirmed pathologies (e.g., OSCC, OPMDs).
- Annotation Software: For manual region-of-interest (ROI) segmentation by expert analysts.
3. Methodology:
- 3.1. Study Design:
- A paired imaging study is conducted where the same set of tissue samples is imaged using two different OCT catheters within a short timeframe (e.g., 24 hours) to minimize biological variation.
- A subset of samples is re-analyzed by the same AI software at a different time point to assess intra-software variability.
3.2. Image Acquisition:
- Acquire volumetric OCT scans of pre-defined ROIs on each sample using the first catheter (Catheter A).
- Repeat the imaging process for the same ROIs using the second catheter (Catheter B), ensuring identical positioning.
3.3. Image Analysis:
- Process all acquired OCT scans through the AI-OCT software to obtain quantitative measurements of key tissue characteristics (e.g., epithelial thickness, detection of basal membrane disruption, optical attenuation coefficient).
- For the re-analysis subset, re-run the same scans through the software in a new session.
3.4. Data Analysis:
- Statistical Comparison: Use paired t-tests or Wilcoxon signed-rank tests to compare measurements from Catheter A vs. Catheter B (inter-catheter) and from first vs. second analysis (intra-software).
- Correlation Analysis: Calculate intraclass correlation coefficients (ICC) to assess reliability.
- Agreement Assessment: Generate Bland-Altman plots to visualize the limits of agreement between the two measurements.
4. Expected Outcomes:
- Narrow limits of agreement on Bland-Altman plots for both inter-catheter and intra-software comparisons.
- High ICC values (>0.9) indicating excellent reliability.
- Small absolute mean differences in quantified tissue characteristics, demonstrating that the software's measurements are reproducible despite changes in hardware or analysis session.
Standardization Framework and Nomenclature
Addressing the "significant heterogeneity in the methodologies used to interpret OCT data" [72] requires a foundational effort in standardizing terminology. A recent international, multidisciplinary consensus exercise (the APOSTEL-AS Panel) provides a model for this process [70].
Protocol: Consensus-Building for OCT Nomenclature in Oncology
1. Objective: To develop a consensus-based nomenclature for annotating normal and pathological tissue structures in OCT images relevant to oncology (e.g., oral mucosa, skin, gastrointestinal tract).
2. Materials:
- OCT Image Database: A curated set of high-quality, cross-sectional OCT images from healthy and diseased tissues.
- Annotation Platform: Software that allows experts to label structures on OCT images.
- Histopathological Correlation: Corresponding histology images for the OCT scans, where ethically and practically feasible.
3. Methodology:
- 3.1. Expert Panel Assembly: Convene a multinational panel of domain experts, including oncologists, pathologists, OCT imaging scientists, and drug development professionals.
- 3.2. Scoping Review: Conduct a literature review to identify all terms currently in use for describing OCT features in the target tissue.
- 3.3. Anonymous Voting (Delphi Method):
- Round 1: Present experts with unannotated images and the list of compiled terms. Experts propose annotations for key landmarks.
- Round 2+: Share the aggregated, anonymized results from the previous round. Experts re-vote on terms and definitions. The process iterates until consensus (e.g., ≥80% agreement) is reached for each term.
- 3.4. Annotation and Publication: Create a definitive set of annotated reference images using the agreed-upon nomenclature. Publish the consensus guidelines.
4. Application Notes:
- The consensus should prioritize descriptive anatomical terms from standard anatomical terminologies (e.g., FCAT) while acknowledging established eponymous terms where necessary [70].
- This protocol can be adapted for specific cancer types (e.g., OSCC, cervical cancer) to create disease-specific lexicons.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Tools for Standardized OCT Cancer Diagnostics
| Item | Function/Description | Application Note |
|---|---|---|
| Swept-Source OCT (SS-OCT) | Uses a tunable laser source; offers high imaging speed and depth, suitable for thicker samples like tumor spheroids [35]. | Ideal for 3D dynamic contrast imaging; axial resolution ~10 μm may limit subcellular detail [35]. |
| Spectral-Domain OCT (SD-OCT) | Uses a broadband light source and spectrometer; provides high axial resolution (~1-2 μm) for layered structures [35]. | Well-suited for imaging layered tissues like oral mucosa and for high-resolution DyC-OCT [72] [35]. |
| Full-Field OCT (FF-OCT) | Generates en-face images using a 2D camera; delivers high isotropic resolution (~1 μm) for cellular imaging [35]. | Best for thin samples (e.g., explants, organoids); penetration depth is limited in scattering tissues [35]. |
| Dynamic Contrast OCT (DyC-OCT) | A label-free technique that analyzes OCT signal fluctuations over time to create contrast-enhanced images of live cells [35]. | Can visualize cell morphology and monitor cellular activity/viability without stains [35]. |
| PyRadiomics Toolkit | A Python-based open-source platform for extracting high-throughput quantitative features from medical images [73]. | Enables radiomic analysis of OCT images to identify sub-visual patterns for predictive modeling [73]. |
| Automated AI-OCT Software | Software (e.g., OctPlus) for automated quantitative and qualitative analysis of OCT data, reducing observer variability [71]. | Crucial for achieving reproducibility in longitudinal studies; requires validation before clinical use [71]. |
Advanced Imaging and AI Integration
The integration of Artificial Intelligence (AI), particularly deep learning, presents a powerful solution to operator dependency. Foundation models (FMs) like MIRAGE, which are trained on vast, unlabeled datasets, have shown superior performance in ophthalmic OCT classification and segmentation tasks compared to models trained on limited annotated data [74]. This approach can be translated to oncology. Similarly, unsupervised machine learning applied to OCT radiomics can identify distinct patient clusters with differential treatment outcomes, revealing underlying disease heterogeneity without prior labels [73]. For instance, in diabetic macular edema, this method stratified patients into four clusters, one of which had a significantly lower incidence of recurrent disease (34.29% vs. higher rates in others) [73].
Application Notes: The Field of Low-Cost, Portable Optical Coherence Tomography
Market Context and Clinical Need
Table 1: Global Optical Coherence Tomography Market Outlook
| Metric | Value | Time Period | Source |
|---|---|---|---|
| Global OCT Market Size (2024) | USD 2.23 billion | 2024 | [75] |
| Projected Market Size (2034) | USD 9.79 billion | 2034 | [75] |
| Projected Compound Annual Growth Rate (CAGR) | 15.94% | 2025-2034 | [75] |
| Cost of Commercial OCT Systems | \$40,000 - \$150,000 | - | [76] |
The high cost of commercial Optical Coherence Tomography (OCT) systems, often exceeding \$100,000, has significantly limited their adoption in low-resource settings and restricted their application outside traditional clinical environments like ophthalmology clinics [76]. This financial barrier is a critical concern in global health, where the burden of diseases such as cancer is rapidly rising. It is estimated that by 2030, over two-thirds of new cancer cases will occur in low- and middle-income countries (LMICs) [77]. The development of low-cost, portable OCT systems presents a transformative opportunity to decentralize cancer diagnostics, enabling early detection and point-of-care (POC) pathological assessment in regions with limited access to central laboratory infrastructure [78].
Technological Paradigms and Performance Trade-offs
Table 2: Comparison of OCT Modalities for Low-Cost Design
| OCT Modality | Operating Principle | Advantages | Drawbacks for Low-Cost Applications |
|---|---|---|---|
| Spectral-Domain OCT (SD-OCT) | Interference signal measured with a spectrometer and line-scan camera [76]. | - Superior imaging speed and sensitivity compared to TD-OCT [76].- Relies on simpler, more cost-effective broadband light sources [76].- Dominates the market (59.4% share in 2025) [79]. | - Complex spectrometer-based detection [76].- Suffers from 'mirror' artifacts and sensitivity roll-off [76]. |
| Swept-Source OCT (SS-OCT) | Rapidly tunable laser scans wavelengths; interference measured with a single photodetector [76]. | - Excellent performance with high speeds [76].- Enables deeper tissue imaging [79]. | - Reliance on expensive tunable laser sources [76].- Generally lower axial resolution and higher cost compared to SD-OCT for comparable performance [76]. |
The core strategy for cost reduction in OCT involves a system-level approach, prioritizing the use of commercial off-the-shelf components to avoid markup on custom assemblies [80]. Key innovations focus on the most expensive subsystems: the light source and the spectrometer. For instance, using a non-temperature controlled superluminescent diode (SLD) with background subtraction algorithms can mitigate cost without sacrificing core functionality [80]. Spectrometer design has been revolutionized by using tall-pixel CMOS sensors, which reduce sensitivity to misalignment, and 3D-printed housings to minimize manufacturing costs [76] [80].
The Scientist's Toolkit: Research Reagent Solutions for a Low-Cost OCT Setup
Table 3: Essential Components for a Low-Cost OCT System
| Component | Example Specification/Model | Function & Rationale for Low-Cost Design |
|---|---|---|
| Light Source | Non-temperature controlled, fiber-coupled SLD (e.g., Exalos BTF14); 840 nm center wavelength, 45 nm bandwidth [80]. | Provides the broadband light for interferometry. Omitting temperature control drastically reduces cost; intensity fluctuations are corrected via software [80]. |
| Spectrometer Detector | Tall-pixel CMOS line-scan camera (e.g., 2048 pixels, 14 μm x 200 μm pixel geometry) [80]. | The tall pixel geometry makes the system more tolerant to optical aberrations and misalignment, allowing the use of simpler, cheaper optics and 3D-printed housings [76] [80]. |
| Scanning Optics | Dual galvanometer mirrors [80]. | Provide fast and precise 2D beam steering for image formation. While MEMS mirrors are an alternative, galvanometers offer a reliable balance of performance and cost for many prototypes [80]. |
| Diffraction Grating | 1852 lines/mm transmission grating (e.g., LightSmyth T-1850-800s) [80]. | Disperses the broadband light in the spectrometer, allowing wavelength-dependent detection across the sensor array. |
| Optical Enclosure | 3D-printed housing (e.g., using materials like PLA or ABS) [76]. | Custom-designed housing protects the optical path. 3D printing enables rapid, low-cost prototyping and production, which is essential for cost-effective development [76]. |
Experimental Protocols
Protocol: Design and Assembly of a Low-Cost SD-OCT Spectrometer
This protocol outlines the steps for constructing a custom spectrometer, a critical component for a low-cost Spectral-Domain OCT (SD-OCT) system, based on demonstrated designs [76] [80].
I. Materials and Equipment
- Light Source: Fiber-coupled SLD (e.g., Exalos BTF14, 840 nm center wavelength, 45 nm FWHM bandwidth).
- Optical Components: Off-axis parabolic mirror, 1852 lines/mm transmission diffraction grating, achromatic doublet lenses (e.g., f=150 mm).
- Detector: Tall-pixel CMOS line-scan camera (e.g., 2048 pixels with 14 μm x 200 μm pixel size).
- Software: Optical design software (e.g., Zemax OpticStudio) for initial simulation.
- Hardware: 3D printer for producing the custom spectrometer housing and mounting fixtures.
II. Procedure
- Optical Simulation: a. Model the "mirror-grating-lens loop" configuration in optical design software. b. Optimize the layout to minimize spot size (aim for <10 μm RMS radius) at the detector plane across the desired bandwidth (e.g., 62 nm for half the sensor array) [80]. c. Confirm that the spot size is well within the pixel size of the chosen CMOS sensor to ensure good spectral resolution.
Housing Fabrication: a. Design a rigid enclosure that precisely positions all optical components based on the optimized simulation. b. Incorporate kinematic mounts or adjustable slots for critical components like the grating to allow for fine-tuning during assembly. c. 3D print the housing using a stable polymer material.
Spectrometer Assembly: a. Mount the optical components sequentially into the 3D-printed housing: i. Couple the input fiber to the system. ii. Position the off-axis parabolic mirror to collimate the beam. iii. Align the transmission grating to receive the collimated beam. iv. Place the achromatic doublets to focus the diffracted light onto the sensor. b. Secure the CMOS line-scan camera at the focal plane.
Alignment and Calibration: a. Use a known wavelength source (e.g., a laser) to verify the linear dispersion of the spectrometer across the sensor array. b. Correlate pixel index to wavelength using a calibration source with known spectral lines. c. The system should achieve a line rate of approximately 5-10 kHz, sufficient for in vivo imaging [80].
III. Data Analysis and Image Processing
- Acquire a background spectrum (without a sample) and subtract it from all subsequent measurements to correct for artifacts from the non-temperature controlled SLD and fixed-pattern noise [80].
- Process the spectral interferograms using standard Fourier-domain OCT processing: apply a k-linearization algorithm, apply a windowing function, and compute the Fast Fourier Transform (FFT) to generate depth profiles (A-scans) [76].
Protocol: Validation of System Performance for Pre-Cancerous Tissue Imaging
This protocol describes the methodology for benchmarking a low-cost OCT system against a commercial system, specifically in the context of detecting structural changes associated with early-stage cancer.
I. Materials
- Samples:
- Ex vivo tissue specimens (e.g., rodent models of epithelial cancer, human biopsy specimens if available).
- Tissue phantom with known optical properties and layered structure (e.g., tape phantom) [80].
- Equipment:
- Prototype low-cost OCT system.
- Commercial OCT system (e.g., a system from Wasatch Photonics, Heidelberg Engineering, or Zeiss) for comparison.
- Standard histology equipment for processing and staining (H&E) of tissue samples.
II. Procedure
- System Characterization: a. Axial Resolution: Measure the FWHM of the point spread function by imaging a mirror. A resolution of ~7.0 μm in air (comparable to commercial systems) is achievable [80]. b. Lateral Resolution: Measure the FWHM of the beam waist at the focus using a knife-edge or beam profiler. A target resolution of ~17.6 μm is viable for tissue imaging [80]. c. Imaging Depth: Determine the depth at which the signal drops to the noise floor in a scattering phantom. A depth of 2.0-2.8 mm is sufficient for many epithelial tissue applications [80]. d. Signal-to-Noise Ratio (SNR): Calculate the SNR from a single A-scan peak from a mirror.
Tissue Imaging and Correlation with Histology: a. Image the ex vivo tissue specimens with both the low-cost OCT system and the commercial system. Acquire B-scans (cross-sections) over the same region of interest. b. Mark the imaged area with tissue dye for precise registration. c. Process the tissue for standard histology (fixation, embedding, sectioning, H&E staining). d. Have a trained pathologist evaluate the H&E-stained sections to identify regions of normal, pre-cancerous (dysplastic), and cancerous morphology.
Image Analysis and AI Integration: a. Co-register the OCT B-scans with the corresponding histology sections. b. Extract quantitative features from the OCT images, such as layer thickness, signal attenuation, and texture patterns. c. Train a convolutional neural network (CNN) to automatically classify OCT images into "normal" or "abnormal" (pre-cancerous/cancerous) categories based on the histology-confirmed ground truth [30]. This AI integration can standardize interpretation and assist non-specialist operators [75] [30].
III. Data Analysis
- Qualitatively compare the architectural features (e.g., epithelial stratification, integrity of the basement membrane, glandular organization) visible in the low-cost OCT images versus the commercial system.
- Quantitatively compare layer thicknesses and SNR measurements between the two systems.
- Report the sensitivity, specificity, and accuracy of the AI model for detecting pre-cancerous changes.
Workflow and System Integration Diagram
The following diagram illustrates the logical workflow and key design considerations for developing a low-cost, portable OCT system for global health applications.
Low-Cost Portable OCT Development Workflow
This workflow outlines the core design philosophy for creating accessible OCT systems, moving from technology selection through to clinical validation, with an emphasis on cost-saving hardware choices and point-of-care usability.
Optical Coherence Tomography (OCT) has emerged as a powerful, non-invasive imaging modality capable of providing high-resolution, cross-sectional, and three-dimensional images of biological tissues in real-time. Originally developed for retinal imaging, OCT's application has expanded into oncology, where it serves as a promising tool for cancer detection, biopsy guidance, and treatment monitoring [16]. Despite its advantages, which include micron-scale resolution (1-15 µm) and imaging depths of up to a few millimeters, conventional OCT suffers from a fundamental limitation: its contrast mechanism relies primarily on the backscattering of light, which offers limited molecular or functional specificity [81]. This lack of biochemical contrast makes it challenging to differentiate between malignant and benign lesions based solely on structural information and hinders the precise characterization of tumor margins and molecular phenotypes [16].
To overcome this limitation, two synergistic strategies have been developed. The first involves the use of exogenous contrast agents, particularly engineered nanoparticles, which can be designed to accumulate preferentially in tumor tissue. The second strategy is multimodal imaging, which combines OCT with complementary modalities like photoacoustic imaging (PAI) to provide co-registered structural, functional, and molecular data [82] [81]. This application note, framed within a broader thesis on advancing cancer diagnostics, details the protocols and methodologies for integrating nanoparticles and multimodal imaging with OCT to enhance its specificity for oncological research and drug development.
Protocol 1: Enhancing OCT Contrast with Targeted Nanoparticles
The functionalization of nanoparticles with targeting ligands enables their specific accumulation in tumor regions, enhancing OCT signal in areas of interest and providing molecular information.
Research Reagent Solutions
Table 1: Key Reagents for Nanoparticle-Enhanced OCT
| Reagent Category | Specific Examples | Function in Protocol |
|---|---|---|
| Nanoparticle Cores | Gold Nanospheres/Rods (AuNPs), Silica Nanoparticles, Superparamagnetic Iron Oxide Nanoparticles (SPIONs) | High-scattering or absorbing cores to enhance OCT signal [16] [83]. |
| Targeting Ligands | Antibodies (e.g., anti-EGFR), Peptides (e.g., RGD), Transferrin, Folic Acid | Mediate specific binding to overexpressed receptors on cancer cells [16] [83]. |
| Surface Coatings | Polyethylene Glycol (PEG), Poly(lactic-co-glycolic acid) (PLGA) | Improve biocompatibility, reduce opsonization, and prolong systemic circulation [84] [83]. |
| Characterization Tools | Dynamic Light Scattering (DLS), Zeta Potential Analyzer | Measure nanoparticle hydrodynamic size, distribution, and surface charge [84]. |
Experimental Workflow and Protocol
The following diagram outlines the complete workflow for preparing and applying targeted nanoparticles for OCT contrast enhancement:
Synthesis and Functionalization of Gold Nanoparticles (AuNPs)
- Objective: To synthesize spherical AuNPs of approximately 60 nm diameter and conjugate them with an anti-EGFR antibody for targeting squamous cell carcinoma.
- Materials: Hydrogen tetrachloroaurate(III) trihydrate, Trisodium citrate dihydrate, Methoxy-PEG-thiol, Anti-EGFR monoclonal antibody, Phosphate Buffered Saline (PBS), Dimethyl sulfoxide (DMSO).
- Procedure:
- Synthesis: Bring 100 mL of 1 mM HAuCl₄ solution to a rolling boil under reflux. Rapidly add 2.5 mL of 38.8 mM trisodium citrate solution. Continue heating and stirring until the solution turns deep red (≈15 minutes). Cool to room temperature [83].
- PEGylation: Add methoxy-PEG-thiol (5kDa) to the AuNP solution at a 10,000:1 molar ratio of PEG to AuNPs. Stir gently for 12 hours at room temperature. Purify via centrifugation (12,000 rpm, 20 minutes) and resuspend in PBS.
- Antibody Conjugation: Activate the PEGylated AuNPs with a heterobifunctional crosslinker (e.g., SMCC) according to the manufacturer's protocol. Incubate with anti-EGFR antibody (50 µg per mL of NP solution) for 2 hours at room temperature. Purify the conjugated AuNPs via centrifugation to remove unbound antibody [16] [83].
- Validation: Characterize the final product using DLS (size: 60-70 nm, PDI < 0.2) and UV-Vis spectroscopy (surface plasmon resonance peak ≈530 nm). The zeta potential should shift towards a slightly negative charge post-PEGylation and conjugation.
In Vivo Imaging Protocol
- Objective: To visualize the accumulation of targeted AuNPs in a murine model of head and neck cancer using a spectral-domain OCT system.
- Animal Model: Athymic nude mouse with a subcutaneously implanted HNSCC xenograft (tumor volume ≈150 mm³).
- Imaging Procedure:
- Baseline Scan: Anesthetize the mouse (e.g., using 2% isoflurane). Position the tumor region under the OCT probe. Acquire 3D-OCT volumes (e.g., 512 x 512 x 1024 pixels over a 2x2 mm area) [16].
- NP Administration: Administer the anti-EGFR-AuNPs intravenously via the tail vein (dose: 100 µL of 2.5 OD₅₂₀ nm solution).
- Longitudinal Imaging: Acquire 3D-OCT volumes at the same tumor location at post-injection time points (e.g., 1, 4, 12, and 24 hours).
- Data Analysis: Co-register pre- and post-injection OCT volumes. Calculate the normalized intensity increase, ∆I/I₀, within the tumor region of interest (ROI). The signal in the tumor region for targeted NPs is expected to be significantly higher than for non-targeted NPs at 4 and 12 hours [16].
Protocol 2: Integrating OCT with Photoacoustic Imaging (PAI)
The combination of OCT and PAI creates a powerful multimodal platform that overcomes the individual limitations of each technique.
Research Reagent Solutions
Table 2: Key Components for an OCT-PAI Multimodal System
| System Component | OCT Specifications | PAI Specifications | Integrated Function |
|---|---|---|---|
| Light Source | Broadband Superluminescent Diode (SLD), λ≈1300 nm [16] | Tunable Pulsed Laser, λ≈700-900 nm [85] | Provides light for deep-tissue scattering (OCT) and absorption (PAI). |
| Detection Unit | Spectrometer/Microphone | Ultrasound Transducer (e.g., 10-50 MHz) [85] | Detects backscattered light (OCT) and emitted acoustic waves (PAI). |
| Scanning System | Galvanometric Mirrors | Galvanometric Mirrors (co-aligned) | Enables co-registration of OCT and PAI imaging planes. |
| Contrast Agents | High-Scattering NPs (e.g., AuNPs) | High-Absorbing NPs (e.g., Gold Nanorods) [86] | Multi-functional NPs can provide contrast for both modalities. |
Multimodal System Workflow
The synergistic relationship and data flow in a combined OCT-PAI system are illustrated below:
Combined OCT-PAI Imaging of Tumor Vasculature and Hypoxia
- Objective: To simultaneously obtain the microvascular network architecture and hemoglobin oxygen saturation (sO₂) from a tumor model using a co-aligned OCT-PAI system.
- System Setup: Integrate a spectral-domain OCT engine (λ=1300 nm, axial resolution ≈5 µm) with a tunable optical parametric oscillator (OPO) laser (λ=700-900 nm, pulse duration ≈10 ns) for PAI. Co-align the beams using a dichroic mirror and scan with a shared pair of galvanometric mirrors. Use a 40 MHz central frequency ultrasound transducer for PAI signal detection [85] [86].
- Imaging Protocol:
- System Calibration: Precisely calibrate the spatial co-registration of the OCT and PAI imaging planes using a phantom containing absorbing and scattering features.
- Animal Preparation: Image an anesthetized mouse with a dorsal skinfold window chamber or a subcutaneous tumor.
- Multispectral PAI Data Acquisition: Acquire PAI data at multiple wavelengths (e.g., 750, 800, 850 nm) to spectrally unmask hemoglobin and deoxygenated hemoglobin [85].
- Synchronous OCT-PAI Scanning: Acquire OCT B-scans and PAI B-scans simultaneously from the same region. The OCT scan provides the structural context, while the multi-wavelength PAI data is used to calculate sO₂ maps.
- Data Analysis and Co-registration:
- OCT Angiography (OCTA): Generate microvasculature maps from the OCT data using speckle variance or decorrelation algorithms [35].
- PAI sO₂ Mapping: Calculate the relative concentrations of HbO₂ and Hb using the known absorption spectra and the measured PA signal intensities at different wavelengths. Compute sO₂ as HbO₂/(HbO₂ + Hb) [85].
- Image Fusion: Overlay the false-colored PAI sO₂ map onto the OCT/OCTA structural image using the pre-calibrated transformation matrix.
Supporting Data and Technical Validation
The efficacy of the described protocols is supported by quantitative data from the literature.
Table 3: Performance Metrics of Contrast-Enhanced and Multimodal OCT
| Imaging Technique | Key Metric | Reported Performance | Experimental Context |
|---|---|---|---|
| OCT + Targeted AuNPs | Signal Enhancement | >70% intensity increase in tumor ROI at 4h post-injection [16] | Murine model of oral cancer |
| OCT + Targeted AuNPs | Tumor-to-Background Ratio | ~3.5 for targeted NPs vs. ~1.5 for non-targeted NPs [16] | Murine model of oral cancer |
| OCT Angiography (OCTA) | Spatial Resolution | ~10-20 µm (lateral) [24] | Human retinal imaging |
| Photoacoustic Imaging (PAI) | Spatial Resolution | ~50-500 µm (lateral, depth-dependent) [85] | Human breast carcinoma |
| Spectroscopic PAI | sO₂ Measurement Accuracy | ±5% (relative values) [85] | Tumor hypoxia monitoring |
| Multimodal OCT-PAI | Co-registration Accuracy | <50 µm [81] | Preclinical system validation |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Core Reagents for Advanced OCT Cancer Imaging Research
| Item Name | Supplier Examples | Critical Function | Application Notes |
|---|---|---|---|
| Gold Nanorods (AuNRs) | NanoComposix, Sigma-Aldrich | PAI contrast agent; tunable absorption in NIR window [86] | Functionalize with PEG for stability; peak absorption ~800 nm for deep tissue. |
| PLGA-PEG-COOH Nanoparticles | PolySciotech, Sigma-Aldrich | Biodegradable polymer for drug delivery & imaging [84] [83] | Can be loaded with dyes or drugs; COOH group allows easy ligand conjugation. |
| Anti-EGFR Antibody | Abcam, BioLegend | Targeting ligand for epithelial cancers [16] | Use Fab fragments for potentially better tissue penetration. |
| RGD Peptide | Tocris Bioscience, MedChemExpress | Targets αvβ3 integrin on tumor vasculature [83] | Cyclic RGD often has higher affinity and stability. |
| Matrigel | Corning | Basement membrane matrix for 3D cell culture & organoids [35] | Essential for creating biologically relevant in vitro tumor models. |
| IVISense PA Imaging Agent | PerkinElmer | Commercially available NIR fluorescent/PA probe [86] | Useful for validating custom PAI agent performance and protocols. |
The integration of targeted nanoparticles and multimodal imaging, particularly with photoacoustics, decisively addresses the critical challenge of specificity in OCT for cancer diagnostics. The detailed protocols provided herein for functionalizing nanoparticles and operating a co-aligned OCT-PAI system empower researchers to extract rich, co-registered datasets that combine structural, molecular, and functional information. These advanced application notes provide a framework for leveraging these sophisticated tools, paving the way for more precise cancer detection, accurate margin assessment, and informed therapeutic monitoring in preclinical research. The continued development of intelligent nanoparticles and robust multimodal systems promises to further solidify the role of OCT in the future of precision oncology.
Application Note: The AI-OCT Paradigm in Oncology
The integration of Artificial Intelligence (AI) with Optical Coherence Tomography (OCT) is revolutionizing cancer diagnostics by addressing critical challenges of data overload and workflow inefficiency. OCT provides high-resolution, cross-sectional images of biological tissues at the micrometer scale in real-time and without invasive procedures, making it indispensable for detecting epithelial cancers such as skin, oral, and gastrointestinal cancers [17]. However, the traditional interpretation of substantial OCT imaging data demands specialized expertise, significant time investment, and often leads to diagnostic variability [17]. AI, particularly through deep learning (DL) and convolutional neural networks (CNNs), automates the analysis of OCT images, enabling faster, more accurate, and consistent diagnoses. This application note details how AI-driven OCT systems extract complex patterns and biomarkers imperceptible to the human eye, enhancing diagnostic precision for cancer, guiding surgical interventions, and ultimately improving patient outcomes by reducing the need for invasive biopsies [17].
Quantitative Landscape of AI-OCT Adoption
The growth of AI in OCT imaging is quantitatively demonstrated through bibliometric analysis and specific clinical performance metrics. The following tables summarize key data points.
Table 1: Bibliometric Analysis of AI in Ophthalmic OCT Research (2012-2023) [87]
| Metric Category | Specific Metric | Value or Finding |
|---|---|---|
| Publication Volume | Total Articles (2012-2023) | 877 |
| Annual Growth | Rapid growth post-2020, exceeding 200 articles in 2022 | |
| Geographic Leadership | Top Country by Publications | USA (261) |
| Top Country by H-index | USA (38) | |
| Top Country by Centrality | USA (0.33) | |
| Institutional Leadership | Leading Institution | University of London (58 publications) |
| Institution with Highest Centrality | University of California System (0.31) |
Table 2: Performance Metrics of AI-OCT in Clinical Applications
| Clinical Application | AI Model / Technology | Reported Performance / Outcome |
|---|---|---|
| Skin Cancer Diagnosis | AI model with LC-OCT and Raman microspectroscopy [62] | 95% accuracy for Basal Cell Carcinoma; 92% accuracy for combined skin cancers |
| General OCT Image Analysis | Deep Learning (DL) [87] | Shift in research focus from traditional ML to DL for automatic segmentation |
| Clinical Decision Support | AI-CDSS (Transparent, usable, reliable systems) [88] | Key enablers for healthcare worker trust and adoption |
AI-Driven Workflow Integration for Clinical Decision Support
The core solution to data overload lies in seamlessly integrating AI-OCT analysis into clinical workflows through AI-based Clinical Decision Support Systems (AI-CDSS). These systems act as virtual assistants, providing clinicians with actionable, evidence-based recommendations at the point of care [89]. The successful integration and adoption of these systems hinge on several key factors identified as critical for building trust among healthcare workers [88]:
- System Transparency: The AI's decision-making process must be clear and interpretable.
- Clinical Reliability: The system must demonstrate consistent accuracy and performance.
- System Usability: The AI must be effectively integrated into existing clinical workflows without causing disruption.
Protocol for Implementing an AI-OCT Analysis System
Experimental Workflow for AI-OCT Model Development and Validation
The following diagram outlines a generalized protocol for developing and validating an AI model for OCT image analysis in a cancer diagnostics context.
Step-by-Step Experimental Methodology
Phase 1: Data Curation and Preprocessing
- Image Acquisition: Acquire OCT volumes using clinical OCT systems. For cancer diagnostics, ensure imaging of confirmed cancerous, pre-cancerous, and healthy control tissues. The dataset should be large-scale (e.g., thousands of volumes) to reflect the "high-volume" challenge and empower DL models [17].
- Data Preprocessing:
- Quality Control: Manually or automatically exclude images with significant artifacts (e.g., motion blur, poor signal).
- Standardization: Normalize pixel intensity values across all images to a standard range (e.g., 0-1).
- Augmentation: Artificially expand the training dataset using techniques like rotation, flipping, and elastic deformations to improve model robustness.
Phase 2: Ground Truth Annotation and Dataset Construction
- Expert Annotation: Clinical experts (e.g., oncologists, dermatopathologists) should annotate OCT images. This involves delineating regions of interest (ROIs) such as tumor boundaries, specific tissue layers, or pathological features. This serves as the ground truth for supervised learning [17].
- Dataset Partitioning: Randomly split the annotated dataset into three subsets:
- Training Set (~70%): Used to train the AI model.
- Validation Set (~15%): Used to tune hyperparameters and monitor for overfitting during training.
- Test Set (~15%): Used only once for the final, unbiased evaluation of model performance.
Phase 3: AI Model Training and Validation
- Model Selection: Implement a Deep Learning architecture, typically a Convolutional Neural Network (CNN), which is the state-of-the-art for image analysis [17] [87]. Models like U-Net are suitable for segmentation tasks, while architectures like ResNet or DenseNet can be adapted for classification.
- Training Loop:
- Input preprocessed OCT images and their corresponding annotations into the model.
- Use an optimization algorithm (e.g., Adam) to minimize the difference between the model's predictions and the expert annotations (the loss function).
- Iterate for a sufficient number of epochs until validation loss stabilizes.
- Validation: Continuously evaluate the model on the validation set during training. Performance metrics (e.g., Dice coefficient for segmentation, Accuracy/AUC for classification) should be logged to guide hyperparameter tuning and prevent overfitting.
Phase 4: Blinded Testing and Clinical Workflow Integration
- Performance Evaluation: Execute a final evaluation on the held-out test set. Report standard metrics including Sensitivity, Specificity, Accuracy, and Area Under the Curve (AUC) to provide a comprehensive view of clinical utility [62].
- Integration as a CDSS: Deploy the validated model within a clinical software interface. The system should:
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Computational Tools for AI-OCT Development
| Item / Solution | Function / Description | Application in AI-OCT Protocol |
|---|---|---|
| High-Resolution OCT System | Generates the primary volumetric image data. Systems with line-field confocal (LC-OCT) capabilities can provide cellular-level resolution [62]. | Foundation for all data acquisition in Phase 1. |
| Annotation Software Platform | Software that allows clinical experts to digitally label and segment regions of interest on OCT images. | Critical for creating ground truth data in Phase 2. |
| Deep Learning Framework | Software libraries such as TensorFlow or PyTorch. | Provides the programming environment to build, train, and validate CNN models in Phase 3. |
| High-Performance Computing (HPC) Cluster | Computing resources with powerful GPUs (Graphics Processing Units). | Necessary to handle the computational load of training complex DL models on large OCT datasets in Phase 3. |
| Clinical Decision Support System (CDSS) Interface | A software platform that integrates the AI model into the clinical workflow, often part of the hospital's imaging or EHR systems [89]. | Enables the final deployment and real-world use of the developed model, as described in Phase 4. |
| Validation & Statistical Analysis Suite | Tools for calculating performance metrics (e.g., Dice coefficient, AUC) and performing statistical analysis. | Used in Phase 3 and 4 to objectively quantify and report the model's diagnostic performance. |
Validating Performance: Comparative Analysis of OCT Against Gold Standards and Competing Modalities
Within the context of a broader thesis on optical coherence tomography (OCT) for cancer diagnostics research, this document establishes detailed application notes and protocols for the critical process of benchmarking OCT technology against the gold standard of histopathology. The transition of OCT from an emerging imaging technique to a clinically validated tool for cancer detection and surgical guidance hinges on rigorous, quantitative comparison to traditional tissue analysis. This protocol provides researchers, scientists, and drug development professionals with a standardized framework for evaluating the diagnostic accuracy of OCT systems, focusing on key metrics such as sensitivity, specificity, and overall diagnostic concordance. By outlining specific methodologies for study design, data analysis, and interpretation, this document aims to ensure that validation studies are conducted with the highest level of scientific rigor, producing reliable and comparable data to support clinical translation and regulatory approval.
Quantitative Benchmarks from Meta-Analyses
A meta-analysis provides high-level evidence for the diagnostic performance of OCT by aggregating data from multiple studies. The following table summarizes key findings from a meta-analysis comparing OCT to Frozen Section (FS) analysis for assessing surgical margins during breast-conserving surgery [90].
Table 1: Diagnostic Performance of OCT vs. Frozen Section in Breast-Conserving Surgery Margin Assessment (Meta-Analysis)
| Imaging Modality | Sensitivity (95% CI) | Specificity (95% CI) | Number of Studies (Patients/Specimens) | Clinical Context |
|---|---|---|---|---|
| Optical Coherence Tomography | 0.93 (0.90 - 0.96) | 0.89 (0.83 - 0.94) | 16 studies (10,289 specimens) | Ex vivo margin assessment in breast-conserving surgery [90] |
| Frozen Section | 0.82 (0.71 - 0.92) | 0.97 (0.95 - 0.99) | 20 studies (8,058 patients) | Intraoperative margin assessment in breast-conserving surgery [90] |
This data demonstrates that OCT offers superior sensitivity compared to FS, making it highly effective at ruling out disease when a negative result is observed. However, FS currently holds an advantage in specificity, which reduces the number of false positives [90]. These metrics are crucial for researchers to consider when defining the clinical use case for an OCT system.
Furthermore, validation studies against histopathology in other anatomical contexts reinforce the value of OCT. For example, an ex vivo study of peripheral artery specimens using objective OCT image criteria reported high sensitivity and specificity for characterizing different plaque types compared to histopathology [91].
Table 2: OCT Performance for Characterifying Atherosclerotic Plaques in Peripheral Arteries
| Plaque Type | Sensitivity | Specificity |
|---|---|---|
| Fibrous Plaques | 86% | 86% |
| Lipid-Rich Plaques | 78% | 93% |
| Calcified Segments | 84% | 95% |
Experimental Protocol for Benchmarking OCT Against Histopathology
This protocol provides a detailed methodology for conducting a validation study to benchmark OCT image findings against histopathological diagnosis, the gold standard.
Phase 1: Specimen Preparation and Imaging
Objective: To acquire high-quality OCT images from tissue specimens with a precisely maintained orientation for accurate correlation with histology sections.
Materials:
- Fresh or properly fixed (e.g., 10% Neutral Buffered Formalin) tissue specimens from biopsy or resection.
- Optical Coherence Tomography system (e.g., frequency-domain OCT, full-field OCT).
- Tissue embedding medium (e.g., OCT compound for frozen sections, paraffin for permanent sections).
- Microtome or cryostat.
- Glass slides and coverslips.
- Histological stains (e.g., Hematoxylin and Eosin (H&E)).
Procedure:
- Tissue Preparation:
- Orient the tissue specimen and mark a reference surface with inert dye or a suture to ensure consistent spatial tracking between OCT imaging and histological processing.
- If using ex vivo specimens, gently wash with saline to remove residual blood or debris that may cause imaging artifacts [91].
- OCT Image Acquisition:
- Mount the specimen securely in the OCT sample holder to prevent motion artifacts.
- Acquire OCT cross-sectional images (B-scans) or three-dimensional volumetric scans (C-scans) of the region of interest. System parameters (e.g., wavelength, power, axial and lateral resolution) must be documented.
- For large specimens, systematically image the entire surface in a raster pattern, ensuring a small overlap between adjacent scans.
- Save the OCT data in a raw or standardized format (e.g., .TIFF, .DICOM) along with all acquisition metadata.
- Histological Processing:
- After OCT imaging, process the imaged tissue block for histology using standard protocols: dehydration, clearing, infiltration, and embedding in paraffin or freezing medium.
- Section the tissue block serially at a standard thickness (e.g., 4-5 µm) using a microtome. The first section should correspond as closely as possible to the plane of the OCT image.
- Mount tissue sections on glass slides and stain with H&E or other relevant stains (e.g., special stains, immunohistochemistry markers) [92].
- Digitize the stained slides using a whole-slide scanner to create high-resolution digital images for analysis [93].
Phase 2: Image Registration and Correlation
Objective: To establish a precise, point-to-point correspondence between the OCT image and the histopathology slide.
Procedure:
- Landmark Identification:
- Identify at least three distinct, recognizable anatomical landmarks (e.g., unique gland structures, blood vessels, tissue borders) in both the OCT image and the corresponding digitized histology slide.
- Image Co-Registration:
- Use image analysis software (e.g., ImageJ with registration plugins, MATLAB, or commercial digital pathology software) to perform rigid or non-rigid (elastic) image registration.
- The software will align the histology image to the OCT image using the identified landmarks, creating a fused image or a coordinate transformation map.
- Region of Interest (ROI) Definition:
- Based on the co-registered images, a certified pathologist will delineate specific ROIs on the histology slide. These ROIs should represent definitive pathological diagnoses (e.g., "normal mucosa," "invasive carcinoma," "dysplasia," "fibrous plaque," "lipid-rich plaque") [91].
- These annotated ROIs are then transferred to the exact corresponding locations on the co-registered OCT image using the transformation map.
Phase 3: Quantitative Analysis and Metric Calculation
Objective: To calculate standard diagnostic performance metrics by comparing OCT interpretations to the ground-truth histopathological diagnoses.
Procedure:
- Blinded Reading:
- The OCT images, with the transferred ROIs, are presented to one or more readers (e.g., scientists, clinicians) trained in OCT interpretation. The readers are blinded to the histopathological diagnosis.
- For each ROI, the reader classifies the OCT image based on predefined diagnostic criteria into one of the possible pathological states.
- Data Compilation:
- Compile the reader's classifications for all ROIs into a contingency table (2x2 table for binary outcomes) against the known histopathology truth.
- Metric Calculation:
- Calculate the following metrics for each diagnostic category and for the overall performance [90] [93]:
- Sensitivity: True Positives / (True Positives + False Negatives)
- Specificity: True Negatives / (True Negatives + False Positives)
- Diagnostic Accuracy: (True Positives + True Negatives) / Total Number of ROIs
- Area Under the Curve (AUC): Calculate by plotting the Receiver Operating Characteristic (ROC) curve, which graphs sensitivity against (1 - specificity) across different diagnostic thresholds.
- Calculate the following metrics for each diagnostic category and for the overall performance [90] [93]:
The workflow for the entire benchmarking protocol is summarized in the following diagram:
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and reagents essential for conducting the experiments described in this protocol.
Table 3: Essential Research Reagents and Materials for OCT-Histopathology Correlation Studies
| Item Name | Function/Application | Critical Notes |
|---|---|---|
| 10% Neutral Buffered Formalin | Tissue fixation to preserve morphology and prevent degradation. | Standardized fixation time is critical to avoid over-fixation, which can mask antigens for IHC [92]. |
| Hematoxylin and Eosin (H&E) Stain | Routine histochemical staining for general tissue morphology assessment. | Allows visualization of nuclear (blue) and cytoplasmic (pink) details; the primary stain for initial diagnosis [92]. |
| OCT Compound | Water-soluble embedding medium for freezing tissue specimens. | Used for preparing frozen sections, often employed in intraoperative settings. Do not confuse with Optical Coherence Tomography. |
| Paraffin Embedding Medium | Solid embedding medium for creating formalin-fixed, paraffin-embedded (FFPE) tissue blocks. | The standard for permanent histology sections; provides excellent morphological preservation [92]. |
| IHC Primary Antibodies & Detection Kits | Specific detection of protein biomarkers (e.g., PD-L1, Ki-67) via Immunohistochemistry. | Provides objective, quantitative data on biomarker expression; kits include secondary antibodies and chromogens (e.g., DAB) [92]. |
| Digital Whole-Slide Scanner | Digitizes glass histology slides to create high-resolution whole-slide images (WSIs). | Enables digital pathology workflows, image analysis, and easy archiving and sharing of slides [93]. |
Advanced Considerations: The Role of Artificial Intelligence
The integration of Artificial Intelligence (AI), particularly deep learning, is transforming the benchmarking of OCT. AI models, such as Convolutional Neural Networks (CNNs), can be trained to automatically extract features from OCT images that correlate with histopathological diagnoses [30] [17]. These models can enhance diagnostic accuracy by identifying subtle patterns imperceptible to the human eye. Furthermore, foundation models in computational pathology, trained on millions of whole-slide images, are demonstrating remarkable pan-cancer detection capabilities, achieving high specimen-level AUC (Area Under the Curve) values (e.g., 0.95) [94]. This suggests that AI can serve as a powerful intermediary, learning the complex mapping between OCT's microstructural data and the corresponding cellular pathology features seen in histology, thereby refining the benchmarking process itself.
Optical coherence tomography (OCT) has emerged as a powerful, non-invasive imaging technology for cancer diagnostics, providing high-resolution, cross-sectional images of biological tissues in real-time. This application note synthesizes recent clinical validation data and standardized protocols for utilizing OCT in the detection and margin assessment of skin, breast, and gastrointestinal malignancies, with a focus on translating research findings into actionable clinical workflows. The performance metrics outlined herein establish OCT as a complementary tool to histopathology, offering the distinct advantage of non-destructive, real-time tissue analysis.
Table 1: Diagnostic Performance of OCT Across Various Cancers
| Cancer Type | Application Context | Sensitivity (%) | Specificity (%) | Accuracy (%) | AUC | Evidence Level | Citation |
|---|---|---|---|---|---|---|---|
| Basal Cell Carcinoma (Skin) | Detection & Subtyping of Facial Lesions | 96.8 | 98.2 | 97.5 | 0.97 | Prospective Diagnostic Study (n=220 lesions) | [53] |
| Breast Cancer | Margin Assessment in Breast-Conserving Surgery | 91.0 (Pooled) | 88.0 (Pooled) | - | 0.94 (Pooled) | Systematic Review & Meta-Analysis | [47] |
| Lymph Node Metastases (Gynecological) | Detection of Metastases (≥0.2 mm) in Fresh ex vivo LNs | 92.3 | 98.2 | 97.6 | - | Prospective Observational Study (n=74 LNs) | [95] |
Table 2: Performance of OCT in Subtyping Basal Cell Carcinoma (BCC)
| BCC Subtype | Sensitivity (%) | Notable OCT Features |
|---|---|---|
| Superficial BCC | 93.1 | Hyporeflective nests confined to the upper dermis |
| Nodular BCC | 92.1 | Well-circumscribed, round nests with palisading edges |
| Infiltrative BCC | 90.0 | Thin, irregular hyporeflective strands infiltrating deeper dermis |
| Micronodular BCC | 89.3 | - |
Detailed Experimental Protocols
Protocol for Basal Cell Carcinoma Detection and Subtyping
This protocol is adapted from a prospective, single-center diagnostic accuracy study using in vivo OCT for facial BCCs, with histopathology as the gold standard [53].
1. Pre-Scanning Preparation:
- Patient Inclusion: Adult patients (≥18 years) with untreated, clinically suspicious facial lesions (e.g., pearly borders, telangiectasia, ulceration).
- Lesion Documentation: Record lesion characteristics and measure dimensions (length, width, height) using calibrated digital calipers.
- Equipment: VivoSight OCT system (Michelson Diagnostics) or equivalent high-resolution dermatological OCT. Ensure lateral resolution of ~7.5 μm and axial resolution of ~5 μm using a 1305 nm wavelength light source.
2. Imaging Procedure:
- Scanning Pattern: Systematically scan the lesion in the X-Y-Z axes to capture comprehensive three-dimensional data.
- Margin Assessment: Extend scanning approximately 5 mm beyond the clinically visible borders of the lesion to assess surrounding tissue and facilitate preoperative margin evaluation.
- Data Acquisition: Complete imaging within approximately 5 minutes per lesion. Acquire both en face and cross-sectional images of the epidermis, dermoepidermal junction (DEJ), and upper dermis.
3. Image Analysis Criteria:
- BCC Detection: Identify architectural disintegration at the DEJ and the presence of ovoid, hyporeflective structures corresponding to tumor nests.
- Subtyping:
- Superficial BCC: Look for hyporeflective nests attached to the epidermis or located in the superficial dermis.
- Nodular BCC: Identify large, well-defined, hyporeflective nodules often with peripheral palisading.
- Infiltrative/Micronodular BCC: Detect irregular, cord-like or small, hyporeflective nodules infiltrating the dermis.
4. Post-Scanning Validation:
- Surgically excise the lesion after imaging using standard margins.
- Process tissue for histopathological examination (H&E staining).
- Correlate OCT findings with histology results, ensuring pathologists are blinded to OCT data.
Protocol for Intraoperative Lymph Node Metastasis Detection
This protocol is based on a study evaluating full-field OCT (FF-OCT) for the rapid assessment of lymph node (LN) metastases in gynecological cancers [95].
1. Sample Collection and Preparation:
- Sample Source: Collect fresh ex vivo LNs from patients undergoing LN dissection for gynecological malignancies (e.g., endometrial, ovarian, cervical cancer).
- Tissue Preparation: Carefully free LN samples from surrounding adipose tissue. Slice the LN with a microtome and place it in a dedicated specimen container without any further tissue preparation (e.g., no fixation or staining).
2. FF-OCT Imaging:
- Equipment: CelTivity Biopsy System (AQUYRE Biosciences) or equivalent FF-OCT system featuring a Linnik interferometer.
- Image Acquisition: Perform "en face" image acquisition using a scanning unit of 1.24 mm × 1.24 mm. Combine sequential scans to create a larger field of view.
- Scanning Parameters: Acquire images at a depth of 15 μm. The process should be completed rapidly (within 2 seconds per scan unit), with total scanning time under 15 minutes per sample.
3. Image Interpretation:
- Normal LN Architecture: Identify round, nodular areas of homogeneous cells (dark gray) separated by thin, bright white lines corresponding to vessels and connective tissue.
- Metastatic Involvement: Look for patchy, highly cellular areas forming nodular or pseudonodular foci with a heterogeneous, lighter gray appearance. Key features include capsular infiltration, hilum effacement, and disruption of physiological compartments.
- Pitfalls: Exercise caution in highly cellular samples where normal lymphatic tissue may resemble cancer; the presence of irregular, brighter fibrosis can help locate metastatic foci.
4. Post-Imaging Processing:
- After FF-OCT imaging, transfer specimens to standard containers for histopathological analysis.
- Mark and orient specimens to ensure histological sections correspond to the FF-OCT acquisition plane.
- Process tissue for standard H&E staining and diagnosis.
Protocol for Breast Cancer Surgical Margin Assessment
This protocol is informed by a systematic review and meta-analysis on the diagnostic accuracy of OCT for margin assessment in breast-conserving surgery (BCS) [47].
1. Specimen Handling:
- Sample: Freshly excised lumpectomy specimens from BCS.
- Orientation: Orient the specimen using sutches or inks as per standard surgical practice to allow correlation of OCT findings with specific margins.
2. OCT Scanning of Margins:
- Technology: Utilize a volumetric OCT system capable of providing 3D images with 6.5–15 μm resolution.
- Procedure: Systematically scan all surfaces of the specimen corresponding to the surgical margins. The technique is label-free and non-destructive.
- Depth of Imaging: OCT can typically provide real-time microscopic images 2–3 mm beneath the tissue surface.
3. Real-Time Image Analysis:
- Healthy Tissue: Appears as a structured, layered architecture.
- Cancerous Tissue: Manifests as heterogeneous, highly scattering regions with the loss of normal tissue patterns.
- Integration with ML: For enhanced accuracy, implement a convolutional neural network (CNN) based classification method to automatically analyze the OCT images and flag suspicious margins. The meta-analysis found that OCT combined with machine learning algorithms significantly improved assessment accuracy compared to OCT alone [47].
4. Intraoperative Decision-Making:
- Based on the OCT findings, surgeons can identify margins suspected of being positive and perform immediate re-excisions if necessary.
- This real-time feedback aims to reduce the need for secondary surgeries.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for OCT Cancer Diagnostics Research
| Item | Function/Application | Example Product/Specification |
|---|---|---|
| High-Resolution Dermatological OCT Scanner | In vivo cross-sectional imaging of skin layers | VivoSight Scanner (Michelson Diagnostics) with 5 μm axial resolution [53] |
| Full-Field OCT (FF-OCT) System | Ex vivo microscopic imaging of unstained tissues with 1 μm resolution | CelTivity Biopsy System (AQUYRE Biosciences) with Linnik interferometer [95] |
| Microtome | Slicing fresh tissue samples to a suitable thickness for FF-OCT imaging | Standard laboratory microtome for fresh tissue [95] |
| Specimen Containers (Dedicated) | Holding tissue samples during FF-OCT scanning without altering tissue | Containers compatible with the FF-OCT system stage [95] |
| H&E Staining Kit | Gold standard histopathological processing for validation | Standard laboratory H&E staining reagents [53] [95] |
| AI/ML Image Analysis Software | Automated image segmentation, classification, and disease detection | Convolutional Neural Network (CNN) platforms for OCT image analysis [47] |
Workflow and Pathway Visualizations
Title: BCC Diagnostic Pathway
Title: LN Metastasis Assessment Workflow
Optical Coherence Tomography (OCT) has emerged as a powerful label-free optical imaging technique that provides high-resolution, cross-sectional images of biological tissues in real-time. Within oncology, OCT offers non-invasive microscopy capabilities using non-ionizing light, presenting distinct advantages and limitations compared to established imaging modalities. This analysis provides a comparative evaluation of OCT against Magnetic Resonance Imaging (MRI), Computed Tomography (CT), Ultrasound, and Fluorescence Microscopy for cancer diagnostics research, with detailed protocols for their application in investigative studies.
Comparative Imaging Characteristics
Table 1: Technical specifications and performance metrics of different imaging modalities in cancer diagnostics.
| Imaging Modality | Spatial Resolution | Penetration Depth | Key Strengths | Primary Limitations | Key Cancer Applications |
|---|---|---|---|---|---|
| OCT | ~1-20 μm [72] [52] | 1-3 mm [72] [52] | High resolution, real-time imaging, non-ionizing, label-free | Limited penetration depth, operator-dependent interpretation [72] [52] | Early detection of oral cancers [72] [52], assessment of resection margins [72] [52] |
| MRI | 50-500 μm [96] | Whole-organ | Excellent soft tissue contrast, multi-parametric imaging, non-ionizing | High cost, long acquisition time, limited accessibility [96] | Liver cancer detection and characterization [96], brain tumor imaging |
| CT | 200-500 μm | Whole-body | Fast acquisition, excellent bone imaging, widely available | Ionizing radiation, poor soft tissue contrast [97] | Tumor staging, lung cancer screening |
| Ultrasound | 50-500 μm | Centimeter | Real-time imaging, portable, low cost | Operator-dependent, limited in obese patients | Breast cancer, thyroid nodules, abdominal masses |
| Fluorescence Microscopy | <1 μm | <1 mm | Cellular resolution, molecular specificity | Limited penetration, requires exogenous agents [98] [99] | Intraoperative guidance [98], cellular imaging |
Table 2: Functional and molecular imaging capabilities for cancer characterization.
| Modality | Functional Imaging Capabilities | Molecular Imaging Approach | Sensitivity | Quantitative Strengths |
|---|---|---|---|---|
| OCT | Doppler flow, polarization-sensitive [99] | Contrast-enhanced with nanoparticles [100] | 250 pM for LGNRs [100] | Microvascular mapping, tissue birefringence |
| MRI | DWI, DCE-MRI, MRE [96] | Targeted molecular probes [101] [102] | μM-mM for contrast agents [102] | Tumor perfusion, cellularity, tissue stiffness [96] |
| CT | Perfusion imaging | Iodine-based contrast agents | mM for contrast agents | Vascular permeability, blood volume |
| Ultrasound | Doppler, elastography | Microbubble contrast agents | nM-μM for targeted bubbles | Blood flow, tissue stiffness |
| Fluorescence Microscopy | FRET, calcium imaging | Targeted fluorescent probes [98] [102] | pM-nM for NIR probes [101] | Molecular concentration, protein interactions |
OCT Imaging Protocols for Cancer Diagnostics
Protocol for Ex Vivo Oral Cancer Tissue Assessment
Purpose: To identify malignant changes in excised oral squamous cell carcinoma (OSCC) tissue and assess resection margins [72] [52].
Materials and Equipment:
- Michelson Diagnostics EX1301 OCT microscope or equivalent SD-OCT system [72] [52]
- Freshly excised human oral tissue specimens
- Tissue embedding medium (OCT compound)
- Microtome for sectioning
- Standard histopathology equipment for H&E staining
Procedure:
- Sample Preparation:
- Collect fresh oral tissue specimens from surgical resection immediately after excision.
- Place specimens in standard pathology transport containers on ice.
- Embed tissue in optimal cutting temperature (OCT) compound without freezing for immediate imaging.
- For correlation with histology, subsequently freeze embedded tissue at -80°C for cryosectioning.
OCT Imaging:
- Mount the OCT system on a vibration-isolated table.
- Position tissue specimen on the imaging stage with the region of interest facing the objective.
- Apply ultrasound gel between the objective and tissue if using a contact probe.
- Acquire cross-sectional images (B-scans) in multiple regions of interest with a minimum of 100 B-scans per specimen.
- Set axial resolution to 1-15 μm and lateral resolution to 5-20 μm depending on system capabilities.
- Use a scanning protocol that covers the entire specimen surface in a raster pattern.
Image Analysis:
- Process raw interferometric data using Fourier transformation to generate structural images.
- Evaluate epithelial thickness, architectural disruption, and basement membrane integrity.
- Identify regions with altered scattering properties indicative of neoplasia.
- Compare OCT findings with corresponding histology sections after H&E staining.
Quality Control:
- Calibrate system with a reference sample before each imaging session.
- Ensure signal-to-noise ratio remains above 90 dB for optimal image quality.
- Maintain consistent imaging parameters across all samples in a study.
Interpretation: Normal oral mucosa appears as a structured, layered architecture with intact basement membrane. OSCC demonstrates epithelial thickening, loss of layered structure, and disruption of the basement membrane [72] [52]. The accuracy for distinguishing normal from malignant tissue exceeds 90% in validated systems [72] [52].
Protocol for In Vivo Cutaneous Tumor Microvasculature Imaging
Purpose: To non-invasively image tumor microvasculature and lymphatic drainage using contrast-enhanced OCT [100].
Materials and Equipment:
- Spectral-domain OCT system with broad bandwidth source (800-1000 nm)
- Large gold nanorods (LGNRs) with tuned resonance peaks (815 nm and 925 nm)
- Animal preparation station with anesthesia system
- Custom spectral processing software
Procedure:
- Contrast Agent Preparation:
- Synthesize LGNRs (~100 × 30 nm) according to established protocols [100].
- Functionalize LGNR surface with thiolated poly(ethylene glycol) (PEG-SH) for biostability.
- Characterize LGNR optical properties using spectrophotometry.
- Resuspend in sterile phosphate-buffered saline at 250 pM concentration for injection.
Animal Preparation:
- Anesthetize mice using approved anesthetic protocol (e.g., ketamine/xylazine).
- Position animal on temperature-controlled stage to maintain body temperature.
- Depilate imaging area if necessary for optimal light penetration.
Image Acquisition:
- Acquire baseline OCT images prior to contrast agent administration.
- Intravenously administer 100 μL of LGNR solution via tail vein.
- Acquire post-contrast images at 1, 5, 15, 30, and 60-minute time points.
- For lymphatic imaging, administer 20 μL LGNR solution subcutaneously in the footpad.
- Image lymphatic drainage in real-time with high temporal resolution.
Spectral Processing:
- Divide raw SD-OCT interferograms into two spectrally-distinct subsets (800-900 nm and 900-1000 nm).
- Apply adaptive dispersion compensation to minimize band decorrelation.
- Implement depth-dependent artifact compensation using neutral tissue regions as reference.
- Generate spectral contrast images by calculating normalized difference between bands.
- Apply flow-gating using speckle variance to detect LGNRs in circulation.
Interpretation: LGNRs produce ~110-fold greater spectral signal per particle than conventional GNRs, enabling detection of tumor microvasculature at up to 750 μm depth [100]. Multiplexed detection of spectrally-distinct LGNRs allows observation of lymphatic drainage patterns and identification of functional lymphatic valves.
Research Reagent Solutions
Table 3: Essential research reagents and materials for advanced imaging applications.
| Reagent/Material | Function | Application Examples | Key Considerations |
|---|---|---|---|
| Large Gold Nanorods (LGNRs) [100] | OCT contrast agent | Tumor vasculature imaging, lymphatic drainage studies | ~100 × 30 nm size, 815-925 nm resonance, PEG-coated for stability |
| Targeted Fluorescent Probes [98] [102] | Molecular-specific imaging | Fluorescence-guided surgery, cellular imaging | NIR-I (700-900 nm) or NIR-II (1000-1700 nm) for better penetration |
| Bimodal MR/Fluorescence Probes [101] | Multimodal imaging | Precise tumor delineation, intraoperative guidance | Combine deep tissue MRI with cellular-resolution fluorescence |
| Gadolinium-Based Contrast Agents [96] | MRI contrast enhancement | Tumor vascularity assessment, lesion characterization | Risk of nephrogenic systemic fibrosis in renal impairment |
| Molecularly Imprinted Polymers [101] | Enhanced targeting | Specific biomarker detection, improved probe accumulation | Synthetic antibodies with high stability and affinity |
Integration Pathways and Workflow Strategies
Advanced Technical Considerations
Resolution and Penetration Trade-offs
The fundamental trade-off between resolution and penetration depth dictates modality selection for specific cancer applications. OCT excels in high-resolution imaging of superficial tissues (<3 mm), providing cellular-level detail without biopsy [72] [52]. While MRI offers superior soft tissue contrast and whole-organ penetration, its resolution remains limited to hundreds of microns [96]. Fluorescence microscopy achieves subcellular resolution but suffers from minimal penetration (<1 mm), restricting its utility to intraoperative guidance or endoscopic applications [98] [99].
Quantitative Biomarker Development
OCT enables quantitative tissue characterization through:
- Scattering coefficient quantification: Derived from signal intensity decay with depth
- Texture analysis: Algorithmic assessment of tissue microarchitecture
- Polarization-sensitive measurements: Birefringence mapping of collagen organization
- Doppler flow quantification: Microvascular blood flow velocity measurement
Comparative studies demonstrate OCT's capacity to distinguish cancerous from normal tissues based on quantitative parameters. In hepatocellular carcinoma, fluorescence lifetime imaging microscopy (FLIM) of H&E-stained sections revealed significantly longer fluorescence lifetimes in cancerous regions (2000-2500 ps) compared to peritumoral tissues (500-1000 ps) [103].
Multimodal Integration Strategies
OCT occupies a unique niche in the cancer imaging landscape, bridging the resolution gap between macroscopic clinical imaging and microscopic histology. While limited by penetration depth, its superior resolution, real-time capability, and lack of ionizing radiation make it invaluable for superficial tissue imaging and surgical guidance. The integration of OCT with established modalities like MRI and emerging technologies like targeted fluorescence creates powerful multimodal platforms that leverage complementary strengths. For researchers and drug development professionals, these advanced imaging approaches provide robust tools for investigating tumor biology, evaluating therapeutic efficacy, and developing novel diagnostic strategies that span from molecular detection to clinical application.
Optical Coherence Tomography (OCT) is a powerful, non-invasive optical imaging technique that generates high-resolution, cross-sectional images of biological tissues in real-time. Functioning as a type of "optical biopsy," OCT provides tissue visualization at near-histological resolution without the need for physical tissue removal [76] [17]. While traditionally established in ophthalmology, technological advancements have enabled the development of portable, cost-effective OCT systems suitable for point-of-care (POC) cancer screening applications in resource-limited settings [76] [78].
The transition of OCT from specialized clinical settings to point-of-care environments represents a paradigm shift in cancer diagnostics. This evolution is particularly crucial for low- and middle-income countries (LMICs), where cancer mortality rates remain disproportionately high due to limited access to traditional diagnostic infrastructure [78]. Point-of-care OCT systems address this gap by offering rapid, real-time imaging capabilities that can identify malignant and pre-malignant changes in epithelial tissues, enabling earlier detection and intervention for cancers affecting the oral cavity, skin, and other accessible anatomical sites [104] [52].
Comparative Advantages of Point-of-Care OCT Systems
Point-of-care OCT systems offer several distinct advantages over traditional diagnostic modalities in resource-limited settings, making them particularly suitable for cancer screening applications.
Table 1: Performance Characteristics of Point-of-Care OCT in Cancer Detection
| Cancer Type | Sensitivity | Specificity | Clinical Setting | Reference |
|---|---|---|---|---|
| Oral Potentially Malignant Lesions | 95% | N/S | Community and tertiary care settings | [104] |
| Oral Malignant Lesions | 93% | N/S | Community and tertiary care settings | [104] |
| High-Grade Oral Dysplasia | 83% | N/S | SVM model over ANN | [104] |
| Dysplastic OPMD and Malignant Lesions | 81.5% | 87% | Surgical margin assessment | [52] |
Table 2: Comparative Analysis of OCT Imaging Modalities
| Feature | Time-Domain OCT (TD-OCT) | Spectral-Domain OCT (SD-OCT) | Swept-Source OCT (SS-OCT) |
|---|---|---|---|
| Light Source | Broadband light source with moving reference mirror | Broadband light with spectrometer detection | Tunable laser swept across wavelengths with single photodetector |
| Axial Resolution | 8-10 µm | 5-7 µm | ~11 µm |
| Scan Rate | 400 A-scans/s | 20,000-52,000 A-scans/s | 100,000-236,000 A-scans/s |
| Cost Considerations | Lower cost | Moderate cost | Higher cost |
| Suitability for POC | Limited by speed | Good balance of performance and cost | Excellent performance but cost-prohibitive for many resource-limited settings |
The cost-effectiveness of POC-OCT systems represents a significant advantage for resource-constrained healthcare environments. Traditional commercial OCT systems can range from \$40,000 to \$150,000, limiting their accessibility to large medical centers [76] [52]. In contrast, emerging low-cost OCT systems utilize innovative design approaches, including 3D-printed enclosures and off-the-shelf optical components, to substantially reduce manufacturing costs without compromising essential imaging capabilities [76]. This cost reduction expands the potential for population-scale screening programs in settings where traditional diagnostic methods are economically unsustainable.
The non-invasive nature of OCT imaging eliminates the need for biopsy procedures in many cases, reducing patient discomfort, minimizing procedural risks, and decreasing the burden on pathological services [17] [52]. Furthermore, OCT's ability to provide real-time imaging results enables immediate clinical decision-making during screening events, potentially allowing for same-day interventions or referrals when necessary [104] [17].
Experimental Protocols for POC-OCT in Cancer Detection
Protocol for Oral Cancer Screening with POC-OCT
The following protocol outlines the standardized methodology for implementing POC-OCT in oral cancer screening programs in resource-limited settings, based on validated clinical studies [104].
Equipment Setup:
- Portable spectral-domain OCT system with handheld imaging probe
- Disposable probe covers or appropriate sterilization materials
- Data processing unit with automated image analysis algorithm
- Power source (battery or electrical connection)
Imaging Procedure:
- Position patient comfortably with adequate head support
- Perform visual inspection of oral cavity under appropriate illumination
- Gently place OCT probe perpendicular to tissue surface of target lesion and adjacent normal mucosa
- Acquire multiple cross-sectional images (B-scans) across the lesion with overlapping regions
- Ensure adequate image quality by monitoring signal strength in real-time
- Repeat imaging for all suspicious areas and corresponding contralateral normal sites
Image Analysis:
- Process acquired images through automated classification algorithm
- Algorithm extracts multiple neural network-based features (14 distinct features in validated systems)
- Support vector machine (SVM) model classifies lesions based on extracted features
- Generate diagnostic output indicating probability of malignancy or degree of dysplasia
Quality Control:
- Regular calibration of OCT system using standardized phantoms
- Validation of image quality metrics before patient imaging
- Periodic assessment of algorithm performance against histological standards
This protocol has demonstrated efficacy in distinguishing benign lesions, oral potentially malignant disorders (OPMDs), and malignant lesions across community and tertiary care settings, achieving sensitivity of 95% for dysplastic OPMDs and 93% for malignant lesions [104].
Workflow Diagram: POC-OCT Implementation Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Components for POC-OCT Development
| Component Category | Specific Examples | Function in POC-OCT Development |
|---|---|---|
| Optical Components | Broadband light sources, diffraction gratings, MEMS mirrors | Enable compact spectrometer design for SD-OCT systems |
| Detection Systems | High-speed line scan cameras, photodetectors | Capture interference patterns for image reconstruction |
| Computational Tools | Convolutional Neural Networks (CNNs), Support Vector Machines (SVMs), Artificial Neural Networks (ANNs) | Automated image analysis and diagnostic classification |
| Manufacturing Materials | 3D-printing filaments, compact lens assemblies | Create cost-effective, portable system enclosures and optical paths |
| Calibration Standards | Optical phantoms with standardized scattering properties | Validate system performance and ensure quantitative imaging |
Implementation Challenges and Technical Considerations
Despite the promising advantages of POC-OCT systems in resource-limited settings, several implementation challenges must be addressed to ensure successful deployment.
The limited penetration depth of OCT technology (typically 1-2 mm) restricts its application to superficial epithelial tissues, which may result in underestimation of tumor staging for invasive cancers [52]. This limitation necessitates complementary imaging modalities for comprehensive assessment of deeply invasive malignancies. Additionally, operator dependency in image acquisition can introduce variability in diagnostic accuracy, particularly when deployed by minimally trained healthcare workers in remote settings [52].
The integration of artificial intelligence algorithms for automated image interpretation helps mitigate this limitation by standardizing diagnostic criteria and reducing reliance on specialist expertise [30] [17]. However, these AI algorithms require extensive training on diverse datasets to ensure robust performance across different population groups and clinical environments [30].
Infrastructure constraints in resource-limited settings, including unreliable electricity and limited internet connectivity for data transmission, present practical challenges for POC-OCT implementation [78]. These limitations can be addressed through system design innovations such as battery-powered operation and onboard image processing capabilities that function without continuous network connectivity.
The ongoing development of point-of-care OCT systems for cancer screening in resource-limited settings is advancing through several key technological innovations. The integration of artificial intelligence and deep learning algorithms continues to enhance the diagnostic capabilities of POC-OCT systems, with convolutional neural networks demonstrating remarkable proficiency in distinguishing normal and pathological tissues [30] [105]. These AI-driven systems can extract subtle imaging biomarkers that may be imperceptible to human observers, potentially enabling earlier detection of malignant changes [17].
Further cost reduction strategies through component miniaturization, simplified optical designs, and manufacturing innovations will expand the accessibility of POC-OCT technology [76]. The development of multimodal imaging systems that combine OCT with complementary techniques such as fluorescence imaging or Raman spectroscopy offers promise for enhanced diagnostic specificity by providing correlated structural and biochemical information [78] [17].
In conclusion, point-of-care OCT systems represent a transformative technology for cancer screening in resource-limited settings, offering high-resolution imaging capabilities in portable, cost-effective platforms. The comparative advantages of these systems, including their non-invasive nature, real-time imaging capabilities, and integration with automated diagnostic algorithms, position them as powerful tools for addressing global disparities in cancer detection and outcomes. As technological innovations continue to enhance their performance and accessibility, POC-OCT systems hold significant potential to revolutionize early cancer detection in underserved populations worldwide.
Optical Coherence Tomography (OCT) has emerged as a powerful, non-invasive imaging modality capable of delivering high-resolution, real-time visualization of tissue microstructure at the micrometer scale. Initially revolutionizing ophthalmology, OCT is now positioned to transform oncologic diagnostics and therapeutic monitoring. This transition is driven by continuous technological innovations that provide functional and metabolic contrast beyond structural imaging alone. The integration of OCT into oncology addresses critical clinical needs, particularly in intraoperative margin assessment during cancer surgeries, where current techniques have failed to significantly reduce re-excision rates [24] [18]. For researchers and drug development professionals, understanding the regulatory and commercial pathways for OCT translation is essential for effectively deploying these technologies in clinical practice and advancing precision oncology initiatives.
Current State of OCT in Cancer Diagnostics
Technical Advancements and Functional Extensions
The evolution of OCT from a structural imaging tool to a multimodal platform has significantly expanded its utility in cancer diagnostics. Several functional extensions now provide complementary contrast mechanisms essential for differentiating malignant from benign tissues:
Dynamic OCT (d-OCT): Detects intrinsic tissue motility caused by cellular and subcellular movements. By analyzing the temporal variance of the OCT signal, d-OCT provides quantitative indicators of cellular viability and metabolic activity [106] [18]. This technique establishes a direct mathematical relationship between the autocorrelation function decay and the active diffusion movement of organelles, using the dynamic diffusion coefficient as a quantitative metric for cellular function.
OCT Angiography (OCTA): Enables visualization and quantification of microvascular networks without exogenous contrast agents. This functional extension is particularly valuable for imaging tumor vasculature, detecting pathological vessel patterns like neovascularization, and monitoring anti-angiogenic therapy responses [24] [66].
Optical Coherence Elastography (OCE): Maps tissue mechanical properties by measuring its response to applied force. As cancerous tissues often exhibit different mechanical properties (e.g., higher stiffness) compared to benign tissues, OCE provides additional contrast for tumor detection and characterization [66] [18].
Visible Light OCT and Optoretinography: Shifting the operating wavelength to the visible spectrum allows for higher-resolution structural imaging and enables functional assessments like retinal oximetry. Similarly, optoretinography measures stimulus-evoked intrinsic optical signals from photoreceptors, demonstrating OCT's potential for functional imaging beyond morphology [24].
Demonstrated Clinical Applications in Oncology
Recent studies have validated OCT's potential across multiple cancer types, establishing its clinical relevance and informing regulatory strategies:
Table 1: Demonstrated Clinical Applications of OCT in Oncology
| Cancer Type | Application | Key Findings | Clinical Impact |
|---|---|---|---|
| Breast Cancer [18] | Margin assessment during breast-conserving surgery | 3-D d-OCT consistently showed higher contrast between malignant (IDC, DCIS, ILC, LCIS) and benign regions compared to OCT intensity alone. | Potential to reduce 20-30% re-excision rate; assessment within 15-30 minutes per specimen. |
| Squamous Cell Carcinoma [43] | Non-invasive diagnosis and classification | Green subchannel maximum pixel intensities (representing cellular content) were lower in SCC than normal skin and decreased with increasing lesion size. | Enables telemedicine applications for lesion classification in remote areas. |
| Drug Screening [106] | In vitro cell viability measurement | Established direct relationship between autocorrelation function decay and active diffusion movement of intracellular organelles. | Facilitates rapid screening of cancer drugs for targeted therapy and precision medicine. |
Quantitative Analysis of OCT Performance Characteristics
For regulatory submission and commercial deployment, quantitative performance data is essential. The following tables summarize key metrics from recent studies demonstrating OCT's diagnostic capabilities.
Table 2: Quantitative Performance Metrics of OCT in Clinical Studies
| Study Focus | Sensitivity | Specificity | Accuracy | Key Quantitative Differentiators |
|---|---|---|---|---|
| Breast Tumor Margin Assessment [18] | Not explicitly quantified | Not explicitly quantified | Not explicitly quantified | Consistent improvement in contrast-to-noise ratio in d-OCT vs. standard OCT across all cancer subtypes (IDC, DCIS, ILC, LCIS). |
| Retinal Pathology Diagnosis [107] | 0.59 (MORG AI) vs. 0.72 (Ophthalmologist) | 0.72 (MORG AI) vs. 0.77 (Ophthalmologist) | 0.75 (MORG AI) vs. 0.86 (Ophthalmologist) | AI-assisted report generation reduced ophthalmologist drafting time by 58.9% (38.36s to 13.47s average). |
| Carotid Artery Stenosis Screening [66] | Not explicitly quantified | Not explicitly quantified | Statistically significant correlation (p=0.025-0.045) between OCTA parameters (FAZ, NFA, VFA) and carotid Doppler velocities. | OCTA parameters showed strong correlation with carotid stenosis severity, enabling microvascular change monitoring. |
Table 3: Technical Specifications of Representative OCT Systems in Research
| Parameter | Spectral-Domain OCT (Telesto 320) [18] | Swept-Source OCT (Triton) [107] | Lab-built System (Lumedica OQ 2.0) [43] |
|---|---|---|---|
| Central Wavelength | 1300 nm | 1060 nm | 840 nm |
| Axial Resolution | 4.8 µm in air | Not specified | Not specified |
| Lateral Resolution | 7.2 µm | Not specified | Not specified |
| Imaging Depth | ~1 mm in turbid tissue | Not specified | Not specified |
| A-line Rate | Not specified | Not specified | 13,000 frames per second |
| Key Applications | Breast tissue margin assessment, 3D d-OCT | Retinal imaging, AI-based reporting | Squamous cell carcinoma, vibrational studies |
Experimental Protocols for Key OCT Applications
Protocol 1: Dynamic OCT for Breast Tumor Margin Assessment
This protocol outlines the methodology for 3-D d-OCT imaging of freshly excised breast specimens, optimized for intraoperative margin assessment [18].
Sample Preparation:
- Obtain fresh breast tissue samples (~30 × 20 × 5 mm³) containing both malignant and benign tissues from mastectomy or wide local excision procedures.
- Perform excision within one hour of imaging to preserve tissue motility characteristics.
- Hydrate specimens with saline and compress against an imaging window to minimize surface topology variation and bulk tissue motion.
- Process control samples through standard histology protocol (inking, formalin fixation, paraffin embedding, sectioning, H&E staining) for validation.
Image Acquisition:
- Equipment: Use a commercial SD-OCT system (e.g., Telesto 320, Thorlabs) with a central wavelength of 1300 nm and a 200 nm bandwidth.
- Wide-field Scan: Acquire nine partially overlapping 10 × 10 × 3.5 mm³ sub-volumes in a 3 × 3 grid to construct a mosaiced image (~28 × 28 × 3.5 mm³) with voxel size of 10 × 10 × 3.5 µm³.
- d-OCT Scan: Select a region of interest (3 × 3 mm²) based on wide-field images. Acquire multiple repeated B-scans at the same lateral location with optimal spatial and temporal sampling trade-off (e.g., 1000 × 1024 pixels over 3 × 3.5 mm²).
Image Processing and Visualization:
- Process time-series data using Fourier power spectral analysis.
- Generate dynamic contrast using one of three methods:
- RGB Method: Sum spectral power within three frequency ranges and map to red, green, and blue channels [18].
- HSV Method: Map statistical metrics from frequency distribution to hue, saturation, and value channels [18].
- Phase Variance: Utilize phase-sensitive detection for higher sensitivity to tissue motion [18].
- Co-register d-OCT images with histology slides annotated by a pathologist for validation.
Dynamic OCT Experimental Workflow
Protocol 2: OCT-Based Cell Viability Measurement for Drug Screening
This protocol describes a quantitative dynamic OCT approach for measuring cell viability, enabling rapid screening of anti-cancer drugs [106].
Theoretical Foundation:
- Develop a theoretical model of organelle motion based on first-order field autocorrelation function analysis.
- Establish a direct mathematical relationship between the autocorrelation function decay and the active diffusion movement of organelles, proteins, and other macromolecules.
- Use the dynamic diffusion coefficient as a quantitative indicator for precise quantification and evaluation of cellular function and activity.
Experimental Implementation:
- Cell Culture: Maintain cancer cell lines in appropriate culture conditions relevant to the drug screening application.
- OCT Imaging: Acquire time-series OCT images at the same spatial location to detect changes in interference phase caused by active diffusion movement of intracellular components.
- Data Analysis: Calculate the autocorrelation function decay from the OCT interference signals and compute the dynamic diffusion coefficient according to the theoretical model.
- Drug Exposure: Apply anti-cancer compounds at various concentrations and time points, measuring changes in the diffusion coefficient as an indicator of cell viability and treatment response.
Protocol 3: Vibrational OCT for Skin Cancer Diagnosis
This protocol combines standard OCT with vibrational analysis to characterize squamous cell carcinomas [43].
System Configuration:
- Modify a commercial OCT system (e.g., Lumedica OQ Labscope 2.0) by adding a 2-inch diameter speaker positioned approximately 2 inches from the tissue.
- Generate sinusoidal sound waves at 55 dB using a computer app, applying both sound and light to the tissue surface along the beam axis.
Data Collection and Analysis:
- Collect raw OCT image data and process using MATLAB and ImageJ software.
- Color-code grayscale scans and generate pixel intensity versus depth plots by scanning parallel to the sample surface.
- Analyze subchannel images:
- Green channel: Represents cellular content (low pixel intensity)
- Blue channel: Provides collagen information (medium pixel intensity)
- Red channel: Shows high-intensity reflections throughout tissue depth
- Measure tissue displacement in phase with sound application by analyzing frequency dependence of tissue deformation based on reflected infrared light.
- Plot displacement amplitude against vibration frequency to create a mechanovibrational spectrum, identifying resonant frequencies of tissue components (cells: 50-80 Hz, dermal collagen: 100-120 Hz).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for OCT in Oncology
| Item | Function/Application | Specifications/Examples |
|---|---|---|
| Spectral-Domain OCT System [18] | Primary imaging hardware for 3D microstructural tissue imaging. | Central wavelength: 1300 nm; Axial resolution: <5 µm; Lateral resolution: ~7 µm. |
| Vibrational Excitation System [43] | Applies controlled sound frequencies to measure tissue mechanical properties. | 2-inch speaker generating 55 dB sound waves at frequencies of 50-260 Hz. |
| MATLAB Software [43] [18] | Processing raw OCT data, generating pixel intensity plots, calculating tissue displacements. | Custom scripts for Fourier analysis, RGB/HSV color mapping, phase variance calculation. |
| ImageJ Software [43] | Image processing and analysis; color-coding grayscale OCT images. | Open-source platform with custom plugins for OCT-specific analyses. |
| Tissue Preparation Materials [18] | Standardized sample preparation for ex vivo imaging. | Saline hydration solution; compression imaging window; formalin fixation. |
| Histology Processing Supplies [18] | Gold standard validation of OCT findings. | 10% neutral-buffered formalin; paraffin embedding; H&E staining. |
Regulatory and Commercial Translation Pathways
Regulatory Strategy and Approval Pathways
Successful clinical translation of OCT technologies requires careful navigation of regulatory landscapes:
Device Classification: Most OCT systems for cancer diagnosis will likely be classified as Class II medical devices, requiring 510(k) premarket notification if substantial equivalence can be demonstrated to predicate devices. Novel applications or significantly different technological characteristics may necessitate De Novo classification or Premarket Approval (PMA).
Clinical Validation Requirements: Regulatory submissions must include robust clinical validation data demonstrating:
- Analytical performance (resolution, accuracy, precision)
- Clinical performance (sensitivity, specificity, PPV, NPV)
- Safety profile (non-invasive nature of OCT is advantageous)
- Substantial equivalence to predicate devices or superior performance for novel claims
Benefit-Risk Profile: Emphasize OCT's non-invasive nature, real-time imaging capability, and potential to reduce unnecessary procedures (e.g., re-excision surgeries) while improving diagnostic accuracy.
Commercialization and Integration into Clinical Practice
Effective integration of OCT into oncology practice requires addressing practical implementation challenges:
Clinical Workflow Integration: Design systems for seamless integration into existing clinical workflows, with particular attention to intraoperative settings where time constraints are critical (e.g., 15-30 minutes per specimen for margin assessment) [18].
Reimbursement Strategy: Develop comprehensive economic models demonstrating cost-effectiveness through reduced reoperation rates, shorter procedure times, and improved patient outcomes.
Training and Implementation: Create standardized training protocols for clinicians and technicians to ensure consistent operation and interpretation across institutions.
AI Integration: Leverage artificial intelligence, particularly deep learning algorithms, to automate image interpretation and report generation, reducing interpretation time and expanding accessibility to non-specialist settings [24] [107].
Regulatory & Commercial Translation Pathway
The translation of OCT from a research tool to clinical oncology practice requires coordinated advancement across multiple fronts. Technologically, continued development of functional extensions like d-OCT, OCE, and OCTA will enhance diagnostic specificity. The integration of artificial intelligence for automated image analysis and report generation will address workflow integration challenges and improve accessibility [107]. Commercially, demonstrating improved patient outcomes and cost-effectiveness through well-designed clinical trials will be essential for market adoption. Regulatory success will depend on constructing robust validation studies that clearly establish clinical utility for specific indications. As these pathways converge, OCT is positioned to significantly impact cancer diagnosis, treatment guidance, and therapeutic monitoring, ultimately advancing the field of precision oncology through non-invasive, high-resolution tissue characterization.
Conclusion
Optical Coherence Tomography has firmly established itself as a powerful, non-invasive imaging modality with immense value across the cancer care continuum, from initial screening to surgical guidance. The integration of artificial intelligence is poised to overcome key challenges in image interpretation, standardization, and workflow integration, thereby enhancing diagnostic accuracy and accessibility. Future directions point toward the development of multimodal platforms that combine OCT with complementary techniques like photoacoustic imaging and spectroscopy, offering a more comprehensive 'optical palpation' of tissue. Furthermore, the ongoing miniaturization and cost-reduction of OCT technology will be critical for its deployment in point-of-care and global health settings, ultimately democratizing advanced cancer diagnostics. For researchers and drug developers, OCT presents not only a robust tool for preclinical research but also a promising companion diagnostic technology for monitoring novel therapeutic responses in clinical trials, heralding a new era of image-guided precision oncology.
References
- 1. How Low-Coherence Interferometry (LCI) Works [https://www.novacam.com/technology/how-lci-works/]
- 2. Review of optical coherence tomography in oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5741100/]
- 3. Optics for Micron-Scale Resolution & Low-Noise OCT [https://avantierinc.com/resources/knowledge-center/micron-scale-resolution-low-noise-oct/]
- 4. Nanometer resolution of 2d single-shot low-coherence & ... [https://www.sciencedirect.com/science/article/abs/pii/S0030401823005503]
- 5. Cancer imaging by optical coherence tomography: preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3560400/]
- 6. Application of Targeted Optical Coherence Tomography in ... [https://pubmed.ncbi.nlm.nih.gov/39410651/]
- 7. Analyzing spatial correlations in tissue using angle- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4929650/]
- 8. Quantitative comparison of automated OCT and ... [https://www.nature.com/articles/s41598-024-71496-y]
- 9. Recent advances in optical coherence tomography for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3393648/]
- 10. Endoscopic optical coherence tomography [https://pmc.ncbi.nlm.nih.gov/articles/PMC5480489/]
- 11. EB-OCT: a potential strategy on early diagnosis and ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1156218/full]
- 12. Manually scanned single fiber optical coherence ... [https://www.nature.com/articles/s41598-021-95118-z]
- 13. Variations in optical coherence tomography resolution and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4102349/]
- 14. Adaptability and Performance of Low-Cost OCT System for ... [https://opg.optica.org/abstract.cfm?uri=microscopy-2018-JW3A.32]
- 15. Endoscopic en-face optical coherence tomography and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8884237/]
- 16. OCT in Oncology and Precision Medicine: From Nanoparticles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189282/]
- 17. Artificial intelligence in advancing optical coherence ... [https://www.sciencedirect.com/science/article/abs/pii/S074879832500616X]
- 18. Three-dimensional dynamic optical coherence tomography for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339312/]
- 19. Light and metabolism: label-free optical imaging of ... [https://opg.optica.org/boe/abstract.cfm?uri=boe-16-9-3770]
- 20. Enhancing polarization contrast with depolarization ... [https://www.nature.com/articles/s41598-025-00327-5]
- 21. Microenvironmental regulation and remodeling of breast ... [https://link.springer.com/article/10.1007/s12672-025-03797-1]
- 22. Quantitative microvessel orientation biomarkers derived from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238592/]
- 23. NIR-II Dual-Modal Photoacoustic and OCT/OCTA Contrast ... [https://pubmed.ncbi.nlm.nih.gov/41083813/]
- 24. Advances in optical coherence tomography: Celebrating its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456903/]
- 25. Advances in Doppler optical coherence tomography and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7523705/]
- 26. Optical coherence tomography for cancer detection [https://experts.illinois.edu/en/publications/optical-coherence-tomography-for-cancer-detection/]
- 27. Optical Coherence Tomography Angiography, Elastography ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025902/]
- 28. Optical coherence elastography detects increased corneal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12513859/]
- 29. Intracoronary Optical Coherence Tomography [https://link.springer.com/article/10.1007/s11936-025-01103-4]
- 30. Artificial intelligence in advancing optical coherence ... [https://pubmed.ncbi.nlm.nih.gov/40839924/]
- 31. The path to clinical translation for visible light optical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456912/]
- 32. Chromatic optical coherence tomography for high ... [https://opg.optica.org/prj/fulltext.cfm?uri=prj-13-10-2888]
- 33. Optical Coherence Tomography (OCT): Principle and ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK554044/]
- 34. High speed, long range, deep penetration swept source ... [https://www.nature.com/articles/s41598-022-04784-0]
- 35. Dynamic contrast optical coherence tomography (DyC ... [https://www.nature.com/articles/s42003-024-05973-5]
- 36. The 7-step “P” technique: a novel manual push method ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1621424/full]
- 37. Development of spectral domain optical coherence ... [https://livrepository.liverpool.ac.uk/2008048/]
- 38. A Review of the Applications of OCT for Analysing ... [https://www.mdpi.com/2076-3417/8/12/2700]
- 39. Fiber-Optics 'See' Early Cancers - Duke Today [https://today.duke.edu/node/112953]
- 40. 光学相干层析成像技术原理及研究进展 [https://chineseoptics.net.cn/article/id/906e45f4-3f2b-4cc5-9592-08bb4b53c201]
- 41. Application of Targeted Optical Coherence Tomography in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11475057/]
- 42. Optical coherence tomography and ... - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456916/]
- 43. Noninvasive OCT Imaging for Squamous Cell Carcinoma [https://esmed.org/noninvasive-oct-imaging-for-squamous-cell-carcinoma/]
- 44. Leveraging pretrained vision transformers for automated ... [https://opg.optica.org/boe/abstract.cfm?uri=boe-16-8-3283]
- 45. Optical percutaneous needle biopsy in oncology [https://www.light-am.com/article/doi/10.37188/lam.2025.072]
- 46. Advances in Intraoperative Margin Assessment for Breast- ... [https://pubmed.ncbi.nlm.nih.gov/41226096/]
- 47. Diagnostic accuracy of optical coherence tomography for ... [https://www.sciencedirect.com/science/article/abs/pii/S1572100023004453]
- 48. Diagnostic feasibility study of stereoscopic optical palpation ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14871-w]
- 49. Intraoperative Evaluation of Breast Tumor Margins with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2782920/]
- 50. Three-dimensional dynamic optical coherence tomography ... [https://opg.optica.org/boe/abstract.cfm?uri=boe-16-8-3061]
- 51. Breast cancer Intraoperative Margin Assessment using ... [https://www.nature.com/articles/s41523-025-00818-8]
- 52. Critical review of OCT in clinical practice for the ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1569197/full]
- 53. In Vivo Optical Coherence Tomography for the Detection ... [https://www.mdpi.com/2077-0383/14/3/949]
- 54. A pilot Study of Squamous Cell Carcinoma [https://esmed.org/MRA/mra/article/view/6543]
- 55. A Retrospective Study of the Diagnostic Accuracy of In Vivo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6518285/]
- 56. Optical Imaging Technology for Real-time Tumor Monitoring [https://www.jkslms.or.kr/journal/view.html?doi=10.25289/ML.2021.10.3.123]
- 57. Non-Invasive Imaging in Post-Radiotherapy Monitoring of ... [https://medscimonit.com/abstract/full/idArt/949669]
- 58. Clinical Applications of Optical Coherence Tomography and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523779/]
- 59. Heterogeneous tumor blood oxygenation dynamics during ... [https://www.nature.com/articles/s44384-025-00012-x]
- 60. Low-dose photodynamic therapy promotes vascular E ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12161339/]
- 61. AI-powered application enables clinicians to diagnose ... [https://www.endocrine.org/news-and-advocacy/news-room/endo-annual-meeting/endo-2025-press-releases/sethuraj-onco-press-release]
- 62. Dual-mode optical imaging system offers new noninvasive ... [https://ecancer.org/en/news/26830-dual-mode-optical-imaging-system-offers-new-noninvasive-approach-to-skin-cancer-diagnosis]
- 63. Automated retinal boundary segmentation of optical ... [https://www.nature.com/articles/s41598-022-05550-y]
- 64. A Complete Review of Automatic Detection, Segmentation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10670378/]
- 65. Recent advances and applications of optical coherence ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1438739/full]
- 66. Advances in Optical Coherence Tomography in 2025 [https://www.mdpi.com/journal/diagnostics/special_issues/MR08814H31]
- 67. Automatic Segmentation and Classification Methods Using ... [https://www.mdpi.com/2076-3417/11/20/9734]
- 68. Enhanced penetration depth in optical coherence ... [https://opg.optica.org/optica/abstract.cfm?uri=optica-12-1-24]
- 69. Visible Light Optical Coherence Tomography: Technology ... [https://www.mdpi.com/2306-5354/12/7/770]
- 70. Proposed Nomenclature for Landmarks in Anterior-Segment ... [https://pubmed.ncbi.nlm.nih.gov/40810988/]
- 71. Implications for the design of longitudinal studies [https://www.sciencedirect.com/science/article/abs/pii/S1553838923007005]
- 72. Critical review of OCT in clinical practice for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12095244/]
- 73. Unsupervised machine learning analysis of optical ... [https://www.nature.com/articles/s41598-025-96988-3]
- 74. Multimodal foundation model and benchmark for ... [https://www.nature.com/articles/s41746-025-01852-3]
- 75. Optical Coherence Tomography Market Size 2025 to 2034 [https://www.precedenceresearch.com/optical-coherence-tomography-market]
- 76. A review of low-cost and portable optical coherence tomography [https://pmc.ncbi.nlm.nih.gov/articles/PMC10465117/]
- 77. The Role of Affordable, Point-of-Care Technologies for Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5706528/]
- 78. Emerging Trends in Point-of-Care Technology Development ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312415/]
- 79. Optical Coherence Tomography Market Insights 2025–2035 [https://www.futuremarketinsights.com/reports/optical-coherence-tomography-equipment-market]
- 80. Design and implementation of a low-cost, portable OCT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5846526/]
- 81. Multimodal Optical Medical Imaging Concepts Based on ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2018.00114/full]
- 82. Advances in multimodal imaging techniques in nanomedicine [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03255e]
- 83. Smart nanoparticles for cancer therapy [https://www.nature.com/articles/s41392-023-01642-x]
- 84. Intelligent Nanoparticles for Advanced Drug Delivery in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4303181/]
- 85. Photoacoustic imaging in cancer detection, diagnosis, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3080445/]
- 86. Advancements in photoacoustic imaging for cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517324009700]
- 87. Artificial intelligence applications in ophthalmic optical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11589439/]
- 88. Trust in Artificial Intelligence–Based Clinical Decision ... [https://www.jmir.org/2025/1/e69678]
- 89. AI-Driven Clinical Decision Support Systems - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11073764/]
- 90. Comparing the diagnostic efficacy of optical coherence ... [https://pubmed.ncbi.nlm.nih.gov/38862215/]
- 91. Intravascular Optical Coherence Tomography [https://www.sciencedirect.com/science/article/abs/pii/S1051044307600396]
- 92. Quantitative Image Analysis for Tissue Biomarker Use [https://pmc.ncbi.nlm.nih.gov/articles/PMC8354563/]
- 93. A systematic review about the diagnostic test accuracy of ... [https://www.sciencedirect.com/science/article/pii/S2153353922007301]
- 94. A foundation model for clinical-grade computational ... [https://www.nature.com/articles/s41591-024-03141-0]
- 95. Microscopic assessment of lymph node status in ... [https://www.nature.com/articles/s41598-025-16570-9]
- 96. Recent Advances in Magnetic Resonance Imaging for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12386106/]
- 97. Magnetic Resonance Imaging and Computed Tomography ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206961/]
- 98. Fluorescence visualization for cancer DETECTION [https://www.sciencedirect.com/science/article/pii/S2405844024004213]
- 99. Label-free optical imaging for brain cancer assessment [https://www.sciencedirect.com/science/article/abs/pii/S2405803324000542]
- 100. Contrast-enhanced optical coherence tomography with ... [https://www.nature.com/articles/srep23337]
- 101. Implication of Bimodal Magnetic Resonance and ... [https://www.dovepress.com/implication-of-bimodal-magnetic-resonance-and-fluorescence-imaging-pro-peer-reviewed-fulltext-article-IJN]
- 102. Molecular imaging using (nano)probes - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03927d]
- 103. Fluorescence lifetime imaging microscopy approach reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339318/]
- 104. Validation of a Point-of-Care Optical Coherence Tomography ... [https://pubmed.ncbi.nlm.nih.gov/34298796/]
- 105. Recent Optical Coherence Tomography (OCT) Innovations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12108957/]
- 106. Quantitative Dynamic OCT for Cell Viability Measurement [https://opg.optica.org/abstract.cfm?uri=ECBO-2025-Tu3C.3]
- 107. A deep learning based automatic report generator for ... [https://www.nature.com/articles/s41746-025-01988-2]