Advanced Calibration Techniques for Foot Plantar Pressure Sensors: A Guide for Biomedical Research and Clinical Application
This article provides a comprehensive guide to the calibration of foot plantar pressure sensors, a critical process for ensuring data accuracy in biomechanical research and clinical diagnostics.
Advanced Calibration Techniques for Foot Plantar Pressure Sensors: A Guide for Biomedical Research and Clinical Application
Abstract
This article provides a comprehensive guide to the calibration of foot plantar pressure sensors, a critical process for ensuring data accuracy in biomechanical research and clinical diagnostics. It covers foundational principles, including the distinct calibration needs of rigid platforms versus in-shoe systems, and explores advanced methodological approaches for both normal and shear stress measurement. The content details common calibration challenges and optimization strategies, emphasizing the impact of loading conditions and anatomical specificity. Finally, it outlines rigorous validation protocols and comparative analyses of different measurement technologies, offering researchers and drug development professionals a validated framework for implementing reliable and accurate plantar pressure assessment in studies ranging from gait analysis to diabetic foot ulcer prevention.
Understanding Plantar Pressure Sensing and the Critical Role of Calibration
FAQs: System Selection, Calibration, and Data Integrity
1. What are the fundamental differences between pressure platforms and in-shoe systems, and how do I choose?
Pressure platforms and in-shoe systems serve complementary roles in research. Rigid pressure platforms are typically embedded in a walkway and are considered the most accurate method for measuring plantar pressures, especially during barefoot walking or standing [1] [2]. They offer high spatial resolution and sampling frequency, making them ideal for detailed, step-by-step gait analysis in lab conditions [1] [3].
Conversely, in-shoe systems are flexible sensor arrays placed inside footwear. They are most suitable for collecting data in the field during daily living or dynamic sporting movements, as they are often wireless and can capture multiple consecutive steps [1] [4]. Their key advantage is the ability to assess the effects of footwear and orthotics on plantar pressures directly [1]. However, they usually have lower spatial resolution and sampling frequency than platform systems [1] [3].
Selection Guide:
- Use a pressure platform for high-fidelity, barefoot gait analysis in a controlled laboratory environment.
- Use an in-shoe system for studies requiring ecological validity, such as evaluating sports performance, orthotic interventions, or activities of daily living in real-world settings [1] [4] [3].
2. What calibration considerations are critical for my research validity?
Calibration is paramount for data validity. Users must consider the suitability of the manufacturer's calibration procedures for their specific application [1].
- Dynamic Calibration: Many standard testing machines used for dynamic calibration have loading rates lower than those seen in walking, let alone sporting movements. For studies involving high-impact activities, a bespoke calibration procedure that matches the expected loading rates is required to improve validity and reliability [1] [2].
- Sensor Performance: Be aware of key sensor characteristics like linearity (how linear the pressure-response curve is) and hysteresis (the difference in output between loading and unloading). Sensors with high linearity and low hysteresis simplify data processing and improve accuracy [4].
- Frequency: While some manufacturers factory-calibrate sensors and suggest they do not require frequent re-calibration, the need can vary. In applications where the sensor is re-mounted or undergoes shape changes, more frequent calibration is necessary [5].
3. How many walking trials are needed for reliable data?
Reliability improves with the number of trials. Studies suggest that for platform systems, a minimum of five trials is sufficient for many parameters to reach a value within 90% of an unbiased estimate of the mean for an individual [6]. For in-shoe systems, the required steps can be higher and depend on the walking condition. One study found that for linear walking, a distance of 207 meters was needed to achieve excellent reliability, with curved walking requiring more steps [7]. Using a two-step protocol (where the participant lands on the platform on the second step) prior to contacting the pressure plate is recommended for reliable data [1].
4. My in-shoe data seems noisy or unreliable. What could be the cause?
In-shoe systems are prone to specific artifacts that can compromise data:
- Shear Forces: These are a primary cause of sensor damage and unreliable readings. Shear forces can occur between the foot, insole, and shoe during movement [5].
- Sensor Migration: If sensors are not securely fixed, they can slip within the shoe, leading to incorrect regional pressure mapping [7].
- Environmental Factors: Sensors are often not waterproof, and sweat or moisture can affect performance. Using protective, removable sheaths is recommended [5].
- Sensor Saturation: Ensure the pressure range of your system is appropriate for the activity. High-impact movements may exceed the sensor's maximum range.
Troubleshooting Common Experimental Issues
| Problem | Possible Cause | Solution |
|---|---|---|
| Low Intra-platform Reliability | Inconsistent gait velocity; insufficient number of trials; targeting the platform. | Standardize walking speed; collect a minimum of 5 trials [6]; use a two-step protocol and instruct participants not to look at the platform [1]. |
| Data Drift Over Session | Sensor hysteresis; temperature sensitivity. | Allow sensors to settle; choose sensors with low hysteresis and temperature sensitivity for the 20°C–37°C range [4]. |
| Unexpected Pressure Spikes | Sensor damage (folding, shear stress); debris on platform. | Inspect sensors for physical damage; avoid folding sensors [5]; clean the platform surface according to manufacturer guidelines. |
| Inconsistent In-shoe Readings | Sensor migration; shear forces; loose wiring. | Ensure secure fixation of the insole and sensors; check all connections for integrity [7]. |
The Researcher's Toolkit: Essential Materials & Methods
Key Research Reagent Solutions
| Item | Function in Research |
|---|---|
| High-Resolution Pressure Platform (e.g., emed-x) | Provides a high-fidelity benchmark for barefoot plantar pressure measurement with high spatial resolution, ideal for validating other systems or detailed gait studies [6] [8]. |
| Wireless In-shoe System (e.g., Pedar or custom smart insoles) | Enables mobile data collection during dynamic activities and sports, allowing for the assessment of footwear and orthotic interventions in real-world conditions [3] [7]. |
| Calibration Apparatus | Testing machines or custom weights for dynamic and static calibration. Critical for ensuring measurement accuracy, especially when designing bespoke protocols for high-loading activities [1]. |
| Piezoresistive Sensor Arrays | The core sensing technology in many systems. Advanced versions use materials like carbon-based inks (e.g., Carbon-Epoxy-Elastomer) screen-printed onto flexible substrates, offering high sensitivity and a wide pressure range [4] [9]. |
Standardized Experimental Protocol for Device Comparison
When comparing plantar pressure devices or conducting validation studies, follow this rigorous methodology adapted from recent research [6] [3] [7]:
- Participant Preparation: Recruit a cohort of healthy adults with no known gait abnormalities. Obtain informed consent and record demographic and anthropometric data.
- Equipment Setup: Ensure all platforms and in-shoe systems are calibrated according to manufacturer specifications immediately prior to data collection. For inter-device reliability, use multiple platforms of the same and different manufacturers.
- Data Collection: Participants should complete a minimum of 10 satisfactory walking trials per condition. Use the two-step method to collect data, where the target foot lands on the sensing area on the second step to avoid targeting behavior and ensure natural gait.
- Variables Analyzed: Extract key parameters from the processed data for the whole foot and specific anatomical regions (e.g., hallux, metatarsal heads, heel). Core metrics include:
- Peak Pressure (PP)
- Pressure-Time Integral (PTI)
- Contact Area
- Maximum Force
- Center of Pressure Excursion Index (CPEI)
- Statistical Analysis: Calculate Intraclass Correlation Coefficients (ICCs) to determine intra-device and inter-device reliability. An ICC greater than 0.70 is generally considered acceptable, with values over 0.90 indicating excellent reliability [6].
Future Directions: AI and Advanced Sensor Technology
The future of plantar pressure sensor calibration and analysis is moving toward intelligent automation. There is clear potential for AI techniques to assist in the analysis and interpretation of complex plantar pressure data, which could lead to more automated clinical diagnoses and monitoring [1] [2]. Furthermore, material science is driving innovation with novel sensors, such as high-density, screen-printed piezoresistive arrays using carbon-based nanomaterials. These sensors offer remarkable sensitivity, flexibility, and cost-effective manufacturing, paving the way for more accessible and high-resolution monitoring systems [9]. Integrating these advanced sensors with wireless communication protocols like Bluetooth Low Energy (BLE) enables the development of truly mobile, wearable systems for long-term monitoring outside the lab [9] [7].
In foot plantar pressure research, calibration is not merely a recommended best practice but a fundamental prerequisite for generating valid, reliable, and clinically meaningful data. Plantar pressure measurement systems provide crucial information about the pressure field between the foot and supporting surface during locomotor activities, with applications spanning from diagnosing lower limb problems and footwear design to sport biomechanics and injury prevention [4]. The accuracy of these measurements directly impacts clinical decisions, making proper calibration non-negotiable for both research integrity and patient outcomes.
Without rigorous calibration protocols, measurement errors can propagate through data analysis pipelines, potentially leading to flawed conclusions about foot function, inappropriate therapeutic interventions, and compromised patient safety. This article establishes why calibration is indispensable through technical specifications, experimental evidence, and practical troubleshooting guidance for researchers working with plantar pressure measurement systems.
Technical Foundations: Plantar Pressure System Requirements
System Types and Configurations
Plantar pressure measurement systems generally fall into two primary categories, each with distinct calibration considerations:
Platform Systems: Constructed from flat, rigid arrays of pressure sensing elements arranged in a matrix configuration and embedded in the floor. These systems are typically used for both static and dynamic studies but are generally restricted to laboratory environments due to their stationary nature [4].
In-Shoe Systems: Feature flexible sensors embedded within footwear, measuring the interface between the foot and shoe. These portable systems enable studies across various gait tasks, footwear designs, and terrains but may have lower spatial resolution compared to platform systems and require careful sensor securing to prevent slippage [4].
Key Metrological Requirements
For any plantar pressure measurement system, several performance characteristics must be calibrated and maintained within specified tolerances [4]:
Linearity: The sensor's response should be proportional to the applied pressure throughout its measurement range. High linearity simplifies signal processing circuitry and improves measurement accuracy.
Hysteresis: This refers to the difference in sensor output when pressure is applied versus when it is released. Minimal hysteresis ensures consistent readings regardless of loading history.
Temperature Sensitivity: Sensors must maintain calibration across typical operating temperatures (20°C-37°C) encountered during human movement studies.
Pressure Range: Systems must be calibrated for the specific pressure ranges expected in target applications, from normal gait to pathological conditions.
Quantitative Evidence: Calibration Impact on Data Reliability
Consequences of Improper Calibration
Research demonstrates that calibration methodologies significantly impact measurement accuracy. A recent investigation into in-shoe plantar shear stress sensors revealed that calibration with different indenter areas (ranging from 78.5 mm² to 707 mm²) and varying positions (up to 40 mm from sensor center) produced measurement variations of up to 80% and 90%, respectively [10]. These findings highlight how seemingly minor calibration protocol deviations can profoundly affect data validity.
Reliability Metrics for Plantar Pressure Systems
Recent studies have established test-retest reliability metrics for properly calibrated wearable plantar pressure systems:
Table 1: Reliability Metrics for a Wearable Plantar Pressure System Across Different Walking Conditions
| Walking Condition | Intraclass Correlation Coefficient (ICC) | Minimum Distance for ICC ≥0.90 | Key Parameters Measured |
|---|---|---|---|
| Linear Walking | ~0.9 | 207 meters | Peak Pressure (PP), Pressure-Time Integral (PTI), Full Width at Half Maximum (FWHM) |
| Clockwise Curved Walking | ~0.9 | 255 meters | Maximum Pressure Gradient (MaxPG), Average Pressure (AP) |
| Counterclockwise Curved Walking | ~0.9 | 467 meters | Measurements across 8 foot regions |
The system demonstrated excellent reliability for most parameters across all walking conditions when proper calibration was maintained, with all variables presenting ICCs >0.60 for whole-foot analysis [7].
Sensor Performance Specifications
Table 2: Typical Technical Specifications for Plantar Pressure Measurement Systems
| Parameter | Platform Systems | In-Shoe Systems | Impact of Poor Calibration |
|---|---|---|---|
| Spatial Resolution | High (matrix configuration) | Lower (fewer sensors) | Misalignment of pressure points |
| Sampling Frequency | Up to 100 Hz | ~4 Hz to 20 Hz | Failure to capture peak pressures |
| Pressure Range | 1-112 mmHg | 10-75 mmHg | Data clipping or insufficient resolution |
| Sensor Hysteresis | Minimal | Varies by technology | Inconsistent loading/unloading data |
| Temperature Sensitivity | Compensated | Often uncompensated | Drift during prolonged use |
Calibration Protocols and Methodologies
General Calibration Workflow
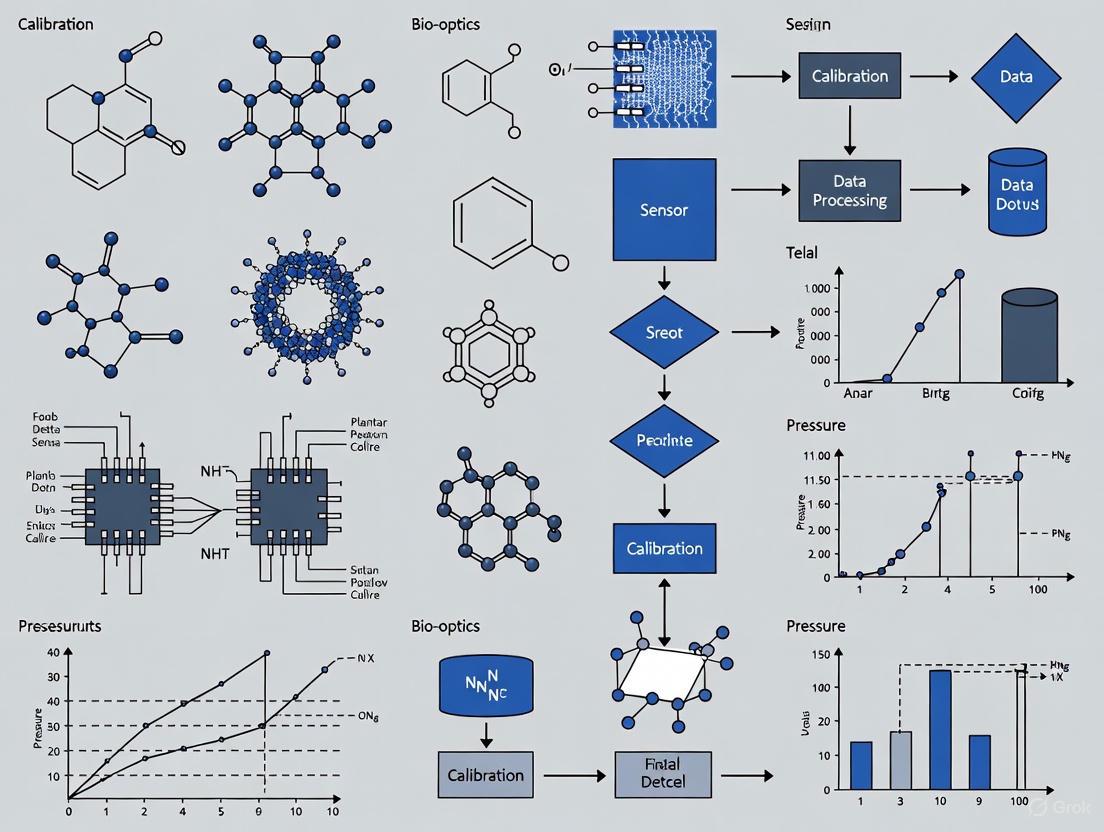
The following diagram illustrates a comprehensive calibration workflow for plantar pressure measurement systems:
Anatomically-Specific Calibration Protocol
For in-shoe systems, calibration should account for anatomical variations across foot regions:
Sensor-Specific Calibration: Calibrate each sensor individually rather than applying uniform calibration factors across all sensors [10].
Region-Specific Loading: Apply calibration forces that approximate the expected loading patterns for specific anatomical regions (heel, metatarsal heads, toes).
Indenter Selection: Use calibration indenters with surface areas and geometries that match the anatomical structures applying pressure to each sensor region.
Mechanical Coupling: Account for the mechanical coupling between embedded sensors and insole materials during calibration [10].
Validation Against Gold Standard Systems
When introducing new plantar pressure devices, comparative validation against established gold standard systems is essential. One study comparing a novel plantar sensory replacement unit (PSRU) to a gold standard pressure-sensing device (Pedar-X) found:
- Good-to-very-good correlations (r-value range 0.67-0.86) for six out of eight PSRU sensors
- Poor correlation for two sensors (r=0.41, p=.15; r=0.38, p=.18) when measuring pressures greater than 32 mmHg [11]
These results highlight that even within the same system, calibration quality may vary across individual sensors, necessitating comprehensive validation protocols.
Troubleshooting Guide: Common Calibration Issues and Solutions
Frequently Asked Questions
Q1: Our plantar pressure measurements show unexpected variations between testing sessions. What could be causing this?
A: Test-retest variations can stem from multiple sources:
- Environmental factors: Temperature fluctuations can affect sensor sensitivity, particularly in piezoresistive systems. Maintain stable laboratory conditions (20°C-24°C) [4].
- Sensor drift: Some sensor technologies exhibit time-dependent drift. Implement regular recalibration schedules based on manufacturer recommendations and usage intensity.
- Donning consistency: For in-shoe systems, variations in how sensors are positioned and secured can affect measurements. Use standardized donning procedures.
- Insufficient acclimation: Participants may need 1-2 minutes to adjust to wearing the measurement system before data collection begins [7].
Q2: How often should we calibrate our plantar pressure measurement system?
A: Calibration frequency depends on:
- Manufacturer specifications: Always follow recommended intervals (typically every 6-12 months for formal metrological calibration).
- Usage intensity: Systems used heavily may require more frequent calibration.
- Criticality of measurements: For clinical applications, pre-study verification is recommended.
- Environmental conditions: Systems exposed to temperature extremes or mechanical shocks need more frequent calibration.
- Evidence of drift: Implement routine verification checks between formal calibrations.
Q3: What is the appropriate number of steps needed for reliable plantar pressure assessment?
A: The required number of steps varies by walking condition:
- Linear walking: Minimum 207 meters of walking distance [7]
- Clockwise curved walking: Minimum 255 meters [7]
- Counterclockwise curved walking: Minimum 467 meters [7] For treadmill-based assessments, other studies suggest 400 steps may be necessary for accurate measurement of step length variations [7].
Q4: How does calibration affect the ability to detect clinically significant changes in plantar pressure?
A: Proper calibration directly impacts the minimal detectable change (MDC) - the smallest change that represents a true difference rather than measurement error. Well-calibrated systems demonstrate:
- Higher intraclass correlation coefficients (ICCs >0.9) [7]
- Reduced measurement variability (<21% during 15-minute walking trials) [10]
- Improved accuracy (mean absolute error <±18 kPa in benchtop tests) [10] This enhanced precision enables researchers and clinicians to detect smaller, clinically meaningful changes in plantar pressure distribution.
Q5: What are the key differences between calibrating platform systems versus in-shoe systems?
A:
Table 3: Calibration Differences Between Platform and In-Shoe Systems
| Calibration Aspect | Platform Systems | In-Shoe Systems |
|---|---|---|
| Reference Standards | Certified pressure mats or force plates | Known weights with specific indenters |
| Environmental Controls | Laboratory conditions with stable temperature | Variable conditions during use |
| Spatial Verification | Grid-based uniformity assessment | Individual sensor verification |
| Temperature Compensation | Often built-in | May require manual compensation |
| Wear Considerations | Minimal | Regular replacement due to material degradation |
Advanced Troubleshooting Scenarios
Scenario 1: Consistent underestimation of peak pressures in specific foot regions
- Potential cause: Sensor saturation or non-linear response in high-pressure ranges
- Solution: Implement multi-point calibration covering the entire expected pressure range, with additional calibration points in high-pressure regions
- Verification: Test with known weights approximating peak pressures (often 500-800 kPa in metatarsal regions)
Scenario 2: Discrepancies between laboratory and field measurements
- Potential cause: Temperature dependence of sensor characteristics
- Solution: Characterize temperature sensitivity and implement temperature compensation algorithms
- Verification: Collect simultaneous temperature data during field measurements
Scenario 3: Progressive signal drift during prolonged data collection
- Potential cause: Material creep in sensor elements or embedding materials
- Solution: Pre-condition sensors with loading cycles before calibration
- Verification: Implement periodic zeroing during extended data collection sessions
Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for Plantar Pressure Sensor Calibration
| Item | Specification | Function/Application |
|---|---|---|
| Certified Calibration Weights | Class M1 or better, various masses | Providing known forces for static calibration |
| Calibration Indenters | Various surface areas (78.5-707 mm²) and geometries | Simulating anatomical loading patterns |
| Force Plate/Reference System | Minimum accuracy 0.5% FS | Gold standard validation |
| Temperature Control Chamber | Range: 15°C-40°C, stability ±0.5°C | Temperature sensitivity characterization |
| Signal Conditioning Equipment | 24-bit ADC, appropriate sampling rates | High-fidelity signal acquisition |
| Mechanical Test Fixtures | Capable of applying combined normal/shear loads | Shear stress sensor calibration [10] |
| Reference Pressure Mats | Certified accuracy, spatial resolution <1cm² | Cross-validation of pressure distribution |
Calibration represents the fundamental link between raw sensor outputs and scientifically valid, clinically useful plantar pressure data. As demonstrated through the technical specifications, experimental evidence, and troubleshooting guidelines presented in this article, rigorous calibration protocols are non-negotiable for ensuring data validity and generating reliable clinical outcomes. The continued advancement of plantar pressure research depends on unwavering commitment to metrological rigor throughout the data collection and analysis pipeline.
By implementing the comprehensive calibration framework outlined here—including anatomical-specific protocols, regular verification schedules, and systematic troubleshooting approaches—researchers can ensure their plantar pressure measurements maintain the accuracy and reliability required for both scientific discovery and clinical application.
The table below summarizes the core characteristics of piezoresistive, capacitive, and piezoelectric sensor technologies.
| Characteristic | Piezoresistive | Capacitive | Piezoelectric |
|---|---|---|---|
| Fundamental Principle | Change in electrical resistance under strain [12] | Change in electrical capacitance from diaphragm movement [12] | Generation of an electric charge under applied force [12] [13] |
| Output Signal | Change in resistance (typically measured via voltage from a Wheatstone bridge) [12] | Change in capacitance or resonant frequency [12] | High-impedance electrostatic charge [13] |
| Response to Static Load | Excellent; provides stable output for constant loads [12] | Excellent; suitable for static pressure measurement [12] | Poor; inherent charge leakage prevents static load measurement [12] [13] |
| Response to Dynamic Load | Good; response time typically <1ms [12] | Good; response time in the order of milliseconds [12] | Excellent; ideal for dynamic and impact forces, with very fast response [12] [13] |
| Key Advantages | Linear output, simple construction, robust, high-pressure range capability [12] | Low power, robust, tolerant of overpressure, good for low-pressure applications [12] | Robust, self-powered, high-temperature tolerance, high-frequency response [12] |
| Key Limitations | Temperature sensitive, requires external power, scaling limitations [12] | Non-linear output (can be corrected), sensitive to stray capacitance and vibration [12] | Cannot measure static forces, sensitive to vibration/acceleration, requires special low-noise cables (charge mode) [12] [13] |
Troubleshooting Guides
FAQ: Piezoresistive Sensor Issues
Q: My piezoresistive sensor output is drifting significantly with ambient temperature changes. What could be wrong? A: Temperature drift is a known disadvantage of piezoresistive sensors [12]. First, verify that your sensor has built-in temperature compensation. If it does, ensure you are operating within the specified temperature range. For precise measurements, perform a system calibration at the expected operating temperature or implement your own temperature compensation algorithm in software based on sensor-specific data.
Q: The sensor has no output or an unstable reading. What are the initial checks? A: Follow these steps [14]:
- Visual Inspection: Check for physical damage like cracks or corrosion.
- Wiring: Ensure all connections are secure and correctly wired according to the datasheet.
- Power Supply: Verify the sensor is receiving the correct and stable supply voltage with a multimeter.
- Pressure Source: Apply a known, calibrated pressure to the sensor and compare the output to the expected value.
FAQ: Capacitive Sensor Issues
Q: The readings from my capacitive sensor are non-linear, especially at lower pressures. Is the sensor faulty? A: Not necessarily. The fundamental principle of a capacitive sensor leads to a non-linear output because the capacitance is inversely proportional to the gap between electrodes [12]. Many capacitive sensors, particularly MEMS devices, have built-in signal conditioning circuits that linearize the output. Check the sensor datasheet for its linearity specifications. For raw sensing elements, linearization must be performed in software.
Q: My capacitive system is prone to noise and erratic signals. What should I investigate? A: Capacitive sensors are highly susceptible to stray capacitance and electromagnetic interference [12]. To mitigate this:
- Keep the signal conditioning electronics as close to the sensing element as possible.
- Use shielded cables and ensure proper grounding.
- Verify that the design of your system minimizes the length of unshielded traces or wires connected to the sensor.
FAQ: Piezoelectric Sensor Issues
Q: I am trying to measure a constant force, but the output from my piezoelectric sensor decays to zero. Why? A: This is normal behavior and the primary limitation of piezoelectric sensors. They generate a charge only when the force is changing and cannot be used for true static measurements [12] [13]. The inherent electrical insulation is finite, so the generated charge will slowly leak away [13]. For long-duration, quasi-static measurements, use a sensor with a very long discharge time constant (DTC) and a charge amplifier with a long time constant setting [13].
Q: The low-frequency response of my ICP piezoelectric sensor system is poor. What factors affect this? A: The low-frequency response is governed by the system's discharge time constant (DTC). For ICP sensors, you must consider two factors [13]:
- Sensor DTC: This is a fixed value determined by the internal electronics of the sensor itself (check the datasheet).
- Coupling Circuit DTC: The AC-coupling capacitor in your signal conditioner or data acquisition system creates another high-pass filter. The system DTC is dominated by the shortest of these time constants. To improve low-frequency response, use a sensor with a long DTC and ensure your signal conditioner supports DC coupling or has a very long AC-coupling time constant.
Q: My charge-mode piezoelectric sensor system is producing noisy data. What is the likely cause? A: This is often caused by triboelectric noise [13]. Standard coaxial cable generates electrical noise when flexed. For charge-mode systems, you must always use special "low-noise" cable, which has a conductive lubricant layer to minimize this effect [13]. Also, ensure the sensor, connector, and cable are clean and dry, as moisture and dirt can provide a path for the charge to leak, causing signal drift [13].
Experimental Protocols for Plantar Pressure Research
Protocol 1: Sensor Selection & Characterization for an In-Shoe System
This protocol outlines the steps for selecting and validating sensors for foot plantar pressure measurement.
1. Define Application Requirements:
- Objective: Determine if the goal is dynamic impact analysis (e.g., running) or static/postural assessment [15].
- Sensor Type: Choose between in-shoe systems (for gait with footwear) platform systems (for barefoot analysis) [4] [15].
- Key Specifications: Based on your objective, define required pressure range, linearity, hysteresis, and sampling frequency [4].
2. Pre-Calibration Characterization:
- Linearity & Hysteresis Test: Using a calibrated materials tester or precision weights, apply known pressures from zero to maximum and back to zero. Record the sensor output at each step. Plotting the output versus input will reveal linearity and hysteresis (the difference between loading and unloading curves) [4].
- Temperature Sensitivity Test: Place the sensor in a thermal chamber and record the output under a constant load while varying the temperature across the expected range (e.g., 20°C to 37°C for biomechanical applications) [4].
3. Sensor System Integration:
- Placement: Based on foot anatomy, place sensors in key areas: heel, midfoot, metatarsal heads, and toes [4] [16]. A common model uses 15 sensors per foot [4].
- Data Acquisition: Interface sensors with a microcontroller (e.g., Arduino MEGA) and data acquisition software (e.g., LabVIEW) to convert raw voltage signals into pressure values [16].
Protocol 2: In-Situ Calibration of a Plantar Pressure Measurement System
This protocol ensures measurements are accurate after the system is built and installed in a shoe.
1. Equipment:
- Your integrated in-shoe sensor system.
- A calibrated, standalone force plate or load cell.
- A subject and a stable platform.
2. Procedure:
- Step 1: Have the subject stand perfectly still on the calibrated force plate, which measures the true total ground reaction force (Body Weight, BW).
- Step 2: Simultaneously, record the output from all sensors in the in-shoe system.
- Step 3: The sum of the pressures from all in-shoe sensors (converted to force) should equal the total force measured by the force plate.
- Step 4: Apply a calibration factor to each in-shoe sensor (or to the system's sum) to ensure the total measured force matches the known force from the plate. This can be done at multiple load levels (e.g., by having the subject shift weight) to create a multi-point calibration.
3. Validation:
- Have the subject perform a different activity (e.g., a slow heel raise) and check that the force data from the in-shoe system remains physiologically plausible when compared to the known dynamics of the movement.
The Scientist's Toolkit
Essential Research Reagents & Materials
The table below lists key components for developing a foot plantar pressure measurement system, as referenced in the research.
| Item | Function / Explanation |
|---|---|
| FSR 402 Sensors | A specific model of force-sensing resistor (piezoresistive); thin, flexible, and used in many low-cost, high-sensor-count plantar pressure platforms [16]. |
| Arduino MEGA 2560 Microcontroller | A common, programmable microcontroller board used to read analog voltage outputs from an array of sensors (e.g., FSRs) before sending data to a computer [16]. |
| LabVIEW with DAQ Hardware | Data acquisition (DAQ) software and hardware from National Instruments; widely used in research for configuring sensor input, real-time data processing, visualization, and logging [16]. |
| Low-Noise Cable | Specialized cable required for piezoelectric charge-mode sensors. Contains a conductive lubricant to minimize "triboelectric noise" generated by cable movement [13]. |
| Charge Amplifier | An electronic circuit that converts the high-impedance charge output from a piezoelectric sensor into a low-impedance voltage signal. Essential for quantitative measurement [12] [13]. |
| ICP Signal Conditioner | A constant current power source/signal conditioner for Integrated Electronics Piezoelectric (ICP) sensors. Provides the required power and decouples the AC signal from the sensor's DC bias voltage [13]. |
Sensor Operational Principles
Systematic Calibration Workflow
Key Metrics for Plantar Pressure Sensor Calibration
For researchers calibrating foot plantar pressure sensors, three metrics are paramount for ensuring data validity and reliability. Their definitions and importance in a calibration context are summarized below.
| Metric | Definition in Calibration Context | Impact on Data Quality & Research Outcomes |
|---|---|---|
| Accuracy | The closeness of agreement between a sensor's pressure reading and a true, reference value traceable to a standard [1] [17]. | Ensures clinical and biomechanical conclusions are valid. Poor accuracy can lead to misdiagnosis, incorrect athletic form assessment, and flawed research data [18]. |
| Sensitivity | The minimum change in pressure a sensor can detect, often expressed as the magnitude of output signal change per unit of applied pressure (e.g., -0.322 kPa⁻¹) [9]. | High sensitivity allows detection of subtle gait events and pressure variations, which is crucial for detailed biomechanical analysis and early-stage pathology identification [9]. |
| Spatial Resolution | The density of individual sensing elements per unit area (e.g., 4 sensors/cm²) [8]. Determines the fineness of the pressure distribution "image" [9]. | Low resolution forces interpolation of data, obscuring critical localized pressure points (e.g., under a metatarsal head). High resolution enables precise Center of Pressure (CoP) tracking [9] [1]. |
Troubleshooting Common Sensor Issues
Q1: My sensor system shows a persistent zero offset, providing a positive reading even when no pressure is applied. What could be the cause and how can I resolve it?
- Potential Causes: Residual pressure in the system, temperature fluctuations, mechanical stress on the sensor from improper mounting, or inherent manufacturing tolerances [17] [18].
- Troubleshooting Steps:
- Initial Check: Perform a zero balance check with the sensor at ambient conditions and confirmed zero pressure [17].
- Visual Inspection: Check for physical damage, corrosion, or loose connections [14].
- Re-mount/Re-seat: Ensure the sensor is mounted correctly per manufacturer guidelines, without misalignment or excessive torque that could cause stress [17].
- Recalibrate: If the hardware is intact, perform a zero calibration to correct the offset [18].
Q2: After a period of use, the sensor's output has become unstable or drifts over time, especially during long monitoring sessions. What should I investigate?
- Potential Causes: Temperature drift due to changes in ambient conditions or body heat, low battery power in wireless systems, electrical noise interference, or contamination of the sensor elements [14] [18].
- Troubleshooting Steps:
- Power Supply: Verify the sensor or data acquisition unit is receiving a stable and correct supply voltage. For wireless systems, ensure batteries are fully charged [14] [19].
- Environmental Factors: Check for sudden changes in room temperature or humidity. For in-shoe sensors, sweat can be a factor; some systems are more robust to humid conditions than others [14].
- Signal Check: Investigate potential sources of electrical interference from nearby equipment. Ensure all cabling and connectors are secure [14] [20].
- Routine Calibration: Implement a routine calibration schedule (e.g., every 6–12 months) to correct for drift due to ageing or cyclic stress [17].
Q3: My high-resolution sensor array is showing a slow or delayed response during dynamic gait activities. How can I diagnose this issue?
- Potential Causes: Problem with the sensor's internal electronics, insufficient sampling rate setting, or issues with the data transmission system (e.g., Bluetooth latency) [14] [19].
- Troubleshooting Steps:
- Check Sampling Rate: Ensure the system is configured for a sufficiently high sampling rate. For running or other high-speed motions, 100 Hz or more may be required, whereas 10 Hz might suffice for slow walking [19].
- Wiring/Connectivity: For wired systems, check connections for corrosion or damage. For wireless systems, ensure a strong, stable connection and check for data packet loss [14] [19].
- Sensor Self-Check: Some advanced insole systems feature continuous self-checks; consult the system's software for any diagnostic alerts [19].
Experimental Protocols for Calibration and Validation
Multi-Point Calibration Protocol for Accuracy and Linearity
To ensure accuracy across the entire expected pressure range, a multi-point calibration is essential. This protocol is designed to identify and correct for zero offset, span offset, and non-linearity errors [17].
Title: Multi-Point Calibration Workflow
Procedure:
- Preparation: Use a calibrated pressure source (e.g., pneumatic or mechanical tester) with a certificate of calibration traceable to international standards (e.g., ISO/IEC 17025) [17]. Ensure the sensor and environment are at a stable, controlled temperature.
- Zero Point: With no load applied, record the sensor's output. This identifies the zero offset [17] [18].
- Increasing Pressure Cycle: Apply known pressures at a minimum of 5 points (e.g., 0%, 25%, 50%, 75%, 100% of the sensor's full-scale range) and record the output at each step. This characterizes the sensor's linearity and identifies span offset at full scale [17].
- Decreasing Pressure Cycle (Optional): For a more rigorous calibration, repeat the pressure application in descending order. The difference between readings at the same pressure during loading and unloading indicates hysteresis error [17].
- Data Processing: The calibration software uses all recorded data points to construct a transfer function (calibration curve) that converts raw sensor output into accurate pressure values.
Protocol for Validating Spatial Resolution in Gait Analysis
This protocol validates whether a system's spatial resolution is sufficient for capturing critical gait features.
Procedure:
- Setup: Use a high-resolution pressure sensing walkway (as a reference) with a density of 4 sensors/cm² or higher [8]. Simultaneously, fit the subject with the in-shoe sensor system to be validated.
- Data Collection: Have the subject walk at a self-selected pace across the walkway while wearing the instrumented insoles. The walkway captures barefoot steps, while the insoles capture in-shoe pressure.
- Analysis: For the in-shoe system, assess its ability to resolve key anatomical landmarks from the pressure map, such as the hallux, 1st and 5th metatarsal heads, and the heel. Compare the sharpness of these features and the smoothness of the Center of Pressure (CoP) trajectory to the high-resolution walkway data. A system with insufficient resolution will show blurred landmarks and a CoP path with fewer, more abrupt data points [9] [1].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and equipment essential for the calibration and experimental use of plantar pressure sensors.
| Item Name | Function/Application | Technical Specifications & Variants |
|---|---|---|
| Calibrated Pressure Source / Tester | Applies known, precise pressures to sensors for calibration. Serves as the reference standard. | Types: Pneumatic (for low pressures), hydraulic (for high pressures), mechanical deadweight testers (gold standard). Must have a valid calibration certificate traceable to NIST or similar bodies [17]. |
| High-Resolution Pressure Sensing Walkway | Provides a reference for validating the spatial accuracy of in-shoe systems during dynamic tasks like gait. | Example: 1.2m x 3.6m runway with 240 x 720 sensors (4 sensors/cm²) [8]. Used for barefoot pressure analysis and as a benchmark. |
| Screen-Printed Piezoresistive Sensor Array | The core sensing element in many advanced research insoles. Converts mechanical pressure into a measurable change in electrical resistance [9]. | Example: 173 sensors on a flexible printed circuit board (fPCB) using a Carbon-Epoxy-Elastomer (CE2) ink. Offers high sensitivity (-0.322 kPa⁻¹) and flexibility [9]. |
| Wireless Data Acquisition (DAQ) System | Enables untethered, real-world data collection from sensor insoles, critical for capturing natural gait. | Features: Bluetooth Low Energy (BLE) for real-time transmission, onboard memory for standalone recording, IMU integration for motion context, and synchronization capabilities with other MOCAP systems [19]. |
| Trimmable In-Shoe Sensor | Allows for a custom fit within different shoe sizes and types, ensuring the sensor placement is consistent and comfortable for the subject. | Example: Sensors can be trimmed to fit up to a men's size 14 shoe. Cutting must avoid damaging the conductive silver traces and sensing elements [21]. |
The pursuit of peak athletic performance and injury prevention increasingly relies on data from sophisticated measurement systems like plantar pressure sensors and motion capture technologies. However, a significant "calibration gap" exists between standardized laboratory calibration procedures and the dynamic, high-intensity movements characteristic of sports. This gap can compromise data reliability, leading to flawed conclusions and suboptimal interventions. This technical support center addresses why bespoke, sport-specific calibration protocols are essential and provides researchers with the tools to implement them.
Core Problem: Traditional calibration methods often fail under sporting conditions due to factors like:
- High Loading Rates: Sporting movements (e.g., sprinting, jumping) exert forces far exceeding those in standard walking calibrations [1] [2].
- Environmental Variability: Conditions in aquatic, outdoor field, and indoor court environments differ vastly from controlled labs [22].
- Dynamic & Unpredictable Movements: Athletic motions involve complex, multi-directional forces that generic protocols do not capture [22].
Understanding the Technology and Its Limits
Plantar pressure measurement is a key tool for assessing foot function and locomotion in sports and health [1] [2]. Researchers typically use two main types of systems:
| System Type | Best For | Key Strengths | Major Limitations |
|---|---|---|---|
| Rigid Pressure Platforms [1] [2] | Barefoot assessment in lab settings; standing, walking. | High accuracy; high spatial resolution and sampling frequency. | Limited to lab environment; not for use with footwear. |
| In-shoe Pressure Systems [1] [2] | Field-based measurements during dynamic sports; assessing footwear/orthotics. | Wireless, portable; allows multiple steps in realistic conditions. | Lower spatial resolution and sampling frequency than platforms. |
Quantifying system performance under realistic conditions is crucial. The table below summarizes accuracy metrics for related motion capture technologies, illustrating the performance variations across different environments [22]:
| Technology | Typical Accuracy | Key Environmental Challenges |
|---|---|---|
| Optical Marker-Based Systems | Sub-millimeter positional accuracy [22] | Controlled lab environments; reflections and marker occlusion in the field [22]. |
| Inertial Measurement Unit (IMU) Systems | 2–8° angular accuracy [22] | Performance varies with movement complexity [22]. |
| Markerless Computer Vision Systems | Sagittal plane: 3–15°; Transverse plane: 3–57° [22] | Variable accuracy, especially in transverse plane [22]. |
| GNSS-Integrated Tracking | ±0.3–3 m positional accuracy [22] | Performance challenges in outdoor fields [22]. |
Troubleshooting Guides
Guide 1: Addressing Inconsistent Data During High-Impact Activities
Problem: Plantar pressure data becomes noisy or unreliable during movements like sprinting or landing from a jump.
Solution: Implement a dynamic calibration protocol that matches the loading rates of your sport.
- Verify Manufacturer's Calibration Specifications: Check the dynamic loading rates used by the manufacturer for calibration. Many testing machines use loading rates "less than even those found in walking" [2].
- Develop a Bespoke Calibration: If the factory calibration is insufficient, create a custom procedure. This involves:
- Cross-Validate with a Supplementary System: In the lab, use a force plate or a high-speed motion capture system (e.g., optical marker-based) simultaneously with your in-shoe sensors during sport-specific tasks. This provides a "gold-standard" reference to check the accuracy of your pressure data [22] [24].
Guide 2: Managing Data Artifacts from Environmental Factors
Problem: Data is affected by factors like temperature, moisture (sweat/water), or uneven flooring.
Solution: Proactively control and document environmental variables.
- For Aquatic Sports or High-Sweat Conditions:
- Use sensors with waterproofing or moisture-wicking interfaces.
- Conduct pre- and post-session calibration checks in the same environment to quantify drift. IMU systems, for example, can show an additional 2° orientation error in aquatic settings [22].
- For Outdoor Field Testing:
- Be aware that systems like GNSS can have positional accuracy from ±0.3m to 3m [22].
- Note the ground surface (e.g., artificial turf vs. natural grass) and weather conditions in your metadata, as these can affect both the sensor and the movement itself.
Guide 3: Ensuring Results are Reproducible Across Multiple Sites
Problem: A study involving multiple labs or testing locations yields inconsistent results.
Solution: Standardize protocols and equipment across all sites, focusing on reproducibility.
- Create a Detailed Standard Operating Procedure (SOP): Document every step, including:
- Sensor Preparation: Exact sensor placement and securing method within the shoe.
- Subject Preparation: Standardized footwear and warm-up routine.
- Data Collection Protocol: The exact sequence of movements (e.g., "three consecutive jumps at maximal effort").
- Conduct Inter-Site Reliability Testing: Have a small group of athletes perform the same protocol at each testing site. Analyze the data to ensure consistency (low inter-site variability) before beginning the full study [24].
Frequently Asked Questions (FAQs)
Q1: Why can't I just use the manufacturer's standard calibration for my sports study? Standard calibrations are often designed for clinical applications like walking or standing. Sporting movements involve much higher forces, faster loading rates, and different foot strike patterns. Using a generic calibration can lead to significant under-reporting of peak pressures and inaccurate data [1] [2].
Q2: How often should I re-calibrate my pressure measurement system? The frequency depends on usage intensity. For daily research use with high-impact activities, a weekly verification check is recommended. Perform a full calibration before starting a new study or if you suspect the system has been subjected to a physical shock. Always follow manufacturer guidelines as a minimum standard.
Q3: What is the difference between repeatability and reproducibility, and why does it matter?
- Repeatability is about getting consistent results when the same user measures the same subject multiple times under identical conditions.
- Reproducibility is about getting consistent results across different users, different locations, or over time. In sports science, both are critical. High repeatability ensures your internal data is reliable. High reproducibility allows other researchers to trust and build upon your findings [24].
Q4: How can AI help with the analysis of plantar pressure data? AI and machine learning techniques have clear potential to assist in analyzing complex pressure data. They can help identify subtle patterns related to injury risk or performance optimization that might be missed by traditional analysis, enabling more complete use of the rich dataset these systems generate [1] [2].
Experimental Protocols for Bespoke Calibration
Protocol 1: Sport-Specific Dynamic Calibration
Objective: To calibrate an in-shoe plantar pressure system for forces and loading rates typical of basketball vertical jumps.
Materials:
- In-shoe pressure measurement system.
- High-capacity materials testing machine (e.g., Instron).
- A calibrated force plate (for cross-validation).
Workflow:
- Setup: Place the sensor or insole in the testing machine, ensuring even contact.
- Parameter Setting: Program the machine to apply a loading profile that mimics the impact force and rate observed in a basketball jump. This profile should be based on pilot data from force plates.
- Data Collection: Run multiple cycles (e.g., 20-30) to ensure sensor reliability.
- Validation: Have an athlete perform vertical jumps on a force plate while wearing the calibrated in-shoe system. Compare the peak force and loading rate from both systems to validate the calibration.
The following workflow outlines the key stages of this protocol:
Protocol 2: Multi-Site Reproducibility Assessment
Objective: To ensure a plantar pressure protocol for running gait analysis yields consistent results across three different research laboratories.
Materials:
- Identical in-shoe pressure systems at each site.
- Standardized running shoes.
- A treadmill.
Workflow:
- SOP Development: Create a detailed protocol document covering sensor placement, shoe model, treadmill speed/incline, and data output requirements.
- Centralized Training: Train all technicians from the three sites on the SOP.
- Test with Traveling Subjects: A small cohort of runners visits all three sites and performs the running protocol.
- Data Analysis: Compare key metrics (e.g., center of pressure trajectory, peak heel pressure) across sites using statistical tests for agreement (e.g., ICC). Revise the SOP if reproducibility is low.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in Experiment |
|---|---|
| Rigid Pressure Platform | Provides high-accuracy "ground truth" data for barefoot static or low-dynamic assessments in a lab setting [1] [2]. |
| In-shoe Pressure System | Enables the measurement of plantar pressures in ecological settings during dynamic sporting movements and with footwear [1] [2]. |
| Materials Testing Machine | Used for developing bespoke dynamic calibration protocols by applying controlled, sport-specific loading rates and forces to sensors [1] [2]. |
| Gravimetric Calibration Setup | The primary method for flow measurement traceability; uses precision balances to measure mass over time, providing a foundational reference [23]. |
| High-Speed Cameras | Used for motion capture (e.g., markerless systems) and optical calibration methods (e.g., front track, pending drop) to track movement with high temporal resolution [22] [23]. |
| Force Plates | Integrated with motion capture and pressure data to provide synchronized kinetic (force) information, crucial for validating sensor output during high-impact tasks [22]. |
Key Takeaways for Researchers
- Move Beyond Standard Calibration: For sport science, bespoke protocols matching the movement's intensity and complexity are non-negotiable for data accuracy [1] [2].
- Quantify the Gap: Use frameworks like the STRN Quality Framework to systematically evaluate your technology's accuracy, repeatability, and reproducibility in a sporting context [24].
- Embrace a Multi-Method Approach: No single system is perfect. Combine technologies (e.g., in-shoe sensors with force plates or IMUs) to cross-validate data and gain a more complete biomechanical picture [22].
- Prioritize Reproducibility: Detailed SOPs and inter-site reliability testing are essential for producing credible, collaborative research that can be replicated by others [24].
Implementing Calibration Protocols: From Bench Top to Real-World Application
Standard Dynamic Calibration Procedures and Testing Machines
In foot plantar pressure research, dynamic calibration is a critical process that ensures measurement systems accurately capture the rapid, high-magnitude loads encountered during human locomotion. Unlike static calibration, dynamic calibration validates sensor performance under conditions that simulate real-world gait and athletic movements, accounting for factors like loading rate and impact force. This technical support center document provides researchers, scientists, and drug development professionals with comprehensive guidance on calibration protocols, testing equipment, and troubleshooting for plantar pressure measurement systems. Proper calibration is foundational to obtaining valid and reliable data for applications ranging from footwear design and sports performance to clinical diagnosis and rehabilitation [2] [4].
Frequently Asked Questions (FAQs) on Calibration and Testing
Q1: Why is dynamic calibration specifically necessary for plantar pressure sensors, beyond static calibration? Dynamic calibration is essential because it accounts for the loading rates experienced during actual human movement. Static calibration alone is insufficient for characterizing sensor performance during gait or impact. Research indicates that many testing machines used for dynamic calibration have loading rates lower than those found even in walking, let alone running or jumping [2]. Dynamic calibration ensures the validity and reliability of data collected during dynamic sporting movements and daily activities by verifying sensor response time, hysteresis, and accuracy under realistic loading conditions.
Q2: What are the key performance metrics for a plantar pressure measurement system? When selecting and calibrating a system, researchers should evaluate several critical technical specifications [25] [4] [26]:
- Linearity: Indicates how directly the sensor's output corresponds to the applied pressure. A highly linear sensor simplifies signal processing.
- Hysteresis: The difference in output signal when the sensor is loaded versus unloaded. Lower hysteresis (e.g., <7% as specified for the pedar system) means less energy loss and better accuracy during the cyclic loading of gait [26] [27].
- Sampling Frequency: The rate at which pressure data is captured. For dynamic activities, higher frequencies (e.g., 150 Hz [25] to 400 Hz [26] [27]) are necessary to accurately capture rapid pressure changes.
- Pressure Range: The span of pressures the system can measure. It must be suited to the application, from low pressures in balanced standing to very high pressures in athletic jumps (e.g., ranges up to 1200 kPa are available) [26] [27].
- Spatial Resolution: The number of sensors (sensels) per unit area. Higher resolution provides more detailed pressure maps, which is crucial for identifying localized high-pressure points [25] [4].
Q3: What is the recommended protocol for clinical gait analysis using pressure insoles? For reliable data collection in gait analysis, a standardized protocol is vital. The literature recommends a "two-step" protocol prior to the foot contacting the measurement area [2]. This approach helps ensure that the subject's gait has reached a natural and consistent state before data is recorded, minimizing artifacts from initiation or adjustment steps.
Q4: How often should a plantar pressure measurement system be calibrated? Best practices recommend that systems are factory calibrated before use, and their calibration should be checked by the user regularly using a dedicated calibration device [26] [27]. For example, the pedar system is designed to be used with the trublu calibration device, which allows users to verify and ensure the accuracy and reproducibility of their data at any time [26] [27]. The specific calibration interval may depend on usage intensity and the manufacturer's guidelines.
Dynamic Calibration Procedures & Testing Machines
Standard Calibration Methodologies
Dynamic calibration for plantar pressure sensors involves applying known, rapidly varying pressures to the sensor and correlating the system's output with the reference input. A key challenge in this field is that many existing testing machines operate at loading rates lower than those generated by common human movements, which can lead to an overestimation of system accuracy in real-world scenarios [2]. Therefore, developing calibration protocols that match the loading rates of the target activities (e.g., running, cutting, jumping) is an active area of research and is critical for high-quality studies.
Commercial systems often use dedicated calibration devices. For instance, the pedar system is individually calibrated with the trublu calibration device, which applies a known air pressure to all sensors simultaneously, ensuring each sensor provides accurate and reproducible data [26] [27]. These systems are designed with calibration stability in mind, allowing for the collection of thousands of gait cycles with minimal set-up time and drift [25].
The following table summarizes the technical specifications of several plantar pressure measurement systems as identified in the literature, highlighting the performance parameters relevant to calibration and experimental use.
Table 1: Technical Specifications of Commercial Plantar Pressure Measurement Systems
| System / Feature | Intelligent Insoles | Pro (XSENSOR) | pedar System (novel) |
|---|---|---|
| Primary Use | Gait & motion research, sports performance [25] | In-shoe pressure distribution, versatile applications [26] [27] |
| Calibration Approach | Factory calibrated with proven stability [25] | Individual insole calibration via trublu device [26] [27] |
| Sampling Frequency | Up to 150 Hz [25] | Up to 400 Hz [26] [27] |
| Sensor Resolution (per insole) | Up to 235 sensels [25] | 99 or 175 sensels [26] [27] |
| Hysteresis | Not explicitly stated | < 7% [26] [27] |
| Pressure Range | 0.7-88.3 n/cm² (1-128 psi) [25] | 15-600 kPa or 30-1200 kPa [26] [27] |
| Key Features | Lab-quality data in the field; integrated IMU [25] | High-conformity capacitive sensors; WiFi telemetry; on-board storage [26] [27] |
Workflow for Sensor Setup and Validation
The diagram below outlines a generalized workflow for setting up and validating a plantar pressure measurement system prior to an experiment, incorporating best practices from the literature.
Troubleshooting Common Experimental Issues
Systematic Problem Diagnosis Framework
When experimental data appears erroneous, a structured approach to diagnosis is crucial. The following workflow guides researchers through a logical series of checks to identify the root cause of common pressure measurement problems, from simple connection errors to complex environmental factors.
Troubleshooting Guide: Symptoms, Causes, and Solutions
The table below details specific symptoms, their potential root causes, and recommended corrective actions based on general pressure sensor troubleshooting principles and application-specific challenges in biomechanics research.
Table 2: Plantar Pressure Sensor Troubleshooting Guide
| Symptom | Potential Root Cause | Recommended Solution |
|---|---|---|
| No Output or Unstable Output | - Loose or incorrect wiring [14] [28].- Inadequate or no power supply [14].- Internal sensor failure. | - Verify all electrical connections and wiring according to datasheet [14].- Confirm the sensor is receiving the correct supply voltage with a multimeter [14].- Contact technical support if hardware is suspected to be faulty [14]. |
| Inaccurate Reading / Drift | - Calibration drift over time [28].- Temperature drift due to lack of compensation [14].- Exposure to extreme temperatures or thermal cycling [29]. | - Perform a new calibration using a certified calibration device [26].- Check sensor specifications for temperature compensation range [4].- Allow system to acclimate to lab temperature and protect from rapid temperature changes [29]. |
| Slow or Delayed Response | - Problem with internal electronics or signal conditioning [14].- Clogged pressure port (if applicable) from contamination [14].- Use of an electrical output type (e.g., millivolt) prone to interference over long distances [28]. | - Inspect and clean sensors, ensure no obstructions [14].- For wireless systems, ensure high sampling frequency is selected and check for data transmission lag.- Use voltage or current output systems for better noise immunity in industrial/field environments [28]. |
| Erratic Data During Movement | - Sensor insole slipping or folding inside the shoe.- Low battery power in wireless units.- Electromagnetic interference (EMI) from other lab equipment [29]. | - Secure the insole properly to prevent movement relative to the foot.- Ensure full battery charge before experiments.- Use systems with digital outputs and proper shielding; increase distance from EMI sources [29]. |
The Scientist's Toolkit: Essential Research Reagents & Materials
For researchers designing experiments in foot plantar pressure, having the right "toolkit" is essential for generating valid and reproducible data. The following table lists key equipment and materials as identified in the scientific literature and commercial product documentation.
Table 3: Essential Research Materials for Plantar Pressure Experiments
| Item | Function / Purpose | Representative Examples / Specs |
|---|---|---|
| Calibrated Pressure Insoles | The primary sensor for measuring pressure distribution at the foot-shoe interface. | XSENSOR Intelligent Insoles | Pro [25]; novel pedar insoles [26] [27]. |
| Dedicated Calibration Device | Applies a known, uniform pressure to validate and/or calibrate all sensors on the insole, ensuring accuracy. | novel trublu calibration device [26] [27]. |
| Wireless Data Acquisition Unit | Transmits sensor data without restricting natural movement, crucial for field-based and dynamic activities. | plidar electronics (54g, WiFi, 400 Hz) [26] [27]; XSENSOR systems with on-board memory [25]. |
| Analysis Software | Visualizes, processes, and quantifies pressure data (e.g., peak pressure, force, center of pressure trajectory). | XSENSOR Pro Foot & Gait software [25]; novel Scientific Studio & E-Expert packages [26]. |
| Standardized Testing Platforms | Creates controlled and repeatable conditions for dynamic tasks like stair descent. | Custom steps of varying heights (e.g., 5cm, 15cm, 25cm, 35cm) [30]. |
| Reference Measurement Systems | Provides synchronized biomechanical data for more comprehensive analysis (multi-modal data). | Motion capture systems, force platforms, electromyography (EMG) [26]. |
Technical Support & Troubleshooting Hub
Frequently Asked Questions (FAQs)
Q1: Why is my shear stress sensor measurement inaccurate even after a standard calibration?
A: A primary cause is the use of a generic calibration protocol that does not match the anatomical loading conditions of the foot. Research demonstrates that calibration accuracy is highly sensitive to the indenter area and location used during bench testing. Using an indenter that does not match the size and position of specific foot anatomical structures (like the metatarsal heads) can introduce errors of up to 80-90% [31]. Furthermore, shear and normal stress are coupled; the sensor's response to shear force is influenced by the simultaneous normal load, a factor that must be accounted for in the calibration model [31].
Q2: My data shows poor agreement with other studies. Could the issue be with the measurement system itself?
A: Yes, significant discrepancies exist even between different commercial systems. A systematic comparison of plantar pressure devices revealed poor to moderate agreement, even among devices using similar sensor technologies [32]. The data from different devices should not be used interchangeably [32]. Ensure you are comparing results from the same sensor technology and calibration methodology, and report these details thoroughly in your methods.
Q3: Why do my sensor readings drift during a walking trial?
A: Drift is a common challenge, often linked to the sensor technology and environmental factors. Materials like the elastomers used to embed sensors can exhibit properties like creep and hysteresis [33] [31]. Additionally, temperature and humidity variations inside the shoe can affect sensor output [33]. To mitigate this, precondition the sensors by loading them for a period before calibration and use a calibration method that accounts for time-dependent behavior [33].
Q4: What is the most critical factor for achieving accurate in-shoe shear stress measurements?
A: The consensus across recent research is the mechanical coupling between the embedded shear sensors and the insole materials, and the use of an anatomically-specific calibration method [31]. A generic, one-size-fits-all calibration is insufficient. The calibration must replicate the specific loading profile, area, and location of the anatomical region of interest.
Troubleshooting Guide
| Problem | Possible Cause | Solution |
|---|---|---|
| High variability (>20%) in repeated walking trials | Poor mechanical coupling; sensor shifting inside shoe; inconsistent calibration. | Secure sensor firmly within the insole material. Use an indenter matching the anatomical area for calibration [31]. |
| Shear stress values are consistently unrealistic (too high/too low) | Incorrect calibration factors; normal-shear stress coupling not accounted for. | Re-calibrate using a protocol that decouples normal and shear stress effects. Use the mathematical model: σS = E * kS * (SN+S - SN) / (1 + ε) [31]. |
| Measurements disagree with force platform gold standard | Systemic device error; different sensor technologies; improper calibration method. | Do not expect perfect agreement. Validate your system against a force platform and report the expected error margins [32] [33]. Use a participant weight-based calibration to improve impulse accuracy [33]. |
| Sensor signal is noisy or unstable | Loose electrical connections; environmental interference (temperature, humidity). | Check all wiring and connections. Use shielded cables. Allow the system to acclimate to the testing environment before calibration and data collection [33]. |
Experimental Data & Protocols
Quantitative Calibration Data
The following data, derived from controlled bench tests, highlights the critical parameters for anatomical calibration.
Table 1: Impact of Calibration Indenter Parameters on Measurement Accuracy [31]
| Calibration Parameter | Variation Tested | Effect on Measurement Accuracy |
|---|---|---|
| Indenter Area | 78.5 mm² to 707 mm² | Measurements varied by up to 80% |
| Indenter Position | Up to 40 mm from sensor center | Measurements varied by up to 90% |
| Calibration Method | Anatomically-specific vs. Generic | Anatomical calibration reduced mean absolute error to < ±18 kPa |
Table 2: Comparison of Insole System Calibration Methods [33]
| Calibration Method | Description | Pros & Cons |
|---|---|---|
| Manufacturer's Standard | Proprietary protocol provided by the insole manufacturer. | Pro: Standardized. Con: May lead to significant inaccuracies in impulse values (≈30-50% error). |
| Participant Weight-Based | Uses the participant's body weight to adjust the static calibration. | Pro: Can improve qualitative representation. Con: Can consistently underestimate impulse values. |
| Anatomically-Specific | Uses indenters matching the size/location of foot anatomy. | Pro: Highest accuracy, accounts for real-world loading. Con: More complex and time-consuming. |
Detailed Experimental Protocol: Anatomically-Specific Sensor Calibration
This protocol is designed to minimize the errors identified in the FAQs and tables above.
Objective: To calibrate a plantar shear stress sensor using indenter parameters that match the anatomical region of interest (e.g., first metatarsal head).
Materials:
- Shear stress sensor embedded in silicone insole
- Custom mechanical test rig capable of applying controlled normal and shear forces
- Indenters with various surface areas (e.g., 78.5 mm², 707 mm²)
- Data acquisition system
- Force platform (for optional validation)
Procedure:
- Preconditioning: Cycle the sensor by applying a load equivalent to the expected maximum force for 10-15 cycles to minimize the effects of hysteresis and creep [33].
- Indenter Selection: Select an indenter whose contact area closely matches the surface area of the anatomical structure being studied (e.g., a metatarsal head).
- Normal Stress Calibration:
- Apply normal force to the sensor using the selected indenter in increments from 0% to 100% of the expected load.
- Record the output from the normal stress sensor (NN) at each increment.
- Generate a normal force-to-output voltage calibration curve.
- Shear Stress Calibration:
- Apply a constant normal load (e.g., 50% of maximum).
- Apply shear force in the anterior-posterior and medial-lateral directions in increasing increments.
- Record the output from the shear strain gauge (SN+S) at each increment.
- Repeat for different levels of constant normal load to capture the coupled relationship.
- Positional Sensitivity Mapping:
- Place the indenter at the center of the sensor and perform a normal and shear calibration.
- Offset the indenter by 5mm, 10mm, 20mm, and 40mm and repeat the calibration process to map the positional sensitivity [31].
- Data Processing:
- Use the recorded data to solve for the calibration constants (kN, kS) in the following equation, which decouples the normal and shear effects [31]:
σS = E * kS * (SN+S - SN) / (1 + ε)whereEis the silicone's Young's Modulus andεis the strain.
- Use the recorded data to solve for the calibration constants (kN, kS) in the following equation, which decouples the normal and shear effects [31]:
Workflow Visualization
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Plantar Sensor Research
| Item | Function & Application |
|---|---|
| Strain Gauge Rosette | The core sensing element for measuring shear stress. A 3-element rosette (0°-45°-90°) allows for calculation of resultant shear in both anterior-posterior and medial-lateral directions [31]. |
| Hyperelastic Silicone Elastomer | An incompressible, isotropic embedding material that couples plantar loads to the shear sensor. Its non-linear stress-strain relationship must be characterized for accurate calibration [31]. |
| Custom Mechanical Test Rig | A calibrated system to apply precise and combined normal and shear forces to the sensor-insole assembly during the benchtop calibration process [31]. |
| Anatomically-Matched Indenters | Indenters with varying surface areas and shapes (e.g., circular, elliptical) used to simulate the loading from specific foot anatomical structures during calibration [31]. |
| Calibration Management Software | Software used to document calibration procedures, track intervals, analyze historical drift data, and manage calibration certificates for traceability [34]. |
Troubleshooting Common Sensor and Calibration Issues
Q1: Our screen-printed piezoresistive sensors exhibit significant signal drift over time. What could be causing this and how can we mitigate it?
A: Signal drift in piezoresistive sensors can stem from material instability, poor contact, or environmental factors. To mitigate:
- Material Properties: Ensure the carbon-based nanomaterial ink is thoroughly homogenized before printing to prevent filler sedimentation, which causes inconsistent percolation networks [35] [36].
- Stabilization Cycle: "Condition" new sensors by applying a series of loading and unloading cycles (e.g., 100-1000 cycles at expected operating pressures) to stabilize the conductive network's response before formal data collection [35].
- Environmental Control: Monitor laboratory temperature and humidity, as these can affect the electrical properties of polymeric and carbon-based materials. Conduct calibrations in a controlled environment [32].
Q2: When comparing data from our in-shoe system to a pressure platform, we observe poor agreement in key metrics like peak pressure. Why is this happening?
A: Discrepancies between systems are common and well-documented [32]. Key reasons include:
- Fundamental Design Differences: In-shoe systems and pressure platforms use different sensor technologies, densities, and are used in different conditions (shod vs. barefoot) [1] [32].
- Calibration Protocol Mismatch: The two systems may be calibrated using different protocols and loading rates. Develop a unified, application-specific calibration that mimics the dynamics of your movements, such as sporting actions, if applicable [1].
- Shear Stress: In-shoe systems can experience shear forces that platform systems do not, which may affect sensor output [7]. Ensure sensors are securely fixed within the insole to minimize migration.
Q3: We are getting inconsistent readings between adjacent sensors in our high-density array. What are the likely causes of this crosstalk?
A: Crosstalk in high-density arrays is a known challenge caused by electrical interference or mechanical coupling [37].
- Electrical Isolation: Implement anti-crosstalk designs in your flexible printed circuit board (PCB). This includes using separate ground lines, shielded traces, and sufficient spacing between sensor electrodes [37].
- Mechanical Decoupling: Use a substrate with appropriate stiffness or design isolated sensing elements to prevent force applied to one sensor from mechanically deforming and affecting its neighbor [37]. Research has successfully used polydimethylsiloxane (PDMS) doped with carbon nanotubes to create isolated sensing elements that suppress crosstalk [37].
Q4: What is the minimum number of steps or distance required to obtain reliable plantar pressure data during curved walking experiments?
A: For reliable data in curved walking, the required distance is greater than for linear walking. One study found that to achieve excellent reliability (ICC ≥ 0.90), a minimum distance of 467 meters is recommended for counter-clockwise curved walking, compared to 207 meters for linear walking [7]. Always conduct a reliability analysis for your specific system and protocol to determine the appropriate number of steps.
Frequently Asked Questions on Experimental Protocols
Q1: What are the best practices for calibrating a low-cost FSR insole system to predict metrics like the Center of Pressure (CoP)?
A: A modern approach involves using recurrent neural networks (RNNs) to map data from low-cost sensors to high-fidelity systems [38].
- Data Collection: Simultaneously collect data from your low-cost FSR insole and a gold-standard system (e.g., F-Scan) while subjects perform a variety of activities (standing, walking, turning) [38].
- Virtual Forces: Instead of using raw pressure values, define "virtual forces" in expanded areas around each FSR sensor. This provides a more robust input for the prediction model [38].
- Model Training: Train an RNN model (such as a Long Short-Term Memory network) using the FSR data as input and the CoP/GRF data from the gold-standard system as the target output. RNNs are particularly effective at capturing the time-series nature of gait data [38]. This method has been shown to improve prediction accuracy by more than 30% compared to conventional techniques [38].
Q2: How can I validate the test-retest reliability of my custom-built smart insole system?
A: Follow a standardized test-retest protocol [7]:
- Study Design: Recruit a cohort of participants (e.g., ~30 individuals) to perform two testing sessions, 4-7 days apart.
- Walking Conditions: Include linear walking, clockwise curved walking, and counter-clockwise curved walking to comprehensively assess reliability across different movement patterns.
- Statistical Analysis: Calculate Intraclass Correlation Coefficients (ICCs) for key parameters (Peak Pressure, Pressure-Time Integral, etc.). An ICC > 0.90 is generally considered indicative of excellent reliability. Use Bland-Altman plots and Minimal Detectable Change (MDC) values for further validation [7].
Q3: What key parameters should I extract and analyze from plantar pressure data for clinical gait analysis?
A: Standardize your analysis around a core set of metrics. The following table summarizes essential parameters and their clinical relevance [32] [7]:
Table 1: Key Plantar Pressure Parameters for Gait Analysis
| Parameter | Description | Clinical/Biomechanical Significance |
|---|---|---|
| Peak Pressure (PP) | The highest pressure value recorded in a specific foot region during a step. | Identifies areas of potential tissue overload; useful for ulcer risk assessment in diabetic patients. |
| Pressure-Time Integral (PTI) | The integral of pressure over time for a step or stance phase. | Represents the cumulative load on a tissue; a high PTI is linked to injury risk. |
| Maximum Force | The highest vertical force value recorded. | Indicates overall limb loading and can be used to assess symmetry between limbs. |
| Contact Area | The total area of the foot in contact with the ground at a point of maximum loading. | Assesses foot structure and function; a changing area can indicate altered biomechanics. |
| Center of Pressure (CoP) Trajectory | The path of the center of pressure under the foot during the stance phase. | Crucial for evaluating balance control and dynamic stability. |
| Contact Time | The duration of foot-ground contact during a step. | Helps characterize gait cycle timing and detect asymmetries. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials for Fabricating Piezoresistive Sensor Insoles
| Material / Component | Function | Examples & Notes |
|---|---|---|
| Conductive Fillers | Creates the piezoresistive composite; resistance changes with applied force. | Carbon Black (CB) [35], Carbon Nanotubes (CNTs) [37], Graphene Oxide (GO) [37], MXene [37]. |
| Elastomeric Matrix | Forms the flexible, stretchable substrate that houses the conductive filler. | Silicone (e.g., PDMS) [35] [37], Polyurethane (PU) [37]. |
| Rheological Modifiers | Tunes the ink's viscosity and viscoelasticity for printability (e.g., in Direct Ink Writing). | Cellulose Nanocrystals (CNCs) - enable 3D printing of complex structures [35]. |
| Flexible Substrate/Insole | The base platform onto which sensors are printed or embedded. | Flexible PCB, Textile, or a pre-fabricated elastomeric insole [39] [36]. |
| Screen-Printing Interface | The stencil or mesh used to define the high-density sensor pattern. | High-density array fabrication, crucial for scalable and cost-effective manufacturing [36] [37]. |
| Data Acquisition System | A wearable, low-profile circuit to capture, digitize, and transmit sensor data. | Includes a microcontroller, analog-to-digital converter, and wireless module (e.g., Bluetooth) for real-time monitoring [39] [7]. |
Experimental Workflow and Signaling Pathway Diagrams
Calibration and Validation Workflow for Smart Insoles
Piezoresistive Signal Generation Pathway
Troubleshooting Common Calibration Issues
Q1: My in-shoe pressure data shows inconsistent readings between tests, even with the same subject. What could be causing this?
A: Inconsistent readings often stem from sensor drift or improper calibration protocols not matched to your specific application [1]. For diabetic foot monitoring, ensure:
- Re-calibration Frequency: Re-calibrate sensors before each testing session, as flexible in-shoe sensors are prone to hysteresis and drift [1] [4].
- Environmental Control: Conduct calibration in a controlled environment, as temperature fluctuations can affect sensor output, especially in piezoresistive sensors [4].
- Loading Rate: For dynamic activities, verify that your calibration protocol uses loading rates representative of actual movements. Many standard testing machines use rates lower than those found in walking, leading to invalid data for sporting applications or abnormal gait patterns [1].
Q2: When measuring plantar pressures in diabetic patients, our platform system data doesn't match the clinical presentation. Why?
A: This discrepancy is common when using a barefoot platform system to assess a shod condition. Platform systems are highly accurate for barefoot assessment but fail to account for the pressure redistribution provided by therapeutic footwear or orthotics [1] [2]. For diabetic foot applications focused on preventing ulceration, in-shoe systems are more suitable for evaluating the real-world effect of footwear interventions [1] [40].
Q3: What are the critical specifications to check when selecting a sensor for a bespoke diabetic foot monitoring system?
A: Focus on these core sensor requirements outlined in research [4]:
- Linearity: A highly linear sensor simplifies signal processing and improves measurement accuracy.
- Hysteresis: Low hysteresis is critical to ensure the sensor output is consistent during loading and unloading phases of gait.
- Pressure Range: The sensor must cover the expected pressure range, which is particularly important for areas of peak pressure on the diabetic foot.
- Temperature Sensitivity: The sensor should have low temperature sensitivity in the 20°C to 37°C range to account for both ambient conditions and skin temperature changes.
Calibration Methodologies and Data
Table 1: Comparison of Plantar Pressure Measurement Systems
| Feature | Platform Systems | In-Shoe Systems |
|---|---|---|
| Primary Application | Barefoot assessment in lab settings (standing, walking) [1] | In-field measurement during daily living or sports; assessing footwear/orthotics [1] |
| Accuracy/Resolution | Highest accuracy and spatial resolution [1] [2] | Typically lower spatial resolution and sampling frequency [1] [2] |
| Best for Diabetic Foot | Diagnosing barefoot foot function and pressure anomalies [4] | Monitoring pressure in shod conditions; evaluating therapeutic footwear efficacy [1] [40] |
| Key Calibration Note | Requires standardized two-step protocol for reliable data [1] [2] | Requires bespoke calibration for validity; check for sensor drift [1] |
Table 2: Essential Research Reagent Solutions
| Item | Function in Research Context |
|---|---|
| Material Testing Machine | Provides controlled, measurable force for dynamic sensor calibration. Must be capable of replicating human movement loading rates [1] [41]. |
| Data Acquisition (DAQ) System | Acquires raw electrical signals (e.g., resistance, voltage) from sensors at high sampling rates (e.g., 500 Hz) for synchronization with applied force [41]. |
| Linearity & Hysteresis Testing Setup | Apparatus to apply and release known pressures to quantify a sensor's linearity and hysteresis, which are critical for data accuracy and reliability [4]. |
| Strain Gauge Adhesive | Bonds sensor components (e.g., a crack-based sensor to a stainless steel substrate) without compromising the mechanical properties being measured [41]. |
The Scientist's Toolkit: Experimental Protocol for Bespoke Dynamic Calibration
Objective: To establish a calibration protocol for an in-shoe plantar pressure sensor that is valid for the high loading rates encountered in a specific activity (e.g., gait of a diabetic patient with altered biomechanics).
Background: Standard calibration machines often use loading rates lower than those found in walking. A bespoke protocol ensures the sensor's output is accurate under real-world conditions [1].
Methodology:
- Sensor Fixturing: Secure the sensor or instrumented insole to the platen of a material testing machine (e.g., Instron UTM) that can achieve high loading rates [41].
- Data Synchronization: Synchronize the clock of the data acquisition (DAQ) system reading the sensor's output with the material testing machine. Use an identical sampling rate (e.g., 500 Hz) for both systems to simplify data combination [41].
- Application of Force: Program the machine to apply a series of known forces across the expected pressure range. The loading rate and profile (e.g., impulse to mimic heel strike) should be designed to replicate the target activity as closely as possible [1].
- Data Collection & Calculation: Record the simultaneous output from both the sensor (e.g., resistance change) and the testing machine (applied force). Calculate the applied pressure by dividing the known force by the sensor's active area [41].
- Model Generation: Plot the sensor's output (e.g., resistance) against the applied pressure to generate a transfer function. This model is used to convert future sensor readings into accurate pressure values.
Calibration Workflow
Frequently Asked Questions (FAQs)
Q4: How can artificial intelligence (AI) be used in plantar pressure data analysis and calibration?
A: AI has clear potential to assist in the analysis and interpretation of complex plantar pressure data. It can be used to identify patterns in large datasets that might be missed by traditional analysis, aiding in clinical diagnoses and monitoring. This could lead to AI-driven calibration models that automatically compensate for sensor-specific non-linearities and drift [1] [40].
Q5: For long-term monitoring of a diabetic patient, what besides pressure should I consider measuring?
A: A holistic approach is recommended. Quantifying both mechanical and physiological/wound-associated parameters provides a more complete picture for assessment [40]. Consider integrating sensors for:
- Temperature: To detect inflammation, a precursor to ulceration [40].
- Shear Forces: These are critically damaging but harder to measure than pressure [40].
- Humidity: To monitor skin maceration risk [40].
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Why is the choice of indenter size so critical for calibrating plantar shear stress sensors?
The indenter size directly influences the mechanical coupling between the sensor and the surrounding insole material, which drastically affects the calibration output. Research demonstrates that using indenters of different areas (from 78.5 mm² to 707 mm²) can cause variations in measurements of up to 80% [31]. Using an indenter that does not approximate the actual anatomical loading area of the foot (e.g., a metatarsal head) will lead to a calibration that does not accurately represent in-shoe conditions, resulting in significant measurement errors during gait analysis [31].
Q2: How does indenter location during calibration impact the accuracy of sensor measurements?
The position of the indenter relative to the sensor's center is a major source of inaccuracy. Studies show that varying the indenter location by up to 40 mm from the sensor centre can lead to measurement variations as high as 90% [31]. This underscores the necessity of ensuring that calibration loads are applied precisely to the sensor's active area in a manner consistent with how the foot will load the sensor during use. This is particularly important for sensors embedded in soft, hyperelastic elastomers where force distribution is non-uniform [31].
Q3: What are the consequences of using an inappropriate calibration protocol for Force-Sensing Resistors (FSRs)?
Using an inappropriate protocol can lead to significant inaccuracies, including:
- Lack of Repeatability: Output can vary between identical loading cycles [42].
- Hysteresis: The output during loading differs from the output during unloading [42].
- Drift: Sensor output can increase over time even under a constant load [42].
- Inter-cell Variation: In an array of sensors, individual cells can have unique outputs with a maximum variation of about ±50% of the mean output if not properly equilibrated [42]. A strict protocol involving in-situ calibration and cyclic pre-loading is essential to minimize these effects [42].
Q4: How can I improve the accuracy of my in-shoe pressure measurement system?
Key strategies include:
- Anatomical Calibration: Calibrate sensors using indenter sizes, shapes, and load ranges that closely mimic the anatomical regions of the foot and the expected pressures during gait [31].
- In-Situ Calibration: Calibrate the sensors after they have been fixed in their final position (e.g., bonded inside a shoe or socket) to account for the effects of curvature and material properties of the surrounding structure [42].
- Cyclic Pre-conditioning: Subject the sensors to a series of cyclic loads (e.g., equivalent to 30 gait steps) prior to final calibration to stabilize their output [42].
- Use Absolute Values: Report absolute pressure values in research to allow for proper comparison and validation of methodological setups [43].
Troubleshooting Common Experimental Problems
Problem: Inconsistent readings between identical sensors in an array.
- Possible Cause: Inter-cell variation inherent to the sensor technology, or "defective" cells [42].
- Solution: Use the manufacturer's equilibrium software (if available) to balance all cell outputs at a known, selected pressure. Visually inspect data and ignore outputs from consistently outlying or "defective" cells [42].
Problem: Sensor readings drift over time during a static load.
- Possible Cause: Signal drift, a known issue with technologies like FSRs [42].
- Solution: Perform calibrations immediately before data collection. Be aware of the drift specification of your sensors (e.g., Tekscan FSRs can drift 5% after 10 seconds of static load) and minimize the time between calibration and measurement [42].
Problem: Measurements are inaccurate when sensors are placed inside a curved shoe or prosthetic socket.
- Possible Cause: 3-dimensional curvatures alter how force is transferred to the sensing element, especially for FSRs [42].
- Solution: Bond the sensors to the rigid inner wall of the structure and perform the calibration in-situ using a pressurised gel-filled "condom" or similar system to apply uniform pressure for calibration [42].
Quantitative Data on Indenter Influence
The following table summarizes key experimental data on how indenter parameters affect calibration accuracy, derived from a study on a novel shear stress sensing system [31].
Table 1: Impact of Indenter Parameters on Calibration Accuracy
| Parameter | Tested Range | Observed Effect on Measurement | Implication for Calibration Protocol |
|---|---|---|---|
| Indenter Area | 78.5 mm² to 707 mm² | Variation in measurements of up to 80% [31] | The indenter contact area must be representative of the anatomical structure being studied (e.g., metatarsal head, heel). |
| Indenter Location | Up to 40 mm from sensor center | Variation in measurements of up to 90% [31] | The load must be applied precisely to the center of the sensor's active area during calibration. |
| System Performance | Bench-top mechanical tests | Mean Absolute Error < ±18 kPa; High repeatability (>97%) when properly calibrated [31] | A rigorous calibration protocol that considers indenter specifics can yield highly accurate and repeatable results. |
| System Performance | 15-min treadmill walking | Less than 21% variability within walking trials [31] | The calibration method provides stable performance for dynamic, in-shoe measurements. |
Detailed Experimental Protocols
Protocol 1: Comprehensive Calibration for Plantar Shear Stress Sensors
This protocol is adapted from Haron et al. (2024) for calibrating a novel shear stress sensing insole [31].
1. Sensor System Design:
- The sensing element is a 3-element strain gauge rosette (0°-45°-90°) embedded in a hyperelastic silicone insole.
- A commercial normal pressure sensor is placed underneath the silicone to decouple the effects of normal force on the shear measurements.
- The system calculates resultant shear stress in the Anterior-Posterior (AP) and Medial-Lateral (ML) directions based on the strain gauge readings and the known material properties of the silicone [31].
2. Calibration Rig Setup:
- A custom mechanical test rig with an indenter is used to exert controlled normal and shear forces.
- The indenter size, shape, and location are variable and form the core of the investigation.
3. Calibration Procedure:
- Varied Indenter Area: Apply loads using indenters with different surface areas (e.g., 78.5 mm², 707 mm²) to quantify the effect on measurement accuracy.
- Varied Indenter Location: Apply loads at different offsets (e.g., up to 40 mm) from the sensor centre to quantify positional sensitivity.
- Data Collection: For each indenter configuration, record the output from both the strain gauge rosette (for shear) and the normal pressure sensor.
- Calibration Factor Calculation: Use the known applied stresses and the sensor outputs to derive calibration factors that relate electrical output (mV) to applied shear stress (kPa). The relationship accounts for the non-linear stress-strain behavior of the silicone by using piecewise linear approximations for low, medium, and high strain regions [31].
4. Validation:
- Validate the calibrated system by testing it on participants during treadmill walking and comparing the results to bench-top mechanical tests [31].
Protocol 2: Minimizing Inaccuracies in Force-Sensing Resistors (FSRs)
This protocol, based on the work of Buis & Convery (1997), is designed to address the known hysteresis, drift, and inter-cell variation of FSRs [42].
1. Pre-Calibration Cyclic Conditioning:
- Place the FSR sensor in the calibration rig (e.g., a pressure rig with a mylar membrane for uniform air pressure application).
- Apply a cyclic pressure (e.g., 100 kPa at 0.5 Hz) for a period of 60 seconds (equivalent to ~30 gait steps) to stabilize the sensor output before the static calibration step [42].
2. In-Situ Calibration for Curved Surfaces:
- For sensors used in prosthetic sockets or footwear, bond the FSRs to the inner wall of the rigid structure.
- Use a gel-filled "condom" sealed inside the structure; pressurize the gel to a known level to apply uniform pressure for calibration.
- Use the manufacturer's software to equilibrate and calibrate all sensor cells at this known pressure. This ensures consistent readings irrespective of socket curvature [42].
3. Iterative Load Input for Software:
- When the calibration software requests an input load, calculate the initial value as
Total Sensing Area (mm²) × Applied Pressure (kPa). - If the sensor output after cyclic loading does not match the known applied pressure, adjust the input load iteratively. For example, if a 10% error is observed, increase the input load by 10% for the next calibration attempt [42].
Experimental Workflow and Signaling Pathways
The following diagram illustrates the logical workflow and decision-making process for establishing a robust sensor calibration protocol, highlighting the critical role of indenter parameters.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials for Plantar Pressure Sensor Research
| Item | Function / Application | Key Considerations |
|---|---|---|
| Strain Gauge Rosette | Measures multi-directional shear stress when embedded in an elastomer [31]. | A 0°-45°-90° configuration allows calculation of resultant shear in Anterior-Posterior and Medial-Lateral directions [31]. |
| Hyperelastic Silicone | Serves as the embedding medium for shear sensors, mimicking insole properties [31]. | Its non-linear stress-strain relationship must be characterized and accounted for in the calibration model [31]. |
| Force-Sensing Resistors (FSRs) | Thin, flexible sensors for measuring interface pressure in arrays [16] [42]. | Prone to hysteresis, drift, and inter-cell variation; require strict calibration protocols [42]. |
| Custom Mechanical Test Rig | Applies controlled normal and shear forces for sensor calibration [31]. | Must allow for variation in indenter size, shape, and location to ensure anatomical relevance [31]. |
| Pressure Calibration Rig | Applies uniform air pressure for simultaneous calibration of multiple sensor cells (e.g., FSR arrays) [42]. | Uses a mylar membrane and calibrated pressure regulator to verify accuracy against reference strain gauges [42]. |
| MEMS Pressure Sensors | Micro-electromechanical systems proposed for compact, linear, low-hysteresis wireless systems [4]. | Offer high linearity, accuracy, and reliability for high-pressure distributions under the foot [4]. |
Solving Common Calibration Challenges and Optimizing for Accuracy
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What is the difference between sensor drift and hysteresis? Sensor drift is a change in the sensor's output over time, even when the measured input (pressure) remains constant [44] [45]. Hysteresis, conversely, is a phenomenon where the sensor's output depends on the history of past pressures; specifically, the reading at a given pressure will differ depending on whether the pressure was reached by increasing from a lower value or decreasing from a higher value [4] [46].
Q2: Why are my in-shoe sensor readings becoming less accurate over a long study? This is likely caused by sensor drift. Over time and with long-term use, the materials within the sensor can age and degrade. Physical factors like repeated mechanical stress from walking and environmental factors like temperature fluctuations or humidity from sweat can accelerate this process, causing the sensor's baseline output to shift [44] [45] [47].
Q3: When I test my pressure platform by applying and releasing pressure, I get different values at the same point. What is this? This describes hysteresis. It is often caused by the inherent properties of the sensor materials. During loading and unloading, the mechanical components (like the sensing element or diaphragm) do not follow the same path, leading to a lag or difference in the output signal [4] [46]. Contamination inside the instrument can also worsen this effect.
Q4: How can I minimize the impact of environmental temperature on my plantar pressure measurements? Temperature changes are a major cause of drift. To mitigate this, you can:
- Stabilize the Temperature: Keep the sensor in a constant temperature state as much as possible before and during calibration [44].
- Use Temperature Compensation: Employ hardware circuits with thermistors or software algorithms that correct the output based on a measured temperature [44] [45].
- Select Appropriate Sensors: Choose sensors with low specified temperature drift for critical applications [29].
Q5: My pressure sensor was accidentally subjected to a strong impact. What problems should I look for? Physical damage, especially to the diaphragm, is a common cause of zero drift [47]. After an impact, you should check for a permanent shift in the zero-pressure output and a change in the sensor's calibration curve. Mechanical shock can also cause internal damage that manifests as increased hysteresis [46] [29].
Troubleshooting Guide
| Problem Symptom | Potential Error Source | Diagnostic Steps | Recommended Solutions |
|---|---|---|---|
| Gradual decrease in accuracy over weeks/months; baseline shift. | Sensor Drift [44] [45] | 1. Perform a zero calibration check at regular intervals.2. Compare readings against a known reference standard.3. Track performance trend data over time. | 1. Implement regular re-calibration schedules.2. Use software compensation (e.g., polynomial fitting, neural networks) [44] [45].3. Select high-precision, low-drift sensors. |
| Different output readings at the same pressure during loading vs. unloading cycles. | Hysteresis [4] [46] | 1. Conduct an "up and down" calibration: record values while increasing and then decreasing pressure.2. Plot the input vs. output to visualize the hysteresis loop. | 1. Choose sensors with low hysteresis specifications.2. Follow consistent calibration procedures that include up/down cycles [46].3. Ensure instruments are clean and free of contaminants. |
| Sudden or cyclical inaccuracies correlated with lab temperature or humidity changes. | Environmental Factors [44] [45] [29] | 1. Log ambient temperature and humidity during experiments.2. Analyze sensor output for correlations with environmental data. | 1. Control the lab environment (stable temperature/low humidity).2. Use sensors with environmental compensation.3. For in-shoe systems, use encapsulation to protect from sweat [9]. |
| Erratic or noisy signals, especially in environments with heavy electrical equipment. | Electrical Interference [45] [29] | 1. Check for proper cable shielding and grounding.2. Use an oscilloscope to analyze signal noise. | 1. Use shielded cables and ensure proper grounding.2. Install filters on the power supply and signal lines.3. Physically separate sensor cables from noise sources. |
Detailed Experimental Protocols for Error Identification
Protocol 1: Isolating and Quantifying Hysteresis
This protocol is designed to measure the hysteresis error of a plantar pressure sensing system.
- Equipment: Device Under Test (DUT - pressure platform or in-shoe system), certified pressure calibrator or deadweight tester, data acquisition system, environmental monitoring tool.
- Procedure:
- Stabilize the DUT and calibration equipment in a controlled environment (e.g., 23±2°C).
- Loading Cycle: Starting from zero, apply increasing pressure to the DUT in defined steps (e.g., 10% of full scale) up to 100% of the measurement range. At each step, allow the reading to stabilize and record the DUT output.
- Unloading Cycle: From the maximum pressure, decrease the pressure in the same defined steps back to zero. Again, record the stabilized DUT output at each step.
- Repeat this cycle at least three times to assess repeatability.
- Data Analysis:
- Plot the applied pressure versus the DUT output for both loading and unloading cycles. The hysteresis loop will be visible.
- Calculate the maximum hysteresis error as the maximum difference between the loading and unloading curves at any identical pressure point, expressed as a percentage of full-scale output [46].
Protocol 2: Monitoring Long-Term Sensor Drift
This protocol assesses the stability of a sensor's output over an extended period.
- Equipment: DUT, stable pressure source (or zero-pressure condition), data logger, constant temperature chamber.
- Procedure:
- Place the DUT in a constant temperature environment to eliminate thermal effects.
- Apply a constant input condition. For zero drift, this means no load (zero pressure). For span drift, a constant, known pressure can be applied.
- Log the output of the DUT at regular intervals (e.g., every hour) over a prolonged period (e.g., 7-30 days).
- Data Analysis:
- Plot the sensor output against time.
- The drift can be quantified as the total change in output (or the slope of a trend line) over the test period, typically expressed as a percentage of full scale per unit of time [47].
Research Reagent Solutions and Essential Materials
The following table details key materials used in advanced plantar pressure research, as exemplified by the development of a high-density smart insole.
| Item | Function / Explanation |
|---|---|
| Carbon-Epoxy-Elastomer (CE2) Ink | A piezoresistive composite material that is screen-printed to form sensors. Its electrical resistance decreases predictably under applied pressure, enabling force measurement [9]. |
| Flexible Printed Circuit Board (fPCB) | A thin, bendable substrate that hosts the sensor electrode array and connecting traces. Its flexibility is critical for user comfort and integration into an insole [9]. |
| Polydimethylsiloxane (PDMS) | An elastomer added to the carbon-epoxy ink to optimize the sensor's performance. It enhances sensitivity by promoting the "percolation effect" where conductive pathways form under load [9]. |
| Parylene Encapsulation | A thin, protective polymer coating applied over the sensor array. It provides a critical barrier against environmental damage, such as moisture from sweat, ensuring long-term reliability [9]. |
| High-Resolution Pressure Tiles/Walkway | A platform system with a dense array of sensors (e.g., 4 sensors/cm²) used for barefoot gait analysis. It serves as a high-accuracy benchmark for validating in-shoe systems [8]. |
Workflow for Diagnosing Pressure Sensor Errors
The following diagram illustrates a systematic methodology for troubleshooting common error sources in plantar pressure measurement systems.
Signal Compensation Methods for Drift
This diagram categorizes the primary techniques for compensating sensor drift, a critical process for maintaining data accuracy in long-term studies.
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What are the most common sensor placement errors that lead to measurement inaccuracies? Incorrect sensor placement is a primary source of error. Placing sensors outside key anatomical weight-bearing areas or using insufficient sensor density fails to capture a complete pressure picture [4]. Furthermore, sensor slippage within the shoe can invalidate data by shifting measurement locations during activity [4]. For accurate Center of Pressure (COP) trajectory measurement, research indicates that optimal, data-driven sensor placement is superior to simple anatomical assumptions [48].
Q2: How does loading area specifically affect calibration and measurement validity? The area over which a load is applied is fundamental to accurate pressure calculation (Pressure = Force/Area) [48]. Using an incorrect or unrepresentative loading area during calibration will systematically skew all subsequent measurements [1]. For instance, calibration protocols often use loading rates that are lower than those seen in sporting movements, leading to invalid data when the system is used for high-impact activities [1]. Ensuring the calibration load area matches the intended application is critical for validity.
Q3: What environmental and system factors can mimic symptoms of poor loading area/position? Several factors can present as placement errors but originate elsewhere. Electrical interference from nearby equipment can cause signal noise and erratic readings [49]. Sensor drift over time, often due to thermal stress or mechanical fatigue, leads to a gradual loss of accuracy that can be mistaken for a calibration issue [49]. Additionally, hysteresis—the difference in sensor output during loading versus unloading—can cause inaccuracies if the sensor material is not sufficiently linear [4].
Troubleshooting Guide: Loading Area and Position
| Problem | Root Cause | Diagnostic Steps | Solution |
|---|---|---|---|
| Inconsistent COP Trajectory | Non-optimal sensor placement; insufficient sensor number [48]. | Compare COP from sparse sensor layout vs. high-resolution system [48]. | Use Deep Reinforcement Learning to optimize sensor placement [48]. |
| Low Spatial Resolution Data | Large sensels or low sensor count miss pressure gradients [4] [50]. | Inspect pressure maps for large, uniform areas with no detail. | Use high-density sensor arrays (e.g., 173 sensors/insole) [9]. |
| Data Drift During Static Load | Sensor creep under prolonged pressure [50]. | Apply fixed load for 30+ seconds and monitor output for drift [50]. | Use piezoresistive sensors; avoid capacitive sensors for static loads [9] [50]. |
| Inaccurate Peak Pressure | Calibration with unrepresentative load area/rate [1]. | Bench-test with known pressures and areas different from calibration [50]. | Implement bespoke calibration protocols matching target movements [1]. |
| Sensor Slippage | Improperly secured in-shoe sensor sheets [48]. | Visual inspection of sensor position after activity. | Use double-sided tape and secure fittings to prevent movement [48]. |
Experimental Protocols for Validation
Protocol for Validating Sensor Placement for COP Accuracy
This protocol is based on research that used Deep Reinforcement Learning (DRL) to optimize sensor placement without prior anatomical knowledge [48].
- Objective: To determine the minimal and optimal sensor configuration for accurately reconstructing the center of pressure (COP) trajectory during dynamic tasks.
- Materials:
- High-resolution in-shoe pressure measurement system (e.g., Tekscan F-Scan with a 21x60 sensor array) [48].
- Standardized footwear.
- Treadmill.
- Methodology:
- Data Collection: Record plantar pressure videos at a high frequency (e.g., 100 Hz) from multiple subjects performing the target activity (e.g., self-selected speed running) [48].
- Preprocessing:
- Segment the data to isolate numerous stance-phase videos.
- Crop and downsample each pressure frame to a standardized, lower-resolution grid (e.g., 7x20) for processing [48].
- DRL Training: Implement a sensor placement environment where a DRL agent (e.g., using Soft Actor-Critic) is tasked with placing a limited number of sensors (e.g., 8) on the 7x20 grid.
- Reward System: The agent's reward is based on the mean square error between the COP trajectory calculated from the limited sensor placement and the "ground truth" COP from the full high-resolution system [48].
- Validation: The final sensor placement pattern generated by the DRL agent is validated on a separate set of plantar pressure data.
Protocol for System-Level In-Shoe Pressure Validation
This protocol assesses the validity and reliability of an in-shoe system, focusing on how load application affects measurements [50].
- Objective: To evaluate the accuracy and repeatability of in-shoe pressure measurements across different loading areas and pressures.
- Materials:
- In-shoe pressure measurement system (e.g., XSENSOR X4).
- Calibration device capable of applying uniform pressure (e.g., TruBlue calibration device) [50].
- Regional loading cylinders of different areas (e.g., 3.1 cm² and 15.9 cm²).
- Data analysis software (e.g., Python with custom scripts).
- Methodology:
- Whole Insole Protocol:
- Use the calibration device to apply a series of uniform pressures (e.g., 50, 100, 200, 300, 400, 500, 600 kPa) across the entire insole surface [50].
- Hold each pressure for 30 seconds while recording.
- Calculate the Root Mean Square Error (RMSE) of the mean and peak pressures reported by the system versus the target pressure [50].
- Regional Protocol:
- Apply regional loads to specific areas of the insole (e.g., heel) using cylinders of different surface areas.
- Apply weights to generate realistic pressures (e.g., 50, 110, 200 kPa) [50].
- Hold for 30 seconds and record.
- Calculate the contact area error (AErr) as the RMSE between the measured active sensel area and the known cylinder area [50].
- Analysis:
- Assess time-dependence by analyzing drift in pressure and area readings over the 30-second period.
- Determine between-day reliability by repeating the protocol on a second day and calculating Intra-class Correlation Coefficients (ICCs) [50].
- Whole Insole Protocol:
Research Workflow Visualization
DOT Script for Experimental Validation Workflow
DOT Script for Sensor Placement Optimization
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 1: Key Materials for Plantar Pressure Research
| Item | Function | Key Specification Considerations |
|---|---|---|
| Pressure Sensing Platform | Measures barefoot plantar pressure in lab settings. Provides high-resolution reference data [1] [8]. | High spatial resolution (e.g., 4 sensors/cm²); Rigid and accurate for benchmarking [1] [8]. |
| In-Shoe Pressure Insoles | Measures foot-shoe interface pressure in the field during dynamic activities [1] [4]. | Flexibility; Wireless operation; Number of sensors (e.g., 173 for high-density) [4] [9]. |
| Calibration Device (e.g., TruBlue) | Applies known, uniform pressures for system validation and calibration [50]. | Ability to apply a range of pressures and areas representative of target movements [1] [50]. |
| Piezoresistive Sensors | Sensor technology that changes resistance with applied pressure. Preferred for dynamic and static load measurement [9]. | High linearity; Low hysteresis; Sensitivity (e.g., -0.322 kPa⁻¹) [4] [9]. |
| Capacitive Sensors | Sensor technology that changes capacitance with applied pressure. | Can be prone to signal drift (creep) under sustained static loads [50]. |
| Screen-Printed Sensor Arrays | Fabrication method for creating high-density, flexible sensor matrices on insoles [9]. | Ink composition (e.g., Carbon-Epoxy-Elastomer); Number of printed layers; Cracking resistance [9]. |
Optimizing Sensor-Insole Mechanical Coupling for Reliable Signal Transmission
Within foot plantar pressure research, the mechanical coupling between the sensor and the insole is a critical, yet often overlooked, factor that directly impacts the validity and reliability of collected data. A poor coupling can lead to signal artifacts, inaccurate pressure readings, and ultimately, compromised research findings. This guide provides researchers with targeted troubleshooting and methodologies to optimize this interface, ensuring high-fidelity signal transmission for both clinical and sports applications.
Troubleshooting FAQs
Q1: My sensor insoles are failing to connect or transmit data reliably. What are the primary causes?
A: Connection and data transmission issues are frequently traced to power and communication settings.
- Bluetooth and Permissions: Ensure that Bluetooth is enabled and that the mobile application has been granted all necessary location and Bluetooth permissions [51] [52].
- Battery Charge: A low battery is a common cause of intermittent connectivity or failure to connect. Verify that the coin cell batteries are fully charged [52].
- Wireless Range: Be aware that the typical operational range for wireless sensor insoles is often limited (e.g., approximately 10 meters). Conduct experiments within this specified range to ensure a stable connection [52].
Q2: The plantar pressure data from my in-shoe system appears noisy or inaccurate. What mechanical factors should I investigate?
A: In-shoe systems are susceptible to specific mechanical issues that platform systems are not. Data inaccuracy can stem from [1] [4]:
- Sensor Slippage: If sensors are not securely fixed within the shoe, movement will create artifacts. Ensure the insole and sensors are properly secured to prevent slippage.
- Poor Sensor-Insole Contact: Voids or uneven surfaces between the sensor and the insole substrate can lead to unreliable signal transmission. The coupling must be uniform.
- External Interference: A lack of proper shielding can allow environmental electromagnetic noise to corrupt the signal. Some advanced insole designs incorporate a conductive fabric shielding layer to mitigate this [53].
- Calibration Validity: The system's calibration must be appropriate for the dynamic movements of your study. Calibration protocols designed for walking may not be valid for high-impact sporting movements [1] [2].
Q3: How can I verify the mechanical integrity and performance of the sensors themselves?
A: Sensor performance can be quantified through standardized metrics. Researchers should validate these parameters, which are often reported in prototype studies [53]:
- Hysteresis: Test the sensor by loading and unloading it while observing the output signal. A significant difference between the two curves indicates hysteresis, which leads to measurement error [4].
- Linearity: A highly linear sensor response simplifies signal processing and improves accuracy. Plot the sensor's response to a known applied pressure to check for linearity [4].
- Durability: Perform long-term cycle testing (e.g., 15,000 cycles) under typical load conditions (e.g., ~50 kPa) to ensure the sensor maintains its performance characteristics over time [53].
Troubleshooting Guide: Common Coupling and Data Issues
Table 1: Troubleshooting common mechanical and data transmission problems.
| Symptom | Possible Cause | Corrective Action |
|---|---|---|
| Unstable Bluetooth connection | Low battery; exceeded wireless range; incorrect device permissions. | Charge battery; move data receiver closer; check app permissions for location/Bluetooth [51] [52]. |
| Drifting baseline or noisy signal | Poor electrical contact; insufficient shielding; loose sensor mounting. | Check electrode connections; ensure shielding layer is grounded; secure sensor to insole substrate [53]. |
| Data does not reflect expected pressure patterns | Sensor slippage; incorrect calibration protocol for the activity. | Ensure insole is fixed securely inside the shoe; use a calibration protocol specific to the movement being studied (e.g., running vs. walking) [1] [4]. |
| Signal loss under high load | Mechanical failure due to overloading; poor coupling integrity. | Verify sensor's pressure range specification; inspect for physical damage; ensure uniform coupling to insole [53]. |
| Hysteresis in pressure readings | Material fatigue or viscoelastic properties of the dielectric layer. | Characterize the sensor's hysteresis curve and apply software compensation; select sensors with lower inherent hysteresis [4]. |
Experimental Protocol: System Validation and Calibration
This protocol provides a methodology for validating the mechanical coupling and data acquisition of a sensor-insole system within a research setting.
1. Objective: To verify the functional performance and calibration of a smart insole system for static and dynamic plantar pressure measurement.
2. Materials and Reagents: Table 2: Essential research reagents and materials for insole system validation.
| Item | Function |
|---|---|
| Smart Insole Prototype | The device under test, typically incorporating an array of sensors (e.g., 24 capacitive sensors). |
| Data Acquisition (DAQ) System | Hardware for reading analog sensor signals, converting them to digital data, and wirelessly transmitting them [53]. |
| PC Terminal with Receiver & Software | For receiving data, visualizing real-time pressure maps, and recording data for post-processing [53]. |
| Calibration Rig | A mechanical testing system (e.g., with a linear motor) capable of applying known pressures to individual sensors. |
| LCR Meter | For precise measurement of capacitance during sensor characterization [53]. |
3. Methodology:
Part A: Pre-Experimental Setup
- System Assembly: Integrate the smart insole, DAQ system, and PC terminal. Verify wireless connectivity and data streaming for all sensor channels.
- Sensor Securing: Fix the sensor insole firmly inside the research footwear to prevent any movement during data collection [4].
Part B: Sensor Characterization
- Linearity and Sensitivity: Using the calibration rig, apply a series of known pressures (e.g., from 0 to 200 kPa) to individual sensors. Record the output (e.g., capacitance change). Plot the response curve and calculate sensitivity [53].
- Hysteresis Assessment: Load and unload the sensor while measuring the output. Calculate the hysteresis as the maximum difference between the loading and unloading curves at the same pressure [4].
- Durability Testing: Subject key sensors to long-term cyclic loading (e.g., 15,000 cycles at ~50 kPa) to monitor for performance degradation [53].
Part C: In-Situ Functional Testing
- Static Posture Analysis: Have a subject stand on the insoles in a neutral stance. Observe the pressure map for expected patterns (e.g., higher pressure in heel and forefoot) and symmetry.
- Dynamic Activity Analysis: Record data during prescribed activities (e.g., walking, running, or going upstairs). Analyze the data for expected temporal-spatial patterns and center of pressure (CoP) trajectory [53].
Technical Data for Research Design
Table 3: Performance metrics from an optimized capacitive pressure sensor for insoles [53].
| Performance Characteristic | Optimized Value | Notes / Method of Measurement |
|---|---|---|
| Sensitivity | 12 × 10⁻³ kPa⁻¹ | Achieved with a hexagonal pore (600 µm) dielectric layer. |
| Detection Range | 0 – 200 kPa | Suitable for wide range of activities from walking to running. |
| Linearity | Superior linearity across full range | Simplifies data processing and improves accuracy. |
| Response Time (Rise) | ~132 ms | Constrained by measurement equipment; indicates real-time capability. |
| Durability (Cycles) | 15,000 cycles at ~50 kPa | Demonstrates excellent stability with minimal performance loss. |
Foundational Concepts: FAQs on Conductive Inks and Sensitivity
FAQ 1: What is the relationship between conductive ink composition and sensor sensitivity? The composition of conductive ink directly determines the electrical and mechanical properties of the sensing layer, which in turn governs sensitivity. Sensitivity is a measure of how much the sensor's electrical output (e.g., resistance) changes in response to an applied pressure. In piezoresistive sensors, this change occurs through the percolation effect, where applied pressure forces conductive particles (like carbon black) closer together, creating new conductive pathways and decreasing electrical resistance. The type and ratio of conductive fillers, polymer binders, and elastomer additives in the ink formulation control the ease with which these new pathways form under pressure, thus defining the sensor's sensitivity [9] [54].
FAQ 2: Why is tuning the carbon-to-elastomer ratio critical for performance? The carbon-to-elastomer ratio must be carefully balanced to achieve optimal conductivity without compromising mechanical integrity. A higher carbon content improves conductivity but can make the ink brittle and prone to cracking, especially on flexible substrates. Conversely, a higher elastomer content enhances flexibility and durability but can drastically increase electrical resistivity, reducing the sensor's responsiveness. Experimental data has shown that an optimized ratio of 70:30 (wt%) of carbon-epoxy ink to polydimethylsiloxane (PDMS) elastomer achieves a baseline resistance of ~5 kΩ while avoiding cracks, leading to a high sensitivity of -0.322 kPa⁻¹ [9].
FAQ 3: What manufacturing methods are suitable for applying conductive inks in sensor fabrication? Screen printing is a widely used method for fabricating plantar pressure sensors. It is uniquely suited for rapidly creating thin, uniform layers over high-resolution, large-area patterns with minimal processing steps. This method offers fine control over the deposited ink's thickness and geometry, which is crucial for ensuring consistency and performance across a high-density sensor array. Its compatibility with industry-standard processes also makes it suitable for cost-effective, high-throughput manufacturing [9].
Optimization Protocols and Data Analysis
Experimental Protocol: Optimizing a Carbon-Based Piezoresistive Ink
This protocol details the optimization of a Carbon-Epoxy-Elastomer (CE2) ink for a high-sensitivity piezoresistive sensor array [9].
- Objective: To determine the optimal carbon-epoxy to PDMS ratio and the ideal number of screen-printed layers for a plantar pressure sensor.
- Materials:
- Carbon-epoxy conductive ink
- Polydimethylsiloxane (PDMS) elastomer
- Flexible Printed Circuit Board (fPCB) substrate with Interdigitated Electrodes (IDEs)
- Screen-printing apparatus
- 4-point probe or digital multimeter
- Methodology:
- Ink Formulation: Prepare multiple batches of CE2 ink with varying carbon-epoxy to PDMS weight ratios (e.g., from 90:10 to 50:50).
- Sensor Fabrication: Use a screen-printing process to deposit each ink formulation onto the fPCB substrates. Fabricate multiple sensor samples for each ratio.
- Layer Stacking: For the optimal ratio, print multiple layers (e.g., 1 to 5 layers) on separate sensors to study the effect of thickness.
- Electrical Characterization: Measure the baseline electrical resistance of each sensor using a 4-point probe or multimeter.
- Mechanical Inspection: Visually inspect printed layers for cracks or defects, especially for formulations with lower elastomer content.
- Performance Calibration: Subject the sensors to a range of known pressures using a material testing machine and record the corresponding resistance changes to calculate sensitivity.
Table 1: Experimental Data for Carbon-Epoxy-PDMS Ink Optimization
| Ink Ratio (Carbon-Epoxy:PDMS) | Number of Printed Layers | Average Baseline Resistivity | Key Observations |
|---|---|---|---|
| 90:10 | 3 | Low | High crack formation |
| 80:20 | 3 | Low | Some cracking |
| 70:30 | 3 | Medium | No cracks, optimal |
| 60:40 | 3 | High | Flexible, no cracks |
| 50:50 | 3 | Very High | Flexible, no cracks |
| 70:30 | 1 | High | - |
| 70:30 | 3 | Medium | - |
| 70:30 | 5 | Low (~5 kΩ) | Optimal conductivity |
Workflow for Ink Optimization
The following diagram illustrates the iterative process of developing and calibrating a conductive ink for enhanced sensitivity.
Troubleshooting Common Experimental Issues
Issue 1: High Baseline Resistance or Sensor Non-Responsiveness
- Potential Cause: Insufficient conductive filler in the ink formulation or too few printed layers.
- Solution: Increase the ratio of conductive material (e.g., carbon-epoxy) in the ink. Alternatively, increase the number of screen-printed layers, as additional layers provide more conductive pathways. Data shows that increasing from 1 to 5 printed layers can cause a large decrease in resistivity [9].
Issue 2: Cracking of the Printed Conductive Film
- Potential Cause: Ink formulation is too brittle, often due to an excessively high conductive filler-to-elastomer ratio.
- Solution: Increase the content of elastomer additive (e.g., PDMS) in the mixture. A formulation with 30% PDMS has been shown to effectively avoid cracks while maintaining good conductivity [9].
Issue 3: Inconsistent Sensitivity Across the Sensor Array
- Potential Cause: Inconsistent ink viscosity or screen-printing process parameters, leading to variations in the thickness of the sensing layer.
- Solution: Standardize the ink preparation and printing process. Ensure the ink viscosity is uniform and optimize screen-printing parameters (squeeqee pressure, speed, and snap-off distance) to achieve a consistent deposition thickness across all sensors in the array [9].
Issue 4: Sensor Performance Degradation Under High/Long-Term Loads
- Potential Cause: Material creep or permanent deformation of the sensing layer or substrate, which hinders its ability to return to its original state.
- Solution:
- Ensure the ink formulation has adequate resilience. Alternative materials like highly compressible and resilient PMMA conductive iongels have demonstrated self-recovery within seconds and stability for over 100,000 cycles [55].
- Consider substrate design. Using hierarchical wrinkled microstructures in the sensing layer can enhance durability and distribute stress more effectively [56].
Table 2: Advanced Material Solutions for Enhanced Performance
| Material System | Mechanism | Reported Performance Advantages | Best For Applications Needing: |
|---|---|---|---|
| Carbon-Epoxy-PDMS (CE2) [9] | Percolation effect in a screen-printed composite | Sensitivity of -0.322 kPa⁻¹ | Cost-effective, high-density arrays, high sensitivity |
| PMMA Conductive Iongels [55] | Capacitive sensing with soft, ionic electrodes | High compression strength (>10 MPa), resilience (>100,000 cycles) | Extreme durability, reliability under heavy/repetitive loads |
| MXene/Paper Composites [56] | Hierarchical wrinkled structure for contact area change | Wide sensing range (>600 kPa), sensitivity >15 kPa⁻¹ | Wide pressure range, fast response, eco-friendly materials |
| Crack-Based Sensor [41] | Disconnection/reconnection of nanocracks in a metal layer | High sensitivity, robust design, durability (20,000 cycles) | Detecting very subtle pressures or vibrations |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Conductive Ink Development
| Reagent/Material | Function in Experiment | Specific Example & Notes |
|---|---|---|
| Carbon-Epoxy Ink | Serves as the primary conductive component. | Commercial carbon-epoxy ink can be used as a base and modified with additives [9]. |
| Elastomer Additive (e.g., PDMS) | Enhances ink flexibility, prevents cracking, and tunes mechanical properties. | PDMS is mixed with carbon-epoxy in ratios from 10-50% (wt) to optimize the balance of conductivity and flexibility [9]. |
| Polymeric Binders & Crosslinkers | Forms the matrix that holds conductive fillers and provides structural integrity. | Polymethyl Methacrylate (PMMA) and triethylene glycol dimethacrylate (TEGDMA) can be used to create robust, resilient conductive iongel networks [55]. |
| Advanced Conductive Fillers (e.g., MXene) | Provides high electrical conductivity and facilitates the formation of microstructures. | Ti₃C₂Tx MXene nanosheets can be coated onto tissue paper or other substrates to create highly sensitive, hierarchical wrinkled structures for pressure sensing [56]. |
| Flexible Substrates (fPCB, PI film) | Provides a flexible, durable base for printing sensor circuits and electrodes. | Flexible Printed Circuit Boards (fPCB) with gold-treated interdigitated electrodes (IDEs) or 7.5 µm thick polyimide (PI) films are commonly used [9] [41]. |
Technical Support Center: FAQs & Troubleshooting Guides
This support center provides targeted assistance for researchers integrating AI-based analysis and drift correction into foot plantar pressure measurement systems.
Frequently Asked Questions (FAQs)
Q1: What is model drift and why is it a critical issue in long-term plantar pressure studies? A1: Model drift is the degradation of a machine learning model's performance over time, caused by changes in the underlying data or the relationships between input and output variables [57]. In the context of plantar pressure research, this can manifest as a gradual shift in the sensor output or the AI's interpretation of the data, leading to faulty predictions and incorrect scientific conclusions [57]. This is critical in longitudinal studies where consistent measurement is essential for tracking patient recovery, disease progression, or the effectiveness of a treatment.
Q2: What are the common types of drift, and how do I identify them in my sensor data? A2: The primary types of drift that can affect your system are:
- Concept Drift: The statistical properties of the target variable (what you are predicting) change over time. For example, the relationship between a specific pressure distribution and a clinical outcome (like ulcer risk) might evolve [57].
- Data Drift (Covariate Shift): The distribution of the input data from the plantar pressure sensors changes. This can be caused by sensor aging, changes in environmental conditions, or a shift in the patient population [57].
- Upstream Data Change: A change occurs in the data pipeline itself, such as a firmware update to the sensor system that alters the raw data format or units [57].
Q3: Our lab uses capacitive plantar pressure sensors. Are there specific drift concerns for this technology? A3: Yes. While capacitive sensors are generally reported to be more valid and reliable than resistive sensors for prolonged use, they are not immune to issues [58]. A primary concern is hysteresis and drift, where the sensor's output does not perfectly follow the applied pressure and may change over time [58] [55]. AI can monitor for these gradual shifts in the raw signal, flagging when a sensor may need recalibration or replacement.
Q4: Can AI correct for drift without requiring constant re-labeling of data by a human expert? A4: Yes, methods like Unsupervised Prediction Alignment (UPA) have been developed for this purpose. UPA can automatically realign model predictions from a shifted data distribution (e.g., data from a new sensor batch or after a software update) to the original reference distribution without needing new ground-truth annotations. This preserves the intended performance metrics, such as sensitivity and specificity [59].
Q5: What are the key material properties to consider for stable, long-life plantar pressure sensors? A5: For reliable, future-proofed data collection, sensor materials should possess:
- High Compressibility and Resilience: To withstand repeated high-load cycles (body weight) and return to their original shape [55].
- Low Hysteresis: To ensure the output is consistent regardless of whether pressure is increasing or decreasing [55].
- Long-Term Stability: The material should maintain its electrical and mechanical properties through many thousands of loading cycles [55].
Troubleshooting Guide: AI and Sensor Performance
Use this guide to diagnose and address common problems.
| Symptom | Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|---|
| Gradual decrease in AI model accuracy over months. | Data Drift from gradual sensor material fatigue [58] [55]. | Perform a Kolmogorov-Smirnov (K-S) test or calculate the Wasserstein distance to compare current input data distribution with the original training data [57]. | Implement automated drift detection. Retrain the AI model with a new dataset that includes recent samples [57]. |
| Sudden, significant drop in AI performance. | Upstream Data Change from a sensor firmware update or Sudden Concept Drift [57]. | Check system logs for recent software/firmware updates. Analyze a sample of recent data for format or unit changes. | Verify input data format. Apply an unsupervised recalibration method like Unsupervised Prediction Alignment (UPA) if the data relationship has shifted [59]. |
| AI model performs well in lab validation but fails in clinical deployment. | Mismatch between training data (high-resolution, ideal conditions) and production data (noisy, real-world) [57]. | Use the Population Stability Index (PSI) to compare feature distributions between lab and clinical data [57]. | Retrain the model using data that is representative of the real-world deployment environment [57]. |
| In-shoe pressure readings become unreliable and noisy over time. | Sensor Hysteresis and Drift; physical degradation of flexible sensor materials (e.g., microcracks in conductive iongels) [58] [55]. | Perform a controlled calibration check against a reference sensor. Analyze the sensor's response curve for increased hysteresis. | Replace the physical sensor. For future designs, select materials with high resilience and proven long-term stability (>100,000 cycles) [55]. |
Experimental Protocol: Implementing Drift Detection
This protocol outlines how to set up a continuous drift monitoring system for a plantar pressure analysis pipeline.
Objective: To automatically detect data and concept drift in real-time data streams from a wearable plantar pressure monitoring system.
Materials:
- Deployed AI model for pressure analysis (e.g., for gait event detection or ulcer risk prediction).
- Historical training data (the reference dataset).
- Stream of new, unlabeled plantar pressure data.
- Computational environment (e.g., Python with Scikit-learn, SciPy).
Methodology:
- Establish Baseline: Use the original training dataset as your reference distribution (P).
- Define Monitoring Window: Continuously collect new sensor data in batches (e.g., daily or weekly). This is your target distribution (Q).
- Calculate Drift Metrics: For each new batch of data:
- For Data Drift: Apply the Kolmogorov-Smirnov test to compare the distribution of key input features (e.g., peak heel pressure) between P and Q. A low p-value (<0.05) suggests significant drift [57].
- For Prediction Drift: Monitor the distribution of the AI's output scores. A shift in this distribution can invalidate calibrated decision thresholds [59].
- Set Alert Threshold: Define a threshold for the drift metric (e.g., PSI > 0.1) that triggers an alert for the research team [57].
- Root Cause Analysis: Upon triggering an alert, investigate potential causes (sensor hardware issues, changes in participant demographics, etc.).
Workflow Diagram for Drift Management
The following diagram illustrates the logical workflow for maintaining an AI-powered plantar pressure analysis system, from detecting drift to implementing a correction.
Research Reagent Solutions: Essential Materials for Stable Plantar Sensing
This table details key materials and components for developing reliable plantar pressure sensors, as identified in the research literature.
| Item | Function / Description | Relevance to Research |
|---|---|---|
| PMMA Conductive Iongel | A flexible electrode material with high compression strength (>10 MPa) and rapid self-recovery [55]. | Ideal for creating durable, long-life capacitive pressure sensors that can withstand repetitive body-weight loading. |
| Capacitive Pressure Sensor Array | A grid of sensors that measures pressure distribution by changes in capacitance [55]. | The preferred sensing mechanism for high-resolution spatial and temporal plantar pressure mapping. |
| Flexible Pressure Platforms | Thin, in-shoe systems that are minimally obtrusive; often wireless for natural movement [58]. | Critical for collecting valid ecological data during daily activities or sports, improving participant compliance. |
| Surface EMG (sEMG) | Measures myoelectric activity of muscles (e.g., gastrocnemius) to validate fatigue or gait changes [60]. | Used as a ground-truth measurement to correlate changes in plantar pressure with neuromuscular activity. |
| Unsupervised Prediction Alignment (UPA) | An AI algorithm that corrects performance drift without new labeled data [59]. | A core software tool for maintaining the accuracy of analytical models over long-term studies despite sensor or population shifts. |
Validating Calibration and Comparing Measurement System Performance
FAQ: Understanding ICCs and Reliability
What does the Intraclass Correlation Coefficient (ICC) measure in the context of plantar pressure assessment? The Intraclass Correlation Coefficient (ICC) quantifies the test-retest reliability of a measurement system. It assesses how consistently plantar pressure measurement systems produce similar results under the same conditions across multiple testing sessions. An ICC value provides a statistical measure of agreement, indicating whether the device can reliably detect true changes in a patient's condition versus measurement error. Values range from 0 to 1, with higher values indicating greater reliability [61] [62].
What ICC value indicates "excellent" reliability for plantar pressure systems? For plantar pressure measurement systems, ICC values are generally interpreted as follows:
- ICC > 0.90: Excellent reliability
- ICC = 0.75 - 0.90: Good reliability
- ICC < 0.75: Poor to moderate reliability
Multiple studies on in-shoe pressure systems have reported ICC values greater than 0.75 and often approximately 0.9 for key parameters like peak pressure across various walking conditions, which confirms their high reliability for both research and clinical applications [61] [63] [62].
Why is test-retest reliability crucial for plantar pressure research? High test-retest reliability is fundamental for:
- Accurate Long-Term Tracking: It ensures that observed changes in plantar pressure over time (e.g., due to disease progression or rehabilitation) reflect true physiological changes rather than measurement error.
- Confident Clinical Decision-Making: Reliable data is essential for diagnosing foot pathologies, assessing the severity of conditions, and evaluating the efficacy of treatments or orthotic interventions.
- Valid Research Outcomes: It underpins the integrity of scientific studies investigating gait, footwear, or therapeutic interventions [61] [11].
Troubleshooting Guide: Addressing Common Reliability Issues
Problem: Low ICC Values Indicating Poor Test-Retest Reliability
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Insufficient Step Count | Review the number of steps analyzed per trial. | Increase the number of steps collected. One study recommended 50 steps for excellent reliability of dynamic variables (peak force, pressure, contact area), while another suggested minimum walking distances of 207m (LIN), 255m (CW), and 467m (CCW) to achieve an ICC ≥ 0.90 [61] [62]. |
| Inconsistent Sensor Placement | Verify insole positioning between sessions. Check for sensor migration or shear. | Use standardized, well-fitting shoes. Mark the insole and shoe to ensure consistent placement across test sessions. Consider systems where sensors are embedded in the footwear to minimize this risk [61] [62]. |
| Variable Gait Speed | Check if walking/running speed was controlled and consistent between tests. | Use photoelectric cells or a treadmill to control and monitor speed during testing. Standardize speeds across sessions (e.g., walking at 1.2–1.4 m/s) [63]. |
| Environmental & Device Factors | Inspect sensors for physical damage or contamination. Check power supply and wiring. | Perform regular calibration according to the manufacturer's instructions. Store insoles properly and inspect them before use. Ensure a stable power supply and secure connections [64] [65]. |
Problem: Inconsistent or Erratic Pressure Readings
| Potential Cause | Diagnostic Steps | Corrective Action |
|---|---|---|
| Electrical Connection Issues | Use a multimeter to check for correct supply voltage and stable output. | Ensure all wiring connections are secure and correct according to the datasheet. Check for reversed polarity [64] [65]. |
| Sensor Blockage or Damage | Inspect the pressure port for obstructions (e.g., from an over-compressed sealing ring). | Choose sealing rings of appropriate hardness and thickness. Avoid over-tightening the sensor during installation. Clean ports regularly to prevent blockage [65]. |
| Environmental Stressors | Evaluate exposure to extreme temperatures, humidity, or mechanical vibration. | Protect the system from harsh environmental conditions. For extreme environments, use specialized sensors designed with features like remote electronics or high-temperature materials [29]. |
Experimental Protocols for Establishing Reliability
Standard Test-Retest Protocol for Plantar Pressure Systems
The following workflow outlines a general methodology for conducting a test-retest reliability study, synthesized from established research protocols [61] [63] [62].
Key Procedural Details:
- Participant Preparation: Participants should wear standardized footwear and socks. A familiarization period of 1-10 minutes is critical to minimize learning effects [61] [63].
- Walking Conditions: Protocols often include a mix of:
- Linear Walking (LIN): A straight-path walk of sufficient distance (e.g., 20m).
- Curved Walking (CW/CCW): Walking along a circular path (e.g., 1.2m radius) to simulate natural gait. This is important as patients with neurological disorders may show more pronounced deficits on curved paths [61] [62].
- Other Movements: Static standing, running, or jumping [63].
- Data Collection: Multiple trials (e.g., 2 trials of 20m) should be performed for each condition. The first and last steps of a trial are often excluded from analysis due to acceleration and deceleration [62].
- Consistency is Critical: The same tester, instructions, laboratory environment, and time of day should be maintained across sessions to reduce variability [62].
Statistical Analysis Workflow
Once data is collected, the following statistical procedure is used to calculate and interpret reliability metrics.
Analysis Details:
- ICC Model: For test-retest reliability, a two-way mixed-effects model assessing absolute agreement (ICC(3,k)) is often appropriate because the same subjects are measured by the same fixed set of raters (the device) on two occasions [62].
- Supplementary Metrics:
- Standard Error of Measurement (SEM): Provides an estimate of measurement error in the same units as the original measure.
- Minimal Detectable Change (MDC): The smallest change in a score that must be observed to be considered a true change, beyond measurement error. This is calculated as MDC = SEM × z-value × √2 [62].
The table below consolidates key reliability findings from recent studies on different plantar pressure measurement systems.
| Pressure System / Study | Key Parameters Analyzed | Walking Conditions | Reported ICC Values | Minimum Steps / Distance for ICC ≥0.90 |
|---|---|---|---|---|
| Wearable In-Shoe System [61] | PP, PTI, FWHM, MaxPG, AP | LIN, CW, CCW | ICC ≈ 0.9 for most parameters | LIN: 207 mCW: 255 mCCW: 467 m |
| Pedar-X System [62] | PF, PP, CA, S (Temporal) | LIN, CW, CCW | PF, PP, CA: >0.90 (all regions)S: >0.60 (with 50 steps) | 50 steps for PF, PP, CA. >200 steps for temporal variable (S) |
| GP MobilData WiFi [63] | vGRF during static and dynamic movements | Standing, Walking, Running, Jumping | Excellent agreement (ICC > 0.75) for validity and reliability | Not Specified |
PP (Peak Pressure), PTI (Pressure-Time Integral), FWHM (Full Width at Half Maximum), MaxPG (Maximum Pressure Gradient), AP (Average Pressure), PF (Peak Force), CA (Contact Area), S (Stance Duration), vGRF (vertical Ground Reaction Force).
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in Research | Example / Specification |
|---|---|---|
| Gold Standard Criterion Device | Serves as a benchmark for validating new insole systems. | Force Plates (e.g., Kistler), established lab-based systems like the Pedar-X [63] [11]. |
| Calibration Unit | Ensures the accuracy and consistency of pressure sensor readings before data collection. | Manufacturer-provided calibration device (e.g., Trublu for Pedar) [62]. |
| Standardized Footwear | Controls for the confounding effect of different shoe types on plantar pressure. | Identical shoe model (e.g., sneakers) in various sizes for all participants [61] [62]. |
| Speed Monitoring System | Controls and monitors gait speed, a critical factor affecting plantar pressure. | Photoelectric cells (e.g., WITTY, Microgate) or treadmills [63]. |
| Data Acquisition & Analysis Software | Used for collecting, processing, and analyzing plantar pressure data. | Manufacturer software (e.g., Novel Pedar, GP Manager) or custom scripts in MATLAB/Python [63] [62]. |
Frequently Asked Questions (FAQs)
Fundamental Concepts
Q1: What is the primary purpose of Bland-Altman analysis in method comparison studies? Bland-Altman analysis is used to assess the agreement between two quantitative measurement techniques. Unlike correlation, which measures the strength of a relationship, it quantifies the agreement by evaluating the differences between paired measurements. The analysis involves plotting these differences against the averages of the two methods and calculating limits of agreement (LoA), which define the range within which 95% of the differences between the two methods are expected to fall [66] [67].
Q2: When should I use the Minimal Detectable Change (MDC) in my research? The MDC is used when you need to determine whether a change in a measured variable for a single subject or a group represents a true change that is greater than the measurement error. It is the smallest change in a score that must be observed to be confident that a real change has occurred. This is paramount in monitoring patient progress over time, such as after a rehabilitation program, or in evaluating the effectiveness of an intervention in clinical research [68] [69] [70].
Q3: My data shows that the differences between methods get larger as the average measurement increases. Which Bland-Altman method should I use? For data that exhibits this pattern, known as heteroscedasticity, the standard parametric Bland-Altman plot may be misleading. In this case, you should use one of the following alternative methods available in statistical software [66]:
- Plot ratios: This option uses ratios instead of absolute differences.
- Plot differences as a percentage: This expresses the differences as a percentage of the measurement magnitude.
- Regression-Based Bland-Altman method: This advanced method models the bias and the limits of agreement as functions of the measurement magnitude, providing more accurate LoA across the measurement range.
Implementation and Calculation
Q4: How do I calculate the 95% Limits of Agreement in a standard Bland-Altman analysis? The calculation is straightforward [66] [67]:
- Calculate the differences between the two paired measurements (e.g., Method A - Method B).
- Compute the mean of these differences (this represents the average bias).
- Calculate the standard deviation (SD) of the differences.
- The 95% Limits of Agreement are then: Mean difference ± 1.96 × SD of the differences.
Q5: How is the Minimal Detectable Change (MDC) calculated? The MDC is derived from the Standard Error of Measurement (SEM). The common calculation steps are [68] [69] [70]:
- Calculate the SEM: This can be estimated from test-retest data. One common method is using the square root of the mean square error term from an Analysis of Variance (ANOVA) model, or from the residuals of a Linear Mixed-Effects Model (LMM) if a steady-state between tests cannot be assumed [68]. The SEM can also be calculated as SD√(1-ICC), where SD is the standard deviation of the baseline scores and ICC is the intraclass correlation coefficient [69].
- Calculate the MDC: The formula for the 95% confidence level is: MDC = SEM × 1.96 × √2 The √2 accounts for the additional uncertainty introduced when comparing two measurements, each containing error.
Q6: What is the difference between relative and absolute reliability measures?
- Absolute Reliability quantifies the measurement error in the actual units of the measurement. The SEM, Limits of Agreement, and MDC are all measures of absolute reliability. They are directly interpretable in the context of the measurement's scale (e.g., MDC of 0.13 m/s for gait speed) [68] [69].
- Relative Reliability assesses how well subjects can be distinguished from each other despite measurement error, often expressed as a ratio. The Intraclass Correlation Coefficient (ICC) is a common measure of relative reliability. It is important to note that a high ICC (good relative reliability) does not guarantee a small MDC (good absolute reliability) [69].
Interpretation and Reporting
Q7: How do I know if the limits of agreement from my Bland-Altman analysis are acceptable? The Bland-Altman plot itself does not define acceptability. The limits of agreement must be compared to a pre-defined clinically acceptable difference (Δ). This value is not a statistical calculation but is determined based on clinical requirements, biological considerations, or other goals. If the limits of agreement fall within the range -Δ to +Δ, the two methods can be considered to agree sufficiently for your intended purpose [66] [67].
Q8: I've calculated an MDC% of 15% for my Timed Up and Go test duration. How should I interpret this? An MDC% of 15% means that for an individual patient, the TUG test duration must change by at least 15% from its baseline value for you to be 95% confident that this change is real and not just due to measurement error. For example, if a patient's baseline TUG duration is 20 seconds, their score would need to decrease to below 17 seconds (85% of 20 seconds) to indicate a true improvement [68].
Troubleshooting Guides
Issue 1: Disagreement Between Correlation and Bland-Altman Results
Problem: You find a high correlation coefficient (r > 0.9) between two measurement methods, but the Bland-Altman plot shows a wide spread of differences and a significant bias.
Explanation: This is a common and critical misunderstanding. A high correlation only indicates that the two methods produce results that are linearly related; it does not mean they agree. The two methods could consistently differ by a large amount (bias) and still have a perfect correlation. The Bland-Altman analysis is the correct tool for assessing agreement [67].
Solution:
- Ignore the correlation coefficient for agreement studies.
- Focus on the Bland-Altman plot. Examine the mean difference (bias) and the limits of agreement.
- Judge clinically: Determine if the observed bias and the width of the limits of agreement are acceptable for your specific application [66].
Issue 2: Handling Non-Normal Distribution of Differences in Bland-Altman Analysis
Problem: The differences between your two measurement methods do not follow a normal distribution, violating an assumption of the standard parametric Bland-Altman analysis.
Solution:
- Non-Parametric Method: Use the non-parametric Bland-Altman method. Instead of using the mean and standard deviation, this method defines the limits of agreement using the 2.5th and 97.5th percentiles of the differences [66].
- Data Transformation: Try transforming your data (e.g., a natural log transformation) to achieve normality. After analysis, the results can be back-transformed and expressed as percentages, as was done in the gait study for TUG duration and angular velocity peak [68].
Issue 3: Calculating MDC with Intervention Between Test Sessions
Problem: You have collected data before and after a rehabilitation program, but the conventional MDC calculation requires a steady-state condition (no real change) between test and retest.
Solution:
- Use Linear Mixed-Effects Models (LMMs): A novel method allows for the estimation of SEM even when the steady-state assumption is violated. LMMs can incorporate time and treatment effects as fixed effects, while using random effects to account for inter-individual variation. The SEM is then estimated from the model's residuals, allowing for a valid MDC calculation from pre-post intervention data [68].
Decision Workflow for Selecting the Appropriate MDC Calculation Method
Issue 4: High MDC Value Making Clinical Interpretation Difficult
Problem: Your calculated MDC is very large, meaning that a huge change in the measure is required to be considered real, which reduces the clinical utility of your measurement tool.
Solution:
- Investigate the source of error: A high MDC indicates large measurement error. Investigate potential sources, such as:
- Improve your protocol: Implement stricter standardization of testing procedures, provide more training for raters, or use the average of multiple trials to improve reliability [68] [69].
Experimental Protocols & Data Presentation
Detailed Protocol: Establishing MDC for a Gait Measure
This protocol is adapted from research on neurological patients [68].
Objective: To determine the Minimal Detectable Change for gait speed and Timed Up and Go (TUG) test parameters in older adults with neurological diseases.
Participants:
- Inclusion Criteria: Adults over 65 with a neurologically-based gait impairment (e.g., stroke, peripheral neuropathy).
- Exclusion Criteria: Inability to complete tests without assistance, severe visual/hearing impairment, completing the TUG test in >30 seconds.
Materials:
- Inertial Measurement Unit (IMU) sensors.
- Stopwatch.
- Standard chair, traffic cone.
- A 10-meter walkway.
Procedure:
- Session 1 (T0): At the beginning of a rehabilitation program.
- 10-meter walk test: Participants walk 10 meters at a comfortable speed. Time is recorded for the central 6 meters to calculate gait speed (m/s). Perform two trials.
- TUG test: Participants stand from a chair, walk 3 meters, turn around a cone, walk back, and sit down. Time is recorded with a stopwatch (TTD). Trunk kinematics are recorded with an IMU to extract measures like peak turning angular velocity (ωpeak). Perform two trials.
- Session 2 (T1): Repeat the exact same assessment procedure at the end of the rehabilitation program.
Statistical Analysis:
- Data Preparation: For each participant and session, calculate the mean value of the two trials for each measure (gait speed, TTD, ωpeak).
- SEM Estimation using LMMs: Fit a Linear Mixed-Effects Model for each measure. The model includes the session (T0/T1) as a fixed effect and random intercepts and slopes for participants. The SEM is calculated as the square root of the residual variance from the model.
- MDC Calculation: Compute the MDC at the 95% confidence level: MDC = SEM × 1.96 × √2.
Quantitative Data from Literature
Table 1: Minimal Detectable Change (MDC) Values for Various Measures
| Measure | Population | MDC | MDC% | Notes | Source |
|---|---|---|---|---|---|
| Gait Speed | Older neurological adults | 0.13 m/s | - | Calculated via LMMs | [68] |
| TUG Duration (TTD) | Older neurological adults | 15% of baseline | 15% | Ln-transformed, expressed as % change | [68] |
| TUG Peak Angular Velocity (ωpeak) | Older neurological adults | 25% of baseline | 25% | Ln-transformed, expressed as % change | [68] |
| Step Time Variability | Younger Adults | - | - | Smaller MDC than older adults | [69] |
| Older Adults | - | - | Larger MDC than younger adults | [69] | |
| Purdue Pegboard (Dominant Hand) | Patients with schizophrenia | 3.0 pins | 22.9% | Based on SEM | [70] |
Table 2: Comparison of Bland-Altman Analysis Methods
| Method | Key Feature | Best Used When... | Limits of Agreement Calculation |
|---|---|---|---|
| Parametric (Conventional) | Assumes normal distribution of differences and constant variance (homoscedasticity). | Data meets assumptions of normality and homoscedasticity. | Mean difference ± 1.96 × SD of differences |
| Non-Parametric | Makes no assumption about the distribution of differences. | Differences are not normally distributed. | 2.5th and 97.5th percentiles of the differences |
| Regression-Based | Models changing bias and variance across the measurement range. | Variance of differences changes with magnitude (heteroscedasticity). | Complex; based on regressing differences and absolute residuals on the averages. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Plantar Pressure and Gait Validation Studies
| Item | Function / Application | Example / Specification |
|---|---|---|
| Pressure Measurement Platforms | High-accuracy, high-spatial-resolution measurement of barefoot plantar pressure in lab settings. Considered the "gold standard" for static and walking analyses [1] [2] [4]. | Rigid, floor-embedded systems (e.g., from companies like Tekscan, RSscan). |
| In-Shoe Pressure Measurement Systems | Portable assessment of foot-shoe interface pressure during dynamic activities, sports, and daily life. Essential for orthotic and footwear design validation [1] [2] [4]. | Flexible insoles with sensor arrays (e.g., F-Scan, Pedar). Systems can be wireless. |
| Inertial Measurement Units (IMUs) | Objective quantification of balance and mobility characteristics beyond simple timing. Provides kinematic data (acceleration, angular velocity) during functional tests [68]. | Lightweight sensors placed on the lower trunk or limbs (e.g., mHT system). |
| Calibration Equipment | Ensuring the validity and reliability of pressure sensor outputs. Critical for converting raw sensor signals (e.g., capacitance) into accurate pressure values [71] [72]. | Force plates, tensile/compression test machines (e.g., Hounsfield H10KS), or custom isotropic pressure chambers [71]. |
| Linear Mixed-Effects Models (LMMs) | Advanced statistical software for calculating the Standard Error of Measurement (SEM) in complex longitudinal studies where the steady-state assumption is violated [68]. | Statistical packages in R (lme4), Python (statsmodels), SPSS, or SAS. |
General Workflow for Calibrating a Sensorized Insole
The measurement of foot plantar pressure is a critical biomechanical tool for diagnosing lower limb problems, footwear design, sport biomechanics, and injury prevention [4]. Plantar pressure refers to the pressure field that acts between the foot and the support surface during everyday locomotor activities [4]. These measurement systems have evolved significantly, with current technologies broadly classified into two categories: platform systems (also called pressure platforms or force plates) and in-shoe systems (wearable sensor-equipped insoles) [4] [3]. Understanding the fundamental differences, accuracy parameters, and optimal use-cases for each system is essential for researchers conducting sensor calibration studies and clinical professionals implementing these technologies in practice.
Platform systems are constructed from flat, rigid arrays of pressure sensing elements arranged in a matrix configuration and embedded in the floor to allow assessment of normal gait [4]. These systems are typically used in laboratory settings for both static and dynamic studies. In contrast, in-shoe systems incorporate flexible sensors embedded within footwear to measure the interface pressure between the foot plantar surface and the shoe sole [4] [3]. This fundamental distinction in implementation drives differences in data characteristics, calibration requirements, and appropriate applications that researchers must consider when designing experiments and interpreting results.
Technical Specifications and Performance Comparison
Key Technical Differences
The technical specifications of platform and in-shoe systems diverge significantly due to their distinct design paradigms and operational environments. Platform systems generally offer higher spatial resolution and sampling frequencies, making them suitable for detailed biomechanical analysis of barefoot gait [3]. In-shoe systems prioritize portability and real-world applicability, typically featuring lower spatial resolution due to fewer sensors but enabling assessment of shod conditions over multiple steps [4] [3].
Table 1: Technical Specification Comparison Between Systems
| Parameter | Platform Systems | In-Shoe Systems |
|---|---|---|
| Spatial Resolution | High (dense sensor arrays) | Lower (fewer sensors) [4] [3] |
| Sampling Frequency | Typically high (often >100Hz) | Variable (e.g., 20-75Hz cited) [7] [73] |
| Sensor Type | Rigid array sensors | Flexible sensors (resistive, capacitive, piezoelectric) [3] |
| Measurement Environment | Laboratory setting | Real-world, various terrains [4] |
| Typical Applications | Barefoot analysis, posture assessment | Therapeutic footwear, daily activity monitoring [4] [3] |
| Data Collection | Limited to platform contact | Multiple steps during continuous walking [7] |
| Key Strength | High accuracy for barefoot assessment | Ecological validity for shod conditions [3] |
Accuracy and Reliability Metrics
Recent studies have quantified the performance characteristics of both system types. A 2025 comparative analysis reported that pressure platform systems like Physiosensing provide more uniform measurement of contact area, proving efficient for weight distribution and stability analysis [3]. The same study found that in-shoe systems such as Pedar demonstrate higher capacity in peak pressure point detection, making them more suitable for applications requiring precise high-pressure zone localization [3].
Test-retest reliability assessments of wearable in-shoe systems have shown excellent performance, with intraclass correlation coefficients (ICCs) of approximately 0.9 for most parameters across various walking conditions, including linear and curved trajectories [7]. For whole-foot analysis, all measured variables presented ICCs > 0.60, confirming high reliability [7]. The minimum distances required to achieve excellent reliability (ICC ≥ 0.90) were established at 207 meters for linear walking, 255 meters for clockwise curved walking, and 467 meters for counterclockwise curved walking [7].
Validation studies of specific in-shoe systems like the XSENSOR X4 have demonstrated measurement errors of <10% for average peak and mean pressures, with reliability error of 3-10% for peak pressure, falling within the 15% threshold defined as an analytical goal for clinical applications [73]. Regional analysis showed mean contact area errors of less than 1 cm² for both insoles and high repeatability (ICC ≥ 0.939) [73].
Table 2: Quantitative Performance Metrics from Recent Studies
| Performance Metric | Platform Systems | In-Shoe Systems | Study Details |
|---|---|---|---|
| Contact Area Accuracy | More uniform measurement [3] | Mean error <1 cm² [73] | Regional protocol validation [73] |
| Peak Pressure Detection | Standard accuracy | Higher capacity for localization [3] | Comparative device analysis [3] |
| Test-Retest Reliability (ICC) | Not specified | 0.60->0.90 across parameters [7] | Linear and curved walking [7] |
| Minimum Distance for Reliability | Not applicable | 207-467 meters depending on path [7] | Healthy participants (n=31) [7] |
| Whole Insole Measurement Error | Not applicable | <10% for peak/mean pressure [73] | Pressure range 50-600 kPa [73] |
Troubleshooting Guides and FAQs
Common Experimental Challenges and Solutions
Q: Our in-shoe pressure data shows significant variability between trials. What might be causing this and how can we address it?
A: Variability in in-shoe pressure data can stem from multiple sources. First, ensure adequate familiarization with the footwear system, as adaptation periods of 1-2 minutes are recommended before formal data collection [7]. Second, verify that sensors are securely positioned to prevent slippage, which can cause unreliable results [4]. Third, consider the number of steps collected - recent research indicates that for linear walking, approximately 207 meters of walking distance (equivalent to multiple steps) is needed to achieve excellent reliability (ICC ≥ 0.90) [7]. Finally, implement standardized protocols for donning/doffing procedures between trials to ensure consistent sensor placement.
Q: We're observing discrepancies between platform and in-shoe measurements for the same participants. Which system should we trust?
A: Discrepancies are expected as these systems measure fundamentally different interfaces [74]. Platform systems capture barefoot or shod foot-to-ground pressure, while in-shoe systems measure foot-to-shoe interface pressure [4] [3] [74]. A 2010 comparative study confirmed significant differences in parameters such as center of pressure displacement and average peak pressure across conditions [74]. The choice of system should align with your research question: use platforms for barefoot biomechanical assessment and in-shoe systems for evaluating footwear interventions or real-world gait patterns [3]. Never treat data from these systems as interchangeable without appropriate validation studies [74].
Q: Our pressure sensors demonstrate drift during extended static measurements. Is this normal and how can we compensate?
A: Drift, particularly in capacitive-based sensor systems, is a recognized technical limitation [73]. This creep effect occurs when sensors are exposed to extended loading periods [73]. For static or prolonged protocols, consider implementing baseline corrections and limiting measurement duration. Research indicates that systems like the Pedar demonstrate high repeatability between days, while others like the Tekscan may show significant creep (19% within 15 minutes) [73]. If your protocol requires extended static measurements, select systems with known performance characteristics for such applications or incorporate regular recalibration intervals.
Q: What are the key considerations for sensor calibration in plantar pressure research?
A: Effective calibration must address several critical sensor performance parameters [4]:
- Hysteresis: Determine by observing output signals when sensors are loaded and unloaded, as differing responses indicate hysteresis [4]
- Linearity: Assess response to applied pressure; highly linear responses simplify signal processing circuitry [4]
- Temperature sensitivity: Evaluate in the 20°C to 37°C range as ambient temperature affects readings [4]
- Pressure range: Select sensors appropriate for your expected pressure ranges, as different applications require different operating pressures [4] Implement both whole insole protocols (even loading across surface at range of pressures: 50-600 kPa) and regional protocols (targeted loading with different surface areas) for comprehensive calibration [73].
Protocol Implementation Issues
Q: How many steps are sufficient for reliable plantar pressure assessment during walking?
A: The required number of steps depends on the walking condition and desired reliability level. Recent research established that for linear walking, 207 meters is needed to achieve ICC ≥ 0.90, while clockwise curved walking requires 255 meters, and counterclockwise curved walking requires 467 meters [7]. Previous studies have suggested varying requirements, with some systems like the Pedar-X needing 400 steps in treadmill exercise for accurate measurement, while others found 5-8 steps sufficient for reliable gait parameters during linear walking [7]. For clinical applications, err on the side of more steps, particularly when assessing curved paths which show greater variability.
Q: What factors most significantly impact the validity of in-shoe pressure measurements?
A: Key factors affecting validity include [4] [73]:
- Sensor type and technology: Capacitive sensors may succumb to creep during extended loading
- Spatial resolution: Higher resolution systems (more sensels) provide more precise contact area measurements
- Calibration procedures: Implement both whole insole and regional calibration protocols
- Sampling frequency: Must be appropriate for the activity (e.g., running requires higher frequencies)
- Environmental factors: Temperature fluctuations can affect sensor readings
- User factors: Body weight, gait speed, and foot morphology influence pressure distributions
Experimental Design and Methodologies
System Selection Workflow
The following diagram illustrates the decision process for selecting between platform and in-shoe measurement systems based on research objectives:
Comprehensive Validation Protocol
For researchers validating plantar pressure measurement systems, the following integrated methodology combines elements from multiple established protocols:
Whole Insole Validation Protocol:
- Apparatus Setup: Use calibrated pressure application device (e.g., TruBlue calibration device) capable of applying even pressure across entire insole surface [73]
- Pressure Application: Apply pressures from 50-600 kPa in increments (50, 100, 200, 300, 400, 500, 600 kPa), maintaining each pressure for 30 seconds at ±2% tolerance [73]
- Data Collection: Record measurements at multiple time points (0, 2, 10, and 30 seconds) to assess temporal effects [73]
- Analysis: Calculate mean and peak pressure measurement errors (MErr) compared to target pressures [73]
Regional Validation Protocol:
- Test Apparatus: Prepare cylinders with different surface areas (3.14 cm² and 15.9 cm²) representing anatomical regions like metatarsal heads and calcaneus [73]
- Loading Conditions: Apply pressures of 50, 110, and 200 kPa to each insole region using weights [73]
- Measurement: Record three trials of 30 seconds for each condition [73]
- Analysis: Calculate contact area error (AErr) as root mean square error compared to known cylinder area [73]
Clinical/Gait Validation:
- Participant Preparation: Standardize footwear and provide 1-2 minute adaptation period before data collection [7]
- Walking Protocols: Implement linear and curved walking conditions with sufficient distance (≥207m for linear, ≥467m for curved paths) [7]
- Data Collection: Ensure consistent starting positions and eliminate initial/terminal steps from analysis [7]
- Reliability Assessment: Calculate intraclass correlation coefficients (ICCs), Bland-Altman plots, and minimal detectable changes (MDCs) [7]
Essential Research Reagents and Materials
Table 3: Essential Research Materials for Plantar Pressure Experiments
| Item | Function/Application | Technical Specifications |
|---|---|---|
| Calibration Device | Even pressure application across insole surface | Capable of 50-600 kPa range with ±2% stability [73] |
| Test Cylinders | Regional loading simulation | Multiple surface areas (3.14 cm², 15.9 cm²) [73] |
| Standardized Footwear | Consistent experimental conditions | Multiple sizes, neutral design to minimize interference [7] |
| Weight Application System | Precise pressure application for regional protocols | Calibrated weights for 50, 110, 200 kPa pressures [73] |
| Data Processing Software | Analysis of pressure parameters | Custom scripts (Python) for specialized calculations [73] |
| Temperature Monitoring | Environmental control | Ambient temperature recording (20-37°C range) [4] |
| Motion Capture Equipment | Complementary gait analysis | Synchronization with pressure data for comprehensive assessment |
The comparative analysis reveals that platform and in-shoe plantar pressure measurement systems serve complementary rather than interchangeable roles in research and clinical practice. Platform systems excel in laboratory-based assessment of barefoot biomechanics, offering high spatial resolution and uniform contact area measurement [3]. In-shoe systems provide superior ecological validity for evaluating footwear interventions and monitoring real-world activity patterns, with demonstrated reliability for both linear and curved walking trajectories [7] [3].
Researchers must align system selection with specific experimental questions rather than seeking a universal solution. For barefoot posture assessment and detailed biomechanical analysis, platform systems remain the gold standard. For therapeutic footwear development, orthotic evaluation, and real-world gait assessment, in-shoe systems offer irreplaceable benefits despite their lower spatial resolution [4] [3]. Future developments in sensor technology, wireless communication, and data processing algorithms will continue to enhance both approaches, but the fundamental distinction in their measurement paradigms will maintain their complementary roles in plantar pressure assessment.
FAQs: Utilizing Public Datasets for Plantar Pressure Research
1. What are the key advantages of using public datasets like UNB StepUP-P150 for validating plantar pressure sensor calibration?
Public datasets provide large-scale, standardized data that allows researchers to benchmark their calibration algorithms against a common reference. The UNB StepUP-P150 dataset, for instance, offers over 200,000 footsteps from 150 individuals across varying conditions (barefoot, different footwear, and walking speeds) [8]. This volume and diversity help ensure that your calibration method is robust across a representative population and different real-world scenarios, reducing the risk of overfitting to limited, custom-collected data.
2. How can I address the challenge of different hardware systems when using multicenter public data for calibration validation?
Variations in hardware (e.g., sensor type, resolution, and manufacturer) between public datasets and your own system are a common challenge. A strategy is to leverage machine learning models that demonstrate robustness across multiple data sources. One approach is to use a U-Net model for segmenting the plantar pressure image into anatomical zones, which has been shown to maintain high accuracy (Median Dice Scores ≥ 0.88) even when trained on data from different pressure measurement systems [75]. Focusing on relative metrics and normalized data during analysis can also mitigate hardware-specific discrepancies.
3. My research involves low-cost sensor systems. How can public datasets, often collected with high-end equipment, be relevant?
Public datasets are highly valuable for low-cost sensor research through a supervised learning approach. You can use the high-fidelity data from a system like F-Scan (often used in labs) as the ground truth to train a model that predicts the same metrics from your low-cost sensor data. For example, one study successfully used data from an F-Scan system to train a Recurrent Neural Network (RNN) that accurately predicts Ground Reaction Force (GRF) and Center of Pressure (CoP) using input from only six low-cost Force-Sensing Resistor (FSR) sensors [38]. This transfers the accuracy of the lab-grade system to your affordable platform.
4. What should I look for in a public dataset to ensure it is suitable for validating my calibration technique?
When selecting a public dataset, verify that it includes:
- Detailed Metadata: Information about participant demographics (age, weight, foot dimensions), footwear conditions, and walking speeds is crucial for testing your calibration's robustness across covariates [8].
- Raw and Processed Data: Access to raw data allows you to apply your own preprocessing and segmentation routines, while pre-processed data (e.g., footsteps already segmented and aligned) can accelerate prototyping [8].
- Technical Specifications: The sensor type (e.g., capacitive, piezoresistive), spatial resolution (e.g., sensors/cm²), and sampling frequency should be documented to understand the data's characteristics and limitations [1] [8].
5. How can AI and machine learning be integrated with public datasets to improve calibration?
AI can automate and enhance several aspects of calibration and validation:
- Automated Segmentation: ML models can replace manual, proportion-based foot segmentation, which is especially useful for atypical foot structures and low-quality data [75].
- Data Prediction: Neural networks, including RNNs, can learn the complex relationship between low-fidelity sensor outputs and high-fidelity ground truth data from public datasets, enabling accurate prediction of key metrics like GRF and CoP [38].
- Trend Analysis: AI can assist in the analysis and interpretation of complex plantar pressure data, identifying patterns that might be missed by traditional methods, thus informing the calibration process [1].
Troubleshooting Guides
Issue 1: Poor Correlation Between Custom Sensor Data and Public Dataset Ground Truth
Problem: After collecting data with your custom plantar pressure system, the calculated metrics (e.g., GRF, CoP trajectory) show a weak correlation with the ground truth values derived from a public dataset or a laboratory validation system.
Solution: Follow this structured diagnostic workflow.
Additional Considerations:
- Data Sufficiency: For machine learning approaches, ensure you have a sufficient amount of simultaneous data from your sensor and a reference system to train the model effectively [38].
- Environmental Factors: If testing in harsh environments, consider factors like temperature extremes or humidity, which can cause accuracy drift and require specialized calibration troubleshooting [29].
Issue 2: Inconsistent Results When Applying a Model Trained on a Public Dataset
Problem: A calibration or analysis model (e.g., a segmentation U-Net or GRF-prediction RNN) that performed well on a public dataset produces inaccurate results when applied to your in-house data.
Solution:
- Action 1: Check Data Fidelity and Formatting: Ensure your data is preprocessed to match the input specifications of the model. This includes matching the spatial resolution, data type, value normalization, and file format used in the original training dataset.
- Action 2: Perform Domain Adaptation: The public dataset and your data may be from different "domains" (e.g., different sensor types or populations). If possible, fine-tune the pre-trained model on a small, labeled subset of your own data. This helps the model adapt to the specific characteristics of your system [75].
- Action 3: Validate Against a Subset: Collect a small but statistically significant validation set in your lab where you simultaneously record data from your system and a gold-standard reference (if available). This will help you quantify the performance drop and identify the specific conditions under which the model fails.
Issue 3: High Error in Anatomical Landmark Detection from Plantar Pressure Data
Problem: When using an automated tool to identify key points like the center of the metatarsal area or interdigital spaces, the error is high, affecting subsequent analysis like hallux angle calculation.
Solution:
- Action 1: Evaluate Segmentation Quality: The accuracy of key point detection often depends on precise prior segmentation. Verify the quality of the foot mask segmentation. For the center of metatarsal area 1, calculating it directly from a high-quality segmentation mask can be more accurate (lower median Euclidean distance) than using a separate regression model [75].
- Action 2: Use an Ensemble Model: For landmarks that are difficult to predict, such as the interdigital space, employing an ensemble of models (e.g., combining segmentation and regression outputs) can reduce error and improve robustness compared to a single model [75].
- Action 3: Implement Expert Review: For critical applications, incorporate a manual review step where an expert can correct the most egregious errors. This is especially valuable for cases with ambiguous boundaries, such as around metatarsal area 1 [75].
Research Reagent Solutions: Essential Materials for Plantar Pressure Experiments
The following table details key hardware and software components used in advanced plantar pressure research, as identified in the literature.
| Item/Reagent | Function & Application in Research | Key Specifications & Examples |
|---|---|---|
| High-Resolution Pressure Platform [1] [8] | Serves as a gold-standard ground truth for barefoot gait analysis. Used for validating in-shoe systems and collecting large-scale public datasets. | Spatial Resolution: e.g., 4 sensors/cm² [8].Active Area: e.g., 1.2m x 3.6m walkway [8].Manufacturers: Tekscan, Novel GmbH, XSENSOR [76]. |
| Instrumented Insoles (Lab-Grade) [1] | Provides reference data for in-shoe calibration and studies involving footwear or orthotics. Can be used as an output target for low-cost sensor models. | Systems: F-Scan, Pedar [38] [76].Use Case: Directly monitoring GRF and CoP values for algorithm training [38]. |
| Low-Cost Sensor Units [77] [38] | The target system for cost-effective calibration research. Data from these is mapped to lab-grade system outputs using machine learning. | Types: Force-Sensing Resistors (FSR), capacitive sensors [77] [38].Configuration: Often arranged in an array (e.g., 6-10 sensors) on the insole [38]. |
| Soft Robotic Sensors (SRS) [77] | Used in novel wearable form-factors (e.g., smart socks) to capture kinetic and kinematic data without requiring shoes. | Technology: Capacitive-based stretch and pressure sensors [77].Advantage: Can measure foot-ankle kinematics alongside pressure [77]. |
| Machine Learning Models [38] [75] | Software "reagents" for tasks like anatomical segmentation, landmark detection, and predicting high-quality metrics from low-cost sensor input. | U-Net: For robust, automated segmentation of plantar pressure images into anatomical zones [75].Recurrent Neural Network (RNN): For modeling time-series data to predict GRF and CoP from sequential sensor data [38]. |
Standard Experimental Protocol: Validating a Low-Cost Insole Using a Public Dataset Reference
This protocol outlines a methodology for using a public dataset to validate the calibration of a custom or low-cost plantar pressure measurement system.
Objective: To determine the accuracy of a low-cost insole system by benchmarking its output against the ground truth data from a public dataset, using a machine learning approach.
Workflow Diagram:
Step-by-Step Instructions:
Data Acquisition & Alignment:
- Simultaneous Collection: Fit participants with both the low-cost insole system (e.g., one equipped with 6 FSR sensors) and a lab-grade reference system like the F-Scan [38].
- Protocol: Have participants perform a series of activities that will be used for validation, such as walking at preferred, slow, and fast speeds. The conditions (e.g., barefoot vs. shod) should be chosen based on the scope of your calibration.
- Temporal Alignment: Synchronize the data collection start time and use a clear kinematic event (like a distinctive heel strike or a voluntary action like standing on toes) to align the data streams from both systems precisely during preprocessing [77].
Data Preprocessing:
- Segmentation: Segment the continuous data stream from both systems into individual footsteps.
- Feature Engineering: Instead of using raw pressure values, some studies calculate virtual forces from areas around the physical sensors to improve the prediction of GRF and CoP [38].
- Normalization: Normalize the input and output data to a common scale (e.g., 0-1) to facilitate model training.
Model Selection & Training:
- Architecture: Choose a model suitable for sequential data. A Recurrent Neural Network (RNN) is recommended as it can capture temporal dependencies within a gait cycle, leading to more accurate predictions of GRF and CoP than simple perceptron models [38].
- Training: Use the preprocessed data from the low-cost sensors as the input (X) and the corresponding data from the lab-grade system as the target output (Y). Train the model to learn the mapping from one to the other.
Model Validation & Benchmarking:
- Testing: Evaluate the trained model on a held-out test set of data that was not used during training.
- Metrics: Quantify performance using root mean square error (RMSE) and R-squared (R²) values. Compare the model's predictions against the lab-grade system's data. A strong model should show a high Pearson’s correlation coefficient (e.g., >0.85) and R-squared value (e.g., >0.88) [77] [38].
- Benchmarking: To claim robust validation, the final model should be tested on a completely separate, public dataset like UNB StepUP-P150 (if compatible) to demonstrate its generalizability beyond the original training data [8].
Technical Support Center: Troubleshooting Guides and FAQs
This section provides targeted support for researchers and professionals working with foot plantar pressure measurement systems, addressing common challenges in calibration, data reliability, and system operation.
Frequently Asked Questions (FAQs)
Q: What are the most frequent causes of calibration problems in sensing systems?
- A: Common issues include the use of contaminated or out-of-date buffer solutions, contamination of the reference electrolyte or diaphragm, and using an old or defective electrode. Additional problems arise from electrodes that were not hydrated long enough after dry storage, mechanically damaged membranes, or large temperature differences (>10°C) between the electrode and the buffer solution [78].
Q: For reliable in-shoe pressure data, how many steps are needed during a walking trial?
- A: The number of steps required depends on the walking condition. For excellent reliability (ICC ≥ 0.90), minimum distances are approximately 207 meters for linear walking, 255 meters for clockwise curved walking, and 467 meters for counterclockwise curved walking [61].
Q: My pressure data seems noisy and inconsistent between sessions. What should I check?
- A: First, verify your calibration protocol. Ensure it is representative of the movements in your study, as calibration with low loading rates (less than those in walking) is a known source of unreliable data [1]. Second, confirm the test-retest reliability of your system and ensure you are collecting a sufficient number of steps as per established guidelines [61].
Q: What is the key difference between rigid pressure platforms and in-shoe systems, and when should I use each?
- A: Rigid pressure platforms are the most accurate for measuring plantar pressures during standing and barefoot walking, typically in lab settings. In-shoe systems are most suitable for field measurements during daily living or dynamic sports, as they are often wireless and can measure multiple steps. They are the preferred equipment for assessing the effects of footwear and orthotics on plantar pressures [1].
Q: Can artificial intelligence assist in analyzing plantar pressure data?
- A: Yes. There is clear potential for AI techniques to assist in the analysis and interpretation of plantar pressure data, which can enable more complete use of the data in clinical diagnosis and monitoring [1]. Machine learning and deep learning are also being used to classify gait patterns and recognize human activities from sensor data [79].
Troubleshooting Guide: Common Experimental Issues
| Problem | Possible Cause | Solution |
|---|---|---|
| Low Intraclass Correlation Coefficient (ICC) in test-retest data | Insufficient number of steps or walking distance for the specific condition [61]. | Follow established minimum distance guidelines: 207m (linear), 255m (clockwise curved), 467m (counterclockwise curved) [61]. |
| Inconsistent measurements between lab and free-living environments | System calibration not representative of dynamic, real-world movements [1]. | Develop and use bespoke calibration procedures with loading rates that match the sporting or daily living movements being studied [1]. |
| Data artifacts or signal dropouts in wireless in-shoe systems | Sensor migration or shear stress at the foot-insole interface [61]. | Use a system where sensors are embedded between the sole and insole to minimize movement, and ensure a proper fit of the shoe [61]. |
| Unexpected user behavior during data collection | Unintended modification of behavior due to the awareness of being monitored [80]. | Implement acclimatization periods in the protocol and consider the potential for "device addiction" or anxiety in your study design and participant instructions [80]. |
Experimental Protocols and Methodologies
This section outlines detailed methodologies for key experiments cited in the troubleshooting guides, providing a reproducible framework for evaluating system performance.
Protocol 1: Test-Retest Reliability for Linear and Curved Walking
Objective: To validate the reliability of a wearable in-shoe plantar pressure system across different walking trajectories [61].
- Participants: Recruit a cohort of healthy participants (e.g., 31 individuals) capable of independent walking and with no known musculoskeletal disorders [61].
- Equipment: A wearable footwear system with embedded pressure sensors (e.g., 8 sensors per insole), wireless data transmission capability, and a dedicated mobile application for data collection [61].
- Procedure:
- Session 1: Participants perform three walking conditions in a randomized order: Linear Walking (LIN), Clockwise Curved Walking (CW), and Counterclockwise Curved Walking (CCW).
- Session 2: Repeat the exact same protocol 4-7 days after the first session to assess test-retest reliability.
- For each condition, conduct multiple trials (e.g., 2 trials per condition per session) [61].
- Data Analysis: Calculate key parameters such as Peak Pressure (PP), Pressure-Time Integral (PTI), and Average Pressure (AP) across eight foot regions. Assess reliability using Intraclass Correlation Coefficients (ICCs), Bland-Altman plots, and Minimal Detectable Changes (MDCs) [61].
The workflow for this validation protocol is as follows:
Protocol 2: High-Resolution Plantar Pressure Data Collection for Gait Analysis
Objective: To collect a comprehensive dataset of plantar pressures across varying footwear and walking speeds for gait analysis and recognition [8].
- Participants: A large and diverse cohort (e.g., 150 individuals) spanning various ages, sexes, and body sizes to ensure demographic representation [8].
- Equipment: A high-resolution pressure-sensing walkway (e.g., 1.2m x 3.6m, with 4 sensors/cm²) [8].
- Procedure:
- Each participant completes 16 walking conditions, combining 4 walking speeds (preferred, slow-to-stop, fast, slow) with 4 footwear types (barefoot, standard shoes, two types of personal shoes).
- Data is collected over a total of 24 minutes per participant (90 seconds per condition) to capture a large number of footsteps (e.g., ~1,400 steps/individual) [8].
- Data Management: Data should undergo thorough quality control and preprocessing, including footstep segmentation, foot alignment, and temporal normalization. Both raw and preprocessed data should be made available in standard formats (e.g., NPZ for Python, MAT for MATLAB) [8].
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and technologies used in modern plantar pressure research, as featured in the cited experiments.
| Item / Technology | Function & Application in Research |
|---|---|
| Rigid Pressure Platform [1] | High-accuracy system for measuring plantar pressures during barefoot standing and walking in laboratory settings. Ideal for fundamental assessments of foot function. |
| Wearable In-Shoe System [1] [61] | Mobile system for measuring plantar pressures in field environments (daily living, sports). Essential for studying the effects of footwear, orthotics, and real-world gait. |
| High-Density Piezoresistive Sensor Array [9] | A flexible insole integrated with a dense array of sensors (e.g., 173 sensors) for high spatial resolution mapping of pressure distribution. Enables detailed gait analysis and accurate center of pressure tracking. |
| Screen-Printed Nanomaterial Inks [9] | Conductive inks (e.g., Carbon-epoxy-elastomer) used to fabricate sensitive, robust, and cost-effective piezoresistive sensors on flexible substrates for smart insoles. |
| Inertial Measurement Units (IMUs) [81] [79] | Wearable sensors (accelerometers, gyroscopes) used for motion capture and gait analysis. Often combined with pressure data for comprehensive movement analysis. |
| AI/Machine Learning Algorithms [1] [79] | Techniques used to analyze and interpret complex plantar pressure data, classify gait patterns, and assist in clinical diagnosis and monitoring. |
System Selection and Calibration Workflows
Choosing the correct measurement system and applying a proper calibration is foundational to data integrity. The following diagram illustrates the decision pathway for selecting and calibrating a plantar pressure measurement system based on the research application.
Conclusion
The accurate calibration of foot plantar pressure sensors is a cornerstone of valid biomechanical research and effective clinical diagnostics. This review synthesizes key takeaways: that calibration must be anatomically specific and representative of real-world loading conditions, that rigorous validation using statistical methods like ICC and Bland-Altman plots is essential, and that different technologies (platform vs. in-shoe) serve complementary roles. The future of sensor calibration points towards greater standardization, the integration of AI for data interpretation and error correction, and the development of protocols capable of capturing the high loading rates of sporting movements. These advancements will directly enhance applications in drug development by providing more reliable endpoints for clinical trials, particularly in areas like diabetic foot ulcer prevention, rehabilitation monitoring, and the assessment of neuromuscular therapeutics, ultimately leading to improved patient outcomes.
References
- 1. Testing protocols and measurement techniques when ... [https://www.sciencedirect.com/science/article/pii/S0958259224000270]
- 2. Testing protocols and measurement techniques when ... [https://pubmed.ncbi.nlm.nih.gov/38579518/]
- 3. Comparative Analysis of Pressure Platform and Insole ... [https://www.mdpi.com/2076-3417/15/13/7575]
- 4. Foot Plantar Pressure Measurement System: A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC3444133/]
- 5. Technical Support - PPS [https://pressureprofile.com/technical-support]
- 6. Reliability of plantar pressure platforms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3732469/]
- 7. Test-retest reliability and usability evaluation of a wearable ... [https://www.nature.com/articles/s41598-025-21016-3]
- 8. A dataset of high-resolution plantar pressures for gait ... [https://www.nature.com/articles/s41597-025-05792-1]
- 9. Flexible Smart Insole and Plantar Pressure Monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371697/]
- 10. In-shoe plantar shear stress sensor design, calibration and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11373826/]
- 11. Validation of Plantar Pressure Measurements for a Novel In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3876360/]
- 12. Capacitive vs Piezoresistive vs Piezoelectric Pressure ... [https://my.avnet.com/abacus/solutions/technologies/sensors/pressure-sensors/core-technologies/capacitive-vs-piezoresistive-vs-piezoelectric/]
- 13. Introduction to Piezoelectric Force Sensors [https://www.pcb.com/resources/technical-information/introduction-to-force-sensors]
- 14. Pressure Sensor Not Working Troubleshooting Guide [https://wfsensors.com/blog/pressure-sensor-not-working-troubleshooting-guide.html/]
- 15. An In-Depth Buyer's Guide to Pressure Mapping in Sport [https://simplifaster.com/articles/depth-buyers-guide-pressure-mapping-sport/]
- 16. A Simple Foot Plantar Pressure Measurement Platform ... [https://www.mdpi.com/2571-5577/3/3/33]
- 17. Common Calibration Errors in Pressure Sensors [https://sensorsandgauges.com/pages/common-calibration-errors-in-pressure-sensors-avoid-costly-downtime-with-sensors-and-gauges?srsltid=AfmBOoogCevh0ob5Oy1K4KUSqJX6TL6ZDb34UwpBo6rschqBvIQa_X2A]
- 18. What Causes Zero and Span Offset in Pressure ... [https://blog.ashcroft.com/what-causes-zero-and-span-offset-in-pressure-transducers]
- 19. OpenGo Sensor Insoles - Wireless pressure, force & ... [https://moticon.com/opengo/sensor-insoles]
- 20. Testing and Troubleshooting Pressure Transducers | Omega [https://www.dwyeromega.com/en-us/resources/pressure-transducers-troubleshooting?srsltid=AfmBOopEoHz-Uu7L77o9MOlD209FWYtfKKTIwL9aHoaij6YekLWs26jx]
- 21. FAQs [https://www.tekscan.com/support/faqs]
- 22. Motion Capture Technologies for Athletic Performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299843/]
- 23. Advancing calibration techniques for accurate micro and ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1600426/full]
- 24. Is Your Motion Capture Data Actually Reliable? [https://www.theiamarkerless.com/blog/motion-capture-strn-quality-framework]
- 25. Gait & Motion Research [https://www.xsensor.com/solutions-and-platform/human-performance/gait-motion-insoles]
- 26. pedar® [https://www.novelusa.com/pedar.php]
- 27. Footwear pressure distribution measurement- pedar [https://novel.de/products/pedar/]
- 28. Testing and Troubleshooting Pressure Transducers | Omega [https://www.dwyeromega.com/en-us/resources/pressure-transducers-troubleshooting?srsltid=AfmBOopm1J3IdmmND2D2QlbdF6kZwiaW4RCEzJf2D-3Oqf8l7OfyrXkF]
- 29. Pressure Transducer Troubleshooting Extreme Environments [https://sucoesi.com/pressure-transducer-troubleshooting-extreme-environments/]
- 30. Frontiers | Dynamic balance control in healthy young women during... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1517471/full]
- 31. In-shoe plantar shear stress sensor design, calibration and ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0309514]
- 32. Discrepancies between plantar pressure devices [https://www.sciencedirect.com/science/article/pii/S0958259225000355]
- 33. Assessing the validity of pressure-measuring insoles in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6453056/]
- 34. Pressure Sensor Calibration [https://sucoesi.com/pressure-sensor-calibration/]
- 35. Digital manufacturing of personalised footwear with ... [https://www.nature.com/articles/s41598-023-29261-0]
- 36. "Smart Insole with Nanomaterials and Sensors for Plantar ... [https://www.linkedin.com/posts/w-hong-yeo-8498b3169_georgiatech-smartinsole-wearabletech-activity-7357612495584325632-bjRe]
- 37. Advances in micro/nano-engineered flexible sensor arrays ... [https://www.oaepublish.com/articles/ss.2025.11]
- 38. Calibrating Low-Cost Smart Insole Sensors with Recurrent ... [https://www.mdpi.com/1424-8220/24/15/4765?]
- 39. Flexible smart insole and plantar pressure monitoring ... [https://spie.org/spie-smart-structures-and-materials-nondestructive-evaluation/presentation/Real-Time-Monitoring-of-Peripheral-Arterial-Stents-Using-a-Chip/13948-48]
- 40. Diabetic foot prevention, assessment, and management ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12273060/]
- 41. Foot Plantar Pressure Measurement System Using Highly ... [https://www.mdpi.com/1424-8220/19/24/5504]
- 42. Calibration problems encountered while monitoring stump ... [http://www.oandplibrary.org/poi/1997_03_179.asp]
- 43. Potentialities and Criticalities of Plantar Pressure ... [https://www.intechopen.com/chapters/19660]
- 44. What causes pressure sensor drift? [https://wfsensors.com/blog/what-causes-pressure-sensor-drift.html/]
- 45. Sensor Drift: Causes, Mechanisms, and Effective ... [https://zeroinstrument.com/sensor-drift-causes-mechanisms-and-effective-compensation-methods/]
- 46. Hysteresis in pressure calibration: What you need to know [https://blog.beamex.com/hysteresis-in-pressure-calibration]
- 47. Preventing Pressure Transducers Drifting [https://txsensors.com/2020/07/08/preventing-pressure-transducers-from-drifting/?srsltid=AfmBOopJx9Zg4ssY2Csa5mCzAIRUXNMw44RFepR7x45U34KAgfjTM4fv]
- 48. Optimizing the Sensor Placement for Foot Plantar Center of ... [https://www.mdpi.com/1424-8220/20/19/5588]
- 49. How to solve 5 common pressure measurement problems [https://www.bdsensors.us/company/news/detail/5-common-pressure-measurement-problems-and-how-to-solve-them]
- 50. Validity and reliability of the XSENSOR in-shoe pressure ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0277971]
- 51. I cannot connect to sensor insoles [https://moticon.com/opengo-i-cannot-connect-to-sensor-insoles]
- 52. OpenGo frequently asked technical questions [https://moticon.com/opengo/faqs]
- 53. Real-time pressure mapping smart insole system based on ... [https://www.nature.com/articles/s41378-020-0171-1]
- 54. A review of recent progress in flexible capacitance ... [https://link.springer.com/article/10.1007/s42114-025-01304-2]
- 55. Developing excellent plantar pressure sensors for ... [https://www.sciencedirect.com/science/article/abs/pii/S0021979724008658]
- 56. High sensitive pressure sensors with a wide detection ... [https://www.sciencedirect.com/science/article/abs/pii/S138589472511752X]
- 57. What Is Model Drift? | IBM [https://www.ibm.com/think/topics/model-drift]
- 58. Review Commercially available pressure sensors for sport ... [https://www.sciencedirect.com/science/article/pii/S0958259223000871]
- 59. Automatic correction of performance drift under acquisition ... [https://www.nature.com/articles/s41467-023-42396-y]
- 60. Effectiveness of Using a Digital Wearable Plantar Pressure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11731697/]
- 61. Test-retest reliability and usability evaluation of a wearable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552487/]
- 62. Test-retest reliability of an insole plantar pressure system to ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/1743-0003-11-95]
- 63. Concurrent Validity and Test–Retest Reliability of Pressure ... [https://www.mdpi.com/1424-8220/23/10/4913]
- 64. Pressure Sensor Not Working Troubleshooting Guide - [https://wfsensors.com/fi/blog/pressure-sensor-not-working-troubleshooting-guide.html/]
- 65. Common Issues and Troubleshooting of Pressure Sensors [https://zeroinstrument.com/common-issues-and-troubleshooting-of-pressure-sensors/]
- 66. Bland-Altman plot - MedCalc Statistical Software Manual [https://www.medcalc.org/en/manual/bland-altman-plot.php]
- 67. Understanding Bland Altman analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4470095/]
- 68. Minimal detectable change of gait and balance measures in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10986034/]
- 69. The test–retest reliability and minimal detectable change of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4806559/]
- 70. The test–retest reliability and the minimal detectable ... [https://www.sciencedirect.com/science/article/pii/S0929664612001891]
- 71. Modeling and Calibration of Pressure-Sensing Insoles via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10181679/]
- 72. The Development of a Built-In Shoe Plantar Pressure ... [https://www.mdpi.com/1424-8220/22/21/8327]
- 73. Validity and reliability of the XSENSOR in-shoe pressure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9844836/]
- 74. Plantar Pressure Measurements Using An In-Shoe System ... [https://www.academia.edu/445153/Plantar_Pressure_Measurements_Using_An_In_Shoe_System_and_a_Pressure_Platform_A_Comparison]
- 75. Toward automated plantar pressure analysis [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1579072/full]
- 76. Foot Plantar Pressure Measurement System in the Real ... [https://www.linkedin.com/pulse/foot-plantar-pressure-measurement-system-real-fwudf/]
- 77. Validating Capacitive Pressure Sensors for Mobile Gait ... [https://www.mdpi.com/2673-7078/5/3/54]
- 78. What are the most frequent causes of calibration problems? [https://www.hamiltoncompany.com/knowledge-base/faq/what-are-the-most-frequent-causes-of-calibration-problems?srsltid=AfmBOoo6JSo7yYdAEdqBceWHiqXVrXyMH4iWWOvzNzsQXEZkxxGx04g4]
- 79. Evolution and Challenges of Smart Shoes from Gait Analysis ... [https://ai-scholar.tech/en/articles/healthcare/Smart-Footwear-Healthcare]
- 80. Unintended Consequences of Wearable Sensor Use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5171570/]
- 81. IMU Calibration Guide [https://www.noraxon.com/article/imu-calibration-guide]